Ackley, BJ, Ladwig, GB. Nursing diagnosis handbook: an evidence-based guide to planning care, ed 9. St Louis: Mosby; 2011.
American Association of Respiratory Care (AARC). clinical practice guideline: incentive spirometry. Respir Care. 2011;56(10):1600.
American Association of Respiratory Care (AARC), AARC clinical practice guideline, directed cough. Respir Care 1993;38(5):495. http://www.rcjournal.com/cpgs/dccpg.html
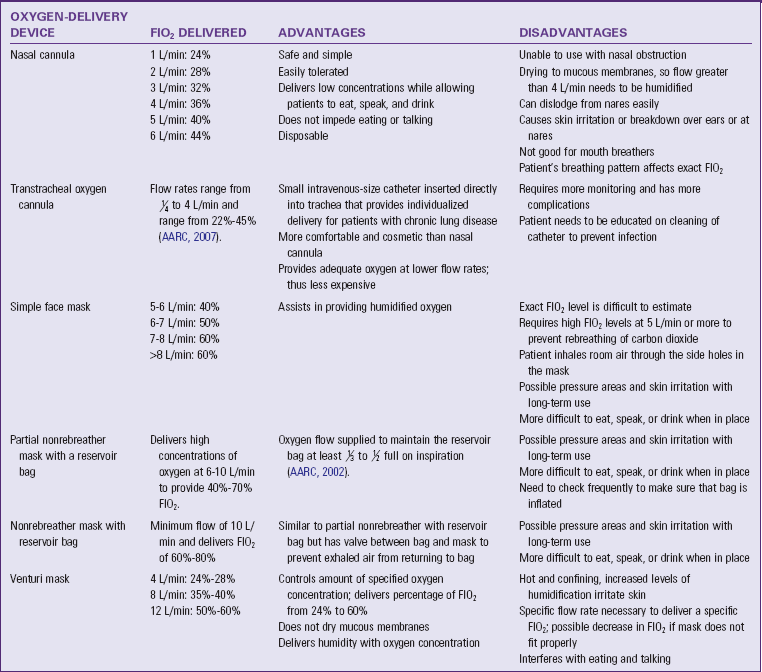
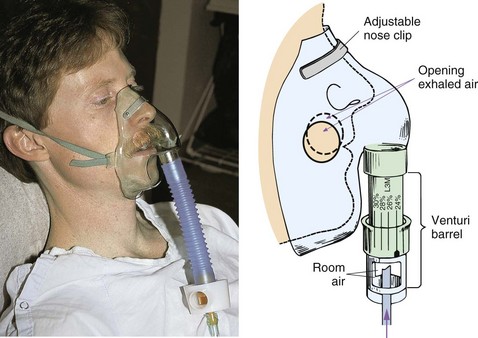
American Association of Respiratory Care (AARC). AARC clinical practice guideline, oxygen therapy for adults in the acute care facility—2002 revision and update. Respir Care. 2002;47:717.
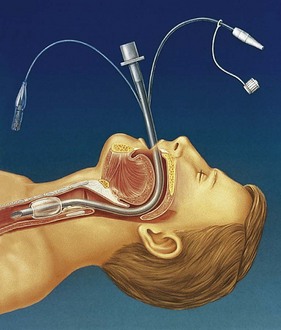
American Association of Respiratory Care (AARC). AARC clinical practice guideline, nasotracheal suction—2004 revision and update. Respir Care. 2004;49:1080.
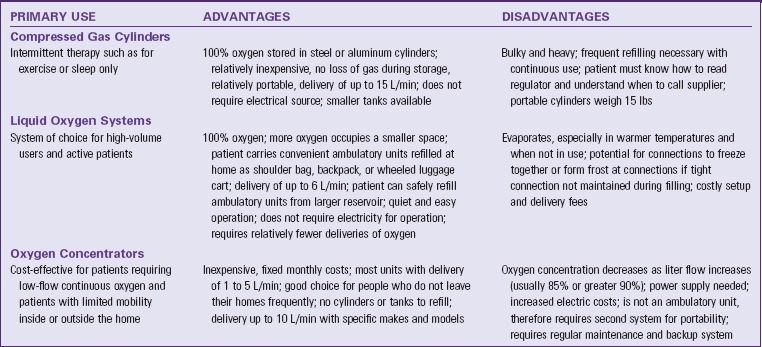
American Association of Respiratory Care (AARC). AARC clinical practice guideline, oxygen therapy in the home or alternate site health care facility—2007 revision and update. Respir Care. 2007;52:1063.
