Visual Impairment
Visual impairment is a common problem during childhood. In North America the prevalence of serious visual impairment in the pediatric population is estimated to be between 30 and 64 children per 100,000 population. Visual impairment such as refractive error, amblyopia, strabismus, and astigmatism affects 5% to 10% of all preschoolers (Tingley, 2007). Early detection and prompt treatment of ocular disorders in children are important to avoid lifelong visual impairment. The nurse’s role is one of assessment, detection, prevention, referral, and, in some instances, rehabilitation.
Definition and Classification
Visual impairment has many causes and may be due to multiple defects affecting any structure or function along the visual pathways (Olitsky, Hug, and Smith, 2007a). Legal blindness is defined as a visual acuity of 20/200 or lower or a visual field of 20 degrees or less in the better eye. Partial sight is defined as a visual acuity of better than 20/200 but worse than 20/70 in the better eye with correction. These children can generally use normal-sized print, since near vision is nearly always better than distance vision. Visual impairment is a general term that includes both these categories. Children who are visually impaired, including those who are legally blind, often have considerable useful vision and are able to use printed material, such as large-print books, as their major method of learning. It is important to keep in mind that legal blindness is not a medical diagnosis but a legal definition. Educational and governmental agencies in the United States use the legal definition of blindness to determine tax status, eligibility for entrance into special schools, and eligibility for financial aid and other benefits.
Etiology
A number of genetic and prenatal or postnatal conditions can cause visual impairment. These include perinatal infections (herpes, chlamydial infection, gonorrhea, rubella, syphilis, or toxoplasmosis); retinopathy of prematurity; trauma; postnatal infections (meningitis); and disorders such as sickle cell disease, juvenile rheumatoid arthritis, Tay-Sachs disease, albinism, and retinoblastoma. In many instances, such as with refractive errors, the cause of the defect is unknown.
Refractive errors are the most common type of visual disorder in children. The term refraction means bending and refers to the bending of light rays as they pass through the lens of the eye. Normally light rays enter the lens and fall directly on the retina. However, in refractive disorders the light rays fall either in front of the retina (myopia) or beyond it (hyperopia). Other eye problems, such as strabismus, may or may not include refractive errors, but they are important because, if untreated, they result in visual impairment from amblyopia. Box 24-9 summarizes these along with other, less frequent visual disorders. In addition to these disorders, other visual problems can result from infection or trauma.
Trauma: Trauma is a common cause of visual impairment in children. Injuries to the eyeball and adnexa (supporting or accessory structures, such as eyelids, conjunctiva, and lacrimal glands) can be classified as penetrating or nonpenetrating. Penetrating wounds are most often caused by sharp instruments, such as sticks, knives, or scissors; propulsive objects, such as firecrackers, guns, bows and arrows, or slingshots; or a blunt object. Devastating eye injuries have been caused by the popular gas-propulsion paintball guns and air-powered BB guns, used primarily by boys 11 to 15 years of age (Michaud and American Academy of Pediatrics, 2004; Listman, 2004; Olitsky, Hug, and Smith, 2007b). Nonpenetrating injuries may result from foreign objects in the eyes, lacerations, a blow from a blunt object (in baseball, softball, basketball, or racquet sports) or a fist, or thermal or chemical burns.
Treatment is directed toward preventing further ocular damage and is primarily the responsibility of the ophthalmologist. It involves adequate examination of the injured eye (with the child sedated or anesthetized in cases of severe injury); appropriate immediate intervention, such as removal of the foreign body or suturing of the laceration; and prevention of complications, such as administration of antibiotics or steroids and complete bed rest to allow the eye to heal and blood to reabsorb (see Emergency Treatment box). The prognosis varies depending on the type of injury. It is usually guarded in all cases of penetrating wounds because of the high risk of serious complications.
Infections: Infections of the adnexa and the structures of the eyeball or globe are not infrequent in children. The most common eye infection is conjunctivitis. (See Chapter 16.) Treatment is usually with ophthalmic antibiotics. Severe infections may require systemic antibiotic therapy. Steroids are used cautiously because they exacerbate viral infections such as herpes simplex, increasing the risk of damage to the involved structures.
Nursing Care Management
Nursing care of visually impaired children is a specialized area requiring additional training in vision testing and habilitation. However, general measures that focus on assessment, prevention, and rehabilitation of the child with visual impairment are every nurse’s responsibility. In addition, nurses may have to care for a visually impaired child who is hospitalized and must know how to best meet the child’s and family’s special needs.
