Medication Administration
• Discuss the nurse’s role and responsibilities in medication administration.
• Describe the physiological mechanisms of medication action.
• Differentiate among different types of medication actions.
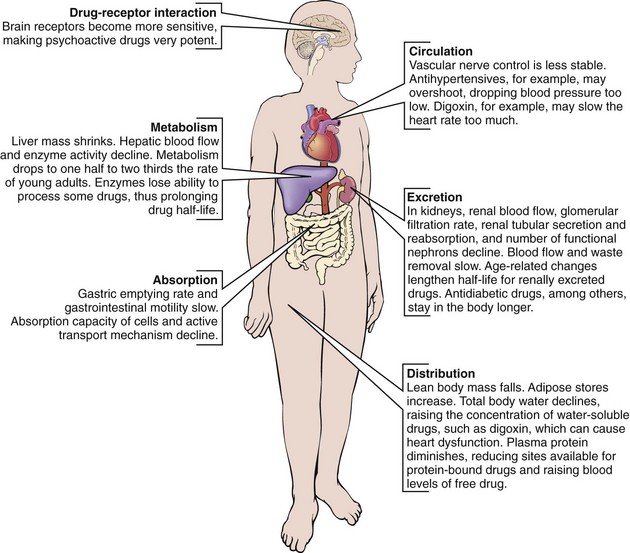
• Discuss developmental factors that influence pharmacokinetics.
• Discuss factors that influence medication actions.
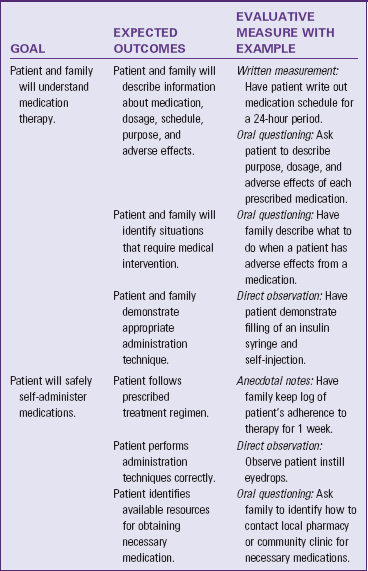
• Discuss methods used to educate patients about prescribed medications.
• Compare and contrast the roles of the prescriber, pharmacist, and nurse in medication administration.
• Implement nursing actions to prevent medication errors.
• Describe factors to consider when choosing routes of medication administration.
• Calculate prescribed medication doses correctly.
• Discuss factors to include in assessing a patient’s needs for and response to medication therapy.
• Identify the six rights of medication administration and apply them in clinical settings.
http://evolve.elsevier.com/Potter/fundamentals/
Patients with acute or chronic health problems restore or maintain their health using a variety of strategies. One of these strategies is medication, a substance used in the diagnosis, treatment, cure, relief, or prevention of health problems. No matter where they receive their health care—hospitals, clinics, or home—nurses play an essential role in safe medication preparation, administration, and evaluation of medication effects. When patients cannot administer their own medications at home, family members, friends, or home care personnel are often responsible for medication administration. In all settings, nurses are responsible for evaluating the effects of medications on the patient’s ongoing health status, teaching them about their medications and side effects, ensuring adherence to the medication regimen, and evaluating the patient’s and family caregiver’s ability to self-administer medications.
Scientific Knowledge Base
Medications are frequently used to manage diseases. Because medication administration and evaluation are a critical part of nursing practice, nurses need to have knowledge about the actions and effects of the medications taken by their patients. Administering medications safely requires an understanding of legal aspects of health care, pharmacology, pharmacokinetics, the life sciences, pathophysiology, human anatomy, and mathematics.
Medication Legislation and Standards
The U.S. government regulates the pharmaceutical industry to protect the health of the people by ensuring that medications are safe and effective. The first American law to regulate medications was the Pure Food and Drug Act. This law simply requires all medications to be free of impure products. Subsequent legislation has set standards related to safety, potency, and efficacy. Enforcement of medication laws currently rests with the Food and Drug Administration (FDA), which ensures that all medications on the market undergo vigorous testing before they are sold to the public. Federal medication law extends and refines controls on medication sales and distribution; testing, naming, and labeling; and the regulation of controlled substances. Official publications such as the United States Pharmacopeia (USP) and the National Formulary set standards for medication strength, quality, purity, packaging, safety, labeling, and dose form. In 1993 the FDA instituted the MedWatch program. This voluntary program encourages nurses and other health care professionals to report when a medication, product, or medical event causes serious harm to a patient by completing the MedWatch form. The form is available on the MedWatch website (USFDA, 2010).
State and Local Regulation of Medication
State and local medication laws must conform to federal legislation. States often have additional controls, including control of substances not regulated by the federal government. Local governmental bodies regulate the use of alcohol and tobacco.
Health Care Institutions and Medication Laws
Health care agencies establish individual policies to meet federal, state, and local regulations. The size of the agency, the types of services it provides, and the types of professional personnel it employs influence these policies. Agency policies are often more restrictive than governmental controls. For example, a common agency policy is the automatic discontinuation of narcotics after a set number of days. Although a prescriber can reorder the narcotic, this policy helps to control unnecessarily prolonged medication therapy and requires the prescriber to review the need for this class of medication on a regular basis.
Medication Regulations and Nursing Practice
State Nurse Practice Acts (NPAs) have the most influence over nursing practice by defining the scope of nurses’ professional functions and responsibilities. Most NPAs are purposefully broad so nurses’ professional responsibilities are not limited. Health care agencies often interpret specific actions allowed under NPAs; but they are not able to modify, expand, or restrict the intent of the act. The primary intent of NPAs is to protect the public from unskilled, undereducated, and unlicensed personnel.
The nurse is responsible for following legal provisions when administering controlled substances such as opioids, which are carefully controlled through federal and state guidelines. Violations of the Controlled Substances Act are punishable by fines, imprisonment, and loss of nurse licensure. Hospitals and other health care agencies have policies for the proper storage and distribution of narcotics (Box 31-1).
Pharmacological Concepts
Some medications have as many as three different names. The chemical name of a medication provides an exact description of its composition and molecular structure. Nurses rarely use chemical names in clinical practice. An example of a chemical name is N-acetyl-para-aminophenol, which is commonly known as Tylenol. The manufacturer who first develops the medication gives the generic or nonproprietary name, with United States Adopted Names (USAN) Council approval (AMA, 2010). Acetaminophen is an example of a generic name. It is the generic name for Tylenol. The generic name becomes the official name listed in official publications such as the USP. The trade name, brand name, or proprietary name is the name under which a manufacturer markets a medication. The trade name has the symbol (™) at the upper right of the name, indicating that the manufacturer has trademarked the name of the medication (e.g., Panadol,™ Tempra,™ and St. Joseph Aspirin-Free Fever Reducer for Children™).
Manufacturers choose trade names that are easy to pronounce, spell, and remember. Many companies produce the same medication, and similarities in trade names are often confusing. Therefore be careful to obtain the exact name and spelling for each medication you administer to your patients. Because similarities in drug names are a common cause of medical errors, The Institute for Safe Medication Practices (ISMP) (2010a) (http://www.ismp.org/Tools/confuseddrugnames.pdf) and The Joint Commission (TJC) (2011a) (http://www.jointcommission.org/standards_information/npsgs.aspx) publish a list of medications that are frequently confused with one another. TJC’s list includes recommendations to prevent mixing these medications.
Classification
Medication classification indicates the effect of the medication on a body system, the symptoms the medication relieves, or its desired effect. Usually each class contains more than one medication that is used for the same type of health problem. For example, patients who have asthma often take a variety of medications to control their illness such as beta2-adrenergic agonists. The beta2-adrenergic classification contains at least eight different medications (Lehne, 2010). Some are part of more than one class. For example, aspirin is an analgesic, an antipyretic, and an antiinflammatory medication.
Medication Forms
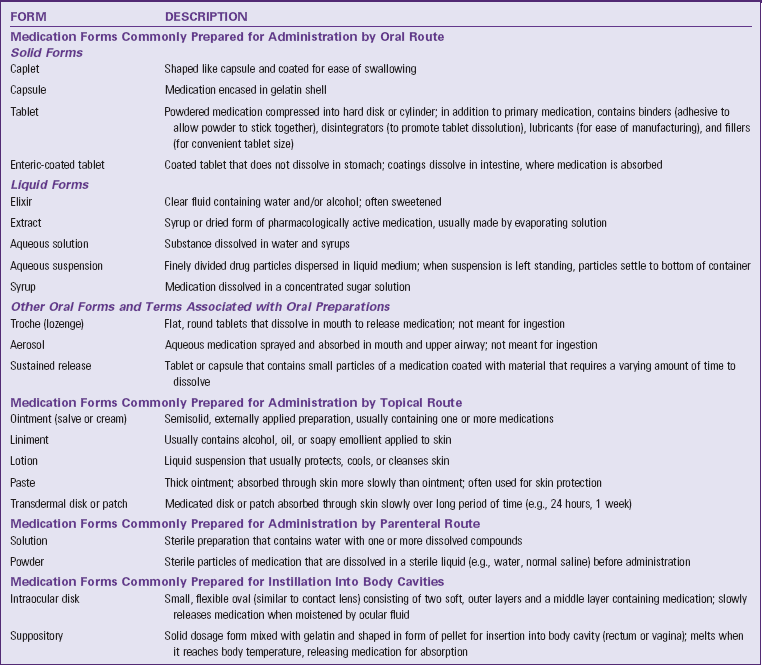
Medications are available in a variety of forms, or preparations. The form of the medication determines its route of administration. The composition of a medication enhances its absorption and metabolism. Many medications come in several forms such as tablets, capsules, elixirs, and suppositories. When administering a medication, be certain to use the proper form (Table 31-1).
Pharmacokinetics As the Basis of Medication Actions
For medications to be therapeutic they must be taken into a patient’s body; be absorbed and distributed to cells, tissues, or a specific organ; and alter physiological functions. Pharmacokinetics is the study of how medications enter the body, reach their site of action, metabolize, and exit the body. Use knowledge of pharmacokinetics when timing medication administration, selecting the route of administration, considering the patient’s risk for alterations in medication action, and evaluating the patient’s response.
Absorption
Absorption is the passage of medication molecules into the blood from the site of medication administration. Factors that influence absorption are the route of administration, ability of the medication to dissolve, blood flow to the site of administration, body surface area (BSA), and lipid solubility of medication.
Route of Administration: Each route of medication administration has a different rate of absorption. When applying medications on the skin, absorption is slow because of the physical makeup of the skin. Medications placed on the mucous membranes and respiratory airways are absorbed quickly because these tissues contain many blood vessels. Because orally administered medications pass through the gastrointestinal (GI) tract, the overall rate of absorption is usually slow. Intravenous (IV) injection produces the most rapid absorption because medications are immediately available when they enter the systemic circulation.
Ability of the Medication to Dissolve: The ability of an oral medication to dissolve depends largely on its form or preparation. The body absorbs solutions and suspensions already in a liquid state more readily than tablets or capsules. Acidic medications pass through the gastric mucosa rapidly. Medications that are basic are not absorbed before reaching the small intestine.
Blood Flow to the Site of Administration: Medications are absorbed as blood comes in contact with the site of administration. The richer the blood supply to the site of administration, the faster the medication is absorbed.
Body Surface Area: When a medication comes in contact with a large surface area, it is absorbed at a faster rate. This helps explain why the majority of medications are absorbed in the small intestine rather than the stomach.
Lipid Solubility: Because the cell membrane has a lipid layer, highly lipid-soluble medications cross cell membranes easily and are absorbed quickly. Another factor that often affects medication absorption is whether or not food is in the stomach. Some oral medications are absorbed more easily when administered between meals because food changes the structure of a medication and sometimes impairs its absorption. When some medications are administered together, they interfere with one another, which impairs the absorption of both medications.
Safe medication administration requires knowledge of factors that alter or impair absorption of prescribed medications. You need an understanding of medication pharmacokinetics, the patient’s health history, the physical examination, and knowledge gained through daily interactions with patients. Use this knowledge to ensure that you administer medications at the correct time for best absorption. When medications interact with food, know which medications must be administered before or between meals or on an empty stomach. When medications interact with one another, ensure that they are not given at the same time. Consult and collaborate with the patient’s prescribers to ensure that the patient achieves the therapeutic effect of all medications. Before administering any medication, check pharmacology books, drug references, or package inserts or consult with pharmacists to identify medication-medication or medication-food interactions.
Distribution
After a medication is absorbed, it is distributed within the body to tissues and organs and ultimately to its specific site of action. The rate and extent of distribution depend on the physical and chemical properties of the medication and the physiology of the person taking it.
