Family-Centered Care of the Child with Chronic Illness or Disability
Perspectives in the Care of Children with Special Needs
Impact of Chronic Illness or Disability on the Child
The Family of the Child with Special Needs
Assessing Family Strengths and Adjustment
Accepting the Child’s Condition and Receiving Support at the Time of Diagnosis
Managing the Condition on an Ongoing Basis
Meeting the Child’s Normal Developmental Needs
Meeting Developmental Needs of Other Family Members
Coping with Ongoing Stress and Periodic Crises
http://evolve.elsevier.com/wong/ncic
Birth of a Child with a Physical Defect, Ch. 11
The Child with Cognitive, Sensory, or Communication Impairment, Ch. 24
Childhood Morbidity, Ch. 1
Communicating with Families, Ch. 6
Developmental Assessment, Ch. 6
Discharge Planning and Home Care (High-Risk Newborn), Ch. 10
Facilitating Parent-Infant Relationships (High-Risk Newborn), Ch. 10
Family-Centered Care, Ch. 1
Family-Centered Care of the Child During Illness and Hospitalization, Ch. 26
Family-Centered End-of-Life Care, Ch. 23
Family-Centered Home Care, Ch. 25
Family Structure, Ch. 6
Health Promotion: Infant, Ch. 12; Toddler, Ch. 14; Preschooler, Ch. 15; School-Age Child, Ch. 17; Adolescent, Ch. 19
School Phobia, Ch. 18
Social, Cultural, and Religious Influences on Child Health Promotion, Ch. 2
Perspectives in the Care of Children with Special Needs
Significant changes in the health care system have increased the need for services and benefits to children with chronic illness or disability (Stein, Shenkman, Wegener, et al, 2003). A major obstacle in the effort to provide these services has been the issue of how best to define populations of children with chronic conditions. For many years a number of terms have been used to classify and describe children with special health care needs (Box 22-1).
More recently there has been a drive to develop a definition of children with special health care needs that could be used by federal and state programs to facilitate planning of comprehensive, family-centered, community-based services for this population (Jackson, 2009; Beers, Kemeny, Sherritt, et al, 2003; Miller, Recsky, and Armstrong, 2004). To date, children with special health care needs, as defined by the federal Maternal and Child Health Bureau (Msall, Avery, Tremont, et al, 2003), are “children who have or are at increased risk for a chronic physical, behavioral, developmental, or emotional condition and who also require health and related services of a type or amount beyond that required by children in general.”
Each year in the United States, 6 million children ranging from newborns to 17-year-olds are hospitalized for a variety of conditions, and the average length of stay for those patients is approximately  days (Weiner, 2008). Advances in biomedical science and technology have resulted in dramatic improvement in the health care of pediatric chronic conditions (Varni, Limbers, and Burwinkle, 2007). There is now improved management of infectious diseases, identification of children with previously unrecognized illnesses, and implementation of preventive and public health measures (Jackson, 2009). With these medical advances and decreasing patient lengths of stay, many more patients are requiring care in the home setting. The burden of care is then carried by the family and outpatient care facilities to provide services required.
days (Weiner, 2008). Advances in biomedical science and technology have resulted in dramatic improvement in the health care of pediatric chronic conditions (Varni, Limbers, and Burwinkle, 2007). There is now improved management of infectious diseases, identification of children with previously unrecognized illnesses, and implementation of preventive and public health measures (Jackson, 2009). With these medical advances and decreasing patient lengths of stay, many more patients are requiring care in the home setting. The burden of care is then carried by the family and outpatient care facilities to provide services required.
For example, the median life expectancy of children with cystic fibrosis today is more than 30 years, in contrast to 5 years in 1955. In 1955, 90% of children born with spina bifida died in infancy. Today 90% survive infancy and have a normal life expectancy if they have appropriate and timely medical intervention such as improved surgical advances and management of urinary tract infections (Jackson, 2009). In addition, advances in combination antiretroviral therapy have resulted in a decreased mortality rate for children infected with human immunodeficiency virus (HIV) (Fahrner and Mario, 2009; Yogev and Chadwick, 2007). Infants with very low birth weight and extreme prematurity are living longer (Jackson, 2009), and more than 80% of children diagnosed with cancer today will be cured of their disease (Gurney and Bondy, 2010; Horner, Ries, Krapcho, et al, 2008).
The dramatic decline in mortality rates has led to an increase in the number of children with special health care needs and has implications for the provision of comprehensive, long-term health care services for these patients (Jackson, 2009; Palfrey and Richmond, 2005). Chronic illness has surpassed acute illness as the major health concern for children (Perrin, Bloom, and Gortmaker, 2007). In the United States an estimated 18% of children (12.6 million) have a chronic illness or disability that requires health care services beyond those usually required by children (Perrin, Bloom, and Gortmaker, 2007; Arango, 2005; Newacheck, McManus, Fox, et al, 2000).
The most common chronic childhood conditions causing disability are respiratory diseases (primarily asthma), impairments of speech and sensory functions, and mental and nervous system disorders (Arango, 2005). Asthma is the single most prevalent cause of disability in children and has been largely responsible for much of the recent increase in childhood disability. Mental and nervous system disorders account for about one sixth of all childhood disability. The prevalence of disability is higher in boys, in children older than 5 years of age, and in children from single-parent and low-income families (Newacheck and Halfon, 2000; Schiller, Adams, and Nelson, 2005).
The impact of chronic illness and disability on children’s health and functional status is profound. Children with disabilities spend three times as many days ill in bed and days absent from school as other children. They make 26 million more visits per year to the physician than typical children and spend 5 million more days in the hospital annually (Arango, 2005). They are limited in their daily activities for slightly more than 2 weeks each year, and one tenth of all children with disabilities are unable to play or attend school (Arango, 2005). In addition, children with disabilities are more likely to be a victim of emotional or sexual abuse, have behavioral problems, drop out of school, and be involved in the juvenile justice system than are their peers without disabilities (Perrin, Bloom, and Gortmaker, 2007).
Chronic illness and disability have substantial effects on family functioning. Chronic conditions present most families with additional tasks, responsibilities, and concerns such as the additional caretaking needs of the child, identification of and access to educational and medical services, payment for services, uncertainty about the future, emotional grieving, stigmatizing reactions from the community, social isolation, and lost social opportunities. These demands can be grouped according to their personal impact on a parent, the financial impact on the family, and the impact on social and family relationships.
Parents are caught in a juggling act of meeting their child’s normal growth and development needs and dealing with the consequences of the chronic illness (Sullivan-Bolyai, Knafl, Sadler, et al, 2004). Parents of children with disabilities are more likely to report depression than parents of children without disabilities (Sullivan-Bolyai, Sadler, Knafl, et al, 2003). Family members of children with disabilities are more likely to experience behavioral and psychologic symptoms. Parents may miss days from work, experience financial strain, and be challenged both physically and emotionally while they deal with caring for a child with a chronic illness or disability. Siblings may experience a wide range of feeling and concerns and often have to identify and deal with these concerns in the absence of the parent, who is either physically separated or emotionally unavailable to the well sibling (Pearson, 2005). Frequently, siblings’ lives reflect the routines imposed by the affected child’s chronic condition.
The increased prevalence of chronic illness and disability in children and the far-reaching effects on the child and family members have many implications for nursing. Nurses need to take an active role in early screening, case finding, and assessment and provide supportive and educational interventions that decrease the disruptive effects of the chronic condition on the child and family members. In addition, nurses should attempt to prevent disabling conditions by removing their known causes; this entails encouraging adherence with immunization programs, identifying infants and mothers at risk, recognizing the disability early, fostering injury prevention programs and policies, and providing innovative health education programs. Skilled case management is necessary to ensure that the family of a child with special needs has the support to successfully adapt to the consequences of the child’s chronic condition. This includes providing community-based, comprehensive, and culturally appropriate care to the child with special needs (McPherson, Weissman, Strickland, et al, 2004).
Trends in Care
Because of advances in technology, economic effects, and the demand for more meaningful models of care, care has changed not only in the types of services and care children receive, but also in where services are provided and by whom.
Developmental Focus
Using a developmental approach rather than one based on chronologic age when caring for children with special health care needs helps the nurse to determine where children are at present and to understand their response to the chronic illness or disability. Developmental changes in the child continue despite the added stress of coping with a chronic illness. The chronic condition imposes a dimension of behavioral and developmental risk (Rittey, 2003). Because children with chronic conditions are more alike than different, a noncategorical approach emphasizing the commonalities of these children, rather than solely the illness, is beneficial. Referring to children by the names of their disabilities or illnesses affects professional and parental attitudes, as well as the assessment of the child’s present abilities and future expectations (Green, 2003). Therefore parents and the health care team should work jointly for the benefit of the child who has an illness rather than allowing the illness to define the child. Knowledge of the developmental theory perspective is paramount in providing the support necessary for children to successfully adjust to a stressful life experience such as a chronic illness or disability.
Family Development
A developmental approach also includes an assessment of family development. The family life cycle focuses on the changing ages and developmental tasks of both children and adults and on the changing external demands as the family grows older. Families are expected to accomplish certain tasks at various stages (e.g., finding, furnishing, and maintaining their first home during the married couple stage). A diagnosis of chronic illness in a family member has a profound effect on every member of the family unit (Sullivan-Bolyai, Sadler, Knafl, et al, 2003). As with individual development, family development may be interrupted or even regress to a previous level of functioning. For example, having a child with a chronic illness may impose an added stress on the newly married couple who are in the midst of establishing a family identity. Nurses can apply family developmental theory when planning interventions for families of children with special health care needs. (See Developmental Theory, Chapter 3.)
Family-Centered Care
Family-centered care is paramount in the care of children with special health needs. Over the past 40 years significant changes have occurred in parents’ responsibilities for providing and coordinating the care of their ill child. Today families of chronically ill children have comprehensive and complex caretaking responsibilities in the hospital and at home (Sullivan-Bolyai, Knafl, Sadler, et al, 2004).
The increasing numbers of chronically ill children and the families who are assuming the major burden of coordinating their children’s care have reinforced the demand for new approaches in the health care system. The outcome has been the emergence of family-centered care to reflect, recognize, and facilitate the changing roles of families in care delivery. Because a cure is not likely for a number of chronic conditions, health care professionals must focus their efforts on care.
The federal legislation Public Law (PL) 99-457, which affords states the opportunity to extend the benefits of PL 94-142 (Education for All Handicapped Children Act of 1975) to children from birth to age 5 years, targets family-centered care. This legislation establishes a process whereby families become active participants in decision making about the care of their children.
The goal of care is to minimize the manifestations of the illness and maximize the child’s cognitive, physical, and psychosocial potential. Advocating a family-centered approach to care facilitates attainment of this goal (Vessey and Mebane, 2009). (See Family-Centered Care, Chapter 1.) Integrating family-centered care in practice requires health professionals to (1) acknowledge and respect the family’s individuality and strengths, (2) foster the family’s competence and confidence in caring for the child, and (3) empower the family to advocate for the child when dealing with the health care system (Vessey and Mebane, 2009). In the family-centered framework, consistent attention is given to the effects of the child’s chronic illness on all family members, not only on the affected child. This is paramount, because the best predictors of the well-being of children with special health needs include factors associated with family functioning.
As parents become knowledgeable about their child’s special health needs, they frequently become experts in providing care. As part of the health care team, nurses are adjuncts in the child’s care and need to build alliances with parents, respecting and drawing on their expertise. One of the key principles in family-centered care is the involvement of family members in decision making about their child’s physical care. Collaboration—consistent sharing of information about the illness, responsibility, and decision making—is necessary to establish effective and trusting partnerships with parents.
Care conferences with the child’s family and members of the health care team, including nurses, offer opportunities for mutual sharing of thoughts and concerns about the child’s care. Being attentive the parent’s observations helps assure them that their role is valued and their opinions important.
In fostering effective family-centered care, the nurse not only acknowledges that the family is a key component of the child’s care and illness experience but also recognizes and respects the family’s expertise in caring for the child within and outside of the hospital milieu. In the absence of the child’s family during hospitalization, the nurse should try to maintain routines established by the family. In the family’s presence, the nurse, child, and parent form a relationship in which the process of care negotiation occurs. This relationship is pivotal to the needs of the child and family and is where roles are defined and guidelines are developed. Through open communication, the nurse values the parents’ roles by viewing them as the ultimate experts in caring for their child. Simultaneously the family looks to the nurse for empowerment, support, education, and expertise in caring for their child (Fazil, Wallace, Singh, et al, 2004; Sullivan-Bolyai, Knafl, Sadler, et al, 2004).
Normalization
Normalization refers to establishing a normal pattern of living (see Nursing Care Guidelines box, p. 855). Normalization occurs on several levels. It implies child and family access to services in as usual a fashion and environment as possible, with a focus placed on the home and community. Application of the principles of normalization means that daily routines for the child with illness or disability should be fitted to the family’s schedule, rather than vice versa. Age-appropriate expectations for the child’s behavior should be applied. As necessary, the environment should be structured to encourage the child’s engagement in age-appropriate activities. Thus consequences of the illness are minimized, and the child and family live as normal a life as possible given the disability.
Nurses can facilitate the normalization process for families of children with special needs by acknowledging their normalcy, strengths, and weaknesses. Being supportive of the child’s illness and treatment and actively including the family in all aspects of the care will improve their self-esteem and promote further development (Shepard and Mahon, 2009).
Home Care
Along with the trend toward normalization, there has also been a trend of earlier discharge of children from acute or chronic care facilities to the family and community. Home care refers to the return to a system and set of priorities whereby family values are as significant in the care of a child with a chronic illness as they are in the care of healthy children. The primary incentive for home care of children with special health needs was a parental need to keep these children at home and professionals’ willingness to work with families to attain this goal. The goal of home care is to:
• Normalize the life of the child with special needs, including the child with technologically complex care, in a community and family setting
• Lessen the disruptive impact of the child’s condition on the family
With appropriate support and training, families today can accomplish complex treatments and procedures in the home. Parents are challenged to maintain a homelike setting in the midst of ventilators, monitors, and other sophisticated equipment. Throughout this text home care is discussed as appropriate for specific conditions. Chapter 25 focuses on family-centered home care; the process of transition from the hospital to the home setting is described in Chapter 26.
Mainstreaming
Mainstreaming refers to a process of integrating children with special needs into regular classrooms and child care centers. Attending school allows these children to acquire a sense of self and understanding of their place with respect to their peers. It also provides important opportunities for socialization with nondisabled children, which enables the latter group to develop respect for and acceptance of their peers with special needs. A crucial developmental task for children 5 years of age and older is to move beyond the family environment into the school community, where social competence, academic achievement, and regular attendance are important goals (Vessey and Jackson, 2009). A variety of supplemental programs exist in the school system to accommodate children with special needs and thereby afford them equal educational opportunity.
