Chapter 10 Periapical radiography
Periapical radiography describes intraoral techniques designed to show individual teeth and the tissues around the apices. Each image usually shows two to four teeth and provides detailed information about the teeth and the surrounding alveolar bone.
MAIN INDICATIONS
The main clinical indications for periapical radiography include:
• Detection of apical infection/inflammation
• Assessment of the periodontal status
• After trauma to the teeth and associated alveolar bone
• Assessment of the presence and position of unerupted teeth
• Assessment of root morphology before extractions
• Preoperative assessment and postoperative appraisal of apical surgery
• Detailed evaluation of apical cysts and other lesions within the alveolar bone
IDEAL POSITIONING REQUIREMENTS
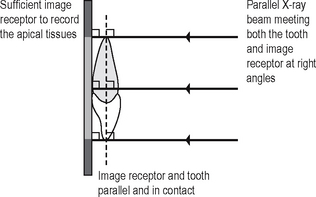
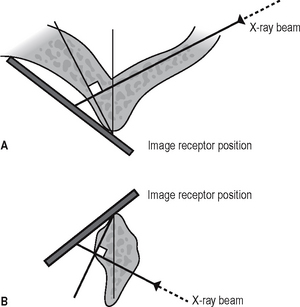
The ideal requirements for the position of the image receptor (film packet or digital sensor) and the X-ray beam, relative to a tooth, are shown in Figure 10.1. They include:
• The tooth under investigation and the image receptor should be in contact or, if not feasible, as close together as possible
• The tooth and the image receptor should be parallel to one another
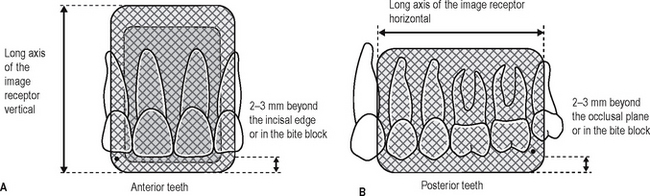
• The image receptor should be positioned with its long axis vertically for incisors and canines, and horizontally for premolars and molars with sufficient receptor beyond the apices to record the apical tissues
• The X-ray tubehead should be positioned so that the beam meets the tooth and the image receptor at right angles in both the vertical and the horizontal planes
RADIOGRAPHIC TECHNIQUES
The anatomy of the oral cavity does not always allow all these ideal positioning requirements to be satisfied. In an attempt to overcome the problems, two techniques for periapical radiography have been developed:
Paralleling technique
Theory
1. The image receptor is placed in a holder and positioned in the mouth parallel to the long axis of the tooth under investigation.
2. The X-ray tubehead is then aimed at right angles (vertically and horizontally) to both the tooth and the image receptor.
3. By using a film/sensor holder with fixed image receptor and X-ray tubehead positions, the technique is reproducible.
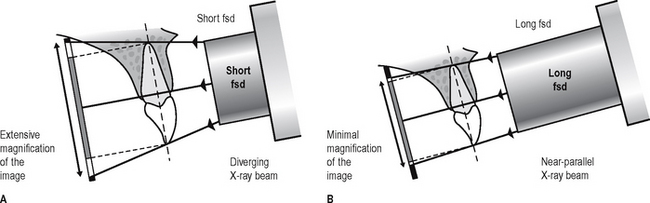
This positioning has the potential to satisfy four of the five ideal requirements mentioned earlier. However, the anatomy of the palate and the shape of the arches mean that the tooth and the image receptor cannot be both parallel and in contact. As shown in Figure 10.2, the image receptor has to be positioned some distance from the tooth.
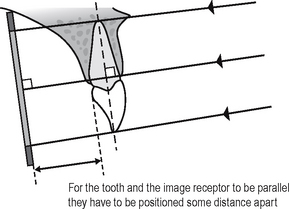
Fig. 10.2 Diagram showing the position the image receptor has to occupy in the mouth to be parallel to the long axis of the tooth, because of the slope of the palate.
To prevent the magnification of the image that this separation would cause, an X-ray beam as non-divergent as possible is required (see Fig. 10.3). As explained in Chapter 5, this is achieved by having a long focal spot to skin distance (fsd), ideally of 200 mm.
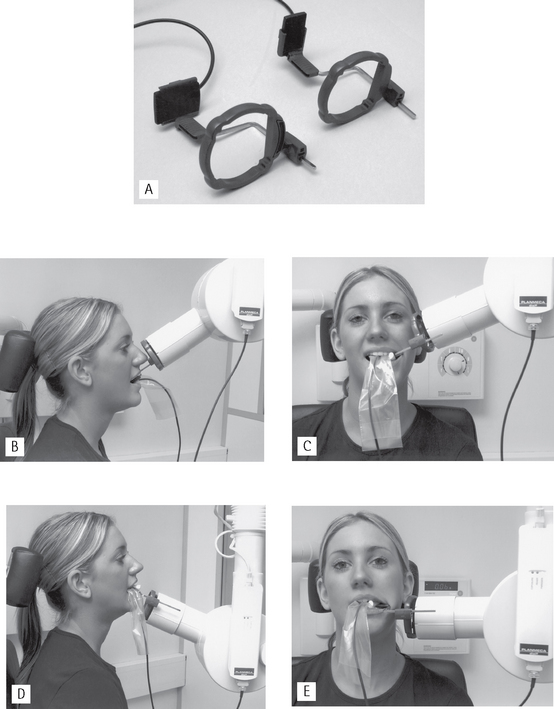
Film packet/sensor holders
A variety of holders has been developed for this technique. The choice of holder is a matter of personal preference and dependent upon the type of image receptor — film packet or digital sensor (solid-state or phosphor plate) — being used. The different holders vary in cost and design, as shown in Figure 10.4, but essentially consist of three basic components:
• A mechanism for holding the image receptor parallel to the teeth that also prevents bending of the receptor
• An X-ray beam-aiming device. This may or may not provide additional collimation of the beam.
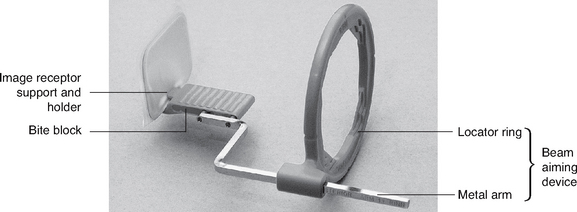
Fig. 10.4 Posterior Rinn XCP image receptor holder showing the three basic components common to most holders.
The different components of the various holders usually need to be assembled together before the holder can be used clinically. The holder design used depends upon whether the tooth under investigation is:
These variables mean that assembling the holder can be confusing, but it must be done correctly. To facilitate this assembly some manufacturers now colour code the various components. Once assembled correctly the entire image receptor should be visible when viewed through the beam-aiming device as shown in Figure 10.5.
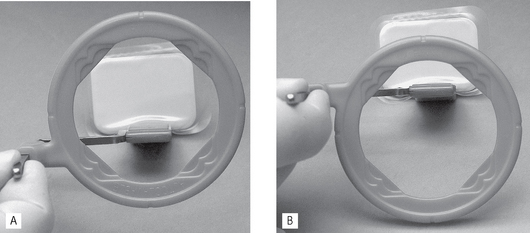
Fig. 10.5 A The appearance of the film packet when viewed through the locator ring of a correctly assembled Rinn XCP holder. B The appearance when the film holder has been assembled incorrectly.
