CHAPTER 76 Biomechanics, Treatment Planning, and Prosthetic Considerations
Clinical research has demonstrated excellent long-term success rates for implant-supported restorations in fully and partially edentulous patients. The replacement of missing teeth with an implant-retained prosthesis restores function and esthetics, improves confidence and self-esteem, and enhances quality of life. However, it is important to recognize that implant success is achieved by following sound principles. Good treatment planning is essential for predictability. Perhaps, the most critical factor to be considered in the planning is the control and distribution of stress for preservation of the “biologic” connection between the implants and bone. The quantity and quality of bone available to support implants play an important role in stress distribution,2 maintenance of bone apposition, and support under functional loading.
This chapter discusses important biomechanical considerations and treatment-planning guidelines for the use of dental implants in fully edentulous, partially edentulous, and single-tooth cases. Occlusal design, cantilevers, and connecting implants to teeth are addressed as well.
Biomechanical Considerations
Osseointegrated dental implants provide a predictable means of replacing missing teeth and restoring dental function. It is now clear that a thorough understanding of implant biomechanics is essential if implant-retained restorations are to be employed predictably. The load-bearing capacity of implants supporting the restoration must be greater than the anticipated loads during function. If applied loads exceed load-bearing capacity, it may lead to mechanical and/or biologic failure. In the case of mechanical failure, screws that secure the restoration may bend, loosen, or fracture. The most devastating type of mechanical failure is fracture of the implant. In the case of biologic failure, a resorption-remodeling response of the bone around the implant(s) is provoked, leading to progressive bone loss.10,18 In some cases, bone loss around the implant progresses until the implant is no longer supported and osseointegration is lost.
The function and support of implant-retained restorations is quite different from tooth-retained restorations. Teeth are suspended within the supporting alveolar bone by a periodontal ligament, which allows slight physiologic “movement” of teeth in function. If forces are excessive, teeth have the capacity to adjust or move in response to the applied forces. In the absence of inflammatory periodontal disease, teeth will adapt to these forces without appreciable bone loss. Orthodontic movement of teeth through alveolar bone is the ultimate example of the capacity of teeth to adapt to excessive applied forces. As orthodontic forces move a tooth, bone resorbs in response to pressure and forms in response to tension applied by the “attached” periodontal ligament fibers. Osseointegrated dental implants, by definition, are in direct contact with the alveolar bone without intervening soft tissues; there is no periodontal ligament and should movement occur, it would indicate a loss of osseointegration (e.g., fibrous encapsulation).9 Excessive forces are destructive. Thus it is crucial to have a good understanding of the biomechanical properties and the limitations of dental implants to ensure proper treatment planning that will sustain the anticipated occlusal forces.
Load-Bearing Capacity
The load-bearing capacity of implants is influenced by several factors, including the number and size of implants, the arrangement and angulation of implant positions, and the quality of the bone-to-implant interface (Box 76-1). The bone appositional index (percentage of bone-to-implant contact) may be the most important factor to consider when evaluating the load-bearing capacity of any given implant(s). Less bone density and lower bone-to-implant contact provide less support and resistance to occlusal loading. As an example, consider the bone support of implants in the posterior maxilla; the bone quality is particularly poor as compared with the anterior mandible. The trabecular bone is less dense and the cortical bone layer is thin in the posterior maxilla. As a result, the bone appositional index in the posterior maxilla is significantly less than what can be achieved in the anterior mandible, where the trabecular bone is typically dense with a thick cortical bone layer. The bone appositional index for implants in the posterior maxilla typically ranges from 30% to 60%, whereas the bone appositional index for implants placed in the anterior mandible typically ranges from 65% to 90% (Figure 76-1).

Figure 76-1 Bone quality influences the load-bearing capacity. In these histologic images obtained with light microscopy, note the difference in bone appositional index achieved in A, sparse “poor-quality” bone, often found in the posterior maxilla, versus B, dense bone, typical of the anterior mandible.
Technologic advances in surface modification (as compared to the original machined Brånemark surface) may enhance bone apposition and support for implants placed in poor quality/quantity bone, thereby gaining anchorage and improving the biomechanics.4,24,25,42 These “rougher” implant surfaces appear to have a significant effect on bone anchorage.24,25,34 Surfaces with an altered microtopography achieve higher bone appositional indices than the machined surfaces and appear to facilitate the biologic processes of bone formation, resulting in greater deposition of bone onto the surface of the implant. In addition, bone deposited on the surface of acid-etched implants appears to be harder and denser and may be more resistant to resorptive remodeling.40
A lack of bone height limits the amount of available bone for placement of long implants and reduces the potential for bone-to-implant contact. In the posterior mandible the inferior alveolar nerve and vessels travel through the body of the mandible until exiting the mental foramen in the premolar region (see Chapter 53). The height of bone available for placement of implants in the posterior mandible is determined by the location of the neurovascular bundle and the resorption of the alveolar ridge. Lateral nerve repositioning is possible but has a moderately high morbidity rate and is not advised. In the posterior maxilla, pneumatization of the maxillary sinus combined with loss of alveolar bone results in a decreased total height of available bone in the posterior maxilla, which limits the length of implants that can be used. Sinus floor elevation and bone augmentation procedures have enabled clinicians to increase the height of bone available in the posterior maxilla, allowing for the placement of longer implants with improved success. Vertical ridge augmentation is challenging and less predictable for all sites.
Historically, the use of longer (>7 mm) implants has been advocated as the result of reported higher rates of failure for shorter (≤7 mm) implants.17,20,29,39 Logic suggests that biomechanical stress around “short” implants leads to greater bone loss and a higher rate of implant failure. On the other hand, Pierrisnard37 showed that the maximum implant stress increased somewhat with implant length and bicortical anchorage, encouraging use of short implants in selected cases. He also states that the low anchorage stiffness of short implant might reduce the mechanical stress to the implant because of the flexibility of the bone. Using the finite element analysis (FEA), Pierrisnard and colleagues36 showed that greater implant length did not positively affect the way stresses were transferred to the implant but found that increasing implant diameter reduced the intensity of stress along the length of the implant. Iplikcioglu and Akca19 using the same method observed that wider implants rather than longer implants registered lower stress value to the whole system, suggesting that the use of short, wide implants could increase the load-bearing capacity of implants and implant prosthesis. Baggi and colleagues also used FEA to show that increases in implant width reduced stress more than increases in length5 (Box 76-2).