For the most part this change facilitating normalization for these children has resulted from the passage of PL 94-142, the Education for All Handicapped Children Act of 1975, which provides children with “free and appropriate public education,” including special education and related services, rendered at public expense, under public supervision, and without charge, that meet the standards of the state educational agency (Vessey and Jackson, 2009). The 1990 amendment to this law, PL 101-476, changed the name of the act to the Individuals with Disabilities Education Act (IDEA). Passage of PL 101-476, along with current federal child care mandates and increasing public concern about child care, demonstrates a national commitment to the concept that early services are crucial if children with disabilities are to achieve their full potential. In December 2004 PL 108-446 was passed, resulting in a major reauthorization and revision of IDEA. This reauthorized state and local aid for special education and related services for children with disabilities, specifically in development and maintaining early intervention programs for infants and toddlers with disabilities.
PL 94-142 requires states to identify, diagnose, teach, and provide related services to children with disabilities from 5 to 18 years of age. In 1977 the age range was extended to include children 3 to 21 years of age, with services for children ages 3 to 5 years optional. In accordance with this law, a multidisciplinary team writes an individualized education program (IEP), which includes specific therapeutic and educational goals and strategies for each eligible child referred for special education. Parents may intervene in educational decisions and have the right to a hearing when they believe the team’s decision is harmful or inappropriate. Because many parents are unaware of this or other laws providing rights for disabled children, it is imperative that nurses inform them of what the laws are and where to obtain information. Nurses may also be involved in formulating IEPs.
Early Intervention
Early intervention includes any systematic and sustained effort to assist young, disabled, and developmentally vulnerable children from birth to 3 years of age. PL 99-457, the Education of the Handicapped Act Amendments of 1986, directs states to develop and enact statewide coordinated, comprehensive, multidisciplinary interagency programs of early intervention services for infants and toddlers with disabilities, in addition to support services for their families.
An important component of the law’s implementation is the individualized family service plan (IFSP). As a product of collaboration between professionals and families, the IFSP consists of information relating to the infant’s or toddler’s current level of development, family needs and strengths for improving development, main outcomes anticipated, services required, designation of a case manager, and transition steps to preschool services. All outcomes and services concern the needs of the child and family. The IFSP represents a commitment to families and children that their strengths will be acknowledged and built on, that their needs will be satisfied in a manner that respects their values and beliefs, and that their aspirations will be fostered and empowered.
Nurses can provide many services for children covered by PL 99-457. Implementation of family-centered care and clinical expertise in practice provide nurses with a role in early identification and assessment of children at risk for disability, in multidisciplinary assessment, and in case management. Nurses can assess children in preschool settings, implement ongoing staff and patient education, coordinate care with the heath care team, become actively involved in community nursing networks, and develop health promotion programs for school personnel and family members.
Managed Care
Managed care health plans have become the primary form of health care coverage in the United States (Jackson, 2009; Smucker, 2001). An evaluation of out-of-pocket expenditures for insured versus uninsured children with special health care needs revealed higher out-of-pocket burden and financial problems among the uninsured (Jeffrey and Newacheck, 2006). Not only has managed care expanded rapidly, particularly for Medicaid-eligible patients, but the roles and responsibilities of state Title V programs for children with special health needs have changed as well (McPherson, Weissman, Strickland, et al, 2004; Inkelas, 2005). Provision of direct services by specialty clinics funded through Title V were reduced while managed care systems attempted to provide services to children within the managed care organization.
Implementing managed care for children with disabilities differs from providing care for adults with disabilities in three ways (McPherson, Weissman, Strickland, et al, 2004): (1) the changing dynamics of child development affect the needs of these children at various developmental stages and change their anticipated outcomes; (2) the prevalence and epidemiology of childhood disabilities, with few common conditions and many low-incidence or rare ones, vary considerably from those of adults, for whom there are many common conditions and few rare ones; and (3) because of children’s need for adult guidance and protection, their development and health rely heavily on their families’ socioeconomic status and health. These differences have implications for monitoring care provided to children with chronic conditions in managed care settings. The diverse effects of managed care on these children are seen in seven major domains: access to care, use of services, quality of care, satisfaction with care, cost of care, health outcomes, and family impact (Newacheck, Hung, and Wright, 2002; van Dyck, Kogan, Heppel, et al, 2004).
Families offer four basic suggestions for improving services for their children with chronic conditions: (1) reduce barriers to programs and services; (2) improve the quality of services; (3) improve the training given to families, health care professionals, and the community relating to chronic conditions and their management; and (4) increase the availability and quality of community-based services (van Dyck, Kogan, Heppel, et al, 2004). All of these suggestions require two factors: universality of care and adequate funding (Vessey and Jackson, 2009). Health care providers play an important role in working jointly with the leaders of managed care programs to ensure high-quality care for children with chronic conditions.
Cultural Issues
Increasing migration around the world in the past 10 years has led to heterogeneity in many nations, including the United States. For this reason, cultural competence is an important goal of nursing practice.
For many minority and ethnic populations, cultural understanding of disability and illness, social roles for disabled individuals, the structure of family life, and other factors associated with the perception of children vary from those of “mainstream” American culture. These factors may affect family choices regarding the care of the child with special needs.
Although culture cannot fully define how an individual will act and think, knowledge of cultural perspectives can assist nurses in anticipating and understanding why families make certain decisions. Cultural attributes, including beliefs and values concerning disability or illness and its causes, family structure, social roles for the disabled, the role of children, childrearing practices, spirituality, and time orientation, also influence a family’s reaction to a chronic condition. Although eliciting health beliefs and negotiating interventions can be challenging, it is necessary for compliance, collaboration, patient/family satisfaction, and optimal care (see Nursing Care Guidelines box).
Recognizing the growing cultural diversity in our society, nurses must incorporate cultural competence in their clinical practice to promote delivery of effective and sensitive care to children with chronic illness and their families. Care should be consistent with the cultural practices and beliefs of the child’s family whenever possible; increasing cultural competence will improve communication and promote respect for human diversity (Rehm, 2009) (see Cultural Competence box).
Impact of Chronic Illness or Disability on the Child
A child’s reaction to chronic illness or disability depends largely on his or her developmental level. Knowledge of developmental stages is essential for nurses to understand how children interpret events. Because children’s cognitive abilities change as they grow, they require varied explanations of their chronic illness as they mature. Normal development should occur in the context of the child’s temperament, intelligence, motor skills, and relationships with family and friends. Identifying the child’s coping strategies and promoting successful adaptation to the illness are essential. Factors influencing coping include the developmental stage, age, gender, type and duration of illness, and family cohesion (Schmidt, Petersen, and Bullinger, 2003). Caring for the child involves health education efforts, normalization principles, and assistance to the growing child in planning realistic future goals.
Promoting Normal Development
Normative developmental tasks throughout childhood center on developing a sense of self and acquiring autonomy in all areas of life (Turkel and Pao, 2007). The impact of a chronic illness or disability on a child is affected by the child’s age at the onset of the illness or disability (Vessey and Mebane, 2009). Chronic illness can affect children of all age-groups, although each age-group faces its own specific challenges. Children redefine their illness and its implications as they develop and grow. Accordingly, nurses must plan and implement care that promotes the child’s successful progression from one stage of development to the next.
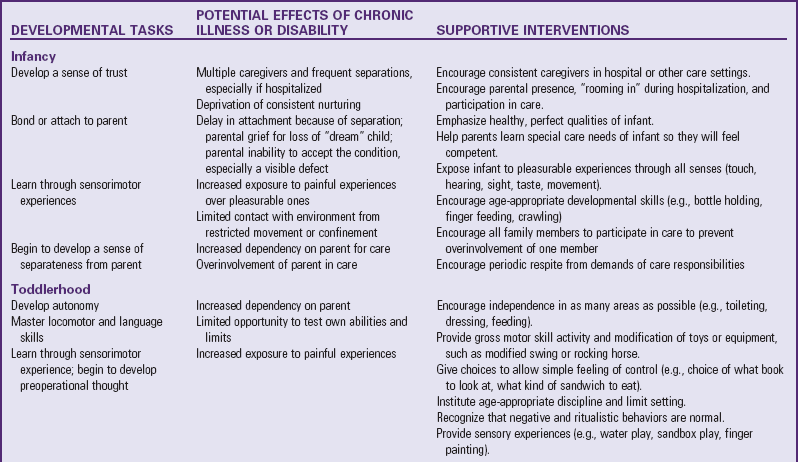
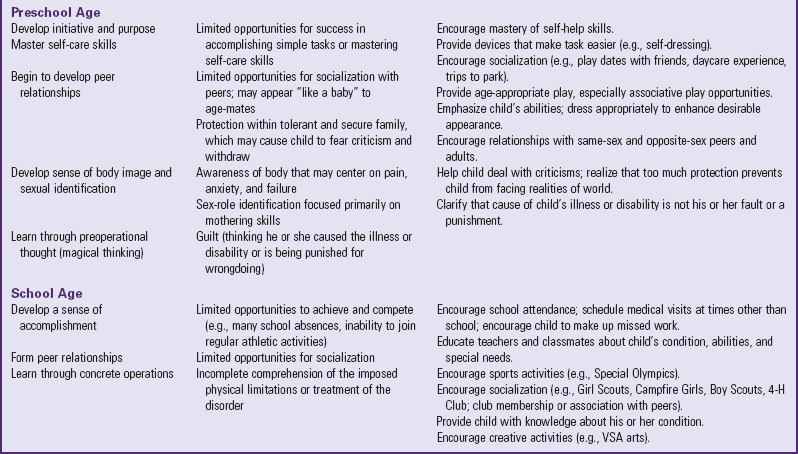
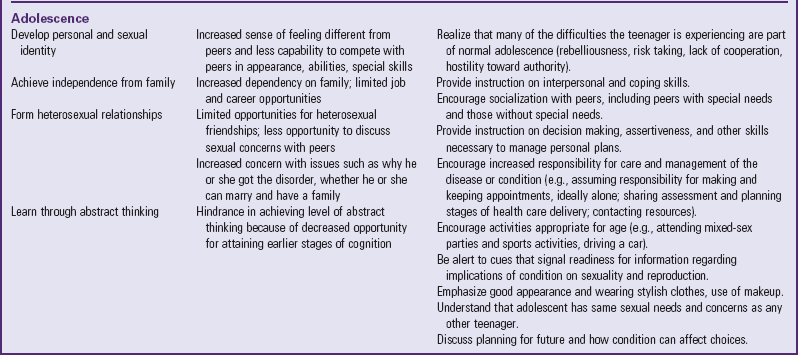
In addition to learning about the illness and its effects on the child’s abilities, the family needs to acquire strategies to promote appropriate development in their child. Even with delays in achievement of developmental milestones, nurses need to be instrumental in teaching parents how best to help their child reach his or her developmental potential (Vessey and Mebane, 2009). Table 22-1 describes developmental aspects of chronic illness or disability in children and accompanying supportive interventions.
Infant
During infancy the child is establishing trust and learning about the environment through sensorimotor exploration (Vessey and Mebane, 2009). However, the diagnosis of a chronic illness, accompanied by a disruption in routines and physical discomfort, may compromise the dependability and consistency of an infant’s environment and hinder the development of basic trust. Disability or chronic illness frequently impairs the child’s motor abilities, restricting the child to a crib and decreasing contact with the environment. Illness may influence the infant’s growth and developmental parameters by its effects on mobility, sleeping, feeding, and sensory functions. Separation of infant and parent as a result of frequent hospitalizations may prevent attachment and the emergence of a trusting relationship for the infant.
For the infant with a painful illness, exploration of his or her environment is restricted, which further curtails development (Vessey and Mebane, 2009). Messages transmitted to infants about their bodies are affected by the amount of pain and discomfort they experience. Associating pain with touch can lessen the infant’s ability to give and receive affection. Lack of pleasant sensations can result in an irritable and unhappy child. Parents may interpret this behavior as indicative of their inadequacy in satisfying the child’s emotional and physical needs, which further affects the parent-child relationship and the development of trust. Illness may threaten the parents’ feelings of confidence and competence in their newly acquired parenting roles.
The presence of a visible or serious defect can hinder parental attachment while the parents mourn the loss of the perfect child. They may gain little comfort from trying to satisfy their child’s basic needs despite their best efforts. Physical deformity or fatigue may influence a child’s responsiveness to his or her parents, who may in turn react differently to their child. A poor prognosis for the child may cause some parents to emotionally detach themselves from their infant to protect themselves from future emotional pain (Vessey and Mebane, 2009).
Nurses can be pivotal in helping parents care for their infant with special needs. They may need assistance in learning how best to meet their infant’s needs, for example, how to hold a flaccid or rigid infant, how to comfort an irritable infant, how to feed a child with dyspnea or tongue thrust, or how to stimulate a child unable to develop common skills.
Nurses should advocate for practices and policies that support the developmental needs of the infant and the family. Twenty-four-hour visitation in the neonatal intensive care unit and other infant units is paramount and lessens the infant’s experience of separation. In addition, nurses need to limit the number of caregivers for the infant to enhance consistency and continuity of care. Showing parents how to hold and touch their infant will foster their competence and confidence. Kangaroo care (with skin-to-skin contact) has been demonstrated to be both beneficial and safe for the infant. (See Chapter 10.) Give support to mothers who want to breast-feed, and provide a private room with refrigerated storage for the woman who pumps or nurses. Promote sibling visitation as well.
Toddler
The toddler is acquiring a sense of autonomy, developing self-control, and forming symbolic representation through language acquisition. The need for parental involvement in managing the child’s illness may interfere with the toddler’s need for increasing independence and impede his or her sense of autonomy and self-control. Mobility is possibly the primary tool used by the toddler to experiment with attaining control. For the toddler who is incapacitated, a sense of helplessness results that is difficult to overcome at a later time.
If a child’s chronic illness prevents daily activities, this may impede autonomy in tasks such as feeding, toileting, and building larger social networks. Developmental tasks that have just been mastered are often easily lost in the toddler suffering from an acute exacerbation of the illness. Behavioral regression, commonly seen in toddlers, is worsened by stress related to pain and separation.
Because of the toddler’s desire for autonomy, the mastery of language and locomotor skills is very important. The child learning to talk and walk progresses toward being a separate individual, both psychologically and physically. A toddler’s limited ability to verbally communicate thoughts and feelings makes it especially difficult for the child to cope with the stresses imposed by a chronic illness. In the presence of disability or illness, mobility to explore and master the environment is impeded, and the child is prevented from acquiring these skills. Within the constraints of the illness or disability, the nurse should help parents provide safe opportunities that foster independence in these and other areas for their toddler, both at home and in the hospital (Fig. 22-1).

Fig. 22-1 Wheelchairs designed for children can help a child with disabilities gain mobility and promote growth and development.
Illness can impose separations that cause anxiety in the toddler. A disability or chronic illness can entail frequent painful procedures and hospitalizations. The latter may hinder the normal development of trusting relationships within the family. If the hospital does not help maintain the parent-child relationship, the child may become depressed and eventually detach from parents. Children appear to have a great ability to withstand stress as long as they retain their attachment to the parent.
