CHAPTER 15 Components of the nursing process
• Discuss the five steps used in the nursing process
• Identify actual and potential client issues
• Explain the benefits of using a client-centred approach
• Differentiate between subjective data and objective data
• Describe the process for taking a nursing history
• Plan Specific, Measurable, Attainable/Achievable, Realistic/Relevant, Time bound (SMART) goals
The nursing process is a systematic problem-solving approach which enables nurses to plan for and provide care for clients. Through a process of clinical judgment and critical thinking, the nurse is able to identify the client’s actual or potential problems and to formulate a nursing care plan based on the five dynamic and interrelated components of the nursing process. These components are: assessment, identification, planning, implementation and evaluation. This chapter examines the five components of the nursing process and provides nurses with a framework for care planning, which is systematic and methodical.
In essence, the nursing process is a cyclic process of steps used to identify actual or potential client problems or needs. It enables nurses to plan and implement the nursing interventions required to care for a client and to evaluate the effectiveness of those interventions. By using critical thinking skills in a logical sequence, nurses are able to make informed clinical judgments about clients’ nursing needs in a systematic manner.
It was my second week on placement in the Rehabilitation Unit when Aneta the RN asked if I would like to admit the new client, Mrs Forster, who was arriving that afternoon. She was being transferred to us for rehabilitation after a fractured neck of femur. The orthopaedic ward had emailed her discharge information to the ward administrator, so I read through that as a way to get to know Mrs Forster before she actually arrived.
AN OVERVIEW OF THE NURSING PROCESS
The nursing process provides an organised framework of actions. It consists of five interrelated components that allow the nurse to use critical thinking skills to collect, review and validate client data, so that they can use clinical judgment to plan, implement and then evaluate the effectiveness of those nursing interventions. The data from the nursing process is used to formulate a nursing care plan. The nursing care plan is a legal document recoding all pertinent nurse–client interactions such as assessment, identification of issues, planning, implementation and evaluation.
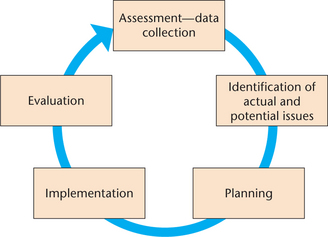
It is important for the nurse to recognise that the nursing process is both continuous and cyclical, relying on the step preceding and the step following. Figure 15.1 is a diagrammatic representation of the nursing process.
As clients’ needs are continually changing, it is essential to have ongoing evaluation, revision and updating of the nursing care plan. Through the continuous evaluation of care, nurses are in a position to improve client care (Crisp & Taylor 2009).
Assessment
The first component of the process is client assessment. This is the process of obtaining data about a client, through a variety of methods. The purpose of obtaining this information is to identify areas in which nursing interventions are required. The data may be obtained directly from the client, from others of significance to them, from other members of the health team and from the client’s past or present medical and nursing records. This data needs to be actual, factual, complete and relevant in nature. It may be either subjective or objective.
Subjective data includes the client’s unique perceptions, ideas, experiences and sensations about an issue that they share with the nurse. For example, a client may supply information about their sensations of pain in their lower abdomen; they may say it feels as if it is gripping or burning and that it is increasing in intensity.
Objective data consists of information that can be observed or measured directly by the nurse. For example, while a client may report the location and intensity of abdominal pain (subjective data) an increase in blood pressure, pulse and respirations recorded by the nurse provides measurable objective data.
A variety of methods are used to obtain both subjective and objective data, including taking a nursing history, carrying out a physical examination and observations and reviewing laboratory and diagnostic tests. However the process usually commences with the nurse interviewing the client. If the nurse is able to, they should make themselves as familiar as possible with the client’s past and current nursing and medical history. The nurse should review the latest laboratory and diagnostic results, as these could help guide the assessment interview and can provide additional prompts for the nurse in talking with the client.
