Chapter 28 Differential diagnosis of lesions of variable radiopacity in the jaws
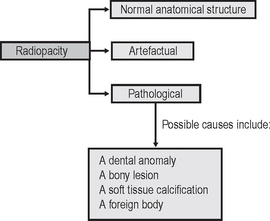
As explained in Chapter 26, a variety of conditions that can affect the jaws are radiopaque relative to the surrounding bone, although the degree of opacity can be very variable. A step-by-step guide, similar to that suggested for radiolucent lesions in Chapter 27, is outlined to emphasize the importance of a methodical approach when producing a differential diagnosis. The suggested approach is summarized in Figure 28.1. Although most lesions are still detected using plain radiographs, this process can be greatly facilitated in many cases if advanced imaging modalities, described in Chapter 19, such as computed tomography (CT), cone beam CT or magnetic resonance (MR) are available.
Step I
Describe the variable radiopacity noting in particular:
• Site or anatomical position — is the opacity actually within bone or is it within the surrounding soft tissues and thus superimposed on the bone? To localize the opacity, two radiographs are usually required ideally at right angles to one another.
• Outline or periphery — a particularly useful differentiating feature, since if the opacity is surrounded by a thin radiolucent line, it is invariably of dental tissue origin.
Step II
Decide whether the variable radiopacity is:
2. Artefactual
These depend largely on the type of radiograph, but examples include:
• Real or ghost earring shadows — seen on dental panoramic radiographs (see Ch. 17)
Step III
If the radiopacity is pathological, decide within which of the following major categories it should be placed:
Step IV
Consider the subdivisions of these pathological categories. A typical list is shown in Table 28.1.
Table 28.1 Classification of the more common lesions that can present as variable radiopacities in the jaws
| Abnormalities of the teeth | |
| Conditions of variable radiopacity affecting the bone | |
| Developmental | Exostoses including tori — mandibular or palatal |
| Inflammatory | |
| Tumours | |
| Odontogenic (late stages) | |
| Non-odontogenic | |
| Bone-related lesions | |
| Osseous dysplasias (Fibro-cemento-osseous lesions) (late stages) | |
| Other lesions | |
| Bone diseases | |
| Superimposed soft tissue calcifications | |
| Foreign bodies | |
Step V
Compare the radiological features of the unknown opacity with the typical radiological features of these possible conditions. Then construct a list showing, in order of likelihood, all the conditions that the lesion might be. As mentioned in Chapter 27, this list forms the radiological differential diagnosis.
The typical radiographic features of the important radiopacities are described below using a similar style to that adopted in Chapter 27. It must be emphasized that this is a simplified approach and that most lesions can produce a variety of appearances.
TYPICAL RADIOGRAPHIC FEATURES OF ABNORMALITIES OF THE TEETH
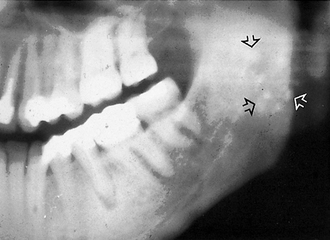
Unerupted or misplaced teeth including supernumeraries (Fig. 28.2)
Radiopacities caused by unerupted or misplaced teeth and supernumeraries are readily identifiable as such radiographically, by their characteristic shape and radiodensity.