Toddlers are especially sensitive to changes in familiar routines, in addition to hospitalizations. They may perceive disruption of normal daily activities and hospitalization as punishment. If invasive and painful medical procedures are required in the treatment of the child’s illness, this perception is further validated. Therefore encourage parents to bring in familiar toys for the toddler during hospitalization, and establish routines so the child can become acclimated.
Parents of toddlers may seek out daycare or respite care, which can be difficult to find for the child with special needs.* Caregivers need time away from caring for their child to allow for their own growth and development. The Americans with Disabilities Act (ADA) requires that daycare providers make “reasonable modifications” for equal access to program participation (Mahoney, Wheeden, and Perales, 2004). Special medical daycare facilities are emerging in some areas (Mahoney, Wheeden, and Perales, 2004).
Preschooler
The preschooler is focused on acquiring a sense of initiative to successfully meet the challenges of his or her growing world. Preschoolers with a chronic illness may lack the resources or energy to plan and engage in such activities; thus opportunities for building social relationships, learning about the environment, and developing a sense of purpose and self-confidence are often limited. Illness may restrict the preschooler to the home and cause the child to fall behind in social skills beneficial in school or group settings.
It may be difficult for preschoolers to build a healthy sexual identity and body image, especially if most of their body awareness is linked with pain and disability. Children’s understanding of their body is confined to what they see, feel, and use. In the presence of a chronic illness, their body awareness may be focused on the anxiety and pain elicited. The chronically ill child may lose control over newly acquired bowel and bladder function, which results in feelings of embarrassment and inferiority. The child with a disability may find it difficult to form a mental image of impaired body parts, for example, paralyzed extremities. This poorly developed sense of body integrity causes children to be particularly fearful of mutilating or intrusive experiences, which can occur frequently during a lengthy illness. Thus before any medical procedure children should be given a brief, honest explanation of what the procedure is, how it will be performed, and the duration and intensity of any accompanying pain.
When the young child has a disability that affects motor development, there is the risk of shifting to development of compensatory intellectual pursuits before the child is ready. This could compromise attainment of initiative and autonomy and place the child at risk for emotional problems. Thus intervention must focus on providing activities that allow maximum motor development. For example, if a child has paraplegia, it is not enough to strengthen the upper extremities to compensate for the lower ones. Rather, the activity must consider the child’s need for a sense of control over the body, social interaction, feeling of achievement and competence, and outlet for aggression. Appropriate activities may include ball throwing; play with building blocks; water and swimming activities such as bubble blowing, splashing, and racing; or pounding with a hammer.† Children with disabilities may be able to ride a tricycle with minor changes such as self-adhering straps to protect the hands or feet.
One of the more crucial effects of chronic illness or disability on preschoolers is the feeling of guilt that they “caused” the illness through an imagined or real misdeed. This is less of an issue if the child is born with the condition than if it occurs during the preschool period. Such guilt can significantly affect the child’s developing but fragile self-esteem, especially if the child experiences frequent insults. In contrast, the child with a temporary physical disability has added opportunities for attaining mastery and overcoming feelings of inferiority and guilt. Structuring situations to foster success can assist a child in developing a sense of confidence and competence.
Another critical component for normal child development is discipline. Discipline is essential to the child’s sense of security because boundaries are necessary for the child to test behavior. It also teaches the child socially acceptable behavior. Applying appropriate discipline to the child who is chronically ill or disabled can also limit the resentment and hostility that can develop among siblings if parents apply different standards to each child. The nurse’s responsibility is to help parents learn successful methods of guiding the child.
When a chronic illness imposes restrictions that cause difficulty with mastery, it can inflict a lasting sense of failure. Preschoolers are egocentric and have naive reasoning, which may affect their interpretation and understanding of their illness.
Because preschoolers need to explore and acquire experience with pretend situations and objects before they really experience them, nurses need to facilitate opportunities for imaginative play (e.g., using dolls and syringes) and to give simple answers to children’s questions about their illness and treatment.
School-Age Child
School-age children focus on increasing mastery over their environment and independence. A lack of physical stamina may prevent the child with a chronic illness from engaging in school and extracurricular activities and result in feelings of inferiority or inadequacy. These activities help the child acquire social skills, develop a sense of achievement, gain the skills to achieve self-sufficiency, and learn to effectively deal with stress. School-age children should be involved as much as possible in their own care and in decision making about their treatment to facilitate their sense of control and mastery.
School-age children are mostly concerned with learning to take initiative. School initiates the processes of working toward independence from parents, gaining academic skills, and building peer relationships. Along with the family, school is the major context in which children develop their sense of self and understanding of their place relative to their peers.
During the school-age period, the child is increasingly able to distinguish fantasy from reality, self from others, and he or she advances to inductive reasoning and beginning logic. Coupled with this limited sense of causality comes a deeper understanding of differences. Children with an illness that is not obvious may try to hide its existence once they realize that it differentiates them from their peers (Vessey and Mebane, 2009).
School-age children also begin active inquiry. They are usually verbal regarding their condition and ask for information about all phases of the illness and treatment. In addition, they experience pride after they learn the correct label for the illness, treatment, and medication. From the beginning, nurses should respond to the child’s questions in a simple, direct manner.
The school-age child separates from parents more easily and becomes more active in peer relationships. Peers strongly influence school-age children’s opinions of themselves and their self-esteem (Murray, 2000). If not provided with the required skills to disseminate information about their illness to peers, school-age children may withdraw with a diminished self-concept (Vessey and Mebane, 2009).
The number of children with chronic illnesses who return to school continues to increase (Kliebenstein and Broome, 2000). Children need preparation before entering or resuming school. Having a tutor in the hospital or home as soon as children are physically able helps them realize that school will continue and gives them time to consider this prospect. They need to investigate possible answers to the many questions others will ask. One method of anticipatory preparation is to role-play, with the child as the “returned pupil” and the nurse as “other schoolmates.” The nurse asks questions about the reason for the child’s absence, the name of the disease, and so on. The child is provided with a safe opportunity to explore possible answers and to experience some of the possible reactions of others. If the child returns to school with some obvious physical change, such as hair loss, an amputation, or a visible scar, the nurse might also ask questions about these alterations to prompt preparatory responses from the child.
Initially the child may find it easier to attend half-day school sessions or to participate in a limited number of activities. It is preferable to plan the school program with as much participation and leadership from the child as possible. Once the child returns, regular assessments of the child’s progress in various areas (academic, social, physical) are essential to ensure a satisfactory adjustment.
Classroom peers also need preparation, and a joint plan involving the schoolteacher, nurse, parents, and child is best. At a minimum the classmates should be given a description of the child’s condition, prepared for any visible changes in the child, and allowed an opportunity to ask questions. The child should have the option to attend this session. As the child’s condition changes, particularly if the illness is potentially fatal, school personnel, including the students, need periodic apprisal of the child’s status and preparation for what to expect. (See Chapter 23.)
Children with special needs should maintain or reestablish relationships with peers and to participate according to their capabilities in any age-appropriate activities. Alternative activities may be substituted for those that are impossible or that place a strain on their health. It is important for these children to have the opportunity to interact with healthy peers, as well as to engage in activities with groups or clubs composed of similarly affected age-mates. Such organizations as ostomy clubs, diabetic clubs, and cerebral palsy groups share information and provide support related to the special problems the members face.
Programs such as the Special Olympics (www.specialolympics.org) offer children with physical disabilities an opportunity to compete with their peers and to achieve athletic skill. Summer camps* also provide children unique opportunities to associate with similarly affected peers and to develop a wide variety of skills, including increased independence in activities of daily living and self-care associated with their condition. With creativity, parents can make many adaptations in children’s environments to increase their mobility and independence.† Technology is rapidly advancing, especially in the application of computers, and parents should be directed to the latest developments that may help their child.
Children with special needs obtain enormous benefits from expressive activities, such as art, music, poetry, dance, and drama. With adaptive equipment and imagination, children can participate in a variety of activities. Organizations such as VSA (vision, strength, and artistic expression) arts* encourage children to celebrate and share their accomplishments.
Adolescent
Adolescence marks the transitional period from childhood to adulthood and is characterized by important changes in intellectual, physical, social, and psychologic growth and development. Adolescence is the time for achieving independence. This may be difficult for adolescents with chronic illness, especially those who are dependent on others for daily care or therapy.
Chronic illness may impose the additional burden of hospitalization, pain, surgery, extensive diagnostic testing, medications, school absences, and activity restrictions on the adolescent. Such stressors may provoke many anxieties, fears, and grief reactions. Illness-related fears include loss of physical integrity, inability to separate successfully from one’s parents, loss of control, being different from peers, and death. They must cope not only with complex normative developmental tasks but also with the stress related to the diagnosis and treatment of life-threatening or long-term illness (see Research Focus box).
Adolescents are striving for autonomy, which is threatened by the forced dependence, need for compliance, and loss of control associated with an illness and treatment. Consequently, dealing with the illness may be more difficult and adolescents may be at greater risk for depression, anxiety, and adjustment problems. Many adolescents wish to assume total responsibility for their care despite their inexperience; however, their extensive care needs may prevent this from occurring (Newacheck, Wong, Galbraith, et al, 2003). If the chronic illness is associated with mobility limitations forcing dependence on caregivers for basic needs, it may compromise the emergence of a secure sexual and physical identity and peer relationships.
Adolescence is a time for achieving independence from the family and planning for future goals and responsibilities. Adolescents with long-term chronic illness may be less future directed and less independent than well peers. Enforced dependency from physical impairment can exacerbate the parent-child conflicts surrounding independence. Lack of understanding by both parties can result in bitter feelings and intrafamilial turmoil. The tendency toward rebellion may be directed at the disorder and reflected in decreased compliance with treatment; denial of the disorder to preserve a sense of normalcy with peers; and risk-taking behavior that can place the teenager in jeopardy, such as driving a car despite a disorder that increases the chance of an accident. Such behaviors can further strain an already tense parent-child relationship.
On the other hand, parents can promote independence by giving the adolescent a greater role in his or her own treatment regimen, encouraging the adolescent to develop a relationship with the physicians and nurses that is not mediated by parents, and promoting normalization principles.
During adolescence hormonal changes accompany the onset of puberty and a simultaneous preoccupation with body image. The major task of the adolescent is to develop his or her own identity. Hormone-related changes must be integrated into the self-image while the adolescent is gaining mastery and control over sexuality and increased physical abilities. During early adolescence this process occurs mostly within the peer group. The beginning of puberty, a period of uncertainty and rapid change, is even more confusing for teenagers with chronic illnesses.
Most adolescents are embarrassed by their appearance and emerging sexuality. For chronically ill adolescents the illness or its treatment may be most embarrassing and may influence their body image and hinder their sense of mastery and control over a changing body. It is difficult for the adolescent with a disability to incorporate the disability into a changing self-concept and body image. The young person who has a disability or is diagnosed with an illness during the critical adolescent years has more difficulty accomplishing these tasks than does the adolescent who has been affected since childhood. The earlier the onset of a limiting illness, the better the individual is able to adjust to it. The youngster with a newly acquired condition has the added task of grieving the loss while adapting to the changes occurring as a natural course of events. The adolescent often feels rejected because of personal appearance or inability to participate in activities expected of a healthy teenager.
Adolescence is a most difficult period to be seen as different by one’s peers, and some adolescents may withdraw from social relationships and activities that foster healthy psychosexual development. Appearance, abilities, and skills are highly regarded by peers; an adolescent who is limited in any of these qualities is subject to rejection by this influential group. A sense of feeling different from peers can cause isolation, loneliness, and depression. To be accepted by peers, some adolescents may decide to participate in risky behaviors such as unprotected sex and smoking, despite the possible harmful effects. Participation in groups of teenagers with chronic illnesses or disabilities can alleviate feelings of isolation and ease the transition to a meaningful relationship with one person in adulthood.
The topic of sexuality related to the effects of the illness is an important concern of adolescents, although they seldom initiate a discussion of this sensitive subject. Discuss any likely interference in sexual function due to the disability candidly and openly with the adolescent. Unfortunately, many nurses are reluctant to discuss sexual issues with teenagers. Adults often underestimate the degree to which adolescents participate in unrealistic fantasies about sexual activities and related matters, or even in sexual activity itself.
Nurses can facilitate the adolescent’s striving for autonomy by allowing and encouraging the adolescent’s participation in medical decisions by signing an assent as part of the informed consent document. Within the confines of the specific treatment center, the adolescent can be given control over the scheduling of procedures and treatments, allowed to view test results or radiographs, and included in discussions of alternative therapies. Adolescents should assume increasing responsibility for management of their illness consistent with their developmental stage, level of maturity, and understanding of their illness. Areas of responsibility may include monitoring their condition, assessing indicators of exacerbation and change, self-medicating, asking for assistance, and maintaining insurance coverage (Newacheck, Wong, Galbraith, et al, 2003).
Helping the Child Cope
Through ongoing contact with the child, the nurse (1) observes the child’s reactions to chronic illness or disability, ability to function, and adaptive behaviors within the environment and with significant others; (2) explores the child’s own understanding of his or her illness; and (3) provides support while the child learns to cope with his or her feelings. Encourage children to verbalize their concerns rather than allowing others to verbalize for them, since open discussions may lessen anxiety.
Parents often express concern because their child cannot communicate the anxieties he or she is feeling. If the child will not or cannot speak, the child may need to play out his or her feelings. Toys can be provided to facilitate expression of the meaning of stressful or threatening emotions. The nurse may realize that the child responds best to telling stories or drawing pictures. (See Chapter 6.)
Coping Mechanisms
Children’s innate and learned coping mechanisms are crucial in their ability to cope with their condition. Children with special needs are likely to use distinct coping patterns (Box 22-2). Children with more accepting and positive attitudes about their chronic illness use a more adaptive coping style, characterized by competence, optimism, and compliance. They display fewer behavior problems at school and at home.
Because it is often easier to recognize children who cope poorly with illness or disability, it is helpful to describe those behaviors typical of well-adjusted children. Well-adapted children gradually learn to accept their physical limitations.
Normalization: One of the most important interventions to promote coping is alleviating the child’s feeling of being different and normalizing his or her life as much as possible. The principles in the Nursing Care Guidelines box are fundamental in implementing the normalization process. The nurse can help parents assess the child’s daily routine for indications of normalizing practices. For example, the child who remains in a bedroom all day needs a restructured daily routine to provide activities in different parts of the house, such as eating in the kitchen with the family, and the inclusion of social, recreational, and academic activities in the care plan.
Children who are concerned that their condition detracts from their physical attractiveness need attention focused on the normal aspects of appearance and capabilities. Health professionals can help parents strengthen the child’s self-image by emphasizing the normal, while at the same time allowing children to express anger, isolation, fear of rejection, sadness, and loneliness. Parents should encourage anything that might improve attractiveness and contribute to a positive self-image, such as makeup for a teenager with a scar, clothing that disguises a prosthesis, or a hairstyle or wig to cover a deformity or lost hair.