Assess for Visual Concerns: Assessment of children for visual impairment is a critical nursing responsibility. Discovery of a visual impairment as early as possible is essential to prevent social, physical, and psychologic damage to the child. Assessment involves (1) identifying those children who by virtue of their history are at risk; (2) observing for behaviors that indicate a vision loss; and (3) screening all children for visual acuity and signs of other ocular disorders, such as strabismus. Clinical manifestations of various types of visual problems are listed in Box 24-9. Chapter 6 discusses vision testing.
Infancy: At birth the nurse should observe the neonate’s response to visual stimuli, such as following a light or object and cessation of body movement. The intensity of the response may vary, depending on the infant’s state of alertness.
Of special importance in detecting visual impairment during infancy are parental concerns regarding visual responsiveness in their child. Their concerns, such as lack of eye contact from the infant, must be taken seriously. During infancy the child should be tested for strabismus. Lack of binocularity after 4 months of age is considered abnormal and must be treated to prevent amblyopia.
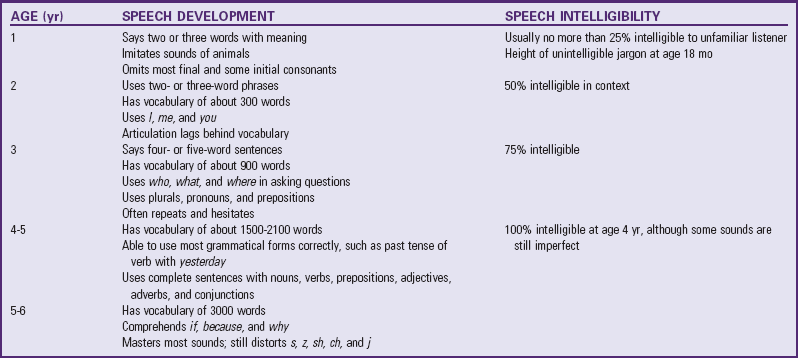
Childhood: Because the most common visual impairment during childhood is refractive error, testing for visual acuity is essential. The school nurse usually assumes major responsibility for vision screening in schoolchildren. In addition to assessing for refractive errors, the nurse should be aware of signs and symptoms that indicate other ocular problems. If the family is given a referral requesting further eye testing, the school nurse is responsible for follow-up concerning the recommendation.
Support the Child and Family: Learning that their child is visually impaired or only partially sighted precipitates an immense crisis for families. Of all types of disabilities, many people fear loss of sight the most. Vision is involved in almost every activity of daily living. Parents need support during the initial phase of learning about the diagnosis and help to gain a realistic understanding of their child’s abilities. Encourage the family to investigate appropriate early intervention and educational programs for their child as soon as possible. Sources of information include state commissions for the blind; local schools for the blind; and the American Foundation for the Blind,* National Federation of the Blind,† National Association for Parents of Children with Visual Impairments,‡ National Association for Visually Handicapped,§ and American Council of the Blind.
With newly acquired visual impairment, children need a great deal of support to help them adjust to the disability. They are usually frightened and confused by the sudden or progressive loss of sight and benefit from an environment that provides security and familiarity.
Promote Parent-Child Attachment: A crucial time in the life of a visually impaired infant is when the infant and its parents are getting acquainted with each other. Pleasurable patterns of interaction between the infant and parents may be lacking if there is not enough reciprocity. For example, if a parent gazes fondly at the infant’s face and seeks eye contact but the infant fails to respond because he or she cannot see the parent, a troubled cycle of responses may occur. The nurse can help parents learn to look for other cues that indicate the infant is responding to them, for example, blinking of the eyelids; acceleration or slowing of the activity level; change in respiratory patterns, such as faster or slower breathing when the parents come near; and production of throaty sounds by the infant when they speak to the infant. In time parents learn that the infant has unique ways of relating to them. Encourage them to show affection using nonvisual methods, such as talking or reading, cuddling, and walking the child.
Promote the Child’s Optimum Development: Promoting the child’s optimum development requires rehabilitation in a number of important areas. These include learning self-help skills and appropriate communication techniques to become independent. Although nurses may not be directly involved in such programs, they can provide direction and guidance to families regarding the availability of programs and the importance of promoting these activities in their child.
Development and Independence: Motor development depends on sight almost as much as verbal communication depends on hearing. Encourage parents to expose the infant with any sight to as many visual-motor experiences as possible from earliest infancy, such as by having the infant sit supported in an infant seat or swing and providing opportunities for holding up the head, sitting unsupported, reaching for objects, and crawling.
Despite visual impairment, a child can become independent in all aspects of self-care. The same principles used for promoting independence in sighted children apply, with additional emphasis given to nonvisual cues. For example, the child may need help in dressing, such as special arrangement of clothing for style coordination and Braille tags to distinguish colors and prints.
