Dental Caries
Dental caries is a multifactorial disease with interaction between three factors, the tooth, the microflora, and the diet. If not disturbed, bacteria accumulate at specific tooth sites to form what is known as bacterial plaque (biofilm). The development of caries requires both the presence of bacteria and a diet containing fermentable carbohydrates. Caries is an infectious disease because it is the lactic acid produced by bacteria from the fermentation of carbohydrates that causes the dissolution, or demineralization, of the dental hard tissues. The Streptococcus mutans group plays a central role in the demineralization. In the initial stages of the disease bacteria are located on the tooth surface. It is only after severe demineralization or cavity formation has occurred that bacteria penetrate into the hard tissues. The demineralized tooth surface, called the carious lesion, is thus not the disease but a reflection of continuing or past microbial activity in the plaque.
The initial carious lesion is a subsurface loss of mineral in the outer tooth surface. It appears clinically as a chalky white (indicating present activity) or an opaque or dark, brownish spot (indicating past activity). A lesion beneath active bacterial plaque will progress, slowly or fast, but if the biofilm is removed or disturbed, the lesion will arrest. An arrested lesion may become reactive, however, and progress any time there is activity in the biofilm. Alternatively, remineralization in the outer parts of an arrested lesion can occur, for example, after the use of fluorides. Caries is therefore an ever-dynamic process.
The rate and extent of mineral loss depends on many factors. Mineral loss occurs faster in an active lesion when intercrystalline voids form. Demineralization may extend well into dentin before a breakdown of the outer surface (cavitation) occurs, resulting in a clinically visible cavity. With lesion progression and no intervention, demineralization may progress through the enamel, the dentin, and eventually into the pulp and may destroy the tooth (Fig. 17-1).
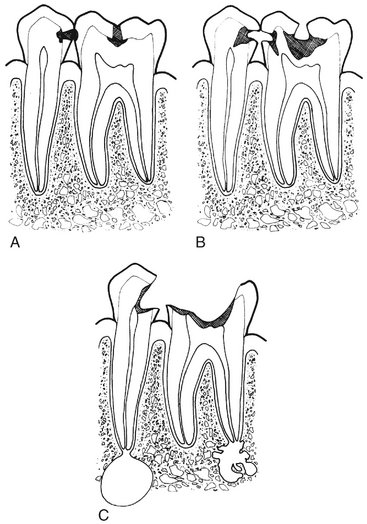
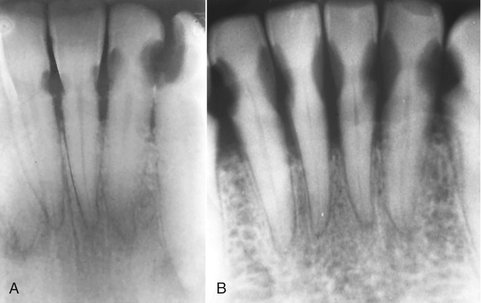
FIG. 17-1 A, Proximal and occlusal demineralization penetrating through tooth enamel and into the dentin. B, Proximal and occlusal tissue demineralization and cavitation nearing the pulp chamber of two vital teeth. C, Severe demineralization and cavitation reaching the pulp chamber resulting in two nonvital pulps and periapical inflammatory disease.
Radiologic Examination to Detect Caries
Radiography is useful for detecting carious lesions because the caries process causes demineralization of enamel and dentin. The lesion is seen in the radiograph as a radiolucent (darker) zone because the demineralized area of the tooth does not absorb as many x-ray photons as the unaffected portion. It is important to keep in mind, though, that the lesion detected in the radiograph is merely a result of the bacterial activity on the tooth surface and radiography cannot reveal whether the lesion is active or arrested. An old inactive lesion will still appear as a demineralized “scar” in the hard tissues (Fig. 17-2). The reason is that remineralization takes place only in its outermost surface because mineral-containing solutions from saliva cannot diffuse into the body of the lesion. Because the radiograph only mirrors the current extent of demineralization, one radiograph alone cannot distinguish between an active and an arrested lesion. Only a second radiograph taken at a later time can reveal whether the disease is active. When a decision is made to monitor a lesion, factors such as oral hygiene, fluoride exposure, saliva flow, diet, caries history, extent of restorative care, and age should be considered in determining the time interval between the radiologic examinations (Chapter 15).
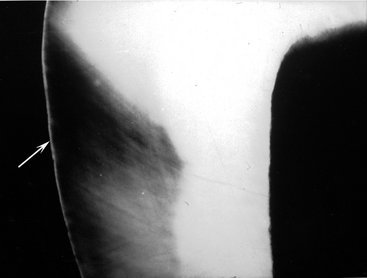
FIG. 17-2 Microradiograph of an inactive carious lesion (dark region) halfway through enamel with an intact, well mineralized surface (arrow). The inner dark area represents dentin.
Radiography is a valuable supplement to a thorough clinical examination of the teeth for detecting caries. A careful clinical examination assessing the carious activity on the tooth surface may be possible for smooth surfaces and to some extent for occlusal surfaces. However, when the surface is clinically intact (i.e., no breakdown leading to cavitation has occurred), even the most meticulous examination may fail to reveal demineralizations beneath the surface, including occlusal surfaces. Clinical access to proximal tooth surfaces in contact is limited. Indeed, numerous clinical studies have shown that a radiologic examination can reveal carious lesions that would otherwise remain undetected both in occlusal and proximal surfaces.