American Association of Respiratory Care (AARC). AARC clinical practice guideline, endotracheal suctioning of mechanically ventilated patients with artificial airways—2010 update. Respir Care. 2010;55(60):758.
American Association of Respiratory Care (AARC). AARC clinical practice guideline, providing patient and caregiver training—2010. Respir Care. 2010;55:765.
American Cancer Society (ACS). Questions about smoking, tobacco, and health. http://www.cancer.org/Cancer/CancerCauses/QuestionsaboutSmokingTob, 2010. [Accessed August 18, 2010].
American Heart Association (AHA). Women and coronary heart disease. http://www.americanheart.org/presenter.jhtml?identifier=2859, 2006. [Accessed June 29, 2007].
American Heart Association (AHA). Community lay rescuer automated external defibrillator programs. Circulation. 2006;113:1260.
American Heart Association (AHA). Cardiopulmonary resuscitation (CPR) statistics. http://www.americanheart.org/print_presenter.jhtml;jsessionid=GZVUF13G0X1LACQFCX 2010. [Accessed September 1, 2010].
American Heart Association (AHA). Part 1: Executive Summary: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(suppl):S640–S656.
American Lung Association. Big tobacco on campus: ending the addiction. http://www.lungusa.org/stop-smoking/tobacco-control-advocacy/reports-resources/tobacco-policy-trend-reports/college-report.pdf, 2008. [Accessed September 27, 2011].
American Lung Association. Many lung diseases more prevalent in diverse populations. Accessed July 16, 2010 http://www.lungusa.org/press-room/press-releases/many-lung-diseases-more.html 2010. [from].
American Lung Association. State of the lung disease in diverse communities 2010. http://www.lungusa.org/assets/documents/publications/lung-disease-data/solddc_2010.pdf, 2010. [Accessed September 27, 2011].
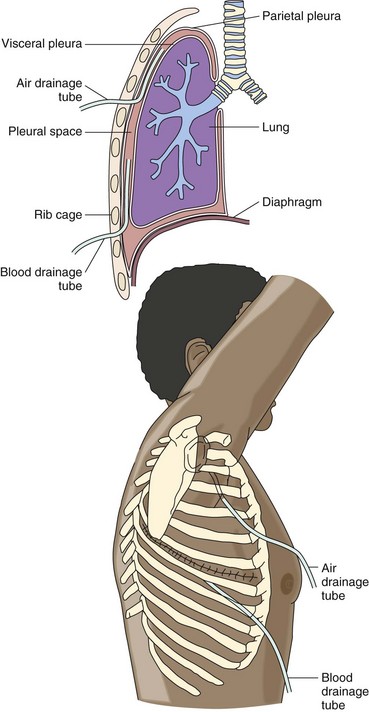
Carroll, P. Keeping up with mobile chest drains. RN. 2005;68(10):26.
Centers for Disease Control and Prevention (CDC). 2008 Smoking cessation clinical practice guideline. http://www.cdc.gov/tobacco/quit_smoking/cessation/index.htm, 2008. [Accessed August 18, 2010].
Centers for Disease Control and Prevention (CDC), Testing for TB infection. Atlanta: Centers for Disease Control and Prevention; 2010. http://www.cdc.gov/tb/topic/testing/default.htm
Centers for Disease Control and Prevention (CDC). Tuberculin testing and diagnosis. Atlanta http:www.cdc.gov/tb/topic/testing/default.htm, 2010. [Accessed September 8, 2010].
Centers for Disease Control and Prevention (CDC), Adult immunization schedule 2010–11, National immunization program. Atlanta: Centers for Disease Control and Prevention; 2010. http://www.cdc.gov/vaccines/pubs/vis/default.htm
Centers for Disease Control and Prevention (CDC, Vaccines & immunizations: pneumococcal disease in short. Atlanta: Centers for Disease Control and Prevention, Vaccines and Preventable Diseases; 2010. http://www.cdc.gov/vaccines/vpd-vac/pneumo/in-short-both.htm
Centers for Disease Control and Prevention (CDC), Recommended adult immunization schedule—United States. Atlanta: Centers for Disease Control and Prevention, Morbidity and Mortality Weekly; 2011. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm604a10.htm?s_cid=mm6004a10_e
Cleveland Clinic, Information for patients: tracheostomy care. Cleveland Clinic Head and Neck Institute; 2010. http://my.clevelandclinic.org/head_neck/patients/head_neck_cancer/tracheostomy_care.aspx [Accessed July 14, 2010].
