CHAPTER 22 Medications
At the completion of this chapter and with further reading, students should be able to
• Identify the different formulations of medications
• Identify a drug by its three names (generic, trade and chemical names)
• List the drug administration routes
• Discuss factors affecting drug absorption
• Define ‘first-pass metabolism’ and discuss its impact on drug dosage
• Discuss the role of plasma proteins in drug distribution
• Compare enzyme induction and enzyme inhibition
• List the organs involved in drug excretion
• Discuss the reasons for therapeutic drug monitoring
• Define drug action, desired outcome, side effects, toxic effects, allergic reaction and drug interactions
• Discuss the legal and other responsibilities of the Enrolled Nurse (EN) regarding drug administration
• Demonstrate an ability to correctly calculate drug dosages
• Demonstrate knowledge of the correct preparation and administration of: subcutaneous, intramuscular, intradermal and intravenous injections; topical skin preparations; oral preparations; ophthalmic, otic and nasal drops; vaginal instillations; rectal preparations; and inhalers.
• Demonstrate an understanding of the actions of the different drug groups in order to monitor drug effectiveness
• Show an understanding of safe handling of hazardous substances
• Discuss the importance of discharge planning and education in client compliance with drug therapy
The use of medication is an important part of many clients’ treatment regimens. It is therefore vital for the nurse to have both the knowledge and the skills to administer medications safely and correctly. Administering medication is one of the nurse’s most important responsibilities and should be treated with the importance it deserves. It is not merely another task to be completed quickly before another is undertaken. Medication administration offers nurses the opportunity to increase their knowledge and skills, to observe the client for expected and unexpected actions and to ensure that clients have been adequately educated about medications. The topics included in this chapter provide the nurse with a basis for being equipped to safely and competently administer medications to clients.
After Mum died, Dad remained well and relatively independent. He grew his vegetables and tended his chooks. Dad was on blood pressure tablets and another one for his heart. He knew when to take them and had his routine—he would put the coffee on, feed the chooks then have breakfast and take his tablets. Then he developed a hernia which eventually needed to be operated on. Dad became really confused when he was in hospital and it wasn’t helped because the nurses gave him his medications at a different time to what he was used to. When he came home from hospital, it took Dad ages to get back into his old routine. He couldn’t remember when to take his medicines or, sometimes, wouldn’t remember if he had taken them at all. I was scared that he was taking too many or not at all and would end up having a stroke! For a while I thought we were going to have to look for a nursing home. But then Dad came good, the local pharmacist suggested a Dosett box, and now, everything is back to normal.
PHARMACOLOGY
‘Pharmakon’ is the Greek word for drug, and pharmacology is the study of the actions, uses and adverse effects of drugs. The definition of ‘drug’ is ‘any substance that alters the structure or function of a living organism’ (Kester et al 2007:1). The term drug can be further divided into medicinal drugs (or medications), which are substances used in the treatment, prevention and diagnosis of a disease; and non-medicinal drugs (or social drugs), which are substances used for recreational use and include caffeine, alcohol, nicotine, cannabis, heroin and cocaine. The distinction between the two is not always clear cut, as some non-medicinal substances can be used in a medicinal way (e.g. caffeine is included in some preparations to treat migraine) and some medicinal substances can be used in non-medicinal ways (e.g. opioid analgesics such as pethidine and morphine can be used recreationally for their mind-altering properties). In the general community, however, the term ‘drug’ tends to be associated with non-prescription or illicit substances. The term ‘poison’ refers to ‘any substance that irritates, damages or harms tissues’ (Kester et al 2007:1). However, if medicinal drugs are given at high doses, their effects will be similar to a poison. Over-the-counter (OTC) medications are those that are non-prescription drugs and are generally used for short term, self-limiting illnesses such as headache, heartburn and constipation. OTC medications also include vitamins, minerals and herbal drugs and remedies (e.g. St John’s wort, ginseng) and, unfortunately, many people consider them to be safe because they are natural. However, many herbal drugs and remedies interact with prescription medications (e.g. St John’s wort interacts with warfarin, increasing its metabolism) and non-prescription medications such as aspirin and ibuprofen can cause gastrointestinal bleeding and must only be taken at recommended doses.
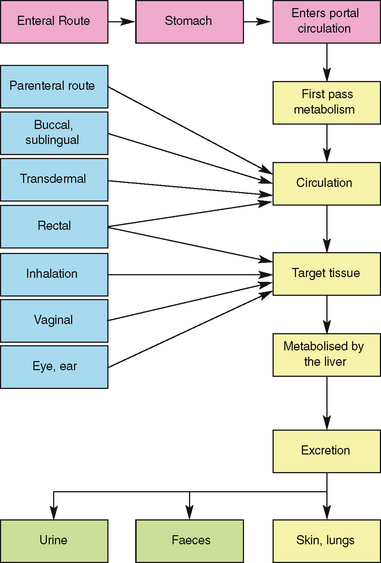
Pharmacology can further be subdivided into pharmacokinetics, which is the way the body affects the drug with time (e.g. absorption, distribution, metabolism and excretion), and pharmacodynamics, which are the effects of the drug on the body (e.g. actions and side effects). Before considering these two areas of pharmacology, it is important to consider drug nomenclature, as well as drug formulations and administration routes.
Drug nomenclature
The nurse should be aware that each drug has various names—its chemical, generic and trade (brand or proprietary) names. The chemical name provides an exact description of the drug’s chemical composition. This is usually only used by chemists and pharmacologists. Occasionally a drug’s generic name may describe its chemical compositions, as with lithium carbonate or potassium chloride.
The generic name is given by the manufacturer who first develops the drug. Even generic names are not standardised and nurses should be careful when using textbooks published in countries other than the one where they are practising nursing. Examples of different names used in different countries include adrenaline (Australia) = epinephrine (US), pethidine (Australia) = meperidine (US), and paracetamol (Australia) = acetaminophen (US). Generic names are written with a lower-case first letter. Strictly speaking, drugs should be prescribed using their generic rather than trade name (e.g. cephalexin rather than Keflex), however not all prescribers will do this. Generic prescribing avoids confusion as some trade names are similar; it also assists in reducing costs to the consumer (as costs can vary dramatically between brands). In recent times, the Pharmaceutical Benefits Scheme (PBS) has allowed brand substitution for tablets of the same dose, unless the prescriber has ticked ‘brand substitution not permitted’ on the prescription form (Bryant & Knights 2011). While brand substitution can save the consumer money, it can also cause confusion as the drug may appear different (e.g. colour (e.g. 40 mg frusemide tablets can be white (Uremide) or yellow/cream (Lasix)), shape of tablet, packaging) and could result in the person taking more than one form of the same drug.
The trade (brand or proprietary) name is the name under which a manufacturer markets a drug and is copyrighted to that particular drug and restricts others from using the trade name (and hence, multiple names for the same generic drug). Examples includes the diuretic frusemide, marketed as Urex, Lasix, Frusid and Uremide and antibacterial agent amoxicillin marketed as Alphamox, Amoxil, Cilamox and Maramox. Trade/brand names are written with an initial upper case letter.
Drug formulations and administration routes
Drugs are given by two general methods: enteral and parenteral administration. Enteral administration involves the gastrointestinal tract. Methods of administration include oral, sublingual (dissolving the drug under the tongue) and rectal. Parenteral routes involve all routes other than the gastrointestinal tract. They include intravenous, intramuscular, subcutaneous, topical, intramuscular, intranasal, intradermal, intrathecal, inhalational, vaginal, endotracheal, umbilical and intraosseous. A drug may be presented in a variety of forms (Table 22.1, Fig 22.1) and administered via several different routes.
| Capsule | Gelatine container enclosing a drug in liquid, powder or granule form |
| Tablet | A drug mixed with a base compound and compressed into a variety of shapes. Tablets are sometimes coated, which delays release of the drug until the tablet reaches the intestine. Tablets are coated if the drug could cause gastric irritation or if it would be destroyed by gastric juice. Another form of tablet is ‘slow release’ (or sustained release), which contains a drug that is released over a prolonged period |
| Granules | Small rounded pellets that are usually coated |
| Lozenge | Small tablet containing a medicinal agent in a flavoured fruit or mucilage base, which dissolves in the mouth to release the drug |
| Mixture | Aqueous vehicle in which drugs are dissolved or suspended |
| Suspension | Liquid in which insoluble particles of a drug are dispersed |
| Elixir | Sweetened, flavoured alcoholic solution containing a drug |
| Linctus | Sweetened syrup containing a drug |
| Tincture | Alcoholic solution containing a drug |
| Emulsion | Mixture of oil and water containing a drug |
| Syrup | Concentrated sugar solution containing a drug |
| Cachet | Envelope of rice paper that encloses a drug |
| Injection | Sterile aqueous or oily solutions and suspensions containing a drug, which are administered parenterally |
| Suppository | Solid preparation containing a drug, which melts when inserted into the rectum |
| Pessary | Solid preparation containing a drug, which is administered vaginally |
| Drops | Aqueous or oily solution containing a drug. Drops may be instilled into the eye, ear or nose |
| Cream | Aqueous or oily emulsion for topical application |
| Ointment | Semi-solid greasy preparation for topical application |
| Paste | Similar to ointment but contains a high proportion of powders. Pastes have a very stiff consistency and will adhere to lesions at body temperature |
| Liniment | Oily or alcoholic preparation for topical application |
| Paint | Liquid preparation for application to the skin or mucous membranes |
| Lotion | Aqueous, alcoholic or emulsified vehicle for topical application |
| Powder (dusting) | Medicated substance for topical application |
Routes of administration of drugs include:
• Oral (PO)—the most convenient, least expensive way of administering drugs as most drugs are available in oral preparations. Effects are often not seen for 30 to 45 minutes after administration. Major disadvantages are slow absorption, irritation to the gastric mucosa, possible unpleasant taste, inability/decreased absorbency in critically ill clients as the gut may not be functioning, in those who are vomiting or are unable or unwilling to swallow (e.g. unconscious person, child, person with dementia)
• Orogastric/nasogastric/percutaneous endoscopic gastrostomy (OG/NG/PEG)—this route is generally used for oral medications when the client already has the tube in place for other reasons. (See Ch 28 for information about nasogastric and PEG tubes.)
• Intravenous (IV)—drug delivery IV is rapid, as the absorption phase is bypassed. It is the route of choice in an emergency situation. Other advantages include availability (e.g. the unconscious person), large quantities can be given over a long time and constant blood levels can be maintained. However, one disadvantage is that due to rapid drug delivery it is very difficult to retrieve if a mistake is made. Other disadvantages include pain/discomfort, irritation, need for aseptic technique and unsuitability for self-administration
• Intramuscular (IM)—the drug is injected into the muscle tissue, from which it is absorbed into the bloodstream. Drug absorption IM is generally fast because of the vascular nature of muscle. However, this can be slowed by the addition of oily substances (termed a depot preparation). A disadvantage of this route is that administration can be painful, especially if treatment is prolonged and muscles are used repeatedly
• Subcutaneous (subcut)—medications are injected into fatty, subcutaneous tissue under the skin and overlying the muscle. Drug absorption subcut is relatively slow because of the poor blood supply in subcutaneous tissue. Adrenaline added to a subcutaneous preparation will make the absorption even slower because adrenaline causes constriction of blood vessels. Another disadvantage of subcut is that only small volumes (≤ 1 mL) can be given
• Intradermal (ID)—medications are administered into the dermis (under the epidermis). Drugs are not commonly given via this route. Substances such as local anaesthetics are sometimes administered intradermally and this route is used for allergy testing; for example, Mantoux tests are performed intradermally
• Intrathecal (IT)—injections are given directly into the central nervous system (CNS) via the cerebrospinal fluid, bypassing the blood–brain barrier. (See Ch 33 for an explanation of the blood–brain barrier.) Epidural injections are given into the space between the arachnoid mater and the dura mater and are often used as regional anaesthetics during surgical procedures involving the pelvic region
• Intraarticular—injections are given directly into articular joints. Examples include corticosteroids to reduce joint inflammation and radio-opaque contrast to view structures. Disadvantages to this route are that it can be painful and is often required to be done under radiological imaging to ensure that it is administered into the joint cavity
• Transdermal—drugs given via this route require low doses over long periods of time; Transdermal preparations include hormones, antiemetic agents, antianginal agents and nicotine patches
• Topical—absorption is generally very slow and preparations include antiseptics, creams and lotions. Some preparations have systemic as well as local effects, as a small amount is absorbed systemically
• Inhalation—the large surface area of the lungs facilitates rapid absorption. Agents given via this route include oxygen, anaesthetic agents, mucolytic agents and bronchodilators. A proportion of inhaled drugs will reach the systemic circulation
• Mucous membranes—some drugs administered via this route have both local and systemic effects. Drugs designed to be absorbed through the mucous membranes can be administered sublingually (SL), that is, under the tongue (e.g. sprays, lozenges) (Fig 22.2); intranasally, that is, aerosolised and instilled in the nose, where the drug is rapidly absorbed through the vascular network in the nasal tissues (e.g. sprays, drops, metered sprays); rectally (PR), where it may have both local and systemic effects (e.g. suppositories); vaginally (e.g. pessaries and creams) or via the conjunctiva of the eyes (e.g. drops and inserts)
PHARMACOKINETICS
Pharmacokinetics describes the way the body affects the drug over time and relates to the processes of absorption, distribution, metabolism and excretion (Fig 22.3).
Absorption
Absorption is the movement of a drug from the site of administration into the bloodstream. The rate and amount of drug absorbed depends on different factors including:
• Degree of blood flow to the area: a drug will be absorbed rapidly from a highly vascular area and less rapidly from poorly vascularised areas such as fat
• Solubility of the drug: to be effectively absorbed across the cell membrane, a drug should be lipophilic (fat-loving). Acidic drugs are readily absorbed in the stomach, while alkaline drugs are better absorbed in the intestine. However, because most drugs pass rapidly through the stomach, most absorption takes place in the intestine
• Route of administration: the route of administration affects the speed with which a drug takes effect. An oral medication has to undergo absorption in the gastrointestinal tract before it reaches the bloodstream and can take effect. It is therefore slower acting than if the same drug were given by injection. A drug given by injection avoids the need for absorption because it bypasses the gastrointestinal tract. The fastest effect from a drug occurs via the IV route because the drug is injected directly into circulating blood.
• Dissolvability of the medication: how fast an oral medication dissolves depends on its form or preparation. If it is already in a liquid state it will be absorbed more readily than a tablet or capsule. If the tablet is enteric coated, absorption will be delayed.
• Food: can delay the passage and therefore absorption of some drugs.
• Body surface area: some diseases can alter the rate of drug absorption; for example, diseases where gastric motility is increased (e.g. Crohn’s disease, ulcerative colitis) or decreased (e.g. diabetic gastroparesis) or malabsorptive syndromes (Kester et al 2007).
First-pass metabolism
Medication is absorbed from the gastrointestinal tract and enters the hepatic portal system, where it reaches the liver and is metabolised. Some drugs are almost entirely metabolised during this hepatic first pass, resulting in only very small amounts being available for therapeutic use. These drugs are better given via another route. An example of this is glyceryl trinitrate (Anginine), which is used to treat angina pectoris. If given orally, almost 96% is destroyed in this hepatic first-pass metabolism. Given sublingually, the drug bypasses the liver and is able to reach the target organs to have its therapeutic effect. First-pass metabolism is also the reason why oral doses and parenteral doses are not equal — giving drugs via the parenteral route bypasses the first-pass metabolism and means that smaller doses can be given to achieve the same therapeutic effect.