Most importantly, the nurse should work towards establishing an effective therapeutic relationship with the client, which enables the client to trust the nurse. By adopting a client-centred approach, the nurse works with the client as a partner. This partnership approach is based on mutual respect and a sharing of power. It is underpinned by the client being actively empowered and supported to make informed decisions about their healthcare.
The nursing history
A nursing history is gained by talking with the client and/or significant other(s) by way of a structured interview. It enables the nurse to initiate a plan of care, one that can be developed to meet the unique needs of the client. The information gained is documented and used as part of the data collection. How this data/information is recorded is determined by the individual healthcare facility. For example, it could be through written words or direct input into a computer client management program or electronic medical record (EMR).
Through the use of effective interviewing skills, the nurse is able to obtain information about the client’s current and past health problems, their lifestyle, activities of living and their psychosocial history. A nursing history centres on the client’s description of their physical, psychological and emotional reactions to their healthcare needs and on the resultant actual and potential changes to their lifestyle. A nursing history:
• is the first stage of problem solving and planning for immediate and long-term client care
• establishes an information base on which nursing diagnoses and plans for care can be built
• helps the nurse to initiate a therapeutic relationship with the client and enables the nurse to observe the client from a verbal and non-verbal communication perspective
• provides clients with an opportunity to discuss their feelings about themselves and their health problems
• helps to reveal any past, present and potential issues that may require nursing intervention
• helps clients to remember certain aspects of their health that may have been forgotten or omitted
• provides a written framework in which to record information about the client’s physical, functional, social, psychological, spiritual and emotional state
• identifies personal strengths and weaknesses, health risks such as hereditary and environmental factors, potential and existing health problems and what the person does to maintain a healthy lifestyle (Dempsey et al 2009).
A nursing history should be obtained as soon as possible after the client’s admission to the healthcare agency and should be conducted, when feasible, by the nurse with primary responsibility for planning the client’s care. A culturally sensitive approach needs to be taken and the nurse should reflect on any cultural considerations; for instance, the client may want to be accompanied by their partner or other family members and have them remain with them throughout their healthcare journey.
Before beginning the interview the nurse must explain its purpose so the client can understand why certain questions will be asked. The interview setting should be quiet and private for the client to feel comfortable about discussing personal details. If a client is unable to communicate effectively an appropriate aid must be utilised. This may include the use of an interpreter or communication aids such as visual cues and writing pads. An interpreter must be arranged prior to the nursing history being obtained if required; it is not acceptable practice to utilise family or friends in this setting. It is important to record on the nursing assessment form what aids were utilised to obtain the client assessment information. It is essential that nurses safeguard the client’s right to privacy, by carefully protecting any sensitive information gained in the nursing history (Crisp & Taylor 2009).
The process of history taking will vary depending on the age of the person. It is usual for a parent or other adult to provide information for a young child, but older children may be able to give their own factual account. It is important for the nurse to use terminology that the child can easily understand. Additionally, questions about reaching milestones and immunisations should be included. Likewise, in any interaction with an older person, as a communication and understanding assessment, observe for signs that the client can both see and hear you properly (O’Shea 2010).
It is essential that any information obtained during the interview is documented accurately and concisely, as the nursing assessment form is a legal document that needs to be retained for future reference together with other documentation. The basic information, which should be obtained in a nursing history, includes:
• Client demographics, age, gender, marital status, next of kin or significant other(s), preferred name of address
• Reason for requiring medical/nursing intervention and the client’s understanding of why they are there
• Past and current medical history
• Cultural considerations such as dietary requirements, the use of traditional healing practices and specific religious practices
• Current medications and treatments including any allergies
• The use of any aids or prosthetics
• Baseline information regarding their normal level of ability to carry out the activities of daily living (breathing, eating and drinking, maintaining a safe environment, communicating, eliminating, personal hygiene and dressing, controlling body temperature, mobilising, expressing sexuality, working and playing, sleeping and concerns about death and dying).
