Chapter 174 Staphylococcus
Staphylococci are hardy, aerobic, gram-positive bacteria that grow in pairs and clusters and are ubiquitous as normal flora of humans and present on fomites and in dust. They are resistant to heat and drying and may be recovered from nonbiologic environments weeks to months after contamination. Strains are classified as Staphylococcus aureus if they are coagulase positive or as 1 of the many species of coagulase-negative staphylococci (e.g., Staphylococcus epidermidis, Staphylococcus saprophyticus, Staphylococcus haemolyticus, etc). Often, S. aureus produces a yellow or orange pigment and β-hemolysis on blood agar and S. epidermidis produces a white pigment with variable hemolysis results, although definitive species confirmation requires further testing. S. aureus has many virulence factors that mediate various serious diseases, whereas coagulase-negative staphylococci tend to be less pathogenic unless an indwelling foreign body (e.g., intravascular catheter) is present. Emerging antimicrobial resistance has become important, especially to the β-lactam antibiotics and less often to vancomycin.
174.1 Staphylococcus aureus
S. aureus is the most common cause of pyogenic infection of the skin and soft tissue, causing impetigo, furuncles (boils), cellulitis, abscess, lymphadenitis, paronychia, omphalitis, and wound infection. Bacteremia (primary and secondary) is common and can be associated with or result in osteomyelitis, suppurative arthritis, deep abscesses, pneumonia, empyema, endocarditis, pyomyositis, pericarditis, and rarely meningitis. Toxin-mediated diseases, including food poisoning, staphylococcal scarlet fever, scalded skin syndrome, and toxic shock syndrome (TSS), are caused by certain S. aureus strains. Methicillin resistance is a global problem.
Etiology
Disease may result from tissue invasion or injury caused by various toxins and enzymes produced by the organism. Strains of S. aureus can be identified by the virulence factors they produce and can be classified by various molecular techniques.
Adhesion of S. aureus to mucosal cells is mediated by teichoic acid in the cell wall; exposure to the submucosa or subcutaneous sites increases adhesion to fibrinogen, fibronectin, collagen, and other proteins. Different strains of S. aureus produce many different virulence factors that have 1 or more of 4 different roles: protect the organism from host defenses, localize infection, cause local tissue damage, and act as toxins affecting noninfected tissue sites.
Most strains of S. aureus possess factors that protect the organism from host defenses. Many staphylococci produce a loose polysaccharide capsule, or slime layer, which may interfere with opsonophagocytosis. Production of coagulase and/or clumping factor differentiates S. aureus from S. epidermidis and other coagulase-negative staphylococci. Clumping factor interacts with fibrinogen to cause large clumps of organisms, interfering with effective phagocytosis. Coagulase causes plasma to clot by interacting with fibrinogen and this may have an important role in localization of infection (abscess formation). Protein A is present in most strains of S. aureus but not coagulase-negative staphylococci and reacts specifically with immunoglobulin G1 (IgG1), IgG2, and IgG4. It is located on the outermost coat of the cell wall and can absorb serum immunoglobulins, preventing antibacterial antibodies from acting as opsonins and thus inhibiting phagocytosis. Other enzymes elaborated by staphylococci include catalase (inactivates hydrogen peroxide, promoting intracellular survival), penicillinase or β-lactamase (inactivates penicillin at the molecular level), and lipase (associated with skin infection).
Many strains of S. aureus produce substances that cause local tissue destruction. A number of immunologically distinct hemolysins that act on cell membranes and cause tissue necrosis have been identified (α-toxin, β-hemolysin, δ-hemolysin). Panton-Valentine leukocidin (PVL), which is produced by many current strains of S. aureus and has been associated with invasive skin disease, combines with the phospholipid of the phagocytic cell membrane, producing increased permeability, leakage of protein, and eventual death of the cell.
Many strains of S. aureus release 1 or more exotoxins. Exfoliatins A and B are serologically distinct proteins that produce localized (bullous impetigo) or generalized (scalded skin syndrome, staphylococcal scarlet fever) dermatologic complications (Chapter 651). Exfoliatins produce skin separation by splitting the desmosome and altering the intracellular matrix in the stratum granulosum.
One or more staphylococcal enterotoxins (types A, B, C1, C2, D, E) are elaborated by most strains of S. aureus. Ingestion of preformed enterotoxin A or B is associated with food poisoning, resulting in vomiting and diarrhea and, in some cases, profound hypotension. By 10 yr of age, almost all individuals have antibodies to at least 1 enterotoxin.
Toxic shock syndrome toxin-1 (TSST-1) is associated with TSS related to menstruation and focal staphylococcal infection. TSST-1 is a superantigen that induces production of interleukin-1 and tumor necrosis factor, resulting in hypotension, fever, and multisystem involvement. Enterotoxin A and enterotoxin B also may be associated with nonmenstrual TSS.
Epidemiology
Many neonates are colonized within the 1st wk of life, and 20-40% of normal individuals carry at least 1 strain of S. aureus in the anterior nares at any given time.
The organisms may be transmitted from the nose to the skin, where colonization seems to be more transient. Persistent umbilical, vaginal, and perianal carriage may occur.
Heavily colonized nasal carriers (often aggravated by a viral upper respiratory tract infection) are particularly effective disseminators. Exposure to S. aureus generally occurs by auto-inoculation or direct contact with the hands of other colonized individuals. Handwashing between patient contacts is essential to decrease the nosocomial spread of staphylococci. Spread via fomites is rare.
Invasive disease may follow colonization. Antibiotic therapy with a drug to which S. aureus is resistant favors colonization and the development of infection. Other factors that increase the likelihood of infection include wounds, skin disease, ventriculoperitoneal shunts, intravenous or intrathecal catheterization, corticosteroid treatment, malnutrition, and azotemia. Viral infections of the respiratory tract, especially influenza virus, may predispose to secondary bacterial infection with staphylococci.