The choice of holder is a matter of personal preference and dependent upon the type of image receptor — film packet or digital sensor (solid-state or phosphor plate) — being used. A selection of different holders is shown in Figure 10.6.
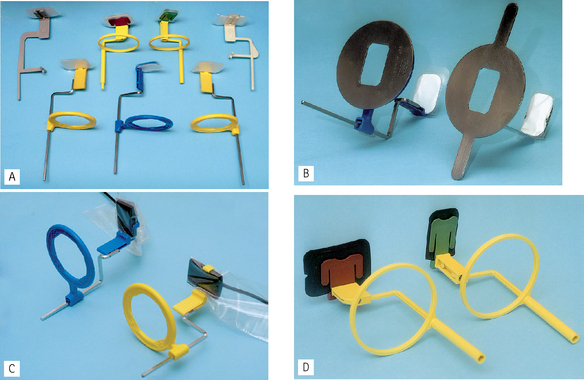
Fig. 10.6 A selection of film packet and digital phosphor plate holders designed for the paralleling technique. Note how some manufactuters use colour coding to identifiy holders for differenct parts of the mouth. B Holders incorporating additional rectangular collimation — the Masel Precision all-in-one metal holder and the Rinn XCP holder with the metal collimator attached to the locator ring. C Blue anterior and yellow posterior Rinn XCP-DS solid-state digital sensor holders. DGreen/yellow anterior and red/yellow posterior Hawe-Neos holders suitable for film packets and digital phosphor plates (shown here).
Typically, the same anterior holder can be used for right and left maxillary and mandibular incisors and canines utilizing a small image receptor (22 × 35 mm) with its long axis vertical. Four images in the maxilla and three images in the mandible are usually required to cover the right and left incisors and canines as shown in Figure 10.7.
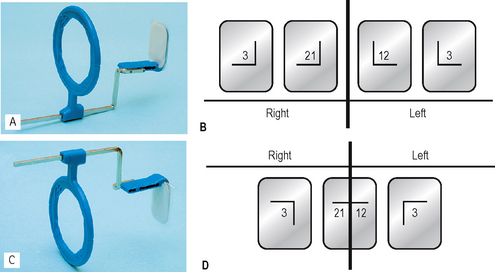
Fig. 10.7 A The anterior Rinn XCP holder suitable for imaging the maxillary incisors and canines. B Diagram showing the four small image receptors required to image the right and left maxillary incisors and canines. C The anterior Rinn XCP holder suitable for imaging the mandibular incisors and canines. D Diagram showing the three small image receptors required to image the right and left mandibular incisors and canines
Typically different holders are required for the right and left premolar and molar maxillary and mandibular posterior teeth. The different designs allow the holders to hook around the cheek and corner of the mouth. A large image receptor (31 × 41 mm) is ideally utilized with its long axis horizontal. Two images are usually required to cover the premolar and molar teeth in each quadrant as shown is Figure 10.8.
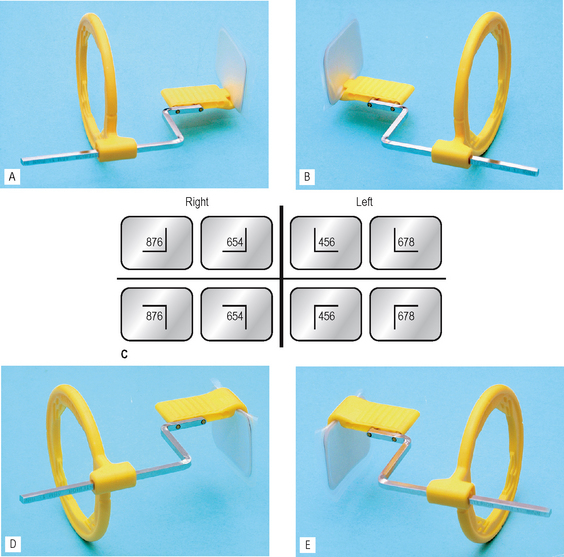
Fig. 10.8 A The posterior Rinn XCP holder assembled for imaging the RIGHT maxillary premolars and molars. B The posterior Rinn XCP holder assembled for imaging the LEFT maxillary premolars and molars. C Diagram showing the two large image receptors required to image the right and left premolars and molars in each quadrant. D The posterior Rinn XCP holder assembled for imaging the RIGHT mandibular premolars and molars. E The posterior Rinn XCP holder assembled for imaging the LEFT mandibular premolars and molars.
Positioning techniques
The radiographic techniques for the permanent dentition can be summarized as follows:
1. The patient is positioned with the head supported and with the occlusal plane horizontal.
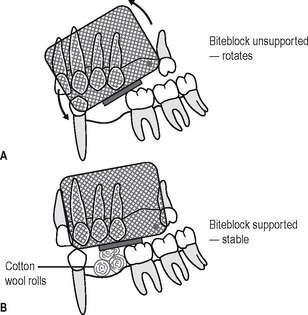
2. The holder and image receptor are placed in the mouth as follows:
3. The holder is rotated so that the teeth under investigation are touching the bite block.
4. A cottonwool roll is placed on the reverse side of the bite block. This often helps to keep the tooth and image receptor parallel and may make the holder less uncomfortable.
5. The patient is requested to bite gently together, to stabilize the holder in position.
6. The locator ring is moved down the indicator rod until it is just in contact with the patient’s face. This ensures the correct focal spot to film distance (fsd).
7. The spacer cone is aligned with the locator ring. This automatically sets the vertical and horizontal angles and centres the X-ray beam on the image receptor
Positioning clinically using film packets and digital phosphor plates is shown in Figures 10.9-10.16 for the following different areas of the mouth:
Maxillary central incisor (Fig. 10.9)
Maxillary canine (Fig. 10.10)
Maxillary premolars (Fig. 10.11)
Maxillary molars (Fig. 10.12)
Mandibular incisors (Fig. 10.13)
Mandibular canine (Fig. 10.14)
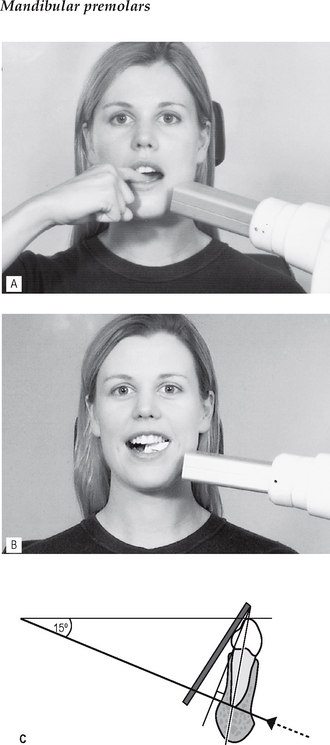
Mandibular premolars (Fig. 10.15)
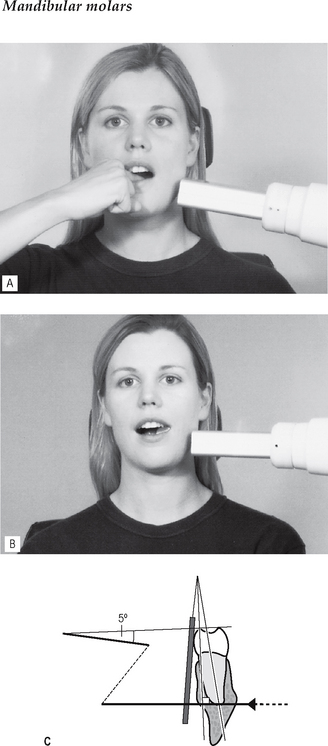
Mandibular molars (Fig. 10.16)
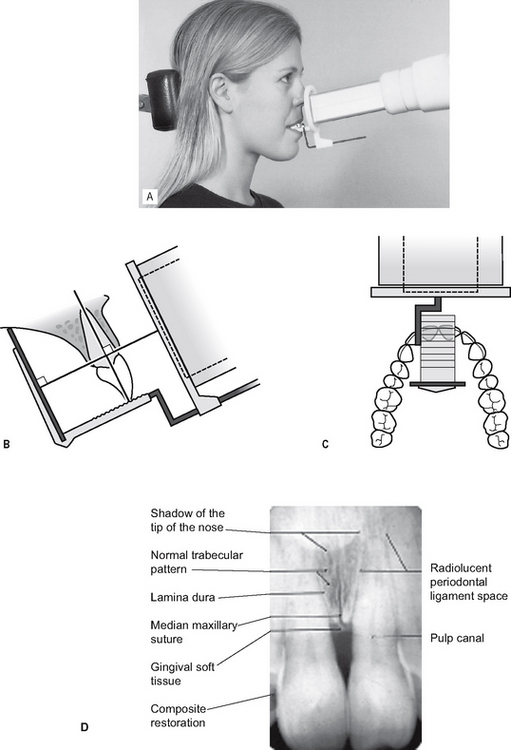
Fig. 10.9 A Patient positioning (maxillary central incisor). B Diagram of the positioning. C Plan view of the positioning. D Resultant radiograph with the main radiographic features indicated.
