Energy Metabolism And Nutrition
Nutrition is the science that deals with food and nutrients and the way the body uses them. It also deals with interaction of nutrients and their balance in relation to health and disease. The word nutrient refers to certain parts of food that the body uses for energy, growth and replacement of worn out structures. Thus, nutrition is the process of utilization of food by living organisms.
Human nutrition can be divided into three categories: undernutrition, overnutrition and ideal nutrition. In a developing country like India, undernutrition is the major concern, whereas in some affluent societies overnutrition is a serious problem. The concept of ideal nutrition is attracting attention presently. It explores long-term effects of nutrition on health.
A balanced intake of nutrients in quantities required by the body is essential to maintain good health. This ensures adequate growth and development as well. Carbohydrates, fats, proteins, vitamins, and minerals are some nutrients present in diet. Carbohydrates and fats are required primarily for providing energy. The dietary proteins, on the other hand, are mainly required for growth. Moreover, they provide amino acids which serve as precursors for a number of specialized products. Carbohydrates, fats and proteins are collectively referred to as macronutrients since they are required in relatively larger quantities, that is, to the extent of several grams per day. In contrast, vitamins and minerals are required in much smaller quantities: few micrograms to few milligrams per day. Accordingly, they are referred to as micronutrients.
After going through this chapter, the student should be able to understand:
Calorific values of food materials, components of energy requirements of the body; basal metabolic rate, specific dynamic action and physical activity; recommended dietary intake of nutrients: and proximate principles of food.
Nutritional importance of carbohydrates, dietary fibres, fats and proteins; parameters defining protein quality such as biological value, chemical score, protein efficiency ratio and net protein utilization; nitrogen balance; and protein sparing action of carbohydrates and fats.
I Calorific Values
The chemical energy in food is released in the body by oxidation to provide for the human energy requirements. The calorific value refers to the energy content of a food material. Its estimation involves measurement, of the energy produced by the combustion of foodstuffs in calorimeter. This method of estimation is based on Hess’ Law, which states that the energy given off in a chemical reaction is the same, no mater by which intermediate steps it is carried out. Thus, the energy liberated (as heat) in the combustion of glucose (C6H12O6 + 6O2 → 6CO2 + 6H2O) is exactly the same whether it is carried out in the laboratory or in the body, so long as the end products in each case are carbon dioxide and water. Therefore, by measuring the heat released in a calorimeter on burning a given quantity of fat, carbohydrate or protein, it is possible to say what must be the energy liberated by the body consuming known quantities of the three foodstuffs. A correction, however, has to be made especially in case of proteins, as discussed later. The calorimeter used is usually the bomb calorimeter, which can be filled with oxygen and ignited electrically.
In nutritional studies, the unit of energy used traditionally, has been the calorie. One calorie represents the thermal energy required to raise the temperature of 1 gm of water by 1°C (15°–16°C). In human physiology, energy is generally expressed in terms of kilocalories (kcal); one kcal is equals 1000 cal. In the International system of units, the unit of energy is kilo-joule (kJ); one 1 kJ is the energy required to move a mass of 1 kg by 1 meter distance by a force of one Newton. It is related to kcal as below:
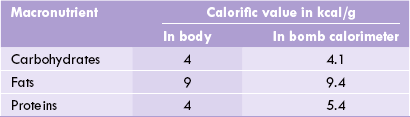
Table 28.1 gives energy yield from various macronutrients during body metabolism. It may be observed that the energy content of fat is more than twice as that of carbohydrate and protein. The calorific values of the latter two macronutrients are nearly the same. This is because both are completely oxidized to the same end products, carbon dioxide and water, both within the body and in the bomb calorimeter (see Hess’ Law). Proteins, however, are not completely burnt; one of the biological end products, urea, is different from that obtained in a calorimeter. Since urea molecule contains some amount of chemical energy, the calorific value of protein in the body (4 kcal/mole) is significantly less than that obtained in a bomb-calorimeter (5 kcal/mole 4 kcal/mole).
Unlike these three principal foodstuffs, the other nutrients, namely vitamins and minerals have zero calorific value. However, they play a supplementary role by promoting several reactions that generate metabolic energy from the principal foodstuffs.
A Respiratory Quotient (RQ)
This is defined as the molar ratio of carbon dioxide produced per unit of oxygen consumed during combustion of a foodstuff. For the combustion of glucose, the RQ is 6/6 = 1, which is assumed to be the case for all carbohydrates. The RQ for fats is lower because of their lower oxygen content. For the combustion of palmitic acid, the RQ is 16/23 = 0.71, which is assumed to be the case for all fats. For proteins, which are sums of their component amino acids that may show considerable variants, the RQ also varies accordingly; its value is generally taken as 0.8. On a mixed diet, the RQ value varies with relative proportions of different foodstuffs. For a normal Indian diet, its value is around 0.84.
RQ may be used to measure energy expenditure of an organism. This method may be referred to as indirect calorimetry (because it does not involve direct measurement of heat evolved by burning of the foodstuff). It is important to remember that average kcal yield per liter oxygen consumed is 4.65 when fats are metabolized (RQ = 0.71), and 5.11 per liter oxygen when carbohydrates are burnt (RQ = 1). Since the difference is small, it may be neglected, or an average value of 4.825 kcal is taken for a person on a mixed diet. An apparatus for measuring gas exchange gives oxygen consumption over a given period, and total energy spent by the individual is calculated based on the formula that each liter of oxygen consumed represents energy production of 4.825 kcal.
II Components of Energy Requirements
Total energy required by an average normal person is the sum of three energy-requiring body processes. These are:
1. The basal requirement (the basal metabolic rate).
2. The requirement for diet-induced thermo-genesis (specific dynamic action of food).
Besides the above three, extra provision of energy has to be made for growth, pregnancy and lactation.
A Basal Metabolic Rate (BMR)
BMR is defined as the energy expended by the body when the voluntary activity is at a minimum. The subject should be awake, at complete physical and mental rest, 12-hour after the last meal, and at an equable temperature (about 25°C). The metabolic rate during sleep is less than BMR.
