Nursing Diagnosis
• Discuss the purposes of using nursing diagnosis in practice.
• Differentiate among a nursing diagnosis, medical diagnosis, and collaborative problem.
• Discuss the relationship of critical thinking to the nursing diagnostic process.
• Describe the steps of the nursing diagnostic process.
• Explain how defining characteristics and the etiological process individualize a nursing diagnosis.
http://evolve.elsevier.com/Potter/fundamentals/
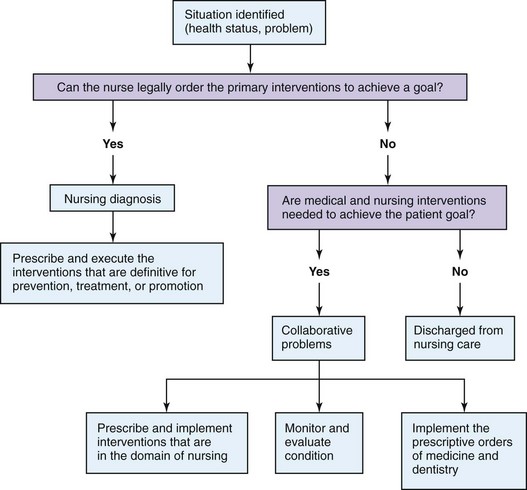
During the nursing assessment process (see Chapter 16) a nurse gathers the information needed to make diagnostic conclusions about patient care. A diagnosis is a clinical judgment based on information. You review information collected about a patient, see cues and patterns in the data, and identify the patient’s specific health care problems. Some of the conclusions lead to identifying nursing diagnoses, whereas others do not. Diagnostic conclusions include problems treated primarily by nurses (nursing diagnoses) and those requiring treatment by several disciplines (collaborative problems). Together nursing diagnoses and collaborative problems represent the range of patient conditions that require nursing care (Carpenito-Moyet, 2009).
When physicians refer to commonly accepted medical diagnoses such as diabetes mellitus or osteoarthritis, they all know the meaning of the diagnoses and the standard approaches for treatment. A medical diagnosis is the identification of a disease condition based on a specific evaluation of physical signs, symptoms, the patient’s medical history and the results of diagnostic tests and procedures. Physicians are licensed to treat diseases and conditions described in medical diagnostic statements.
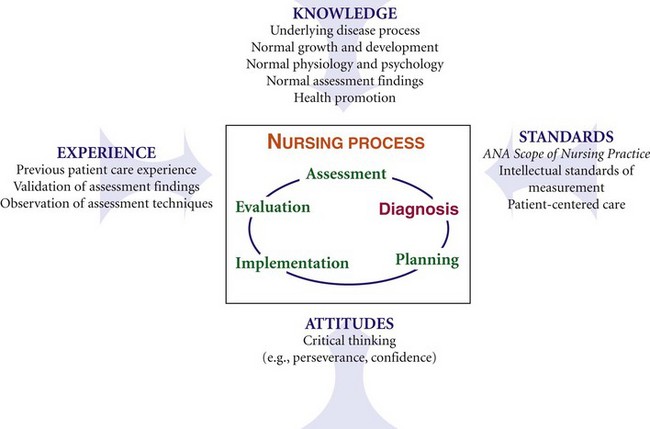
Nursing has a similar diagnostic language. Nursing diagnosis, the second step of the nursing process (Fig. 17-1), classifies health problems within the domain of nursing. A nursing diagnosis such as acute pain or nausea is a clinical judgment about individual, family, or community responses to actual and potential health problems or life processes that the nurse is licensed and competent to treat (NANDA International, 2012). What makes the nursing diagnostic process unique is having patients involved, when possible, in the process.
A collaborative problem is an actual or potential physiological complication that nurses monitor to detect the onset of changes in a patient’s status (Carpenito-Moyet, 2009). When collaborative problems develop, nurses intervene in collaboration with personnel from other health care disciplines. Nurses manage collaborative problems such as hemorrhage, infection, and paralysis using medical, nursing, and allied health (e.g., physical therapy) interventions. For example, a patient with a surgical wound is at risk for developing an infection; thus a physician prescribes antibiotics. The nurse monitors the patient for fever and other signs of infection and implements appropriate wound care measures. A dietitian recommends a therapeutic diet high in protein and nutrients to promote wound healing.
Selecting the correct nursing diagnosis on the basis of an assessment involves diagnostic expertise (i.e., being able to make quick and accurate conclusions from patient data) (Cho, Staggers, and Park, 2010). This is essential because accurate diagnosis of patient problems ensures that you select more effective and efficient nursing interventions. Diagnostic expertise improves with time. Consider the case study involving Mr. Jacobs and his nurse, Tonya Moore.
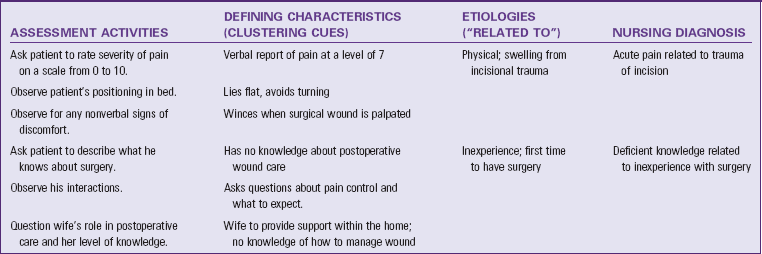
During her assessment Tonya gathers information suggesting that Mr. Jacobs possibly has a number of health problems. The data about Mr. Jacobs show patterns in four areas: comfort, requesting information about postoperative care, mobility restriction, and worries about his future and his relationship with Mrs. Jacobs. Selecting specific diagnostic labels for these problem areas allows Tonya to develop a relevant and appropriate plan of care. For example, with respect to Mr. Jacobs’ request for information, there are two accepted nursing diagnostic labels for problems related to knowledge: deficient knowledge and readiness for enhanced knowledge. Knowing the difference between these two diagnoses and identifying which one applies to Mr. Jacobs is key to selecting the right type of interventions for his problem. A physician needs to rule out rheumatoid arthritis versus osteoarthritis to be sure that a patient receives the right form of medical treatment. Tonya analyzes her information about Mr. Jacobs and identifies the factors that show the pattern that fits a specific diagnosis. This means that Tonya considers that the patient has no knowledge about or experience with postoperative wound care and freely asks questions. Tonya knows that these factors are defining characteristics that allow her to make an accurate nursing diagnosis.