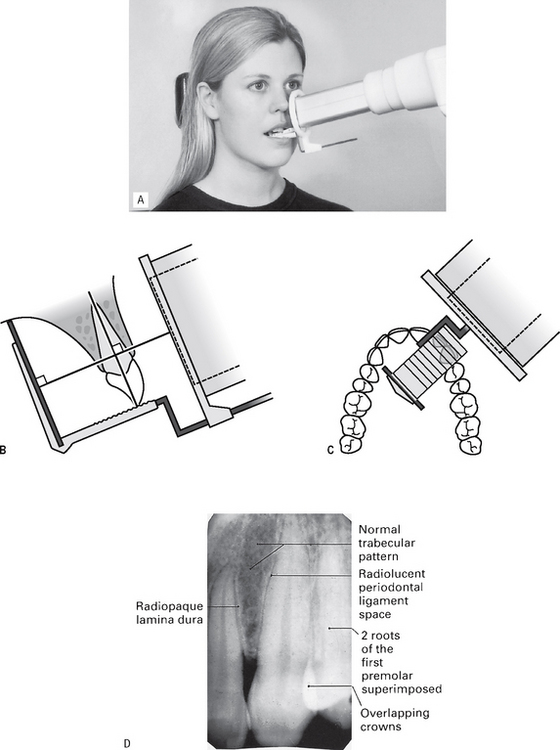
Fig. 10.10 A Patient positioning (maxillary canine). B Diagram of the positioning. C Plan view of the positioning. D Resultant radiograph with the main radiographic features indicated.
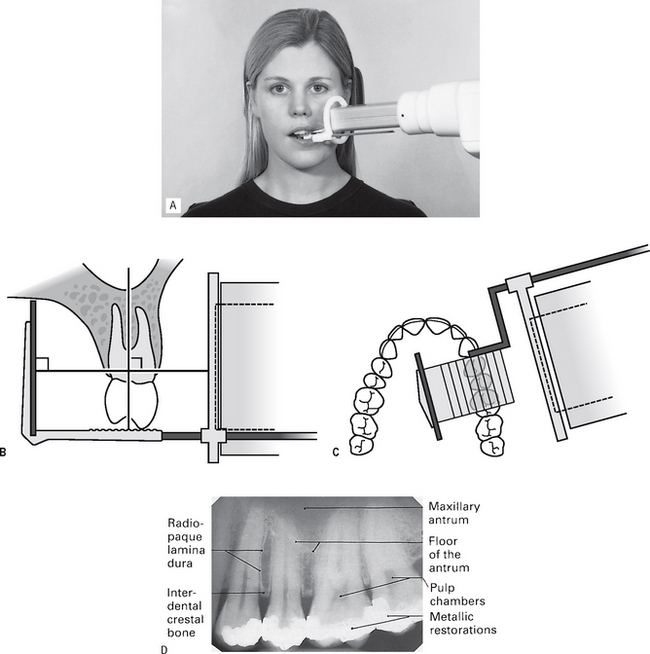
Fig. 10.11 A Patient positioning (maxillary premolars). B Diagram of the positioning. C Plan view of the positioning. D Resultant radiograph with the main radiographic features indicated.
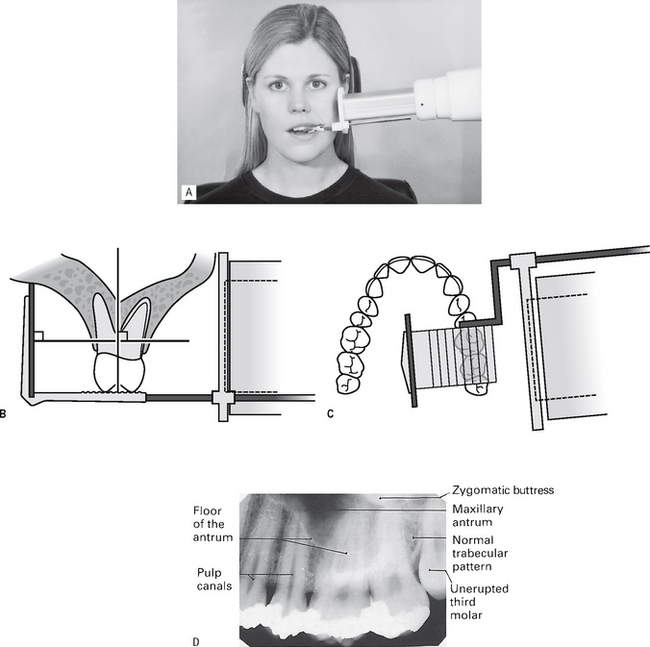
Fig. 10.12 A Patient positioning (maxillary molars). B Diagram of the positioning. C Plan view of the positioning. D Resultant radiograph with the main radiographic features indicated.
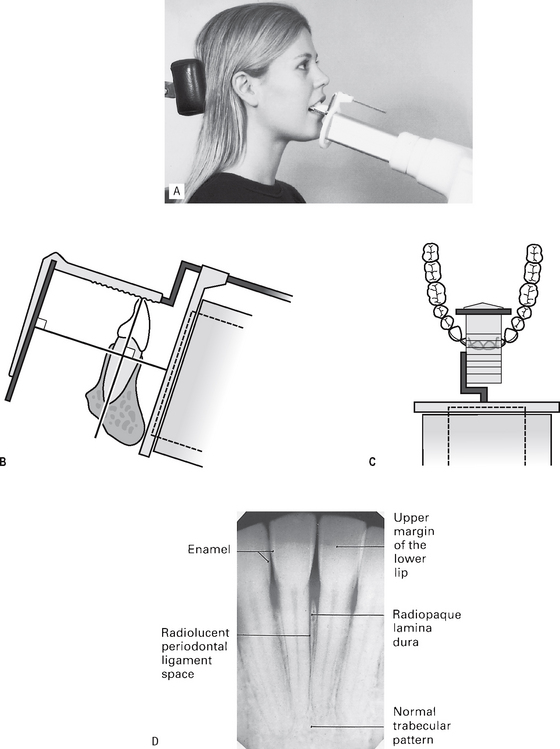
Fig. 10.13 A Patient positioning (mandibular incisors). B Diagram of the positioning. C Plan view of the positioning. D Resultant radiograph with the main radiographic features indicated.