Why should there be any expenditure of energy in absence of physical activity? To find the answer one must envision the body as an unlikely agglomeration of essentially unstable compounds, dissolved in or surrounded by a very precise but unusual salt solution. This combination has to be maintained for survival, as a rule, above the temperature of its surroundings. This is not possible without expenditure of a good deal of energy, which is tentatively identified with BMR. Thus, BMR reflects the energy required for maintaining the integrity of the organism and for sustaining vital functions under basal conditions. Some such functions include pumping of blood by heart, conduction of nerve impulse, gastrointestinal motility and work of breathing. BMR also accounts for such processes as protein turnover, glycoside bond biosynthesis and maintenance of cation differences across membrane, especially the sodium-potassium gradient. A large proportion of the BMR is ascribable to the need to maintain this gradient (Chapter 7).
Normal Values
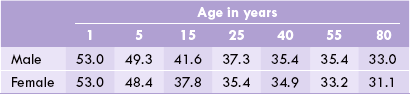
BMR is in the order of 1 kcal/kg body weight/h for human beings. It is higher in children than in adults, a little higher in younger adults than in the elderly and a little higher in males than in females. BMR takes into account the body surface area as well, and therefore, expressed as kcal expended per square meter body surface area per hour (kcal/sqm/h respectively). Variations to the extent of ± 15% of these are considered normal.
Measurement of BMR
The BMR is measured after some 12 hours of fasting in the post-absorptive state to avoid the so-called specific dynamic action: a surge of heat production after eating. The subject should be at complete rest, but awake, and in comfortable surroundings (at about 25°C). Any deviations from these conditions may alter the measured BMR to a significant extent.
Most commonly, the Benedict-Roth apparatus is used for the measurement of BMR. The subject is asked to breathe into the mouth piece of the apparatus and the volume of oxygen consumed over a 6-minute period is determined. This is multiplied by 10 to obtain the oxygen consumption in one hour. An approximation of how much calories of energy the subject is generating in an hour is provided by multiplying the oxygen consumption by the factor of 4.825, which represents the average kilocalorie yield per liter oxygen consumed. A person consuming 15 L oxygen per hour is generating 15 L/h × 4.825 kcal/ L = 72.3 kcal/h. This multiples to 1737 kcal per day.
BMR is generally calculated on the basis of the person’s surface area, which is estimated using the Du Bois equation:
log A = 0.425 log W + 0.725 log H + 1.8564
where A is the subject’s surface area in m2, W is the weight in kilograms and H is the height in centimeter. A 75 kg person who is 1.8 m (5.91 feet) tall has a surface area of about 1.94 m2. In all mammals, BMR expressed in this fashion is approximately the same, 900 kcal/m2/day.
Factors Affecting BMR
A number of physiological and pathological conditions affect BMR.
Body size and weight
The BMR shows wide variations, taking into account individual size and weight variations. For instance, BMR in humans is about 32 kcal/kg/ day, whereas in a mouse it is 212 kcal/kg/day.
Among humans, BMR varies with body weight, but the rise is not proportional. For instance, in males with body weight 60 kg, 70 kg, and 80 kg, the BMR is 2590, 3010, and 3710 kcal/day, respectively. This is because adipose tissue is not as metabolically active as lean body mass. In fact, BMR is more appropriately expressed per kilogram of lean body mass or fat-free mass.
Surface area, which is related to body weight and height, also affects BMR, as mentioned earlier. Person of lean built of a given body weight has a greater surface area compared to an obese subject of the same body weight, and therefore, BMR is higher in the lean individual.
Age
The BMR is significantly higher in infant and growing child than in adult, and a little higher in young adult than in the elderly. After 40 years of age, the BMR decreases at the rate of about 2% per decade of life (Table 28.2 ). Age affects BMR, largely through a decrease in lean body mass after adulthood. The decrease in BMR with advancing years is usually not accompanied by changes in eating habits, which is partly the reason for overweight and hypothermia in old age.
Sex
The gender differences in BMR (higher in males by about 5%) usually reflect the lower proportion of lean body mass in women, when compared to men of the same body weight.
Genetic differences
The BMR may vary by up to 10% between subjects of the same sex, age, body weight and fat content.
Racial differences
The BMR in Eskimos is significantly higher compared to that in other ethnic groups. However, studies to find differences between various ethnic groups, such as Asians, Africans and Caucasians have so far proved conflicting and inconclusive.
Nutritional status
In starvation, there is an adaptive decrease in the BMR, over and above that which results from the decrease in lean body mass. The converse is true when energy intake is increased.
Endocrinal state
BMR is increased in hyperthyroidism because thyroid hormones have a stimulatory effect on metabolism. In hypothyroidism, BMR may decrease by up to 40%, leading to weight gain. Other hormones, such as epinephrine and growth hormones, tend to raise BMR.
Climate
BMR increases in cold climate. In the persons living in tropical climate, BMR is about 10% less than those living in temperate zones.
Drugs
Smoking (nicotine) and coffee (caffeine and theophylline) increase the BMR, whereas ß-blockers tend to decrease it.
B Specific Dynamic Action (SDA)
Another component of energy expenditure is specific dynamic action of food, which refers to increased heat production after eating. It is also called diet-induced thermogenesis or post-prandial thermogenesis. SDA is believed be due to the energy expended in digestion, absorption, transport and subsequent processing of food. SDA was originally attributed solely to the metabolic handling of proteins, but it is now recognized as an effect produced by the consumption of all dietary fuels. The consumption of protein does, however, produce the greatest loss of energy (20–30% of intake), compared to fats (11–13%) or carbohydrates (5–6%). Relatively higher SDA of proteins is primarily to meet the energy requirements for oxidative-deamination, synthesis of urea and biosynthesis of proteins.
SDA is a wasteful expenditure from viewpoint of cellular energetics. Out of every 100 g of proteins consumed, the energy available for doing useful work is 20–30% less than the calculated value. For instance, assume a person taking 250 g of protein, which should produce 250 × 4 = 1000 kcal. But the body must spend some energy (about 20% = 200 kcal) to extract this 1000 kcal. So the net value of 25 g protein is 800 kcal (1000 minus 200).
On mixed diet, value of SDA is around 10%. The percentage of energy lost being 10% a person must take food worth 110 kcal to obtain 100 kcal. Thus, additional calories must be added during diet planning to account for SDA. Finally, SDA shows considerable individual variation and this has been implicated as an important factor, which allows some persons to maintain their normal body weight after overeating.
