Patient Radiation Dose Management
At the completion of this chapter, the student should be able to do the following:
1 Indicate three ways that patient dose can be reported
2 Discuss ALARA principles applied to patient radiation dose management
3 Discuss factors that affect patient radiation dose
4 Discuss the radiosensitivity of the stages of pregnancy
5 Describe the recommended management procedures for the pregnant patient
6 Describe the intensity and distribution of radiation dose in mammography and computed tomography
7 Identify screening x-ray examinations that are no longer performed routinely
ALL MEDICAL health physics activity is directed in some way toward minimizing the radiation exposure of radiologic personnel and the radiation dose to patients during x-ray examination. Radiation exposure of radiologists and radiologic technologists is measured with the use of occupational radiation monitors. Patient dose usually is estimated by conducting simulated x-ray examinations with human phantoms and test objects.
If radiation control procedures are adopted, occupational radiation exposure and patient dose can be kept acceptably low. Health physicists subscribe to ALARA—keep radiation exposure as low as reasonably achievable. Radiologic technologists should follow this guide as well.
Patient Dose Descriptions
Exposure of patients to medical x-rays is commanding increasing attention in our society for two reasons.
First, the frequency of x-ray examination is increasing among all age groups, at a rate of approximately 18% per year in the United States. This indicates that physicians are relying more and more on x-ray diagnosis to assist them in patient care, even taking into account the newer imaging modalities.
This is to be expected. X-ray diagnosis is considered much more accurate today than in the past. More rigorous training programs required of radiologists and radiologic technologists and improvements in diagnostic x-ray imaging systems allow for more difficult, but more substantive, x-ray examinations. Efficacy and diagnostic accuracy are much improved.
Second, concern among public health officials and radiation scientists is increasing regarding the risk that is associated with medical x-ray exposure. Acute effects on superficial tissues after angiointerventional procedures are reported with increasing frequency.
The possible late effects of diagnostic x-ray exposure are of concern; therefore, attention must be given to good radiation control practices. When a diagnosis can be obtained with a low radiation dose, it should be used because of reduced risk. This is in keeping with ALARA.
Estimation of Patient Dose
Patient dose from diagnostic x-rays usually is reported in one of three ways. Exposure to the entrance surface, or entrance skin dose (ESD), is reported most often because it is easy to measure.
The gonadal dose is important because of possible genetic responses to medical x-ray exposure. The dose to the gonads is not difficult to measure or estimate.
The dose to the bone marrow is important because bone marrow is the target organ believed responsible for radiation-induced leukemia. Bone marrow dose cannot be measured directly; it is estimated from ESD.
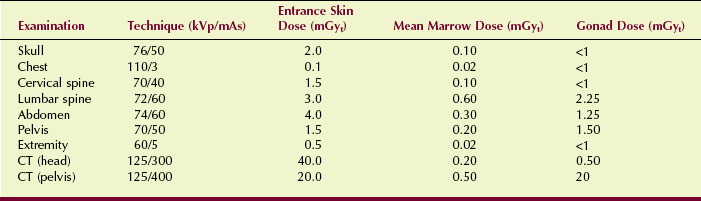
Table 37-1 presents some representative values of ESD and gonadal dose for various x-ray examinations. The mean marrow dose for each procedure also is presented. Note that these are only approximate values and should not be used to estimate patient dose at any facility.
In any given x-ray facility, actual doses delivered may be considerably different. Efficiency of x-ray production and image receptor speed are the most important variables. These values provide for relative dose comparisons among various radiologic examinations. Doses during fluoroscopy are too dependent on technique, equipment, and beam-on time to be estimated easily. Usually, such doses must be measured.
Entrance Skin Dose
ESD most often is referred to as the patient dose. It is used widely because it is easy to measure, and reasonably accurate estimates can be made in the absence of measurements.
Thermoluminescence dosimeters (TLDs) are used most often. The size, sensitivity, and accuracy of TLDs make them very satisfactory patient radiation monitors.
A small grouping or pack of 3 to 10 TLDs can be taped easily to the patient’s skin in the center of the x-ray field. Because the response of the TLD is proportional to exposure and dose, the TLD can be used to measure all levels experienced in diagnostic radiology. With proper laboratory technique, the results of such measurements are accurate to within 5%.
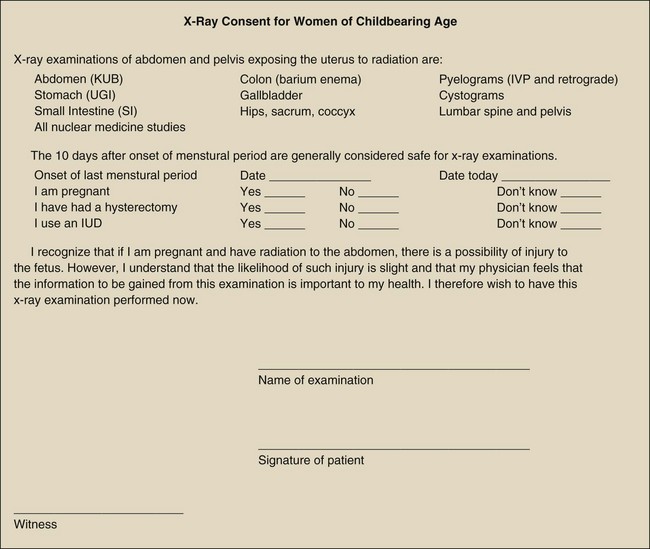
Two rather straightforward methods for estimating ESD are available in the absence of patient measurements. The first requires the use of a nomogram such as that shown in Figure 37-1. This figure contains a family of curves from which one can estimate the output intensity of a radiographic unit if the technique is known or assumed. The output intensity of different x-ray imaging systems varies widely, so the use of this nomogram method is good only to perhaps 50%.
