Chapter 22 The periapical tissues
INTRODUCTION
This chapter explains how to interpret the radiographic appearances of the periapical tissues by illustrating the various normal appearances, and describing in detail the typical changes associated with apical infection and inflammation following pulpal necrosis. To help explain the different radiographic appearances, they are correlated with the various underlying pathological processes. In addition, there is a summary of the other, sometimes sinister, lesions that can affect the periapical tissues and may simulate simple inflammatory changes.
NORMAL RADIOGRAPHIC APPEARANCES
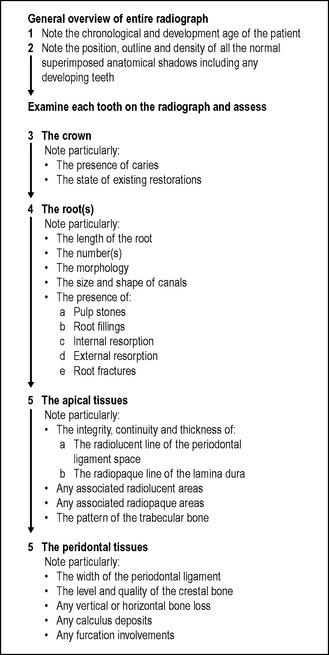
A reminder of the complex three-dimensional anatomy of the hard tissues surrounding the teeth in the maxilla and mandible, which contribute to the two-dimensional periapical radiographic image, is given in Figure 22.1.
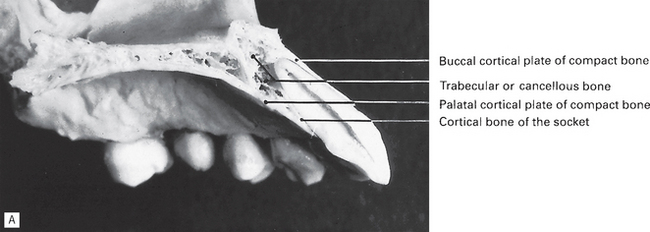
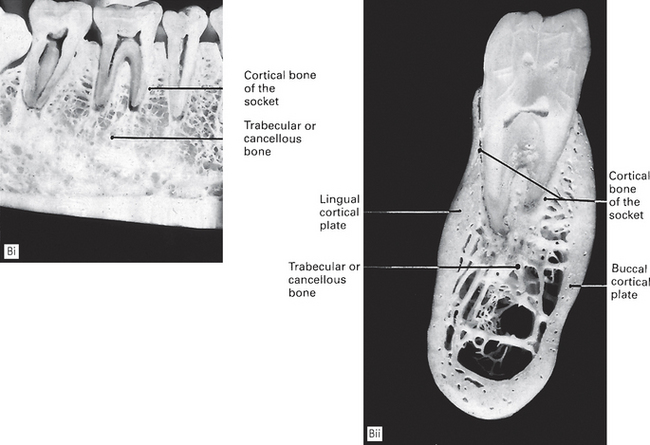
Fig. 22.1A Sagittal section through the maxilla and central incisor showing the hard tissue anatomy.
Fig. 22.1B (i) Sagittal and (ii) coronal sections through the mandible in the molar region showing the hard tissue anatomy.
The appearances of normal, healthy, periapical tissues vary from one patient to another, from one area of the mouth to another and at different stages in the development of the dentition. These different normal appearances are described below.
The periapical tissues of permanent teeth (Fig. 22.2)
The three most important features to observe are:
• The radiolucent line that represents the periodontal ligament space and forms a thin continuous black line around the root outline
• The radiopaque line that represents the lamina dura of the bony socket and forms a thin, continuous, white line adjacent to the black line
• The trabecular pattern and density of the surrounding bone:
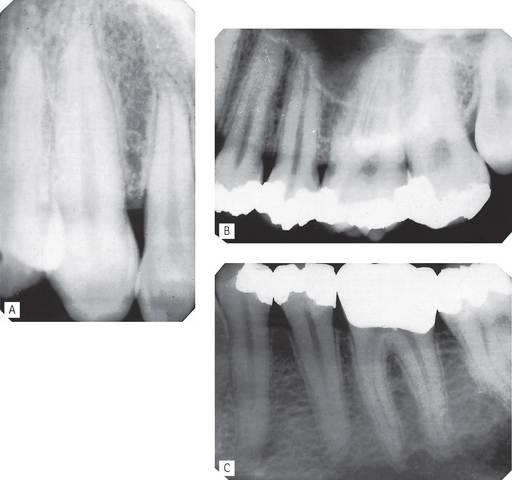
Fig. 22.2 Periapical radiographs of A  , B
, B  , C
, C  showing the normal radiographic anatomy of the periapical tissues in different parts of the jaws. Note the continuous radiolucent line of the periodontal ligament shadow and the radiopaque line of the lamina dura outlining the roots.
