CHAPTER 80 Results of Implant Treatment
The landmark Goteborg study, as well as the replica study at the University of Toronto, set the stage for success and predictability expectations of root-form dental implants. The study, conducted over a 15-year period at the University of Goteborg, Sweden, by P.I. Brånemark and co-workers began in 1965 and concluded in 1980. The results, reported in several articles, defined the concept of osseointegration, described protocols for success, and shared clinical experiences. Perhaps the most significant article from the study, published in 1981, was a paper on osseointegrated implants in the treatment of the edentulous jaw.2 Briefly stated, the Goteborg study included 2768 root-form implants placed into 410 edentulous jaws in 371 consecutive patients. The data were most often reported in subsets according to the three study phases (initial, developmental, and routine). Those cases treated in the routine period with standardized procedures and an observation time of 5 to 9 years were thought to reflect the potential of the method and were the basis of data reported in that historic publication. This subset consisted of 895 implants placed in 130 jaws. Implant survival was 81% in the maxilla and 91% in mandible. Prosthesis survival (continuous stability) was 89% in the maxilla and 100% in the mandible. The replica study, conducted at the University of Toronto, demonstrated that comparable results could be predictably achieved using the same implant design and treatment protocols.5,72-74 Together, these studies demonstrated that implant survival of 81% or more and prosthesis survival of 89% or more could be expected in the edentulous patient.
In the decades since the landmark discovery of osseointegration and the documentation of its clinical effectiveness, clinicians have experienced tremendous success replacing missing teeth with endosseous, root-form dental implants in partially edentulous, as well as edentulous, patients.1,46 Yet, despite the high level of success and long-term predictability, achieving success all the time, in every patient, and in each situation is not 100%. Complications and implant failures do occur.2,12 Some implants fail to achieve osseointegration, some achieve osseointegration only to lose bone progressively over time leading to failure, and other implants rapidly lose bone and fail in a short time. Just as importantly, some implants may achieve and maintain osseointegration but fail because they do not meet the patient’s or clinician’s esthetic expectations.
The reporting of implant success varies widely in the literature, which makes defining an absolute implant success rate impractical. This chapter considers implant treatment results in light of the factors that influence implant survival and success. The intent is to outline important aspects that need to be considered in evaluating implant outcomes and to offer the reader guidelines for understanding published results.
Defining Implant Outcomes
Implant outcomes are reported in a variety of ways in the literature. Various levels of implant success and failure are described in case reports, case series, retrospective studies, controlled studies, and prospective studies. The type of study and method of reporting is decided by the authors and often influenced by the information (data) collected and the study objectives. Each type of study or report has recognized limitations, but because of the tremendous variation that exists in the way individual investigators measure, interpret, and report implant outcomes, differences in the results from one study to another may not be obvious. Some implant outcomes are reported simply as the presence or absence of the implant(s) at the time of the last examination, regardless of whether the implant was in function, suffered from bone loss, or had other problems. This type of assessment is a measure of implant survival and should not be confused with implant success. In contrast to such an overly simplified assessment, some investigators report implant outcomes using very specific criteria to determine implant success.
Implant success is defined by specific criteria used to evaluate the condition and function of the implant. Criteria for implant success have been proposed in the literature but not used consistently. The problem is that a universally accepted definition of implant success has not been established. In the classic definition, Albrektsson et al3 defined implant success as an implant with no pain, no mobility, no radiolucent periimplant areas, and less than 0.2 mm of bone loss annually after the first year of loading.3 Bone loss in the first year was recognized but it was not defined or quantified as part of the success criteria until later in a separate definition by Roos.57 The real challenge in comparing reported data from study to study is that authors use different criteria of success in their work. As a result, it is difficult or impossible to make comparisons between studies and drawing conclusions about implant success or failure from data reported in different studies is tenuous.
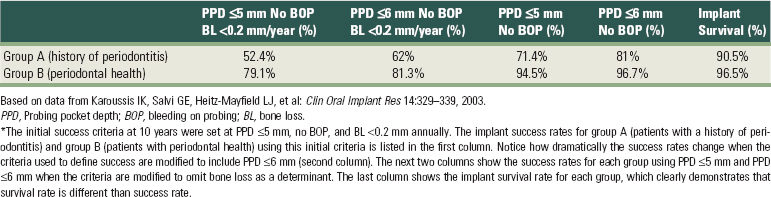
It is important to recognize that success rates are dramatically affected by variations in the criteria used to define them. In strict terms, if one considers “implant success” to be the outcome without any adverse effects or problems, then the treatment would be performed as planned, implants would remain stable and functioning without problems, periimplant tissues would be stable and healthy, and both the patient and the treating clinician(s) would be pleased with the outcome (Figure 80-1). If such strict criteria are used, implant success rates would be undoubtedly lower than those determined using less stringent criteria. Table 80-1 illustrates the powerful effect that small changes in success criteria have on the reported success rates. The data demonstrates that simply changing the criteria of success to include probing pocket depth (PPD) ≤5 mm to ≤6 mm changed the implant success rates from 52.4% to 62% and from 79.1% to 81.3% in patients with and without a history of periodontitis, respectively.40 It also shows that implant survival (last column) is quite different than implant success.

