14 PARTICULAR PAEDIATRIC POINTS
Children are not—medically—simply little adults.
Some pathological processes are shared by children and adults—the CXR patterns are often identical or similar. In this chapter we will concentrate on aspects of chest radiology that are different on a child’s CXR.
Normal anatomy
The thymus
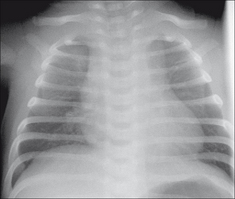
Figure 14.1 33 weeks gestation. One day old. Mediastinum widened to the right and to the left by a normal thymus.
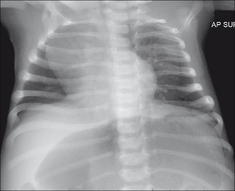
Figure 14.2 Four weeks old. Lordotic AP projection. The rounded shadow projected over the right upper zone is a normal thymus.
The heart1,2
 Two rules of thumb: CXR evidence of cardiac enlargement.
Two rules of thumb: CXR evidence of cardiac enlargement.
 On a child’s PA radiograph the normal CTR can be slightly above 50%, though by the second year it rarely exceeds 50%1 (Fig. 14.5).
On a child’s PA radiograph the normal CTR can be slightly above 50%, though by the second year it rarely exceeds 50%1 (Fig. 14.5).ABNORMAL CXRS—CHILD: ADULT
SIMILAR CXR PATTERNS
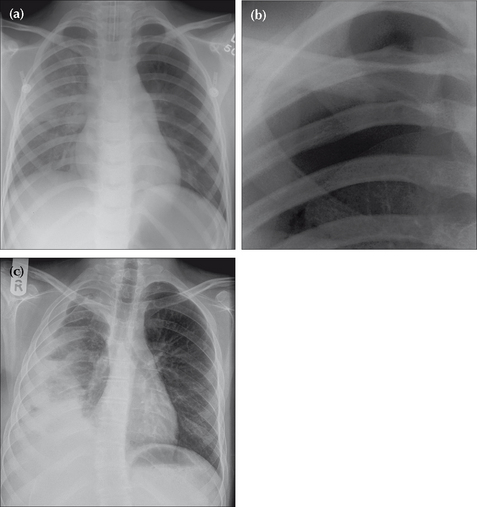
Several conditions that affect both children and adults show similar CXR features. For example: lobar collapse (pp. 52–66), pleural effusion (pp. 82–88), pneumothorax (pp. 96–104). See Figs 14.7-14.9.
Primary tuberculosis (PTB)
The CXR appearances are similar to those occurring in an adult with PTB. The possible CXR findings are described on pp. 134–136 but are worth repeating here:
CXR PATTERNS SPECIFIC TO CHILDREN
Bronchiolitis3-5
Infection occurring in children up to two years of age and caused by the respiratory syncytial virus. The inflammation mainly affects the bronchioles. These are narrowed by the inflammatory exudate and the narrowing causes air trapping (i.e. persistent distension) on expiration.
The CXR features of viral infection are not always recognised by those who have only episodic involvement with the CXRs of young children. Note:
 Bronchiolitis typically shows:
Bronchiolitis typically shows:
 Peribronchial cuffing (i.e. bronchial wall thickening) beyond the inner one third of the lung (Fig. 14.10).
Peribronchial cuffing (i.e. bronchial wall thickening) beyond the inner one third of the lung (Fig. 14.10). Small areas of linear collapse/peripheral atelectasis. These small shadows may change in position on subsequent CXRs4.
Small areas of linear collapse/peripheral atelectasis. These small shadows may change in position on subsequent CXRs4. A small or poor inspiration in an infant (i.e. without bronchiolitis) often produces hazy peri-hilar shadows that can be misinterpreted as inflammatory change. In reality this appearance strongly suggests normality.