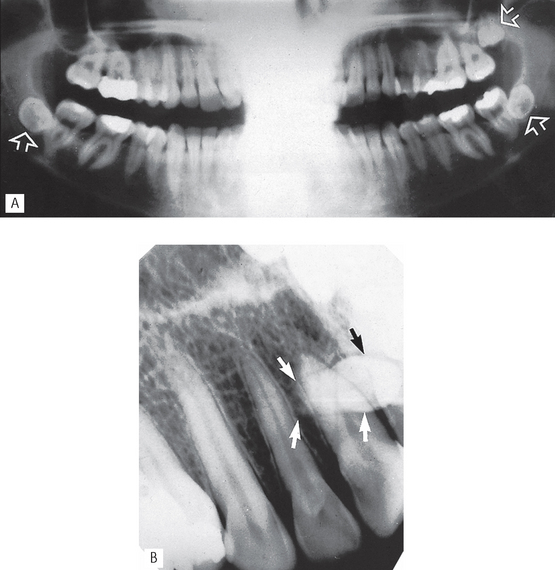
Fig. 28.2 Examples of opacities caused by unerupted teeth. A Panoramic radiograph showing the typical appearance of unerupted and misplaced wisdom teeth (arrowed) —  are positioned transversely. B Periapical showing a conically shaped mesiodens (arrowed) overlying
are positioned transversely. B Periapical showing a conically shaped mesiodens (arrowed) overlying  . Density, shape and outline confirm that the opacity is composed of dental tissue.
. Density, shape and outline confirm that the opacity is composed of dental tissue.
Odontomes
Although both compound and complex odontomes are more accurately classified as epithelial odontogenic tumours with odontogenic ectomesenchyme showing dental hard tissue formation (WHO Classification 2005), they are often also described as dental developmental anomalies (see Ch. 25).
Compound odontome
This odontome is made up of several small tooth-like denticles. The miniature tooth shapes are of dental tissue radiodensity, with a surrounding radiolucent line, and are easily identified radio-graphically (Fig. 28.3).
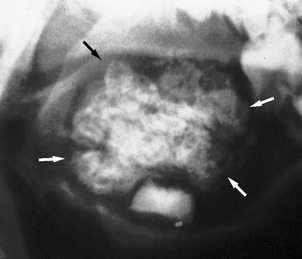
Complex odontome
This odontome is made up of an irregular, confused mass of dental tissues bearing no resemblance in shape to a tooth. The enamel content provides the dense radiopacity, suggestive of dental tissue and again the mass is surrounded by a radiolucent line (Fig. 28.4).
Root remnants (Fig. 28.5)
Deciduous and permanent root remnants remaining in the alveolar bone, following attempted extraction, are common. The site, shape and density make radiographic identification relatively simple. Additional diagnostic radio-graphic features include the surrounding radiolucent line of the periodontal ligament shadow and sometimes evidence of a root canal.
Hypercementosis (Fig. 28.6)
The formation of excessive amounts of cementum, usually around the apical portion of the root, is common. The cause is unknown, but it is sometimes seen in Paget’s disease of bone and is then typically craggy and irregular. Diagnostically hypercementosis is not a problem — the resultant opacity being part of the tooth root and producing an alteration to the root outline.
TYPICAL RADIOGRAPHIC FEATURES OF CONDITIONS OF VARIABLE OPACITY AFFECTING BONE
Developmental
Exostoses, including tori (mandibular or palatal)
Exostoses are small, irregular overgrowths of bone sometimes developing on the surface of the alveolar bone. They consist primarily of compact bone and produce an ill-defined radiopacity when superimposed over the bulk of the alveolar bone. Usually two views are required to establish the exact site (see Fig. 28.7).
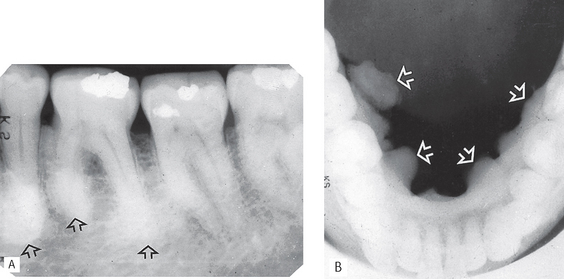
Fig. 28.7 A Periapical of  showing ill-defined areas of radiopacity (arrowed) overlying the teeth. B Lower 90° occlusal of the same patient showing the large irregular exostoses (mandibular tori) on the lingual aspect of the mandible (arrowed).
showing ill-defined areas of radiopacity (arrowed) overlying the teeth. B Lower 90° occlusal of the same patient showing the large irregular exostoses (mandibular tori) on the lingual aspect of the mandible (arrowed).