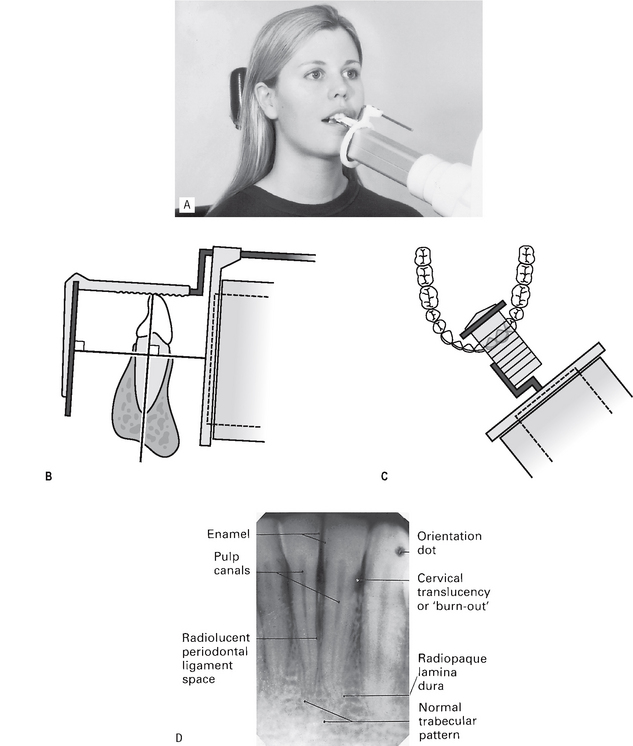
Fig. 10.14 A Patient positioning (mandibular lateral and canine). B Diagram of the positioning. C Plan view of the positioning. D Resultant radiograph with the main radiographic features indicated.
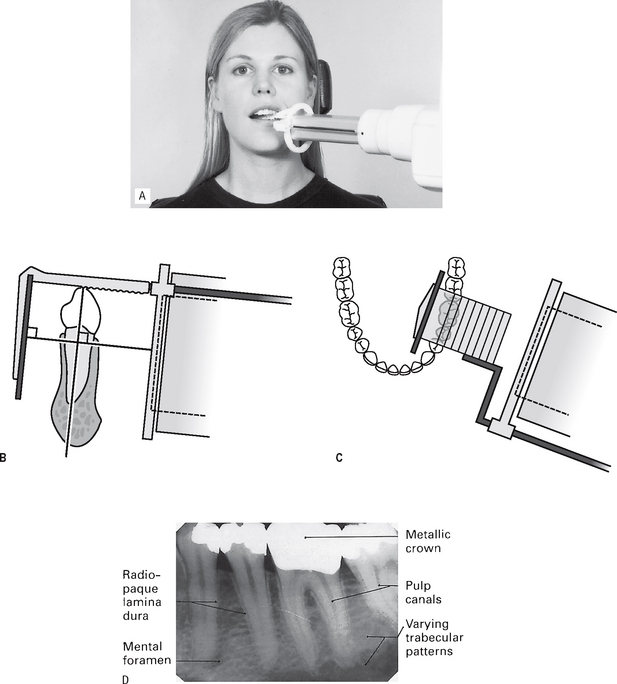
Fig. 10.15 A Patient positioning (mandibular premolars). B Diagram of the positioning. C Plan view of the positioning. D Resultant radiograph with the main radiographic features indicated.
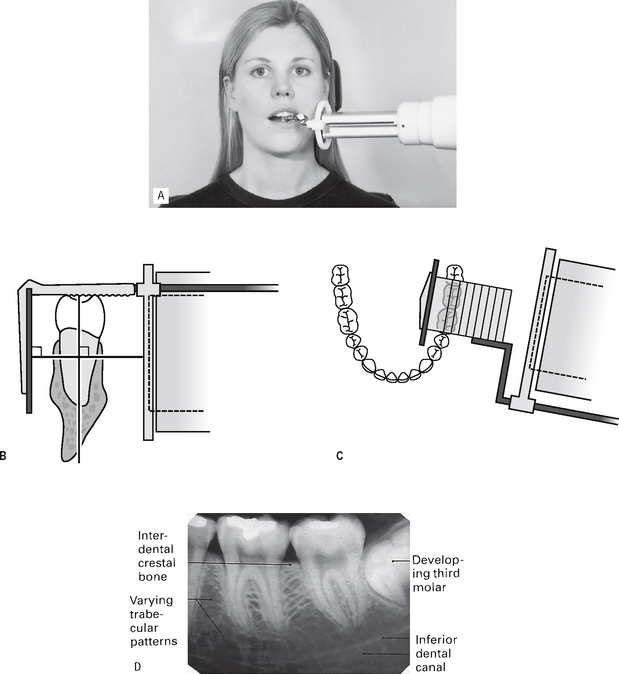
Fig. 10.16 A Patient positioning (mandibular molars). B Diagram of the positioning. C Plan view of the positioning. D Resultant radiograph with the main radiographic features indicated.
Note:
1. Full mouth survey is the terminology used to describe the full collection of 15 periapical radiographs (seven anterior and eight posterior) showing the full dentition.
2. When using film packets and digital phosphor plates the end of the receptor with the orientation dot should be placed opposite the crowns of the teeth to avoid subsequent superimposition of the dot over an apex.
Positioning using solid-state digital sensors
Clinical positioning of holders for the paralleling technique when using solid-state digital sensors can be more difficult because of the bulk and absolute rigidity of the sensor. Those systems employing cables also require extra care with regard to the position of the cable to avoid damaging it. Once the holder is inserted into the mouth, the positioning of the tubehead is the same as described previously when using other types of image receptors and is shown in Figure 10.17 for different parts of the mouth.
Bisected angle technique
Theory
The theoretical basis of the bisected angle technique is shown in Figure 10.18 and can be summarized as follows:
1. The image receptor is placed as close to the tooth under investigation as possible without bending the packet.
2. The angle formed between the long axis of the tooth and the long axis of the image receptor is assessed and mentally bisected.
3. The X-ray tubehead is positioned at right angles to this bisecting line with the central ray of the X-ray beam aimed through the tooth apex.
4. Using the geometrical principle of similar triangles, the actual length of the tooth in the mouth will be equal to the length of the tooth on the image.
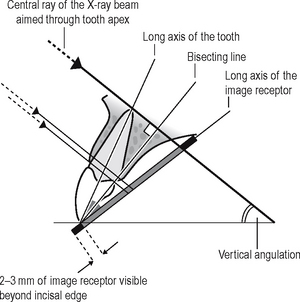
Fig. 10.18 Theoretical basis of the bisected angle technique. The angle between the long axes of the tooth and image receptor is bisected and X-ray beam aimed at right angles to this line, through the apex of the tooth. With this geometrical arrangement, the length of the tooth in the mouth is equal to the length of the image of the tooth on the image receptor, but, as shown, the periodontal bone levels will not be represented accurately.
Vertical angulation of the X-ray tubehead
The angle formed by continuing the line of the central ray until it meets the occlusal plane determines the vertical angulation of the X-ray beam to the occlusal plane (see Fig. 10.18).
