Guidelines for Prescribing Dental Radiographs
The decision to conduct a radiographic examination should be based on the individual needs of the patient. These needs are determined by findings from the dental history and clinical examination and modified by patient age and general health. A radiographic examination is necessary when the history and clinical examination have not provided enough information for complete evaluation of a patient’s condition and formulation of an appropriate treatment plan. Radiographic exposures are necessary only when, in the dentist’s judgment, it is reasonably likely that the patient will benefit by the discovery of clinically useful information on the radiograph.
Role of Radiographs in Disease Detection and Monitoring
The goal of dental care is to preserve and improve patients’ oral health while minimizing other health-related risks. Although the diagnostic information provided by radiographs may be of definite benefit to the patient, the radiographic examination does carry the potential for harm from exposure to ionizing radiation. One of the most effective means of reducing possible harm is to avoid making radiographs that will not contribute information pertinent to patient care. The judgment that underlies the decision to make a radiographic examination centers on several factors, including the following:
• Prevalence of the diseases that may be detected radiographically in the oral cavity
• Ability of the clinician to detect these diseases clinically and radiographically
• Consequences of undetected and untreated disease
• Impact of asymptomatic anatomic and pathologic variations detected radiographically on patient treatment
As a general principle, radiographs are indicated when a reasonable probability exists that they will provide valuable information about a disease that is not evident clinically. Conversely, radiographs are not indicated when they are unlikely to yield information contributing to patient care. Radiographic information considered clinically useful includes data that are valuable in detecting disease and in monitoring the progression of known diseases.
For many clinical situations it is not readily apparent to the practitioner whether radiographs have a reasonable probability of providing valuable information. In these situations it is up to the practitioner’s clinical judgment after weighing the patient factors to decide whether radiographs are indicated.
The philosophy of taking radiographs only when there is a high probability of obtaining clinically useful information has been advocated by all the organizations responsible for developing or endorsing guidelines for ordering radiographs. However, many dentists use radiographs as a screening tool, simply to see “what’s there,” without having a specific suspicion of disease arising from the dental history or clinical examination. There are probably a number of reasons for doing this. Some dentists think that they have not provided an adequate service to their patients if they cannot assure them that they have searched diligently for disease with all reasonable diagnostic methods, including radiographs. They may state that having complete information, regardless of whether it affects the treatment plan, is of such benefit that it outweighs the risk of the radiation exposure. Other dentists raise medicolegal issues, stating fear of lawsuits if they fail to detect disease. Others express concern about the effect on the efficiency of the dental office of the extended examinations required for prescribing radiographs on the basis of signs and symptoms. The next few paragraphs will address these concerns.
Unlike their use in dentistry, screening radiographs are rarely used in medicine, with the exception of mammography for women above a certain age or with increased risk factors for breast cancer, and there is controversy over whether even this type of examination should be used as frequently as it is today. Breast cancer is a relatively common yet serious disease that should be detected early, before the cancer becomes large enough to be found clinically. On the other hand, diseases of the jaws (with the exceptions of caries, periapical and periodontal disease) are rare and concentrated in certain ages, sexes, and ethnicities. These diseases are unlikely to be discovered on routine screening radiographs before they have produced signs or symptoms that could be found on a thorough clinical examination and history. Periodontal disease can be diagnosed clinically, although radiographs are used to determine the extent of bone loss and the presence of other factors that may affect prognosis. Periapical disease is usually associated with extensive restorations or caries that can be detected clinically. Dental caries on proximal surfaces, however, may not be detectable on clinical examination until it has reached an advanced stage; thus this is one occult disease for which screening radiographs are considered appropriate. Regarding the threat of lawsuits for failure to diagnose, dentists who follow guidelines on radiographs developed or endorsed by authoritative bodies that help establish the standard of care should have no concerns. Although lawsuits can be filed for many reasons, it is unlikely that they will be successful if it can be shown that the practitioner did a thorough clinical examination and history and carefully considered the guidelines when determining whether to order radiographs.
Some dentists set up their practices so that new patients are automatically seen first by the dental hygienist, who takes a predetermined set of radiographs at the first appointment, before the dentist sees the patient. Although this may make efficient use of the dentist’s time, it is contrary to the recommendations of the American Dental Association (ADA) that the selection of radiographs should be based on the findings of the clinical examination. Performing a thorough examination before radiographs are ordered should not be an insurmountable obstacle for an efficient dental practice.
Regarding the issue of cost versus benefit of radiographs, for any individual patient there is little risk of harm from a set of radiographs, even if no important diagnostic information is revealed. However, there is a large societal cost, both in terms of health care dollars and radiation risk, if millions of dental patients receive unproductive radiographic examinations, as would happen if routine screening were widespread.
Our philosophy is that radiographs should be based on the need for diagnostic information for patients on a case-by-case basis. For that reason, the next section will discuss some of the clinical situations that may call for a radiographic examination.
CARIES
Dental caries is the most common dental disease, affecting people of all ages. Although the caries prevalence rates of developed countries have been decreasing since the 1970s, probably partially as a result of the widespread use of fluoride, increasing numbers of older adults are maintaining their teeth throughout their lifetimes, leaving them at risk for developing both coronal and root caries. Although occlusal, buccal, and lingual carious lesions are reasonably easy to detect clinically, interproximal caries and caries associated with existing restorations are much more difficult to detect with only a clinical examination (see Chapter 17). Studies have repeatedly demonstrated that clinicians using radiographs detect caries not evident clinically, both in enamel and in dentin. Although a radiographic examination is very important for diagnosis of dental caries, the optimal frequency for such an examination should be based on mitigating features such as the patient’s age, medical condition, diet, oral hygiene practices, oral health status, and the nature of the caries process itself.