Specific exostoses develop in particular sites and are often bilateral:
Tumours
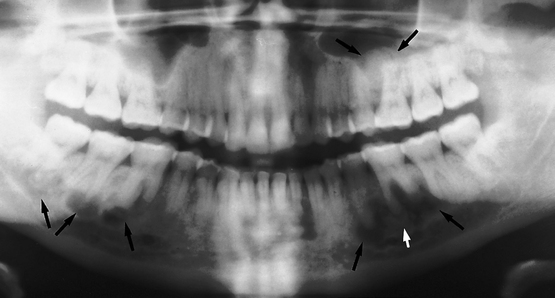
Calcifying epithelial odontogenic tumour (CEOT or Pindborg tumour) (Fig. 28.8)
Defined by the WHO as a locally invasive epithelial odontogenic neoplasm, characterized histologically by amyloid material that may become calcified.
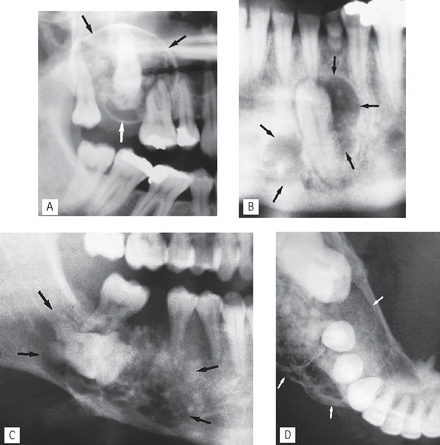
Fig. 28.8 A Right side of a panoramic radiograph showing a calcifying epithelial odontogenic tumour in the maxilla (arrowed) associated with the unerupted  . There are obvious areas of calcification within the lesion. B Part of a panoramic radiograph showing another CEOT (arrowed) associated with the unerupted lower left canine, with only faint internal calcification. C Right side of a panoramic radiograph showing a poorly defined calcifying epithelial odontogenic tumour (arrowed) associated with the unerupted molar. D Lower 90° occlusal of the same patient showing the expansive, multilocular nature of the lesion and the discrete internal calcifications.
. There are obvious areas of calcification within the lesion. B Part of a panoramic radiograph showing another CEOT (arrowed) associated with the unerupted lower left canine, with only faint internal calcification. C Right side of a panoramic radiograph showing a poorly defined calcifying epithelial odontogenic tumour (arrowed) associated with the unerupted molar. D Lower 90° occlusal of the same patient showing the expansive, multilocular nature of the lesion and the discrete internal calcifications.
• Frequency: Rare — approximately 1% of all odontogenic tumours.
• Site: —Molar/premolar region of the mandible.
• Shape: — Unilocular or multilocular
• Outline: — Variable definition, frequently scalloped
• Radiodensity: — Radiolucent in early stages then numerous scattered radiopacities usually become evident within the lesion often most prominent around the crown of any associated unerupted tooth
• Effects: — Adjacent teeth sometimes displaced, sometimes resorbed
Ameloblastic fibro-odontoma (Fig. 28.9)
These rare, unilocular or multilocular odontogenic tumours resemble closely ameloblastic fibromas (see Fig. 25.10), and also affect children. However, they are often associated with an unempted tooth and usually contain enamel or dentine, either as multiple, small opacities or as a solid mass.
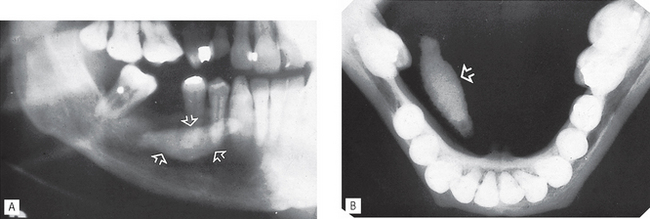
Adenomatoid odontogenic tumour (AOT) (Fig. 28.10)
Described by the WHO as being composed of odontogenic epithelium embedded in a mature connective tissue stroma and characterized by slow but progressive growth.