Distribution
After the drug has been absorbed into the general circulation, it will then be distributed to different tissues for drug action to occur. To be transported in the blood, the drug molecules become protein bound (i.e. bind loosely to blood proteins); however, there is always some unbound (or free) drug. Equilibrium exists between the bound and unbound drug but only the unbound drug molecules are able to bind with the tissue.
The blood plasma contains a variety of plasma proteins (e.g. albumin, corticosteroid-binding globulin (CBG) and glycoproteins), which are able to bind to drugs to produce a drug–protein complex. If a client has a condition which causes decreased levels of plasma proteins (e.g. liver disease, malnutrition or extensive burns) a greater portion of the drug remains unbound and is available to bind to the tissue, increasing the effects of the drug and requiring a decrease in the dose. Conversely, if there is an increased level of plasma proteins (e.g. in a client who has multiple myeloma) there is an increase in the amount of bound drug, reducing the drug’s effectiveness, requiring an increase in dose.
Drugs may also compete for the same binding site on the plasma protein when more than one drug is administered concurrently. The drug with the higher affinity (or greater attraction) will be bound and displace the other(s) from the protein-binding site, resulting in the plasma concentration of the now unbound drug increasing. For example, aspirin will displace phenytoin (an antiepileptic or anticonvulsant) from the plasma protein, resulting in an increased level of unbound phenytoin and, potentially, phenytoin toxicity. The effect is the same as giving an increased dose of the drug.
The blood–brain barrier of the central nervous system is generally very selective and allows very few drugs to pass through it. However, some conditions alter the permeability of the blood–brain barrier. For example, meningitis renders it permeable to penicillin, which it would otherwise be unable to pass through. The placental barrier is not as effective as the blood brain barrier, and many drugs are able to cross the placenta to the fetus. Drugs that can reach the fetus in this way have the potential to cause significant damage, including congenital malformations. Unless absolutely necessary, drugs should not be taken during pregnancy and especially not during the first trimester, when organ development in the fetus occurs.
Metabolism
Metabolism is the process whereby a substance is chemically altered, making it hydrophilic (water-loving) so that it can be readily excreted. The metabolism of drugs into inactive forms for excretion involves enzymes that are mainly found in the smooth endoplasmic reticulum in the liver. However, some enzymes are also found in the plasma, intestine and other organs. There are two types of enzymes involved in metabolism. During Phase I metabolism, enzymes modify the drugs by a series of chemical processes such as oxidation, reduction, hydrolysis and addition or removal of an active group from the drug molecule. During Phase II metabolism, the metabolite from Phase I, or a drug, may be directly conjugated (joined to another substance) by the enzymes, making the end product soluble for excretion.
Normally, these enzymes are present in small amounts. However, in some circumstances the amount of enzymes can alter, thereby also altering the rate of metabolism. For example, alcohol stimulates production of hepatic enzymes in habitual drinkers, resulting in the alcohol being more rapidly metabolised than in a non-drinker. This process of causing the amount of enzymes to be increased is called enzyme induction. Alcohol can also cause the levels of other enzymes involved in drug metabolism to increase, leading to the drug being more rapidly metabolised and therefore having a reduced therapeutic effect. Enzyme induction can be due to environmental pollutants, including benzopyretics in cigarette smoke, pesticides, some drugs (e.g. warfarin and phenytoin) and also some foods and natural products (e.g. cabbage, broccoli, oregano) (Kester et al 2007). Enzyme inhibition is the opposite effect and is the decreased synthesis of enzymes, resulting in the slowing down of the metabolic steps and an increased therapeutic effect. Some drugs are known enzyme inhibitors and include cimetidine, erythromycin, diltiazem, verapamil and ketaconazole. Foods and natural products which are enzyme inhibitors include grapefruit juice, St John’s wort, ginger, chamomile and liquorice (Kester et al 2007).
Drug excretion
After metabolism, drug excretion may be through the kidneys, lungs, exocrine glands (e.g. sweat glands, saliva, tears), liver and/or intestine. The chemical composition of the drug determines the organ(s) of excretion, for example, 100% of frusemide, 80% of digoxin and 50% of salbutamol are excreted in the urine. The kidneys are the main organs for drug excretion and, if a client’s renal function is impaired, the client is at risk of drug toxicity. Drugs that depend on renal function for excretion are eliminated more slowly in the very young and in older people. Gaseous compounds such as general anaesthetic agents are eliminated via the lungs. Alcohol is also partially excreted via the lungs and this is the basis of the police random breath testing to detect drink-drivers.
Some drugs, penicillin for example, are excreted unchanged in the urine, while others must undergo transformation in the liver before being excreted by the kidneys. Many drugs enter the hepatic circulation to be broken down by the liver and excreted into the bile and then into the bowel. The liver has a large metabolic capacity so, in people with liver disease, drug elimination is generally not affected until a large portion of the liver’s functional capacity is lost. Some drugs can be secreted in breast milk with concentrations of up to 1% of the total maternal dose being detected (Kester et al 2007).
Importance of therapeutic drug monitoring
For drugs to be therapeutic, a certain blood level needs to be reached and maintained. It is therefore a priority that medications are administered on time. If they are administered late, the level of the medication in the blood may drop below a therapeutic level; for example, if the level of an antibiotic is too low, it provides an opportunity for microorganisms to multiply and also potentially develop resistance. If the blood levels are too high, toxicity and serious consequences might occur. The main aim of therapeutic drug monitoring is to optimise drug therapy by achieving adequate drug levels, while minimising toxicity. This is especially important in clients at the extremes of age, infants/children and the older person. Clinical Interest Box 22.1 outlines some signs and symptoms of toxicity commonly seen in older clients.
CLINICAL INTEREST BOX 22.1 Indicators of drug toxicity in older adults
• Abnormalities in cardiac rhythm; for example, palpitations, tachycardia
• Depression of bone marrow activity (causing anaemia, leucopenia or other abnormalities of the blood)
• Increasing confusion and irritability
• Alterations in gait; for example, stumbling
• Unusual drowsiness or insomnia
• Blurred vision or other vision abnormalities
• Ototoxicity (changes in hearing and balance)
• Intolerance to heat or cold (changes in temperature regulation)
• Anticholinergic effects (ranging from dry mouth and hot dry skin to serious mental impairment and seizures)
(Adapted from Ebersole et al 2008)
Clinical Interest Box 22.2 identifies changes related to ageing that influence pharmacokinetics.
CLINICAL INTEREST BOX 22.2 Changes related to ageing that influence pharmacokinetics and pharmacodynamics
Many age-related changes to the body impact on the way that a drug may be absorbed, distributed, metabolised and excreted from the body. Because of these differences, all drug therapy should be given cautiously and monitored carefully in the older client. Age-related changes that may affect the pharmacokinetics of a drug include:
• Altered nutritional habits and ingestion of non-prescription drugs that may alter drug absorption; for example, ingestion of antacids and laxatives
• Dry mouth and decreased saliva leading to potential difficulty swallowing oral drugs
• Changes in the quantity and quality of digestive enzymes
• Decrease in gastric motility
• Decrease in intestinal blood flow
• Decreases in total body water and lean body mass and increase in body fat, which may all lead to an altered distribution of the drug, as well as potential decrease in absorption of transdermal or topical medications
• Decreased levels of plasma proteins and therefore decreased protein binding of drugs if malnutrition or acute illness is present
• Changes in liver mass and blood flow leading to reduction in the Phase I metabolism in the liver, involving the microsomal enzymes
• Alteration in bioavailability of drugs (e.g. some drugs undergoing extensive first-pass metabolism may have significant increase in availability while others may be reduced or decreased, such as ACE inhibitors available as prodrugs)
• Reduction of the liver’s ability to recover from injury such as hepatitis
• Hepatic function may also be affected by severe nutritional deficiencies
• Decreased cardiac output and reserve
• Decreased blood flow to liver and kidneys
• Congestive cardiac failure reduces both the capacity of the liver to metabolise drugs as well as the hepatic flow
• Creatinine clearance decreases with age, resulting in a longer half life of many drugs and the subsequent risk of accumulation
• Changes in response to drugs related to changes in drug concentration (related to above factors)
• Individualise the dose to the client; for example, lithium (a mood-stabilising drug commonly used to modify or prevent recurrent episodes of mania or depression (Healy 2009)), phenytoin (a drug used to control convulsive seizures and sometimes cardiac arrhythmias) and warfarin (an anticoagulant used to manage or prevent the formation of a thrombus (blood clot) (Tiziani 2010)). With each of these drugs the optimal dose is highly individual, the effects need careful monitoring and the dose may need to be adjusted periodically
• Avoid toxicity; for example, digoxin and vancomycin. Digoxin is a drug that slows and strengthens the heartbeat. Therapeutic levels of digoxin are very close to toxic levels, leaving only a narrow margin of safety. Before each dose of digoxin the client’s heart rate and rhythm should be checked and the drug withheld and the senior nurse and/or medical officer notified if the client’s heart rate is less than 60 beats/min (adult client) or there is any arrhythmia or other concern. Concerns that may indicate toxicity include slow or irregular heartbeat, anorexia, nausea, vomiting, diarrhoea, drowsiness and extreme tiredness, weakness, confusion, abdominal pain, blurred vision or visual disturbances (Tiziani 2010). Vancomycin is a powerful antibiotic reserved for the treatment of severe infections that are not responding to other antibiotics. This drug can produce severe adverse effects that include rash, itching, fever, tachycardia, nausea, vomiting, diarrhoea and, sometimes, hearing loss or kidney damage (Tiziani 2010).
• Ensure effective blood levels; for example, prophylactic anticonvulsants (antiepileptics) such as phenytoin, sodium valproate and carbamazepine, used to avoid convulsive (epileptic) seizures
• Check client compliance/concordance/adherence
• Check that comorbidities that may alter drug metabolism and elimination are not having an effect on blood levels; for example, renal impairment, hepatic failure, shock, sepsis
• Ensure that concurrent drug administration is not affecting blood levels
• Change route of administration; for example, from IV or IM to oral administration, or change dosage.
PHARMACODYNAMICS
Pharmacodynamics relates to how a drug acts on the body, including the strength and duration of its effects.
Drug action
The extent of the response to a drug depends on its concentration at the site of action, which in turn depends on dosage, absorption, metabolism and elimination. Other factors which may influence a person’s response to a drug include their age, weight, gender, disease state and route of administration. However, more than any other factor, the route of administration determines the onset of drug effect. Drugs that are administered directly into the bloodstream provoke a rapid response, whereas drugs administered orally or topically must be absorbed into the bloodstream before they can take effect. Drugs act by affecting or controlling changes in biochemical or physiological processes in the body. Drugs produce their actions in one of three ways: altering body fluids, altering cell membranes or interacting with receptor sites.
Most drugs act at specific cell receptor sites. A specific drug forms a complex with only one type of receptor but may produce multiple effects because of the location of those receptors in cells of different tissues or organs. For example, the anticholinergic drug atropine sulfate not only reduces the production of saliva, bronchial, nasal and gastric secretions, but it also increases heart rate, stimulates ventilation and raises intraocular pressure. A ‘selective’ drug acts at a receptor in a particular type of body tissue and produces little effect on similar receptors in other organs. For example, the bronchodilator salbutamol has specific selectivity for receptors in bronchial smooth muscle but produces little or no stimulation of similar receptors in cardiac muscle.
A drug may produce more than one effect:
• The desired action is the physiological response the drug is expected to cause
• Side effects (also called adverse effects or adverse reactions) are secondary effects caused by most drugs and are generally undesirable. Although the terms are sometimes used interchangeably, side effects tend to be mild in nature, whereas adverse reactions are more serious (e.g. an adverse effect of acetylsalicylic acid (aspirin) is increased bleeding time; and a common side effect of morphine is nausea)
• Toxic effects develop after prolonged administration of high doses of medication, or when a drug accumulates in the blood because of impaired metabolism or excretion. Some drugs such as digoxin and lithium have a very narrow safety margin and toxicity can occur at recommended or therapeutic doses
• Allergic reactions are unpredictable responses to a drug that acts as an antigen, triggering the release of antibodies. Allergic reactions may be mild, such as urticaria (hives) and pruritus (itching), or they may be severe; for example, severe wheezing and respiratory distress, or life-threatening anaphylactic reaction. Some reactions occur within minutes of the drug being given while other allergic reactions may be delayed for hours or days (Roach 2005)
• Idiosyncratic reactions are those where the client’s body either overreacts or underreacts to a drug, or when the reaction is unusual and there is no known cause (e.g. the antihistamine promethazine (Phenergan) is sometimes used for sedation, however n some people it can cause insomnia and agitation)
• Pharmacogenetic reactions occur because a person may have a genetic trait which leads to abnormal reactions to drugs (e.g. those with glucose-6-phosphate dehydrogenase (G6PD) deficiency may experience haemolysis if given aspirin, chloramphenicol or sulfonamides) (Roach 2005)
• Drug tolerance may also occur where a person has a decreased response to a drug over time, necessitating an increase in dosage to achieve the required response (e.g. tolerance to opioids such as morphine may occur if given for more than 10 to 14 days) (Roach 2005)
• Drug interactions occur when one drug modifies the action of another drug; for example, a drug may either increase or decrease the action of other drugs. A drug interaction may be synergistic (enhances the effects of another drug) (e.g. probenecid may be given orally before IM procaine penicillin to increase and prolong the serum concentration of penicillin) or antagonistic (opposes the effects of another drug) (e.g. protamine sulfate can be given to neutralise the anticoagulant effects of heparin) or additive (where the two drug actions are added together) (e.g. when alcohol is consumed by a person on heparin, the risk of bleeding is significantly increased).
NURSING CARE AND ADMINISTRATION OF MEDICATIONS
The nurse’s role in drug administration is a complex one, requiring both knowledge and skill. To promote safe and correct drug administration, the nurse requires knowledge about the drugs being administered, including:
The nurse also requires certain skills to:
• Administer drugs by various routes
• Calculate the correct amount of drug to administer
• Evaluate the effects of drugs
• Educate clients about drug therapy
• Record the drugs administered and the client’s response to them.
Legal aspects of drug administration
Before a drug can be administered safely, the nurse needs to be aware of the legal aspects of drug administration. This includes knowledge of the laws governing the possession, use and dispensation of drugs and of the directives of the nurse’s registering body on the administration of medications to clients. It also means observing the employing healthcare facility’s occupational health and safety (OHS) regulations that are designed to promote safe storage, handling and use of drugs.
The Nursing and Midwifery Board of Australia (NMBA) is one of the national boards of the Australian Health Practitioner Regulation Agency (AHPRA). With the changes to registration of nurses by AHPRA from 2010, it was decided that enrolled nurses no longer required endorsement for medication administration. The NMBA’s goal is for all enrolled nurses to undertake relevant units of study which will enable them to administer medicines safely as part of their education program. However, for enrolled nurses who have not completed the required units, a notation reading ‘Does not hold Board-approved qualifications in administration of medicines’ will appear on the register against that nurse’s name (NMBA 2010). Jurisdictional legislation and policy specifies the routes and schedules of medicines that the enrolled nurse is able to administer and it is therefore of paramount importance that the nurse and employer understand and comply with the drugs and poisons legislation and policy. Furthermore, to administer intravenous medication, the nurse is required to have completed a separate NMBA-approved unit on the administration and monitoring of intravenous medications (NMBA 2010).
