Respiration: Applied Aspects
Introduction
Applied respiratory physiology forms a link between the basics of respiration and clinical manifestations of respiratory diseases. This chapter is concerned with some of the important applied aspects of respiration which include:
Respiratory adjustments to stresses in health
Respiratory adjustments to stresses in health illustrate the integrated operation of the respiratory regulatory mechanisms. The stresses faced by respiration requiring adjustments in day-to-day life include the following.
1. Respiratory adjustments during exercise. Exercise is the most frequently faced stress in day-to-day life. Since during exercise many complex adjustments of muscular blood flow, metabolism, respiration, circulation and temperature are required, so they have been discussed on page 263.
2. Respiratory adjustments at high altitude. When a person is exposed to high altitude, particularly by a rapid ascent, the different systems of the body cannot cope with the lowered O2 tension and the effects of hypoxia start. Respiratory adjustments are thus a part of changes in the body at high attitude, so these have been discussed on page 255.
3. Respiratory adjustments to high atmospheric pressure form a part of the physiological problems faced by the body while going under the sea, and have been discussed on page 255.
Disturbances of respiration
From the physiological viewpoint disturbances of respiration can be discussed under the following headings:
Abnormal respiratory patterns
Eupnoea refers to the normal respiratory pattern, which implies a normal rate, rhythm and depth of respiration. Various abnormal respiratory patterns (Fig.5.7-1) can be produced by the changes in the environment or diseases affecting the respiratory system, cardiovascular system or brain. The terms used for the altered pattern of respiration are the following:
• Tachypnoea refers to an increase in the rate of respiration.
• Bradypnoea means decrease in the rate of respiration.
• Polypnoea is used to denote the rapid but shallow breathing resembling panting in dogs. In this, the rate of respiration is increased but the force does not change significantly.
• Apnoea refers to the temporary cessation of breathing.
• Hypoventilation term is used to describe a decrease in the rate and force of respiration.
• Hyperventilation refers to an increase in the rate as well as force of respiration.
• Hyperpnoea signifies a marked increase in the pulmonary ventilation due to an increase in rate and/or force of respiration.
• Dyspnoea. When hyperpnoea involves fourfold to fivefold increase in the pulmonary ventilation, an unpleasant sensation or discomfort is felt. This type of respiration is called dyspnoea.
• Periodic breathing refers to a respiratory pattern characterized by alternate periods of respiratory activity and apnoea. Some of the abnormal respiratory patterns are discussed in detail.
Apnoea
Apnoea refers to a temporary cessation of breathing. Depending upon the cause, apnoea may be of following types.
1. Voluntary apnoea refers to a temporary arrest of breathing due to the voluntary control of respiration. It is also called breath holding. The breath-holding time or apnoea time during which breathing can be withheld voluntarily is about 40–60 s in a normal person after a deep inspiration (for details see page 244).
2. Apnoea after hyperventilation occurs due to the reduced stimulation of respiratory centre owing to CO2 wash caused by hyperventilation (for details see page 249).
3. Deglutition apnoea occurs reflexly during swallowing (about 0.5 s). During pharyngeal stage of swallowing, the fluid or food stimulates the sensory nerve endings (5th, 9th and 10th cranial nerves) around the pharynx. Nerve impulses from these irritant receptors via the swallowing centres specifically inhibit the respiratory centre, stopping the breathing at any point of the cycle (deglutition apnoea). Simultaneously, there is closure of glottis (the opening between vocal cords). Both these effects prevent aspiration of fluid or food into the lungs (also see page 315).
Hypoventilation
Hypoventilation is used to describe a decrease in the rate and force of respiration. Thus, in hypoventilation, the amount of air moving in and out of lungs is reduced.
Causes of hypoventilation are:
Effects. Hypoventilation leads to hypoxia and hypercapnia (respiratory acidosis), which results in an increase in rate and force of respiration and the patient may develop dyspnoea.
Hyperventilation
Hyperventilation refers to an increase in the rate as well as force of respiration. Thus, in hyperventilation, the amount of air moving in and out of lungs is increased.
Causes of hyperventilation are:
• During exercise due to stimulation of respiratory centres by increased pCO2,
Effects of hyperventilation on respiration are described on page 249.