A small or poor inspiration in an infant (i.e. without bronchiolitis) often produces hazy peri-hilar shadows that can be misinterpreted as inflammatory change. In reality this appearance strongly suggests normality.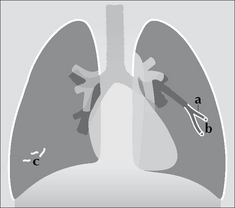
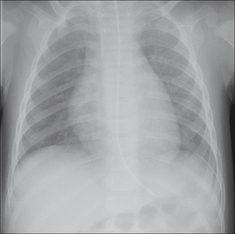
Figure 14.10 Bronchiolitis. CXR features: (a) inflammation causes narrowing of the bronchioles and air trapping; (b) thickened bronchioles seen end-on will occasionally appear as small ring like densities (i.e. peri-bronchial cuffing); (c) small areas of linear collapse.
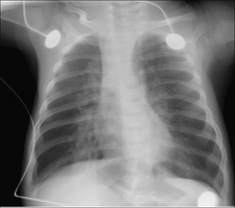
Figure 14.11 Three months old. Bronchiolitis. Note that the domes of the diaphragm are low due to the air trapping. Some streaky peri-hilar densities are also present; they represent inflammation of the bronchial walls and adjacent interstitium5.
Rule of thumb: If the CXR shows poor expansion of the lungs, i.e. they are not over-inflated…this suggests that the infant does not have bronchiolitis.
Bacterial pneumonia1,3,6,7
Usually the CXR pattern will be identical to lobar pneumonia or broncho-pneumonia (p. 44) as they appear on an adult’s CXR. Two additional specific features are worth noting:
 Lymphadenopathy. Obvious hilar lymph node enlargement is fairly common. This contrasts with adults in whom a simple pneumonia rarely causes a lymphadenopathy that is detectable on a CXR.
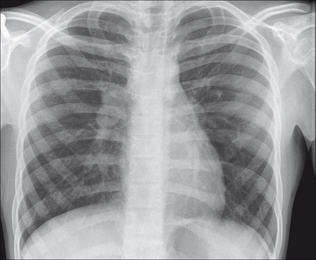
Lymphadenopathy. Obvious hilar lymph node enlargement is fairly common. This contrasts with adults in whom a simple pneumonia rarely causes a lymphadenopathy that is detectable on a CXR. Round pneumonia (pseudotumour). Sometimes pneumonic consolidation will appear as a rounded density simulating a lung mass. This rounded appearance does occur in adults—but it is much less common. It has been suggested that the round configuration is due to a gravitational effect in a child who sleeps in the supine position. Others offer a different explanation: an infant’s system of collateral ventilation is relatively underdeveloped (i.e. few pores of Kohn and canals of Lambert). Inflammatory exudates accumulating in the alveoli cannot use these pathways to diffuse to adjacent alveoli as they would in an adult. Consequently, the exudate adopts the form of a sphere—the so-called round, or rounded, pneumonia. The importance of a round pneumonia appearance is that it can be misread as a primary or secondary tumour3,6.
Round pneumonia (pseudotumour). Sometimes pneumonic consolidation will appear as a rounded density simulating a lung mass. This rounded appearance does occur in adults—but it is much less common. It has been suggested that the round configuration is due to a gravitational effect in a child who sleeps in the supine position. Others offer a different explanation: an infant’s system of collateral ventilation is relatively underdeveloped (i.e. few pores of Kohn and canals of Lambert). Inflammatory exudates accumulating in the alveoli cannot use these pathways to diffuse to adjacent alveoli as they would in an adult. Consequently, the exudate adopts the form of a sphere—the so-called round, or rounded, pneumonia. The importance of a round pneumonia appearance is that it can be misread as a primary or secondary tumour3,6.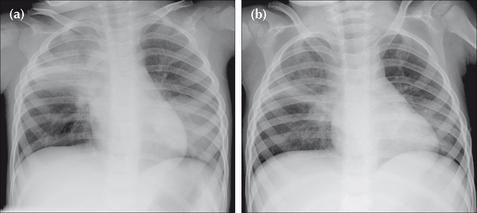
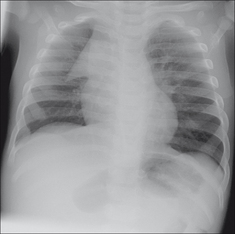
Figure 14.12 Male. Two years old. Cough and fever. CXR (a) shows right upper lobe consolidation (pneumonia). A large round opacity in the left lower zone mimics a tumour. Following antibiotic treatment CXR (b) was obtained one week later. Both areas of shadowing have almost cleared. The spherical shadow represented a round pneumonia.