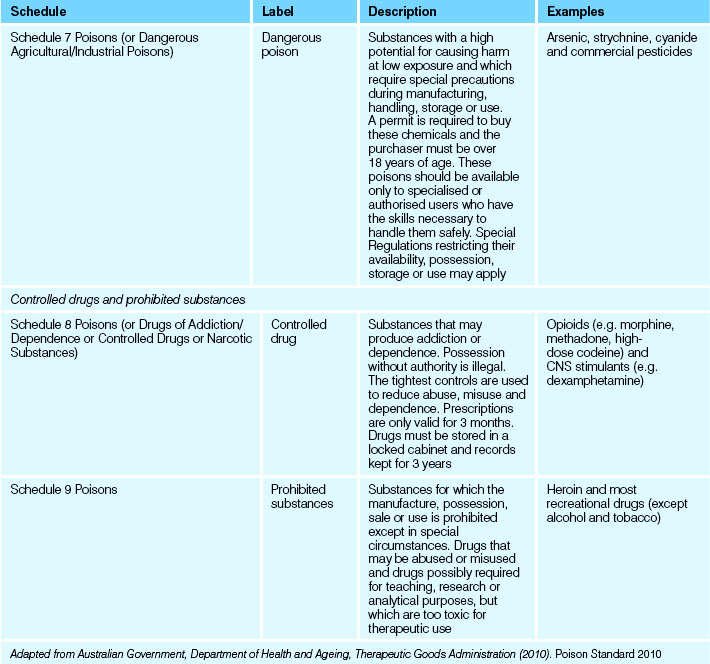
Legal Acts concerning poisons and the poisons regulatory bodies in New Zealand and each state and territory in Australia deal with the control of all drugs, from prescription medication through to agricultural poisons and research drugs. The laws and Regulations apply to sale, supply, storage, dispensing and labelling. The drugs and poisons schedules divide drugs into groups according to their mode of action, therapeutic use, potency, potential for abuse and addiction and safety. While there is currently no national medicines and poisons schedule in Australia, the recommendations of two expert advisory committees (Advisory Committee on Medicines Scheduling and Advisory Committee on Chemical Scheduling) in the form of the Standard for the Uniform Scheduling of Medicines and Poisons (SUSMP, Table 22.2) are usually incorporated into the legislation and Regulations of each state and territory of Australia and New Zealand (Australian Government, TGA 2010). Aims of this document include promoting uniform scheduling, labelling and controls on availability and use of medicines throughout Australia and New Zealand (Australian Government, TGA 2010). SUSMP applies for all medicines and poisons in Australia and medicines in Schedules 2, 3 and 4 in New Zealand. New Zealand-specific legislation exists for medicines which fall outside these schedules.
Administration of drugs
Before administering medications in any form or by any route the nurse must check that the client does not have any drug allergies. The nurse also observes the client who is starting a new medication for any signs of allergy or adverse reaction, and reports and records such responses promptly to the medical officer and the nurse in charge. If the situation arises that a client chooses not to take a prescribed medication, this must be recorded on the client’s medication chart and also reported to the client’s medical officer and the nurse in charge. The principles of asepsis (See Ch 20) are employed during the preparation and administration of all medications.
To ensure that medications are administered correctly and safely, the nurse must observe the seven rights of drug administration (Reiss et al 2007):
Before any medication is administered the client medication chart (Fig 22.4) must be checked thoroughly and systematically to determine the name of the drug, the route, the dosage and the date and time for administration of the medication prescribed.
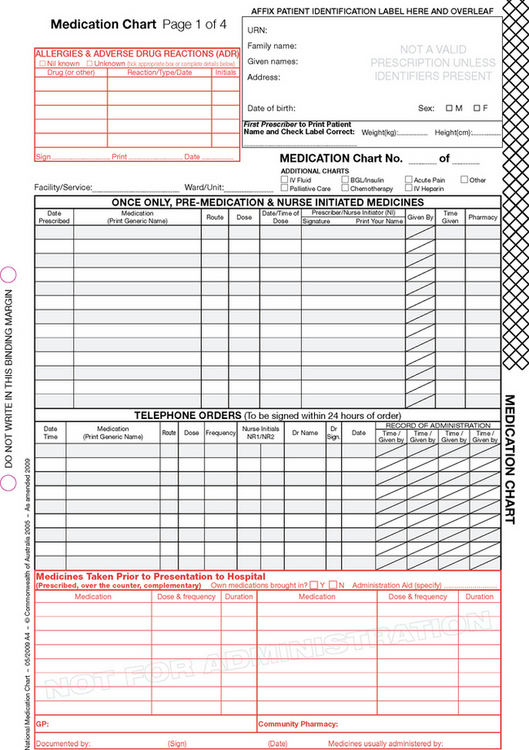
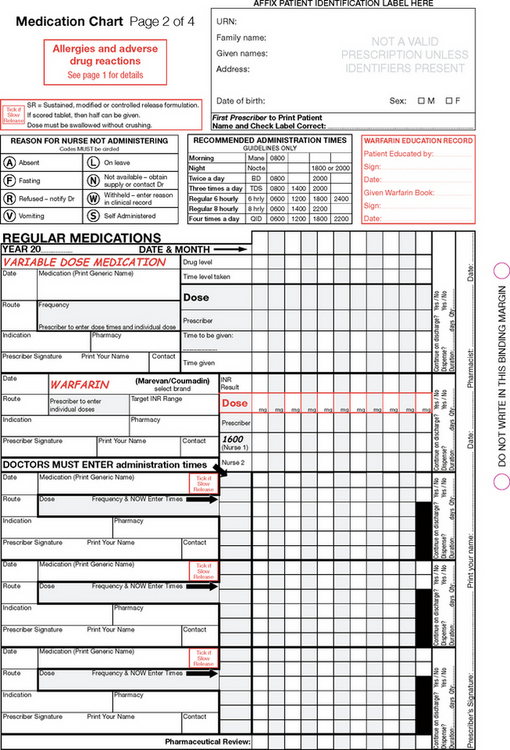
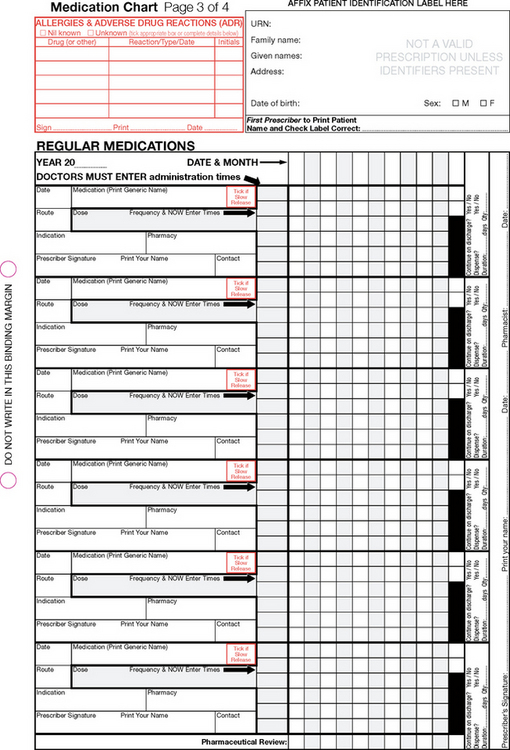
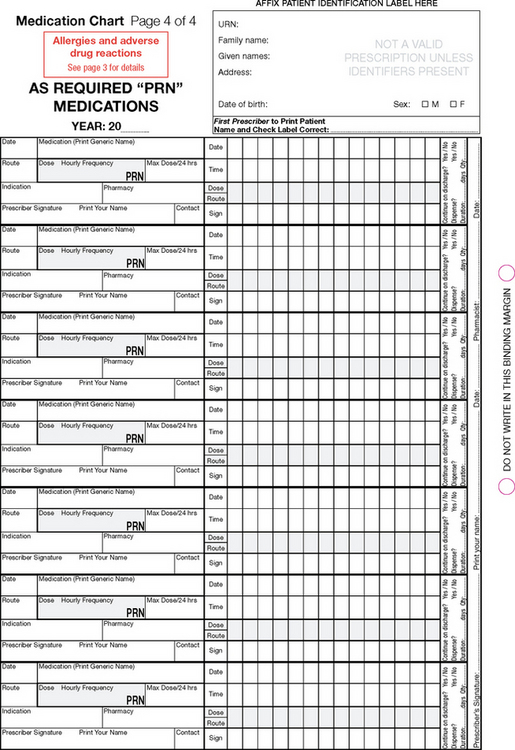
Figure 22.4 Example of the National Inpatient Medication chart
(Australian Commission on Safety and Quality in Health Care 2006)
The nurse compares the label of the drug container with the client medication chart three times:
1. Before removing the container from the trolley or cupboard
2. Before removing the drug from the container
3. Before returning the container to the trolley or cupboard.
To identify a client correctly, before a drug is administered, the nurse:
• Checks the drug order form against the client’s identity bracelet
Special care should be taken when identity bracelets are not worn (e.g. in residential care settings) or where the client is unable to state their own name, because of dementia or mental disturbance, for example. One safety measure that has been implemented in some aged care residential settings is to have a current photograph of each resident that can help with identification.
Most medication errors occur when a nurse fails to follow the recommended safety guidelines, or when the nurse is distracted while preparing or administering medications. To prevent drug administration errors the nurse should:
• Check the date and time to be given
• Be aware that many drugs have similar names
• Check the expiry date on the drug label
• Check the decimal point on prescriptions and drug container labels
• Not administer a drug if the prescription or drug label is illegible (or if the nurse has any doubt at all about the order)
• Be proficient in calculating dosages
• Use administration equipment (e.g. a medicine glass or syringe) with distinct markings
• Not administer any drug prepared by another person (unless the nurse was present throughout the whole time it was being prepared)
• Not prepare medications in advance of the prescribed time for administration
• Not leave prepared medications (e.g. a loaded syringe, transdermal patch or oral medication in a medicine cup) unattended and, most importantly,
Errors in administration
Errors can arise for many reasons. Information on ways to avoid errors in administration is provided throughout this chapter, and also in Clinical Interest Box 22.3. Each healthcare facility has its own protocol for dealing with medication errors, and the nurse must understand and adhere to that protocol.
CLINICAL INTEREST BOX 22.3 Safe medication management guidelines
• All medications must be kept in a locked cupboard or medication trolley, the key of which is kept by an RN at all times. Some preparations (e.g. suppositories, vaccines and insulin) require refrigeration and are stored in a lockable refrigerator. Nothing else should be stored in this refrigerator. Drugs or preparations for external use are stored apart from those intended for internal use
• Drugs of addiction (e.g. Schedule 8 (Victoria)) are kept in a separate locked cupboard that is firmly fixed to a wall. It is customary for this cupboard to be within another locked cupboard. The key is kept in the possession of an RN at all times
• A register must be maintained of all drugs of addiction, and the records must contain full details of all receipt of drugs and all disposal of drugs, whether by administration to a client, return to the pharmacy department or by any other means. The nurse who administers the drug and the nurse who checks the drug both sign their names in the register.
• Healthcare facilities implement a protocol that conforms to the relevant state or territory Regulations whereby certain drugs (usually drugs of addiction such as morphine) are checked at regular intervals (e.g. every 8 hours). Two nurses, one of whom should be an RN, count the drugs together and document their findings in a register. The number of drugs in the containers is compared with the number of drugs already recorded in the register. Both nurses sign the register to indicate that the count is correct. If the count is not correct, the healthcare facility protocol should be followed
• Drugs of addiction and restricted substances can be supplied only with a written order by a medical officer or dentist
• A qualified pharmacist has complete responsibility for all containers issued from the pharmacy department. No one else is permitted to label a container, alter the wording on a label or transfer the contents of one container to another
• There should be a written medical officer’s order for all drugs administered to clients. Verbal orders, including telephone orders, are open to misinterpretation. A written prescription must contain the date of prescribing, the client’s full name, the name and dosage of the drug, the route of administration, the frequency of administration and the signature of the medical officer who is writing the prescription. If the nurse has any doubt about the meaning of an order, the medical officer must be contacted immediately for clarification (before the drug is administered)
• An RN must check every dose of medication to be administered by an undergraduate student nurse. Nursing regulations dictate that an RN must accompany student nurses during administration of a drug
• A nurse should administer only a medication that has been prepared personally; for example, the nurse should not administer any medication that has been prepared by someone else and not witnessed personally
• The nurse who administers a drug to be taken orally must remain with the client until the drug has been swallowed
• If the nurse is checking a drug that is to be administered by another nurse (e.g. a drug of addiction or intravenous antibiotic), in addition to the safety measures already stated, the checker must observe the dose being measured, reconstituted and drawn up, and then witness the drug being administered
• After administering any drug the nurse records it immediately on the appropriate medication record form. Prompt recording prevents errors. Details recorded on the client’s medication chart include the name of the drug, dosage, route and exact time of administration. The nurse who administers the drug must sign the record sheet
If the nurse does make a medication error (e.g. administering the wrong drug, wrong dose or via the wrong route, wrong client) or if a nurse identifies an error made by another nurse, the incident must be reported immediately to the nurse in charge. The nurse has a professional and ethical responsibility for reporting any error, no matter how minor or trivial it may seem at the time. Measures to counteract the effects of the error may be necessary, such as administering an antidote (with a medical officer’s order) or monitoring the drug’s effects over time. The nurse is also responsible for completing an incident report describing the nature of the incident. The incident report provides an objective analysis of why the incident occurred and is a means for the facility’s safety personnel to monitor such events and to implement measures to prevent recurrence. The incident, measures taken and outcomes should also be recorded in the client’s medical notes (see Ch 16 for information on nursing documentation).
SYSTEMS OF MEASUREMENT
To promote accurate and safe administration of drugs, the nurse must understand the system of weights and measures used in prescriptions and correctly calculate dosages. Three systems of measure are used in Australia and New Zealand. They are the metric, apothecary and household systems. The metric is the standard system used for measurement. The apothecary system is outdated and not recommended. Household measures are inaccurate when compared to metric measures. They include drops, teaspoons, tablespoons and cups. The utensils vary in size and are often not well calibrated, and as such are not recommended for use in measuring medications.
SI units
The International System of Units (SI units) is the modern metric system of measurement for length, mass, time, electric current, thermodynamic temperature, luminous intensity and amount of substance. Commonly used in drug administration are mass (kilograms (kg)), volume (litres (L)) and amount of substance (mole (mol)). Smaller measures of mass commonly used are:
Smaller units of volume commonly used are millilitres (mL: 1000 mL = 1 L) and microlitres (μL).
The strength of a pharmaceutical preparation used in electrolyte replacement therapy is normally expressed in millimoles (mmol) per tablet or millimoles per given volume of solution (e.g. mmol/L). A millimole is one thousandth of a mole, which is the molecular weight of a substance expressed in grams. For example, sodium has a molecular weight of 23, so a mole of sodium weighs 23 g, a millimole of sodium weighs 23 mg, and a 1 mM aqueous solution of sodium chloride, for example, contains 1 mmol of sodium chloride (containing 23 mg of sodium) in 1 L of water. Millimoles are also used to express the concentration of substances other than electrolytes and are used widely in laboratories, for example, in haematology reports.
It is important to note that units are not capitalised (e.g. kilogram, not Kilogram); full stops should not be used in unit abbreviations (e.g. mL, not m.L or mL.); quantities less than 1 should have a zero to the left of the decimal point to avoid potential errors (e.g. 0.35 mg, not .35 mg) and abbreviations should not be plural (e.g. 100 mL, not 100 mLs). A trailing zero should not be added after the decimal point (e.g. 1.0 mg) as it may be mistaken as 10 mg if the decimal point is not seen.
Drug calculations
Competence in calculating the required dose of prescribed drugs is an important factor in preventing an administration error.