Figure 80-1 Clinical example of implant success. A single implant was placed in the mandible to replace the lower second premolar (as planned). The implant integrated and was successfully restored in function. Both the patient and clinician(s) are pleased with the outcome. A, Clinical photograph of dentition in occlusion (from left side). B, Close-up clinical photograph of dentition in occlusion. Mandibular second premolar is an implant supported crown. C, Occlusal view of implant supported crown in the second premolar position. Notice that the replacement of the mandibular second premolar with an implant is a conservative treatment, obviating the need to prepare adjacent teeth. D, Periapical radiograph of the posterior mandibular teeth and implant in the second premolar position. Bone support is good and bone loss is minimal and consistent with expectations for this implant design.
TABLE 80-1 Effect of Slight Modifications in Implant Success Criteria on Implant Success Rate Outcomes*
“Implant survival,” on the other hand, is simply defined as any implant that remains in place at the time of evaluation, regardless of any untoward signs, symptoms, or history of problems. Clearly, there is a difference between implants that are present, healthy, and functioning under an implant-retained restoration, implants that are present but suffering from periimplant bone loss, or implants that are present but not connected to any restoration and not functioning (Figure 80-2). Implants that are osseointegrated but not restored into function are referred to as “sleepers” and should not be considered successful merely because they are present and osseointegrated. To reiterate, implant survival and implant success are distinctly different outcome measures. As an example, consider the dramatic difference between survival and success rate for implants reported in a systematic review (21 studies included) of implants supporting fixed partial dentures; the reported 5-year implant survival rate was 95.4%, whereas the 5-year patient success rate,* defined as free of any complications, was only 61.3%.55

Figure 80-2 Panoramic radiograph of an individual with an implant placed in the position of a missing maxillary right central incisor. The implant appears to be placed in a nonrestorable position. It is osseointegrated and could technically be counted as a “surviving” implant but must be considered a failure because it does not meet the intended goal and has not been restored into function.
Defining implant results in absolute terms is difficult and confusing. Implant survival, which is almost always reported in studies, may actually overestimate implant outcomes. Implant success, on the other hand, which is less often reported, could be a better measure of actual implant outcomes if specific success criteria were universally defined, accepted, and used. Currently, implant success is difficult or impossible to compare across studies because of differences in evaluation criteria used by investigators. Implant success in a single study (or series of studies that use the same success criteria) is meaningful only in the context of that study (or series). At present, the usefulness of implant success rates from multiple different studies is limited. Implant survival is important but is only an indicator of surviving implants and does not reveal whether implants are functioning or whether any problems were associated with them over time.
Factors that Influence Implant Outcomes
Many factors influence implant outcomes, including available bone, implant design, placement and loading protocols, and host-related factors. Some of the factors thought to affect implant outcomes are briefly discussed here.
Anatomic Location
Osseointegration depends on the availability of an adequate quantity and quality of bone at the implant site(s). Areas with abundant bone volume in the desired location will be better than areas with deficient bone volume. Likewise, areas with good bone density provide more predictable outcomes than areas with poor bone density. The bone classification system described by Lekholm and Zarb47 was intended to define bone sites that would have different levels of bone support for implants and that would likely impact survival and success. The quality of bone support is greatly influenced by the anatomic location, thus implant outcomes are sometimes categorized according to anatomic location. Extreme examples are the anterior mandible and the posterior maxilla. The anterior mandible typically consists of dense cortical bone, which offers great support and high bone-to-implant contact, whereas the posterior maxilla is often limited in volume because of alveolar resorption and sinus pneumatization and typically consists of a loose, trabecular structure and a thin cortical bone shell.
Implants placed in the posterior maxilla are less well supported compared to implants placed in the anterior mandible. Jaffin and Berman34 demonstrated the significance of bone quality on implant survival in a report of 1054 Brånemark implants. Ninety percent of these implants were placed in type I, II, and III bone with only 3% failures. However, of the 10% that were placed in type IV bone, 35% failed.34 Excluding those placed in the mandible, 23/52 implants placed in type IV bone in the maxilla failed for a dismal 56% survival rate (44% failed). They concluded that bone quality stood out as the single greatest determinant of implant loss.
