CHAPTER 77 Implant-Related Complications and Failures
Patients have experienced much success with endosseous dental implants.2,85 Yet, despite the long-term predictability and success of implants, complications do occur in a percentage of cases.3,25 Some complications are relatively minor and easy to correct, but others are more significant, resulting in loss of implants, failure of prostheses, and occasionally in severe loss of tissues in the area of implant failure. Complications may be surgical, biologic, mechanical, or esthetic.
Biologic complications are those that involve the periimplant supporting hard and soft tissues. Changes in the periimplant soft tissues may be minor, such as inflammation and proliferation, or more significant, involving progressive bone loss. The ultimate biologic complication is implant loss or failure, which may also result in soft and hard tissue defects. Biologic loss of implants may be caused by a lack of osseointegration in the early stages before restoration or by a loss of osseointegration as a result of bone loss after the restoration is installed and functioning.
Surgical complications are those problems or adverse outcomes that result from surgery, including procedures used for implant placement, implant exposure, and augmentation procedures. Complications arising from implant malposition are those resulting from an implant being placed in a nonideal position. Malpositioned implants, which usually are the result of poor presurgical treatment planning and/or surgical technique, can lead to an array of implant problems ranging in severity from minor to major. These complications include compromised esthetic and/or prosthetic results, soft tissue and bone dehiscences, impingement on anatomic structures, and possibly implant failure. Unfortunately, the extent of the problems that arise from implant malposition are often not recognized until the time of implant restoration.
Prosthetic or mechanical complications and failures typically occur in the form of material failure such as abutment and prosthetic screw loosening or fractures. The patient can recover from many of these mechanical problems if they are minor and recognized early. However, some complications, such as implant fractures, are not salvageable.
Esthetic complications arise when patient expectations are not met. Patient satisfaction with the esthetic outcome of the implant prosthesis will vary from patient to patient, depending on several factors. The risk for esthetic complications is increased for patients with high esthetic expectations and less-than-optimal patient-related factors (e.g., high smile line, thin gingival tissues, or inadequate bone quantity and quality).
This chapter reviews several of the more common implant-related complications. A summary of findings from the literature is presented to offer some insight into the prevalence of various types of implant-related complications. Implant failure, surgical complications related to site development, and different implant placement protocols are discussed as well.
Definition of Implant Survival and Implant Success
Implant success (or failure) is reported in many ways. Case reports, case series, retrospective studies, controlled studies, and prospective studies all report levels of success and failure as related to the population being evaluated. Each type of report or study has recognized limitations. However, recognizing the tremendous variation in the way individual investigators measure and interpret success may be more important. At times, outcomes are measured simply by the presence or absence of the implant(s) at the time of the last examination, which is only a measure of implant survival and should not be confused with implant success. In contrast to this simplified assessment, some investigators use detailed criteria to measure implant success and failure, with variations of successful outcomes separated and defined by additional criteria.
Implant survival is simply defined as any implant that remains in place at the time of evaluation, regardless of any untoward signs, symptoms, or history of problems. Clearly, there is a difference between implants that are present and functioning under an implant-retained restoration and implants that are present but not connected to any restoration and not providing support or function. These implants are sometimes referred to as “sleepers” and should not be considered successful merely because they are present and remain osseointegrated. Rather, sleeper implants should be included in the discussion as “surviving” but counted as “failures” because they failed to fulfill the originally intended treatment.
Implant success, on the other hand, is defined not only by the presence of the implant but also by criteria evaluating the condition and function of the implant at the time of examination. Criteria for implant success and failure have been defined over the years, but not all investigators use them. In the classic definition, Albrektsson et al6 defined implant success as an implant with no pain, no mobility, no radiolucent periimplant areas, and no more than 0.2 mm of bone loss annually following the first year of loading. Roos-Jansaker et al115 added to this definition by defining a successful implant as one that lost no more than 1 mm of bone during the first year in function. Sometimes these criteria are used as proposed, whereas at other times, they are used by investigators with modifications and new criteria. Consequently, it is inherently difficult to make comparisons between studies and often impossible to make absolute conclusions about any aspect of implant success or failure based on one or a few studies.
If one considers “success” using a strict definition as the outcome without any adverse effects or problems, then “implant success” should be defined as any implant-retained restoration in which (1) the original treatment plan is performed as intended without complications, (2) all implants that were placed remain stable and functioning without problems, (3) periimplant hard and soft tissues are healthy, and (4) both the patient and the treating clinician(s) are pleased with the results. When these strict criteria are used, implant success (i.e., absence of complications) is projected to be only about 61% after 5 years for implant-supported fixed partial dentures (FPDs) and 50% after 10 years for combined tooth/implant FPDs.83
An additional criteria of implant success that is often unreported but that must be considered is the “esthetic” success or patient satisfaction with the outcome. There have been a number proposed methods to evaluate esthetic results. A restorative index was proposed by Jensen et al72 to appraise the esthetics of the final restoration. The index uses a scale from 1 to 10 with 1 being an extremely poor result and 10 being a superlative esthetic result. The index, based on both subjective and objective criteria, evaluates the size and shape of the implant restoration in comparison to the equivalent contralateral tooth, blending into the arch, as well as the presence of the papillae, gingival form, color, and other factors considered essential in determining an esthetic result. The pink esthetic score (PES) is an index proposed by Furhauser et al55 that considers seven soft tissue parameters, including an evaluation of the color, contour, and texture of the surrounding soft tissues (papilla and facial mucosa). Each parameter is given a score of 0, 1, or 2, which allows the best score of 14 to determine the highest level of esthetics. Other indices were proposed for single-tooth implant restorations in the esthetic zone.19,89 The most recent, proposed by Belser et al,19 combines a modified PES index with a white esthetic score (WES) focusing on the visible part of the implant restoration scoring five parameters from general tooth form to hue, value, surface texture, and translucency. The maximum possible WES score is 10. These indices are aimed at quantifying the esthetic result, which could then present an objective method of judging “implant esthetic success.”
Types and Prevalence of Implant Complications
The prevalence of implant-related complications has been reported in several reviews. In a systematic review of reports on the survival and complication rates of implant-supported FPDs, Pjetursson et al83 found that the most common technical complication was fracture of veneers (13.2% after 5 years), followed by loss of the screw access hole restoration (8.2% after 5 years), abutment/occlusal screw loosening (5.8% after 5 years), and abutment/occlusal screw fracture (1.5% after 5 years; 2.5% after 10 years). Fracture of implants occurred infrequently (0.4% after 5 years; 1.8% after 10 years). A retrospective evaluation of 4937 implants by Eckert et al44 found that implant fractures occur more frequently in partially edentulous restorations (1.5%) than in restorations of completely edentulous arches (0.2%), and all observed implant fractures occurred with commercially pure 3.75-mm diameter threaded implants.
In a literature review that included all types of implant-retained prostheses, Goodacre et al59 found that the most common technical complications were loosening of the overdenture retentive mechanism (33%), resin veneer fracture with FPDs (22%), overdentures needing to be relined (19%), and overdenture clip/attachment fracture (16%). Their review, with the inclusion of edentulous patients having overdentures, seemed to indicate a significantly higher percentage of complications than Pjetursson’s systematic review107 of patients with implant-supported FPDs. Goodacre et al58 found it impossible to calculate an overall prosthesis complication rate because most studies included in their review did not report on several of the complication categories.
The most common complication reported for single crowns was abutment or prosthesis screw loosening. Abutment screw loosening varied dramatically from one study to another, ranging from 2% to 45%.59 The highest rate of abutment screw loosening was associated with single crowns, followed by overdentures. The rate of prosthesis screw loosening was similar, ranging from 1% to 38% in various studies. A higher frequency was reported for single crowns in the posterior areas (premolar and molar) than in the anterior region.
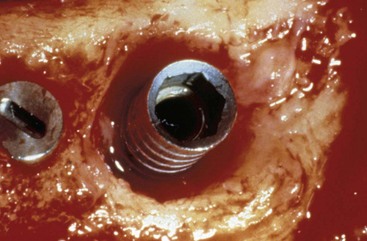
Implant fracture is an uncommon but significant complication. Goodacre et al58reported a 1.5% incidence in their literature review. The incidence of implant fracture was higher in FPDs supported by only two implants. Consistent with this finding, Rangert et al111 reported that most fractured implants occurred in single- and double-implant–supported restorations. They also indicated that most of these fractures were in posterior partially edentulous segments, in which the generated occlusal forces can be greater, as opposed to anterior segments (Figure 77-1).
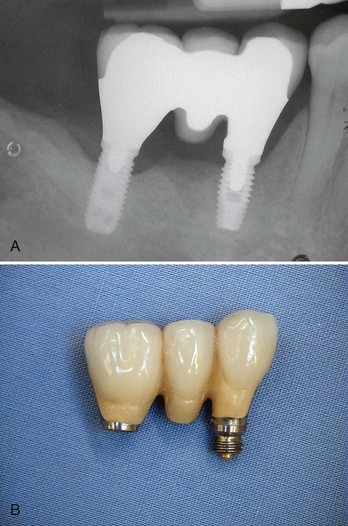
Figure 77-1 A, Radiograph of a three-unit, posterior, fixed partial denture (FPD) supported by two standard-diameter, screw-shaped threaded implants. Notice long crown height, relatively short implant length, and bone loss around posterior implant. B, Photograph of the ultimate implant-supported restoration failure. The anterior implant fractured between the second and third threads, which resulted in loss of the restoration.
In a systematic review of prospective longitudinal studies (minimum of 5 years) reporting both biologic and technical complications associated with implant therapy (all restoration types included), Berglundh et al20 found that the incidence of technical complications was consistent with Pjetursson’s findings, with implant fracture occurring in less than 1% (0.08% to 0.74%) of cases. Interestingly, consistent with the findings in Goodacre’s review, technical complications were higher for implants used in overdenture therapy than implants supporting fixed prostheses.
In Pjetursson’s systematic review83 of survival and complication rates for implant-supported FPDs, biologic complications, such as periimplantitis and soft tissue lesions, occurred in 8.6% of implant-supported FPDs after 5 years. However, in a more recent literature review of the prevalence of periimplant diseases, Zitzmann and Berglundh144 reported that although cross-sectional studies are rare, data from the only 2 studies available showed that periimplant mucositis occurred in 80% of the subjects and 50% of implant sites. Periimplantitis on the other hand was identified in 28% and ≥56% of subjects and in 12% and 43% of implant sites in the two studies that followed subjects with implants in function at least 5 years. A critical review of the literature by Esposito et al51 included 73 publications reporting early and late failures of Brånemark implants; biologically-related implant failures were relatively low at 7.7%. The treatments involved all anatomic areas and all types of prosthetic design. The authors concluded that the predictability of implant treatment was especially good for partially edentulous patients compared with totally edentulous patients, with failures in the latter population being twice as high. Also, the incidence of implant failure was three times higher for the edentulous maxilla than for the edentulous mandible, whereas failure rates for the partially edentulous maxilla were similar to those for the partially edentulous mandible.