EXAMINATION WITH CONVENTIONAL INTRAORAL FILM
The bitewing projection is the most useful radiologic examination for detecting caries (Chapter 9). The use of a film holder with a beam-aiming device reduces the number of overlapping contact points and improves image quality, thus minimizing interpretation errors. Periapical radiographs are useful primarily for detecting changes in the periapical bone. Use of a paralleling technique for obtaining periapical radiographs increases the value of this projection in detecting caries of both anterior and posterior teeth, especially with heavily restored teeth.
Traditionally, size-2 “adult” films are used for a bitewing examination from the age of approximately 7 to 8 years onward. When it is necessary to examine all the contact surfaces from the cuspid to the most distal molar, one or two bitewing films per side are required, depending on the number of teeth that are present (Fig. 17-3). The use of a single size-3 film often results in overlapping contact points and “cone-cut” images and is not recommended. In small children the size-0 or “child” film may be used instead of a size-2 film (Fig. 17-4).
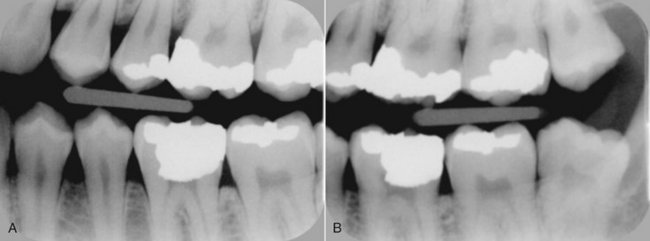
FIG. 17-3 Two bitewing images from the patient’s left side covering the surfaces from the distal surface of the canine to the distal surface of the most posterior molar.
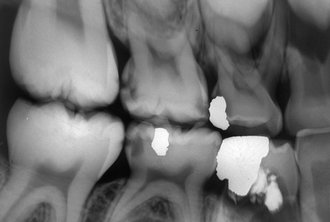
FIG. 17-4 This bitewing image of the mixed dentition demonstrates dentinal carious lesions involving the mesial and distal surfaces of the second deciduous molars and small enamel lesions in the mesial surfaces of the first permanent molars. An extensive lesion involves the crown and root structure of the mandibular first deciduous molar.
In recent decades there has been a dramatic decline in the prevalence of caries in all Western countries, leaving a smaller fraction of the population with rapidly progressing carious lesions. Accordingly, the interval between examinations should be customized for each patient on the basis of the perceived caries activity and susceptibility. For caries-free individuals the interval may be lengthened, whereas for caries-active individuals the interval should be shorter.
Radiographs used to detect carious lesions should be mounted in frames with dark borders and interpreted with use of a light box with sufficient luminance and a magnifying viewer. Figure 17-5 is a series of radiographs showing early lesions with and without magnification.
EXAMINATION WITH DIGITAL IMAGING
Digital image receptors may replace film for intraoral radiography. There are two different methods available: (1) solid-state sensors (charge-coupled device [CCD] and complementary metal oxide semiconductor technology [CMOS]) with a cord that connects the receptor to the computer or without a cord (signal is transferred by radio wave) and (2) storage phosphors (PSP plates) that use a filmlike plate that is processed (scanned) after exposure (Chapter 7). The holders available for bitewing examinations with phosphor plates appear like those for film, and universal sensor holders are also available. However, there may be some problems when solid-state sensors are used for bitewing examination. First, the surface area of the sensor is smaller than the surface area of a size-2 film, resulting in the display of fewer interproximal tooth surfaces per bitewing image than with film. Further, the stiffness and increased thickness of these sensors may result in more projection errors and retakes. When digital bitewing images are used, they should be displayed on a monitor in their full resolution for interpretation and viewed in a room with subdued light.
Radiographic Detection of Lesions
Typical Radiographic Appearance
The shape of the early radiolucent lesion in the enamel is classically a triangle with its broad base at the tooth surface (Fig. 17-5) spreading along the enamel rods, but other appearances are common, such as a “notch,” a dot, a band, or a thin line (Fig. 17-6). When the demineralizing front reaches the dentinoenamel junction (DEJ), it spreads along the junction, frequently forming the base of a second triangle with apex directed toward the pulp chamber (Fig. 17-7). This triangle typically has a wider base than in the enamel and progresses toward the pulp along the direction of the dentinal tubules. Again, more irregular shapes of decalcification may be seen.
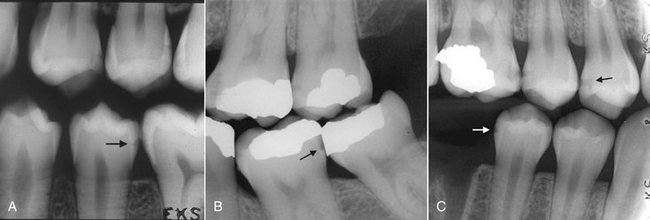
FIG. 17-6 A, This bitewing image demonstrates bandlike lesions involving the enamel of the maxillary premolars and a triangular lesion (arrow) in the mandibular second premolar. B, This bitewing image shows an enamel lesion (arrow) and a lesion extending into the dentin involving the mesial surface of the maxillary second molar. C, This bitewing image reveals lesions involving the enamel of the mandibular second premolar (white arrow) and the distal surface of the maxillary second premolar and lesions extending into the dentin of the mesial surface of the maxillary first molar and the distal surface of the first premolar (black arrow).