showing the normal radiographic anatomy of the periapical tissues in different parts of the jaws. Note the continuous radiolucent line of the periodontal ligament shadow and the radiopaque line of the lamina dura outlining the roots.
These features hold the key to the interpretation of periapical radiographs, since changes in their thickness, continuity and radiodensity reflect the presence of any underlying disease, as described later.
Important points to note
• There is considerable variation in the definition and pattern of these features from one patient to another and from one area of the jaws to another, owing to variation in the density, shape and thickness of the surrounding bone.
• The limitations imposed by contrast, resolution and superimposition can make radiographic identification of these features particularly difficult, hence the need for ideal viewing conditions and digital image enhancement software.
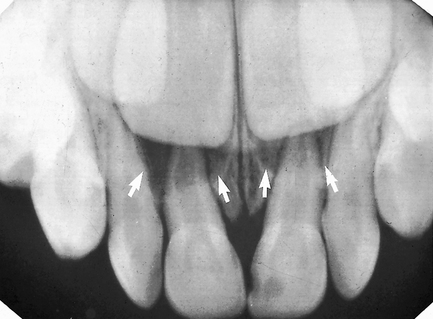
The periapical tissues of deciduous teeth (Fig. 22.3)
The important features of normality (thin lamina dura and periodontal ligament shadows) are the same as for permanent teeth, but can be complicated by:
The periapical tissues of developing teeth (Fig. 22.4)
The important features of normal apical tissues, where the root is partially formed and the radicular papilla still exists, include:
The effects of normal superimposed shadows
Normal anatomical shadows superimposed on the apical tissues can be either radiolucent or radiopaque, depending on the structure involved.
Radiolucent shadows
Such cavities in the alveolar bone decrease the total amount of bone that would normally contribute to the final radiographic image, with the following effects:
• The radiolucent line of the periodontal ligament may appear MORE radiolucent or widened, but will still be continuous and well demarcated
• The radiopaque line of the lamina dura may appear LESS obvious and may not be visible
• There will be an area of radiolucency in the alveolar bone at the tooth apex (see Figs 22.5 and 22.6).
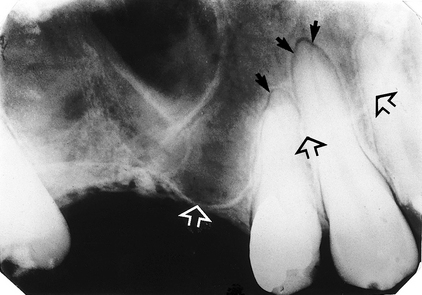
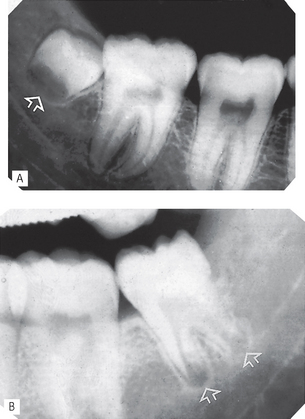
Fig. 22.5 Periapical of  showing normal healthy apical tissues but with the radiolucent shadow of the antrum superimposed (the antral floor is indicated by the open arrows). As a result the radiolucent line of the periodontal ligament appears widened and more obvious around the apices of the canine and premolar, but it is still well demarcated, while the radiopaque line of the lamina dura is almost invisible (solid arrows).
showing normal healthy apical tissues but with the radiolucent shadow of the antrum superimposed (the antral floor is indicated by the open arrows). As a result the radiolucent line of the periodontal ligament appears widened and more obvious around the apices of the canine and premolar, but it is still well demarcated, while the radiopaque line of the lamina dura is almost invisible (solid arrows).