Carious lesions demonstrate one of three behaviors: progression, arrest, or regression. Only about 50% of lesions progress beyond the initial, just-detectable defect, and in most instances the lesions demonstrate a slow rate of progression through enamel (months to years). Mechanisms are also in use to enhance remineralization of early enamel lesions. However, the rate of caries progression is significantly faster in deciduous than in permanent enamel, and patients vary widely in their rates of formation of caries and in their rates of caries progression.
Because the presence of caries cannot be determined with confidence by clinical examination alone, it is necessary to expose patients periodically through bitewing radiography to monitor dental caries. The length of the exposure intervals varies considerably because of different patient circumstances. For most patients in good physical health with adequate oral hygiene, an infrequent radiographic examination is needed to monitor dental caries. However, if the patient history and clinical examination suggest that the individual has a relatively high caries experience, shorter intervals allow careful monitoring of disease.
PERIODONTAL DISEASES
Some form of periodontal disease affects most people at some point during their lives, gingivitis more often in younger individuals and periodontitis more commonly in older adults. Periodontal diseases are responsible for a substantial portion of all teeth lost. A consensus exists among practitioners that radiographic examinations play an important role in the evaluation of patients with periodontal disease after the disease is initially detected on clinical examination (see Chapter 18). In addition to providing a picture of the extent of alveolar bone support for the dentition, radiographic examinations help demonstrate local factors that complicate the disease, including the presence of gingival irritants such as calculus and faulty restorations. Occasionally the length and morphologic features of roots, visible on periapical radiographs, are crucial factors in the prognosis of the disease. These observations suggest that, when clinical evidence exists of periodontal disease other than nonspecific gingivitis, it is appropriate to make radiographs, generally a combination of periapicals and bitewings, to help establish the severity of the disease. Follow-up radiographs after therapy is complete will help the clinician monitor the progression of disease and determine whether the destruction of alveolar bone has been halted.
DENTAL ANOMALIES
Abnormal formation of teeth may be manifested as deviations in number, size, and composition. These abnormalities in dental development occur more frequently, and are more likely to have a serious impact, in the permanent dentition than in the primary dentition. The most frequently encountered anomalies are the presence of supernumerary teeth, usually mesiodens, or developmentally absent teeth, usually second premolars (see Chapter 19).
Few anomalies exist for which orthodontic treatment or surgical correction or modification must start at an early age. When the dentist suspects an abnormality requiring treatment, radiographs to confirm and localize it are not required until the time when the treatment is most appropriate. For example, a panoramic examination of a 5-year-old child to determine the presence or absence of permanent teeth may be ill timed. Although the examination provides evidence that one or more second premolars or lateral incisors are developmentally missing, this information usually does not influence the current treatment plan. When examination for dental anomalies is appropriate, both the radiation dose and the anticipated diagnostic benefit should be considered. Projections that best demonstrate the required diagnostic information should be selected. A panoramic radiograph of the lower face is usually best for observing the presence or absence of teeth in all quadrants, although a periapical film or an occlusal film is sufficient for an examination limited to one area.
GROWTH AND DEVELOPMENT AND DENTAL MALOCCLUSION
Children and adolescents are often examined to assess the growth and development of the teeth and jaws. This assessment considers the relationship of one jaw to the other and to the soft tissues. An examination of occlusion, growth, and development requires an individualized radiographic examination that may include periapicals or a panoramic examination to supplement any radiographs ordered to assess dental disease. In addition, a patient of any age group who is being considered for orthodontic treatment may need other radiographs, such as a lateral or frontal cephalograph, occlusal view, carpal index, or temporomandibular joint (TMJ) radiograph, depending on the clinical findings (Fig. 15-1).
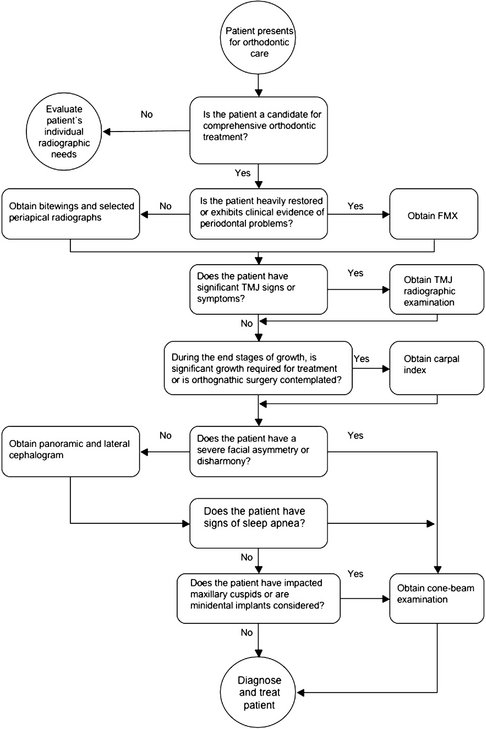
FIG. 15-1 An example of a clinical algorithm to order radiographs for orthodontic patients. Selected radiographs are ordered after the dentist’s consideration of the patient’s history and clinical characteristics.
Cone-beam computed tomography (CBCT) is being used increasingly frequently for orthodontic evaluation, to provide three-dimensional information about jaw relationships, and to substitute for multiple other imaging examinations (see Chapter 14). At this time it is not yet clear which patients will benefit from CBCT in terms of treatment considerations.
The dentist who is the primary provider of orthodontic treatment should select the number and type of radiographs needed. The needs of each patient should be considered individually. Selected radiographs should allow a maximal diagnostic yield with a minimal radiographic exposure after consideration of the clinical examination, the study of plaster models and photographs, and the optimal time to initiate treatment.
