Chapter 9 Dental radiography — general patient considerations including control of infection
This short chapter is designed as a preface to the radiography section. It summarizes the general guidelines relating to patient care, pertinent to all aspects of dental radiography, thus avoiding unnecessary repetition in subsequent chapters. Measures aimed at the control of infection during radiography are also discussed.
GENERAL GUIDELINES ON PATIENT CARE
• For intraoral radiography the patient should be positioned comfortably in the dental chair, ideally with the occlusal plane horizontal and parallel to the floor. For most projections the head should be supported against the chair to minimize unwanted movement. This upright positioning is assumed in subsequent chapters when describing radiographic techniques. However, some clinicians elect to X-ray their patients in the supine position along with most other dental surgery procedures. All techniques need to be modified accordingly, but it can sometimes be more difficult to assess angulations and achieve accurate alignment of film and tubehead with the patient lying down.
• For extraoral views the patient should be reassured about the large, possibly frightening or unfriendly-looking equipment, before being positioned within the machine. This is of particular importance with children.
• The procedure should be explained to the patients in terms they can understand, including warning them not to move during the investigation.
• Spectacles, dentures or orthodontic appliances should be removed. Jewellery including earrings may also need to be removed for certain projections.
• A protective lead thyroid collar, if deemed appropriate for the investigation being carried out, should be placed on the patient (see Ch. 8).
• The exposure factors on the control panel should be selected before positioning the intraoral image receptor and X-ray tubehead, in order to reduce the time of any discomfort associated with the investigation.
• Intraoral image receptor should be positioned carefully to avoid trauma to the soft tissues taking particular care where tissues curve, e.g. the anterior hard palate, lingual to the mandibular incisor teeth and distolingual to the mandibular molars.
• The radiographic investigation should be carried out as accurately and as quickly as possible, to avoid having to retake the radiograph and to lessen patient discomfort.
• The patient should always be watched throughout the exposure to check that he/she has obeyed instructions and has not moved.
SPECIFIC REQUIREMENTS WHEN X-RAYING CHILDREN AND PATIENTS WITH DISABILITIES
These two groups of patients can present particular problems during radiography, including:
As a result of these difficulties, the following additional guidelines should be considered:
• Only radiographic investigations appropriate to the limitations imposed by the patient’s age, cooperation or disability should be attempted
• Select intraoral image receptor of appropriate size, modifying standard techniques as necessary
• Utilize assistant(s) to help hold the image receptor and/or steady and reassure the patient. This can be accomplished by using an accompanying relative, rather than repeatedly using a member of staff.
NOTE: In the UK, the Ionising Radiations Regulations 1999 require that during an exposure a designated controlled area must exist around the X-ray set and theoretically only the patient is allowed in this area (see Ch. 8). Therefore, if assistance is needed and this requirement cannot be fulfilled, the radiation protection adviser (RPA) must advise on the appropriate protective measures for the assistant.
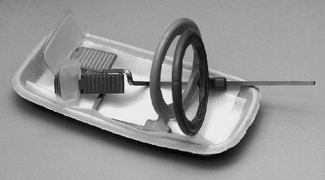
• Perform any necessary radiography under general anaesthesia, if an uncooperative patient is having their dental treatment in this manner (see Fig. 9.1). Radiographs taken are usually restricted to oblique laterals and periapicals although bitewings can be taken.
• Avoid dental panoramic radiography because of the need for the patient to remain still for approximately 18 seconds (see Ch. 17). Oblique lateral radiographs should be regarded as the extraoral views of choice.
• Use the paralleling technique, if possible, for periapical radiography because with this technique the relative positions of the image receptor, teeth and X-ray beam are maintained, irrespective of the position of the patient’s head (see Ch. 10).
