CHAPTER 12 Diagnosis and Treatment Planning
Purpose and Uniqueness of Treatment
The purpose of dental treatment is to respond to a patient’s needs, both the needs perceived by the patient and those demonstrated through a clinical examination and patient interview. Although similarities have been noted between partially edentulous patients (such as Classification designations), significant differences exist, making each patient, and the ultimate treatment, unique.
The delineation of each patient’s uniqueness occurs through the patient interview and diagnostic clinical examination process. This includes four distinct processes: (1) understanding the patient’s desires or chief concerns/complaints regarding his or her condition (including its history) through a systematic interview process, (2) ascertaining the patient’s dental needs through a diagnostic clinical examination, (3) developing a treatment plan that reflects the best management of desires and needs (with influences unique to the medical condition or oral environment), and (4) executing appropriately sequenced treatment with planned follow-up. The ultimate treatment is individualized to address disease management and the coordinated restorative and prosthetic needs that are unique to the patient. Provision of the best care for a patient may involve no treatment, limited treatment, or extensive treatment, and the dentist must be prepared to help patients decide the best treatment option given his or her individual circumstances.
Patient Interview
Although oral health is an important aspect of overall health, it is an elective health pursuit for most individuals. Consequently, the patient presents for professional evaluation (1) to address some perception of an abnormality that requires correction, or (2) to maintain optimum oral health. In either situation, but especially for the patient presenting with some chief complaint (often with an important history related to that complaint), it is mandatory that the dentist clearly understand what brings the patient to this evaluation. Failure to do so leads to the chance that the patient will be unhappy with the treatment result, as it might not address the very reason he or she came for help. With experience, this subtle point becomes a major component of a clinician’s management focus.
A fundamental objective of the patient interview, which accompanies the diagnostic examination, is to gain a clear understanding of why the patient is presenting for evaluation; this involves having the patient describe the history related to the chief complaint. For complicated clinical problems, the interview and diagnostic examination require two appointments to allow complete gathering of all diagnostic information needed to formulate a complete plan of treatment.
The interview, an opportunity to develop rapport with the patient, involves listening to and understanding the patient’s chief complaint or concern about his or her oral health. This can include clinical symptoms of pain (provoked or unprovoked), difficulty with function, concern about appearance, problems with an existing prosthesis, or any combination of symptoms related to the teeth, periodontium, jaws, or previous dental treatment. It is important to listen carefully to what the patient has stated is the reason for presenting for evaluation; this is because all subsequent information gathered will be used to discuss these concerns and to relate whether the proposed treatment will affect the patient in any way. Such a discussion at the outset of patient care helps to outline realistic expectations.
Although formats for sequencing the patient interview (and clinical examination) vary, to ensure thoroughness the dentist should follow a sequence that includes:
It is from the above interaction that patient uniqueness, as mentioned earlier, is best defined. The expectations described by the patient are critical to an understanding of whether a removable partial denture will satisfy the stated treatment goal(s). The fact that removable partial dentures by necessity require material bulk and often use oral soft tissues for support may be hard to comprehend by patients with no such prosthetic history. Helping the patient understand the normal phase of accommodation to such a prosthesis is an important discussion point in selection of a prosthesis. For those patients with a negative past prosthesis experience, it is necessary to determine before treatment is started whether the design, fit, occlusion, or lack of maintenance of the prosthesis can be improved to provide a more positive experience.
Shared Decision Making
When helping patients understand their oral health status, comprising both disease and deficit considerations, and the means to address both, we should carefully consider what it is they need to hear from us. For most partially edentulous patients, the discussion may involve fairly complex rehabilitation options for addressing their missing teeth. Because of this complexity, our responsibility is to help them sort through the options in an attempt to help them come to the best decision for them. Using a communication model termed shared decision making gives structure to a process where the provider and the patient identify together the best course of care. This process recognizes that there may be complex “trade-offs” in care choice, and it addresses the need to fully inform patients about risks and benefits of care options, as well as ensuring that patient values and preferences play a prominent role in the process. Although it is clear that not all patients desire to participate equally in care decisions, because the options can vary significantly (some are more invasive, have greater risks, are accompanied by higher treatment burden than others; there are often varying maintenance needs between options), we should actively engage them in the process. This is more important given the fact that the tooth replacement is often an elective pursuit, and because of this, there is seldom great urgency involved in making a decision.
Clinical Examination
Objectives of Prosthodontic Treatment
The objectives of any prosthodontic treatment may be stated as follows: (1) the elimination of disease; (2) the preservation, restoration, and maintenance of the health of the remaining teeth and oral tissues (which will enhance the removable partial denture design); and (3) the selected replacement of lost teeth; for the purpose of (4) restoration of function in a manner that ensures optimum stability and comfort in an esthetically pleasing manner. Preservation is a principle that protects from decisions that place too high a premium on cosmetic concerns, and it is the dentist’s obligation to emphasize the importance of restoring the total mouth to a state of health and of preserving the remaining teeth and surrounding tissues.
Diagnosis and treatment planning for oral rehabilitation of partially edentulous mouths must take into consideration the following: control of caries and periodontal disease, restoration of individual teeth, provision of harmonious occlusal relationships, and the replacement of missing teeth by fixed (using natural teeth and/or implants) or removable prostheses. Because these procedures are integrally related, the appropriate selection and sequencing of treatment should precede all irreversible procedures.
The treatment plan for the removable partial denture, which is often the final step in a lengthy sequence of treatment, should precede all but emergency treatment. This allows abutment teeth and other areas in the mouth to be properly prepared to support, stabilize, and retain the removable partial denture. This means that diagnostic casts, for designing and planning removable partial denture treatment, must be made before definitive treatment is undertaken. After the major factors that create functional forces are evaluated and those that resist it are understood, the removable partial denture design is drawn on the diagnostic cast, along with a detailed chart of mouth conditions and proposed treatment. This becomes the master plan for the mouth preparations and the design of the removable partial denture to follow.
As was pointed out in Chapter 1, failure of removable partial dentures can usually be attributed to factors that result in poor stability. These can result from inadequate diagnosis and failure to properly evaluate the conditions present. This results in failure to prepare the patient and the oral tissues properly before the master cast is fabricated. The importance of the examination, the consideration of favorable and unfavorable aspects relative to movement control, and the importance of planning the elimination of unfavorable influences cannot be overemphasized (see Chapter 2).
As was mentioned earlier, for complex treatment, two appointments are often required. The first will likely include a preliminary oral examination (to determine the need for management of acute needs), a prophylaxis, full-mouth radiographs, diagnostic casts, and mounting records if baseplates are not required. The follow-up appointment includes mounting of the diagnostic casts (when baseplates and occlusion rims are needed), a definitive oral examination, review of the radiographs to augment and correlate with clinical findings, and arrangement of additional consultations when required. Following collection and synthesis of all patient and clinical information, including surveying of the casts, a treatment plan (often with options) is presented.
Oral Examination
A complete oral examination should precede any treatment decisions. It should include visual and digital examination of the teeth and surrounding tissues with a mouth mirror, explorer, and periodontal probe, vitality tests of critical teeth, and examination of casts correctly oriented on a suitable articulator. Clinical findings are augmented by and correlated with a complete intraoral radiographic survey.
During the examination, the objective to be kept foremost in mind should be the consideration of possibilities for restoring and maintaining the remaining oral structures in a state of health for the longest period of time. This is best accomplished by an evaluation of factors that generate functional forces and those that resist them. The stability of tooth and prosthesis position is the goal of such an evaluation. The following sequence of examination allows attention to be paid to aspects of each of these critical features of evaluation for removable partial denture service.
Sequence for Oral Examination
An oral examination should be accomplished in the following sequence: visual examination, pain relief and temporary restorations, radiographs, oral prophylaxis, evaluation of teeth and periodontium, vitality tests of individual teeth, determination of the floor of the mouth position, and impressions of each arch.
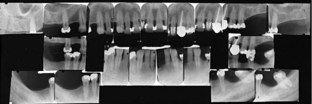
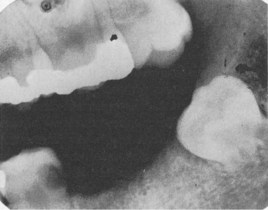
Figure 12-1 Complete intraoral radiographic survey of remaining teeth and adjacent edentulous areas reveals much information vital to effective diagnosis and treatment planning. The response of bone to previous stress is of particular value in establishing the prognosis of teeth that are to be used as abutments.
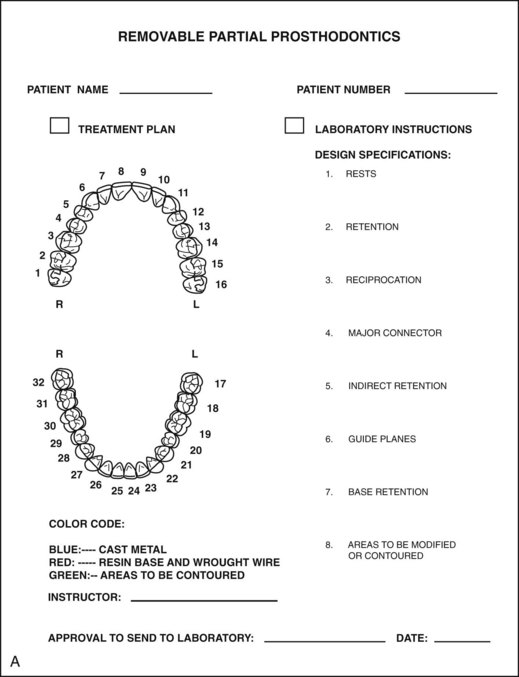
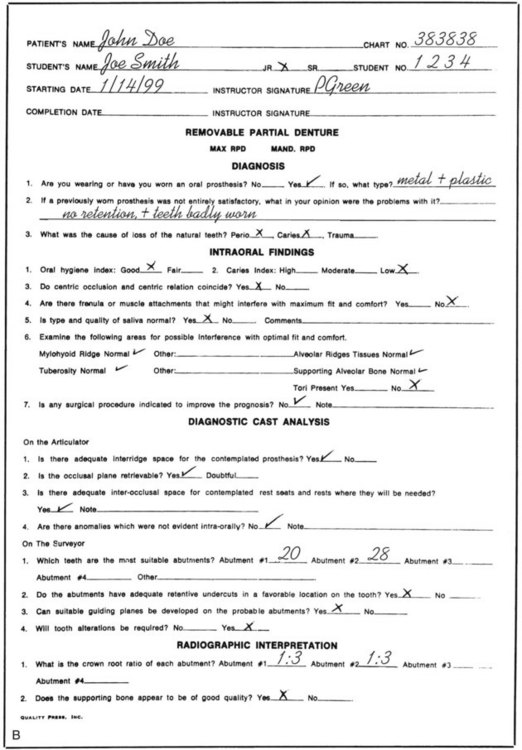
Figure 12-2 A, Diagnosis record for recording pertinent data.B, Treatment record chart for recording treatment plan and treatment progress.
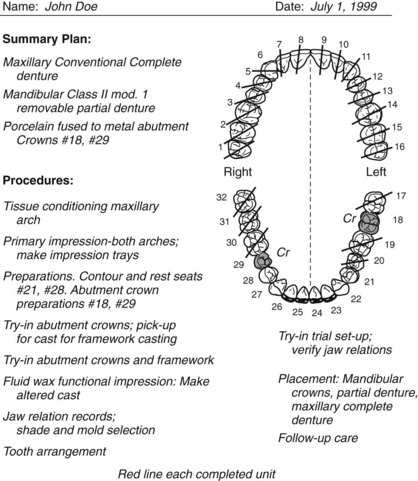
Figure 12-3 Simple working chart. Restorations for individual teeth, crowns, and fixed partial dentures to be made may be marked on the chart and checked off as completed during mouth preparations.
Visual examination will reveal many of the signs of dental disease. Consideration of caries susceptibility is of primary importance. The number of restored teeth present, signs of recurrent caries, and evidence of decalcification should be noted. Only those patients with demonstrated good oral hygiene habits and low caries susceptibility should be considered good risks without resorting to prophylactic measures such as the restoration of abutment teeth. At the time of the initial examination, periodontal disease, gingival inflammation, the degree of gingival recession, and mucogingival relationships should be observed. Such an examination will not provide sufficient information to allow a definitive diagnosis and treatment plan. For this purpose, complete periodontal charting that includes pocket depths, assessment of attachment levels, furcation involvement, mucogingival problems, and tooth mobility should be performed. The extent of periodontal destruction must be determined with appropriate radiographs and use of the periodontal probe.
The number of teeth remaining, the location of the edentulous areas, and the quality of the residual ridge will have a definite bearing on the proportionate amount of support that the removable partial denture will receive from the teeth and edentulous ridges. Tissue contours may appear to present a well-formed edentulous residual ridge; however, palpation often indicates that supporting bone has been resorbed and has been replaced by displaceable, fibrous connective tissue. Such a situation is common in maxillary tuberosity regions. The removable partial denture cannot be supported adequately by tissues that are easily displaced. When the mouth is prepared, this tissue should be recontoured or removed surgically, unless otherwise contraindicated. A small but stable residual ridge is preferable to a larger unstable ridge for providing support for the denture. The presence of tori or other bony exostoses must be detected and their presence in relation to framework design must be evaluated. Failure to palpate the tissue over the median palatal raphe to ascertain the difference in its displaceability as compared with the displaceability of the soft tissues covering the residual ridges can lead to a rocking, unstable, uncomfortable denture and to a dissatisfied patient. Adequate relief of the palatal major connectors must be planned, and the amount of relief required is directly proportionate to the difference in displaceability of the tissues over the midline of the palate and the tissues covering the residual ridges.