Pathogenesis
The development of staphylococcal disease is related to resistance of the host to infection and to virulence of the organism (Fig. 174-1). The intact skin and mucous membranes serve as barriers to invasion by staphylococci. Defects in the mucocutaneous barriers produced by trauma, surgery, foreign surfaces (sutures, shunts, intravascular catheters), and burns increase the risk for infection.
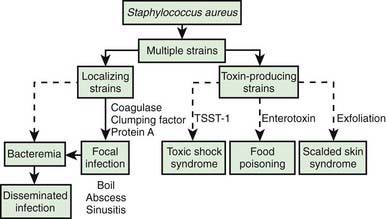
Figure 174-1 Relationship of virulence factors and diseases associated with Staphylococcus aureus. TSST-1, toxic shock syndrome toxin-1.
Infants may acquire type-specific humoral immunity to staphylococci transplacentally. Older children and adults develop antibodies to staphylococci as a result of colonization or minor infections. Antibody to the various S. aureus toxins appears to protect against those specific toxin-mediated diseases, but humoral immunity does not necessarily protect against focal or disseminated S. aureus infection with the same organisms.
Congenital defects in chemotaxis (Job syndrome, Chédiak-Higashi syndrome, Wiskott-Aldrich syndrome) and defective phagocytosis and killing (neutropenia, chronic granulomatous disease) increase the risk for staphylococcal infections. Patients with HIV infection have neutrophils that are defective in their ability to kill S. aureus in vitro. Patients with recurrent staphylococcal infection should be evaluated for immune defects, especially those involving neutrophil dysfunction.
Clinical Manifestations
The signs and symptoms vary with the location of the infection, which is most commonly the skin but may be any tissue. Disease states of various degrees of severity are generally a result of local suppuration, systemic dissemination with metastatic infection, or systemic effects of toxin production. Although the nasopharynx and skin of many persons may be colonized with S. aureus, disease due to this organism is relatively uncommon. Skin infections due to S. aureus are considerably more prevalent among persons living in low socioeconomic circumstances and particularly among those in tropical climates.
Skin
S. aureus is an important cause of pyogenic skin infections, including impetigo contagiosa, ecthyma, bullous impetigo, folliculitis, hydradenitis, furuncles, carbuncles, staphylococcal scalded skin syndrome, and staphylococcal scarlet fever. Infection may also complicate wounds or occur as superinfection of other noninfectious skin disease (eczema). Recurrent furunculosis is associated with repeated episodes of pyoderma over months to years. Recurrent skin and soft tissue infections are commonly noted with community-associated methicillin-resistant S. aureus (MRSA) and often affect the lower extremities and buttocks. S. aureus is also an important cause of wound infections and can cause deep soft tissue involvement, including cellulitis and rarely necrotizing fasciitis.
Respiratory Tract
Infections of the upper respiratory tract due to S. aureus are rare, in particular considering the frequency with which the anterior nares are colonized. In normal hosts, otitis media (Chapter 632) and sinusitis (Chapter 372) are rarely caused by S. aureus. S. aureus sinusitis is relatively common in children with cystic fibrosis or defects in leukocyte function and may be the only focus of infection in some children with toxic shock syndrome. Suppurative parotitis is a rare infection, but S. aureus is a common cause. A membranous tracheitis that complicates viral croup may be due to infection with S. aureus, but other organisms are also possible. Patients typically have high fever, leukocytosis, and evidence of severe upper airway obstruction. Direct laryngoscopy or bronchoscopy shows a normal epiglottis with subglottic narrowing and thick, purulent secretions within the trachea. Treatment requires careful airway management and appropriate antibiotic therapy.
Pneumonia (Chapter 392) due to S. aureus may be primary (hematogenous) or secondary after a viral infection such as influenza. Hematogenous pneumonia may be secondary to septic emboli from right-sided endocarditis or septic thrombophlebitis, with or without the presence of intravascular devices. Inhalation pneumonia is caused by alteration of mucociliary clearance (see cystic fibrosis, Chapter 395), leukocyte dysfunction, or bacterial adherence initiated by a viral infection. Common symptoms and signs include high fever, abdominal pain, tachypnea, dyspnea, and localized or diffuse bronchopneumonia or lobar disease. S. aureus often causes a necrotizing pneumonitis that may be associated with development of empyema, pneumatoceles, pyopneumothorax, and bronchopleural fistulas.
Sepsis
S. aureus bacteremia and sepsis may be primary or associated with any localized infection. The onset may be acute and marked by nausea, vomiting, myalgia, fever, and chills. Organisms may localize subsequently at any site (usually a single deep focus) but are found especially in the heart valves, lungs, joints, bones, and abscesses.
In some instances, especially in young adolescent males, disseminated S. aureus disease occurs, characterized by fever, persistent bacteremia despite antibiotics, and focal involvement of 2 or more separate tissue sites (skin, bone, joint, kidney, lung, liver, heart).
In these cases, endocarditis and septic thrombophlebitis must be ruled out.
Muscle
Localized staphylococcal abscesses in muscle associated with elevation of muscle enzymes sometimes without septicemia have been called pyomyositis. This disorder has been reported most frequently from tropical areas but also occurs in the USA in otherwise healthy children. Multiple abscesses occur in 30-40% of cases. History may include prior trauma at the site of the abscess. Surgical drainage and appropriate antibiotic therapy are essential.
Bones and Joints
S. aureus is the most common cause of osteomyelitis and suppurative arthritis in children (Chapters 676 and 677).
Central Nervous System
Meningitis (Chapter 595.1) caused by S. aureus is not common; it is associated with penetrating cranial trauma and neurosurgical procedures (craniotomy, cerebrospinal fluid [CSF] shunt placement) and less frequently with endocarditis, parameningeal foci (epidural or brain abscess), diabetes mellitus, or malignancy. The CSF profile of S. aureus meningitis is indistinguishable from that in other forms of bacterial meningitis.
