Chapter 8 Radiation protection and legislation
Ionizing radiation is the subject of considerable safety legislation designed to minimize the risks to radiation workers and to patients. The International Commission on Radiological Protection (ICRP) regularly publishes data and general recommendations based on the following general principles:
• No practice shall be adopted unless its introduction produces a positive net benefit (Justification)
• All exposures shall be kept as low as reasonably practicable (ALARP), taking economic and social factors into account (Optimization)
• The dose equivalent to individuals shall not exceed the limits recommended by the ICRP (Limitation).
Their recommendations are usually incorporated eventually into national legislation and guidelines, although the precise details may vary from one country to another. By way of illustration, this chapter summarizes the current recommendations, guidelines and legislative requirements in force in the UK, together with the practical radiation protection measures that apply to patients and dental staff.
CURRENT UK LEGISLATION AND GUIDELINES
Legislation
There are two sets of regulations in the UK governing the use of ionizing radiation. They both form part of The Health and Safety at Work Act 1974 and comply with the provisions of the European Council Directives 96/29/Euratom and 97/43/Euratom:
• The Ionising Radiations Regulations 1999 (SI 1999 No. 3232) (IRR 99) which replace the Ionising Radiations Regulations 1985 (SI 1985 No. 1333).
• The Ionising Radiation (Medical Exposure) Regulations 2000 (SI 2000 No. 1059) (IR(ME) R 2000) which replace the Ionising Radiation (Protection of Persons Undergoing Medical Examination or Treatment) Regulations 1988 (SI 1988 No. 778).
Guidelines
There are three sets of guidelines, namely:
• Guidelines on Radiological Standards in Primary Dental Care published in 1994 by the National Radiological Protection Board (NRPB) and the Royal College of Radiologists. These guidelines and their recommendations cover all aspects of dental radiology and set out the principles of good practice.
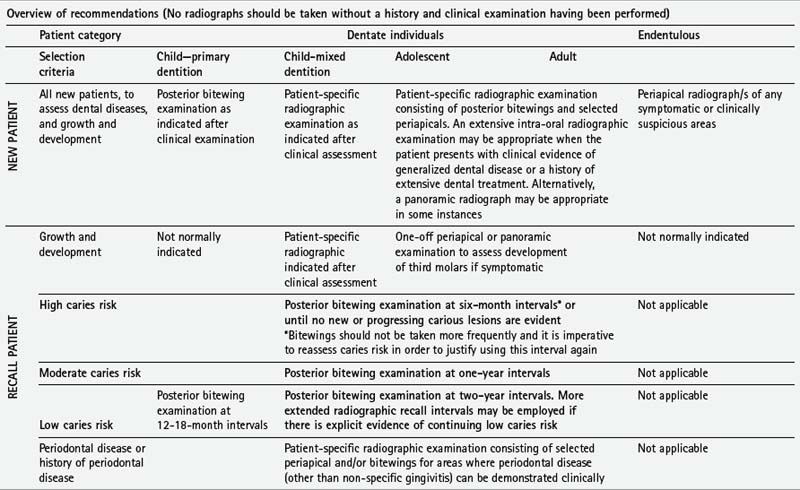
• Selection Criteria for Dental Radiography 2nd edn. published in 2004 by the Faculty of General Dental Practice (UK) of the Royal College of Surgeons of England. This booklet reviews the evidence for, and provides guidance on, which radiographs are appropriate for different clinical conditions and how frequently they should be taken. The overview of their recommendations is reproduced later in this chapter.
• Guidance Notes for Dental Practitioners on the Safe Use of X-ray Equipment published by the Department of Health in 2001 which brings together the requirements of IRR99 and IR(ME) R 2000 as they relate to dentists and includes the principles of good practice established in the 1994 Guidelines. The main points and various extracts from these 2001 Guidance Notes are reproduced below with kind permission from the Radiation Protection Division of the Health Protection Agency (formerly the National Radiological Protection Board (NRPB)).
NOTE: These points are not intended to cover all aspects of the guidance notes and legislation. The various publications mentioned above, particularly the 2001 Guidance Notes and the 2004 Selection Criteria, should be regarded as essential reading for all members of the dental profession, whether in general practice, dental hospitals or community clinics.
SUMMARY OF THE LEGISLATION AND EXTRACTS FROM THE 2001 GUIDANCE NOTES FOR DENTAL PRACTITIONERS ON THE SAFE USE OF X-RAY EQUIPMENT
Ionising Radiations Regulations 1999 (IRR99)
Essential legal requirements
• Authorization. Use of dental X-ray equipment for research purposes should be in accordance with a generic authorization granted by the Health and Safety Executive (HSE).
• Notification. The HSE must be notified of the routine use of dental X-ray equipment and of any material changes to a notification including a change in ownership of the practice or a move to new premises.