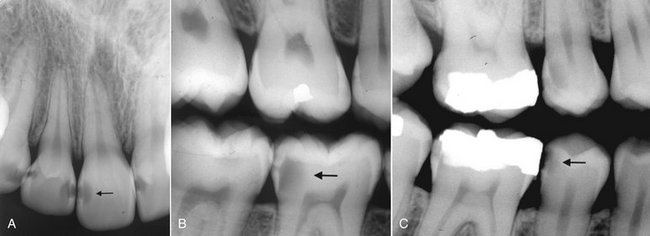
FIG. 17-7 A, This periapical image demonstrates several proximal carious lesions that have extended into the dentin. Note that the lesions extend along the dentinoenamel junction to involve a greater amount of dentin than enamel (arrow). B, This bitewing image demonstrates an extensive proximal carious lesion involving the distal aspect of the mandibular first molar (arrow). Note that the pulp horn has been reduced as a result of the formation of tertiary (irritation) dentin. C, This bitewing image shows two lesions involving the dentin in the distal surfaces of the second premolars, and one lesion has resulted in cavitation (arrow).
Lesions involving proximal surfaces most commonly are found in the area between the contact point and the free gingival margin (Fig. 17-8). The fact that this type of lesion does not start below the gingival margin helps distinguish a carious lesion from cervical burnout. Close attention should be paid to intact proximal surfaces adjacent to a tooth surface with a restoration because occasionally this surface is inadvertently damaged during the restorative procedure and is thus at greater risk for caries (Fig. 17-9).
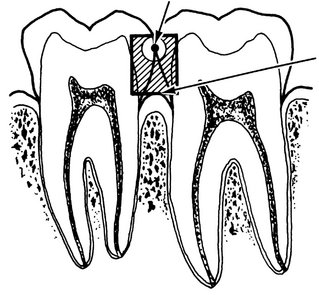
FIG. 17-8 Proximal caries-susceptible zone. This region extends from the contact point down to the height of the free gingival margin. It increases with recession of the alveolar bone and gingival tissues.
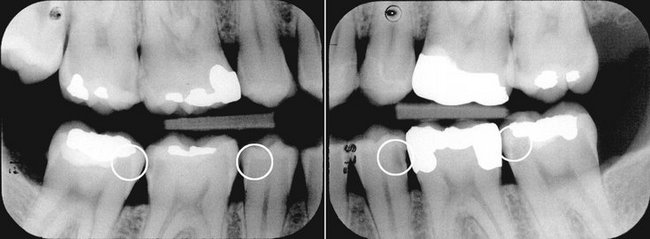
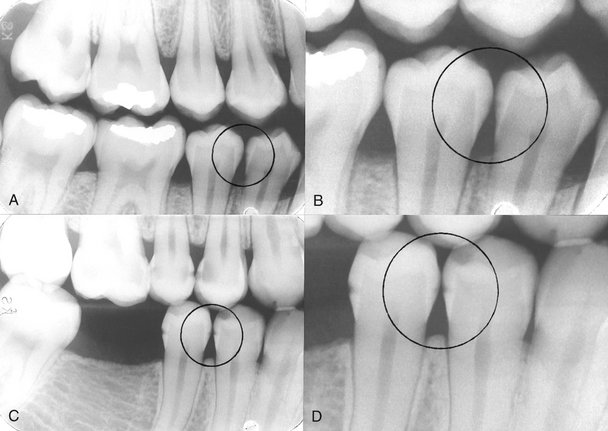
FIG. 17-9 A pair of bitewing images. Note (circles) that dentinal lesions have developed in surfaces adjacent to a restored surface in the patient’s left side, but not in the same surfaces of the teeth in the right side.
Because the proximal surfaces of posterior teeth are often broad, the loss of small amounts of mineral from incipient lesions and the advancing front of active lesions are often difficult to detect in the radiographic image. Lesions confined to enamel may not be evident radiographically until approximately 30% to 40% demineralization has occurred. For this reason, the actual depth of penetration of a carious lesion is often deeper than seen radiographically.
False Interpretations
Even experienced dentists often do not agree on the presence or absence of carious lesions when examining the same set of radiographs, especially when the lesions are limited to the enamel. On occasion a carious lesion may be incorrectly detected when the tooth surface is actually unaffected (a false-positive outcome). Various morphologic phenomena, such as pits and fissures, cervical burnout, and Mach band effect, and dental anomalies, such as hypoplastic pits and concavities produced by wear, can mimic the appearance of a carious lesion (Fig. 17-10). In cases where the demineralization is not yet radiographically visible, failure to detect the lesion is a false-negative outcome (Fig. 17-11). Also, overlapping contact points in the radiographic image may obscure a lesion (Fig. 17-12). Approximately half of all proximal lesions in enamel cannot be detected by radiography. The possibility of false-positive diagnoses of small lesions, combined with the knowledge that caries progresses slowly in most individuals, argues for a conservative approach to caries diagnosis and treatment. A lesion extending into the dentin in the radiograph may be easier to detect with greater agreement among experienced observers. Occasionally demineralization in the enamel is not obvious and a dentinal lesion is overlooked (see Fig. 17-6, A, distal surface of the maxillary second premolar and, B, mesial surface of the maxillary first molar).