• Social data including accommodation and home circumstances, education, occupation, religion
• Personal habits including alcohol usage, smoking or the use of illegal drugs.
Physical examination and observation
Traditionally medical officers have been the profession performing the initial physical examination of the client. However, increasingly this is being carried out by nurses. A physical examination uses the techniques of inspection, palpation, percussion and auscultation to detect any abnormalities that may provide information about the client’s health. This information is recorded in the client’s notes and may be relevant to the planning and implementation of nursing care.
Observation of the client is performed by the nurse during the interview and requires a head-to-toe assessment. This relies on the nurse using all their senses and utilising effective communication skills. By asking open-ended questions, such as ‘Can you describe the pain you have in your chest?’ the client is able to elaborate their answers. It helps the client to tell their story, expressed in their own words, which allows a greater depth of information to be collected. Closed questions, such as ‘Do you get short of breath?’, elicits either a yes or a no answer, or a more limited response, and provides little opportunity for the development of a therapeutic relationship between the client and the nurse. Chapter 6 elaborates further on the importance of communication in the therapeutic relationship. The student can refer to Chapter 17 for a more in-depth discussion of the health assessment.
Clinical pathways
Some healthcare agencies use clinical pathways as a communication tool between healthcare clinicians. A clinical or care pathway is a document which outlines a standardised, evidence-based multidisciplinary management plan. The pathway identifies the appropriate sequence of clinical interventions, time frames, milestones and expected outcomes for a common client group. The clinical or care pathway identifies the expected course of events for the majority of clients (approximately 70%).
As there will always be exceptions, the pathway should be followed in accordance with the clinician’s assessment of each individual case. A process for charting by exception should be in place. Charting by exception involves the nurse only charting significant findings or exceptions to the standards or norms of the predicted care pathway for the client. See Chapter 40 for an example of a clinical pathway or Chapter 16 for more information on documentation.
Cultural considerations in health assessment
Culture may be defined as a shared system of beliefs, values and behavioural expectations that provide social structure for daily living (Dempsey et al 2009). For nurses to be able to carry out culturally safe nursing care, they need to have developed an awareness of their own cultural identity, values and beliefs and acknowledge the potential impact this can have on their interactions with clients from other cultures.
A cultural assessment allows the nurse to ask the client from another culture how they would like to be cared for, based on their individual cultural beliefs. By doing this, it provides the basis for power sharing between the client and the nurse and acknowledges the value of client diversity. Nurses should have an awareness of a wide range of different cultures, but it is equally import that the nurse does not stereotype the client as part of the cultural assessment. For more information on cultural diversity, see Chapter 8.
Laboratory and diagnostic tests
Laboratory and diagnostic tests, which are the most objective form of assessment data, provide another source of information about the client. Both subjective and objective data are required to create a comprehensive assessment. For example, during the nursing interview a client may reveal that they feel constantly tired (subjective data). The nurse visually observes that the client looks extremely pale (objective data) and the laboratory test results indicate that their haemoglobin level is below normal (objective data). In this situation, the laboratory results (low haemoglobin level) verified the personal feelings of the client (feeling tired) and the visual observations of the nurse (client looks pale).
While it is usually the role of a medical officer to order laboratory and diagnostic tests, increasingly this is becoming part of advanced practice nursing roles, such as the nurse practitioner. A nursing role is to ensure that the client understands why they are having the test and to prepare and support them for the test. This may be by providing client education or preparing them by keeping them nil by mouth for tests such as fasting blood sugar tests or some abdominal ultrasound scans. See Clinical Scenario Box 15.1 for a case study of the assessment phase.
Clinical Scenario Box 15.1
The assessment phase
Mrs Francesca Brown is a 67-year-old lady admitted to the orthopaedic ward at 1400 hours on 21 May for surgery the following day. Registered Nurse Judith has been allocated to admit and care for Mrs Brown on the afternoon shift. Mrs Brown is planned to have a right total knee joint replacement (RTKJR), due to severe osteoarthritis. Both knees are swollen and crepitus can be heard when the knee joints are moved. The right knee is the more severely affected and the most painful. Judith introduced herself and explained that part of the admission process was to obtain a nursing history, so that the information given could be utilised to develop a care plan for Mrs Brown.
