Pediatric Variations of Nursing Interventions
Chapter Outline
General Concepts Related to Pediatric Procedures,
Subcutaneous and Intradermal Administration,
Nasogastric, Orogastric, or Gastrostomy Administration,
http://evolve.elsevier.com/wong/ncic
Communicating with Families, Ch. 6
Dental Health: Infant, Ch. 12; Toddler, Ch. 14; Preschooler, Ch. 15; School-Age Child, Ch. 17
Family-Centered Home Care, Ch. 25
Febrile Seizures, Ch. 37
Feeding Resistance, Ch. 10
Injury Prevention: Infant, Ch. 12; Toddler, Ch. 14; Preschooler, Ch. 15; School-Age Child, Ch. 17; Adolescent, Ch. 19
Limit Setting and Discipline, Ch. 3
Nursing Care of the Surgical Neonate, Ch. 11
Nutritional Assessment, Ch. 6
Pain Assessment; Pain Management, Ch. 7
Parenteral Fluid Therapy, Ch. 28
Preparation for Hospitalization, Ch. 26
Skin Care (Neonatal), Ch. 10
Temperature (Measurement), Ch. 6
Using Play and Expressive Activities to Minimize Stress, Ch. 26
Venous Access Devices, Ch. 28
Wounds, Ch. 18
Many aspects of the nursing role encompass safe implementation of procedures with emphasis on comfort and support. An evidence-based approach to care provides nursing interventions with a foundation on which to build quality care. Throughout this chapter Evidence-Based Practice boxes provide the basis for pediatric nurses to promote excellence in direct patient care.
General Concepts Related to Pediatric Procedures
Before undergoing any invasive procedure, the patient or the patient’s legal surrogate must receive sufficient information on which to make an informed health care decision. Informed consent should include the expected care or treatment; potential risks, benefits, and alternatives; and what might happen if the patient chooses not to consent. To obtain valid informed consent, health care providers must meet the following three conditions:
1. The person must be capable of giving consent; he or she must be over the age of majority (usually age 18 years) and must be considered competent (i.e., possessing the mental capacity to make choices and understand their consequences).
2. The person must receive the information needed to make an intelligent decision.
3. The person must act voluntarily when exercising freedom of choice without force, fraud, deceit, duress, or other forms of constraint or coercion.
The patient has the right to accept or refuse any health care. If a patient is treated without consent, the hospital or health care provider may be charged with assault and held liable for damages.
Requirements for Obtaining Informed Consent
Written informed consent of the parent or legal guardian is usually required for medical or surgical treatment of a minor, including many diagnostic procedures. One universal consent is not sufficient. Separate informed permissions must be obtained for each surgical or diagnostic procedure, including:
• Minor surgery (e.g., cutdown, biopsy, dental extraction, suturing a laceration [especially one that may have a cosmetic effect], removal of a cyst, closed reduction of a fracture)
• Diagnostic tests with an element of risk (e.g., bronchoscopy, angiography, lumbar puncture, cardiac catheterization, bone marrow aspiration)
• Medical treatments with an element of risk (e.g., blood transfusion, thoracentesis or paracentesis, radiotherapy)
Other situations that require patient or parental consent include:
• Photographs for medical, educational, or public use
• Removal of the child from the health care institution against medical advice
• Postmortem examinations, except in unexplained deaths, such as sudden infant death, violent death, or suspected suicide
Decision making involving the care of older children and adolescents should include the patient’s assent (if feasible), as well the parent’s consent. Assent means the child or adolescent has been informed about the proposed treatment, procedure, or research and is willing to permit a health care provider to perform it. Assent should include:
• Helping the patient achieve a developmentally appropriate awareness of the nature of his or her condition
• Telling the patient what he or she can expect
• Making a clinical assessment of the patient’s understanding
• Soliciting an expression of the patient’s willingness to accept the proposed procedure
Health care providers should use multiple methods to provide information, including age-appropriate methods (e.g., videos, peer discussion, diagrams, and written materials). The nurse should provide an assent form for the child to sign, and the child should keep a copy. By including the child in the decision-making process and gaining his or her acceptance, staff members demonstrate respect for the child. Assent is not a legal requirement but an ethical one to protect the rights of children.
Eligibility for Giving Informed Consent
Informed Consent of Parents or Legal Guardians: Parents have full responsibility for the care and rearing of their minor children, including legal control over them. As long as children are minors, their parents or legal guardians are required to give informed consent before medical treatment is rendered or any procedure is performed. If the parents are married to each other, consent from only one parent is required for nonurgent pediatric care. If the parents are divorced, consent usually rests with the parent who has legal custody (Berger and American Academy of Pediatrics Committee on Medical Liability, 2003). Parents also have a right to withdraw consent later.
Evidence of Consent: Regulations on obtaining informed consent vary from state to state, and policies differ at each health care facility. It is the physician’s legal responsibility to explain the procedure, risks, benefits, and alternatives. The nurse witnesses the patient’s, parent’s, or legal guardian’s signature on the consent form and may reinforce what the patient has been told. A signed consent form is the legal document that signifies that the process of informed consent has occurred. If parents are unavailable to sign consent forms, verbal consent may be obtained via the telephone in the presence of two witnesses. Both witnesses record that informed consent was given and by whom. Their signatures indicate that they witnessed the verbal consent.
Informed Consent of Mature and Emancipated Minors: State laws differ with regard to the age of majority, the age at which a person is considered to have all the legal rights and responsibilities of an adult. In most states, 18 is the age of majority. Competent adults can give informed consent on their own behalf. An emancipated minor is one who is legally under the age of majority but is recognized as having the legal capacity of an adult under circumstances prescribed by state law, such as pregnancy, marriage, high school graduation, independent living, or military service.
Treatment Without Parental Consent: Exceptions to requiring parental consent before treating minor children occur in situations in which children need urgent medical or surgical treatment and a parent is not readily available to give consent or refuses to give consent. For example, a child may be brought to an emergency department accompanied by a grandparent, child care provider, teacher, or others. In the absence of parents or legal guardians, persons in charge of the child may be given permission by the parents to give informed consent by proxy. In emergencies, including danger to life or the possibility of permanent injury, appropriate care should not be withheld or delayed because of problems obtaining consent (Berger and American Academy of Pediatrics Committee on Medical Liability, 2003; American Academy of Pediatrics, 2003). The nurse should document any efforts made to obtain consent.
Refusal to give consent can occur when the treatment, such as blood transfusions, conflicts with the parents’ religious beliefs. All states recognize such exceptions and have statutory procedures to permit treatment if the life or health of such a minor is in jeopardy or if delayed treatment would create a risk to the minor’s health. Evaluation for child abuse or neglect can occur without parental consent and without notification to the state before evaluation in most states.
Adolescents, Consent, and Confidentiality: The Health Insurance Portability and Accountability Act of 1996 (HIPAA) was passed to help protect and safeguard the security and confidentiality of a person’s health information. Because adolescents are not yet adults, parents have the right to make most decisions on their behalf and receive information. Adolescents, however, are more likely to seek care in a setting in which they believe their privacy will be maintained. All 50 states have enacted legislation that entitles adolescents to consent to treatment, without the parents’ knowledge, to one or more “medically emancipated” conditions such as sexually transmitted infections, mental health services, alcohol and drug dependency, pregnancy, and contraceptive advice (Anderson, Schaechter, and Brosco, 2005; Tillett, 2005; American Academy of Pediatrics, 2003). Consent to abortion is controversial, and statues vary widely by state. State law preempts HIPAA regardless of whether that law prohibits, mandates, or allows discretion about a disclosure.
Informed Consent and Parental Right to the Child’s Medical Chart: Some state statutes give parents the unrestricted right to a copy of children’s medical records. In states without statues, the best practice is to allow parents to review or have a copy of minors’ charts under reasonable circumstances. Practitioners should avoid restrictive requirements such as review permitted only in the presence of a clinician. Rather, an appropriate practitioner should be available to answer any questions that parents may have during their reviews.
Preparation for Diagnostic and Therapeutic Procedures
![]() Technologic advances and changes in health care have resulted in more pediatric procedures being performed in a variety of settings. Many procedures are both stressful and painful experiences. For most procedures the focus of care is psychologic preparation of the child and family. However, some procedures require the administration of sedatives and analgesics.
Technologic advances and changes in health care have resulted in more pediatric procedures being performed in a variety of settings. Many procedures are both stressful and painful experiences. For most procedures the focus of care is psychologic preparation of the child and family. However, some procedures require the administration of sedatives and analgesics.
![]() Skill—Preparing the Child for Procedures
Skill—Preparing the Child for Procedures
Psychologic Preparation
Preparing children for procedures decreases their anxiety, promotes their cooperation, supports their coping skills and may teach them new ones, and facilitates a feeling of mastery in experiencing a potentially stressful event. Many institutions have developed preadmission teaching programs designed to educate the pediatric patient and family by offering hands-on experience with hospital equipment, the procedure performed, and departments they will visit. Preparatory methods may be formal, such as group preparation for hospitalization. Most preparation strategies are informal, focus on providing information about the experience, and are directed at stressful or painful procedures. The most effective preparation includes the provision of sensory-procedural information and helping the child develop coping skills, such as imagery, distraction, or relaxation.