Risk factors, such as smoking, diabetes, and periodontal disease, may contribute to implant failure and complications. Several studies with numerous implants and years of follow-up have concluded that smoking is a definite risk factor for implant survival.11,41,42,46,97 A systematic review of the effect of risk factors on implant outcomes concluded that smoking has an adverse affect on implant survival and success, with the effects being more pronounced in areas of loose trabecular bone (i.e., posterior maxilla).81 The review suggested that type 2 diabetes may have an adverse effect on implant survival rates but did not have enough studies to permit a definitive conclusion.81 Finally, the same review also concluded that while patients with a history of treated periodontitis did not show any decrease in implant survival, they did experience more implant complications and lower success rates.81
Different Types of Dental Implants
When analyzing the data concerning prevalence of implant complications (i.e., failure, fracture, periimplantitis, etc) in the published systematic reviews, the reader should be cognizant of the fact that many of the studies reviewed for these complications reported on implants with previous designs (i.e., machined surfaces and external connections). Currently, nearly all implant systems feature surfaces with an altered microtopography (rough) and many have internal connections. As a result, the prevalence and type of complications associated with these newer implant designs may be different.
Many modifications have been developed to try to improve the long-term success rates of implants. More than 1300 types of dental implants are now available, in different materials, shapes, sizes, lengths, and with different surface characteristics or coatings. There is limited evidence to show that implants with relatively smooth surfaces (i.e., machined) are less prone to bone loss from chronic infection (periimplantitis) than implants with rougher surfaces. On the other hand, implants with a turned (smoother) surface might be at greater risk to fail early than implants with roughened surfaces since the bone-to-implant contact is comparatively less. To date, there is no evidence showing that any particular type of dental implant has superior long-term success.48
Different implant designs and surfaces must be studied in prospective human trials over long periods of time. At present, these data are not available, and the clinician should be aware that the data we currently have, even on rates of implant failure, may not reflect the outcome for implants being used today. Moreover, new implant surfaces and designs are continually being introduced with even less data available on potential complications.*
Surgical Complications
As with any surgical procedure, there are risks involved with implant surgery. Proper precautions must be taken to prevent the risk of injury resulting from surgical procedures, including but not limited to (1) a thorough review of the patient’s past medical history, (2) a comprehensive clinical and radiographic examination, and (3) good surgical techniques. Surgical complications include perilous bleeding, damage to adjacent teeth, injury to nerves, and iatrogenic jaw fracture. Postoperative complications include bleeding, hematoma, and infection. They may be minor, transient, and easily managed or more serious and require postoperative treatment.
Hemorrhage and Hematoma
Bleeding during surgery is expected and usually easily controlled. However, if a sizable vessel is incised or otherwise injured during surgery, the hemorrhage can be difficult to control. Smaller vessels will naturally constrict or retract to slow the hemorrhage. If bleeding continues, it may be necessary to apply pressure or to suture the hemorrhaging vessel. This can be especially difficult if there is a vascular injury to an artery that is inaccessible such as in the floor of the mouth or posterior maxilla. Serious bleeding from an inaccessible vessel can be life threatening, not by exsanguination but rather as a result of airway obstruction. This is most problematic when the point of bleeding is inaccessible and internal (within the connective tissues and soft tissue spaces).
Postoperative bleeding is an equally important problem to manage (Figure 77-2). Patients should be given postoperative instructions on normal expectations for bleeding and how to prevent and manage minor bleeding. Historically, standard practice has recommended that they should be advised, with their physician’s approval, to discontinue or reduce medications that increase bleeding tendency 7 to 10 days before surgery. However, recent evidence suggests that this may not be necessary and may increase the risk of hematologic or cardiovascular problems73,74,97,116 (see Chapter 37). Dental health care providers should consult with medical health care providers regarding the best management for each individual patient. Furthermore, dental health care providers and patients should always include the treating medical practitioner in the management decisions if postoperative bleeding is excessive or persistent. Submucosal or subdermal hemorrhage into the connective tissues and soft tissue spaces can result in hematoma formation. Postoperative bruising is a typical example of minor submucosal or subdermal bleeding into the connective tissues (Figure 77-3). Bruising and small hematomas typically resolve without special treatment or consequence. However, larger hematomas or those that occur in medically compromised individuals are susceptible to infection as a result of the noncirculating blood that sits in the space. Thus it is prudent to prescribe antibiotics for patients who develop a noticeably large hematoma.

Figure 77-2 Clinical photograph of postoperative bleeding around healing abutments after second-stage implant exposure surgery.

Figure 77-3 Clinical photograph of postoperative (extraoral) bruising indicative of subdermal bleeding into connective tissues spaces. This is a normal expectation that resolves within 7 to 14 days.
Although the incidence of a life-threatening hemorrhage from implant surgery is extremely low, the seriousness of the problem warrants the attention of everyone who participates in this type of surgery. Potentially fatal complications have been reported for implant surgical procedures in the mandible (especially the anterior region).* Massive internal bleeding in the highly vascular region of the floor of the mouth can result from instrumentation or implants that perforate the lingual cortical plate and sever or injure the arteries running along the lingual surface. Depending on the severity and location of the injury, bleeding may be apparent immediately or only after some delay. In either case, the progressively increasing hematoma dissects and expands to displace the tongue and soft tissues of the floor of the mouth, ultimately leading to upper airway obstruction. Emergency treatment includes airway management (primary importance) and surgical intervention to isolate and stop the bleeding. Clinicians must be aware of this risk and must be prepared to act quickly. It is important to recognize that bleeding, although considered a complication at the time of surgery, may be a serious complication in the hours and days after surgery.38
Neurosensory Disturbances
One of the more problematic surgical complications is an injury to nerves. Neurosensory alterations caused by damage to a nerve may be temporary or permanent. Neuropathy can be caused by a drilling injury (cut, tear, or puncture of the nerve) or by implant compression or damage to the nerve (Figure 77-4; also see Figure 70-16). In either case, the injury produces neuroma formation, and two patterns of clinical neuropathy may follow. Hypoesthesia is a neuropathy defined by impaired sensory function that is sometimes associated with phantom pain. Hyperesthesia is a neuropathy defined by the presence of pain phenomena with minimal or no sensory impairment.61 Some neuropathies will resolve, whereas other will persist. The type of neuropathy is not indicative of the potential for recovery.
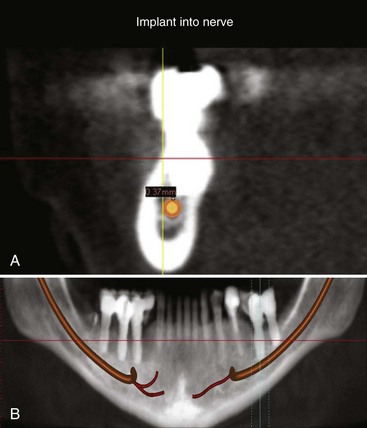
Figure 77-4 A, Cross-sectional image from computed tomography (CT) scan showing implant impinging on inferior alveolar nerve canal. B, Panoramic image of CT scan showing implant in lower left first molar area impinging on inferior alveolar nerve canal. Nerve is marked by tracing with software.
It is likely that neurosensory disturbances occur more frequently after implant surgery than currently reported in the literature for several reasons. First, many of these changes are transient in nature, and most patients recover completely or at least recover to a level that is below a threshold of annoyance or daily perception. Second, wide variation exists in the postoperative evaluation of patients by clinicians. Some clinicians do not examine or inquire about postsurgical neurosensory disturbances at all, thus allowing this complication to go unnoticed. Likewise, some patients may think that the altered sensation is part of the expected “side effect” of surgery and may never acknowledge or comment on its presence, especially if the disturbance is minor. Therefore it is likely that minor neuropathies exist but go unrecognized and unreported.
Neurosensory disturbances reported in the literature are most prevalent and significant when they are more serious and occur more frequently, such as those associated with lateral transposition of the mandibular nerve.71,78 This relatively uncommon procedure is used to reposition the nerve and allow longer implants to be placed in the atrophic posterior mandible. Lateral nerve transposition procedures are associated with almost 100% incidence of neurosensory dysfunction immediately after surgery. More than 50% of these neurosensory changes are permanent (ranging from 30% to 80%).78
Implant Malposition
Many of the aforementioned complications that arise during implant surgery can be attributed to the dental implant being placed in an undesired or unintended position. Malpositioning of dental implants is usually the result of poor treatment planning before the implant surgery, lack of surgical skill by the implant surgeon, and/or poor communication between implant surgeon and restorative dentist. Optimal implant esthetics and the avoidance of positional complications can be achieved by placing the implant in a prosthetically driven manner.90,102 In other words, the implant should be placed with reference to the three dimensions dictated by the position of the final restoration and not by the availability of bone. The angulation is another important determinant (fourth dimension) of implant position that will affect outcome esthetics. The ideal implant position entails an accurate preparation, insertion, and placement of the implant into the alveolus in a proper three-dimensional geometry according to apicocoronal, mesiodistal, and buccolingual parameters, as well as implant angulation relative to the final prosthetic restoration and gingival margins.82,117 (see Chapter 71).
Apicocoronally, the implant should be placed so the dental implant platform is 2 to 3 mm apical to the gingival margin of the anticipated restoration.24 The actual implant position varies slightly from one implant system to another, depending on abutment design and space requirements. If the implant platform is placed too coronal, there will not be sufficient room to develop a natural-looking emergence profile and the tooth may have a squarish, unesthetic contour. If the platform is placed at or above the level of the gingival margin, a metal collar or implant exposure can occur yielding an unesthetic result (Figure 77-5). Conversely, if the implant platform is placed too apically, a long transmucosal abutment will be necessary to restore the implant. This can lead to a deep pocket and difficult hygiene access for the patient and clinician.

Figure 77-5 Clinical photograph of gingival recession around a maxillary anterior implant (left central incisor) resulting in exposure of the crown margin, the implant collar, and several threads of the implant.
Mesiodistal implants should be placed at a distance of 1.5 to 2 mm from a natural tooth and 2 to 3 mm from an adjacent implant to maintain an adequate biologic dimension.62 Similar to natural teeth, violation of biologic width around an implant can lead to bone loss.67 Implants that are placed too close to each other (Figure 77-6) or natural teeth can be difficult to restore. Impression copings and impression-taking techniques must be modified. Improperly spaced implants invariably lead to chronic inflammation and periimplantitis.47,136 Conversely, implants placed with excessive distance from an adjacent tooth or implant may require prosthetic compensation in the form of mesial or distal cantilevers, which may predispose the implant to biologic (e.g., bone loss) and mechanical (e.g., screw loosening,59 screw fracture,133 or implant fracture111) complications, as well as difficulties with hygiene.136

Figure 77-6 Radiograph of two mandibular anterior implants placed too close together (no proximal space) resulting in implants that will be impossible to restore.