During the examination, not only each arch but also its occlusal relationship with the opposing arch must be considered separately. A situation that looks simple when the teeth are apart may be complicated when the teeth are in occlusion. For example, an extreme vertical overlap may complicate the attachment of anterior teeth to a maxillary denture. Extrusion of a tooth or teeth into an opposing edentulous area may complicate the replacement of teeth in the edentulous area or may create occlusal interference, which will complicate the location and design of clasp retainers and occlusal rests. Such findings subsequently will be evaluated further by careful analysis of mounted diagnostic casts.
A breakdown of the fee may be recorded on the back of this chart for easy reference if adjustments or substitutions become necessary because of changes in diagnosis as the work progresses.
The fee for examination, which should include the cost of the radiographic survey and the examination of articulated diagnostic casts, should be established before the examination is performed and should not be related to the cost of treatment. It should be understood that the fee for examination is based on the time involved and the service rendered, and that the material value of the radiograph and diagnostic casts is incidental to the effectiveness of the examination.
The examination record should always be available in the office for future consultation. If consultation with another dentist is requested, respect for the hazards of unnecessary radiation justifies loaning the dentist the radiograph for this purpose. However, duplicate films should be retained in the dentist’s files.
Diagnostic Casts
A diagnostic cast should be an accurate reproduction of all the potential features that aid diagnosis. These include the teeth locations, contours, and occlusal plane relationship; the residual ridge contour, size, and mucosal consistency; and the oral anatomy delineating the prosthesis extensions (vestibules, retromolar pads, pterygomaxillary notch, hard/soft palatal junction, floor of the mouth, and frena). Additional information provided by appropriate cast mounting includes occlusal plane orientation and the impact on the opposing arch; tooth-to-palatal soft tissue relationship; and tooth-to-ridge relationships both vertically and horizontally.
A diagnostic cast is usually made of dental stone because of its strength and the fact that it is less easily abraded than is dental plaster. Generally the improved dental stones (die stones) are not used for diagnostic casts because of their cost. Their greater resistance to abrasion does, however, justify their use for master casts.
The impression for the diagnostic cast is usually made with an irreversible hydrocolloid (alginate) in a stock (perforated or rim lock) impression tray. The size of the arch will determine the size of the tray to be used. The tray should be sufficiently oversized to ensure an optimum thickness of impression material to avoid distortion or tearing on removal from the mouth. The technique for making impressions is covered in more detail in Chapter 15.
Purposes of Diagnostic Casts
Diagnostic casts serve several purposes as an aid to diagnosis and treatment planning. Some of these are as follows:
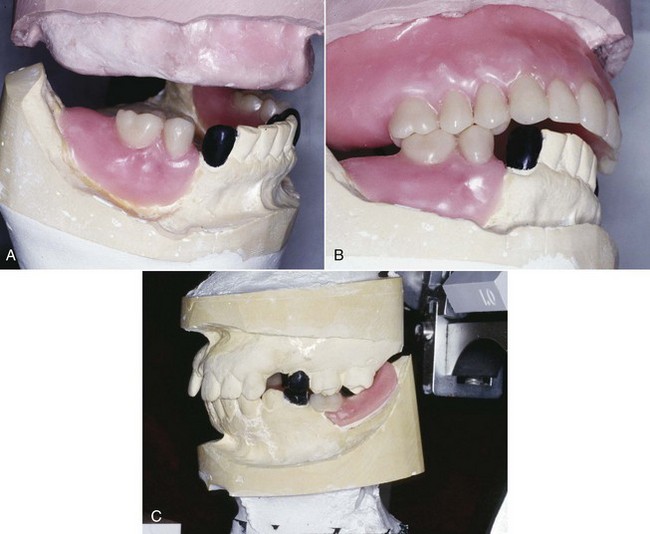
Figure 12-4 A, Following mounting of the diagnostic casts, tooth arrangement for the mandibular occlusal plane requirements can be accomplished. B, Following placement of the maxillary anterior teeth in an ideal position, diagnostic arrangement of occlusion results in a space posterior to surveyed crown #27. If such a finding were objectionable, alternative arrangements could be investigated. This is not possible unless a diagnostic workup is completed. C, Occlusion of the mandibular removable partial denture will be enhanced by improving the maxillary posterior occlusal plane of the super-erupted molars.
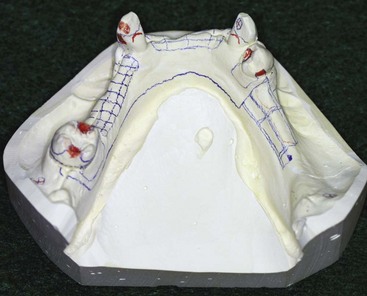
Figure 12-5 Proposed mouth changes and design of the removable partial denture framework are indicated in pencil on the diagnostic cast in relation to the previously determined path of placement. This serves as a means of communicating with the patient and as a chair-side guide to tooth modification.
Mounting Diagnostic Casts
For diagnostic purposes, casts should be related on an anatomically appropriate articulator to best understand the role occlusion may have in the design and functional stability of the removable partial denture. This becomes increasingly important as the prosthesis replaces more teeth. If the patient presents with a harmonious occlusion and the edentulous span is a tooth-bound space, simple hand articulation is generally all that is required. However, when the natural dentition is not harmonious and/or when the replacement teeth must be positioned within the normal movement patterns of the jaws, the diagnostic casts must be related in an anatomically appropriate manner for diagnosis. This means placement of the maxillary cast in a position relative to the opening axis on the articulator, which is similar to the position of the maxilla in relation to the temporomandibular joint of the patient (Figure 12-6). The mandibular cast is then placed beneath the maxillary cast in a horizontal position dictated by mandibular rotation without tooth contact, at a minimal vertical opening.
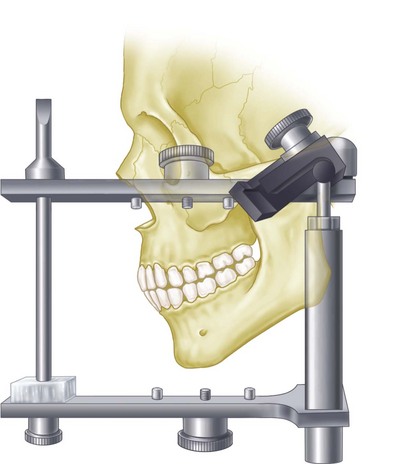
Figure 12-6 Use of the facebow makes possible the recording of the spatial relationship of the maxillae to some anatomic reference points and transference of this relationship to an articulator.
The Glossary of Prosthodontic Terms* describes an articulator as a mechanical device that represents the temporomandibular joints and jaw members, to which maxillary and mandibular casts may be attached. Because the dominant influence on mandibular movement in a partially edentulous mouth is the occlusal plane and the cusps of the remaining teeth, an anatomic reproduction of condylar paths is probably not necessary. Still, movement of the casts in relation to one another as influenced by the occlusal plane and the cusps of the remaining teeth, when mounted at a reasonably accurate distance from the axis of condylar rotation, permits a relatively valid analysis of occlusal relations. This is more anatomically accurate than a simple hinge mounting.
It is better that the casts be mounted in relation to the axis-orbital plane to permit better interpretation of the plane of occlusion in relation to the horizontal plane. Although it is true that an axis-orbital mounting has no functional value on a nonarcon instrument because that plane ceases to exist when opposing casts are separated, the value of such a mounting lies in the orientation of the casts in occlusion. (An arcon articulator is one in which the condyles are attached to the lower member as they are in nature, the term being a derivation coined by Bergström from the words articulation and condyle. Many of the more widely used articulators such as the Hanau H series, Dentatus, and improved Gysi have the condyles attached to the upper member and are therefore nonarcon instruments.)
Sequence for Mounting Maxillary Cast to Axis-Orbital Plane
The initial steps allow recording of the maxilla–temporomandibular joint (TMJ) relationship:
The next steps allow transfer of the recorded relationship to the articulator:
The facebow is a relatively simple device used to obtain a transfer record for orienting a maxillary cast on an articulating instrument. Originally, the facebow was used only to transfer a radius from condyle reference points, so that a given point on the cast would be the same distance from the condyle as it is on the patient. The addition of an adjustable infraorbital pointer to the facebow and the addition of an orbital plane indicator to the articulator make possible the transfer of the elevation of the cast in relation to the axis-orbital plane. This permits the maxillary cast to be correctly oriented in the articulator space comparable with the relationship of the maxilla to the axis-orbital plane on the patient. To accommodate this orientation of the maxillary cast and still have room for the mandibular cast, the posts of the conventional articulator must be lengthened. The older Hanau model H articulator usually will not permit a facebow transfer with an infraorbital pointer.
A facebow may be used to transfer a comparable radius from arbitrary reference points, or it may be designed so that the transfer can be made from hinge axis points. The latter type of transfer requires that a hinge-bow attached to the mandible should be used initially to determine the hinge axis points, to which the facebow is then adjusted for making the hinge axis transfer.
A facebow transfer of the maxillary cast, which is oriented to the axis-orbital plane in a suitable articulator, is an uncomplicated procedure. The Hanau series Wide-Vue 183-2, all 96H2-0 models, the Whip-Mix articulator (Whip-Mix Corp, Louisville, KY), and the Dentatus model ARH (Dentatus USA, New York, NY) will accept this transfer. The Hanau earpiece facebow models 153 and 158, the Hanau fascia facebow 132-2SM, and the Dentatus facebow type AEB incorporate the infraorbital plane to the articulator. None of these are hinge axis bows; they are used instead at an arbitrary point.
The location of the arbitrary point or axis has long been the subject of controversy. Gysi and others have placed it 11 to 13 mm anterior to the upper third of the tragus of the ear on a line extending from the upper margin of the external auditory meatus to the outer canthus of the eye. Others have placed it 13 mm anterior to the posterior margin of the center of the tragus of the ear on a line extending to the corner of the eye. Bergström has located the arbitrary axis 10 mm anterior to the center of a spherical insert for the external auditory meatus and 7 mm below the Frankfort horizontal plane.
In a series of experiments reported by Beck, it was shown that the arbitrary axis suggested by Bergström falls consistently closer to the kinematic axis than do the other two. It is desirable that an arbitrary axis is placed as close as possible to the kinematic axis. Although most authorities agree that any of the three axes will permit transfer of the maxillary cast with reasonable accuracy, it would seem that the Bergström point compares most favorably with the kinematic axis.
The lowest point on the inferior orbital margin is taken as the third point of reference for establishing the axis-orbital plane. Some authorities use the point on the lower margin of the bony orbit in line with the center of the pupil of the eye. For the sake of consistency, the right infraorbital point is generally used and the facebow assembled in this relationship. All three points (right and left axes and infraorbital point) are marked on the face with an ink dot before the transfer is made.
Casts are prepared for mounting on an articulator by placing three index grooves in the base of the casts. Two V-shaped grooves are placed in the posterior section of the cast and one groove in the anterior portion (Figure 12-7).

Figure 12-7 The base of the cast has been prepared for mounting by placing three triangular grooves to allow indexing when mounted. The grooves are prepared with a 3-inch stone mounted in a laboratory lathe.
An occlusion rim properly oriented on a well-fitting record base should be used in facebow procedures involving the transfer of casts representative of the Class I and II partially edentulous situations. Without occlusion rims, such casts cannot be located accurately in the imprints of the wax covering the facebow fork. Tissues covering the residual ridges may be displaced grossly when the patient closes into the wax on the facebow fork. Therefore the wax imprints of the soft tissues will not be true negatives of the edentulous regions of the diagnostic casts.
For purposes of illustration, a facebow using the external auditory meatus as the posterior reference point, the Whip-Mix Facebow technique (DB 2000, Whip-Mix Corp, Louisville, KY), will be shown. The facebow fork is covered with a polyether, polyvinyl siloxane or a roll of softened baseplate wax with the material distributed equally on the top and on the underneath side of the facebow fork. Then the fork should be pressed lightly on the diagnostic casts with the midline of the facebow fork corresponding to the midline of the central incisors (Figure 12-8). This will leave imprints of the occlusal and incisal surfaces of the maxillary casts and occlusion rim on the softened baseplate wax and is an aid in correctly orienting the facebow fork in the patient’s mouth. The facebow fork is placed in position in the mouth, and the patient is asked to close the lower teeth into the wax to stabilize it in position. It is removed from the mouth and chilled in cold water and then replaced in position in the patient’s mouth. An alternative method of stabilizing the facebow fork and recording bases is to enlist the assistance of the patient.
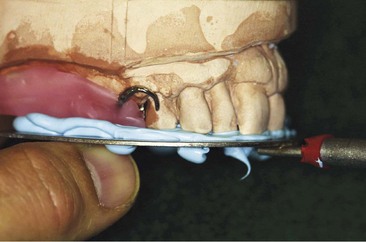
Figure 12-8 Orienting the facebow fork to the maxillary cast and occlusion rims will avoid displacing the occlusion rim in the mouth through patient closure or another uneven force. Polyvinyl siloxane material has been evenly distributed around the facebow fork, and care is exercised to position the fork to be centered at the mid-incisal position without any fork extension posterior to the record base, which could cause discomfort.
If an earpiece facebow is to be used, the patient should be reminded that the plastic earpieces in the auditory canals will greatly amplify noise. With the facebow fork in position, the facebow toggle is slipped over the anterior projection of the facebow fork (Figure 12-9). The patient can assist in guiding the plastic earpieces into the external auditory meatus. The patient can then hold the arms of the facebow in place with firm pressure while the operator secures the bite fork to the facebow. This accomplishes the radius aspect of the facebow transfer.