The parent’s behavior, particularly in relation to childrearing, is one of the most critical influences on the child’s adaptation to chronic illness. For example, children who are raised by parents who establish reasonable limits are likely to develop independence that is appropriate for their age and achievement equal to their limitations. They frequently exhibit confidence and pride in their ability to cope successfully with the challenges resulting from their condition. On the other hand, children whose parents are overprotective are likely to show fearfulness, marked dependency, and inactivity and to have few outside interests. Using anticipatory guidance and encouragement of normalizing practices, the nurse may assist parents in facilitating positive adaptation in their children. Normalization is important because it focuses on the child, not the condition.
Nurses can demonstrate the process of normalization to the child’s family by acknowledging the strengths and weaknesses of the family unit, by being supportive and open about the child’s condition and treatment, and by actively including the family in all aspects of care (Shepard and Mahon, 2009). If the child’s family adopts a normalized view of management of the chronic illness, the child may be more confident in the home as well as in social and community situations. Thus the family’s perception of the impact and the integration of the chronic illness may directly or indirectly improve the child’s adaptation (Sullivan-Bolyai, Knafl, Sadler, et al, 2004).
Nurses also can assist parents by identifying and building on family strengths, promoting family and child competence, and fostering the development of a nurturing environment that addresses the needs of siblings and parents, as well as of the child with special needs.
Hopefulness: Children, especially adolescents, are sensitive to the presence or absence of hope. From a psychologic perspective, Erikson’s theory of psychosocial growth and development proposes that hope is a basic ego quality that is initially experienced in infancy and is the positive outcome of successful resolution of the developmental stage of trust versus mistrust (Ritchie, 2001).
Hopefulness helps protect the adolescent from incapacitating despair and assists the adolescent in coping with unmet personal needs. A sense of hopefulness can result in increased participation in health-seeking behaviors and an improved sense of well-being. Nurses can be instrumental in fostering hopefulness through environmental and interpersonal means (see Nursing Care Guidelines box).
Health Education and Self-Care: Health education teaches children self-care behaviors and self-advocacy skills for dealing with the health care community. These are important skills for children and adolescents with chronic conditions to master because they are likely to use the health care system frequently throughout their lives (Vessey and Mebane, 2009). Active participation in care requires comprehensive family and patient education. Empowerment of individuals with disabilities is the philosophy that is currently advocated for provision of services. Gaining access to information helps the individual make informed decisions and acquire some control over the environment.
Children need information about how the body works, the characteristics of their condition, the treatment plan, the impact of illness or therapy, and, when age-appropriate, the intricacies of the health care system. Education is a primary component of self-care, and teaching methods must be modified to meet the child’s developmental age. In addition, children near puberty need to understand the maturation process and how their disability may change this event. For example, the child with Crohn disease should know that this illness is linked with delayed puberty and growth failure. The child with diabetes needs to understand that increased growth needs and hormonal changes will change insulin and food requirements at this time. The sexually active girl with systemic lupus erythematosus or sickle cell anemia needs to be aware of the risks of pregnancy. The information should not be provided during a single teaching session but rather timed appropriately to meet the child’s changing needs, and it should be described and repeated as frequently as the situation warrants.
For young children the information presented needs to be concise, simple, and honest, even if the news is not positive. Answer questions openly, since children need answers to the questions they are able to ask. If they have no confidence in the answer provided or are ignored, the only alternative left to them is to relate their experience to something fantasized or seen on television. If young children state that they do not want to learn more, then respect their wishes.
Developing the judgment and expertise for participating in self-care of chronic illness or disability is a process that occurs gradually. Self-care necessitates negotiation between child and parents. Nurses are instrumental in providing information on strategies for teaching children of various ages in self-care.
Realistic Future Goals: Because medical advances have led to prolonged survival for children with many chronic illnesses, these individuals are confronted with new decisions and problems such as employment,* marriage, medical and dental care access, and insurance coverage. Adolescents usually look forward to what their lives will be like in the future.
For some chronic illnesses or severe disabilities, one of the most difficult adjustments is establishing realistic goals for the child and for those involved in the child’s continual care. Occasionally the impact of these decisions does not surface until the child graduates from school or the parents move toward retirement, when a crisis can arise because of disruptions in the family roles and relationships that maintained stability.
For children with severe disabilities, preparing for the future should be a gradual process. All along the child and parents should consider realistic vocational options. For example, children with physical disabilities can be directed to artistic, intellectual, or musical pursuits. Children with developmental disabilities can be instructed in manual skills. Thus the child’s development progresses to self-support through gainful employment.
Unfortunately, vocational pursuits and independence are not realistic goals for all individuals. Persons with multiple or severe disabilities may require lifelong care and assistance. In these situations parents must look to the time when they will no longer be able to care for their child. Advance financial planning should be considered. Residential placement may be difficult unless the family mutually participates in the decision-making and planning processes. Parents should not view care outside the home as abandonment. Often it is the only way to preserve the family unit. The nurse should help the family investigate suitable placements, discuss their feelings regarding this decision, and explore measures to maintain meaningful communication with the member who has a disability. The nurse can take a larger advocacy role in educating the public regarding persons with special needs and helping normalize the experience for the child, the family, and the community.
Determining readiness for transfer to adult providers is a primary consideration. Arbitrary transfer to adult services based solely on an age criterion can compromise both psychosocial and physical care for some young adults. Many adolescents have received care in the same medical setting since birth and have established a trusting relationship with practitioners and staff. Moreover, age is not an indicator of adolescent readiness for transfer to an adult care provider. Important factors include (Reiss, Gibson, and Walker, 2005):
• Knowledge of the condition and its management
• Readiness to assume responsibility for treatment management
• Prior involvement in and compliance with the treatment regimen
• Demonstration of responsible and independent judgment
Nurses can take steps to help the adolescent prepare for the transition. These include presenting the idea of transfer; assessing the readiness of the adolescent and parent; coordinating a meeting with the adolescent, the family, and both pediatric and adult care providers; and formally acknowledging the transfer (Reiss, Gibson, and Walker, 2005).
Nurses are instrumental in assisting and supporting adolescents in assuming responsibility for managing their own care as much as possible. Adolescents should actively participate in the planning and decision-making processes for transition to adult care. In addition, nurses can foster continuity of care by providing information to adult health care providers about the adolescent’s needs relating to disease management and his or her compliance with the treatment regimen. The ultimate goal of transition care to adulthood for the adolescent with a chronic illness is to promote the achievement of responsible self-care and linkages to adult health care services and thus to provide the best prospects for educational options, social networks and relationships, community living, and employment.
The Family of the Child with Special Needs
A major goal in working with the family of a child with special needs is to support the family’s coping and help them function as best as they can throughout the child’s life. Long-term, comprehensive, family-centered approaches extend beyond supporting the child and family during the crucial periods of diagnosis and hospitalization. Comprehensive care involves building parent-professional partnerships that can support a family’s adaptation to the many changes that may be necessary in everyday life, defining expectations of and for the child, and providing a long-term perspective (Box 22-3).
Assessing Family Strengths and Adjustment
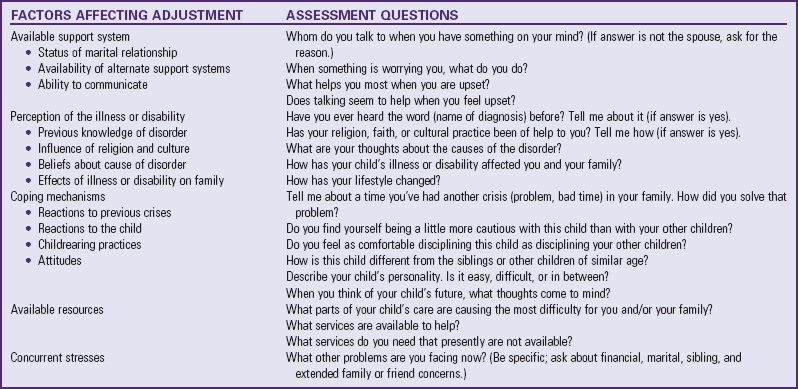
The purpose of a family assessment is to determine what assistance a family may need or want in managing their child’s care. Ideally the nurse should initiate an assessment as soon as the family learns the diagnosis. Integral to the family-centered care philosophy is the conception that the family should be an active participant in the process. Sample questions designed to elicit information for assessing the family’s adjustment are listed in Table 22-2. Family members should always be informed of the purpose of the assessment, including the rationale for asking personal questions. They should be afforded the opportunity to participate or not as they choose.
A number of instruments can be used to assess the family’s overall functioning and support system. In addition, specific tools have been developed for families of children with chronic illness or disability. For example, the Coping Health Inventory for Parents (CHIPTS) is an 80-item checklist that provides self-report information about how parents perceive their overall response to the management of family life with a child with a chronic illness. Coping behaviors (e.g., “believing that my child[ren] will get better” or “talking with the hospital staff [nurses, social workers] when we visited the medical center”) are listed, and parents are asked to rate how helpful the coping items are to them in managing the home situation. Chapter 25 describes tools that a family can use to assess the home environment and resources.
Regardless of the approach, assessment is a continual process. Because support systems and the perception of events may change at any time during an illness, nurses must assist families on an ongoing basis in evaluating the effectiveness of changes and interventions in support needs.
Accepting the Child’s Condition and Receiving Support at the Time of Diagnosis
The impact of a child’s developmental or medical condition is often experienced as a crisis at the time of diagnosis, which may be during birth, after a long period of psychologic and/or physical testing, or soon after a tragic injury. It may also begin before the diagnosis, when parents know that something is wrong with their child but there has been no medical confirmation.
Interventions facilitating the parents’ adjustment to the diagnosis of their child’s chronic illness or disability and their ability to care for their child include planning the setting for informing parents, assessing the family’s prior knowledge of and experience with chronic conditions (see Family-Centered Care box), selecting strategies that best meet the family’s needs and situation, evaluating the family’s understanding of the information presented, and providing ongoing follow-up. Effectively discussing the diagnosis provides a vital foundation for a strong collaborative relationship between parents and health care providers that will be needed in the future.
The physician or advanced practice nurse usually informs the family of the child’s diagnosis. Nurses are also responsible for providing follow-up information and coordinating services with other agencies. Whatever role nurses assume, they can follow the guidelines in the Nursing Care Guidelines box during disclosure of the diagnosis to offer the family support at this crucial time.
The informing conference should take place in a private, comfortable setting free of interruptions and distractions (Fig. 22-2). The environment should be one in which parents feel free to show their emotions. If parents can express their emotions openly, the nurse will be able to determine their need for additional counseling. Parents often sense a certain attitude of rejection, acceptance, hope, or despair that may affect their ability to assimilate the shock and begin adapting to the implications of the illness for their future.

Fig. 22-2 Informing sessions should take place in a private, comfortable setting free of distractions and interruptions.
The parents’ emotional needs at the time of diagnosis are acknowledged by exhibiting acceptance of such expressions as sadness, crying, disappointment, and anger. Emotional support is provided by having tissues available if a family member cries and by showing through body and facial language that indeed this is a painful and difficult time. Even though touching is a strong expression of empathy, it must be used cautiously. For example, it can prematurely terminate free expression of feelings, particularly when combined with statements such as, “Everything will be all right.” Nurses should also be cognizant of cultural sensitivity regarding touching. (See Chapter 2.)
Nurses should observe the responses of family members on hearing the diagnosis. Their facial expressions, their ability to maintain eye contact with the nurse, the times they look down, behaviors that indicate they are avoiding what the nurse is saying (such as turning their heads, looking away, or looking around), and any other activities that demonstrate they are dealing with a difficult matter are observed.
One of the most supportive interventions is to accept the family’s emotional reactions to the diagnosis in a nonjudgmental manner. Although all families react differently and with varying degrees of intensity, three reactions are common and are frequently poorly managed: guilt, denial, and anger.
Parents should receive the kind of information they want. Most parents prefer a simple, clear explanation of the diagnosis, including what is and is not known about the diagnosis, a prediction of possible prospects for the child, advice on what to do next, an opportunity to ask questions, a sympathetic and warm listener, and, most important, time. Determine the family’s level of understanding and expectations. Assess comprehension of explanations with questions such as, “Is this clear to you?” or “Do you see what I mean?” Take notes for the family to refer to in the future. Provide parents with supplemental written information or a written summary of the diagnosis in keeping with their emotional readiness.
A crucial task for parents is to decide when, what, and how to tell their child about the diagnosis. Like parents, children later remember vividly what happened when the diagnosis was disclosed. Ideally the parents should be responsible for sharing this information with their child. However, they need much guidance in communicating information about the nature of the illness and the changes imposed on physical appearance and energy using a calm and honest approach. This is because parents frequently use euphemisms and try to protect their child from the harsh realities of the diagnosis and illness. Nurses can promote open communication between parents and ill child by providing them with information about how young children think and respond to illness and to changes in their parents (crying or increased concern).
The informing conference should not only include the presentation of devastating news, but emphasize the child’s strengths and potential for development. Also assure the parents that the nurse will be available to answer questions and to provide further assistance as needed. Because of the need for long-term follow-up of chronic conditions, the initial informing conference is only one in a series of ongoing discussions. In all interactions the family’s input is requested and included in the care plan (see Nursing Care Guidelines box, p. 872).
Managing the Condition on an Ongoing Basis
Promoting the family’s adaptation to the day-to-day management of the child’s condition involves education about the child’s condition, general health care, and developmental needs and about realistic goal setting. Emotional support and assessment of the family also play a pivotal role in adaptation. Encourage families to articulate their goals and approaches to managing their children’s condition, which provides vital information on how to intervene more thoughtfully with families based on their treatment approach.
Because the majority of mothers and fathers of children with special needs have little or no experience with children who have chronic or disabling conditions, the nurse can remind them of their child’s many strengths and normal traits. Mothers and fathers need to experience happiness, success, and pride with regard to their child. The nurse can model appropriate interventions with the child. Most important, the nurse should ensure that the siblings and parents learn to perceive the child as a child first, with unique and individual needs and characteristics. The nurse needs to convey an accepting, humanistic attitude toward the child so that the parents can observe this acceptance. This attitude of having concern for, liking, and demonstrating acceptance of the child should begin in early infancy and continue throughout the child’s life.
Special Information Needs
Educating the family about the child’s condition is actually a continuation of the diagnostic talk (see Nursing Care Guidelines box, p. 859). Education involves providing technical information regarding management of the condition, such as how to administer insulin injections, and assessing both parental skills and understanding. In childhood cancer, educational components may include understanding and following a chemotherapy protocol, administering chemotherapy medications at home, anticipating and treating side effects, managing the child’s adjustment to the illness, and arranging support and care from home health agencies and community resources (Hockenberry and Kline, 2010). Discussions with parents must also address the impact of the condition on the child. For example, children who have lost a limb require more than an explanation about the prosthetic leg. They need to know what restrictions it imposes on their activity level and how to function with it.