OCCULT DISEASE
Occult disease refers to disease that presents no clinical signs or symptoms. Occult diseases in the jaws include a combination of dental and intraosseous findings. Dental findings may include incipient carious lesions, resorbed or dilacerated roots, and hypercementosis. Intraosseous findings include osteosclerosis, unerupted teeth, periapical disease, and a wide variety of cysts and benign and malignant tumors (see Chapters 20 through 25). Small carious lesions, resorption of root structure, and bony lesions may go unnoticed until signs and symptoms develop.
Although the consequences of some occult diseases may be quite serious, most serious diseases are rare. Often a historical or clinical sign or symptom of intraosseous disease suggests its presence. For instance, an unusual contour of bone or an absent third molar, not explained by a history of extraction, suggests the possibility of an impaction with the potential for an associated dentigerous cyst. Although patient history and clinical signs and symptoms do not always accurately predict the finding of dental and intraosseous findings, the majority of these true occult diseases are not clinically relevant or they are so rare that, except for caries as described previously, the dentist need not obtain a radiographic examination of the jaws solely to screen for them in dentate individuals in the absence of unusual clinical signs or symptoms. Caries is an exception because of its much higher prevalence than other occult diseases.
There is a considerable difference of opinion on whether asymptomatic edentulous patients seen for routine denture construction should have screening radiographs taken to look for occult disease. Several studies have demonstrated a relatively large number of lesions on radiographs of edentulous patients, including retained root tips and areas of sclerotic bone, but almost all these findings required no treatment and did not affect the outcome of care. For that reason, some recommend no radiographs of edentulous patients if the clinical examination is negative for signs and symptoms of disease. Others still think that screening radiographs of these patients are of value. As the standard of care for completely or partially edentulous patients moves toward dental implants rather than removable prosthetics, imaging to assess the quantity and quality of bone available for implants is gaining in importance.
There has been increasing interest in the last few years in using panoramic radiographs to screen patients for the presence of calcified atheromas in the bifurcation of the carotid artery, a finding that may indicate an increased risk for the development of a cerebrovascular accident (stroke). However, the value of this finding has been questioned recently because a noncalcified vulnerable plaque, which is not visible on panoramic radiographs, may put the patient at more risk for stroke than a more stable calcified plaque. Nevertheless, the general consensus at this time is that panoramic radiographs made for dental purposes should be evaluated for this calcification, particularly in patients older than 55 years, but that these radiographs should not be made simply to screen for atheromas without other dental indications. (See Chapter 28 for more details.)
JAW DISEASE
Imaging of known jaw lesions, such as fibro-osseous diseases or neoplastic diseases, before biopsy and definitive treatment is also important for appropriate management of the patient. For small lesions of the jaws, periapical or panoramic radiographs may be enough as long as the lesion can be seen in its entirety. If clinical evidence of swelling exists, some type of radiograph at 90 degrees to the original plane should be made to determine whether there is expansion of the jaw or perforation of the buccal or lingual cortical bone. If lesions are too large to fit on standard dental films, extend into the maxillary sinus or other portions of the head outside the jaws, or are suspected of malignancy, additional imaging such as computed tomography (CT) or CBCT is appropriate before biopsy (see Chapters 13 and 14). This type of imaging can define the extent of the lesion, suggest an operative approach, and provide information about the nature of the lesion. The person performing the biopsy or managing the patient should order the advanced images to decrease confusion and increase coordination of care.
TEMPOROMANDIBULAR JOINT
Many types of diseases affect the TMJ, including congenital and developmental malformations of the mandible and cranial bones; acquired disorders such as disk displacement, neoplasms, fractures, and dislocations; inflammatory diseases that produce capsulitis or synovitis; and arthritides of various types, including rheumatoid arthritis and osteoarthritis. The goal of TMJ imaging, similar to that for imaging other body parts, should be to obtain new information that will influence patient care. Radiologic examination may not be needed for all patients with signs and symptoms referable to the TMJ region, particularly if no treatment is contemplated (see Chapter 26). The decision of whether and how to image the joints should depend on the results of the history and clinical findings, the clinical diagnosis, and results of prior examinations, as well as the tentative treatment plan and expected outcome.
The cost of the examination and the radiation dose should also influence the decision if more than one type of examination can provide the desired information. For example, information about the status of the osseous tissues can be obtained from panoramic radiographs, plain films, conventional tomography, CT, CBCT, and magnetic resonance imaging (MRI). The subtlety of the expected findings and the amount of detail required should be considered when selecting the examination to perform. If soft tissue information such as disk position is necessary for patient care, MRI or arthrography is appropriate.
IMPLANTS
An increasingly common method of replacing missing teeth is with osseointegrated implants, metal screws that are inserted into the mandible or maxilla. Prosthetic appliances are then affixed to the screws after a period of healing. Preoperative planning is crucial to ensure success of the implants. The dentist must evaluate the adequacy of the height and thickness of bone for the desired implant; the quality of the bone, including the relative proportion of medullary and cortical bone; the location of anatomic structures such as the mandibular canal or maxillary sinus; and the presence of structural abnormalities such as undercuts that may affect placement or angulation of the implant (see Chapter 32).
Standard periapical and panoramic radiographs can supply information regarding the vertical dimensions of the bone in the proposed implant site. However, some type of cross-sectional imaging (conventional tomography, CT, or CBCT) is recommended before implant placement for visualization of important anatomic landmarks, determination of size and path of insertion of implant, and evaluation of the adequacy of the bone for anchorage of the implant. There is also increasing use of implant planning software and preparation of surgical drilling guides, which require the three-dimensional data from CT or CBCT. Postoperative evaluation of implants may be needed at later times to judge healing, assess complete seating of fixtures, and ensure continued health of the surrounding bone.