Heart
S. aureus is a common cause of acute endocarditis (Chapter 431) on native valves. Perforation of heart valves, myocardial abscesses, heart failure, conduction disturbances, acute hemopericardium, purulent pericarditis, and sudden death may ensue.
Kidney
S. aureus is a common cause of renal and perinephric abscess (Chapter 532), usually of hematogenous origin. Pyelonephritis and cystitis due to S. aureus are unusual.
Toxic Shock Syndrome (TSS)
S. aureus is the principal cause of TSS (Chapter 174.2), which should be suspected in anyone with fever, shock, and/or a scarlet fever-like rash.
Intestinal Tract
Staphylococcal enterocolitis rarely follows overgrowth of normal bowel flora by S. aureus, which can occur as a result of broad-spectrum oral antibiotic therapy. Diarrhea is associated with blood and mucus. Peritonitis associated with S. aureus in patients receiving long-term ambulatory peritoneal dialysis usually involves the catheter tunnel. Removal of the catheter is required to achieve a bacteriologic cure.
Food poisoning (Chapter 332) may be caused by ingestion of preformed enterotoxins produced by staphylococci in contaminated foods. Approximately 2-7 hr after ingestion of the toxin, sudden, severe vomiting begins. Watery diarrhea may develop, but fever is absent or low. Symptoms rarely persist longer than 12-24 hr. Rarely, shock and death may occur.
Diagnosis
The diagnosis of S. aureus infection depends on isolation of the organism from nonpermissive sites such as cellulitis aspirates, abscess cavities, blood, bone or joint aspirates, or other sites of infection. Swab cultures of surfaces are not as useful, as they may reflect surface contamination rather than the true cause of infection. Tissue samples or fluid aspirates in a syringe provide the best culture material. Isolation from the nose or skin does not necessarily imply causation because these sites may be normally colonized sites. Because of the high prevalence of MRSA, the increasing severity of S. aureus infections, and the fact that bacteremia is not universally present even in severe S. aureus infections, it is usually important to obtain a nonpermissive culture of any potential focus of infection as well as a blood culture prior to starting antibiotic treatment. The organism can be grown readily in liquid and on solid media. After isolation, identification is made on the basis of Gram stain and coagulase, clumping factor, and protein A reactivity. Patterns of susceptibility to antibiotics should be assessed in serious cases, as antimicrobial resistance is increasingly common.
Diagnosis of S. aureus food poisoning is made on the basis of epidemiologic and clinical findings. Food suspected of contamination should be cultured and can be tested for enterotoxin.
Differential Diagnosis
Skin lesions due to S. aureus may be indistinguishable from those due to group A streptococci; the former usually expand slowly, while the latter are more prone to spread rapidly. S. aureus pneumonia can be suspected on the basis of chest roentgenograms that reveal pneumatoceles, pyopneumothorax, or lung abscess (Fig. 174-2). Fluctuant skin and soft tissue lesions also can be caused by other organisms, including Mycobacterium tuberculosis, atypical mycobacteria, Bartonella henselae (cat-scratch disease), Francisella tularensis, and various fungi, among others.
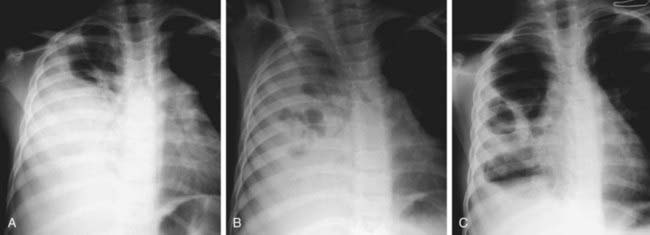
Figure 174-2 Pneumatocele formation. A, A 5 yr old child with Staphylococcus aureus pneumonia initially demonstrated consolidation of the right middle and lower zones. B, Seven days later, multiple lucent areas are noted as pneumatoceles develop. C, Two wk later, significant resolution is evident, with a rather thick-walled pneumatocele persisting in the right midzone associated with significant residual pleural thickening.
(From Kuhn JP, Slovis TL, Haller JO: Caffey’s pediatric diagnostic imaging, vol 1, ed 10, Philadelphia, 2004, Mosby, pp 1003–1004.)
Treatment
Antibiotic therapy alone is rarely effective in individuals with undrained abscesses or with infected foreign bodies. Loculated collections of purulent material should be relieved by incision and drainage. Foreign bodies should be removed, if possible. Therapy always should be initiated with an antibiotic consistent with the local staphylococcal susceptibility patterns as well as the severity of infection. Penicillin and amoxicillin are not appropriate, because more than 90% of all staphylococci isolated, regardless of source, are resistant to these agents. For serious infections, parenteral treatment is indicated, at least at the outset, until symptoms are controlled. Serious S. aureus infections, with or without abscesses, tend to persist and recur, necessitating prolonged therapy.
The antibiotic used as well as the dose, route, and duration of treatment depend on the site of infection, the response of the patient to treatment, and the susceptibility of the organisms recovered from blood or from local sites of infection. For most patients with serious S. aureus infection, intravenous treatment is recommended until the patient has become afebrile and other signs of infection have improved. Oral therapy is often continued for a period of time, especially in patients with chronic infection or underlying host defense problems. Treatment of S. aureus osteomyelitis (Chapter 676), meningitis (Chapter 595.1), and endocarditis (Chapter 431) are discussed in their respective chapters.