Conversions
Drugs are not always supplied in the order of measure in which they are ordered. Nurses are then required to convert the available units of volume and weight to the desired dosages. This is a relatively simple process. To change milligrams to grams, divide by 1000, moving the decimal point three places to the left:
450 mg = 0.45 g
To convert litres to millilitres, multiply by 1000, or move the decimal point three places to the right:
0.6 L = 600 mL
Calculating dosages
Although the introduction of unit doses and prepared solutions has meant that the need for nurses to undertake calculations has decreased, there are certain situations where the nurse will need to perform basic calculations in connection with administration of drugs and other pharmaceutical products. The calculation of dosages must be performed with total accuracy and therefore the nurse must be competent in dealing with decimals, fractions, percentages, ratios and proportions. If any doubt exists, it is important that the nurse double check all calculations with another health professional, such as another nurse, medical officer or pharmacist.
Formulae for calculating drug doses include:
Liquid drugs
Example. A medical officer prescribes fentanyl 100 micrograms intramuscularly (IM). The medication in stock is available in ampoules containing 50 micrograms per mL.
Dose required = 100 micrograms
Stock strength = 50 micrograms/mL
Volume in stock strength = 1 mL
Amount in stock strength = 50 micrograms
Solid drugs
Example. A medical officer prescribes morphine 15 mg orally. The medication in stock is available as tablets containing 30 mg.
Drugs measured in units
Example. A medical officer prescribes insulin 10 units subcutaneous (subcut). The insulin is available in 100 units per mL.
Number of units in stock solution = 100
Volume in stock strength = 1 mL
Calculation of paediatric dosages
Children do not always metabolise medications in the same way as adults, due to a greater body water content and immaturity of their liver and kidneys. Children’s dosages are not always standard. In most cases the prescriber will calculate the dose based on height and/or weight before ordering the medication.
One possible way of calculating paediatric dosages is Clarke’s Rule. This rule is based on child’s weight (Arcangelo & Peterson 2006). Dosages based on weight use kilograms of body weight and per kilogram recommendations to arrive at the approximate and safe dose.
The most accurate way of calculating paediatric dosages, however, is based on body surface area. Body surface area is calculated using the child’s height and weight and a nomogram. It should be noted that preparing medications for infants and children requires additional skills. Nurses caring for children are recommended to consult paediatric textbooks for more information. Procedural Guideline 22.1 provide general guidelines concerning administering medications to infants and children.
Procedural Guideline 22.1 Administering medications to infants and children
| Review and carry out the standard steps for all nursing procedures/interventions |
| Action | Rationale |
|---|---|
| Perform hand hygiene and follow infection control procedures. | Prevents cross infection |
| Oral medications | |
| When possible use liquid rather than tablet form | Children find it difficult to swallow tablets |
| Offer a pleasant tasting drink or treat after medication is swallowed | Removes unpleasant after-taste, makes compliance/concordance/adherence more likely with next dose |
| Mix medication with tiny amount of pleasant tasting substance, such as honey (unless contraindicated by pharmacist) to help persuade a reluctant child to take medication | Makes the experience less negative, improves compliance/concordance/adherence |
| Avoid mixing the medication in food | The food may not all be consumed and the full dose of medication will not be ingested |
| Measure liquid doses using a small measuring cup: hold the measuring cup at eye level | Ensures correct amount is poured |
| Discard any excess amount poured from the bottle | Prevents contamination of unused medication in the bottle |
| Use a small plastic syringe (1 or 2 mL) to measure very small amounts | It is difficult to accurately measure tiny amounts of liquid any other way |
| Administer liquids to young infants via a syringe without a needle | Liquid can be administered into side of mouth between cheek and gums to reduce possibility of it being spat out |
| Injections | |
| Select site for intramuscular injection where muscle is developed | Careful site selection is imperative to avoid pain and bruising because infants and children do not have well developed muscles |
| Have at least two people present during administration, at least one familiar person if possible | One person needs to hold the child securely. Children may be frightened and move suddenly and with vigour, making administration difficult or causing the needle to dislodge. A familiar face is reassuring |
| Use distraction techniques such as a toy that makes a noise, or a conversation | Distraction can help focus away from a frightening event and may reduce the perception of pain |
| Administer the injection firmly and quickly | Reduces pain and length of time child is fearful |
| Ensure that child is awake and held closely | Administering pain to a sleeping child causes awakening to trauma. The distress may instil fear of going to sleep |
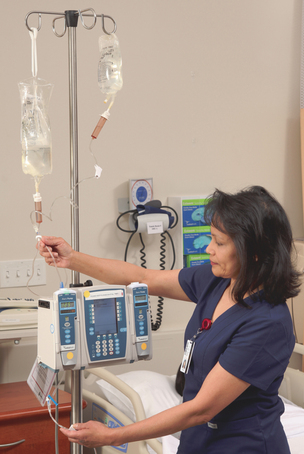
Intravenous administration calculations
The fluid being infused passes from the IV infusion bag into a drip chamber or into a volumetric infusion pump. The drip chamber is part of the IV administration set and has a fixed drop size and an adjustable rate of flow. The volumetric pump is adjustable and is designed to maintain a steady flow rate; however, it should still be checked at regular intervals.
Calculation of intravenous infusion rate (mL/hour)
Hourly rates are calculated by dividing the total infusion volume by the total infusion time in hours.
Example. A medical officer orders sodium chloride 0.9% (normal saline) 1 L to be delivered over 24 hours via an infusion pump.
Volume to be delivered = 1 L = 1000 mL
Calculation of intravenous infusion rate (drops/minute)
The number of drops delivered per millilitre of solution varies with different brands and types of infusion sets. This rate is called the drip or drop factor and is usually printed on the back of the package. In Australia and New Zealand, the macrodrops IV infusion sets most commonly used are those with a 20 drops/mL drip factor. The drop factor for microdrip is always 60 drops/mL.
If the infusion is not delivered via an infusion device, the nurse may be required to regulate the drops per minute to ensure that the prescribed volume will be delivered. Drops per minute are calculated by the following formula:
Example. A medical officer orders sodium chloride 0.9% (normal saline) 1 L to be delivered over 24 hours. The IV infusion set delivers 20 drops/mL.
Volume to be delivered (mL) = 1 L = 1000 mL
Time = 24 × 60 (to convert hours to minutes)
Medical abbreviations
When writing prescriptions, the medical officer frequently uses abbreviations that are derived from Latin. From 2008, standard prescribing terminology, abbreviations and symbols have been introduced in an attempt to reduce the number of associated errors. Abbreviations are also used when referring to strength of medications such as grams (g) and milligrams (mg). For example, the abbreviation for micrograms using the Greek letter μ (mu), that is, μg, is not recommended, nor is mcg, as these may lead to errors; microg is the preferred and recommended abbreviation, or the whole word (microgram) should be used. Other error-prone abbreviations and symbols which should be avoided include IU (international units—can be mistaken for IV), IVI (intravenous injection—mistaken for IV 1) and qd (every day—mistaken as Qid (four times daily) (Australian Commission on Safety and Quality in Health Care 2011).
ADMINISTERING MEDICATIONS
Administering oral medications
The oral route is the most common route by which medications are administered. Oral medications would not be given to clients who are unconscious, unable to swallow or unable to retain the drug in the stomach (vomiting, gastric or intestinal suction). Oral medications may be presented in solid or liquid form. The nurse must know whether solid medications must be swallowed whole, chewed or sucked, or whether the medication may be crushed for administration. Powdered medications and some drugs in granule form are mixed with a liquid before administration. Enteric-coated or sustained-release preparations must never be crushed, chewed or opened. They must be swallowed whole. Enteric coatings are used to:
• Prevent chemically sensitive drugs such as penicillin G and erythromycin from being decomposed by gastric secretions
• Prevent the side effects of nausea and vomiting caused if the drug is broken down in the stomach
• Prevent the drug from being diluted before it reaches the bowel
• Allow a delayed effect on the release of the drug (Bryant & Knights 2011).
Effervescent powders and tablets should be taken immediately after dissolving. All liquid preparations should be shaken before they are poured. Any mixture that stains the teeth should be taken through a straw, and the client should rinse out the mouth after each dose.
In certain circumstances oral drugs may be administered through a nasogastric or PEG tube. Clinical Interest Box 22.4 provides tips to ensure safe administration of medications via a nasogastric or PEG tube. More information about nasogastric and PEG tubes can be found in Chapter 28. The pharmacist should be consulted before crushing any tablets and administering them orally or via a nasogastric or PEG tube. It is often the case that the medication is manufactured and available in a preferable formulation, for example liquid instead of solid.
CLINICAL INTEREST BOX 22.4 Tips for administering medications via a nasogastric or PEG tube
• Do not crush or open any medications without first checking with the pharmacist
• Crush the medication using a mortar and pestle
• Mix with a small amount of water
• Stop and restart feeding, as required by specific medication (e.g. some medications may require feeding to be stopped for a set length of time to allow for the most effective absorption). Again, check with the pharmacist if you are unsure
• Check the fluid status of the client; that is, check to see if there is a fluid restriction that may determine the amount of fluid used to flush the line before and after drug administration
• Check the position of the nasogastric or PEG tube
• Flush the tube with water (20–30 mL)
• Administer the medication either by gentle syringing or by allowing to flow by gravity. Each medication should be administered separately
• Flush the tube with water between each medication and after the last medication
• Restart the tube feeding when appropriate. If the tube is connected to suction, disconnect and clamp the tube for 20 to 30 minutes after giving the medication
• Document the medication on the medication chart. Document the fluid administered on the client’s fluid balance chart
• Administering medication via a nasogastric or PEG tube is the main reason that tubes become blocked, so nurses must ensure that flushing is thorough and that they never mix medications together to instil via a feeding tube because this causes the clumping responsible for blocking the tube
(Adapted from deWit 2009)
Some medications are administered by buccal or sublingual application. These routes are indicated for drugs that tend to be destroyed by gastric juice, or those that are rapidly detoxified by the liver. Buccal tablets are placed in the space between the upper molar teeth and gums. Clients should be advised to alternate cheeks with each administration to prevent mucosal irritation occurring. Sublingual tablets are placed under the tongue. Both forms remain in place while they dissolve. The client should be advised not to chew or swallow such tablets. Before administering any oral medication the nurse must ascertain if any clients have a nil by mouth status, such as may apply to clients who are to have certain tests or surgery.
Suggested guidelines for safely administering oral medications are provided in Procedural Guideline 22.2. The equipment required comprises a drug order sheet and medication record, a medicine glass, the prescribed medication and a glass of water, with a drinking straw or spoon if necessary.
Procedural Guideline 22.2 Administering oral medications*
| Review and carry out the standard steps for all nursing procedures/interventions |
* Safe medication management guidelines, outlined in Clinical Interest Box 22.3, should be incorporated into relevant aspects of this procedure and the nurse must act only within the laws and policies governing nursing practice in the geographical area of employment
Administering drugs by injection
Drugs are given by injection for a variety of reasons, including:
• The drug may be one that is not absorbed when given orally (e.g. aminoglycoside antibacterial agents)
• The drug may be one that is destroyed by digestive juices (e.g. insulin)
• A rapid onset of action may be required
Drugs may be administered by injection subcutaneously (subcut), intramuscularly (IM) or intravenously (IV). The administration of an injection is an invasive procedure that must be performed using aseptic technique. When a needle pierces the skin there is a risk of infection. Infection is avoided by handwashing, preventing contamination of the solution, preventing needle and syringe contamination and by preparing the skin before injection.
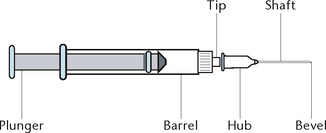
A variety of syringes and needles is available, most of which are single use and disposable. Syringes (Fig 22.5) are available in a range of sizes, varying in capacity from 1 to 50 mL. A syringe consists of a cylindrical barrel with a tip designed to fit the hub of a needle, and a close-fitting plunger. The barrel of the syringe is calibrated into millilitres and tenths of a millilitre or, in the case of an insulin syringe, into units. Needles (Fig 22.5) are available in various lengths and gauges, with different sizes of bevels. A needle has three parts: The hub, which fits onto the tip of a syringe, the shaft and the bevel or slanted tip. Needle gauge is determined by the lumen of the needle: as the diameter of the lumen increases, the gauge decreases. For example, a 16-gauge needle is substantially larger in diameter than a 22-gauge needle.
Selecting an appropriate syringe and needle depends mainly on the prescribed route, viscosity of the medication, amount of medication to be administered and the client’s body size and amount of fat. Generally a 2–3 mL syringe is adequate for subcutaneous, IM and most IV injections. Subcutaneous injections are generally given through a small-diameter needle (e.g. 25-gauge) while IM injections usually require a 21–23-gauge needle. Intravenous injections are generally administered through a 20-gauge needle.
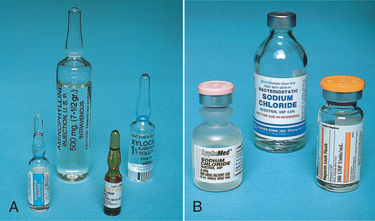
Medications for injection are presented as liquids in glass or plastic ampoules or rubber-capped vials, or in powder form requiring reconstitution before administration (Fig 22.6). An ampoule is made of clear glass or plastic, with a constricted neck that must be snapped off to allow access to the medication. Ampoules contain volumes from 1 mL to 10 mL or more. A vial is a single- or multiple-dose glass container with a rubber seal at the top, which is protected by a metal cap until it is ready for use. Multiple-dose vials are generally not recommended because of the risk of cross-infection between clients. Vials contain medications in either liquid or powder form. Sterile water (often labelled ‘water for injection’) and sodium chloride 0.9% (normal saline) are commonly used as diluents to dissolve drugs in powder form. The vial label or the manufacturer’s information specifies which diluent to use, as well as any other recommendations for administration (e.g. compatibilities, how fast to administer, how much diluent to use). These instructions should be consulted before the preparation and administration of the medication. Table 22.3 illustrates the procedure for the preparation of medications from ampoules and vials.
Table 22.3 Preparation of medications from ampoules and vials
Some medications are available in disposable, single-dose pre-filled syringes that relieve the nurse of the need to calculate and prepare doses of the medication. It may be necessary to advance the plunger a small way to expel some medication if the dose ordered is less than that in the syringe. The nurse still needs to check the name, strength, expiry date and amount of the medication. Particular care is needed because many pre-filled syringes look the same but contain very different drugs. Some medications are available in an injection system that requires a device similar to the plunger in a standard syringe to be screwed into the end of a pre-filled vial with an inbuilt needle. After use the whole injection unit is discarded into the appropriate sharps safe container. This device is designed to minimise the risk of needlestick injury (Crisp & Taylor 2009).
Injection sites
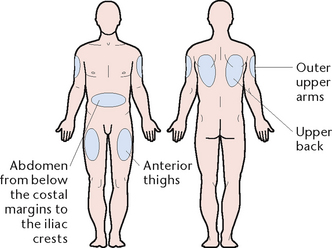
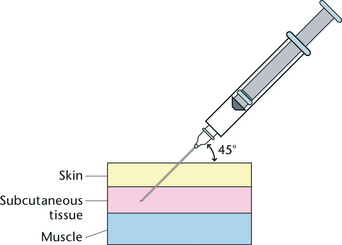
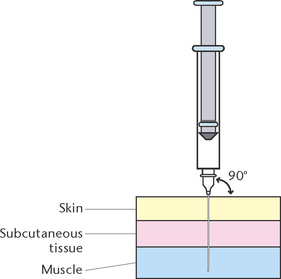
Subcutaneous injection (subcut) involves injecting medication into the loose connective tissue under the dermis. Only small volumes of medication and only medications that will not damage subcutaneous tissue are administered by this route. Subcutaneous sites that are commonly used are the upper outer aspect (middle third) of the upper arm, the upper anterior thighs and the abdomen below the costal margins to the iliac crests (Fig 22.7). The site chosen should be free of skin lesions, bony prominences and large underlying muscles or nerves. Subcutaneous injections are administered with the needle inserted at an angle of 45 degrees (Fig 22.8) or 90 degrees, depending on the size of the needle used. Figure 22.9 illustrates the most common site for subcutaneous administration of heparin.