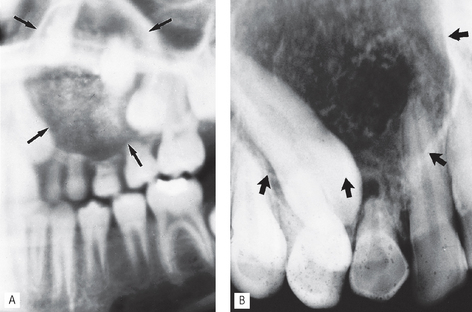
Fig. 28.10 A Part of a panoramic radiograph showing a monolocular adenomatoid odontogenic tumour in the anterior maxilla (arrowed) surrounding the unerupted  . Internal calcification is evident. B Periapical of the anterior maxilla showing another adenomatoid odontogenic tumour (arrowed) with internal calcification, associated with an unerupted canine.
. Internal calcification is evident. B Periapical of the anterior maxilla showing another adenomatoid odontogenic tumour (arrowed) with internal calcification, associated with an unerupted canine.
(Reproduced from A Radiological Atlas of Diseases of the Teeth and Jaws with kind permission from the authors R.M. Browne, H.D. Edmondson and P.G.J. Rout.)
• Age: Variable, but 90% develop before the age of 30 with most diagnosed in the second decade.
• Frequency: Rare — approximately 2–7% of all odontogenic tumours.
• Site: — Anterior maxilla — incisor/canine region
• Outline: — Smooth and well defined
• Radiodensity: —Initially radiolucent, but small opacities (snowflakes) within the central radiolucency may be seen peripherally as the lesion matures.
Calcifying cystic odontogenic tumour (calcifying odontogenic cyst or Gorlin’s cyst) (Fig. 28.11)
As stated earlier, the new name of this lesion reflects its classification by the WHO as an odontogenic tumour, who described it as a benign cystic neoplasm of odontogenic origin characterized histologically by ameloblastoma-like epithelium with ghost cells that may calcify. It presents typically anteriorly in either the mandible or the maxilla as a unilocular, well-defined, well-corticated radiolucency resembling other odontogenic cysts, but, as it develops, a variable amount of calcified material becomes evident, scattered throughout the radiolucency. The opacities can range from small flecks to large masses.
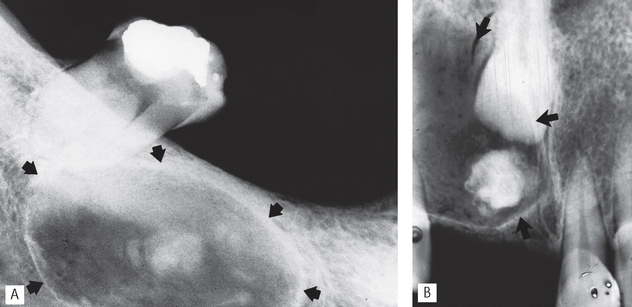
Fig. 28.11 A Periapical showing a well-defined calcifying cystic odontogenic tumour (arrowed) in the mandible with obvious areas of internal calcification. B Periapical showing a calcifying cystic odontogenic tumour (arrowed) in the anterior maxilla. The central incisor is unerupted and there is internal calcification of tooth-like density.
• Age: Variable, reported in patients between 5–92 years old.
• Site: Mandible or maxilla — anterior or premolar regions, one third associated with an unerupted tooth or odontome.
• Size: Usually small, up to 4 cm in diameter.
• Shape: Variable, but usually unilocular.
• Outline: — Smooth, well defined
• Radiodensity: —Initially radiolucent but in more advanced stages contains a variable amount of calcified radiopaque material of tooth-like density.
• Effects: — Adjacent teeth usually displaced, causing root divergence, and/or resorbed
Cementoblastoma (Fig. 28.12)
As indicated in Table 27.1, the cementoblastoma is classified by the WHO as an odontogenic tumour which is characterized by the formation of cementum-like tissue in connection with the root of a tooth.