Note: Vertical angles are often quoted but inevitably they are only approximate. Patient differences including head position, and individual tooth position and inclination mean that each positioning should be assessed independently. The vertical angulations suggested should be taken only as a general guide.
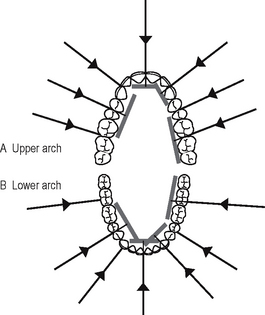
Horizontal angulation of the X-ray tubehead
In the horizontal plane, the central ray should be aimed through the interproximal contact areas, to avoid overlapping the teeth. The horizontal angulation is therefore determined by the shape of the arch and the position of the teeth (see Fig. 10.19).
Positioning techniques
The bisected angle technique can be performed either by using an image receptor holder to support the image receptor in the patient’s mouth or by asking the patient to support the image receptor gently using either an index finger or thumb. Both techniques are described.
Note: the 2001 Guidance Notes recommend that the image receptor should only be held by the patient when it cannot otherwise be kept in position.
Using film packet/digital sensor holders
Various holders are available, a selection of which are shown in Figure 10.20. The Rinn Bisected Angle Instruments (BAI) closely resemble the paralleling technique holders and consist of the same three basic components — image receptor holding mechanism, bite block and an X-ray beam-aiming device — but the image receptor is not held parallel to the teeth. The more simple holders and the disposable bite blocks hold the image receptor in the desired position but the X-ray tubehead then has to be aligned independently. In summary:
1. The image receptor is pushed securely into the chosen holder. Either a large or small size of image receptor is used so that the particular tooth being examined is in the middle of the receptor, as shown in Figure 10.21. When using a film packet the white surface faces the X-ray tubehead and the film orientation dot is opposite the crown.
2. The X-ray tubehead is positioned using the beam-aiming device if available OR the operator has to assess the vertical and horizontal angulations by observation and then position the tubehead without a guide.
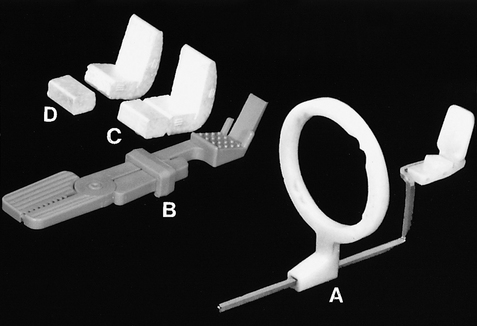
Fig. 10.20 A selection of film packet/phosphor plate holders for the bisected angle technique. A The Rinn bisected angle instrument (BAI). B The Emmenix® film holder. C The Rinn Greene Stabe® bite block. D The Rinn Greene Stabe® bite block reduced in size for easier positioning and for use in children.
Using the patient’s finger
1. The appropriate sized image receptor is positioned and orientated in the mouth as shown in Figure 10.18 with about 2 mm extending beyond the incisal or occlusal edges, to ensure that all of the tooth will appear on the image. The patient is then asked to gently support the image receptor using either an index finger or thumb.
2. The operator then assesses the vertical and horizontal angulations by observation and positions the tubehead without a guide. The effects of incorrect tubehead position are shown in Figure 10.22.
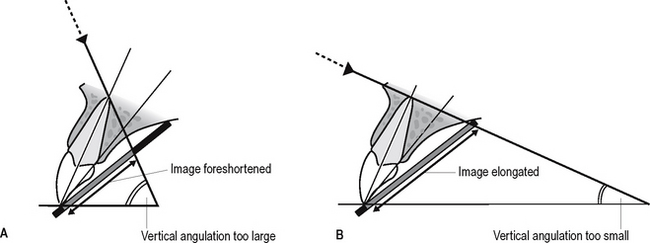
Fig. 10.22 Diagrams showing the effects of incorrect vertical tubehead positioning. A Foreshortening of the image. B Elongation of the image.
The specific positioning for different areas of the mouth, using both simple holders and the patient’s finger to support the image receptor, is shown in Figures 10.23-10.30.
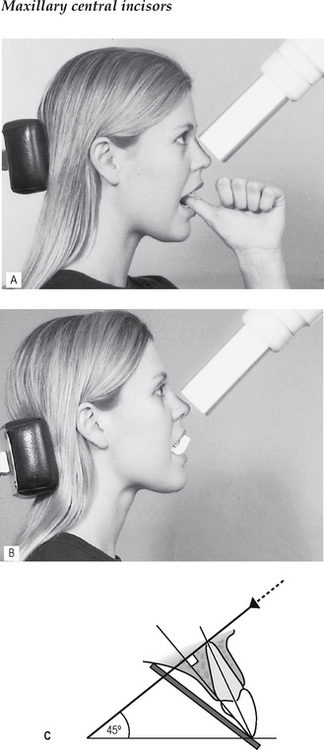
Fig. 10.23 Patient positioning with the patient A supporting the image receptor with the ball of the left thumb and B using the Rinn Greene Stabe® bite block. C Diagram of the relative positions of image receptor, incisor and X-ray beam.
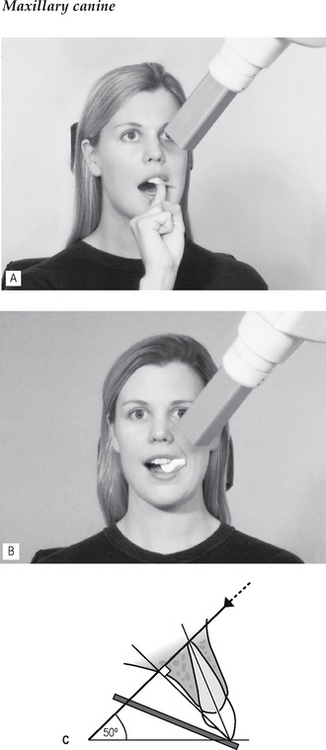
Fig. 10.24 Patient positioning with the patient A supporting image receptor with the ball of the right index finger and B using the Rinn Greene Stabe® bite block. C Diagram of the relative positions of image receptor, canine and X-ray beam.
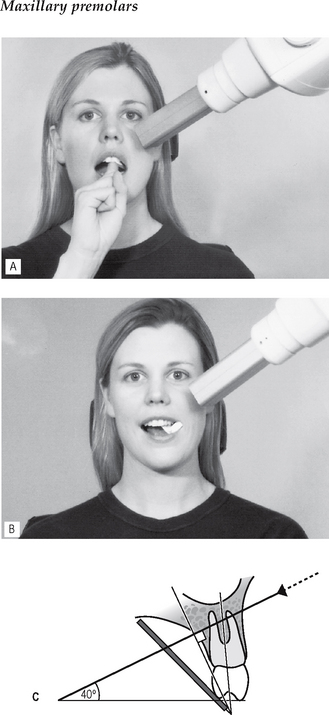
Fig. 10.25 Patient positioning with the patient A supporting the image receptor and B using the Rinn Greene Stabe® bite block. C Diagram of the relative positions of image receptor, premolar and X-ray beam.