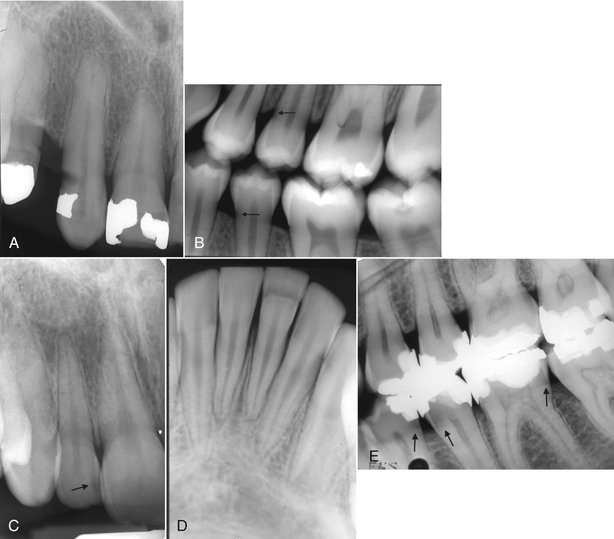
FIG. 17-10 A, This periapical image reveals a radiolucent region similar in appearance to a carious lesion in the distal cervical aspect of the maxillary cuspid, which is caused by abrasion from a clasp from a partial denture. B, In this bitewing image cervical burnout (arrows) can mimic carious lesions. C, In this periapical image a small concavity in the mesial surface of the lateral incisor creates a radiolucent region similar in appearance to a carious lesion (arrow). D, In this periapical image a band of enamel hypoplasia involving the left central incisor produces a linear radiolucent region that may be misinterpreted as carious lesion. E, In this bitewing image the overlapping shadow of the alveolar process creates a Mach band effect (arrows) resulting in apparent radiolucent regions in the crowns of the premolars and first molar that may mimic carious lesions.
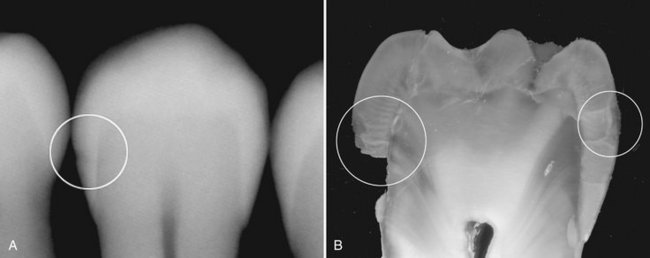
FIG. 17-11 A, A radiograph of an extracted tooth with a lesion just into dentin in the left side (circle) but no visible lesion in the right side. B, The same tooth after sectioning assessed under a microscope reveals lesions in both sides; the lesion in the right side is only in enamel. Note that enamel in the left side has broken off during sectioning.

FIG. 17-12 A, In this periapical image a proximal carious lesion involving the distal surface of the cuspid is not apparent. however, in the periapical image (B), the change in the horizontal orientation of the x-ray beam has separated the overlapping images of the opposing surfaces of the premolar and cuspid, revealing the presence of the lesion (arrow).
Lesions with and Without Clinical Cavitation
Potentially a progressing proximal lesion may be arrested if cavitation has not developed. If cavitation has occurred, the lesion will always be active because the bacteria that colonize within the cavity cannot be removed. Unfortunately, the presence of cavitation cannot be accurately determined radiographically, although the greater the radiographic depth of the lesion the greater the likelihood of cavitation. Because extensive demineralization must occur before the surface breaks down, the percentage of enamel lesions with surface cavitation is very small. Approximately half of lesions that are just into dentin have surface cavitation. The deeper the lesion has penetrated into dentin, the more likely it is cavitated, and dentinal lesions extending more than halfway to the pulp are always cavitated. Temporarily separating proximal surfaces with orthodontic elastics or springs may allow direct inspection to determine whether there is cavitation. This method is easier in children than adults.
Treatment Considerations
These considerations mean that operative treatment is usually not indicated for lesions detected in enamel and the dentist and the patient may arrest lesion progression with conservative intervention. Cavitated lesions, on the other hand, will need operative treatment. For dentinal lesions, the decision whether to provide operative treatment is individualized for each patient. In cases where it is decided to monitor the lesion, a follow-up radiograph should be taken to evaluate whether the lesion has arrested or is progressing. The interval between the radiologic examinations should be determined individually, taking into account previous caries history, age and, not least, the site of the lesion because the progression rate differs highly among the various tooth surfaces. Care should be taken to reproduce the same image geometry in the follow-up radiographs by using standardized film holders to provide a means of accurate comparison of depth of the lesion. When digital images are made with reproducible geometry, they can be superimposed and the information in the one image can be subtracted from the other, resulting in a subtraction image, which displays the changes that have occurred between the two examinations (Fig. 17-13).
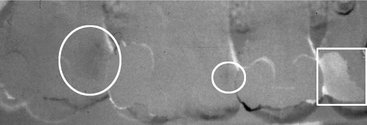
FIG. 17-13 A subtraction image made from two bitewing images taken with a 2-year interval. The contours of four maxillary teeth can be seen. Between the two examinations a filling was placed (rectangle), a new deep dentinal lesion has developed (large circle), and a lesion has progressed from enamel into dentin (small circle).
Progression of a lesion indicates the need for operative therapy. With highly motivated patients who clean the surface and with topical fluoride treatment, more than half of shallow dentinal lesions can be arrested, thus avoiding restorative therapy.