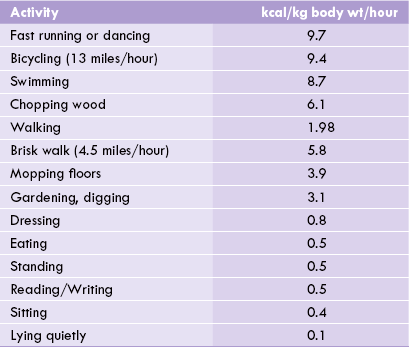
C Physical Activity
It is the third important factor that must be taken into account while calculating the energy requirements. Its value varies from one individual to another, and even in the same individual from time to time. It depends on the occupation, physical activity and lifestyle of the individual. For convenience, the activity level may be divided into three groups: sedentary, moderate and heavy.
To calculate total amount of energy for carrying out the muscular activities in 24 hours, the type and duration of all activities are carefully recorded. Table 28.3 shows energy expenditure for some of the common body activities. In general, a sedentary person requires about 30–50% more energy than the BMR requirement, whereas a highly active person may require 100% or more calories above the BMR.
D Total Energy Requirement of an Average Normal Person
Total energy requirement of a person is calculated by adding the above three components of energy requirement:
• Physical activity: The energy required for different grades of physical activities carried out in last 24 hours, is calculated. Consider energy requirement of an 80 kg man with the following daily activities: sitting, 8 h; lying down, 4 h; walking, 1 h, standing, 0.5 h driving, 1 h; reading/writing, 1 h; gardening, 0.5 h; cycling, 0.2 h. These activities account for 828 kcal in 24 hours (the student is advised to refer to Table 28.3 and calculate).
• BMR: The energy requirement for physical activity is added to BMR. The BMR may be calculated from the approximation:
This equals 1 × 80 × 24 = 1920 kcal. Adding the two numbers, 828 and 1920, we get a total of 2748.
• SDA: The above value of 2748 equals calorie requirement excluding the SDA. A 10% surcharge is added to take into account the SDA. This amounts to about 274 kcal to give a grand total calorie requirement of 274 + 2748 = 3022 kcal/day.
Daily energy demands of most adult men vary between 2400 kcal (in sedentary workers) to 4000 kcal (in heavy workers). The corresponding figures in women are 19002600 kcal per day. Table 28.4 shows recommended kcal allowances for individuals of different age groups and body weights.
Table 28.4
Recommended kcal allowances per day
| ICMR recommendation | |
| Man (55 kg) | |
| Sedentary work | 2400 |
| Moderate work | 2800 |
| Heavy work | 4000 |
| Women (45 kg) | |
| Sedentary work | 1900 |
| Moderate work | 2200 |
| Heavy work | 2600 |
| Later half of pregnancy | + 300 |
| Lactation | + 700 |
| Infants | |
| 0–6 months | 120/kg body wt |
| 7–12 months | 100/kg body wt |
| Children | |
| 1–3 years | 1200 |
| 4–6 years | 1500 |
| 7–9 years | 1800 |
| 10–12 years | 2100 |
| 13–15 years | |
| Boys | 2500 |
| Girls | 2300 |
As noted earlier, an extra provision of energy must be made during infancy, childhood and pre-pubertal growth spurts (during 10–15 years of age). This is because biosynthesis of new tissues occurs during these stages of life, which requires input of considerable chemical energy. It has been estimated that laying down of 1 kg of new tissue in a year requires about 81 kcal/day extra energy. Likewise, an extra provision must be made during pregnancy to meet the requirements of the growing fetus. During lactation, an extra provision for synthesizing milk is needed; elaboration of one liter of milk (containing 642.8 kcal) requires at least 1285 kcal of energy.
III Recommendations for Dietary Nutrients
Amount of nutrients required to meet the physiological needs of an individual is termed recommended dietary allowance (RDA). The Indian Council of Medical Research has prescribed RDAs for all essential nutrients, after suitably modifying the recommendations of WHO and FAO for Indian conditions.
RDA of a given nutrient must be differentiated from the amount that must be consumed merely to avoid deficiency disease. RDA refers to the amount that is required for optimizing health, and not the amount merely to avoid the disease. For example, RDA for vitamin C is about 60 mg, but the amount required for preventing scurvy is only about 10 mg/day. Intake of a nutrient at or near RDA provides considerable safety margin against the development of deficiency disorders.
RDA for proteins is 70 g for a 70 kg adult man. The same individual would require about 80 g fats and 365 g carbohydrates each day. RDA for the micronutrients is much smaller, for example, RDA for vitamin E is 10 mg/ day of α-tocopherol equivalents (see Chapter 18).
Factors Affecting RDA
Age, sex and several other factors determine RDA (Table 28.5 ). For example, infants require about 2.4 times as much proteins per day as required by adults to support growth; males require greater amount of a given nutrient since their body mass is more; and RDA is enhanced in physiologically stressful states such as pregnancy and lactation and in patients with injury or illness. However, certain exceptions do occur; for example, RDA for iron in women is more than in men since women must replace the amount lost during menstruation.
Table 28.5
Recommended daily allowance (RDA) of proteins in different age groups
| Nutrient | Requirement per day per kg body weight |
| Proteins | |
| Males | 1g |
| Females | 1g |
| Children | |
| Infants | 2.4 g |
| Up to 10 years | 1.75 g |
| Boys (> 10 years) | 1.6 g |
| Girls (> 10 years) | 1.4 g |
| Pregnancy and lactation | |
| Pregnancy | 2 g |
| Lactation | 2.5 g |
Recent studies have indicated that for optimal health, it is sometimes necessary to consume certain nutrients in amounts larger than RDA. For example, daily intake of vitamin E in amounts three times the RDA significantly reduces risk of coronary artery disease. Conversely, excessive intake of certain nutrients is hazardous, for example, risk of coronary artery disease is enhanced if fats are taken in excessive amounts.