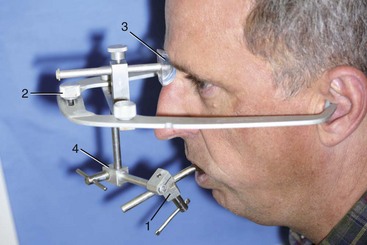
Figure 12-9 The horizontal toggle clamp of the Whip-Mix earpiece facebow (1) is slid onto the shaft of the facebow fork protruding from the patient’s mouth. The patient then helps guide plastic earpieces into the external auditory meatus and holds them in place while the operator tightens three thumb screws (2) and centers the plastic nosepiece (3) securely on the nasion. The horizontal toggle clamp is positioned and secured near (but not touching) the lip. The T screw (4) on the vertical bar is tightened. note: Extreme care should be exercised not to tilt the facebow out of position when tightening.
If an infraorbital pointer is used, it is placed on the extreme right side of the facebow and angled toward the infraorbital point previously identified with an ink dot. It is then locked into position with its tip lightly touching the skin at the dot. This establishes the elevation of the facebow in relation to the axis-orbital plane. Extreme care must be taken to avoid any slip that might injure the patient’s eye.
With all elements tightened securely, the patient is asked to open, and the entire assembly is removed intact, rinsed with cold water, and set aside. The facebow records not only the radius from the condyles to the incisal contacts of the upper central incisors, but also the angular relationship of the occlusal plane to the axis-orbital plane.
The facebow must be positioned on the articulator in the same axis-orbital relation as on the patient. If an arbitrary-type facebow is used, the calibrated condyle rods of the facebow ordinarily will not fit the condyle shafts of the articulator unless the width between the condyles just happens to be the same. With a Hanau model 132-25M facebow, the calibrations must be reequalized when in position on the articulator. For example, they have read 74 (mm) on each side of the patient but must be adjusted to read 69 (mm) on each side of the articulator. Some later model articulators have adjustable condyle rods and may be adjusted to fit the facebow. It is necessary that the facebow be centered in either case. Some facebows are self-centering, as is the Hanau Spring-Bow (Whip-Mix Corp, Louisville, KY).
The third point of reference is the orbital plane indicator, which must be swung to the right so that it will be above the tip of the infraorbital pointer. The entire facebow with maxillary cast in place must be raised until the tip of the pointer contacts the orbital plane indicated. The elevation having thus been established, for all practical purposes the orbital plane indicator and the pointer may now be removed because they may interfere with placing the mounting stone.
An auxiliary device called a cast support is available; it is used to support the facebow fork and the maxillary cast during the mounting operation (Figure 12-10). With this device, the weight of the cast and the mounting stone are supported separately from the facebow, thus preventing possible downward movement resulting from their combined weight. The cast support is raised to supporting contact with the facebow fork after the facebow height has been adjusted to the level of the orbital plane. Use of some type of cast support is highly recommended as an adjunct to facebow mounting.
The keyed and lubricated maxillary cast is now attached to the upper arm of the articulator with the mounting stone, thus completing the facebow transfer (Figure 12-11). Not only will the facebow have permitted the upper cast to be mounted with reasonable accuracy, it also will have served as a convenient means of supporting the cast during mounting. Once mastered, its use becomes a great convenience rather than a time-consuming nuisance.

Figure 12-11 Facebow mounting is complete. The relationship of the maxillary cast to the articulator condylar components is anatomically similar to that between the patient’s maxilla and the bilateral temporomandibular joint (TMJ) complex. Any subsequent tooth arrangement and occlusal contact development will represent the mouth more accurately than more arbitrary mountings. The benefits of the anatomic similarity are seen in more accurate occlusion for the finalized prosthesis (i.e., less intraoral adjustment required).
It is preferable that the maxillary cast be mounted while the patient is still present, thus eliminating a possible reappointment if the facebow record is unacceptable for some reason. Not too infrequently, the facebow record has to be redone with the offset-type facebow fork repositioned to avoid interference with some part of the articulator.
Jaw Relationship Records for Diagnostic Casts
One of the first critical decisions that must be made in a removable partial denture service involves selection of the horizontal jaw relationship to which the removable partial denture will be fabricated (centric relation or the maximum intercuspal position). All mouth-preparation procedures depend on this analysis. Failure to make this decision correctly may result in poor prosthesis stability, discomfort, and deterioration of the residual ridges and supporting teeth.
It is recommended that deflective occlusal contacts in the maximum intercuspal and eccentric positions be corrected as a preventive measure. Not all dentists agree that centric relation and the maximum intercuspal position must be harmonious in the natural dentition. Many dentitions function satisfactorily with the opposing teeth maximally intercusped in an eccentric position without either diagnosable or subjective indications of temporomandibular joint dysfunction, muscle dysfunction, or disease of the supporting structures of the teeth. In many such situations, no attempt should be made to alter the occlusion. It is not a requirement to interfere with an occlusion simply because it does not completely conform to a relationship that is considered ideal.
If most natural posterior teeth remain and if no evidence of temporomandibular joint disturbances, neuromuscular dysfunction, or periodontal disturbances related to occlusal factors exists, the proposed restorations may be fabricated safely with maximum intercuspation of remaining teeth. However, when most natural centric stops are missing, the proposed prosthesis should be fabricated so that the maximum intercuspal position is in harmony with centric relation. By far the greater majority of removable partial dentures should be fabricated in the horizontal jaw relationship of centric relation. In most instances in which edentulous spaces have not been restored, the remaining posterior teeth will have assumed malaligned positions through drifting, tipping, or extrusion. Correction of the remaining natural occlusion to create a coincidence of centric relation and the maximum intercuspal position is indicated in such situations.
Regardless of the method used in creating a harmonious functional occlusion, an evaluation of the existing relationships of the opposing natural teeth must be made and is accomplished with a diagnostic mounting. This evaluation is performed in addition to, and in conjunction with, other diagnostic procedures that contribute to an adequate diagnosis and treatment plan.
Diagnostic casts provide an opportunity to evaluate the relationships of remaining oral structures when correctly mounted on a semiadjustable articulator with use of a facebow transfer and interocclusal records. Diagnostic casts are mounted in centric relation (most retruded relation of the mandible to the maxillae) so that deflective occlusal contacts can be correlated with those observed in the mouth. Deflective contacts of opposing teeth are usually destructive to the supporting structures involved and should be eliminated. Diagnostic casts demonstrate the presence and location of such interfering tooth contacts and permit visualization of the treatment that would be necessary for their correction. Necessary alteration of teeth to harmonize the occlusion can be performed initially on duplicates of the mounted diagnostic casts to act as guides for similar necessary corrections in the mouth. In many instances the degree of alteration required will indicate the need for crowns or onlays to be fabricated, or for recontouring, repositioning, or elimination of extruded teeth.
As was previously mentioned, the maxillary cast is correctly oriented to the opening axis of the articulator by means of the facebow transfer and becomes spatially related to the upper member of the articulator in the same relationship that the maxilla has to the hinge axis and the Frankfort plane. Similarly, when a centric relation record is made at an established vertical dimension, the mandible is in its most retruded relation to the maxilla. Therefore when the maxillary cast is correctly oriented to the axis of the articulator, the mandibular cast automatically becomes correctly oriented to the opening axis, when attached to and mounted with an accurate centric relation record.
Unlike recording the fixed relationship of the maxilla to the mandibular opening axis (using the facebow transfer record), the mandibular position is recorded in space and is not a fixed point. Consequently, it is necessary to prove that the relationship of the mounted casts is correct. This can be done simply by making another interocclusal record, at centric relation, fitting the casts into the record, and checking to see that the condylar elements of the articulator are snug against the condylar housings. If this is not seen, another record is made until duplicate records are produced. Because centric relation is the only jaw position that can be repeated by the patient, mountings in this position can be replicated and verified for correctness.
A straightforward protrusive record is made to adjust the horizontal condylar inclines on the articulator. Lateral eccentric records are made so that the lateral condylar inclinations can be properly adjusted. All interocclusal records should be made as near the vertical relation of occlusion as possible. Opposing teeth or occlusion rims must not be allowed to contact when the records are made. A contact of the inclined planes of opposing teeth will invalidate an interocclusal record.
In some instances, a mounting of a duplicate diagnostic cast in the maximum intercuspal position may also be desirable to definitively study this relationship on the articulator. Because articulators simulate only jaw movements, it is not unreasonable to assume that the relationship of the casts mounted in centric relation may differ minutely from the maximum intercuspal position seen on the articulator and observed in the mouth. When diagnostic casts are hand related by maximum intercuspation for purposes of mounting on an articulator, it is essential that three (preferably four) positive contacts of opposing posterior teeth are present, having widespread molar contacts on each side of the arch. If occlusion rims are necessary to correctly orient casts on an articulator, a centric relation should usually be the horizontal jaw relationship to which the removable partial denture will be constructed.
Materials and Methods for Recording Centric Relation
Materials available for recording centric relation are (1) wax; (2) modeling plastic; (3) quick-setting impression plaster; (4) metallic oxide bite registration paste; (5) polyether impression materials; and (6) silicone impression materials. Of these, wax is likely to be least satisfactory unless carefully handled. If not uniformly softened when introduced into the mouth, it can record a position with unequal tissue placement. Also, it does not remain rigid and dimensionally stable after removal unless carefully chilled and handled upon removal (Figure 12-12).
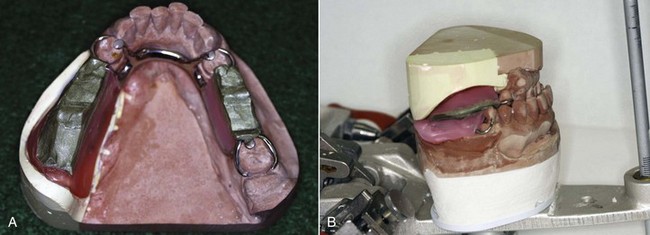
Figure 12-12 A wax interocclusal record made on a cast framework. The modification spaces first had baseplate wax added; these were adjusted intraorally to provide space at the occlusal vertical dimension for recording wax, the wax was softened using a wax spatula and a hot water bath, the framework was placed in the mouth, and care was exercised to guide the patient to close into a previously verified (and practiced) interocclusal position deemed appropriate (in this instance, centric relation position). The record was recovered from the mouth, excess wax was removed with a warm scalpel, and the wax was chilled and replaced in the mouth to verify the record. If not verified, the wax was resoftened (with additional wax added as needed) and the procedure was repeated. B, Immediately after verification, the framework with interocclusal registration was replaced on the mandibular cast and inverted on the maxillary cast for mounting.
Modeling plastic is a satisfactory record medium because it can be flamed and tempered until uniformly soft before it is placed into the mouth. After modeling plastic is chilled, it is sufficiently stable to permit the mounting of casts with accuracy. For these reasons, it is a satisfactory medium for recording occlusal relations for complete or partial dentures. It also can be used with opposing natural teeth.
Impression plaster has advantages of softness when introduced and rigidity when set, which make it a satisfactory material for recording jaw relations. Its use is highly recommended when occlusion rims are used to mount casts correctly or to adjust articulators with interocclusal eccentric records.
Metallic oxide bite registration paste offers many of the advantages of plaster, with less friability. Although not strong enough to be used alone, when supported by a gauze mesh attached to a metal frame, it is a satisfactory recording medium. Also it may be used with occlusion rims. After the paste sets, the frame is removed from the mouth and the buccal side of the gauze released where it was secured with sticky wax. The tube on the lingual side may then be slid off the lingual extension of the frame. The frame is not needed when casts are mounted with this type of registration because the tube alone lends sufficient support to the interocclusal record.
Elastomeric materials are excellent for recording interocclusal relationships (Figure 12-13). Some are specially formulated for this purpose and have the qualities of extremely low viscosity, minimal resistance to closure, rapid set, low rebound, lack of distortion, and stability after removal from the mouth. Care should be exercised to ensure that no elastic rebound results when the record is related to the cast during the mounting procedure.
The mandibular cast should be mounted on the lower arm of the articulator, with the articulator inverted (Figure 12-14A). The articulator is first locked in centric position, and the incisal pin is adjusted so that the anterior distance between the upper and lower arms of the articulator will be increased 2 to 3 mm greater than the normal parallel relationship of the arms. This is done to compensate for the thickness of the interocclusal record so that the arms of the articulator will again be nearly parallel when the interocclusal record is removed and the opposing casts come into contact.
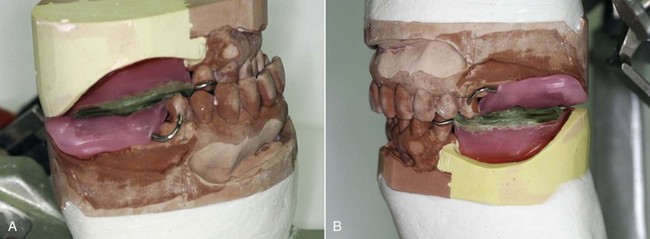
Figure 12-14 A, Mandibular cast inverted on the mounted maxillary cast, making sure that the cast is fully seated into the interocclusal record and stabilized to the opposing cast. It is important to check the posterior occlusion rim contact to ensure that no interfering contact has altered the record. Space should be observed between the opposing record bases (or record base and opposing occlusion). B, Mounted casts demonstrating the occlusal plane as found in the mouth. The Frankfort plane of the patient is oriented parallel to the articulator base and the floor. Also, inspection of the posterior rims demonstrates space between the rims, which ensures that the recorded position was registered without influence from rigid contacting components, only from softened wax.
The base of the cast should be keyed and lightly lubricated for future removal. With the diagnostic casts accurately seated and secured in the occlusal record, the mandibular cast is affixed with stone to the lower member of the inverted articulator.
An articulator mounting thus made will have related the casts in centric relation (Figure 12-14B). The dentist then can proceed to make an occlusal analysis by observing the influence of cusps in relation to one another after the articulator has been adjusted by using eccentric interocclusal records.
After an occlusal analysis has been made, the casts may be removed from their mounting for the purpose of surveying them individually and for other purposes as outlined previously. The indexed mounting ring record also should be retained throughout the course of treatment in the event that further study should be needed. It is advisable that the mounting be identified with the articulator that is used, so that it may always be placed back onto the same articulator.