OCCLUSAL SURFACES
Typical Radiographic Appearance
Carious lesions in children and adolescents most often occur on occlusal surfaces of posterior teeth. The demineralization process originates in enamel pits and fissures where bacterial plaque can gather. The lesion spreads along the enamel rods and, if undisturbed, penetrates to the DEJ, where it may be seen as a thin radiolucent line between enamel and dentin.
Occlusal lesions commonly start in the sides of a fissure wall rather than at the base and then tend to penetrate nearly perpendicularly toward the DEJ. Early lesions appear clinically as chalky white, yellow, brown, or black discolorations of the occlusal fissures. Finding such discolored fissures in a clinically intact occlusal surface suggests that a radiologic examination is indicated to determine whether a carious lesion has penetrated beyond the DEJ. If the lesion has not crossed the DEJ, it may not be visible in the radiograph.
The classic radiographic appearance of lesions extending into the dentin is a broad-based, radiolucent zone, often beneath a fissure, with little or no apparent changes in the enamel. The deeper the occlusal lesion, the easier it is to detect on the radiograph (Fig. 17-14).
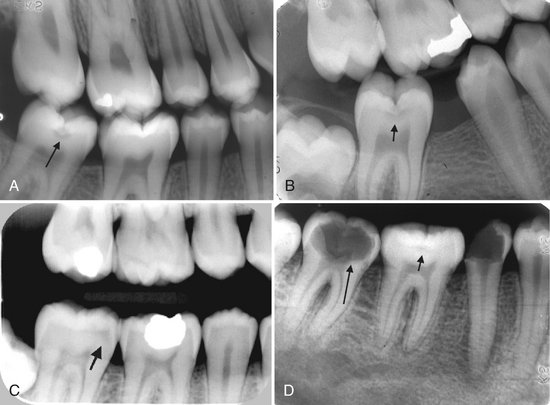
FIG. 17-14 A and B, These bitewing images demonstrate a classic appearance of an occlusal carious lesion with a triangular shape in the enamel with the base oriented to the dentinoenamel junction (arrows). The bitewing image (C) is not as clear, but there is an ill-defined radiolucent region under the occlusal enamel surface (arrow). In the periapical image (D) there is a subtle occlusal lesion in the first molar (short arrow) and an extensive cavitated lesion in the second molar (long arrow).
False Interpretations
Pitfalls in the interpretation of dentinal occlusal lesions include superimposition of the image of the buccal pit with or without an associated carious lesion or a composite restoration, which may simulate an occlusal lesion or a deep occlusal fissure. Direct clinical inspection of the tooth most often eliminates any such confusion.
When an occlusal lesion is confined to enamel, the surrounding enamel often obscures the lesion. As the carious process progresses, a radiolucent line extends along the DEJ. As the lesion extends into the dentin, the margin between the carious and noncarious dentin is diffuse and may obscure the fine radiolucent line at the DEJ. Therefore false-positive detection rates may be as high as false-negative ones for shallow lesions. A false-negative outcome may not represent a severe mistake because in most cases the process progresses slowly and the lesion is detected at a later time. A false-positive outcome may result in a sound surface being irreversibly damaged. Also, when there is a sharply defined density difference, such as between enamel and dentin, there may appear to be a more radiolucent region immediately adjacent to the enamel. This is an optical illusion referred to as the Mach band (see Fig. 17-10, E). This can contribute to the number of false-positive interpretations; therefore when there are no clinical signs of a lesion, it would be reasonable to observe these cases and withhold operative treatment.
Cavitation and Treatment Considerations
As an occlusal lesion spreads through the dentin, it undermines the enamel, and eventually masticatory forces cause cavitation. When the cavitation is visible on clinical inspection, it is usually an indication that the lesion is already well into dentin and if information regarding extent relative to the pulp chamber is needed, then a radiologic examination is required. Without cavitation, fissure discoloration may indicate the need for radiologic examination. Dentinal lesions without clinically apparent cavitation but with a radiolucent change indicate that the carious lesions have passed the DEJ (see Fig. 17-14) and require operative treatment.
RAMPANT CARIES
Severe, rapidly progressing carious destruction of teeth is usually termed rampant caries and is usually seen in children with poor dietary and oral hygiene habits (see Fig. 17-4). This condition, however, is becoming increasingly rare because of widespread availability of fluoride in water supplements and topical application and enlightened practices of good nutrition and hygiene. Rampant caries may also be seen in people with xerostomia. Radiographs of individuals with rampant caries demonstrate severe (advanced) carious destructions, especially of the mandibular anterior teeth.
BUCCAL AND LINGUAL SURFACES
Buccal and lingual carious lesions often occur in enamel pits and fissures of teeth. When small, these lesions are usually round; as they enlarge, they become elliptic or semilunar. They demonstrate sharp, well-defined borders.
It may be difficult to differentiate between buccal and lingual carious lesions on a radiograph. When viewing buccal or lingual lesions, the clinician should look for a uniform noncarious region of enamel surrounding the apparent radiolucency (Fig. 17-15). This well-defined circular area represents parallel noncarious enamel rods surrounding the buccal or palatal lesion. Occlusal lesions, however, ordinarily are more extensive than lingual or buccal caries, and their outline is not as well defined. Clinical evaluation with visual and tactile methods is usually the definitive method of detecting buccal or lingual lesions.