Circulation: Once a medication enters the bloodstream, it is carried throughout the tissues and organs. How fast it reaches the site depends on the vascularity of the various tissues and organs. Conditions that limit blood flow or blood perfusion inhibit the distribution of a medication. For example, patients with heart failure have impaired circulation, which slows medication delivery to the intended site of action. Therefore the efficacy of medications in these patients is often delayed or altered.
Membrane Permeability: Membrane permeability refers to the ability of the medication to pass through tissues and membranes to enter target cells. To be distributed to an organ, a medication has to pass through all of the tissues and biological membranes of the organ. Some membranes serve as barriers to the passage of medications. For example, the blood-brain barrier allows only fat-soluble medications to pass into the brain and cerebral spinal fluid. Therefore central nervous system infections often require treatment with antibiotics injected directly into the subarachnoid space in the spinal cord. Some older patients experience adverse effects (e.g., confusion) as a result of the change in the permeability of the blood-brain barrier, with easier passage of fat-soluble medications. The placental membrane also has a nonselective barrier to medications. Fat-soluble and nonfat-soluble agents often cross the placenta and produce fetal deformities. After birth neonates often experience respiratory depression and withdrawal symptoms when their mothers use or abuse narcotics.
Protein Binding: The degree to which medications bind to serum proteins such as albumin affects their distribution. Most medications partially bind to albumin. Medications bound to albumin cannot exert pharmacological activity. The unbound or “free” medication is its active form. Older adults have a decrease in albumin, probably caused by a change in liver function. The same is true for patients with liver disease or malnutrition. In both examples patients are at risk for an increase in medication activity, toxicity, or both.
Metabolism
After a medication reaches its site of action, it becomes metabolized into a less active or inactive form that is easier to excrete. Biotransformation occurs under the influence of enzymes that detoxify, break down, and remove biologically active chemicals. Most biotransformation occurs within the liver, although the lungs, kidneys, blood, and intestines also metabolize medications. The liver is especially important because its specialized structure oxidizes and transforms many toxic substances. The liver degrades many harmful chemicals before they become distributed to the tissues. If a decrease in liver function occurs such as with aging or liver disease, a medication is usually eliminated more slowly, resulting in its accumulation. Patients are at risk for medication toxicity if organs that metabolize medications are not functioning correctly. For example, a small sedative dose of a barbiturate sometimes causes a patient with liver disease to lapse into a coma.
Excretion
After medications are metabolized, they exit the body through the kidneys, liver, bowel, lungs, and exocrine glands. The chemical makeup of a medication determines the organ of excretion. Gaseous and volatile compounds such as nitrous oxide and alcohol exit through the lungs. Deep breathing and coughing (see Chapter 40) help patients eliminate anesthetic gases more rapidly after surgery. The exocrine glands excrete lipid-soluble medications. When medications exit through sweat glands, the skin often becomes irritated, requiring you to instruct patients in good hygiene practices (see Chapter 39). If a medication is excreted through the mammary glands, there is a risk that a nursing infant will ingest the chemicals. Check the safety of any medication used in breastfeeding women.
The GI tract is another route for medication excretion. Medications that enter the hepatic circulation are broken down by the liver and excreted into the bile. After chemicals enter the intestines through the biliary tract, the intestines resorb them. Factors that increase peristalsis (e.g., laxatives and enemas) accelerate medication excretion through the feces, whereas factors that slow peristalsis (e.g., inactivity and improper diet) often prolong the effects of a medication.
The kidneys are the main organs for medication excretion. Some medications escape extensive metabolism and exit unchanged in the urine. Others undergo biotransformation in the liver before the kidneys excrete them. If renal function declines, a patient is at risk for medication toxicity. When the kidney cannot adequately excrete a medication, it is necessary to reduce the dose. Maintenance of an adequate fluid intake (8 to 9 cups, or about 2 L of water/day) promotes proper elimination of medications for the average adult.
Types of Medication Action
Medications vary considerably in the way they act and their types of action. Patients do not always respond in the same way to each successive dose of a medication. Sometimes the same medication causes very different responses in different patients. Therefore it is essential to understand all the effects that medications have on patients.
Therapeutic Effects
The therapeutic effect is the expected or predicted physiological response that a medication causes. Each medication has a desired therapeutic effect. For example, nitroglycerin reduces cardiac workload and increases myocardial oxygen supply. Some medications have more than one therapeutic effect. For example, prednisone, a steroid, decreases swelling, inhibits inflammation, reduces allergic responses, and prevents rejection of transplanted organs. Knowing the desired therapeutic effect for each medication allows you to provide patient education and accurately evaluate its desired effect.
Side Effects/Adverse Effects
Every medication has a potential to harm a patient. Side effects are predictable and often unavoidable secondary effects produced at a usual therapeutic dose. They are either harmless or cause injury. For example, some antihypertensive medications cause impotence in men. If the side effects are serious enough to negate the beneficial effects of the therapeutic action of the medication, the prescriber discontinues the medication. Patients often stop taking medications because of side effects. Adverse effects are unintended, undesirable, and often unpredictable severe responses to medication. Some adverse effects are immediate, whereas others take weeks or months to develop. Early recognition is important. When adverse responses to medications occur, the prescriber discontinues the medication immediately. Health care providers report adverse effects to the FDA using the MedWatch program (USFDA, 2010).
Toxic Effects: Toxic effects develop after prolonged intake of a medication or when a medication accumulates in the blood because of impaired metabolism or excretion. Excess amounts of a medication within the body sometimes have lethal effects, depending on its action. For example, toxic levels of morphine, an opioid, cause severe respiratory depression and death. Antidotes are available to treat specific types of medication toxicity. For example, naloxone (Narcan), an opioid antagonist, reverses the effects of opioid toxicity.
Idiosyncratic Reactions: Medications sometimes cause unpredictable effects such as an idiosyncratic reaction, in which a patient overreacts or underreacts to a medication or has a reaction different from normal. For example, a child who receives diphenhydramine (Benadryl), an antihistamine, becomes extremely agitated or excited instead of drowsy. It is not always possible to predict if a patient will have an idiosyncratic response to a medication.
Allergic Reactions: Allergic reactions also are unpredictable responses to a medication. Some patients become immunologically sensitized to the initial dose of a medication. With repeated administration the patient develops an allergic response to it, its chemical preservatives, or a metabolite. The medication or chemical acts as an antigen, triggering the release of the antibodies in the body. A patient’s medication allergy symptoms vary, depending on the individual and the medication (Table 31-2). Among the different classes of medications, antibiotics cause a high incidence of allergic reactions. Severe or anaphylactic reactions, which are life threatening, are characterized by sudden constriction of bronchiolar muscles, edema of the pharynx and larynx, and severe wheezing and shortness of breath. Immediate medical attention is required to treat anaphylactic reactions. A patient with a known history of an allergy to a medication needs to avoid exposure to that medication in the future and wear an identification bracelet or medal (Fig. 31-1), which alerts nurses and physicians to the allergy if the patient is unconscious when receiving medical care.
TABLE 31-2
| SYMPTOM | DESCRIPTION |
| Urticaria | Raised, irregularly shaped skin eruptions with varying sizes and shapes; eruptions have reddened margins and pale centers |
| Rash | Small, raised vesicles that are usually reddened; often distributed over entire body |
| Pruritus | Itching of skin; accompanies most rashes |
| Rhinitis | Inflammation of mucous membranes lining nose; causes swelling and clear, watery discharge |
Medication Interactions
When one medication modifies the action of another, a medication interaction occurs. Medication interactions are common in individuals taking several medications. Some medications increase or diminish the action of others and may alter the way another medication is absorbed, metabolized, or eliminated from the body. When two medications have a synergistic effect, their combined effect is greater than the effect of the medications when given separately. For example, alcohol is a central nervous system depressant that has a synergistic effect on antihistamines, antidepressants, barbiturates, and narcotic analgesics. Sometimes a medication interaction is desired. Prescribers often combine medications to create an interaction that has a beneficial effect. For example, a patient with high blood pressure takes several medications such as diuretics and vasodilators that act together to control the blood pressure when one medication is not effective on its own.
Timing of Medication Dose Responses
Medications administered intravenously enter the bloodstream and act immediately, whereas medications given in other routes take time to enter the bloodstream and have an effect. The quantity and distribution of a medication in different body compartments change constantly. Medications are ordered at various times, depending on when their response begins, becomes most intense, and ceases.
The minimum effective concentration (MEC) is the plasma level of a medication below which the effect of the medication does not occur. The toxic concentration is the level at which toxic effects occur. When a medication is prescribed, the goal is to achieve a constant blood level within a safe therapeutic range, which falls between the MEC and the toxic concentration (Fig. 31-2). When a medication is administered repeatedly, its serum level fluctuates between doses. The highest level is called the peak concentration, and the lowest level is called the trough concentration. After reaching its peak, the serum concentration of the medication falls progressively. With IV infusions the peak concentration occurs quickly, but the serum level also begins to fall immediately. Some medication doses (e.g., vancomycin) are based on peak and trough serum levels. The trough level is generally drawn 30 minutes before administering the drug, and the peak level is drawn whenever the drug is expected to reach its peak concentration. The time it takes for a drug to reach its peak concentration varies, depending on the pharmacokinetics of the medication.
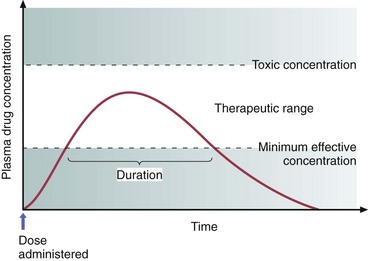
FIG. 31-2 The therapeutic range of a medication occurs between the minimum effective concentration and the toxic concentration. (From Lehne RA: Pharmacology for nursing care, ed 7, St Louis, 2010, Saunders.)
All medications have a biological half-life, which is the time it takes for excretion processes to lower the amount of unchanged medication by half. A medication with a short half-life needs to be given more frequently than a medication with a longer half-life. The half-life does not change, no matter how much medication is given. For example, if the nurse gives 1 g of a medication that has a half-life of 8 hours, the patient excretes 500 mg of the medication in 8 hours. In the next 8 hours the patient excretes 250 mg. This process continues until the medication is totally eliminated from the body.
To maintain a therapeutic plateau the patient must receive regular fixed doses. For example, current evidence shows that pain medications are most effective when they are given around the clock (ATC) rather than when the patient intermittently complains of pain because ATC allows the body to maintain an almost constant level of pain medication. After an initial medication dose, the patient receives each successive dose when the previous dose reaches its half-life.
Safe drug administration involves adherence to prescribed doses and dosage schedules (Table 31-3). Some agencies set schedules for medication administration. However, nurses are able to alter this schedule based on knowledge about a medication. For example, at some agencies medications that are to be taken once a day are given at 9:00 am. However, if a medication works best when given before bedtime, the nurse administers it before the patient goes to sleep. In addition, acute care agencies use guidelines from the Institute for Safe Medication Practices (CMS, 2011; ISMP, 2011) to determine safe, effective, and timely administration of scheduled medications. According to the ISMP guidelines, hospitals need to determine which medications are time-critical and which are non–time-critical. Time-critical medications are medications in which early or delayed administration of maintenance doses (more than 30 minutes before or after the scheduled dose) will most likely cause harm or result in subtherapeutic responses in a patient. Non–time-critical medications include medications in which the timing of administration will most likely not affect the desired effect of the medication if given 1 to 2 hours before or after its scheduled time. You need to administer time-critical medications at a precise time or within 30 minutes before or after the scheduled time. You administer medications identified as non–time-critical within 1 to 2 hours of their scheduled time. Follow your agency’s medication administration policies about the timing of medications to ensure you administer medications at the right time (CMS, 2011; ISMP, 2011).
TABLE 31-4
Terms Associated with Medication Actions
| TERM | MEANING |
| Onset | Time it takes after a medication is administered for it to produce a response |
| Peak | Time it takes for a medication to reach its highest effective concentration |
| Trough | Minimum blood serum concentration of medication reached just before the next scheduled dose |
| Duration | Time during which the medication is present in concentration great enough to produce a response |
| Plateau | Blood serum concentration of a medication reached and maintained after repeated fixed doses |
When teaching patients about dosage schedules, use language that is familiar to the patient. For example, when teaching a patient about medication dosing twice a day, instruct him or her to take it in the morning and again in the evening. Use knowledge about the time intervals and terms used to describe medication actions to anticipate the effect of a medication and educate the patient about when to expect a response (Table 31-4).