Intramuscular injections (IM) involve injecting medication into deep muscle tissue. Muscle is less sensitive to irritating or viscous drugs, and up to 3 mL can be injected into muscle without causing severe discomfort (2 mL for elderly or frail clients, those with less developed muscle mass or children). The sites chosen are areas where there is minimal risk of the needle penetrating a large blood vessel, nerve or bone. Intramuscular sites that are commonly used are the middle third of the anterior lateral aspect of the thigh (vastus lateralis muscle), the upper outer quadrant of the buttock (gluteal muscle) and the upper outer aspect (middle third) of the upper arm (deltoid muscle) (Fig 22.10). It should be noted that a volume less than 2 mL is recommended for injection into the deltoid muscle. Figure 22.11 illustrates the IM injection site of the upper outer quadrant of the buttock, showing the relationship to the sciatic nerve. Intramuscular injections are administered with the needle inserted at an angle of 90 degrees (Fig 22.12).
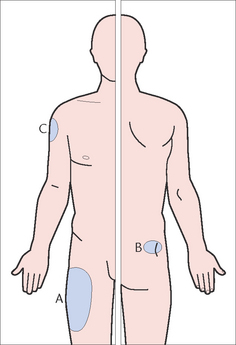
Figure 22.10 Sites for intramuscular injections. A: Vastus lateralis muscle. B: Gluteal muscle. C: Deltoid muscle
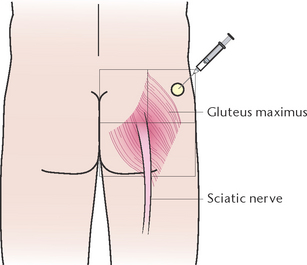
Figure 22.11 Intramuscular injection site of the upper outer quadrant of the buttock, showing the relationship to the sciatic nerve
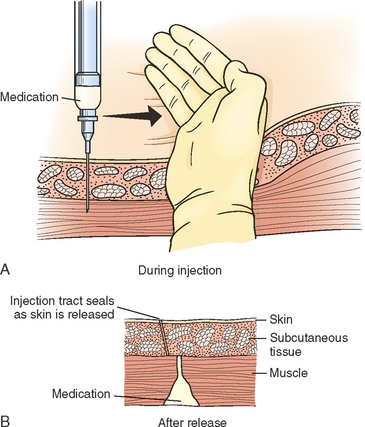
The Z-track method of injection (Fig 22.13) is a technique used when irritating preparations such as iron are given IM. A new needle is attached to the syringe after preparing the drug so that no solution remains on the outside of the needle. The subcutaneous tissue is drawn to one side before inserting the needle, to promote absorption and prevent skin staining and pain. The Z-track method of injection deposits medication into the muscle without tracking residual medication through sensitive tissues.
Promoting safety and comfort
To ensure correct subcutaneous or IM administration of an injectable medication and to minimise the client’s discomfort, the nurse should:
• Position the client comfortably to reduce muscular tension
• Use a sharp needle in the smallest suitable length and gauge
• Select the correct injection site, using anatomical landmarks
• Sites should be rotated to minimise discomfort and tissue damage and aid absorption. This may be achieved by asking the client the site of the last injection and/or documenting the site in the client’s clinical notes or care plan or on the medication chart
• Insert the needle smoothly and quickly
• Hold the syringe steady while the needle remains in the tissues
• Aspirate the syringe before injecting a medication, to check that the needle has not entered an artery or vein
• Press on, or gently massage, the area for several seconds after administration, unless contraindicated.
Injection sites should be assessed as free of any bruising, hardness, signs of inflammation or other abnormality.
Suggested guidelines for administering subcutaneous and intramuscular injections are outlined in Procedural Guideline 22.3. The equipment required comprises:
• Drug order sheet and medication record
• Syringe, selected according to the volume of medication to be administered
• Needles, selected according to the route and body size of the client
• Antiseptic swabs; for example, alcohol swabs
• Prescribed drug in ampoule or vial
Procedural Guideline 22.3 Administering subcutaneous and intramuscular injections*
| Review and carry out the standard steps for all nursing procedures/interventions |
| Action | Rationale |
|---|---|
| Explain procedure to the client, and the purpose of the medication | Reduces anxiety. Understanding improves compliance/concordance/adherence with drug therapy |
| Ensure privacy | Prevents embarrassment |
| Gain the assistance of another nurse if the client is a child, or an adult who is restless or irrational or may need assistance with positioning | Promotes safety during administration |
| Check the drug order sheet for the client’s name, name of medication, dose, route, time of last administration and frequency of administration | Promotes correct and safe administration of the drug |
| Perform hand hygiene and follow infection control procedures. | Prevents cross-infection |
| Calculate the dose and prepare the medication from the ampoule or vial, having checked the label and expiry date. Have two nurses check according to safe administration guidelines | Promotes safety during administration |
| Check the client’s identity band and ask them to state their name and, if possible, the site of the last injection and whether they have any allergies | Confirms the client’s identity and prevents all injections being given into the same site. Prevents allergic reaction from occurring |
| Select an appropriate injection site and assist the client into a comfortable position. Select a site that has not been used frequently. | Appropriate site selection aids absorption, reduces likelihood or injury and discomfort. Rotating sites minimises tissue damage. Comfort promotes relaxation and helps to reduce anxiety |
| Locate the site using anatomical landmarks. Check site for any masses, lumps, signs of infection, scars or skin lesions | Insertion of medication into the correct site avoids injury to underlying structures. Masses, scars, etc will interfere with drug absorption |
| Cleanse the site with an antiseptic swab and allow to dry | Removes microorganisms from the skin |
| Remove the needle cap and hold the syringe in the dominant hand. Hold the client’s skin between the thumb and forefinger and either pull it taut or pinch it up | A needle penetrates tight skin more easily than it does loose skin. Pinching the skin up may be necessary when an SC injection is given to an obese client, or when an IM injection is given to a client with small muscle mass |
| Insert the needle quickly and firmly, at a 45° or 90° angle for subcutaneous injection, and at a 90° angle for IM injection | Quick, firm insertion minimises anxiety and discomfort |
| Slowly pull back on the plunger. If blood appears in the syringe, the needle is withdrawn and the injection repeated at another site, using a fresh dose, syringe and needle | Checks whether needle has penetrated a blood vessel |
| If no blood appears inject the medication slowly | Slow injection reduces tissue trauma and pain |
| Place an antiseptic swab over the injection site and withdraw the needle | Support of tissues minimises discomfort as the needle is withdrawn |
| Dispose of syringe into kidney dish without recapping or place directly into a sharps safe disposal container | Recapping used needles may result in a needle-stick injury |
| Massage the area gently. Do not massage a subcutaneous heparin injection site | Massage improves dispersal and absorption of the drug. Massaging a heparin injection site may result in severe bruising |
| Assist the client into a comfortable position | Promotes comfort |
| Record each drug administered on the medication chart, including the site of injection | Prompt documentation prevents errors. Sites should be rotated for long-term therapy such as insulin, as repeatedly using same site leads to thickening of skin and tissue atrophy |
| Discard syringe and needle into an appropriately labelled rigidwalled sharps container without recapping the needle | Proper disposal prevents sharps injury to personnel or visitors |
| Perform hand hygiene and follow infection control procedures. | Prevents cross-infection |
* Safe medication management guidelines, outlined in Clinical Interest Box 22.3, should be incorporated into this procedure and the nurse must act only within the laws and policies governing nursing practice in the geographical area of employment
Administering drugs via the intravenous route
Intravenous (IV) medications may be administered in a number of different ways, including:
• Large volume infusions—as a mixture in a large volume (e.g. 500 or 1000 mL) of compatible IV fluid. Potassium chloride and some vitamins are administered in this manner
• Intravenous push—as an IV bolus (also called an IV push). A bolus is a small volume introduced either into an already existing IV infusion or into an IV access port (this may also be referred to as a heparin or IV lock). This method is convenient if the client has a fluid restriction. However, because the small volume is introduced directly into the circulatory system, there is little margin for error if a mistake is made. It is difficult, if not impossible, to ‘retrieve’ the medication once it has been administered
• Intermittent intravenous infusions—as a mixture in a small volume (e.g. 50–100 mL) of compatible fluid in a secondary fluid container separate from the primary infusion.
The two most commonly used additive or secondary setups are:
• The piggyback or tandem infusion (Fig 22.14)
Both are acceptable procedures for intermittent medications to be administered.
The client will already have an existing infusion line or an intermittent venous access port. The advantages of the intermittent venous access port include increased client mobility, comfort and safety, cost benefit in not having continuous IV therapy and nurse convenience in not having to monitor flow rates.
Nurses must be aware of their responsibilities and limitations to their scope of practice in relation to the law (e.g. the relevant Nurses or Health Professions Regulation Act) and the rules stipulated by the nursing regulatory bodies in the geographical area of employment. They must also practise according to the policy of the employing hospital or other agency regarding the administration of IV medications. Procedural Guideline 22.4 provides guidelines for the administration of IV medications.
Procedural Guideline 22.4 Administration of intravenous medications*
| Review and carry out the standard steps for all nursing procedures/interventions |
| Action | Rationale |
|---|---|
| General procedures for administration of all IV medications | |
| Calculate the correct dose and prepare the medication according to Table 22.3: Preparation of medications from ampoules and vials | Promotes correct and safe administration of the medication |
| Collect all necessary information about the medication, including action, purpose, normal dose, side effects, any special administration information and compatibility of fluids and medication | Promotes correct and safe administration of the drug and enables the nurse to monitor the therapeutic effects of the medication |
| Ensure the correct medication is given by checking the ‘seven rights’. Two nurses must complete the checking procedures for IV drugs—nurses must adhere to regulations regarding the qualifications of nurses eligible to prepare and check | Promotes correct and safe administration of the medication |
| Explain the procedure to the client and the purpose of the medication | Reduces client anxiety. Understanding improves with drug therapy and keeps the client informed of planned therapy |
| Check cannula insertion site for any signs of redness, warmth, swelling or pain/tenderness on palpation | Ensures safe administration of medication into venous system rather than into surrounding tissues |
| Assess the patency of the IV infusion line or intermittent access port | Ensures safe administration of medication |
| If necessary, check vital signs before, during and after infusion of medication | Allows nurse to monitor client’s response to medication |
| Perform hand hygiene and follow infection control procedures. Put on disposable gloves | Prevents cross-infection |
| Safely dispose of uncapped needle and syringe after use | Prevents accidental needle-stick injuries |
| Record medication administration promptly on medication administration sheet | Prevents medication errors from occurring; for example, dose being duplicated |
| Report any adverse reactions to medical officer and nurse in charge; document in client’s medical notes | Allows medical officer to stop or change medication promptly if an adverse reaction occurs and to treat symptoms of adverse reaction |
| Record volume of fluid in medication bag (used for piggyback/tandem administration) or burette on client’s intake/output form | Prevents circulatory overload |
| Large volume infusions (e.g. potassium chloride) | |
| Before adding medication, ensure that it is compatible with the IV fluid | Prevents chemical reaction occurring, which may result in clouding or crystallisation of the IV fluid |
| Clean injection port with alcohol swab and allow alcohol to dry | Prevents introduction of microorganisms |
| Insert syringe and add required medication to the IV infusion bag via the medication injection port | Correct addition prevents infection, as medication port is self-sealing to prevent the introduction of microorganisms |
| After withdrawing syringe, gently mix contents of infusion | Ensures even distribution of medication throughout the infusion fluid |
| Complete a medication additives label, with details of medication added to fluid, date, time and nurses’ signatures | Informs all staff of the contents of the infusion |
| Ensure infusion rate is correct. A volumetric pump or burette may be added (according to hospital policy) | Prevents circulatory overload |
| Intravenous bolus into existing infusion line | |
| As well as preparing medication, prepare two syringes with 1 mL normal saline each, for flushing line before and after medication | Prevents blockage of line |
| Select injection port closest to client | Allows for easier aspiration for blood return to check placement |
| Clean injection port with alcohol swab and allow alcohol to dry | Prevents introduction of microorganisms |
| Connect syringe containing normal saline to IV line by either inserting needle into injection port (needle system) or removing cap of needleless injection port and connecting syringe tip directly | |
| Occlude infusion line above port by pinching tubing. Gently pull back on syringe plunger to aspirate blood | Checks position of cannula and ensures medication to be administered is into venous system |
| Slowly inject 1 mL normal saline | Clears reservoir of blood and checks patency of access port |
| Inject medication slowly over several minutes (or as directed by manufacturer’s information), continuing to occlude tubing above port | Ensures medication is given at the correct rate. Rapid administration may cause pain or phlebitis or be fatal |
| Withdraw syringe and flush with 1 mL of normal saline. (Some agencies have a policy to follow this with a heparin solution—check policy.) | Flushes medication into venous system. Heparin is an anticoagulant that prevents the formation of a blood clot that could block the cannula |
| Release tubing and regulate infusion rate if necessary | Occluding tubing may affect the infusion rate |
| Clean injection port with alcohol swab and allow alcohol to dry or if using a needleless system, replace injection port cap with a new sterile cap | Prevents introduction of microorganisms |
| Piggyback/tandem infusion | |
| Connect infusion tubing to medication bag and allow solution to fill tubing | Tubing should be filled with solution and free of air to prevent air embolus |
| Hang medication bag and connect tubing to infusion port (e.g. stopcock, needleless system, tubing port) on the primary infusion line after having wiped port with alcohol swab | Prevents introduction of microorganisms |
| Regulate flow rate using regulator clamp | Ensures medication is introduced at the correct rate to maintain therapeutic levels |
| When completed, remove and discard secondary infusion bag in a safe and appropriate manner | |
| Ensure primary infusion is running at the correct rate | Secondary infusion may have interfered with the flow of the primary infusion |
| Burette | |
| Fill burette with desired amount of fluid from infusion bag | |
| Clean injection port on top of burette with alcohol swab | Prevents introduction of microorganisms |
| Inject medication into port and gently mix with fluid in burette | Ensures even distribution of medication throughout fluid |
| Regulate infusion rate to allow medication to infuse at the required rate | Ensures medication is introduced at the correct rate to maintain therapeutic levels |
| Label burette with medication administration label containing name of medication, total volume, time of starting administration and client details | Ensures all staff are aware of medication infusion occurring; prevents other medication being added to burette at same time |
| When infusion is complete, remove label from burette and return infusion to previous rate | Alerts staff that medication infusion is complete |
| If more than one medication is to be administered, ensure that burette and line are ‘flushed’ in between the medications | Prevents incompatible medications coming into contact with each other |
* Safe medication management guidelines, outlined in Clinical Interest Box 22.3, should be incorporated into this procedure and the nurse must act only within the laws and policies governing nursing practice in the geographical area of employment
Needleless systems
Where possible, alternatives to needles should be considered, including needleless intravenous systems, the use of blunt needles for drawing up sterile solutions from ampoules or the use of retractable needle and syringe systems. Needleless IV systems are systems that administer medications through an IV access device without using needle connections.