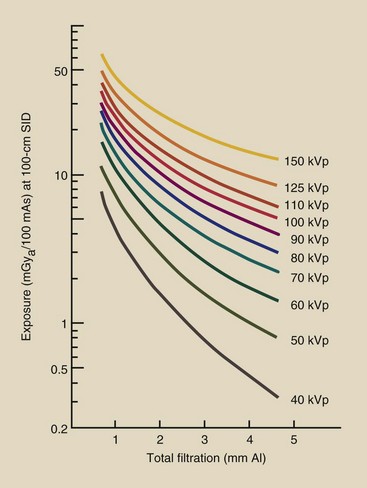
FIGURE 37-1 This family of curves is a nomogram for estimating output x-ray intensity from a single-phase radiographic unit. (Courtesy John R. Cameron,† University of Wisconsin.)
Use of this nomogram first requires knowledge of the total filtration in the x-ray beam. This is usually available from the medical physics report, but if not, 3 mm Al is a good estimate. Next, the kVp and mAs of the intended examination should be identified.
A vertical line rising from the value of total filtration should be drawn until it intersects with the kVp of the examination. From this intersection, a horizontal line is drawn to the left until it intersects the mGyt/mAs axis. The resultant mGyt/mAs value is the approximate output intensity of the radiographic unit. This value should be multiplied with the examination mAs value to obtain the approximate patient exposure.
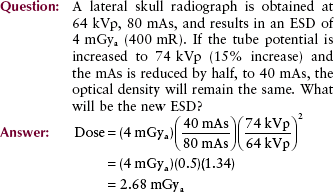
| Question: | With reference to Figure 37-1, estimate the ESD from a lateral cervical spine image made at 66 kVp, 150 mAs, with a radiographic unit having 2.5 mm Al total filtration. |
| Answer: | Estimate the intersection between a vertical line rising from 2.5 mm Al and a horizontal line through 66 kVp. Extend the horizontal line to the y-axis and read 38 µGyt/mAs. 38 µGyt/mAs × 150 mAs = 5700 µGyt = 5.7 mGyt |
A better approach requires that a medical physicist construct a nomogram such as that shown in Figure 37-2 for each radiographic unit. A straight edge between any kVp and mAs value will cross the ESD scale at the correct mGyt value.
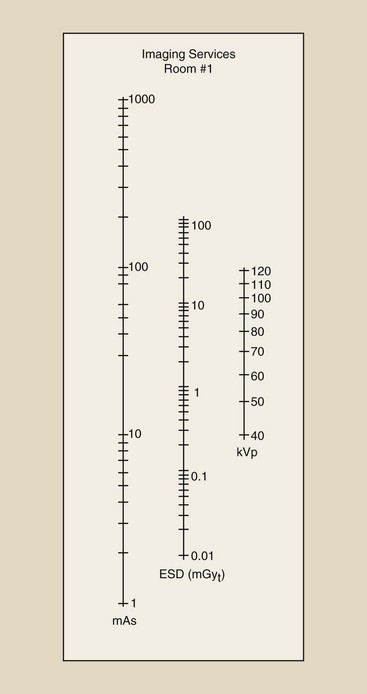
FIGURE 37-2 This type of nomogram is very accurate but must be fashioned individually for each radiographic unit. (Courtesy Michael D. Harpen, University of South Alabama.)
| Question: | Using the nomogram in Figure 37-2, identify the ESD when a radiographic exposure is made at 66 kVp, 150 mAs. |
| Answer: | The line is drawn as shown and crosses the ESD scale at 10 mGyt. |
A third method for estimating ESD requires that one know the output intensity for at least one operating condition. During the annual or special radiation control survey and calibration of an x-ray imaging system, the medical physicist measures this output intensity, usually in units of mGyt/mAs at 80 cm—the approximate source-to-skin distance (SSD)—or at 100 cm—the source-to-image receptor distance (SID). At 70 kVp, radiographic output intensity varies from approximately 20 to 100 µGyt/mAs at 80 cm SSD.
With this calibration value available, one first would make adjustment for a different SSD by applying the inverse square law.
| Question: | The output intensity of a radiographic unit is reported as 37 µGya/mAs (3.7 mR/mAs) at 100 cm SID. What is the intensity at 75 cm SSD? |
| Answer: | At 75 cm SSD, the intensity will be greater by (100/75)2 = (1.32)2 = 1.78 37 µGya/mAs × 1.78 = 66 µGya/mAs |
With the ESD, one scales this according to the kVp and mAs of the examination. Output intensity varies according to the square of the ratio in terms of the change in kVp. Refer to Chapter 8 to review this relationship.
| Question: | The output intensity at 70 kVp and 75 cm SSD is 66 µGya/mAs (6.6 mR/mAs). What is the output intensity at 76 kVp? |
| Answer: | At higher kVp, the output intensity is greater by the square of the ratio of the kVp. (76/70)2 = (1.09)2 = 1.18 66 µGya/mAs × 1.18 = 78 µGya/mAs |
The final step in estimating ESD is to multiply the output intensity in mGya/mAs by the examination mAs value because these values are proportional.
| Question: | If the radiographic technique for an intravenous pyelogram calls for 80 mAs, what is the ESD when the output intensity is 78 µGya/mAs (7.8 mR/mAs)? |
| Answer: | 78 µGya/mAs × 80 mAs = 6240 µGya = 6.24 mGya |
These steps can be combined into a single calculation, as illustrated in the following example.