IV Proximate Principles of Food
Food plays a much wider role than merely providing energy and biochemical needs of life. In fact, culture, availability, economics, religion, fads and several other factors play an important role in determining the type of food consumed in a given society. Agricultural societies, including those in India, subsist mainly on cereals. However, in non-agricultural societies like Eskimos of Greenland and hunters of Africa, meat is the major food. In such foods, nearly one-third of the total energy is provided by proteins and a major contribution for the rest comes from animal oils and fats. This is in sharp contrast with the average Indian diet where carbohydrates, proteins and fats account for about 75–80%, 10–12% and 10–15%, respectively, of the total energy provided. In between these two extremes lies the continental diet of the affluent Western societies. In a typical continental diet, contribution by carbohydrates is much less (40–45%), whereas fats and proteins account for more energy as discussed later.
V Nutritional Importance of Carbohydrates
Dietary carbohydrates are major components of an Indian diet, contributing up to 60–70% of the total caloric requirements of the body. However, from nutritional viewpoint they are not essential for human beings as all carbohydrates can be synthesized in the body. They are regarded as a relatively cheap source of energy: the carbohydrate-rich foods cost less. There are two groups of carbohydrates in the diet: available carbohydrates that can be assimilated and utilized for energy production: and dietary fibres that are indigestible, and therefore constitute unavailable carbohydrates in the diet.
A Available Carbohydrates
Some important available carbohydrates present in diet are starch, sucrose, lactose, fructose and glucose. Of these, starch is the most abundant and cheapest source of energy, being present in most commonly available foods such as cereals, pulses, tubers, etc. On cooking it becomes more soluble and accessible to digestive enzymes. Amylase hydrolyzes the α(1→4) linkages of starch to form maltose, and oligosaccharide units, which are further hydrolyzed to glucose by the brush-border enzymes (Chapter 26). Glucose is the major source of energy for most organs and tissues; erythrocytes, brain and other parts of central nervous system depend almost exclusively on glucose as a fuel.
Lactose is present in milk, and is therefore the major carbohydrate for the breast-fed infants. Sucrose imparts sweetness to the diet because of its excessive sweetening property. However, the same property restricts its consumption; the daily intake may be as low as 4 g/day. It has been observed in experimental animals that feeding of excess sucrose results in hypercholesterolaemia and hypertriglyceridaemia. In humans, it predisposes to the development of dental caries. In view of these observations, only a limited intake of sucrose has been suggested; and avoided altogether in diabetic individuals and in those attempting weight reduction. Jaggery, a sweetening agent, is better since besides sucrose it provides iron as well.
Rates of assimilation of different saccharides differ to a significant extent. This is indicated by the observation that following consumption of these saccharides different responses are obtained in the
The above responses are lower with the complex carbohydrates (for example starch) than with the simple carbohydrates (glucose or fructose). The elevation of blood glucose level following fructose intake is less than the elevation seen after intake of an isocaloric amounts of glucose. Lactose is least effective in this regard, causing the least elevation of the glucose response curve.
Functions
Carbohydrates play a major role in body’s energy balance and are involved in a number of other vital functions, discussed earlier chapter. To summarize a few important ones, carbohydrates are required for the synthesis of fats and non-essential amino acids, for oxidation of fats (acetyl CoA, a product of fatty acid oxidation combines with oxaloacetate, a product of carbohydrate metabolism), and have protein sparing action (discussed later).
B Dietary Fibres
Fibres, an important component of the diet, comprise plant cell components that cannot be broken down by human digestive enzymes. It is, however, incorrect to assume that fibres are completely indigestible, since some of them are at least partially broken down by intestinal bacteria. Fibres are complex carbohydrates having varying degrees of solubility. The more insoluble fibres include cellulose and lignin; soluble ones include pectins and gums; and, partly soluble ones are arabinoglycans (mucilage).
Physiological Significance
Being largely indigestible, the dietary fibres do not provide any energy. Yet, certain invaluable health benefits are provided by dietary fibres, as discussed here:
1. Increased bowel motility: Fibres can absorb significant amount of water because of their predominantly hydrophilic nature. Thus, the ingested fibres attract large quantity of water into intestinal lumen, which results in increased bowel motility. This is especially useful in constipation and in patients with haemorrhoids, diverticulosis and colon cancer.
2. Elimination of toxic compounds: Fibres can bind various toxic compounds, including certain carcinogens and bacterial toxins, and eliminate them through fecal route.
3. Cholesterol lowering effect: The binding properties of fibres enable them to absorb organic substances such as cholesterol and eliminate them in faeces, so as to lower plasma cholesterol concentration.
Further, fibres bind bile salts and reduce their enterohepatic circulation. This in turn enhances cholesterol to bile salts conversion and promotes its disposal from the body.
Water-soluble fibres act by additional mechanisms: they lower serum cholesterol levels either due to their effect on insulin levels (insulin stimulates cholesterol synthesis and export), or other metabolic effects (perhaps caused by end products of partial bacterial digestion).
Thus, high fibre diet is recommended in patients with hypercholesterolaemia.
4. Antihyperglycaemic effect: Fibres form a vicious gel in stomach and intestine to slow the rate at which various nutrients, most importantly carbohydrates, are digested and absorbed from intestine. Thus, the rise in blood glucose as also the subsequent rise in insulin levels are significantly impaired if fibres are ingested along with carbohydrate-containing foods. This accounts for their utility in diabetes mellitus.
4. Satiety effect: Fibres significantly increase bulk of the diet, so that one gets a feeling of fullness after ingestion. This bulk-enhancing property gives a feeling of satiety even without consumption of excess calories.
Chemical nature and physiological effects of some dietary fibres are given in Table 28.6 .
Table 28.6
| Fibre | Chemical nature | Physiological effect |
| Cellulose | Polymer of glucose | Increases weight and bulk of faeces, promotes colonic peristalsis, decreases fecal transit time |
| Hemi-cellulose | Polymer of pentoses, hexoses and uronic acid | Retains water to increase bulk of faeces, increases bile acid excretion |
| Lignin | Aromatic alcohol | Antioxidant, hypocholesterolaemic |
| Pectin | Polymers of galactose, galacturonic acid, rhamnose and arabinose | Improves glucose tolerance in diabetes, increases bile acid excretion |
| Mucilage | Branched arabinoglycan | Increases bile acid excretion, hypocholesterolaemic |
VI Nutritional Importance of Fats
Fats are considered as richer source of energy compared to carbohydrates and protein since they provide more energy per unit mass (Table 28.1). From energy perspective, the most important dietary fat is triacylglycerol (TAG) since it constitutes more than 90% of the total dietary lipids. The TAG may contain saturated, monounsaturated and polyunsaturated fatty acids (PUFA). Smaller amounts of other lipids, e.g. phospholipids, glycolipids, cholesterol, etc. may also be present in foods.