SPECIFIC CLINICAL PROBLEMS
There are three common clinical scenarios in which the CXR may—or may not—play an important role: asthma; possible inhaled foreign body; and swallowed foreign body.
Wheezing—is it asthma?7-9
 The child with an established diagnosis of asthma does not require a routine CXR when an acute exacerbation occurs. However, if there is clinical deterioration then a CXR is indicated in order to exclude a complication (pneumothorax, pneumonia or lobar collapse).
The child with an established diagnosis of asthma does not require a routine CXR when an acute exacerbation occurs. However, if there is clinical deterioration then a CXR is indicated in order to exclude a complication (pneumothorax, pneumonia or lobar collapse). Atypical CXR features should always raise the suspicion of another cause for wheezing, particularly foreign body inhalation. There is an important aphorism: beware the wheezing child too readily labelled as asthma who has a foreign body aspiration5,8-10.
Atypical CXR features should always raise the suspicion of another cause for wheezing, particularly foreign body inhalation. There is an important aphorism: beware the wheezing child too readily labelled as asthma who has a foreign body aspiration5,8-10. The lungs are over-distended when more than nine posterior ribs are visible above the domes of the diaphragm. Rule of thumb: Over-inflated lungs. Age two years and younger—likely viral infection. Older than two years—likely asthma (Table 14.1).
The lungs are over-distended when more than nine posterior ribs are visible above the domes of the diaphragm. Rule of thumb: Over-inflated lungs. Age two years and younger—likely viral infection. Older than two years—likely asthma (Table 14.1).Table 14.1 Over-distended lungs. Bronchiolitis or asthma?
| Pathology | CXR features | Note |
|---|---|---|
| Bronchiolitis | The CXR appearances may be very similar in bronchiolitis and asthma. In a child under two years old bronchiolitis is the more likely diagnosis. | |
| Asthma |
HAS A FOREIGN BODY BEEN INHALED?7-14
The most commonly inhaled foreign body is food, frequently a peanut8–12. A history of choking is usually obtained. Common clinical signs include coughing, stridor, wheezing and sternal retraction. Rapid recognition and treatment are essential. This is a medical emergency.
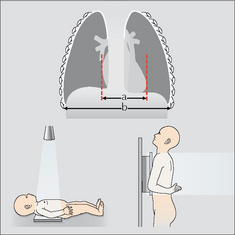
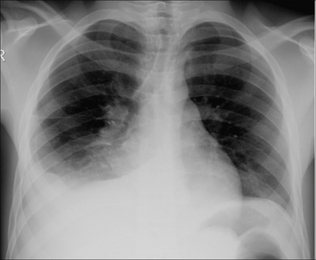
 Radiography: if the child is able to cooperate then a frontal CXR should be obtained following a rapid forced expiration. Air trapping on the affected side is then more obvious (Fig. 14.13). Alternatively, fluoroscopy and observing the movement of the domes of the diaphragm relative to each other is an excellent method of detecting whether there is unilateral air trapping.
Radiography: if the child is able to cooperate then a frontal CXR should be obtained following a rapid forced expiration. Air trapping on the affected side is then more obvious (Fig. 14.13). Alternatively, fluoroscopy and observing the movement of the domes of the diaphragm relative to each other is an excellent method of detecting whether there is unilateral air trapping. An inhaled foreign body may produce any one of three appearances5,8,9,14:
An inhaled foreign body may produce any one of three appearances5,8,9,14:
 Normal CXR. This is not necessarily reassuring. If a strong clinical suspicion persists (i.e. that a foreign body has been inhaled) then urgent referral for MRI or bronchoscopy is essential.
Normal CXR. This is not necessarily reassuring. If a strong clinical suspicion persists (i.e. that a foreign body has been inhaled) then urgent referral for MRI or bronchoscopy is essential. Air trapping because the bronchial blockage has caused a ball valve effect. The affected lung appears blacker and larger than the opposite normal side (Fig. 14.13).