Ideally, implants should be placed, buccolingually so there is at least 2 mm of bone circumferentially around the implant.127 Implant exposure through the lingual or buccal cortex can predispose an individual to abscess and/or suppuration.32 Implants that are placed too far palatally/lingually require prosthetic compensation in the form of a buccal ridge lap, which may be difficult for the patient to clean and could lead to tissue inflammation.18
To obtain ideal esthetics, to avoid potential esthetic complications, and to correct bodily placement of the dental implant, the implant must be correctly angulated on insertion. In most anterior cases, it is desirable to have the implant long axis directed so it is emerging toward the cingulum. In the posterior region, the implant axis should be directed toward the central fossa or the stamp cusp of the opposing tooth. Implants that are placed with mild-to-moderate misangulations can often be corrected prosthetically with implant abutments. Minor misangulations (up to 15 or 20 degrees) can be corrected by with prefabricated stock-angled abutments; moderate misangulations (20 to 35 degrees) can usually be managed with customized UCLA-type abutments; extreme errors in implant angulations (more than 35 degrees) may deem an implant unrestorable and require it to be left submerged (i.e., sleeper) or to be removed (Figure 77-7).

Figure 77-7 Clinical photograph of maxillary anterior implant (left central incisor) placed with an extreme facial angulation resulting in an implant that emerges through the gingiva at a level that is more apical than the adjacent natural tooth gingival margins. A, Surgical exposure of malpositioned implant. B, Surgically removed implant. C, Alveolar defect resulting from surgical removal of malpositioned implant.
The ultimate complication of malposed implant(s) is implant or instrument invasion into vital structures. The most common violation of neighboring anatomy is the placement of the dental implant into the adjacent tooth root. Surgical procedures used to prepare osteotomy sites and place implants adjacent to teeth can injure the teeth either by directly cutting into the tooth structure or by damaging nearby supporting tissues and nerves. Instrumentation (e.g., drills) directed at or near the adjacent tooth may cause injury to the periodontal ligament, tooth structure, and nerve of the tooth. Depending on the extent of the injury, the tooth may require endodontic therapy or extraction. On insertion, dental implants will follow the trajectory of the osteotomy prepared by the surgical drills. Care must be taken when preparing the osteotomy to stay true to the planned path of insertion. Guidepin location radiographs taken during implant surgery can greatly reduce the potential for damaging adjacent teeth (see Figure 70-13). Radiographic analysis before implant surgery should include detection of curved, convergent, and/or dilacerated root structures of adjacent teeth that can limit implant placement.
Particular care must be taken when placing implants in the mandible so as to not encroach on the inferior alveolar canal or the mental foramen (see Chapter 53) for a description of this anatomy. Encroachment on the mandibular canal or mental foramen during osteotomy or implant placement via direct contact or mechanical compression of bone can result in injury to nerves and blood vessels. Paresthesia, hypoesthesia, hyperesthesia, dysesthesia, or anesthesia of the lower lip, skin, mucosa, and teeth may result, as well as arterial or venous bleeding.60 The incidence of sensory disturbances after mandibular implant placement has been reported to range from 0% to 17.5%.15
In the maxilla, care must be taken to avoid dental implant perforation into the maxillary sinus. Displacement of the entire dental implant into the maxillary sinus cavity may require a Caldwell-Luc procedure for retrieval. See online section on sinus augmentation for further information about complications related to the maxillary sinus.
The risks of surgery are always present, but the complications can be minimized with an understanding of the etiologies and with proper diagnosis and treatment planning. Three-dimensional imaging (e.g., computed tomography [CT] and cone-beam CT [CBCT] scans) provides the surgeon with useful presurgical information for proper diagnosis and treatment planning (see Chapter 70). Careful surgical exposure for direct visualization and identification of the mental nerve may be indicated as well. Once identified, it is recommended to establish a “zone of safety” and to keep instrumentation and implants a safe margin away from the nerve (e.g., ≥2 mm).60
Biologic Complications
Biologic complications involve pathology of the surrounding periimplant hard and soft tissues. Frequently, soft tissue problems are an inflammatory response to bacterial accumulation. The cause of bacterial accumulation around implants is key to understanding the problem. For example, bacteria may accumulate at the junction of an ill-fitting implant-abutment or abutment-crown connection. Some of the highly textured, macroscopically rough implant surfaces (e.g., titanium plasma-sprayed [TPS] or hydroxyapatite [HA] coated) may also perpetuate the accumulation of bacteria on the implant surface.
Inflammation and Proliferation
Inflammation in the periimplant soft tissues has been found to be similar to the inflammatory response in gingival and other periodontal tissues. Not surprisingly, the clinical appearance is similar as well. Inflamed periimplant tissues demonstrate the same erythema, edema, and swelling seen around teeth. Occasionally, however, the reaction of periimplant soft tissues to bacterial accumulation is profound, almost unusual, with a dramatic inflammatory proliferation (Figure 77-8). This type of lesion is somewhat characteristic around implants and is indicative of either a loose-fitting implant to abutment connection or trapped excess cement that remains buried within the soft tissue space or “pocket.” The precipitating local factor ultimately becomes infected with bacterial pathogens, leading to mucosal hypertrophy or proliferation and possible abscess formation (Figure 77-9). Correction of the precipitating factors (e.g., loose connection, retained cement) effectively resolves the lesion. Another type of lesion resulting from a loose abutment connection is the fistula (Figure 77-10). Again, correcting the etiologic factor quickly resolves the fistula.

Figure 77-8 Inflammatory proliferation caused by a loose-fitting connection between the abutment and the implant.
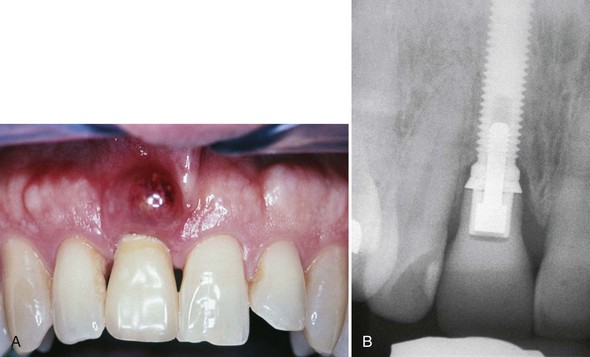
Figure 77-9 A, Clinical photograph of abscess caused by excess cement trapped within the soft tissues. B, Radiograph of implant with cemented crown (same patient as in A). Notice the subgingival depth of the crown-abutment (cement line) junction, which is below the level of the adjacent interproximal bone and therefore impossible to adequately access with explorer to remove excess cement.
Dehiscence and Recession
Dehiscence or recession of the periimplant soft tissues occurs when support for those tissues is lacking or has been lost. Recession is a common finding after implant restoration and should be anticipated especially when soft tissues are thin and not well supported (Figure 77-11). Improper implant positioning also predisposes periimplant tissues to recession. As noted earlier, placement or angulation of the implant too far to the buccal causes the buccal plate to resorb and has been shown to result in greater recession.126 Another factor to consider is the thickness of the buccal plate of bone. Spray et al127 recommended this thickness to be 2 mm or greater to support the buccal soft tissue. If this thickness is not present presurgical or simultaneous site development using guided bone regeneration is indicated. Recession is a problem that is particularly disconcerting in anterior esthetic areas. Patients with a high smile line or high esthetic demands consider such recession a failure (Figure 77-12).
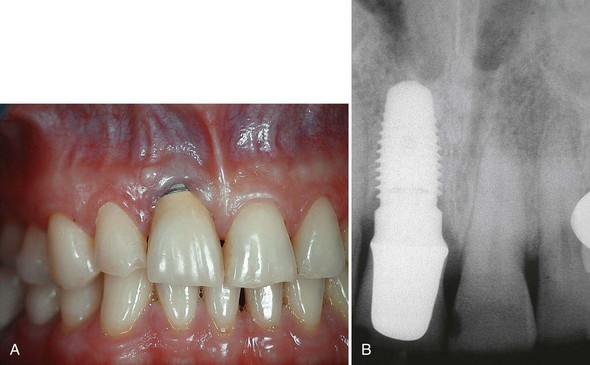
Figure 77-11 A, Clinical photograph of single-tooth implant crown (maxillary right central) with moderate recession that occurred 1 year after delivery of final restoration. Recession, in this case, most likely occurred because the labial bone around this wide-diameter implant was very thin or nonexistent. B, Radiograph of wide-diameter (6 mm) implant supporting maxillary central incisor crown (same patient as in A).

Figure 77-12 Poor esthetics resulting from gingival recession and exposure of crown margins, implant collars, and threads of several maxillary and mandibular implants supporting full-arch fixed partial dentures (FPDs). Notice the thin labial tissues and erythema (especially around mandibular implant sites).
The anatomy and soft tissue support around implants is different than that around teeth. Specifically, periodontal tissues have the distinct advantage of soft tissue support from circumferential and transeptal connective tissue fibers that insert into the cementum at a level that is more coronal than the supporting bone. In the absence of inflammation, these fibers support periodontal soft tissues far above the level of crestal bone. As a result, gingival margins and interdental papillae are supported and maintained around teeth even when the periodontal tissues are very thin. Periimplant soft tissues, on the other hand, are entirely dependent on the surrounding bone for support. Soft tissue thickness accounts for some soft tissue height, but there are no supracrestal inserting connective tissue fibers to aid in the soft tissue support around an implant. Therefore soft tissue height around implants typically does not exceed about 3 to 4 mm, and bone loss around implants often leads to recession.
Periimplantitis and Bone Loss
Periimplantitis is defined as an inflammatory process affecting the tissues around an osseointegrated implant in function, resulting in loss of supporting bone.94 To diagnose a compromised implant site, soft tissue measurements using manual or automated probes have been suggested. Although some reports state that probing is contraindicated, careful monitoring of probing depth over time seems useful in detecting changes of the periimplant tissue.35,110,129,130 Standardized radiographic techniques, with or without computerized analysis, have been well documented and found to be useful in evaluating periimplant bone levels.3,21,25,76,110 Together with periodic evaluation of tissue appearance, probing depth changes, and radiographic assessment as the best means of detecting changes in bone support. Clinicians should monitor the surrounding tissues for signs of periimplant disease by monitoring changes in probing depth and radiographic evidence of bone destruction, suppuration, calculus buildup, swelling, color changes, and bleeding.95,99 Periimplantitis may be perpetuated by bacterial infection that has contaminated a rough (e.g., TPS, HA-coated) implant surface and by excessive biomechanical forces.141,142 A classic trough-type defect is typically associated with periimplantitis (Figure 77-13). In cases with severely reduced bone support extending into the apical half of the implant (Figure 77-14) or in cases demonstrating mobility, implant removal should be considered.6,98 The number and distribution of implants and the occlusal relationships influence the biomechanical forces applied to implants109,112 (see Chapter 76). A recent review by Lindhe and Meyle from the Consensus Report of the Sixth European Workshop on Periodontology concluded that risk indicators for periimplantitis included (1) poor oral hygiene, (2) a history of periodontitis, (3) diabetes, (4) cigarette smoking, (5) alcohol consumption, and (6) implant surface.87 Most of these risk factors (1 to 4) have been recognized and reported in the literature.81 The report suggests that although data for the latter two risk factors (5 and 6) are limited, they appear to be relevant to periimplantitis.87
Implant Loss or Failure
Implant loss or failure is generally considered relative to the time of placement or restoration. Early implant failures occur before implant restoration. Late implant failures occur after the implant has been restored. When an implant fails before restoration, it probably did not achieve osseointegration, or the integration was weak or jeopardized by infection, movement, or impaired wound healing (Figure 77-15). Late implant failures occur after prosthesis installation for a variety of reasons, including infection and implant overload (Figure 77-16). In a review of the literature to evaluate biologic causes for implant failure, Esposito et al50 found that infections, impaired healing, and overload were the most important contributing factors.