History of Nursing Diagnosis
Nursing diagnosis was first introduced in the nursing literature in 1950 (McFarland and McFarlane, 1989). Fry (1953) proposed the formulation of nursing diagnoses and an individualized nursing care plan to make nursing more creative. This emphasized the nurse’s independent practice (e.g., patient education and symptom relief) compared with the dependent practice driven by physicians’ orders (e.g., medication administration and intravenous fluids). Initially professional nursing did not support nursing diagnoses. The Model Nurse Practice Act of the American Nurses Association (ANA) (1955) excluded diagnosis or prescriptive therapies. As a result, few nurses used nursing diagnoses in their practice.
When Yura and Walsh (1967) developed the theory of the nursing process, it included four parts: assessment, planning, implementation, and evaluation. However, nurse leaders soon recognized that assessment data needed to be clustered into patterns and interpreted before nurses could complete the remaining steps of the process (NANDA International, 2012). You cannot plan and then intervene correctly if you do not know the problems with which you are dealing. In 1973 the first national conference to identify the interpretations of data that represent the health conditions that are of a concern to nursing was held. The first conference on nursing diagnosis identified and defined 80 nursing diagnoses (Gebbie, 1998). The list continues to grow on the basis of nursing research and the work of members of the North American Nursing Diagnosis Association International (NANDA-I) (NANDA International, 2012).
With use of the term nursing diagnosis, nurses make diagnostic conclusions and therefore the clinical decisions necessary for safe and effective nursing practice. The ANA’s paper Scope of Nursing Practice (1987), which defined nursing as the diagnosis and treatment of human responses to health and illness, helped strengthen the definition of nursing diagnosis. In 1980 and 1995 the ANA included diagnosis as a separate activity in its publication Nursing: a Social Policy Statement (ANA, 2003). It continues today in the ANA’s most recent policy statement (ANA, 2010). As a result, most state Nurse Practice Acts include nursing diagnosis as part of the domain of nursing practice.
Research in the field of nursing diagnosis continues to grow (Box 17-1). As a result, NANDA-I continually develops and adds new diagnostic labels to the NANDA International listing (Box 17-2). The use of standard formal nursing diagnostic statements serves several purposes in nursing practice:
• Provides a precise definition of a patient’s problem that gives nurses and other members of the health care team a common language for understanding the patient’s needs
• Allows nurses to communicate (e.g., written and electronic) what they do among themselves with other health care professionals and the public
• Distinguishes the nurse’s role from that of the physician or other health care provider
• Helps nurses focus on the scope of nursing practice
• Fosters the development of nursing knowledge
• Promotes creation of practice guidelines that reflect the essence of nursing
Critical Thinking and the Nursing Diagnostic Process
The diagnostic process requires you to use critical thinking (see Chapter 15). In the practice of nursing it is important for you to know nursing diagnoses, their definitions and the defining characteristics for making diagnoses, related factors pertinent to the diagnoses, and the interventions suited for treating the diagnoses (NANDA International, 2012). This means that you need to know how to access this information easily within the agency in which you work because the information is much too extensive for you to memorize. Sources of information about nursing diagnoses include faculty, advanced practice nurses, documentation systems, and in some settings practice guidelines or protocols. Experience also plays a role in becoming adept at nursing diagnosis. Learn from the patients for whom you care because this helps you think more carefully about your assessment information and what it means. The application of critical thinking attitudes and standards helps you to be thorough, comprehensive, and accurate when identifying nursing diagnoses that apply to your patients.
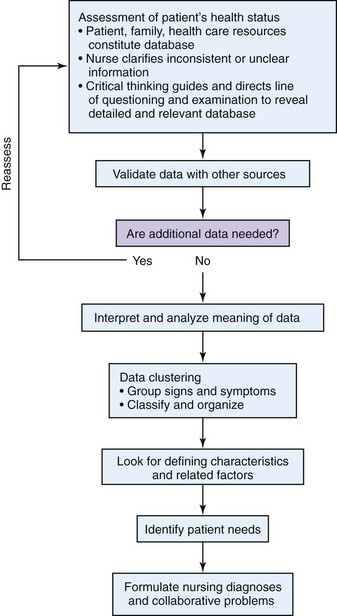
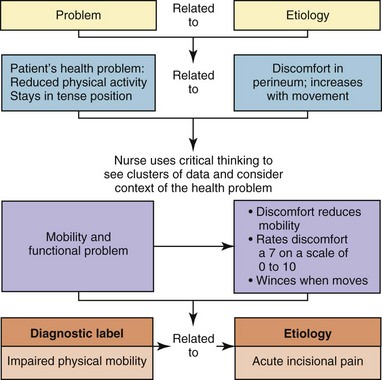
The diagnostic reasoning process involves using the assessment data you gather about a patient to logically explain a clinical judgment, in this case a nursing diagnosis. The diagnostic process flows from the assessment process and includes decision-making steps (Fig. 17-2). These steps include data clustering, identifying patient health problems, and formulating the diagnosis.
Data Clustering
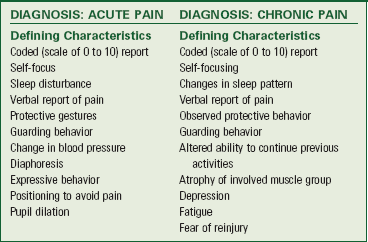
A data cluster is a set of signs or symptoms gathered during assessment that you group together in a logical way. In the case of Mr. Jacobs, Tonya clustered together the signs and symptoms of “patient wincing when incision palpated,” “patient acknowledges discomfort over incision,” “patient rates discomfort a 7 on a scale of 0 to 10,” and “pain increases with movement.” Tonya analyzed these data to recognize the pattern of a comfort problem. Data clusters are patterns of data that contain defining characteristics, the clinical criteria that are observable and verifiable. Each clinical criterion is an objective or subjective sign, symptom, or risk factor that, when analyzed with other criteria, leads to a diagnostic conclusion. Each NANDA-I–approved nursing diagnosis has an identified set of defining characteristics that support identification of a nursing diagnosis (NANDA International, 2012). You learn to recognize patterns of defining characteristics from your patient assessments and then readily select the corresponding diagnosis. Working with similar patients over a period of time helps you recognize clusters of defining characteristics, but remember that each patient is unique and requires an individualized diagnostic approach. Box 17-3 shows two examples of approved nursing diagnoses and their associated defining characteristics.