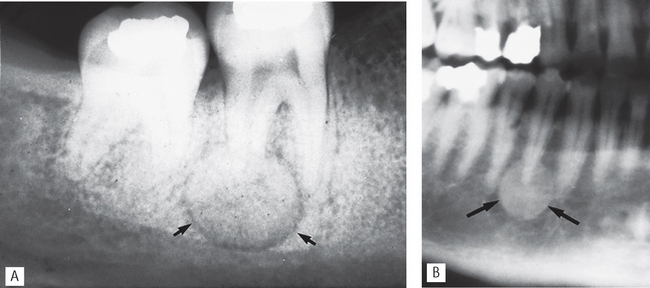
Fig. 28.12 A Periapical showing the typical radiopaque mass at the apex of the  of a cementoblastoma, the so-called golf ball appearance. The mass is attached to the root and has a thin radiolucent line around it (arrowed). B Part of a panoramic radiograph showing a radiopaque cementoblastoma at the apex of
of a cementoblastoma, the so-called golf ball appearance. The mass is attached to the root and has a thin radiolucent line around it (arrowed). B Part of a panoramic radiograph showing a radiopaque cementoblastoma at the apex of  (arrowed).
(arrowed).
• Age: Reported in patients between 8–44 years old, with a mean age of 20.
• Site: Apex of mandibular first permanent molars, occasionally premolars. Exceptionally associated with the primary dentition.
• Size: Variable, but up to 2–3 cm in diameter.
• Shape: — Round or irregular, sometimes described as resembling a golf ball
• Radiodensity:—Radiopaque but often surrounded by a thin radio-lucent line owing to an outer zone of osteoid.
• Effects: — Attached to the tooth root which is usually obscured as a result of resorption and fusion to the tooth
Osteomas (Fig. 28.13)
Osteomas of the jaws may be located in the medullary bone (endosteal osteoma) or arise on the surface of the bone as a pedunculated mass (periosteal osteoma). They are usually detected in young adults and are typically asymptomatic, solitary lesions. Multiple jaw osteomas are a feature of the rare inherited condition Gardner’s syndrome.
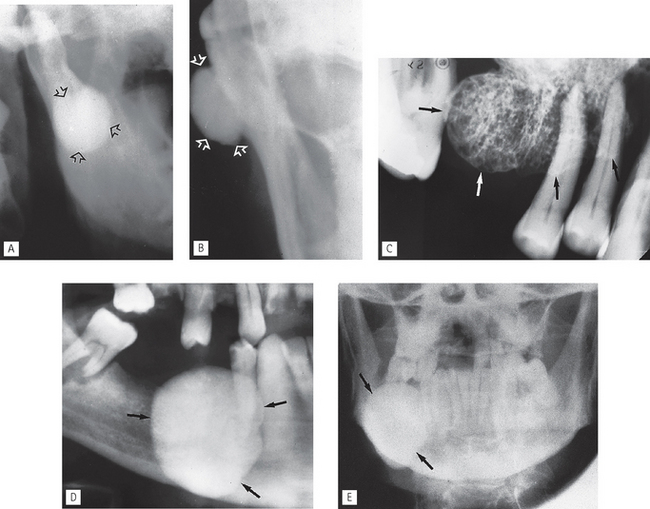
Fig. 28.13 A Oblique lateral of right ramus of the mandible showing a round radiopaque compact osteoma (arrowed). B Part of a PA jaws of the same patient showing the lesion (arrowed) arising from the lateral surface of the mandible confirming a periosteal osteoma. C Periapical showing a periosteal cancellous osteoma (arrowed). D Part of a panoramic radiograph and E PA jaws of the same patient showing a very large endosteal compact osteoma (arrowed) in the body of the mandible.
• Compact — consisting of dense lamellae of bone and including the so-called ivory osteoma occasionally seen in the frontal sinus (see Ch. 29).
Both tumours are uncommon. The type of bone making up the tumour determines the degree of radiopacity.
