Medical-Surgical Problems in Pregnancy
• Describe the management of cardiovascular disorders in pregnant women.
• Identify nursing interventions for a pregnant woman with a cardiovascular disorder.
• Discuss anemia during pregnancy.
• Explain the care of pregnant women with pulmonary disorders.
• Examine the effect of a gastrointestinal disorder on gastrointestinal function during pregnancy.
• Identify the effects of neurologic disorders on pregnancy.
• Describe the care of women whose pregnancies are complicated by autoimmune disorders.
• Differentiate signs and symptoms and management during pregnancy of urinary tract infections.
• Explain the basic principles of care for a pregnant woman having surgery.
For most women, pregnancy represents a normal part of life. This chapter discusses the care of women for whom pregnancy represents a significant risk because it is superimposed on a preexisting medical condition. Care of women with normal pregnancies who develop medical or surgical problems that could happen to anyone at any time of life but occur during pregnancy is also discussed. With the active participation of well-motivated women in the treatment plan and careful management from a multidisciplinary health care team, positive pregnancy outcomes are often possible in both of these situations.
This chapter focuses on cardiovascular disorders, along with selected respiratory, integumentary, neurologic, autoimmune, gastrointestinal, and urinary tract diseases. Care of the pregnant woman undergoing surgery is also discussed.
Cardiovascular Disorders
During a normal pregnancy the maternal cardiovascular system undergoes many changes that place a physiologic strain on the heart. The major cardiovascular changes that occur during a normal pregnancy and that affect the woman with cardiac disease are increased intravascular volume, decreased systemic vascular resistance, cardiac output changes occurring during labor and birth, and the intravascular volume changes that occur just after childbirth. These physiologic changes are present during pregnancy and continue for a few weeks after birth. The normal heart can compensate for the increased workload so that pregnancy, labor, and birth are generally well tolerated, but the diseased heart is hemodynamically challenged.
If the cardiovascular changes are not well tolerated, cardiac failure can develop during pregnancy, labor, or the postpartum period. In addition, if myocardial disease develops, valvular disease exists, or a congenital heart defect is present, cardiac decompensation (inability of the heart to maintain a sufficient cardiac output) may occur.
About 1% of pregnancies are complicated by serious heart disease. The risk of maternal morbidity and mortality ranges from low to high, depending on the cardiac defect (Tomlinson, 2006). Congenital diseases and mitral valve disease are increasing in women of childbearing age, whereas the incidence of rheumatic fever has diminished. The presence of a maternal congenital cardiac defect increases the risk to the fetus for a congenital heart defect from 1% to about 4% to 6% (Easterling & Stout, 2007). A perinatal mortality of up to 50% is anticipated with persistent cardiac decompensation. Box 30-1 lists maternal cardiac disease risk groups.
The degree of disability experienced by the woman with cardiac disease is often more important in the treatment and prognosis of cardiac disease complicating pregnancy than is the diagnosis of cardiovascular disease. The New York Heart Association’s (NYHA) functional classification of organic heart disease is a widely accepted standard:
• Class I: asymptomatic without limitation of physical activity
• Class II: symptomatic with slight limitation of activity
• Class III: symptomatic with marked limitation of activity
• Class IV: symptomatic with inability to carry on any physical activity without discomfort
No classification of heart disease can be considered rigid or absolute, but the NYHA classification offers a basic practical guide for treatment, assuming that frequent prenatal visits, good client cooperation, and appropriate obstetric care occur. The functional classification may change for the pregnant woman because of the hemodynamic changes that occur in the cardiovascular system during pregnancy. A 30% to 45% increase in cardiac output occurs compared with nonpregnancy resting values, with most of the increase in the first trimester and the peak at 20 to 26 weeks of gestation (Blanchard & Shabetai, 2009). The functional classification of the disease is determined at 3 months and again at 7 or 8 months of gestation. Pregnant women may progress from class I or II to III or IV during the pregnancy. Women with cyanotic congenital heart disease do not fit into the NYHA classification because their exercise-induced symptoms have causes unrelated to heart failure.
A diagnosis of cardiac disease depends on the history, physical examination, radiographic and electrocardiographic findings, Holter monitoring, and, if indicated, ultrasonographic results. Most diagnostic studies are noninvasive and can be safely performed during pregnancy. The differential diagnosis of heart disease also involves ruling out respiratory problems and other potential causes of chest pain.
The maternal mortality rate in women with cardiac events is higher than that for abortion, genital tract sepsis, and hemorrhage (Setaro & Caulin-Glaser, 2004). The highest risk of complications or death occurs in women with pulmonary hypertension, complicated coarctation of the aorta, and Marfan syndrome with aortic involvement (Tomlinson, 2006).
Cardiac diseases vary in their effect on pregnancy depending on whether they are acute or chronic conditions. The following discussion focuses on selected congenital and acquired cardiac conditions and other cardiac disorders. A review of the care of the pregnant woman who has had a heart transplant concludes this section.
Congenital Cardiac Disease
Atrial Septal Defect: Atrial septal defect (ASD) (an abnormal opening between the atria), one of the causes of a left-to-right shunt, is one of the most common congenital defects seen during pregnancy. This defect may go undetected because the woman usually is asymptomatic. The pregnant woman with an ASD will most likely have an uncomplicated pregnancy. Some women may have right-sided heart failure or arrhythmias as the pregnancy progresses as a result of increased plasma volume. The risk to the fetus of a woman with ASD for congenital heart disease is 3% to 10% (Tomlinson, 2006).
Ventricular Septal Defect: Ventricular septal defect (VSD) (an abnormal opening between the right and left ventricles), another cause of a left-to-right shunt, is usually diagnosed and corrected early in life. As a result, a VSD is not very common in pregnancy. Women with small, uncomplicated VSDs usually do not have pregnancy complications. For women with a large VSD, there is a higher risk for arrhythmias, heart failure, and pulmonary hypertension. Medical management includes rest and decreased physical activity, as well as administration of anticoagulants, if indicated. The fetus has a 6% to 10% risk of a congenital heart defect (Tomlinson, 2006).
Acyanotic Lesions
Coarctation of the Aorta: Coarctation of the aorta (localized narrowing of the aorta near the insertion of the ductus) is an example of an acyanotic congenital heart lesion. If at all possible, the lesion should be corrected surgically before pregnancy. However, pregnancy is usually relatively safe for the woman with uncomplicated, uncorrected, coarctation. Maternal mortality is about 3% for uncorrected defects (Blanchard & Shabetai, 2009). Complications that can occur include hypertension, congestive heart failure, aortic dissection, aneurysm, and rupture. The mainstays of treatment for uncorrected coarctation of the aorta during pregnancy are rest and antihypertensive medications, preferably beta-adrenergic blocking agents. Vaginal birth is preferable, with epidural anesthesia and shortening of the second stage with vacuum extraction or use of forceps, if necessary. Beta-blockers should be continued throughout labor. Because of the risk of endocarditis, antibiotic prophylaxis is recommended at birth (see later discussion).