Judith drew the curtains around the bed, sat down and began to talk with Mrs Brown. She began by asking Mrs Brown what name she preferred to be known by and was informed that she would like to be known as Fran, as that was the name her late husband, family and friends called her. During the 20-minute discussion with Fran, Judith obtained and recorded the following information:
• Fran’s husband had been 15 years older than she. He had died 2 years ago after having a stroke 4 years earlier. She had two daughters who both lived overseas and one son, who lived locally. She was very close to her son and daughter-in-law and their two teenage daughters. She kept in touch with both daughters and their families by email and Skype.
• Fran lived by herself in the house she had shared with her husband since their marriage. The house was single level and had been adapted, so that she could care for her husband, who was non-mobile and dependent on a wheelchair. Her son saw to the garden and any maintenance the house required. Fran had one cat, which her grand-daughters would feed while she was in hospital.
• Fran had been an active member of several organisations but had given up some of her social activities over the past 18 months when she found it increasingly difficult to mobilise. She still enjoyed reading, watching television and playing mahjong.
• Fran had been a hospital client 4 times, 3 times for the birth of her children by caesarean section and 12 years ago as a day client, to have several skin lesions removed, which she said ‘fortunately turned out to be benign’.
• Fran’s past health problems included a deep vein thrombosis and a fractured wrist. She was currently being treated for hypothyroidism and osteoarthritis.
Her current admission is to have a RTKJR. Both of Fran’s knees show severe arthritic changes and she is due to have her left knee joint replaced once she has recovered from this first surgery. Over the past 2 years the pain in her knees has increased and despite being well supported by her general practitioner (GP), the anti-inflammatory medication was becoming ineffective. The large doses of analgesia she was taking often made her very constipated. Her GP had referred her to an orthopaedic surgeon, who recommended bilateral knee replacement surgery. Fran did not express any anxiety over the surgery, as she was looking forward to the benefits, especially when both knees had been operated on and she was no longer in pain or her mobility restricted. All she asked for was ‘a good result’. Fran stated, however, that she had some worries about the anaesthetic. This was because each time after giving birth, she had had issues with vomiting, which the medical officers thought was related to the anaesthetic. Judith asked Fran to mention this to the anaesthetist who would see her later that day.
Fran found it difficult to stand for longer than 5–10 minutes at a time and on a ‘good day’ could manage to walk around the local supermarket. She stated she had a good appetite and there was nothing she didn’t like to eat; she ate a lot of fruit during the day to help avoid constipation. She usually went to bed at about 2230 hours after taking her night-time doses of analgesia and often did not sleep well due to pain.
Fran appeared to be generally healthy. She wore glasses for reading and watching television and had no issues with hearing
Recordings of Fran’s vital signs showed that her temperature was 37ºC, pulse 76/min and regular, respirations18/min, blood pressure 130/70 mmHg. She weighed 64 kg and her urine sample showed no evidence of any abnormalities.
After the interview with Fran, Judith looked at her medical history to see if there was any further information relevant to the delivery of nursing care. She observed that the medical officer who had examined Fran had not detected any additional pathological abnormalities. The results of her chest x-ray, electrocardiogram and full blood examination were within acceptable ranges. Judith made a note for the anaesthetist, alerting him to the issue of Fran vomiting postoperatively.
Identification of client issues
The second component of the nursing process is the identification of client issues. This involves using all information gained at the assessment stage to identify actual or potential issues. These issues are from the client’s perspective and are constructed in collaboration with the client.