Parents also need guidance on how the child’s condition may interfere with activities of daily living, such as dressing, eating, toileting, and sleeping* (see Family-Centered Care box). Common nutritional problems include overnutrition, which results from a caloric intake in excess of energy expenditure and may be related to boredom and lack of stimulation in other areas, and undernutrition, usually caused by inappropriate restriction of food, vomiting, loss of appetite, increased metabolic needs, or motor deficits that interfere with feeding. Although the child has the same basic needs as other children, the daily requirements may vary. Special nutritional considerations are discussed throughout the text.
Another major area in which modifications are necessary is car transportation. Children with conditions such as orthopedic, respiratory, or neuromuscular problems or low birth weight often cannot safely use conventional car restraints. For example, children with hip spica casts are unable to sit properly in child safety seats. (See Developmental Dysplasia of the Hip, Chapter 11.) Alterations can be made to some commercial models,† and for older children a special vest‡ is available that secures the child in a lying-down position to the back seat. Children in wheelchairs present special challenges because the wheelchair should be anchored with four points of attachment to the vehicle (two in front and two behind) and should always face forward. The family should contact the wheelchair manufacturer for specific instructions to ensure safe car transportation.
Children with special needs require the usual primary health care recommended for any child. Anticipatory guidance, including attention to immunizations, injury prevention, dental health, and regular physical examinations, is important. Nurses play a pivotal role in reminding parents regarding these issues that are so frequently neglected when the concern is focused on the child’s specific illness or disability. (See General Approaches Toward Examining the Child, Chapter 6, for information on assessing the general aspects of health maintenance. Specific discussions of sleep and activity, nutrition, dental health, and injury prevention are presented in the chapters on health promotion for particular age-groups. See Chapter 12 for a discussion of immunizations.)
Parents also need to be aware of the importance of communicating the child’s condition in the event of an emergency. Young children are unable to give information regarding their condition, and older children may be unable or unwilling to speak after an accident. Thus all children with any type of chronic condition that may affect medical care should carry some type of identification, such as a medical alert bracelet (www.medicalert.org), which lists the medical condition and a collect telephone number for access to emergency medical records and other vital information.
Family Management Styles
Families who have a child with a chronic illness often face multiple challenges. This includes making sense of the illness in regard to its meaning for their life, mastering demanding treatment regimens, accommodating the family budget and routine to the demands of the illness, creating a normal life for the child despite the illness, and negotiating with school and health care professionals.
Family management style is the configuration formed by individual family members, the management behaviors they engage in with regard to the chronic condition, and the sociocultural context in which these behaviors occur (Shepard and Mahon, 2009). Five distinct family management styles have been identified: thriving, accommodating, enduring, struggling, and floundering.
Thriving and accommodating families perceive the condition and the child as “normal.” Parents are confident in their ability to manage the illness; children see themselves as “healthy.” Accommodating families differ from thriving families in that they perceive their situation as essentially normal but view it somewhat more negatively. They also take a more compliant approach to illness management. Enduring families view having a child with a chronic illness as difficult and as having major consequences for family life, and describe illness management as a burden. In contrast to families with thriving and accommodating management styles, these families perceive their child as a tragic figure, someone whose life chances have been irreparably compromised because of the illness, and are more protective of the child. Struggling families are characterized by conflict over how best to manage their child’s condition. Struggling parents perceive less support and mutuality from one another; this is especially true of mothers, who feel that they receive inadequate support from their spouses in illness management. In floundering families the overriding theme is confusion. Parents view the illness negatively and perceive the child as a tragic figure. They are uncertain about the best management approaches, and they view illness management as burdensome and difficult (Shepard and Mahon, 2009).
Understanding the various ways in which families may respond to a chronic illness—specifically, how they define the situation, manage daily life, handle conflict, and work jointly—can help nurses develop interventions tailored to the unique problems individual families encounter in managing the illness and the strengths on which they can draw. Tailored interventions may best foster optimal adaptation (see the discussion of coping strategies, p. 867).
Meeting the Child’s Normal Developmental Needs
General strategies for meeting a child’s normal developmental needs in both the home and school settings include normalizing practices such as emphasizing abilities, deemphasizing limitations, structuring the environment to promote age-appropriate development, and providing appropriate discipline (see earlier discussion of these issues under Impact of Chronic Illness or Disability on the Child, p. 849).
For parents the task of meeting the child’s normal developmental needs is integrally related to accepting the child’s condition. Thus helping a family become aware of their reactions to the diagnosis and their reactions to managing the condition can help them evaluate their readiness to support the child’s needs (see Table 22-2 for assessment questions).
While questioning parents about their reactions and understanding, the nurse can help them focus on the child’s and sibling’s knowledge of the condition. It is not uncommon for parents who appear knowledgeable and well adjusted to acknowledge that they have never told the children the truth about the illness. Conflict arises when the siblings or child learns of the diagnosis from nonparental sources. Parents may need assistance in deciding how best to explain a condition to children of various ages. (See Awareness of Dying in Children with Life-Threatening Illness, Chapter 23.)
Special challenges are present when assessing children’s feelings about having a disability. The discussion on communication techniques in Chapter 6 focuses on a number of approaches to encourage children to discuss feelings regarding their diagnosis and future. For example, using play and drawing as a method of communication is appropriate for any child dealing with difficult feelings or a child who lacks verbal skills.
School is the second most important setting for a child. Teachers have a profound influence on the child’s developmental progress, learning ability, feelings of self-esteem, and formation of social relationships. Whenever possible, nurses should ask parents for permission to visit the school to observe the child’s interaction and behavior with classmates and teachers. A summary of objectives for home and school visits is given in the Nursing Care Guidelines box.
Meeting Developmental Needs of Other Family Members
Each family that has a child with special needs is affected by the experience. The effects on the parents and their responses are so critical that they directly influence the other members’ reactions and the child’s own coping.
Parents
Grieving for the loss of a perfect child and managing the demands of caregiving can place many strains on parents (Box 22-4). In addition, parents may or may not receive positive feedback from interactions with their child. Many parents of children with special needs feel satisfaction and fulfillment from the parenting role. Adequate information, parent-to-parent support, collaboration with health care providers, and other resources can support and empower many parents. However, for others, parenting a child with a disability or chronic illness may be a series of unrewarding experiences that continually undermine the parents’ feelings of adequacy and competence. These responses may be most evident in parents who are responsible for the child’s care. For example, they may become preoccupied with their ability to carry out certain procedures, perhaps overlooking the child’s personal comfort and satisfaction or failing to offer praise for anything less than perfect cooperation or performance. For these parents several strategies may be helpful: education regarding what can reasonably be expected of their child, assistance in identifying the child’s strengths, praise for a parental job well done, and help in finding respite care so that the parent can renew his or her own energies.
Parental Roles: Caring for a child with chronic illness or disability may place tremendous demands on the parents’ energy, time, and financial resources. In many cases the mother performs the bulk of the traditional child care and household responsibilities, and the father shoulders the financial responsibilities. However, with changing gender roles these responsibilities may be shared, and parents may divide the tasks according to their level of comfort or skills. For example, the parent with patience for waiting may be the logical person to bring the child for tests, procedures, and examinations. In contrast, the parent who deals best with the illness and side effects of therapy can prepare the home for the child’s return. On the other hand, involving both parents in decision making and in education regarding the care of the child with special needs can decrease some of the burden of care often placed inadvertently on mothers.
In some families, changing gender roles signify additional responsibilities for one parent. For example, the working mother may feel the need to remain employed to help pay expenses, but this adds to the burden of increased home and child care responsibilities. This may result in conflict, because one parent may perceive an unequal sharing of tasks with the partner.
In addition, the parent who is not involved in the caregiving activities may feel neglected because much attention is directed toward the child and resentful that he or she is not adequately informed to be competent in the care. Without active participation in the care of the child, the parent may have little understanding of the time and energy needed to perform those activities. When the less competent parent makes an effort to become involved, the other parent often criticizes the less skillful efforts. As a result, communication may break down, and neither is able to support the other.
Nurses can help parents avoid role conflict by providing anticipatory guidance early in the child’s diagnosis. Teaching should address the stressors often identified as having an impact on the marriage: (1) home care with the burden assumed primarily by one parent, (2) the financial burden, (3) fear of the child’s dying, (4) pressure from relatives, (5) the hereditary nature of the illness (if applicable), and (6) fear of pregnancy. Other causes of marital stress may concern the inconveniences related to care, for example, long waiting times for appointments, lack of overnight accommodations, and lack of parking near health care facilities. These stressors are certainly within the realm of health care professionals to minimize, if not eliminate, for parents.
Mother-Father Differences: Clarke, McCathy, Downie, and colleagues (2009) recently published a systematic review of 30 articles on gender differences in role perceptions; illness beliefs; psychologic distress; coping strategies; and perceptions of marital, family, and child functioning. Findings in relation to parent psychologic distress and preferred coping strategies were mixed, with trends toward increased distress, more emotion-focused coping, and greater need for social support in mothers.
To foster communication between parents who are adjusting to their child’s chronic illness, the nurse can encourage them to recognize and accept differences in coping behaviors. This may increase mutual support and effect positive outcomes for their child’s care.
Fathers: Fathers of children with chronic illness or disability face formidable challenges that are distinct from those of mothers (see Research Focus box). Fathers must reexamine priorities, come to terms with losses, and develop and strengthen caretaking abilities. Many fathers experience feelings of guilt and failure and may suffer from isolation because fewer social supports are available for men than for women. Feelings of isolation can be intensified by a health care system that frequently excludes, disenfranchises, and disregards men. Nurses can be instrumental in helping fathers of children with special needs overcome these challenges by addressing their concerns and engaging them in becoming supportive and important figures in the lives of their children (see Nursing Care Guidelines box).
Because the traditional paternal role, particularly with sons, emphasizes joint recreation over caregiving, fathers appear to have more difficulty adjusting to a son with special needs than to a daughter with special needs. With today’s increasing emphasis on fathers’ involvement in the lives of their children, this loss is felt more profoundly than in the past. However, fearful of losing control or being perceived as ineffectual or weak, a father may hide his feelings and exhibit an outward confidence that can lead others to believe that everything is fine (Goble, 2004).
Traditionally the mother and child have actively participated in and received professional care, whereas the father and siblings have been excluded. However, for the family unit to achieve optimum functioning, each member must be included. This means scheduling home and office visits at times when other family members can be present, which may dictate early morning, early evening, or late afternoon hours. Fathers often adjust their work schedule to meet with a health care professional once an invitation is offered.
Approach the task of including other members of a family in a visit positively. If they have not been included in the past, they may view such an invitation as a sign of more bad news or an indication of their own problems. One approach for welcoming others to participate is to remark that, after hearing so often about the father and the other siblings, the nurse wishes to meet them. This carries a friendly connotation and is nonthreatening.
Single-Parent Families: The field of pediatric chronic illness has not kept pace with the demographic changes that now characterize our society, changes that have the potential to profoundly affect child and family functioning (Brown, Wiener, Kupst, et al, 2008). Single-parent families of children with special needs are of particular concern. The proportion of children in two-parent families has decreased from 85% to 69% in the last 30 years; thus nearly 3 in 10 children live in single-parent homes (Shudy, de Almeida, Ly, et al, 2006). A parent may be absent due to death, divorce, or the parents never having married. Make special efforts to assist the single parent in obtaining support and financial services that can lessen the burden of care. Nurses can also be advocates for the single parent by suggesting helping roles for which friends and relatives can be enlisted. Some single parents are reluctant to join support groups because they feel out of place if the group is largely composed of married couples. Nurses need to assist single parents in mobilizing a positive social support network and must be empathetic to the concerns of single parents by locating appropriate resources to meet their needs.
Foster or Adoptive Families: Foster or adoptive families may benefit from information and support to encourage effective early adaptation to a chronic illness or developmental disability in the child. Information on the child’s condition, unique needs, available services, warning signs of problems, and sources of both respite and support care can assist families in coping. Supporting foster families may promote longer-term placements or adoption of children with special needs.
Siblings
Many parents express concern regarding when and how to inform the other children in the family about the disability of a newborn sibling. The answer depends on each child’s level of understanding and sophistication. Adolescents and even younger siblings routinely use the Internet to obtain information. What siblings piece together or overhear is often much worse than the truth. Often they imagine gruesome things regarding the experiences related to a sibling’s illness, treatment, and hospitalization (Shepard and Mahon, 2009). Health care professionals need to anticipate questions and provide answers to children about the medical condition of their siblings in an age-appropriate manner that respects their constant need for information. Children need to be informed throughout the course of their sibling’s illness. Parents are usually in the best position to impart this information, although they are often overwhelmed with the medical crisis at hand (Fleitas, 2000). Nurses can encourage parents to talk with the siblings about how they perceive their sick brother or sister and to be accepting of the siblings’ feelings. Provisions should be made to allow siblings to visit the child in the hospital.
Nurses also can provide information to parents about teaching children of various ages and developmental stages. If the parents are unable to talk to the siblings, it is essential to find someone else who can do so in an appropriate manner. Nurses are ideal individuals to educate and counsel siblings during the course of their brother’s or sister’s illness (Shepard and Mahon, 2009).
Siblings must be prepared for the physical changes that their brother or sister will experience and for the possible role changes occurring in the family. Siblings must realize that their concerns, thoughts, and questions are important and acceptable. This includes jealousy toward the sick child and feelings of anger toward their parents. Siblings need reassurance that they will be kept abreast of their brother’s or sister’s treatment progress and, when possible, be involved in the care. When treatment necessitates parental absence from home or hospitalization of the sick child, a regularly scheduled time should be arranged for the siblings and parents to speak by telephone. This helps decrease separation anxiety and allows the siblings a sense of consistency, belonging, and involvement in the sick child’s care (see Critical Thinking Exercise).
Some siblings, particularly younger male or older female children, develop behavior or adjustment difficulties. Younger children tend to become irritable and withdrawn, whereas older siblings tend to act out. Some common difficulties include bed-wetting, headaches and other physical complaints, school phobia, changes in school performance, proneness to injury, sleep problems, depression, and severe separation anxiety.
Some problems for siblings arise from demands imposed by the child’s condition. For example, at diagnosis the child with special needs by necessity becomes the focus of parental concern and attention. Frequent visits to a health care facility or hospitalizations disrupt the family routine. Siblings are pushed to the background, often staying at the homes of friends and relatives. The affected child’s condition may interfere with vacations, holiday celebrations, and other special events. Siblings may resent these intrusions, which often require self-sacrifice. For a while parents may miss the siblings’ ball games, school functions, or other activities and at times may be emotionally and physically unavailable to them. The family’s emotional and financial resources may be directed toward the child with special needs. When this happens, there is often not only a decrease in normal family activities but a decrease in personal items and attention for the other children as well. Feelings of jealousy, anger, and resentment are not uncommon (see Research Focus Box). Siblings may worry about “catching” the condition or worry that playing rough with their brother or sister or even thinking bad thoughts about the sibling caused the condition. Nurses need to reassure siblings that their emotions are acceptable, but correct any misconceptions.