Cyanotic Lesions
Tetralogy of Fallot: Tetralogy of Fallot is by far the most common cyanotic heart disease observed during pregnancy (Blanchard & Shabetai, 2009). Components of tetralogy of Fallot include a VSD, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy, leading to a right-to-left shunt. Women with tetralogy of Fallot are encouraged to have surgical repair before conception because pregnancy does not cause a significant risk once the VSD and pulmonary stenosis have been repaired. Women with uncorrected tetralogy of Fallot, however, experience more right-to-left shunting during pregnancy, resulting in reduced blood flow through the pulmonary circulation and increasing hypoxemia, which can cause syncope or death. Maintenance of venous return in women with uncorrected tetralogy of Fallot is critical. Therefore, the most dangerous time for these women is the late third trimester of pregnancy and the early postpartum period, when venous return is reduced by the large pregnant uterus and by peripheral venous pooling after birth. Use of pressure-graded support hose is recommended. Blood loss during birth may also adversely affect venous return, thus blood volume must be adequately maintained. Prophylactic antibiotics should be given during the intrapartum period (Blanchard & Shabetai).
Acquired Cardiac Disease
Mitral valve stenosis (narrowing of the opening of the mitral valve caused by stiffening of valve leaflets, which obstructs blood flow from the left atrium to the left ventricle) is the characteristic lesion resulting from rheumatic heart disease (RHD) (Tomlinson, 2006). As the mitral valve narrows, dyspnea worsens, occurring first on exertion and eventually at rest. A tight stenosis plus the increase in blood volume and cardiac output of normal pregnancy may cause pulmonary edema, atrial fibrillation, right-sided heart failure, infective endocarditis, pulmonary embolism, and massive hemoptysis (Blanchard & Shabetai, 2009; Cunningham, Leveno, Bloom, Hauth, Rouse, & Spong, 2010). Maternal mortality is related to functional capacity. Almost all maternal deaths related to mitral stenosis occur in women who are classified as NYHA class III or class IV (Cunningham et al.).
Pharmacologic treatment for women with a history of rheumatic heart disease includes beta-blockers or calcium channel blockers to prevent tachycardia (Easterling & Stout, 2007). A combination of drugs will most likely be needed. Cardioversion may be needed for new-onset atrial fibrillation. Women who have chronic atrial fibrillation may require digoxin or beta-blockers to control the heart rate. In addition, anticoagulant therapy may be needed to prevent embolism (Blanchard & Shabetai, 2009). About 25% of women with mitral valve stenosis experience cardiac failure for the first time during pregnancy (Cunningham et al., 2010). The care of the woman with mitral stenosis typically is managed by reducing her activity, restricting dietary sodium, and monitoring weight. The pregnant woman with mitral stenosis should be assessed clinically for symptoms and with echocardiograms to monitor the atrial and ventricular size, as well as heart valve function. Prophylaxis for intrapartum endocarditis and pulmonary infections may be provided for women at high risk (Blanchard & Shabetai; Easterling & Stout) (Box 30-2).
During labor adequate pain control is required to prevent tachycardia. Epidural analgesia for labor is preferred (Tomlinson, 2006). Shortening the second stage of labor is also important to decrease the cardiac workload. Even with close monitoring, the woman with moderate to severe mitral stenosis is at risk for pulmonary edema, right-sided heart failure, and hypotension. Central hemodynamic monitoring may be necessary for some women during labor, birth, and the postpartum period because fluid shifts can place the woman at risk for pulmonary edema.
For women with NYHA class III or IV cardiac disease, percutaneous balloon mitral valvuloplasty can be performed, but this procedure should be considered only when symptoms cannot be controlled by standard means. Mitral balloon valvuloplasty is optimally performed after the first trimester to decrease radiation risks to the fetus. This relatively safe nonsurgical procedure is now performed more frequently during pregnancy than surgical valvotomy. The balloon procedure is just as successful as surgical repair but is associated with a lower perinatal mortality rate (Cunningham et al., 2010).
Mitral Valve Prolapse
Mitral valve prolapse (MVP) is a fairly common, usually benign, condition. More specific echocardiographic diagnostic criteria have resulted in significantly reduced prevalence estimates for MVP (perhaps 1% of the female population) than previously thought (Blanchard & Shabetai, 2009). The mitral valve leaflets prolapse into the left atrium during ventricular systole, allowing some backflow of blood. Midsystolic click and late systolic murmur are hallmarks of this syndrome. Most cases are asymptomatic. A few women have atypical chest pain (sharp and located in the left side of the chest) that occurs at rest and does not respond to nitrates. They may also have anxiety, palpitations, dyspnea on exertion, and syncope. Specific treatment usually is not necessary except for symptomatic tachyarrhythmias and rarely, heart failure. Women usually are treated with beta-adrenergic blockers such as atenolol or metoprolol (Lopressor) (Blanchard & Shebetai). Pregnancy and its associated hemodynamic changes may change or alleviate the murmur and click of MVP, as well as symptoms. Antibiotic prophylaxis is usually given before birth to prevent bacterial endocarditis (see Box 30-2). Pregnancy usually is well tolerated unless bacterial endocarditis occurs (Cunningham et al. 2010; Easterling & Stout, 2007).
Aortic Stenosis
Aortic stenosis (narrowing of the opening of the aortic valve leading to an obstruction to left ventricular ejection) is rarely encountered as a complication of pregnancy because most women who develop this condition do so after their childbearing years are over. In the past, the maternal mortality rate was reported to be as high as 17%, but it has decreased over the last several decades (Easterling & Stout, 2007). Medical management is similar to that for mitral stenosis.
Ischemic Heart Disease
Myocardial infarction (MI) (an acute ischemic event) is a rare event in women of childbearing age, usually occurring in the third trimester with a maternal mortality rate of 20% (Tomlinson, 2006). It is estimated to occur in only 1 in 10,000 women during pregnancy and usually in women older than 33 years of age (Blanchard & Shabetai, 2009). It is anticipated that the incidence of MIs will rise, however, considering the increase in the age of childbearing women. No cardiac risk factors are present in approximately 40% of women (Tomlinson). One study, however, found that the three most likely predictors of MI were chronic hypertension, advancing age, and diabetes. Women with intrapartum diagnoses were most likely to have severe preeclampsia or eclampsia. Prenatal or postpartal MIs were most likely related to diabetes, coronary artery disease, and lipid disorders (Martin & Foley, 2007). Women who have MIs during pregnancy or the postpartum period should be assessed for thrombophilias (deficiency of proteins involved in coagulation inhibition), such as antiphospholipid antibody.