BOX 76-2 Finite Element Analysis
Finite element analysis (FEA) is a computerized investigative method that uses a mathematic model to assess stress in various objects and their surroundings when subjected to forces. It is useful in generating a hypothesis and testing basic biomechanical mechanisms but cannot be relied on for definitive answers. Only hard clinical evidence is undisputed and any assumption or predictions that are made by FEA needs to be validated clinically.
Angulation and Arrangement
The angulation and arrangement of implants used to retain and support a prosthesis influence the load-bearing capacity of the system (i.e., implants, components, prosthesis, and supporting bone).
In the 1980s, conventional dogma stated that once an implant became “osseointegrated,” it did not matter whether occlusal loads were applied axially. However, as more clinical follow-up and animal research data became available, the adverse effect of nonaxial loads on implants became increasingly more apparent. The angulation of implants in relation to the plane of occlusion and the direction of the occlusal load is an important factor in optimizing the transfer of occlusal forces to implants and surrounding bone. Axial loads are tolerated well. Minor discrepancies in angulation are probably not clinically significant, but if loads are applied at an angle of 20 degrees or more to the long axis of the implant, load magnification can result, provoking a resorptive remodeling response of the adjacent bone.
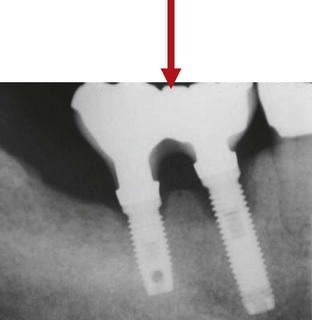
Nonaxial loads lead to implant overload through load magnification at the bone-to-implant interface, which in turn precipitates a resorptive remodeling response of the bone around the neck of the implants. This concept is supported by numerous finite element analysis (FEA) studies, which clearly demonstrate that nonaxial forces significantly increase the stress concentration to the cortical bone around the neck of the implant (Figure 76-2).3,11,33,44
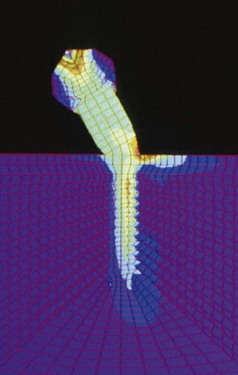
Figure 76-2 Nonaxial loads result in load magnification. Using finite element analysis, Cho and co-workers demonstrated that nonaxial loads concentrated stresses around the neck of the implant.
(Courtesy Dr. In Ho Cho.)
When excessive loads persist, bone loss continues and may progress to implant failure. Brunski et al10 proposed that excessive occlusal loads lead to microdamage (fractures, cracks, delamination) of the bone adjacent to the implant, which provokes a resorptive remodeling response. The bone remodeling at the implant surface results in less bone density adjacent to the implant, especially around the coronal aspect of the implant. This bone has a poor capacity for repair that is the result in part to the absence of a periodontal ligament fiber attachment (i.e., no bone-forming tension exists). Thus a vicious cycle ensues in which continued excessive loading leads to more microdamage and progressive bone loss until the implant fails (Box 76-3).
When implants are arranged in a linear fashion, the biomechanics with respect to anticipated bone response are quite unfavorable compared with a configuration in which the implants are arranged in a nonlinear (curvilinear or staggered) fashion. Arranging implants in a nonlinear configuration creates a more stable base that is more resistant to the torquing forces created by off-center contacts and lateral loads (Figure 76-3).
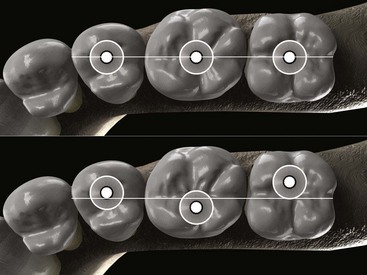
Figure 76-3 Placement of implants in a linear arrangement for a short-span, unilateral posterior restoration allows lateral forces to induce adverse bending of the implants leading eventually to bone loss and implant failure. If the implants are placed in a nonlinear “staggered” or “tripod” arrangement, lateral forces will be greatly diminished, and with a good occlusal scheme, will be counteracted by more favorable axial forces.
Short-span, linear implant configurations in the posterior segments are particularly prone to bone loss when loads are not applied axially. Bone loss in posterior areas can be more damaging because implants in these areas are primarily supported by the cortical bone around the most coronal aspect of the implant. In the posterior maxilla, the cortical bone can be very thin, and unless the implant is positioned to engage the superior cortical bone (floor of maxillary sinus), the apical aspect of the implant is usually poorly supported by loose trabecular bone. The load-bearing capacity is poor, and nonaxial loads can be very destructive.
Therefore every attempt should be made to position posterior implants with the long axis directed toward the opposing stamp cusp and aligned perpendicular to the occlusal plane. Then, occlusal forces can be directed down the long axis of the implant, which is tolerated far better than nonaxial forces. The restoration is also simpler and more cost effective to fabricate, since angled or custom abutments are not required.