Initial treatment for serious infections thought to be due to methicillin-susceptible S. aureus (MSSA) should include semisynthetic penicillin (e.g., nafcillin, oxacillin) or less often a 1st generation cephalosporin (e.g., cefazolin). MRSA is both an important hospital and community-acquired pathogen. Community-associated MRSA infections are common throughout the USA, even in children without pre-existing risk factors. Resistance to semisynthetic penicillins and cephalosporins is related to a novel penicillin-binding protein (PB2A) that is relatively insensitive to antibiotics containing a β-lactam ring. MRSA strains appear to be at least as virulent as their methicillin-sensitive counterparts. Vancomycin (40-60 mg/kg/24 hr divided every 6 hr IV) can be used as the initial treatment for penicillin-allergic individuals and those with suspected serious S. aureus infections that might be due to MRSA. Serum levels of vancomycin should be monitored, with trough concentrations of 10-20 µg/mL, depending on the case. MRSA is also resistant to cephalosporins and carbapenems and is unreliably susceptible to the quinolones. Linezolid, daptomycin, quinupristin-dalfopristin, vancomycin with linezolid and gentamicin, and vancomycin with trimethoprim-sulfamethoxazole may be useful for serious S. aureus infections highly resistant to other antibiotics (Table 174-1).
Table 174-1 PARENTERAL ANTIMICROBIAL AGENT(S) FOR TREATMENT OF BACTEREMIA AND OTHER SERIOUS STAPHYLOCOCCUS AUREUS INFECTIONS
| SUSCEPTIBILITY | ANTIMICROBIAL AGENTS | COMMENTS |
|---|---|---|
| I. INITIAL EMPIRIC THERAPY (ORGANISM OF UNKNOWN SUSCEPTIBILITY) | ||
| Drugs of choice: | Vancomycin ± gentamicin or rifampin | For life-threatening infections (i.e., septicemia, endocarditis, CNS infection); linezolid could be substituted if the patient has received several recent courses of vancomycin |
| Nafcillin or oxacillin* | For non–life-threatening infection without signs of sepsis (e.g., skin infection, cellulitis, osteomyelitis, pyarthrosis) when rates of MRSA colonization and infection in the community are low | |
| Clindamycin | For non–life-threatening infection without signs of sepsis when rates of MRSA colonization and infection in the community are substantial and prevalence of clindamycin resistance is low | |
| Vancomycin | For non–life-threatening, hospital-acquired infections | |
| II. METHICILLIN-SUSCEPTIBLE, PENICILLIN-RESISTANT S. AUREUS (MSSA) | ||
| Drugs of choice: | Nafcillin or oxacillin*,† | |
| Alternatives (depending on susceptibility results): | Cefazolin* | |
| Clindamycin | ||
| Vancomycin | Only for penicillin- and cephalosporin-allergic patients | |
| Ampicillin + sulbactam | ||
| III. MRSA | ||
| A. Health Care–Associated (Multidrug-Resistant) | ||
| Drugs of choice: | Vancomycin ± gentamicin or ± rifampin† | |
| Alternatives: susceptibility testing results available before alternative drugs are used | ||
| Trimethoprim-sulfamethoxazole | ||
| Linezolid‡ | ||
| Quinupristin-dalfopristin‡ | ||
| Fluoroquinolones | Not recommended for people younger than 18 yr of age or as monotherapy | |
| B. Community (Not Multidrug-Resistant) | ||
| Drugs of choice: | Vancomycin† | For life-threatening infections |
| Vancomycin ± gentamicin (or ± rifampin†) | For pneumonia, septic arthritis, osteomyelitis, skin or soft tissue infections | |
| For skin or soft tissue infections | ||
| Alternatives: | Clindamycin (if strain susceptible by “D test) | |
| Trimethoprim-sulfamethoxazole | ||
| IV. VANCOMYCIN INTERMEDIATELY SUSCEPTIBLE OR VANCOMYCIN-RESISTANT S. AUREUS† | ||
| Drugs of choice: | Optimal therapy is not known | Dependent on in vitro susceptibility test results |
| Linezolid‡ | ||
| Daptomycin§ | ||
| Quinupristin-dalfopristin‡ | ||
| Alternatives: | Vancomycin + linezolid ± gentamicin | |
| Vancomycin + trimethoprim-sulfamethoxazole† | ||
CNS, central nervous system; MRSA, methicillin-resistant S. aureus.
* Penicillin- and cephalosporin-allergic patients should receive vancomycin as initial therapy for serious infections.
† One of the adjunctive agents, gentamicin or rifampin, should be added to the therapeutic regimen for life-threatening infections such as endocarditis or CNS infection or infections with a vancomycin-intermediate or vancomycin-resistant S. aureus strain. Consultation with an infectious diseases specialist should be considered to determine which agent to use and duration of use.
‡ Linezolid and quinupristin-dalfopristin are 2 agents with activity in vitro and efficacy in adults with multidrug-resistant, gram-positive organisms, including S. aureus. Because experience with these agents in children is limited, consultation with an infectious diseases specialist should be considered before use.
§ Daptomycin is active in vitro against multidrug-resistant, gram-positive organisms, including S. aureus, but has not been used often in children. Daptomycin is approved by the U.S. Food and Drug Administration only for the treatment of complicated skin and skin structure infections in patients 18 yr of age and older.
From the American Academy of Pediatrics: Red book: 2009 report of the Committee on Infectious Diseases, ed 28, Elk Grove Village, IL, 2009, American Academy of Pediatrics, pp 610–611.
Rare vancomycin intermediate and vancomycin-resistant strains have also been reported, mostly in patients being treated with vancomycin, emphasizing the need for restricting the prescription of unnecessary antibiotics and the importance of isolation of the causative organism and susceptibility testing in serious infections.
Serious S. aureus infections (septicemia, endocarditis, central nervous system infections, TSS) should be treated initially with intravenous vancomycin or methicillin, nafcillin, or oxacillin depending on the local staphylococcal resistance pattern until the causative organism is isolated and its susceptibility determined. Rifampin or gentamicin may be added for synergy in serious infections (endocarditis).