Medical management for pregnant women after MI is the same as for nonpregnant women and includes the administration of oxygen, aspirin, beta-blockers, nitrates, and heparin. Labor should be postponed for at least 2 weeks, if possible, in order to allow the myocardium to heal (Martin & Foley, 2007). Women who have had symptomatic cardiac disease during the pregnancy should continue cardiac medications and receive oxygen during labor. Because pain can lead to tachycardia and increased cardiac demands, pain control during labor is crucial. The side-lying position is preferred to avoid pressure on the vena cava. Vaginal birth is preferable, with avoidance of maternal pushing and a vacuum- or forceps-assisted birth (Easterling & Stout, 2007).
Other Cardiac Diseases and Conditions
Primary Pulmonary Hypertension
Women with primary pulmonary hypertension (PPH) have constriction of the arteriolar vessels in the lungs, leading to an increase in the pulmonary artery pressure. As a result of this pathology, there is right ventricular hypertension, right ventricular hypertrophy and dilation, and finally, right ventricular failure with tricuspid regurgitation and systemic congestion. The major physiologic difficulty in PPH is maintaining blood flow to the lungs. Any event that significantly decreases venous return to the heart, such as hypotension, impairs the ability of the right ventricle to pump blood through the pulmonary vessels with their high, fixed vascular resistance. Because hypotension can occur quickly and is often unresponsive to medical therapy, it must be avoided at all costs (Blanchard & Shabetai, 2009).
Symptoms may be nonspecific, such as fatigue and shortness of breath. Dyspnea on exertion is the most common symptom (Cunningham et al., 2010).
PPH is diagnosed by electrocardiography. The diagnosis is confirmed by right-sided cardiac catheterization, which may be deferred during pregnancy (Cunningham et al., 2010). Mortality rates reported during pregnancy are as high as 50%, so pregnancy is not advised in women with this condition (Blanchard & Shabetai, 2009). The most dangerous times for women with this condition are the intrapartal and early postpartal periods because of increases in cardiac output and fluid shifts.
Medical management of pregnant women with PPH during pregnancy includes limiting activity and avoiding supine positioning. Diuretics, supplemental oxygen, and vasodilator medications will also be ordered. During labor and birth hypotension must be avoided by carefully establishing epidural analgesia and preventing blood loss (Cunningham et al., 2010).
Marfan Syndrome
Marfan syndrome is an autosomal dominant genetic disorder characterized by generalized weakness of the connective tissue, resulting in joint deformities, ocular lens dislocation, and weakness of the aortic wall and root. Associated cardiovascular changes include mitral valve prolapse, mitral regurgitation, aortic regurgitation, aortic root dilation, and possible dissection or rupture of the aortic root (Easterling & Stout, 2007). Excruciating chest pain is the most common symptom of aortic dissection. Aortic dissection most often occurs in the third trimester or postpartum. Preconception genetic counseling is recommended to make women aware of the risks of pregnancy with this condition. Because the condition is inherited, each child born to a woman with Marfan syndrome has a 50% chance of having the disorder (Martin & Foley, 2007). Baseline data should be gathered about the aortic root before pregnancy or at the first prenatal visit by noninvasive imaging with transesophageal echocardiography, computed tomography (CT), or magnetic resonance imaging (MRI).
Management during pregnancy includes restricted activity and use of beta-blockers; surgery may be indicated in some women. Vaginal birth is considered safe for women with aortic root diameters less than 4 cm. Some authorities, however, recommend that women with larger aortic root diameters give birth by elective cesarean because of concerns about increased pressure in the aorta during labor (Blanchard & Shabetai, 2009; Easterling & Stout, 2007).
Infective Endocarditis
Infective endocarditis is inflammation of the innermost lining—the endocardium—of the heart, caused by invasion of microorganisms. Children and adults who have had corrective surgery for congenital heart disease are at greatest risk for developing infective endocarditis. The disease may also be seen in women who use street drugs intravenously (Cunningham et al., 2010). Bacterial endocarditis, leading to incompetence of heart valves and thus congestive heart failure and cerebral emboli, can result in death. Treatment is with antibiotics. Prophylactic treatment with antibiotics is used only for women at highest risk for this condition.
Eisenmenger Syndrome
Eisenmenger syndrome is a right-to-left or bidirectional shunting that can occur either at the atrial or the ventricular level of the heart and is combined with elevated pulmonary vascular resistance (Blanchard & Shabetai, 2009). The syndrome is associated with high mortality (50% in mothers and 50% in fetuses). Because of the risk for poor pregnancy outcomes, pregnancy should be avoided by women with Eisenmenger syndrome (Blanchard & Shabetai).
In women who continue pregnancy despite the risks, physical activity is strictly limited. Hospitalization may be necessary to provide optimal care, which includes oxygen administration, rest, and fetal monitoring. During labor and birth, intrathecal or epidural morphine sulfate is recommended in order to maintain hemodynamic stability. Hypotension must be avoided at all costs because it results in more right-to-left shunting (Easterling & Stout, 2007). Pulse oximetry is a useful assessment tool to guide the treatment plan during labor and birth. Cesarean birth should be performed only for obstetric indications and avoided whenever possible (Easterling & Stout).
Peripartum Cardiomyopathy
Peripartum cardiomyopathy (PCM) is congestive heart failure with cardiomyopathy. The classic criteria for the diagnosis of PCM include development of congestive heart failure in the last month of pregnancy or within the first 5 postpartum months, absence of heart disease before the last month of pregnancy, and, most important, lack of another cause for heart failure. The cause of the disease is unknown. The incidence is 1 in 3000 to 4000 live births in the United States (Blanchard & Shabetai, 2009).
Associated risk factors for PCM include maternal age older than 35 years, multifetal gestation, preeclampsia, gestational hypertension, multiparity, African descent, and prolonged tocolytic therapy (Klein & Galan, 2004). Maternal mortality has been estimated in the range of 30% to 40% (Martin & Foley, 2007). Clinical findings are those of congestive heart failure (left ventricular failure). Clinical manifestations include dyspnea, fatigue, and edema, as well as radiologic findings of cardiomegaly.
Medical management of PCM includes a regimen used for congestive heart failure: diuretics, sodium and fluid restriction, afterload-reducing agents, and digoxin. Anticoagulation may be necessary if the cardiac chambers are significantly dilated and contract poorly because of the increased risk for clot formation. During labor epidural anesthesia is often used for pain control to decrease the cardiac workload and reduce tachycardia. Cesarean birth should be performed only for obstetric indications (Easterling & Stout, 2007).
In half of all women with PCM, left ventricular dysfunction resolves within 6 months. These women generally do well. If left ventricular dysfunction does not resolve within 6 months, however, approximately 85% of women with PCM will die in the next 4 to 5 years. Death is usually the result of progressive congestive heart failure, arrhythmia, or thromboembolism (Easterling & Stout, 2007). The recurrence rate for cardiomyopathy in a subsequent pregnancy is high—anywhere from 20% to 50%. The risk of recurrence is increased in women who did not have complete recovery of left ventricular function after the initial episode of PCM (Blanchard & Shabetai, 2009).