• Prior risk assessment. This must be undertaken before work commences and be subject to regular review. All employers are recommended to record the findings of their risk assessment, but it is a requirement for employers with five or more employees. A five-step approach is recommended by the HSE:
• Restriction of exposure. There is an over-riding requirement to restrict radiation doses to staff and other persons to as low as reasonably practicable (ALARP) (see later).
• Maintenance and examination of engineering controls. Applies particularly to safety and warning features of dental X-ray equipment.
• Contingency plans. These should arise out of the risk assessment and be provided within the Local Rules (see later).
• Radiation Protection Adviser (RPA). A suitably trained RPA must be appointed in writing and consulted to give advice on IRR99. The RPA should be an expert in radiation protection and will be able to advise on compliance with the Regulations and all aspects of radiation protection, including advice on:
• Information, instruction and training. Must be provided, as appropriate, for all persons associated with dental radiology.
• Designated areas. During an exposure, a controlled area will normally be designated around the X-ray set as an aid to the effective control of exposures. The controlled area may be defined as within the primary X-ray beam until it has been sufficiently attenuated by distance or shielding and within 1.5 m of the X-ray tube and the patient, as shown in Figure 8.1. Normally, only the patient is allowed in this area. This can be facilitated by the use of appropriate signs, as shown in Figure 8.2.
• Radiation Protection Supervisor (RPS). An RPS—usually a dentist or senior member of staff in the practice—should be appointed to ensure compliance with IRR99 and the Local Rules. The RPS must be adequately trained, should be closely involved with the radiography and have the authority to adequately implement their responsibilities.
• Local Rules. All practices should have a written set of Local Rules relating to radiation protection measures within that practice and applying to all employees. Information should include:
• Classified persons. Division of staff into classified and non-classified workers and the dose limits that apply to each group are discussed later. In dental practice, most staff are non-classified unless their radiography workload is very high.
• Duties of manufacturers. The installer is responsible for the critical examination and report of all new or significantly modified X-ray equipment, which should include:
• X-ray equipment. All equipment must be critically examined and acceptance tested before being put into clinical use and then routinely tested as part of a QA programme (see Ch. 18). The acceptance test, in addition to the features covered in the critical examination outlined above, should include:
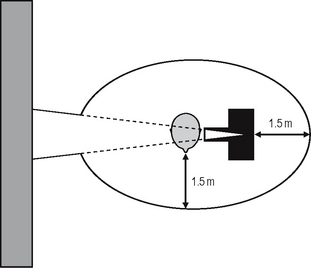
Fig. 8.1 Diagram showing the size of the controlled area, 1.5 m in any direction from the patient and tubehead and anywhere in the line of the main beam until it is attenuated by a solid wall.
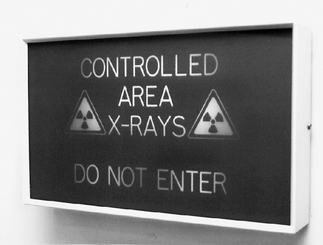
Fig. 8.2 An example of a controlled area warning sign. The words DO NOT ENTER are illuminated when the exposure button is pressed.
A permanent record should be made of the results and conclusions of all tests and this should be retained as part of the QA programme and all deficiencies should be rectified.
All equipment (X-ray generating and image receptors) should comply with the general requirements in the regulations namely:
* Panoramic radiography (see Ch. 17)
* Cephalometric radiography (see Ch. 15)
• Duties of employees. Notwithstanding the many and varied responsibilities placed on the person legally responsible, the so-called legal person, IRR99 places over-riding responsibilities on employees which include:
Ionising Radiation (Medical Exposure) Regulations 2000 (IR(ME)R 2000)
General points
Essential legal requirements
• Duties of employers. The employer (legal person) is the person or body corporate with natural or legal responsibility for a radiological installation. He/she is responsible for providing the overall safety of the practice and for ensuring that staff and procedures conform with the regulations. In addition, the legal person must provide a framework of written procedures for medical exposures which should include information on:
It is recommended that these employers written procedures and the Local Rules (see earlier) are kept together as a radiation protection file and that all staff are made aware of the contents.
• Duties of the Practitioner, Operator and Referrer.
The operator must be adequately trained for his/her role in the exposure (see later).
• Justification of individual medical exposures. Before an exposure can take place, it must be justified (i.e. assessed to ensure that it will lead to a change in the patient’s management and prognosis) by an IRMER practitioner and authorized as the means of demonstrating that it has been justified. Every exposure should be justified on the grounds of:
Note: The 2004 Selection Criteria in Dental Radiography (see later) states that there can be no possible justification for routine radiography of ‘new’ patients prior to clinical examination. A history and clinical examination are the only acceptable means of determining that the most appropriate, or necessary, radiographic views are requested.