In Western countries, the percentage of calories derived from fats is high (about 40°C) compared to developing countries (about 15%). Regarding Indian conditions, the fat intake is highest in Punjab and lowest in Orissa and Kerala. Current recommendations are—a maximum of 35% of the energy intake as fats. These recommendations, which are aimed primarily at influencing cholesterol metabolism, further suggest intake of less than 300 mg/ day of cholesterol; 30 gm/day of PUFAs, and only 10% of the total energy intake as saturated fatty acids.
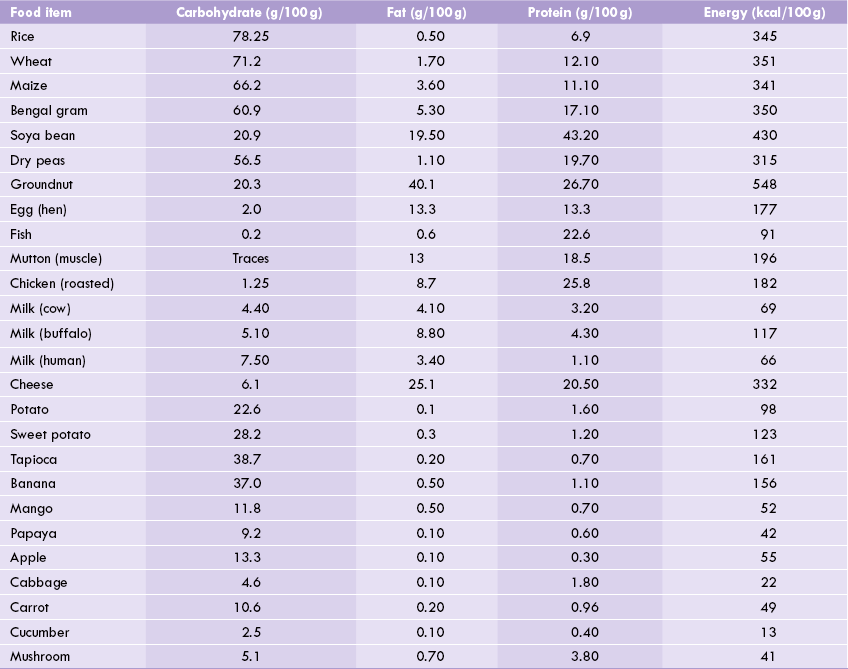
Dietary fat content of some common food items are shown in Table 28.7 . The dietary fats may be divided into two types: visible fats and invisible fats. The visible fats are oils, butter, ghee, etc. which are pure lipid forms. The invisible fats are part of other food items, e.g. egg, fish, meat, cereals and oil seeds. Recommended daily intake of visible fats is 10% of total calorie intake or about 20 g/day.
Functions
In addition to providing energy, fats increase the palatability of food and are mainly responsible for the feeling of satiety after meals. They constitute the favoured, cooking medium all over the world. Dietary fats are also required for the intestinal absorption of fat-soluble vitamins (A, D, E and K). Moreover, the dietary fats provide the polyunsaturated fatty acids (PUFAs) that are required for various body functions.
Role of PUFAs
1. They are components of phospholipids and form biomembranes.
2. They are required for esterification of cholesterol.
3. They serve as precursors of prostaglandins and leukotrienes.
4. They have hypocholesterolaemic effect and, therefore, offer protection against atherogenesis.
The ω-6 bring down the plasma LDL level. However, they lower plasma levels of HDL as well, thus reducing the cardioprotective effect. The ω-3 PUFAs reduce serum triglyceride levels. Moreover, they increase production of TXA3, which is less thrombogenic than TXA2. Thus, consumption of the ω-3 PUFAs decreases platelet aggregation, which accounts for their anti-thrombogenic properties. The monounsaturated fatty acids also lower the serum cholesterol levels when substituted for the saturated fatty acids. An additional advantage is that they do not lower HDL levels.
However, in recent times various hazardous effects following over-consumption of PUFAs have been reported. Excess PUFA may lead to production of free radicals that may be injurious to the cell unless antioxidants are available. It is, therefore, advisable to consume a proper mixture of fats, containing a balanced proportion of saturated and unsaturated fatty acids. The present recommendation is that not more than 30% of the total fats should be in the form of PUFA.
There has been considerable debate regarding utility of fats from plant sources vis-à-vis those from animal sources. The animal fats generally contain a higher proportion of saturated fatty acids (with the exception of fish which contains mostly unsaturated fatty acids), whereas the fatty acids from plants are mostly unsaturated (with the exception of coconut oil which contains mostly saturated fatty acids). Finally, though vegetable oils are rich in PUFA, they are mostly unpalatable because of unpleasant odour and unpleasant taste. Free fatty acids and substances responsible for bad odour, taste and rancidity are, therefore, removed to yield refined oils. Vegetable oils are refined by treating them with steam, alkali, etc.
VII Nutritional Importance of Proteins
Recommended daily intake of proteins is 1.0 g/kg body weight. Dietary protein intake is considered adequate if it supplies up to 12% of body’s energy needs. In children, the protein requirement is higher because of a higher growth rate. The protein requirement is higher in both, pregnancy and lactation (Table 28.5).
Dietary proteins are needed for:
1. Body growth, and repair and maintenance of tissues.
2. Replenishing the amino acids lost in urine, faeces, saliva, skin, hair and nails.
3. Replenishing amino acids in the (amino acids) pool, after these amino acids are used up for the synthesis of non-protein nitrogenous compounds and for other bodily activities.
Excess dietary intake of proteins, or low intake of carbohydrates and fats results in protein degradation for obtaining energy.
A Protein Quality
Proteins from different sources differ in their ability to support growth and to maintain and repair the body tissues. This ability is an indicator of quality of protein.
Protein quality depends on amino acid composition, digestibility and efficiency with which the amino acids are absorbed and subsequently incorporated in the body proteins. Some of the parameters used to define protein quality are biological value, protein efficiency ratio and chemical score.