In many of these infections, oral antimicrobials may be substituted to complete the course of treatment after an initial period of parenteral therapy and determination of antimicrobial susceptibilities. Despite in vitro susceptibility of S. aureus to ciprofloxacin and other quinolone antibiotics, these agents should not be used in serious staphylococcal infections, because their use has been associated with rapid development of resistance. Trimethoprim-sulfamethoxazole may be an effective oral antibiotic for many strains of both methicillin-susceptible S. aureus (MSSA) and MRSA.
Dicloxacillin (50-100 mg/kg/24 hr divided 4 times per day PO) and cephalexin (25-100 mg/kg/24 hr divided 3 to 4 times per day PO) are absorbed well orally and are effective for MSSA. Amoxicillin-clavulanate (40-80 mg amoxicillin/kg/24 hr divided 3 times per day PO) is also effective. Clindamycin (30-40 mg/kg/24 hr divided 3 to 4 times per day PO) has proved effective for the treatment of skin, soft tissue, bone, and joint infections due to susceptible S. aureus strains confirmed by a clinical microbiology laboratory using the “D-test.” Clindamycin is bacteriostatic and should not be used to treat endocarditis, brain abscess, or meningitis due to S. aureus. Given that the mechanism of action of clindamycin involves inhibition or protein synthesis, many experts use clindamycin to treat S. aureus toxin–mediated illnesses (TSS) to inhibit toxin production. The duration of oral therapy depends on the response as determined by the clinical response and roentgenographic and laboratory findings.
Skin and soft tissue infection and respiratory tract infection may often be managed by oral therapy or by an initial brief course of parenteral antibiotics followed by oral medication. Ceftaroline (IV) is approved for MRSA skin infections in adults.
Prognosis
Untreated S. aureus septicemia is associated with a high fatality rate, which have been reduced significantly by appropriate antibiotic treatment. S. aureus pneumonia can be fatal at any age but is more likely to be associated with high morbidity and mortality in young infants or in patients whose therapy has been delayed. Prognosis also may be influenced by numerous host factors, including nutrition, immunologic competence, and the presence or absence of other debilitating diseases. In most cases with abscess formation, surgical drainage is necessary.
Prevention
S. aureus infection is transmitted primarily by direct contact. Strict attention to handwashing techniques is the most effective measure for preventing the spread of staphylococci from one individual to another (Chapter 166). Use of a hand wash containing chlorhexidine or alcohol is recommended. In hospitals or other institutional settings, all persons with acute S. aureus infections should be isolated until they have been treated adequately. There should be constant surveillance for nosocomial S. aureus infections within hospitals. When MRSA is recovered, strict isolation of affected patients has been shown to be the most effective method for preventing nosocomial spread of infection. Thereafter, control measures should be directed toward identification of new isolates and strict isolation of newly colonized or infected patients. Clusters of cases may be defined by molecular typing. If associated with a singular molecular strain, it may also be necessary to identify colonized hospital personnel and eradicate carriage in affected individuals.
Patients with recurrent S. aureus skin infection may be treated with hypochlorite baths (1 teaspoon common bleach solution per gallon of water), an appropriate oral antibiotic, and nasal mupirocin in an attempt to prevent recurrences.
Food poisoning (Chapter 332) may be prevented by excluding individuals with S. aureus infections of the skin from the preparation and handling of food. Prepared foods should be eaten immediately or refrigerated appropriately to prevent multiplication of S. aureus with which the food may have been contaminated.
Appelbaum PC. Microbiology of antibiotic resistance in Staphylococcus aureus. Clin Infect Dis. 2007;45:S165-S170.
Baranwal AK, Singhi SC, Jayashree M. A 5-year PICU experience of disseminated staphylococcal disease, part 2: management, critical care needs and outcome. J Trop Pediatr. 2007;53:252-258.
Centers for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus skin infections from and elephant calf—San Diego, California, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:194-198.
Centers for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus among players on a high school football team—New York City, 2007. MMWR Morb Mortal Wkly Rep. 2009;58:52-55.
Climo MW, Sepkowitz KA, Zuccotti G, et al. The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med. 2009;37:1858-1865.
Creech CB, Beekmann SE, Chen Y, et al. Variability among pediatric infectious diseases specialists in the treatment and prevention of methicillin-resistant Staphylococcus aureus skin and soft tissue infections. Pediatr Infect Dis J. 2008;27:270-272.
Day MD, Gauvreau K, Shulman S, et al. Characteristics of children hospitalized with infective endocarditis. Circulation. 2009;119:865-870.
DeLeo FR, Otto M, Kreiswirth B, et al. Community-associated methicillin-resistant Staphylococcus aureus. Lancet. 2010;375:1557-1566.
Duong M, Markwell S, Peter J, et al. Randomized, controlled trial of antibiotics on the management of community-acquired skin abscesses in the pediatric patient. Ann Emerg Med. 2010;55:401-407.
Fisher RG, Chain RL, Hair PS, et al. Hypochlorite killing of community-associated methicillin-resistant Staphylococcus aureus. Pediatr Infect Dis J. 2008;27:934-935.
Fontanilla JM, Kirkland KB, Talbot EA, et al. Outbreak of skin infections in college football team members due to an unusual strain of community-acquired methicillin-susceptible Staphylococcus aureus. J Clin Microbiol. 2010;48:609-611.
Fortunov RM, Hulten KG, Hammerman WA, et al. Community-acquired Staphylococcus aureus infections in term and near-term previously healthy neonates. Pediatrics. 2006;118:874-881.
Frederiksen MS, Espersen F, Frimodt-Moller N, et al. Changing epidemiology of pediatric Staphylococcus aureus bacteremia in Denmark from 1971 through 2000. Pediatr Infect Dis J. 2007;26:398-405.
Frymoyer A, Hersh AL, Benet LZ, et al. Current recommended dosing of vancomycin for children with invasive methicillin-resistant Staphylococcus aureus infections is inadequate. Pediatr Infect Dis J. 2009;28:398-402.