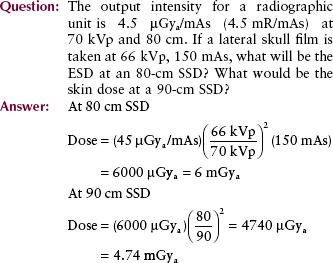
ESD in fluoroscopy is much more difficult to estimate because the x-ray field moves and sometimes varies in size. If the field were of one size and stationary, ESD would be directly related to exposure time.
| Question: | A fluoroscopic procedure requires 2.5 min at 90 kVp, 2 mA. What is the approximate ESD? |
| Answer: | ESD = (40 mGyt/min) (2.5 min) = 100 mGyt |
Mean Marrow Dose
The hematologic effects of radiation are rarely experienced in diagnostic radiology. It is appropriate, however, that we understand the mean marrow dose, which is one measure of patient dose during diagnostic procedures.
The mean marrow dose is the average radiation dose to the entire active bone marrow. For instance, if during a particular examination, 50% of the active bone marrow were in the primary beam and received an average dose of 250 µGyt (25 mrad), the mean marrow dose would be 125 µGyt (12.5 mrad).
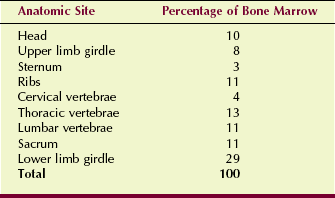
Table 37-1 includes the approximate mean marrow dose in adults for various radiographic examinations. In children, these levels generally would be lower because the radiographic techniques used are considerably less. Table 37-2 shows the distribution of active bone marrow in the adult, and this gives some clue as to which diagnostic x-ray procedures involve exposure to large amounts of bone marrow.
In the United States, the mean marrow dose from diagnostic x-ray examinations averaged over the entire population is approximately 1 mGyt/yr (100 mrad/yr). Such a dose never results in the hematologic responses described in Chapter 32. It is a dose concept, however, that is used to estimate, on a population basis, the risk of one late effect of radiation—leukemia.
Genetically Significant Dose
Measurements and estimates of gonad dose are important because of the suspected genetic effects of radiation. Although the gonad dose from diagnostic x-rays is low for each individual, this may have some significance in terms of population effects.
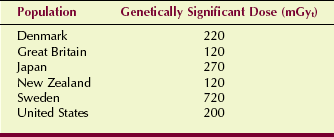
The population gonad dose of importance is the GSD, the radiation dose to the population gene pool. Thus, it is a weighted-average gonad dose. It takes into account those persons who are irradiated and those who are not, with averaging of the results. The GSD can be estimated only through large-scale epidemiologic studies.
For computational purposes, therefore, the GSD considers the age, sex, and expected number of children for each person examined with x-rays. It also acknowledges the various types of examinations and the gonadal dose per examination type.
Estimates of GSD have been conducted in many different countries (Table 37-3). The estimate reported by the U.S. Public Health Service is 0.2 mGyt/yr (20 mrad/yr). Thus, this is a genetic radiation burden over and above the existing natural background radiation level of approximately 1 mGyt/yr (100 mrad/yr). The genetic effects of this total GSD—1.2 mGyt/yr (120 mrad/yr)—are not detectable.
Patient Dose in Special Examinations
Because of the considerable application of x-rays for examination of the female breast and concern for the induction of breast cancer by radiation, it is imperative that we have some understanding of the radiation doses involved in such examinations.
An ESD of approximately 8 mGya/view (800 mR/view) is normal. Increasing the x-ray tube potential much beyond 26 kVp degrades the image unacceptably; therefore, further dose reduction by technique manipulation is unlikely.
Radiographic grids are used in most screen-film mammography examinations. Grid ratios of 4 : 1 and 5 : 1 are most popular. The contrast enhancement produced by the use of such grids is significant, but so is the increase in patient dose. Patient dose is increased by approximately two times with the use of such grids compared with the nongrid technique.
The values stated for patient dose in mammography can be misleading. Because of the low x-ray energies used in mammography, the dose falls off very rapidly as the x-ray beam penetrates the breast. If the ESD for a craniocaudad view is 8 mGya (800 mR), the dose to the midline of the breast may be only 1.0 mGyt (100 mrad).
Fortunately, it is known that the risk of an adverse biologic response from mammography is small. Certainly, it is nothing about which a patient should be concerned. Any possible response, however, is related to the average radiation dose to glandular tissue, and not to skin exposure. Glandular dose (Dg) varies in a complicated way, with variations noted in x-ray beam quality and quantity.
Specification of an ESD can be misleading when one considers a two-view examination, such as that used for screening (Figure 37-3). Consider an examination that consists of craniocaudad and mediolateral oblique views, each of which produces an ESE of 8 mGya (800 mR).
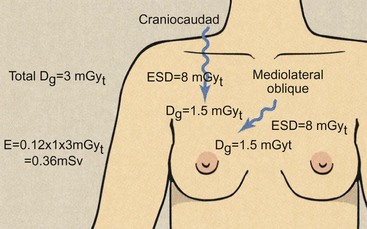
FIGURE 37-3 Two mammographic exposures result in a total glandular dose that is the sum of the individual glandular doses.
It would be incorrect to describe this total examination procedure as resulting in an ESD of 16 mGya (1.6 R). Skin doses from different projections cannot be added. We must specify the skin dose for each view or attempt to estimate the total Dg.
Total Dg can be estimated by approximating that the contribution from each view will be 15% of the ESD. Consequently, the total Dg would be the sum of (0.15 × 8 = 1.2 mGyt) as the contribution from each of the craniocaudad and mediolateral oblique views. The total Dg would, therefore, be 2.4 mGyt.