Interpretation—Identifying Health Problems
While analyzing clusters of data, you begin to consider the patient’s health problems. Your interpretation of the information allows you to select among various diagnoses the ones that apply to your patient. It is critical to select the correct diagnostic label for a patient’s need. Usually from assessment to diagnosis you move from general information to specific. It helps to think of the problem identification phase in assessment as the general health care problem and the formulation of the nursing diagnosis as the specific health problem. For example, after analyzing Mr. Jacob’s problem with comfort, Tonya begins to identify data needed for a specific pain diagnosis.
Often a patient has defining characteristics that apply to more than one diagnosis. For example, Mr. Jacobs provided a verbal report of pain and showed protective behavior in minimizing movement while lying in bed. Both of these defining characteristics possibly indicates that the patient has either acute pain or chronic pain as nursing diagnoses. Knowing that there are similar diagnoses directs you to gather more information to clarify your interpretation. For example, Tonya checks Mr. Jacobs’ blood pressure after he rates his discomfort a 7 on a 10-point rating scale. She notes that his blood pressure is elevated, a defining characteristic unique to the diagnosis of acute pain. When interpreting data to form a diagnosis, remember that the absence of certain defining characteristics suggests that you reject a diagnosis under consideration. Thus in the same example, if Tonya’s assessment eliminates the signs of fatigue, fear of reinjury, and depression, it is less likely Mr. Jacobs’ is having chronic pain. In addition, Tonya recognizes that the pain source is the patient’s incision and not some underlying chronic problem. The correct diagnosis for Mr. Jacobs is acute pain. Always examine the defining characteristics in your database carefully to support or eliminate a nursing diagnosis. To be more accurate, review all characteristics, eliminate irrelevant ones, and confirm the relevant ones.
Formulating a Nursing Diagnosis
To individualize a nursing diagnosis further, you identify the associated related factor. A related factor is a condition, historical factor, or etiology that gives a context for the defining characteristics and shows a type of relationship with the nursing diagnosis (NANDA International, 2012). A related factor allows you to individualize a nursing diagnosis for a specific patient. For example, Mr. Jacobs has just undergone surgery and has an incision in the perineal area. This information is important in the context of the nature of his discomfort, and it is used in making a final diagnosis. Placing a diagnosis into the context of the patient’s situation clarifies the nature of the patient’s health problem. Tonya considers the nature of Mr. Jacobs’ pain and identifies his diagnosis as acute pain related to trauma of an incision. When Tonya is ready to form her plan of care and select nursing interventions, this concise nursing diagnosis allows her to select therapies suited to postoperative pain management. For example, acute pain related to trauma of an incision is more prescriptive for Mr. Jacobs’ situation than a nursing diagnosis of acute pain related to muscular injury.
While focusing on patterns of defining characteristics, you also compare a patient’s pattern of data with data that are consistent with normal, healthful patterns. Use accepted norms as the basis for comparison and judgment. This includes using laboratory and diagnostic test values, professional standards, and normal anatomical or physiological limits. When comparing patterns, judge whether the grouped signs and symptoms are expected for the patient and whether they are within the range of healthful responses. Isolate any defining characteristics not within healthy norms to allow you to identify a specific problem.
Nursing diagnoses provide the basis for selection of nursing interventions to achieve outcomes for which you, as a nurse, are accountable (NANDA International, 2012). A nursing diagnosis focuses on a patient’s actual or potential response to a health problem rather than on the physiological event, complication, or disease. A nurse cannot independently treat a medical diagnosis such as a tumor of the prostate. However, Tonya manages Mr. Jacobs’ postoperative care, monitoring his postoperative progress and wound care, fluid administration, and medication therapy to prevent collaborative problems from developing. Collaborative problems occur or probably will occur in association with a specific disease, trauma, or treatment (Carpenito-Moyet, 2009). You need nursing knowledge to assess a patient’s specific risk for these problems, identify the problems early, and take preventive action (Fig. 17-3). Critical thinking is necessary in identifying nursing diagnoses and collaborative problems so you appropriately individualize care for your patients.
Types of Nursing Diagnoses
NANDA-I (2012) identifies three types of nursing diagnoses: actual diagnoses, risk diagnoses, and health promotion diagnoses. An actual nursing diagnosis describes human responses to health conditions or life processes that exist in an individual, family, or community. Defining characteristics support the diagnostic judgment (NANDA International, 2012). The selection of an actual diagnosis indicates that there are sufficient assessment data to establish the nursing diagnosis. Tonya assessed Mr. Jacobs as having discomfort from the prostatectomy incision with a severity rated at 7 on a 10-point rating scale. The pain increased with movement. As a result of the pain, Mr. Jacobs has limited movement in bed. Acute pain is an actual nursing diagnosis. Examples of other actual diagnoses include:
A risk nursing diagnosis describes human responses to health conditions or life processes that may develop in a vulnerable individual, family, or community (NANDA International, 2012). These diagnoses do not have related factors or defining characteristics because they have not occurred yet. Instead a risk diagnosis has risk factors. Risk factors are the environmental, physiological, psychological, genetic, or chemical elements that place a person at risk for a health problem. For example, after Mr. Jacobs’ surgery, the presence of his incision, an open wound, poses a risk for a hospital-acquired infection. The key assessment for a risk diagnosis is the presence of risk factors (e.g., an incision and the hospital environment) that support a patient’s vulnerability. The risk factors are the diagnostic-related factors that help in planning preventive health care measures. In Mr. Jacobs’ case risk for infection is appropriate for his condition. Other examples of risk nursing diagnoses include:
A health promotion nursing diagnosis is a clinical judgment of a person’s, family’s, or community’s motivation, desire, and readiness to increase well-being and actualize human health potential as expressed in their readiness to enhance specific health behaviors such as nutrition and exercise. Health promotion diagnoses can be used in any health state and do not require current levels of wellness (NANDA International, 2012). A person’s readiness is supported by defining characteristics. Examples of health promotion nursing diagnoses include:
Components of a Nursing Diagnosis
When communicating a nursing diagnosis, through either discussions with health care colleagues or documentation of your care, it is important to use the language adopted within an agency. Most settings use a two-part format in labeling a nursing diagnosis: the NANDA-I diagnostic label followed by a statement of a related factor (Table 17-1). The two-part format provides a diagnosis meaning and relevance for a particular patient.