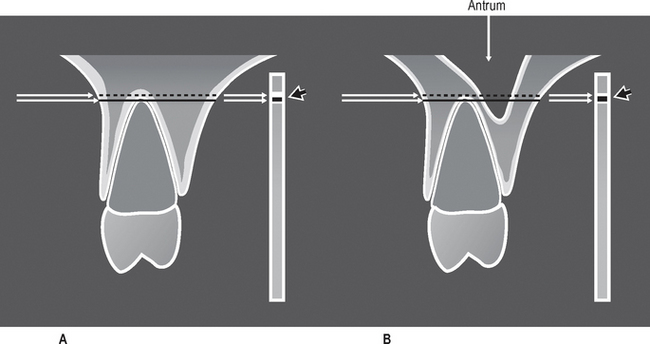
Fig. 22.6 Diagrams of  showing the anatomical tissues that the X-ray beam passes through to reach the film. A Without a normal anatomical cavity superimposed. B With the antral cavity in the path of the X-ray beam. The different resultant radiopaque (white) and radiolucent (black) lines of the apical lamina dura and periodontal ligament are shown on the film (arrowed).
showing the anatomical tissues that the X-ray beam passes through to reach the film. A Without a normal anatomical cavity superimposed. B With the antral cavity in the path of the X-ray beam. The different resultant radiopaque (white) and radiolucent (black) lines of the apical lamina dura and periodontal ligament are shown on the film (arrowed).
Important points to note
• The fact that the radiopaque lamina dura shadow may not be visible does not mean that the bony socket margin is not present clinically. It only means that there is now not enough total bone in the path of the X-ray beam to produce a visible opaque shadow. Since the bony socket is in fact intact, it still defines the periodontal ligament space. Thus, the radiolucent line representing this space still appears continuous and well demarcated.
• Although confusing, this effect of normal anatomical radiolucent shadows on the apical tissues is very important to appreciate, so as not to mistake a normal area of radiolucency at the apex for a pathological lesion.
Radiopaque shadows
Such radiopacities complicate periapical interpretation by obscuring or obliterating the detailed shadows of the apical tissues, as shown in Figure 22.7.
RADIOGRAPHIC APPEARANCES OF PERIAPICAL INFLAMMATORY CHANGES
Types of inflammatory changes
Following pulpal necrosis, either an acute or chronic inflammatory response is initiated in the apical tissues. The inflammatory response is identical to that set up elsewhere in the body from other toxic stimuli, and exhibits the same signs and symptoms.
Cardinal signs of acute inflammation
In the apical tissues, inflammatory exudate accumulates in the apical periodontal ligament space (swelling), setting up an acute apical periodontitis. The affected tooth becomes periostitic or tender to pressure (pain), and the patient avoids biting on the tooth (loss of function). Heat and redness are clinically undetectable. These signs are accompanied by destruction and resorption, often of the tooth root, and of the surrounding bone, as a periapical abscess develops, and radiographically a periapical radiolucent area becomes evident.
Hallmarks of chronic inflammation
These include the processes of destruction and healing which are going on simultaneously, as the body’s defence systems respond to, and try to confine, the spread of the infection. In the apical tissues, a periapical granuloma forms at the apex and dense bone is laid down around the area of resorption. Radiographically, the apical radiolucent area becomes circumscribed and surrounded by dense sclerotic bone. Occasionally, under these conditions of chronic inflammation, the epithelial cell rests of Malassez are stimulated to proliferate and form an inflammatory periapical radicular cyst (see Ch. 27) or there is an acute exacerbation producing another abscess (the so-called phoenix abscess).
The type and progress of the inflammatory response at the apex and the subsequent spread of apical infection is dependent on several factors relating to:
The result is a wide spectrum of events ranging from a very rapidly spreading acute periapical abscess to a very slowly progressing chronic periapical granuloma or cyst. This variation in the underlying disease processes is mirrored radiographically, although it is often not possible to differentiate between an abscess, granuloma or cyst.
A summary of the different inflammatory effects and the resultant radiographic appearances is shown in Table 22.1. The effects are shown diagrammatically in Figure 22.8. Various examples are shown in Figures 22.9-22.12.