Air trapping because the bronchial blockage has caused a ball valve effect. The affected lung appears blacker and larger than the opposite normal side (Fig. 14.13).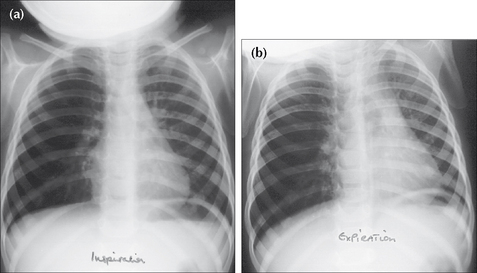
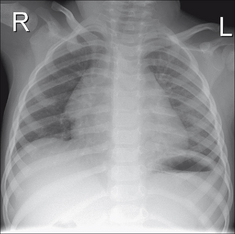
Figure 14.13 Inhaled peanut has lodged in the right main bronchus. Inspiration CXR (a): the right lung is hypertransradiant (i.e. blacker) as compared with the left lung. Following a rapid expiration, CXR (b) shows the severe air trapping in the right lung with displacement of the mediastinum to the left side. These CXR findings indicate a medical emergency.
IS THERE A FOREIGN OBJECT IN THE OESOPHAGUS?15,16
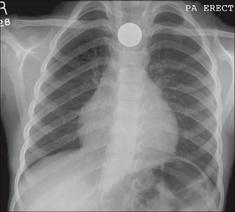
 Occasionally, a coin will lodge in the oesophagus (Figs 14.14-14.16). Some of these patients may be asymptomatic. Erosion of the mucosa by a coin can cause an abscess or mediastinitis.
Occasionally, a coin will lodge in the oesophagus (Figs 14.14-14.16). Some of these patients may be asymptomatic. Erosion of the mucosa by a coin can cause an abscess or mediastinitis. There is no danger to the child if the coin has passed into the stomach or the intestine. A radiograph of the abdomen (AXR) represents unjustified radiation exposure. Only a CXR is indicated.
There is no danger to the child if the coin has passed into the stomach or the intestine. A radiograph of the abdomen (AXR) represents unjustified radiation exposure. Only a CXR is indicated. If the CXR is normal, then the parents can be reassured that the coin has passed into the gut, will cause no harm and will be excreted within the next few days.
If the CXR is normal, then the parents can be reassured that the coin has passed into the gut, will cause no harm and will be excreted within the next few days. A caveat. Presently, coins minted in the UK are inert. In other countries this is not always the case. If a coin has a zinc core and a copper coating then gastric acid can dissolve the coating and the zinc can cause ulcers and anaemia. In countries where coins are potentially poisonous then an abdominal radiograph (if negative, to be followed by a CXR) would represent correct practice.
A caveat. Presently, coins minted in the UK are inert. In other countries this is not always the case. If a coin has a zinc core and a copper coating then gastric acid can dissolve the coating and the zinc can cause ulcers and anaemia. In countries where coins are potentially poisonous then an abdominal radiograph (if negative, to be followed by a CXR) would represent correct practice.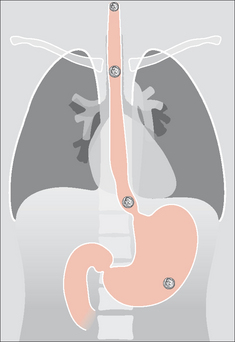
Figure 14.14 Swallowed foreign bodies. A coin may impact in the oesophagus. Impaction usually occurs at one of three sites: in the cervical oesophagus, at the level of the arch of the aorta, or at the gastro-oesophageal junction. Once a coin passes into the stomach it invariably travels uneventfully through, and out of, the gastro-intestinal tract.
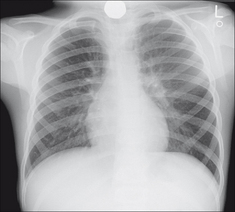
Figure 14.15 Five years old. A coin has impacted in the cervical oesophagus. The neck must always be included on a child’s CXR when a swallowed foreign body is a clinical possibility.
AN INTERESTING CONDITION—CONGENITAL LOBAR EMPHYSEMA5,7,17
Aetiology/pathology
Most cases are thought to result from a bronchial obstruction affecting a lobe of the lung. Occasionally a structural occlusion (e.g. bronchial atresia) has been demonstrated. Usually one lobe alone is affected—invariably an upper lobe. Occasionally (less than 10%) two lobes are involved. Air enters the lobe via the canals of Lambert and pores of Kohn (collateral air drift) but cannot exit. Consequently the lobe gradually becomes very distended and it balloons to many times its normal size.
