CHAPTER 49 Occlusal Evaluation and Therapy
Among the numerous local and systemic factors with the potential to influence the progression of periodontitis, the patient’s occlusion remains a variable requiring exacting diagnosis. All the disciplines of dentistry include comprehensive analysis of occlusal relationships as essential to the determination of appropriate care. The functional demands of the occlusion may fall well within or may exceed the tolerances and the adaptability of a patient’s periodontium and their entire masticatory system. The full range of knowledge and skill to analyze all aspects of occlusal anatomy and function is beyond the scope of this text. Rather, this chapter presents practical guidelines for the assessment and management of the occlusion specific to a patient’s unique susceptibility to periodontitis.
Pathogenesis
Our understanding of the host-driven inflammatory response of each patient to a pathogenic bacterial biofilm is growing exponentially.32 Each individual’s susceptibility appears to be so specific that they are actually their only reference in the interpretation of possible contributing factors to progressive loss of supporting bone. Additionally, we observe that destructive events may be episodic and are clearly site specific. Our diagnostic responsibility includes careful measuring of periodontal structures in the entire circumference of each tooth, accurate documentation, and timely reassessment. Periodontal deterioration that occurs rapidly or is excessive for a person’s age should prompt the clinician to investigate any variable that might amplify that patient’s periodontitis. If a local factor, such as an occlusal relationship, can influence the course of the disease, then its analysis must be as precise as any other aspect of the periodontal examination.
Evidence-Based Decision Making
Ideally, all our diagnostic and therapeutic decisions would reflect evidence from multiple prospective clinical trials subject to systematic review. Prospective human investigations of occlusal trauma are considered unethical so periodontics has conscientiously struggled to reach discipline-wide consensus about the interaction of patient’s occlusion and their periodontal status.11 To be clinically applicable, the investigation’s methodology must parallel the clinical diagnosis and treatment of an individual patient with periodontitis.13 Historically, data management and statistical credibility and methodology within retrospective studies limited the ability of dedicated researchers to interpret the role of occlusion in an individual’s periodontitis experience.14,31,34 Grouping of data points, especially in large study populations, departs from the site specificity that periodontal diagnosis requires. If occlusal trauma is affecting a tooth, the effect on the periodontium is site specific for only that tooth. Treatment for a patient with periodontitis would never be based on an average of diagnostic references but rather on their unique susceptibility, anatomy, occlusion, and history.
Nunn and Harrell28 reported in 2001 the retrospective findings of a group of patients with periodontitis in which the analysis was based on the measurement of loss of attachment of each individual tooth and the presence or absence of occlusal interferences. This study and a similar investigation4 confirmed that trauma from occlusion amplified loss of attachment. Harrell and Nunn12 also reported that eliminating occlusal interferences had a positive influence on the outcome of treatment when trauma from occlusion was found to be a contributing local factor. The positive influence of occlusal adjustment on the outcome of both surgical and nonsurgical periodontal therapies had also been reported by Burgett.5 Evidence now appears to support the possibility that trauma from occlusion has the capability to amplify damage to an inflamed periodontium.
Interest in the occlusion within the discipline of periodontics appears to be increasing, especially with the rapid growth of implant replacement of missing teeth. Despite some conflicting evidence in the literature, common ground for consensus exists. There is general agreement that occlusal force has an effect on the periodontium, as described in Chapter 15, and that susceptibility to periodontitis is unique to each patient. Occlusal forces present themselves across a broad spectrum. No or minimal occlusal contact on a tooth results in disuse atrophy of the periodontium, which may result in instability of that tooth. Harmonious occlusal force on a tooth stimulates physiologic arrangement of its periodontal attachment fibers and osseous architecture and encourages its stability. Forces that exceed the tolerance of the periodontium result in resorption of the bone and disruption of the attachment.16,25,27 In the healthy person, the periodontium around teeth subject to excessive occlusal force experiences adaptation and repair or remodeling with no loss of attachment, as often occurs with orthodontics. For the patient who is losing bone as the result of periodontitis, coupling the ongoing inflammatory disease with excessive occlusal force may result in the amplification of destruction and damage to the periodontium of affected teeth.28 If this conclusion is valid, then the clinician has the responsibility to correlate the precise analysis of the periodontal status of each tooth with its occlusal responsibilities and its possible occlusal excesses.