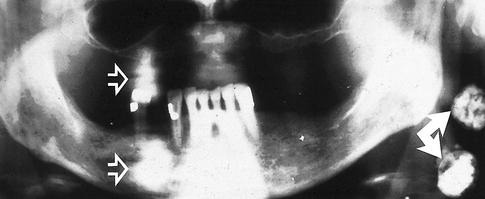
Osteosarcoma (Fig. 28.14)
Rare, rapidly destructive malignant tumour of bone. From a radiological viewpoint, there are three main types:
• Osteolytic — no neoplastic bone formation.
• Osteosclerotic — neoplastic osteoid and bone formed.
• Mixed lytic and sclerotic — patches of neoplastic bone formed.
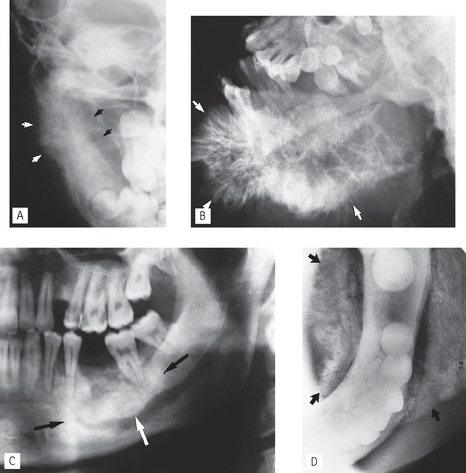
Fig. 28.14 A Right side of a PA jaws of a 7-year-old showing an osteosarcoma in the ascending ramus of the mandible. The sunray or sunburst appearance is evident medially and laterally (arrowed). B Oblique lateral showing a very extensive osteogenic osteosarcoma of the mandible with obvious sunray or sunburst bone formation. C Left side of a panoramic radiograph showing an irregular, poorly defined area of radiopacity (arrowed) in the body of the mandible. D Lower 90° occlusal of the same patient showing extensive buccal and lingual abnormal bone formation (arrowed) of another osteogenic osteosarcoma.
Osseous dysplasias
Periapical osseous dysplasia (Fig. 28.15)
Focal osseous dysplasia (Fig. 28.16)
This usually solitary fibrocemento-osseous lesion occupies a portion of the spectrum between the periapical and florid cemento-osseous dysplasias.
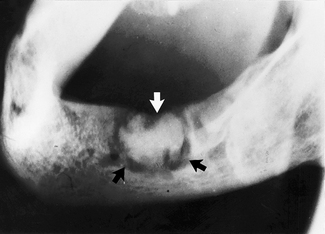
Fig. 28.16 Oblique lateral showing relatively late-stage focal osseous dysplasia in the region of the  extraction site (arrowed). An appreciable amount of internal calcification is evident.
extraction site (arrowed). An appreciable amount of internal calcification is evident.
• Age: Adults between 40 and 50 years old (typically white women).
• Site: Any areas of the jaws (dentulous or edentulous), but mainly posterior mandible, and often in extraction sites.
• Size: Small, less than 1.5 cm in diameter.
• Outline: — Well defined but irregular
Florid osseous dysplasia (Fig. 28.17)
• Age: Middle-aged adults (typically black women).
• Site: Widespread, often in all four quadrants (dentulous and edentulous) but associated with the apices of the teeth if present.
• Size: Variable, but individual lesions up to 2–3 cm in diameter.
• Outline: — Smooth but lobular
Bone-related lesions
As shown in Table 27.1, the WHO classify a number of different conditions under the general heading bone-related. Two of these can present as mixed radiolucent/radiopaque lesions in the jaws including:
Fibrous dysplasia (Fig. 28.18)
Fibrous dysplasia is described by the WHO as a genetically-based sporadic disease of bone affecting single or multiple bones. The jaws and other bones in the skull can be affected as well as other bones in the skeleton. The general radiological features of fibrous dysplasia are covered in Chapter 32.