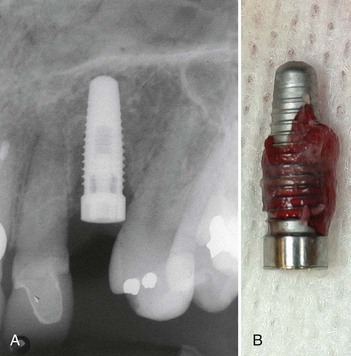
Figure 77-15 A, Radiograph of early failed implant caused by lack of osseointegration. In addition to the crestal bone loss, notice the radiolucency along the sides of the implant. B, Photograph of the failed (nonintegrated) implant (shown in A) that was easily removed along with surrounding connective tissue.
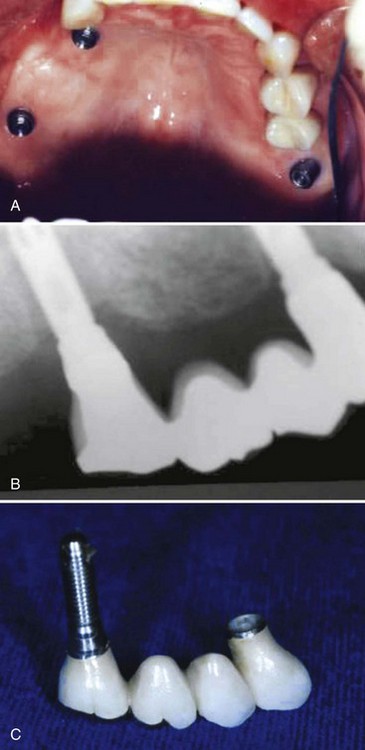
Figure 77-16 Four-unit fixed partial denture (FPD) in the posterior maxilla supported by only two implants. A, Clinical photograph of implant abutments in the posterior maxilla. B, Radiograph taken 30 months after restoration. Note the bone loss around the distal implant. C, Failed distal implant attached to failed prosthesis. The biologic failure of one (posterior) implant resulted in a long-span cantilever extension from the other (anterior) implant that ultimately led to its mechanical failure (i.e., abutment screw fracture).
(Courtesy Dr. John Beumer, UCLA Maxillofacial Prosthetics, Los Angeles, CA.)
Complications Related to Augmentation Procedures
A common problem encountered in implant dentistry is insufficient bone quantity to allow implant placement according to standard procedures. Deficiencies in alveolar bone result from developmental defects, periodontal disease, tooth loss, and trauma.8,28,121 For most cases with alveolar ridge resorption, bone regenerative procedures are required to correct the defects before or simultaneous with implant placement. The success of bone augmentation procedures has been assessed by experienced clinicians in several workshops.4,32,53,64,65 One systematic review of literature (the 2003 Workshop on Contemporary Science in Clinical Periodontics) found that survival rates of dental implants in augmented bone achieved a high level of predictability and showed that these rates were similar to implants placed in natural bone.53 However, a more-recent systematic review of the literature (the 2008 Consensus Report of the Sixth European Workshop on Periodontology) concluded that bone augmentation procedures can fail and that implants placed in these areas do not enjoy the high long-term survival rates of dental implants placed in pristine sites.137 The consensus emphasized that research is needed to answer questions concerning (1) long-term performance of dental implants placed in augmented bone, (2) the clinical performance of dental implants placed in augmented or pristine sites, and (3) the clinical benefits of bone augmentation with respect to alternative treatments.
The procedures most often used to regenerate bone include autogenous bone harvesting/grafting, guided bone regeneration, and sinus bone augmentation (see Chapters 72 and 73 for detailed descriptions of these procedures). The following is a brief review of the most common complications related to these three augmentation procedures.
Autogenous Bone Harvesting/Grafting
Autogenous bone from a histologic and biologic point of view has been considered the gold standard for osseous reconstruction. Bone block grafts of autogenous bone from extraoral and intraoral sources have been documented as a predictable procedure for reconstruction of defective or atrophic alveolar ridges.93 Complications can occur either at the donor or recipient sites. The most common extraoral donor sites include the ilium and tibia. Complications related to extraoral donor sites are beyond the scope of this chapter. The most common intraoral donor sites include the mandibular symphysis, mandibular ramus, and maxillary tuberosity. Although each donor area has specific associated complications, the most common complications of intraoral autogenous harvesting/grafting concern those from the mandibular symphysis.
The ramus donor site is associated with a much lower incidence of complications compared to the symphysis area.63,92 Potential complications associated with surgical harvesting of bone from the ramus include damage to the inferior alveolar nerve and trismus after surgery. Damage to the buccal nerve, although rare, has been reported as well. Surgical harvesting of bone from the mandibular symphysis region are associated with a higher incidence of altered neurosensory disturbances to the mandibular anterior teeth and soft tissues of the chin area. The incidence of mental nerve paresthesia after symphysis grafts has been reported to be as high as 43%.108 Many of these paresthesias are temporary.
In addition, fracture of the mandible has been reported after bone graft harvesting from the symphysis.34 Many of these complications can be avoided by proper surgical technique, good planning, and an experienced operator.
Recipient site complications include wound dehiscence, flap necrosis, graft exposure, graft contamination, infection, and problems with bone graft incorporation and resorption. Proper flap reflection, intimate fixation of the graft, and flap coverage without tension can avoid many of the potential postsurgical complications. Bone graft material including barrier membranes should be immobilized (fixated if possible). Provisional restorations should be adjusted to prevent pressure over grafted areas. Block grafts, as well as other augmentation procedures, require experience in handling hard and soft tissue, as well as a clinician who is prepared to recognize and treat complications should they arise.
Guided Bone Regeneration
Guided bone regeneration (GBR) is a procedure that utilizes a barrier membrane to isolate an area for bone growth. The technique has been well documented for horizontal (and limited vertical) ridge augmentation23,35,77 (see Chapter 72). The most common complication associated with GBR is premature exposure of the barrier membrane and necrosis of the overlying flap (Figure 77-17). Exposure rates of expandable polytetrafluoroethylene (ePTFE) membranes during various GBR procedures range from 41% when the technique was first introduced in the early 1990s for horizontal ridge augmentation23 to 12.5% when surgical techniques improved and clinician’s became more familiar with handling the material.124 Once exposed to the oral environment, the membrane becomes colonized with bacteria within 3 to 4 weeks and the potential for bone regeneration under the membrane is limited to an area that is at least 2 to 3 mm from the contaminated surface.17,125 Topical application of chlorhexidine to the exposed membrane has been advocated as a method of reducing the amount of bacteria, but it does not solve the problem and removal of the exposed membrane is necessary.

Figure 77-17 Clinical view of flap necrosis over area treated with guided bone regenerative procedure.
Other complications associated with GBR procedures include soft tissue or bone graft infection, failure to regenerate adequate bone volume and mucogingival problems, including loss of keratinized tissue and decrease in the vestibule.23 Most of these complications are related to insufficient soft tissue healing after tooth extraction, inadequate flap design, movement of the membrane and/or graft caused by transmucosal loading and improper provisionalization, flap suturing under tension, poor surgical technique, contamination of the membrane or surgical site, compromise of the vascular supply and flap advancement for graft coverage that reduces the keratinized tissue, and vestibular depth. To prevent complications associated with GBR procedures, proper surgical technique should be employed.
Sinus Bone Augmentation
Lateral Window Sinus Lift
The lateral window sinus lift and bone augmentation procedure has been well documented and reviewed in three published systematic reviews.4,40,139 Although survival rates of implants placed in sinus-grafted areas has been shown to be high (95%), there are intraoperative and postoperative complications associated with this procedure. The most common intraoperative complications include bleeding and perforation of the Schneiderian membrane. Bleeding usually occurs when the vascular supply to the lateral wall of the sinus is severed or damaged.45 In most cases, if the patient does not have an underlying bleeding problem and is not taking anticoagulants, the bleeding is usually minor and relatively easy to control with local measures. Perforation of the Schneiderian membrane, as reported in the literature, has an incidence that varies from 11%143 to 56%80 with most clinicians reporting an incidence of approximately 20% to 30%. Minor membrane perforations can be treated by reflection of the membrane that folds on itself, whereas medium-to-large membrane perforations require the use of an absorbable membrane placed over the perforation to “patch” the opening (Figure 77-18). Very large membrane tears may be too big to repair and require aborting the procedure. Careful surgical technique and the use of newer instruments (e.g., piezoelectric surgery) have been shown to significantly reduce this complication140 (see Chapter 75).
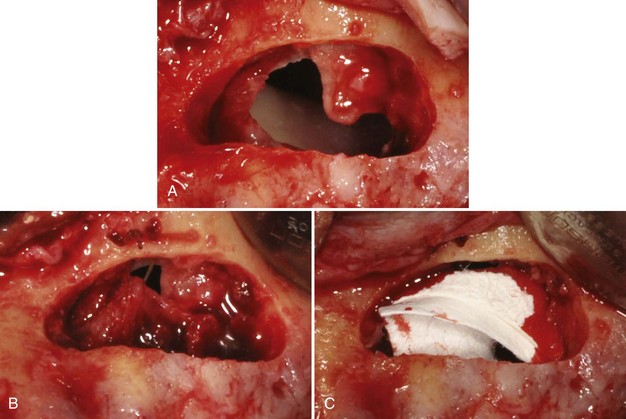
Figure 77-18 A, Large perforation of the Schneiderian membrane during a sinus elevation procedure. B, Attempts to close or reduce the size of the perforation with resorbable sutures. C, Use of resorbable barrier membranes to cover the perforation.
The most common, although infrequent, postsurgical complication associated with sinus bone augmentation is infection.14,80,93 The incidence of infection has been reported to vary from 2% to 5.6%. Careful surgical techniques, adherence to sterility, and the judicious use of antibiotics can minimize the risk of postoperative infections. Some infections resolve with antibiotic treatment alone, whereas others require surgical debridement of the infected area. Consultation or referral to a specialist may be indicated for persistent infections.