Terminology
The following is a list of key descriptive terms used in this chapter, along with common synonyms:
Occlusal Function and Dysfunction
Excellent sources of comprehensive understanding of dental anatomy and function include texts by Wheeler,3 McNeill,23 and Dawson.8,9 The determination if trauma from occlusion is occurring is based on the conclusion that the composite of all occlusal forces on a specific tooth exceeds the tolerance or adaptability of its periodontium. The identification of masticatory system disharmonies begins with appreciation of physiologic norms allowing the clinician to recognize dysfunctional relationships, which might influence the accuracy of diagnosis.9,27,29
Centric relation is a term used to describe the position of both condyles when they are fully seated in the fossa of their respective temporomandibular joints (TMJs). Rotation of the mandible around an axis through both condyles is called the centric relation closure arc (see Chapter 20). This is strictly a skeletal relationship until tooth contact occurs. Maximum intercuspation occurs when opposing teeth make contact, with optimal interdigitation, at the most stable endpoint of mandibular closure. Stability is enhanced by simultaneous bilateral contact of multiple posterior teeth with occlusal forces in the long axis of most posterior teeth. If the initial tooth contact in the centric relation arc of closure occurs simultaneously with maximum intercuspation, then the teeth do not displace condyles. Conversely, if the teeth are firm and any contact occurs before maximum intercuspation, then incline relationships of opposing occlusal surfaces will guide the mandible into intercuspal position, requiring one or both condyles to become dislocated from their fossa.9,28 If teeth are mobile and contact first in the centric relation closure arc, then they may move away from opposing teeth rather than cause condylar displacement.
Cusp-fossa or cusp-marginal ridge relationships of posterior teeth provide resistance to vertical loading and functional stability to a patient’s dentition. When occlusal forces load teeth in their long axis, the periodontium is the most resistant and supportive.8,9 The anterior teeth can be stable with little occlusal loading in centric occlusion if favorably influenced by oral musculature. If the anterior teeth are in contact in maximum intercuspation, they are coupled. Movement of the mandible from centric occlusion is called an excursion. Movement forward is called a protrusive excursion, and movement to either side is called a lateral excursion. If the mandible can move posteriorly, it is called retrusion. There is evidence that contact of posterior teeth in excursions can overload those teeth with negative dental, periodontal, muscular, and TMJ consequences.* The ideal relationship might be light coupling of anterior teeth in centric occlusion with immediate separation, called disclusion, of all posterior teeth in all excursions.38 During a lateral excursion, posterior teeth that contact on the same side as the direction of mandibular movement are described as having a working contact. Posterior teeth that contact on the side opposite the direction of the lateral excursion are described as having a nonworking contact. Although nonworking contacts are classically associated with more potential negative consequences,39 analysis of working contacts and the function of anterior teeth is critically important. Contacts disruptive to mandibular movement or stressful to individual teeth are called occlusal interferences or discrepancies. Our ability to analyze the occlusion to identify contacts that may amplify a patient’s periodontitis affecting certain teeth is strategic to correct diagnosis.
Inflammation disrupts the integrity of the attachment apparatus, resulting in less resistance to force from opposing teeth. When bone loss has occurred, there is less root surface area supported2,15 and fewer sensory fibers in the periodontal ligament, limiting protective muscle modulation of occlusal forces.33 The clinician must differentiate between inflammation-caused intolerance to occlusal forces, normal forces on teeth with reduced periodontal support, excessive occlusal forces, and well-tolerated forces on teeth affected by periodontitis.