Dyspnoea
Dyspnoea literally means distressed breathing. Increased respiration without discomfort is called hyperpnoea. One is not aware of one's respiration till resting pulmonary ventilation becomes more than double. When hyperpnoea involves fourfold to fivefold increase in pulmonary ventilation, an unpleasant sensation or discomfort is felt. This type of respiration is called dyspnoea. The word ’air hunger’ is used as synonym to dyspnoea in general language.
Pulmonary reserve (PR) or breathing reserve
PR refers to the maximum amount of the air above the pulmonary ventilation that can be inspired or expired in 1 min.
It equals MVV minus pulmonary ventilation (MV), i.e.
Pulmonary reserve is usually expressed as percentage of MVV and is known as percentage pulmonary reserve or dyspnoeic index (DI), i.e.
Normal values of DI or %PR range from 70% to 95% with an average of 75%.
Dyspnoea is usually present when the value of DI becomes less than 60%.
Dyspnoea point refers to the height of hyperpnoea at which dyspnoea appears.
Periodic breathing
Periodic breathing is characterized by the alternate periods of respiratory activity and apnoea.
Cheyne–Stokes respiration
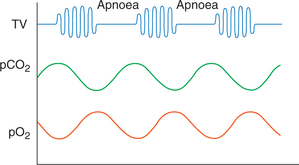
The Cheyne–Stokes respiration is a periodic type of breathing in which the alternate periods of respiratory activity and apnoea occur at regular intervals, and during the period of respiratory activity there is waxing and waning of tidal volume. The duration of one cycle is about 1 min. The arterial pO2 and pCO2 fluctuate during each cycle. The pO2is lowest and the pCO2 is highest at the end of apnoea (Fig.5.7-2).
Disturbances related to respiratory gases
Respiratory disturbances related to respiratory gases include:
Hypoxia
The term hypoxia is used to denote deficiency of oxygen supply at the tissue level. It has almost replaced the term anoxia (complete absence of oxygen), which rarely occurs practically.
Causes and types
Causes. Hypoxia can occur because of any one or more of the following defects:
• Decreased oxygen tension (pO2) of the arterial blood
• Decreased oxygen carrying capacity of the blood
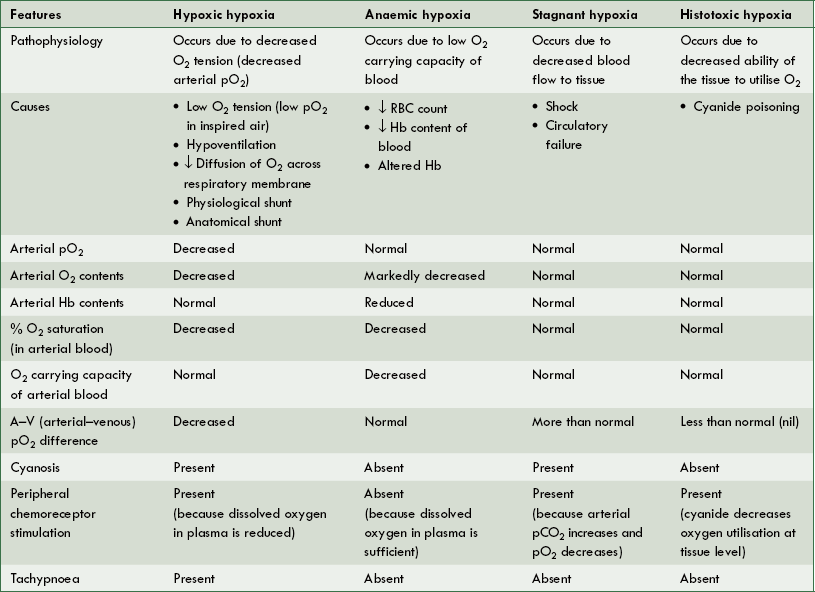
Types. Depending upon the mechanism of occurrence there are four types of hypoxia:
Characteristic features of four types of hypoxia are summarized in Table5.7-1.
Signs and symptoms of hypoxia
Symptoms of hypoxia depend upon:
1. Cyanosis is the bluish discolouration of skin and mucous membrane caused by the presence of more than 5 g of deoxyhaemoglobin/100 mL of the capillary blood.