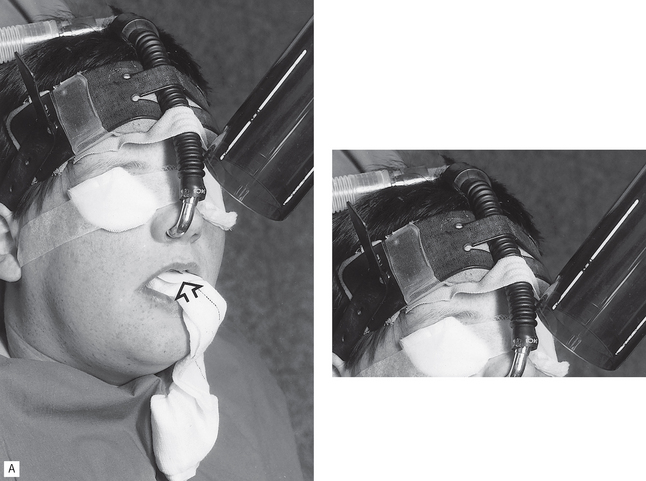
Fig. 9.1 Patient positioning for radiography under general anaesthesia. A Periapical radiography of upper incisor teeth. Note the film packet (arrowed) supported in the desired position by a gauze pack. B Oblique lateral radiography. Note the tape used to stabilize the cassette and maintain the correct patient position.
(Kindly provided by Mr P. Erridge.)
CONTROL OF INFECTION
In the UK, The Health and Safety at Work, Etc, Act of 1974 states that every person working in hospitals or general practice (referred to as health care workers or HCWs) has a legal duty to ensure that all necessary steps are taken to prevent cross-infection to protect themselves, their colleagues and the patients. In addition, The Management of Health and Safety Regulations 1992 requires that a risk assessment is carried out for all procedures to reduce the possibility of harm to staff and patients. Effective infection control measures are therefore required in dental radiography even though most investigations are regarded as non-invasive or non-exposure prone procedures, because they do not involve breaches of the mucosa or skin. The main risk of cross-infection is from one patient to another from salivary contamination of work areas and equipment. HCWs themselves are not at great risk during radiography but there are no grounds for complacency.
Main infections of concern
• Infective hepatitis caused by hepatitis B (HBV) or hepatitis C (HCV) viruses. The WHO estimates that of the 2 billion people that have been infected with HBV, more than 350 million have chronic (lifelong) infections. In the developing world, 8% to 10% of people in the general population become chronically infected. HBV is thought to be 50 to 100 times more infectious than HIV. The WHO estimates that 3% of the world’s population has been infected with HCV.
• Human immunodeficiency virus (HIV disease and AIDS caused by HIV).
• Tuberculosis (TB). The incidence of all forms of TB is rising and now approximately one-third of the world’s population is infected. Many of the people with active TB are also infected with HIV.
• Cold sores caused by herpes simplex virus (HSV). HCWs are at risk of getting herpetic whitlow, a painful finger infection.
• Transmissible spongiform encephalopathies (TSEs), e.g. Creutzfeldt–Jakob disease (CJD).
A thorough medical history should therefore be obtained from all patients. However, the medical history and examination may not identify asymptomatic carriers of infectious diseases.
It is therefore safer for HCWs to accept that ALL patients may be an infection risk — age or class is no barrier — and universal precautions should be adopted. This means that the same infection control measures should be used for all patients, the only exception being for patients known to have or suspected of having TSEs and the small number of patients in the defined risk groups for TSEs.
Infection control measures
As mentioned previously, in dental radiography the main concerns arise from salivary contamination of work areas and equipment. Suitable precautions include:
• Training of all staff in infection control procedures and monitoring their compliance.
• All clinical staff should be vaccinated against hepatitis B, have their response to this vaccine checked and maintain this vaccination.
• Open wounds on the hands should be covered with waterproof dressings.
• Protective non-sterile, non-powdered medical gloves (e.g. latex or nitrile) should be worn for all radiographic procedures and changed after every patient.
• Eye protection — either safety glasses or visors (see Fig. 9.2) should be worn but masks are not usually necessary for radiography.
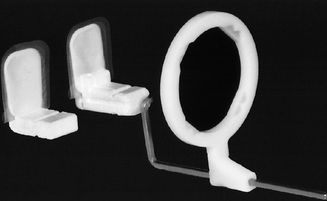
• All required image receptors and holders should be placed on disposable trays to avoid contamination of work surfaces (see Fig. 9.3).
• To prevent salivary contamination of film packets, they should be placed in small barrier envelopes or preferably purchased pre-packed in such envelopes, before use (see Fig. 9.4). After being used in the mouth, the film packet should be emptied out of the barrier envelope onto a clean surface after which it can be handled safely.