Parafunction
Bruxism may cause occlusal forces on teeth susceptible to periodontitis to be increased in intensity and/or frequency, magnifying potential amplification of damage.7,18,19,35 Daytime occlusal parafunction is commonly limited to clenching of the teeth during incidents requiring a person’s focused effort or mental concentration. Nighttime bruxing of the teeth can take the form of grinding the teeth in various excursions and/or clenching of the teeth. Sleep bruxism is probably an extension of the rhythmic masticatory muscle activity that is also observed in nonbruxers. Why nuclei in the brainstem allow bruxing to occur with some individuals while others are spared is unclear.7,18,19 Bruxing is associated with greater frequency and persistence of TMJ dysfunction, orofacial pain, and possibly periodontal attachment loss.35 Sensory input of teeth subject to bruxism is probably dampened, which may interfere with both diagnosis and treatment.30 There seems to be limited influence on bruxing tendencies from occlusal interferences.20 Selective serotonin reuptake inhibitors, such as Prozac, have been reported to encourage bruxism.10
Clinical Examination
Before clinical evaluation, a conversation with the patient can be very helpful in acquiring a more complete diagnosis. With minimal symptoms, a patient may not associate loose teeth or significant dental wear with TMJ dysfunction and/or orofacial pain with occlusal function or parafunction. The list of questions in Chapter 20 and inquiries specific to the condition of their teeth can help the clinician open lines of communication and set the tone for patient education during the clinical examination. Comprehensive evaluation of occlusal anatomy and relationships is accomplished by the analysis of many factors in the clinical setting and on mounted diagnostic casts.
The clinical evaluation of the occlusion is sequenced to support the patient’s learning and should always include a clinical assessment of masticatory system function and identification of any disharmony.
Temporomandibular Disorders Screening Evaluation
The complete assessment of the masticatory system and identification of temporomandibular disorders (TMDs) are carefully described in Chapter 20 and should be part of a patient’s initial comprehensive examination. The TMD screening clinical evaluation then becomes part of each subsequent examination. The patient’s range of motion is observed, maximal opening and both lateral and protrusive excursions are measured, and any deviation from the midline during opening and closing is defined. Light finger pressure applied over each TMJ can detect deflection of the tissue while the patient opens and closes, suggesting condyle-disc discoordination. Tenderness on palpation may indicate a TMJ capsulitis. Listening to the joint with a stethoscope or a Doppler instrument during opening and closing may detect sounds consistent with uncoordinated condyle-disc relationships, arthritic changes, and other diagnostic sounds.9 Palpation of the muscles of mastication and related head and neck musculature may reveal muscle tension or spasm related to compensation for occlusal or TMJ disharmonies.9,29 Load testing of the TMJ is described in Chapter 20. Any significant discovery that is revealed during the screening examination summarized on Box 49-1 should lead the clinician to complete the comprehensive evaluation.
Testing For Mobility Of Teeth
There are two basic methods to assess the firmness or looseness of a tooth. Classically, a dental instrument is used to exert pressure in facial or lingual direction and the dentist places his or her finger on the opposite side of the tooth to both feel and see movement if it occurs, as described in Chapter 30. Recording a numeric value for the degree of mobility in a range of zero to three allows the clinician to track changes in response to therapy. The other method is to test for movement of teeth subject to pressure the patient generates. Fremitus, vibration, or micromovement of a tooth can be felt when patients tap their teeth together. When the patient mimics clenching the teeth and then attempts to move the mandible in excursions, tooth movement can be observed. The patient placing finger where the clinician felt tooth movement helps the patient appreciate looseness of their teeth (Figure 49-1). If the mobility of teeth exceeds that expected based on the loss of support or the level of inflammation observed, then trauma from occlusion is included in the diagnosis. The assimilation of all the occlusal and periodontal diagnostic references may also lead the clinician to conclude that even without mobility there may be evidence of amplification of periodontal damage based on unfavorable occlusal forces.

Figure 49-1 A, Tactile and visual testing for mobility with a dental instrument by the dentist. B, Tactile and visual testing for mobility with patient clenching and beginning right lateral excursion by the dentist. C, Patient feeling movement of her tooth when lateral excursion attempted while teeth clenched.