Anatomic location appears to have a significant effect on implant outcomes. This is particularly true for the posterior maxilla. It should be recognized that the implants used in this study were machined surface implants and that current implants with altered microtopography are expected to perform better in the posterior maxilla. Not surprisingly, when all 1054 implants are considered together, the combined implant survival rate (93.9%) in this study falls within (or slightly higher than) the range of reported survival rates of implants in the Goteborg study (with similar implants).
Implant Design
One of the many factors thought to influence implant outcomes is implant design. Today, there are hundreds of companies that manufacture and market dental implants worldwide and the number continues to grow. Implant dimensions, geometries, and surface characteristics vary tremendously and continue to evolve as innovation and research findings pave the way to changes that are thought to improve outcomes. Very few of these implant designs have been studied and rely on being clinically similar to the other researched and approved implant designs without studies or documentation to support their effectiveness. Thus, in most cases, it is impossible to appreciate the effect of particular implant design features on implant outcomes. Nonetheless, these new, different implant designs are being used and outcomes are being reported in studies that evaluate other aspects of treatment (i.e., not specific to the implant design) only to make comparisons and assessments more confusing and difficult.
Those studies that have documented the success of dental implants based on implant design characteristics have shaped some of the tenets for current implant standards, selection, and use. For example, many clinicians adhere to the premise that longer implants are better, threaded implants are better, rough-surfaced implants are better, etc. Over time, as changes in design and utilization evolved, some beliefs have been disproved, and continued advances and research will also refute other firmly held beliefs.
What are the best implant design characteristics? Is there an implant design that performs better than the rest? Actually, it is nearly impossible to determine which implant design characteristics are important because there are many variables to consider and implants are successful most of the time. Given the generally high success, it seems that subtle differences in implant design are probably not significant for the majority of patients and situations.22,26 However, in compromised patients, inadequate sites, or challenging circumstances, certain implant designs may perform better than others. A prime example is the effect of implant surface characteristics. Implants with an altered surface microtopography (i.e., acid-etched, blasted, etc.) have been shown to enhance the bone-to-implant interface42,43 and are thought to improve implant outcomes, especially in compromised sites.66,67 Lower success rates have been associated with smooth surface (i.e., machined) implants.35,56,60 Implant length is another consideration. Implant length is a factor that has long been held as important for success (i.e., longer is better), and many studies have supported this dogma,61,62 but recent studies are challenging it.29
Placement and Loading Protocols
The traditional implant placement protocol required a healed edentulous ridge into which implants were placed and allowed to osseointegrate for a period of time without occlusal loading (see Chapter 71). The nonloading period after implant placement was empirically determined to be 3 to 4 months in the mandible and 6 months in the maxilla.10 A strongly held belief at the time was that early loading would lead to higher failure rates.11 In contrast to these early standards, some current protocols advocate dramatically different approaches, including implant placement immediately after tooth extraction and implant occlusal loading immediately or shortly after placement. Each of these approaches has distinct advantages, but they are also accompanied by challenges that have the potential to adversely affect implant outcomes.
Immediate Implant Placement.
The immediate implant placement protocol describes the procedure in which an implant is placed in an extraction socket after tooth removal and socket debridement. This procedure, originally described by Schulte et al64 and later by Lazzara,45 has been reported with survival rates equivalent to that of implants placed into healed ridges.14,49 The advantages of immediate placement include decreased surgery, cost, and healing time.65 Immediate implant placement introduces additional risks of complications, including poor implant position, compromised esthetic outcome, and implant failure (see Chapter 77). Despite the increased risks, high long-term (1- to 16-year) survival rates of 96% have been reported for implants immediately placed into extraction sockets.69
Immediate Occlusal Loading.
Brånemark established the concept of the osseointegrated dental implant as a predictable modality of treatment for the edentulous patient based on the empirically based requirement that the implant remain submerged and unloaded for a healing period of 3 to 6 months.10 This original protocol, requiring the implant to remain stress free, was based on the concern that premature loading would cause micromotion of the dental implant leading to fibrous encapsulation and implant failure. However, studies have shown this assumption to be incorrect, demonstrating that immediately loaded implants can achieve success rates (>90%) similar to conventionally loaded dental implants.15,18,27,31,38 The long-term predictability of immediately loaded implants requires strict surgical and prosthodontic protocols.7
Bone Augmentation
A common problem encountered in implant dentistry is insufficient bone quantity to allow implant placement. Deficiencies in alveolar bone result from developmental defects, periodontal disease, tooth loss, and trauma.6,13,63 For most cases with alveolar ridge resorption, bone regenerative procedures are required to correct the defects before or simultaneous with implant placement (see Chapters 72 and 73). The obvious question is whether implants placed in sites that are reconstructed with bone augmentation procedures will achieve the same survival and success rates as implants placed in native bone sites.