PARANASAL SINUSES
Because dentists are not usually the primary providers of treatment for acute or chronic sinus disease, the necessity to perform sinus imaging may be limited in general dental practice. However, because sinus disease can present as pain in the maxillary teeth and because periapical inflammation of maxillary molars and premolars can also lead to changes in the mucosa of the maxillary sinus, circumstances occur in which the dentist needs to obtain an image of the maxillary sinus. Another reason to image this area is to assess the need for bone augmentation/sinus lift before implant placement in the posterior maxilla. Periapical and panoramic radiographs demonstrate the floor of the maxillary sinus well, but visualization of other walls requires additional imaging techniques such as occipitomental (Waters) view, CBCT, or CT. These radiographs are best ordered by the person treating the patient so that diagnostic and therapeutic measures may be coordinated (see Chapter 27).
TRAUMA
Patients who have sustained trauma to the oral region may visit a dentist for evaluation and management of the injuries. For proper management it is important to determine the full extent of the injuries. Periapical or panoramic radiographs are helpful for evaluation of fractures of the teeth. If a suspected root fracture is not visible on a periapical radiograph, a second radiograph made with a different angulation may be helpful. A fracture that is not perpendicular to the beam may not be detectable unless root resorption is present. Thus a tooth with a history of trauma should be monitored and evaluated radiographically on a periodic basis, even if the original radiograph is negative.
Fractures of the mandible can frequently be detected with panoramic radiographs, supplemented by images at 90 degrees such as a posteroanterior or reverse-Towne view (see Chapter 29). Trauma to the maxilla and midface may require CT or CBCT for a thorough evaluation. Affected patients are more likely to report to a hospital emergency department than to a general dental office. The hospital may have a standard protocol for trauma cases. Ideally the clinician responsible for managing care determines the appropriate radiographs for the specific case.
Radiographic Examinations
After concluding that a patient requires a radiograph, the dentist should consider which radiographic examination is most appropriate to meet all the patient’s diagnostic and treatment planning needs. A variety of radiographic projections is available. In choosing one, the dentist should consider the anatomic relationships, the size of the field, and the radiation dose from each view. Table 15-1 summarizes the more common types of radiographic examinations for general dental patients and factors to consider in choosing the most appropriate one. For example, a panoramic radiograph provides broad area coverage with moderate resolution. Intraoral films give more detailed information but a significantly higher radiation dose per unit area exposed. The clinician must use clinical judgment to weigh these factors. Examples of all these radiographs can be found in previous chapters.
TABLE 15-1
Dental Radiographic Examinations and Their Properties
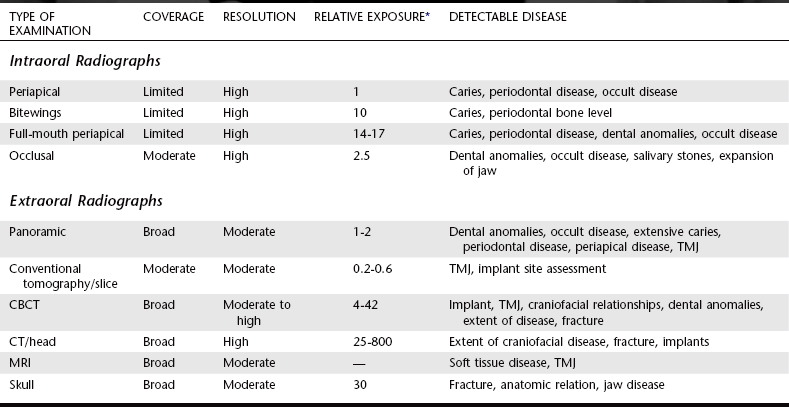
*The parameters assume use of F-speed film and rectangular collimation for periapical films, round collimation for bitewings and occlusal views, and rare-earth screens for panoramic examinations. With D-speed film the intraoral values are more than doubled compared with F-speed film, and with round collimation the periapical values increase by 2.5 times compared with rectangular collimation.
From Frederiksen N, Benson B, Sokolowski T: Effective dose and risk assessment from computed tomography of the maxillofacial complex, Dentomaxillofac Radiol 24:55-58, 1995; Scaf G, Lurie AG, Mosier KM et al: Dosimetry and cost of imaging osseointegrated implants with film-based and computed tomography, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83:41-48, 1997; White SC: 1992 assessment of radiation risks from dental radiology, Dentomaxillofac Radiol 21:118-126, 1992; Ludlow JB, Davies-Ludlow LE, Brooks SL et al: Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT, Dentomaxillofac Radiol 35:219-226, 2006.
INTRAORAL RADIOGRAPHS
Intraoral radiographs are examinations made by placing the x-ray film within the patient’s mouth during the exposure. These exposures offer the dentist a high-detail view of the teeth and bone in the area exposed. Such views are most appropriate for revealing caries and periodontal and periapical disease in a localized region. A complete-mouth or full-mouth examination (FMX) consists of periapical views of all the tooth-bearing regions as well as interproximal views (see Chapter 9).
Periapical Radiographs
Periapical views show all of a tooth and the surrounding bone and are very useful for revealing caries and periodontal and periapical disease. These views may be made of a specific tooth or region or as part of an FMX.
Interproximal Radiographs
Interproximal views (bitewings) show the coronal aspects of both the maxillary and mandibular dentition in a region, as well as the surrounding crestal bone. These views are most useful for revealing proximal caries and evaluating the height of the alveolar bony crest. They can be made in either the anterior or posterior region of the mouth.