Biological Value (BV)
It is the percentage of absorbed nitrogen retained in the body
BV is an empirical measure of the efficiency of protein as a supply of essential amino acids. For example, biological value of egg protein is very high (96) because it contains an adequate quantity of all essential amino acids and more importantly, it supplies these amino acids in the needed proportions.
Generally speaking, the animal proteins have higher biological value (Table 28.8 ). However, gelatin, prepared from animal collagen, is an exception since it lacks several essential amino acids. Consequently its biological value is low.
Table 28.8
Protein quality of some foods items
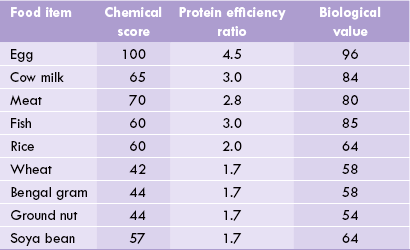
Biological value is most commonly used parameter for assessing protein quality.
The proteins obtained from plant sources have lower biological value since they lack one or other essential amino acid. The missing amino acids are called the limiting amino acids. This limitation of plant foods is overcome when these foods are consumed in combinations. For example, wheat is deficient in lysine but contains other essential amino acids in adequate amounts. Kidney beans contain lysine in adequate amounts, though deficient in methionine. When these two food items are combined, the body gets the required supply of both methionine and lysine.
Thus, dietary combinations of higher biological value are designed by appropriate combination of foodstuffs. This is referred to as the mutual supplementation of proteins. The following combinations are commonly seen in Indian diets: rice + pulses; wheat + pulses; soya bean + wheat; and cereals + legumes + curd. Another way to improve biological value is addition of the limiting amino acid to a foodstuff, e.g. lysine can be added to wheat flour. This process is called fortification with (limiting) amino acid. Likewise, vegetable proteins can be fortified with their limiting amino acids: lysine, methionine, threonine and tryptophan. The amino acids for fortification are commercially manufactured at economic prices and then mixed in appropriate proportions to foods.
Protein Efficiency Ratio (PER)
It is a less commonly used parameter for assessing the protein quality. It is defined as gain in body weight for each unit weight of protein ingested. Apparently, the amount of dietary protein used for maintenance is ignored.
Eggs, milk and meat have high PER (2.5) and legumes, lentils, cereals and nuts have PER between 0.5 and 2.5. PER of gelatin is less than 0.5.
Chemical Score
The essential amino acid content can also be expressed in terms of chemical score. It is calculated as here:
The egg protein is taken as the reference protein; its’ chemical score is 100.
Digestibility Coefficient (DC)
It refers to the percentage of ingested protein absorbed into the bloodstream (after digestion) in the gastrointestinal tract.
Net Protein Utilization (NPU)
This is a measure of utilization of dietary protein for synthesizing body proteins, calculated by the formula:
NPU is a better index than biological value since it takes into account the digestibility factor also. In fact, it depends on both digestibility coefficient and biological value.
B Nitrogen Balance
Nitrogen balance refers to comparative amounts of the nitrogen entering the body and that leaving it. A normal adult with adequate protein intake should be in nitrogen equilibrium: the amounts of incoming and outgoing nitrogen are equal. Since the exclusive source of nitrogen in the body are dietary proteins (16% of which is nitrogen), the nitrogen balance studies are used for assessing utilization of dietary amino acids for synthesis and for studying the balance between anabolic and catabolic processes.
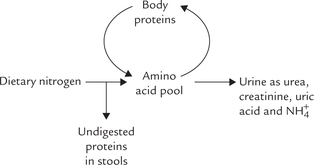
A 100 g sample of dietary protein contains approximately 16 g nitrogen, of which, approximately 83% leaves the body as urea, 7% as ammonium ion, and 10% as organic waste products such as uric acid and creatinine. Most of this nitrogen is eliminated via urine but 1-2 g of nitrogen from undigested protein are excreted in stools also. These observation are diagrammed here.
In addition to the state of nitrogen balance in a normal healthy body, there are two abnormal states, positive and negative-nitrogen balance.
A positive nitrogen balance is observed when nitrogen intake exceeds nitrogen excretion, it implies that amount of body protein increases. It is seen in situations where tissue growth occurs; for example, in growing children, convalescing adults and in pregnant women.
Negative nitrogen balance, on the other hand, reflects nitrogen excretion exceeding the nitrogen intake. It occurs when the dietary protein intake is inadequate, or when some physiological stress is encountered, such as trauma, burns, or emaciating illness.
C Protein Sparing Action
Dietary intake of carbohydrates and fats indirectly influences protein requirement of an adult. If dietary consumption of carbohydrates and fats is inadequate, some dietary protein must be used for energy generation. Thus, protein becomes unavailable for building and replacing tissues; consequently, dietary requirement of protein increases to make up this loss. Conversely, when sufficient calories are obtained from carbohydrates and fats, protein is no longer required for providing energy, and therefore it can be used for building up body proteins. The proteins are thus spared by carbohydrates and fats; this action is referred to as protein sparing action.
Carbohydrates are more efficient in sparing proteins than fats, probably because carbohydrates can be used by almost all tissues.
D Reasons for Increase in Protein Requirement
• In active growth, more dietary proteins are required to supply amino acids to the growing tissue. Pregnancy, infancy, childhood and adolescence are some examples.
• Prolonged illness, trauma and surgery cause a major catabolic response to meet the increased energy needs of the body. This response is mediated by epinephrine, glucocorticoids, glucagon and certain cytokines which are secreted in increased amounts. Breakdown of body proteins occurs, which must be replaced by dietary intake so as to prevent negative nitrogen balance.
• In old age also, increased dietary protein intake is required. This appears paradoxical as the requirement should fall since there is little growth. However, older people need and generally consume fewer calories. Therefore, proteins should provide a larger percentage of total calories. Further, absorption of dietary proteins may be less due to digestion and absorption problems, common in old age.