The Nursing Care Guidelines boxes describe general guidelines for preparing children for procedures, along with age-specific guidelines that consider children’s developmental needs and cognitive abilities. In addition to these suggestions, nurses should consider the child’s temperament, existing coping strategies, and previous experiences in individualizing the preparatory process. Children who are distractible and highly active or those who are “slow to warm up” may need individualized sessions—shorter for the active child or more slowly paced for the shy child. Youngsters who tend to cope well may need more emphasis on using their present skills, whereas those who appear to cope less adequately can benefit from more time devoted to simple coping strategies, such as relaxing, breathing, counting, squeezing a hand, or singing. Children with previous health-related experiences still need preparation for repeat or new procedures; however, the nurse must assess what they know, correct misconceptions, supply new information, and introduce new coping skills as indicated by their previous reactions. Especially for painful procedures, the most effective preparation includes providing sensory-procedural information and helping the child develop coping skills, such as imagery or relaxation (see Nursing Care Guidelines box).
Children differ in their “information-seeking dimension.” Some actively ask for information about the intended procedure, whereas others characteristically avoid information. Parents can often guide nurses in deciding how much information is enough for the child, since parents know whether the child is typically inquisitive or satisfied with short answers. Asking older children their preferences about the amount of explanation is also important.
The exact timing of the preparation for a procedure varies with the child’s age and the type of procedure. No exact guidelines govern timing, but in general the younger the child, the closer the explanation should be to the actual procedure to prevent undue fantasizing and worrying. With complex procedures, more time may be needed for assimilation of information, especially with older children. For example, the explanation for an injection can immediately precede the procedure for all ages, but preparation for surgery may begin the day before for young children and a few days before for older children, although the nurse should elicit the older children’s preferences. (See Preparation for Hospitalization, Chapter 26.)
Establish Trust and Provide Support: The nurse who has spent time with and established a positive relationship with a child usually finds it easier to gain cooperation. If the relationship is based on trust, the child will associate the nurse with caregiving activities that give comfort and pleasure most of the time, rather than discomfort and stress. If the nurse does not know the child, it is best for the nurse to be introduced by another staff person whom the child trusts. The first visit with the child should not include any painful procedure and ideally should focus on the child first and then on an explanation of the procedure.
Parental Presence and Support: Children need support during procedures, and for young children the greatest source of support is the parents. They represent security, protection, safety, and comfort. Several studies have reported a positive impact on parental distress and satisfaction and no difference in technical complications when parents remain with children (Piira, Sugiura, Champion, et al, 2005). Controversy exists regarding the role parents should assume during the procedure, especially if discomfort is involved. (See Evidence-Based Practice box, Family Presence During Resuscitation of a Child, Chapter 31.) Several professional associations support the option of family presence during invasive procedures (Emergency Nurses Association, 2005; American Association of Critical Care Nurses, 2006; American Academy of Pediatrics, American College of Emergency Physicians, O’Malley, et al, 2006). The nurse should assess the parents’ preferences for assisting, observing, or waiting outside the room, as well as the child’s preference for parental presence. Respect the child’s and parents’ choices. Give parents who wish to stay appropriate explanation about the procedure and coach them about where to sit or stand and what to say or do to help the child through the procedure. Support parents who do not want to be present in their decision and encourage them to remain close by so that they can be available to support the child immediately after the procedure. Parents should also know that someone will be with their child to provide support. Ideally, this person should inform the parents after the procedure about how the child did.
Provide an Explanation: Age-appropriate explanations are one of the most widely used interventions for reducing anxiety in children undergoing procedures. Before performing a procedure, explain what is to be done and what is expected of the child. The explanation should be short, simple, and appropriate to the child’s level of comprehension. Long explanations may increase anxiety in a young child. When explaining the procedure to parents with the child present, the nurse uses language appropriate to the child, since unfamiliar words can be misunderstood (see Nursing Care Guidelines box). If the parents need additional preparation, this is done in an area away from the child. Teaching sessions are planned at times most conducive to the child’s learning (e.g., after a rest period) and for the usual span of attention.
Special equipment is not necessary for preparing a child, but for young children who cannot yet think conceptually, using objects to supplement verbal explanation is important. Allowing children to handle actual items that will be used in their care, such as a stethoscope, sphygmomanometer, or oxygen mask, helps them develop familiarity with these items and reduces the fear often associated with their use. Miniature versions of hospital items such as gurneys and x-ray and intravenous (IV) equipment can be used to explain what the children can expect and permit them to safely experience situations that are unfamiliar and potentially frightening. Written and illustrated materials are also valuable aids to preparation.*
Physical Preparation
![]() One area of special concern is the administration of appropriate sedation and analgesia before stressful procedures. Chapter 7 describes sedative medications used for procedures.
One area of special concern is the administration of appropriate sedation and analgesia before stressful procedures. Chapter 7 describes sedative medications used for procedures.
Performance of the Procedure
Supportive care continues during the procedure and can be a major factor in a child’s ability to cooperate. Ideally, the same nurse who explains the procedure should perform or assist with the procedure. Before beginning, all equipment is assembled and the room is readied to prevent unnecessary delays and interruptions that increase the child’s anxiety. Minimizing the number of people present during the procedure also can decrease a child’s anxiety.
To promote long-term coping and adjustment, give special consideration to the patient’s age, coping skills, and procedure to be performed in determining where a procedure will occur. Treatment rooms should be used for procedures requiring sedation, such as bone marrow aspirates and lumbar punctures in younger children. Traumatic procedures should never be performed in “safe” areas, such as the playroom. If the procedure is lengthy, avoid conversation that could be misinterpreted by the child. As the procedure is nearing completion, the nurse should inform the child that it is almost over in language the child understands.
Expect Success: Nurses who approach children with confidence and who convey the impression that they expect to be successful are less likely to encounter difficulty. It is best to approach a child as though cooperation is expected. Children sense anxiety and uncertainty in an adult and respond by striking out or actively resisting. Although it is not possible to eliminate such behavior in every child, a firm approach with a positive attitude tends to convey a feeling of security to most children.
Involve the Child: Involving children helps to gain their cooperation. Permitting choices gives them some measure of control. However, a choice is given only in situations in which one is available. Asking children, “Do you want to take your medicine now?” leads them to believe they have an option and provides them the opportunity to legitimately refuse or delay the medication. This places the nurse in an awkward, if not impossible, position. It is much better to state firmly, “It’s time to drink your medicine now.” Children usually like to make choices, but the choice must be one that they do indeed have (e.g., “It’s time for your medicine. Do you want to drink it plain or with a little water?”).
Many children respond to tactics that appeal to their maturity or courage. This also gives them a sense of participation and achievement. For example, preschool children will be proud that they can hold the dressing during the procedure or remove the tape. The same is true for the school-age child, who often cooperates with minimal resistance.
Provide Distraction: Distraction is a powerful coping strategy during painful procedures (Uman, Chambers, McGrath, et al, 2006). It is accomplished by focusing the child’s attention on something other than the procedure. Singing favorite songs, listening to music with a headset, counting aloud, or blowing bubbles to “blow the hurt away” are effective techniques. (For other nonpharmacologic interventions, see Chapter 7.)
Allow Expression of Feelings: The child should be allowed to express feelings of anger, anxiety, fear, frustration, or any other emotion. It is natural for children to strike out in frustration or to try to avoid stress-provoking situations. The child needs to know that it is all right to cry. Behavior is children’s primary means of communication and coping and should be permitted unless it inflicts harm on them or those caring for them.
Postprocedural Support
After the procedure the child continues to need reassurance that he or she performed well and is accepted and loved. If the parents did not participate, the child is united with them as soon as possible so that they can provide comfort.
Encourage Expression of Feelings: Planned activity after the procedure is helpful in encouraging constructive expression of feelings. For verbal children, reviewing the details of the procedure can clarify misconceptions and garner feedback for improving the nurse’s preparatory strategies. Play is an excellent activity for all children. Infants and young children should have the opportunity for gross motor movement. Older children are able to vent their anger and frustration in acceptable pounding or throwing activities. Play-Doh is a remarkably versatile medium for pounding and shaping. Dramatic play provides an outlet for anger and places the child in a position of control, in contrast to the position of helplessness in the real situation. Puppets also allow the child to communicate feelings in a nonthreatening way. One of the most effective interventions is therapeutic play, which includes well-supervised activities such as permitting the child to give an injection to a doll or stuffed toy to reduce the stress of injections (Fig. 27-1).
Positive Reinforcement: Children need to hear from adults that they did the best they could in the situation—no matter how they behaved. It is important for children to know that their worth is not being judged on the basis of their behavior in a stressful situation. Reward systems, such as earning stars, stickers, or a badge of courage, are appealing to children.
Returning to the child a short while after the procedure helps the nurse strengthen a supportive relationship. Relating with the child in a relaxed and nonstressful period allows him or her to see the nurse not only as someone associated with stressful situations but as someone with whom to share pleasurable experiences.
Use of Play in Procedures
The use of play is an integral part of relationships with children. As such, its value in specific situations is discussed throughout this book, such as in Chapter 26 in relation to hospitalization. Many institutions have elaborate and well-organized play areas and programs under the direction of child life specialists. Other institutions have limited facilities. No matter what the institution provides for children, nurses can include play activities as part of nursing care. Play can be used to teach, express feelings, or achieve a therapeutic goal. Consequently, it should be included in preparing children for and encouraging their cooperation during procedures. Play sessions after procedures can be structured, such as directed toward needle play, or general, with a wide variety of equipment available for children to play with.