The visually impaired child also must learn to become independent in navigation. The two main techniques are the tapping method (use of a cane to survey the environment for direction and to avoid obstacles) and the use of guides, such as a human sighted guide or a dog guide (e.g., a Seeing Eye dog). Partially sighted children may benefit from ocular aids, such as a monocular telescope.
Play and Socialization: Visually impaired children do not learn to play automatically. Because they cannot imitate others or actively explore the environment as sighted children do, they depend much more on others to stimulate them and teach them how to play. Parents need help in selecting appropriate play materials, especially those that encourage fine and gross motor development and stimulate the senses of hearing, touch, and smell. Toys with educational value, such as dolls with various clothing closures, are especially useful.
Visually impaired children have the same needs for socialization as sighted children. Because they have little difficulty learning verbal skills, they are able to communicate with age-mates and participate in suitable activities. The nurse discusses with parents opportunities for socialization outside of the home, especially regular preschools. The trend is to include these children with sighted children to help them adjust to the outside world to promote eventual independence.
To compensate for inadequate stimulation, these children may develop self-stimulatory activities such as body rocking, finger flicking, or arm twirling. Discourage such habits because they delay the child’s social acceptance. Behavior modification is often successful in reducing or eliminating the self-stimulatory activities.
Education: The main obstacle to learning is the child’s total dependence on nonvisual cues. Although the child can learn via verbal lecturing, he or she is unable to read the written word or to write without special education. Therefore the child must rely on Braille, a system that uses raised dots to represent each letter and number. The child can read the Braille with the fingers and can write a message using a small typewriter-like device called a braillewriter. However, this type of communication is not useful for communicating with others unless they read Braille. A more portable system for written communication is the use of a Braille slate and stylus or a microcassette tape recorder. A recorder is especially helpful for leaving messages for others and for taking notes during classroom lectures. For mathematic calculations, portable calculators with voice synthesizers are available.*
Records and tapes are significant sources of reading material other than Braille books, which are large and cumbersome. The Library of Congress† has talking books, Braille books, and a special records program; these materials are available at many local and state libraries and directly from the Library of Congress. The talking book machine and tape player are provided at no cost to families, and there is no postage fee for returning the materials. Recording for the Blind and Dyslexic‡ also provides texts and tapes of books, which are helpful for secondary and college students who are visually impaired.
Learning to use a regular typewriter is another means of writing but has the disadvantage that the visually impaired person is unable to check the accuracy of the typing. Computers eliminate this drawback; a home computer with a voice synthesizer can speak each letter or word that has been typed.
The child with partial sight benefits from specialized visual aids that produce a magnified retinal image. The basic methods are accommodative techniques, such as bringing the object closer; devices such as special plus lenses, handheld and stand magnifiers, telescopes, and video projection systems; and the use of large-print materials. Special equipment is available to enlarge print. Information about services for the partially sighted is available from the National Association for Visually Handicapped and the American Foundation for the Blind. Children with diminished vision often prefer to do close work without their glasses and compensate by bringing the object very near to their eyes. This should be allowed. The exception is the child with vision in only one eye, who should always wear glasses for protection. The National Federation of the Blind* has information on job opportunities for the visually impaired.
Care for the Child During Hospitalization: Because nurses are more likely to care for children who are hospitalized for procedures that involve temporary loss of vision, the following discussion concentrates primarily on the needs of such children. The nursing care objectives in either situation are to (1) reassure the child and family throughout every phase of treatment, (2) orient the child to the surroundings, (3) provide a safe environment, and (4) encourage independence. Whenever possible, the same nurse should care for the child to ensure consistency in the approach. These same principles also apply to caring for any visually impaired child who requires hospitalization.
When sighted children temporarily lose their vision, almost every aspect of the environment becomes bewildering and frightening. They often rely on nonvisual senses for help in adjusting to the visual impairment without the benefit of any special training. Nurses have a major role in minimizing the effects of temporary loss of vision. They need to talk to the child about everything that is occurring, emphasizing aspects of procedures that are felt or heard. They should always identify themselves as soon as they enter the room and before they approach the child. Because unfamiliar sounds are especially frightening, these are explained. Encourage parents to room with their child and participate in the child’s care. A familiar object, such as a teddy bear or doll, from home will help lessen the strangeness of the hospital. As soon as the child is able to be out of bed, orient him or her to the immediate surroundings. If the child is able to see on admission, take this opportunity to point out significant aspects of the room. Encourage the child to practice ambulation with the eyes closed to become accustomed to this experience.