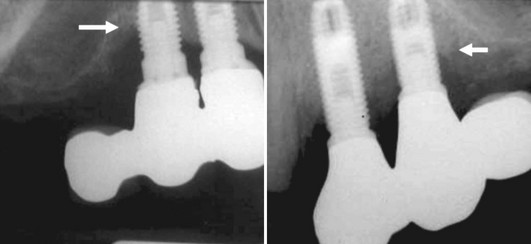
Before the widespread use of bone augmentation procedures in the posterior maxilla (i.e., sinus augmentation), many implants were positioned with excessive buccal angulations or were restored with buccal cantilevers. Similarly, distal cantilevered pontics were used to replaced missing maxillary posterior teeth. Implant-supported restorations with a cantilevered pontic transfer nonaxial occlusal forces to the adjacent implant and surrounding bone resulting in bone loss. Occlusal forces directed to the pontic created torquing forces around the implant adjacent to the cantilever. As a result, load magnification caused bone loss around the neck of the implant closest to the cantilever (Figure 76-4). Excessive distal angulations, which also created nonaxial loading and bone loss were also recognized problems. These implants often exhibit signs of overload (i.e., progressive and irreversible bone loss around neck of implant) when nonaxial occlusal loads are applied to the prosthesis (Figure 76-5).
Treatment Planning with Dental Implants
The success of implant-retained restorations is measured not only by successful osseointegration but also by the lack of problems associated them. Implant complications and failures have taught clinicians that the “engineering” of implant support for prosthetic appliances is an essential part of treatment planning and the key to success for implant-retained restorations (see Chapter 77 for a description of implant complications and failures). Treatment planning with dental implants in the edentulous or partially edentulous patient must carefully consider biomechanical issues to minimize failures and optimize success.
Edentulous Maxilla
Prosthetic options for the patient with an edentulous maxilla include a conventional complete denture, an implant-assisted denture or an implant-supported fixed prosthesis. For many patients, a conventional complete denture does not provide the comfort and quality of life that they desire. An implant-assisted or implant-supported prosthesis can provide stability comfort and restore confidence to the patient, especially in patients with one or more of the following conditions:

Figure 76-6 The hammer and anvil effect is a useful analogy for the clinician to keep in mind, evoking the combination syndrome, when treatment planning an edentulous maxilla opposing a partially dentate mandible. A, Illustration of an edentulous maxilla opposing a mandible that is missing posterior teeth. The lack of posterior occlusion leads to overclosure of the mandible and results in increased forces being applied to the anterior maxilla by the mandibular anterior natural dentition. B, Illustration of the hammer and anvil effect of combination syndrome.
The design of a maxillary implant-retained prosthesis is greatly influenced by the anatomy of the maxilla. Most notably, the maxillary sinus limits the height of bone available for implant placement in the posterior region. As a result, implant placement is confined to the anterior region, and the A-P spread that can be achieved is often limited (Figure 76-7). If the A-P spread is inadequate to provide support, a full-palatal-coverage overlay denture is recommended.
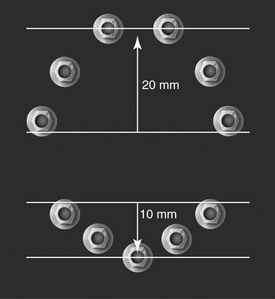
Figure 76-7 Diagram demonstrating the anterior-posterior (A-P) implant spread. It is defined as the distance from the middle of the most anterior implant to the distal edge of the most posterior implant.
Most patients are best served with an implant-assisted overlay denture. Lower cost, improved hygiene access, and predictable speech articulation are additional benefits that favor the use of an overlay denture in the edentulous maxilla over an implant-supported fixed prosthesis. The four-implant–assisted, palateless overlay denture ideally addresses the needs of most patients (Figure 76-8). Many patients who are edentulous in the maxilla have lost a significant amount of structure in the premaxillary region resulting in a lack of support for the upper lip. An implant-assisted maxillary overdenture is preferred over an implant-supported fixed prosthesis because the labial flange can provide the needed lip support. The usual resorption pattern of the alveolus places the gingival margin of a fixed restoration too far superiorly, too far palatally, or both. Even if the patient has a low enough smile line to hide the appearance of long crowns and deficient soft tissue height (Figure 76-9), a lack of lip support just beneath the nose can be unsightly with fixed prostheses.
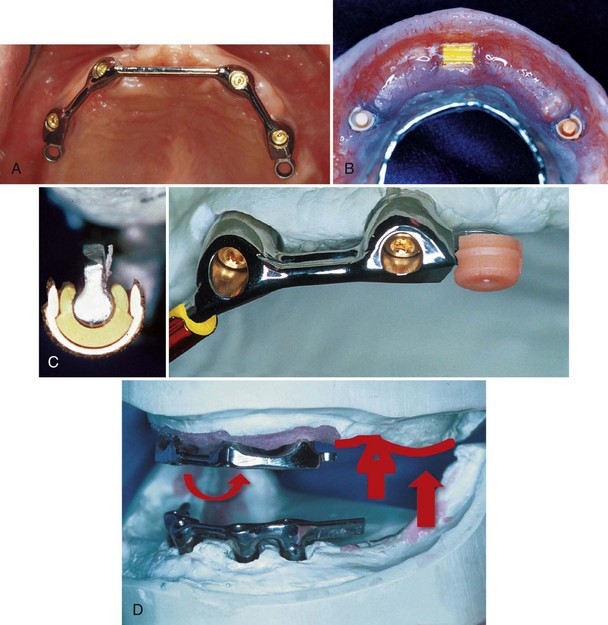
Figure 76-8 Implant-assisted overlay denture. A, Clinical photograph of four-implant bar in the maxilla designed to retain a palateless overlay denture. B, Photograph of clip and attachment design of palateless overlay denture. Anterior Hader clip attaches to anterior bar, and posterior extracoronal resilient attachments (ERAs) attach to female connectors at posterior ends of the bar. C, Cross-section of Hader bar clip attached to anterior bar (inset). View of overdenture bar with Hader clip (left) and ERA (right) attached. These plastic components will be embedded in the overdenture as in (B). D, Axis of rotation and function of resilient attachment. When posterior occlusal forces (solid vertical arrow) are applied, the denture rotates around the bar clip anteriorly (curved arrow), and resilient attachment (arrow) allows the denture to be compressed to primary denture-support areas posteriorly (open arrow).