Actual issues are those that the client is currently experiencing. For example, from the assessment data collected from Mrs Brown (talking with her, observing her mobilise and reading her clinical records) it is clear she has pain in both knees. For Mrs Brown, pain is an actual issue. Potential issues are those that the client does not currently have, but may be at risk of developing. Because Mrs Brown is in pain she is taking regular analgesia. A risk from some analgesia such as codeine is constipation; hence for Mrs Brown a potential problem for her could be constipation. Though it is not an issue she has at present, it is one that nursing staff should be aware of. By taking preventative actions, nursing staff can reduce the risk of actual problems developing for patients. This is especially important when patients are unable to make those decisions themselves. This could be due to lack of knowledge about the risks or because the patient is dependent on nursing staff.
Once actual and potential issues are identified the nurse and the client can work together to plan the care that needs to be implemented.
Planning
The third component of the nursing process is planning. After the client’s issues have been identified, the nurse plans the care that needs to be implemented to achieve the outcomes required. This is accomplished by setting client-centred goals, prioritising those goals, determining what nursing interventions are required to meet those goals and updating the care plan.
Setting SMART goals
Ideally nurses and clients work together to determine what the goals and desired outcomes of the nursing interventions will be (Hood 2010). Goals establish the framework for a nursing care plan and are the stages that need to be met to reach a desired outcome. Hence, for each nursing problem the nurse, in conjunction with the client, sets the goals to be achieved. A short term goal may be one that is expected to be achieved in a relatively short time frame such as hours or days, while a long-tem goal is one to be achieved in the future, perhaps in several weeks or months.
A goal needs to be something quite specific and unambiguous (Werle Lee 2010). An acronym to assist in writing goals is SMART:
(See Clinical Interest Boxes 15.1 and 15.2 for examples.)
CLINICAL INTEREST BOX 15.1 Not using SMART goals
Goal: After knee surgery Mrs Fran Brown will be able to mobilise
 |
||
 |
||
 |
||
 |
||
 |
CLINICAL INTEREST BOX 15.2 Using SMART goals
Goal: After knee surgery Mrs Fran Brown will be able to mobilise with a walking frame 20 metres across the ward, 2 days postsurgery
 |
||
 |
||
 |
||
 |
||
 |
SMART goals are used to express behaviours that are observable and measurable: in that way it is easy to determine if the goal has been met or not. Following knee surgery a client may have the long-term goal to return to their normal level of being able to mobilise fully independently. However, before the client is able to return to their normal state, short-term goals may need to be set to measure their progress towards once again being fully and independently mobile.
Take, for example, ‘After knee surgery Mrs Brown will be able to mobilise’. This goal does not define if Mrs Brown will be able to mobilise independently or with assistance, does not tell the nurse how far Mrs Brown expects to be able to mobilise or within what time frame.
Using the SMART approach this goal can be defined as ‘Mrs Brown will be able to mobilise with a walking frame, 20 metres across the ward, 2 days after surgery’. It is:
• Specific; the goal states exactly what Mrs Brown is to achieve, which is to mobilise with a walking frame
• Measurable; the goals states how far the client has to mobilise, which is 20 metres
• Attainable/Achievable; using clinical judgment this goal is attainable for this particular client, based on their expectations and clinical presentation
• Realistic/Relevant; with a long-term goal of returning to being fully and independently mobile, a short-term goal such as this is both realistic and relevant to Mrs Brown’s recovery
• Time bound; the goal clearly indicates that there is a time frame of two days after surgery by which this is the expected outcome.
By using SMART goals it is easy to establish when these goals are achieved. In a similar way when goals are not being achieved, the goals can be re-established between the client and the nurse. Goals are not achieved for a number of reasons which may include the development of complications or unforeseen events.
Priorities
Priorities are established after specific goals have been set, by grading them in order of importance. Basic physiological needs, such as the need for oxygen, nutrition or water, are given priority over the other needs. However, in using a client-centred approach to prioritising the goals, the nurse works with the client to establish which goals the client perceives as being of most importance and value to them after these most basic of needs. From this discussion high-priority goals that require immediate attention take precedence over low-priority goals that may not need to be attained as quickly.