Routine procedures such as measuring blood pressure and oral administration of medication may be of concern to children. Box 27-1 describes suggestions for incorporating play into nursing procedures and activities for the hospitalized child that facilitate learning and adjustment to a new situation.
Surgical Procedures
Children experiencing surgical procedures require both psychologic and physical preparation. An important concern is restriction of food and fluids before surgery to avoid aspiration during anesthesia. Infants require special attention to fluid needs. They should not be without oral fluids for an extended period preoperatively to avoid glycogen depletion and dehydration. Table 27-1 contains current preoperative fasting guidelines.
TABLE 27-1
FASTING RECOMMENDATIONS TO REDUCE THE RISK OF PULMONARY ASPIRATION*
| INGESTED MATERIAL | MINIMUM FASTING PERIOD (hr)† |
| Clear liquids‡ | >2 |
| Breast milk | 4 |
| Infant formula | 6 |
| Nonhuman milk§ | 6 |
| Light meal¶ | 6 |
*These recommendations apply to healthy patients who are undergoing elective procedures. They are not intended for women in labor. Following the guidelines does not guarantee complete gastric emptying has occurred.
†Fasting periods noted in chart apply to all ages.
‡Examples of clear liquids include water, fruit juices without pulp, carbonated beverages, clear tea, and black coffee.
§Because nonhuman milk is similar to solids in gastric emptying time, the amount ingested must be considered when determining appropriate fasting period.
¶Light meal typically consists of toast and clear liquids. Meals that include fried or fatty foods or meat may prolong gastric emptying time. Both amount and type of foods ingested must be considered when determining appropriate fasting period.
From American Society of Anesthesiologists: Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures, Anesthesiology 90(3):896-905, 1999.
In general, psychologic preparation is similar to that discussed earlier for any procedure and employs many of the same techniques used in preparing a child for hospitalization, such as films, books, brochures, play, and tours. (See Chapter 26.) Stress points before and after surgery include the admission process, blood tests, injection of preoperative medication (if prescribed), transport to the operating room, the mask on the face during induction, and the stay in the postanesthesia care unit (PACU). Wearing a hospital gown without the security of underpants or pajama bottoms can also be traumatic. Therefore these articles of clothing should be allowed to be worn into the operating room and removed after induction of anesthesia. Children are at higher risk of ineffective response to anesthesia due to higher anxiety associated with stranger anxiety (infants), separation anxiety (toddlers and preschoolers), and fear of injury or death (adolescents) (Romino, Keatley, Secrest, et al, 2005).
Psychologic intervention consisting of systematic preparation, rehearsal of the forthcoming events, and supportive care at each of these points has shown to be more effective than a single-session preparation or consistent supportive care without systematic preparation and rehearsal (Kain, Caldwell-Andrews, Mayes, et al, 2007). A family-centered preoperative preparation program may consist of a tour of the perioperative areas with short explanations of the events 5 to 7 days before surgery, a video to take home and review a couple of times with additional explanations and demonstrations of perioperative processes, a mask to take home and practice with, pamphlets to guide parents on supporting children during induction, phone calls to coach parents on preparing children 1 or 2 days before surgery, and toys and supplies in the holding area. Therapeutic play is an effective strategy in preparing children, and increased familiarity with medical procedures decreases anxiety (Li, Lopez, and Lee, 2007).
Parental Presence: Some institutions support parental presence during induction of anesthesia (see Fig. 27-2 and Research Focus box). Appropriate education is essential to help parents understand the stages of anesthesia, what to expect, and how to support their child. When parents choose not to or are not allowed to attend the induction, leaving a favorite possession with the child and uniting the child and parents as soon as possible after surgery (preferably in the PACU) are important interventions. During surgery the family should have a designated place to wait and should be kept informed of the child’s progress. They also should know where and when they can visit the child after surgery.
Preoperative Sedation: Historically the most upsetting event for children has been the preoperative injection. An increasing number of anesthesiologists use preoperative sedative premedication, usually midazolam (Versed), and parental presence for children undergoing surgery (Kain, Caldwell-Andrews, Krivutza, et al, 2004).
The goals for using preoperative medications include (1) anxiety reduction, (2) amnesia, (3) sedation, (4) antiemetic effect, and (5) reduction of secretions (Manworren and Fledderman, 2000). (Chapter 7 includes an extensive discussion of pain management strategies for children undergoing surgery.) When drugs are administered, they should be delivered atraumatically via oral or IV routes. Numerous preanesthetic drug regimens are used with children, and no consensus exists on the optimal method. Midazolam provides excellent preoperative anxiety reduction, amnesia, and sedation. It is popular because of its short duration, predictable onset, and rare occurrence of respiratory depression. Oral transmucosal fentanyl (OTFC, or Fentanyl Oralet) is available as a sweetened lozenge on a plastic stick. When first approved, this appeared to be an excellent, atraumatic route of administration. However, nausea and vomiting, respiratory depression, and the need for more intensive monitoring and observation than with other oral sedatives have limited its popularity (Klein, Diekema, Paris, et al, 2002). If children have no preoperative pain, are well prepared psychologically for surgery, and have their parents nearby, however, preoperative medication may be unnecessary.
Anesthesia induction of the pediatric patient is commonly accomplished by administering inhalation agents in combination with nitrous oxide and oxygen by mask. Children may fear induction of anesthesia by mask. Practices that can minimize anxiety related to inhalation anesthesia are (1) disguising the unpleasant odor of anesthetic gases by applying a pleasant-smelling substance on the mask; (2) using a transparent plastic mask rather than an opaque black mask and gradually bringing it toward the face; (3) directing a stream of gas toward the child’s face from the bare tube until the child becomes drowsy, then using the mask; (4) allowing the child to sit up rather than lie down for anesthesia induction; and (5) allowing preoperative play with a mask and a doll or manikin.
Postoperative Care
Various psychologic and physical interventions and observations help prevent or minimize possible unpleasant effects from anesthesia and the surgical procedure. Although the incidence of serious postoperative complications in healthy children undergoing surgery is less than 1% (Maxwell and Yaster, 2000), continuous monitoring of the child’s cardiopulmonary status is essential during the immediate postoperative period. Postanesthesia complications such as airway obstruction, postextubation croup, laryngospasm, and bronchospasm make maintaining a patent airway and maximum ventilation critical.
![]() Monitoring the patient’s oxygen saturation and providing supplemental oxygen as needed, maintaining body temperature, and promoting fluid and electrolyte balance are important aspects of immediate postoperative care. Vital signs are continuously monitored, and each vital sign is evaluated in terms of side effects from anesthesia, shock, or respiratory compromise (Table 27-2).
Monitoring the patient’s oxygen saturation and providing supplemental oxygen as needed, maintaining body temperature, and promoting fluid and electrolyte balance are important aspects of immediate postoperative care. Vital signs are continuously monitored, and each vital sign is evaluated in terms of side effects from anesthesia, shock, or respiratory compromise (Table 27-2).
TABLE 27-2
POTENTIAL CAUSES OF POSTOPERATIVE VITAL SIGN ALTERATIONS IN CHILDREN
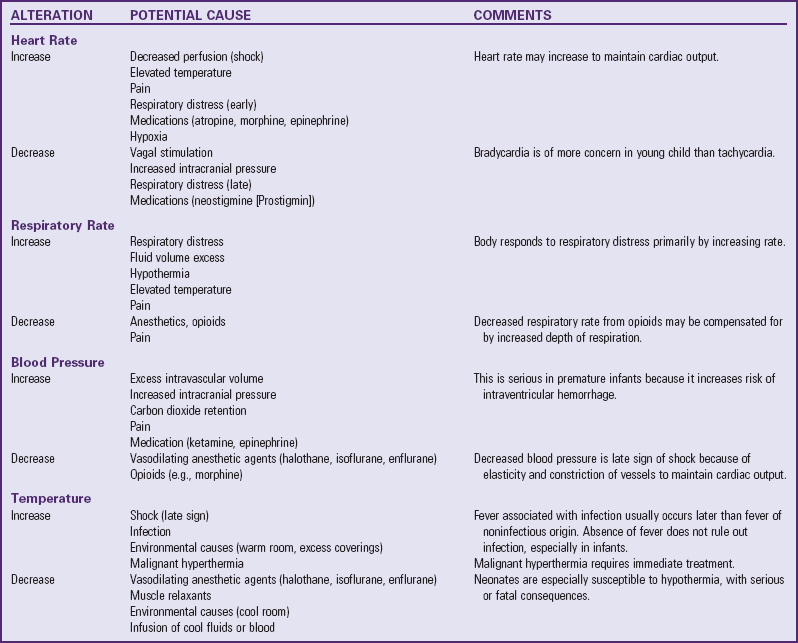
From Smith DP: Comprehensive child and family nursing skills, St Louis, 1991, Mosby.