The results of implants and bone augmentation procedures reported in the literature have been assessed by expert clinicians in several workshops.16,28,32,33 One systematic review of literature (2003 Workshop on Contemporary Science in Clinical Periodontics), including 13 studies (guided bone regeneration) with 1741 patients and 5 studies (distraction osteogenesis) with 92 patients, found that survival rates of dental implants in augmented bone achieved a high level of predictability that was similar to implants placed in natural bone.28 A more recent systematic review of the literature (the 2008 Consensus Report of the Sixth European Workshop on Periodontology) pointed out that the bone augmentation procedures can fail and that implants placed in these areas do not enjoy the high long-term survival rates of dental implants placed in pristine sites.68 The 2003 systematic review did not include an assessment of whether bone augmentation procedures failed, rather it intentionally focused on implants placed in sites that were successfully treated with bone augmentation. More research is needed to determine the long-term performance of dental implants placed in augmented bone and the clinical benefits of bone augmentation with respect to alternative treatments (i.e., the use of short implants).
Risk Factors
In general, most patients enjoy a similar rate of survival and success with dental implants. It is a minority of patients who experience implant failure. In addition to factors previously discussed, host-related factors may adversely affect healing, osseointegration, and maintenance of dental implants. Smoking, diabetes, and periodontitis have been identified as “risk factors” that may adversely affect implant outcomes. In a systematic review of the literature, Klokkevold and Han41 evaluated the influence of smoking, diabetes, and periodontal disease on implant outcomes and found that smoking has an adverse affect on implant survival and success, with the effects being more pronounced in areas of loose trabecular bone (i.e., the posterior maxilla). The review also suggested that type 2 diabetes may have an adverse effect on implant survival rates, but the limited number of included studies did not permit a definitive conclusion.41 Finally, their review also concluded that while patients with a history of treated periodontitis did not show any decrease in implant survival, they did experience more implant complications and lower success rates.41
Smoking.
Above all other risk factors, smoking has been shown to have a significant negative impact on implant survival and success. In a study of 2194 implants, Bain and Moy reported a significantly greater rate of failure in smokers (11.28%) compared to nonsmokers (4.76%).8 De Bruyn and Colleart reported an early failure rate of 9% in smokers compared to 1% in nonsmokers.17 Two other studies, one of 10 years23 and the other with follow-up ranging from 6 months to 21 years,53 concluded that smoking was a definite risk factor for implant survival.19,20
Diabetes.
The role of diabetes mellitus as a risk factor for implant outcomes is less clear. Although it is expected that a metabolic disease such as diabetes would have an adverse affect on bone healing70 and tissue support for implants, the research has not definitively determined that diabetes has a negative impact on implant survival or success.4 Moy and co-workers53 reported a significantly lower patient* success rate (68.7%) for patients with diabetes compared to the patient success rate (85.1%) for the entire study population (1140 patients with 4680 implants). However, this low success rate (high failure rate) may be an overestimate of the actual implant failure rate for patients with diabetes because it counts the number of patients with implant failures regardless of how many implants they had (i.e., implants that may have been successfully inserted and maintained in these patients are not counted). The number of patients with diabetes included in the study was 48/1140 or 4.2% of the total. Of these, 15 patients experienced implant failure(s). Conversely, in a systematic review of the literature (33 studies), Javed and Romanos found that patients with good metabolic control (hemoglobin A1c in normal range) achieve similar success with osseointegrated implants as patients without diabetes.36 Dowell and co-workers21 also found similar success for implants placed in patients with controlled diabetes.
Periodontitis.
There are a limited number of studies available to assess the prognosis of implant treatment in patients with a history of periodontitis.39 Most of these studies suggest that implants are equally successful in patients with a past history of chronic periodontitis. Short-term studies demonstrate 90% to 100% implant survival in patients with a history of chronic periodontitis.50,52 Long-term studies report 90% to 97% implant survival rates for patients with a history of chronic periodontitis.40,48,58,71 Short-term implant survival rates for patients treated for aggressive periodontitis are 95% to 100%.50,51 One long-term study reported an 88.8% implant survival over 5 years for patients treated for aggressive periodontitis.52 Implant survival in patients with a history of periodontitis appears to be highly predictable. However, the lack of long-term studies to support implant survival in patients treated for aggressive periodontitis leaves the prognosis in these patients open to question.39
Long-term studies evaluating implant treatment in periodontally compromised patients suggest that they may experience more periimplant problems.40 When these patients are followed for extended periods of time, there appear to be more complications (i.e., periimplantitis) associated with implants compared to periodontally healthy patients. In a 10-year prospective study of patients with or without a history of chronic periodontitis, biologic complications (i.e., periimplantitis) was higher for those with a history of chronic periodontitis (28.6%) compared to those with periodontal health (5.8%).40 This controlled study by Karoussis and co-workers40 found a statistically significant difference in mean periimplant bone loss between patients with a history of chronic periodontitis and periodontally healthy patients. These periimplant problems may be attributed to a continuous increase in the percentage of implants exhibiting probing pocket depths ≥4 mm over time.24
Esthetic Results and Patient Satisfaction
The ultimate test for implant outcomes is achieving natural appearing, as well as optimally functional, implant-supported tooth replacements. Proper tooth dimensions, contours, and ideal soft tissue support are key factors for successful esthetic outcomes.44 If crown form, dimension, and shape and gingival harmony around the implants are not ideal, the patient may consider the implant restoration unacceptable because the result does not represent a natural dental profile (Figure 80-3). For some patients, such as those with severe alveolar deficiency, an ideal esthetic outcome may be impossible because reconstructive surgical procedures are complex, require extensive time, and remain unpredictable. For others, a “less than ideal” esthetic outcome may be perfectly acceptable (see Chapter 74).