Diagnostic Findings
The information gathered in the patient interview and clinical examination provides the basis for establishing whether treatment is indicated, and if so, what specific treatment should be considered. More than one treatment option can be considered, and financial implications need to be considered against long-term expectations if the best decision is to be reached. Provision of a removable partial denture does not often preclude future consideration for other treatments, a fact that is not often the case for alternative treatments. The patient interview can reveal medical considerations that influence the decision to provide any prosthesis. When it is felt that general medical health is being neglected, patients should be strongly encouraged to seek a general medical examination. Alternatively, patients who regularly see their physician may be found to take multiple medications that can contribute to a dry mouth and, potentially, an altered oral microflora with some increased risk for plaque-induced disease. Although such a condition can influence any prosthodontic care, given the unique features of removable partial denture service relative to the need for increased hygiene awareness and care, any factor that places an additional risk for plaque-induced disease should be emphasized with the patient and corrected if possible. Health conditions that negatively affect oral mucosal health (e.g., diabetes mellitus, Sjögren’s syndrome, lupus, atrophic changes) may pose a risk for patient comfort for a tissue-supported prosthesis and factor into a treatment decision.
For the patient who has had previous experience with some form of prosthesis, the patient interview provides additional information that can influence treatment decisions. Identifying possible reasons (or more importantly, a lack of any reason) for both positive and negative past prosthesis experiences is important for determining whether a patient can predictably be helped. Although the clinical examination will point out the oral tissue responses to such therapy, the interview will highlight the subjective patient response to therapy and provides significant information that should be pursued. As was mentioned previously, a patient complaint regarding the prosthesis needs to be confirmed through evaluation. The patient generally expresses concern about a symptom that can be related to support, stability, retention, and/or appearance. Confirmation of a design feature or oral condition that can explain the symptom is required if one is to have a chance to correct it with a similar prosthesis. If examination does not confirm any such relationship, it would be difficult to proceed without some concern for repeating the patient response to therapy unless a different form of therapy is selected (e.g., replacing a problematic removable partial denture with an implant-supported prosthesis).
Interpretation of Examination Data
As a result of the oral examination, several diagnoses are made that are related to the various tissues, conditions, and clinical information gathered. The integration of these diagnoses serves as the basis for decisions that will ultimately identify the suggested treatment. The treatment decision reflects a confluence of several aspects of the patient’s past, present, and potential oral health status.
It is helpful to consider how the various diagnoses are integrated; consequently, a suggested framework is provided that highlights aspects of disease management, followed by reconstruction considerations for (1) prosthesis support, and (2) prosthesis design-specific aspects.
Disease management takes into account findings from the radiographic examination, periodontal disease and caries assessments, and pathology requiring endodontic considerations. Reconstruction considerations include diagnoses relative to prosthesis support (teeth and residual ridges) and prosthesis-specific design elements. Prosthesis support related to the remaining teeth requires radiographic examination of alveolar support and root morphology, endodontic evaluation, analysis of occlusal factors, assessment of the benefit for fixed prostheses or orthodontics, and evaluation of the need for extraction. Residual ridge support involves radiographic examination of ridge contours and height, and evaluation of the need for pre-prosthetic surgical intervention. Prosthesis-specific design considerations include determination of anatomic relationships related to mandibular major connector design, the need for tooth modification to facilitate prosthesis function, and analysis of the occlusion. Each of these is considered in the following sections.
Radiographic Interpretation
Many of the reasons for radiographic interpretation during oral examination are outlined herein and are considered in greater detail in other texts. Aspects of such interpretation that are most pertinent to removable partial denture construction are those relative to the prognosis of remaining teeth that may be used as abutments.
Disease Validation
It is important to verify by clinical examination disease found through radiographic interpretation. Also, if the clinical examination reveals dental caries and/or periodontal disease, its severity can be confirmed by radiographic interpretation. It would be important to delineate caries severity, in terms of numbers of lesions and dentin/pulpal involvement, to gain insight as to level of disease risk associated with the patient, as well as to identify what therapy is required to maintain teeth. The same is true for periodontal disease risk and severity, as such a diagnosis affects both current and future tooth prognosis for prosthesis support.
Radiographic interpretation allows diagnosis of bone lesions associated with both the jaws and the teeth. The implications for tooth stability and ridge support are important to factor into prosthesis prognosis. Surgical and postoperative management of such lesions can vary significantly with diagnosis (benign vs. malignant), and definitive prosthesis treatment is often complicated by resective procedures.
Tooth Support
The quality of the alveolar support of an abutment tooth is of primary importance because the tooth will have to withstand greater stress loads when supporting a dental prosthesis. Abutment teeth providing total abutment support to the prosthesis, whether fixed or removable, will have to withstand a greater load and especially greater horizontal forces. The latter may be minimized by establishing a harmonious occlusion and by distributing the horizontal forces among several teeth through the use of rigid connectors. Bilateral stabilization against horizontal forces is one of the attributes of a properly designed tooth-supported removable prosthesis. In many instances, abutment teeth may be aided more than weakened by the presence of a bilaterally rigid removable partial denture.
In contrast, abutment teeth adjacent to distal extension bases are subjected not only to vertical and horizontal forces but to torque as well because of movement of the tissue-supported base. Vertical support and stabilization against horizontal movement with rigid connectors are just as important as they are with a tooth-supported prosthesis, and the removable partial denture must be designed accordingly. In addition, the abutment tooth adjacent to the extension base will be subjected to torque in proportion to the design of the retainers, the size of the denture base, the tissue support received by the base, and the total occlusal load applied. With this in mind, each abutment tooth must be evaluated carefully as to the alveolar bone support present and the past reaction of that bone to occlusal stress.
It is important to judge whether the teeth and their respective periodontium can favorably respond to the demands of a prosthesis. Can radiographic interpretation provide clues to predicting tooth response to increased loading from prostheses? Assessment of regions within the mouth that have been subjected to increased loading can provide some clues as to the predictability of future similar response. An understanding of bone density, index areas, and lamina dura response is helpful for these judgments.
Bone Density
The quality and quantity of bone in any part of the body are often evaluated by radiographic means. A detailed treatise concerning bone support of the abutment tooth should include many considerations not possible to include in this text because of space limitations. The reader should realize that subclinical variations in bone may exist but may not be observed because of the limitations inherent in technical methods and equipment.
Of importance to the dentist in evaluating the quality and quantity of the alveolar bone are the height and the quality of remaining bone. In estimating bone height, care must be taken to avoid interpretive errors resulting from angulation factors. Technically, when a radiographic exposure is made, the central ray should be directed at right angles to both the tooth and the film. The short-cone technique does not follow this principle; instead the ray is directed through the root of the tooth at a predetermined angle. This technique invariably causes the buccal bone to be projected higher on the crown than the lingual or palatal bone. Therefore in interpreting bone height, it is imperative to follow the line of the lamina dura from the apex toward the crown of the tooth until the opacity of the lamina materially decreases. At this point of opacity change, a less dense bone extends farther toward the tooth crown. This additional amount of bone represents false bone height. Thus the true height of the bone is ordinarily where the lamina shows a marked decrease in opacity. At this point, the trabecular pattern of bone superimposed on the tooth root is lost. The portion of the root between the cementoenamel junction and the true bone height has the appearance of being bare or devoid of covering.
Radiographic evaluation of bone quality is hazardous but is often necessary. It is essential to emphasize that changes in bone mineralization up to 25% often cannot be recognized by ordinary radiographic means. Optimum bone qualities are ordinarily expressed by normal-sized interdental trabecular spaces that tend to decrease slightly in size as examination of the bone proceeds from the root apex toward the coronal portion. The normal interproximal crest is ordinarily shown by a relatively thin white line crossing from the lamina dura of one tooth to the lamina dura of the adjacent tooth. Considerable variation in the size of trabecular spaces may exist within normal limits, and the radiographic appearance of crestal alveolar bone may vary considerably, depending on its shape and the direction that the ray takes as it passes through the bone.
Normal bone usually responds favorably to ordinary stresses. Abnormal stresses, however, may create a reduction in the size of the trabecular pattern, particularly in that area of bone directly adjacent to the lamina dura of the affected tooth. This decrease in size of the trabecular pattern (i.e., so-called bone condensation) is often regarded as a favorable bone response, indicative of an improvement in bone quality. This is not necessarily an accurate interpretation. Such bone changes usually indicate stresses that should be relieved because if the resistance of the patient decreases, the bone may exhibit a progressively less favorable response on future radiographs.
Increased thickness of the periodontal space ordinarily suggests varying degrees of tooth mobility. This should be evaluated clinically. Radiographic evidence coupled with clinical findings may suggest to the dentist the inadvisability of using such a tooth as an abutment. Furthermore, an irregular intercrestal bone surface should make the dentist suspicious of active bone deterioration.
It is essential that the dentist realize that radiographic evidence shows the result of changes that have taken place and may not necessarily represent the present condition. For example, periodontal disease may have progressed beyond the stage visibly demonstrated on the radiograph. As was pointed out earlier, radiographic changes are not observed until approximately 25% of the mineral content has been depleted. On the other hand, bone condensation probably does represent the current situation.
Radiographic findings should serve the dentist as an adjunct to clinical observations. Too often the radiographic appearance alone is used to arrive at a diagnosis; therefore radiographic findings should always be confirmed by clinical examination. Radiographic interpretation will also serve an important function if used periodically after the prosthesis has been placed. Future bone changes of any type suggest traumatic interference from some source. The nature of such interference should be determined and corrective measures taken.
Index Areas
Index areas are those areas of alveolar support that disclose the reaction of bone to additional stress. Favorable reaction to such stress may be taken as an indication of future reaction to an added stress load. Teeth that have been subjected to abnormal loading because of the loss of adjacent teeth or that have withstood tipping forces in addition to occlusal loading may be better risks as abutment teeth than those that have not been called on to carry an extra occlusal load (Figures 12-15 and 12-16). If occlusal harmony can be improved and unfavorable forces minimized by the reshaping of occlusal surfaces and the favorable distribution of occlusal loading, such teeth may be expected to support the prosthesis without difficulty. At the same time, other teeth, although not at present carrying an extra load, may be expected to react favorably because of the favorable reaction of alveolar bone to abnormal loading elsewhere in the same arch.

Figure 12-15 The reaction of bone adjacent to teeth that have been subjected to abnormal stress serves as an indication of probable reactions of that bone when such teeth are used as abutments for fixed or removable restorations. Such areas are called index areas.

Figure 12-16 A, The canine has provided support for the distal extension removable partial denture for 10 years. There has obviously been positive bone response (arrow) to increased stress generated by the removable partial denture. B, The mandibular first premolar has provided support for the distal extension denture for 3 years. Bone response (arrow) to past additional stress has been unfavorable.
Other index areas are those around teeth that have been subjected to abnormal occlusal loading; that have been subjected to diagonal occlusal loading caused by tooth migration; and that have reacted to additional loading, such as around existing fixed partial denture abutments. The reaction of the bone to additional stresses in these areas may be either positive or negative, with evidence of a supporting trabecular pattern, a heavy cortical layer, and a dense lamina dura, or the reverse response. With the former, the patient is said to have a positive bone factor, which means the ability to build additional support wherever needed. With the latter, the patient is said to have a negative bone factor, which means the inability to respond favorably to stress.
Alveolar Lamina Dura
The alveolar lamina dura is also considered in a radiographic interpretation of abutment teeth. The lamina dura is the thin layer of hard cortical bone that normally lines the sockets of all teeth. It affords attachment for the fibers of the periodontal membrane, and, as with all cortical bone, its function is to withstand mechanical strain. In a roentgenogram, the lamina dura is shown as a radiopaque white line around the radiolucent dark line that represents the periodontal membrane.
When a tooth is in the process of being tipped, the center of rotation is not at the apex of the root, but in the apical third. Resorption of bone occurs where there is pressure, and apposition occurs where there is tension. Therefore during the active tipping process, the lamina dura is uneven, with evidence of both pressure and tension on the same side of the root. For example, in a mesially tipping lower molar, the lamina dura will be thinner on the coronal mesial and apicodistal aspects and thicker on the apicomesial and coronal distal aspects because the axis of rotation is not at the root apex but is above it. When the tooth has been tipped into an edentulous space by some change in the occlusion and becomes set in its new position, the effects of leverage are discontinued. The lamina dura on the side to which the tooth is sloping becomes uniformly heavier, which is nature’s reinforcement against abnormal stresses. The bone trabeculations are most often arranged at right angles to the heavier lamina dura.
Thus it is possible to say that for a given individual, nature is able to build support where it is needed and on this basis to predict future reactions elsewhere in the arch to additional loading of teeth used as abutments. However, because bone is approximately 30% organic, and this mostly protein, and because the body is not able to store a protein reserve in large amounts, any change in body health may be reflected in the patient’s ability to maintain this support permanently. When systemic disease is associated with faulty protein metabolism and when the ability to repair is diminished, bone is resorbed and the lamina dura is disturbed. Therefore the loading of any abutment tooth must be kept to a minimum inasmuch as the patient’s future health status and the eventualities of aging are unpredictable.
Root Morphology
The morphologic characteristics of the roots determine to a great extent the ability of prospective abutment teeth to resist successfully additional rotational forces that may be placed on them. Teeth with multiple and divergent roots will resist stresses better than teeth with fused and conical roots, because the resultant forces are distributed through a greater number of periodontal fibers to a larger amount of supporting bone (Figure 12-17).