![]() Skill—Measuring Oxygen Saturation
Skill—Measuring Oxygen Saturation
A change in vital signs that demands immediate attention in the perioperative period is caused by malignant hyperthermia (MH), a potentially fatal pharmacogenetic disorder involving a defective calcium channel in the sarcoplasmic reticulum membrane. In susceptible children, inhaled anesthetics (e.g., halothane, sevoflurane, desflurane) and the muscle relaxant succinylcholine trigger the disorder, producing hypermetabolism. Symptoms of MH include hypercarbia (increasing end-tidal carbon dioxide), elevated temperature, tachycardia, tachypnea, acidosis, muscle rigidity, and rhabdomyolysis (Rosenberg, Davis, and James, 2007). A family or previous history of sudden high fever associated with a surgical procedure and myotonia increase the risk for MH. Children who have successfully undergone prior surgery without adverse effects may still be considered susceptible.
Treatment of MH includes immediate discontinuation of the triggering agent, hyperventilation with 100% oxygen, and IV dantrolene sodium. If the child is hyperthermic, initiate cooling measures such as ice packs to the groin, axillae, and neck and iced nasogastric lavage. The surgery may be discontinued, or if it is emergent, it may be continued with a different anesthetic agent. The patient should be transferred to an intensive care unit for at least 36 hours and is closely monitored for stabilization of vital signs, metabolic state, and possible recurrence of symptoms.
Managing pain is a major nursing responsibility after surgery. The nurse should assess pain frequently and administers analgesics to provide comfort and facilitate cooperation with postoperative care such as ambulation and deep breathing. Opioids are the most commonly used analgesics. Routinely scheduled IV analgesics, patient-controlled analgesia, and epidural infusions, rather than as-needed orders, provide excellent analgesia in postoperative pediatric patients.
Because respiratory tract infections are a potential complication of anesthesia, make every effort to aerate the lungs and remove secretions. The lungs are auscultated regularly to identify abnormal sounds or any areas of diminished or absent breath sounds. To prevent pneumonia, encourage respiratory movement with incentive spirometers or other motivating activities (see Box 27-1). If these measures are presented as games, the child is more likely to comply. The child’s position is changed every 2 hours, and deep breathing is encouraged.
During the recovery period, spend some time with the child to assess his or her perceptions of surgery. Play, drawing, and storytelling are excellent methods of discovering the child’s thoughts. With such information the nurse can support or correct the child’s perceptions and boost his or her self-esteem for having endured a stressful procedure.
Many pediatric patients are discharged shortly after surgery. Preparation for discharge begins with the preadmission preparation visit. The nurse should discuss instructions for postoperative care and review them throughout the perioperative visit. After discharge, the nursing staff often makes phone calls to check the patient’s status. Patient education and compliance with discharge instructions can also be assessed during these phone calls (Barnes, 2000) (see Nursing Care Guidelines box).
Compliance
Compliance, also termed adherence, refers to the extent to which the patient’s behavior coincides with the prescribed regimen in terms of taking medication, following diets, or executing other lifestyle changes. In developing strategies to improve compliance, the nurse must first assess level of compliance. Because many children are too young to assume partial or total responsibility for their care, parents are usually primarily responsible for home management.
Factors relating to the care setting are important in ensuring compliance and should be considered in planning strategies to improve compliance. Basically, any aspect of the health care setting that increases the family’s satisfaction with the physical setting and the relationship with the practitioner positively influences adherence to the treatment regimen. However, the more complex, expensive, inconvenient, and disruptive the treatment protocol, the less likely the family is to comply. During long-term conditions that involve multiple treatments and considerable rearrangement of lifestyle, compliance is severely affected.
Although it is helpful to know those factors that influence compliance, assessment must include more direct measurement techniques. A number of methods exist, each with advantages and disadvantages. The most successful approach includes a combination of at least two of the following methods:
Clinical judgment—This is subject to bias and inaccuracy unless the nurse carefully evaluates the criteria used in assessment.
Self-reporting—Most people overestimate their compliance by about 20%, even when they admit to lapses.
Direct observation—This is difficult to employ outside the health care setting and awareness of being observed frequently affects performance.
Monitoring appointments—Keeping appointments indirectly indicates compliance with the prescribed care.
Monitoring therapeutic response—Few treatments yield directly measurable results (e.g., decreased blood pressure, weight loss); record on a graph or chart.
Pill counts—The nurse counts the number of pills remaining in the original container and compares the number missing with the number of times the medication should have been taken. Although this is a simple method, families may forget to bring the container or deliberately alter the number of pills to avoid detection. This method is also poorly suited to liquid medication. Another technique is the use of pill container caps that record every opening as a presumptive dose.
Chemical assay—For certain drugs, such as digoxin, measurement of plasma drug levels provides information on the amount of drug recently ingested. However, this method is expensive, indicates only short-term compliance, and requires precise timing of the assay for accurate results.
Compliance Strategies
Strategies to improve compliance involve interventions that encourage families to follow the prescribed treatment regimen. Some evidence suggests that higher levels of self-esteem and increased autonomy favorably affect adolescent compliance (Kyngas, Kroll, and Duffy, 2000). However, family factors are important, and characteristics associated with good compliance include family support, family reminders, good communication, and expectations for successful completion of the therapeutic regimen. No one approach is always successful, and the best results occur when at least two strategies are employed.
Organizational strategies involve the care setting and the therapeutic plan. This may involve increasing the frequency of appointments, designating a primary practitioner, reducing the cost of medication by prescribing generic brands, reducing the treatment’s disruption of the family’s lifestyle, and using “cues” to minimize forgetting. Numerous devices are available commercially or can be improvised for cueing, such as pill dispensers; watches with alarms; charts to record completed therapy; messages on the refrigerator or morning coffee pot; and treatment schedules that incorporate the treatment plan into the daily routine, such as physical therapy after the evening bath.
The nurse instructs the family about the treatment plan. Although education is an important factor in enhancing compliance and patients who are more knowledgeable about their condition are more likely to comply, education alone does not ensure compliant behavior. The nurse should incorporate teaching principles known to enhance understanding and retention of material. Written materials are essential, especially in any regimen requiring multiple or complex treatments, and they need to be understandable to the average individual, who reads at about the fourth-grade level. Involvement of the immediate and extended family (e.g., grandparents) in education sessions may enhance compliance.
Treatment strategies relate to the child’s refusal or inability to take the prescribed medication. The family may also have difficulty following a prescribed treatment regimen. They may remember and understand the instructions but may not be able to give the medicine as prescribed. Assess the reason for refusal. For example, the child may not be able to swallow pills. In this case, perhaps pills could be crushed or a liquid medication substituted (always review medication to ensure that crushing is acceptable before giving this instruction).
Assess the treatment and medication schedule to determine whether it is reasonable for a home situation. Although an every-6-hour or every-8-hour schedule is reasonable for hospitals, a parent would have difficulty getting up once or twice nightly. Instead the patient could take a medication during the day at times that would be easy to remember.
Behavioral strategies are designed to modify behavior directly. There are several effective strategies that the nurse can use with children to encourage the desired behavior. Positive reinforcement is one strategy that strengthens the behavior. One example of this is the child earning stars or tokens, which can be exchanged for a special privilege or gift. At times, however, disciplinary techniques, such as time-out for young children or withholding privileges for older children, may be needed to improve compliance.
General Hygiene and Care
Maintaining an IV line, removing a dressing, positioning a child in bed, changing a diaper, using electrodes, or using restraints have the potential to contribute to skin injury. Skin care must go beyond the daily bath and become a part of each nursing intervention. General guidelines for skin care are listed in the Nursing Care Guidelines box. (Specific guidelines for skin care of neonates are provided in Chapter 10 under Skin Care.)
Assessment of the skin is easiest to accomplish during the bath. Examine for early signs of injury. Risk factors include impaired mobility, protein malnutrition, edema, incontinence, sensory loss, anemia, infection, failure to turn the patient, and intubation. Critically ill children are at higher risk of pressure ulcers and skin breakdown, since they often have several risk factors combined. The incidence in these children has been reported as high as 27% (Curley, Quigley, and Lin, 2003). Identification of risk factors helps to determine those children who need a more thorough skin assessment. Several risk assessment scales are available for use in pediatrics, such as the Braden Q Scale (Curley, Razmus, Roberts, et al, 2003) and the Glamorgan Scale (Willock, Baharestani, and Anthony, 2009). Assessment should occur within 24 hours of admission to identify pressure ulcers and wounds that occurred before admission. Pressure ulcers in children typically occur on the occiput, ears, sacrum, and scapula (Amlung, Miller, and Bosley, 2001), whereas the heels and sacrum are common sites in adults.
When capillary blood flow is interrupted by pressure, the blood flows back into the tissue when the pressure is relieved. As the body attempts to reoxygenate the area, a bright red flush appears. This reactive hyperemia, or flush, is the earliest sign of tissue compromise and pressure-related ischemia. If pressure is prolonged, reactive hyperemia will not be sufficient to revitalize ischemic tissue. Pressure ulcers in hospitalized children are uncommon, with reported rates of 1% to 13% (Noonan, Quigley, and Curley, 2006). Risk factors associated with pressure ulcers in pediatric ICU patients include edema, length of stay, increasing positive end-expiratory pressure, lack of turning, use of a specialty bed in the turning mode, and weight loss (McCord, McElvain, Sachdeva, et al, 2004). Medical devices such as pulse oximeter probes, bilevel and continuous positive airway pressure masks, oxygen cannulas, orthotics, and casts can also cause pressure ulcers.