Cyanosis is not a reliable sign of hypoxia because:
• Anaemic patients may never develop cyanosis, even though they are extremely hypoxic because of an inadequate haemoglobin concentration.
• Cyanosis does not occur in histotoxic hypoxia either because the O2 saturation of haemoglobin is normal.
2. Tachycardia. It occurs as a peripheral chemoreceptor reflex response to the low arterial oxygen tension.
3. Tachypnoea presents in the hypoxic hypoxia where arterial pO2 is low, but absent in both anaemic hypoxia and stagnant hypoxia in which the arterial pO2 is normal.
Physiological compensatory responses to chronic hypoxia
Two types of physiologic compensatory responses known to occur in hypoxia are accommodation and acclimatization.
Accommodation refers to immediate reflex adjustments of the respiratory and cardiovascular systems to hypoxia. These include:
Acclimatization refers to the changes in body tissues in response to long-term exposure to hypoxia, such as when a person living at sea level goes and stays at high altitude for a long time. With longer stay the person gradually gets acclimatized to low pO2 by following changes in the body tissues.
1. Increase in red blood cell count or the polycythaemia secondary to tissue hypoxia. For details see page 72.
2. Increase in pulmonary ventilation. There is gradual increase in ventilation to an average of about five times the normal.
3. Cardiovascular changes in the form of increased heart rate, force of contraction and increased cardiac output which occur in the initial accommodation period, and later on decrease back to normal once the O2 supply to tissues becomes normal due to changes in blood.
4. Pulmonary hypertension. It occurs secondary to the generalized hypoxic pulmonary vasoconstriction.
5. Increase in total lung capacity and diffusing capacity of the lung occurs in high-altitude natives as compared to their sea level counterparts. The increase in total lung capacity is evidenced by the enlarged chest that high-altitude natives develop.
6. Cellular and tissue acclimatization occurs after a long stay at high altitude. These include the following:
Treatment of hypoxia
Treatment of hypoxia basically includes:
Physiological basis of oxygen therapy in hypoxia
Oxygen therapy is of great value in certain types of hypoxia and at the same time of almost no value in other types.
In general, simple O2 therapy is not of much help in treatment of hypoxia because diffusion across respiratory membrane depends upon the partial pressure of gases; therefore, alveolar pO2 can be increased by:
Oxygen therapy with 100% pure oxygen at atmospheric pressure, i.e. at 760 mm Hg
1. Oxygen therapy is useful in most types of the hypoxic hypoxia. It is useful in different causes of hypoxic hypoxia including:
2. Oxygen therapy is of limited value in an anaemic hypoxia, stagnant hypoxia and hypoxic hypoxia caused by the physiological or anatomical shunts because in all these conditions oxygen is already available in the alveoli. However, in these conditions hyperbaric O2 therapy is more useful than O2 therapy at atmospheric pressure.
Hypercapnia
Hypercapnia refers to an increase in the arterial pCO2(normal value 40 mm Hg). When hypercapnia is the primary problem, it is associated with the respiratory acidosis (see page 248) since an increase in CO2 promptly generates excess H+.
Causes of hypercapnia
Hypercapnia occurs due to the following.
1. Defective elimination of CO2 as occurs in:
2. Accidental inhalation of CO2 in persons working in breweries and refrigeration plants. For further details see page 247.
Hypocapnia
Hypocapnia, i.e. reduced pCO2 is usually associated with respiratory alkalosis. Hypocapnia occurs due to hyperventilation.
Asphyxia
Asphyxia refers to a condition in which hypoxia (decreased pO2) is associated with hypercapnia (increased pCO2).
Carbon monoxide poisoning
Carbon monoxide (CO) is a dangerous gas present in exhaust of gasoline engines, coal mines, gases from deep wells and underground drainage systems.
Toxic effects. Carbon monoxide produces anaemic hypoxia and derangement of cellular metabolic system.
Anaemic hypoxia. When CO is inhaled accidentally from the above mentioned sources, carbon monoxide having 200 times more affinity than O2 for haemoglobin combines with it to form carboxyhaemoglobin. The carboxyhaemoglobin produces severe anaemic hypoxia.
Derangement of cellular metabolic system. Carbon monoxide causes toxic effects on cytochrome system of the cells causing derangement of the cellular metabolic system.