Table 22.1 Summary of the effects of different inflammatory processes on the periapical tissues and the resultant radiographic appearances
| State of inflammation | Underlying inflammatory changes | Radiographic appearances |
|---|---|---|
| Initial acute inflammation | Inflammatory exudate accumulates in the apical periodontal ligament space | Widening of the radiolucent line of the periodontal ligament space |
| — acute apical periodontitis | OR | |
| No apparent changes evident | ||
| Initial spread of inflammation | Resorption and destruction of the apical bony socket — periapical abscess | Loss of the radiopaque line of the lamina dura at the apex |
| Further spread of inflammation | Further resorption and destruction of the apical alveolar bone | Area of bone loss at the tooth apex |
| Initial low-grade chronic inflammation | Minimal destruction of the apical bone | No apparent bone destruction but dense sclerotic bone evident around the tooth apex (sclerosing osteitis) |
| The body’s defence systems lay down dense bone in the apical region | ||
| Latter stages of chronic inflammation | Apical bone is resorbed and destroyed and dense bone is laid down around the area of resorption — periapical granuloma or radicular cyst | Circumscribed, well-defined radiolucent area of bone loss at the apex, surrounded by dense sclerotic bone |
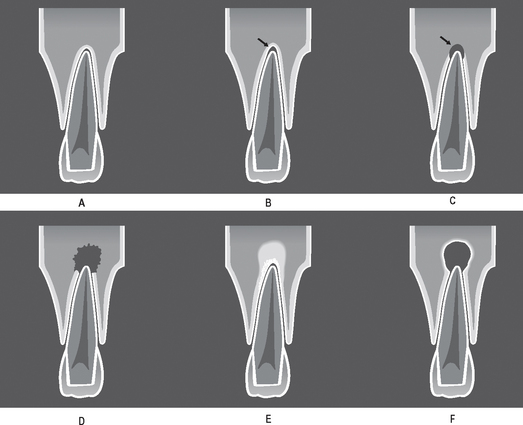
Fig. 22.8 Diagrams showing the various radiographic appearances of infection and inflammation in the apical tissues. A Normal. B Early apical change — widening of the radiolucent periodontal ligament space (acute apical periodontitis) (arrowed). C Early apical change — loss of the radiopaque lamina dura (early periapical abscess) (arrowed). D Extensive destructive acute inflammation — diffuse, ill-defined area of radiolucency at the apex (periapical abscess). E Low grade chronic inflammation — diffuse radiopaque area at the apex (sclerosing osteitis). F Longstanding chronic inflammation — well-defined area of radiolucency surrounded by dense sclerotic bone (periapical granuloma or radicular cyst).
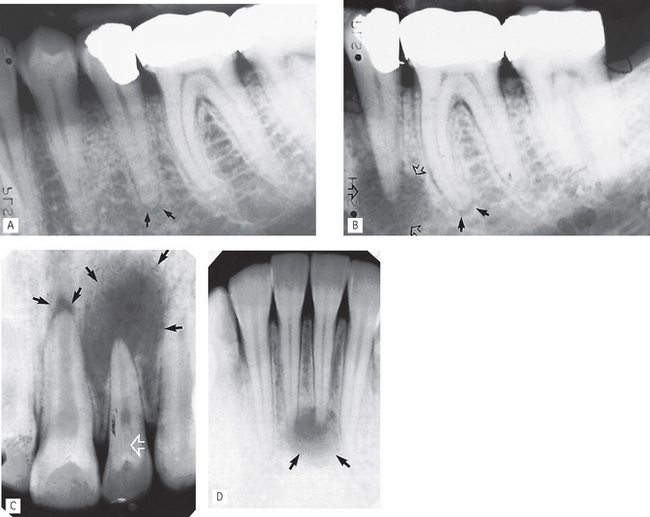
Fig. 22.9 Periapicals showing examples of inflammatory changes in the periapical tissues. A Early apical change on  showing widening of the periodontal ligament space and thinning of the lamina dura (acute apical periodontitis) (arrowed). B Same patient 6 months later — the area of bone destruction at the apex
showing widening of the periodontal ligament space and thinning of the lamina dura (acute apical periodontitis) (arrowed). B Same patient 6 months later — the area of bone destruction at the apex  has increased considerably (open arrows) and there is now early apical change associated with the mesial root
has increased considerably (open arrows) and there is now early apical change associated with the mesial root  (solid arrows). C Large, diffuse area of bone destruction associated with
(solid arrows). C Large, diffuse area of bone destruction associated with  and a smaller area associated with
and a smaller area associated with  (black arrows) (periapical abscess).