Crestal (Osteotome) Sinus Lift
Another method of sinus elevation and bone augmentation involves the use of osteotomes. This technique is indicated when there is enough native bone to stabilize the implant and a minimal need for sinus floor elevation. Bone is added through the crestal osteotomy by means of osteotomes and a mallet, the floor of the sinus is fractured, and the Schneiderian membrane lifted by the bone graft (see Chapter 73). This method is thought to be a relatively less invasive technique of great utility in certain patients. However, it has been associated with the complication of benign paroxysmal positional vertigo (BPPV),105 which has been described as a consequence of working the implant bed with osteotomes. During the osteotomy preparation and sinus floor elevation using the osteotome technique, the trauma induced by percussion with the surgical hammer, along with hyperextension of the neck during the operation, can displace otoliths in the inner ear and induce BPPV. It has been reported that 1.25% of the patients treated suffered vertigo when trying to sit up immediately after surgery and were diagnosed with BPPV. Because implant treatment is increasingly being carried out on older patients, and because of the widespread use of bone expansion technique with osteotomes, the incidence of BPPV can be expected to increase.106 In suspected cases of BPPV, the patient should be informed about the condition and then referred to an otoneurologic specialist to determine which semicircular canal is affected and to carry out the appropriate otolithic reinstatement maneuver.
To prevent this complication, care should be taken when using the osteotome technique. The application of manual force instead of hammer percussion and the use of a surgical fraise in combination with osteotomes can minimize the trauma to the craniofacial area, especially in older patients. Many alternative techniques for a crestal approach to sinus elevation and bone augmentation have been developed including the use of selective drill systems and piezoelectric surgical instruments that cut bone while leaving the Schneiderian membrane intact (see Chapters 73 and 75). These newer methods should be considered to avoid BPPV.
Complications Related to Placement and Loading Protocols
The traditional implant placement protocol required a healed edentulous ridge into which implants were placed and allowed to osseointegrate for a period of 3 to 6 months without occlusal loading (see Chapter 71). In contrast to these early standards, some current protocols advocate dramatically different approaches, including (1) implant placement immediately after tooth extraction, (2) implant loading immediately after placement, and (3) flapless implant placement surgery. Each of these approaches has distinct advantages but are also accompanied by specific risks of complications. The most common complications associated with these newer, developing protocols are discussed in this section.
Immediate Implant Placement
Immediate implant placement (IIP) is a protocol that places an implant in an extraction socket immediately after tooth removal and socket debridement. This procedure was originally described by Schulte et al122 and Lazzara84 and has been reported to have similar implant survival rates as implants placed into healed ridges30,88 with long-term survival rates of approximately 94%.138 The advantages of this protocol include fewer surgical procedures (and decreased morbidity), decreased time of treatment, decreased cost, and decreased soft tissue healing time by avoiding flap reflection and advancement.123 However, as with any surgical protocol, complications are possible and there are specific complications associated with IIP. These include implant failure, poor implant position, bone loss, recession of the periimplant marginal soft tissues, and compromised esthetic outcomes.
After tooth extraction, there may be a compromised socket as the result of pathology (periodontal, endodontal, or fracture) of the hopeless tooth. Proper implant position may be difficult to establish when the socket walls are missing or deficient. For example, the implant osteotomy for extracted maxillary anterior teeth should be made on the lingual incline of the lingual wall of the socket. Quite often the burs will “slip” buccally causing the osteotomy to be made too far to the buccal or at an undesired angulation. Careful use of a surgical stent, round bur, sharp initial bur, and side cutting burs can avoid slipping and improve the accuracy of implant site preparation (see Chapter 75). Although success rates of implants placed with an IIP are excellent, failure to attain primary stability in native bone apical or lateral to the socket may increase failure rates. Inability or lack of thorough debridement of an infected or compromised (e.g., tooth with an apicoectomy) socket may also increase the risks of failure.86 Buccal plate resorption and gingival margin recession postimplant placement may expose the implant surface following integration of the implant (see Figures 77-5 and 77-11). This may, in turn, compromise the esthetic results or necessitate hard and soft tissue augmentation procedures to improve the esthetic outcome.80 A recent published case series documented this problem for IIP postextraction without flap elevation.52 The risk of the previously mentioned complications may be decreased with proper case selection, proper procedures, and experience in using this protocol. Until the clinician has the knowledge and experience to use an IIP protocol, they should avoid using it in the esthetic zone.
Immediate Loading After Implant Placement
Brånemark established the concept and predictability of the osseointegrated dental implant based on a requirement for an unloaded healing period of 3 to 6 months.22 This original protocol purported that premature loading would cause micromotion of the dental implant leading to fibrous encapsulation and implant failure. However, several studies in the dental literature have shown that immediately loaded dental implants can have success rates similar to that of conventionally loaded dental implants.* Whether restoring a single tooth or a complete dentition, there are many advantages to early or immediate loading. It is critical to recognize that these advantages may come with increased risks for complications and failures. The most significant complications are failure to achieve primary stability and implant failure.
Studies have shown that using longer and wider implants can provide increased success rates when immediately loading the dental implant.119,120 In addition, the implants should be placed in a fashion that maximizes the anterior to posterior spread leading to a greater distribution of forces over a wider area and a reduction in cantilever forces. Studies have suggested that implants placed around the arch lead to what is known as cross-arch stabilization, which can decrease the individual force and motion experienced by any individual implant.114,131 For the fully edentulous case a minimum of 4 to 6 implants of adequate size, good stability, and properly spaced throughout the ridge is recommended to improve success with immediate load case.37 Mandibular cases may require fewer implants than maxillary cases because of greater bone density, especially in the interforaminal region. If the opposing arch is restored with a removable prosthesis, fewer implants may be needed to immediately support a restoration because of a decreased opposing occlusal force.
Other contributing factors associated with increased failure rates of immediately loaded implants include implant surface and implant design. Lower success rates with immediately loaded implants have been reported with smooth (i.e., turned/machined) surface implants, especially in cases of single tooth immediately loaded restorations.69,113,118 Studies have also suggested that the macrodesign features of an implant (e.g., threaded versus cylindrical) can affect initial stability and success rates in immediately loaded cases.29,79
Complications of immediately loaded implants can also arise from a poorly constructed or inserted restoration despite all things going well with the surgical placement. Extreme care must be taken to achieve a passive fit of restoration and to eliminate nonworking or balancing contacts on the restoration. In addition, in full arch cases that were immediately loaded, the restoration must be designed to withstand direct occlusal force. This can be accomplished via a rigid connection and splinting the implants together in cross-arch fashion. Loosening or unseating of the provisional restoration usually indicates mismanagement of occlusal forces and be an early predictor of failure.
Immediately loading dental implants is a technique that offers many advantages but can also increase the incidence of complications and failure. This technique should only be performed by an experienced operator that is prepared and informed. Controlling micromotion postloading is tantamount to success. Meticulous case selection, which incorporates cross-arch stabilization, controlling occlusal overload, minimizing cantilevers, and increasing the anterior-posterior distribution of implant placement, can significantly increase the success rates of loading dental implants immediately after placement.
Implant Placement using a Flapless Approach
Flapless implant surgery is the placement of a dental implant without the elevation of the epithelium, connective tissue, and periosteum covering the alveolar bone. Flapless surgery is performed by either drilling through soft tissue with the implant twist drills or by removing a small circular section of tissue (“punch” procedure) before the creation of the osteotomy.5 Flapless surgery has been shown to be successful and has many advantages because it is minimally invasive.26,27 The benefits of flapless surgery include a decrease in associated surgical morbidity, including postoperative pain, ecchymosis, and swelling, as well as a reduction in surgical time and intraoperative bleeding.105 Studies show that when a full-thickness mucoperiosteal flap is raised, there is loss of bone volume57 and a flapless approach results in less bone resorption. However, the lack of operator visualization of the alveolus when preparing osteotomies and placing implants may increase the potential for complications. The most common problems associated with flapless surgery are the loss of keratinized tissue when excising the crestal “circle” of soft tissue and improper positioning of the dental implant placed without direct vision. Improper positioning may result in a dehiscence/fenestration defect (Figure 77-19) or damage to adjacent vital structures.
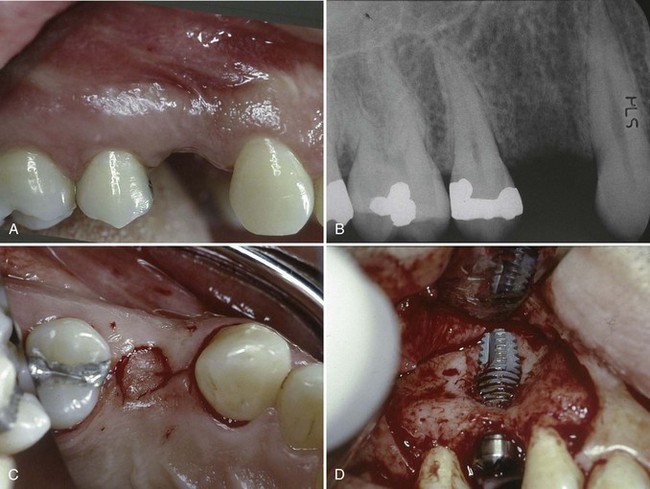
Figure 77-19 A, Preoperative clinical view of missing single tooth #5. There appears to be good alveolar ridge shape with adequate keratinized gingiva. B, Radiograph showing good bone height and mesial-distal space available for single tooth implant. C, Occlusal view of circular “punch” incision used to access bone and prepare implant osteotomy. D, Full flap reflection (after noticing suspicious protrusion in labial vestibule) revealed implant protruding out of alveolar bone on buccal surface.
Although flapless implant surgery has many beneficial features, it is a technique sensitive procedure that requires surgical experience, an accurate surgical guide and a knowledge of the anatomy surrounding the planned implant site.
Prosthetic or Mechanical Complications
Prosthetic or mechanical complications occur when the strength of materials is no longer able to resist the forces that are being applied. As materials fatigue, they begin to stretch and bend; ultimately, depending on the applied forces, they will fracture. Material failures, in turn, lead to prosthetic complications such as loose, broken, and failed restorations.
Screw Loosening and Fracture
Screw loosening has been reported to occur quite frequently in screw-retained FPDs. Screw-retained single crowns attached to externally hexed implants (i.e., those with narrow- or standard-diameter restorative interface connection surfaces) are particularly prone to this type of mechanical complication. Studies have reported screw loosening in 6% to 49% of cases at the first annual check-up.70,96 Screw loosening was a more prevalent problem with earlier designs. For example, abutment screws were previously made with titanium, which did not offer the clamping forces of current materials. Newer abutment designs and improved abutment screws allow for an increased clamping force to be achieved without excessive torque levels, which has helped to reduce the rate of screw loosening.
Abutment or prosthesis screw loosening is often corrected by retightening the screws. Over time, however, if screws continue to be stretched, they become fatigued and eventually fracture. This problem is evident in the patient with a loose single crown. However, in the patient with a prosthesis retained by multiple implants, the ability to detect a loose screw is greatly diminished and the problem may go unnoticed until additional screws stretch, fatigue, and fracture. In either case, the biomechanical support (and resistance) for the restoration must be evaluated and if possible, changed to prevent recurrence of the problem.