Occlusal Radiographs
Occlusal views are intraoral radiographs in which the film is positioned in the occlusal plane. They are often used in lieu of periapical views in children because the small size of the patient’s mouth limits film placement. In adults, occlusal radiographs may supplement periapical views, providing visualization of a greater area of teeth and bone. They are useful for demonstrating impacted or abnormally placed maxillary anterior teeth or visualizing the region of a palatal cleft. Occlusal views may also demonstrate buccal or lingual expansion of bone or presence of a sialolith in the submandibular duct.
EXTRAORAL RADIOGRAPHS
Extraoral radiographs are examinations made of the orofacial region by use of films located outside the mouth. The relationships among patient position, film location, and beam direction vary depending on the specific radiographic information desired. The standard technique for making several extraoral radiographs is discussed in Chapter 12. Only the panoramic radiograph is described here because it has common use as a radiographic examination for general dental patients.
Panoramic Radiographs
Panoramic radiographs provide a broad view of the jaws, teeth, maxillary sinuses, nasal fossa, and TMJs (see Chapter 11). They show which teeth are present, their relative state of development, the presence or absence of dental abnormalities, and many traumatic and pathologic lesions in bone. Panoramic radiographs are the technique of choice for initial examinations of edentulous patients. Because this system is an extraoral technique and uses intensifying screens, the resolution of the images is less than with the intraoral nonscreen films (see Chapter 5). Panoramic radiographs are also susceptible to artifacts from improper patient positioning that negatively affect the image. Consequently this system is generally considered inadequate for independent diagnosis of caries, root abnormalities, and periapical changes.
In the majority of dental patients, oral disease involving the teeth or jaw bones lies within the area imaged by periapical radiographs. Therefore when a full-mouth set of radiographs is available, a panoramic examination is usually redundant because it does not add information that alters the treatment plan. However, situations may exist in which a panoramic radiograph may be preferred over a periapical examination, such as for assessing growth and development in a child or adolescent. Panoramic views are most useful when the required field of view is large but the need for high resolution is of less importance. Although the selection of a radiographic examination should be based on the extent of the expected information it is likely to provide, the relatively low dose of radiation from the panoramic examination should also be a qualifying factor.
Advanced Imaging Procedures
A variety of advanced imaging procedures such as CT, CBCT, MRI, ultrasonography, and nuclear medicine scans may be required in specific diagnostic situations. These techniques are discussed in Chapter 13, although in general the dentist refers the patient to a hospital or other imaging center for these procedures rather than performing them in the dental office.
Guidelines for Ordering Radiographs
The ADA has issued guidelines recommending which radiographs to make and how often to repeat them:
• Make radiographs only after a clinical examination.
• Order only those radiographs that directly benefit the patient in terms of diagnosis or treatment plan.
• Use the least amount of radiation exposure necessary to generate an acceptable view of the imaged area.
PREVIOUS RADIOGRAPHS
Most patients have been seen previously by a dentist and have already had radiographs made. These radiographs are helpful regardless of when they were exposed. If they are relatively recent, they may be adequate to the diagnostic problem at hand. Even if they were made so long ago that they are not likely to reflect the current status of the patient, they may still prove useful. These previous radiographs may demonstrate whether a condition has worsened, has remained unchanged, or has shown healing, such as in the progression of caries or periodontal disease.
ADMINISTRATIVE RADIOGRAPHS
Administrative radiographs are those made for reasons other than diagnosis, including those made for an insurance company or for an examining board. We think that it is appropriate to expose patients only when it benefits their health care. Most administrative radiographs do not serve such an objective. Unfortunately, this recommendation is often not adhered to in practice, and dentists are left to sort out the most appropriate criteria to use in their practices.
Use of Guidelines to Order Dental Radiographs
At any time, patients generally have a combination of diseases that the clinician must consider. Therefore guidelines specify not only which examinations to order but also which specific patient factors influence the number and type of x-ray films to order.
A panel of individuals was convened in the mid 1980s at the request of a branch of the Food and Drug Administration (FDA) to develop a set of guidelines for the making of dental radiographs. The panel addressed the topic of appropriate radiographs for an adequate evaluation of a new or recall asymptomatic patient seeking general dental care. The guidelines were updated in 2004 to reflect changes in technology and to address situations not considered in the first document (Table 15-2). However, there was no change in philosophy between the original and current guidelines.
TABLE 15-2
U.S. Food and Drug Administration Guidelines for Prescribing Dental Radiographs*
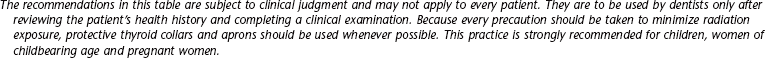
*Reprinted from U.S. Department of Health and Human Services, Public Health Service, Food and Drug Administration; and American Dental Association, Council on Dental Benefit Programs, Council on Scientific Affairs.
†Clinical situations for which radiographs may be indicated, but are not limited to, include the following: Positive historical findings: Previous periodontal or endodontic treatment, history of pain or trauma, familial history of dental anomalies, postoperative evaluation of healing, remineralization monitoring, presence of implants or evaluation for implant placement. Positive clinical signs/symptoms: clinical evidence of periodontal disease, large or deep restorations, deep carious lesions, malposed or clinically impacted teeth, swelling, evidence of dental/facial trauma, mobility of teeth, sinus tract (“fistula”), clinically suspected sinus pathology, growth abnormalities, oral involvement in known or suspected systemic disease, positive neurologic findings in the head and neck, evidence of foreign objects, pain and/or dysfunction of the temporomandibular joint, facial asymmetry, abutment teeth for fixed or removable partial prosthesis, unexplained bleeding, unexplained sensitivity of teeth, unusual eruption, spacing or migration of teeth, unusual tooth morphology, calcification or color, missing teeth with unknown reason, clinical erosion.