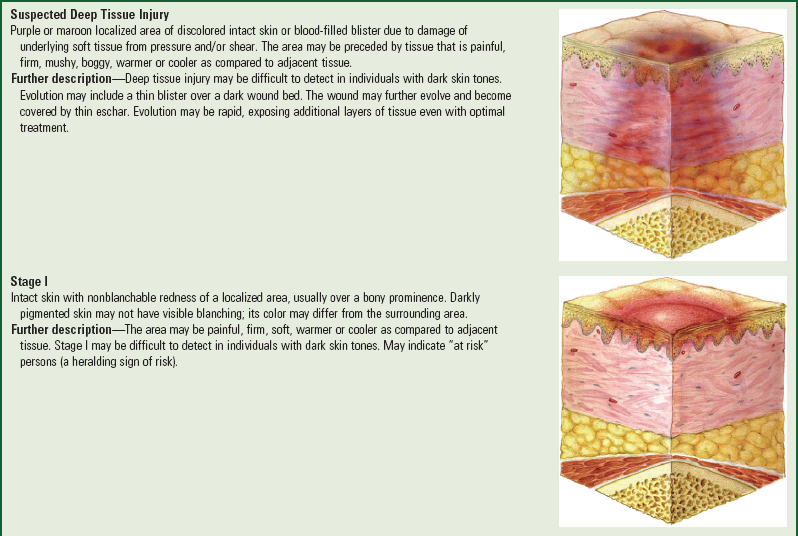
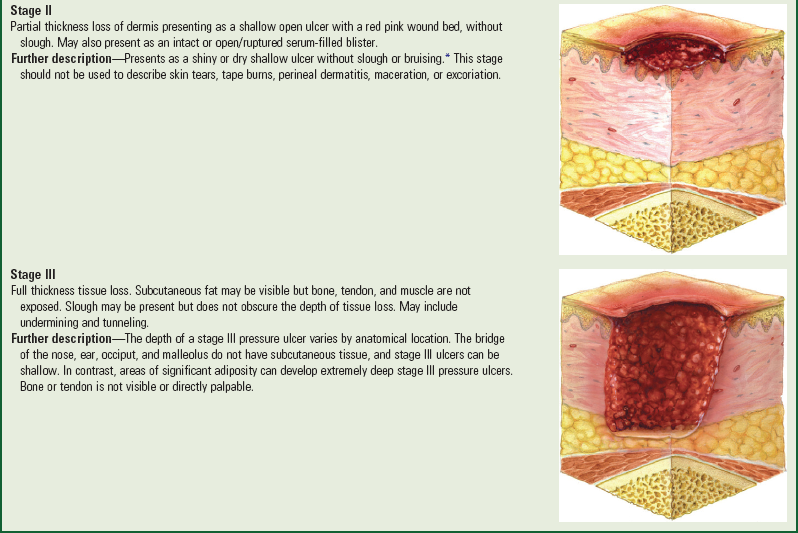
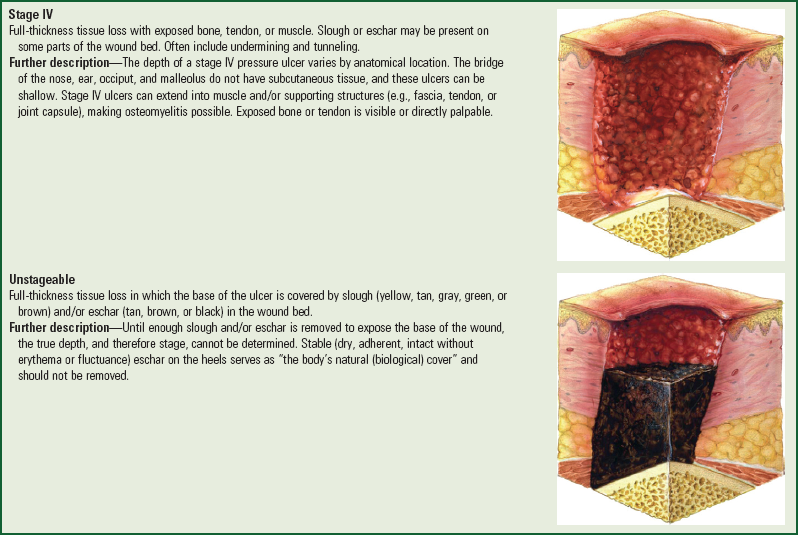
Pressure ulcers are staged to classify the amount of tissue damage that has occurred.* Necrotic tissue must be removed so that the tissue depth can accurately be assessed (Box 27-2). Accurate documentation of redness or obvious skin breakdown is essential. Color, size (diameter and depth), location, presence of sinus tracts, odor, exudate, and response to treatment are observed and recorded at least daily. (For treatment of wounds, see Chapter 18.)
Pressure ulcers can develop when the pressure on the skin and underlying tissues is greater than the capillary closing pressure, causing capillary occlusion. If the pressure remains unrelieved, vessels can collapse, resulting in tissue anoxia and cellular death. Pressure ulcers most often occur over bony prominences. These lesions are usually very deep (stage IV), extending into subcutaneous tissue or even more deeply into muscle, tendon, or bone.
A pressure reduction device reduces pressure but does not prevent pressure from causing capillary closure; therefore turning and repositioning are always included when using these devices. Most of these items are overlays that are placed on top of the regular mattress. A pressure-relief device maintains pressure below that which would cause capillary closure. These devices are usually high-technology beds that are used for patients who have multiple problems and cannot be turned effectively.
Friction and shear contribute to pressure ulcers. Friction occurs when the surface of the skin rubs against another surface, such as bed sheets. The skin may have the appearance of an abrasion. The skin damage is usually limited to the epidermal and upper layers. It most often occurs over the elbows, heels, or occiput. Prevention of friction injury includes the use of customized splinting over infants’ heels; gel pillows under the head of infants and toddlers; moisturizing agents; transparent dressings over susceptible areas; and soft, smooth bed linens and clothing (Baharestani and Ratliff, 2007). By itself, friction does not cause tissue necrosis, but when it acts with gravity, it results in shear injury.
Shear is the result of the force of gravity pushing down on the body and friction of the body against a surface, such as the bed or chair. For example, when a patient is in the semi-Fowler position and begins to slide to the foot of the bed, the skin over the sacral area remains in the same place because of the resistance of the bed surface. The blood vessels in the area are stretched and may cause small-vessel thrombosis and tissue death (Bryant and Doughty, 2000). Prevention of shear injury includes using lift sheets when repositioning a patient, elevating the bed no more than 30 degrees for short periods, and using the knee gatch to interrupt the pull of gravity on the body toward the foot of the bed.
Epidermal stripping results when the epidermis is unintentionally removed when tape is removed. These lesions are usually shallow and irregularly shaped. Babies are at increased risk for epidermal injury. Prevention includes using no tape when possible, securing dressings with laced binders (Montgomery straps) or stretchy netting (Spandage or stockinette). Using porous or low-tack tapes (e.g., Medipore, paper, hydrogel), using alcohol-free skin sealants (No Sting Barrier Film), or picture framing wounds with hydrocolloid or wafer barriers (e.g., DuoDERM, Coloplast, Stomahesive) and then taping on top of the barrier also will reduce epidermal stripping.
Tape is placed so that there is no tension, traction, or wrinkles on the skin. To remove tape, slowly peel the tape away while stabilizing the underlying skin. Adhesive remover may be used to break the adhesive bond but may be drying to the skin. Avoid adhesive removers in preterm neonates, since absorption rates vary and toxicity may occur. Remove the adhesive with water to prevent absorption and irritation. Wetting the tape with water or alcohol-based foam hand cleansers may facilitate removal.
Chemical factors can also lead to skin damage. Fecal incontinence, especially when mixed with urine; wound drainage; or gastric drainage around gastrostomy tubes can erode the epidermis. The skin can quickly progress from redness to denudement if exposure continues. Moisture barriers, gentle cleansing as soon after exposure as possible, and skin barriers can be used to prevent damage caused by chemical factors. In addition, foam dressings that wick moisture away from the skin are helpful around gastrostomy tubes and tracheostomy sites.
Bathing
![]() Most infants and children can be bathed in a basin at the bedside or on the bed, in a standard bathtub or shower. For infants and young children confined to bed, use the towel method. Immerse two towels in a dilute soap solution and wring them damp. With the child lying supine on a dry towel, place one damp towel on top of the child and use it to gently clean the body. Discard this towel, and dry the child and turn him or her prone. Repeat the procedure using the second damp towel. Commercially available bath cloths may also be used.
Most infants and children can be bathed in a basin at the bedside or on the bed, in a standard bathtub or shower. For infants and young children confined to bed, use the towel method. Immerse two towels in a dilute soap solution and wring them damp. With the child lying supine on a dry towel, place one damp towel on top of the child and use it to gently clean the body. Discard this towel, and dry the child and turn him or her prone. Repeat the procedure using the second damp towel. Commercially available bath cloths may also be used.
Infants and small children are never left unattended in a bathtub, and infants who are unable to sit alone are securely held with one hand during the bath. The nurse securely supports the infant’s head with one hand, or grasps the infant’s farther arm while the head rests comfortably on the nurse’s arm. Children who are able to sit without assistance need only close supervision and a pad placed in the bottom of the tub to prevent slipping and loss of balance.