Routes of Administration
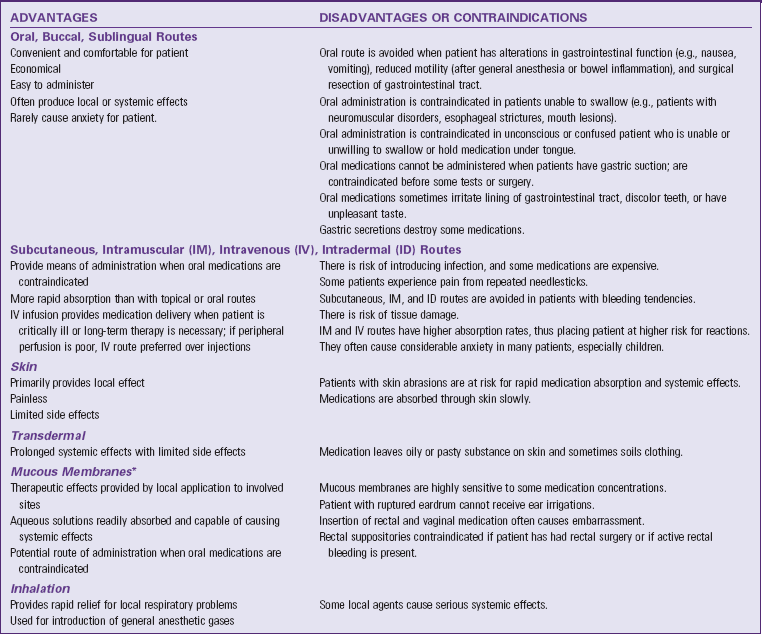
The route prescribed for administering a medication depends on the properties and desired effect of the medication and the patient’s physical and mental condition (Table 31-5). Work with the prescriber in determining the best route for a patient’s medication.
Oral Routes
The oral route is the easiest and the most commonly used route. Medications are given by mouth and swallowed with fluid. Oral medications have a slower onset of action and a more prolonged effect than parenteral medications. Patients generally prefer the oral route.
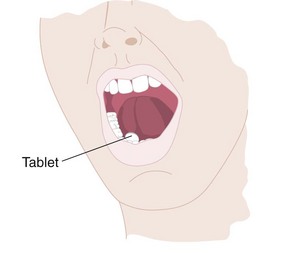
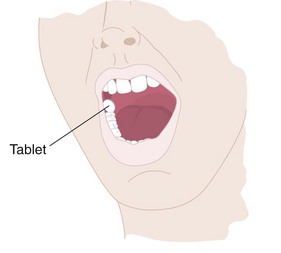
Sublingual Administration: Some medications are readily absorbed after being placed under the tongue to dissolve (Fig. 31-3). A medication given by the sublingual route should not be swallowed because the medication does not have the desired effect. Nurses often give nitroglycerin by the sublingual route. Tell the patient not to drink anything until the medication is completely dissolved.
Buccal Administration: Administration of a medication by the buccal route involves placing the solid medication in the mouth against the mucous membranes of the cheek until it dissolves (Fig. 31-4). Teach patients to alternate cheeks with each subsequent dose to avoid mucosal irritation. Warn patients not to chew or swallow the medication or to take any liquids with it. A buccal medication acts locally on the mucosa or systemically as it is swallowed in a person’s saliva.
Parenteral Routes
Parenteral administration involves injecting a medication into body tissues. The following are the four major sites of injection:
1. Intradermal (ID): Injection into the dermis just under the epidermis
2. Subcutaneous: Injection into tissues just below the dermis of the skin
Some medications are administered into body cavities other than the four types listed here. These additional routes include epidural, intrathecal, intraosseous, intraperitoneal, intrapleural, and intraarterial. Nurses usually are not responsible for the administration of medications through these advanced techniques. Whether or not you actually administer the medication, you remain responsible for monitoring the integrity of the medication delivery system, understanding the therapeutic value of the medication, and evaluating the patient’s response to the therapy.
Epidural: Epidural medications are administered in the epidural space via a catheter, which is placed by a nurse anesthetist or an anesthesiologist. This route is used for the administration of regional analgesia for surgical procedures (see Chapter 43). Nurses who have advanced education in the epidural route can administer medications by continuous infusion or by a bolus dose.
Intrathecal: Physicians and specially educated nurses administer intrathecal medications through a catheter placed in the subarachnoid space or one of the ventricles of the brain. Intrathecal administration is often associated with long-term medication administration through surgically implanted catheters.
Intraosseous: This method of medication administration involves the infusion of medication directly into the bone marrow. It is most commonly used in infants and toddlers who have poor access to their intravascular space and when an emergency arises and IV access is impossible.
Intraperitoneal: Medications administered into the peritoneal cavity are absorbed into the circulation. Chemotherapeutic agents, insulin, and antibiotics are administered in this fashion.
Intrapleural: A syringe and needle or a chest tube is used to administer intrapleural medications directly into the pleural space. Chemotherapeutic agents are the most common medications administered via this method. Physicians also instill medications that help resolve persistent pleural effusion. This is called pleurodesis, which promotes adhesion between the visceral and parietal pleura.
Intraarterial: Intraarterial medications are administered directly into the arteries. Intraarterial infusions are common in patients who have arterial clots. The nurse manages a continuous infusion of clot-dissolving agents and carefully monitors the integrity of the infusion to prevent inadvertent disconnection of the system and subsequent bleeding.
Other methods of medication administration that are usually limited to physician administration are intracardiac, an injection of a medication directly into cardiac tissue, and intraarticular, an injection of a medication into a joint.
Topical Administration
Medications applied to the skin and mucous membranes generally have local effects. You apply topical medications to the skin by painting or spreading the medication over an area, applying moist dressings, soaking body parts in a solution, or giving medicated baths. Systemic effects often occur if a patient’s skin is thin or broken down, the medication concentration is high, or contact with the skin is prolonged. A transdermal disk or patch (e.g., nitroglycerin, scopolamine, and estrogens) has systemic effects. The disk secures the medicated ointment to the skin. These topical applications are left in place for as little as 12 hours or as long as 7 days.
Nurses administer medications to mucous membranes in a variety of ways, including the following, by:
1. Directly applying a liquid or ointment (e.g., eyedrops, gargling, or swabbing the throat).
2. Inserting a medication into a body cavity (e.g., placing a suppository in rectum or vagina or inserting medicated packing into vagina).
3. Instilling fluid into a body cavity (e.g., eardrops, nose drops, or bladder and rectal instillation [fluid is retained]).
4. Irrigating a body cavity (e.g., flushing eye, ear, vagina, bladder, or rectum with medicated fluid [fluid is not retained]).
5. Spraying a medication into a body cavity (e.g., instillation into nose and throat).
Inhalation Route
The deeper passages of the respiratory tract provide a large surface area for medication absorption. Nurses administer inhaled medications through the nasal and oral passages or endotracheal or tracheostomy tubes. Endotracheal tubes enter the patient’s mouth and end in the trachea (Fig. 31-5), whereas tracheostomy tubes enter the trachea directly through an incision made in the neck. Inhaled medications are readily absorbed and work rapidly because of the rich vascular alveolar capillary network present in the pulmonary tissue. Many inhaled medications have local or systemic effects.
Intraocular Route
Intraocular medication delivery involves inserting a medication similar to a contact lens into the patient’s eye. The eye medication disk has two soft outer layers that have medication enclosed in them. The nurse inserts the disk into the patient’s eye, much like a contact lens, and it can remain there for up to 1 week.
Systems of Medication Measurement
The proper administration of a medication depends on your ability to compute medication doses accurately and measure medications correctly. Mistakes in calculating or measuring medications correctly often lead to fatal errors. As a nurse you are responsible for checking calculations carefully before giving a medication.
Medication therapy uses the metric, apothecary, and household systems of measurement. The apothecary system is used infrequently today. Although the U.S. Congress has not officially adopted the metric system, most health professionals in the United States use it. Health care providers usually write prescriptions to be self-administered in household measures for patients.
Metric System
As a decimal system, the metric system is the most logically organized. Metric units are easy to convert and compute through simple multiplication and division. Each basic unit of measurement is organized into units of 10. Multiplying or dividing by 10 forms secondary units. In multiplication the decimal point moves to the right; in division the decimal moves to the left. For example:
The basic units of measurement in the metric system are the meter (length), the liter (volume), and the gram (weight). For medication calculations only use the volume and weight units. In the metric system use lowercase or capital letters to designate basic units:
Use lowercase letters for abbreviations for other units:
A system of Latin prefixes designates subdivision of the basic units: deci- ( or 0.1), centi- (
or 0.1), centi- ( or 0.01), and milli- (
or 0.01), and milli- ( or 0.001). Greek prefixes designate multiples of the basic units: deka- (10), hecto- (100), and kilo- (1000). When writing medication doses in metric units, prescribers and nurses use fractions or multiples of a unit. Convert fractions to decimals.
or 0.001). Greek prefixes designate multiples of the basic units: deka- (10), hecto- (100), and kilo- (1000). When writing medication doses in metric units, prescribers and nurses use fractions or multiples of a unit. Convert fractions to decimals.
Many actual and potential medication errors happen with the use of fractions and decimal points. Follow practice standards when medications are ordered in fractions to prevent medication errors. For example, to make the decimal point more visible, a leading zero is always placed in front of a decimal (e.g., use 0.25 not .25). Never use a trailing zero (i.e., a zero after a decimal point) because, if a health care worker does not see the decimal point, the patient may receive 10 times more medication than that prescribed (e.g., use 5 not 5.0) (ISMP, 2010b; TJC, 2011).
Household Measurements
Household units of measure are familiar to most people. Their disadvantage is their inaccuracy. Household utensils such as teaspoons and cups vary in size. Scales to measure pints or quarts are not well calibrated. Household measures include drops, teaspoons, tablespoons, and cups for volume and pints and quarts for weight. The advantage of household measurements is their convenience and familiarity. When the accuracy of a medication dose is not critical (e.g., [OTC medications]), it is safe to use household measures. To calculate medications accurately, you need to know common equivalents of metric and household units (Table 31-6).
TABLE 31-6
| METRIC | APOTHECARY | HOUSEHOLD |
| 1 mL | 15-16 minims* | 15 drops (gtt) |
| 5 mL | 1 dram* | 1 teaspoon (tsp) |
| 15 mL | 4 drams* | 1 tablespoon (tbsp) |
| 30 mL | 1 fluid ounce | 2 tablespoons (tbsp) |
| 240 mL | 8 fluid ounces | 1 cup (c) |
| 480 mL (approximately 500 mL) | 1 pint (pt) | 1 pint (pt) |
| 960 mL (approximately 1 L) | 1 quart (qt) | 1 quart (qt) |
| 3840 mL (approximately 4 L) | 1 gallon (gal) | 1 gallon (gal) |
*Minums and drams are no longer acceptable units of measure for medication administration although some medication cups and syringes still have them listed. Use mL for safe medication preparation (Morris, 2010).
Solutions
The nurse uses solutions of various concentrations for injections, irrigations, and infusions. A solution is a given mass of solid substance dissolved in a known volume of fluid or a given volume of liquid dissolved in a known volume of another fluid. When a solid is dissolved in a fluid, the concentration is in units of mass per units of volume (e.g., g/L, mg/mL). A concentration of a solution can also be expressed as a percentage. For example, a 10% solution is 10 g of solid dissolved in 100 mL of solution. A proportion also expresses concentrations. A  solution represents a solution containing 1 g of solid in 1000 mL of liquid or 1 mL of liquid mixed with 1000 mL of another liquid.
solution represents a solution containing 1 g of solid in 1000 mL of liquid or 1 mL of liquid mixed with 1000 mL of another liquid.
Nursing Knowledge Base
The IOM (2003) published the book To Err Is Human: Building a Safer Health System. This book created a new national awareness of problems within the health care system. It estimated that up to 98,000 people die in any given year from medical errors that occur in hospitals. This means that more people die from medical errors than from motor vehicle accidents, breast cancer, acquired immunodeficiency syndrome (AIDS), and workplace injuries. Health care experts estimate that medication-related errors for hospitalized patients cost more than $3.5 billion annually (IOM, 2007).
Nurses play an important role in patient safety, especially in the area of medication administration. The safe administration of medications is also an important topic for current nursing researchers (Box 31-2). Nurses need to know how to calculate medication doses accurately and understand the different roles that members of the health care team play in prescribing and administering medications. All of the nurse’s previous learning is important and is often applied to ensure safe medication administration.
Clinical Calculations
To administer medications safely, you need to have an understanding of basic mathematics skills to calculate medication doses, mix solutions, and perform a variety of other activities. This is important because medications are not always dispensed in the unit of measure in which they are ordered. Medication companies package and bottle medications in standard dosages. For example, the patient’s health care provider orders 20 mg of a medication that is available only in 40-mg vials. Nurses frequently convert available units of volume and weight to desired doses. Therefore be aware of equivalents in all major measurement systems. You use equivalents when performing other nursing actions such as when calculating patients’ intake and output and IV flow rates.