• Optimization. All doses must be kept as low as reasonably practicable (ALARP) consistent with the intended purpose. This includes the need to apply QA procedures to the optimization of patient dose (see Ch. 18).
• Clinical audit. Provisions must be made for clinical audit. Suitable topics could include the various aspects of the QA programme (see Ch. 18), the appropriateness of radiographic requests and the clinical evaluation of radiographs.
• Expert advice. The regulations lay down the need for, and involvement of a Medical Physics Expert (MPE) who would give advice on such matters as the measurement and optimization of patient dose. However, the need for medical physics support in dental practice is fairly limited and in most cases the RPA should be able to act as the MPE.
• Equipment. The keeping and maintenance of an up-to-date inventory of each item of equipment is required and should include:
• Adequate training and continuing education. Operators and practitioners must have received adequate training and must undertake continuing education and training after qualification. The nature of this training is then specified in the Guidance Notes:
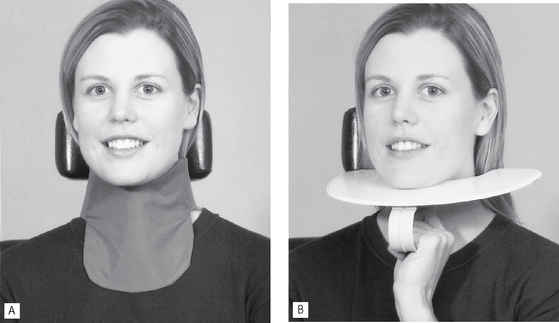
Fig. 8.3 Examples of thyroid lead protection. ALead collar (0.5mm Pb equivalent). BHand-held neck shield (0.5mm Pb equivalent).
Specific requirements for women of childbearing age.
The developing fetus is most susceptible to the dangers of ionizing radiation during the period of organogenesis (2–9 weeks) — often before the woman knows that she is pregnant. IR(ME)R 2000 prohibits the carrying out of a medical exposure of a female of childbearing age without an enquiry as to whether she is pregnant if the primary beam is likely to irradiate the pelvic area. This is highly unlikely in dental radiography. Even so, it is recommended, essentially for psychological reasons, that the operator should enquire of all women of childbearing age whether they are pregnant or likely to be pregnant. If the answer is yes, then, in addition to the routine protective measures appropriate for all patients, the following specific points should be considered:
DOSE LIMITATION AND ANNUAL DOSE LIMITS
For the purposes of dose limitation, the ICRP has divided the population into three groups:
Patients
Radiographic investigations involving patients are divided into four subgroups:
• Examinations directly associated with illness
• Systematic examinations (periodic health checks)
• Examinations for occupational, medicolegal or insurance purposes
Examinations directly associated with illness
• There are no set dose limits.
• The decision to carry out such an investigation should be based on:
• The number, type and frequency of the radiographs requested or taken (selection criteria) are the responsibility of the clinician. Selection criteria recommendations have been published in different countries in recent years to provide guidance in this clinical area of radiation protection. In the UK, the Selection Criteria in Dental Radiography 2nd Ed booklet was published in 2004 by the Faculty of General Dental Practice of the Royal College of Surgeons of England and, as stated earlier, should be regarded as essential reading for all dentists. The expert group responsible for this document reviewed the available scientific evidence to formulate evidence-based recommendations as far as was possible. In some areas, where scientific evidence was lacking, their recommendations were based on expert clinical opinion. The overview of their recommendations are reproduced in Table 8.1 together with a summary Table in Chapter 21.
Systematic examinations (periodic health checks)
• There are no set dose limits.
• There should be a high probability of obtaining useful information—see Selection Criteria recommendations in Table 8.1.
• The information obtained should be important to the patient’s health.
Examinations for occupational, medicolegal or insurance purposes
• There are no set dose limits.
• The benefit is primarily to a third party.
• The patient should at least benefit indirectly.
• The 2001 Guidance Notes emphasize that the need for, and the usefulness of, these examinations should be critically examined when assessing whether they are justified. They also recommend that these types of examinations should only be requested by medical/dental practitioners and that the patient’s consent should be obtained.
Radiation workers
Radiation workers are those people who are exposed to radiation during the course of their work. This exposure carries no benefit only risk. The ICRP further divides these workers into two subgroups depending on the level of occupational exposure:
The ICRP sets maximum dose limits for each group, based on the principle that the risk to any worker who receives the full dose limit, will be such that the worker will be at no greater risk than a worker in another hazardous, but non-radioactive, environment. The annual dose limits have been revised under the Ionising Radiations Regulations 1999 and these are shown in Table 8.2.