Figure 80-3 Clinical photograph of maxillary anterior fixed restoration supported by two malpositioned implants in the central incisor positions. The patient is dissatisfied with the esthetic outcome. The left implant is positioned between the central and lateral incisor and angled toward the facial surface at a level above the gingival margin. A tooth-colored material was used to mask the exposed framework in the gingival area.
Esthetic problems and patient dissatisfaction happen when results are inferior to what was expected. Patient satisfaction with the esthetic outcome of the implant prosthesis varies from patient to patient, depending on a number of factors. The risk for esthetic failure is increased for patients with high esthetic expectations. The risk is also higher when patients present with patient-related risk factors such as a high smile line, thin periodontal soft tissues, and compromised bone support. Patient perceptions and desires greatly influence and determine how well an individual patient accepts the implant outcome.
Although infrequently reported, the “esthetic success” and “patient satisfaction” of implant therapy needs to be included when considering the results of implant therapy. There have been a number of proposed methods to evaluate esthetic results, yet the reporting of esthetic parameters in the scientific literature is scarce.9 There is a restorative index that appraises the “white” esthetics of the final restoration,37 a soft tissue or “pink” esthetic score that considers soft tissue parameters,30 and an esthetic index that uses a combination of pink and white esthetic scores focusing on the visible part of the implant restoration.8 These indices are aimed at quantifying the esthetic result, which could then present an objective method of judging “implant esthetic success.”
In a survey of patient satisfaction, more than 90% were completely satisfied both in terms of function and esthetics.54 The study consisted of a questionnaire given to 104 patients 5 to 15 years (mean = 10.2 years) after implant placement to assess their subjective perception of implant treatment. Of these patients, 48% were treated with single implant crowns and 52% were treated with fixed partial dentures. The survival rate for all implants was 93%. A great majority of patients had favorable responses to the questions regarding function, esthetics, hygiene and cost. Table 80-2 lists the percentage of patients responding with highly satisfied or satisfied to each category. Comparing chewing comfort for teeth or implants, 72.1% perceived no difference, 17.3% felt more secure chewing on teeth, and 7.7% felt more secure chewing on implants.
TABLE 80-2 Patient Satisfaction with Implant Treatment*
| Implant Experience | Highly Satisfied or Satisfied (%) |
|---|---|
| Function/chewing | 97 |
| Phonetics | 96 |
| Esthetics | 97 |
| Oral hygiene ease | 93 |
| Complete fulfillment | 92 |
| Do treatment again | 94 |
| Recommend to friend or relative | 89 |
| Reasonable/justified cost | 87 |
* This table lists the percentage of patients subjectively responding with highly satisfied or satisfied to survey questions about their implant experience. More than 90% responded favorably and felt that implant treatment was positive.
Based on data from Pjetursson BE, Karoussis I, Burgin W, et al: Clin Oral Implants Res 16:185–193, 2005.
In another survey study, patient satisfaction with implant-supported prostheses in totally edentulous jaws was evaluated.59 Patient experience with an implant-supported prosthesis was over a period of 10 years. Most of the 135 patients (97%) reported overall satisfaction with treatment. Chewing satisfaction was reported as good or very good by all but one patient (99.3%). Improved lifestyle and greater self-confidence in public was reported by 75% and 82% of patients, respectively.
A systematic review of the literature including all randomized controlled trials published in English or French up to April 2007 comparing mandibular conventional dentures and implant overdentures in adult edentulous patients identified eight publications for metaanalysis.25 The study reported that patients were more satisfied with implant overdentures when compared with conventional mandibular dentures. However, there was a lack of evidence to show a patient’s perception on the impact of mandibular implant overdentures on general health.