From this discussion, it would seem that patient dose in mammography can be considerably reduced if the number of views is restricted. The axillary view should not be done routinely. For screening programs, no more than two views per breast are advisable. Digital mammography should result in lower Dg than that attained with screen-film mammography.
Dose in Computed Tomography Imaging
An important consideration in computed tomography (CT) imaging, as with any x-ray procedure, is not only the skin dose but also the distribution of dose to internal organs and tissues during imaging. On the basis of skin dose, CT results in a higher dose than other diagnostic x-ray procedures. The skin dose delivered by a series of contiguous CT slices is much higher than that delivered by a single radiographic view. A typical radiographic head or body examination, however, often involves several views.
Because of increasing use of multislice helical CT, CT must be considered a high-dose procedure. U.S. Public Health Service data suggest that 10% of all x-ray examinations are now CT, yet CT accounts for 70% of total patient effective dose. The CT tissue dose is approximately equal to the average fluoroscopic dose.
As was pointed out in Chapter 28, CT differs in many important ways from other x-ray examinations. A radiograph can be likened to a photograph taken with a flash in that the patient is “floodlighted” with x-rays to directly expose the image receptor.
On the other hand, CT images the patient with a fine, collimated beam of x-rays. This difference in radiation delivery also means that the dose distribution from CT is different from that in radiographic procedures.
The CT dose is nearly uniform throughout the imaging volume for a head examination. The CT dose is approximately 50% of the ESD for body CT. Radiographic and fluoroscopic doses are high at the entrance surface and very low at the exit surface.
Part of the dose efficiency of CT is attributable to the precise collimation of the x-ray beam. Scatter radiation increases patient dose and reduces radiographic contrast. Because CT uses narrow, well-collimated x-ray beams, scatter radiation is reduced significantly, and contrast resolution is improved significantly. Thus, a larger percentage of the x-ray beam contributes usefully to the image.
The precise collimation used in CT means that only a well-defined volume of tissue is irradiated for each image. The ideal x-ray beam for CT would have sharp boundaries. No overlap between adjacent images would be seen. Thus, the dose delivered to a patient from a series of ideal contiguous CT images should be the same as that from a single slice.
Figure 37-4 illustrates, however, why this ideal situation cannot be attained in practice. The size of the focal spot of the x-ray tube blurs the sharp boundaries of the section. Also, the x-ray beam is not precisely parallel, and some spreading occurs as the beam crosses the image field.
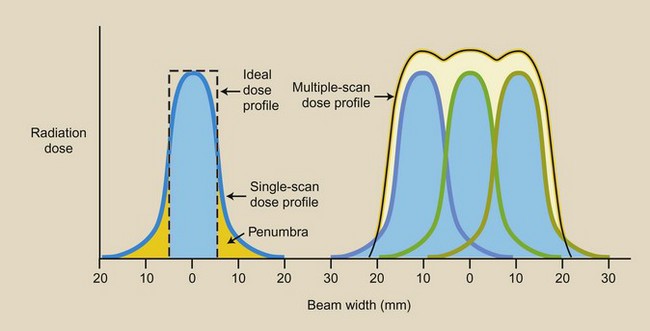
FIGURE 37-4 Patient dose distribution in step-and-shoot multislice spiral computed tomography is complicated because the profile of the x-ray beam cannot be made sharp.
If a series of adjacent images is performed with an automatically indexed patient couch, the couch movement must be precise. If the couch moves too much between images, some tissue will be missed. If it moves too little, some tissue in each image will be doubled-exposed.
Multislice helical CT results in lower patient radiation dose than step-and-shoot CT because fewer tails are seen on the dose profile for a given volume of tissue. The dose profile tail is called a penumbra.
Typical CT doses range from 30 to 50 mGyt (3000 to 5000 mrad) during head imaging and from 20 to 40 mGyt (2000 to 4000 mrad) during body imaging. These values are only approximate and vary widely depending on the type of CT imaging system and the examination technique used. The effective dose for each examination is approximately 10 mSv (1000 mrem).
A 64-slice CT imaging system will result in a lower patient dose than fewer slices because a lower contribution is made from the penumbra for the same volume of tissue (Figure 37-5). Additional patient dose saving occurs when the same beam width is imaged with combined pixel rows (Figure 37-6) because the mA can be reduced without compromising image noise and therefore contrast resolution.
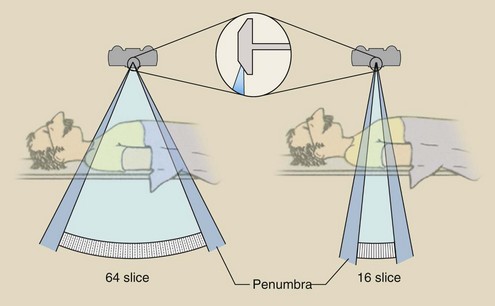
FIGURE 37-5 Patient radiation dose is lower with higher multislice computed tomography because the beam penumbra is less for a given imaged anatomy.
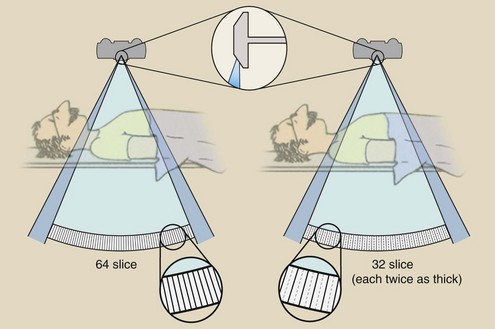
FIGURE 37-6 When two detector rows are combined for the same beam width, patient dose will be lower.