Treatment of CO poisoning. When diagnosed timely, following measures should be taken promptly:
High-altitude physiology
Composition of air and effect of altitude on it. Composition of air does not change with altitude, i.e. composition of atmosphere (percentage of gases) remains constant from sea level to about 30,000 ft.
Barometric pressure and partial pressure of gases. Barometric pressure at sea level is 760 mm Hg and it falls progressively with the increasing height. With decrease in total pressure of air at increasing altitude partial pressure of gases will change.
• According to Dalton's law the total pressure of air (P) is equal to the sum of partial pressures of the gases contained, i.e. P = pO2 + pCO2 + pN2 + pH2O.
• Changes in the body at high altitude are produced mainly by hypoxic hypoxia produced by falling pO2. Other factors which produce changes in the body at high altitude are effects of expansion of gases, fall in atmospheric temperature, light rays and gravity.
Hypoxia at high altitude
The effects of hypoxic hypoxia produced by decreasing pO2at high altitude depend upon:
• The rate at which hypoxia develops, i.e. hypoxia occurs due to a rapid ascent (acute hypoxia) or slow ascent (subacute hypoxia) and
• Duration of exposure to hypoxia, i.e. whether short-term stay or long-term stay (chronic hypoxia).
For details of hypoxic hypoxia see page 253.
Physiology of high atmospheric pressure
Introduction
Atmospheric pressure of 760 mm Hg at sea level is considered 1 atmospheric pressure.
Pressure increases by 1 atm for a depth of every 10 m (33 ft) as one descends beneath the sea. As the depth under sea increases the pressure also increases proportionately (Table5.7-2).
Table 5.7-2
Effect of depth on pressure and volume of gas
| Depth [m (ft)] | Pressure (atm) | Volume (L) |
| Sea level | 1 | 1 |
| 10 (33) | 2 | 1/2 (0.5) |
| 20 (66) | 3 | 1/3 (0.33) |
| 30 (100) | 4 | 1/4 (0.25) |
| 40 (133) | 5 | 1/5 (0.2) |
| 50 (166) | 6 | 1/6 (0.167) |
| 60 (200) | 7 | 1/7 (0.143) |
| 90 (300) | 10 | 1/10 (0.1) |
| 120 (400) | 13 | 1/13 (0.077) |
| 10 (500) | 16 | 1/16 (0.062) |
Decrease in volume of gases occurs due to compression as the pressure increases under sea. According to the Boyle's law the volume to which a given quantity of gas is compressed is inversely proportional to the pressure. With increase in the pressure the volume is decreased proportionately (Table5.7-2).
High atmospheric pressure is met under following conditions:
• G oing under the sea in submarines and
• Caisson's workers, i.e. the men who dig underwater tunnel, work in a chamber (Caisson's chamber) in which atmospheric pressure is high to prevent entry of water.
Physiological problems associated with life under high pressure may be divided into:
• Physiological problems at depth (due to compression effect of high atmospheric pressure) and
• Physiological problems of ascent (due to decompression phenomenon).
Physiological problems due to effect of high pressure on respiratory gases
Air under high atmospheric pressure is breathed under the sea. At high atmospheric pressure of air the partial pressure of oxygen (pO2), nitrogen (pN2) and carbon dioxide (pCO2) is also increased producing the following physiological problems.
1. Effects of increased pO2 (oxygen toxicity)
Acute oxygen toxicity occurs on exposures to 4 atm pressure of oxygen (pO2 in lungs about 3000 mm Hg).
2. Effects of increased pN2 (nitrogen narcosis)
Due to increased pN2, the nitrogen dissolves gradually into the body fluids and more easily into fats. The cell membrane of neurons contain high lipid content, so more nitrogen is dissolved in the neurons of brain producing nitrogen toxicity known as nitrogen narcosis. Nitrogen narcosis is characterized by the following.
Physiological problems of ascent
The two physiological problems which occur when an individual ascends back to sea level after sufficient exposure to high atmospheric pressure in the deep sea are:
Decompression sickness
Decompression sickness is also known as Caisson's disease, dysbarism, compressed air sickness, the bends and diver's palsy. When the individual ascends rapidly to the sea level after sufficient exposure to high atmospheric pressure deep in the sea, nitrogen is decompressed and escapes from the tissues at a faster rate. Being gas it forms bubbles while escaping rapidly from the tissues. The gas bubbles block the blood vessels producing tissue ischaemia and sometimes the tissue death.