Feelings of resentment are also reported by siblings when their brother or sister with special needs becomes the focus of parental attention or is overprotected, indulged, or permitted to exhibit unacceptable behaviors. Parents may not realize that they are applying different standards to their children or they may feel that the child’s condition calls for leniency.
Discipline provides structure and limits and should be consistent between siblings and within families (see Family-Centered Care box). When a child becomes seriously ill or disabled, the entire family is affected and role changes occur. Siblings, particularly older sisters, are often asked to assume increased responsibilities.
When children have complex disabilities or medical needs, particularly those that involve some degree of physical difference (e.g., hair loss), siblings must cope with the responses of others to these differences in appearance or behavior. This causes embarrassment for the siblings; however, at the same time they want to protect their brother or sister from the sarcastic remarks or stares of others (Fleitas, 2000). Having a child in the family who is disfigured, ill, or disabled labels the family as “different” (see Family-Centered Care box). When siblings perceive an illness to be life threatening, the power of the unspoken sibling bond is manifested. The child may demonstrate feelings of sadness when their future together as siblings is threatened. Finally, siblings report confusion arising from lack of information and poor communication with them about their brother’s or sister’s condition (Fleitas, 2000).
Often overlooked is the positive caring that exists between children with special needs and their brothers and sisters. Siblings feel pride and satisfaction in their own contributions to the family, happiness and excitement in their brother’s or sister’s achievements, and genuine love. Some siblings express that they sense more closeness in their families.
Research has shown positive aspects of sibling resilience when a child is ill. Children in families in which a sibling has a disability exhibit greater independence and maturity than do their peers. These children acknowledge feeling good about themselves and are proud of their patience and sense of responsibility. They also have a great appreciation of family closeness and health (Fleitas, 2000). Parental attitudes about the child and efforts promoting normalization are crucial in the development of positive reactions in siblings.
Nurses must be aware of and responsive to the reactions of siblings to their brother’s or sister’s illness or disability. Screening for sibling social support, mood, and self-esteem, both at the time of diagnosis and periodically, may help prevent mental health problems in siblings.
Focusing on strengths rather than problems requires nurses to impart an appreciation of how family members proceed with their lives despite the presence of a child with a chronic illness. Whenever possible, nurses need to intervene to foster positive adaptation. Siblings often state that they are expected to assume additional responsibilities to help parents care for the child. It is not unusual for them to display a positive reaction to taking on the extra duties but a negative reaction to feeling unappreciated for doing so. The nurse can help minimize such feelings by encouraging the siblings to discuss this with the parents and by advocating ways of showing gratitude, such as an increase in allowance, special privileges, and, most important, verbal praise (see Family-Centered Care box).
Extended Family Members and Friends
In addition to parents and siblings, a child’s chronic illness or disability can have an impact on significant family members or friends. Although extended family relationships are often helpful to parents in rearing a child with special needs, they may also be sources of stress. For example, grandparents or other well-meaning relatives may attempt to reassure the parents that the child “will grow out of” his or her slowness at a time when parents are struggling to accept reality.
The nurse must be aware of the family’s cues concerning sources of stress from extended family members such as grandparents. Encourage parents, when appropriate, to provide literature or to invite the grandparents to be present during one of the child’s visits to the outpatient health care facility during the diagnostic period or during a conference with the health care team. Including grandparents in a discussion in which they can share their concerns may assist them in coping with their feelings and thereby lessen stress on the entire family. Grandparents may adapt even less well than parents because they lack adequate information, have limited involvement in decision making, and have less responsibility for the child’s care. Often they feel helpless to provide assistance. Grandparents’ feelings of anger and blame should be openly discussed. Grandparents can be helped to understand the impact of their behavior on the family with an appropriate statement such as, “Your son is presently experiencing a lot of pain and anguish. We realize that this is difficult for you, as well as your son; however, you can be of great help by being supportive of him.”
Most grandparents experience some ambivalence because they love their grandchild yet feel personal disappointment when a diagnosis is made. They often experience two types of grief: for their grandchild who is ill and for their child, the parent, who is suffering. The future is now unpredictable, not only for the grandchild but for the child’s parents as well. Behavioral disturbances such as poor decision making, disorganization, and disorientation, already seen in some older adults, may be intensified during grief. Grandparents do not often admit these emotions, and they are left to adjust on their own. Although support groups for grandparents are uncommon, they can be helpful. Special support may be needed for the grandparent assuming the role of a primary caregiver for the child.
Significant stress can also arise from nonfamilial sources, such as neighbors, friends, or strangers. Neighbors display various reactions to the child’s diagnosis. Some turn away, some pry, and some ask inappropriate questions or make insensitive remarks. Inability to deal with comments about the condition or curious stares by others may promote the tendency to protect and isolate the child in the home. The family needs guidance in preparing for these inevitable encounters. One approach is encouraging parents to dress the child as much as possible like his or her peers. Good grooming is extremely important in minimizing differences in appearance. Through role playing, parents can rehearse responses to comments such as, “Is your child retarded?” or “Has he always been crippled?” Parent groups can allow family members to share experiences and learn from each other about dealing with unkind remarks or probing questions. They also provide a type of support parents cannot obtain from relatives, friends, and neighbors.
Some neighbors and friends will not allow their children to play with the child or siblings for fear of contagion or formation of a close friendship with a child who might die. For some parents friendships may be difficult to maintain because they have little time and energy for social gatherings. Friends may withdraw for a number of reasons, such as being uncomfortable with the situation and feeling unable to help.
Parents have to decide how much and what to tell relatives, friends, baby-sitters, and teachers. Concerns regarding discrimination are very real for parents and must be balanced with the need to share information so that the child receives proper care.
Nurses can address the issue of discrimination by asking parents if they have worries about how to inform others of the child’s condition. Intervention strategies not only must focus on problems confronting children and families but also must discreetly consider the many sources from which discrimination may develop. Nurses may also be able to provide suggestions regarding essential education for others who will care for the child.
Coping with Ongoing Stress and Periodic Crises
Families of children with chronic conditions face ongoing stress associated with factors such as the child’s condition and financial concerns (see Box 22-4). They also may undergo periodic crises, including uncertainty regarding the diagnosis and the need to cope with recurrent hospitalizations. Some families are strengthened by being able to deal with these stresses. Others become overwhelmed when stresses exceed resources. The increasing stress can overwhelm family resources and result in a financial crisis (Goble, 2004). Concurrent stresses such as out-of-pocket expenditures related to the chronic condition pose additional challenges (Newacheck and Kim, 2005).
Health care professionals can assist families in coping with stress by providing anticipatory guidance, offering emotional support, helping the family to assess and recognize specific stressors, assisting the family in developing problem-solving strategies and coping mechanisms, continuing efforts to meet developmental needs, encouraging spiritual beliefs to find hope and meaning, and working collaboratively with parents so they become empowered in the process.
Concurrent Stresses Within the Family
The ability to cope with the overwhelming stresses of a lifelong illness or disability is challenged further when additional stresses are present. Ongoing stresses and strains in the family accumulate, increasing the family’s vulnerability and lessening its ability to adapt to a child with special needs. For some family members, non-illness-related stressors are perceived as more stressful than those related to a child’s chronic condition.
Stressors may be developmental or situational. They may be associated with sibling needs, marital discord, homelessness, or social isolation. Even the more minor stresses, such as managing the home, arranging care for siblings, and commuting to distant treatment centers, can challenge a family’s ability to cope successfully (see Box 22-4).
Family or child developmental stressors exacerbate situational stresses. For example, a common developmental stressor in the family life cycle is the birth of a child, an event that necessitates adjustment by the parents. The birth of a child with a congenital health problem adds situational stress to the equation.
The majority of families, regardless of their insurance coverage or income, have financial concerns. The costs of caring for a child with special needs can be overwhelming. Children with functional limitations account for one third of child hospital days, and their hospital stays are twice as long; they also visit physicians twice as often as children without limitations. Direct medical expenses, transportation costs, nonprescription medication, wigs or cosmetics to conceal the effects of the illness or treatment, parking, meals, housing, and child care can consume a high percentage of a family’s income.
Additional loss of family income occurs when parents take time off work or quit a job to care for a child.* The family breadwinner may also have to sacrifice career opportunities to remain close to the child’s treatment center.
Nurses can make appropriate referrals to case managers and social workers to assist a family in reviewing various options for financial assistance, including insurance, health maintenance organization or managed care policies, Medicaid, the Supplemental Security Income (SSI) program, Women, Infants, and Children (WIC) program, the state program for children with special health needs, disease-related associations, and local philanthropic organizations.
Coping Mechanisms
Coping mechanisms are those behaviors directed at reducing the tension elicited by a crisis. Approach behaviors are coping mechanisms resulting in movement toward adjustment and resolution of the crisis. Avoidance behaviors result in movement away from adjustment or maladaptation to the crisis. Several approach and avoidance behaviors used in coping with a chronic illness or disability are listed in the Nursing Care Guidelines box. None of the indicators can be used alone to assess possible success or failure in resolving the crisis. Each behavior must be seen in the context of all of the variables influencing the family. For example, the observation of many avoidance behaviors in an emotionally healthy family may indicate significantly less risk to the successful resolution of the crisis than an equal number of avoidance behaviors in an individual who has few available supports.
Two long-term coping strategies of familial adaptation to severe and chronic childhood illness have been found to be significantly related to a high level of family functioning. The first is the parents’ ability to assign the illness meaning within an existing medical-scientific or spiritual philosophy of life. They have an optimistic belief that things work out for the best and an emphasis on the positive qualities of the situation. Statements such as “God has chosen our family to care for this special child” reflect the religious philosophy.
The second long-term coping strategy of family adaptation is an ability to share the burdens imposed by the illness with individuals both inside and outside the family network. Intrafamilial relationships promote togetherness of the family members and support a mutual recognition that all members are vital contributors to the family unit. Extrafamilial supports help preserve meaningful external contacts and provide needed assistance to the family.
The chronic illness trajectory model recognizes that chronic conditions have a course that changes over time (Corbin and Strauss, 1995). The course of the illness is influenced by several psychologic and medical factors, including resources (interpersonal, intrapersonal, and instrumental), technology, motivation, experience, the type and severity of the illness, lifestyle, and the social climate. Most chronic illness management occurs in the home, not in the hospital. This model advocates that the goal of nursing care in chronic illness is to assist the family in shaping the course of the illness medically while maintaining quality of life for the child and family. This is achieved through assessment, teaching, monitoring, and initiation of referrals.
Fostering normalization, teaching coping skills, and assisting the family in using or further defining their social support networks are other nursing interventions that can encourage and empower the parents and promote positive adaptation in the family and optimum mental health for the child.
Parental Empowerment
Empowerment can be viewed as a personal process through which individuals develop and use the necessary knowledge, confidence, and competence to make their voices heard. Nurses can provide resources and support to parents of chronically ill children based on their individual level of empowerment. Nurses can also encourage parent membership on staff, boards, and committees and include parents in presentations at conferences and meetings. Nurses can help keep parents abreast of pending legislation on child health issues and take action when appropriate.*
Assisting Family Members in Managing Their Feelings
Considerable individual variation is seen in reactions to the diagnosis, use of defense mechanisms, and time frames for coming to terms with a diagnosis. It is imperative that professionals recognize and respect the vast range of reactions and coping mechanisms. In fact, members of a family of a child with chronic illness or disability may experience many difficult emotions, such as guilt, fear, anger, resentment, and anxiety (see Nursing Care Guidelines box). Support from health professionals, extended family members, and friends can help family members deal with their feelings. When parents are able to cope successfully with the stress of caring for their disabled child, all family members experience positive outcomes such as a sense of increased love and warmth within the family, discovery of meaning for one’s life, a strong sense of having done a good job parenting, a sense of pride in the disabled child’s achievements no matter how small, and discovery of meaning in the presence of a disabled child in the family.
Shock and Denial
The initial diagnosis of a chronic illness or disability is often met with intense emotion characterized by shock, disbelief, and sometimes denial, especially if the disorder is not obvious, such as in chronic illness. Denial as a defense mechanism is a necessary cushion to prevent disintegration and is a normal response to grieving for any type of loss. Probably all family members experience various degrees of adaptive denial as they learn of the impact that the diagnosis has on their lives.
Shock and denial can last from days to months, sometimes even longer. Manifestations of denial that may occur at the time of diagnosis include (1) physician shopping; (2) attributing the symptoms of the actual illness to a minor condition; (3) refusing to believe the diagnostic test results; (4) delaying in agreeing to treatment; (5) acting happy and optimistic despite the revealed diagnosis; (6) refusing to tell or talk to anyone about the condition; (7) insisting that no one is telling the truth, regardless of others’ attempts to do so; (8) denying the reason for hospital admission; and (9) asking no questions about the diagnosis, treatment, or prognosis. Generally, these behaviors should be respected as short-term responses that allow individuals to protect themselves from a tremendous emotional impact and to collect and mobilize their energies toward goal-directed, problem-solving behaviors.
In some instances, various indicators of denial can actually be adaptive behaviors. Searching for another professional opinion may mean that parents cannot obtain answers to their questions or that they are looking for a different approach to treatment that better meets the needs of their child and family. When parents discuss their strengths and the benefits they derive from caring for their child with special needs, it does not necessarily reflect refusal to accept their difficult circumstances. Sometimes a delay in making decisions or a failure to ask questions simply reflects a lack of information.
Families with children who have life-threatening conditions commonly exhibit partial denial, such as seeking additional professional consultations or occasionally acting as if nothing were wrong. Without such a temporary protective mechanism, few people could survive the constant emotional drain of anticipating their own death or the death of a family member. Partial denial allows the child and family to absorb stressful information or “dose” themselves in amounts they can personally manage at the time.
In children denial has repeatedly been demonstrated as an important factor in their positive coping with the diagnosis. Denial allows the child to maintain hope in the face of overwhelming odds and to function adaptively and productively. Like hope, denial may be an adaptive mechanism for dealing with loss that persists until the family or patient is ready or needs other responses.
Denial is probably the reaction that is least understood and most poorly handled. Health care professionals commonly label denial as maladaptive and act inappropriately by attempting to strip it away through repeated and often blunt explanations of the prognosis. Because denial is based on fear, nurses need to address parental feelings of inadequacy. It is imperative that health professionals understand that denial is a necessary coping mechanism.
Denial becomes maladaptive only when it impedes recognition of treatment or rehabilitative goals essential for the child’s optimum development or survival. For example, protracted denial may be evident in the response of a family to cognitive impairment. As long as the family can maintain a function of normality and manage the difference within the existing familial values and roles, they may not recognize the diagnosis. Rather, the problem is explained as an easily treated condition or as slow maturation. The child’s social development may strengthen the denial, which disguises the degree of speech and motor impairment. Not uncommonly, this ability to rationalize delayed development is successful until the child begins school and is compared with other children, which makes his or her differences apparent. At this point the family may start to perceive the illness as a crisis and respond with shock and disbelief. Denial is no longer beneficial to the family, and other coping mechanisms must be used.