Conversions Within One System
Converting measurements within one system is relatively easy; simply divide or multiply in the metric system. To change milligrams to grams, divide by 1000, moving the decimal 3 points to the left.
To convert liters to milliliters, multiply by 1000 or move the decimal 3 points to the right.
To convert units of measurement within the household system, consult an equivalent table. For example, when converting fluid ounces to quarts, you first need to know that 32 ounces is the equivalent of 1 quart. To convert 8 ounces to a quart measurement, divide 8 by 32 to get the equivalent,  or 0.25 quart.
or 0.25 quart.
Conversion Between Systems
Nurses frequently determine the proper dose of a medication by converting weights or volumes from one system of measurement to another. Thus sometimes you convert metric units to equivalent household measures for use at home. To calculate medications it is necessary to work with units in the same measurement system. Tables of equivalent measurements are available in all health care institutions. The pharmacist is also a good resource.
Before converting, compare the measurement system available with that ordered. For example, the prescriber orders Robitussin 30 mL, but the patient only has tablespoons at home. To properly instruct the patient, you convert mL to tablespoons, which requires you to know the equivalent or refer to a table such as Table 31-6.
Dose Calculations
Methods used to calculate medication doses include the ratio and proportion method, the formula method, and dimensional analysis. Before completing any calculation, make a mental estimate of the approximate and reasonable dosage. If the estimate does not match the calculated solution, recheck the calculation before preparing and administering the medication. Many nursing students are anxious when calculating medication doses. To enhance accuracy and reduce anxiety, think critically about the processes used during the calculation and practice doing calculations until you feel confident about your mathematics skills (Walsh, 2008). In addition, choose the method of calculation with which you are most comfortable and use it consistently (Morris, 2010). Most health care agencies require a nurse to double-check calculations with another nurse before giving medications, especially when the risk for giving the wrong medication is high (e.g., heparin, insulin). Always have another nurse double-check your work if you are unsure about the answer or if the answer to a medication calculation seems unreasonable or inappropriate.
The Ratio and Proportion Method: A ratio indicates the relationship between two numbers separated by a colon (:). The colon in the ratio indicates the need to use division. Think of a ratio as a fraction; the number to the left is the numerator, and the number to the right is the denominator. For example, the ratio 1 : 2 is the same as  . Write a proportion in one of three ways:
. Write a proportion in one of three ways:
In a proportion the first and last numbers are called the extremes, and the second and third numbers are called the means. When multiplying the extremes, the answer is the same when multiplying the means. For example, in the previous proportions, multiplying the extremes (1 × 8 = 8) is the same result as multiplying the means (2 × 4 = 8). Because of this relationship, if you know three of the numbers in the proportion, calculating the unknown fourth number is easy. The numbers need to all be in the same unit and system of measurement. To solve a calculation using the ratio and proportion method, first estimate the answer in your mind. Then set up the proportion, labeling all the terms. Put the terms of the ratio in the same sequence (e.g., mg : mL = mg : mL). Cross multiply the means and the extremes and divide both sides by the number before the x to obtain the dosage. Always label the answer; if the answer is not close to the estimate, recheck the calculation.
Example: The prescriber orders 500 mg of amoxicillin to be administered in a gastric tube every 8 hours. The bottle of amoxicillin is labeled 400 mg/5 mL. Use the following steps to calculate how much amoxicillin to give:
1. Estimate the answer: The amount to be given is a little more than the amount that is provided in the solution; therefore the answer is a little more than 5 mL.
3. Cross multiply the means and the extremes:
4. Divide both sides by the number before x:
5. Compare the estimate in Step 1 with the answer in Step 4: The answer (6.25 mL) is close to the estimated amount (a little more than 5 mL). Therefore the answer is correct; prepare and administer 6.25 mL in the patient’s gastric tube.
The Formula Method: Using this method requires you to first memorize the formula. Estimate the answer and then place all the information from the medication order into the formula. Label all the parts of the formula and ensure that all measures in the formula are in the same units and system of measurement before calculating the dosage. If the measures are not in the same measurement system, convert the numbers to the same system before calculating the dose. Calculate and label the answer and compare the answer with the estimated answer. If the estimate is not similar to the answer, recheck the calculation. Use the following basic formula when using the formula method:
The dose ordered is the amount of medication prescribed. The dose on hand is the dose (e.g., mg, units) of medication supplied by the pharmacy. The amount on hand is the basic unit or quantity of the medication that contains the dose on hand. For solid medications the amount on hand is often one capsule; the amount of liquid on hand is sometimes 1 mL or 1 L, depending on the container. For example, a liquid medication comes in the strength of 125 mg per 5 mL. In this case 125 mg is the dose on hand, and 5 mL is the amount on hand. The amount to administer is the actual amount of medication the nurse administers. Always express the amount to administer in the same unit as the amount on hand.
Example: The prescriber orders morphine sulfate 2 mg IV. The medication is available in a vial containing 10 mg/mL. The formula is applied as follows:
1. Estimate the answer: The medication is a liquid; thus the answer will be in milliliters (mL). The amount to be given is less than  of the dose; thus the answer will be less than
of the dose; thus the answer will be less than  mL.
mL.
4. Compare the estimate in Step 1 with the answer in Step 3: The answer is less than  mL; thus it is close to the estimated answer. Prepare 0.2 mL of the medication in a syringe and administer it to the patient.
mL; thus it is close to the estimated answer. Prepare 0.2 mL of the medication in a syringe and administer it to the patient.
Dimensional Analysis: Dimensional analysis is the factor-label or the unit factor method. There is no need to memorize a formula since only one equation is needed and the same steps are used in solving every medication calculation. One research study shows that nursing students who use dimensional analysis often calculate medications more accurately than when they use the formula method (Greenfield, Whelan, and Cohn, 2006). Use the following steps to calculate medication doses by dimensional analysis:
1. Identify the unit of measure that you need to administer. For example, if you are giving a pill, you usually give a tablet or a capsule; for parenteral or liquid oral medications, the unit is milliliters.
3. Place the name or appropriate abbreviation for x on the left side of the equation (e.g., x tab, x mL).
4. Place available information from the problem in a fraction format on the right side of the equation. Place the abbreviation or unit that matches what you are going to administer (determined in Step 1) in the numerator.
5. Look at the medication order and add other factors into the problem. Set up the numerator so it matches the unit in the previous denominator.
6. Cancel out like units of measurement on the right side of the equation. You should end up with only one unit left in the equation, and it should match the unit on the left side of the equation.
7. Reduce to the lowest terms if possible, and solve the problem or solve for x. Label your answer.
8. Compare your estimate from Step 1 with your answer in Step 2.
Example: The prescriber orders 0.45 g penicillin V potassium through a gastric tube. The bottle says: penicillin V potassium 125 mg/5 mL.
1. Identify the unit of measure that you need to administer. This medication is given in a gastric tube, which is a liquid medication; therefore the answer will be in milliliters (mL).
2. Estimate the answer. The medication order is more than three times but less than four times is the amount in the vial; thus the answer is more than 15 mL but less than 20 mL.
3. Place the name or appropriate abbreviation for x on the left side of the equation.
4. Place available information from the problem in a fraction format on the right side of the equation. Since the medication will be administered in milliliters, place mL in the numerator.
5. Look at the medication order and add other factors into the problem. Set up the numerator so it matches the unit in the previous denominator. The order is for 0.45 g, and the medication is available in 125-mg bottles. Knowing that 1 g = 1000 mg, add this conversion to the calculation.
6. Cancel out like units of measurement on the right side of the equation.
7. Reduce to the lowest terms if possible and solve the problem or solve for x. Label your answer.
8. Compare the estimate from Step 2 with the answer in Step 7. The calculated answer is 18 mL, which is between 15 mL and 20 mL. This matches the estimate made in Step 2. Prepare and administer 18 mL of medication as ordered.
Pediatric Doses
Current evidence shows that children are three times more at risk for experiencing a medication error than adults (TJC, 2008). Medication errors involving children frequently happen for the following reasons (Morris, 2010):
• Confusion between formulations for adults and children
• Availability of multiple pediatric concentrations of oral liquid medications
• Inaccurate preparation of medications that need to be diluted
• Similar packaging of medications and names of medications that look alike and sound alike
• Parents who do not understand how to correctly prepare and administer medications
• Errors in calculation and use of inaccurate measuring devices (e.g., household teaspoons and tablespoons) as opposed to devices made to measure small volume doses
Calculating children’s medication doses requires caution (Hockenberry and Wilson, 2009). Even small errors or discrepancies in medication amounts can negatively affect a child’s health (Morris, 2010). The child’s age, weight, and maturity of body systems affect the ability to metabolize and excrete medications. Nurses sometimes have difficulties evaluating the child’s response to a medication, especially when he or she cannot communicate verbally. For example, a side effect of vancomycin is ototoxicity. If a child cannot talk yet, it is challenging to assess for ototoxicity.
Use the following guidelines when calculating pediatric doses:
1. Most pediatric medications are ordered in milligrams per kilogram (mg/kg). Therefore ensure that the patient’s weight is expressed in kilograms. Avoid converting the patient’s weight whenever possible. If you have to convert pounds to kilograms, remember that 1 kg = 2.2 lb and convert the patient’s weight before calculating the medication dosage.
2. Pediatric doses are usually a lot smaller than adult doses for the same medication. You frequently use micrograms and small syringes (e.g., tuberculin or 1 mL).
3. IM doses are very small and usually do not exceed 1 mL in small children or 0.5 mL in infants.
4. Subcutaneous dosages are also very small and do not usually exceed 0.5 mL.
5. Most medications are not rounded off to the nearest tenth. Instead they are rounded to the nearest thousandth.
6. Measure dosages that are less than 1 mL in syringes that are marked in tenths of a milliliter if the dosage calculation comes out even and does not need to be rounded. Use a tuberculin syringe for medication preparation when the medication needs to be rounded to the nearest thousandth.
7. Estimate the patient’s dose before beginning the calculation; label and compare the answer with the estimate before preparing the medication.
8. To determine if a dose is safe before giving the medication, compare and evaluate the amount of medication ordered over 24 hours with the recommended dosage.
Different formulas and methods are used to calculate drug dosages in children. The two most common methods of calculating pediatric dosages are based on a child’s weight or BSA. BSA is used in rare situations (e.g., determining chemotherapy doses). To estimate a child’s BSA, use Mosteller’s formula or the standard nomogram (e.g., the West nomogram). Refer to a pediatric or pharmacology resource and consult with the patient’s health care provider or the pharmacist if you have to calculate a medication based on BSA.
Most of the time you calculate medications based on a child’s weight. You can use the ratio and proportion method, the formula method, or dimensional analysis to calculate a pediatric dose using body weight. The example that follows explains how to use dimensional analysis to calculate pediatric doses. Refer to the previous sections on ratio and proportion and the formula method if you decide that they are easier for you to use.
Example: You receive an order to give ticarcillin/clavulanate 50 mg/kg q4h for a 5-year-old child who weighs 18 kg. The medication label says that there is 200 mg of ticarcillin/clavulanate in 1 mL of normal saline. How much ticarcillin/clavulanate do you give?
1. Identify the unit of measure that you need to administer. This medication is given IV piggyback, which is a parenteral medication. Therefore your answer will be in milliliters.
2. Estimate the answer. The medication is ordered 50 mg/kg. Round the child’s weight up to 20 kg and multiply it by 50 mg to estimate the total amount of mg to be given. In your estimate the patient needs about 1000 mg. Because the medication comes in a vial of 200 mg in 1 mL and 1000 mg is 5 times larger than the dose of the medication and because you rounded the patient’s weight up to 20 kg, you need to give a little less than 5 mL.
3. Place the name or appropriate abbreviation for x on the left side of the equation.
4. Place available information from the problem in a fraction format on the right side of the equation. Set up the numerator so it matches the unit in the previous denominator: You are going to administer the medication in milliliters; therefore place the mL in the numerator.
5. Look at the medication order and add other factors into the problem. Set up the numerator so that it matches the unit in the previous denominator. You know that you need to give 50 mg/kg and that your patient weighs 18 kg.
6. Cancel out like units of measurement on the right side of the equation.
7. Reduce to the lowest terms if possible and solve the problem or solve for x. Label your answer.
8. Compare the estimate from Step 2 with the answer in Step 7. The answer is 4.5 mL, which is a little less than 5 mL. Since this is close to the estimate you made in Step 2, the calculation is correct, and you can continue with medication preparation at this time.
Prescriber’s Role
The physician, nurse practitioner, or physician’s assistant prescribes medications by writing an order on a form in the patient’s medical record, in an order book, or on a legal prescription pad. Some prescribers use a desktop, laptop, or handheld electronic device to enter medication orders. Many hospitals are implementing computerized physician order entry (CPOE) to handle medication orders to decrease medication errors. In these systems the prescriber completes all computerized fields before the order for the medication is filled, thus avoiding incomplete or illegible orders.