Centric Relation Assessment
Bimanual manipulation of the mandible in the axis of rotation of the condyles in their respective glenoid fossa has become a standard method of assessing centric relation.3,8,9,29 This method is illustrated in Figure 49-2 and utilizes gentle guidance, not forced positioning of the mandible. This technique is essential to load testing of the TMJs and is effective in generating centric relation records for mounting diagnostic casts. Telling the patient he or she will feel modest lifting pressure on the inferior borders of the mandible and light depressing force in the mental region often allows for relatively free and comfortable hinging of the mandible.8,9 If the hinging is uncomfortable and/or not repeatable, then muscle deprogramming, as described in Chapter 20, may be beneficial. Other methods for guiding the condyles toward a seated position, such as leaf gauges or anterior bite stops, can also be effective.9 Asking the patient to identify the first tooth to touch in the centric relation arc of closure may indicate that interferences to closure into maximum intercuspation exist. Asking the patient to close further may demonstrate a slide from centric relation to centric occlusion because teeth are firm enough to dislocate one or both condyles.29 Drying the occlusal surfaces and positioning marking paper, and then guiding the patient to the initial contact in centric relation will mark occlusal contact points, identifying any interference. Then asking the patient to close into maximum intercuspation will mark the points or surfaces that contact during the slide. An early occlusal contact in centric relation before closure to centric occlusion is obtained that does not cause a slide may indicate the early contact that occurs on teeth mobile enough to move, allowing maximal intercuspation to be gained without condylar accommodation (Figure 49-3). The confirmation of permissive intercuspation is a product of marking the teeth clinically and comparing those marks with the ones on mounted diagnostic casts, which demonstrates that mobile teeth can move out of the way to allow others to contact.
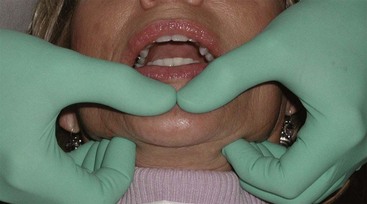
Figure 49-2 Bimanual manipulation to hinge the mandible in centric relation and load test the temporomandibular joints (TMJs).
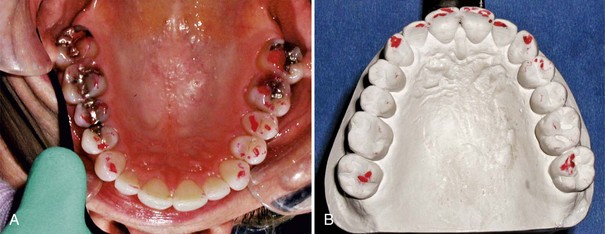
Figure 49-3 A, Teeth marked clinically in maximum intercuspation and in excursions while clenching. B, Teeth marked in centric relation and maximum intercuspation on diagnostic cast mounted in centric relation. Marks only on second molars indicate they were mobile and that they moved to permit contact of other teeth.
Evaluation of Excursions
Marking of the teeth in all excursions will reveal the pathways of contact of opposing occlusal or incisal surfaces during function and may identify interferences to harmonious function.3,9,23 Movement of any teeth during marking may lessen the intensity of the marks and the assessed severity of the forces experienced by the affected teeth. Vectors of force and the steepness of the opposing inclines are studied to determine if force is excessive. Interpreting those contacts on a tooth-by-tooth basis can suggest or deny occlusal trauma as a contributing factor to the loss of attachment of each affected tooth. When patients are engaged in the evaluation of their occlusion, they can be given suggestions to observe certain habits such as clenching their teeth during the day or sleeping with pressure on their mandible. As they contribute to their own diagnosis, they become better prepared to make informed choices about the treatment options.
Articulated Diagnostic Casts
When the maxillary diagnostic cast is mounted on an articulator with a facebow transfer technique, the occlusal surfaces become oriented to the axis of rotation of the patient’s condyles. The centric relation transfer record orients the mandibular teeth to the maxillary teeth in centric relation.8,9 Study of the accurately mounted diagnostic casts may reveal occlusal discrepancies between initial contact in the centric relation closure arc and maximum intercuspation and occlusal disharmonies in excursions. Mobile teeth may produce a mark on a solid model but little or no mark in that patient’s mouth during clinical assessment. Accuracy of the observations made on the models should be confirmed clinically to the degree possible.