TABLE 17-1
NANDA International Two-Part Nursing Diagnosis Format
| DIAGNOSTIC STATEMENT | EXAMPLES OF RELATED FACTORS |
| Acute pain | Biological, chemical, physical, or psychological injury agents (e.g., inflammation, edema, burn) |
| Anxiety | Change (economic status, environment, health status, role), familial association, maturational crisis, situational crisis, stress, threat of death, unmet needs |
| Impaired urinary elimination | Anatomical obstruction, urinary tract infection, sensory motor impairment) |
| Impaired skin integrity | Fluid retention, age extremes, hyperthermia, mechanical factors (e.g., shearing, pressure), medications, moisture, physical immobilization, impaired sensation |
Diagnostic Label
The diagnostic label is the name of the nursing diagnosis as approved by NANDA International (see Box 17-2). It describes the essence of a patient’s response to health conditions in as few words as possible. All NANDA-I approved diagnoses also have a definition. The definition describes the characteristics of the human response identified. You refer to definitions of nursing diagnoses to assist in identifying a patient’s correct diagnosis, which helps especially when selecting between two diagnoses with similar defining characteristics. The diagnostic labels include descriptors used to give additional meaning to the diagnosis. For example, the diagnosis impaired physical mobility includes the descriptor impaired to describe the nature or change in mobility that best describes the patient’s response. Examples of other descriptors include compromised, decreased, deficient, delayed, effective, imbalanced, impaired, and increased.
Related Factors
The related factor is identified from the patient’s assessment data and is the reason the patient is displaying the nursing diagnosis. The related factor is associated with a patient’s actual or potential response to the health problem and can change by using specific nursing interventions. Related factors for NANDA-I diagnoses include four categories: pathophysiological (biological or psychological), treatment-related, situational (environmental or personal), and maturational (Carpenito-Moyet, 2009). The “related to” phrase is not a cause-and-effect statement. It indicates that the etiology contributes to or is associated with the patient’s diagnosis (Fig. 17-4). The inclusion of the “related to” phrase requires you to use critical thinking to individualize the nursing diagnosis and then select nursing interventions (Table 17-2).
TABLE 17-2
Comparison of Interventions for Nursing Diagnoses with Different Related Factors
| NURSING DIAGNOSES | RELATED FACTOR | INTERVENTIONS |
| Patient A | ||
| Anxiety | Uncertainty over surgery | Provide detailed instructions about the surgical procedure, recovery process, and postoperative care activities. Plan formal time for patient to ask questions. |
| Impaired physical mobility | Acute pain | Administer analgesics 30 minutes before planned exercise. Instruct patient in technique to splint painful site during activity. |
| Patient B | ||
| Anxiety | Loss of job | Consult with social worker to arrange for job counseling. Encourage patient to continue health promotion activities (e.g., exercise, routine social activities). |
| Impaired physical mobility | Musculoskeletal injury | Have patient perform active range-of-motion exercises to affected extremity every 2 hours. Instruct patient on use of three-point crutch gait. |
The etiology or related factor of a nursing diagnosis is always within the domain of nursing practice and a condition that responds to nursing interventions. Sometimes health care providers record medical diagnoses as the etiology of the nursing diagnosis. This is incorrect. Nursing interventions do not change a medical diagnosis. However, you direct nursing interventions at behaviors or conditions that you are able to treat or manage. For example, the nursing diagnosis acute pain related to prostatectomy is incorrect. Nursing actions do not affect the medical diagnosis of the surgical removal of the prostate gland. Rewording the diagnosis to read acute pain related to trauma of incision results in nursing interventions directed at appropriate wound care, using turning techniques to reduce stress on the suture line and offering nonpharmacological comfort measures (see Chapter 43). In the case of a risk nursing diagnosis, a risk factor is the related factor. Table 17-3 demonstrates the association between a nurse’s assessment of a patient, the clustering of defining characteristics, and the formulation of nursing diagnoses. The diagnostic process results in the formation of a total diagnostic label that allows you to develop an appropriate, patient-centered plan of care. The defining characteristics and relevant etiologies are from NANDA International (2012).
The PES Format
Some agencies prefer a three-part nursing diagnostic label. In this case the diagnostic label consists of the NANDA-I label, the related factor, and the defining characteristics (Ackley and Ladwig, 2011). This approach makes a diagnosis even more patient specific. The acronym PES stands for problem, etiology, and symptoms.
• P (problem)—NANDA-I label—Example: impaired physical mobility
• E (etiology or related factor)—Example: incisional pain
• S (symptoms or defining characteristics)—briefly lists defining characteristic(s) that show evidence of the health problem. Example: evidenced by restricted turning and positioning
PES diagnostic statement: Impaired physical mobility related to incisional pain, evidenced by restricted turning and positioning.
Cultural Relevance of Nursing Diagnoses
When you select nursing diagnoses, consider your patients’ cultural diversity. This includes knowing the cultural differences that affect how a patient defines health and illness and wants to be treated (Smith, 2007). It is important to consider your own cultural competence so you are more sensitive to a patient’s health care problems and the implications.
Here are examples of questions that contribute to making culturally competent nursing diagnoses (Smith, 2007):
• How has this health problem affected you and your family?
• What do you believe will help or fix the problem?
• What worries you the most about this problem?
• What do you expect from us, your nurses, to help maintain some of your cultural practices?
• What cultural practices do you do to keep yourself and your family well?