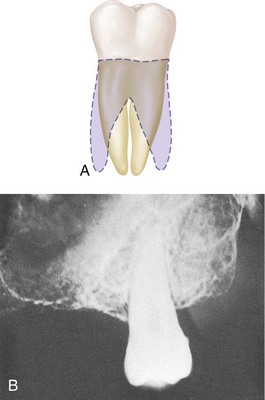
Figure 12-17 A, The prognosis for abutment service is more favorable for a molar with divergent roots (shaded) than for the same tooth if its roots were fused and conical. B, Evidence that prospective abutment has conical and fused roots indicates the necessity for formulating a framework design that will minimize additional stresses placed on the tooth by the abutment service.
Third Molars
Unerupted third molars should be considered as prospective future abutments to eliminate the need for a distal extension removable partial denture (Figure 12-18). The increased stability of a tooth-supported denture is most desirable to enhance the health of the oral environment.
Periodontal Considerations
An assessment of the periodontium in general and abutment teeth in particular must be made before prosthetic restoration. One must evaluate the condition of the gingiva, looking for adequate zones of attached gingiva and the presence or absence of periodontal pockets. The ideal periodontal condition is a disease-free periodontium with adequate attached mucosa in regions at or adjacent to removable partial denture component parts that cross the gingival margins to best resist the mechanical challenges posed as the result of function and use. The condition of the supporting bone must be evaluated, with specific attention to reduced bone support and mobility patterns recorded. If mucogingival involvements, osseous defects, or mobility patterns are recorded, the causes and potential treatment must be determined.
Oral hygiene habits of the patient must be determined, and efforts made to educate the patient relative to plaque control. The most decisive evidence of oral hygiene habits is the condition of the mouth before the initial prophylaxis. Good or bad oral hygiene is basic to the patient’s nature, and although it may be influenced somewhat by patient education, the long-range view must be taken. It is reasonably fair to assume that the patient will do little more in the long-term future than he has done in the past. In making decisions as to the method of treatment based on oral hygiene, the future in years, rather than in weeks and months, must be considered. It is probably best not to give the patient the benefit of any doubt as to future oral hygiene habits. Rather, the benefit should come from protective measures where any doubt exists about future oral hygiene habits. Therefore for patients at greatest risk, an oral prophylaxis with continued oral hygiene instructions should be scheduled for 3- to 4-month intervals. In addition, the patient must be advised of the importance of regular maintenance appointments for tissue-supported prostheses to maintain occlusal relationships. When these ongoing observations and prophylactic requirements are described, the patient is faced with the realization that he or she must be willing to share responsibility for maintaining the health of the mouth after restorative and prosthodontic treatment.
The remaining teeth and prosthesis will require meticulous plaque control after placement of a removable partial denture. Because of the nature of material coverage of oral tissues, the oral microflora can change with the use of a removable prosthesis. Coupled with this microbial change is the potential for a mechanical challenge to tissue integrity if the appropriate relationship of the prosthesis and soft tissues of the residual ridge, as well as the marginal gingival, is not maintained.
Caries Risk Assessment Considerations
Caries activity in the mouth, past and present, and the need for protective restorations must be considered. The decision to use full coverage is based on a need to reshape abutment teeth to accommodate the components of the removable partial denture, prevention of restoration breakdown when abutments have large direct restorations, or evidence of recurrent caries risk. Occasionally, three-quarter crowns may be used where buccal or lingual surfaces are completely sound, but intracoronal restorations (inlays) are seldom indicated in any mouth with evidence of past extensive caries or precarious areas of decalcification, erosion, or exposed cementum.
Frequent consumption of sugars can lead to carious involvement of roots, caries around restorations, or caries associated with clasps of removable partial dentures. Intelligent consumption of sweets (smaller amounts and less frequent consumption) and frequent plaque removal are the recommended countermeasures. Excellent protection from caries can be provided by fluoride applications via toothpastes, mouth rinses, or (in extreme cases, such as postradiation xerostomia) 1% NaF gels applied daily with plastic trays.
Xerostomia, caused by degeneration of salivary glands (Sjögren’s syndrome) or various medications, will enhance the occurrence and severity of caries, as well as contribute to irritation of the oral mucosa. A possible way to alleviate xerostomia is the use of synthetic saliva, with a carboxymethylcellulose base, which can be enriched with fluoride in an effort to counteract caries. Frequent use provides an excellent means of maintaining high fluoride intraorally for long periods of time, thus enhancing the remineralization of incipient caries. Although providing instructions for improvement of oral hygiene is a duty of the dental team, suspected problems of dietary deficiencies should be referred to a nutritionist.
Evaluation of the Prosthesis Foundation—Teeth and Residual Ridge
An evaluation of the prosthesis foundation is required to ensure that an appropriately stable base of sound teeth and/or residual ridge(s) is provided to maximize prosthesis function and patient comfort. To that end, the evaluation focuses on the identification of conditions that are inconsistent with sound support and predictably stable function.
Surgical Preparation
The need for pre-prosthetic surgery or extractions must be evaluated. The same criteria apply to surgical intervention in the partially edentulous arch as in the completely edentulous arch. Grossly displaceable soft tissues covering basal seat areas and hyperplastic tissue should be removed to provide a firm denture foundation. Mandibular tori should be removed if they will interfere with the optimum location of a lingual bar connector or a favorable path of placement. Any other areas of bone prominence that will interfere with the path of placement should be removed also. The path of placement will be dictated primarily by the guiding plane of the abutment teeth. Therefore some areas may present interference to the path of placement of the removable partial denture by reason of the fact that other unalterable factors such as retention and esthetics must take precedence in selecting that path.
Clinical research in pre-prosthetic surgical concepts has contributed significant developments to management of the compromised partially edentulous patient. Bone augmentation and guided bone regeneration procedures have been used with varying degrees of success as an alternative method of improving ridge support for the denture base areas. Skill and judgment must be exercised in patient selection, procedural planning, and surgical and prosthetic management to optimize clinical results. Use of osseointegrated implants can provide a foundation for developing suitable abutment support for removable partial dentures. As in any surgical procedure, results depend on careful treatment planning and cautious surgical management.
Extraction of teeth may be indicated for one of the following three reasons:
Another consideration for pre-prosthetic surgery involves the decision between use of a removable partial denture and an implant-supported prosthesis. The following categories of tooth loss are presented with comparative comments germane to such decisions.
Short Modification Spaces
For short spans (≤3 missing teeth), natural tooth– and implant-supported fixed prostheses as well as removable partial dentures can generally be considered. Implant placement requires the decision that ample bone volume exists, or can be provided with minimal morbidity, to adequately house sufficient implants to support prosthetic teeth. Implant prostheses have the advantage of not requiring the use of teeth for support, stability, and retention requirements, and consequently do not increase the functional burden on the natural dentition. Although the predictability of contemporary implant procedures (surgery and prosthodontics) makes them a consideration for short span prostheses, the main advantage is the opportunity to provide replacement teeth without involving adjacent teeth in the reconstruction. Therefore, when the adjacent teeth are in need of restoration, a conventional prosthesis should be considered.
Longer Modification Spaces
Longer span modification spaces (≥4 missing teeth) present a greater challenge for natural tooth–supported fixed prostheses. Consequently, options for treatment include the removable partial denture and the implant-supported prosthesis. An implant prosthesis has the same bone volume requirements as stated above, and for an increased span will likely require additional implants. Because residual ridge resorption can be greater with longer spans, the need for augmentation may also be greater. Both of these characteristics of longer spans cause implant use to be more costly and can significantly increase the cost difference between treatment options. The increased morbidity associated with augmentation procedures can also limit universal application. Because the removable partial denture remains largely tooth supported (unless the span includes anterior and posterior segments that may cause it to function similar to a distal extension), the functional stability requirements should be efficiently met through the tooth support.
Distal Extension Spaces
Without tooth support at each end of the missing teeth, the removable partial denture and the implant-supported prosthesis are the primary treatment considerations (double-abutted cantilevered fixed prostheses opposing maxillary complete dentures have been suggested to be a reasonable option for some patients). It then becomes obvious that when anatomic limitations to implant placement exist and surgical measures cannot be taken to correct this, the removable partial denture is the only option (unless no treatment is elected). Current surgical options are available to correct most anatomic limitations, yet frequently implant therapy is not elected because of patient medical factors, concerns for the risk of surgical morbidity, increased time required for treatment, and costs. It is important to note that a comparison of long-term maintenance requirements between these two options may demonstrate little cost difference over time. This is related to the effects of continued residual ridge resorption acting on the removable prosthesis and not the implant prosthesis.
Endodontic Treatment
Abutments for removable partial dentures are required to withstand various forces depending on the classification. The requirement for a distal extension abutment is different than that of a tooth-supported prosthesis in that torsional forces exist in the distal extension situation. For this reason, an abutment for a distal extension that is endodontically treated carries a greater risk for complications than a similar tooth not involved in removable partial denture function.
Because tooth support helps control prosthesis movement, the need for endodontic treatment should include assessment of overdenture abutments for removable partial dentures, especially to control movement of distal extensions.
Analysis of Occlusal Factors
From the occlusal analysis made by evaluating the mounted diagnostic casts, the dentist must decide whether it is best to accept and maintain the existing occlusion or to attempt to improve on it by means of occlusal adjustment and/or restoration of occlusal surfaces. It must be remembered that the removable partial denture can supplement the occlusion that exists only at the time the prosthesis is constructed. The dominant force that dictates the occlusal pattern will be the cuspal harmony or disharmony of the remaining teeth and their proprioceptive influence on mandibular movement. The goal of artificial tooth placement is to harmonize with the functional parameters of the existing occlusion providing bilateral, simultaneous functional contact.
Chapter 17 identifies schemes of occlusion recommended for partially edentulous configurations. A review of these recommendations will provide a guide for modifying the existing occlusion or developing the appropriate occlusal scheme for each partially edentulous configuration.
Improvements in the natural occlusion must be accomplished before the prosthesis is fabricated, not subsequent to its fabrication. The objective of occlusal reconstruction by any means should be occlusal harmony of the restored dentition in relation to the natural forces already present or established. Therefore one of the earliest decisions in planning reconstructive treatment must be whether to accept or reject the existing vertical dimension of occlusion and the occlusal contact relationships in centric and eccentric positions. If occlusal adjustment is indicated, cuspal analysis always should precede any corrective procedures in the mouth by selective grinding. On the other hand, if reconstruction is to be the means of correction, the manner and sequence should be outlined as part of the overall treatment plan.
Fixed Restorations
There may be a need to restore modification spaces with fixed restorations rather than include them in the removable partial denture, especially when dealing with isolated abutment teeth. The advantage of splinting must be weighed against the total cost, with the weight of experience always in favor of using fixed restorations for tooth-bounded spaces unless the space will facilitate simplification of the removable partial denture design without jeopardizing the abutment teeth. One of the least successful removable partial denture designs is seen when multiple tooth-bounded areas are replaced with removable partial dentures in conjunction with isolated abutment teeth and distal extension bases. Biomechanical considerations and the future health of the remaining teeth should be given preference over economic considerations when such a choice is possible.
Orthodontic Treatment
Occasionally, orthodontic movement of malposed teeth followed by retention through the use of fixed partial dentures makes possible a better removable partial denture design mechanically and esthetically than could otherwise be used. Although adequate anchorage for tooth movement can be a major limitation in partially edentulous arches, carefully placed implants that subsequently can be used for prosthesis support have been used to expand orthodontic applications for this patient group.
Need for Determining Type of Mandibular Major Connector
As was discussed in Chapter 5, one of the criteria used to determine the use of the lingual bar or linguoplate is the height of the floor of the patient’s mouth when the tongue is elevated. Because the inferior borders of the lingual bar and the linguoplate are placed at the same vertical level, and because subsequent mouth preparations depend in part on the design of the mandibular major connector, determination of the type of major connector must be made during the oral examination. This determination is facilitated by measuring the height of the elevated floor of the patient’s mouth in relation to the lingual gingiva with a periodontal probe and recording the measurement for later transfer to diagnostic and master casts. It is most difficult to make a determination of the type of mandibular major connector to be used solely from a stone cast that may or may not accurately indicate the active range of movement of the floor of the patient’s mouth. Too many mandibular major connectors are ruined or made flexible because subsequent grinding of the inferior border is necessary to relieve impingement of the sensitive tissues of the floor of the mouth.
Need for Reshaping Remaining Teeth
The clinical crown shapes of anterior and posterior teeth are not capable of supporting a removable partial denture framework without appropriate modification. Without the required modifications, the prosthesis does not adequately benefit from the support and stability offered by the teeth and consequently will not be comfortable to the patient. Many failures of removable partial dentures can be attributed to the fact that the teeth were not reshaped properly to establish guiding planes or to receive clasp arms and occlusal rests before the impression for the master cast was made. Of particular importance are the paralleling of proximal tooth surfaces to act as guiding planes, the preparation of adequate rest areas, and the reduction of unfavorable tooth contours (Figure 12-19). To neglect planning such mouth preparations in advance is inexcusable and leads to unsuccessful removable prosthesis service.
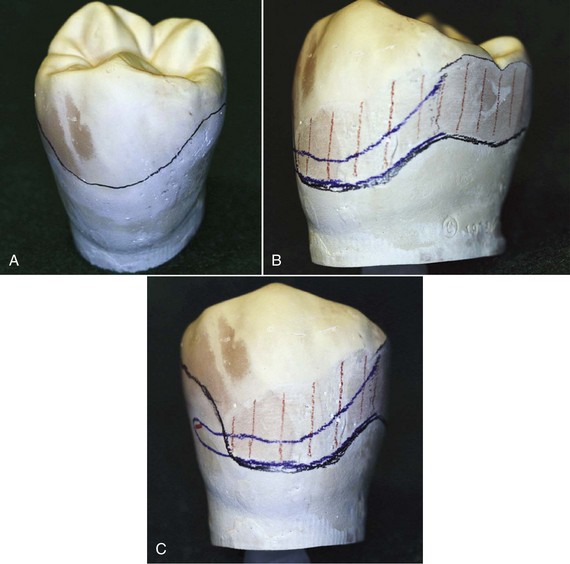
Figure 12-19 A, Unmodified buccal surface of the mandibular premolar illustrates a typical height of contour location natural for this tooth (middle and occlusal thirds of the tooth). B, Proximal surface modification is required (hatched region) to produce a guide-plane surface. C, Buccal surface modification is needed to position the height of contour for favorable clasp location. The tooth modification is a continuation of the proximal surface modification onto the buccal surface, and generally requires less than 0.5 mm of tooth removal.