Valve Replacement
Pregnant women with mechanical or bioprosthetic heart valves require specialized care for this high risk situation. The primary medical management, anticoagulation, is both controversial and complicated. A high risk for thromboembolism exists because of the hypercoagulability of pregnancy. At the same time, the use of anticoagulants during pregnancy presents the possibility of maternal and fetal hemorrhage. Some oral anticoagulants pose a significant risk to the fetus for abnormalities and intracranial hemorrhage. Prosthetic heart valve thrombosis is a life-threatening emergency during pregnancy and requires clot removal surgery, which carries a high mortality rate (Tomlinson, 2006).
Women with bioprosthetic heart valves usually do not require anticoagulation during pregnancy. This type of valve is an ideal replacement for women of childbearing age. A disadvantage of this valve, however, is premature failure, which may occur within 10 to 15 years of placement. Premature valve failure may be exacerbated by pregnancy (Tomlinson, 2006).
The recommendations for pregnant women with mechanical prosthetic valves who need anticoagulation therapy include several different treatment regimens. Because the most effective and safest management has not been determined through controlled trials, the decision regarding choice of therapy should be made between the physician and the woman, who should be fully informed about the potential risks of the various options to her and her unborn child. One option is to use subcutaneous heparin for the first 12 weeks of gestation. Warfarin (Coumadin) then is used until week 35 of gestation, followed by a return to heparin (intravenous) until after the birth. If prothrombin time (PT) results are reported in international normalized ratio (INR) values, then the desired range is between 2 and 4.9 (Tomlinson, 2006). A second option is to use warfarin for the entire pregnancy up to 35 weeks of gestation followed by intravenous heparin until labor begins. Data are inconclusive regarding the use of low-molecular-weight heparin (Lovenox). Anticoagulation therapy should be discontinued during active labor and resumed in the postpartum period. Warfarin does not adversely affect breastfeeding.
Heart Transplantation
Increasing numbers of heart recipients are successfully completing pregnancies. It is recommended that pregnancy be avoided for at least 1 year after the transplant (Blanchard & Shabetai, 2009). Before conception the woman should be assessed for quality of ventricular function and potential rejection of the transplant. She also should be considered to be stabilized on her immunosuppressant regimen. Women who have no evidence of rejection and have normal cardiac function at the beginning of the pregnancy appear to do well during pregnancy, labor, and birth. Risks to the woman include hypertension, preeclampsia, preterm birth, and mild rejection episodes (Martin & Foley, 2007).
Care Management
The presence of cardiac disease is a significant influencing factor in the decision-making process for or against becoming pregnant. Couples planning a pregnancy must understand the risks involved in their situation. If the pregnancy is unplanned, the nurse should explore the couple’s desire to continue the pregnancy in light of the risks involved. Pregnancy termination is one option, depending on the severity of the cardiac defect. The family may need further information in order to make an informed decision regarding the future of the pregnancy.
The pregnant woman with a cardiac disorder is in a high risk situation. Her care will be provided by a multidisciplinary team, including a cardiologist, obstetrician, perinatologist, and registered nurse experienced in the care of women with high risk pregnancies. If she chooses to continue the pregnancy, the woman’s condition may be assessed as often as weekly (see the Nursing Process box: Cardiac Disease). For additional information on cardiac disease, visit the American Heart Association’s website at www.americanheart.org.
Antepartum
Therapy for the pregnant woman with heart disease is focused on minimizing stress on the heart, which is greatest between 28 and 32 weeks of gestation as the hemodynamic changes reach their maximum. Factors that increase the risk of cardiac decompensation are avoided. The workload of the cardiovascular system is reduced by appropriate treatment of any coexisting emotional stress, hypertension, anemia, hyperthyroidism, or obesity.
Signs and symptoms of cardiac decompensation are taught at the first prenatal visit and reviewed at each subsequent visit (see the Signs of Potential Complications box; see also the Nursing Process box: Cardiac Disease for other information to include in client teaching).
Infections are treated promptly because respiratory, urinary, or gastrointestinal (GI) tract infections can complicate the condition by accelerating the heart rate and by direct spread of organisms (e.g., streptococci) to the heart structure. The woman should notify her physician at the first sign of infection or exposure to an infection. Vaccination against influenza and pneumococci can be given.
Nutrition counseling is necessary, optimally with the woman’s family present. The pregnant woman needs a well-balanced diet with iron and folic acid supplementation, high protein
levels, and adequate calories to gain weight. Iron supplements tend to cause constipation so the woman should increase her intake of fluids and fiber. A stool softener may also be prescribed. It is important that the woman with a cardiac disorder avoid straining during defecation, thus causing the Valsalva maneuver (forced expiration against a closed airway, which when released, causes blood to rush to the heart and overload the cardiac system). A referral to a registered dietitian may be necessary for a nutritional plan of care.
Cardiac medications are prescribed as needed, with attention to fetal well-being. The hemodynamic changes that occur during pregnancy, such as increased plasma volume and increased renal clearance of drugs, can alter the amount of medication needed to establish and maintain a therapeutic drug level. Therefore, monitoring drug levels during pregnancy is crucial in order to maintain effective therapy for the woman while minimizing risk to the fetus. Table 30-1 lists information on medications that are often used to treat cardiac disorders during pregnancy.
TABLE 30-1
SELECTED DRUGS USED IN TREATMENT OF CARDIAC DISORDERS IN THE PREGNANT WOMAN
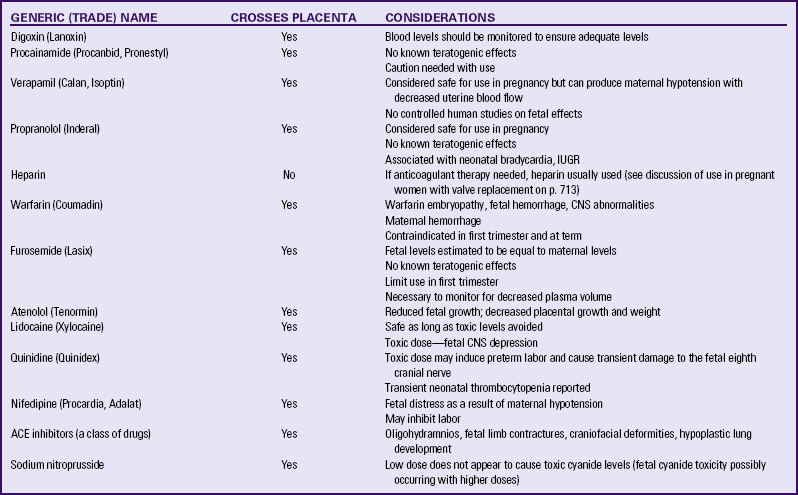
ACE, Angiotensin-converting enzyme; CNS, central nervous system; IUGR, intrauterine growth restriction.