‡Factors increasing risk for caries may include, but are not limited to, the following: high level of caries experience or demineralization, history of recurrent caries, high titers of cariogenic bacteria, existing restoration of poor quality, poor oral hygiene, inadequate fluoride exposure, prolonged nursing (bottle or breast), diet with high sucrose frequency, poor family dental health, developmental or acquired enamel defects, developmental or acquired disability, xerostomia, genetic abnormality of teeth, many multisurface restorations, chemotherapy/radiation therapy, eating disorders, drug/alcohol abuse, irregular dental care.
The guidelines describe circumstances (patient age, medical and dental history, and physical signs) that suggest the need for radiographs. These circumstances are called selection criteria. The guidelines also suggest the types of radiographic examinations most likely to benefit the patient in terms of yielding diagnostic information. They recommend that radiographs not be made unless some expectation exists that they will provide evidence of diseases that will affect the treatment plan. The ADA was an equal partner with the FDA in the revision of the guidelines and recommends their use.
These guidelines also form the basis of the recommendations in this chapter. However, the practitioner, who is the only one who knows the patient’s dental history and susceptibility to oral disease, must make the ultimate decision on whether to order radiographs, using the guidelines as a resource, not as a standard of care or a regulation.
Central to the guidelines is the idea that dentists should expose patients to radiation only when they reasonably expect that the resulting radiograph will benefit patient care. Accordingly, two situations mandate a radiograph: some clinical evidence of an abnormality that requires further evaluation for a complete assessment or a high probability of disease that warrants a screening examination.
Selection criteria for radiographs are those signs or symptoms found in the patient history or clinical examination that suggest that a radiographic examination will yield clinically useful information. A key concept in the use of selection criteria is recognition of the need to consider each patient individually. Prescription of radiographs should be decided on an individual basis according to the patient’s demonstrated need.
The guidelines include a description of clinical situations in which radiographs are likely to contribute to the diagnosis, treatment, or prognosis. Two examples highlight the differences between ordering radiographs for dental diseases with clinical signs and symptoms and dental diseases with no clinical indicators but high prevalences. In the first case, a patient has a hard swelling in the premolar region of the mandible with expansion of the buccal and lingual cortical plates. The clinical sign of swelling alerts the dentist to the need for a radiograph to determine the nature of the abnormality causing the swelling.
An example of the second situation is the patient who comes seeking general dental care after having not seen a dentist for many years. Even without clinical evidence of caries, bitewings are indicated because of the prevalence of dental caries in the population. Because this patient has not had interproximal radiographs for many years, it is reasonable to assume that the patient may benefit from the radiograph by the detection of interproximal caries. Although no clinical signs exist that predict the presence of early caries, the dentist relies on clinical knowledge of the prevalence of caries to decide that this radiograph has a reasonable probability of finding disease.
Without some specific indication, it is inappropriate to expose the patient “just to see if there is something there.” The major exception to this rule is the use of interproximal films for caries when no clinical signs exist of early lesions. The probability of finding occult disease in a patient with all permanent teeth erupted and no clinical or historical evidence of abnormality or risk factors is so low that making a periapical or panoramic radiographic survey just to look for such disease is not indicated.
PATIENT EXAMINATION
The ordering of radiographs requires a reasonable expectation that they will provide information that will contribute to solving the diagnostic problem at hand. Accordingly, the first step is a careful examination of the patient, including transillumination of the anterior teeth to evaluate for interproximal decay. The clinical examination provides indications as to the nature and extent of the radiographic examination appropriate to the situation.
A team of dentists tested the ability of the ADA guidelines to reduce the number of intraoral radiographs while still offering adequate diagnostic information. This testing of the use of selection criteria demonstrated that a small but significant number of radiographic findings was not 100% covered in the anterior region if only posterior interproximal and selected periapical radiographs were used. The testing suggested that anterior interproximal radiographs or anterior periapicals are also indicated to detect interproximal caries and periodontal disease in the anterior region, specifically for patients with high levels of dental disease. A panoramic radiograph could be made in place of the periapical radiographs to supplement the posterior bitewings if the totality of the disease expected indicates a broad area of coverage and fine detail is not required.
In the ADA/FDA guidelines patients are classified by stage of dental development, by whether they are being evaluated for the first time (without previous documentation) or being reevaluated during a recall visit, and by an estimate of their risk for having dental caries or periodontal disease. A footnote to Table 15-2 also outlines some other clinical findings that indicate when radiographs are likely to contribute to a complete description of the asymptomatic patient.
Applying these guidelines to the specific circumstances with each patient requires clinical judgment and an amalgamation of knowledge, experience, and concern. Clinical judgment is also required to recognize situations that are not described by the guidelines but in which patients will need radiographs nonetheless.
Initial Visit
The guidelines recommend that a child with primary dentition who is cooperative and has closed posterior contacts have only interproximal radiographs to examine for caries. Additional periapical/occlusal views are recommended only in the case of clinically evident diseases or specific historic or clinical indications such as those listed at the footnote of Table 15-2. If the molar contacts are not closed, interproximal radiographs are not necessary because the proximal surfaces may be examined directly.
For radiographic examination of a new patient in the transitional dentition, after eruption of the first permanent tooth the guidelines recommend interproximal radiographs to assess for dental caries and a panoramic radiograph or selected periapical/occlusal views to evaluate growth and development, this being a time when management of dental anomalies might begin.
The guidelines group adolescents and dentate adults together to identify the kind and extent of appropriate radiographic examination. The guidelines recommend that these patients receive an individualized examination consisting of interproximal views and panoramic or periapical views selected on the basis of specific historical or clinical indications. The presence of generalized dental disease often indicates the need for a full-mouth examination. Alternatively, the presence of only a few localized abnormalities or diseases suggests that a more limited examination consisting of interproximal and selected periapical views may suffice. In circumstances with no evidence of current or past dental disease, only interproximal views may be necessary for caries examination.