Conclusion
The utilization of dental implants to replace missing teeth is highly predictable, advantageous, and beneficial for patients. Because of variations in implant design, study protocols, and populations studied, results are difficult to compare and an absolute definition of implant success is elusive. The results of implant treatment are reported using a wide range of criteria from simply being present (survival) to being in function without complications (success). It is challenging to compare the results of one study to another because of the number of variables that continue to change. Clinical research suggests that certain risk factors may decrease success rates for some patients. Understanding what is being reported in the literature will help readers to appreciate implant treatment results.
![]() Science Transfer
Science Transfer
Successful implant therapy has many varied criteria. In some studies, implant survival was considered a success and in these cases, success rates were over 90%. However, in contrast to a tooth, an implant can lose a high proportion of its bone support, but if there is still osseointegration at the apical part of the implant, it may remain in function without symptoms. If the presence of unfavorable responses to implants, such as bone loss, periimplantitis, and pocket depth, are considered, the success rates will be lower than that associated with survival.
Clinicians should be aware that unfavorable responses and implant loss are more common in the type IV bone found in the posterior maxilla compared to the denser bone seen in the anterior mandible. Implants placed in bone augmentation sites have an increased complication rate compared to implants placed in native bone, but the survival rates are similar.
Smoking and uncontrolled diabetes are associated with higher failure rates and a higher incidence of complications, thus these patients need to get control of their diabetes and stop smoking to optimize implant therapy.
New generation implants with roughened surface topology have better osseointegration than the machined surface implants, and clinicians can expect higher success and higher survival using a variety of improved surface technologies.
1 Adell R, Eriksson B, Lekholm U, et al. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990;5:347-359.
2 Adell R, Lekholm U, Rockler B, et al. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387-416.
3 Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11-25.
4 Anner R, Grossmann Y, Anner Y, et al. Smoking, diabetes mellitus, periodontitis, and supportive periodontal treatment as factors associated with dental implant survival: a long-term retrospective evaluation of patients followed for up to 10 years. Implant Dent. 2010;19:57-64.
5 Apse P, Zarb GA, Schmitt A, et al. The longitudinal effectiveness of osseointegrated dental implants. The Toronto Study: peri-implant mucosal response. Int J Periodontics Restorative Dent. 1991;11:94-111.
6 Araujo M, Linder E, Lindhe J. Effect of a xenograft on early bone formation in extraction sockets: an experimental study in dog. Clin Oral Implants Res. 2009;20:1-6.
7 Attard NJ, Zarb GA. Immediate and early implant loading protocols: a literature review of clinical studies. J Prosthet Dent. 2005;94:242-258.
8 Belser UC, Grutter L, Vailati F, et al. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol. 2009;80:140-151.
9 Belser UC, Schmid B, Higginbottom F, et al. Outcome analysis of implant restorations located in the anterior maxilla: a review of the recent literature. Int J Oral Maxillofac Implants. 2004;19(Suppl):30-42.
10 Brånemark PI. Osseointegration and its experimental background. J Prosthet Dent. 1983;50:399-410.
11 Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1-132.
12 Buser D, Weber HP, Bragger U, et al. Tissue integration of one-stage ITI implants: 3-year results of a longitudinal study with Hollow-Cylinder and Hollow-Screw implants. Int J Oral Maxillofac Implants. 1991;6:405-412.
13 Cardaropoli D, Cardaropoli G. Preservation of the postextraction alveolar ridge: a clinical and histologic study. Int J Periodontics Restorative Dent. 2008;28:469-477.
14 Chen ST, Wilson TGJr. Hammerle, CH: Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004;19(Suppl):12-25.
15 Chiapasco M. Early and immediate restoration and loading of implants in completely edentulous patients. Int J Oral Maxillofac Implants. 2004;19(Suppl):76-91.
16 Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006;17(Suppl 2):136-159.
17 De Bruyn H, Collaert B. The effect of smoking on early implant failure. Clin Oral Implants Res. 1994;5:260-264.
18 Del Fabbro M, Testori T, Francetti L, et al. Systematic review of survival rates for immediately loaded dental implants. Int J Periodontics Restorative Dent. 2006;26:249-263.
19 DeLuca S, Habsha E, Zarb GA. The effect of smoking on osseointegrated dental implants. Part I: implant survival. Int J Prosthodont. 2006;19:491-498.
20 DeLuca S, Zarb G. The effect of smoking on osseointegrated dental implants. Part II: Peri-implant bone loss. Int J Prosthodont. 2006;19:560-566.
21 Dowell S, Oates TW, Robinson M. Implant success in people with type 2 diabetes mellitus with varying glycemic control: a pilot study. J Am Dent Assoc. 2007;138:355-361. quiz 397-358
22 Eckert SE, Choi YG, Sanchez AR, et al. Comparison of dental implant systems: quality of clinical evidence and prediction of 5-year survival. Int J Oral Maxillofac Implants. 2005;20:406-415.