Sometimes a prescriber orders a medication by talking directly to the nurse or by telephone. An order for a medication or medical treatment made over the telephone is called a telephone order. If the order is given verbally to the nurse, it is called a verbal order. When a verbal or telephone order is received, the nurse who took the order writes the complete order or enters it into a computer, reads it back, and receives confirmation from the prescriber to confirm accuracy. The nurse indicates the time and name of the prescriber who gave the order, signs it, and follows agency policy to indicate that it was read back. The prescriber countersigns the order at a later time, usually within 24 hours after giving it. Follow guidelines for taking verbal or telephone orders for medications safely (Box 31-3). Institutional policies vary regarding personnel who can take verbal or telephone orders. Nursing students cannot take them. They only give newly ordered medications after a registered nurse has written and verified the order.
Common abbreviations are often used when writing orders. Abbreviations indicate dosage frequencies or times, routes of administration, and special information for giving the medication (see Table 31-3). Medication errors frequently involve the use of abbreviations. Table 31-7 lists abbreviations that are associated with a high incidence of medication errors. Do not use these abbreviations when documenting medication orders or other information about medications (ISMP, 2010b; TJC, 2011b). Sometimes abbreviations used in different agencies vary. Check agency policy to determine which abbreviations are acceptable to use and their meaning.
TABLE 31-7
ISMP List of Error-Prone Abbreviations, Symbols, and Dose Designations
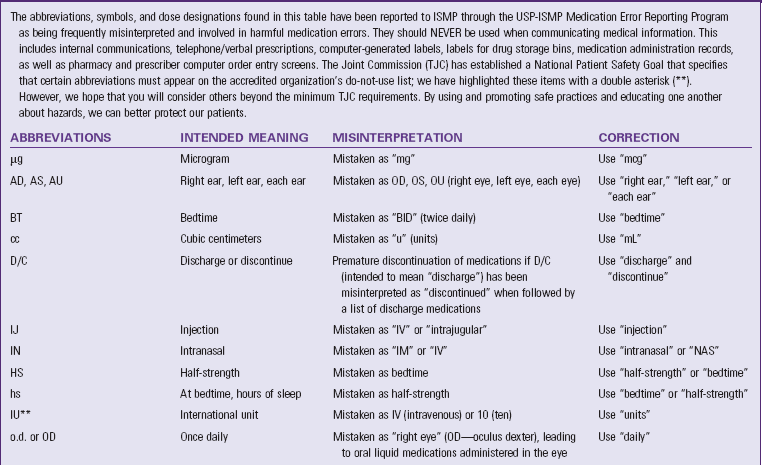
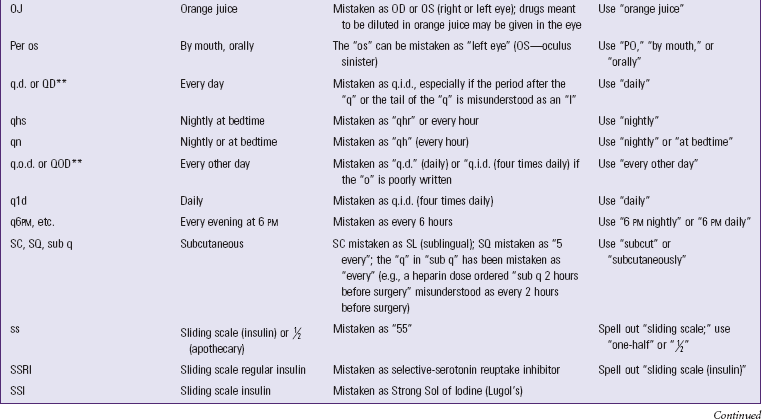
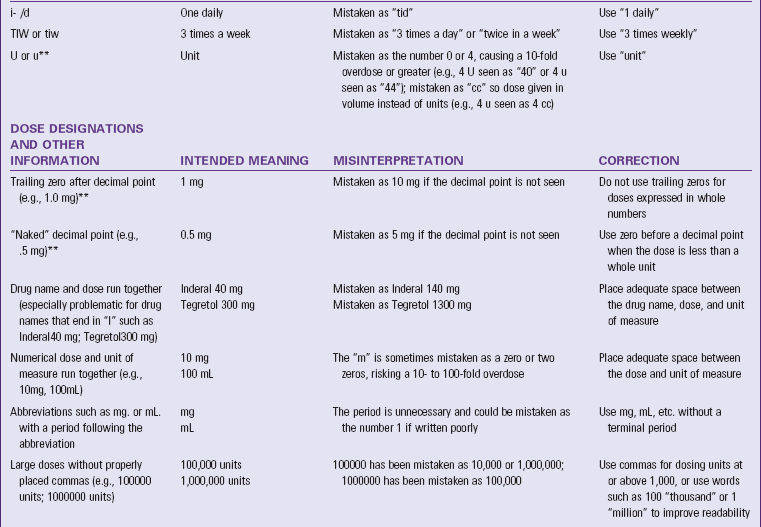
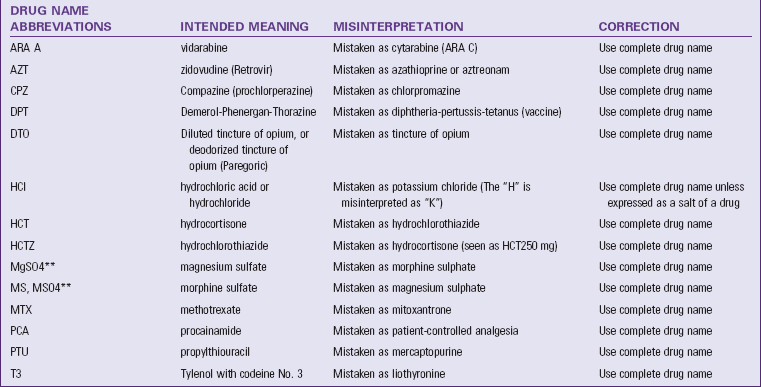
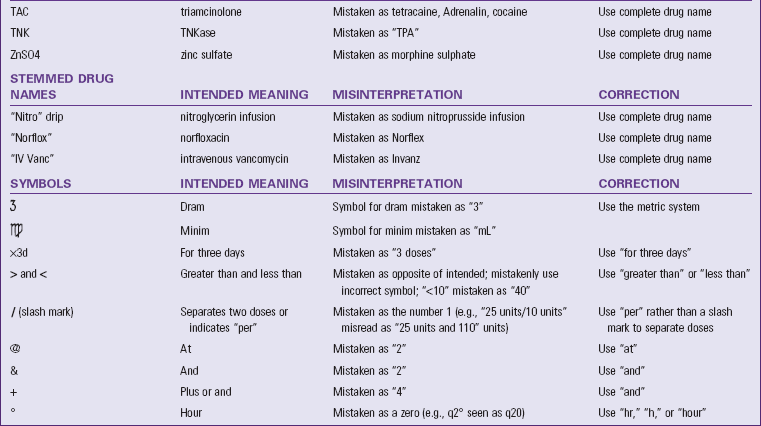
ISMP, Institute for Safe Medication Practices.
**These abbreviations are included on TJC’s “minimum list” of dangerous abbreviations, acronyms and symbols that must be included on an organization’s “Do Not Use” list, effective January 1, 2004. Visit www.jointcommission.org for more information about this TJC requirement.
Permission is granted to reproduce material for internal newsletters or communications with proper attribution. Other reproduction is prohibited without written permission. Unless noted, reports were received through the USP-ISMP Medication Errors Reporting Program (MERP). Report actual and potential medication errors to the MERP via the web at www.ismp.org or by calling 1-800 FAIL-SAF(E). ISMP guarantees confidentiality of information received and respects reporters’ wishes as to the level of detail included in publications.
Types of Orders in Acute Care Agencies
You must have a medication order before giving a medicine to a patient. Five common types of medication orders are based on the frequency and/or urgency of medication administration. Some conditions change the status of a patient’s medication orders. For example, in some agencies the patient’s preoperative medications are automatically discontinued, and the health care provider writes new medication orders after surgery (see Chapter 50). Agency policies that surround medication orders often vary. Nurses need to be aware of and follow these policies.
Standing Orders or Routine Medication Orders
A standing order is carried out until the prescriber cancels it by another order or a prescribed number of days elapse. A standing order often indicates a final date or number of treatments or doses. Many agencies have policies for automatically discontinuing standing orders. The following are examples of standing orders:
prn Orders
Sometimes the prescriber orders a medication to be given only when a patient requires it. This is a prn order. Use objective and subjective assessment and discretion in determining whether or not the patient needs the medication. An example of a prn order is:
This order indicates that the patient needs to wait at least 2 hours between doses and can take the medication if experiencing pain at the incision. When administering medications, document the assessment findings that show why the patient needs the medication and the time of administration. Frequently evaluate the effectiveness of the medication and record findings in the appropriate record. Orders for prn medications that include a range (e.g., morphine sulfate IM 5-10 mg every 4-6 hours) are unclear and a source of medication errors. If a range order is written, ensure that the order follows agency policy for these types of orders. An example of a safer range order is to increase morphine dosage 50% to 100% if pain is moderate to severe.
Single (One-Time) Orders
Sometimes a prescriber orders a medication to be given only once at a specified time. This is common for preoperative medications or medications given before diagnostic examinations, for example:
STAT Orders
A STAT order signifies that a single dose of a medication is to be given immediately and only once. STAT orders are often written for emergencies when a patient’s condition changes suddenly. For example:
Now Orders
A now order is more specific than a one-time order and is used when a patient needs a medication quickly but not right away, as in a STAT order. When receiving a now order, the nurse has up to 90 minutes to administer the medication. Only administer now medications one time. For example:
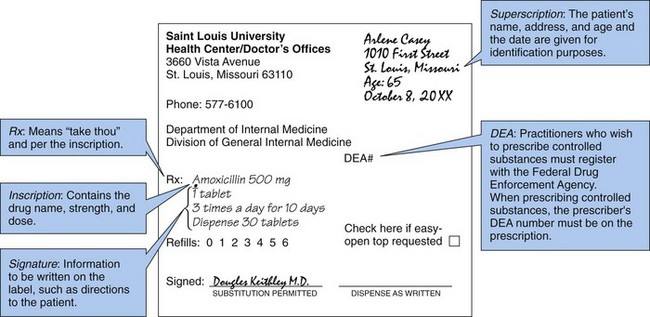
Prescriptions
The prescriber writes prescriptions for patients who are to take medications outside the hospital. The prescription includes more detailed information than a regular order because the patient needs to understand how to take the medication and when to refill the prescription if necessary. Some agencies require prescribers to write prescriptions for controlled substances on a special prescription pad that is different (e.g., a different color) than the prescription pad used for other medications. Fig. 31-6 illustrates the parts of a prescription.
Pharmacist’s Role
The pharmacist prepares and distributes prescribed medications. Pharmacists work with nurses, physicians, and other health care providers to evaluate the efficacy of patients’ medications. They are responsible for filling prescriptions accurately and being sure that prescriptions are valid. Pharmacists in health care agencies rarely mix compounds or solutions, except in the case of IV solutions. Most medication companies deliver medications in a form ready for use. Dispensing the correct medication, in the proper dosage and amount, with an accurate label is the pharmacist’s main task. He or she also provides information about medication side effects, toxicity, interactions, and incompatibilities.
Distribution Systems
Systems for storing and distributing medications vary. Pharmacists provide the medications, but nurses distribute them to patients. Institutions providing nursing care have a special area for stocking and dispensing medications. Special medication rooms, portable locked carts, computerized medication cabinets, and individual storage units next to patients’ rooms are examples of storage areas used. Medication storage areas need to be locked when unattended.
Unit Dose
The unit-dose system uses carts containing a drawer with a 24-hour supply of medications for each patient. Each drawer is labeled with the name of the patient in his or her designated room. The unit dose is the ordered dose of medication that the patient receives at one time. Each tablet or capsule is wrapped in a foil or paper container. At a designated time each day the pharmacist or a pharmacy technician refills the drawers in the cart with a fresh supply. The cart also contains limited amounts of prn and stock medications for special situations. Controlled substances are not kept in the individual patient drawer. Instead they are kept in a larger locked drawer to keep them secure. The unit-dose system reduces the number of medication errors and saves steps in dispensing medications.