Sources: Blanchard, D., & Shabetai, R. (2009). Cardiac diseases. In R. Creasy, R. Resnik, J. Iams, C. Lockwood, & T. Moore (Eds.), Maternal-fetal medicine: Principles and practice (6th ed.). Philadelphia: Saunders; Klein, L., & Galan, H. (2004). Cardiac disease in pregnancy. Obstetrics and Gynecology Clinics of North America, 31(2), 429-459.; Niebyl, J., & Simpson, J. (2007). Drugs and environmental agents in pregnancy and lactation: Embryology, teratology, epidemiology. In S. Gabbe, J. Niebyl, & J. Simpson (Eds.), Obstetrics: Normal and problem pregnancies (5th ed.). Philadelphia: Churchill Livingstone.
Anticoagulant therapy may be prescribed during pregnancy for several conditions, such as recurrent venous thrombosis, pulmonary embolus, rheumatic heart disease, prosthetic valves, or cyanotic congenital heart defects. If anticoagulant therapy is required during pregnancy a number of various regimens may be recommended. (See the section on valve disorders for more discussion of anticoagulant therapy.) The nurse should be aware of the goals of therapy and monitor the PT and INR accordingly. The woman may need to learn to self-administer injectable agents such as heparin or low-molecular-weight heparin. A woman taking warfarin (Coumadin) requires specific nutritional teaching to avoid foods high in vitamin K, such as raw, dark green leafy vegetables, which counteract the effects of warfarin. In addition, she will require a folic acid supplement.
Tests for fetal maturity and well-being and placental sufficiency may be necessary. Other therapy is directly related to the functional classification of heart disease. The nurse must reinforce the need for close medical supervision (see the Nursing Care Plan).
Heart Surgery During Pregnancy: Ideally surgery to correct a cardiac lesion should be performed prior to pregnancy. In some women, however, cardiac disease is diagnosed for the first time during pregnancy. The maternal mortality risk does not increase, but there is a fetal mortality risk of 10% to 15% if heart surgery is performed, especially if cardiopulmonary bypass is used. If possible, surgery should be postponed until the third trimester of pregnancy, when the risk to the fetus is considerably decreased (Blanchard & Shabetai, 2009).
The woman, the fetus, and uterine activity must be monitored carefully during surgery. Electrocardiographic monitoring and intraarterial and Swan-Ganz catheters are usually recommended for intraoperative and postoperative assessment. In some cases, transesophageal echocardiography may be required (Blanchard & Shabetai, 2009). Closed cardiac surgery, such as release of a stenotic mitral valve, can be accomplished with little risk to mother or fetus. Open heart surgery, however, requires extracorporeal circulation, and fetal bradycardia may occur as a result of low blood-flow rates. Periods of hypoxemia for the fetus can lead to various kinds of neurologic insults. Increase in flow rates on cardiopulmonary bypass as well as intravenous nitroprusside may correct fetal bradycardia. Preterm labor occurs more frequently in women having cardiac surgery (Blanchard & Shabetai).
Intrapartum
For all pregnant women, the intrapartum period is the one that evokes the most apprehension in clients and caregivers. The woman with impaired cardiac function has additional reasons to be anxious because labor and giving birth place an additional burden on her already compromised cardiovascular system.
Assessments include the routine assessments for all laboring women, as well as assessments for cardiac decompensation. In addition, arterial blood gases (ABGs) may be needed to assess for adequate oxygenation. A pulmonary artery catheter may be inserted to monitor hemodynamic status accurately during labor and birth (see Chapter 31). ECG monitoring and continuous monitoring of blood pressure and oxygen saturation (pulse oximetry) are usually instituted for the woman, and continuous fetal monitoring is used to monitor the fetus.
Nursing care during labor and birth focuses on the promotion of cardiac function. Minimize anxiety by maintaining a calm atmosphere in the labor and birth rooms. Provide anticipatory guidance by keeping the woman and her family informed of labor progress and events that will probably occur, as well as
answering any questions they have. Support the woman’s childbirth preparation method to the degree it is feasible for her cardiac condition. Nursing techniques that promote comfort, such as back massage, are also used.
Cardiac function is supported by keeping the woman’s head and shoulders elevated and body parts resting on pillows. The side-lying position usually facilitates positive hemodynamics during labor. Discomfort is relieved with medication and supportive care. Epidural regional analgesia provides better pain relief than narcotics and causes fewer alterations in hemodynamics (Easterling & Stout, 2007).
Beta-adrenergic agents such as terbutaline (Brethine) are associated with various side effects, including tachycardia, irregular pulse, myocardial ischemia, and pulmonary edema. Therefore, these medications should not be used in women with known or suspected heart disease (Gilbert, 2011; Iams & Romero, 2007; Iams, Romero, & Creasy, 2009). A synthetic oxytocin (Syntocinon) can be used to induce labor. This drug does not appear to cause significant coronary artery constriction in doses prescribed for labor induction or control of postpartum uterine atony. Cervical ripening agents containing prostaglandin are usually tolerated well, but should be used cautiously.
If no obstetric problems exist, vaginal birth is recommended and may be accomplished with the woman in the side-lying position to facilitate uterine perfusion. If the supine position is used, position a pad under one hip to displace the uterus laterally and minimize the danger of supine hypotension. Have the woman flex her knees and place her feet flat on the bed. To prevent compression of popliteal veins and an increase in blood volume in the chest and trunk as a result of the effects of gravity, do not use stirrups. Open-glottis pushing is recommended. The woman should avoid the Valsalva maneuver when pushing in the second stage of labor because it reduces diastolic ventricular filling and obstructs left ventricular outflow. Mask oxygen is important. Episiotomy and vacuum extraction or outlet forceps can be used to decrease the length of the second stage of labor and decrease the workload of the heart in second stage labor. Cesarean birth is not routinely recommended for women who have cardiovascular disease because of the risks of dramatic fluid shifts, sustained hemodynamic changes, and increased blood loss.
Penicillin prophylaxis may be ordered for nonallergic pregnant women with class II or higher cardiac disease to protect against bacterial endocarditis in labor and during the early puerperium (see Box 30-2). Oxytocin is usually given immediately after birth to prevent hemorrhage. Ergot products should not be used because they increase blood pressure. Fluid balance should be maintained and blood loss replaced. If tubal sterilization is desired, surgery is delayed at least several days to ensure homeostasis.
Postpartum
Monitoring for cardiac decompensation in the postpartum period is essential. The first 24 to 48 hours after birth are the most hemodynamically difficult for the woman. Hemorrhage or infection, or both, may worsen the cardiac condition. The woman with a cardiac disorder may continue to require a pulmonary artery catheter and ABG monitoring.