(black arrows) (periapical abscess).  shows evidence of a dens-in-dente (invaginated odontome) (open white arrow). D Reasonably well-defined area of bone destruction (arrowed) associated with
shows evidence of a dens-in-dente (invaginated odontome) (open white arrow). D Reasonably well-defined area of bone destruction (arrowed) associated with  (periapical abscess, granuloma or cyst).
(periapical abscess, granuloma or cyst).
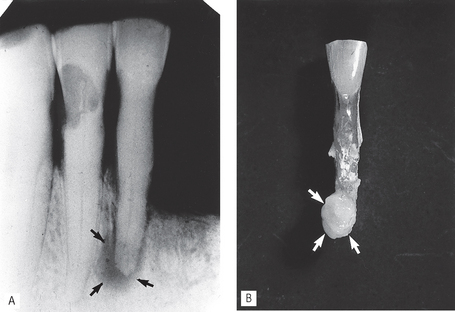
Fig. 22.10A Periapical showing a well-defined area of radiolucency at the apex of  (arrowed). The surrounding bone is relatively dense and opaque suggesting a chronic periapical granuloma or radicular cyst. B The extracted
(arrowed). The surrounding bone is relatively dense and opaque suggesting a chronic periapical granuloma or radicular cyst. B The extracted  , showing the granuloma attached to the root apex (arrowed).
, showing the granuloma attached to the root apex (arrowed).
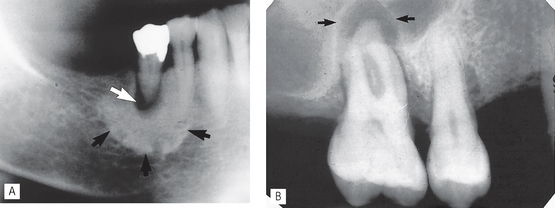
Fig. 22.11 Radiographic examples of other chronic inflammatory changes in the periapical tissues. A Long-standing low grade chronic infection associated with  resulting in a radiolucent periapical granuloma or radicular cyst (white arrow), surrounded by florid opaque sclerosing osteitis (black arrow). B Well-defined area of bone destruction associated with
resulting in a radiolucent periapical granuloma or radicular cyst (white arrow), surrounded by florid opaque sclerosing osteitis (black arrow). B Well-defined area of bone destruction associated with  which has resulted in remodelling of the antral floor, producing the so-called antral halo appearance (black arrow) (see also Fig. 29.6C).
which has resulted in remodelling of the antral floor, producing the so-called antral halo appearance (black arrow) (see also Fig. 29.6C).
Treatment and radiographic follow-up
Most inflammatory periapical lesions are treated by conventional endodontic treatment. The Faculty of General Dental Practice (UK)’s 2004 booklet Selection Criteria in Dental Radiography, 2nd edn, recommends:
• A good quality pre-operative radiograph
• At least one good quality radiograph to determine working length
• A mid-fill radiograph if there is any doubt about the apical constriction
• A postoperative radiograph to assess success of the obturation and to act as a baseline for assessment of apical disease or healing
• A further follow-up radiograph after one year following completion of treatment (see Fig. 22.13), even for asymptomatic teeth and large periapical radiolucencies should be monitored more frequently.
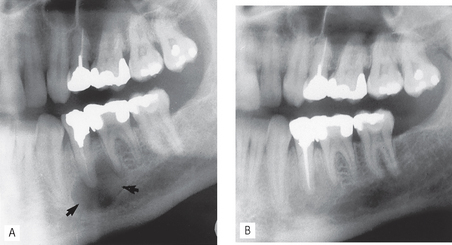
Fig. 22.13A Part of a panoramic radiograph showing a round, well-defined area of radiolucency — a likely radicular cyst (arrowed), associated with the poorly root-filled  . B Same patient 12 months later following successful root filling at
. B Same patient 12 months later following successful root filling at  . Note the bony fill-in in the apical area.
. Note the bony fill-in in the apical area.