Automated Medication Dispensing Systems
Automated medication dispensing systems (AMDSs) are used throughout the country (Fig. 31-7). The systems within an agency are networked with one another and with other agency computer systems (e.g., computerized medical record). AMDSs control the dispensing of all medications, including narcotics. Each nurse accesses the system by entering a security code. Some systems require bioidentification as well. In these systems you place your finger on a screen to access the computer. You select the patient’s name and his or her drug profile before the AMDS dispenses a medication. In these systems you are allowed to select the desired medication, dosage, and route from a list displayed on the computer screen. The system causes the drawer containing medication to open, records it, and charges it to the patient. Systems that are connected to the patient’s computerized medical record then record information about the medication (e.g., medication name, dose, time) and the nurse’s name in the patient’s medical record. Some systems require nurses to scan bar codes to identify the patient, the medication, and the nurse administering the medication before recording this information in the patient’s computerized medical record. Agencies that implement AMDS with bar-code scanning often reduce the incidence of medication errors (see Box 31-2).
Nurse’s Role
Administering medications to patients requires knowledge and a set of skills that are unique to a nurse. You first assess that the medication ordered is the correct medication. Do not assume that all medications that are in the patient’s “drawer” or pillbox are to be given to him or her. Assess the patient’s ability to self-administer medications, determine whether a patient should receive a medication at a given time, administer medications correctly, and closely monitor their effects. Patient and family education about proper medication administration and monitoring is an integral part of your role. Do not delegate any part of the medication administration process to nursing assistive personnel (NAP) and use the nursing process to integrate medication therapy into care.
Medication Errors
A medication error can cause or lead to inappropriate medication use or patient harm. Medication errors include inaccurate prescribing, administering the wrong medication, giving the medication using the wrong route or time interval, and administering extra doses or failing to administer a medication. Preventing medication errors is essential. The process of administering medications has many steps and involves many members of the health care team. Because nurses play an essential role in preparing and administering medications, they need to be vigilant in preventing errors (Box 31-4). Advances in technology have helped to decrease the occurrence of medication errors (Box 31-5).
Medication errors are related to practice patterns, health care product design, or procedures and systems such as product labeling and distribution. When an error occurs, the patient’s safety and well-being become the top priority. The nurse first assesses and examines the patient’s condition and notifies the health care provider of the incident as soon as possible. Once the patient is stable, the nurse reports the incident to the appropriate person in the institution (e.g., manager or supervisor). The nurse is responsible for preparing a written occurrence or incident report that usually needs to be filed within 24 hours of the error. The report includes patient identification information; the location and time of the incident; an accurate, factual description of what occurred and what was done; and the signature of the nurse involved. The occurrence report is not a permanent part of the medical record and is not referred to anywhere in the record (see Chapters 23 and 26). This legally protects the nurse and institution. Agencies use occurrence reports to track incident patterns and initiate quality improvement programs as needed.
Report all medication errors, including those that do not cause obvious or immediate harm or near misses. It is important to feel comfortable in reporting an error and not fear repercussions from managerial staff. Even when a patient suffers no harm from a medication error, the institution can still learn why the mistake occurred and what can be done to avoid similar errors in the future.
Medication errors often happen when patients experience changes in the health care setting, level of care, or health care provider (e.g., goes to a health care provider’s office, transfers from one patient care unit to another, is discharged from a health care setting). Reconciling the list of a patient’s medications is essential to medication safety (TJC, 2011a). Nurses play an essential role in medication reconciliation (Box 31-6). Whenever a nurse admits a patient to a health care setting, he or she compares the medications that the patient took in the previous setting (e.g., home or another nursing unit) with his or her current medication orders (Mayhew, 2010). When the patient leaves that setting for another setting (e.g., skilled care facility or intensive care unit), the nurse communicates the patient’s current medications with the health care providers in the new setting. The nurse also reconciles the patient’s medications when he or she is discharged from an agency or is seen in an outpatient setting. Many agencies have computerized or written forms to facilitate the process of medication reconciliation. The process is challenging and takes a lot of time and concentration. Eliminate distractions and go slowly when reconciling patients’ medications. Always clarify information when needed. Nurses need to consult with the patient, caregivers, family members, pharmacists, and other members of the health care team when reconciling medications.
Critical Thinking
You will use knowledge from many disciplines when administering medications to understand why a particular medication is prescribed for a patient and how the medication will alter the patient’s physiology to have a therapeutic effect. For example, in physiology you learn that potassium is a major intracellular ion. When patients do not have enough potassium in their body (hypokalemia), they experience signs and symptoms such as muscle fatigue or weakness. In some cases severe hypokalemia is fatal as a result of associated cardiac dysrhythmias. Prescribed medications help to restore the patient’s potassium level to normal, which then relieves the signs and symptoms of hypokalemia. In another example knowledge about child development indicates that children often associate medication administration with a negative experience. Use principles from child development to ensure that the child cooperates with the medication experience.
Nurses administer a variety of medications, and new medications are constantly approved. As a result, they do not always have knowledge about the medications they are asked to administer. Critical thinkers admit what they do not know and acquire the knowledge needed to safely administer unfamiliar medications. This means consulting more expert nurses, a pharmacist, the prescriber, or a medication book.
Experience
Nursing students have limited experience with medication administration as it applies to professional practice. Clinical experiences provide you with opportunities to use the nursing process as it applies to medication administration. As you gain experience in medication administration, your psychomotor skills (“the how-to”) become more refined. However, psychomotor skills represent a small part of medication administration. Patient attitudes, knowledge, physical and mental status, and responses make medication administration a complex experience.
Attitudes
To administer medications safely, many critical thinking skills are essential. For example, be disciplined and take adequate time to prepare and administer medications. Take the time to read your patient’s medical record before administering medications and carefully review his or her history, physical examination, and orders. Look up medications that you do not know in a medication reference and determine why each patient is taking each of his or her prescribed medications. Every step of safe medication administration requires a disciplined attitude and a comprehensive, systematic approach. Following the same procedure each time medications are administered ensures safe administration.
Responsibility and accountability are other critical thinking attitudes essential to safe medication administration. Accept full accountability and responsibility for all actions surrounding the administration of medications. Do not assume that a medication that is ordered for a patient is the correct medication or the correct dose. Be responsible for knowing that the medications and doses ordered are correct and appropriate. You are accountable if you give an ordered medication that is knowingly inappropriate for the patient. Therefore be familiar with each therapeutic effect, usual dosage, anticipated changes in laboratory data, and side effects of a drug. You are also responsible for ensuring that patients or caregivers who self-administer medications have been properly informed about all aspects of self-administration (TJC, 2010). If it is determined that a patient cannot safely self-administer medications, design interventions such as involving family caregivers to ensure safe self-administration of medications.
Standards
Standards are actions that ensure safe nursing practice. Standards for medication administration are set by individual health care agencies and the nursing profession. Agency policy usually sets limits on the nurse’s ability to administer medications in certain units of the acute care setting. Sometimes nurses are limited by certain medication routes or dosages. Most institutions have nursing procedure manuals that contain policies that define the types of medications nurses can and cannot administer. The types and dosages of medications that nurses deliver often vary from unit to unit within the same facility. For example, phenytoin (Dilantin), a powerful medication for treating seizures, may be administered by mouth or IV push. In large dosages phenytoin affects heart rhythm. Therefore some agencies place limits on how much nurses can give to a patient on a nursing unit that does not have the ability to monitor the patient’s heart rate and rhythm. Not all prescribers are aware of all of the limitations and sometimes prescribe medications that nurses cannot give in a particular health care setting. Recognize these limitations and inform the prescriber accordingly. Take appropriate actions to ensure that patients receive medications as prescribed and within the time prescribed in the appropriate environment.
Professional standards such as Nursing: Scope and Standards of Practice (American Nurses Association [ANA], 2010) (see Chapters 1 and 23) apply to the activity of medication administration. To prevent medication errors, follow the six rights of medication administration consistently every time you administer medications. Many medication errors can be linked, in some way, to an inconsistency in adhering to these six rights:
Right Medication
A medication order is required for every medication that you administer to a patient. Sometimes prescribers write orders by hand in the patient’s medical record. However, many agencies use CPOE. CPOE allows prescribers to electronically order medications, eliminating the need for written orders and enhancing medication safety (Sowan et al., 2010). Regardless of how the nurse receives a medication order, he or she compares the prescriber’s written orders with the medication administration record (MAR) or electronic medication administration record (eMAR) when it is initially ordered. Nurses verify medication information whenever new MARs are created or distributed or when patients transfer from one nursing unit or health care setting to another (TJC, 2011a).
Once you determine that information on the patient’s MAR is accurate, use it to prepare and administer medications. When preparing medications from bottles or containers, compare the label of the medication container with the MAR three times: (1) before removing the container from the drawer or shelf, (2) as the amount of medication ordered is removed from the container, and (3) at the patient’s bedside before administering the medication to the patient. Never prepare medications from unmarked containers or containers with illegible labels (TJC, 2010). With unit-dose prepackaged medications, check the label with the MAR when taking medications out of the medication dispensing system. Finally verify all medications at the patient’s bedside with the patient’s MAR and use at least two identifiers before giving the patient any medications (TJC, 2011a).
Patients who self-administer medications need to keep them in their original labeled containers, separate from other medications, to avoid confusion. Many hospitals request that all medication administration in the hospital setting be completed through nurses rather than letting patients self-administer to ensure that patients are not receiving double doses. Because the nurse who administers the medication is responsible for any errors related to it, nurses administer only the medications they prepare. You cannot delegate preparation of medication to another person and then administer the medication to the patient. If a patient questions the medication, do not ignore these concerns. An alert patient or a family caregiver familiar with a patient’s medications knows whether a medication is different from those received before. In most cases the patient’s medication order has changed; however, some patient questions reveal an error. When this occurs, withhold the medication and recheck it against the prescriber’s orders. If a patient refuses a medication, discard it rather than returning it to the original container. Unit-dose medications can be saved if they are not opened. If a patient refuses narcotics, follow proper hospital procedure by having someone else witness the “wasted” medication.
Right Dose
The unit-dose system is designed to minimize errors. When preparing a medication from a larger volume or strength than needed or when the prescriber orders a system of measurement different from that which the pharmacy supplies, the chance of error increases. When performing medication calculations or conversions, have another qualified nurse check the calculated doses. After calculating doses, prepare the medication using standard measurement devices. Use graduated cups, syringes, and scaled droppers to measure medications accurately. At home have patients use kitchen measuring spoons rather than household teaspoons and tablespoons, which vary in volume.
Medication errors often occur when pills need to be split. To promote patient safety in inpatient settings, pharmacists split the medications, label and package them, and then send them to the nurse for administration. Because pill splitting is particularly problematic in the home care setting, the Institute for Safe Medication Practices (ISMP) (2006) developed suggestions to help with this process. Determine if the patient has the motor dexterity or visual acuity to split tablets. If at all possible, prescribers need to avoid ordering medications that require splitting.
Tablets are sometimes crushed and mixed with food. Be sure to completely clean a crushing device before crushing the tablet. Remnants of previously crushed medications increase the concentration of a medication or result in the patient receiving a portion of a medication that was not prescribed. Mix crushed medications with very small amounts of food or liquid (e.g., a single tablespoon). Do not use the patient’s favorite foods or liquids because medications alter their taste and decrease the patient’s desire for them. This is especially a concern for pediatric patients.
Not all medications are suitable for crushing. Some medications (e.g., extended-release capsules) have special coatings to prevent them from being absorbed too quickly. These medications should not be crushed. Refer to the “Do Not Crush List” (ISMP, 2010d, http://www.ismp.org/Tools/DoNotCrush.pdf) to ensure that a medication is safe to crush.
Right Patient
Medication errors often occur because one patient gets a drug intended for another patient. Therefore an important step in safe medication administration is being sure that you give the right medication to the right patient. It is difficult to remember every patient’s name and face. Before administering a medication, use at least two patient identifiers (TJC, 2010). Acceptable patient identifiers include the patient’s name, an identification number assigned by a health care agency, or a telephone number. Do not use the patient’s room number as an identifier. To identify a patient correctly in an acute care setting, compare the patient identifiers on the MAR with the patient’s identification bracelet while at the patient’s bedside. If an identification bracelet becomes smudged or illegible or is missing, obtain a new one. In health care settings that are not acute care settings, TJC (2008) does not require the use of armbands for identification. However, nurses still need to use a system that verifies the patient’s identification with at least two identifiers before administering medications.
Patients do not need to state their names and other identifiers when administering medications. Collect patient identifiers reliably when the patient is admitted to a health care setting. Once the identifiers are assigned to the patient (e.g., putting identifiers on an armband and placing the armband on the patient), the nurse uses the identifiers to match the patient with the MAR, which lists the correct medications. Asking patients to state their full names and identification information provides a third way to verify that the nurse is giving medications to the right patient.
In addition to using two identifiers, some agencies use a wireless bar-code scanner to help identify the right patient (Fig. 31-8). This system requires the nurse to scan a personal bar code that is commonly placed on the nurse’s name tag first. Then he or she scans a bar code on the single-dose medication package. Finally the nurse scans the patient’s armband. All this information is then stored in a computer for documentation purposes. This system helps eliminate medication errors because it provides another step to ensure that the right patient receives the right medication.