Care in the postpartum period is tailored to the woman’s functional capacity. Postpartum assessment of the woman with cardiac disease includes vital signs, oxygen saturation levels, lung and heart auscultation, presence and degree of edema, amount and character of bleeding, uterine tone and fundal height, urinary output, pain (especially chest pain), the activity-rest pattern, dietary intake, mother-infant interactions, and emotional state. The head of the bed is elevated, and the woman is encouraged to lie on her side. Bed rest may be ordered, with or without bathroom privileges. Progressive ambulation may be permitted as tolerated. The nurse may help the woman meet her grooming and hygiene needs and other activities. Bowel movements without stress or strain for the woman are promoted with stool softeners, diet, and fluids.
The woman may need a family member to help in the care of the infant. Breastfeeding is not contraindicated, but some women with heart disease (particularly those with life-threatening disease) may be unable to breastfeed. The woman who chooses to breastfeed will need the support of her family and the nursing staff to be successful. For example, she may need assistance in positioning herself and/or the infant for feeding. To further conserve the woman’s energy, the infant can be brought to the mother and taken from her after the feeding. Most medications used to manage cardiac disorders are compatible with breastfeeding. Thiazide diuretics, however, may suppress lactation (Blanchard & Shabetai, 2009). Because diuretics can cause neonatal diuresis that can lead to dehydration, lactating women must be monitored closely to determine if medication doses can be reduced and still be effective.
If the woman is unable to breastfeed and her energies do not allow her to bottle feed the infant, the baby can be kept at the bedside so she can look at and touch her baby to establish an emotional bond, with a low expenditure of energy. The infant should be held at the mother’s eye level and near her lips and brought to her fingers. At the same time, involving the mother passively in her infant’s care helps the mother feel vitally important—as she is—to the infant’s well-being (e.g., “You can offer something no one else can: you can provide your baby with your sounds, touch, and rhythms that are so comforting”). Perhaps the woman can be encouraged to make a tape recording of her talking, singing, or whispering, which can be played for the baby in the nursery to help the infant feel her presence and be in contact with her voice. This also enhances maternal-infant bonding.
Preparation for discharge is carefully planned with the woman and family. Provision of help for the woman in the home by relatives, friends, and others must be addressed. If necessary, the nurse refers the family to community resources (e.g., for assistance with household activities). Rest and sleep periods, activity, and diet must be planned. The couple may need information about reestablishing sexual relations and contraception or sterilization.
Women with congenital heart disease should be offered contraceptive counseling. In general, for women with congenital heart disease, the complications associated with pregnancy are usually greater than the risks associated with any form of contraception (Easterling & Stout, 2007). Women at particular risk for thromboembolism should avoid combined estrogen-progestin oral contraceptives, but progestin-only pills may be used. Parenteral progestins (e.g., Depo-Provera) are safe and effective for women with cardiac disease. An intrauterine device (IUD) may be used by some women with congenital heart lesions. Although a theoretical risk exists for developing endocarditis, the actual risk for women using an IUD is probably very minimal (Easterling & Stout).
Monitoring for cardiac decompensation continues through the first few weeks after birth because of hormonal shifts that affect hemodynamics. Maternal cardiac output is usually stabilized by 2 weeks postpartum (Easterling & Stout, 2007).
Men and women with congenital heart disease are at increased risk for having children who also have congenital heart disease. The risk for affected mothers is greater, approximately two to more than three times that of affected fathers. Children born with congenital heart disease to parents with congenital heart defects appear to inherit the risk for cardiac maldevelopment in general because they often do not have the same defect as the parent (Easterling & Stout, 2007). Therefore preconception counseling and genetic counseling before a subsequent pregnancy are essential.
Cardiopulmonary Resuscitation of the Pregnant Woman
Trauma, cardiac abnormalities, embolism, magnesium overdose, sepsis, intracranial hemorrhage, anesthetic complications, eclampsia, and uterine rupture are the most common causes of cardiac arrest in a pregnant woman (Martin & Foley, 2009). Special modifications are necessary when cardiopulmonary resuscitation (CPR) is performed during the second half of pregnancy. In nonpregnant women, chest compressions produce a cardiac output of only about 30% of normal. Cardiac output in pregnant women may be even less due to aortocaval compression caused by the gravid uterus. Therefore, uterine displacement during resuscitation efforts is critical (Cunningham et al., 2010). The uterus may be displaced laterally either manually or by placing a wedge, rolled blanket, or towel under one of the woman’s hips. If defibrillation is needed, the paddles must be placed one rib interspace higher than usual because the heart is displaced slightly by the enlarged uterus (see the Emergency box).
If CPR is not effective within 4 to 5 minutes, perimortem cesarean birth is often recommended if the fetus is viable and maternal cardiopulmonary arrest appears to be untreatable. According to one study, 98% of infants born within 5 minutes of maternal cardiac arrest were neurologically normal. The rate of intact neonatal survival decreases, however, as the time from maternal arrest to birth increases (Cunningham et al., 2010; Lu & Curet, 2007). Cesarean birth may also facilitate maternal resuscitative efforts. Therefore, the American College of Obstetricians and Gynecologists (ACOG) recommends that performing a cesarean birth be considered within 4 minutes of cardiac arrest in the third trimester of pregnancy (ACOG, 2009).
Complications may be associated with CPR on a pregnant woman. These complications may include laceration of the liver, rupture of the spleen or uterus, hemothorax, hemopericardium, or fracture of ribs or the sternum. Fetal complications, including cardiac arrhythmia or asystole related to maternal defibrillation and medications, and central nervous system (CNS) depression related to antiarrhythmic drugs and inadequate uteroplacental perfusion, with possible fetal hypoxemia and acidemia, also may occur.
If the resuscitation is successful, the woman must be carefully monitored afterward. She remains at increased risk for recurrent cardiac arrest and arrhythmias (e.g., ventricular tachycardia, supraventricular tachycardia, bradycardia). Therefore, her cardiovascular, pulmonary, and neurologic status should be assessed continuously. If the pregnancy remains intact, uterine activity and resting tone must be monitored. Fetal status and gestational age should also be determined and used in decision making regarding the continuation of the pregnancy or the timing and route of birth.
Another common reason for performing CPR on a pregnant woman is airway obstruction caused by choking. Clearing an airway obstruction is usually accomplished by performing abdominal thrusts (formerly known as the Heimlich maneuver). During the second and third trimesters of pregnancy, however, chest thrusts, rather than abdominal thrusts, should be used (see the Emergency box and Fig. 30-1).