Determining nursing interventions
This step involves selecting the activities or interventions that are expected to help the client achieve the set goals, which in turn create the expected or desired outcomes. All possible options need to be discussed in consultation with the client, and time given for them to be able to make informed decisions about their healthcare needs. Critical thinking and good decision-making skills assist the nurse to select the most appropriate nursing activities or interventions to discuss with their clients. Appropriate nursing interventions must be based on sound clinical judgment using an evidence-based practice approach to problem solving. Evidence-based practices are those that have been researched and shown to provide the best possible outcome for clients. After a decision has been made by the client, in consultation with the nurse and sometimes with other members of the multidisciplinary team, the proposed actions or interventions to be implemented are formulated into statements and written in the nursing care plan. For example, one selected nursing activity may be for the nurse to assist the client to shower each morning.
All proposed nursing interventions must be written specifically and in adequate detail to enable all nursing personnel to carry them out correctly. Interventions may consist of activities that the nurse will perform, or actions to be taken by the client with or without assistance from the nurse; however, all actions should be client and outcome focused.
Nursing care plans
A nursing care plan is a document developed by the healthcare agency to record all aspects of the client–nurse relationship. The structure of the care plan may vary between health agencies. Some agencies use paper records while others have computerised care plan, electronic medical records and client management systems. Nurses need to be familiar with the nursing care plan and all other documentation used within the healthcare agency in which they are working. Nursing care plans form part of the client’s healthcare records and can be requested and used in legal situations. Nurses need to adhere to the legal and ethical guidelines for documenting. (For more information see Chapter 16.)
Nursing care plans may vary in structure but the basic principles remain the same. The nurse should be able to clearly identify:
Some forms of nursing care plans use the headings of the nursing process and are set out in a table using columns. As mentioned previously, some health agencies are using clinical or care pathways which outline predetermined care plans, interventions and goals for specific diagnosis related groups of clients.
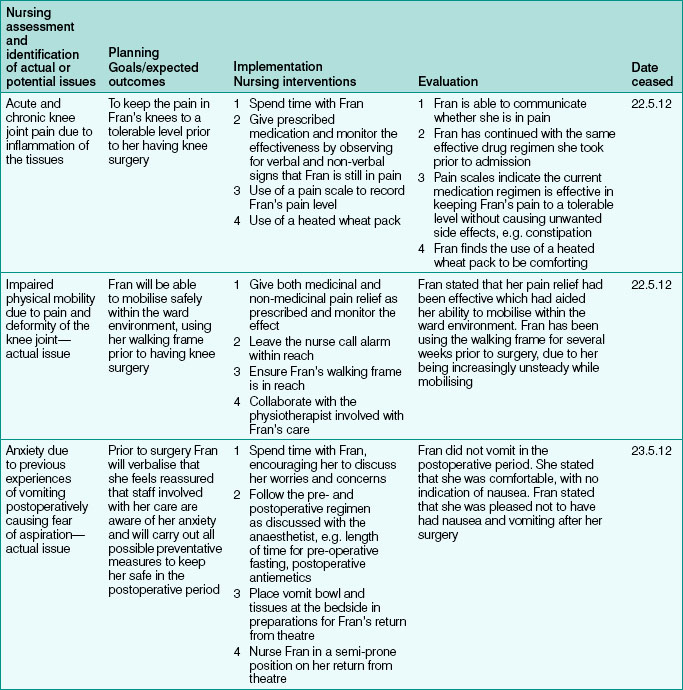
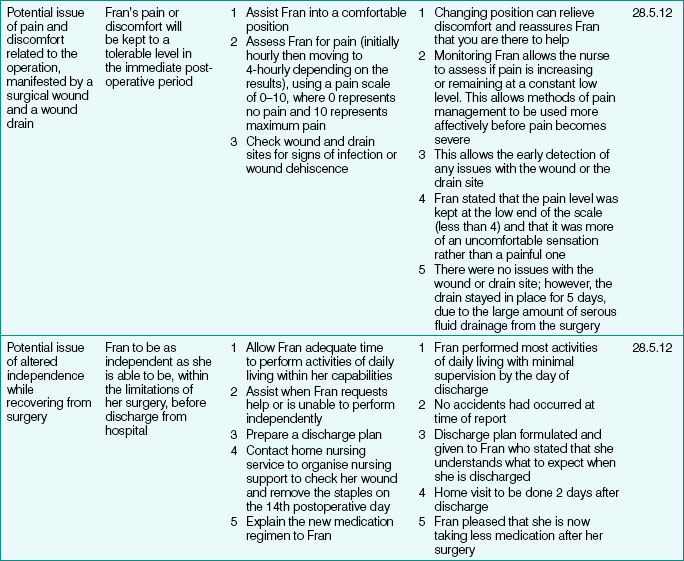
While the structure of a nursing care plan may vary between healthcare settings, the principles of care planning remain the same. A correctly formulated nursing care plan facilitates the coordination and continuity of care for the client. Clinical Interest Box 15.3 is an example of a fully documented care plan, using the case study of Mrs Brown.
Implementation