Right Route
Always consult the prescriber if an order does not designate a route of administration. Likewise, if the specified route is not the recommended route, alert the prescriber immediately. Recent evidence shows that medication errors involving the wrong route are common. For example, enteral and parenteral medications are at risk for confusion in the pediatric population because liquid medications are frequently given orally. When oral medications are prepared in parenteral syringes, there is a high risk for giving an oral medication through the parenteral route (ISMP, 2010c; Paparella, 2008). The injection of a liquid designed for oral use produces local complications such as sterile abscess or fatal systemic effects. Prepare injections from preparations designed for parenteral use only. Medication companies label parenteral medications “for injectable use only.” Label the syringe after preparing the medication and always use different syringes for enteral and parenteral medication administration (ISMP, 2010c). The enteral syringes are often a different color than the parenteral syringes and are clearly labeled for oral or enteral use. The syringe tips of enteral syringes are incompatible with parenteral medication administration systems. Needles do not attach to the syringes, and the syringes cannot be inserted into any type of IV line. In addition, be sure to remove any caps from the tip of an oral syringe before administering the medication. Failure to remove the cap can result in the patient aspirating it, thus blocking his or her trachea (Guenter, 2010; Paparella, 2008).
Right Time
In addition, you need to know why a medication is ordered for certain times of the day and whether you are able to alter the time schedule. For example, two medications are ordered, one q8h (every 8 hours) and the other 3 times a day. Both medications are scheduled for 3 times within a 24-hour period. The prescriber intends the q8h medication to be given around-the-clock to maintain therapeutic blood levels of the medication. In contrast, the nurse needs to give the 3-times-a-day medication during the waking hours. Each agency has a recommended time schedule for medications ordered at frequent intervals. You can alter these recommended times if necessary or appropriate.
The prescriber often gives specific instructions about when to administer a medication. A preoperative medication to be given “on call” means that the nurse gives the medication when the operating room staff members notify him or her that they are coming to get the patient for surgery. Give a medication ordered PC (after meals) within half an hour after a meal, when the patient has a full stomach. Give a STAT medication immediately.
Give priority to time-critical medications that must act and therefore be given at certain times. Hospitals designate which medications are time-critical and which are non–time-critical (CMS, 2011; ISMP, 2011). You administer time-critical medications within 30 minutes before or after their scheduled time. For example, give insulin (a time-critical medication) at a precise interval before a meal. Give antibiotics 30 minutes before or after they are scheduled, around-the-clock to maintain therapeutic blood levels. Give all routinely ordered non–time-critical medications within 1 to 2 hours before or after the scheduled time or per agency policy (CMS, 2011; ISMP, 2011).
Some medications require the nurse’s clinical judgment in deciding the proper time for administration. Administer a prn sleeping medication when the patient is prepared for bed. In addition, use judgment when administering prn analgesics. For example, the nurse sometimes needs to obtain a STAT order from the prescriber if the patient requires a medication before the prn interval has elapsed. Nurses always document whenever they call the patient’s health care provider to obtain a change in a medication order.
Before discharge from the hospital setting, evaluate a patient’s need for home care, especially if he or she was admitted to the hospital because of a problem with medication self-administration. Patients often leave the hospital with a basic knowledge of their medications but are unable to remember or implement this knowledge once back home. Before patients are discharged from the hospital, evaluate whether the medications are adequate or prescribed at therapeutic levels for them.
At home some patients take several medications throughout the day. Help to plan schedules based on preferred medication intervals, the pharmacokinetics of the medications, and the patient’s daily schedule. For patients who have difficulty remembering when to take medications, make a chart that lists the times to take each medication or prepare a special container to hold each timed dose.
Right Documentation
Nurses and other health care providers use accurate documentation to communicate with one another. Many medication errors result from inaccurate documentation. Therefore always document medications accurately at the time of administration and verify any inaccurate documentation before giving medications.
Before administering a medication, ensure that the MAR clearly reflects the patient’s full name; the name of the ordered medication written out in full (no medication name abbreviations); the time the medication is to be administered; and the dosage, route, and frequency. Common problems with medication orders include incomplete information; inaccurate dosage form or strength; illegible order or signature; incorrect placement of decimals, leading to the wrong dosage; and nonstandard terminology. If there is any question about a medication order because it is incomplete, illegible, vague, or not understood, contact the prescribing health care provider before administering the medication. The prescribing health care provider is responsible to provide accurate, complete, and understandable medication orders. If health care providers are unable to do this, nurses implement agency policy (usually a “chain of command” policy) to determine who to contact until they resolve issues related to patients’ medications. You are responsible to begin this chain of command to ensure that patients receive the correct medication. You are also responsible for documenting any preassessment data required of certain medications such as a blood pressure measurement for antihypertensive medications or laboratory values, as in the case of phenytoin, before giving the drug.
After administering a medication, indicate which medication was given on the patient’s MAR per agency policy to verify that it was given as ordered. Record each medication on the patient’s MAR as soon as you give medications to a patient. Inaccurate documentation such as failing to document giving a medication or documenting an incorrect dose leads to errors in subsequent decisions about patient care. For example, errors in documentation about insulin often result in negative patient outcomes. Consider the following situation: a patient receives insulin before breakfast, but the nurse who gave the insulin forgot to document it. The nurse caring for the patient goes home, and the patient has a new nurse for the day. The new nurse notices that the insulin is not documented and assumes that the previous nurse did not give the insulin. Therefore the new nurse gives the patient another dose of insulin. Approximately 2 hours later, the patient experiences a low blood glucose level, which causes him or her to have seizures. Accurate documentation would have prevented this situation from happening.
Never document that you have given a medication until you have actually given it. The name of the medication, the dose, the time of administration, and the route all need to be documented on the MAR. Also document the site of any injections and the patient’s responses to medications, either positive or negative. Nurses notify the patient’s health care provider of any negative responses to medications and document the time, date, and name of the health care provider that was notified in the patient’s medical record. The efforts you make in ensuring proper documentation help provide safe care (Box 31-7).
Maintaining Patients’ Rights
In accordance with The Patient Care Partnership (American Hospital Association, 2003) and because of the potential risks related to medication administration, a patient has the following rights:
• To be informed of the name, purpose, action, and potential undesired effects of a medication
• To refuse a medication regardless of the consequences
• To have qualified nurses or physicians assess a medication history, including allergies and use of herbals
• To be properly advised of the experimental nature of medication therapy and give written consent for its use
• To receive labeled medications safely without discomfort in accordance with the six rights of medication administration
• To receive appropriate supportive therapy in relation to medication therapy
• To not receive unnecessary medications
• To be informed if medications are a part of a research study
Know these rights and handle all inquiries by patients and families courteously and professionally. Do not become defensive if a patient refuses medication therapy, recognizing that every person of consenting age has a right to refusal.
Nursing Process
Apply the nursing process and use a critical thinking approach in your care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care.
Assessment
During the assessment process, thoroughly assess each patient and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care.
Through the Patient’s Eyes
Use professional knowledge, skills, and attitudes to provide compassionate and coordinated care. This requires you to take the patient’s preferences, values, and needs into consideration while determining his or her need for and potential response to medication therapy. Assess patients’ experiences and encourage them to express their beliefs, feelings, and concerns about their medications. Putting patients in the center of their care helps you to see the situation through their eyes and contributes to safe medication administration. Begin your assessment by asking a variety of questions that help you better understand your patients’ current medication management routine, the ability to afford medications, and beliefs and expectations about medications (Box 31-8).
History
Before administering medications, obtain or review the patient’s medical history. A patient’s medical history provides indications or contraindications for medication therapy. Disease or illness places patients at risk for adverse medication effects. For example, if a patient has a gastric ulcer, medications containing aspirin increase the likelihood of bleeding. Long-term health problems (e.g., diabetes or arthritis) require specific medications. This knowledge helps the nurse anticipate the type of medications that a patient requires. A patient’s surgical history indicates use of medications. For example, after a thyroidectomy a patient requires thyroid hormone replacement.
Allergies: Inform the other members of the health care team if the patient has a history of allergies to medications and foods. Many medications have ingredients also found in food sources. For example, propofol (Diprivan), which is used for anesthesia and sedation, includes egg lecithin and soybean oil as inactive ingredients. Therefore patients who have an egg or soy allergy should not receive propofol (Skidmore-Roth, 2011). In some health care settings patients wear identification bands listing medication and food allergies. Ensuring that all allergies and the patient’s reactions are noted on the patient’s admission notes, medication records, and history and physical examination facilitates communication of this essential information to members of the health care team.
Medications: Assess information about each medication that the patient takes, including length of time the medication has been taken, the current dosage, and whether or not the patient experiences side effects or has had adverse effects from the medication. In addition, review the action, purpose, normal dosage, routes, side effects, and nursing implications for administering and monitoring each medication. Often you need to consult several resources to gather necessary information. Pharmacology textbooks and handbooks; electronic medication manuals available on a computer, handheld computer, or AMDS; nursing journals; the Physician’s Desk Reference (PDR); medication package inserts; and pharmacists are valuable resources. Nurses are responsible for knowing as much as possible about each medication given.
Diet History: A diet history reveals a patient’s normal eating patterns and food preferences. An effective dosage schedule is planned around them. Teach the patient to avoid foods that interact with medications. In addition, some medications are more effective when taken with meals; teach patients about specific medications that must be taken with food.
Patient’s Perceptual or Coordination Problems: A patient with perceptual fine-motor or coordination limitations has difficulty self-administering medication. For example, a patient who takes insulin to manage blood glucose and has arthritis has difficulty manipulating a syringe. Assess the patient’s ability to prepare doses and take medications correctly. If the patient is unable to self-administer medications, assess if family or friends are available to assist or make a home care referral.
Patient’s Current Condition
The ongoing physical or mental status of a patient affects whether a medication is given or how it is administered. Assess a patient carefully before giving any medication. For example, check the patient’s blood pressure before giving an antihypertensive. A patient who is nauseated is probably unable to swallow a tablet. Notify the patient’s health care provider if he or she is unable to take a medication. Assessment findings serve as a baseline in evaluating the effects of medication therapy.
Patient’s Attitude About Medication Use
The patient’s attitude about medications sometimes reveals a level of medication dependence or drug avoidance. Some patients do not express their feelings about taking a particular medication, particularly if dependence is a problem. Observe the patient’s behavior for evidence of dependence or avoidance. Also be aware that his or her cultural beliefs about Western medicine sometimes interfere with medication compliance (Box 31-9; see Chapter 9).
Patient’s Understanding of and Adherence to Medication Therapy
The patient’s knowledge and understanding of medication therapy influence the willingness or ability to follow a medication regimen. If the patient has a history of poor adherence (e.g., frequently missed doses or failure to fill prescriptions), investigate if he or she can afford prescribed medications and review resources available for purchase of medications if indicated. Also determine if the patient understands the purpose of the medication, the importance of regular dosage schedules, proper administration methods, and the possible side effects. Without adequate knowledge and motivation, adherence to medication schedules is unlikely.
Patient’s Learning Needs
Health-related information is difficult to understand because of the use of technical terminology. Serious errors can occur when patients do not understand information about their medications. Assess patients’ health literacy regarding medication administration to determine their need for instruction (Cornett, 2009) (see Chapter 25). Consider patient responses to assessment questions that you ask about medications such as those listed in Box 31-8. When a patient is unable to answer questions about medications appropriately, assess him or her for challenges in health literacy.
Nursing Diagnosis
Assessment provides data about the patient’s condition, ability to self-administer medications, and medication adherence, which determine actual or potential problems with medication therapy. Certain data are defining characteristics that, when clustered together, reveal nursing diagnoses. For example, ineffective self-health management related to complexity of medical regimen is indicated when patients do not respond as expected to their medications and admit to having difficulty in managing them. This list of nursing diagnoses may apply to patients during the administration of medications:
• Ineffective health maintenance
• Readiness for enhanced immunization status
• Deficient knowledge (medications)
After selecting the diagnosis, identify the related factor, which drives the selection of nursing interventions. In the example of ineffective self-health management, the related factor of inadequate resources versus lack of knowledge requires different interventions. If the patient’s nursing diagnosis is related to inadequate finances, collaborate with family members, social workers, or community agencies to help him or her receive necessary medications. If the related factor is lack of knowledge, implement a teaching plan with appropriate follow-up.
Planning
Always organize your care activities to ensure the safe administration of medications. Hurrying to give patients medications leads to errors. It is important to minimize distractions or interruptions when preparing and administering medications (Brady, Malone, and Fleming, 2009).
Goals and Outcomes
Setting goals and related outcomes contributes to patient safety and allows for wise use of time during medication administration. For example, the nurse establishes the following goal and related outcomes for a patient with newly diagnosed type 2 diabetes:
Goal: The patient will safely administer all ordered medications before discharge.