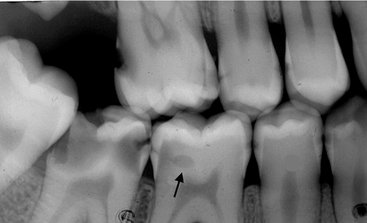
FIG. 17-15 This bitewing image reveals the presence of a small buccal lesion (arrow) involving the mandibular first molar. Note the presence of 12 proximal carious lesions. Also, the abnormal position of the mandibular third molar created an enhanced site for plaque accumulation resulting in an extensive carious lesion involving the second molar.
ROOT SURFACES
Root surface lesions involve both cementum and dentin and are associated with gingival recession. The exposed cementum is relatively soft and usually only 20 to 50 μm thick near the cementoenamel junction, so it rapidly degrades by attrition, abrasion, and erosion. Root surface caries should be detected clinically, and most often radiographs are not needed for diagnosis. In proximal root surfaces radiologic examination may reveal lesions that have gone undetected (Fig. 17-16).
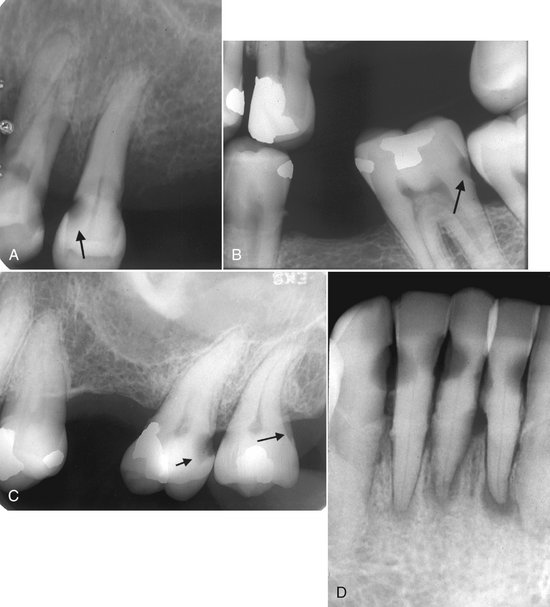
FIG. 17-16 A, This periapical image shows root surface carious lesions involving the distal aspect of the first premolar and the mesial and distal aspect of the second premolar. Note that the lesion undermines the enamel surface (arrow). B, This bitewing image reveals a root surface lesion involving the distal cervical region of the second molar (arrow); this location is in part due to the low third molar contact point on the distal surface, the result of abnormal mesial tipping of both molars. C, This periapical image shows a carious lesion in the distal root surface of the maxillary second molar (short arrow) and an example of cervical burnout (long arrow). Note the sharp line from overlapping roots that delineates the radiolucent cervical burnout. D, This periapical image demonstrates multiple root lesions involving the mandibular incisors. Note the associated periapical inflammatory lesions.
A pitfall in the detection of root lesions is that a surface may appear to be carious as a result of the cervical burnout phenomenon (see Figs. 17-10, B, and 17-16, C). The true carious lesion may be distinguished from the intact surface primarily by the absence of an image of the root edge and by the appearance of a diffuse rounded inner border where the tooth substance has been lost.
ASSOCIATED WITH DENTAL RESTORATIONS
A carious lesion developing at the margin of an existing restoration may be termed secondary or recurrent caries. It should be noted, though, that a lesion developing in a restored surface is most frequently a new primary demineralization, either because of faulty shaping or inadequate extension of the restoration leading to plaque accumulation (Fig. 17-17). These lesions (secondary caries) should be treated as any new carious lesion. It is important not to confuse secondary (primary) caries with residual caries, which is caries that remain if the original lesion is not completely removed. In situations where the radiographic lesion is very close to the pulp, carious dentin may be left on purpose during operative treatment. Medication that stimulates the development of tertiary dentin is placed in the cavity (indirect pulp capping). After some months the remaining carious dentin is removed and a permanent filling placed.
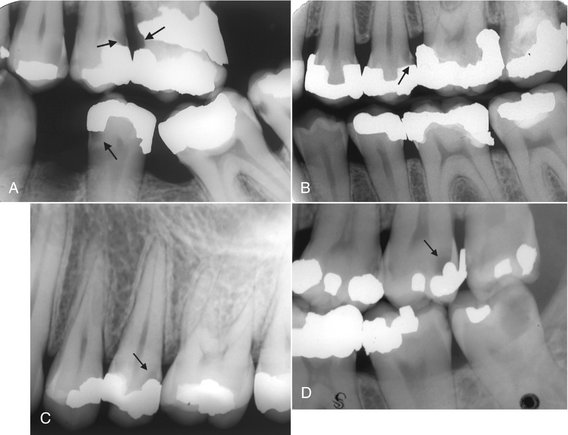
FIG. 17-17 A, This bitewing image reveals several interproximal carious lesions; three are recurrent caries (arrows). B, This bitewing image demonstrates a recurrent carious lesion in the distal surface of the maxillary second premolar (arrow). Note the overhang to the restoration placed on the mesial surface of the first molar. C, This periapical image reveals a recurrent carious lesion (arrow) involving the distal surface of the second premolar. D, Note that there is an overhang to the restoration on the distal aspect of this maxillary second molar and an associated recurrent carious lesion (arrow).
A lesion next to a restoration may be obscured by the radiopaque image of the restoration. Thus two radiographic views made at different horizontal or vertical angulations of the central ray can be an aid where there are multiple radiopaque restorations. Also, the detection of secondary carious lesions depends on a careful clinical examination. Recurrent lesions at the mesiogingival and distogingival margins are most frequently detected radiographically.