The design of clasps is dependent on the location of the retentive, stabilizing, reciprocal, and supporting areas in relation to a definite path of placement and removal. Failure to reshape unfavorably inclined tooth surfaces and, if necessary, to place restorations with suitable contours not only complicates the design and location of clasp retainers but also often leads to failure of the removable partial denture because of poor clasp design.
A malaligned tooth or one that is inclined unfavorably may make it necessary to place certain parts of the clasp so that they interfere with the opposing teeth. Unparallel proximal tooth surfaces not only will fail to provide needed guiding planes during placement and removal but also will result in excessive blockout. This inevitably results in placement of the connectors so far out of contact with tooth surfaces that food traps are created. To pass lingually inclined lower teeth, clearance for a lingual bar major connector may have to be so great that a food trap will result when the restoration is fully seated. Such a lingual bar will be located so that it will interfere with tongue comfort and function. These are only some of the objectionable consequences of inadequate mouth preparations.
The amount of reduction of tooth contours should be kept to a minimum, and all modified tooth surfaces not only should be repolished after reduction but also should be subjected to fluoride treatment to lessen the incidence of caries. If it is not possible to produce the contour desired without perforating the enamel, then the teeth should be recontoured with an acceptable restorative material. The age of the patient, caries activity evidenced elsewhere in the mouth, and apparent oral hygiene habits must be taken into consideration when one is deciding between reducing the enamel or modifying tooth contours with protective restorations.
Some of the areas that frequently need correction are the lingual surfaces of mandibular premolars, the mesial and lingual surfaces of mandibular molars, the distobuccal line angle of maxillary premolars, and the mesiobuccal line angle of maxillary molars. The actual degree of inclination of teeth in relation to the path of placement and the location of retentive and supportive areas are not readily interpretable during visual examination. These are established during comprehensive analysis of the diagnostic cast with a surveyor, which should follow the visual examination.
Infection Control
The American Dental Association follows the Centers for Disease Control (CDC)–recommended infection control procedures for dentistry. The most recent recommendations were made in 2003 and included updates from the previous 1993 guidelines. Most of the updates will be familiar to practitioners and are already largely practiced routinely. They are designed to prevent or reduce the potential for disease transmission from patient to DHCW (Dental Health Care Worker), from DHCW to patient, and from patient to patient. The document emphasizes the use of “standard precautions” (which replaces the term “universal precautions”) for the prevention of exposure to and transmission of not only bloodborne pathogens, but also other pathogens encountered in oral health care settings.
Major updates and additions include application of standard precautions rather than universal precautions, work restrictions for health care personnel infected with, or occupationally exposed to, infectious diseases; management of occupational exposure to bloodborne pathogens, including postexposure prophylaxis for work exposures to hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV); selection and use of devices with features designed to prevent sharps injury, contact dermatitis, and latex hypersensitivity; hand hygiene; dental unit waterlines; and biofilm and water quality; special considerations include dental handpieces and other devices attached to air lines and waterlines, saliva ejectors, radiology, parenteral medications, single-use or disposable devices, pre-procedural mouth rinses, oral surgical procedures, handling of biopsy specimens and extracted teeth, laser/electrosurgery plumes, Mycobacterium tuberculosis, Creutzfeldt-Jakob disease and other prion diseases, program evaluation, and research considerations. The recommendations provide guidance for measures to be taken that will reduce the risks of disease transmission, among both dental health care workers (DHCWs) and their patients.
Dental patients and DHCWs potentially may be exposed to a variety of microorganisms. Exposure can occur via blood and/or oral or respiratory secretions. The microorganisms may include viruses and bacteria that infect the upper respiratory tract in general, as well as cytomegalovirus, HBV, HCV, herpes simplex virus types 1 and 2, HIV, Mycobacterium tuberculosis, staphylococci, and streptococci. The transmission of infection in the dental operatory can occur through several routes. These include direct contact (blood, oral fluids, or other secretions), indirect contact (contaminated instruments, operatory equipment, or environmental surfaces), and contact with airborne contaminants present in droplet spatter or in aerosols of oral and respiratory fluids. For infection to occur via any of these routes, the “chain of infection” must be present. This includes a susceptible host, a pathogen with sufficient infectivity and numbers to cause infection, and a portal through which the pathogen may enter the host. For infection control procedures to be effective, one or more of these “links” in the chain must be broken.
Studies from the CDC report that clothing exposed to the acquired immunodeficiency syndrome (AIDS) virus may be safely used after a normal laundry cycle. A high-temperature (140° F to 160° F, 60° C to 70 °C) wash cycle with normal bleach concentrations, followed by machine drying (212° F, 100° C, or higher), is preferable if clothing is visibly soiled with blood or other body fluids. Dry cleaning and steam pressing will also kill the AIDS virus, according to these studies. Patients with oral lesions suggestive of infectious disease and patients with a known history of hepatitis B, AIDS, AIDS-related complex, or other infectious diseases should be referred for appropriate medical care. In addition to environmental surface and equipment disinfection, all instruments, stones, burs, and other reusable items should be disinfected in 2% glutaraldehyde for 10 minutes, cleaned of debris, rinsed, and patted dry before the sterilizing process is initiated. Heat-sensitive items can be sterilized with the use of ethylene oxide (gas).
For items that have been used in the mouth, including laboratory materials (e.g., impressions, bite registrations, fixed and removable prostheses, orthodontic appliances), cleaning and disinfection are required before they are manipulated in the laboratory (whether on-site or at a remote location). Any item manipulated in the laboratory should also be cleaned and disinfected before placement in the patient’s mouth. Fresh pumice with iodophor should be used for each polishing procedure, and the pumice pan should be washed, rinsed, and dried after each procedure. Because materials are constantly evolving, DHCWs are advised to follow manufacturers’ suggested procedures for specific materials relative to disinfection procedures. As a guide, use of a chemical germicide that has at least an intermediate level of activity (i.e., “tuberculocidal hospital disinfectant”) is appropriate for such disinfection. Careful communication between dental office and dental laboratory regarding the specific protocol for handling and decontamination of supplies and materials is important to prevent any cross contamination.
Differential Diagnosis: Fixed or Removable Partial Dentures
Total oral rehabilitation (disease management, defective tooth restoration, and tooth replacement) is an objective in treating the partially edentulous patient. Although replacement of missing teeth by means of fixed partial dentures, either tooth or implant supported, is generally the method of choice, there are many reasons why a removable partial denture may be the better method of treatment for a specific patient.
The dentist must follow the best procedure for the welfare of the patient, who is always free to seek more than one opinion. Ultimately, the choice of treatment must meet the economic limitations and personal desires of the patient. The exception to this guideline is the Class III arch with a modification space on the opposite side of the arch, which will provide better cross-arch stabilization and a simpler design for the removable partial denture (Figure 12-20).
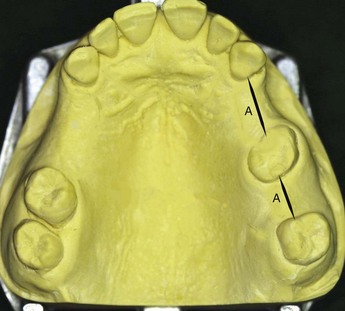
Figure 12-20 Class III, modification 2 arch, in which modification spaces on the patient’s left (spaces designated at A) will be included in the design of the removable partial denture rather than restored with a long-span fixed partial denture. The design for a removable restoration is greatly simplified, resulting in significantly enhanced stability.
Although uncommon, unilateral tooth loss is sometimes inappropriately treated with a unilateral removable partial denture in place of a fixed partial denture. This type of prosthesis is not enhanced by cross-arch stabilization and places excessive stress on abutment teeth. Possibly more important, the risk for aspiration is significant if such a prosthesis is dislodged during use. For these reasons, use of the unilateral removable partial denture is strongly discouraged.
Indications for Use of Fixed Restorations
Tooth-Bounded Edentulous Regions
Generally any unilateral edentulous space bounded by teeth suitable for use as abutments should be restored with a fixed partial denture cemented to one or more abutment teeth at either end. The length of the span and the periodontal support of the abutment teeth will determine the number of abutments required. As was mentioned earlier, such a span could be managed with the use of dental implants if deemed feasible and elected by the patient. The fact that implant support does not place additional functional demands on adjacent teeth likely contributes to their preservation, although this has not been universally demonstrated.
For conventional fixed prostheses, lack of parallelism of the abutment teeth may be counteracted with copings or locking connectors to provide parallel sectional placement. Sound abutment teeth make possible the use of more conservative retainers, such as partial-veneer crowns, or resin-bonded-to-metal restorations, rather than full crowns. The age of the patient, evidence of caries activity, oral hygiene habits, and the soundness of remaining tooth structure must be considered in any decision to use less than full coverage for abutment teeth.
Two specific contraindications for the use of unilateral fixed restorations are known. One is a long edentulous span with abutment teeth that would not be able to withstand the trauma of nonaxial occlusal forces. The other is abutment teeth, which exhibit reduced periodontal support due to periodontal disease, which would benefit from cross-arch stabilization. In either situation, a bilateral removable restoration can be used more effectively to replace the missing teeth.
Modification Spaces
A removable partial denture for a Class III arch is better supported and stabilized when a modification area on the opposite side of the arch is present. A fixed partial denture need not be used to restore such an edentulous area because its inclusion may simplify the design of the removable partial denture. However, when a modification space is bound by a lone-standing single-rooted abutment, it is better restored by means of a fixed partial denture. This acts to stabilize the at-risk tooth, and the denture is made less complicated by not having to include other abutment teeth for the support and retention of an additional edentulous space or spaces.
When an edentulous space that is a modification of a Class I or Class II arch exists anterior to a lone-standing abutment tooth, this tooth is subjected to trauma by the movements of a distal extension removable partial denture far in excess of its ability to withstand such stresses. The splinting of the lone abutment to the nearest tooth is mandatory. The abutment crowns should be contoured for support and retention of the removable partial denture; in addition, a means of supporting a stabilizing component on the anterior abutment of the fixed partial denture or on the occlusal surface of the pontic usually should be provided.
Anterior Modification Spaces
Usually any missing anterior teeth in a partially edentulous arch, except in a Kennedy Class IV arch in which only anterior teeth are missing, are best replaced by means of a fixed restoration. There are exceptions. Sometimes a better esthetic result is obtainable when the anterior replacements are supplied by a removable partial denture, at other times treatment is simplified by inclusion of an anterior modification space into the removable partial denture (Figure 12-21). This is also true when excessive tissue and bone resorption necessitates placement of the pontics in a fixed partial denture too far palatally for good esthetics or for an acceptable relation with the opposing teeth. However, in most instances, from mechanical and biological standpoints, anterior replacements are best accomplished with fixed restorations. The replacement of missing posterior teeth with a removable partial denture is then made much less complicated and gives more satisfactory results.
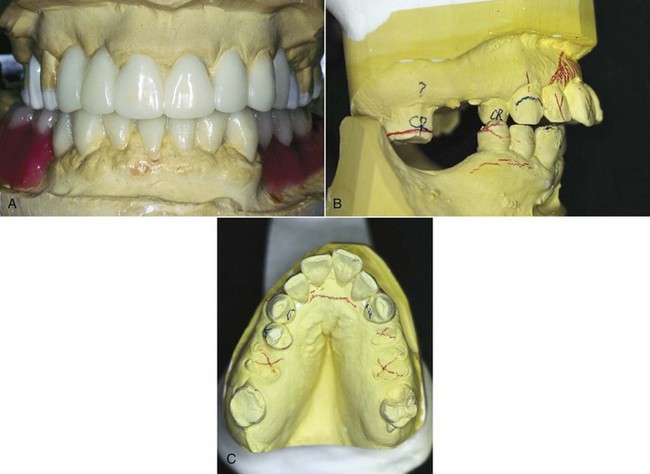
Figure 12-21 A, Diagnostic waxing of this complex case revealed the best means to manage replacement of tooth #’s 6 and 7 was with a fixed prosthesis, especially since the ridge defect was not severe and the adjacent teeth offered good retainer support. B, In contrast, this complex situation requires the maxillary anterior to be repositioned palatally to address an esthetic concern caused by the condition of the maxillary canines and the need to replace the posterior teeth as well. C, The anterior teeth will be more easily managed as part of the removable partial denture.
(Courtesy Dr. M. Alfaro, Columbus, OH.)
Replacement of Unilaterally Missing Molars (Shortened Dental Arch)
Often the decision must be made to replace unilaterally missing molars (Figure 12-22). The decision must balance the impact of the treatment on the remaining oral structures with the potential benefit to the patient long term. To restore the missing molars with a fixed partial denture would require a cantilever prosthesis or the use of dental implants. A cantilever-fixed prosthesis is most applicable if the second molar is to be ignored, then only first molar occlusion need be supplied with the use of a cantilever-type fixed partial denture. Occlusion need be only minimal to maintain occlusal relations between the natural first molar in the one arch and the prosthetic molar in the opposite arch. The cantilevered pontic should be narrow buccolingually and need not occlude with more than one half to two thirds of the opposing tooth. Often such a restoration is the preferred method of treatment. However, at least two abutments should be used to support a cantilevered molar opposed by a natural molar.