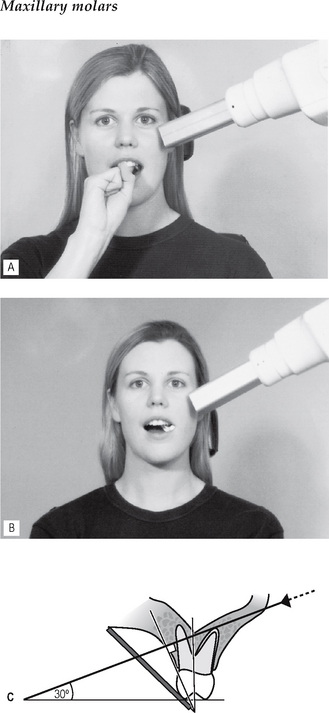
Fig. 10.26 Patient positioning with the patient A supporting the image receptor and B using the Rinn Greene Stabe® bite block. C Diagram of the relative positions of image receptor, molar and X-ray beam.
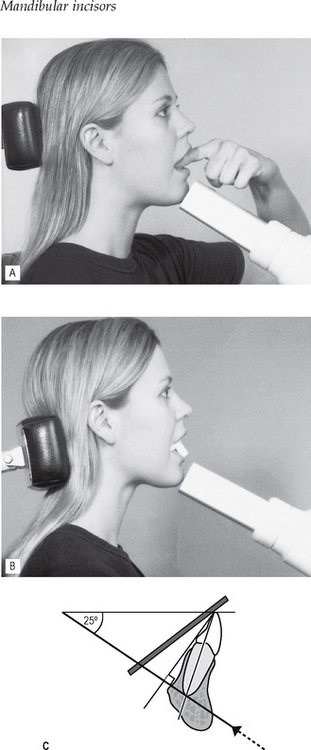
Fig. 10.27 Patient positioning with A the patient’s index finger on the upper edge of the image receptor, supporting and depressing it into the floor of the mouth and B using the Rinn Greene Stabe® bite block. C Diagram of the relative positions of image receptor, incisor and X-ray beam.
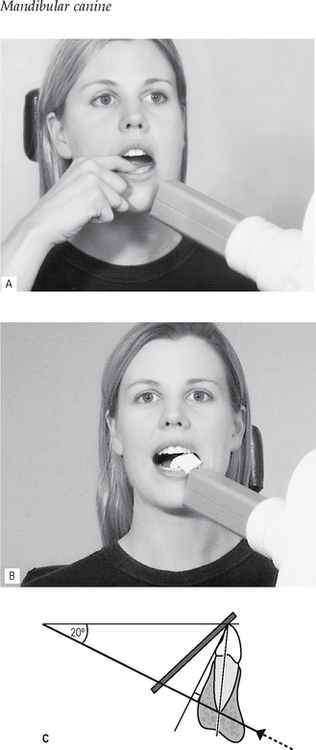
Fig. 10.28 Patient positioning with the patient A supporting and depressing the upper edge of the image receptor and B using the Rinn Greene Stabe® bite block. C Diagram of the relative positions of image receptor, canine and X-ray beam.
Comparison of the paralleling and bisected angle techniques
The advantages and disadvantages of the two techniques can be summarized as follows:
Advantages of the paralleling technique
• Geometrically accurate images are produced with little magnification.
• The shadow of the zygomatic buttress appears above the apices of the molar teeth.
• The periodontal bone levels are well represented.
• The periapical tissues are accurately shown with minimal foreshortning or elongation.
• The crowns of the teeth are well shown enabling the detection of approximal caries.
• The horizontal and vertical angulations of the X-ray tubehead are automatically determined by the positioning devices if placed correctly.
• The X-ray beam is aimed accurately at the centre of the image receptor — all areas of the image receptor are irradiated and there is no coning off or cone cutting.
• Reproducible radiographs are possible at different visits and with different operators.
• The relative positions of the image receptor, teeth and X-ray beam are always maintained, irrespective of the position of the patient’s head. This is useful for some patients with disabilities.
Disadvantages of the paralleling technique
• Positioning of the image receptor can be very uncomfortable for the patient, particularly for posterior teeth, often causing gagging.
• Positioning the holders within the mouth can be difficult for inexperienced operators particularly when using solid-state digital sensors.
• The anatomy of the mouth sometimes makes the technique impossible, e.g. a shallow, flat palate.
• The apices of the teeth can sometimes appear very near the edge of the image.
• Positioning the holders in the lower third molar regions can be very difficult.
• The technique cannot be performed satisfactorily using a short focal spot to skin distance (i.e. a short spacer cone) because of the resultant magnification.
Advantages of the bisected angle technique
• Positioning of the image receptor is reasonably comfortable for the patient in all areas of the mouth.
• Positioning is relatively simple and quick.
• If all angulations are assessed correctly, the image of the tooth will be the same length as the tooth itself and should be adequate (but not ideal) for most diagnostic purposes.
Disadvantages of the bisected angle technique
• The many variables involved in the technique often result in the image being badly distorted.
• Incorrect vertical tube head angulation will result in foreshortening or elongation of the image.
• The periodontal bone levels are poorly shown.
• The shadow of the zygomatic buttress frequently overlies the roots of the upper molars.
• The horizontal and vertical angles have to be assessed by observation for every patient and considerable skill is required.
• It is not possible to obtain reproducible views.
• Coning off or cone cutting may result if the central ray is not aimed at the centre of the image receptor, particularly if using rectangular collimation.
• Incorrect horizontal tube head angulation will result in overlapping of the crowns and roots.
• The crowns of the teeth are often distorted, thus preventing the detection of approximal caries.
• The buccal roots of the maxillary premolars and molars are foreshortened.
A visual comparison between the two techniques, showing how dramatic the variation in image quality and reproductibility can be, is shown in Figures 10.31 and 10.32.

Fig. 10.31 A Bisected angle and B paralleling technique periapical radiographs of  , on the same phantom head, taken by 12 different experienced operators. The obvious reproducibility and accurate imaging show why the paralleling technique should be regarded as the technique of choice.
, on the same phantom head, taken by 12 different experienced operators. The obvious reproducibility and accurate imaging show why the paralleling technique should be regarded as the technique of choice.
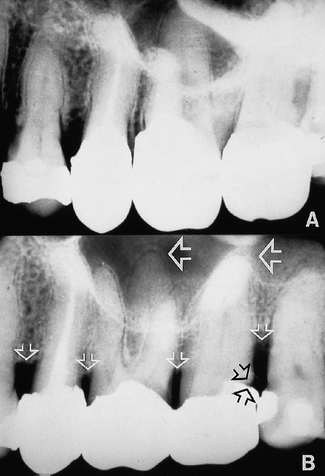
Fig. 10.32 A Bisected angle and B paralleling technique periapicals of the  taken on the same patient, by the same operator, on the same day. Note the difference in the periodontal bone levels (small white open arrows), the restoration in
taken on the same patient, by the same operator, on the same day. Note the difference in the periodontal bone levels (small white open arrows), the restoration in  (black open arrows) and the apical tissues
(black open arrows) and the apical tissues  (large white open arrows).
(large white open arrows).
Conclusion
The diagnostic advantages of the accurate, reproducible images produced by the paralleling technique using image receptor holders and beam-aiming devices ensure that this technique should be regarded as the technique of choice for periapical radiography. The 2001 Guidance Notes recommend that whenever practicable, techniques using image receptor holders with beam aiming devices should be adopted (see Ch. 8).
POSITIONING DIFFICULTIES OFTEN ENCOUNTERED IN PERIAPICAL RADIOGRAPHY
Placing the image receptor intraorally in the textbook-described positions is not always possible. The radiographic techniques described earlier often need to be modified. The main difficulties encountered involve:
• Patients with disabilities (see Ch. 9).
Problems posed by mandibular third molars
The main difficulty is placement of the image receptor sufficiently posteriorly to record the entire third mandibular molar (particularly when it is horizontally impacted) and the surrounding tissues, including the inferior dental canal (see Fig. 10.33).