Implant Fracture
The ultimate mechanical failure is implant fracture because it results in loss of the implant and possibly the prosthesis (Figure 77-20). Furthermore, removal of a fractured implant creates a large osseous defect. Factors such as fatigue of implant materials (Figure 77-21) and weakness in prosthetic design or dimension are the usual causes of implant fractures.3,13 Balshi13 listed three categories of causes that may explain implant fractures: (1) design and material, (2) nonpassive fit of the prosthetic framework, and (3) physiologic or biomechanical overload. Patients with bruxism seem to be at higher risk for such events and therefore need to be screened, informed, and managed accordingly.12,13 These patients should be fitted with occlusal guards in conjunction with placement of the final prostheses.
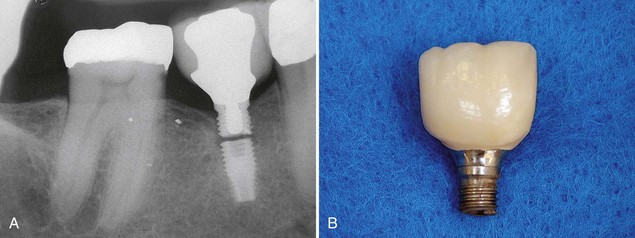
Figure 77-20 A, Radiograph of fractured implant (standard diameter) used to support a molar-sized single crown in the posterior mandible. B, Crown and coronal portion of implant (same as A) that fractured between the third and fourth threads.
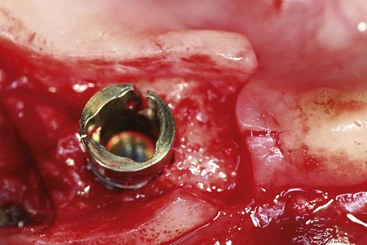
Figure 77-21 Implant fractured at internal connection collar resulting from fatigue. This collar fracture was caused by rotational forces applied to the implant at the time of placement into dense bone. The fracture was likely the result of a combination of material weakness and density of the prepared site.
Fracture of Restorative Materials
Fracture or failure of materials used for implant-retained restorations can be a significant problem. This is particularly true for veneers (acrylic, composite, or ceramic) that are attached to superstructures (Figure 77-22).
Esthetic and Phonetic Complications
Esthetic Complications
The challenge of modern implant dentistry is achieving an esthetic, as well as a functional, implant restoration. Harmonious tooth shape, size, and ideal soft tissue contours are key factors for successful esthetic outcomes.82
Esthetic complications arise when patient expectations are not met. Patient satisfaction with the esthetic outcome of the implant prosthesis vary from patient to patient, depending on a number of factors. As mentioned earlier, the risk for esthetic complications is increased for patients with high esthetic expectations and less-than-optimal patient-related factors (e.g., high smile line, thin periodontal soft tissues, or inadequate bone quantity and quality). In addition to the actual appearance of the final restoration, individual perceptions and desires determine the acceptance of the results. Esthetic complications result from poor implant position and deficiencies in the existing anatomy of the edentulous sites that were reconstructed with implants. An important prerequisite for achieving optimal gingival tissue contour is sufficient periimplant bone to support the soft tissues. Hard tissue defects can be treated by a variety of bone augmentation procedures.
Implant placement in the esthetic zone requires precise three-dimensional tissue reconstruction and ideal implant placement.62,117 This reconstructive procedure enables the restorative dentist to develop a natural emergence profile of the implant crown. If the amount of available bone does not allow for ideal implant placement and if the implant is positioned too apical, buccal, or in the proximal space, an unesthetic prosthetic profile will be developed (Figure 77-23).
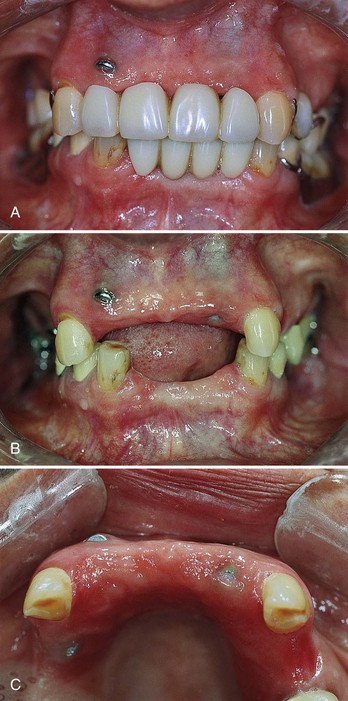
Figure 77-23 Poor implant position makes it impossible to restore with an esthetic, “natural appearing” restoration. A, Anterior view with removable partial dentures RPDs inserted. B, Anterior view without removable partial dentures. Notice the high level of implant cover screw/head exposure (maxillary right lateral incisor) that is significantly apical to the level of the adjacent natural tooth (cuspid) gingival margin. C, Occlusal view of same patient. Again, notice the labial projection of same implant (maxillary right lateral incision), as well as the palatal position of the implant in premolar area. Any attempt to restore the anterior implants would not be esthetically acceptable.
If crown contours and dimensions are not ideal or if gingival harmony around the implant restoration is unesthetic, the patient may consider the implants or restorations as complications because the outcome does not represent a natural appearance (Figure 77-24). Gingiva-colored materials utilized to replace lost gingival anatomy can offer an alternative to surgical augmentation in patients undergoing implant therapy (Figure 77-25). These restorations provide numerous advantages over conventional restorations, including improved lip support, masking of interproximal spaces, and restoration of gingival symmetry in selected cases.66

Figure 77-24 High gingival margin on single-tooth implant crown in the maxillary lateral incisor position. Notice the discrepancy between gingival margin levels of the implant and the adjacent natural teeth.

Figure 77-25 Pink porcelain used on implant-supported fixed restoration to mask the high gingival margin and long implant crowns resulting from an uncorrected alveolar ridge defect.
If the patient is truly dissatisfied with the esthetic result and there is a problem with the position of the implants that can be corrected (i.e., the patient’s expectations are reasonable), the implants could be removed; the case could be reevaluated and possibly retreated. However, the clinician should consider prosthetic solutions before implant removal. Use of angulated abutments, superstructures, and gingiva-colored materials may result in an acceptable esthetic result, thus avoiding multiple surgeries necessary to rebuild hard and soft tissue if an integrated implant is removed.
Careful patient evaluation and treatment planning along with a solid understanding and appreciation for the predictability and limitations of implant procedures will minimize esthetic complications. Patients with a high smile line, high esthetic demands, thin periodontium, or lack of hard and soft tissue support in the anterior esthetic region are some of the most difficult cases to treat and should only be treated after extensive planning by experienced clinicians.
Phonetic Problems
Implant prostheses that are fabricated with unusual palatal contours (e.g., restricted or narrow palatal space) or that have spaces under and around the superstructure can create phonetic problems for the patient. This is particularly problematic when full-arch, implant-supported, fixed restorations are fabricated for patients who have a severely atrophied maxilla. These patients are probably best served with an implant-assisted maxillary overdenture because the design facilitates replacement of missing alveolar structure and avoids creating spaces that allow air to escape during speech.
![]() Science Transfer
Science Transfer
Implant treatment in general has a high success rate, although the clinician has the obligation to each patient to reduce the possibility of failure and complications in that particular case.
Many surgery-related problems can be avoided by proper presurgical work-ups. This includes the use of three-dimensional radiographs to clearly ascertain bone dimensions and anatomic structures. Appropriate three-dimensional radiologic data should preclude the risk of damage or injury to the inferior mandibular nerve and the mental nerve, and the use of intraoperative periapical radiographs is essential to prevent damage to adjacent tooth roots. Penetration of surgical burs or implants through the lingual plate of the mandible must be avoided because it can lead to serious hemorrhage into the sublingual tissues with risk of subsequent airway obstruction.
The most common prosthetic-related problems are fractures of veneers caused by heavy occlusal loading and loosening of prostheses from the implant by screw loosening or cement failure. Control of occlusal loading by narrowing occlusal tables and ensuring no balancing and minimal working and centric contacts should be part of all implant therapy. Screw-retained prostheses can be easily removed and repaired, whereas cemented restoratives often cannot be retrieved and can have excess cement causing periimplantitis. The use of torque-controlled screwdrivers and implants with internal fixation can reduce the risk of screw fracture and loosening.
Conclusion
Although implants offer a highly predictable treatment option for the replacement of single and multiple missing teeth, there are a variety of potential complications that may be surgical, biologic, mechanical, prosthetic, or esthetic. Careful diagnosis and treatment planning, along with the use of diagnostic imaging, surgical guides, meticulous techniques, and adherence to proven principles can prevent many of the problems discussed in this chapter. A thorough understanding of anatomy, biology, and wound healing can reduce the incidence of complications. However, there is no substitute for training, knowledge, and clinical experience for preventing, recognizing, and successfully managing complications. This chapter is a start. The clinician who places and/or restores implants must be aware of techniques and procedures for early intervention should a complication arise.
1 Achilli A, Tura F, Euwe E. Immediate/early function with tapered implants supporting maxillary and mandibular posterior fixed partial dentures: preliminary results of a prospective multicenter study. J Prosthetic Dent. 2007;97:S52-S58.
2 Adell R, Eriksson B, Lekholm U, et al. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990;5:347-359.
3 Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387-416.
4 Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007;22(Suppl):49-70.
5 al-Ansari BH, Morris RR. Placement of dental implants without flap surgery: a clinical report. Int J Oral Maxillofac Implants. 1998;13:861-865.
6 Albrektsson T, Zarb G, Worthington P, et al. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11-25.
7 Andersson P, Verrochi D, Pagliant L, et al. Immediate/early loading of Neoss implants. Preliminary results from an ongoing study. App Osseointe Res. 2008;6:27-30.
8 Araujo M, Linder E, Lindhe J. Effect of a xenograft on early bone formation in extraction sockets: an experimental study in dog. Clin Oral Implants Res. 2009;20:1-6.
9 Astrand P, Engquist B, Dahlgren S, et al. Astra Tech and Brånemark System implants: a prospective 5-year comparative study. Results after one year. Clin Implant Dent Related Res. 1999;1:17-26.
10 Attard NJ, Zarb GA. Immediate and early implant loading protocols: a literature review of clinical studies. J Prosthet Dent. 2005;94:242-258.
11 Bain CA, Moy PK. The association between the failure of dental implants and cigarette smoking. Int J Oral Maxillofac Implants. 1993;8:609-615.
12 Balshi TJ. Preventing and resolving complications with osseointegrated implants. Dent Clin North Am. 1989;33:821-868.
13 Balshi TJ. An analysis and management of fractured implants: a clinical report. Int J Oral Maxillofac Implants. 1996;11:660-666.
14 Barone A, Santini S, Sbordone L, et al. A clinical study of the outcomes and complications associated with maxillary sinus augmentation. Inter J Oral Maxillofac Implants. 2006;21:81-85.
15 Bartling R, Freeman K, Kraut RA. The incidence of altered sensation of the mental nerve after mandibular implant placement. J Oral Maxillofac Surg. 1999;57:1408-1412.