The main types of needleless IV systems are split septum systems and Luer-activated mechanical valve systems. The split septum system involves a resealable port that attaches to the hub of the client’s access device and promotes a closed system. A blunt cannula penetrates the septum, eliminating the need for a sharp needle. Medications are administered by connecting the blunt cannula to the secondary administration set and inserting it into the prepierced septum. The Luer-activated device (LAD) controls a valve that prevents the outflow of fluid through the connector until a standard Luer connector is inserted, allowing the valve to open and fluid to be inserted or withdrawn.
Topical applications
Topical medications are applied locally to the skin or mucous membranes such as the ear, eye, vagina, rectum and nose. They can be in the form of lotions, pastes or ointments.
Applying transdermal medications
Certain medications can be applied to the skin to supply drugs directly into the bloodstream for prolonged systemic effect. The medications are applied via an adhesive patch or disc which releases a known amount of drug per time (e.g. 5 mg over 24 hours). Transdermal medications include glyceryl trinitrate (known as nitroglycerine in the US) (to relieve angina pectoris), nicotine (for nicotine withdrawal) and oestrogen (for hormone replacement therapy). Drugs administered transdermally avoid being broken down by the liver before they have had a chance to take effect.
Adhesive patches or discs which are applied to the skin are composed of an adhesive layer, a rate-limiting membrane, a drug reservoir and a waterproof external layer. The discs are applied to a dry, clean, hairless area of the body. The waterproof external layer enables the client to shower or bathe without adversely affecting the drug’s action. Drugs applied in this manner can exert their effects for as long as 24–72 hours. Client education should include the correct application of the transdermal patch or disc (including the removal of the old disc), the frequency of application, the need to rotate application sites to prevent skin irritation occurring, correct storage of the discs, the need to wash the hands after application and correct disposal of the discs after use. Education should particularly stress the importance of keeping the discs out of reach of children. Hands should be washed immediately after applying the discs to avoid the nurse absorbing any of the drug transdermally through the hands.
Skin applications
Topical preparations such as those used in the treatment of dermatological conditions may be formulated as an ointment, lotion, cream, jelly, powder, paint, paste or spray. Drugs may be applied to the skin by painting, spreading or spraying medication over an area, applying moist dressings or by soaking body parts in a solution. Drugs applied to the skin have local effects, with the exception of transdermal preparations that are designed to produce systemic effects. To avoid medication being absorbed through the skin of the hands, the nurse should wear disposable gloves for protection or use an applicator during administration of topical medications. To prevent accumulation, any residual medication on the skin should be removed before reapplication. When applying a prescribed topical preparation, the manufacturer’s directions must be followed.
Instilling eye drops and ointments
Eye drops or ointment prescribed may include those that combat infection, dilate or constrict the pupil, act as a local anaesthetic, stain the cornea, reduce inflammation or reduce intraocular pressure. Key aspects regarding the use of ophthalmic medications include checking the:
• Name, strength and amount of drops or ointment to be instilled
• Frequency, and time of last administration
• Eye into which the eye medication is to be instilled (e.g. left, right or both eyes)
• Expiry date on the container, and discarding the medication if the expiry date has passed.
Eye drops are supplied in a squeeze bottle with a nozzle top through which the drops are delivered. To prevent cross-infection a separate container of drops or ointment is supplied for each client. Single-dose packaging is preferred, as contamination of the medication is likely to occur if a container such as a dropper bottle is used repeatedly. Guidelines for instilling eye drops and ointment are presented in Procedural Guideline 22.5.
Procedural Guideline 22.5 Instilling eye drops or ointment*
| Review and carry out the standard steps for all nursing procedures/interventions |
| Action | Rationale |
|---|---|
| Explain the procedure and ensure privacy | Reduces anxiety |
| Check the drug order sheet for the client’s name, name of medication, dose (number of drops), route (including whether drug will be administered to right or left eye or both), time of last administration and frequency of administration. Check the expiry date of the medication | Promotes correct and safe administration of the drug |
| Assist the client to a position with the head tilted well back (if possible) | Facilitates correct instillation of medication |
| Perform hand hygiene and follow infection control procedures | Prevents cross-infection |
| If eye contains any discharge or crusting, it should be cleaned with normal saline and gauze swabs before instilling drops or ointment | Discharge or crusting prevents good absorption of medication |
| Gently pull down the lower lid to form a pouch | Facilitates correct instillation of medication |
| Remove the cap of the container and hold the dropper or tube slightly away from the eye | Avoids contacting any part of the eye and contaminating the nozzle |
| If drops are being instilled, the prescribed number is dropped into the pouch of the lower lid | Medications should be instilled correctly; for example, into the pouch of the lower lid and not directly onto the eyeball |
| If ointment is being instilled, the first 1.25 cm is discarded onto a swab. Directing the nozzle of the tube near the lid, a ribbon of ointment is squeezed into the pouch of the lower lid | Reduces the risk of instilling contaminated ointment |
| Request the client to close the eyelid gently. Wipe away any excess with a gauze swab. Request that the client blink gently several times | Facilitates even distribution of the medication over the eye’s surface |
| Apply an eye pad if required | A pad may be prescribed for comfort or protection |
| Assist the client into a comfortable position | Promotes comfort |
| Remove and attend to the equipment appropriately. Perform hand hygiene | Prevents cross-infection |
| Record each drug administered on the medication record | Prompt documentation prevents errors |
| Report and document the procedure | Care can be evaluated |
* Safe medication management guidelines, outlined in Clinical Interest Box 22.3, should be incorporated into relevant aspects of this procedure and the nurse must act only within the laws and policies governing nursing practice in the geographical area of employment
The equipment required comprises:
The use of gauze swabs rather than cotton wool balls is recommended when cleansing the eyes before administering eye drops. Cotton wool is not recommended because it contains particles that may irritate and damage they eye (Elliott et al 2007).
Instilling ear drops
Ear drops prescribed may include those that combat infection or soften wax. Guidelines for instilling ear drops are presented in Procedural Guideline 22.6. The equipment required comprises:
• Drug order sheet and medication record
• Prescribed drops, warmed to body temperature
• Two or three cotton wool swabs
Procedural Guideline 22.6 Instilling ear drops*
| Review and carry out the standard steps for all nursing procedures/interventions |
| Action | Rationale |
|---|---|
| Explain the procedure and ensure privacy | Reduces anxiety |
| Check the drug order sheet for the client’s name, name of medication, dose (number of drops), route (right or left ear or both), time of last administration and frequency of administration. Check the expiry date of the medication | Promotes correct and safe administration of the drug |
| Assist the client to lie on the side opposite to the affected ear side | Facilitates instillation of the drops into the ear |
| Perform hand hygiene and follow infection control procedures | Prevents cross-infection |
| Inspect the ear for any wax or drainage. Wipe out gently using a cotton bud, ensuring that wax is not forced inwards | Any occlusion will prevent drops from being evenly distributed |
| Gently pull the auricle up and back. For a child under 3 years, the earlobe is pulled down and back | Straightens the ear canal |
| Ensure that the drops are at room temperature. Instil the prescribed number of drops so that they fall against the sides of the canal and not on the tympanic membrane | Cold drops may cause vertigo and nausea. Avoids discomfort |
| Gently massage or apply pressure to the projection in front of the meatus (the tragus) | Ensures that the drops flow into the canal |
| Wipe the outer ear free of excess drops | Promotes comfort |
| If prescribed, place a cotton wool swab loosely into the meatus, or instruct the client to lie with affected ear upwards for 10 minutes | Prevents the medication from leaking out |
| Dispose of equipment appropriately. Perform hand hygiene | Prevents cross-infection |
| Record each drug administered on the medication record | Prompt documentation prevents errors |
| Report and document the procedure | Care can be evaluated |
* Safe medication management guidelines, outlined in Clinical Interest Box 22.3, should be incorporated into relevant aspects of this procedure and the nurse must act only within the laws and policies governing nursing practice in the geographical area of employment
Administering drugs via the rectal route
Medication may be given rectally in the form of suppositories or retention enemas. The rectal route may be used when drugs cannot be taken orally; for example, when clients are vomiting or unconscious or when a local action is required. Some clients will be able to insert suppositories themselves without the assistance of a nurse, which may prevent embarrassment. Other clients will need the nurse to administer the suppository. The nurse should be aware of the different types of suppositories and enemas available. Types of medications that may be administered rectally by suppository include analgesics and antiemetics. Suppositories prescribed to promote a bowel action are composed of various substances, such as glycerine. Evacuant suppositories act by softening and lubricating the faeces to facilitate easier passage and excretion, or by increasing peristalsis through the irritation of intestinal sensory nerve endings. Suggested guidelines for administering rectal suppositories are presented in Procedural Guideline 22.7.
Procedural Guideline 22.7 Inserting a rectal suppository
| Review and carry out the standard steps for all nursing procedures/interventions |
| Action | Rationale |
|---|---|
| Explain the procedure | Reduces anxiety |
| Assemble the equipment and follow the nursing policies related to checking medications | The correct type, size and quantity must be administered |
| Ensure adequate privacy | Reduces embarrassment |
| Place the client in a left lateral position with the right leg flexed | Anatomical site of the lower colon means that this position is the most effective for the introduction and retention of suppositories |
| Ensure that the person is adequately covered, with only the buttocks exposed | Promotes warmth and comfort |
| Perform hand hygiene and follow infection control procedures. Put on disposable gloves | Prevents cross-infection |
| Lubricate finger of glove and suppository | Facilitates insertion of suppository |
| Gently insert the suppository by directing it with the finger, through the anus about 3.5 cm into the rectum | Suppository must pass the internal anal sphincter and come in contact with rectal mucosa |
| During insertion, encourage the client to take deep breaths through the mouth | Helps to relax the anal sphincters |
| Encourage the client to retain the suppository for the correct length of time. A suppository administered to cause a bowel action should be retained for at least 20 minutes | Client must be aware whether the suppository is to be retained to allow any medication to be dissipated, or whether to expect a bowel action. Suppositories to promote a bowel action must be retained long enough to be effective |
| Ensure the client has easy access to toilet facilities and the signal device; for example, nurse call bell | Reduces anxiety related to accidental expulsion of the suppository or faeces |
| Dispose of used equipment appropriately, perform hand hygiene | Prevents cross-infection |
| If a bowel action results, the faeces are observed and the observations reported and documented | Helps to assess the effectiveness of the treatment and detects any abnormalities |
| Attend to the client’s hygiene and position | Helps promote comfort |
| If a prescribed medication was used, ensure that each drug administered is recorded on the medication record | Prompt documentation prevents errors |
| Report and document the procedure | Appropriate care may be planned and implemented |
*Safe medication management guidelines, outlined in Clinical Interest Box 22.3, should be incorporated into relevant aspects of this procedure and the nurse must act only within the laws and policies governing nursing practice in the geographical area of employment
The equipment required comprises:
• Drug order sheet and medication record
• Prescribed suppository/suppositories
• A small disposable sheet to protect bed linen
• Receiver (e.g. paper bag) for used articles
• Appropriate toilet facilities; for example, bedpan, toilet paper
• Soap, face washer and towel for client use after bowel motion or insertion of suppository.
Instilling vaginal medications
Vaginal medications are available as creams or pessaries. Both forms are generally administered with an inserter or applicator, allowing the medication to be placed high in the vaginal vault for maximum effect. Vaginal pessaries are presented in conical, oval or cylindrical shapes and are supplied in individual foil or plastic wrappers. Vaginal anti-infective medications are prescribed to treat vaginal infections, and vaginal hormone preparations are prescribed to treat conditions such as senile vaginitis. Unlike the rectum, the vagina does not have a sphincter and therefore creams may run out. To help avoid this, vaginal preparations should be instilled at night whenever possible, when the client is in bed ready for sleep. Sanitary pads are recommended to prevent staining or soiling of underwear. The use of tampons is not recommended.
Clients who require vaginal medication may prefer to self-administer to avoid embarrassment. The nurse may be required to perform the technique or to instruct the client in how to instil vaginal medications. A suggested procedure is outlined in Procedural Guideline 22.8.
Procedural Guideline 22.8 Instilling vaginal medications*
| Review and carry out the standard steps for all nursing procedures/interventions |
| Action | Rationale |
|---|---|
| Check the drug order sheet for the client’s name, the name and dose of medication, frequency and time of last administration. Check the client’s identity. Check the label and expiry date of the medication | Promotes correct and safe administration of the medication |
| Explain the procedure and the purpose of the medication | Reduces anxiety. Understanding improves compliance with drug therapy |
| Ensure privacy and assist the client into the dorsal recumbent position, with legs flexed and extended apart | Position provides easy access to and adequate exposure of the vaginal canal |
| Perform hand hygiene and follow infection control procedures. Put on disposable gloves | Prevents cross-infection |
| Attach the applicator to the tube of cream or place the pessary in the applicator | Promotes correct and safe administration of the medication |
| Gently retract the labial folds | Exposes the vaginal orifice |
| Insert the applicator into the vagina in an upward and backward direction, about 7.5 cm. Push the plunger to deposit the medication | Proper placement ensures equal distribution of medication along the walls of the vaginal cavity |
| Withdraw the applicator, wipe any residual cream from the labia and apply a perineal pad | Promotes comfort; perineal pad prevents staining of clothing |
| Encourage the client to remain in the recumbent position for at least 10 minutes after administration | Allows medication to melt and be absorbed into the vaginal mucosa |
| Wash applicator in warm soapy water, rinse and dry. The applicator is stored for future use by that client only. Remove gloves. Perform hand hygiene | Prevents cross-infection |
| Record administration on the medication record | Prompt documentation prevents errors |
* Safe medication management guidelines, outlined in Clinical Interest Box 22.3, should be incorporated into relevant aspects of this procedure and the nurse must act only within the laws and policies governing nursing practice in the geographical area of employment
Administering drugs by inhalation
Drugs can be inhaled to produce a local or systemic effect via the respiratory tract by steam inhalation, nebuliser, atomiser or aerosol spray. Most commonly, drugs are delivered to the lungs as sprays from pressurised aerosol dispensers, or as dry powder from an inhaler.
Aerosol inhalers are widely used to administer bronchodilators for the management of asthma. The drug and its inert propellant are maintained under pressure in a small canister. When the valve is activated, a measured quantity of propellant carrying the drug is released through the mouthpiece. It is important that the client is instructed in the correct technique on inhaler use, otherwise the drug will be deposited on the tongue and not into the airways. A spacer may be used to ensure maximal benefit from inhalation and can be particularly beneficial for young children or clients who find it difficult to manage aerosol inhalation without one. The bronchodilator is released into the plastic spacing device and then inhaled. A dry powder inhaler (e.g. Rotahaler Inhalational Device, Accuhaler) may be used if a client is unable to coordinate aerosol inhalation. When the mouth is placed on the mouthpiece, the client inhales through the device causing drug particles (in powder form) to be drawn into the respiratory tract. If two inhalers are to be used, the bronchodilator medications should be given before the other medication. If steroids are used care must be given to rinsing the mouth to prevent fungal infections.
A nebuliser adds moisture and/or medications to inspired air, using the aerosol principle. Nebulisation is often used for administering bronchodilators or mucolytic agents. A high-pressure gas source (air or oxygen) is used to draw up the medication from a chamber. Small-volume nebulisers are generally used for administering medications. Before administering the medication, sufficient sterile 0.9% w/v sodium chloride solution must be added to the medication. To prevent cross-infection, each client should be provided with their own nebuliser and mask for use on repeated occasions. The mask and nebuliser should be cleaned at regular intervals and disposed of when treatment is discontinued or the client is discharged.