Symptoms of decompression sickness
• Pain in joints and muscles of legs or arms. The joint pain accounts for the term ’bends’ that is often used to describe the decompression sickness.
• The chokes. The chokes refer to the serious shortness of breath, which is often followed by severe pulmonary oedema, and occasionally death.
• Paralysis of muscles may occur temporarily due to escape of nitrogen bubbles from the myelin sheath of motor nerves. This is called diver's palsy (one of the names of this disease).
• Coronary ischaemia or myocardial infarction may occur due to the blockage of coronary capillaries by the nitrogen bubbles.
• Neurological symptoms like dizziness, paralysis of muscles, or collapse and unconsciousness may occur due to the blockage of blood vessels of brain and spinal cord.
Treatment of decompression disease. Tank decompression is used for treatment of the decompression disease.
Prevention of physiological problems occurring at depth and on ascent
Deeper and longer dives can be made safe by following preventive measures.
2. Use of breathing mixture containing helium and low oxygen concentration
Use of breathing mixture containing helium and low oxygen concentration is less harmful than natural air because of the following.
Low oxygen concentration prevents occurrence of oxygen toxicity.
Helium when replaced with nitrogen provides following advantages:
3. Slow ascent or use of decompression tank
Slow ascent with short stay at regular intervals, i.e. slow and stepwise ascent, ensures that only a small amount of bubbles are formed at a time.
Decompression tank is based on the principle of slow ascent. After a rapid ascent the individual is put into a pressurized tank whose pressure is lowered gradually up to a normal atmospheric pressure.
Artificial respiration and cardiopulmonary resuscitation
Artificial respiration
Artificial respiration (AR) alone is required as an emergency life-saving procedure.
I When there is sudden stoppage of breathing as seen in:
II Artificial respiration may also be needed when breathing is expected to stop gradually as in paralysis of muscles in:
It is important to note that the tissues of brain, particularly cerebral cortex, develop irreversible damage if oxygen supply is stopped for 5 min. So, the resuscitation must be started quickly without any delay before the development of cardiac failure.
Methods of artificial respiration
Mouth-to-mouth breathing method
Various manual methods of AR have been described in past and discarded. Presently, the only manual method employed is mouth-to-mouth breathing (exhaled air ventilation) (Fig.5.7-3) because:

Fig. 5.7-3 Mouth-to-mouth breathing: A, the neck is extended by placing one hand under the neck and pressing the forehead with other hand; B, nostrils are closed with thumb and index finger, and resuscitator exhales into the patient's airway by tightly placing his mouth over the patient's mouth and C, allows the pati ent to exhale passively by unsealing nose and mouth.
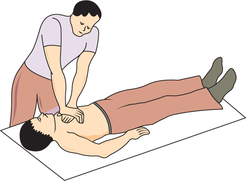
Cardiopulmonary resuscitation
Cardiopulmonary resuscitation (CPR) is required in some patients when heart and respiration both stop. Breathing usually stops before the heart stops, so AR should be started immediately.
Emergency plan of cardiopulmonary resuscitation
The following plan called ABC of CPR has proved useful in reviving such patients.
A Airway care is required in the unconscious patients. Immediately, tilt head back with a hand under the neck to maintain an open airway (Fig.5.7-3).
B Breathing by AR method is required when the patient is not breathing. Mouth-to-mouth respiration should be immediately started. Feel carotid pulse, if present continue AR only.
C Cardiac massage is required when carotid pulse cannot be felt. During external cardiac massage sternum should be depressed by 4–5 cm at a rate of 80–90 times/min. The cardiac compression should be alternated with mouth-to-mouth respiration at a rate of one ventilation to five chest compression (Fig.5.7-4).
 Abnormal respiratory patterns
Abnormal respiratory patterns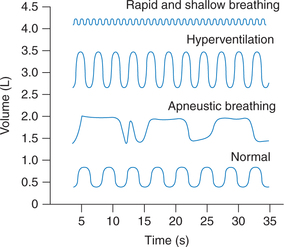
 Important note
Important note