16 Bavitz JB, Harn SD, Homze EJ. Arterial supply to the floor of the mouth and lingual gingiva. Oral Sur Oral Med Oral Pathol. 1994;77:232-235.
17 Becker W, Dahlin C, Becker BE, et al. The use of e-PTFE barrier membranes for bone promotion around titanium implants placed into extraction sockets: a prospective multicenter study. Int J Oral Maxillofac Implants. 1994;9:31-40.
18 Belser UC, Buser D, Hess D, et al. Aesthetic implant restorations in partially edentulous patients–a critical appraisal. Periodontol 2000. 1998;17:132-150.
19 Belser UC, Grutter L, Vailati F, et al. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol. 2009;80:140-151.
20 Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29(Suppl 3):197-212. discussion 232-193
21 Bragger U, Burgin W, Fourmoussis I, et al. Image processing for the evaluation of dental implants. Dentomaxillofac Radiol. 1992;21:208-212.
22 Brånemark PI. Osseointegration and its experimental background. J Prosthet Dent. 1983;50:399-410.
23 Buser D, Bragger U, Lang NP, et al. Regeneration and enlargement of jaw bone using guided tissue regeneration. Clin Oral Implants Res. 1990;1:22-32.
24 Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(Suppl):43-61.
25 Buser D, Weber HP, Bragger U, Balsiger C. Tissue integration of one-stage ITI implants: 3-year results of a longitudinal study with hollow-cylinder and hollow-screw implants. Int J Oral Maxillofac Implants. 1991;6:405-412.
26 Campelo LD, Camara JR. Flapless implant surgery: a 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants. 2002;17:271-276.
27 Cannizzaro G, Leone M, Consolo U, et al. Immediate functional loading of implants placed with flapless surgery versus conventional implants in partially edentulous patients: a 3-year randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2008;23:867-875.
28 Cardaropoli D, Cardaropoli G. Preservation of the postextraction alveolar ridge: a clinical and histologic study. Int J Periodontics Restorative Dent. 2008;28:469-477.
29 Chaushu G, Chaushu S, Tzohar A, et al. Immediate loading of single-tooth implants: immediate versus non-immediate implantation. A clinical report. Int J Oral Maxillofac Implants. 2001;16:267-272.
30 Chen ST, Wilson TGJr, Hammerle CH. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004;19(Suppl):12-25.
31 Chiapasco M. Early and immediate restoration and loading of implants in completely edentulous patients. Int J Oral Maxillofac Implants. 2004;19(Suppl):76-91.
32 Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006;17(Suppl 2):136-159.
33 Cooper L, Felton DA, Kugelberg CF, et al. A multicenter 12-month evaluation of single-tooth implants restored 3 weeks after 1-stage surgery. Int J Oral Maxillofac Implants. 2001;16:182-192.
34 Cordaro L, Rossini C, Mijiritsky E. Fracture and displacement of lingual cortical plate of mandibular symphysis following bone harvesting: case report. Implant Denti. 2004;13:202-206.
35 Dahlin C, Sennerby L, Lekholm U, et al. Generation of new bone around titanium implants using a membrane technique: an experimental study in rabbits. Int J Oral Maxillofac Implants. 1989;4:19-25.
36 Darriba MA, Mendonca-Caridad JJ. Profuse bleeding and life-threatening airway obstruction after placement of mandibular dental implants. J Oral Maxillofac Surg. 1997;55:1328-1330.
37 Degidi M, Piattelli A. Immediate functional and non-functional loading of dental implants: a 2- to 60-month follow-up study of 646 titanium implants. J Periodontol. 2003;74:225-241.
38 Del Castillo-Pardo de Vera JL, Lopez-Arcas Calleja JM, Burgueno-Garcia M. Hematoma of the floor of the mouth and airway obstruction during mandibular dental implant placement: a case report. Oral Maxillofac Surg. 2008;12:223-226.
39 Del Fabbro M, Testori T, Francetti L, et al. Systematic review of survival rates for immediately loaded dental implants. Int J Periodontics Restorative Dent. 2006;26:249-263.
40 Del Fabbro M, Testori T, Francetti L, et al. Systematic review of survival rates for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative Dent. 2004;24:565.
41 DeLuca S, Habsha E, Zarb GA. The effect of smoking on osseointegrated dental implants. Part I: implant survival. Int J Prosthodontics. 2006;19:491-498.
42 DeLuca S, Zarb G. The effect of smoking on osseointegrated dental implants. Part II: Peri-implant bone loss. Int J Prosthodontics. 2006;19:560-566.
43 Doring K, Eisenmann E, Stiller M. Functional and esthetic considerations for single-tooth Ankylos implant-crowns: 8 years of clinical performance. J Oral Implantol. 2004;30:198-209.
44 Eckert SE, Meraw SJ, Cal E, et al. Analysis of incidence and associated factors with fractured implants: a retrospective study. Int J Oral Maxillofac Implants. 2000;15:662-667.
45 Elian N, Wallace S, Cho SC, et al. Distribution of the maxillary artery as it relates to sinus floor augmentation. Int J Oral Maxillofac Implants. 2005;20:784-787.
46 Ellegaard B, Baelum V, Kolsen-Petersen J. Non-grafted sinus implants in periodontally compromised patients: a time-to-event analysis. Clin Oral Implants Res. 2006;17:156-164.
47 Esposito M, Ekestubbe A, Grondahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Branemark implants. Clin Oral Implants Res. 1993;4:151-157.
48 Esposito M, Grusovin MG, Maghaireh H, et al: Interventions for replacing missing teeth: management of soft tissues for dental implants, Cochrane database of systematic reviews (Online):CD006697, 2007.
49 Esposito M, Grusovin MG, Willings M, et al. The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2007;22:893-904.
50 Esposito M, Hirsch J, Lekholm U, et al. Differential diagnosis and treatment strategies for biologic complications and failing oral implants: a review of the literature. Int J Oral Maxillofac Implants. 1999;14:473-490.
51 Esposito M, Hirsch JM, Lekholm U, et al. Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis. Eur J Oral Sci. 1998;106:721-764.
52 Evans CD, Chen ST. Esthetic outcomes of immediate implant placements. Clin Oral Implants Res. 2008;19:73-80.
53 Fiorellini JP, Nevins ML. Localized ridge augmentation/preservation. A systematic review. Ann Periodontol. 2003;8:321-327.
54 Flanagan D. Important arterial supply of the mandible, control of an arterial hemorrhage, and report of a hemorrhagic incident. J Oral Implantol. 2003;29:165-173.
55 Furhauser R, Florescu D, Benesch T, et al. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res. 2005;16:639-644.
56 Ganeles J, Wismeijer D. Early and immediately restored and loaded dental implants for single-tooth and partial-arch applications. Int J Oral Maxillofac Implants. 2004;19(Suppl):92-102.
57 Gomez-Roman G. Influence of flap design on peri-implant interproximal crestal bone loss around single-tooth implants. Int J Oral Maxillofac Implants. 2001;16:61-67.
58 Goodacre CJ, Bernal G, Rungcharassaeng K, et al. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121-132.
59 Goodacre CJ, Kan JY, Rungcharassaeng K. Clinical complications of osseointegrated implants. J Prosthet Dent. 1999;81:537-552.
60 Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol. 2006;77:1933-1943.
61 Gregg JM. Neuropathic complications of mandibular implant surgery: review and case presentations. Ann R Australas Coll Dent Surg. 2000;15:176-180.
62 Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25:113-119.
63 Hallman M, Hedin M, Sennerby L, et al. A prospective 1-year clinical and radiographic study of implants placed after maxillary sinus floor augmentation with bovine hydroxyapatite and autogenous bone. J Oral Maxillofac Surg. 2002;60:277-284. discussion 285-276
64 Hammerle CH, Jung RE, Feloutzis A. A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients. J Clin Periodontol. 2002;29(Suppl 3):226-231. discussion 232-223
65 Hammerle CH, van Steenberghe D. The first EAO Consensus Conference 16-19 February 2006, Pfaffikon, Switzerland. Clin Oral Implants Res. 2006;17(Suppl 2):1.
66 Hannon SM, Colvin CJ, Zurek DJ. Selective use of gingival-toned ceramics: case reports. Quintessence Int. 1994;25:233-238.
67 Hermann JS, Cochran DL, Nummikoski PV, et al. Crestal bone changes around titanium implants. A radiographic evaluation of unloaded nonsubmerged and submerged implants in the canine mandible. J Periodontol. 1997;68:1117-1130.
68 Isaacson T. Sublingual hematoma formation during immedicate placement of mandibular endosseous implants. J Am Dent Assoc. 2004;30:202.
69 Jaffin RA, Kumar A, Berman CL. Immediate loading of dental implants in the completely edentulous maxilla: a clinical report. Int J Oral Maxillofac Implants. 2004;19:721-730.
70 Jemt T. Fixed implant-supported prostheses in the edentulous maxilla. A five-year follow-up report. Clin Oral Implants Res. 1994;5:142-147.
71 Jensen J, Reiche-Fischel O, Sindet-Pedersen S. Nerve transposition and implant placement in the atrophic posterior mandibular alveolar ridge. J Oral Maxillofac Surg. 1994;52:662-668. discussion 669-670
72 Jensen OT, Cockrell R, Kuhike L, et al. Anterior maxillary alveolar distraction osteogenesis: a prospective 5-year clinical study. Int J Oral Maxillofac Implants. 2002;17:52-68.
73 Jeske AH, Suchko GD. Lack of a scientific basis for routine discontinuation of oral anticoagulation therapy before dental treatment. J Am Dent Assoc. 2003;134:1492-1497.
74 Jimenez Y, Poveda R, Gavalda C, et al. An update on the management of anticoagulated patients programmed for dental extractions and surgery. Medicina Oral Patologia Oral y Cirugia Bucal. 2008;13:E176-179.
75 Jokstad A, Carr AB. What is the effect on outcomes of time-to-loading of a fixed or removable prosthesis placed on implant(s)? Int J Oral Maxillofac Implants. 2007;22(Suppl):19-48.
76 Jovanovic SA: Plaque-induced periimplant bone loss in mongrel dogs: a clinical, microbial, radiographic, and histological study. In: Master of Science Thesis Los Angeles, 1994.
77 Jovanovic SA, Spiekermann H, Richter EJ. Bone regeneration around titanium dental implants in dehisced defect sites: a clinical study. Int J Oral Maxillofac Implants. 1992;7:233-245.
78 Kan JY, Lozada JL, Goodacre CJ, et al. Endosseous implant placement in conjunction with inferior alveolar nerve transposition: an evaluation of neurosensory disturbance. Int J Oral Maxillofac Implants. 1997;12:463-471.
79 Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int J Oral Maxillofac Implants. 2003;18:31-39.
80 Kasabah S, Krug J, Simunek A, et al. Can we predict maxillary sinus mucosa perforation? Acta Medica (Hradec Kralove) / Universitas Carolina, Facultas Medica Hradec Kralove. 2003;46:19-23.
81 Klokkevold PR, Han TJ. How do smoking, diabetes, and periodontitis affect outcomes of implant treatment? Int J Oral Maxillofac Implants. 2007;22(Suppl):173-202.