Table 8.2 The previous annual dose limits and those currently in force under the Ionising Radiations Regulations 1999
| Old dose limits | New dose limits (IRR99) | |
|---|---|---|
| Classified workers | 50 mSv | 20 mSv |
| Non-classified workers | 15 mSv | 6 mSv |
| General public | 5 mSv | 1 mSv |
The main features of each group of radiation workers are summarized below:
Non-classified workers (most dental staff)
• Receive low levels of exposure to radiation at work (as in the dental surgery).
• The annual dose limits are 3/10 of the classified workers’ limits. Provided the Local Rules are observed, all dental staff should receive an annual effective dose of considerably less than the limit of 6mSv. Hence, the regulations suggest the setting of ‘Dose Constraints’. These represent the upper level of individual dose that should not be exceeded in a well-managed practice and for dental radiography the following recommendations are made:
| 1 mSv | for employees directly involved with the radiography (operators) |
| 0.3 mSv | for employees not directly involved with the radiography and for members of the general public. |
In addition to the above dose limits, the legal person must ensure that the dose to the fetus of any pregnant member of staff is unlikely to exceed 1mSv during the declared term of the pregnancy.
• Personal monitoring (see later) is not compulsory, although it is recommended if the risk assessment indicates that individual doses could exceed 1mSv per year. The 2001 Guidance Notes state that in practice this should be considered for those staff whose weekly workload exceeds 100 intraoral or 50 panoramic films, or a pro-rata combination of each type of examination.
The radiation dose to dentists and their staff can come from:
The main protective measures to limit the dose that workers might receive are therefore based mainly on a combination of common sense and the knowledge that ionizing radiation is attenuated by distance and obeys the inverse square law (see Fig. 8.4).
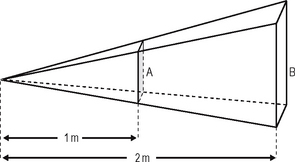
Fig. 8.4 Diagrammatic representation of the inverse square law. Doubling the distance from the source means that the area of B is four times the area of A, thus the radiation per unit area at B is one quarter that at A.
The main dose limitation measures relate to:
• Distance from the source of radiation—staff should stand outside the controlled area (see Fig. 8.1) and not in the line of the primary beam. If these positions cannot be obtained, appropriate lead screens/barriers should be used
• Safe use of equipment—as summarized in the 2001 Guidance Notes
• Radiographic technique—staff should be adequately trained and follow the recommendations summarized in the 2001 Guidance Notes
General public
This group includes everyone who is not receiving a radiation dose either as a patient or as a radiation worker, but who may be exposed inadvertently, for example, someone in a dental surgery waiting room, in other rooms in the building or passers-by. The annual dose limits for this group have been lowered to 1 mSv, as shown in Table 8.2 although the suggested ‘Dose Constraint’ is 0.3 mSv (see earlier). The general public are at risk from the primary beam, so specific consideration should be given to:
• The siting of X-ray equipment to ensure that the primary beam is not aimed directly into occupied rooms or corridors
• The thickness/material of partitioning walls
• Advice from the RPA (see 1999 Regulations) on the siting of all X-ray equipment, surgery design and the placement of radiation warning signs.
MAIN METHODS OF MONITORING AND MEASURING RADIATION DOSE
There are three main devices (shown in Fig. 8.5), for monitoring and measuring radiation dose:
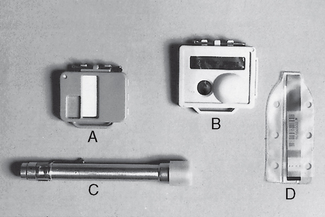
Fig. 8.5 Monitoring devices. APersonal monitoring film badge. BPersonal monitoring TLD badge. CIonization bleeper. DTLD extremity monitor.
Film badges
The main features of film badges are:
• They consist of a blue plastic frame containing a variety of different metal filters and a small radiographic film which reacts to radiation
• They are worn on the outside of the clothes, usually at the level of the reproductive organs, for 1–3 months before being processed
• They are the most common form of personal monitoring device currently in use.
Thermoluminescent dosemeters
The main features of TLDs are:
• They are used for personal monitoring of the whole body and/or the extremities, as well as measuring the skin dose from particular investigations
• They contain materials such as lithium fluoride (LiF) which absorb radiation and then release the energy in the form of light when heated
• The intensity of the emitted light is proportional to the radiation energy absorbed originally
• Personal monitors consist of a yellow or orange plastic holder, worn like the film badge for 1–3 months.
Ionization chambers
The main features of ionization chambers are:
• They are used for personal monitoring (thimble chamber) and by physicists (free-air chamber) to measure radiation exposure
• Radiation produces ionization of the air molecules inside the closed chamber, which results in a measurable discharge and hence a direct read-out