Occlusal Therapy
Effective nonsurgical therapy usually reduces the inflammation within the periodontium and results in some healing of attachment,26 often resulting in mobile teeth becoming more stable. If the clinician concludes that inflammation has been optimally controlled and that occlusal forces on individual teeth still exceed the tolerance of their periodontium, then the basis for intervention is established. Harmonious function of both TMJs and associated muscles is required for occlusal stability. When there is sufficient evidence of excessive occlusal forces on the patient’s teeth and/or masticatory system disharmony exists and the patient desires a more stable occlusion, then an occlusal appliance is prescribed.
A review of the TMJ anatomy in Chapter 20 will be helpful to better understand the therapy.
A well-designed, accurately fitted appliance can benefit masticatory system function while encouraging loose teeth in both arches to tighten as supporting periodontium heals. Bilateral simultaneous contact of all opposing posterior teeth in centric relation, shallow anterior guidance, and immediate disclusion of all posterior teeth in every excursion are essential elements of both maxillary and mandibular occlusal appliances (Figures 49-4 and 49-5). Teeth opposing an appliance should be loaded as close as possible to their long axis. Maxillary appliances engage a portion of the hard palate, which provides substantial bracing of teeth and resistance to vertical and lateral forces. A horseshoe-shaped maxillary appliance relies on other, possibly compromised teeth to attempt to protect the most mobile teeth. Soft or partial coverage appliances are contraindicated for long-term protection and stabilization.26 A protective role of occlusal appliances was reported in the 8-year study by McGuire.22 Occlusal appliances are not expected to cure bruxism21 but often are prescribed for a patient with habitual parafunction as a compensating or protective intervention to limit masticatory system disharmony, damage to the teeth, and overstressing of implants.17

Figure 49-4 A, Occlusal appliance fabricated on accurately mounted diagnostic casts. B, Entire dental and palatal surface carefully relined clinically for optimal stabilizing influence on any mobile teeth. C, Bilateral simultaneous contact of cuspids and all posterior teeth in centric relation, fabricated to enhance axial loading of opposing mandibular teeth. D, Smooth, relatively flat anterior guidance with immediate and sustained disclusion of all posterior teeth in protrusive. E, Smooth, relatively flat anterior guidance with immediate and sustained disclusion of all posterior teeth in right lateral excursions. F, Extreme left lateral excursion with smooth, harmonious transitions across anterior teeth maintaining disclusion of all posterior teeth. G, Marks created by opposing dentition, demonstrating bilateral simultaneous contact in centric relation and immediate disclusion of opposing posterior teeth in all excursions.
As teeth tighten from the consistent use of the appliance, occlusal interferences may become more evident and greater discrepancy between the initial dental contact and maximum intercuspation may be observed. Interferences to harmonious excursive movement of the mandible may also become more obvious. When the clinician confirms that the interferences correlate with greater than expected loss of attachment, then direct intervention with the patient’s occlusion is considered. With the patient’s full understanding and consent, occlusal adjustment or selective reshaping of occluding surfaces of teeth can reduce the magnitude of occlusal interferences or direct the forces more compatibly with the long axis of affected teeth. The clinical analysis of the occlusion should be combined with detailed analysis of diagnostic casts mounted in centric relation on an adjustable articulator. Accurately mounted duplicate models can be used to accomplish a trial occlusal adjustment to determine safety and efficacy for a patient.9,23 Scheduling patients so they leave their appliances on overnight and in place until seated in the dental chair allows assessment of their teeth at maximum firmness when interferences are most readily identifiable. Teeth will usually progressively tighten with continued compliance with the appliance and repeated careful occlusal adjustment. Other methods employed to alter occlusal relationships include orthodontics and restorative dentistry. Provisional restoration of teeth is another method of improving occlusal contacts and stability, often simplifying the process of occlusal adjustment and final restoration.