School-age children and adolescents may shower or bathe. Nurses need to use judgment regarding the amount of supervision the child requires. Some can assume this responsibility unaided, whereas others need someone in constant attendance. Children with cognitive impairments, physical limitations such as severe anemia or leg deformities, or suicidal or psychotic problems (who may commit bodily harm) require close supervision.
Areas that require special attention are ears, between skinfolds, neck, back, and genital area. The genital area should be carefully cleansed and dried, with particular care given to skinfolds. In uncircumcised boys, usually those over 3 years of age, the foreskin should be gently retracted, the exposed surfaces cleansed, and the foreskin then replaced. If the condition of the glans indicates inadequate cleaning, such as accumulated smegma, inflammation, phimosis, or foreskin adhesions, teaching proper hygiene is indicated. In the Vietnamese and Cambodian cultures the foreskin is traditionally not retracted until adulthood. Older children have a tendency to avoid cleaning the genitalia; therefore they may need a gentle reminder.
Oral Hygiene
Mouth care is an integral part of daily hygiene and should be continued in the hospital. For some young children, this is their first introduction to the use of a toothbrush. Infants and debilitated children require the nurse or a family member to perform mouth care. Although young children can manage a toothbrush and are encouraged to use it, most need assistance to perform satisfactorily. Older children, although capable of brushing and flossing without assistance, sometimes need to be reminded.
Hair Care
Children should have their hair brushed and combed at least once daily. The hair is styled for comfort and in a manner pleasing to the child and parents. The hair should not be cut without parental permission, although clipping hair to provide access to a scalp vein for IV insertion may be necessary.
If children are hospitalized for more than a few days, the hair may need shampooing. With infants, the hair may be washed during the daily bath or less frequently. For most children, washing the hair and scalp once or twice weekly is sufficient unless there is an indication for more frequent washing, such as following a high fever and profuse sweating. Adolescents normally have increased oily sebaceous secretions that require frequent hair care and more frequent shampoos.
Almost any child can be transported to an accessible sink for shampooing. Those who are unable to be transported can receive a shampoo in their beds with adequate protection, specially adapted equipment or positioning, or dry shampoo caps. When necessary, a shampoo basin may be used or the child may be positioned near the edge of the bed, towels placed under the shoulders, a large plastic garbage bag draped at the edge of the bed with one open end under the shoulders, and the hair placed inside the opening. The other end is opened and placed in a collection container. Water can be transported in a basin.
For the child with curly hair, most standard combs are inadequate and may cause hair breakage and discomfort. Use a special comb with widely spaced teeth. It is also much easier to comb the hair after shampooing when it is wet. Use a special hair dressing or pomade, which usually has a coconut oil base. Rub the preparation on the hands and then transfer it to the hair to make it more pliable and manageable. Consult the child’s parents regarding the preparation to use on the child’s hair and ask if they can provide some for use during the child’s hospitalization. Petroleum jelly should not be used. If braiding or plaiting the hair, weave it loosely while the hair is damp. The hair tightens as it dries, which could result in tension folliculitis.
Feeding the Sick Child
Loss of appetite is a symptom common to most childhood illnesses. Because an acute illness is usually short, the nutritional state is seldom compromised. Urging food on the sick child may precipitate nausea and vomiting. In most cases children can usually determine their own need for food.
Refusing to eat may also be one way children can exert power and control in an otherwise helpless situation. For young children, loss of appetite may be related to depression caused by separation from their parents. Parents’ concern with eating can intensify the problem. Forcing a child to eat meets with rebellion and reinforces the behavior as a control mechanism. Encourage parents to relax any pressure during an acute illness. Although it is best to provide high-quality nutritious foods, the child may desire foods and liquids that contain mostly empty or nonnutritional calories. Some well-tolerated foods include gelatin, diluted clear soups, carbonated drinks, flavored ice pops, dry toast, and crackers. Even though these substances are not nutritious, they can provide necessary fluid and calories.
Dehydration is always a hazard when children have a fever or anorexia, especially when accompanied by vomiting or diarrhea. Fluids should not be forced, and the child is not awakened to take fluids. Forcing fluids may create the same difficulties as urging the child to eat unwanted food. Gentle persuasion with preferred beverages will usually meet with success. Using play techniques can also be effective (see Nursing Care Guidelines box).
An understanding of children’s feeding habits can also increase food consumption. For example, if children are given all their food at one time, they generally eat the dessert first. Likewise, if they are presented with large portions, they often push the food away because the amount overwhelms them. If young children are not supervised during mealtime, they tend to play with the food rather than eat it. Therefore nurses should present food in the usual order, such as soup first, followed by small portions of meat, potatoes, and vegetables, and ending with dessert. The principles of conservation can also be used to increase food consumption. (See Cognitive Development, Chapter 15.)
Once the child is feeling better, appetite usually begins to improve. It is best to take advantage of any hungry period by serving high-quality foods and snacks. If the child still refuses to eat, offer nutritious fluids, such as prepared breakfast drinks. Parents can help by bringing in food items from home, especially if the family’s cultural eating habits differ from the hospital food. A clinical dietitian may be consulted for alternative food choices.
When children are placed on special diets, such as clear liquids after surgery or during episodes of diarrhea, assessment of their intake and readiness to advance to more complex foods is essential.
Regardless of the type of diet, charting the amount consumed is an important nursing responsibility. Descriptions need to be detailed and accurate, such as “4 oz of orange juice, one pancake, and 8 oz of milk.” Comments such as “ate well” or “ate poorly” are inadequate. Charting the percentage of the meal eaten is also inadequate unless food is measured before serving.
If parents are involved in the child’s care, encourage them to keep a list of everything eaten. Using a premeasured cup for fluids ensures a more accurate estimate of intake. A comparison of the intake at each meal can isolate food deficiencies, such as insufficient intake of meat or vegetables. Behaviors associated with mealtime also identify possible factors influencing appetite. For example, the observation, “Child eats well when with other children but plays with food if left alone in room,” helps the nurse plan mealtime activities that stimulate the child’s appetite.
Although sick children’s appetites may be poor and not characteristic of their home eating habits, the hospital stay provides numerous opportunities for nurses to assess the family’s knowledge of good nutrition and to implement teaching as needed to improve nutritional intake.
Controlling Elevated Temperatures
![]() An elevated temperature, most frequently from fever but occasionally caused by hyperthermia, is one of the most common symptoms of illness in children. This manifestation is a great concern to parents. To facilitate an understanding of fever, the following terms are defined:
An elevated temperature, most frequently from fever but occasionally caused by hyperthermia, is one of the most common symptoms of illness in children. This manifestation is a great concern to parents. To facilitate an understanding of fever, the following terms are defined:
![]() Nursing Care Plan—The Child with Elevated Body Temperature
Nursing Care Plan—The Child with Elevated Body Temperature
Set point—The temperature around which body temperature is regulated by a thermostat-like mechanism in the hypothalamus
Fever (hyperpyrexia)—An elevation in set point such that body temperature is regulated at a higher level; may be arbitrarily defined as temperature above 38° C (100.4° F)
Hyperthermia—Body temperature exceeding the set point, which usually results from the body or external conditions creating more heat than the body can eliminate, such as in heat stroke, aspirin toxicity, seizures, or hyperthyroidism
Body temperature is regulated by a thermostat-like mechanism in the hypothalamus. (See Chapter 6.) This mechanism receives input from centrally and peripherally located receptors. When temperature changes occur, these receptors relay the information to the thermostat, which either increases or decreases heat production to maintain a constant set point temperature. However, during an infection, pyrogenic substances cause an increase in the body’s normal set point, a process that is mediated by prostaglandins. Consequently, the hypothalamus increases heat production until the core temperature reaches the new set point.
During the fever (febrile) state, shivering and vasoconstriction generate and conserve heat during the chill phase of fever, raising central temperatures to the level of the new set point. The temperature reaches a plateau when it stabilizes in the higher range. When the temperature is greater than the set point or when the pyrogen is no longer present, a crisis, or defervescence, of the temperature occurs.
Most fevers in children are of brief duration with limited consequences and are viral in origin. When fever is caused by bacteria, endotoxins are produced that activate the inflammatory process and produce fever (Rote, Huether, and McCance, 2000). Fever has physiologic benefits: increased white blood cell activity, interferon production and effectiveness, and antibody production and enhancement of some antibiotic effects (Considine and Brennan, 2007). Contrary to popular belief, neither the rise in temperature nor its response to antipyretics indicates the severity or etiology of the infection, which casts doubt on the value of using fever as a diagnostic or prognostic indicator.
Therapeutic Management
Treatment of elevated temperature depends on whether it is due to a fever or hyperthermia. Because the set point is normal in hyperthermia but increased in fever, different approaches must be used to lower body temperature successfully.
Fever: The principal reason for treating fever is the relief of discomfort. Relief measures include pharmacologic and environmental intervention. The most effective intervention is the use of antipyretics to lower the set point.