The fourth component of the nursing process is implementation. Implementation means putting the nursing care plan into operation by using nursing actions and interventions. This is the performance of selected nursing actions/interventions to help the client achieve the goals they set. All actions and interventions should utilise the latest evidence-based practices. The nurse needs to identify and evaluate current literature and research and incorporate the findings into the client’s care, as a means of ensuring quality care (Farrell & Dempsey 2011).
The client’s needs are reassessed continuously during the implementation stage so that any new needs can be identified and the nursing care plan modified or adapted to take this into account. An important part of the implementation is the documentation of results, as the care plan serves as a key method of communication between inter-professional members of the healthcare team (Hood 2010). As the client’s condition changes, the nursing actions and interventions need to be reassessed and the care plan reviewed. This may mean that new goals and interventions are added to the nursing care plan and those that are ineffective may need to be modified. The process of implementation is closely linked with the final stage of the nursing process, evaluation.
Evaluation
The fifth component of the nursing process is evaluation of care. Once the planned nursing interventions have been implemented, the nurse must evaluate the results to determine whether the interventions were effective or not. Evaluation is the process of determining the extent to which the set goals have been achieved and the desired outcome obtained. It enables the nurse to monitor the effectiveness of the nursing actions, as documented in the care plan, and to determine if the care plan was a success or not. The success of the care plan can be determined by comparing the initial desired outcomes with those outcomes that were eventually achieved.
Evaluation requires an examination of the results of the interventions, assessing the client for possible side effects and adverse reactions to the nursing interventions and analysing the results. Analysis involves determining whether the client has improved, deteriorated or shows no change.
Based on the data obtained from the evaluation of the care plan, nurses use their clinical judgment to determine what actions or interventions are required next. Evaluation allows the nurse to revise and, if necessary, modify or change the plan at any stage. If the set goals have been achieved, the plan is deemed to be successful and the nursing interventions can usually be changed. If the goals have not been achieved, the client’s needs must be reassessed, new nursing diagnoses formulated and the care plan changed and re-implemented. (See Clinical Scenario Box 15.2 for a case study of the evaluation phase.)
Clinical Scenario Box 15.2
Evaluation
Fran did not have any issues with vomiting postoperatively and was able to have a cup of tea and toast 4 hours after she returned to the orthopaedic ward. She had a surgical drain in situ which remained in place for 5 days as it continued to drain significant amounts of serous fluid. This delayed her discharge by 2 days. She also had a 20 cm anterior midline incision which was healing well with no signs of infection. The wound had been closed using metal staples. These were to remain in place for 14 days and the wound kept covered with a sterile dressing.