Restorative materials vary in their radiographic appearance depending on thickness, density, atomic number, and the x-ray beam energy used to make the radiograph. Some materials can be confused with caries. Older calcium hydroxide liners without barium, lead, or zinc (added to lend radiopacity) appear radiolucent and may resemble recurrent or residual caries. Despite the calcium present, the relatively large proportion of low atomic number material in calcium hydroxide causes its radiodensity to be similar to a carious lesion. Composite, plastic, or silicate restorations also may simulate lesions. It is often possible, however, to identify and differentiate these radiolucent materials from caries by their well-defined and smooth outline reflecting the preparation or from their radiopaque liners (Fig. 17-18).
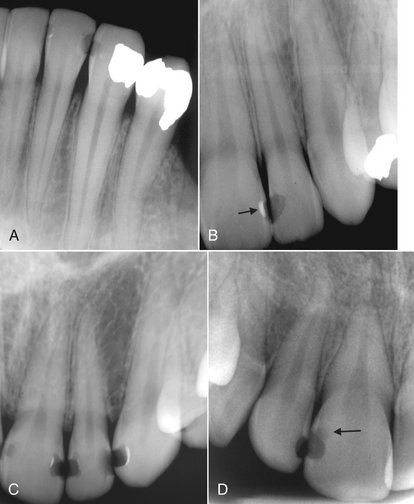
FIG. 17-18 A, This periapical image shows radiolucent restorations placed in the mesial and distal surfaces of the lateral incisor and mesial surface of the cuspid. Note the well-defined margins, useful to differentiate from carious lesions. B, In this periapical image the radiopaque liner on the internal aspect of the restoration placed on the distal surface of the central incisor is useful to differentiate from a carious lesion. Note the sharp margins of the restoration placed in the mesial surface of the lateral incisor. C, In this periapical image there are four radiolucent restorations and one carious lesion. The carious lesion involves the distal surface of the lateral incisor. Note the diffuse margin of the lesion in contrast to the well-defined margins of the restorations. D, This periapical image shows a recurrent carious lesion (arrow) involving the distal surface of the central incisor in contact with the radiolucent restoration. Note the diffuse ill-defined margin of the lesion compared with the well-defined margin of the restoration.
THERAPY AFTER RADIATION
Patients who have received therapeutic radiation to the head and neck may have a loss of salivary gland function, leading to xerostomia (dry mouth) and a change in the bacterial flora and possibly intrinsic change to the tooth structure. Untreated, this induces rampant destruction of the teeth, termed radiation caries (Chapter 2). Typically, the destruction begins at the cervical region and may aggressively encircle the tooth, causing the entire crown to be lost, with only root fragments remaining in the jaws. The radiographic appearance of radiation caries is characteristic: radiolucent shadows appearing at the necks of teeth, most obvious on the mesial and distal aspects. Variations in the depth of destruction may be present, but generally there is uniformity within a given region of the mouth. Figure 17-19 shows examples of radiation caries in patients with xerostomia after therapeutic radiation for cancer of the head and neck. Use of topical fluorides as remineralizing solutions and meticulous oral hygiene can markedly reduce the radiation damage to teeth resulting from xerostomia.
Alternative Diagnostic Tools to Detect Dental Caries
Other methods have been developed in addition to clinical inspection and radiography to detect carious lesions. These include light fluorescence (QLF), “Diagnodent” laser-light fiberoptic transillumination (FOTI), electrical conductance measurements (ECM), and ultrasonography. QLF may be used to quantify mineral loss on smooth surfaces, whereas Diagnodent and ECM have been applied on occlusal surfaces. These two methods operate by displaying a value that provides quantitative information on the depth of the lesion. None of the methods can unequivocally distinguish between enamel and dentin lesions or between shallow and deep dentin lesions. FOTI has been used primarily for proximal surfaces but may also be applied to occlusal surfaces. FOTI is less sensitive than radiography for distinguishing shallow and deep lesions. ECM is better than FOTI in identifying occlusal caries in young children. There is little evidence yet that these methods can substitute traditional diagnostic methods in the clinic.
Treatment Considerations
Carious lesions in enamel require interceptive treatment but rarely operative treatment. The radiographic detection of small areas of demineralization requires a decision as to whether these represent active or inactive arrested lesions. When the radiograph shows a lesion limited to enamel, the probability of cavitation is low and the prospect of arresting or reversing the caries process is good. Also, if the radiograph shows a lesion just into the dentin, treatment should include a means to stop the microbiologic activity and possibly reverse the demineralization process. Treatment of such lesions may include reductions in sugar intake, proper oral hygiene to reduce bacteria, and use of topical fluorides to inhibit microbiologic activity, retard demineralization, and promote remineralization of the outermost parts of the lesion. This may be successful if the surface of the tooth is not cavitated and a follow-up radiograph shows no progression of the lesion. However, when the surface of a lesion is cavitated or follow-up radiographs reveal progression of the lesion in dentin, a restoration is required. Cavitated carious lesions require removal of the infected tissues, possibly stepwise over a period for extensive lesions, and restoration of the tooth to form and function.
Fejerskov, O, Kidd, EAM. Dental caries: the disease and its clinical management, ed 1. Munksgaard: Blackwell; 2003.
Newbrun, E. Cariology, ed 3. Baltimore: Williams & Wilkins; 1989.