If endodontic therapy is clinically unsuccessful, subsequent treatment involves either:
OTHER IMPORTANT CAUSES OF PERIAPICAL RADIOLUCENCY
Many of the conditions described in Chapters 27 and 28 can present occasionally in the apical region of the alveolar bone. Some can simulate the simple inflammatory changes described above including:
• Benign and malignant bone tumours including secondary metastatic deposits (see Fig. 22.14)
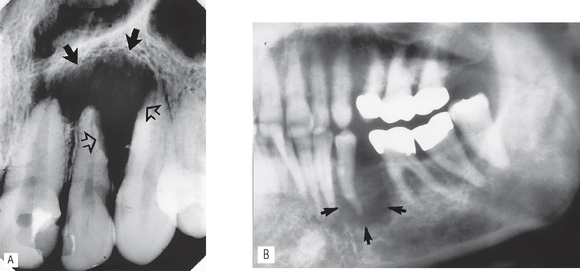
Fig. 22.14A Periapical showing a poorly defined area of radiolucency in the apical region of  . Features of concern are the ragged bone margin (solid arrows) and the extensive resorption of
. Features of concern are the ragged bone margin (solid arrows) and the extensive resorption of  and
and  (open arrows). Initial treatment involved unsuccessful root treatment of
(open arrows). Initial treatment involved unsuccessful root treatment of  . Biopsy revealed an osteosarcoma. B Part of a panoramic radiograph showing a large poorly defined area of radiolucency in
. Biopsy revealed an osteosarcoma. B Part of a panoramic radiograph showing a large poorly defined area of radiolucency in  region (arrowed). Both premolars were caries-free and unrestored, but mobile.
region (arrowed). Both premolars were caries-free and unrestored, but mobile.  was extracted and histopathology revealed a secondary metastatic malignant tumour from a breast primary.
was extracted and histopathology revealed a secondary metastatic malignant tumour from a breast primary.
Although it is uncommon, clinicians should still be alert to the possibility that malignant lesions can present as apparently simple localized areas of infection. The signs of concern include:
SUGGESTED GUIDELINES FOR INTERPRETING PERIAPICAL IMAGES
Although somewhat repetitive, this methodical approach to radiographic interpretation is so important, and so often ignored, that it is described again.
Overall critical assessment
A typical series of questions that should be asked about the quality of a periapical radiographic image based on the ideal quality criteria described in Chapter 10 include:
Technique (film OR digitally-captured images)
Systematic viewing
A systematic approach to viewing periapical radiographs is shown in Figure 22.15. This approach ensures that all areas of the film are observed and that the important features of the tooth apex are examined.
 , B
, B  . Note the circumscribed areas of radiolucency of the radicular papillae (arrowed) and the funnel-shaped roots.
. Note the circumscribed areas of radiolucency of the radicular papillae (arrowed) and the funnel-shaped roots.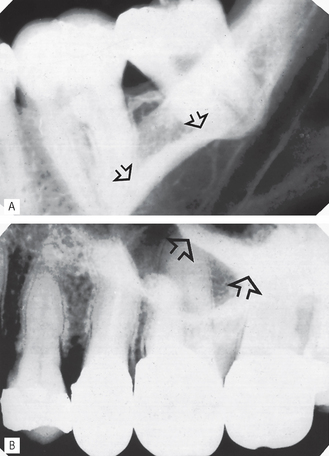
 showing the radiopaque line of the mylohyoid ridge (arrowed) superimposed over the apices. B Periapical of
showing the radiopaque line of the mylohyoid ridge (arrowed) superimposed over the apices. B Periapical of  showing the radiopaque shadow of the zygomatic buttress (arrowed) overlying and obscuring the apical tissues of the molars.
showing the radiopaque shadow of the zygomatic buttress (arrowed) overlying and obscuring the apical tissues of the molars.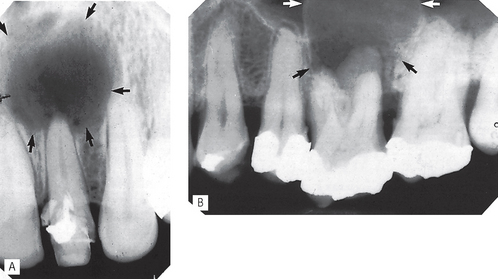
 . B Inflammatory radicular cyst (arrowed) associated with
. B Inflammatory radicular cyst (arrowed) associated with  . The antrum has been displaced by the upper margin of the cyst which is not evident on this radiograph.
. The antrum has been displaced by the upper margin of the cyst which is not evident on this radiograph.