VIII Balanced Diet
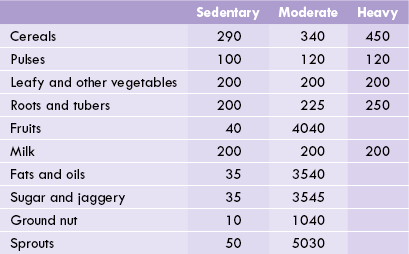
A balance diet is the one that has all the macronutrients and micronutrients recommended for individual’s age, sex, occupation and lifestyle. It supplies all the nutrients in amounts slightly more than the minimum requirement to withstand any stressful state. Composition of balanced diet differs depending on socio-cultural background, economic status, availability of foods, etc. Keeping in view the commonly available foods, in India (cereals, pulses, vegetables, roots & tubers, milk, etc), the composition of balanced diet for a vegetarian adult male, with sedentary lifestyle and moderate and heavy lifestyle, are formulated as shown in Table 28.9 .
Special allowances should be made in the formulation of balanced diet during physiologically stressful states, such as pregnancy and lactation.
IX Nutritional Implications of Diseases
Nutritional disorders can be classified into two broad categories: those arising due to undernutrition and those resulting due to overnutrition. The affluent urban elite of India are becoming more prone to the overnutrition-related health problems.
A Undernutrition: Protein Energy Malnutrition (PEM)
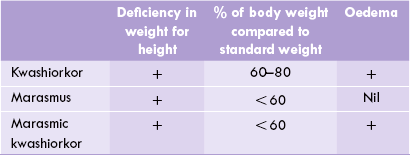
The dietary resources in the developing countries are limited, therefore, protein energy malnutrition is a common problem. Infants and children are the worst sufferers. The signs and symptoms of PEM vary from case to case depending on the degree of inadequacy. However, it is a common practice to divide all cases of PEM into two major categories: marasmus and kwashiorkor.
• Marasmus results from an inadequate intake of both proteins and energy.
• Kwashiorkor, on the other hand, results due to inadequate intake of proteins with relatively adequate energy intake. It is encountered in children between 1 and 4 years of age (marasmus usually occurs under one year of age).
In India, marasmus is the most frequent presentation of severe PEM, pure kwashiorkor is seldom seen. Mostly one comes across marasmic kwashiorkor in which there are clinical features of both the disorders (Table 28.10 ).
Marasmus
It is likely to occur among poor families, when there is a rapid succession of pregnancies, and early and often abrupt weaning, followed by inadequate artificial feeding. Thus, the diet is low in both calories and protein.
A child suffering from marasmus looks like a little old person with skin and bone. He has a thin, wasted appearance and weight is less than the desirable weight for his age. If the dietary deficiency continues for long, the developmental milestones get delayed and the condition ultimately leads to permanent stunting of growth and development. Not only the physical development, but the mental development is also affected (Table 28.10).
Kwashiorkor
In this type of malnutrition, the child has a plump appearance due to oedema. Oedema results from lack of adequate plasma proteins that normally maintain the distribution of fluids between the intra- and the extra-vascular compartments. Protuberant abdomen (due to oedema) is often seen, which is a deceptive presenting feature in view of muscle wasting and stunted growth of the child. Other symptoms associated with kwashiorkor are brittle hair, diarrhoea, dermatitis of various forms, and retarded growth. In contrast to early weaning in marasums, late weaning, often extending over 2 years, is characteristic of kwashiorkor.
Comparative features of marasmus and kwashiorkor are given in Table 28.11 .
Table 28.11
Comparative features of marasmus and kwashiorkor
| Marasmus | Kwashiorkor | |
| 1. | Diet with inadequate calories | Diet insufficient in proteins and calories |
| 2. | Usually seen in early weaning, or infants never breast-fed (under an year of age) | Usually seen in late weaning (1-4 years of age) |
| 3. | Oedema not present | Oedema characteristically present |
| 4. | Severe cachexia is seen | Body weight decreased or normal |
| 5. | Serum albumin normal or slightly decreased | Hypoalbuminaemia present |
| 6. | Somatic protein compartment depleted | Visceral protein compartment depleted |
| 7. | Face shrivelled and monkey-like | Face puffy, protuberant abdomen |
| 8. | Voracious appetite | Impaired appetite (anorexia) |
Both marasmus and kwashiorkor have similar devastating results. There is reduced ability of the afflicted individuals, to ht off infection in both conditions. Mortality is very high, the underlying cause of death is mostly some infection rather than starvation itself. Increased susceptibility to infection is due to decreased immunological response; reflected by: Various components of immune system affected are as follows:
Biochemical Changes in PEM
A number of biochemical parameters are altered in the following conditions:
• Decreased plasma levels of serum albumin and other serum proteins are most commonly seen. In kwashiorkor, the serum albumin may fall to a value as low as 2 g/dl, whereas in marasmus it need not be so low.
The level of retinol-binding protein (RBP) is also characteristically lowered.
• Glucose tolerance is often normal in both the conditions, but hypoglycaemia is often seen in a marasmic child.
• In kwashiorkor, blood urea may decrease and excretion of creatinine in urine is reduced due to loss of muscle mass.
• The cellular immunity tests are also affected.
• Features of associated deficiency of vitamins and minerals (mostly iron) are commonly seen.
• Hypokalaemia and dehydration occur when there is diarrhoea.
B Overnutrition
Diseases due to overnutrition are becoming more prevalent all over the world, especially among city dwellers. These diseases are influenced by dietary excess and dietary imbalances. For example:
• High calorific and high fat diet is associated with ischaemic heart disease—the biggest killer in urban settings. High fibre diet is beneficial for such individuals.
• Saturated fatty acids consumption is associated with increased risk of certain cancers, especially cancer of colon, breast and prostate.
Obesity
Obesity is a state in which excess fats (triacylglycerols) accumulate in the body. Increased number and/or size of adipocytes occurs in obesity.
Common Causes
One of the most serious problems among the urban affluent populations is consumption of excessive calories with inadequate exercise, of which obesity is the natural consequence. But obesity is not a simple problem of excessive calorie consumption; several other factors contribute to its development.
• Genetic predisposition plays an important role. Genetic predisposition has been suggested based on the familial incidence of obesity. If one parent is obese, 40-50% chances are there that the children would also suffer from obesity. However, no single gene is responsible for obesity.
• Leptin (Greek: Leptos = thin) is a 16-kD polypeptide, encoded by the obese genes in adipocytes, that influences appetite control system in the brain. These proteins cause decreased food intake, thus representing “satiety signal” in the body. Defect in the leptin-coding gene is seen in ob/ob mice, who tend to overeat and develop obesity. When injection of leptins is given to these animals, they eat less and lose weight.