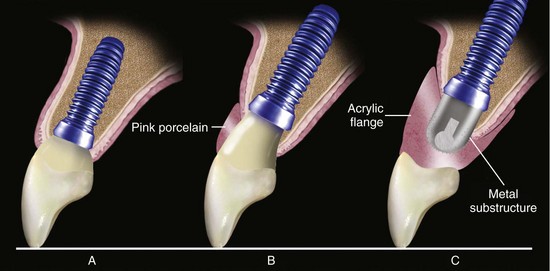
Figure 76-9 Three different scenarios of bone level dictating three different fixed restorations. Note that the incisal edge of all three restorations is at the same level, where ideally it should be, according to esthetics and phonetics. A, Bone resorption is minimal and no need to replace any soft tissue. A conventional implant-supported fixed partial denture is planned. B, Bone resorption is moderate, mainly vertical, and there is a need to replace soft tissue loss. To avoid the unesthetic look of a long porcelain restoration, the laboratory technician is asked to add some facial pink porcelain to mimic the lost soft tissue and reduce visually the length of the fixed partial denture giving the restoration a more acceptable look. C, Bone resorption is severe and it is vertical and horizontal. The soft tissue has followed, and there is a lack of support of the maxillary lip. The fixed restoration has to restore esthetics and function and of course the support of the lip; a fixed-removable (hybrid) prosthesis with a metal substructure and a buccal acrylic flange is the restoration planned in this case.
For those patients who prefer an implant-supported fixed prosthesis (and don’t require additional lip support), six or more implants arranged in an appropriate arc of curvature with at least 2 cm of A-P spread are required (see Figure 76-7). In this situation, the fixed prosthesis can be fabricated with distal extension cantilevers up to half the A-P spread provided it does not exceed 10 mm.
Edentulous Mandible
Similar to the edentulous maxilla, prosthetic options for patients with an edentulous mandible include a conventional complete denture, an implant-assisted denture or an implant-supported prosthesis. A mandibular complete denture is more problematic for patients than a maxillary complete denture, especially for patients with a severely resorbed (atrophic) mandibular ridge. The lack of stability and retention makes it very challenging for patients to control the denture. In this situation, the addition of implants offer unprecedented control (i.e., stability and retention) for a complete removable prosthesis. The two-implant–assisted overdenture is now the treatment of choice for patients with an atrophic, edentulous mandible.
Implant-assisted overlay dentures are designed so that most of the masticatory load is borne by the primary denture-support areas (i.e., retromolar pad, buccal shelf). A common practice is to place two implants in the anterior mandible with a connecting bar. One or two clips retain the denture to the bar (Figure 76-10). When occlusal forces are applied, the denture rotates around the bar (anterior axis of rotation) and depresses slightly in the posterior aspect, directing the forces to the primary denture-bearing areas (Figure 76-11). The implants provide stability and retention while bearing minimal stress from occlusal loads. Individual attachments secured to each implant offer a simple prosthetic alternative (Figure 76-12) to the bar and clip design. However, it is more critical for implants with individual attachments to be parallel to one another to facilitate a proper path of insertion and to minimize stress during prosthetic seating and function.
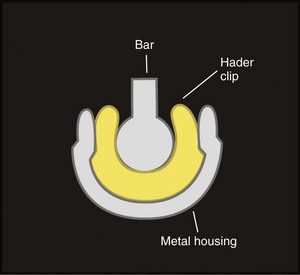
Figure 76-10 Cross-section of a Hader bar with clip. Note that the minimal height of the Hader bar is 2.5 mm and about 1.2 mm for the plastic clip and the metal housing. We should also allow room for acrylic for the retention of these components.

Figure 76-11 Implant-assisted overlay denture. A, Clinical view of overdenture in occlusion. B, Photograph of mandibular overlay denture (tissue-bearing surface) designed for an implant bar attached to two implants in the anterior mandible. Two Hader clips are embedded in the anterior acrylic. C, Clinical view of bar attached to two implants in the anterior mandible. D, Illustration demonstrating how axis of rotation allows denture to rotate around the bar. When the patient applies occlusal force posteriorly, the overlay denture rotates around the bar, and the load is absorbed by primary denture-bearing surfaces posteriorly.
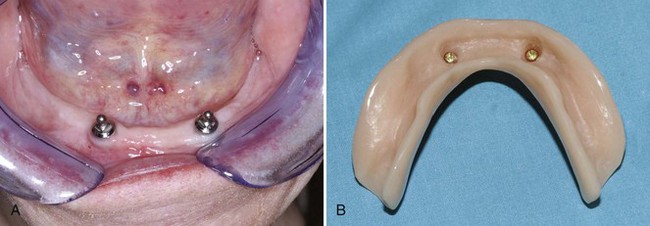
Figure 76-12 Individual attachments can be used on each implant to assist in retention of the mandibular overdenture. A, Clinical view of anterior mandible with individual ball attachments on two implants. B, Tissue-bearing surface of mandibular overdenture showing individual female attachments embedded in the denture.
(Courtesy Dr. Sal Esposito, Beachwood, OH.)
For those patients who prefer an implant-supported fixed prosthesis, four, five, or six implants arranged in an appropriate arc of curvature with at least 1 cm of A-P spread are required (see Figure 76-7). In this situation, the fixed prosthesis can be fabricated with distal extension cantilevers up to twice the A-P spread (Figure 76-13).