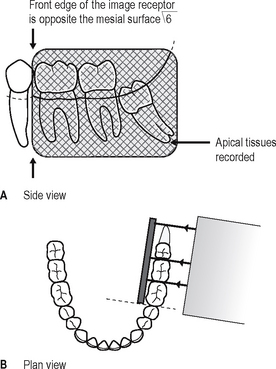
Fig. 10.33 A Side view and B plan view diagrams showing the ideal image receptor position for mandibular third molars to ensure the tooth and apical tissues are recorded.
Possible solutions
• Using specially designed or adapted holders as shown in Figure 10.34 to hold and position the image receptor in the mouth, as follows:
• Taking two radiographs of the third molar using two different horizontal tubehead angulations, as follows:
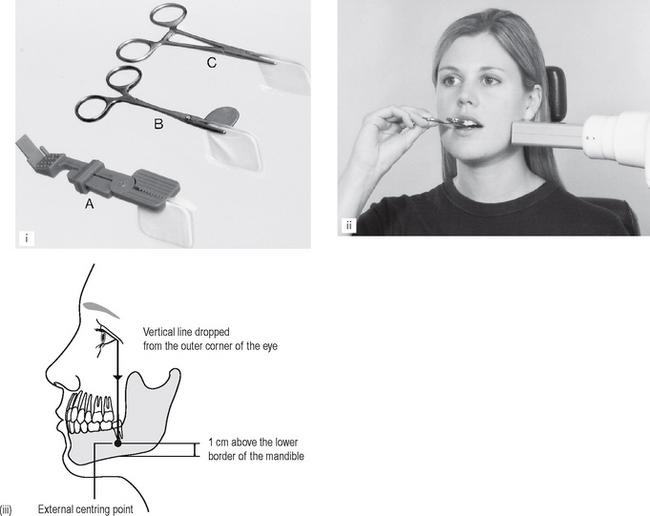
Fig. 10.34 (i) A selection of film packet/phosphor plate holders for mandibular third molars: A Emmenix® film holder. B Worth film holder and C a conventional pair of artery forceps. (ii) Patient positioning — having closed the mouth, the patient is stabilizing the image receptor holder with a hand. (iii) Diagram indicating the external centring point for the X-ray beam.
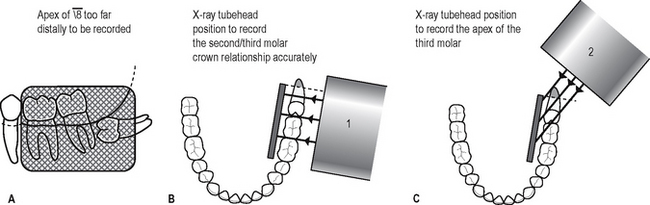
Fig. 10.35 The problem of the horizontal third molar. A Side view showing the often achievable image receptor position. B Plan view showing X-ray tubehead position 1. C Plan view showing X-ray tubehead position 2.
Note: The vertical angulation of the X-ray tubehead is the same for both projections.
Problems of gagging
The gag reflex is particularly strong in some patients. This makes the placement of the image receptor in the desired position particularly difficult, especially in the upper and lower molar regions.
Possible solutions
• Patient sucking a local anaesthetic lozenge before attempting to position the image receptor
• Asking the patient to concentrate on breathing deeply while the image receptor is in the mouth
• Placing the image receptor flat in the mouth (in the occlusal plane) so it does not touch the palate, and applying the principles of the bisected angle technique — the long axes of the tooth and image receptor are assessed by observation and the X-ray tubehead’s position modified accordingly, as shown in Figure 10.36.
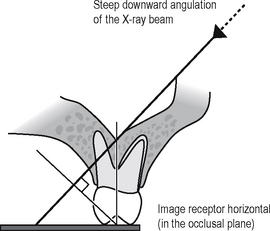
Fig. 10.36 Diagram showing the relative position of the X-ray beam to the maxillary molar and receptor, when the image receptor is placed in the occlusal plane. Note: The length of the image of the tooth on the radiograph should again equal the length of the tooth in the mouth. However, there will be considerable distortion of the surrounding tissues.
Problems encountered during endodontics
The main difficulties involve:
• Image receptor placement and stabilization when endodontic instruments, rubber dam and rubber dam clamps are in position
• Identification and separation of root canals
• Assessing root canal lengths from foreshortened or elongated radiographs.
Possible solutions
• The problem of image receptor placement and stabilization can be solved by:
• The problem of identifying and separating the root canals can be solved by taking at least two radiographs, using different horizontal X-ray tubehead positions, as shown in Figure 10.39.
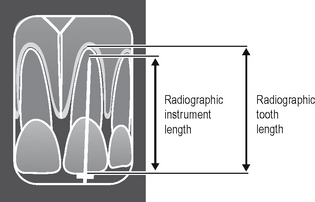
• The problems of assessing root canal length can be solved by:
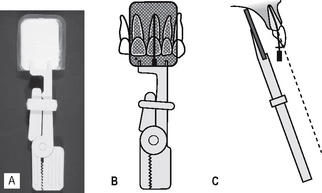
Fig. 10.37 A The Rinn Eezee–Grip® film/phosphor plate holder. B and C Diagrams showing its use in endodontics. (Note: Rubber dam not shown.)
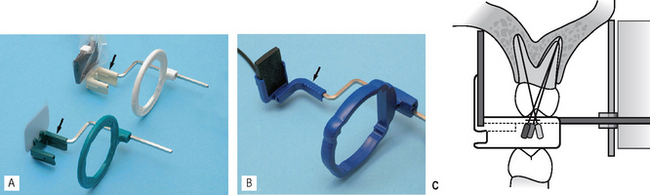
Fig. 10.38 Specially designed image receptor holders and beam aiming devices for use during endodontics A Rinn Endoray® suitable for film packets and digital phosphor plates (green) and solid-state digital sensors (white) B Anterior Planmeca solid-state digital sensor holder. Note the modified designs of the biteblocks (arrowed) to accommodate the handles of the endodontic instruments. Colour coding of instruments by some manufacturers is now used to facilitate clinical use. C Diagram of the Rinn Endoray® in place.
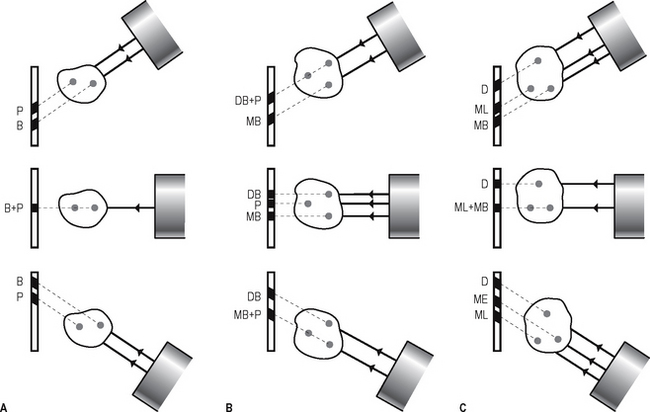
Fig. 10.39 Diagrams showing the effect of different horizontal X-ray tubehead positions on root separation for A maxillary premolars, B maxillary first molars and C mandibular first molars. (The images of the canals are designated: P = palatal, B = buccal, MB = mesiobuccal, DB = distobuccal, ML = mesiolingual and D = distal.)