When you ask questions such as these, you use a patient-centered care approach that allows you to see the patient’s health situation through his or her eyes. When making a diagnosis, be sure to also consider how culture influences the related factor for your diagnostic statement. For example, impaired verbal communication related to cultural differences or noncompliance related to patient value system reflects diagnostic conclusions that consider a patient’s unique cultural needs.
Your own culture potentially influences the cues and defining characteristics that you select from your assessment. In an older but still relevant study, Wieck (1996) examined how cultural differences among nurses influenced the choice of defining characteristics in making nursing diagnoses. The researchers studied the diagnosis of pain within six different cultural groups of nurses. Generally the nurses were consistent in selecting defining characteristics. However, when diagnosing pain, some of the nurses did not select restlessness or grimace as defining characteristics. The nurses were not familiar with such characteristics because they were not common to how their own culture expressed pain. Cultural awareness and sensitivity improve your accuracy in making nursing diagnoses.
Concept Mapping Nursing Diagnoses
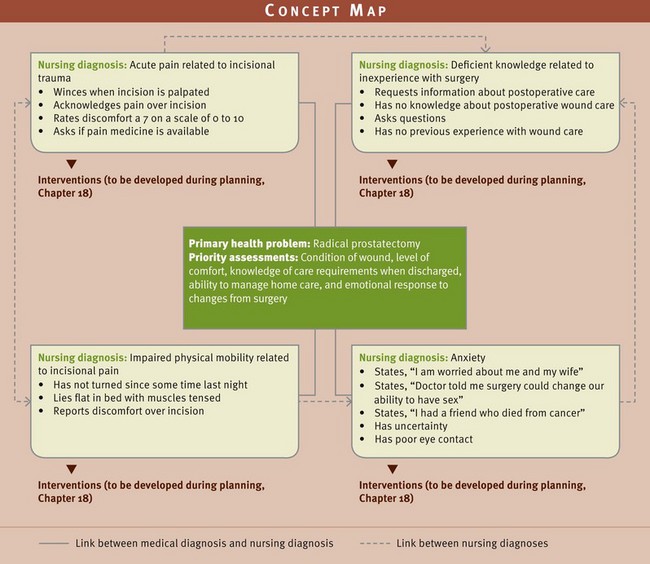
When caring for a patient or groups of patients, think critically about their needs and how to prevent problems from developing. Your holistic view of a patient heightens the challenge of thinking about all patient needs and problems. Few patients have single problems. Often you care for a patient with multiple nursing diagnoses. Therefore a picture of each patient usually consists of several interconnections between sets of data, all associated with identified patient problems. A concept map diagrams the critical thinking associated with making accurate diagnoses. It is one way to graphically represent the connections between concepts (nursing diagnoses) and ideas that are related to a central subject (e.g., the patient’s health problems). For each diagnosis you list defining characteristics and begin to see the connections or association among different diagnostic statements.
As you proceed in applying each step of the nursing process, your concept map expands with more detail about planned interventions (see Chapter 18). A concept map promotes critical thinking because you identify, graphically display, and link key concepts by organizing and analyzing information (Hsu and Hsieh, 2005).
Fig. 17-5 shows the next step in the development of Tonya’s concept map for Mr. Jacobs. Tonya began during the assessment step of the nursing process (see Chapter 16) to gather a database for Mr. Jacobs. Her assessment included Mr. Jacobs’ perspective of his health problems and the objective and subjective data she collected through observation and examination. She validated findings and added to the database as she learned new information. Data sources include physical, psychological, and sociocultural domains. Tonya applies clinical reasoning and intuition that reflect her own basic nursing knowledge, her past experiences with patients, patterns seen in similar situations, and reference to institutional standards and procedures (e.g., pain-management policies or postoperative teaching protocols). As Tonya begins to see patterns of defining characteristics, she places labels to identify the four nursing diagnoses that apply to Mr. Jacobs. She is also able to see the relationship among the diagnoses and connects them on the concept map. If Mr. Jacobs does not receive pain relief, Tonya knows from her experience in caring for patients with pain that he will have continued problems in achieving necessary mobility for recovery. The diagnoses of acute pain and impaired physical mobility are closely related. In addition, if pain is unrelieved, it will be difficult for Mr. Jacobs’ to be receptive to any patient teaching Tonya wants to provide about postoperative care, an intervention that will be later planned for deficient knowledge. If Mr. Jacobs’ remains anxious about the outcome of his surgery and whether he can fulfill his role sexually with his wife, this anxiety can heighten pain perception and influence his ability to learn. Concept mapping organizes and links information to allow you to see new wholes and appreciate the complexity of patient care (Ferrario, 2004). Tonya’s next step on the care map is to identify the appropriate nursing interventions for Mr. Jacobs’ care (see Chapter 18).
The advantage of a concept map is its central focus on the patient rather than the patient’s disease or health alteration. This encourages nursing students to concentrate on patients’ specific health problems and nursing diagnoses. The focus also promotes patient participation with the eventual plan of care.
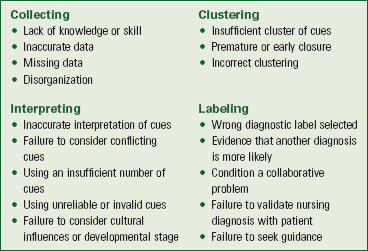
Sources of Diagnostic Errors
Errors may occur in the nursing diagnostic process during data collection, interpretation, clustering, and labeling of the diagnosis (Box 17-4). Chapter 16 reviews how to conduct a systematic assessment so you have all of the data necessary for making accurate and timely nursing diagnoses and collaborative problems. As a nurse always apply methodical critical thinking for an accurate nursing diagnostic process.
Errors in Interpretation and Analysis of Data
Following data collection, review your database to decide if it is accurate and complete. Review data to validate that measurable, objective physical findings support subjective data. For example, when a patient reports “difficulty breathing,” you also want to listen to lung sounds, assess respiratory rate, and measure the patient’s chest excursion. When you are not able to validate data, it signals an inaccurate match between clinical cues and the nursing diagnosis. Begin interpretation by identifying and organizing relevant assessment patterns to support the presence of patient problems. Be careful to consider conflicting cues or decide if there are insufficient cues to form a diagnosis.