23 Ellegaard B, Baelum V, Kolsen-Petersen J. Non-grafted sinus implants in periodontally compromised patients: a time-to-event analysis. Clin Oral Implants Res. 2006;17:156-164.
24 Ellegaard B, Kolsen-Petersen J, Baelum V. Implant therapy involving maxillary sinus lift in periodontally compromised patients. Clin Oral Implants Res. 1997;8:305-315.
25 Emami E, Heydecke G, Rompre PH, et al. Impact of implant support for mandibular dentures on satisfaction, oral and general health-related quality of life: a meta-analysis of randomized-controlled trials. Clin Oral Implants Res. 2009;20:533-544.
26 Esposito M, Grusovin MG, Coulthard P, et al. A 5-year follow-up comparative analysis of the efficacy of various osseointegrated dental implant systems: a systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2005;20:557-568.
27 Esposito M, Grusovin MG, Willings M, et al. The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2007;22:893-904.
28 Fiorellini JP, Nevins ML. Localized ridge augmentation/preservation. A systematic review. Ann Periodontol. 2003;8:321-327.
29 Fugazzotto PA, Beagle JR, Ganeles J, et al. Success and failure rates of 9 mm or shorter implants in the replacement of missing maxillary molars when restored with individual crowns: preliminary results 0 to 84 months in function. A retrospective study. J Periodontol. 2004;75:327-332.
30 Furhauser R, Florescu D, Benesch T, et al. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res. 2005;16:639-644.
31 Ganeles J, Wismeijer D. Early and immediately restored and loaded dental implants for single-tooth and partial-arch applications. Int J Oral Maxillofac Implants. 2004;19(Suppl):92-102.
32 Hammerle CH, Jung RE, Feloutzis A. A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients. J Clin Periodontol. 2002;29(Suppl 3):226-231. discussion 232-223
33 Hammerle CH, van Steenberghe D. The first EAO Consensus Conference 16-19 February 2006, Pfaffikon, Switzerland. Clin Oral Implants Res. 2006;17(Suppl 2):1.
34 Jaffin RA, Berman CL. The excessive loss of Brånemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991;62:2-4.
35 Jaffin RA, Kumar A, Berman CL. Immediate loading of dental implants in the completely edentulous maxilla: a clinical report. Int J Oral Maxillofac Implants. 2004;19:721-730.
36 Javed F, Romanos GE. Impact of diabetes mellitus and glycemic control on the osseointegration of dental implants: a systematic literature review. J Periodontol. 2009;80:1719-1730.
37 Jensen OT, Cockrell R, Kuhike L, et al. Anterior maxillary alveolar distraction osteogenesis: a prospective 5-year clinical study. Int J Oral Maxillofac Implants. 2002;17:52-68.
38 Jokstad A, Carr AB. What is the effect on outcomes of time-to-loading of a fixed or removable prosthesis placed on implant(s)? Int J Oral Maxillofac Implants. 2007;22(Suppl):19-48.
39 Karoussis IK, Kotsovilis S, Fourmousis I. A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin Oral Implants Res. 2007;18:669-679.
40 Karoussis IK, Salvi GE, Heitz-Mayfield LJ, et al. Long-term implant prognosis in patients with and without a history of chronic periodontitis: a 10-year prospective cohort study of the ITI Dental Implant System. Clin Oral Implants Res. 2003;14:329-339.
41 Klokkevold PR, Han TJ. How do smoking, diabetes, and periodontitis affect outcomes of implant treatment? Int J Oral Maxillofac Implants. 2007;22(Suppl):173-202.
42 Klokkevold PR, Johnson P, Dadgostari S, et al. Early endosseous integration enhanced by dual acid etching of titanium: a torque removal study in the rabbit. Clin Oral Implants Res. 2001;12:350-357.
43 Klokkevold PR, Nishimura RD, Adachi M, et al. Osseointegration enhanced by chemical etching of the titanium surface. A torque removal study in the rabbit. Clin Oral Implants Res. 1997;8:442-447.
44 Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001;22:199-206. quiz 208
45 Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9:332-343.
46 Lekholm U, Gunne J, Henry P, et al. Survival of the Brånemark implant in partially edentulous jaws: a 10-year prospective multicenter study. Int J Oral Maxillofac Implants. 1999;14:639-645.
47 Lekholm U, Zarb G: Patient Selection and Preparation. In Brånemark PI, Zarb G and Albrektsson T, editors: Tissue-Integrated Prothesis: Osseointegration in Clinical Dentistry, Chicago, 1987, Quintessence Publishing, Co., Inc.
48 Leonhardt A, Grondahl K, Bergstrom C, et al. Long-term follow-up of osseointegrated titanium implants using clinical, radiographic and microbiological parameters. Clin Oral Implants Res. 2002;13:127-132.