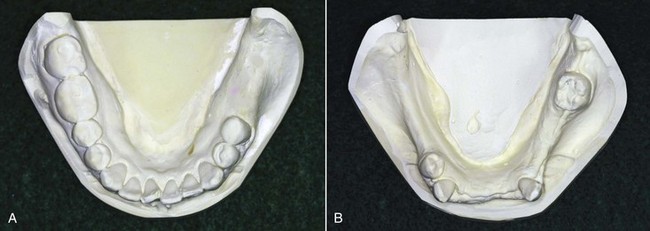
Figure 12-22 A, Unilaterally missing molars. If the patient exhibits opposing contacts to the remaining six posterior teeth (bilateral premolars, right first and second molars), functional gain attained by replacing the left molars may be minimal. B, By contrast, the functional gain resulting from replacement of the posterior occlusion in this patient is likely significant.
To replace unilaterally missing molars with a removable partial denture necessitates the use of a distal extension prosthesis. This involves the major connector joining the edentulous side to retentive and stabilizing components located on the non-edentulous side of the arch. Leverage factors are frequently unfavorable, and the retainers used on the non-edentulous side are often unsatisfactory. Two factors important to consider in making the decision to provide a unilateral, distal extension removable partial denture include the opposing teeth and the future effect of the maxillary tuberosity.
First, the opposing teeth must be considered if it is considered important to prevent extrusion and migration. This influences replacement of the missing molars far more than any improvement in masticating efficiency that might result. Replacement of missing molars on one side is seldom necessary for reasons of mastication alone.
Second, the future effect of a maxillary tuberosity must be considered if concern exists for tuberosity enlargement. Often when left uncovered, the tuberosity increases in size, making future occlusal treatment difficult. However, covering the tuberosity with a removable partial denture base, in combination with the stimulating effect of the intermittent occlusion, helps maintain tuberosity size and position. In such an instance, it may be better to make a removable partial denture with cross-arch stabilization and retention than to leave a maxillary tuberosity uncovered.
Indications for Removable Partial Dentures
Although a removable partial denture should be considered only when a fixed restoration is contraindicated, there are several specific indications for the use of a removable restoration.
Distal Extension Situations
Replacement of missing posterior teeth is often best accomplished with a removable partial denture (see Figure 12-22B), especially when implant treatment is not feasible for the patient. The exception to this includes situations in which the replacement of missing second (and third) molars is inadvisable or unnecessary, or in which unilateral replacement of a missing first molar can be accomplished by means of a multiple-abutment cantilevered fixed restoration or an implant-supported prosthesis. The most common partially edentulous situations are the Kennedy Class I and Class II. With the latter, an edentulous space on the opposite side of the arch is often conveniently present to aid in required retention and stabilization of the removable partial denture. If no space is present, selected abutment teeth can be modified to accommodate appropriate clasp assemblies, or intracoronal retainers can be used. As was previously stated, all other edentulous areas are best replaced with fixed partial dentures.
After Recent Extractions
The replacement of teeth after recent extractions often cannot be accomplished satisfactorily with a fixed restoration. When relining will be required later, or when a fixed restoration using natural teeth or implants will be constructed later, a temporary removable partial denture can be used. If an all-resin denture is used rather than a cast framework removable partial denture, the immediate cost to the patient is much less, and the resin denture lends itself best to future temporary modifications, including those required after implant placement and before restoration.
Tissue changes are inevitable following extractions. Tooth-bounded edentulous areas (as a result of extractions) are best initially restored with removable partial dentures. Relining of a tooth-supported resin denture base is then possible. This is usually done to improve esthetics, oral cleanliness, or patient comfort. Support for such a restoration is supplied by occlusal rests on the abutment teeth at each end of the edentulous space.
Long Span
A long span may be totally tooth supported if the abutments and the means of transferring the support to the denture are adequate, and if the denture framework is rigid. There is little if any difference between the support afforded a removable partial denture and that afforded a fixed restoration by the adjacent abutment teeth. However, in the absence of cross-arch stabilization, the torque and leverage on the two abutment teeth would be excessive. Instead, a removable denture that derives retention, support, and stabilization from abutment teeth on the opposite side of the arch is indicated as the logical means of replacing the missing teeth.
Need for Effect of Bilateral Stabilization
In a mouth weakened by periodontal disease, a fixed restoration may jeopardize the future of the involved abutment teeth unless the splinting effect of multiple abutments is used. The removable partial denture, on the other hand, may act as a periodontal splint through its effective cross-arch stabilizing of teeth weakened by periodontal disease. When abutment teeth throughout the arch are properly prepared and restored, the beneficial effect of a removable partial denture can be far greater than that of a unilateral fixed partial denture.
Excessive Loss of Residual Bone
The pontic of a fixed partial denture must be correctly related to the residual ridge and in such a manner that the contact with the mucosa is minimal. Whenever excessive resorption has occurred, teeth supported by a denture base may be arranged in a more acceptable buccolingual position than is possible with a fixed partial denture (Figure 12-23).
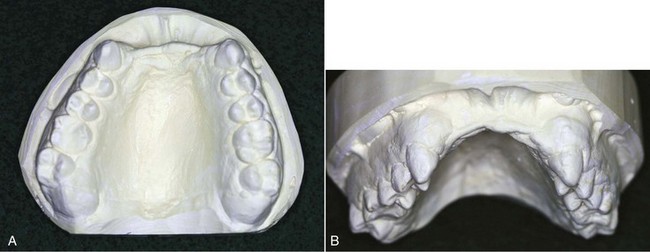
Figure 12-23 A, Occlusal view of the anterior ridge defect (Kennedy Class IV) shows the palatal position of the ridge crest. Incisal edges of opposing dentition require a more labial position, which would create a difficult pontic form. B, Labial view of the same cast shows the significance of the vertical bone loss. Replacement of the teeth and ridge anatomy is best accomplished with a removable partial denture.
Unlike a fixed partial denture, the artificial teeth supported by a denture base can be located without regard for the crest of the residual ridge and more nearly in the position of the natural dentition for normal tongue and cheek contacts. This is particularly true of a maxillary denture.
Anteriorly, loss of residual bone occurs from the labial aspect. Often the incisive papilla lies at the crest of the residual ridge. Because the central incisors are normally located anterior to this landmark, any other location of artificial central incisors is unnatural. An anterior fixed partial denture made for such a mouth will have pontics resting on the labial aspect of this resorbed ridge and will be too far lingual to provide desirable lip support. Often the only way the incisal edges of the pontics can be made to occlude with the opposing lower anterior teeth is to use a labial inclination that is excessive and unnatural, and both esthetics and lip support suffer. Because the same condition exists with a removable partial denture in which the anterior teeth are abutted on the residual ridge, a labial flange must be used to permit the teeth to be located closer to their natural position.
The same method of treatment applies to the replacement of missing mandibular anterior teeth. Sometimes a mandibular anterior fixed partial denture is made six or more units in length, in which the remaining space necessitates leaving out one anterior tooth or using the original number of teeth but with all of them too narrow for esthetics. In either instance, the denture is nearly in a straight line because the pontics follow the form of the resorbed ridge. A removable partial denture will permit the location of the replaced teeth in a favorable relation to the lip and opposing dentition regardless of the shape of the residual ridge. When such a removable prosthesis is made, however, positive support must be obtained from the adjacent abutments.
Unusually Sound Abutment Teeth
Sometimes the reasoning for making a removable restoration is the desire to see sound teeth preserved in their natural state and not prepared for restorations. As was mentioned previously, if this decision is made because it is felt that no tooth modification is necessary for removable partial dentures, then the prosthesis will lack tooth-derived stability and support.
When this condition exists, the dentist should not hesitate to reshape and modify existing enamel surfaces to provide proximal guiding planes, occlusal rest areas, optimum retentive areas, and surfaces on which nonretentive stabilizing components may be placed. Continued durability of the natural teeth is best ensured if the modifications that optimize prosthesis function are provided. This is due to the fact that such modifications also ensure the most harmonious use of the natural dentition.
Abutments With Guarded Prognoses
If the prognosis of an abutment tooth is questionable or if it becomes unfavorable while under treatment, it might be possible to compensate for its impending loss by a change in denture design. The questionable or condemned tooth or teeth may then be included in the original design and, if subsequently lost, the removable partial denture can be modified or remade (Figure 12-24). Most removable partial denture designs do not lend themselves well to later additions, although this eventuality should be considered in the design of the denture.

Figure 12-24 Kennedy Class II, modification 1, where the molar abutment has a guarded prognosis. A, Anterior abutment of the modification space has a clasp assembly that accommodates for potential future loss of the distal molar while currently providing adequate support, stability, and retention. B, Premolar clasp assembly comprises a mesial rest, a distal guide plane, and a wrought-wire retainer design, which will accommodate future distal extension movement. C, Buccal view shows guide-plane contact and a wrought-wire location that is appropriate for a distal extension.
When the tooth in question will be used as an abutment, every diagnostic aid should be used to determine its prognosis as a prospective abutment. It is usually not as difficult to add a tooth or teeth to a removable partial denture as it is to add a retaining unit when the original abutment is lost and the next adjacent tooth must be used for that purpose.
It is sometimes possible to design a removable partial denture so that a single posterior abutment, about which there is some doubt, can be retained and used at one end of the tooth-supported base. Then if the posterior abutment is lost, it could be replaced by adding an extension base to the existing denture framework. Such an original design must include provisions for future indirect retention, flexible clasping of the future abutment, and provisions for establishing tissue support. Anterior abutments that are considered poor risks may not be so freely used because of the problems involved in adding a new abutment retainer when the original one is lost. It is rational that such questionable teeth should be condemned in favor of more suitable abutments, even though the original treatment plan must be modified accordingly.
Economic Considerations
Economics should not be the sole criterion used to arrive at a method of treatment. When, for economic reasons, complete treatment is out of the question and yet replacement of missing teeth is indicated, the restorative procedures dictated by these considerations must be described clearly to the patient as a compromise and not as representative of the best that modern dentistry has to offer. A prosthesis that is made to satisfy economic considerations alone may provide only limited success and result in more costly treatment in the future.
Choice Between Complete Dentures and Removable Partial Dentures
One of the more difficult decisions to make for the partially edentulous patient involves making the choice of a complete denture over a removable partial denture. Many factors need to be considered when one is making such a decision; these generally fall under the categories of tooth-related factors, factors of comparative functional expectations between prostheses, and patient-specific factors. Because the difference between a tooth-tissue–born prosthesis and a tissue-born prosthesis can be significant, especially since it is difficult for the partially edentulous patient to conceptualize the tissue-born situation, such an irreversible decision is not trivial.
An evaluation of the remaining teeth will determine whether any caries or periodontal disease exists. The decision as to whether a tooth is useful for inclusion in a prosthetic treatment plan can be made on the basis of an understanding that with appropriate disease management, the tooth provides a reasonable 5-year prognosis for survival. This takes into account the added functional demand by the prosthesis and a risk assessment for recurrent disease. Because this scenario concerns teeth with disease, the expectation is that tooth structure and/or support is compromised. The added functional burden, along with a potentially increased risk for disease, is an important concern when one is determining the long-term benefit for retaining teeth with a removable partial denture.
If the teeth can be maintained with a reasonable prognosis, the next questions to ask are “Do they require restoration with surveyed crowns?” and “How much improvement to the prosthesis support, stability, and retention do they provide?” If the expected prognosis for a given tooth is questionable, the costs associated with restoration high, and the added benefit to the prosthesis low, the tooth should likely not be maintained unless the patient strongly desires to maintain all teeth. However, if the same scenario exists and the long-term impact on the support, stability, and retention of the prosthesis is great, the decision strongly favors keeping the tooth.
The question of whether retained teeth offer a significant advantage to the prosthesis from a support, stability, and retention standpoint requires comparative evaluation of potential denture-bearing foundations. If the expectation is that an edentulous arch would have unfavorable physical features (poor ridge form, poor arch configuration, displaceable mucosa, high frena attachments, minimum denture bearing area, and/or an unfavorable jaw relationship), then retention of teeth is likely to provide a more significant benefit. If retention of teeth can help to prevent or delay age-related denture-bearing foundation changes seen with complete denture use, then retention of teeth can be of significant benefit.
When evaluation demonstrates that the remaining teeth have no active disease, then the often-negative impact of disease management on prognosis is not a concern. The decision to maintain teeth is again based on risk assessment, costs for use of the teeth, added benefit to prosthesis functional stability, and comparative functional expectations between a mucosal-borne denture and a removable partial denture that uses teeth for some support, stability, and retention.
The remaining tooth location and distribution can also affect the decision to maintain teeth. It makes a difference whether the remaining teeth are located on only one side of the arch. Having bilateral teeth remaining, especially if they are in similar locations (canines-canines, canines/premolars-canines/premolars), offers advantages for prosthesis design and occlusal development compared with asymmetrical tooth locations. Some teeth may not serve well as a stabilizing component for a removable partial denture and should not be maintained. If the remaining terminal tooth adjacent to a distal extension base is an incisor, the likelihood of long-term support, stability, and retention is poor.
An additional factor for consideration when one is deciding between a complete denture and a removable partial denture is whether there is a strong patient desire to maintain teeth. As was mentioned previously, because the change to a complete denture is a significant transformation, sufficient discussion must take place before this decision is made. The dentist must be very clear that the patient understands the functional differences between a mucosal-borne prosthesis for all aspects of function (i.e., chewing, talking, etc.) and the natural dentition or a removable partial denture.