Errors in Data Clustering
Errors in data clustering occur when data are clustered prematurely, incorrectly, or not at all. Premature closure of clustering occurs when you make the nursing diagnosis before grouping all data. For example, before his surgery, Mr. Jacobs experienced urinary incontinence and complained of urgency and nocturia. The nurse in the clinic clustered the available data and considered that impaired urinary elimination was a probable diagnosis. However, incorrect clustering occurs when you try to make a nursing diagnosis fit the signs and symptoms obtained. In this example further assessment revealed that the patient had bladder distention and dribbling and the type of incontinence was likely overflow incontinence. As a result of these findings the nurse was able to make a more accurate diagnosis, urinary retention. Always identify the nursing diagnosis from the data, not the reverse. An incorrect nursing diagnosis affects quality of patient care.
Errors in the Diagnostic Statement
Clinical reasoning leads to a higher quality of nursing diagnosis, which eventually leads to etiology-specific interventions and enhanced patient outcomes (Muller-Staub et al., 2008). The more competent you become in diagnostic reasoning, the more likely it is that you will correctly select diagnostic statements. This results in the appropriate selection of nursing interventions and patient outcomes during planning and implementation (see Chapters 18 and 19). Reduce errors by selecting appropriate, concise, and precise language using NANDA-I terminology. Be sure that the etiology portion of the diagnostic statement is within the scope of nursing to diagnose and treat. Additional guidelines to reduce errors in the diagnostic statement follow.
1. Identify the patient’s response, not the medical diagnosis (Carpenito-Moyet, 2009). Because the medical diagnosis requires medical interventions, it is legally inadvisable to include it in the nursing diagnosis. Change the diagnosis acute pain related to prostatectomy to acute pain related to trauma of an incision.
2. Identify a NANDA-I diagnostic statement rather than the symptom. Identify nursing diagnoses from a cluster of defining characteristics and not just a single symptom. One symptom is insufficient for problem identification. For example, dyspnea alone does not definitively lead you to a diagnosis. However, the pattern of dyspnea, shortness of breath, pain on inspiration, and productive cough with thick secretions are defining characteristics that lead you to the diagnosis of ineffective breathing pattern related to increased airway secretions.
3. Identify a treatable etiology or risk factor rather than a clinical sign or chronic problem that is not treatable through nursing intervention. An accurate etiology allows you to select nursing interventions directed toward correcting the etiology of the problem or minimizing the patient’s risk. A diagnostic test or a chronic dysfunction is not an etiology or a condition that a nursing intervention is able to treat. A patient with fractured ribs likely has pain when inhaling; impaired chest excursion; and slower, shallow respirations. An x-ray film may show atelectasis (collapse of alveolar air sacs) in the area affected. The nursing diagnosis of ineffective breathing pattern related to shallow respirations is an incorrect diagnostic statement. Ineffective breathing pattern related to pain in chest is more accurate.
4. Identify the problem caused by the treatment or diagnostic study rather than the treatment or study itself. Patients experience many responses to diagnostic tests and medical treatments. These responses are the area of nursing concern. The patient who has angina and is scheduled for a cardiac catheterization possibly has a nursing diagnosis of anxiety related to lack of knowledge about cardiac catheterization. An incorrect diagnosis is anxiety related to cardiac catheterization.
5. Identify the patient response to the equipment rather than the equipment itself. Patients are often unfamiliar with medical technology. The diagnosis of deficient knowledge regarding the need for cardiac monitoring is accurate compared with the statement anxiety related to cardiac monitor.
6. Identify the patient’s problems rather than your problems with nursing care. Nursing diagnoses are always patient centered and form the basis for goal-directed care. Potential intravenous complications related to poor vascular access indicates a nursing problem in initiating and maintaining intravenous therapy. The diagnosis risk for infection properly centers attention on patient needs.
7. Identify the patient problem rather than the nursing intervention. You plan nursing interventions after identifying a nursing diagnosis. The statement, “offer bedpan frequently because of altered elimination patterns,” changes to the correct diagnostic statement, diarrhea related to food intolerance. This corrects the misstatement and allows proper implementation of the nursing process. More appropriate interventions are selected rather than a single intervention that will not solve the problem.
8. Identify the patient problem rather than the goal of care. You establish goals during the planning step of the nursing process (see Chapter 18). Goals based on accurate identification of a patient’s problems serve as a basis to determine problem resolution. Change the diagnostic statement, “Patient needs high-protein diet related to potential alteration in nutrition,” to imbalanced nutrition: less than body requirements related to inadequate protein intake.
9. Make professional rather than prejudicial judgments. Base nursing diagnoses on subjective and objective patient data and do not include your personal beliefs and values. Remove your judgment from impaired skin integrity related to poor hygiene habits by changing the nursing diagnosis to read impaired skin integrity related to inadequate knowledge about perineal care.
10. Avoid legally inadvisable statements (Carpenito-Moyet, 2009). Statements that imply blame, negligence, or malpractice have the potential to result in a lawsuit. The statement, “recurrent angina related to insufficient medication,” implies an inadequate prescription by the health care provider. Correct problem identification is chronic pain related to improper use of medications.
11. Identify the problem and etiology to avoid a circular statement. Circular statements are vague and give no direction to nursing care. Change the statement, “impaired breathing pattern related to shallow breathing,” to identify the patient problem and cause, ineffective breathing pattern related to incisional pain.
12. Identify only one patient problem in the diagnostic statement. Every problem has different specific expected outcomes. Confusion during the planning step occurs when you include multiple problems in a nursing diagnosis. Restate pain and anxiety related to difficulty in ambulating as two nursing diagnoses such as impaired physical mobility related to pain in right knee and anxiety related to difficulty in ambulating. It is permissible to include multiple etiologies contributing to one patient problem, as in complicated grieving related to diagnosed terminal illness and change in family role.
Documentation and Informatics
Once you identify a patient’s nursing diagnoses, enter them either on the written plan of care or in the electronic health information record of the agency. In the clinical facility list nursing diagnoses chronologically as you identify them. When initiating an original care plan, place the highest-priority nursing diagnoses first. This depends on the patient’s condition and the nature of the nursing diagnosis (e.g., acute physical health problem versus a long-term chronic health management issue). Thereafter add nursing diagnoses to the list. Date a nursing diagnosis at the time of entry. When caring for a patient, review the list and identify nursing diagnoses with the greatest priority, regardless of chronological order.