• The patient will verbalize understanding of desired and adverse effects of medications.
• The patient will state signs, symptoms, and treatment of hypoglycemia.
• The patient will be able to monitor blood glucose levels to determine if medication is appropriate to take or if a low blood glucose level should be treated.
• The patient will establish a daily routine that will coordinate timing of medication with mealtimes.
Setting Priorities
Prioritize care when administering medications. Use information gathered from the patient’s assessment in determining which medications to give first and if it is appropriate to administer prn medications. For example, if a patient is in pain, it is important to provide pain medication as soon as possible. If the patient’s blood pressure is elevated, administer the blood pressure medications before other medications. Nurses also prioritize when providing patient education about medications. Provide the most important information about the medications first. For example, hypoglycemia is a serious side effect of insulin. The patient taking insulin needs to be able to identify and treat hypoglycemia immediately; thus first teach him or her about the recognition and treatment of hypoglycemia before teaching about how to administer the injection.
Teamwork and Collaboration
Collaborate with a variety of health care providers when administering medications. First it is important to collaborate with the patient’s family or friends whenever possible. Family members often reinforce the importance of medication regimens in the home setting. Nurses often collaborate with the prescriber, the pharmacist, and case managers to ensure that patients are able to afford their medications. On discharge ensure that patients know where and how to obtain medications. Be sure that patients are able to read medication labels and printed medication teaching sheets. Some patients also need to understand how to calculate dosages and prepare complex medication regimens. Collaborate with community resources (e.g., agency on aging, public health department, medical interpreters) when patients are illiterate or have difficulty understanding medication instructions (see Chapter 25).
Implementation
In promoting or maintaining a patient’s health, the nurse identifies factors that improve or diminish well-being. Health beliefs, personal motivations, socioeconomic factors, and habits (e.g., excessive alcohol intake) influence the patient’s adherence with medications. Several nursing interventions promote adherence to the medication regimen and foster independence. Teach the patient and family about the benefit of a medication and the knowledge needed to take it correctly and integrate the patient’s health beliefs and cultural practices into the treatment plan. Help the patient and family establish a medication routine that fits into the patient’s normal schedule. Make referrals to community resources if the patient is unable to afford or cannot arrange transportation to obtain necessary medications.
Patient and Family Teaching: Patients may take medications incorrectly or not at all unless they are properly informed about them. Follow principles of patient education (see Chapter 25). Provide information about the purpose of medications and their actions and effects in a way that patients can understand. Many health care agencies offer easy-to-read teaching sheets about specific types of medications. Patients need to know how to take medications properly and the risks associated with failing to do so. For example, after receiving a prescription for an antibiotic, a patient needs to understand the importance of taking the full prescription. Failure to do this can lead to a worsening of the condition and the development of bacteria resistant to the medication.
Nurses teach patients how to correctly administer their medications. For example, teach a patient how to accurately measure a liquid medication. Provide special education to patients who depend on daily injections (Box 31-10). The patient learns to prepare and administer an injection correctly using aseptic technique. Teach family members or friends how to give injections in case the patient becomes ill or physically unable to handle a syringe. Provide specially designed equipment such as syringes with enlarged calibrated scales or medications with labels in Braille when patients have visual alterations.
Patients need to know the symptoms of medication side effects or toxicity. For example, patients taking anticoagulants learn to notify their health care providers immediately when signs of bleeding or bruising develop. Inform family members or friends of medication side effects such as changes in behavior because they are often the first persons to recognize such effects. Patients cope better with problems caused by medications if they understand how and when to act. All patients need to learn the basic guidelines for medication safety, which ensure the proper use and storage of medications in the home.
Acute Care
Patients are often hospitalized to receive expert nursing observation and documentation of responses to medications. When a nurse receives a medication order, several nursing interventions are essential for safe and effective medication administration.
Receiving, Transcribing, and Communicating Medication Orders: An order is required to administer any medication. Many health care agencies use CPOE. In these systems health care providers directly enter orders for their patients into the computer. Current evidence shows that CPOE helps to reduce medication errors and mortality rates (Longhurst et al., 2010). In the absence of CPOE, the health care provider handwrites orders onto an order sheet in the patient’s chart. If orders are handwritten, be sure that medication names, dosages, and symbols are legible. Rewrite any unclear or illegible transcribed orders.
The process of verifying medical orders varies among health care agencies. Nurses follow agency policy and current national patient safety standards when receiving, transcribing, and communicating medication orders. Nursing students are prohibited from receiving verbal and telephone orders.
Medication orders need to contain all of the elements in Box 31-11. If the medication order is incomplete, inform the prescriber and ensure completeness before carrying it out. Nurses read back verbal or telephone orders to the prescriber to ensure that the correct order is obtained. The registered nurse follows institutional policy regarding receiving, recording, and transcribing verbal and telephone orders. Generally the prescriber must sign them within 24 hours.
Nurses and pharmacists check all medication orders for accuracy and thoroughness several times during the transcription process. They also take patients’ current problems, treatments, laboratory values, and other prescribed medications into consideration to determine if the ordered medication is safe and appropriate. Once the nurse and pharmacist determine that a medication order is safe and appropriate, it is placed on the appropriate medication form, usually called the MAR. The MAR is either printed out on paper or is available electronically. An electronic version of the MAR is called an eMAR. Whether it is handwritten, printed out from a computer, or in an electronic version, it includes the patient’s name, room, and bed number, medical record number, medical and food allergies, other patient identifiers (e.g., birth date); and medication name, dose, frequency, and route and time of administration. Each time a medication dose is prepared, the nurse refers to the MAR.
It is essential to verify the accuracy of every medication you give to your patients with the patients’ orders. If the medication order is incomplete, incorrect, or inappropriate or if there is a discrepancy between the original order and the information on the MAR, consult with the prescriber. Do not give the medication until you are certain that you can follow the six rights of medication administration. When you give the wrong medication or an incorrect dose, you are legally responsible for the error.
Accurate Dose Calculation and Measurement: When measuring liquid medications, use standard measuring containers. The procedure for medication measurement is systematic to lessen the chance of error. Calculate each dose when preparing the medication, pay close attention to the process of calculation, and avoid interruptions from other people or nursing activities. Ask another nurse to double-check your calculations against the original medication order if you are ever in doubt about the accuracy of your calculation or if you are calculating a new or unusual dose.
Correct Administration: For safe administration follow the six rights of medication administration. Verify the patient’s identity by using at least two patient identifiers (TJC, 2011a). In the acute care setting identifiers are usually on a patient’s armband. Carefully compare the patient identifiers with the MAR to ensure that you are giving the medication to the right patient. When they are able, you can also ask patients to state their name as a third identifier. Use aseptic technique and proper procedures when handling and giving medications and perform necessary assessments (e.g., assess heart rate before giving antidysrhythmic medications) before administering a medication to a patient. Carefully monitor the patient’s response to the medication, especially when he or she receives the first dose of a new medication.
Recording Medication Administration: Follow all agency policies when documenting medication administration. After administering a medication, record the name of the medication, dose, route, and exact time of administration immediately on the appropriate record form. Include the site of any injections per agency policy.
If a patient refuses a medication or is undergoing tests or procedures that result in a missed dose, explain the reason that the medication was not given in the nurses’ notes. Some agencies require the nurse to circle the prescribed administration time on the medication record or to notify the health care provider when a patient misses a dose. Be aware of the effects that missing doses have on a patient (e.g., with hypertension or diabetes). Coordinating care with health care providers and other services when testing or diagnostic procedures are being completed helps to ensure patient safety and therapeutic control of the disease.
Restorative Care
Because of the numerous types of restorative care settings, medication administration activities vary. Patients with functional limitations often require a nurse to fully administer all medications. In the home care setting patients usually administer their own medications or receive assistance from family caregivers. Regardless of the type of medication activity, the nurse remains responsible for instructing patients and families in medication action, administration, and side effects. The nurse is also responsible for monitoring compliance with medication and determining the effectiveness of medications that have been prescribed.
Special Considerations for Administering Medications to Specific Age-Groups
A patient’s developmental level is a factor for nurses to consider when administering medications. Knowledge of developmental needs helps you anticipate responses to medication therapy.
Infants and Children: Children vary in age; weight; surface area; and the ability to absorb, metabolize, and excrete medications. Children’s doses are lower than those of adults; thus special caution is necessary when preparing medications for them. Medications are usually not prepared and packaged in standardized dose ranges for children. Preparing an ordered dose from an available amount requires careful calculation. In many pediatric settings the standard of practice is to have another nurse verify all pediatric dose calculations prior to administration.
All children require special psychological preparation before receiving medications. The child’s parents are often valuable resources for determining the best way to give the child medication. Sometimes it is less traumatic for the child if a parent gives the medication and the nurse supervises. Supportive care is necessary if a child is expected to cooperate. Explain the procedure to a child, using words appropriate to his or her level of comprehension. Long explanations increase a child’s anxiety, especially for painful procedures such as an injection. Involving the child in choices when possible usually results in greater success. For example, saying “It’s time to take your tablet now. Do you want it with water or juice?” allows a child to make a choice. Do not give the child the option of not taking a medication. After giving a medication, praise him or her and even offer a simple reward such as a star or token. Tips for administering medication to children are in Box 31-12.
Older Adults: Older adults also require special consideration during medication administration (Box 31-13). In addition to physiological changes of aging (Fig. 31-9), behavioral and economic factors influence an older person’s use of medications.
Polypharmacy: Polypharmacy happens when a patient takes two or more medications to treat the same illness, takes two or more medications from the same chemical class, uses two or more medications with the same or similar actions to treat several disorders simultaneously, or mixes nutritional supplements or herbal products with medications (Ebersole et al., 2008; Maggiore, Gross, and Hurria, 2010). Older adults also often experience polypharmacy when they seek relief from a variety of symptoms (e.g., pain, constipation, insomnia, and indigestion) by using OTC preparations. Sometimes polypharmacy is unavoidable. For example, some patients need to take more than one medication to control their high blood pressure. When the patient experiences polypharmacy, the risk of adverse reactions and medication interactions with other medications and food is increased.
Because many older adults suffer chronic health problems, polypharmacy is common. However, it is also becoming more common in children and patients with mental illnesses. Taking OTC medications frequently, lack of knowledge about medications, incorrect beliefs about medications, and visiting several health care providers to treat different illnesses increase the risk for polypharmacy. To minimize risks associated with polypharmacy, frequent communication among health care providers is essential to make sure that the patients’ medication regimen is as simple as possible.
Evaluation: Evaluation of medication administration is an essential role of professional nursing that requires assessment skills; critical thinking; analysis; and knowledge of medications, physiology, and pathophysiology. Nurses thoroughly and accurately gather data and complete a holistic evaluation of their patients. The goal of safe and effective medication administration involves the patient’s response to therapy and ability to assume responsibility for self-care. When patients do not experience expected outcomes of medication therapy, investigate possible reasons and determine appropriate revisions to the patient’s plan of care.
Through the Patient’s Eyes
Evaluation is more effective when you value your patients’ participation. Therefore partner with your patients and include them in the evaluation process. Ensure that they understand and are able to safely administer their medications. For example, if you are caring for a child who needs an inhaler, be sure to watch the patient use the inhaler. To determine if patients understand their medication schedules, ask them to explain when they take their medications and if they are able to take them as prescribed. When patients struggle with their medication schedule, determine barriers to medication adherence (e.g., cost, lack of knowledge) and remove these barriers if possible. Also remember that patients have different values and define health differently. These values and beliefs influence their perception of the effectiveness of their medications. Therefore ask patients to describe this effectiveness. Ask if they are satisfied with their medications and how they make them feel. Use patients’ statements and responses to questions (e.g., “I feel less anxious now”) when determining the effectiveness of medications. Including patients in the evaluation process empowers them and helps them become more actively involved in their care.
Patient Outcomes
A patient’s clinical condition can change minute by minute. Use knowledge of the desired effect and common side effects of each medication to compare expected outcomes with actual findings. A change in a patient’s condition is often physiologically related to health status or results from medications or both. Be alert for reactions in a patient taking several medications. Nurses use a variety of measures to evaluate patient responses to medications such as direct observation of physiological measures (e.g., blood pressure or laboratory values), behavioral responses (e.g., agitation), and rating scales (e.g., rating on a pain scale). The type of measurement used varies with the action being evaluated, the reading skill and knowledge level of the patient, and the patient’s cognitive and psychomotor ability. The most common type of measurement that the nurse uses is a physiological measure. Examples of physiological measures are blood pressure, heart rate, and visual acuity. Nurses also use patient statements as evaluative measures. Table 31-8 contains examples of goals, expected outcomes, and corresponding evaluative measures.