A suggested procedure for using a hand-held inhaler is outlined in Procedural Guideline 22.9. The equipment required comprises the drug order sheet and medication record, the prescribed drug and inhaler and the spacer if required.
Procedural Guideline 22.9 Using hand-held inhalers*
| Review and carry out the standard steps for all nursing procedures/interventions |
| Action | Rationale |
|---|---|
| Check the drug order sheet for the client’s name, the name and dose of medication, frequency and time of last administration. Check the label on the inhaler, including the expiry date and the client’s identity | Promotes correct and safe administration of the drug |
| Perform hand hygiene and follow infection control procedures | Prevents cross-infection |
| Explain the procedure and the purpose of the medication | Understanding improves compliance with drug therapy |
| Assist the client to assume an upright position | Position facilitates entry of the medication into the respiratory tract |
| Load the inhaler with the canister of medication. Twist to break the capsule | Prepares the inhaler for administration of the medication |
| Remove the mouthpiece cap | |
| Shake the inhaler | |
| Instruct the client to hold the inhaler with the mouthpiece at the bottom | Ensures correct administration of drug |
| Instruct the client to breathe out slowly and fully | Enables subsequent deep inhalation to be performed |
| Instruct the client to place the mouthpiece well into the mouth, close the lips firmly around it and tilt the head back slightly | Tight seal is necessary to prevent the escape of medication into the air |
| The client inhales quickly and deeply through the mouthpiece while administering a metered dose by pressing the canister downwards | Draws the medication into the lungs |
| The client removes the inhaler, holds the breath for as long as possible then breathes out slowly through the mouth | Allows medication to reach the alveoli. Allows increased absorption and diffusion of the drug, and better gas exchange |
| The technique is repeated if necessary until the prescribed dose has been inhaled or a different inhaler is also required. Time between inhalations depends on which medications are being inhaled | Time between inhalations allows deeper penetration of the second inhalation |
| Clean mouthpiece after each use with mild soap and water. Replace the cap on the mouthpiece | Prevents contamination of mouthpiece |
| Perform hand hygiene and follow infection control procedures | Prevents cross-infection |
| Encourage the client to drink, eat or brush teeth immediately after use | Prevents hoarseness, irritated sore throat or oropharyngeal candidiasis |
| Record administration on the medication chart | Prompt documentation prevents errors |
* Safe medication management guidelines, outlined in Clinical Interest Box 22.3, should be incorporated into relevant aspects of this procedure and the nurse must act only within the laws and policies governing nursing practice in the geographical area of employment
MONITORING THE EFFECTS OF MEDICATIONS
The nurse plays a vital role in monitoring the effects of prescribed medications. Evaluating the client’s response is essential and the nurse is required to assess, report and record all responses to medication. This includes the desired effects and any adverse reactions. To monitor the effects of any medication the nurse must first have a clear understanding of the purpose of the drug and its desired effects. Table 22.4 lists the major actions of common drug classes and provides the nurse with a guide to the expected effects of various groups of drugs. For example, the nurse needs to be aware that an analgesic drug is administered for the purpose of alleviating pain, an anti-inflammatory drug to relieve inflammation and an antipyretic to lower body temperature. Documentation should therefore include whether or not the drug has successfully achieved the desired effects; for example, if the pain has been successfully relieved by the analgesic.
Table 22.4 Major actions of common drug classes
| Drug class | Action |
|---|---|
| Drugs acting on the cardiovascular system | |
| Antianginal agents | Relax smooth muscle and reduce myocardial oxygen demand, thereby reducing angina |
| Antihypertensive agents | Reduce high blood pressure |
| Antiarrhythmic agents | Prevent, alleviate or correct cardiac arrhythmias |
| Antiplatelet agents | Decrease platelet aggregation to prevent thrombus formation |
| Cardiac glycosides | Increase force of myocardial contraction |
| Diuretics | Promote the formation and secretion of urine |
| Fibrinolytic agents | Activate the endogenous fibrinolytic system to dissolve intravascular blood clots |
| Lipid-regulating agents | Reduce blood cholesterol level |
| Vasodilators | Dilate blood vessels, improving circulation |
| Drugs acting on the respiratory system | |
| Antiasthma agents | Prevent asthma symptoms |
| Bronchodilators | Relax bronchiole smooth muscle to relieve bronchospasm and improve ventilation |
| Cough suppressants; expectorants and mucolytics | Depress the cough centre in the medulla oblongata; break up mucus, enabling expectoration |
| Drugs acting on the nervous system | |
| Analgesics | Alter the perception of pain |
| Antianxiety agents | Prevent or relieve anxiety |
| Antidepressants | Prevent or relieve depression |
| Antiepileptics | Also called anticonvulsants. Prevent or reduce the severity of epileptic seizures |
| Antimigraine agents | Prevent or relieve migraine headaches |
| Antimuscarinic agents | Also known as anticholinergics. Inhibit the transmission of parasympathetic nerve impulses, resulting in reduced muscle spasm, decreased secretion of sweat, saliva and nasal, bronchial and gastrointestinal secretions |
| Antipsychotic agents | Counteract or reduce symptoms of psychosis |
| Dopaminergic agents | Either stimulate dopamine receptors or replenish supply of dopamine. Commonly used in the treatment of Parkinson’s disease |
| General anaesthetics | Used to induce and maintain anaesthesia during surgery |
| Local anaesthetics | Block nerve conduction |
| Muscle relaxants | Reduce contractility of muscle fibres, thereby reducing muscle spasm |
| Neuromuscular-blocking agents | Have an action at the muscle receptor end-plate and are used as an adjunct to general anaesthetics to relax muscle |
| Opioid analgesics | Alter perception of pain, induce euphoria, depress respiratory and cough reflexes |
| Parasympathomimetic agents | Central nervous system stimulants. Either mimic action of acetylcholine or block acetylcholine breakdown at receptor sites, thereby increasing total amount of acetylcholine |
| Sedatives and hypnotics | Depress the central nervous system |
| Stimulants | Excite the central nervous system |
| Sympathomimetic agents | Mimic noradrenaline and have effects including cardiac stimulation and relaxation of bronchial smooth muscle |
| Drugs acting on the endocrine system | |
| Antidiabetic agents | Regulate the metabolism of glucose |
| Antithyroid agents | Inhibit synthesis of thyroid hormone (thyroxine) |
| Calcium-regulating agents | Lower blood calcium levels |
| Corticosteroids | Hormones that influence or control key processes in the body, including carbohydrate and protein metabolism, electrolyte and water balance |
| Hypothalamic and pituitary hormones | Used as replacement therapy |
| Thyroid agents | Replace thyroid hormones |
| Drugs acting on the gastrointestinal tract | |
| Anorectic and weight loss agents | Suppress hunger sensation |
| Antacids | Neutralise gastric acidity and reduce pepsin activity |
| Antidiarrhoeal agents | Relieve diarrhoea |
| Antiemetics | Prevent and relieve nausea and vomiting |
| Antiulcer agents | Assist in the healing of gastric and duodenal ulcers |
| Laxatives | Promote peristalsis and evacuation of the bowel by increasing the bulk of faeces by softening the stool or by lubricating the intestinal wall |
| Prostaglandins | Inhibit gastric secretion |
| Topical rectal agents | Reduce pain associated with haemorrhoids |
| Drugs acting on the urinary system | |
| Bladder function disorder agents | Treat disorders of the bladder to re-establish normal bladder function |
| Diuretics | Promote the formation and secretion of urine |
| Drugs acting on the reproductive system | |
| Androgens | Control development of and maintenance of male sex organs and male secondary sex characteristics |
| Erectile dysfunction agents | Treats erectile dysfunction by promoting blood fow |
| Oestrogens | Control development and maintenance of female sex organs, secondary sexual characteristics and mammary glands |
| Prostaglandins | May cause contraction or relaxation of smooth muscle in blood vessels, bronchi, uterus or gastrointestinal tract |
| Progestogens | Convert the endometrial proliferative phase to the secretory phase in preparation for a fertilised ovum |
| Progestogens | Convert the endometrial proliferative phase to the secretory phase in preparation for a fertilised ovum |
| Sex hormones | Sex hormones are prescribed for a variety of reasons, including the development or control of male or female sex organs and secondary sex characteristics. Common uses include oral contraceptives, hormone replacement drugs to treat primary amenorrhoea, delayed onset of puberty or to relieve the symptoms of menopause. Sex hormones may also be used therapeutically to treat osteoporosis, to promote sex drive and fertility and in treatment related to breast or prostatic cancer. The sex hormones include anabolic steroids, androgens, antiandrogens, oestrogens and progesterones |
| Drugs acting on the musculoskeletal system | |
| Analgesics | Prevent and reduce pain |
| Non-steroidal anti-inflammatory drugs (NSAIDs) | Reduce inflammation |
| Disease-modifying antirheumatic drugs (DMARDs) | Treat rheumatoid arthritis |
| Antigout agents | Reduce pain and inflammation associated with gout or alter production or distribution of uric acid |
| Muscle relaxants | Reduce contractility of muscle fibres, reducing muscle spasm |
| Drugs acting on the immune system | |
| Antihistamines | Reduce the effects of histamine released from cells |
| Corticosteroids | Hormones that influence or control key processes in the body, including carbohydrate and protein metabolism, electrolyte and water balance |
| Immunomodifiers | Modify the immune system |
| Vaccines, immunoglobulins and antisera | Vaccines induce a specific active artificial immunity. Antisera contain antibodies (immunoglobulins) against a specific disease to confer passive immunity |
| Drugs acting on the blood | |
| Anticoagulants | Prevent or delay the coagulation of blood |
| Antiplatelet agents | Decrease platelet aggregation to prevent thrombus formation |
| Fibrinolytic agents | Activate the endogenous fibrinolytic system to dissolve intravascular blood clots |
| Haemostatics | Treat or prevent haemorrhage by inhibiting fibrin clot breakdown |
| Lipid-regulating agents | Reduce blood cholesterol level |
| Vasodilators | Dilate blood vessels, improving circulation |
| Drugs acting on the skin | |
| Dermatological agents | Prevent or treat skin infections; cleansers; moisturising agents; sunscreen agents; topical anaesthetics; topical analgesics |
| Anti-infective agents | |
| Anthelmintics | Treat worm infestations |
| Antibacterial agents | Inhibit the growth of or destroy bacteria |
| Antifungal agents | Inhibit the growth of or destroy fungal infections |
| Antimalarial agents | Prevent or treat malaria |
| Antimycobacterial agents | Treat tuberculosis and Hansen’s disease (leprosy) |
| Antiprotozoal agents | Treat protozoal infections |
| Antiviral agents | Prevent or treat viral infections |
| Drugs used in neoplastic disorders | |
| Antineoplastic agents | Also called cytotoxics. Prevent the proliferation of malignant cells by attacking them at various stages of the cell cycle |
| Corticosteroids | Hormones that influence or control key processes in the body, including carbohydrate and protein metabolism, electrolyte and water balance |
| Immunomodifiers | Modify the immune system |
Whenever medication of any sort is administered there is always a possibility that side effects or adverse reactions may occur. Adverse reactions to a drug may be due to overdose, idiosyncrasy, toxic effects, allergy or drug interactions. Early detection of the manifestations of an adverse reaction and immediate, factual and concise reporting of these manifestations allows prompt action to be taken. Manifestations of an adverse reaction will depend on the type of medication administered and on each individual. It is important for the nurse to refer to either the manufacturer’s information or a reliable textbook to have all of the information concerning possible adverse reactions. The nurse should be informed and knowledgeable about every medication before it is administered and document and report any adverse or side effect immediately to the nurse in charge and medical officer.
SAFE HANDLING OF HAZARDOUS SUBSTANCES
Cytotoxic drugs (used in chemotherapy) may be prescribed in the treatment of malignant disease. Cytotoxic drugs, which are toxic agents used to inhibit the growth of malignant cells, may be administered orally, IV or by regional perfusion. As cytotoxic agents are harmful to normal as well as malignant cells, extreme care is required during their preparation and administration.
Although the enrolled nurse may not be required to prepare or administer cytotoxic drugs, they may nonetheless assist in the care of a client receiving chemotherapy. It is essential therefore that the nurse is aware of, and understands, the related safety guidelines. Clear guidelines, which are developed by health authorities and are available in healthcare facilities, set down procedures to be followed in the preparation and administration of cytotoxic agents. In addition, the guidelines specify how to deal with spillages, extravasation (leakage of antineoplastic agents into the client’s subcutaneous tissues) and the safe disposal of used equipment and the client’s body wastes. Nurses who are pregnant should avoid contact with any cytotoxic agent, especially during the first trimester, when fetal organs are developing.
A material safety data sheet (MSDS) should be available with every hazardous substance used in a healthcare facility. The MSDS is the primary source of safety information provided for people using hazardous substances in the workplace. It provides essential information, direct from the manufacturer, about what to do in the event of leakage, spillage or any type of accident or incident involving the chemical (Arnold 2003). See Chapter 20 for more information about cleaning and spills.
SAFE STORAGE, ADMINISTRATION AND DISPOSAL OF MEDICATIONS
Safety precautions with medications in the healthcare facility include:
• Locking the area in which medications are stored, to make it inaccessible to unauthorised persons
• Recognising that the pharmacist is responsible for the contents of most medical substances supplied
• Recognising that only the pharmacist may attach or alter a label, fill a container or transfer medication from one container to another. If a label on a container is illegible, the container must be returned to the pharmacist for clarification
• Observing the safety precautions for the administration of all medications.
MEDICATIONS AND THE OLDER ADULT
Older adults are at particular risk of poisoning by prescribed medications, evidenced by them being admitted to hospital with adverse drug reactions more often than younger adults. They are at higher risk of poisoning by medications because age alters the rate at which medications are absorbed, metabolised and excreted from the body. If the process is significantly slow, drug toxicity can occur. This problem can be exacerbated because body weight is often lost as people age, resulting in altered distribution of drugs around the body and the need for a lower dose than has been prescribed (Bryant & Knights 2011).
Older adults generally consume more prescription and over-the-counter drugs than other people and they frequently take a combination of many different drugs on a daily basis. Sometimes older people are referred to specialist medical officers and are prescribed medications by more than one of them. This results in what is known as poly-pharmacy, a potentially dangerous indiscriminate use of multiple medications at the same time (Bryant & Knights 2011). Nurses can help prevent poisoning by prescribed medication in older adults by keeping these factors in mind, and actively:
• Observing for and promptly reporting any signs of toxicity; for example, tinnitus, gastric disturbance, mental status changes, visual disorders
• Advocating for frequent reviews of client medication regimens
• Encouraging older clients to ask questions of the medical officer, registered nurse (RN) or pharmacist about prescribed and non-prescribed herbal or other drugs
• Encouraging older people to discuss with the medical officer the possibility of withdrawing medications that may no longer be essential
• Ensuring that non-pharmacological approaches are considered whenever appropriate
• Checking that the client has understood instructions about taking medications and, if necessary, seeking the help of an RN to clarify instructions.
Enrolled nurses (ENs) can participate in medication-related interventions only in accordance with the code of practice in their geographical area and only in accordance with their level of knowledge and expertise. Clinical Scenario Box 22.1 looks at the use of brand substitution for certain drugs.
Clinical Scenario Box 22.1
Mary is a 75-year-old woman who presents to hospital for a hip replacement.