In some settings data-driven computerized decision support systems are in place that allow you to be more accurate in making nursing diagnoses. A computer-based clinical decision support function involves use of the computer to bring relevant knowledge to bear for the health care of a patient (Cho, Staggers, and Park, 2010). The database within one of these systems includes diagnostic labels (e.g., NANDA-I diagnostic labels), defining characteristics, activities, and indicators for nursing. A nurse enters assessment data, and the computer helps by organizing the data into clusters that enhance the ability to select accurate diagnoses. Once diagnoses are selected, the computer system also directs the nurse to intervention options to select for a patient.
Nursing Diagnoses: Application to Care Planning
Nursing diagnosis is a mechanism for identifying the domain of nursing. Diagnoses direct the planning process and the selection of nursing interventions to achieve desired outcomes for patients. Just as the medical diagnosis of diabetes leads a physician to prescribe a low-carbohydrate diet and medication for blood glucose control, the nursing diagnosis of impaired skin integrity directs a nurse to apply certain support surfaces to a patient’s bed and initiate a turning schedule. In Chapter 18 you will learn how unifying the languages of NANDA-I with the Nursing Interventions Classification (NIC) and Nursing Outcomes Classification (NOC) facilitates the process of matching nursing diagnoses with accurate and appropriate interventions and outcomes (Dochterman and Jones, 2003). The care plan (see Chapter 18) is a map for nursing care and demonstrates your accountability for patient care. By making accurate nursing diagnoses, your subsequent care plan communicates to other professionals the patient’s health care problems and ensures that you select relevant and appropriate nursing interventions.
Key Points
• The diagnostic process is a clinical judgment that involves reviewing assessment information, recognizing cues and patterns in the data, and identifying the patient’s specific health care problems.
• The nursing diagnostic process is unique from that of medical diagnosis in that patients become involved in the diagnostic process when possible.
• Accurate diagnosis of patient problems ensures the selection of more effective and efficient nursing interventions.
• One purpose of nursing diagnosis is that it provides a precise definition of a patient’s problem that gives nurses and other members of the health care team a common language for understanding the patient’s needs.
• The nursing diagnostic process includes data clustering, identifying patient needs or problems, and formulating the nursing diagnosis or collaborative problem.
• Defining characteristics are subjective and objective clinical criteria that form clusters, leading to a diagnostic conclusion.
• When an assessment reveals defining characteristics that apply to more than one nursing diagnosis, gather more information to clarify your interpretation.
• Absence of defining characteristics suggests that you reject a proposed diagnosis.
• A nursing diagnosis is usually written in a two-part format, including a diagnostic label and an etiological or related factor.
• A three-part nursing diagnosis, using a PES format, includes a diagnostic label, etiological statement, and symptoms or defining characteristics.
• The “related to” factor of the diagnostic statement helps you to individualize a patient’s nursing diagnoses and provides direction for your selection of appropriate interventions.
• Risk factors serve as cues to indicate that a risk nursing diagnosis applies to a patient’s condition.
• A concept map is a visual representation of a patient’s nursing diagnoses and their relationship with one another.
• Nursing diagnostic errors occur by errors in data collection, interpretation and analysis of data, clustering of data, or the diagnostic statement.
Clinical Application Questions
Preparing for Clinical Practice
Tonya discusses the concerns Mr. Jacobs has about his sexual relationship with his wife. She knows that a radical prostatectomy can cause nerve damage that impairs a man’s ability to have a normal erection. Tonya says, “You’ve told me that you’re worried about you and your wife. Can you tell me more?” Mr. Jacobs says, “I feel uncertain about my ability to have sex. The doctor said before the surgery that there is a risk of damaging a nerve that can affect my ability to perform sexually.” Tonya observes that Mr. Jacobs has poor eye contact as they talk and his voice quivers. Tonya asks, “How would you describe your relationship with Mrs. Jacobs?” The patient responds, “Oh, it’s been really good. We’ve had our ups and downs like anyone else, but she has been so good to me. I worry that I won’t be able to be the husband she wants any more.” Tonya clarifies, “Has the doctor visited since surgery to discuss your concerns?” Mr. Jacobs replies, “No, he hasn’t been in yet.”
1. Which of the following are defining characteristics from the assessment?
1. Quiver in Mr. Jacobs’ voice
2. Nurse’s statement, “You’ve told me that you’re worried.”
2. Tonya clusters the defining characteristics to select the diagnostic label of anxiety. What would you identify as the related factor for this diagnosis?
3. If Tonya identified the diagnosis as anxiety related to risk of nerve damage during surgery, would this be an accurate nursing diagnosis? Explain.
![]() Answers to Clinical Application Questions can be found on the Evolve website.
Answers to Clinical Application Questions can be found on the Evolve website.
Are You Ready to Test Your Nursing Knowledge?
1. The nurse identified that the patient has pain on a scale of 7, he winces during movement, and he expresses discomfort over the incisional area. He guards the area by resisting movement. The incision appears to be healing, but there is natural swelling. Write a three-part nursing diagnostic statement using the PES format.
2. Review the following nursing diagnoses and identify the diagnoses that are stated correctly. (Select all that apply.)
1. Anxiety related to fear of dying
2. Fatigue related to chronic emphysema
3. A nurse reviews data gathered regarding a patient’s pain symptoms. The nurse compares the defining characteristics for acute pain with those for chronic pain and in the end selects acute pain as the correct diagnosis. This is an example of the nurse avoiding an error in:
4. The nursing diagnosis readiness for enhanced communication is an example of a(n):
5. In the following examples, which nurses are making nursing diagnostic errors? (Select all that apply.)
1. The nurse who listens to lung sounds after a patient reports “difficulty breathing”
2. The nurse who considers conflicting cues in deciding which diagnostic label to choose
3. The nurse assessing the edema in a patient’s lower leg who is unsure how to assess the severity of edema
4. The nurse who identifies a diagnosis on the basis of a single defining characteristic
6. A nurse is reviewing a patient’s list of nursing diagnoses in the medical record. The most recent nursing diagnosis is diarrhea related to intestinal colitis. This is an incorrectly stated diagnostic statement, best described as:
1. Identifying the clinical sign instead of an etiology.
2. Identifying a diagnosis based on prejudicial judgment.
3. Identifying the diagnostic study rather than a problem caused by the diagnostic study.
4. Identifying the medical diagnosis instead of the patient’s response to the diagnosis.
7. A nurse is assigned to a new patient admitted to the nursing unit following admission through the emergency department. The nurse collects a nursing history and interviews the patient. Place the following steps for making a nursing diagnosis in the correct order.