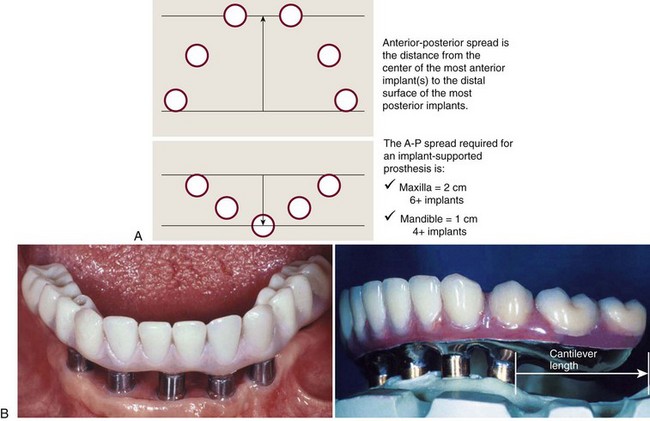
Figure 76-13 Cantilever length relative to A-P spread of implant distribution. A, Clinical view of an implant-supported restoration replacing mandibular teeth. Notice that the restoration is supported by five implants in the anterior and has cantilever extensions in the posterior segments. B, Study model view of similar mandibular implant-supported restoration with posterior cantilever extensions. Cantilever length, in the edentulous mandible, should not exceed twice the A-P spread.
Many patients prefer a fixed option for psychologic reasons, but the mastication efficiency provided by a fixed versus removable prosthesis does not appear to be significant.23 Evidence suggests that such fixed restorations tend to stop resorption of the body of the posterior mandible and in some cases enable regeneration of the bone in this region.26
Prosthetic options for patients who are partially edentulous (missing one to several teeth) include a conventional removable partial denture, a fixed partial denture (tooth-borne), or an implant-supported prosthesis.
Multiple Tooth Sites
Unilateral, implant-supported fixed partial dentures are predictable when they are supported by an adequate number of implants with good quality bone surrounding them. The lowest success rates for implants have consistently been reported for short-span (segmental) restorations in the posterior maxilla.21 Anatomic limitations can prevent placement of implants of adequate length in the posterior sextants. In the posterior maxilla, the maxillary sinus limits the lengths used, and in the mandible, the inferior alveolar nerve limits the lengths of the implants used. The bone-implant interface for osseointegrated implants in the posterior maxilla is compromised because the bone quality is poor. Anchorage for an implant placed in this region may be improved by engaging the cortical bone of the floor of the sinus, but there is generally minimal bone-implant interface along the course of the implant. Because many patients possess insufficient bone in the posterior maxilla to receive an implant of suitable length, bone augmentation of the alveolar ridge or maxillary sinus has been suggested.35,41 Vertical augmentation of the alveolar ridge has not been predictable, but the “sinus lift and graft procedure” appears predictable and has achieved wide acceptance22,43 (see Chapter 73).
The number of implants used will influence the load-bearing capacity. In the 1980s and early 1990s, many posterior quadrants of the maxilla were restored with one or two implants, and in some patients, two implants were used to support restorations with three or four dental units. In many cases, soon after loading, a distinct pattern of bone loss was observed that led to loss of the implants (see Figure 77-16). Additional implants significantly improve the biomechanics of these implant-supported fixed partial dentures.
Currently, it is imperative to “engineer” the treatment of unilateral, posterior segments with an implant used to support each missing tooth that will be restored. If space and available bone permits, it is desirable to use a minimum of three implants to replace three missing posterior teeth in the maxilla. The same rule (one implant for every missing tooth being restored) applies to replacing teeth with implants in the posterior mandible as well. However, greater bone density (i.e., thickness of cortical bone) in the posterior mandible sometimes permits the use of fewer implants. A three-unit bridge supported by two implants in the posterior mandible is widely accepted (Figure 76-14). However, the decision to restore three missing teeth supported by two implants should always be made with consideration for the quantity and quality of bone available to support the implants (i.e., effective load-bearing capacity of the implants).
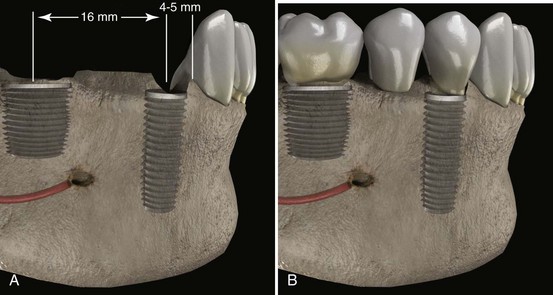
Figure 76-14 A, Placement of two implants in the mandible to replace three missing teeth. Note that the distance from the center of a standard implant (4-mm diameter) to the adjacent root is 4 to 5 mm, which accounts for the minimum of 1.5 distance between implant and root and the radius of the implant body. This distance is double if two implants are to be placed next to each other, making it 3 mm on each side if 3 implants were to be placed in a row. Following these recommendations, the necessary mesiodistal distance from the center of a wide body implant of 6 mm to the center of a standard implant of 4 mm that would replace 3 missing teeth is 15 to 16 mm. B, Restoration of the implants with an implant-supported three-unit fixed partial denture. Note that the spacing of the implants from center to center (15 to 16 mm) allowed a normal esthetically acceptable-size pontic.
Single Tooth Sites
Implants have been used successfully to replace missing single teeth despite the fact that the loading limit of a single implant remains unknown. Single tooth implant restorations have replaced the traditional three-unit bridge and gained acceptance and patient satisfaction.
Standard-diameter implants have been used to restore single-tooth defects in the posterior quadrants of the maxilla and mandible with mixed results. Solitary implants restoring maxillary molars have had unpredictable results, whereas single implants used to restore mandibular molars have had a better prognosis. In the 1980s, clinicians attempted to restore mandibular first molar sites with conventional implants 3.75 or 4.0 mm in diameter. Unfortunately, the results were quite disappointing. Occlusal overload led to bone loss and in some cases, fractured implants, especially for the 3.75 mm diameter implant.12
The most common problem observed, particularly when external hex-headed implants were used, was loosening of the screw retaining the restoration. This problem results because the diameter of the head of the implant is much smaller than the size of the occlusal surface. The buccolingual width of the crown can be minimized by narrowing the dimension of the restoration, but there is less control over the mesiodistal dimension because contacts need to be established and the space is most often filled. Consequently, a mesiodistal cantilever, albeit small, is created. Tipping of the restoration during function eventually leads to stretching and loosening of the screw that secures the crown to the implant fixture. If hex-headed implants are used, the use of wide-diameter implants greatly diminishes the screw-loosening complication (Figure 76-15). The larger platform reduces the potential for tipping forces to stretch or break the screw. Internal connection implants are far less susceptible to screw loosening.