Fran experienced some pain in the immediate postoperative period but this was relieved when analgesic medications were administered. She continued to take analgesia and anti-inflammatory medication for the pain in her left knee.
Fran had been seen by the physiotherapist prior to admission and on a daily basis while on the ward. She was up and out of bed the day after surgery and able to mobilise with a walking frame and one nurse to and from the bathroom. The physiotherapist also arranged passive leg exercises.
On the third day after the operation, Fran was able to mobilise with the zimmer frame, but without a nurse to assist. Her mobility continued to improve and by discharge 7 days after the surgery, she was mobile with a walking stick.
Also by discharge, Fran was no longer taking as many medications. This was because her right knee had always been much more painful than the left and she was able to discontinue some of the stronger analgesia.
Fran’s family had visited her each day and one of her grand-daughters was going to stay with her once she was discharged. The nursing staff on the ward arranged for a district nurse to call to check her wound and to remove her staples 2 weeks after the operation.
Fran was given a rehabilitation program by the physiotherapist that she was to continue over the next few weeks until she was seen again by the orthopaedic surgeon at an outpatient appointment 4 weeks after discharge.
Throughout the process of implementation and evaluation, nursing staff constantly assessed Fran.
While evaluation is proposed as the fifth and final component, it is actually performed continuously throughout the nursing process. It is the most important method of determining the effectiveness of a nursing care plan. The effectiveness of a nursing care plan can also be determined by another method of evaluation, a nursing audit. A nursing audit is a thorough review of a client’s journey to evaluate the overall nursing care received by a client in relation to outcomes achieved. An audit is generally performed by an experienced nurse who is external to the unit carrying out the nursing care, or an external committee. Each healthcare agency develops its own nursing audit form, usually a checklist, which includes specific criteria for each category of care. This regular review of information in client records provides a basis for evaluation of the quality and appropriateness of the care provided in an institution (Crisp & Taylor 2009).
Summary
The nursing process forms the basis for all nursing practice. It is a cyclic process that relies on the five interrelated components of assessment, identification, planning, implementation and evaluation. The nursing process provides nurses with a systematic method of client problem solving, which requires the nurse to use critical thinking and clinical reasoning skills to develop a plan of client care based on evidence-based nursing practice.
1. Mrs Singh is a 46-year-old married woman with two grown-up children, and four grandchildren, whom she looks after several times during the week. She also cares for her elderly mother-in-law. She is dressed in a traditional Indian sari and accompanied by her husband. She looks anxious and appears to rely on her husband to answer the questions being asked. She has a history of hypertension. She is being admitted for a hysterectomy.
References and Recommended Reading
Carpenito-Moyet LJ. Nursing Diagnosis: Application to Clinical Practice, 12th edn. Philadelphia: Lippincott Williams & Wilkins, 2008.
Crisp J, Taylor C. Potter & Perry’s Fundamentals of Nursing, 3rd edn., Sydney: Elsevier, 2009.
Dempsey J, French J, Hillege S, et al. Fundamentals of Nursing and Midwifery, A person-centred approach. Philadelphia: Lippincott Williams & Wilkins, 2009.
Farrell M, Dempsey J. Smeltzer & Bare’s Textbook of Medical-Surgical Nursing, 2nd edn. Philadelphia: Lippincott Williams & Wilkins, 2011.
Glass N. Interpersonal Relating. South Yarra: Palgrave Macmillan, 2010.
Hood LJ. Leddy and Pepper’s Conceptual Bases of Professional Nursing, 7th edn. Philadelphia: Lippincott Williams & Wilkins, 2010.
Jarvis C. Physical Assessment and Health Examination, 5th edn. Canada: Elsevier, 2008.
O’shea Y. Principles of the consultation and client assessment. Practice Nurse. 2010;39(3):17.
Werle Lee KP. Planning for success: setting SMART goals for study. British Journal of Midwifery. 2010;18(11):744–746.