NIH Consensus Development Conference on Diagnosis and Management of Dental Caries Throughout Life. Bethesda, MD, March 26-28, 2001. Conference papers. J Dent Educ. 2001;65:935–1179.
Pitts, NB, Stamm, JW. International Consensus Workshop on Caries Clinical Trials (ICW-CCT)—final consensus statements: agreeing where the evidence leads. J Dent Res. 2004;83(Spec No. C):C125–C128.
Selwitz, RH, Ismail, AI, Pitts, NB. Dental caries. Lancet. 2007;369:51–59.
De Araujo, FB, Rosito, DB, Toigo, E, et al. Diagnosis of approximal caries: radiographic versus clinical examination using tooth separation. Am J Dent. 1992;5:245–248.
Hintze, H, Wenzel, A. A two-film versus a four-film bite-wing examination for caries diagnosis in adults. Caries Res. 1999;33:380–396.
Hintze, H, Wenzel, A, Danielsen, B. Behaviour of approximal carious lesions assessed by clinical examination after tooth separation and radiography: a 2.5-year longitudinal study in young adults. Caries Res. 1999;33:415–422.
Mejáre, I. Bitewing examination to detect caries in children and adolescents—when and how often? Dent Update. 2005;32:588–590. 593-594, 596-597
Mejáre, I, Stenlund, H, Zelezny-Holmlund, C. Caries incidence and lesions progression from adolescence to young adulthood: a prospective 15-year cohort study in Sweden. Caries Res. 2004;38:130–141.
Mjör, IA, Toffenetti, F. Secondary caries: a literature review with case reports. Quintessence Int. 2000;31:165–179.
Nielsen, LL, Hoernoe, M, Wenzel, A. Radiographic detection of cavitation in approximal surfaces of primary teeth using a digital storage phosphor system and conventional film, and the relationship between cavitation and radiographic lesion depth: an in vitro study. Int J Paediatr Dent. 1996;6:167–172.
Nyvad, B, Fejerskov, O. Assessing the stage of caries lesion activity on the basis of clinical and microbiological examination. Community Dent Oral Epidemiol. 1997;25:69–75.
Nyvad, B, Machiulskiene, V, Baelum, V. Reliability of a new caries diagnostic system differentiating between active and inactive caries lesions. Caries Res. 1999;33:252–260.
Petersson, GH, Bratthall, D. The caries decline: a review of reviews. Eur J Oral Sci. 1996;104:436–443.
Poorterman, JHG, Weerheijm, KL, Groen, HJ, et al. Clinical and radiographic judgement of occlusal caries in adolescents. Eur J Oral Sci. 2000;108:93–98.
Qvist, V, Johannesen, L, Bruun, M. Progression of approximal caries in relation to iatrogenic preparation damage. J Dent Res. 1992;71:1370–1373.
Ratledge, DK, Kidd, EA, Beighton, D. A clinical and microbiological study of approximal carious lesions, 1: the relationship between cavitation, radiographic lesion depth, the site specific gingival index and the level of infection of the dentine. Caries Res. 2001;35:3–7.
Wenzel, A. A review of dentists’ use of digital radiography and caries diagnosis with digital systems. Dentomaxillofac Radiol. 2006;35:307–314.
Wenzel, A, Anthonisen, PN, Juul, MB. Reproducibility in the assessment of caries lesion behaviour: a comparison between conventional film and subtraction radiography. Caries Res. 2000;34:214–218.
Wenzel, A, Haiter-Neto, F, Gotfredsen, E. Risk factors for a false positive test outcome in diagnosis of caries in approximal surfaces: impact of radiographic modality and observer characteristics. Caries Res. 2007;41:170–176.
White, SC, Yoon, DC. Comparative performance of digital and conventional images for detecting proximal surface caries. Dentomaxillofac Radiol. 1997;26:32–38.
Bader, JD, Shugars, DA. What do we know about how dentists make caries-related treatment decisions? Community Dent Oral Epidemiol. 1997;25:97–103.
Bader, JD, Shugars, DA. The evidence supporting alternative management strategies for early occlusal caries and suspected occlusal dentinal caries. J Evid Based Dent Pract. 2006;6:91–100.
Bjorndal, L, Kidd, EA. The treatment of deep dentine caries lesions. Dent Update. 2005;32:402–404. 407-410, 413
Pitts, NB. Diagnostic tools and measurements—impact on appropriate care. Community Dent Oral Epidemiol. 1997;25:24–35.
Pitts, NB. Are we ready to move from operative to non-operative/preventive treatment of dental caries in clinical practice? Caries Res. 2004;38:294–304.
Ricketts, DN, Kidd, EA, Innes, N, et al. Complete or ultraconservative removal of decayed tissue in unfilled teeth. Cochrane Database Syst Rev. 2006;3:CD003808.
Rimmer, PA, Pitts, NB. Temporary elective tooth separation as a diagnostic aid in general dental practice. Br Dent J. 1990;169:87–92.
Verdonschot, EH, Angmar-Månsson, B, ten Bosch, JJ, et al. Developments in caries diagnosis and their relationship to treatment decisions and quality of care. ORCA Saturday Afternoon Symposium 1997. Caries Res. 1999;33:32–40.
Woodward, GL, Leake, JL. The use of dental radiographs to estimate the probability of cavitation of carious interproximal lesions, I: evidence from the literature. J Can Dent Assoc. 1996;62:731–736.