The uniqueness of the patient is again appreciated these issues are discussed with the patient. One patient may prefer complete dentures rather than complete oral rehabilitation, regardless of ability to pay. Another may be so determined to keep his own teeth that he will make great financial sacrifice if given a reasonable assurance of success of oral rehabilitation. Listening to the patient during the examination and the diagnostic procedures pays off significantly when the treatment options differ so vastly as complete and removable partial dentures often do. During the presentation of pertinent facts, time should be allowed for patients to express themselves freely as to their desires in retaining and restoring their natural teeth. At this time, a treatment plan may be influenced or even drastically changed to conform to the expressed and implied wishes of the patient. For example, there may be a reasonable possibility of saving teeth in both arches through the use of removable partial dentures. With only anterior teeth remaining, a removable partial denture can be made to replace the posterior teeth with the use of good abutment support and, in the maxillary arch, use of full palatal coverage for retention and stability. If patients express a desire to retain their anterior teeth at any cost, and if the remaining teeth are esthetically acceptable and functionally sound, the dentist should make every effort to provide successful treatment. If patients prefer a mandibular removable partial denture because of fear of difficulty in wearing a mandibular complete denture, then, all factors being acceptable, their wishes should be respected and treatment should be planned accordingly. The professional obligation to present the facts and then do the best that can be done in accordance with the patients’ expressed desires still applies.
Other patients may wish to retain remaining teeth for an indefinite but relatively short period of time, with eventual complete dentures a foregone conclusion. In this instance, the professional obligation may be to recommend interim removable partial dentures without extensive mouth preparation. Such dentures will aid in mastication and will provide esthetic replacements, at the same time serving as conditioning restorations, which will make the later transition to complete dentures somewhat easier. Such removable partial dentures should be designed and fabricated with care, but the total cost of removable partial denture service should be considerably less.
An expressed desire on the part of patients to retain only six mandibular anterior teeth must be considered carefully before this is agreed to as the planned treatment. The advantages for patients are obvious: they may retain six esthetically acceptable teeth; they do not become totally edentulous; and they have the advantages of direct retention for the removable partial denture that would not be possible if they were completely edentulous. Retaining even the mandibular canine teeth would accomplish the latter two objectives. Potential disadvantages relate directly to the patient keeping up with prosthesis maintenance procedures. The disadvantages relate to the poor response of the anterior maxilla to functional stress concentrated from the opposing natural dentition. If the functional forces of occlusion are not well distributed, the natural anterior can concentrate stress to the anterior maxillary arch. The possible result of such poorly distributed functional force includes the loss of residual maxillary bone, loosening of the maxillary denture caused by the tripping influence of the natural mandibular teeth, and loss of the basal foundation for the support of future prostheses. However, if the maxillary anterior teeth are arranged to contact in balanced eccentric positions and if patients comply with periodic recall to maintain these relationships, these problems are minimized. Prevention of this sequence of events lies in the maintenance of positive occlusal support posteriorly and the continual elimination of traumatic influence from the remaining anterior teeth. Such support is sometimes impossible to maintain without frequent relining or remaking of the lower removable partial denture base. The presence of inflamed hyperplastic tissue is a frequent sequela to continued loss of support and denture movement.
Although some patients are able to successfully function with a lower removable partial denture supported only by anterior teeth against a complete maxillary denture, it is likely that undesirable consequences will result unless the patient faithfully follows the instructions of the dentist. In no other situation in treatment planning are the general health of the patient and the quality of residual alveolar bone as critical as they are in this situation.
Clinical Factors Related to Metal Alloys Used for Removable Partial Denture Frameworks
The cast framework offers significant advantages over the all acrylic-resin removable partial denture. In general, the ability to predictably utilize the remaining teeth for support, stability, and retention over time is best assured when the interface between prosthesis and teeth consists of a cast structure and not a polymer. Although the utility of all acrylic-resin prostheses can be extended if wire “rests” are provided, typical polymer properties do not allow for a durable interface, which is required if one is to take advantage of the stabilizing effects of tooth contact. Expectations of how the metal framework improves functional performance are related to the properties of the metal alloy. Various alloys can be considered for use. Following is a discussion of the most common framework alloys in use today.
Practically all cast frameworks for removable partial dentures are made from a chromium-cobalt (Cr-Co) alloy. The popularity of Cr-Co alloys has been attributed to their low density (weight), high modulus of elasticity (stiffness), low material cost, and resistance to tarnish. The term stellite alloy historically has referred to this class of alloy. Today the more common alloys contain 60% to 63% Co, 29% to 31.5% Cr, and 5% to 6% Mo, with the balance including Si, Mn, Fe, N, and C. The addition of controlled amounts of nitrogen (<.5%) is reported to improve physical properties. Titanium is also used as a removable partial denture (RPD) frame material; however, production difficulties continue to hinder its widespread use. The dentist should become familiar with the alloy used by her/his laboratory and should closely monitor fit, density, and rigidity.
The following are comparable characteristics of gold alloys and chromium-cobalt alloys: (1) each is well tolerated by oral tissues; (2) they are equally acceptable esthetically; (3) enamel abrasion by either alloy is insignificant on vertical tooth surfaces; (4) a low-fusing chrome-cobalt alloy or gold alloy can be cast to wrought wire, and wrought-wire components may be soldered to either gold or chrome-cobalt alloys (these characteristics are important in overcoming the objection by some dentists to the increased stiffness of chromium-cobalt alloys for the portions of direct retainers that must engage an undercut of the abutment tooth); (5) the accuracy obtainable in casting either alloy is clinically acceptable under strictly controlled investing and casting procedures; and (6) soldering procedures for the repair of frameworks can be performed on each alloy.
Comparative Physical Properties of Gold and Chromium-Cobalt
Chromium-cobalt alloys generally have less yield strength when compared with gold alloys used for removable partial dentures. Yield strength is the greatest amount of stress an alloy will withstand and still return to its original shape in an unweakened condition. Possessing a lower proportional limit, the chromium-cobalt alloys will deform permanently at lower loads than gold alloys. Therefore the dentist must design the chromium-cobalt framework so that the degree of deformation expected in a direct retainer is less than a comparable degree of deformation for a gold component. The modulus of elasticity refers to the stiffness of an alloy. Gold alloys have a modulus of elasticity approximately one-half that for chromium-cobalt alloys for similar uses. The greater stiffness of the chromium-cobalt alloy is advantageous but at the same time offers disadvantages. Greater rigidity can be obtained with the chromium-cobalt alloy in reduced sections in which cross-arch stabilization is required, thereby eliminating an appreciable bulk of the framework. Its greater rigidity is also an advantage when the greatest undercut that can be found on an abutment tooth is in the nature of 0.05 inch. A gold retentive element would not be as efficient in retaining the restoration under such conditions as would the chromium-cobalt clasp arm.
A high yield strength and a low modulus of elasticity produce greater flexibility. The gold alloys are approximately twice as flexible as the chromium-cobalt alloys; in many instances, this provides a distinct advantage in the optimum location of retentive elements of the framework. The greater flexibility of the gold alloys usually permits location of the tips of retainer arms in the gingival third of the abutment tooth. The stiffness of chromium-cobalt alloys can be overcome by including wrought-wire retentive elements in the framework.
The bulk of a retentive clasp arm for a removable partial denture is often reduced for greater flexibility when chromium-cobalt alloys are used as opposed to gold alloys. This, however, is inadvisable because the grain size of chromium-cobalt alloys is usually larger and is associated with a lower proportional limit, and so a decrease in the bulk of chromium-cobalt cast clasps increases the likelihood of fracture or permanent deformation. The retentive clasp arms for both alloys should be approximately the same size, but the depth of undercut used for retention must be reduced by one half when chromium-cobalt is the choice of alloys. Chromium-cobalt alloys are reported to work/harden more rapidly than gold alloys, and this, associated with coarse grain size, may lead to failure in service. When adjustments by bending are necessary, they must be executed with extreme caution and limited optimism.
Chromium-cobalt alloys have a lower density (weight) than gold alloys in comparable sections and therefore are about one half as heavy as gold alloys. The weight of the alloy in most instances is not a valid criterion for selection of one metal over another because after placement of a removable partial denture, the patient seldom notices the weight of the restoration. The comparable lightness of chromium-cobalt alloys, however, is an advantage when full palatal coverage is indicated for the bilateral distal extension removable partial denture. Weight is a factor that must be considered when the force of gravity must be overcome, so that usually passive direct retainers will not be activated constantly to the detriment of abutment teeth.
The hardness of chromium-cobalt alloys presents a disadvantage when a component of the framework, such as a rest, is opposed by a natural tooth or by one that has been restored. We have observed more wear of natural teeth opposed by some of the various chromium-cobalt alloys as contrasted with type IV gold alloys.
It has been observed that gold frameworks for removable partial dentures are more prone to produce uncomfortable galvanic shock to abutment teeth restored with silver amalgam than are frameworks made of chromium-cobalt alloy. This may not be a valid criterion for the selection of a particular alloy when the dentist has complete control over the choice of restorative materials.
Commercially pure (CP) titanium and titanium in alloys containing aluminum and vanadium, or palladium (Ti-O Pd), should be considered potential future materials for removable partial denture frameworks. Their versatility and well-known biocompatibility are promising; however, long-term clinical trials are needed to validate their potential usefulness. Currently, when CP titanium is cast under dental conditions, the material properties change dramatically. During the casting procedure, the high affinity of the liquid metal for elements such as oxygen, nitrogen, and hydrogen results in their incorporation from the atmosphere. As interstitial alloying elements, their deleterious effect on mechanical properties is a problem. Also, reactions between molten titanium metal and the investment refractory produce gases, which cause porosity. With alpha-beta alloys, such as Ti-6Al-4V, a surface skin of alpha titanium can form (alpha-case zone), which has a tremendous effect on electrochemical behavior and mechanical properties. This could be important for small thin structures, such as clasp assemblies and major and minor connectors. The CP grades of titanium have yield strengths that are too low for clinical use as clasps (450 MPa minimum), although the ductility is high. The much higher yield strengths of the Ti-6Al-4V alloys are the same as that of a typical bench-cooled cobalt-chromium alloy, but with far superior ductility. The typical Young’s modulus of elasticity of titanium alloy is half that of cobalt-chromium and just slightly higher than that of type IV gold alloys. This would require a different approach to clasp design than is used with cobalt-chromium alloys, and would present some advantages. Wrought titanium alloy wires are also flexible because of the same low elastic modulus. Beta alloys, which are used in orthodontics, have two-thirds the elastic modulus of CP titanium and Ti-6Al-4V. The joining of titanium by brazing is a problem because like-casting inert atmospheres must be used. The corrosion and fatigue behavior of brazed joints has yet to be tested for long-term corrosion resistance and clinical efficacy. Clinical use has demonstrated reasonable short-term results, but laboratory fabrication difficulties need to be addressed, and long-term advantages over existing alloys must be demonstrated before titanium will gain broad clinical use.
Wrought Wire: Selection and Quality Control
Wrought-wire direct retainer arms may be attached to the restoration by embedding a portion of the wire in a resin denture base, by soldering to the fabricated framework, or by casting the framework to a wire embedded in the wax pattern (Figure 12-25). The physical (mechanical) properties of available wrought wires are most important considerations when a proper wire for the desired method of attachment is selected. These properties include yield strength or proportional limit, percentage elongation, tensile strength, and fusion temperature. After the wire is selected, the procedures to which the wire is subjected in fabricating the restoration become critical. Improper laboratory procedures can diminish certain desirable physical properties of the wrought structure, rendering it relatively useless for its intended purpose. For example, when wrought wire is heated, as in a cast-to or soldering procedure, its physical properties and microstructure may be considerably altered, depending on temperature, heating time, and cooling operation. All manufacturers of wrought forms for dental applications furnish charts listing their products and the physical properties of each product. The percentage of noble metals is given. In addition, most manufacturers designate wires that may be used in a cast-to procedure. American Dental Association (ADA) Specification No. 7 addresses itself to wrought gold wire in terms of both content and minimum physical properties (Table 12-1).

Figure 12-25 The wrought-wire retainer arm has been contoured to design and incorporated into the wax pattern of this frame, where it will become an integral part of the framework. The wire is contoured in two planes and will be mechanically retained in the casting.
Table 12-1 Comparative Specifications Contained in ADA Specification No. 7
| Type I | Type II | |
|---|---|---|
| Content of metals of the gold, platinum group (minimum) | 75% | 65% |
| Minimum fusion temperature | 1742° F | 1898°F |
| Minimum yield point value (hardened or oven cooled) | 125,000 psi | 95,000 psi |
| Minimum elongation (hardened) | 4% | 2% |
| Minimum elongation (softened) | 15% | 15% |
ADA, American Dental Association.
The tensile strength of the wrought structure is approximately 25% greater than that of the cast alloy from which it was made. The wrought structure’s hardness and strength are also greater. This means that a wrought structure that has a smaller cross section than a cast structure may be used as a retainer arm (retentive) to perform the same function. It has been suggested that a minimum yield strength of 60,000 psi is required for the retentive element of a direct retainer. A percentage elongation of less than 6% is indicative that a wrought wire may not be amenable to contouring without attendant undesirable changes in microstructure.
Regardless of the method of attaching the wrought-wire retainer that is used, that is, embedding, soldering, or cast-to, tapering the wrought arm seems most rational. A retainer arm is in essence a cantilever that can be made more serviceable and efficient by tapering. Tapering to 0.8 mm permits more uniform distribution of service stresses throughout the length of the arm, being readily demonstrated by photoelastic stress analysis. Uniform tapering of an 18-gauge, round wire arm can be accomplished by rapidly rotating the wire in angled contact with an abrasive disk in the dental lathe. It is then polished by rotating the wire in angled contact with a mildly abrasive rubber disk in the dental lathe. The appropriate taper is shown in Figure 12-26.
Summary
In selecting materials, it must be remembered that fundamentals do not change. These are inviolable. It is only methods, procedures, and substances—by which the dentist effects the best possible end result—that change. The responsibility of the decision still rests with the dentist, who must evaluate all factors in relation to the results desired. In any instance therefore, the dentist must weigh the problems involved, compare and evaluate the characteristics of different potential materials, and then make a decision that leads to delivery of the greatest possible service to the patient.