![]() Science Transfer
Science Transfer
Teeth affected by plaque-induced bone loss in periodontitis can have amplification of bone destruction and mobility when occlusal trauma is also present. Occlusal evaluation is integral to treatment planning, and occlusal therapy involving occlusal adjustment and the use of occlusal appliance therapy can not only limit further localized bone loss but also can reduce parafunctional loading of periodontally involved teeth by controlling bruxism and clenching. Implants placed in the partially edentulous patient need to be treated with restorations that allow for load sharing with the more normally mobile teeth, thus centric contacts on implants need to be lighter than those on adjacent teeth and occlusal surfaces should be narrower than the occlusal tables that are present on natural teeth.
Occlusal Stability for Restorative Dentistry
A stable occlusion is considered a prerequisite for any restorative therapy (Box 49-2). Implants replacing teeth in the partially dentate patient add to the occlusal considerations. Osseointegration of implants eliminates micromovement, by which teeth may accommodate to occlusal forces. The extent and timing of occlusal loading and guidance requirement for each tooth and for each implant must be carefully harmonized (see Chapters 66 and 76). This is especially critical if any of the teeth are mobile and/or the patient bruxes to any significant degree.36 If bruxism is suspected or the functional forces are considered to be excessive, then the occlusal appliance as described may have valuable application.17,24
BOX 49-2 Requirements for Occlusal Stability
Summary
Confirmation of appropriateness of occlusal therapy is the product of thorough and complete evaluation of both the patient’s occlusion and their masticatory system. The sequence of occlusal treatment begins with antiinflammatory therapy and progresses through reversible appliance therapy before considering any of the irreversible options. This provides the clinician with the most careful approach to assessing and to treating the occlusion of a patient with periodontitis.
1 Al-Hadi LA. Prevalence of temporomandibular disorders in relation to some occlusal parameters. J Prosthet Dent. 1993;70:345.
2 Alkan A, Keskiner I, Arici S, Sato S. The effect of periodontitis on biting abilities. J Periodontol. 2006;77:1442.
3 Ash MM, Nelson SJ. Wheeler’s dental anatomy, physiology and occlusion, ed 8. St. Louis: Saunders; 2003.
4 Bernhardt O, Gesch D, Look JO, et al. The influence of dynamic interferences on probing depth and attachment level: results of the study of health in Pomerania (SHIP). J Periodontol. 2006;77:506.
5 Burgett F, Ramfjord S, Nissle R, et al. A randomized trial of occlusal adjustment in the treatment of periodontitis patients. J Clin Periodontol. 1992;19:381.
6 Christensen GJ. Abnormal occlusal conditions: a forgotten part of dentistry. J Am Dent Assoc. 1995;126:1667.
7 Clark GT, Ram S. Four oral motor disorders: bruxism, dystonia, dyskinesia and drug-induced dystonic extrapyramidal reactions. Dent Clin N Am. 2007;51:225.
8 Dawson PE. Evaluation, diagnosis, and treatment of occlusal problems, ed 2. St Louis: Mosby; 1989.
9 Dawson PE. Functional occlusion from TMJ to smile design. St. Louis: Mosby; 2007.
10 Gerber PE, Lynd LD. Selective serotonin reuptake inhibitor induced movement disorders. Ann Pharmacother. 1998;32:692.
11 Gher ME. Non-surgical pocket therapy: dental occlusion. Ann Periodontol. 1996;1:567.
12 Harrell SK, Nunn ME. The effect of occlusal discrepancies on treated and untreated periodontitis, part II: relationship of occlusal treatment to the progression of periodontal disease. J Periodontol. 2001;72:495.
13 Harrel SK, Nunn ME, Hallmon WW, Deas DE, Mealey BL. Is there an association between occlusion and periodontal destruction? JADA. 2006;137:1380.
14 Jin L, Cao C. Clinical diagnosis of trauma from occlusion and its relation with severity of periodontitis. J Clin Periodontol. 1992;19:92.