The calculation is done as follows (see Fig. 10.40):
Problems of the edentulous ridge
The main difficulty in the edentulous and partially dentate patient is again image receptor placement.
Possible solutions
• In edentulous patients, the lack of height in the palate, or loss of lingual sulcus depth, contra- indicates the paralleling technique and all periapical radiographs should be taken using a modified bisected angle technique. The long axes of the image receptor and the alveolar ridge are assessed by observation and the X-ray tubehead position adjusted accordingly as shown in Figure 10.41.
• In partially dentate patients, the paralleling technique can usually be used. If the edentulous area causes the image receptor holder to be displaced, the deficiency can be built up by using cottonwool rolls, as shown in Figure 10.42.
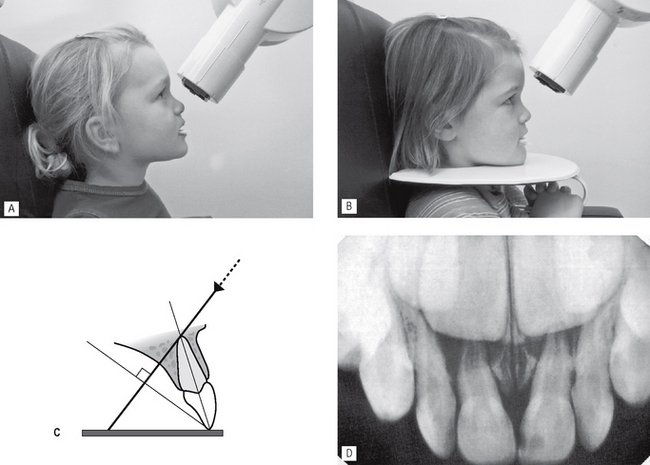
Problems encountered in children
Once again the main technical problem (as opposed to management problems) encountered in children is the size of their mouths and the difficulty in placing the image receptor intraorally. The paralleling technique is not possible in very small children, but can often be used (and is recommended) anteriorly, for investigating traumatized permanent incisors. The reproducibility afforded by this technique is invaluable for future comparative purposes.
A modified bisected angle technique is possible in most children, with the image receptor placed flat in the mouth (in the occlusal plane) and the position of the X-ray tubehead adjusted accordingly, as shown in Figure 10.43.
Assessment of image quality
Assessment of the quality of all radiographic images should be regarded as a routine part of any quality assurance (QA) programme (see Ch. 18). Essentially image quality assessment involves three separate stages, namely:
• Comparison of the image against ideal quality criteria
• Subjective rating of image quality using published standards
• Detailed assessment of rejected films to determine the sources of error.
Ideal quality criteria
Irrespective of the type of image receptor or technique being used, typical quality criteria for a periapical radiograph should include:
• The image should have acceptable definition with no distortion or blurring.
• The image should include the correct anatomical area together with the apices of the tooth/teeth under investigation with at least 3–4 mm of surrounding bone.
• There should be no overlap of the approximal surfaces of the teeth.
• The desired density and contrast for film-captured images will depend on the clinical reasons for taking the radiograph, e.g.
• The images should be free of coning off or cone-cutting and other film handling errors.
• The images should be comparable with previous periapical images both geometrically and in density and contrast.
Subjective rating of image quality
A simple three-point subjective rating scale for all intra-oral and extra-oral film-captured radiographs was published in the UK in 2001 in the Guidance Notes for Dental Practitioners on the Safe Use of X-ray Equipment. A summary is shown in Table 10.1, and is repeated in Chapters 11 and 17. Image quality is discussed in detail, together with the errors associated with exposure factors and chemical processing, in Chapter 18. Patient preparation and positioning errors in periapical radiography are described below.
Table 10.1 Subjective quality rating criteria for film-captured images published in the 2001 Guidance Notes for Dental Practitioners on the Safe Use of X-ray Equipment
| Rating | Quality | Basis |
|---|---|---|
| 1 | Excellent | No errors of patient preparation, exposure, positioning, processing or film handling |
| 2 | Diagnostically acceptable | Some errors of patient preparation, exposure, positioning, processing or film handling, but which do not detract from the diagnostic utility of the radiograph |
| 3 | Unacceptable | Errors of patient preparation, exposure, positioning, processing or film handling, which render the radiograph diagnostically unacceptable |
Assessment of rejected films and determination of errors
Patient preparation and positioning (radiographic technique) errors (Fig. 10.44)
• Failure to remove dentures or orthodontic appliances
• Failure to position the image receptor correctly to capture the area of interest, thereby failing to image the apices and periapical tissues
• Failure to position the image receptor correctly causing it to bend (if flexible) creating geometrical distortion
• Failure to orientate the image receptor correctly and using it back-to-front
• Failure to align the X-ray tubehead correctly in the horizontal plane, either
• Failure to align the X-ray tubehead correctly in the vertical plane, either
• Failure to instruct the patient to remain still during the exposure with subsequent movement resulting in blurring
• Failure to set correct exposure settings (see Ch. 18)
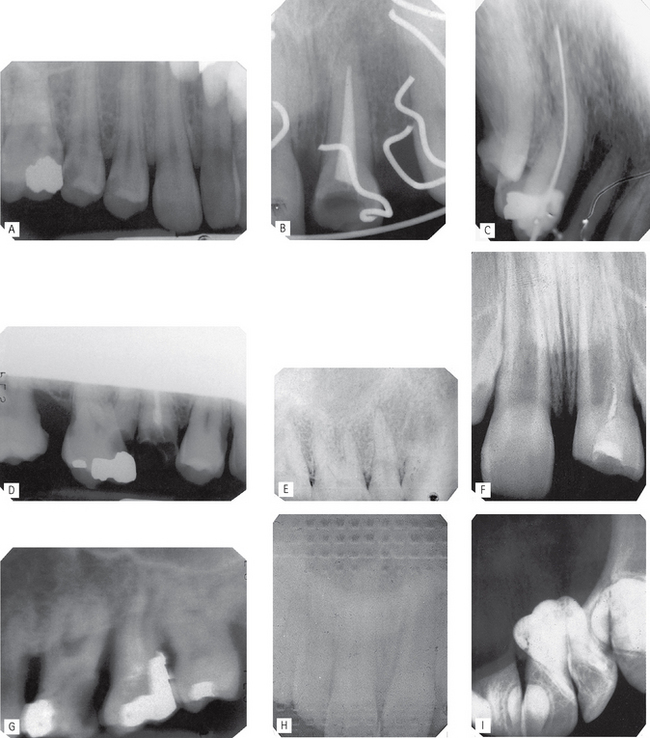
Fig. 10.44 A selection of patient preparation and positioning (radiographic technique) errors.
A Image receptor not positioned sufficiently apically to cover the area of interest — apices and periapical tissues not shown.
B Failure to remove an orthodontic appliance.
C Image receptor positioned incorrectly and bent during exposure — image geometically distorted.
D Failure to align the X-ray tubehead correctly in the vertical plane — coning off of the superior part of the image.
E X-ray tubehead positioned at too steep an angle in the vertical plane — foreshortening and geometrical distortion of the image.
F X-ray tubehead positioned at too shallow an angle in the vertical plane — elongation and geometrical distortion of the image.
G Failure to instruct the patient to remain still — image blurred as a result of movement.
H Image receptor (film packet) incorrectly placed back to front — pattern of the lead foil is evident.
I Image receptor (film packet) inadvertently used twice — double exposure.
Note: Many of these technique errors can be avoided by using the paralleling technique utilizing image receptor holders with beam-aiming devices.