Cleveland Clinic, Home oxygen therapy. Cleveland Clinic Foundation; 2010. http://www.cchs.net/health/health-info/docs/2400/2413.asp?index=8707 [Accessed September 14, 2010].
Coughlin, AM, Parchinsky, C. Go with the flow of chest tube therapy. Nursing 2006. 2006;36(3):36.
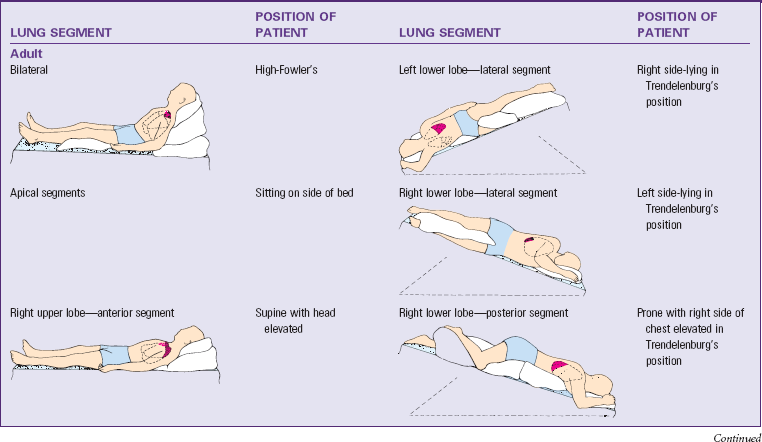
Cystic Fibrosis Foundation (CFF). An introduction to postural drainage & percussion—consumer fact sheet. Bethesda, Md: Cystic Fibrosis Foundation; 2005.
Demir, F, Dramali, A. Requirement for 100% oxygen before and after closed suction. J Adv Nurs. 2005;51(3):245.
Environmental Protection Agency (EPA). A citizen’s guide to radon. http://www.epa.gov/radon/pubs/citguide.html, 2010. [Accessed August 18, 2010].
Hess, DR. Tracheostomy tubes and related appliances. Respir Care. 2005;50:497.
Higgins, D. Basic principles of caring for patients with a tracheostomy. Nurs Times. 2009;105(3):14.
Hockenberry, MJ, Wilson, D. Wong’s nursing care of infants and children, ed 9. St Louis: Mosby; 2011.
Johns Hopkins Medicine. Stoma care. http://www.hopkinsmedicine.org/se/util/display_mod.cfm?MODULE=se_server/mod/mod, 2010. [Accessed July 14, 2010].
The Joint National Committee (JNC). The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure—Complete Report. Hypertension. 2003;42:1206.
Lewis, SL, et al. Medical-surgical nursing: assessment and management of clinical problems, ed 7. St Louis: Mosby; 2007.
Linton, AD, Lach, HW. Matteson & McConnell’s Gerontological nursing: concepts and practice, ed 3. Philadelphia: Saunders Elsevier; 2007.
LungUSA. Facts about secondhand smoke: American Lung Association. http://www.lungusa.org/stop-smoking/health-effects/secondhand-smoke.html, 2010. [Accessed July 16, 2010].
McCance, KL, Huether, SE. Pathophysiology: the biologic basis for disease in adults and children, ed 6. St Louis: Mosby Elsevier; 2010.
Meiner, S. Gerontologic nursing, ed 4. St Louis: Mosby; 2011.
National Heart Lung and Blood Institute, What is CPAP?. National Institutes of Health; 2010. http://www.nhlbi.nih.gov/health/dci/Diseases/cpap/cpap_what.html [Accessed August 25, 2010].
National Institute on Drug Abuse (NIDA), NIDA InfoFacts: marijuana. National Institutes of Health; 2009. http://drugabuse.gov/infofacts/marijuana.html [Accessed August 18, 2010].
National Institute on Drug Abuse (NIDA), InfoFacts: cocaine. National Institutes of Health; 2010. http://www.drugabuse.gov/infofacts/cocaine.html [Accessed August 18, 2010].
Roman, M, Mercado, D. Review of chest tube use. Medsurg Nurs. 2006;15(1):41.