_____ 1. Considers context of patient’s health problem and selects a related factor
_____ 2. Reviews assessment data, noting objective and subjective clinical criteria
8. Match the activity on the left with the source of diagnostic error on the right:
| Activity | Source of Diagnostic Error |
| a. Nurse listens to lungs for first time and is not sure if abnormal lung sounds are present. | __ 1. Collecting data |
| b. After reviewing objective data, nurse selects diagnosis of fear before asking patient to discuss feelings. | __ 2. Interpreting |
| c. Nurse identifies incorrect diagnostic label. | __ 3. Clustering |
| d. Nurse does not consider patient’s cultural background when reviewing cues. | __ 4. Labeling |
| e. Nurse prepares to complete decision on diagnosis and realizes that clinical criteria are grouped incorrectly to form a pattern. |
9. Review the following list of nursing diagnoses and identify those stated incorrectly. (Select all that apply.)
1. Acute pain related to lumbar disk repair
2. Sleep deprivation related to difficulty falling asleep
10. The nurse completed the following assessment: 63-year-old female patient has had abdominal pain for 6 days. She reports not having a bowel movement for 4 days, whereas she normally has a bowel movement every 2 to 3 days. She has not been hospitalized in the past. Her abdomen is distended. She reports being anxious about upcoming tests. Her temperature was 37° C, pulse 82 and regular, blood pressure 128/72. Which of the following data form a cluster, showing a relevant pattern? (Select all that apply.)
11. In question 10, which additional data do you collect to add to the cluster of information? (Short answer)
12. The nurse in a geriatric clinic collects the following information from an 82-year-old patient and her daughter, the family caregiver. The daughter explains that the patient is “always getting lost.” The patient sits in the chair but gets up frequently and paces back and forth in the examination room. The daughter says, “I just don’t know what to do because I worry she will fall or hurt herself.” The daughter states that, when she took her mother to the store, they became separated, and the mother couldn’t find the front entrance. The daughter works part time and has no one to help watch her mother. Which of the data form a cluster, showing a relevant pattern?(Select all that apply.)
13. Which of the following are examples of collaborative problems? (Select all that apply.)
14. Two nurses are having a discussion at the nurses’ station. One nurse is a new graduate who added, “Patient needs improved bowel function related to constipation” to a patient’s care plan. The nurse’s colleague, the charge nurse says, “I think your diagnosis is possibly worded incorrectly. Let’s go over it together.” A correctly worded diagnostic statement is:
1. Need for improved bowel function related to change in diet.
2. Patient needs improved bowel function related to alteration in elimination.
15. The following nursing diagnoses all apply to one patient. As the nurse adds these diagnoses to the care plan, which diagnoses will not include defining characteristics?
Answers: 1. P, acute pain; E, related to incisional trauma; S, evidenced by pain reported at 7, with guarding, and restricted turning and positioning; 2. 1, 4; 3. 3; 4. 3; 5. 3, 4; 6. 4; 7. 2, 3, 4, 1; 8. 1 a, 2 b and d, 3 e, 4 c; 9. 1, 2, 4; 10. 2, 4, 5; 11. See Evolve; 12. 2, 3, 5; 13. 2, 3; 14. 3; 15. 1.
References
Ackley, BJ, Ladwig, GB. Nursing diagnosis handbook, ed 9. St Louis: Mosby; 2011.
American Nurses Association. Model nurse practice act. Washington, DC: The Association; 1955.
American Nurses Association. Scope of nursing practice. Washington, DC: The Association; 1987.
American Nurses Association. Nursing’s social policy statement, ed 2. Washington, DC: The Association; 2003.
American Nurses Association. Nursing’s social policy statement, ed 3. Washington, DC: The Association; 2010.
Carpenito-Moyet, LJ. Nursing diagnoses: application to clinical practice, ed 13. Philadelphia: Lippincott, Williams & Wilkins; 2009.
Dochterman, JM, Jones, DA. Unifying nursing languages: the harmonization of NANDA, NIC, NOC. Washington, DC: American Nurses Association; 2003.
Ferrario, CG. Developing nurses’ critical thinking skills with concept mapping. J Nurses Staff Dev. 2004;20(6):261.
Fry, VS. The creative approach to nursing. Am J Nurs. 1953;53:301.
Gebbie, K. Utilization of a classification of nursing diagnosis. Nurs Diagn. 1998;9(2 suppl):17.
McFarland, GK, McFarlane, EA. Nursing diagnosis and intervention: planning for patient care. St Louis: Mosby; 1989.
NANDA International. Nursing diagnoses: definitions and classification, 2012-2014. Oxford: Wiley-Blackwell; 2012.
Smith, LS. Documenting culturally competent psychosocial nursing diagnoses. Nursing. 2007;37(1):70.
Yura, H, Walsh, M. The nursing process. Norwalk, Conn: Appleton-Century-Crofts; 1967.
Research References
Cho, I, Staggers, N, Park, I. Nurses’ responses to differing amounts and information content in a diagnostic computer-based decision support application. Comput Inform Nurs. 2010;28(2):95.
Hsu, L, Hsieh, S. Concept maps as an assessment tool in a nursing course. J Prof Nurs. 2005;21(3):141.
Muller-Staub, M, et al. Nursing diagnoses, interventions and outcomes—application and impact on nursing practice: systematic review. J Adv Nurs. 2006;56(5):514.
Muller-Staub, M, et al. Implementing nursing diagnostics effectively: cluster randomized trial. J Adv Nurs. 2008;63(3):291.
Wieck, KL. Diagnostic language consistency among multicultural English-speaking nurses. Nurs Diagn. 1996;7(2):70.