Because the CT x-ray beam is well collimated, the area of irradiation can be precisely controlled. Thus, radiosensitive organs such as the eyes can be avoided selectively. Shields as protection from the primary x-ray beam in CT are of little use. Not only does the metal from shields produce artifacts in the image, but the rotational scheme of the x-ray source greatly reduces their effectiveness.
Patient radiation dose during helical CT is somewhat more difficult to assess than the dose during step-and-shoot CT. At a pitch of 1.0 : 1, the patient radiation dose is approximately the same. At a higher pitch, the dose is reduced compared with conventional CT. At a lower pitch, patient dose is increased.
As with any radiographic procedure, many factors influence patient dose. For CT imaging, a generalization is possible.
Note that, as with radiography, patient dose is proportional to x-ray beam intensity. It is also directly proportional to the average beam energy. Other factors are variables that are unique to CT imaging.
Sigma (σ) is noise. This is equivalent to quantum mottle in screen-film radiography and represents random statistical variations in CT numbers. The w stands for the pixel size, one of the determinants of spatial resolution. The last factor, h, is the beam width.
All other factors being equal, a low-noise, high-resolution CT image results in higher patient radiation dose. The challenge with CT, as indeed with all x-ray imaging, is not so much to deliver fantastically good resolution and low noise (because this could be achieved at the cost of very high patient dose) but to use the x-ray beam efficiently, producing the best possible image at a reasonable dose to the patient.
Reduction of Unnecessary Patient Radiation Dose
The radiologic technologist has considerable control over many sources of unnecessary patient radiation dose. Unnecessary patient radiation dose is defined as any radiation dose that is not required for the patient’s well-being or for proper management and care.
Unnecessary Examinations
The radiologic technologist has practically no control over what some consider the largest source of unnecessary patient dose, that is, the unnecessary x-ray examination. This is almost exclusively the radiologist’s or the clinician’s responsibility. Radiologic technologists can help by asking whether the patient has had a previous x-ray examination. If so, perhaps those images should be obtained for review before any other steps are taken.
Unfortunately, this source of unnecessary patient dose presents a serious dilemma for the radiologist and the clinician. Many x-ray examinations are requested when it is known that the yield of helpful information may be extremely low or nonexistent. When such an examination is performed, the benefit to the patient in no way compensates for the radiation dose.
If the examination is not performed, however, the clinician and the radiologist may be criticized severely if management of the patient’s condition results in failure. Even though the examination in question would have contributed little, if anything, to effective patient management, the radiologist may even be sued. In such situations, the radiologist is caught between the proverbial “rock and a hard place.”
Routine x-ray examinations should not be performed when there is no precise medical indication. Substantial evidence shows that such examinations are of little benefit because they are not cost-effective and the disease detection rate is very low. Examples of such cases are discussed in the following sections.
Mass Screening for Tuberculosis
General screening by chest x-ray examination has not been found to be effective. Better methods of tuberculosis testing are now available. Some x-ray screening in high-risk groups (e.g., medical and paramedical personnel), in service personnel posing a potential community hazard (e.g., food handlers, teachers), and in special occupational groups (e.g., miners, workers having contact with beryllium, asbestos, glass, or silica) may be appropriate.
Hospital Admission
Chest x-ray examinations should not be performed for routine hospital admission when no clinical indication of chest disease is found. Among patients who might be candidates for such examination are those admitted to the pulmonary service.
Preemployment Physicals
hest and lower back x-ray examinations are not justified because the knowledge gained about previous injury or disease through this approach is nil.
Periodic Health Examinations
Many physicians and health care organizations promote annual or biannual physical examinations. Certainly, when such an examination is conducted on an asymptomatic patient, it should not include x-ray examination, especially fluoroscopic examination.
Repeat Examinations
One area of unnecessary radiation exposure that the radiologic technologist can influence is that of repeat examinations. The frequency of repeat examinations has been estimated variously to range as high as 10% of all examinations. In the typical busy hospital facility, the rate of repeat examinations should not normally exceed 5%. Examinations with the highest repeat rates include lumbar spine, thoracic spine, chest and abdomen.
Some repeat examinations are performed because of equipment malfunction. However, most are caused by radiologic technologist error. Studies of causes of repeat examinations have shown that improper positioning and poor radiographic technique resulting in an image that is too light or too dark are primarily responsible for repeats.
Motion and improper collimation are responsible for some repeats. Infrequent errors that contribute to repeat examinations include dirty screens, use of improperly loaded cassettes, light leaks, chemical fog, artifacts caused by a dirty processor, wrong projection, improper patient preparation, grid errors, and multiple exposures.
Radiographic Technique
In general, the use of high-kVp technique results in reduced patient dose. Increasing the kVp is always associated with a reduction in mAs to obtain an acceptable radiographic optical density; this, in turn, results in reduced patient radiation dose.
This dose reduction occurs because the patient dose is linearly related to the mAs but is related to approximately the square of the kVp. An area of radiography for which high-kVp technique is widely accepted is examination of the chest.
Of course, the radiologist must be the final judge of radiographic quality. Increasing kVp even slightly may result in images with contrast that is too low for proper interpretation by the radiologist.
Proper collimation is essential to good radiographic technique. Positive beam limitation does not prevent the radiologic technologist from reducing field size still further through collimation. With the use of collimation, not only is patient effective dose reduced, but image quality is improved with enhanced contrast resolution because scatter radiation also is reduced.
Image Receptor
The image receptor should be selected first for the type of examination that is being performed, and second for the radiation dose necessary to produce a good-quality image. It should be kept in mind that it is screen speed rather than film speed that principally controls patient dose.