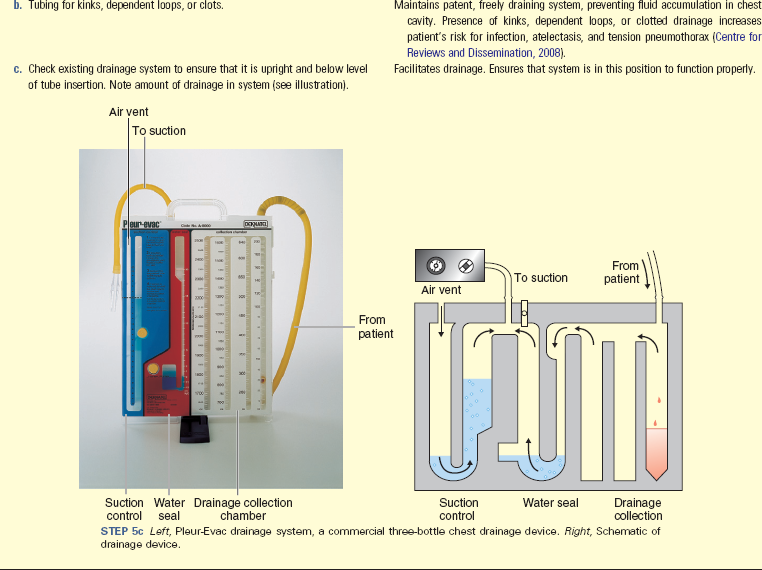
Rushing, J. Managing a water-seal chest drainage unit. Nursing. 2007;379(12):12.
Stoppler, MC, Is your child or teen “huffing”. MedicineNet.com; 2005. http://www.medicinenet.com/script/main/art.asp?articlekey=47975 [Accessed September 8, 2010].
Soo Hoo, GW. Ventilation, noninvasive. http://emedicine.medscape.com/article/304235, 2010. [Accessed August 25].
The Joint Commission, 2011 National Patient Safety Goals (NPGs). TJC; 2011. available at http://www.jointcommission.org/standards_information/npsgs.aspx
Vollman, K. Ask the experts. Crit Care Nurs. 2006;26(4):53.
Woodrow, MA. Caring for patients receiving oxygen therapy. Nurs Older Adults. 2007;19(1):31.
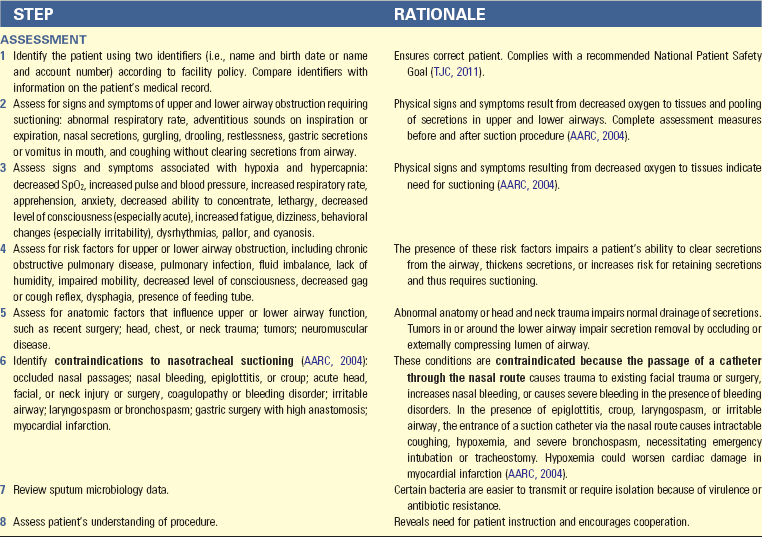
 pack of cigarettes a day and does not participate in any exercise. He does not “see any reason” to increase his fluid intake. His SpO2 ranges from 78% to 84%. He must do his self-care activities slowly because of fatigue. Presently he is admitted for right upper lobe pneumonia. He reports having an intermittent productive cough that occasionally produces thick, yellow sputum. He has more episodes of coughing when lying flat. His vital signs are temperature, 101.4° F (38.5° C); pulse, 102 beats/min; respirations, 30 breaths/min; blood pressure, 130/90 mm Hg; and SpO2, 84%. He has episodes of chilling and diaphoresis. His health care provider has told him that, if he gradually increases his exercise, drinks more fluids, and stops smoking, his respiratory status will improve.
pack of cigarettes a day and does not participate in any exercise. He does not “see any reason” to increase his fluid intake. His SpO2 ranges from 78% to 84%. He must do his self-care activities slowly because of fatigue. Presently he is admitted for right upper lobe pneumonia. He reports having an intermittent productive cough that occasionally produces thick, yellow sputum. He has more episodes of coughing when lying flat. His vital signs are temperature, 101.4° F (38.5° C); pulse, 102 beats/min; respirations, 30 breaths/min; blood pressure, 130/90 mm Hg; and SpO2, 84%. He has episodes of chilling and diaphoresis. His health care provider has told him that, if he gradually increases his exercise, drinks more fluids, and stops smoking, his respiratory status will improve.