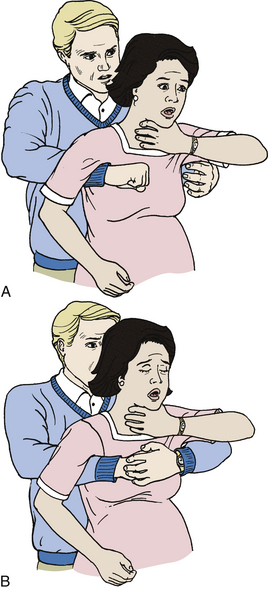
FIG. 30-1 Abdominal thrust maneuver (formerly known as the Heimlich maneuver). Clearing airway obstruction in woman in late stage of pregnancy (can also be used in markedly obese victim). A, Standing behind victim, place your arms under woman’s armpits and across chest. Place thumb side of your clenched fist against middle of sternum, and place other hand over fist. B, Perform backward chest thrusts until foreign body is expelled or woman becomes unconscious. If pregnant woman becomes unconscious because of foreign body airway obstruction, place her on her back and kneel close to her side. (Be sure uterus is displaced laterally by using, for example, a rolled blanket under her hip.) Open mouth with tongue-jaw lift, perform finger sweep, and attempt rescue breathing. If unable to ventilate, position hands as for chest compression. Deliver five chest thrusts firmly to remove obstruction. Repeat this sequence of abdominal thrust maneuver, finger sweep, and attempt to ventilate. Continue sequence until pregnant woman’s airway is clear of obstruction or help has arrived to relieve you. If the woman is unconscious, give chest compressions as for the woman without pulse American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Part 10.8: Cardiac arrest associated with pregnancy. Circulation, 112 (24 Suppl), IV-150-153.)
Other Medical Disorders in Pregnancy
Anemia is a common medical disorder of pregnancy, affecting from 20% to 60% of pregnant women (Kilpatrick, 2009). Anemia results in a reduction of the oxygen-carrying capacity of the blood. Because the oxygen-carrying capacity of the blood is decreased, the heart tries to compensate by increasing the cardiac output. This effort increases the workload of the heart and stresses ventricular function. Therefore, anemia that occurs with any other complication (e.g., preeclampsia) may result in congestive heart failure.
An indirect index of the oxygen-carrying capacity is the packed red blood cell (RBC) volume, or hematocrit level. The normal hematocrit range in nonpregnant women is 37% to 47%. However, normal values for pregnant women with adequate iron stores may be as low as 33%. According to the Centers for Disease Control and Prevention (CDC), anemia in pregnancy is defined as hemoglobin less than 11 g/dl in the first and third trimesters and less than 10.5 g/dl in the second trimester (Kilpatrick, 2009). A hemoglobin level less than 6 to 8 mg/dl is considered severe anemia (Blackburn, 2007).
When a woman has anemia during pregnancy, the loss of blood at birth, even if minimal, is not well tolerated. She is at an increased risk for requiring blood transfusions. Women with anemia have a higher incidence of puerperal complications, such as infection, than pregnant women with normal hematologic values.
Care of the anemic pregnant woman requires that the health care provider distinguish between the normal physiologic anemia of pregnancy and disease states. The majority of cases of anemia in pregnancy are caused by iron deficiency. The other types include a considerable variety of acquired and hereditary anemias, such as folic acid deficiency, sickle cell anemia, and thalassemia.
Iron Deficiency Anemia
Iron deficiency anemia is the most common anemia of pregnancy. It is diagnosed by checking the woman’s serum ferritin level in addition to her hemoglobin and hematocrit levels. The serum ferritin level reflects iron reserves. A serum ferritin value less than 12 mcg/dl in the presence of a low hemoglobin value indicates iron deficiency anemia. An association appears to exist between maternal iron deficiency anemia, especially severe anemia, and preterm birth and low-birth-weight infants, although whether these poor pregnancy outcomes are caused by iron deficiency anemia is uncertain (Samuels, 2007). Usually even the fetus of an anemic woman will receive adequate iron stores from the mother, at the cost of further depleting the mother’s iron level (Blackburn, 2007).
Generally iron deficiency anemia is preventable or easily treated with iron supplements. Because of the increased amounts of iron needed for fetal development and maternal stores, pregnant women are often encouraged to take prophylactic iron supplementation (Blackburn, 2007; Gilbert, 2011). Most women with iron deficiency anemia can absorb as much iron as they need by taking one 325-mg tablet of ferrous sulfate twice each day (Samuels, 2007). An important aspect to teach the pregnant woman is the significance of the iron therapy. Some pregnant women cannot tolerate the prescribed oral iron because of nausea and vomiting associated with the pregnancy and as a side effect of iron therapy. In such cases the woman may be given parenteral iron therapy by intramuscular or intravascular injection. Women who are severely anemic may require blood transfusions (Samuels).
Teach the importance of iron supplements for preventing or treating iron deficiency anemia (see the Teaching for Self-Management box: Iron Supplementation in Chapter 14, p. 325). In addition, teach dietary ways to decrease the GI side effects of iron therapy.
Folate Deficiency Anemia
Folate is a water-soluble vitamin found naturally in dark green leafy vegetables, citrus fruits, eggs, legumes, and whole grains. Even in well-nourished women, folate deficiency is common. Poor diet, cooking with large volumes of water, and increased alcohol use may contribute to folate deficiency. During pregnancy the need for folate increases, both because of fetal demands and because folate is less well absorbed from the GI tract during gestation. Folic acid is the form of the vitamin used in vitamin supplements. The recommended daily intake of folic acid for pregnant women is 600 mcg. Both prescription and nonprescription prenatal vitamins contain more than this amount of folic acid and should be sufficient to prevent and treat folate deficiency. Women at particular risk for folate deficiency include those who have significant hemoglobinopathies, take anticonvulsant medication, or are pregnant with a multifetal gestation. These women will require larger than usual doses of folic acid (Samuels, 2007).
Folate deficiency is the most common cause of megaloblastic anemia during pregnancy, but a vitamin B12 deficiency must also be considered. Megaloblastic anemia rarely occurs before the third trimester of pregnancy (Kilpatrick, 2009; Samuels, 2007). Women with megaloblastic anemia caused by folic acid deficiency have the usual presenting symptoms and signs of anemia: pallor, fatigue, and lethargy, as well as glossitis and skin roughness, which are associated specifically with megaloblastic anemia (Kilpatrick). Folate deficiency usually improves rapidly with folic acid therapy. It rarely occurs in the fetus and is not a significant cause of perinatal morbidity. Iron deficiency often occurs along with folate deficiency (Samuels).
Sickle Cell Hemoglobinopathy
Sickle cell hemoglobinopathy is a disease caused by the presence of abnormal hemoglobin in the blood. Sickle cell trait (SA hemoglobin pattern) is sickling of the RBCs but with a normal RBC life span. Most people with sickle cell trait are asymptomatic. Approximately 1 in 12 African-American adults in the United States have sickle cell trait (Samuels, 2007). Women with sickle cell trait require genetic counseling and partner testing to determine their risk of producing children with sickle cell trait or disease.