Fig. 28.18 Periapical of the upper right maxilla showing the generalized radiolucency with the fine internal trabeculation of monostostic fibrous dysplasia, giving a ground glass appearance. The almost imperceptible junction between abnormal and normal bone is arrowed.
The radiographic features of jaw lesions include:
• Age: 10–20 year-old adolescents.
• Site: Maxilla — usually posteriorly, more commonly than the mandible. Maxillary lesions may spread to involve adjacent bones such as the zygoma, sphenoid, occiput and base of skull.
• Size: Variable and difficult to define.
• Outline: — Poorly defined with the margins merging imperceptibly with adjacent normal bone
• Radiodensity: — Initially radiolucent (but rarely seen clinically at this stage)
Ossifying fibroma (Fig. 28.19)
This lesion has previously been called cementifing fibroma and cemento-ossifying fibroma but the 2005 WHO classification uses the term ossifying fibroma which is described as a well-demarcated lesion composed histologically of fibrocellular tissue and mineralizing material of varying appearance.
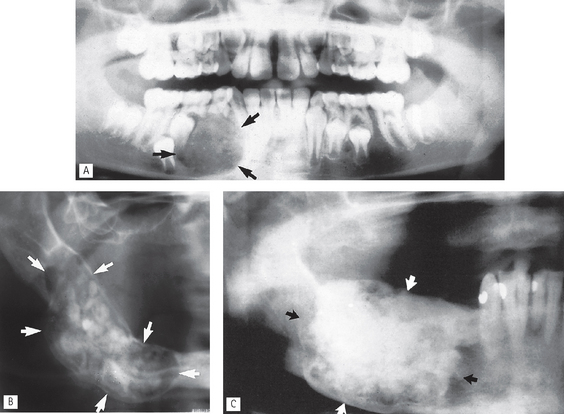
Fig. 28.19 A Part of a panoramic radiograph of a 9-year-old showing an intermediate stage ossifying fibroma, with fine internal calcifications evident, in the right body of the mandible (arrowed). There is also displacement of the unerupted lower premolars and permanent canine. B Part of panoramic radiograph showing a large ossifying fibroma (arrowed) occupying most of the body of the mandible with considerable internal calcification. C Right side of a panoramic radiograph showing a large mature radiopaque ossifying fibroma (arrowed).
• Age: Variable, but usually in the 2nd–4th decades (particularly women).
• Site: Usually posterior mandible, but different variants can affect the maxilla and paranasal sinuses.
• Size: Variable, may grow to several cm in diameter and cause facial asymmetry.
• Outline: — Smooth, well defined
Other important bone conditions
Paget’s disease of bone and osteopetrosis, two generalized conditions that can cause an overall increase in bone radiopacity, are discussed in detail in Chapter 32.
TYPICAL RADIOGRAPHIC FEATURES OF SOFT TISSUE CALCIFICATIONS
A variety of radiopaque calcifications within the overlying soft tissues can present radiographically. Differential diagnosis is relatively straightforward once the site of the opacity has been determined.
Radiopaque salivary calculi (see Ch. 33)
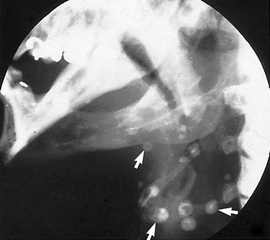
Submandibular gland calculi (Fig. 28.20) are often radiopaque and develop within the main duct or in the gland itself. Those in the main duct can be superimposed on the alveolar bone producing an opacity apparently within the bone. Stones in the gland present usually below the lower border of the mandible.
Calcified lymph nodes (Fig. 28.21)
Calcification of lymphoid tissue is relatively common following chronic infection (e.g. tuberculosis), especially in older patients.
Calcified tonsils (Fig. 28.22)
Calcification of the tonsillar lymphoid tissue is sometimes seen as an incidental finding on dental panoramic radiographs, especially in elderly patients. Areas of calcification appear as small irregular opaque masses overlying the superior aspect of the ramus of the mandible; they are often bilateral.