Clinical features
A few children present in the neonatal period. More commonly, symptoms occur between one and six months of age. Dyspnoea and cyanosis are the main features.
The CXR
 Invariably an upper lobe (usually the left) is distended and hyperlucent. Adjacent lobes are compressed. Extreme distension will displace the mediastinum to the opposite side.
Invariably an upper lobe (usually the left) is distended and hyperlucent. Adjacent lobes are compressed. Extreme distension will displace the mediastinum to the opposite side.AN INTERESTING CONDITION—CYSTIC FIBROSIS1,7,18,19
Aetiology/pathology
Autosomal recessive. 1:1500 live births. An abnormality in chloride ion transport which results in viscid mucus production. Poor clearing of the mucus from the airway predisposes to chest infection, bronchiectasis, and other sequelae of chronic lung infection. Age of presentation in childhood is variable.
Clinical features
Recurrent pulmonary infections. Other organ involvement may suggest the diagnosis (e.g. involvement of pancreas, liver—biliary cirrhosis, paranasal sinuses).
1. Carty H, Shaw D, Brunelle F, Kendall B. Imaging Children. Edinburgh: Churchill Livingstone, 1994.
2. Jefferson K, Rees S. Clinical Cardiac Radiology, 2nd ed. London: Butterworths, 1980.
3. Branson RT, Griscom NT, Cleveland RH. Interpretation of chest radiographs in infants with cough and fever. Radiology. 2005;236:22-29.
4. Griscom NT, Wohl MEB, Kirkpatrick JA. Lower respiratory infections: how infants differ from adults. Radiol Clin North Am. 1978;16:367-387.
5. Rencken I, Patton WL, Brasch RC. Airway obstruction in pediatric patients. Radiol Clin North Am. 1998;36:175-187.
6. Rose RW, Ward BH. Spherical pneumonias in children simulating pulmonary and mediastinal masses. Radiology. 1973;106:179-182.
7. Newman B, Oh KS. Abnormal pulmonary aeration in infants and children. Radiol Clin North Am. 1988;26:323-339.
8. Lloyd-Thomas AR, Bush GH. All that wheezes is not asthma. Anaesthesia. 1986;41:181-185.
9. Roback MG, Dreitlein DA. Chest radiograph in the evaluation of first time wheezing episodes: review of current clinical practice and efficacy. Pediatr Emerg Care. 1998;14:181-184.
10. Breysem L, Loyen S, Boets A, et al. Pediatric emergencies: thoracic emergencies. Eur J Radiol. 2002;12:2849-2865.
11. Baharloo F, Veyckemans F, Francis C, et al. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999;115:1357-1362.
12. Metrangolo S, Monetti C, Meneghini L, et al. Eight years experience with foreign body aspiration in children: what is really important for a timely diagnosis? J Pediatr Surg. 1999;34:1229-1231.
13. Silva AB, Muntz HR, Clary R. Utility of conventional radiography in the diagnosis and management of pediatric airway foreign bodies. Ann Otol Rhinol Laryngol. 1998;107:834-838.
14. Svedstrom E, Puhakka H, Kero P. How accurate is chest radiography in the diagnosis of tracheobronchial foreign bodies in children? Pediatr Radiol. 1989;19:520-522.
15. Macpherson RI, Hill JG, Othersen HB, et al. Esophageal Foreign Bodies in Children: Diagnosis, Treatment, and Complications. AJR. 1996;166:919-924.
16. Raby N, Berman L, de Lacey G. Accident and Emergency Radiology: A Survival Guide, 2nd ed. Philadelphia, PA: Elsevier Saunders, 2005.
17. Panicek DM, Heitzman ER, Randall PA, et al. The Continuum of pulmonary developmental anomalies. Radiographics. 1987;7:747-772.
18. Wood BP. Cystic fibrosis. Radiology. 1997;204:1-10.
19. Robinson TE. Imaging of the chest in cystic fibrosis. Clin Chest Med. 2007;28:405-421.