15 Johansson AS, Svensson KG, Trulsson M: Impaired masticatory behavior in subjects with reduced periodontal tissue support.
16 Kaku M, Uoshima K, Yamashita Y, Miura H. Investigation of periodontal ligament reaction upon excessive occlusal load—osteopontin induction among periodontal ligament cells. J Periodont Res. 2005;40:59.
17 Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances evidence of their efficacy. J Am Dent Assoc. 2001;132:770.
18 Lavigne GJ, Kato T, Koltra A, Sessle BJ. Neurobiological mechanisms involoved in sleep bruxism. Crit Rev Oral Biol Med. 2003;14:30.
19 Lavigne GJ, Khoury S, Abe S, et al. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35:476.
20 Lobbezoo F, Naeije M. Bruxism is regulated centrally not peripherally. J Oral Rehabil. 2001;28:1085.
21 Macedo CR, Silva AB, Machado MA, et al: Occlusal splints for treating slep bruxism (tooth grinding), Cochrane Database Syst Rev 17:CD005514, 2007.
22 McGuire MK, Nunn ME. Prognosis versus actual outcome II: The effectiveness of clinical parameters in developing an accurate prognosis. J Periodontol. 1996;67:658.
23 McNeill C. Science and practice of occlusion. Carol Stream: Quintessence; 1997.
24 Misch CE. The effect of bruxism on treatment planning for implants. Dent Today. 2002;21:76.
25 Motohira H, Hayshi J, Tatsumi J, et al. Hypoxia and reoxygenation augment bone-resorbing factor production from human periodontal ligament cells. J Periodontol. 2007;78:1803.
26 Narita N, Funato M, Ishii T, et al. Effects of jaw clenching while wearing an occlusal splint on awareness of tiredness, bite force and EEG power spectrum. J Prosthodont Res. 2009;53:120.
27 Newman MG, Takei HH, Klokkevold PR, Carranza FA. Carranza’s clinical periodontology, ed 10. St. Louis: Saunders; 2006.
28 Nunn M, Harrell SK. The effect of occlusal discrepancies on treated and untreated periodontitis, part I: relationship of initial occlusal discrepancies to initial clinical parameters. J Periodontol. 2001;72:485.
29 Okeson JP. Management of temporomandibular joint disorders and occlusion, ed 4. St Louis: Mosby; 1998.
30 Ono Y, Suganuma T, Shinya A, et al. Effects of sleep bruxism on periodontal sensation and tooth displacement in the molar region. J Craniomandib Pract. 2008;26:282.
31 Pihlstrom B, Anderson K, Aeppli D, Schaffer E. Association between signs of trauma from occlusion and periodontitis. J Periodontol. 1986;57:1.
32 Proceedings of the 2008 workshop on inflammation and periodontal diseases: a reappraisal. J Periodontol. 2008;79:1501.
33 Rosenbaum RS. The possible effects of periodontal disease on occlusal function. Curr Opin Periodontol. 1993:163-169. (review)
34 Shefter GJ, McFall WTJr. Occlusal relations and periodontal status in human adults. J Periodontol. 1984;55:386.
35 Tokiwa O, Park B, Takezawa Y, et al: Relationship of tooth grinding pattern during sleep bruxism and dental status.
36 Tosun T, Karabuda C, Cuhadaroglu C. Evaluation of sleep bruxism by polysomnographic analysis in patients with dental implants. Oral Maxillofac Implants. 2003;18:286.
37 Watanabe EK, Yatani H, Kuboki T, et al. The relationship between signs and symptoms of temporomandibular disorders and bilateral occlusal contact patterns in lateral excursions. J Oral Rehabil. 1998;25:409.
38 Williamson EH, Ludquist DO. Anterior guidance: its effect on electromyographic activity of the temporal and masseter muscles. J Prosthet Dent. 1983;49:816.
39 Youdelis RA, Mann WVJr. The prevalence and possible role of nonworking contacts in periodontal disease. Periodontics. 1965;3:219.