Gerber JS, Coffin SE, Smathers SA, et al. Trends in the incidence of methicillin-resistant Staphylococcus aureus infection in children’s hospitals in the United States. Clin Infect Dis. 2009;49:65-71.
Gonzalez BE, Teruya J, Mahoney DHJr, et al. Venous thrombosis associated with staphylococcal osteomyelitis in children. Pediatrics. 2006;117:1673-1679.
Hanses F, Spaeth C, Ehrenstein BP, et al. Risk factors associated with long-term prognosis of patients with Staphylococcus aureus bacteremia. Infection. 2010;38:465-470.
Haque NZ, Zuniga LC, Peyrani P, et al. Relationship of vancomycin minimum inhibitory concentrations to mortality in patients with methicillin-resistant Staphylococcus aureus hospital-acquired, ventilator-associated, or health-care-associated pneumonia. Chest. 2010;138(6):1356-1362.
Hulten KG, Kaplan SL, Gonzalez BE, et al. Three-year surveillance of community onset health care-associated Staphylococcus aureus infections in children. Pediatr Infect Dis J. 2006;25:349-353.
Hyun DY, Mason EO, Forbes A, et al. Trimethoprim-sulfamethozazole or clindamycin for treatment of community-acquired methicillin-resistant Staphylococcus aureus skin and soft tissue infections. Pediatr Infect Dis J. 2009;28:57-58.
Jacqueline C, Amador G, Caillon J, et al. Efficacy of the new cephalosporin ceftaroline in the treatment of experimental methicillin-resistant Staphylococcus aureus acute osteomyelitis. J Antimicrob Chemother. 2010;65:1749-1752.
Jang HC, Kim SH, Kim KH, et al. Salvage treatment for persistent methicillin-resistant Staphylococcus aureus bacteremia: efficacy of linezolid with or without carbapenem. Clin Infect Dis. 2009;49:395-401.
Jung YJ, Koh Y, Hong SB, et al. Effect of vancomycin plus rifampicin in the treatment of nosocomial methicillin-resistant Staphylococcus aureus pneumonia. Crit Care Med. 2010;38:175-180.
Liu C. The bundled approach to MRSA surgical site infection prevention. Arch Intern Med. 2011;171(1):73-74.
Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guideline by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52(3):285-292.
Lo WT, Lin WJ, Tseng MH, et al. Risk factors and molecular analysis of panton-valentine leukocidin-positive methicillin-resistant Staphylococcus aureus colonization in healthy children. Pediatr Infect Dis J. 2008;27:713-718.
The Medical Letter. Ceftaroline fosamil (Teflaro)—a new IV cephalosporin. Med Lett Drugs Ther. 2011;53(1356):5-6.
Morales G, Picazo JJ, Baos E, et al. Resistance to linezolid is mediated by the cfr gene in the first report of an outbreak of linezolid-resistant Staphylococcus aureus. Clin Infect Dis. 2010;50:821-825.
Naseri I, Jerris RC, Sobol SE. Nationwide trends in pediatric Staphylococcus aureus head and neck infections. Arch Otolaryngol Head Neck Surg. 2009;135:14-16.
Pannaraj PS, Hulten KG, Gonzalez BE, et al. Infective pyomyositis and myositis in children in the era of community-acquired, methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis. 2006;43:953-960.
Reed C, Kallen AJ, Patton M, et al. Infection with community-onset Staphylococcus aureus and influenza virus in hospitalized children. Pediatr Infect Dis J. 2009;28:572-576.
Ross AC, Toltzis P, O’Riordan MA, et al. Frequency and risk factors for deep focus of infection in children with Staphylococcus aureus bacteremia. Pediatr Infect Dis J. 2008;27:396-399.
Tebruegge M, Pantazidou A, Thorburn K, et al. Bacterial tracheitis: a multi-centre perspective. Scand J Infect Dis. 2009:1-10.
Valente AM, Jain R, Scheurer M, et al. Frequency of infective endocarditis among infants and children with Staphylococcus aureus bacteremia. Pediatrics. 2005;115:e15-19.
Varshney AK, Martinez LR, Hamilton SM, et al. Augmented production of Panton-Valentine leukocidin toxin in methicillin-resistant and methicillin-susceptible Staphylococcus aureus is associated with worse outcome in a murine skin infection model. J Infect Dis. 2010;201:92-96.
Wolkewitz M, Frank U, Philips G, et al. Mortality associated with in-hospital bacteremia caused by Staphylococcus aureus: a multistate analysis with follow-up beyond hospital discharge. J Antimicrob Chemother. 2011;66:381-386.
Yoshinaga M, Niwa K, Niwa A, et al. Risk factors for in-hospital mortality during infective endocarditis in patients with congenital heart disease. Am J Cardiol. 2008;101:114-118.
174.2 Toxic Shock Syndrome
TSS is an acute multisystem disease characterized by fever, hypotension, an erythematous rash with subsequent desquamation on the hands and feet, and multisystem involvement including vomiting, diarrhea, myalgias, nonfocal neurologic abnormalities, conjunctival hyperemia, and strawberry tongue.
Etiology
TSS is caused by TSST-1–producing and some enterotoxin-producing strains of S. aureus, which may colonize the vagina or cause focal sites of staphylococcal infection.
Epidemiology
Many cases occur in menstruating women 15-25 yr of age and who use tampons or other vaginal devices (diaphragm, contraceptive sponge). TSS also occurs in children, nonmenstruating women, and men usually associated with an identifiable focus of S. aureus infection. Nonmenstrual TSS has occurred with S. aureus infection of nasal packing or infections including wound infections, sinusitis, tracheitis, pneumonia, empyema, abscesses, burns, osteomyelitis, and primary bacteremia. Without antimicrobial therapy, menstrual TSS has a 30% recurrence rate if tampons are used, with secondary cases being milder and occurring within 5 mo of the original episode. The overall mortality rate of treated patients is 3-5%. Most strains of S. aureus associated with TSS have been susceptible to the semi-synthetic β-lactam antibiotics, including 1st generation cephalosporins, but some methicillin/cephalosporin–resistant cases have been reported.