Rare Earth and other fast screens should be used when possible. The routine application of such screens in orthopedic, chest, and magnification radiography is appropriate. In some applications, the use of such fast systems may result in bothersome quantum mottle, but this again must be decided by the radiologist. Usually, 400-speed systems are used now for general radiography.
Digital radiographic (DR) image receptors are inherently faster than screen-film. Patient dose should be lower with the use of DR because of increased speed and increased kVp accompanied by reduced mAs.
Patient Positioning
When the upper extremities or the breast is examined, especially with the patient in a seated position, care should be taken that the useful beam does not intercept the gonads. Position the patient lateral to the useful beam and provide a protective apron as a shield.
Specific Area Shielding
X-ray examinations result in partial-body exposure, although most radiation protection guides and radiation response information are based on whole-body exposure. The partial-body nature of the x-ray examination is controlled by proper beam collimation and the use of specific area shielding.
Use of specific area shielding is indicated when a particularly sensitive tissue or organ is in or near the useful beam. The lens of the eye, the breasts, and the gonads frequently are shielded from the primary radiation beam. Two types of specific area shielding devices are used: the contact shield and the shadow shield.
Lens shields are always of the contact type. The contact shielding device is positioned directly on the patient. Gonad shields, on the other hand, can be of the contact or shadow type.
Breast shields are contact shields that are recommended for use during scoliosis examinations. Such examinations often consist of an anterior-posterior (AP) projection, which subjects juvenile breasts to primary beam x-irradiation. The posterior-anterior (PA) projection, however, is equally satisfactory because magnification is of little importance. The PA projection results in a breast dose of only approximately 1% of the AP projection.
Figure 37-7 shows some examples of contact gonad shields. When such contact shields are not purchased commercially, a properly cut piece of protective material is perfectly adequate. Shapes such as hearts, diamonds, triangles, and squares have been used effectively, especially for children.
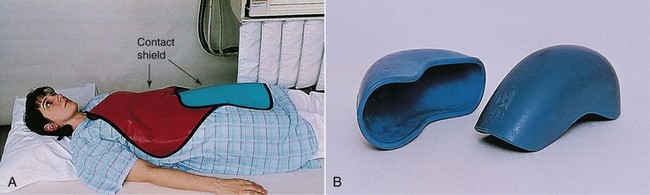
FIGURE 37-7 Examples of useful contact gonad shields, which can be a piece of vinyl lead (A) or shaped (B).
An example of the shadow shield is shown in Figure 37-8. This type of shield is just as effective as the contact shield and is more acceptable for use with adult patients. The use of such devices, however, requires careful attention on the part of the radiologic technologist.
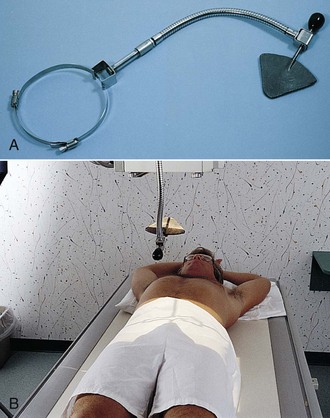
FIGURE 37-8 A, Shadow shield. B, Shadow shield suspended above the beam-defining system casts a shadow over the gonads. (Courtesy Fluke Biomedical.)
The shield must shadow the gonads without interfering with the desired anatomy. Improper positioning of the shadow shield can result in a repeat examination and increased patient dose. Shadow shields are particularly useful during surgery for which sterile procedure is required. Box 37-1 lists the main points of gonadal shielding.
The Pregnant Patient
Two situations in diagnostic radiology require particular care and action. Both are associated with pregnancy. Their importance is obvious from both a physical and an emotional standpoint.
Radiobiologic Considerations
The severity of the potential response to radiation exposure in utero is both time related and dose related, as was discussed in Chapter 36. Unquestionably, the period most sensitive to radiation exposure occurs before birth. Furthermore, the fetus is more sensitive early in pregnancy than late in pregnancy. As a general rule, the higher the radiation dose, the more severe will be the radiation response.
Time Dependence
A grave misunderstanding is that the most critical time for irradiation is during the first 2 weeks, when it is most unlikely that the expectant mother knows of her condition. In fact, this is the time during pregnancy when such irradiation is least hazardous. Pregnancies fail during this period for reasons other than exposure to radiation.
The most likely biologic response to irradiation during the first 2 weeks of pregnancy is resorption of the embryo, and therefore no pregnancy. No other response is likely.
No concern has been expressed over the possibility of induction of congenital abnormalities during the first 2 weeks of pregnancy. Such a response has not been demonstrated in experimental animals or in humans after any level of radiation dose.
The time from approximately the second week to the tenth week of pregnancy is called the period of major organogenesis. During this time, the major organ systems of the fetus are developing. If the radiation dose is sufficiently high, congenital abnormalities may result. Early in organogenesis, the most likely congenital abnormalities are associated with skeletal deformities. Later in this period, neurologic deficiencies are more likely to occur.
During the second and third trimesters of pregnancy, the responses previously noted are unlikely. The results of numerous investigations strongly suggest that if a response occurs after diagnostic irradiation during the latter two trimesters, the principal response would be the appearance of malignant disease during childhood.
These responses to irradiation during pregnancy require a very high radiation dose before the risk of occurrence is significant. No such responses would occur at less than 250 mGy (25 rad).
Such dose levels are highly unlikely, yet they are possible with patients who receive multiple x-ray examinations of the abdomen or pelvis. They are essentially impossible with radiologic technologists because their occupational exposures are so low. No other significant responses have been reported after irradiation in utero.