For the edentulous patient presenting for prosthetic treatment, an individualized examination that is based on clinical signs and symptoms should be performed. This may include a panoramic radiograph or selected periapical/occlusal views, with some type of cross-sectional examination if dental implants are being considered.
Recall Visit
Patients who are returning after initial care require careful examination before determining the need for radiographs. As at the initial examination, selected periapical views should be obtained if any of the historical or clinical signs or symptoms listed in the footnote to Table 15-2 are present and need further evaluation.
The guidelines recommend interproximal radiographs for recall patients to detect interproximal caries. The optimal frequency for these views depends on the age of the patient and the probability of finding this disease. If the patient has clinically demonstrable caries or the presence of high-risk factors for caries (poor diet, poor oral hygiene, and those listed in the footnote to Table 15-2), then bitewings are exposed at fairly frequent intervals (6 to 12 months for children and adolescents and 6 to 18 months for adults) until no carious lesions are clinically evident. The recommended intervals are longer for individuals not at high risk for caries: 12 to 24 months for the child, 18 to 36 months for the adolescent, and 24 to 36 months for the adult. Note that individuals can change risk category, going from high to low risk or the reverse.
Clinical judgment about need for and type of radiographic examination should be used for other circumstances, such as evaluating the status of periodontal disease, monitoring growth and development, and endodontic or restorative considerations. The interproximal examination may be supplemented by a panoramic, selected periapical/occlusal, or an advanced imaging examination, depending on the patient’s specific needs.
A radiographic examination may be required in a number of other situations, such as for patients contemplating orthodontic or implant treatment or patients with intraosseous lesions. The goal should be to obtain the necessary diagnostic information with the minimal radiation dose and financial cost, which can be substantial for advanced imaging procedures such as MRI. The dentist should determine specifically what type of information is needed and the most appropriate technique for obtaining it. An example of a clinical algorithm for ordering radiographs before orthodontic treatment is shown in Figure 15-1, using guidelines endorsed by the American Academy of Orthodontics. Because guidelines for ordering radiographs for other situations are not as well developed, the dentist must rely on clinical judgment.
SPECIAL CONSIDERATIONS
Occasionally it is desirable to obtain radiographs of a woman who is pregnant. The x-ray beam is largely confined to the head and neck region in dental x-ray examinations; thus, fetal exposure is only about 1 microgray (μGy) for a full-mouth examination. This exposure is quite small compared with that received normally from natural background sources. However, concerns have been raised about a possible relationship between maternal radiation dose to the thyroid gland from dental radiographs and low birth-weight babies, prompting the ADA to recommend the use of protective thyroid collars and aprons during dental radiography, especially of children, women of childbearing age, and pregnant women. Because the use of radiographs in all patients is predicated on there being a diagnostic need for them, the guidelines apply to patients who are pregnant as well as those who are not.
Radiation Therapy
Patients with a malignancy in the oral cavity or perioral region often receive radiation therapy for their disease. Some oral tissues receive 50 Gy or more. Although such patients are often apprehensive about receiving additional exposure, dental exposure is insignificant compared with what they have already received. The average skin dose from a dental radiograph is approximately 3 milligrays (mGy), less if faster film or digital imaging is used. Furthermore, patients who have received radiation therapy may have radiation-induced xerostomia and thus are at a high risk for development of radiation caries, which may produce serious consequences if extractions are needed in the future. Accordingly, patients who have had radiation therapy to the oral cavity should be carefully followed up because they are at special risk for dental disease.
EXAMPLES OF USE OF THE GUIDELINES
Consider the ways in which the guidelines can be applied to different clinical situations:
• The first visit of a 5-year-old boy to a dental office. A careful clinical examination reveals that the patient is cooperative and that the posterior teeth are in contact. Posterior bitewings are recommended to detect caries. If all of this patient’s teeth are present, no evidence exists of decay, a reasonably good diet is being observed, and the parent(s) seem(s) well motivated to promote good oral hygiene, no further radiographic examination is required at this time. Radiographs for the detection of development abnormalities are not in order at this age because a complete appraisal cannot be made at age 5 years. Even if it could be made, it is too early to initiate treatment for such abnormalities.
• A 25-year-old woman receiving a 6-month checkup after her last treatment for a fractured incisor. No caries is evident on interproximal radiographs made 6 months ago; currently no clinical signs suggest caries, nor does the patient have high-risk factors for caries. No evidence exists of periodontal disease or other remarkable signs or symptoms in general or associated with the recently fractured tooth. As long as the fractured incisor shows normal vitality testing, no radiographs are recommended for this patient. If the incisor is nonvital, a periapical view of this tooth should be exposed.
• A 45-year-old man returning to the dentist’s office after 1 year. At his last visit you placed two mesial, occlusal, distal amalgam restorations on premolars and performed root canal therapy on number 30. The patient has a 5-mm pocket in the buccal furcation of number 3 but no other evidence of periodontal disease. The guidelines recommend that this patient receive interproximal radiographs to see whether he still has active caries and periapical views of numbers 3 and 30 to evaluate the extent of the periodontal disease and periapical disease, respectively.
• A 65-year-old woman coming to the office for the first time. No previous radiographs are available. A history exists of root canal therapy in two teeth, although the patient is not aware which teeth were treated. Clinical examination reveals multiple carious teeth, multiple missing teeth, and pockets of more than 3 mm involving most of the remaining teeth. The guidelines recommend a full-mouth examination, including interproximal radiographs, for this patient because of the high probability of finding caries, periodontal disease, and periapical disease.