The room is arranged with safety in mind. For example, place a stool or chair next to the bed to help the child climb into and out of bed. The furniture is always placed in the same position to prevent collisions. Remind cleaning personnel of the need to keep the room in order. If the child has difficulty navigating by feeling the walls, attach a rope from the bed to the point of destination, such as the bathroom. Attention to details such as well-fitting slippers and robes that do not hang on the floor is important to prevent tripping. Unlike the child who is visually impaired, these children are not familiar with navigating with a cane.
Encourage the child to be independent in self-care activities, especially if the visual loss may be prolonged or potentially permanent. For example, during bathing, the nurse sets up all the equipment and encourages the child to participate. At mealtime the nurse explains where each food item is on the tray, opens any special containers, and prepares cereal or toast, but encourages the child in self-feeding. Favorite finger foods, such as sandwiches, hamburgers, hot dogs, or pizza, may be good selections. Praise the child for efforts at being cooperative and independent. Any improvements made in self-care, no matter how small, are stressed.
Provide appropriate recreational activities; a child life specialist, if available, can help with planning. Because children with temporary visual loss have a wide variety of play experiences to draw on, they are encouraged to select activities. For example, if they like to read, they may enjoy listening to books on tape or having someone read to them. If they prefer manual activity, they may appreciate playing with clay or building blocks or feeling different textures and naming them. Simple board and card games can be played if the child has a “seeing partner” or if the opponent helps with the game. Children should have familiar toys from home to play with, since familiar items are more easily manipulated than new ones. If parents wish to bring presents, they should be objects that stimulate hearing and touch, such as a radio, music box, or stuffed animal.
Occasionally children who are visual impaired come to the hospital for procedures to restore their vision. Although this is an extremely happy time, intervention is also required to help these children adjust to sight. They need an opportunity to take in all that they see. They should not be bombarded with visual stimuli. They may need to concentrate on people’s faces or their own to become accustomed to this experience. They often need to talk about what they see and to compare the visual images with their mental ones. These children may also go through a period of depression, which must be respected and supported. Encourage them to discuss how it feels to see, especially seeing themselves.
Newly sighted children also need time to adjust to the ability to engage in activities that were impossible before. For example, they may prefer to use Braille to read, rather than learning a new visual approach, because of familiarity with the touch system. Eventually, as they learn to recognize letters and numbers, they will integrate these new skills into reading and writing. However, parents and teachers must be careful not to push them before they are ready. This principle applies to social relationships and physical activities as well as to learning situations.
Assist in Measures to Prevent Visual Impairment: An essential nursing goal is to prevent visual impairment. This involves many of the same interventions discussed under hearing impairment: (1) prenatal screening for pregnant women at risk, such as those with rubella or syphilis infection and family histories of genetic disorders associated with visual loss; (2) adequate prenatal and perinatal care to prevent prematurity and iatrogenic damage from excessive administration of oxygen; (3) periodic screening of all children, especially newborns through preschoolers, for congenital and acquired visual impairments caused by refractive errors, strabismus, and other disorders; (4) rubella immunization of all children; and (5) safety counseling regarding the common causes of ocular trauma. Safety counseling should include instruction regarding safe practices when working with, playing with, or carrying objects such as scissors, knives, and balls.
After detection of eye problems, the nurse should encourage the family to prevent further ocular damage by undertaking corrective treatment. For the child with strabismus, this often necessitates occlusion patching of the stronger eye. Compliance with the procedure is greatest during the early preschool years. It is more difficult to encourage young school-age children to wear the occlusive patch because the poor visual acuity of the uncovered weaker eye interferes with schoolwork and the patch sets them apart from their peers. In school they benefit from being positioned favorably (closer to the chalkboard or primary instructional area) and being allowed extra time to read or complete an assignment. If treatment of the eye disorder requires instillation of ophthalmic medication, teach the family the correct procedure. (See Chapter 27.)
Children who need glasses to correct refractive errors need time to adjust to wearing these. Young children, who often pull glasses off, may benefit from the use of temporal pieces that wrap around the ears or an elastic strap attached to the frames and around the back of the head to hold the glasses on securely. Once children appreciate the value of clear vision, they are more likely to wear the corrective lenses.
Glasses should not interfere with activity. Special protective guards are available to prevent accidental injury during contact sports, and all corrective lenses should be made from safety glass, which is shatterproof. Often corrective lenses improve visual acuity so dramatically that children are able to compete more effectively in sports. This in itself is a tremendous inducement to continue wearing glasses.