Adjustment
For most families, adjustment gradually follows shock and is usually characterized by an open admission that the condition exists. Adjustment may be accompanied by a number of responses that are normal components of the adaptation process. Perhaps the most universal of these feelings are guilt and self-accusation. Guilt is often greatest when the cause of the condition is linked directly to the parent, such as in genetic disorders or accidental injuries. However, it can arise even without any realistic or scientific basis for parental responsibility. Often the guilt develops from a false assumption that the disability is a result of personal wrongdoing or failing, such as not doing something correctly during the pregnancy or the birth. Guilt may be associated with religious or cultural beliefs as well. Some parents are convinced that they are being punished for some earlier misdeed. Others may perceive the condition as a sacrifice required by God to test their religious faith and strength. With appropriate information, support, and time, most parents deal with self-accusation and guilt. The ability to cope with resentful and self-accusatory feelings of having “caused” the child’s condition is a critical factor in determining the parents’ acceptance of their child.
Children also may perceive their serious illness as retribution for past misbehavior. The nurse should be particularly aware of the child who passively accepts all painful procedures. This child may believe that such acts are inflicted because of deserved punishment. It is always best to assure children that the goal during diagnosis or treatment is to make them feel better.
Other common reactions to a diagnosis of chronic illness or disability are anger and bitterness. Anger is a normal and expected reaction to chronic illness that arises when an individual realizes that certain needs, wishes, and plans for the future can no longer be satisfied due to limitations imposed by an illness. An intense feeling of unfairness consequently leads to feelings of frustration and anger. Anger directed inward may be manifested as punitive or self-reproaching behavior, such as verbally degrading oneself and neglecting one’s health. In contrast, anger directed outward may be revealed in either open arguments or withdrawal from communication with several individuals, such as the child, siblings, and spouse. Passive anger toward the child may be manifested in refusal to believe how sick the child is, inability to provide comfort, or decreased visiting. Among the most common targets for parental anger are members of the health care team. Parents may complain about the lack of time physicians spend with them, the nursing care, or the lack of qualified individuals to draw blood or start intravenous infusions (see Critical Thinking Exercise).
Children are likely to respond with anger, and this includes the ill child and the healthy siblings. Children are aware of the loss caused by their illness or disability and may react angrily to the feelings of being different from their peers or to the limitations instituted. Siblings may also feel resentment and anger toward the ill child and parents for the loss of parental attention and daily routines in the home. It is difficult for older children and almost impossible for younger children to understand the plight of the ill child. Their perception is of a sister or brother who has the undivided attention of their parents, is showered with toys and other gifts, and is the focus of everyone’s concern.
Children of various ages exhibit anger differently. Young children may display their uncooperativeness by screaming, yelling, and physically fighting off the adversary. In contrast, older children use abusive language. Passive anger, expressed in such statements as “I don’t know” or “I don’t care,” usually elicits anger in others and may be misconstrued as an obnoxious, sullen, or hostile response. As a result, these statements are effective in keeping people at a distance, when the hidden message really is “I need to talk. Please help me understand what is happening.”
During the period of adjustment, four types of parental reactions to the child affect the child’s eventual response to the condition: (1) overprotection, in which the parents fear allowing the child to achieve any new skill, avoid all discipline, and cater to every desire to impede frustration; (2) rejection, in which the parents detach themselves emotionally from the child but usually constantly nag and scold the child and provide adequate physical care; (3) denial, in which the parents act as if the condition does not exist or attempt to have the child overcompensate for it; and (4) gradual acceptance, in which the parents place realistic and necessary limitations on the child, foster reasonable social and physical activities, and promote self-care. Overprotection (Box 22-5) is such a common parental reaction that it behooves the nurse to assess for its presence and to begin anticipatory guidance with the family when appropriate. Many of these characteristics are also seen in the vulnerable child syndrome and could occur or persist should the child recover from injury or illness. (See Chapter 10.)
Reintegration and Acknowledgment
For many families the adjustment process concludes in the development of realistic expectations for the child and reintegration of family life with the disability or illness in a manageable perspective. Because a significant portion of this phase is one of grief for a loss, total resolution is not possible until the child dies or leaves home as an independent adult. Thus one can regard adjustment as “increased comfort” with day-to-day living rather than as a complete resolution.
This adjustment phase also involves social reintegration in which the family broadens its activities to include relationships outside the home, with the child as a participating and acceptable member of the group. This latter criterion often distinguishes the reaction of gradual acceptance during the adjustment period from total acceptance or possibly is more descriptive of the acknowledgment process.
During the acknowledgment phase of adjustment, individuals take stock of what remains rather than focusing on what is lost and begin to establish new goals for their lives. It is a time when the family is particularly motivated to learn about the restrictions imposed by the child’s illness and to decide how they want to function within those confines. Nursing interventions that emphasize self-control are particularly beneficial because they promote the highest level of function possible and increase a sense of self-worth.
Many parents of children with special needs experience chronic sorrow, an emotional reaction exhibited throughout the span of the parent-child interaction. Chronic sorrow occurs while parents redefine parental expectations and the parameters for appraising the child’s achievements. External events, such as the passage of a child’s expected date of graduation, trigger resurgences of chronic sorrow when the parent is again reminded of what could have been.
Establishing a Support System
The diagnosis of a serious health problem or disability in a child is a major situational crisis affecting the entire family. However, families can experience positive outcomes while they successfully cope with the many challenges that accompany a child with chronic illness or disability. One nursing goal is to assess which families are at lesser or greater risk for succumbing to the effects of the crisis. A number of variables, including available support systems, reactions to the child, perception of the illness or disability, coping mechanisms, available financial resources, and concurrent stresses within the family, may affect the resolution of a crisis. Although most families do cope, the needs of families at risk are considerable. If they receive guidance and emotional support early in the crisis, there is an increased possibility that they will cope successfully.
Although it is easy to assume that families of children with the most severe illnesses or disabilities will have the poorest adjustment, the severity of the condition is only one part of the overall picture. The level of adjustment is greatly influenced by the functional burden on the family. The issues associated with caring for and living with the child must be considered in relation to the family’s resources and coping ability (Box 22-6). The family of a child with multiple disabilities warranting complex care that has many coping strategies and resources may adjust more successfully to the child’s situation than the family of a child with a less serious condition and few resources to counterbalance it.
Intrafamilial resources, social support from friends, parent-to-parent support, parent-professional partnerships, and community resources intertwine to provide a flexible web of support for the family of a child with a chronic condition.
Intrafamilial Resources
Family members’ experience or maturity, education, intelligence, ability and willingness to learn how to provide the child’s care, sense of humor, and sense of optimism are resources they can bring to a situation. Resources within the family, such as adaptability, cohesion, a sense of coherence, and hardiness, can greatly facilitate the family’s adjustment.
The marital relationship is a primary source of potential support and overall is the best predictor of coping behavior and adjustment. Conflicts in parental role definition and differences in paternal and maternal coping patterns can place a strain on the marital relationship. Most health care professionals assume that the rate of family dissolution is greater due to increased familial stress from the presence of a chronic condition in a family member. These families may experience more conflict and strain over the roles of their members, as well as fewer exchanges of affection. Parents of chronically ill children, however, are not more likely to experience higher levels of marital dissatisfaction, economic problems, or depression than families of healthy children (Emerson, 2003). When partners can openly discuss their feelings, there appears to be much less guilt, blame, anger, and indecision. Each crisis during the lengthy period of chronic illness is successfully resolved, which reduces the overlapping and accumulation of multiple stresses.
Social Support Systems
The significant others who are available to individuals for emotional strength during periods of crisis constitute their support system. Support systems may be available through various relationships and may include one significant other, such as a spouse, or a group of significant others, such as the health care team or the extended family. The amount and type of social support received by families is a crucial factor in their adjustment to the child’s chronic condition.
The source of support is a determining factor in the effectiveness of certain forms of support. For example, emotional or expressive support is best provided by individuals with whom one has strong ties and who are like oneself. The ability to verbalize feelings such as guilt, anger, fear, or anxiety helps individuals deal with the particular emotion. Verbalization allows for the validation of thoughts and feelings. When professionals develop a strong therapeutic relationship with the family, they also can be appropriate sources of emotional support (see Parent-Professional Partnerships later in the chapter).
On the other hand, instrumental support can often be provided by those to whom the family has weaker ties and can link the family to a more diverse and broader social network. For example, the most appropriate sources of informational support are both professionals who have practical and theoretic knowledge, and nonprofessionals or parents whose experience makes them experts.
Coping with illness or disability may be a new experience for a family and their support system, and the family may benefit from recommendations on effective ways to use their support system to meet their needs. Providing parents with written information they can share with extended family can often help them reach out to others during a stressful time. In addition, helping family members identify members of their support system and consider practical tasks for which to request assistance (e.g., laundry, care of siblings, and transportation) can mobilize resources.
Health care providers should assess the type of support needed before planning interventions. They may assist families early in the diagnostic and treatment processes by encouraging them to plan for and use helpful resources. Parents may also benefit from the suggestion that it is okay to refuse certain types of well-intended support from friends and family (Shepard and Mahon, 2009). Families often state that they need help finding recreational activities and community resources for their children with chronic conditions. Health care providers can help by identifying the types of support that may be most helpful to the family and by being culturally sensitive and informed about parents’ groups and community resources.
Because of withdrawal and social isolation, some individuals may not be able to reach out to others for practical or emotional support. These individuals are more likely to feel overwhelmed and may benefit from consultation with a social worker or therapist.
Parent-to-Parent Support
The support a parent receives from another parent is unique and cannot be obtained from any other source. Veteran parents provide something that other support systems cannot in shared experiences. They have intimately known the stress related to diagnosis; weathered the many transitional times, such as moving from one program to another; and have sifted through services so that they have a practical knowledge of resources. A growing number of clinics and hospitals now have on staff a parent with a child who is chronically ill or disabled. The services these parents provide are invaluable for parents of children with special needs who are likely to experience lengthy and repeated hospitalizations and many routine outpatient visits.
Just being with another parent who has shared similar experiences can be beneficial. It is not always necessary for this parent to have a child with the same diagnosis. Parents walk a common path in the process of adjusting to a child with special needs or finding respite services, rehabilitative or educational services, special equipment vendors, or financial counseling.
If the child’s treatment center does not have a parent staff position, the nurse can contact parent groups, who will usually send a representative. Another intervention is to ask another parent with a chronically ill or disabled child to talk with the parents. The nurse should seek out a parent who has a nonjudgmental approach to differences in families, is a good listener, and has good problem-solving and advocacy skills.
The parent self-help group is another approach to fostering parent-to-parent support.* Group members feel less alone and have the opportunity to observe both mastery role modeling and coping in other members. Parents’ groups are rich resources for information. Even if parents cannot attend meetings, they can still benefit from the group newsletters and other literature that often accompany membership. The nurse can promote parent participation in self-help groups by serving as a group advisory board member, a referral agent, a resource person, or an assistant in finding a group. Often all that is necessary to start a group is identifying one or two parents as leaders; sharing with them the names, addresses, and telephone numbers of other families; and guiding them in how to organize the first meeting.
Parent-Professional Partnerships
One important component of family-centered care is parent-professional collaboration. By their nature, collaborative relationships show respect and therefore support for families. Collaboration reflects a change from the traditional models of care. For this reason nurses must examine their attitudes to determine their ability to participate in parent-professional partnerships. A basic characteristic is the belief that parents are experts concerning their child. The partnership is based on trust and communication. The Nursing Care Guidelines box offers strategies for developing successful partnerships with parents.
Throughout the lengthy process of caring for a child with special needs, family members become experts in managing their child’s care. Unfortunately, this expertise is not always acknowledged by health care providers, who tend to be directive rather than collaborative in their approach to the family. This is particularly common during periods of hospitalization, when role confusion occurs. At home parents are expected to care for their child, yet in the hospital they may be disregarded as participants in care. Provision of a supportive atmosphere must include respect for parents’ knowledge, coordination of care with family members, and willingness to include their suggestions in the treatment plan.
Partnership depends on good communication. A nurse’s classification or perception of the “difficult” family can influence nurse-family communication. A family whose child is ill responds along what health care providers may perceive as a continuum from the “good” to the “difficult” family stereotype. Nurses readily establish relationships with the “good” family, who perceive staff as having control or power and accept this hierarchy. However, often this is not the case with a family that is considered “difficult” and is characterized as being overinvolved or underinvolved in the child’s care.
Nurses also display patterns of behavior with regard to parents of ill children. First, facilitative nurses acknowledge the parents’ crucial roles and attempt to remove barriers to their involvement in care. Second, nurses who desire a high degree of control over their work may become “rule enforcers” with parents. Third, nurses may establish collegial relationships with parents over time, with respect for the parents as experts regarding their child. Finally, nurses may avoid a parent whose values differ from their own or a parent who is overly demanding from the nurses’ perspective.
The nurse and family come to have explicit and implicit expectations of one another, form views of one another, and negotiate roles in the child’s care. Levels of trust and control are central to their interactions.
Parents who mistrust professionals act differently from those who have trust in the health care team. Nurses trust parents differently as well, based on their judgments of the parenting they observe.
Community Resources
In the past, if coping strategies could not be used to reduce the disruption and stress of maintaining the child in the home, the seriously affected child may have been permanently placed outside the home in a residential facility. Such placements are increasingly difficult to secure. Options vary from one location to another; however, many possibilities can be considered: in-home care by nursing personnel, medical daycare, respite care, transitional and long-term care, and medical or specialized foster care.
A family’s acknowledgment that caring for their child is burdensome is not necessarily maladjustment. Alternative placements may be the only option that will maintain the family’s integrity. Aging parents may be forced to accept such alternatives because of progressive inability to meet the demands of a child’s severe disability. When most of the child’s care is given over to others, abandoning the role of primary caregiver may be followed by an initial sense of loss, guilt, relief, and ambivalence, patterns of reactions not unlike those seen after the death of a terminally ill child. (See Chapter 23.) Besides out-of-home placement options, other community resources, such as parent support groups, health care resources, financial assistance, rehabilitation services, respite care, alternatives for schooling, equipment, and educational facilities and recreational programs,* are major elements in family adjustment.
Local and national disease-oriented organizations may provide needed support and assistance to families that qualify. Many of these organizations are identified elsewhere in the text under discussion of the specific diagnosis. Federal and state departments of health, social services, mental health, and labor may be able to help locate appropriate regional resources. For example, state programs for children with special health needs (formerly crippled children’s services) offer financial assistance for children with various disabling conditions. Nurses should become familiar with those in their communities and with vocational programs for special groups.
Although community resources may exist, it is often difficult for parents to find appropriate services, and coordination among many agencies may be lacking. Fragmented care is a key complaint of families, and specific problems of delayed referral and negative experiences with agency personnel are identified as other concerns. Therefore community networking for improved services is essential.