Antipyretics include acetaminophen, aspirin, and nonsteroidal antiinflammatory drugs (NSAIDs). Acetaminophen is the preferred drug. Aspirin should not be given to children because of its association in children with influenza virus or chickenpox and Reye syndrome. One nonprescription NSAID, ibuprofen, is approved for fever reduction in children as young as 6 months of age (Table 27-3). Dosage is based on the initial temperature level: 5 mg/kg of body weight for temperatures less than 39.2° C (102.6° F) or 10 mg/kg for temperatures greater than 39.2° C. The recommended dosage for pain is 10 mg/kg every 6 to 8 hours, and the recommended maximum daily dose for pain and fever is 40 mg/kg. The duration of fever reduction is generally 6 to 8 hours and is longer with the higher dose.
TABLE 27-3
DOSE RECOMMENDATIONS FOR IBUPROFEN (CHILDREN’S MOTRIN)*
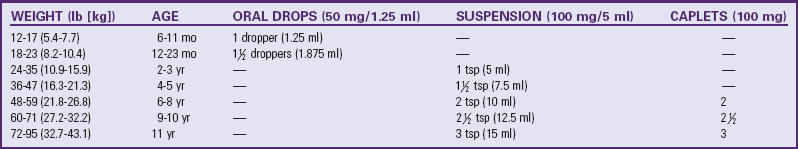
*Dosages based on fever <39.2° C (102.6° F) and a dose of 5 mg/kg. For fever ≥39.2° C, may use 10 mg/kg. Doses administered every 6-8 hr. Another nonprescription ibuprofen is Children’s Advil.
Modified from McNeil Consumer Healthcare: Motrin, 2010, available at www.motrin.com (accessed March 5, 2010).
The recommended doses of acetaminophen are listed in Table 27-4. Acetaminophen should be given every 4 hours, but no more than five times in 24 hours. Because body temperature normally decreases at night, three or four doses in 24 hours will control most fevers. The temperature is usually retaken 30 minutes after the antipyretic is given to assess its effect but should not be repeatedly measured. The child’s level of discomfort is the best indication for continued treatment.
TABLE 27-4
DOSE RECOMMENDATIONS FOR ACETAMINOPHEN (TYLENOL)*
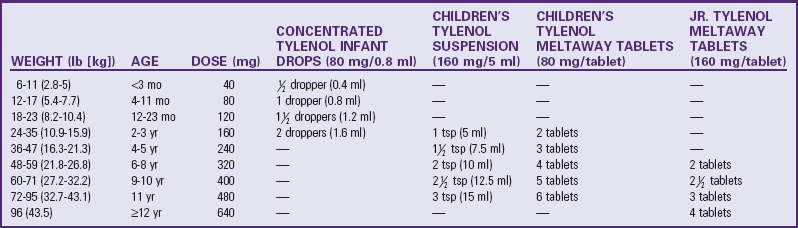
*Doses should be administered 4-5 times daily but should not exceed 5 doses in 24 hr.
The nurse can use environmental measures to reduce fever if they are tolerated by the child and if they do not induce shivering. Shivering is the body’s way of maintaining the elevated set point by producing heat. Compensatory shivering greatly increases metabolic requirements above those already caused by the fever.
Traditional cooling measures, such as wearing minimum clothing, exposing the skin to air, reducing room temperature, increasing air circulation, and applying cool, moist compresses to the skin (e.g., the forehead), are effective if employed approximately 1 hour after an antipyretic is given so that the set point is lowered. Cooling procedures such as sponging or tepid baths are ineffective in treating febrile children (these measures are effective for hyperthermia) either when used alone or in combination with antipyretics, and they cause considerable discomfort (Axelrod, 2000).
Seizures associated with a fever occur in 3% to 4% of all children, usually in those between 6 months and 6 years of age. About 30% of children have subsequent febrile seizures; a younger age at onset and a family history of febrile seizures are associated with increased incidence of recurring episodes. There is little evidence to support the use of antipyretic drugs or anticonvulsants to prevent a second febrile seizure; nursing intervention should focus on ways to provide care and comfort during a febrile illness. Simple febrile seizures lasting less than 10 minutes do not cause brain damage or other debilitating effects (Jones and Jacobsen, 2007; Sadleir and Scheffer, 2007). (See Febrile Seizures, Chapter 37.)
Hyperthermia: Unlike in fever, antipyretics are of no value in hyperthermia because the set point is already normal. Consequently, cooling measures are used. Cool applications to the skin help reduce the core temperature. Cooled blood from the skin surface is conducted to inner organs and tissues, and warm blood is circulated to the surface, where it is cooled and recirculated. The surface blood vessels dilate as the body attempts to dissipate heat to the environment and facilitate this cooling process.
Commercial cooling devices, such as cooling blankets or mattresses, are available to reduce body temperature. Place the patient on the bed and cover with a sheet or lightweight blanket. Frequent temperature monitoring is essential to prevent excessive cooling of the body.
Traditionally, cool compresses decrease high temperature. For tepid tub baths, it is usually best to start with warm water and gradually add cool water until the desired water temperature of 37° C (98.6° F) is reached to acclimate the child to the lower water temperature. Generally the temperature of the water only has to be 1° C (or 2° F) less than the child’s temperature to be effective. The child is placed directly in the tub of tepid water for 15 to 20 minutes while water is gently squeezed from a washcloth over the back and chest or gently sprayed over the body from a sprayer. In the bed or crib, cool washcloths or towels are used, exposing only one area of the body at a time. Continue sponging for approximately 20 minutes.
After the tub or sponge bath, the child is dried and dressed in lightweight pajamas, a nightgown, or a diaper and placed in a dry bed. The child is dried by gently rubbing the skin surface with a towel to stimulate circulation. The temperature is retaken 30 minutes after the tub or sponge bath. The tub or sponge bath should not be continued or restarted until the skin surface is warm or if the child feels chilled. Chilling causes vasoconstriction, which defeats the purpose of the cool applications. In this condition, little blood is carried to the skin surface; the blood remains primarily in the viscera to become heated.
Whether a temperature elevation in the critically ill child is caused by fever or hyperthermia, it should be treated aggressively. The metabolic rate increases 10% for every 1° C increase in temperature and three to five times during shivering, thus increasing oxygen, fluid, and caloric requirements. If the child’s cardiovascular or neurologic system is already compromised, these increased needs are especially hazardous. In all children with an elevated temperature, attention to adequate hydration is essential. Most children’s needs can be met through additional oral fluids.
Family Teaching and Home Care
Fever is one of the most common problems for which parents seek health care. High levels of parental anxiety (fever phobia) surrounding potential complications of fever such as seizures and dehydration are prevalent and can result in overusing antipyretics (Purssell, 2008). Parents need to know that sponging is indicated for elevated temperatures from hyperthermia rather than fever and that ice water and alcohol are inappropriate, potentially dangerous solutions (Axelrod, 2000). Parents should know how to take the child’s temperature, how to read the thermometer accurately, and when to seek professional care (see Family-Centered Care box). Some of the newer temperature-measuring devices, such as plastic strip or digital thermometers, may be better suited for home use. (See Temperature, Chapter 6.) If the use of acetaminophen or ibuprofen is indicated, the parents need instructions in administering the drug. Emphasize accuracy in both the amount of drug given and the time intervals at which the drug is administered. Along with reduced activity, encourage small, frequent sips of clear liquids. Dress the child in light clothing; use a light blanket for children who are cold or shivering (Walsh and Edwards, 2006).
Safety
Safety is an essential component of any patient’s care, but children have special characteristics that require an even greater concern for safety. Because small children in the hospital are separated from their usual environment and do not possess the capacity for abstract thinking and reasoning, it is the responsibility of everyone who comes in contact with them to maintain protective measures throughout their hospital stay. Nurses need to understand the age level at which each child is operating and plan for safety accordingly.
Identification bands are particularly important for children. Infants and unconscious patients are unable to tell or respond to their names. Toddlers may answer to any name or to a nickname only. Older children may exchange places, give an erroneous name, or choose not to respond to their own names as a joke, unaware of the hazards of such practices.
Environmental Factors
All the environmental safety measures for the protection of adults apply to children, including good illumination, floors clear of fluid or objects that might contribute to falls, and nonskid surfaces in showers and tubs. All staff members should be familiar with the area-specific fire plan. Elevators and stairways should be made safe.
All windows should be secured. Blind and curtain cords should be out of reach with split cords to prevent strangulation. Pacifiers should not be tied around the neck or attached to an infant by string.
Electrical equipment should be in good working order and used only by personnel familiar with its use. It should not be in contact with moisture or situated near tubs. Electrical outlets should have covers to prevent burns in small children, whose exploratory activities may extend to inserting objects into the small openings.
Staff members should practice proper care and disposal of small objects such as syringe caps, needle covers, and temperature probes. Staff also must carefully check bathwater before placing the child in it and never leave children alone in a bathtub. Infants are helpless in water, and small children (and some older ones) may turn on the hot water faucet and be severely burned.
Furniture is safest when it is scaled to the child’s proportions, is sturdy, and is well balanced to prevent its being easily tipped over. A special hazard for children is the danger of entrapment under an electronically controlled bed when it is activated to descend. Infants and small children must be securely strapped into infant seats, feeding chairs, and strollers. Baby walkers should not be used because they provide access to hazards, resulting in burns, falls, and poisonings. Infants; young children; and those who are weak, paralyzed, agitated, confused, sedated, or cognitively impaired are never left unattended on treatment tables, on scales, or in treatment areas. Even premature infants are capable of surprising mobility; therefore portholes in incubators must be securely fastened when not in use.