49 Mayfield L. Immediate delayed and late submerged and transmucosal implants. Berlin: Quintessence; 1999. 520-534
50 Mengel R, Flores-de-Jacoby L. Implants in patients treated for generalized aggressive and chronic periodontitis: a 3-year prospective longitudinal study. J Periodontol. 2005;76:534-543.
51 Mengel R, Flores-de-Jacoby L. Implants in regenerated bone in patients treated for generalized aggressive periodontitis: a prospective longitudinal study. Int J Periodontics Restorative Dent. 2005;25:331-341.
52 Mengel R, Schroder T, Flores-de-Jacoby L. Osseointegrated implants in patients treated for generalized chronic periodontitis and generalized aggressive periodontitis: 3- and 5-year results of a prospective long-term study. J Periodontol. 2001;72:977-989.
53 Moy PK, Medina D, Shetty V, et al. Dental implant failure rates and associated risk factors. Int J Oral Maxillofac Implants. 2005;20:569-577.
54 Pjetursson BE, Karoussis I, Burgin W, Bragger U, Lang NP. Patients’ satisfaction following implant therapy. A 10-year prospective cohort study. Clin Oral Implants Res. 2005;16:185-193.
55 Pjetursson BE, Tan K, Lang NP, et al. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004;15:625-642.
56 Rocci A, Martignoni M, Gottlow J. Immediate loading of Brånemark System TiUnite and machined-surface implants in the posterior mandible: a randomized open-ended clinical trial. Clin Implant Dent Relat Res. 2003;5(Suppl 1):57-63.
57 Roos J, Sennerby L, Lekholm U, et al. A qualitative and quantitative method for evaluating implant success: a 5-year retrospective analysis of the Brånemark implant. Int J Oral Maxillofac Implants. 1997;12:504-514.
58 Rosenberg ES, Cho SC, Elian N, et al. A comparison of characteristics of implant failure and survival in periodontally compromised and periodontally healthy patients: a clinical report. Int J Oral Maxillofac Implants. 2004;19:873-879.
59 Sandberg G, Stenberg T, Wikblad K. Ten years of patients’ experiences with fixed implant-supported prostheses. J Dent Hyg. 2000;74:308-316.
60 Schincaglia GP, Marzola R, Scapoli C, et al. Immediate loading of dental implants supporting fixed partial dentures in the posterior mandible: a randomized controlled split-mouth study–machined versus titanium oxide implant surface. Int J Oral Maxillofac Implants. 2007;22:35-46.
61 Schnitman PA, Wohrle PS, Rubenstein JE. Immediate fixed interim prostheses supported by two-stage threaded implants: methodology and results. J Oral Implantol. 1990;16:96-105.
62 Schnitman PA, Wohrle PS, Rubenstein JE, et al. Ten-year results for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants. 1997;12:495-503.
63 Schropp L, Wenzel A, Kostopoulos L, et al. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23:313-323.
64 Schulte W, Kleineikenscheidt H, Lindner K, et al. [The Tubingen immediate implant in clinical studies]. Dtsch Zahnarztl Z. 1978;33:348-359.
65 Schwartz-Arad D, Chaushu G. Immediate implant placement: a procedure without incisions. J Periodontol. 1998;69:743-750.
66 Stach RM, Kohles SS. A meta-analysis examining the clinical survivability of machined-surfaced and osseotite implants in poor-quality bone. Implant Dent. 2003;12:87-96.
67 Sullivan DY, Sherwood RL, Porter SS. Long-term performance of Osseotite implants: a 6-year clinical follow-up. Compend Contin Educ Dent. 2001;22:326-328. 330, 332-324
68 Tonetti MS, Hammerle CH. Advances in bone augmentation to enable dental implant placement: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35:168-172.
69 Wagenberg B, Froum SJ. A retrospective study of 1925 consecutively placed immediate implants from 1988 to 2004. Int J Oral Maxillofac Implants. 2006;21:71-80.
70 Wang F, Song YL, Li DH, et al. Type 2 diabetes mellitus impairs bone healing of dental implants in GK rats. Diabetes Res Clin Pract. 2010.
71 Wennstrom JL, Ekestubbe A, Grondahl K, et al. Oral rehabilitation with implant-supported fixed partial dentures in periodontitis-susceptible subjects. A 5-year prospective study. J Clin Periodontol. 2004;31:713-724.
72 Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part I: Surgical results. J Prosthet Dent. 1990;63:451-457.
73 Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto Study. Part II: The prosthetic results. J Prosthet Dent. 1990;64:53-61.
74 Zarb GA, Schmitt A. Osseointegration and the edentulous predicament. The 10-year-old Toronto study. Br Dent J. 1991;170:439-444.