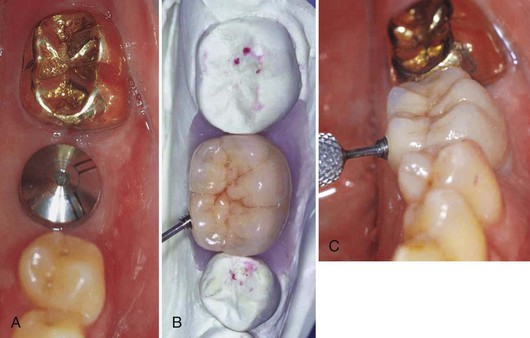
Figure 76-15 Single-tooth restoration in the posterior mandible supported by a wide-diameter implant. A, Clinical photograph of healing abutment on wide-diameter implant. B, Photograph of laboratory model with single molar. C, Clinical photograph of molar crown supported by wide-diameter implant. The use of wide-diameter (external hex) implants eliminates the problem of screw loosening for single-tooth, posterior, implant-supported crowns. NOTE: This crown is secured to the abutment via a lingual set screw (small hex driver seen attaching set screw).
If the first molar is lost and suitable abutments are present, a conventional three-unit, fixed partial denture is still a viable option, especially if the adjacent teeth already have large restorations. However, if adjacent teeth have small or no restorations, it is more conservative and preferable to replace the missing single tooth with an implant. This restoration is cost effective and predictable. In distal extension areas when restoring one molar tooth, two conventionally sized implants may be placed (with appropriate spacing) to improve biomechanical support (see Figure 69-9).
Single implants can be used with a high rate of success in the anterior and premolar areas. The bone-implant interface achieved in this area is good, and the size of the occlusal surface is generally small. Although similar considerations exist regarding screw loosening for single-implant restorations in the anterior and premolar regions, these concerns are less significant because of a more anterior position (lesser forces). Typically, there is better bone quantity and quality compared with more posterior sites.
Strategies to Avoid Implant Overload
Multiunit implant restorations should be splinted to maximize implant support (sharing the loads), and emergence profiles should be developed with open embrasure spaces to facilitate oral hygiene (Figure 76-16).
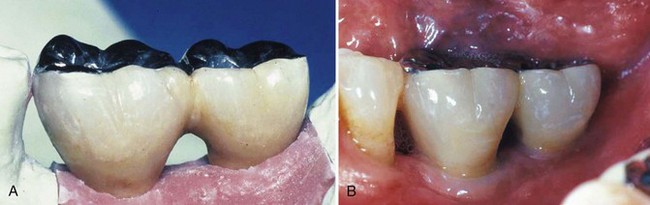
Figure 76-16 Guidelines for restoring posterior quadrants. Embrasures should be large enough for access with a proxy brush. The occlusal table must be narrow, cusp angles flattened, and proper emergence profiles developed. Anterior guidance should be restored with the natural dentition whenever possible. A, Laboratory model and, B, clinical photograph of two-unit, fixed partial denture supported by two implants in the posterior mandible demonstrate these qualities.
It is important to “engineer” implant-retained restorations well. In fact, some advocate “over engineering” to avoid failures. Implants should be adequate number, size and position to sustain the anticipated occlusal loads. Implants with smaller diameters have a lesser capacity to support bending forces than do implants with larger diameters. Implants with a minimum of 4 mm diameter should be used in areas expected to sustain greater occlusal loads (i.e., the posterior regions). Wider-diameter implants can be used when adequate bone and space exists (Figure 76-17). Thus, when the residual ridge and site permits, wide diameter implants should be used for molar replacement. Standard diameter (4 mm) implants may be best for premolar replacement since it approximates the premolar size and will provide a better emergence profile. In the case of multiple implant restorations, when ridge width permits, offsetting the implant location is encouraged.
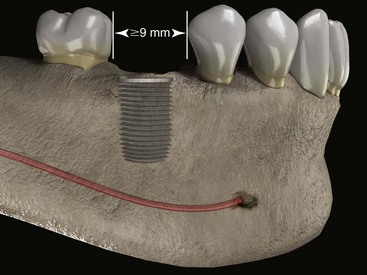
Figure 76-17 Placement of a wide platform implant 6 mm in diameter to replace a first mandibular molar. A minimum distance of 1.5 mm between the walls of the implant and the roots of the adjacent teeth on each side is to be considered, making 9 mm the minimum mesiodistal distance necessary.
Occlusal design for implant-supported prostheses is an essential and integral determinant of overall treatment planning.28,38 The risk of implant overload can be minimized by limiting the width of the occlusal table of the implant-supported fixed partial denture, flattening the cusp angles, avoiding the use of cantilevered restorations, and restoring the anterior guidance provided by the anterior dentition. Box 76-4 lists strategies to avoid implant overload.
The intensity and the vector of the force depend on several variables including the amount of bone contact (osseointegration), the quality and the quantity of the supporting bone and the implant surface characteristics. Regardless of the direction or the amount of this force, it always leads to micromotion at the bone-implant interface, which is translated into a transfer of stress to the adjacent bone. Splinting implant crowns together and placing longer and wider implants, as well as enhanced implant surface features, increase the bone-to-implant contact, or bone appositional index, and reduce stress forces, thereby increasing the load-bearing capacity of the implant(s).
The use of cantilevered implant-supported restorations (i.e., unilateral, linear configurations) in posterior quadrants of the mandible or maxilla is strongly discouraged and should be avoided. Cantilever extensions result in load magnification that can cause overloading of the implant next to the cantilever extension, which in turn may lead to progressive bone loss and implant failure (see Figure 76-4).