Pathogenesis
The primary toxin associated with TSS is TSST-1, which acts as a superantigen causing massive loss of fluid from the intravascular space. TSST-1–negative S. aureus strains have been isolated from patients with TSS, suggesting that other toxins (primarily the enterotoxins) have a role in TSS (especially nonmenstrual). Epidemiologic and in vitro studies suggest that these toxins are selectively produced in a clinical environment consisting of a neutral pH, a high PCO2, and an “aerobic” PO2, which are the conditions found in the vagina with tampon use during menstruation. Approximately 90% of adults have antibody to TSST-1 without a history of clinical TSS, suggesting that most individuals are colonized at some point with a toxin-producing organism at a site (anterior nares) where low-grade or inactive toxin exposure results in an immune response without disease. The risk factors for symptomatic disease include a nonimmune host colonized with a toxin-producing organism, which is exposed to focal growth conditions (menstruation plus tampon use or abscess) that induce toxin production. It appears that some hosts may have a varied cytokine response to exposure to TSST-1, helping to explain a spectrum of severity of TSS that may include staphylococcal scarlet fever.
Clinical Manifestations
The diagnosis of TSS is based on clinical manifestations (Table 174-2). The onset is abrupt, with high fever, vomiting, and diarrhea, and is accompanied by sore throat, headache, and myalgias. A diffuse erythematous macular rash (sunburn-like or scarlatiniform) appears within 24 hr and may be associated with hyperemia of pharyngeal, conjunctival, and vaginal mucous membranes. A strawberry tongue is common. Symptoms often include alterations in the level of consciousness, oliguria, and hypotension, which in severe cases may progress to shock and disseminated intravascular coagulation. Complications, including acute respiratory distress syndrome, myocardial dysfunction, and renal failure, are commensurate with the degree of shock. Recovery occurs within 7-10 days and is associated with desquamation, particularly of palms and soles; hair and nail loss have also been observed after 1-2 mo. Many cases of apparent scarlet fever without shock may be caused by TSST-1-producing S. aureus strains.
Table 174-2 DIAGNOSTIC CRITERIA OF STAPHYLOCOCCAL TOXIC SHOCK SYNDROME
MAJOR CRITERIA (ALL REQUIRED)
MINOR CRITERIA (ANY 3 OR MORE)
EXCLUSIONARY CRITERIA
From the American Academy of Pediatrics Red book: 2009 report of the Committee on Infectious Diseases, ed 28, Elk Grove Village, IL, 2009, American Academy of Pediatrics, p 602.
Diagnosis
There is no specific laboratory test; appropriate selective tests reveal involvement of multiple organ systems, including the hepatic, renal, muscular, gastrointestinal, cardiopulmonary, and central nervous systems. Bacterial cultures of the associated focus (vagina, abscess) before administration of antibiotics usually yield S. aureus, although this is not a required element of the definition.
Differential Diagnosis
Group A streptococcus can cause a similar TSS-like illness, termed streptococcal TSS (Chapter 176), which is often associated with severe streptococcal sepsis or a focal streptococcal infection such as cellulitis, necrotizing fasciitis, or pneumonia.
Kawasaki disease closely resembles TSS clinically but is usually not as severe or rapidly progressive. Both conditions are associated with fever unresponsive to antibiotics, hyperemia of mucous membranes, and an erythematous rash with subsequent desquamation. However, many of the clinical features of TSS are usually absent or rare in Kawasaki disease, including diffuse myalgia, vomiting, abdominal pain, diarrhea, azotemia, hypotension, acute respiratory distress syndrome, and shock (Chapter 160). Kawasaki disease typically occurs in children younger than 5 yr. Scarlet fever, Rocky Mountain spotted fever, leptospirosis, toxic epidermal necrolysis, sepsis, and measles must also be considered in the differential diagnosis.
Treatment
Parenteral administration of a β-lactamase–resistant antistaphylococcal antibiotic (nafcillin, oxacillin, or a 1st generation cephalosporin) or vancomycin in areas where MRSA is common is recommended after appropriate cultures have been obtained. The addition of clindamycin is recommended to reduce toxin production. Drainage of the vagina by removal of any retained tampons in menstrual TSS and of focally infected sites in nonmenstrual TSS is important for successful treatment. Antistaphylococcal therapy may also reduce the risk for recurrence in menstrual TSS.
Fluid replacement should be aggressive to prevent or treat hypotension, renal failure, and cardiovascular collapse. Inotropic agents may be needed to treat shock; corticosteroids and intravenous immunoglobulin may be helpful in severe cases.
Prevention
The risk for acquiring menstrual TSS (1-2 cases/100,000 menstruating women) is low. Changing tampons at least every 8 hr is recommended. If a fever, rash, or dizziness develops during menstruation, any tampon should be removed immediately and medical attention should be sought.
Chan KH, Kraai TL, Richter GT, et al. Toxic shock syndrome and rhinosinusitis in children. Arch Otolaryngol Head Neck Surg. 2009;135:538-542.
Lappin E, Ferguson AJ. Gram-positive toxic shock syndromes. Lancet Infect Dis. 2009;9:281-290.
Zimbelman J, Palmer A, Todd JK. Improved outcome of clindamycin compared with beta-lactam antibiotics treatment of invasive Streptococcus pyogenes infection. Pediatr Infect Dis J. 1999;18:1096-1100.
174.3 Coagulase-Negative Staphylococci
S. epidermidis is just 1 of many recognized species of coagulase-negative staphylococci (CONS) affecting or colonizing humans. Originally thought to be avirulent commensal bacteria, CONS is now recognized to cause infections in patients with indwelling foreign devices, including intravenous catheters, hemodialysis shunts and grafts, CSF shunts (meningitis), peritoneal dialysis catheters (peritonitis), pacemaker wires and electrodes (local infection), prosthetic cardiac valves (endocarditis), and prosthetic joints (arthritis). CONS is a common cause of nosocomial neonatal infection. S. haemolyticus, another CONS species, is an important cause of invasive infection and may develop resistance to vancomycin and teicoplanin.