Crib sides are kept up and fastened securely unless an adult is at the bedside. It is safer to leave crib sides up, regardless of the child’s ability to get out and even when the crib is unoccupied, to remove the temptation to climb in. Anyone attending an infant or small child in a crib with the sides down should never turn away without maintaining hand contact with the child, that is, keeping one hand on the child’s back or abdomen to prevent rolling, crawling, or jumping from the open crib (Fig. 27-3). A child who is likely to climb over the sides of the crib is safest when placed in a specially constructed crib with a cover over the top. (See Injury Prevention, Chapter 12.)
The safest sleeping position to prevent sudden infant death syndrome is wholly supine (American Association of Pediatrics, 2005). No pillows should be placed in a young infant’s crib while the infant is sleeping.
Toys
Toys play a vital role in the everyday life of children, and they are no less important in the hospital setting. Nurses are responsible for assessing the safety of toys brought to the hospital by well-meaning parents and friends. Toys should be appropriate to the child’s age, condition, and treatment. For example, if the child is receiving oxygen, electrical or friction toys or equipment are not safe, since sparks can cause oxygen to ignite. Inspect toys to ensure they are nonallergenic, washable, and unbreakable and that they have no small, removable parts that can be aspirated or swallowed or can otherwise inflict injury on a child. All objects within reach of children younger than 3 years should pass the choke tube test. A toilet paper roll is a handy guide. If a toy or object fits into the cylinder (items  inches across or balls
inches across or balls  inches in diameter), it is a potential choking danger to the child. Latex balloons pose a serious threat to children of all ages. If the balloon breaks, a child may put a piece of the latex in his or her mouth. If it is aspirated or swallowed, the latex piece is difficult to remove, resulting in choking. Latex balloons should never be permitted in the hospital setting.
inches in diameter), it is a potential choking danger to the child. Latex balloons pose a serious threat to children of all ages. If the balloon breaks, a child may put a piece of the latex in his or her mouth. If it is aspirated or swallowed, the latex piece is difficult to remove, resulting in choking. Latex balloons should never be permitted in the hospital setting.
Preventing Falls
Falls prevention begins with identification of children most at risk for falls. Pediatric hospitals use various methods to identify a child’s risk of falls (Child Health Corporation of America, 2009). Once a risk assessment is performed, multiple interventions are needed to minimize pediatric patients’ risk of falling, including education of patient, family, and staff.
To identify children at risk of falling, perform a fall risk assessment on patients on admission and throughout hospitalization. Risk factors for hospitalized children include:
• Medication effects—Postanesthesia or sedation; analgesics or narcotics, especially in those who have never had narcotics in the past and in whom effects are unknown
• Altered mental status—Secondary to seizures, brain tumors, or medications
• Altered or limited mobility—Reduced skill at ambulation secondary to developmental age, disease process, tubes, drains, casts, splints, or other appliances; new to ambulation with assistive devices such as walkers or crutches
• Postoperative children—Risk of hypotension or syncope secondary to large blood loss, a heart condition, or extended bed rest
• Infants or toddlers in cribs with side rails down or on the daybed with family members
Once children at risk of falls have been identified, alert other staff members by posting signs on the door and at the bedside, applying a special colored armband labeled “Fall Precautions,” labeling the chart with a sticker, or documenting information on the chart.
Prevention of falls requires alterations in the environment, including:
• Keep bed in lowest position, breaks locked, and side rails up.
• Place call bell within reach.
• Ensure that all necessary and desired items are within reach (e.g., water, glasses, tissues, snacks).
• Offer toileting on a regular basis, especially if patient is taking diuretics or laxatives.
• Keep lights on at all times, including dim lights while sleeping.
• Lock wheelchairs before transferring patients.
• Ensure that patient has appropriate size gown and nonskid footwear. Do not allow gowns or ties to drag on the floor during ambulation.
• Keep floor clean and free of clutter. Post “wet floor” sign if floor is wet.
• Ensure that patient has glasses on if he or she normally wears them.
Preventing falls also relies on age-appropriate education of patients. Assist the child with ambulation even though he or she may have ambulated well before hospitalization. Patients who have been lying in bed need to get up slowly, sitting on the side of the bed before standing.
The nurse also needs to educate family members:
• Call the nursing staff for assistance, and do not allow patients to get up independently.
• Keep the side rails of the crib or bed up whenever patient is in the crib or bed.
• Do not leave infants on the daybed; put them in the crib with the side rails up.
• When all family members need to leave the bedside, notify staff and ensure the patient is in the bed or crib with side rails up and call bell within reach (if appropriate).
Infection Control
According to the Centers for Disease Control and Prevention, approximately 2 million patients each year develop nosocomial (hospital-acquired) infections. These infections occur when there is interaction among patients, health care personnel, equipment, and bacteria (Quality, Equipment Hold Keys to Infection Control, 2006). Nosocomial infections are preventable if caregivers practice meticulous cleaning and disposal techniques.
Standard Precautions synthesize the major features of Universal (blood and body fluid) Precautions (designed to reduce the risk of transmission of blood-borne pathogens) and body substance isolation (designed to reduce the risk of transmission of pathogens from moist body substances). Standard Precautions involve the use of barrier protection, such as gloves, goggles, gown, or mask, to prevent contamination from (1) blood; (2) all body fluids, secretions, and excretions except sweat, regardless of whether they contain visible blood; (3) nonintact skin; and (4) mucous membranes. Standard Precautions are designed for the care of all patients to reduce the risk of transmission of microorganisms from both recognized and unrecognized sources of infection.
Transmission-Based Precautions are designed for patients with documented or suspected infection or colonization (presence of microorganisms in or on patient but without clinical signs and symptoms of infection) with highly transmissible or epidemiologically important pathogens for which additional precautions beyond Standard Precautions are needed to interrupt transmission in hospitals. There are three types of Transmission-Based Precautions: Airborne Precautions, Droplet Precautions, and Contact Precautions. They may be combined for diseases that have multiple routes of transmission (Box 27-3). They are to be used in addition to Standard Precautions.
Airborne Precautions reduce the risk of airborne transmission of infectious agents. Airborne transmission occurs by dissemination of either airborne droplet nuclei (small-particle residue [≤5 mm] of evaporated droplets that may remain suspended in the air for long periods) or dust particles containing the infectious agent. Microorganisms carried in this manner can be dispersed widely by air currents and may become inhaled by or deposited on a susceptible host within the same room or over a longer distance from the source patient, depending on environmental factors. Special air handling and ventilation are required to prevent airborne transmission. Airborne Precautions apply to patients with known or suspected infection with pathogens transmitted by the airborne route such as measles, varicella, and tuberculosis.
Droplet Precautions reduce the risk of droplet transmission of infectious agents. Droplet transmission involves contact of the conjunctivae or the mucous membranes of the nose or mouth of a susceptible person with large-particle droplets (>5 mm) containing microorganisms generated from a person who has a clinical disease or who is a carrier of the microorganism. Droplets are generated from the source person primarily during coughing, sneezing, or talking and during procedures such as suctioning and bronchoscopy. Transmission requires close contact between source and recipient persons, since droplets do not remain suspended in the air and generally travel only short distances, usually 3 feet or less, through the air. Because droplets do not remain suspended in the air, special air handling and ventilation are not required to prevent droplet transmission. Droplet Precautions apply to any patient with known or suspected infection with pathogens that can be transmitted by infectious droplets (see Box 27-3).
Contact Precautions reduce the risk of transmission of microorganisms by direct or indirect contact. Direct-contact transmission involves skin-to-skin contact and physical transfer of microorganisms to a susceptible host from an infected or colonized person, such as occurs when turning or bathing patients. Direct-contact transmission also can occur between two patients (e.g., by hand contact). Indirect contact transmission involves contact of a susceptible host with a contaminated intermediate object, usually inanimate, in the patient’s environment. Contact Precautions apply to specified patients known or suspected to be infected or colonized with microorganisms that can be transmitted by direct or indirect contact.
Nurses caring for young children are frequently in contact with body substances, especially urine, feces, and vomitus. Nurses need to exercise judgment concerning those situations when gloves, gowns, or masks are necessary. For example, wear gloves and possibly gowns for changing diapers when there are loose or explosive stools. Otherwise, the plastic lining of disposable diapers provides a sufficient barrier between the hands and body substances.
Antimicrobial-resistant organisms are causing increasing numbers of nosocomial infections. In hospitals, patients are the most significant sources of methicillin-resistant Staphylococcus aureus, and the main mode of transmission is patient to patient via the hands of a health care provider (Eaton, 2005; Quality, Equipment Hold Keys to Infection Control, 2006). Hand washing is the most critical infection control practice.
During feedings, wear gowns if the child is likely to vomit or spit up, which often occurs during burping. When wearing gloves, wash the hands thoroughly after removing the gloves, since gloves fail to provide complete protection. The absence of visible leaks does not indicate that gloves are intact.
Another essential practice of infection control is that all needles (uncapped and unbroken) are disposed of in a rigid, puncture-resistant container located near the site of use. Consequently, these containers are installed in patients’ rooms. Since children are naturally curious, extra attention is needed in selecting a suitable type of container and a location that prevents access to the discarded needles (Fig. 27-4). The use of needleless systems allows secure syringe or IV tubing attachment to vascular access devices without the risk of needlestick injury to the child or nurse.