Phleboliths (Fig. 28.23)
Phleboliths are calcifications of thrombi within veins and are occasionally seen in haemangiomas. If the radiograph shows the calcified blood vessel end-on, the phlebolith has a characteristic target appearance — radiopaque around the periphery and radiolucent in the centre.
TYPICAL RADIOGRAPHIC FEATURES OF FOREIGN BODIES
A variety of foreign bodies can produce radiopacities. The appearance depends obviously on the nature of the foreign body, its density and its location. Figure 28.24 shows a selection of foreign bodies.
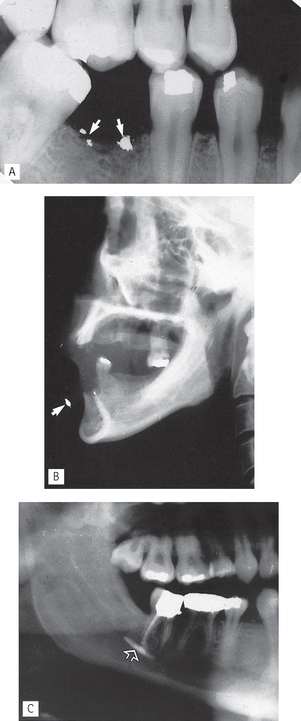
Fig. 28.24 A Bitewing showing amalgam remnants (arrowed), dislodged and left behind after an extraction. If evident clinically, they are referred to as amalgam tattoos. B True lateral skull showing a radiopaque foriegn body (arrowed) in the lower lip. C Right side of a panoramic radiograph showing radiopaque root canal sealant (arrowed) in the inferior dental canal.
FOOTNOTE
It is worth repeating that the radiodensity of many of the lesions mentioned in this chapter changes as they mature. During their early stages of development, there may be no evidence of internal calcification, making radiological differential diagnosis more difficult. For revision purposes Table 28.2 summarizes the main lesions of variable radiodensity which can develop internal radiopaque calcifications and so present with mixed radiolucent/radiopaque appearances.
Table 28.2 Summary of the main lesions that can present with variable radiodensity by developing internal radiopaque calcifications
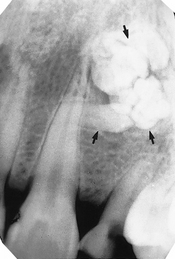
 region showing a radiopaque compound odontome (arrowed), consisting of small denticles.
region showing a radiopaque compound odontome (arrowed), consisting of small denticles.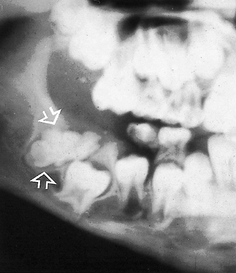
 (arrowed). It is preventing the eruption of
(arrowed). It is preventing the eruption of  . The opacity shows the characteristic surrounding radiolucent line, confirming its dental tissue origin.
. The opacity shows the characteristic surrounding radiolucent line, confirming its dental tissue origin.
 root caused by the root remnants of the deciduous
root caused by the root remnants of the deciduous  . Note that their radiodensity is equivalent to the adjacent roots and their surrounding radiolucent line.
. Note that their radiodensity is equivalent to the adjacent roots and their surrounding radiolucent line.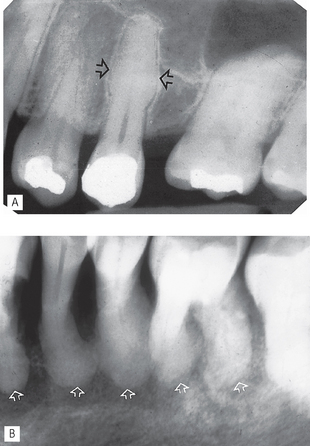
 (arrowed). B Periapical showing marked hypercementosis (arrowed) associated with Paget’s disease of bone. Note also the abnormal orange peel appearance of the bone.
(arrowed). B Periapical showing marked hypercementosis (arrowed) associated with Paget’s disease of bone. Note also the abnormal orange peel appearance of the bone. .
.