• Digital radiography sensors must also be placed inside appropriate barrier envelopes (see Fig. 9.5).
• If barrier envelopes are not used, saliva should be wiped from exposed film packets with disinfectant (e.g. 1% hypochlorite) before handling and processing. This is of particular importance if daylight-loading automatic processors are used because of the risk of salivary contamination of the soft flexible arm sleeves (see Ch. 7 and Fig. 7.3), and if films are collected together during the course of the working day and then processed in batches.
• Film packets must only be introduced into daylight-loading processors using clean hands or washed gloves. Powdered gloves may cause artefacts on the films.
• Contaminated disposable trays, barrier envelopes and image receptor packaging should be discarded directly into suitable clinical waste disposal bags.
• All holders/bite blocks/bite pegs should be rinsed thoroughly to remove saliva, scrubbed in soapy water and autoclaved. Non-autoclavable items such as the aiming ring should be disinfected by soaking in an appropriate solution, e.g. Durr 212 for a minimum of 1 hour.
• Disposable holders should be discarded as clinical waste.
• X-ray equipment, including the tubehead, control panel, timer switch and cassettes which have been touched during the radiographic procedure should be wiped after each patient with a suitable surface disinfectant, e.g. Mikrozid®.
• Alternatively, all pieces of equipment can be covered, for example with cling film, which can be replaced after every patient (see Fig. 9.6).
• Soiled gloves and cleaning swabs should be placed in suitable disposal bags and sealed for incineration.
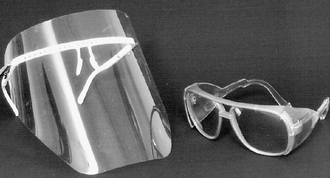
Fig. 9.2 Plastic safety glasses and Vista-Tec visor (Polydentia SA) suitable for eye protection during dental radiography.
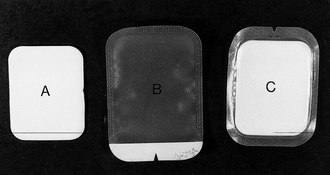
Fig. 9.4 A 31 × 41 mm periapical film packet. B Plastic barrier envelope to take the periapical film. C Pre-packed periapical film packet inside its barrier envelope.

Fig. 9.5 A Solid-state digital sensor inside a barrier envelope. B Barrier wrapped solid-state sensor inserted into a sensor holder. C Barrier envelope for the 31 × 41 mm digital photostimulable phosphor plate shown.
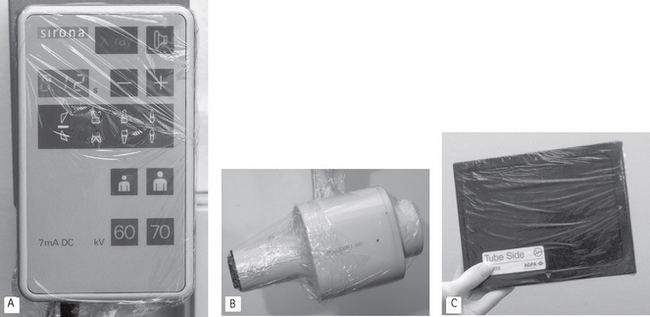
Fig. 9.6 Examples of different pieces of equipment barrier-wrapped in cling film and ready for clinical use A a control panel including the exposure button, B an X-ray tubehead and C a cassette for extraoral use.
Important points to note
• When X-raying known or suspected TSE patients, extraoral radiographic techniques, that avoid salivary contamination, should be chosen whenever possible (preferably using a technique that does not involve any form of intraoral positioning device) and films should be processed immediately and not left on work surfaces.
• If intraoral techniques are necessary, disposable holders should be used (see Fig. 9.7).
• Infection control measures are of particular importance during sialography when the wearing of an eye protective visor and a mask are recommended (see Ch. 33).
FOOTNOTE
The importance of effective control of infection measures during dental radiography cannot be over-emphasized. All health care workers should remember that they have a duty of care to do no harm to their patients. Inadequate infection control measures may put other/subsequent patients at risk from infection whether transmitted directly or indirectly.