Key Points
• Trends in the care of children with chronic illness or disability include increased focus on developmental stages, family development, family-centered care, normalization, mainstreaming, early intervention, and managed care.
• Promoting normal development in the child with a chronic condition or disability involves a variety of individualized strategies of support, normalization, and problem solving at each developmental stage.
• Providers and parents can play an active role in helping the child with a chronic condition or disability to cope. Acknowledging positive and negative coping strategies, applying principles of normalization, fostering hope, providing age-appropriate health education, and assisting the older child in setting realistic future goals are some key strategies.
• The family should play an active role in assessing needs and strengths.
• Supporting the family at the time of diagnosis includes planning the setting, becoming aware of the family’s experiences and background, individualizing support strategies, and ensuring that family members receive the information they want and need.
• Family tasks in adjusting to the child’s condition include managing the child’s condition on a daily basis, meeting the developmental needs of all family members, coping with stress, managing a wide range of feelings stemming from the diagnosis and other stresses, and developing personal and professional supports.
• As families confront the challenges of caring for a child with a chronic condition, nurses can help families realize their abilities and strengths, identify problems, develop problem-solving strategies, and identify new coping strategies. The goal is optimal family functioning, as defined by the family.
• A family-centered approach to care that strengthens parent-professional collaboration empowers parents and provides the best opportunity for appropriate intervention strategies that meet the unique needs of all family members.
Answers to Critical Thinking Exercises
Impact of the Child with Special Needs on the Sibling
1. Yes. The 5-year-old boy’s behavioral change occurs after a 2-week period without his mother and disabled sibling, which is a disruption in his usual family routine.
2. a. The 5-year-old resents the 2-week loss of the mother and brother and develops separation anxiety.
3. The first priority is to encourage communication between the mother and the 5-year-old son by considering when and how to inform him of the purpose of the disabled sibling’s hospitalization in an age-appropriate manner. Encourage the mother to accept the child’s feelings, and allow the child to express his feelings of sadness, anger, fear, guilt, and loneliness in an acceptable manner. If feasible, encourage the mother to have the child brought to the hospital to visit with the mother and disabled sibling. Encourage the mother to spend time with the 5-year-old while a relative, friend, or hospital volunteer remains with the disabled child.
4. Yes. The 5-year-old boy’s acting out is a way of pleading with the mother for an understanding of the loss of her and the sibling’s presence from his daily routine.
Parental Anger
1. Yes. The mother of an obese adolescent newly diagnosed with type 2 diabetes expressed anger and bitterness as she questions the need for insulin injections.
2. a. The mother’s anger and bitterness represent universal feelings expressed by parents of a child newly diagnosed with a chronic illness.
b Parental guilt develops regarding the cause of the type 2 diabetes.
c The parent may target his or her feelings of frustration, anger, and unfairness of the treatment toward the nurse.
3. The first priority is to encourage the expression of the mother’s anger and bitterness through open-ended questions (e.g., “You sound angry about this”). Also encourage expression of the adolescent’s concerns. Encourage the family to discuss the impact of the adolescent’s chronic illness on the marriage, family structure, finances, and plans. Reiterate and repeat the pathophysiology and treatment plan as needed. Interview the parent, adolescent, and family to determine whether their needs and concerns have been adequately addressed.
4. Yes. The first priority is to allow the parent to express his or her thoughts and feelings. The next essential nursing education opportunity is to make sure the parent understands the importance of insulin for the child.
References
Arango, P. Special health care needs. In: Cosby AG, Greenberg RE, Southward LH, et al, eds. About children: an authoritative resource on the state of childhood today. Elk Grove Village, Ill: American Academy of Pediatrics, 2005.
Beers, NS, Kemeny, A, Sherritt, L, et al. Variations in state-level definitions: children with special health care needs. Public Health Rep. 2003;118(5):434–447.
Brown, RT, Wiener, L, Kupst, MJ, et al. Single parenting and children with chronic illnesses: understudied phenomenon. J Pediatr Psychol. 2008;33(4):404–421.
Clarke, NE, McCathy, MC, Downie, P, et al. Gender differences in the psychosocial experience of parents of children with cancer: A review of the literature. Psychooncology. 2009;18(9):907–915.
Corbin, JS, Strauss, A. A nursing model for chronic illness management based upon the trajectory framework. Sch Inq Nurs Pract. 1995;3(3):155–174.
Coyne, I. Children’s experiences of hospitalization. J Child Health Care. 2006;10(4):326–336.
Emerson, E. Mothers of children and adolescents with intellectual disability: social and economic situation, mental health status, and the self-assessed social and psychological impact of the child’s difficulties. J Intellect Disabil Res. 2003;47(Pt 4/5):385–399.
Fahrner, R, Mario, EB. HIV infection and AIDS. In Jackson-Allen PL, Vessey JA, Schapiro M, eds.: Primary care of the child with a chronic condition, ed 5, St Louis: Mosby, 2009.
Fazil, Q, Wallace, LM, Singh, G, et al. Empowerment and advocacy: reflections on action research with Bangladeshi and Pakistani families who have children with severe disabilities. Health Soc Care Commun. 2004;12(5):389–397.
Fleitas, J. When Jack fell down . . . Jill came tumbling after: siblings in the web of illness and disability. MCN Am J Matern Child Nurs. 2000;25(5):267–273.
Goble, LA. The impact of a child’s chronic illness on fathers. Issues Compr Pediatr Nurs. 2004;27(3):153–162.
Green, SE. “What do you mean ‘what’s wrong with her?’”: stigma and the lives of families of children with disabilities. Soc Sci Med. 2003;57(8):1361–1374.
Gurney, JG, Bondy, ML. Epidemiologic research methods and childhood cancer. In Pizzo PA, Poplack DG, eds.: Principles and practice of pediatric oncology, ed 6, Philadelphia: Lippincott Williams & Wilkins, 2010.
Hockenberry, MJ, Kline, NE. Nursing support of the child with cancer. In Pizzo PA, Poplack DG, eds.: Principles and practice of pediatric oncology, ed 6, Philadelphia: Lippincott Williams & Wilkins, 2010.
Horner, MJ, Ries, LAG, Krapcho, M, et al, SEER Cancer Statistics Review, 1975-2006. Bethesda, Md: National Cancer Institute; 2008. available at http://seer.cancer.gov/csr/1975_2006/ [based on November 2008 SEER data submission (accessed July 8, 2009)].
Inkelas, M. Incentives in a Medicaid carve-out: impact on children with special health care needs. Health Serv Res. 2005;40(1):79–102.
Jackson, PL. The primary care provider and children with chronic conditions. In Jackson-Allen PL, Vessey JA, Schapiro M, eds.: Primary care of the child with a chronic condition, ed 5, St Louis: Mosby, 2009.
Jeffrey, AE, Newacheck, PW. Role of insurance for children with special health care needs: a synthesis of the evidence. Pediatrics. 2006;118(4):e1027–e1038.
Kliebenstein, MA, Broome, ME. School re-entry for the child with chronic illness: parent and school personnel perceptions. Pediatr Nurs. 2000;26(6):579–583.
Mahoney, G, Wheeden, CA, Perales, F. Relationship of preschool special education outcomes to instructional practices and parent-child interaction. Res Dev Disabil. 2004;25(6):539–558.
McPherson, M, Weissman, G, Strickland, BB, et al. Implementing community-based systems of services for children and youths with special health care needs: how well are we doing? Pediatrics. 2004;113(5):1538–1544.
Miller, AR, Recsky, MA, Armstrong, RW. Responding to the needs of children with chronic health conditions in an era of health services reform. CMAJ. 2004;171(11):1366–1367.
Msall, ME, Avery, RC, Tremont, MR, et al. Functional disability and school activity limitations in 41,300 school-age children: relationships to medical impairments. Pediatrics. 2003;111(3):548–553.
Murray, JS. Understanding sibling adaptation to childhood cancer. Issues Compr Pediatr Nurs. 2000;23:39–47.
Newacheck, PW, Halfon, N. Prevalence, impact, and trends in childhood disability due to asthma. Arch Pediatr Adolesc Med. 2000;154:287–293.
Newacheck, PW, Hung, Y, Wright, KK. Racial and ethnic disparities in access to care for children with special health care needs. Ambul Pediatr. 2002;2(4):247–254.
Newacheck, PW, Kim, SE, A national profile of health care utilization and expenditures for children with special health care needs. Arch Pediatr Adolesc Med 2005;159(4):10–17. Erratum in Arch Pediatr Adolesc Med 159(4):318, 2005
Newacheck, PW, McManus, M, Fox, HB, et al. Access to health care for children with special health care needs. Pediatrics. 2000;105(4):760–766.
Newacheck, PW, Wong, ST, Galbraith, AA, et al. Adolescent health care expenditures: a descriptive profile. J Adolesc Health. 2003;32(6 Suppl):3–11.
Palfrey, JS, Richmond, JB. Health services: past, present, and future. In: Cosby AG, Greenberg RE, Southward LH, et al, eds. About children: an authoritative resource on the state of childhood today. Elk Grove Village, Ill: American Academy of Pediatrics, 2005.
Pearson, LJ. Children’s hospitalization and other health-care encounters. In Rollins JA, Bolig R, Mahan CC, eds.: Meeting psychosocial needs across the health-care continuum, ed 1, Austin: Pro-Ed, 2005.
Perrin, JM, Bloom, SR, Gortmaker, SL. The increase of childhood chronic conditions in the United States. JAMA. 2007;297(24):2755–2759.
Rehm, RS. Family culture and chronic conditions. In Jackson-Allen PL, Vessey JA, Schapiro M, eds.: Primary care of the child with a chronic condition, ed 5, St Louis: Mosby, 2009.
Reiss, JG, Gibson, RW, Walker, LR. Health care transition: youth, family, and provider perspectives. Pediatrics. 2005;115(1):112–120.
Ritchie, MA. Self-esteem and hopefulness in adolescents with cancer. J Pediatr Nurs. 2001;16(1):35–42.
Rittey, CD. Learning difficulties: what the neurologist needs to know. J Neurol Neurosurg Psychiatry. 2003;74:30–36.
Schiller, JS, Adams, PF, Nelson, ZC, Summary health statistics for the U.S. population: National Health Interview Survey, 2003. Vital and Health Statistics Series 10, No 224. Washington, DC: US Government Printing Office; 2005.
Schmidt, S, Petersen, C, Bullinger, M. Coping with chronic disease from the perspective of children and adolescents: a conceptual framework and its implications for participation. Child Care Health Dev. 2003;29(1):63–75.
Shepard, MP, Mahon, MM. Chronic conditions and the family. In Jackson-Allen PL, Vessey JA, Schapiro M, eds.: Primary care of the child with a chronic condition, ed 5, St Louis: Mosby, 2009.
Shudy, M, de Almeida, ML, Ly, S, et al. Impact of pediatric critical illness and injury on families: A systematic literature review. Pediatrics. 2006;118(Suppl 3):S203–S218.
Smucker, JMRL. Managed care and children with special health care needs. J Pediatr Health Care. 2001;15(1):3–9.
Stein, REK, Shenkman, E, Wegener, DH, et al. Health of children in Title XXI: should we worry? Pediatrics. 2003;112(2):e112–e118.
Sullivan-Bolyai, S, Knafl, KA, Sadler, L, et al. Great expectations: a position description for parents as caregivers: part II. Pediatr Nurs. 2004;30(1):52–56.
Sullivan-Bolyai, S, Sadler, L, Knafl, KA, et al. Great expectations: a position description for parents as caregivers: part I. Pediatr Nurs. 2003;29(6):457–461.
Turkel, S, Pao, M. Late consequences of pediatric chronic illness. Psychiatr Clin North Am. 2007;30(4):819–835.
van Dyck, P, Kogan, MD, Heppel, D, et al. The National Survey of Children’s Health: a new data resource. Matern Child Health J. 2004;8(3):183–188.
Varni, JW, Limbers, CA, Burwinkle, TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL(tm) 4.0 generic core scales. Health Qual Life Outcomes. 2007;5:43.
Vessey, JA, Jackson, PL. School and the child with a chronic condition. In Jackson-Allen PL, Vessey JA, Schapiro M, eds.: Primary care of the child with a chronic condition, ed 5, St Louis: Mosby, 2009.
Vessey, JA, Mebane, DJ. Chronic conditions and child development. In Jackson-Allen PL, Vessey JA, Schapiro M, eds.: Primary care of the child with a chronic condition, ed 5, St Louis: Mosby, 2009.
Weiner, P. Educational consultant for children with a chronic illness. In Hicks M, ed.: Child life beyond the hospital, ed 1, Rockville, Md: Child Life Council, 2008.
Yogev, R, Chadwick, EG. Acquired immunodeficiency syndrome. In Kliegman RM, Behrman RE, Jenson HB, et al, eds.: Nelson textbook of pediatrics, ed 18, Philadelphia: Saunders, 2007.
*Access to Respite Care and Help (ARCH) is available at www.archrespite.org.
†Information on individual toy selection and toy lending libraries for children with sensory deficits, motor disabilities, and developmental delay are available from the National Lekotek Center at 800-366-PLAY; www.lekotek.org.
*A directory of camps for children with a variety of chronic illnesses and general physical disabilities is available at American Camp Association, www.ACAcamps.org; Candlelighters Childhood Cancer Foundation, www.candlelighters.org; and Easter Seals, www.easterseals.com.
†Excellent publications on adapting the environment for children with disabilities are available from National Rehabilitation Information Center, www.naric.com.
*VSA arts is an international organization that creates learning opportunities through the arts for individuals with disabilities; www.vsarts.org.
*Information about employment is available from the Office of Disability Employment Policy (www.dol.gov/odep). The Job Accommodation Network (www.jan.wvu.edu) provides information about job accommodations and the employability of individuals with disabilities.
*Home care instruction sheets, which may be copied and given to families, are available in Hockenberry MJ: Wong’s clinical manual of pediatric nursing, St Louis, ed 6, 2004, Mosby.
†Information on restraints for children with special needs is available from Automotive Safety Program, Riley Hospital for Children, www.preventinjury.org.
‡E-Z-On vest is available from E-Z-On Products, Inc., www.ezonpro.com.
*Information regarding financial issues is available from Family Voices, Inc., a grassroots advocacy network of parents and professionals; www.familyvoices.org.
*An excellent resource for becoming involved in political action is the Public Affairs Public Issues Handbook, available from the American Cancer Society, www.cancer.org; and Family Voices, Inc., see footnote on p. 867.
*Information about self-help groups, as well as books and pamphlets, is available from the National Self-Help Clearinghouse, 365 5th Ave., Suite 3300, New York, NY 10016; 212-817-1822; fax: 212-817-2990; e-mail: info@selfhelpweb.org; www.selfhelpweb.org.
*A general source of information is the National Dissemination Center for Children with Disabilities, www.nichcy.org. A comprehensive list of books and pamphlets for parents and teachers is available from Easter Seals, www.easterseals.com.