Dose Dependence
As one might imagine, virtually no information is available at the human level to construct dose-response relationships for irradiation in utero. However, a large body of data on animal irradiation, particularly that in rats and mice, serves as the basis from which such relationships can be estimated. The statements that follow, although attributed to human exposure, represent estimates based on extrapolation from animal studies.
After an in utero radiation dose of 2 Gy (200 rad), it is nearly certain that each of the effects noted previously will occur. The likelihood is small, however, that an exposure of this magnitude would be experienced in diagnostic radiology.
Spontaneous abortion after irradiation during the first 2 weeks of pregnancy is unlikely at radiation doses less than 250 mGy (25 rad). The precise nature of the dose-response relationship is unknown, but a reasonable estimate of risk suggests that 0.1% of all conceptions would be resorbed after a dose of 100 mGy (10 rad).
The response at lower doses would be proportionately lower. Keep in mind, however, that the incidence of spontaneous abortion in the absence of radiation exposure is estimated to be in the 25% to 50% range.
In the absence of radiation exposure, approximately 5% of all live births exhibit a manifest congenital abnormality. A 1% increase in congenital abnormalities is estimated to follow a 100-mGy (10-rad) fetal dose, with a proportionately lower increase at lower doses.
The induction of a childhood malignancy after irradiation in utero is difficult to assess. Risk estimates are even lower than those reported for spontaneous abortion and congenital abnormalities. The best approach to assessing risk of childhood malignancy is to use a relative risk estimate.
During the first trimester, the relative risk of radiation-induced childhood malignancy is in the range of 5 to 10; it drops to approximately 1.4 during the third trimester. The overall relative risk is accepted to be 1.5—a 50% increase over the naturally occurring incidence.
Patient Information
Safeguards against accidental irradiation early in pregnancy present complex administrative problems. This situation is particularly critical during the first 2 months of pregnancy, when such a condition may not be suspected, and when the fetus is particularly sensitive to radiation exposure. After 2 months, the risk of irradiating an unknown pregnancy becomes small because the patient is usually aware of her condition.
If the state of pregnancy is known, then under some circumstances, the radiologic examination should not be conducted. One should never knowingly examine a pregnant patient with x-rays unless a documented decision to do so has been made. When such an examination does proceed, it should be conducted with all of the previously discussed techniques for minimizing patient dose.
When a pregnant patient must be examined, the examination should be done with precisely collimated beams and carefully positioned protective shields. The use of high-kVp technique is most appropriate in such situations. The administrative protocols that can be used to ensure that we do not irradiate pregnant patients vary from complex (elective booking) to simple (posting).
Elective Booking
The most direct way to ensure against the irradiation of an unsuspected pregnancy is to institute elective booking. This requires that the clinician, radiologist, or radiologic technologist determine the time of the patient’s previous menstrual cycle. X-ray examinations in which the fetus is not in or near the primary beam may be allowed, but they should be accompanied by pelvic shielding.
Ideally, the referring physician should be responsible for determining the menstrual cycle and for withholding the examination request if there is any question about its necessity. This may require a radiologist-sponsored educational program that can be conducted easily at regularly scheduled medical staff meetings.
Patient Questionnaire
An alternative procedure is to have the patient herself indicate her menstrual cycle. In many diagnostic imaging departments, the patient must complete an information form before undergoing examination.
These forms often include questions such as, “Are you or could you be pregnant?” and “What was the date of your last menstrual period?” Figure 37-9 is an example of such a simple, yet effective questionnaire for protecting against irradiation of a pregnant patient.
Posting
If neither elective booking nor the request form seems appropriate to a diagnostic imaging service, an equally successful method is to post signs of caution in the waiting room. Such signs could read, “Are you pregnant or could you be? If so, inform the radiologic technologist,” or “Warning—special precautions are necessary if you are pregnant,” or “Caution—if there is any possibility that you are pregnant, it is very important that you inform the radiologic technologist before you have an x-ray examination.”
Figure 37-10 is a helpful poster that is available from the National Center for Devices and Radiological Health. Such posting satisfies our responsibility to the patient and to the health care facility.
FIGURE 37-10 Wall posters with warnings about radiation and pregnancy are available from the National Center for Devices and Radiological Health. (Courtesy National Center for Devices and Radiological Health.)
It has been estimated that less than 1% of all women referred for x-ray examination are potentially pregnant. If a pregnant patient escapes detection and is irradiated, however, what is the subsequent responsibility of the radiology service to the patient, and what should be done?
The first step is to estimate the fetal dose. The medical physicist should be consulted immediately and requested to estimate the fetal dose. If a preliminary review of the examination techniques used (i.e., type of examination, kVp, and mAs) determines that the dose may have exceeded 10 mGyt (1 rad), a more complete dosimetric evaluation should be conducted.
Table 37-4 presents representative fetal dose levels for many examinations. With knowledge of the types of examinations performed and the techniques and apparatus used, the medical physicist can accurately determine the fetal dose. Test objects and dosimetry materials are available to ensure that this determination can be made with confidence.
TABLE 37-4
Representative Entrance Exposures and Fetal Doses for Radiographic Examinations Frequently Performed With a 400-Speed Image Receptor
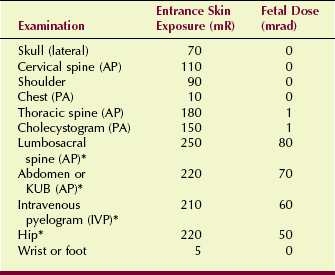
AP, Anteroposterior; IVP, intravenous pyelogram; KUB, kidneys, ureters, bladder; PA, posterior-anterior.
*Gonadal shields should be used if possible.
Once the fetal dose is known, the referring physician and the radiologist should determine the stage of gestation at which x-ray exposure occurred. With this information, only two alternatives are possible: Allow the patient to continue to term, or terminate the pregnancy.