Epidemiology
CONS consist of normal inhabitants of the human skin, throat, mouth, vagina, and urethra. S. epidermidis is the most common and persistent species, representing 65-90% of staphylococci present on the skin and mucous membranes. Colonization, sometimes with strains acquired from hospital staff, precedes infection; alternatively, direct inoculation during surgery may initiate infection of CSF shunts, prosthetic valves, or indwelling vascular lines. For epidemiologic purposes, CONS can be identified on the basis of molecular DNA methods.
Pathogenesis
CONS produce an exopolysaccharide protective biofilm, or slime layer, that surrounds the organism and may enhance adhesion to foreign surfaces, resist phagocytosis, and impair penetration of antibiotics.
Clinical Manifestations
The low virulence of CONS usually requires the presence of another factor, such as immune compromise or a foreign body, for development of clinical disease.
Bacteremia
CONS, specifically S. epidermidis, are the most common cause of nosocomial bacteremia, usually in association with central vascular catheters. In neonates, CONS bacteremia, with or without a central venous catheter, may be manifested as apnea, bradycardia, temperature instability, abdominal distention, hematochezia, meningitis in the absence of CSF pleocytosis, cutaneous abscesses, and persistence of positive blood cultures despite adequate antimicrobial therapy. In most circumstances, CONS bacteremia is indolent and is not usually associated with overwhelming septic shock.
Endocarditis
Infection of native heart valves or the right atrial wall secondary to an infected thrombosis at the end of a central line may produce endocarditis. S. epidermidis and other CONS may rarely produce native valve subacute indolent endocarditis in previously normal patients without a central venous catheter. CONS is a common cause of prosthetic valve endocarditis, presumably due to inoculation at the time of surgery. Infection of the valve sewing ring, with abscess formation and dissection, produces valve dysfunction, dehiscence, arrhythmias, or valve obstruction (Chapter 431).
Central Venous Catheter Infection
Central venous catheters become infected through the exit site and subcutaneous tunnel, which provide a direct path to the bloodstream. S. epidermidis is the most common CONS, owing in part to its high rate of cutaneous colonization. Line sepsis is usually manifested as fever and leukocytosis; tenderness and erythema may be present at the exit site or along the subcutaneous tunnel. Catheter thrombosis may complicate line sepsis.
Cerebrospinal Fluid Shunts
CONS, introduced at the time of surgery, is the most common pathogen associated with CSF shunt meningitis. Most (70-80%) infections occur within 2 mo of the operation and are manifested by signs of meningeal irritation, fever, increased intracranial pressure (headache), and peritonitis due to the intra-abdominal position of the distal end of the shunt tubing.
Urinary Tract Infection
S. saprophyticus is a common cause of primary urinary tract infections in sexually active females. Manifestations are similar to those characteristics of urinary tract infection due to Escherichia coli (Chapter 532). CONS also causes asymptomatic urinary tract infection in hospitalized patients with urinary catheters and after urinary tract surgery or transplantation.
Diagnosis
Because S. epidermidis is a common skin inhabitant and may contaminate poorly collected blood cultures, differentiating bacteremia from contamination is often difficult. True bacteremia should be suspected if blood cultures grow rapidly (within 24 hr), ≥2 blood cultures are positive with the same CONS, and clinical and laboratory signs and symptoms compatible with CONS sepsis are present and subsequently resolve with appropriate therapy. No blood culture that is positive for CONS in a neonate or patient with intravascular catheter should be considered contaminated without careful assessment of the foregoing criteria and examination of the patient. Before initiating presumptive antimicrobial therapy in such patients, it is always prudent to draw 2 separate blood cultures to facilitate subsequent interpretation if CONS is grown.
Treatment
Most CONS strains are resistant to methicillin. Vancomycin is the drug of choice for methicillin-resistant strains. The addition of rifampin to vancomycin may increase antimicrobial efficacy. In many cases of CONS infection associated with foreign bodies, the catheter, valve, or shunt must be removed to ensure a cure. Prosthetic heart valves and CSF shunts usually have to be removed to treat the infection adequately.
Antibiotic therapy given through an infected central venous catheter (through each lumen) may effectively cure CONS line sepsis. If the catheter or reservoir is no longer needed, it should be removed. Unfortunately, removal is not always possible owing to the therapeutic requirements of the underlying disease (nutrition for short bowel syndrome, chemotherapy for malignancy). A trial of intravenous vancomycin is indicated to attempt to preserve the use of the central line as long as systemic manifestations of infection are not severe.
Peritonitis caused by S. epidermidis in patients on continuous ambulatory peritoneal dialysis is an infection that may be treated with intravenous or intraperitoneal antibiotics without removing the dialysis catheter. If the organism is resistant to methicillin, vancomycin adjusted for renal function is appropriate therapy.
Prognosis
Most episodes of CONS bacteremia respond successfully to antibiotics and removal of any foreign body that is present. Poor prognosis is associated with malignancy, neutropenia, and infected prosthetic or native heart valves. CONS increases morbidity, the duration of hospitalization, and mortality rates among patients with underlying complicated illnesses.
Acuna M, O’Ryan M, Cofre J, et al. Differential time to positivity and quantitative cultures for noninvasive diagnosis of catheter-related blood stream infection in children. Pediatr Infect Dis J. 2008;27:681-685.
Karlowicz MG, Furigay PJ, Croitoru DP, et al. Central venous catheter removal versus in situ treatment in neonates with coagulase-negative staphylococcal bacteremia. Pediatr Infect Dis J. 2002;21:22-27.