• Certain metabolic aberrations are commonly associated with obesity. Hypothyroidism, hypogonadism, Cushing’s syndrome and hypopituitarism may lead to obesity. Women are more prone to become obese during puberty, pregnancy, and after menopause.
Biochemical Profile
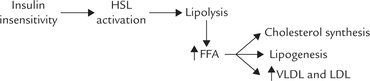
The most commonly affected parameters are the lipid parameters. Elevation of serum concentration of free fatty acids, cholesterol and triacylglycerol commonly occur. These parameters poorly respond to dietary restrictions. The underlying cause of the altered lipid profile can be traced to decreased sensitivity of peripheral tissues (including adipocytes) to insulin. The number of insulin receptors on cell surface is decreased (e.g. down-regulation) so that these tissues respond poorly to insulin, even though plasma insulin level is elevated. Since insulin inhibits activity of the hormone-sensitive lipase within adipocytes, this inhibition is impaired in obesity. Consequently, activity of the hormone-sensitive lipase increases, resulting in mobilization of fatty acids from adipocytes. This leads to increase in circulating free fatty acid levels.
The excess fatty acids are carried to the liver and degraded to acetyl CoA through β-oxidation. Since acetyl CoA is a precursor for cholesterol and fatty acids (and hence triacylglycerols), increased generation of these molecules results. The excess cholesterol and triacylglycerols are released (after incorporation in very low density lipoprotein particles) leading to high circulating levels of these lipid components.
The major ill-effects of obesity are reduced lifespan and coronary artery disease due to the prevailing alterations of lipid profile. Obese individuals are at higher risk of developing diabetes; nearly 80% of the adult onset diabetic individuals are obese. The underlying cause of diabetes in obese people is decrease in number of insulin receptors and decreased sensitivity to insulin. Moreover, decreased sensitivity to insulin results in hyperglycaemia and hence a persistent stimulus for the pancreatic ß-cells. Hyperinsulinaemia is the natural consequence. Hyper-insulinaemia in turn causes stimulation of sympathetic nervous system, which results in vasoconstriction and retention of sodium and water. Both these changes lead to hypertension.
The best treatment for the obese individuals—in fact the only effective mode of treatment—is reduction of body weight. All the aforementioned metabolic changes get significantly reversed if the ideal body weight is attained.
This goal can be accomplished by reducing the intake of calories and performing controlled exercise. Frequent small meals with lots of vegetables have been found especially effective. Fat restricted diet may retard the ageing process also and thus prolong the lifespan.
Diet and Coronary Heart Disease (CHD)
Coronary heart disease is a potentially lethal condition; the mortality is very high if timely diagnosis is not made and proper treatment is not initiated. The underlying defect in CHD is deposition of atherosclerotic plaques on the inner surface of the small- and medium-sized arteries. A plaque consists of deposits of cholesterol, cholesterol esters, and cellular debris. As the disease progresses, these deposits reduce or even block the blood flow. The blood supply to the peripheral tissues is impaired resulting in inadequate supply of oxygen and nutrients to these tissues. The consequences depend on the blood vessel that is affected:
• When the blockage occurs in the coronary vessels, damage to myocardium results. The cardiac tissue may become non-functional, and the condition is termed myocardial infarction (MI), commonly referred to as heart attack.
• Blockage in cerebral blood vessels may result in stroke.
• Risk of developing thrombosis is also greatly enhanced in atherosclerosis.
Several dietary factors are thought to influence the incidence of coronary artery disease, most notably cholesterol. As discussed in Chapter 12 LDL cholesterol is bad cholesterol, whereas HDL cholesterol is cardio-protective. Relatively higher HDL levels are seen in women before menopause, which may account, in part, for lower incidence of CHD in them.
Bearing in mind the above correlations, the following measures are advised in the susceptible individuals.
1. Reduction of dietary intake of cholesterol. Cholesterol, being a product of animal metabolism, is found only in foods of animal origin; egg yolk and organ meats are extremely rich sources. In contrast, the plant products— even vegetable oils—contain no cholesterol. In view of these facts, necessary dietary modifications must be made in diet so that intake of cholesterol rich foods is reduced.
2. Change in lifestyle in such a way that adequate physical exercise becomes part of daily routine.
3. Increased dietary intake of fibres, although exact role of high-fibre diet on coronary artery disease is still controversial. Mode of action of fibres and their beneficial effects have already been discussed in this chapter.
4. Increased intake of dietary antioxidants, such as vitamins C, E, and ß-carotene. These compounds chemically inactivate the oxidative radicals derived from molecular oxygen and hence protect LDL against oxidation. This offers protection against heart diseases as confirmed by certain studies which brought out that daily intake of 100 International Units of vitamin E (RDA 15 IU) may reduce death from coronary artery disease by approximately 40%.
5. Hypocholesterolaemic drugs are usually recommended in middle-aged men with very high plasma cholesterol levels.
Type of fatty acids consumed have a significant bearing on serum cholesterol levels. For example, the saturated fatty acids are harmful because tend to elevate serum cholesterol levels, especially the LDL fraction. Therefore, the foods rich in these fatty acids, such as meat products and some vegetable oils like coconut and palm oil, must be avoided. It is interesting to note that all saturated fatty acids do not have cholesterol raising effects: stearic acid (18-C) and short-chain saturated fatty acids (< 10-C) tend to raise serum cholesterol to a lesser extent than the 12-C to 16-C saturated fatty acids.
Exercises
Essay type questions
1. What is meant by balanced diet? Explain the nutritional principles involved in its formulation. Formulate the balanced diet requirement for a 72 kg adult of 40 years.
2. What are the components of energy expenditure? Discuss various factors that effect BMR.
3. Explain importance of proteins in human nutrition. Why is SDA value of proteins higher than that of other major nutrients?
4. Discuss the protein-energy malnutrition, comparing features of marasmus and kwashiorkor. Mention biochemical findings in kwashiorkor.

 One gram of carbohydrates and proteins provides 4 kcal each, whereas lipids are energy dense, providing 9 kcal per gram. Energy is used to do work and to maintain integrity of the body.
One gram of carbohydrates and proteins provides 4 kcal each, whereas lipids are energy dense, providing 9 kcal per gram. Energy is used to do work and to maintain integrity of the body.