Recommendation for abortion after diagnostic x-ray exposure is rarely indicated. Because the natural incidence of congenital anomalies is approximately 5%, no such effects can reasonably be considered a consequence of diagnostic x-ray doses. Manifest damage to the newborn is unlikely at fetal doses below 250 mGyt (5 rad), although some suggest that lower doses may cause mental developmental abnormalities.
In view of the available evidence, a reasonable approach is to apply a 100- to 250-mGy rule. Below 100 mGyt, a therapeutic abortion is not indicated unless additional risk factors are involved. Above 250 mGyt, the risk of latent injury may justify a therapeutic abortion.
Between 100 and 250 mGyt, the precise time of irradiation, the emotional state of the patient, the effect an additional child would have on the family, and other social and economic factors must be considered carefully.
Fortunately, experience with such situations has shown that fetal doses have been consistently low. The fetal dose rarely exceeds 50 mGyt (5 rad) after a series of x-ray examinations.
Patient Dose Trends
The National Council on Radiation Protection and Measurements (NCRP) issues scientific reports on various aspects of radiation control, including patient radiation dose. The data shown in the pie chart in Figure 1-23 were published in 1990. They show a total annual radiation dose of 3.6 mSv, of which 0.53 mSv results from patient diagnostic radiation exposure.
Figure 37-11 is NCRP data showing the current estimated human radiation exposure profile. Natural sources of radiation exposure remain at 3 mSv, but look what’s happening to medical imaging, 3.2 mSv! The contribution from computed tomography is soaring and represents the overutilization of this imaging modality.
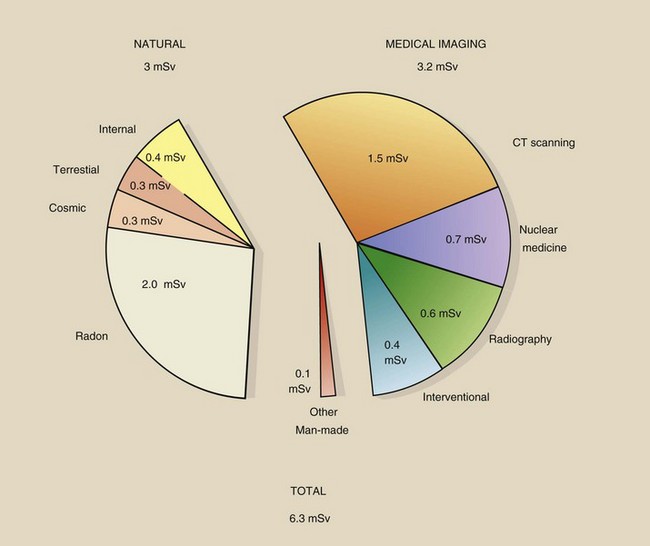
FIGURE 37-11 Current estimated levels of human radiation exposure. (Courtesy Fred Mettler, University of New Mexico.)
This increase in patient radiation dose requires that radiologic technologists and radiologists exercise more control over medical imaging, especially computed tomography, in keeping with ALARA. We must be more aware of appropriateness criteria for diagnostic imaging and gain more control over unnecessary x-ray imaging.
With the introduction of digital imaging we are in a better position to automatically estimate the patient effective dose for each x-ray examination and record that to a continuing patient dose file. We monitor our occupational radiation exposure for life; we will be instituting protocols to do the same for our medical radiation exposure.
Summary
Patient dose from diagnostic x-rays usually is recorded in one of the following three ways: (1) ESD, (2) mean marrow dose, or (3) gonadal dose. TLDs are the monitor of choice for patient radiation dose. By knowing the output intensity of at least one x-ray technique and the SSD, the medical physicist can estimate the ESE for any patient examination. For fluoroscopic examination, a good general assumption for the ESD is 40 mGyt/min.
Patient radiation dose can be reduced easily by eliminating unnecessary examinations and repeat examinations, and by ensuring proper radiographic technique and patient positioning. The radiobiology of pregnancy requires particular attention to the pregnant patient. By posting the waiting room and the examination room with educational signs, we meet our responsibility to the pregnant patient.
1. Define or otherwise identify the following:
2. What is the embryo’s response to irradiation above 250 mGyt during the first 2 weeks after conception?
3. During the fetal period of major organogenesis, what radiation responses are possible?
4. What procedure should be followed if a patient is examined and subsequently discovers that she is pregnant?
5. List five procedures that could result in a measurable fetal dose.
6. How can the three cardinal principles of radiation protection best be applied in diagnostic radiology?
7. What estimate of patient radiation dose usually is measured and reported?
8. How does one use a radiation nomogram?
9. Estimate the entrance skin dose for a PA chest image conducted at 110 kVp/2 mAs.
10. What factors are required to estimate the genetically significant dose?
11. What radiation dose description is most important for x-ray mammography?
12. How do x-ray beam width and beam penumbra affect patient dose during CT?
13. How does the term “dose distribution” affect specification of patient radiation dose in x-ray imaging?
14. Describe how patient radiation dose during multislice CT compares with that during step-and-shoot CT.
15. Name three screening x-ray examinations that should not be performed regularly.
16. Estimate the fetal dose after an AP abdominal image is conducted at 76 kVp/40 mAs.
17. What does the symbol Σ mean?
18. Approximately what percentage of the ESD is Dg for mammography?
19. What is the approximate contribution of CT to total patient radiation dose?
20. What is the approximate fetal dose after a 3.5-min barium enema fluoroscopic examination?
The answers to the Challenge Questions can be found by logging on to our website at http://evolve.elsevier.com.