GUIDELINES FOR ORDERING RADIOGRAPHS
Åkerblom, A, Rohlin, M, Hasselgren, G. Individualised restricted intraoral radiography versus full-mouth radiography in the detection of periradicular lesions. Swed Dent J. 1988;12:151–159.
American Dental Association Council on Scientific Affairs. The use of dental radiographs: update and recommendations. J Am Dent Assoc. 2006;137:1304–1312.
Atchison, KA, Luke, LS, White, SC. An algorithm for ordering pretreatment orthodontic radiographs. Am J Orthod Dentofac Orthop. 1992;102:29–44.
Atchison, KA, White, SC, Flack, VF, et al. Assessing the FDA guidelines for ordering dental radiographs. J Am Dent Assoc. 1995;126:1372–1383.
Bohay, RN, Stephens, RG, Kogon, SL. A study of the impact of screening or selective radiography on the treatment and post delivery outcome for edentulous patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:353–359.
Brooks, SL. A study of selection criteria for intraoral dental radiography. Oral Surg Oral Med Oral Pathol. 1986;62:234–239.
Brooks, SL, Brand, JW, Gibbs, SJ, et al. Imaging of the temporomandibular joint: a position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:609–618.
Bruks, A, Enberg, K, Nordqvist, I, et al. Radiographic examinations as an aid to orthodontic diagnosis and treatment planning. Swed Dent J. 1999;23:77–85.
European Commission. Radiation protection 136, European guidelines on radiation protection in dental radiology: the safe use of radiographs in dental practice. http://ec.europa.eu/energy/nuclear/radioprotection/publication/doc/136_en.pdf, 2004.
Hollender, L. Decision making in radiographic imaging. J Dent Educ. 1992;56:834–843.
Keur, JJ. Radiographic screening of edentulous patients: sense or nonsense? A risk-benefit analysis. Oral Surg Oral Med Oral Pathol. 1986;62:463–467.
Luke, LS, Lee, P, Atchison, KA, et al. Orthodontic residents’ indications for use of the lateral TMJ tomogram and the posteroanterior cephalogram. J Dent Educ. 1997;61:29–36.
Molander, B. Panoramic radiography in dental diagnostics. Swed Dent J. 1996;119(Suppl):1–26.
Pitts, NB, Kidd, EA. Some of the factors to be considered in the prescription and timing of bitewing radiography in the diagnosis and management of dental caries. J Dent. 1992;20:74–84.
Rushton, VE, Horner, K, Worthington, HV. Routine panoramic radiography of new adult patients in general dental practice: relevance of diagnostic yield to treatment and identification of radiographic selection criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:488–495.
Stephens, RG, Kogon, SL. New U.S. guidelines for prescribing dental radiographs: a critical review. J Can Dent Assoc. 1990;56:1019–1024.
Tyndall, DA, Brooks, SL. Selection criteria for dental implant site imaging: a position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2000;89:630–637.
U.S. Department of Health and Human Services, Public Health Service, Food and Drug Administration, and American Dental Association, Council on Dental Benefit Programs, Council on Scientific Affairs. The selection of patients for dental radiographic examinations. revised ed www.ada.org/prof/resources/topics/radiography.asp, 2004. Accessed August 22, 2007
White, SC, Heslop, EW, Hollender, LG, et al. Parameters of radiologic care: an official report of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:498–511.
Atchison, KA, White, SC, Flack, VF, et al. Efficacy of the FDA selection criteria for radiographic assessment of the periodontium. J Dent Res. 1995;74:1424–1432.
Backer Dirks, O. Posteruptive changes in dental enamel. J Dent Res. 1966;45(Suppl):503–511.
Friedlander, AH, Freymiller, EG. Detection of radiation-accelerated atherosclerosis of the carotid artery by panoramic radiography: a new opportunity for dentists. J Am Dent Assoc. 2003;134:1361–1365.
Hall, WB. Decision making in periodontology, ed 3. St. Louis: Mosby; 1998.
Madden, RP, Hodges, JS, Salmen, CW, et al. Utility of panoramic radiographs in detecting cervical calcified carotid atheroma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:543–548.
Moles, DR, Downer, MC. Optimum bitewing examination recall intervals assessed by computer simulation. Commun Dent Health. 2000;17:14–19.
Reddy, MS, Geurs, NC, Jeffcoat, RL, et al. Periodontal disease progression. J Periodontol. 2000;71:1583–1590.
Shwartz, M, Gröndahl, H-G, Pliskin, JS, et al. A longitudinal analysis from bitewing radiographs of the rate of progression of approximal carious lesions through human dental enamel. Arch Oral Biol. 1984;29:529–536.
White, SC, Atchison, KA, Hewlett, ER, et al. Clinical and historical predictors of dental caries on radiographs. Dentomaxillofac Radiol. 1995;24:121–127.
White, SC, Atchison, KA, Hewlett, ER, et al. Efficacy of FDA guidelines for ordering radiographs for caries detection. Oral Surg Oral Med Oral Pathol. 1994;77:531–540.
Frederiksen, N, Benson, B, Sokolowski, T. Effective dose and risk assessment from computed tomography of the maxillofacial complex. Dentomaxillofac Radiol. 1995;24:55–58.
Hujoel, PP, Bollen, AM, Noonan, CJ, et al. Antepartum dental radiography and infant low birth weight. JAMA. 2004;291:1987–1993.
Ludlow, JB, Davies-Ludlow, LE, Brooks, SL, et al. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35:219–226.
Scaf, G, Lurie, AG, Mosier, KM, et al. Dosimetry and cost of imaging osseointegrated implants with film-based and computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:41–48.
White, SC. 1992 assessment of radiation risks from dental radiology. Dentomaxillofac Radiol. 1992;21:118–126.