She has a history of atrial fibrillation, hypertension, gastro-oesophageal reflux disease and type 2 diabetes for which she is stable on her current medication regimen. She is a widow and lives with her son. Mary is ambulant and self-caring with no obvious impaired cognitive function.
Mary’s medications are metformin 500 mg twice daily, glibenclamide 5 mg daily, digoxin 125 micrograms daily, atenolol 50 mg daily, enalapril 5 mg daily, omeprazole 20 mg daily and warfarin usually 5 mg daily. Mary states that the last few times she had scripts filled she was asked if she would like the cheaper alternative, when available, and was reassured that the actual medicine remains the same. Mary was happy about the reduced cost of some of the medicines but remains concerned about different brands being effective and safe.
CONTINUATION OF MEDICATION AFTER DISCHARGE
Before discharge from a healthcare facility with medications, the nurse must ensure that the client:
• Has been instructed adequately and is able to demonstrate safe self-medication techniques
• Understands the medication regimen, including the purpose of the prescribed medications, the frequency of administration and any contraindications
• Understands the importance of any related blood tests
• Understands the importance of not stopping medications abruptly without first discussing the matter with the general practitioner or other medical officer
• Is advised to consult the medical officer about any untoward effects from the medication
• Understands the importance of notifying other health professionals about the medication regimen; for example, the visiting community health nurse
• Understands the reasons for not sharing medications with others
• Knows how to store the medications correctly and safely
• Has the contact numbers for emergency services—for example, ambulance service and Poisons Information Centre—readily at hand (e.g. kept close to the telephone)
• Knows how to discard out-of-date or unwanted medications safely
• Knows how to dispose of used syringes and needles safely if used.
Alternatively, if the client is unable to complete the above, then a family member or friend should be instructed in the safe administration of the medication, covering all the points listed above. Another alternative is a visiting nurse, who may be required to call on the client at home and assist in the administration or monitoring of the drug therapy. The nurse may also be able to gain an understanding of any difficulties the client is experiencing, offer information that may help the client deal with them, and monitor the client’s compliance/concordance/adherence with the medical officer’s directions. Sometimes clients do not comply/adhere with the prescribed medication regimen after they return home. There are a variety of reasons why this may occur (Clinical Interest Box 22.5).
CLINICAL INTEREST BOX 22.5 Non-compliance/concordance/adherence with medication—issues for the nurse to consider
How many of us have been guilty of not completing a course of antibiotics because we ‘feel better’ or forget to take them and decide we are better anyway, or keep a few of those antibiotics for the next time it happens, to save going to the medical officer again? Non-compliance/concordance/adherence with drug therapy can be both deliberate and unintentional. Some reasons for non-compliance/concordance/adherence with drug therapy are that clients:
• Do not understand the information given to them
• Disregard the information given to them, perhaps because they do not believe in, or have a fear of, using drugs or believe another sort of remedy is more likely to be effective. Attitudes and beliefs about drugs can be influenced by cultural background and past experiences with drugs
• Alter the drug regimen to fit with lifestyle; for example, only eating meals twice a day so only taking a drug twice a day instead of as ordered, that is, three times a day with meals
• Decrease dose or stop medication because of adverse effects
• Take double doses to make up for missed doses
• Stop medication because there is no change in condition (‘It isn’t doing me any good’)
• Perceive that they do not need them anymore
• Receive unclear directions (given in a rush, too much jargon, given rapidly in English when English is not the first language of the client)
• Have problems with changing routine; for example, their medication routine differs from their previous regimen
• Have difficulty implementing the regimen; for example, multiple medications to be taken at several different times of the day
Several nursing interventions may enhance the ability and willingness of clients to comply with the prescribed medication regimen (see Clinical Interest Box 22.6).
Measures to assist older clients taking medications safely at home include the use of a controlled dispenser that contains the medications for each day and time in a separate section (Fig 22.15).
When an older client has visual impairment it will help if instructions for taking the medications are clearly printed in large bold letters. If clients are confused it may be necessary for the medications to be taken under the supervision of a family member and kept out of reach at other times. Clinical Interest Box 22.6 provides suggestions to help the nurse enhance client compliance/concordance/adherence with medication regimens after discharge.
CLINICAL INTEREST BOX 22.6 Nursing actions to enhance client compliance/concordance/adherence with medication regimens after discharge
• Ensure the client understands English clearly; if they do not, arrange for an interpreter
• Assess the client’s memory and cognitive function for understanding and retention of information
• Ensure the client can hear you; for example, hearing aid in place and switched on
• Ensure the client will be able to concentrate; for example, is not uncomfortable, needing the toilet, in pain, thirsty, hungry or anxious
• Ensure a quiet, calm private area is available so that client is not distracted while you are providing information and so that the client’s medical condition remains confidential
• Provide verbal and written instructions to the client and family member when appropriate. Other visual material may be available (video instructions are available for education about certain medications, such as insulin)
• Ask the client to repeat instructions back to you to check the accuracy of their understanding, and encourage them to ask any questions they have about the purpose of the medication and when and how to take it. If necessary, arrange for a visiting nurse to check on the client’s ability to cope with more complex medications, such as insulin injections and disposal of sharps. In the home sharps can be safely disposed of in an empty plastic milk container that has a screw top cap and a 1:10 bleach:water solution in the bottom of it. The environmental biohazard waste-management strategies in the local area should be followed when disposing of the full container
• Ensure adequate time is given to educating the client about medication. Avoid giving instructions just as the client is ready to leave the hospital. Provide time for client to practise and demonstrate their ability with devices such as needles and syringes or nebulisers and inhalers
Willingness to follow the medication regimen
• Discuss the client’s feelings, attitudes and beliefs about the medication prescribed. If the client indicates an unwillingness to carry out the medication after being provided with reasons to comply, refer this information to the medical officer and nurse in charge. Alternative therapies may be possible
• Discuss how the regimen fits in with the client’s lifestyle and how any adverse effects might cause a problem to planned activities
Ability to follow the medication regimen
• Ensure that the client will be able to read labels on medication pots and bottles. If vision is a problem, contact the pharmacy about printing bigger labels or providing additional large print information
• Check that motor skills will allow the client to successfully use the medication; for example, that they can open the childproof lid on the container, or are able to pour out liquid medication or instil their own eye or ear drops
• Evaluate the client’s social situation; for example, is the cost of the medication a problem? Is the client sufficiently mobile to go to the pharmacist to fill the prescription?
This is certainly not an exhaustive list. Make a list of your own and see how many more actions you can add to it.
Summary
As part of the holistic care of the client, the enrolled nurse may be required to administer and monitor the effects of medications; it is therefore essential to have the necessary knowledge to ensure the safety of all clients who are receiving medications. Of particular importance is an understanding of the legal responsibilities involved in administering medication. Nurses must be willing to accept that responsibility and work within the boundaries dictated by the nursing registering bodies governing the geographical area of their work. To promote accurate and safe drug administration the nurse must understand the system of weights and measures used in prescriptions, know the meanings of abbreviations and be competent in performing the correct calculation of dosages.
The nurse must have a basic understanding of how drugs are transported in the body, how they act, how they are metabolised and how they are excreted. Furthermore, it is important to have an understanding of the actions of the various drug groups so that the nurse will know what the desired effects of the drug are and will therefore be able to monitor the client’s reaction more adequately.
Drugs are presented in a variety of forms, for example, tablets, capsules, mixtures and injectable solutions, which are administered via a variety of different routes. The nurse should not only be competent in administering medication via these routes, but also in monitoring both the desired effects and any side effects that may occur.
The nurse must observe the seven rights of drug administration (right client, right medication, right dose, right route, right time, right documentation, client right to refuse) at all times and understand the procedure if a medication error does occur. To maintain a safe working environment it is important that the nurse understands the guidelines regarding safe handling of hazardous substances. The nurse has an important role in ensuring that the client understands all aspects of any prescribed drug regimen before being discharged from a healthcare facility. Nurses must follow the principles of asepsis during the preparation and administration of medications via any route and must constantly assess and promote the client’s safety and comfort throughout the administration of any drug therapy.
1. There are many factors that can result in a client not being compliant/concordant/adherent with drug therapy. What are some of the reasons for non-compliance/concordance/adherence? Outline some nursing actions that you could apply before a client is discharged to reduce the risk of non-compliance/concordance/adherence with drug therapy.
2. Children and the elderly are usually prescribed different doses of medications than the ‘average’ adult. What do you think the reasons for this are? Outline nursing actions which could assist these groups in receiving the correct medications in the correct dosage.
3. Describe the nursing actions if a nurse is unable to administer medications due to the client being ‘nil orally’ or refusing to take medications.
1. What are the three different names a drug may have?
2. Name the major routes of drug administration.
3. Drug absorption depends on three (3) factors. Name them.
4. What is first-pass metabolism?
5. What is the role of the plasma proteins in drug distribution?
6. What is the difference between a ‘bound’ drug and an ‘unbound’ drug?
7. Define the terms ‘enzyme induction’ and ‘enzyme inhibition’.
8. How would decreased renal function affect drug excretion?
9. Why is therapeutic drug monitoring important?
10. Explain the differences between side effects, toxic effects and allergic reactions.
11. What do the Poisons Act and Poisons Regulations of each state and territory deal with?
12. Which enrolled nurses may have a notation on their nursing registration and why?
13. What are the ‘seven rights’ the nurse must observe when administering a drug?
14. How does the nurse identify the correct client?
15. What does the nurse do if there is any doubt about a drug order?
16. What is the procedure to follow if a drug error occurs?
17. What are the three (3) most common ways of administering a parenteral drug?
18. Name the common sites for subcutaneous injections.
19. Name the common sites for intramuscular injections.
20. Why is it important to discard used injection needles without recapping them?
1. Convert the following to milligrams (mg)
2. Convert the following to grams (g)
3. Convert the following to micrograms
4. Convert the following to milligrams (mg)
5. Your client is prescribed 450 mg soluble aspirin orally. Stock on hand are 300 mg strength tablets. How many tablets would you administer?
6. Mr Stewart is ordered 0.125 mg digoxin orally daily. Digoxin tablets are available in 62.5 microgram strength. How many tablets should you administer to Mr Stewart?
7. Mr Newton has epilepsy and has been ordered phenobarbitone 140 mg IM stat for seizures. Stock ampoules contain 200 mg/mL. What volume should be administered?
8. Maddy is a 10-month-old infant weighing about 10 kg. She is ordered atropine 10 microgram/kg as a premedication. What volume is required if the atropine ampoule contains 0.1 mg/mL?
9. Your client is prescribed penicillin syrup 250 mg orally 6-hourly. Penicillin syrup is available as 250 mg/5 mL. Calculate the total amount (in mL) that your client will receive in a 24-hour period.
10. Poppy Koulouris is ordered 500 mL normal saline to be delivered over 24 hours.
11. If Alex Brown is ordered 1 L of dextrose 5% to be given over 8 hours, what rate would you set the volumetric pump at?
12. Sara Hart has been ordered 500 mL normal saline. The volumetric pump has been set at 25 mL/hour. How long will the fluid last?
13. Calculate the required drip rate in drops per minute (using a drip chamber that delivers 20 drops/mL) if Alice Ball is to have 100 mL normal saline delivered over 1 hour.
14. Mr Lee is critically ill and has two intravenous lines inserted. One line is running at 45 mL/hour, the second at 30 mL/hour. What volume of fluid would Mr Lee receive over 24 hours?
References and Recommended Reading
Arcangelo V, Peterson A. Pharmacotherapeutics for Advanced Practice: A practical approach, 3rd edn. Philadelphia: Lippincott Williams & Wilkins, 2006.
Arnold N. New NOHSC National Code of Practice for the Preparation of Material Safety Data Sheets. Risk Review. Online. Available: www.noel-arnold.com.au/content/uploads/pdfs/Risk%20Reviews/2003/09_NOHSC_Code_of_Practice_for_MSDS.pdf, 2003.
Australian Commission on Safety and Quality in Health Care. National Inpatient Medication Chart. Online. Available: www.health.gov.au/internet/safety/publishing.nsf/content/80A0EF37F281A8D7CA25718F000CCC2F/$File/chverse.pdf, 2006.
Australian Commission on Safety and Quality in Health Care. National Terminology, Abbreviations and Symbols to be Used in the Prescribing and Administering of Medicines in Australian Hospitals. Online. Available: www.health.gov.au/internet/safety/publishing.nsf/Content/com-pubs_NIMC-terminology/$File/32060v2.pdf, 2011.
Australian Government, Department of Health and Ageing, Therapeutic Goods Administration. Poisons Standard 2010. Online. Available: www.comlaw.gov.au/Details/F2010L02386, 2010.
Bryant B, Knights K. Pharmacology for Health Professionals, 3rd edn. Sydney: Elsevier, 2011.
Crisp J, Taylor C. Potter & Perry’s Fundamentals of Nursing, 3rd edn., Sydney: Elsevier, 2009.
deWit S. Fundamental Concepts and Skills for Nursing, 3rd edn. Philadelphia: WB Saunders, 2009.
Ebersole P, Hess P, Touhy TA, et al. Toward Healthy Ageing: Human Needs & Nursing Response, 7th edn. St Louis: Mosby Elsevier, 2008.
Elliot D, Aitken L, Chaboyer W. Critical Care Nursing. Sydney: Elsevier, 2007.
Galbraith A, Bullock S, Manias E. Fundamentals of Pharmacology, 5th edn. Melbourne: Addison Wesley, 2006.
Gatford J, Phillips N. Nursing Calculations, 7th edn. Melbourne: Churchill Livingstone, 2006.
Healy D. Psychiatric Drugs Explained, 5th edn. Edinburgh: Elsevier, 2009.
Jackson S, Jansen P, Mangoni A. Prescribing for Elderly Clients. Oxford, UK: Wiley-Blackwell, 2009.
Katzung BG. Basic and Clinical Pharmacology, 10th edn. New York: McGraw-Hill Medical, 2007.
Kester M, Vrana KE, Quraishi SA, et al. Elsevier’s Integrated Pharmacology. Philadelphia: Mosby Elsevier, 2007.
National Institute of Standards and Technology (NIST). International System of Units (SI). Online. Available: http://physics.nist.gov/cuu/index.html, 2003.
Nursing and Midwifery Board of Australia (NMBA). Explanatory Note: Enrolled Nurses and Medicine Administration. Online. Available: www.nursingmidwiferyboard.gov.au/FAQ-and-Fact-Sheets.aspx, 2010.
Potter PA, Perry AG. Fundamentals of Nursing, 6th edn. St Louis: Mosby, 2004.
Potter PA, Perry AG. Fundamentals of Nursing, 7th edn. St Louis: Mosby, 2008.
Potter PA, Perry AG, et al. Fundamentals of Nursing, 8th edn. St Louis: Mosby, 2013.
Reiss BS, Evans ME, Broyles BE. Pharmacological Aspects of Nursing Care, 7th edn. New York: Thomson Delmar Publishing, 2007.
Roach S. Pharmacology for Health Professionals. Philadelphia: Lippincott Williams & Wilkins, 2005.
Tiziani A. Havard’s Nursing Guide to Drugs, 8th edn. Sydney: Elsevier, 2010.
Australian Prescriber, www.australianprescriber.com.
Medsafe (NZ), www.medsafe.govt.nz.
National Prescribing Service (NPS), www.nps.org.au.
Paediatric Pharmacopoeia of Royal Children’s Hospital, Melbourne, www.rch.org.au/pharmacy/dev/index.cfm?doc_id=11341.
Pharmaceutical Management Agency New Zealand (PHARMAC), www.pharmac.govt.nz.
Therapeutic Guidelines, www.tg.org.au.