Contact lenses are a popular alternative to conventional glasses. Several types are available, such as gas-permeable and soft lenses, which may be designed for daily or extended wear. Contact lenses offer several advantages over glasses, such as greater visual acuity, total corrected field of vision, convenience (especially with the extended-wear type), and optimum cosmetic benefit. Unfortunately, they are usually more expensive and require much more care than glasses, including considerable practice to learn techniques for insertion and removal. If they are prescribed, the nurse can be helpful in teaching parents or older children how to care for the lenses.
Because trauma is the leading cause of visual impairment, the nurse has the major responsibility for preventing further eye injury until the specific treatment is instituted. The major principles to follow when caring for an eye injury are outlined in the Emergency Treatment box, p. 931. Because patients with a serious eye injury fear visual loss, the nurse should stay with the child and family to provide support and reassurance.
Hearing-Visual Impairment
The most traumatic sensory impairment is loss of both sight and hearing. Historically, one of the chief causes of visual and hearing impairment was congenital rubella syndrome, but immunization has decreased its incidence. Other cases usually occur when one congenital sensory impairment is combined with an acquired impairment, such as congenital visual impairment and acquired hearing deficit from meningitis, or congenital hearing impairment and acquired visual loss from an eye injury. Most children with multisensory impairments have some residual hearing and vision to supplement the senses of touch, smell, and taste.
Combined auditory and visual impairments have profound effects on the child’s development. They interfere with the normal sequence of physical, intellectual, and psychosocial growth. Although the child often achieves the usual motor milestones, they are delayed. Children only learn communication with specialized training. Finger spelling is one desirable method often taught to these children. Words are spelled letter by letter into the hearing-visually impaired child’s hand, and the child spells out ideas to the other person. Another type of tactile communication is the Tadoma method, in which the child places a hand over the speaker’s face and neck to monitor facial movements associated with speech production. Some children with residual hearing or vision impairment can learn to speak. Whenever possible, encourage speech because it allows communication with individuals not familiar with the preceding approaches.
Programs for these children vary. The John Tracy Clinic* offers a home correspondence course for parents, and the American Foundation for the Blind,† Helen Keller Services for the Blind,‡ Perkins School for the Blind,§ and Junior Blind of America provide publications and various special services. The Library of Congress National Library Service for the Blind and Physically Handicapped¶ publishes a reference circular titled Deaf-Blindness: National Resources and Organizations.
provide publications and various special services. The Library of Congress National Library Service for the Blind and Physically Handicapped¶ publishes a reference circular titled Deaf-Blindness: National Resources and Organizations.
Nursing Care Management
One of the major concerns of families with children who are hearing and visually impaired is helping them establish communication. The nurse is in a vital position to help parents with this goal. Because infants may not coo, laugh, or make directed eye movements, they are limited in the cues they can send and receive. Therefore initiating and maintaining communication is the caregiver’s responsibility. The nurse discusses with parents behaviors that signal the infant’s recognition of them, such as quieting behavior, blinking, and change in respiration. Encourage the parents to find ways of increasing stimulation for the child, especially cues that help the child identify each parent. For example, each person involved with the child should choose something that only he or she does, such as a kiss on the forehead or a stroke on the cheek. In this way the infant learns to discriminate among people in the environment.
Provide as many sensory experiences as possible, such as placing children in different positions during the day in relation to light and providing variation in stimuli so that they will be motivated to move toward, reach, touch, and explore the environment. Changing position also encourages muscle development and movement patterns. Bring sounds near and make them interesting to these children. For example, they can participate in hearing by placing the hand on a radio or on a person’s throat. Consistent tactile cues should be associated with a change of position and activities so that the movement is experienced as a positive, nonthreatening experience.
Children who are hearing and visually impaired need secure, safe experiences while learning to walk and gain confidence. Once ambulatory, they need help in exploring the environment on a gradual, planned basis. After they succeed in becoming well oriented to the environment, they are ready for a plan of locomotion. Ambulation with a sighted guide, trailing (movement directed by touching objects, such as the wall), and cane walking are three methods. An individually planned mobility program is based on the child’s age, needs, and functional status and is shared with the child’s therapist, teachers, parents, and siblings.
The future prospects for hearing and visually impaired children are at best unpredictable. Sometimes congenital hearing and visual impairment is accompanied by other physical or neurologic handicaps, which further lessen the child’s learning potential. The most favorable prognosis is for children with acquired hearing and visual impairments and few, if any, associated disabilities. Their learning capacity is greatly potentiated by their developmental progress before the sensory impairments and the assistance of a trained companion. Although total independence, including gainful vocational training, is the goal, some hearing and visually impaired children are unable to develop to this level. They may require lifelong parental or residential care. The nurse working with such families helps them deal with future goals for the child, including possible alternatives to home care during the parents’ advancing years.