In general, it is advisable to keep implant-supported restorations separate from natural teeth because implants and teeth function differently and connecting them can lead to complications such as screw loosening and intrusion of natural dentition. Teeth have the capacity to move under functional occlusal loads while implants do not. Connecting implants to teeth may create a cantilever effect on the implant.8,27,30,31 Furthermore, designing the restoration so that it is independent of the natural dentition simplifies the biomechanics.
In contrast to this widely accepted view, a recent critical review of the literature suggests that these concerns may have been overstated.13 There are situations that may warrant connection of implants to teeth. Several authors have shown (animal and human research) that success is possible when specific guidelines are followed.* Specifically, if implants are to be connected to the natural dentition, it should be done in a rigid manner, either with screw-retained attachments or with copings secured by permanent cement. Tooth preparation should allow good retention, teeth should be periodontally healthy and stable, and the occlusal scheme should be good. Gulbransen15 showed that if implants are connected to the natural dentition with a rigid system of attachment, the implant failure and complication rates were dramatically reduced. It appears that the intrusion problem (and other complications) is increased when implants and natural teeth are connected with “nonrigid” and “semirigid” attachments. In addition, the well-documented phenomenon of intrusion of the natural tooth abutment associated with the use of semiprecision attachments is prevented.14
Conclusion
The importance of biomechanics and the limitations of implant systems were initially underestimated. It was believed that multiunit fixed bridges could be supported by as few as two implants, as it was done with the natural dentition. Over the years, clinical experience and research underscored the importance of biomechanics in the success and predictability of implant-retained prostheses. The rigid nature of implant-retained restorations and the lack of forgiveness in these systems demands a revised approach to treatment planning that is now applied. The biomechanics must be factored into the planning at the beginning of any implant treatment to achieve long-term, predictable success.
When clinicians follow a strategy that avoids implant overload and places an adequate number of implants in optimal positions, abutment selection is simplified, proper emergence profiles can be developed, space is available in interproximal areas for hygienic access and tissue health, the clinician has better control over the occlusal anatomy (narrowed occlusal table and flat cusp angles), and occlusal loads are better controlled.
![]() Science Transfer
Science Transfer
Excessive loading of implants can cause failure by loss of bone integration, fracture and loosening of retaining screws, and even fracture of the implant body. Many implant patients should wear protective occlusal splints to minimize nonfunctional forces. Implants should be as long as possible, and wider implants distribute loads better than narrow implants. Nonaxial forces should be avoided, particularly in posterior implants in which angulations greater than 20 degrees are often destructive.
The occlusal pattern on implant-supported crowns in partially edentulous cases should assure that the immobile implant is not prematurely loaded because natural teeth will be compressible during function. Centric contacts should be lighter on implants than on the adjacent teeth. Working and balancing contacts on implant crowns should be avoided and occlusal surfaces should be narrower than natural teeth to protect against forces transferred by the food bolus.
Sufficient implants should be in place. Most maxillary posterior cases should have one implant per missing tooth. In mandibular posterior cases with long implants in dense bone, two implants can be used to replace three teeth. Cantilevers should be reserved for use in anterior cases where they can assist in providing better soft tissue contours than two adjacent implants.
Fully edentulous maxillas are usually treated with four to six implants together with a removable prosthesis. This will provide lip support for good esthetics and prevent aberrations of speech and stop uncontrolled saliva leakage around crowns. Fully edentulous mandibular cases can be treated with two implants supporting a bar and clip-retained overdenture or four to five implants with a fixed bone-anchored bridge with posterior cantilevers not to exceed 20 mm.
1 Akagawa Y, Hosokawa R, Sato Y, et al. Comparison between freestanding and tooth-connected partially stabilized zirconia implants after two years’ function in monkeys: a clinical and histologic study. J Prosthet Dent. 1998;80:551-558.
2 Akca K, Fanuscu MI, Caputo AA. Effect of compromised cortical bone on implant load distribution. J Prosthodont. 2008;17:616-620.
3 Akca K, Iplikcioglu H. Evaluation of the effect of the residual bone angulation on implant-supported fixed prosthesis in mandibular posterior edentulism. Part II: 3-D finite element stress analysis. Implant Dent. 2001;10:238-245.
4 Avila G, Misch K, Galindo-Moreno P, et al. Implant surface treatment using biomimetic agents. Implant Dent. 2009;18:17-26.
5 Baggi L, Cappelloni I, Di Girolamo M, et al. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: a three-dimensional finite element analysis. J Prosthet Dent. 2008;100:422-431.
6 Biancu S, Ericsson I, Lindhe J. The periodontal ligament of teeth connected to osseointegrated implants. An experimental study in the beagle dog. J Clin Periodontol. 1995;22:362-370.
7 Block MS, Lirette D, Gardiner D, et al. Prospective evaluation of implants connected to teeth. Int J Oral Maxillofac Implants. 2002;17:473-487.
8 Bragger U, Aeschlimann S, Burgin W, et al. Biological and technical complications and failures with fixed partial dentures (FPD) on implants and teeth after four to five years of function. Clin Oral Implants Res. 2001;12:26-34.
9 Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1-132.
10 Brunski JB, Puleo DA, Nanci A. Biomaterials and biomechanics of oral and maxillofacial implants: current status and future developments. Int J Oral Maxillofac Implants. 2000;15:15-46.
11 Canay S, Hersek N, Akpinar I, Asik Z. Comparison of stress distribution around vertical and angled implants with finite-element analysis. Quintessence Int. 1996;27:591-598.
12 Eckert SE, Meraw SJ, Cal E, Ow RK. Analysis of incidence and associated factors with fractured implants: a retrospective study. Int J Oral Maxillofac Implants. 2000;15:662-667.
13 Greenstein G, Cavallaro J, Smith R, et al. Connecting teeth to implants: a critical review of the literature and presentation of practical guidelines. Compend Contin Educ Dent. 2009;30:440-453.
14 Gross M, Laufer BZ. Splinting osseointegrated implants and natural teeth in rehabilitation of partially edentulous patients. Part I: laboratory and clinical studies. J Oral Rehabil. 1997;24:863-870.