82 Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001;22:199-206. quiz 208
83 Lang NP, Pjetursson BE, Tan K, et al. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. II. Combined tooth–implant-supported FPDs. Clin Oral Implants Res. 2004;15:643-653.
84 Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9:332-343.
85 Lekholm U, Gunne J, Henry P, et al. Survival of the Branemark implant in partially edentulous jaws: a 10-year prospective multicenter study. Int J Oral Maxillofac Implants. 1999;14:639-645.
86 Lindeboom JA, Tjiook Y, Kroon FH. Immediate placement of implants in periapical infected sites: a prospective randomized study in 50 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:705-710.
87 Lindhe J, Meyle J. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35:282-285.
88 Mayfield L. Immediate delayed and late submerged and transmucosal implants. Berlin: Quintessence; 1999. pp 520-534
89 Meijer HJ, Stellingsma K, Meijndert L, et al. A new index for rating aesthetics of implant-supported single crowns and adjacent soft tissues—the Implant Crown Aesthetic Index. Clin Oral Implants Res. 2005;16:645-649.
90 Meitner SW, Tallents RH. Surgical templates for prosthetically guided implant placement. J Prosthetic Dent. 2004;92:569-574.
91 Meyer U, Joos U, Mythili J, et al. Ultrastructural characterization of the implant/bone interface of immediately loaded dental implants. Biomaterials. 2004;25:1959-1967.
92 Misch CE. Maxillary sinus augmentation for endosteal implants: organized alternative treatment plans. Int J Oral Implantol. 1987;4:49-58.
93 Misch CE. Contemporary Implant Dentistry. St Louis: Mosby; 2008. pp 905-974
94 Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998;17:63-76.
95 Mombelli A, Marxer M, Gaberthuel T, et al. The microbiota of osseointegrated implants in patients with a history of periodontal disease. J Clin Periodontol. 1995;22:124-130.
96 Mombelli A, van Oosten MA, Schurch EJr, et al. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987;2:145-151.
97 Moy PK, Medina D, Shetty V, et al. Dental implant failure rates and associated risk factors. Int J Oral Maxillofac Implants. 2005;20:569-577.
98 Nakou M, Mikx FH, Oosterwaal PJ, et al. Early microbial colonization of permucosal implants in edentulous patients. J Dent Res. 1987;66:1654-1657.
99 Nevins M, Mellonig JT. Enhancement of the damaged edentulous ridge to receive dental implants: a combination of allograft and the GORE-TEX membrane. Int J Periodontics Restorative Dent. 1992;12:96-111.
100 Niamtu J3rd. Near-fatal airway obstruction after routine implant placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:597-600.
101 Panula K, Oikarinen K. Severe hemorrhage after implant surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:2.
102 Parel SM. Aesthetics and osseointegration. Dentistry today. 1990;9:50-51.
103 Payne AG, Tawse-Smith A, Thompson WM, et al. Early functional loading of unsplinted roughened surface implants with mandibular overdentures 2 weeks after surgery. Clin Implant Dent Relat Res. 2003;5:143-153.
104 Payne AG, Tawse-Smith A, Thomson WM, et al. One-stage surgery and early loading of three implants for maxillary overdentures: a 1-year report. Clin Implant Dent Relat Res. 2004;6:61-74.
105 Penarrocha M, Perez H, Garcia A, et al. Benign paroxysmal positional vertigo as a complication of osteotome expansion of the maxillary alveolar ridge. J Oral Maxillofac Surg. 2001;59:106-107.
106 Penarrocha-Diago M, Rambla-Ferrer J, Perez V, et al. Benign paroxysmal vertigo secondary to placement of maxillary implants using the alveolar expansion technique with osteotomes: a study of 4 cases. Int J Oral Maxillofac Implants. 2008;23:129-132.
107 Pjetursson BE, Tan K, Lang NP, et al. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004;15:667-676.
108 Raghoebar GM, Louwerse C, Kalk WW, et al. Morbidity of chin bone harvesting. Clin Oral Implants Res. 2001;12:503-507.
109 Rams TE, Link CCJr. Microbiology of failing dental implants in humans: electron microscopic observations. J Oral Implantol. 1983;11:93-100.
110 Rangert B, Jemt T, Jorneus L. Forces and moments on Branemark implants. Int J Oral Maxillofac Implants. 1989;4:241-247.
111 Rangert B, Krogh PH, Langer B, et al. Bending overload and implant fracture: a retrospective clinical analysis. Int J Oral Maxillofac Implants. 1995;10:326-334.
112 Richter EJ, Jansen V, Spiekerann H, et al. Langzeitergebnisse von IMZ-und TPS-Implantaten im interforaminalen Bereich des zahnlosen Unterkierfers. Deutsche Zahnarztliche Zeitschrift. 1992;47:449.
113 Rocci A, Martignoni M, Gottlow J. Immediate loading of Branemark System TiUnite and machined-surface implants in the posterior mandible: a randomized open-ended clinical trial. Clin Implant Dent Relat Res. 2003;5(Suppl 1):57-63.
114 Romanos GE, Nentwig GH. Immediate loading using cross-arch fixed restorations in heavy smokers: nine consecutive case reports for edentulous arches. Int J Oral Maxillofac Implants. 2008;23:513-519.
115 Roos J, Sennerby L, Lekholm U, et al. A qualitative and quantitative method for evaluating implant success: a 5-year retrospective analysis of the Branemark implant. Int J Oral Maxillofac Implants. 1997;12:504-514.
116 Sacco R, Sacco M, Carpenedo M, et al. Oral surgery in patients on oral anticoagulant therapy: a randomized comparison of different intensity targets. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e18-21.
117 Salama H, Salama MA, Li TF, et al. Treatment planning 2000: an esthetically oriented revision of the original implant protocol. J Esthetic Dent. 1997;9:55-67.
118 Schincaglia GP, Marzola R, Scapoli C, et al. Immediate loading of dental implants supporting fixed partial dentures in the posterior mandible: a randomized controlled split-mouth study–machined versus titanium oxide implant surface. Int J Oral Maxillofac Implants. 2007;22:35-46.
119 Schnitman PA, Wohrle PS, Rubenstein JE. Immediate fixed interim prostheses supported by two-stage threaded implants: methodology and results. J Oral Implantol. 1990;16:96-105.
120 Schnitman PA, Wohrle PS, Rubenstein JE, et al. Ten-year results for Branemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants. 1997;12:495-503.
121 Schropp L, Wenzel A, Kostopoulos L, et al. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23:313-323.
122 Schulte W, Kleineikenscheidt H, Lindner K, et al. [The Tubingen immediate implant in clinical studies]. Deutsche Zahnarztliche Zeitschrift. 1978;33:348-359.
123 Schwartz-Arad D, Chaushu G. Immediate implant placement: a procedure without incisions. J Periodontol. 1998;69:743-750.
124 Simion M, Fontana F, Rasperini G, et al. Long-term evaluation of osseointegrated implants placed in sites augmented with sinus floor elevation associated with vertical ridge augmentation: a retrospective study of 38 consecutive implants with 1- to 7-year follow-up. Int J Periodontics Restorative Dent. 2004;24:208-221.
125 Simion M, Trisi P, Maglione M, et al. A preliminary report on a method for studying the permeability of expanded polytetrafluoroethylene membrane to bacteria in vitro: a scanning electron microscopic and histological study. J Periodontol. 1994;65:755-761.
126 Small PN, Tarnow DP, Cho SC. Gingival recession around wide-diameter versus standard-diameter implants: a 3- to 5-year longitudinal prospective study. Pract Proced Aesthet Dent. 2001;13:143-146.
127 Spray JR, Black CG, Morris HF, et al. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol Am Acad Periodontol. 2000;5:119-128.
128 Stach RM, Kohles SS. A meta-analysis examining the clinical survivability of machined-surfaced and osseotite implants in poor-quality bone. Implant Dent. 2003;12:87-96.
129 Strub J: Langzeitprognose von enossalen oralen Implantaten unter spezieller Berucksichtigung von periimplantaren, materialkundlichen und okklusalen Gesichtspunkten. In: Quintessenz Verlags Berlin, 1986.
130 Strub JR, Gaberthuel TW, Grunder U. The role of attached gingiva in the health of peri-implant tissue in dogs. 1. Clinical findings. Int J Periodontics Restorative Dent. 1991;11:317-333.
131 Tarnow DP, Emtiaz S, Classi A. Immediate loading of threaded implants at stage 1 surgery in edentulous arches: ten consecutive case reports with 1- to 5-year data. Int J Oral Maxillofac Implants. 1997;12:319-324.
132 Tawse-Smith A, Payne AG, Kumara R, et al. Early loading of unsplinted implants supporting mandibular overdentures using a one-stage operative procedure with two different implant systems: a 2-year report. Clin Implant Dent Relat Res. 2002;4:33-42.
133 Taylor TD, Agar JR. Twenty years of progress in implant prosthodontics. J Prosthetic Dent. 2002;88:89-95.
134 ten Bruggenkate CM, Krekeler G, Kraaijenhagen HA, et al. Hemorrhage of the floor of the mouth resulting from lingual perforation during implant placement: a clinical report. Int J Oral Maxillofac Implants. 1993;8:329-334.
135 Testori T, Galli F, Capelli M, et al. Immediate nonocclusal versus early loading of dental implants in partially edentulous patients: 1-year results from a multicenter, randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2007;22:815-822.
136 Tolman DE, Laney WR. Tissue-integrated prosthesis complications. Int J Oral Maxillofac Implants. 1992;7:477-484.
137 Tonetti MS, Hammerle CH. Advances in bone augmentation to enable dental implant placement: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35:168-172.
138 Wagenberg B, Froum SJ. A retrospective study of 1925 consecutively placed immediate implants from 1988 to 2004. Int J Oral Maxillofac Implants. 2006;21:71-80.
139 Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003;8:328-343.
140 Wallace SS, Mazor Z, Froum SJ, et al. Schneiderian membrane perforation rate during sinus elevation using piezosurgery: clinical results of 100 consecutive cases. Int J Periodontics Restorative Dent. 2007;27:413-419.
141 Zablotsky MH, Diedrich DL, Meffert RM. Detoxification of endotoxin-contaminated titanium and hydroxyapatite-coated surfaces utilizing various chemotherapeutic and mechanical modalities. Implant Dent. 1992;1:154-158.
142 Zablotsky MH, Diedrich D, Meffert R, et al. The ability of various chemotherapeutic agents to detoxify the endotoxin infected HA-coated implant surface. Int J Oral Maxillofac Implants. 1991;8:45.
143 Zijderveld SA, van den Bergh JP, Schulten EA, et al. Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures. J Oral Maxillofac Surg. 2008;66:1426-1438.
144 Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008;35:286-291.
145 Zustein T, Billistrom C. A retrospective follow-up of 50 consecutive patients treated with Neoss implants with or without an adjunctive GBR-procedure. App Osseoint Res. 2008;6:27-30.