15 Gulbransen H: Personal Communication. In: Unpublished data 1995.
16 Gunne J, Astrand P, Lindh T, et al. Tooth-implant and implant supported fixed partial dentures: a 10-year report. Int J Prosthodont. 1999;12:216-221.
17 Hagi D, Deporter DA, Pilliar RM, et al. A targeted review of study outcomes with short (< or = 7 mm) endosseous dental implants placed in partially edentulous patients. J Periodontol. 2004;75:798-804.
18 Hoshaw S, Brunski J, Cochran C. Mechanical loading of Brånemark implants affects interfacial bone modeling and remodeling. Int J Oral Maxillofac Implants. 1994;9:345.
19 Iplikcioglu H, Akca K. Comparative evaluation of the effect of diameter, length and number of implants supporting three-unit fixed partial prostheses on stress distribution in the bone. J Dent. 2002;30:41-46.
20 Jemt T, Hager P. Early complete failures of fixed implant-supported prostheses in the edentulous maxilla: a 3-year analysis of 17 consecutive cluster failure patients. Clin Implant Dent Relat Res. 2006;8:77-86.
21 Jemt T, Lekholm U, Adell R. Osseointegrated implants in the treatment of partially edentulous patients: a preliminary study on 876 consecutively placed fixtures. Int J Oral Maxillofac Implants. 1989;4:211-217.
22 Jensen OT, Shulman LB, Block MS, et al. Report of the Sinus Consensus Conference of 1996. Int J Oral Maxillofac Implants. 1998;13(Suppl):11-45.
23 Kapur KK. Veterans Administration Cooperative Dental Implant Study–comparisons between fixed partial dentures supported by blade-vent implants and removable partial dentures. Part III: Comparisons of masticatory scores between two treatment modalities. J Prosthet Dent. 1991;65:272-283.
24 Kinni ME, Hokama SN, Caputo AA. Force transfer by osseointegration implant devices. Int J Oral Maxillofac Implants. 1987;2:11-14.
25 Klokkevold PR, Johnson P, Dadgostari S, et al. Early endosseous integration enhanced by dual acid etching of titanium: a torque removal study in the rabbit. Clin Oral Implants Res. 2001;12:350-357.
26 Klokkevold PR, Nishimura RD, Adachi M, et al. Osseointegration enhanced by chemical etching of the titanium surface. A torque removal study in the rabbit. Clin Oral Implants Res. 1997;8:442-447.
27 Lang NP, Pjetursson BE, Tan K, et al. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. II. Combined tooth–implant-supported FPDs. Clin Oral Implants Res. 2004;15:643-653.
28 Misch CE, Bidez MW. Implant-protected occlusion: a biomechanical rationale. Compendium. 1994;15:1330. 1332, 1334 passim; quiz 1344
29 Naert I, Koutsikakis G, Duyck J, et al. Biologic outcome of implant-supported restorations in the treatment of partial edentulism. part I: a longitudinal clinical evaluation. Clin Oral Implants Res. 2002;13:381-389.
30 Naert IE, Duyck JA, Hosny MM, et al. Freestanding and tooth-implant connected prostheses in the treatment of partially edentulous patients Part II: An up to 15-years radiographic evaluation. Clin Oral Implants Res. 2001;12:245-251.
31 Naert IE, Duyck JA, Hosny MM, et al. Freestanding and tooth-implant connected prostheses in the treatment of partially edentulous patients. Part I: An up to 15-years clinical evaluation. Clin Oral Implants Res. 2001;12:237-244.
32 Nickenig HJ, Schafer C, Spiekermann H. Survival and complication rates of combined tooth-implant-supported fixed partial dentures. Clin Oral Implants Res. 2006;17:506-511.
33 O’Mahony A, Bowles Q, Woolsey G, et al. Stress distribution in the single-unit osseointegrated dental implant: finite element analyses of axial and off-axial loading. Implant Dent. 2000;9:207-218.
34 Ogawa T, Nishimura I. Different bone integration profiles of turned and acid-etched implants associated with modulated expression of extracellular matrix genes. Int J Oral Maxillofac Implants. 2003;18:200-210.
35 Ogawa T, Ozawa S, Shih JH, et al. Biomechanical evaluation of osseous implants having different surface topographies in rats. J Dent Res. 2000;79:1857-1863.
36 Pierrisnard L, Augereau D, Barquins M. Analyse comparative par la method des elements finis des contraintes osseuses induites par des implants de geometrie variee. 2ieme partie: influence relative de la longueur et de l’orientation des implants. Implants. 2000;6:93-105.
37 Pierrisnard L, Renouard F, Renault P, et al. Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res. 2003;5:254-262.
38 Rangert B, Sennerby L, Meredith N, et al. Design, maintenance and biomechanical considerations in implant placement. Dent Update. 1997;24:416-420.
39 Snauwaert K, Duyck J, van Steenberghe D, Quirynen M, Naert I. Time dependent failure rate and marginal bone loss of implant supported prostheses: a 15-year follow-up study. Clin Oral Investig. 2000;4:13-20.
40 Takeuchi K, Saruwatari L, Nakamura HK, et al. Enhanced intrinsic biomechanical properties of osteoblastic mineralized tissue on roughened titanium surface. J Biomed Mater Res A. 2005;72:296-305.
41 Tolman DE. Reconstructive procedures with endosseous implants in grafted bone: a review of the literature. Int J Oral Maxillofac Implants. 1995;10:275-294.
42 Trisi P, Lazzara R, Rao W, Rebaudi A. Bone-implant contact and bone quality: evaluation of expected and actual bone contact on machined and osseotite implant surfaces. Int J Periodontics Restorative Dent. 2002;22:535-545.
43 Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003;8:328-343.
44 Watanabe F, Hata Y, Komatsu S, et al. Finite element analysis of the influence of implant inclination, loading position, and load direction on stress distribution. Odontology. 2003;91:31-36.