Women with sickle cell trait usually do well in pregnancy. However, they are at increased risk for preeclampsia, intrauterine fetal death, preterm birth and low-birth-weight infants, and postpartum endometritis. They are also at increased risk for urinary tract infections (UTIs) and may be deficient in iron (Kilpatrick, 2009; Samuels, 2007).
Sickle cell anemia (sickle cell disease) is a recessive, hereditary, familial hemolytic anemia that affects persons of African or Mediterranean ancestry. These individuals usually have abnormal hemoglobin types (SS or SC). The average life span of RBCs in a person with sickle cell anemia is only 5 to 10 days, in comparison to the 120-day life span of a normal RBC. Sickle cell anemia occurs in 1 in 708 African-Americans in the United States (Samuels, 2007). Persons with sickle cell anemia have recurrent attacks (crises) of fever and pain, most often in the abdomen, joints, or extremities, although virtually all organ systems can be affected. These attacks are attributed to vascular occlusion when RBCs assume a characteristic sickled shape. Crises are usually triggered by dehydration, hypoxia, or acidosis (Samuels).
Women with sickle cell anemia require genetic counseling before pregnancy. All children born to a woman with sickle cell anemia will be affected in some way by the disease. The woman’s partner must be tested to determine the couple’s risk of producing children with sickle cell disease rather than sickle cell trait. Women with sickle cell anemia are at risk for poor pregnancy outcomes, including miscarriage, IUGR, and stillbirth. Although maternal mortality is rare, maternal morbidity is significant and includes an increased risk for preeclampsia and infection, particularly in the urinary tract and in the lungs. The frequency of painful crises also appears to be increased during pregnancy (Samuels, 2007).
The woman will be monitored carefully during pregnancy for the development of urinary tract infection or preeclampsia. In addition, she will have serial ultrasound examinations to monitor fetal growth and will likely have antepartum fetal testing performed regularly during the third trimester. Infections are treated aggressively with antibiotics. If crises occur they are managed with analgesia, oxygen, and hydration. Some authorities recommend prophylactic transfusions as a way to improve oxygen-carrying capacity and suppress the synthesis of sickle hemoglobin. Others, however, believe that prophylactic transfusions do not improve fetal or neonatal outcome (Samuels, 2007).
If no complications occur, pregnancy can continue until term. Intrapartum, women with sickle cell disease should be encouraged to labor in a side-lying position. They may require supplemental oxygen. Adequate hydration should be
maintained while preventing fluid overload. Conduction anesthesia (e.g., epidural or combined spinal epidural anesthesia) is recommended because it provides excellent pain relief. Vaginal birth is preferred. Cesarean birth should be performed only for obstetric indications (Samuels, 2007).
Thalassemia
Thalassemia is a relatively common anemia in which an insufficient amount of hemoglobin is produced to fill the RBCs. Thalassemia is a hereditary disorder that involves the abnormal synthesis of the alpha or beta chains of hemoglobin. Beta thalassemia is the more common variety in the United States and usually occurs in persons of Mediterranean, North African, Middle Eastern, and Asian descent (Kilpatrick, 2009).
Beta thalassemia minor is the heterozygous form of this disorder. Persons with heterozygous beta thalassemia are carriers of the disorder and are usually asymptomatic (Samuels, 2007). They can expect to have a normal life span despite a moderately reduced hemoglobin level. Pregnancy will not worsen beta thalassemia minor. Neither does the disorder adversely affect pregnancy. Women with beta thalassemia minor do not require antepartum fetal testing (Samuels). Iron therapy should only be prescribed for women who are iron deficient, although folic acid supplementation is recommended for all women with beta thalassemia minor.
The homozygous form of beta thalassemia is known as thalassemia major, or Cooley anemia. Persons with this form of the disease usually have hepatosplenomegaly and bone deformities caused by massive marrow tissue expansion. These individuals usually die of infection or cardiovascular complications fairly early in life. If women live to reach childbearing age, infertility is common. If women with this disorder do become pregnant, they usually experience severe anemia and congestive heart failure, although successful full-term pregnancies have been reported. Women with beta thalassemia major are managed much like those with sickle cell anemia during pregnancy (Samuels, 2007).
Pulmonary Disorders
As pregnancy advances and the uterus presses on the thoracic cavity, any pregnant woman may have increased respiratory difficulty. This difficulty will be compounded by pulmonary disease. A pulmonary disorder in pregnancy requires assessment, planning, and interventions specific to the disease process, in addition to routine peripartum care.
Asthma
Asthma is a chronic inflammatory disorder involving the tracheobronchial airways, with increased airway responsiveness to a variety of stimuli. It is characterized by periods of exacerbations and remissions. Exacerbations are usually triggered by stimuli such as allergens, upper respiratory infection, medications (i.e., aspirin, beta-blockers), environmental pollutants, occupational exposures, exercise, cold air, or emotional stress (Powrie, 2006). In many cases the actual cause may be unknown, although a family history of allergy is common in people with asthma. In response to stimuli, there is widespread but reversible narrowing of the hyperreactive airways, making it difficult to breathe. The clinical manifestations are expiratory wheezing, productive cough, thick sputum, dyspnea, or any combination.
From 4% to 8% of pregnant women have asthma (Whitty & Dombroski, 2009), making it one of the most common preexisting conditions of pregnancy. The effect of pregnancy on asthma is unpredictable. The severity of the disease is unchanged in one third, improved in one third, and worsened in one third of pregnant women. If asthma worsens, the more severe symptoms usually occur between 17 and 24 weeks of gestation (Gilbert, 2011). Asthma appears to be associated with uteroplacental insufficiency, IUGR, and preterm birth (Gilbert; Whitty & Dombrowski).
The ultimate goal of asthma therapy in pregnancy is maintaining adequate oxygenation of the fetus by preventing hypoxic episodes in the mother. Achieving this goal requires monitoring lung function objectively (e.g., peak expiratory flow rate and forced expiratory volume in 1 second), avoiding or controlling asthma triggers (e.g., dust mites, animal dander, pollen, wood smoke), educating clients about the importance of controlling asthma during pregnancy, and drug therapy. Current drug therapy for asthma emphasizes treatment of airway inflammation to decrease airway hyperresponsiveness and prevent asthma symptoms. Decreasing airway inflammation with inhaled corticosteroids is the preferred treatment for managing persistent asthma during pregnancy (Whitty & Dombrowski, 2009) (see the Nursing Process box: Asthma).
Although asthma exacerbations during labor are very rare, medications for asthma are continued during labor and the postpartum period. Pulse oximetry should be instituted during labor. Epidurals are recommended for pain relief. Morphine and meperidine are histamine-releasing narcotics and should be avoided. Fentanyl may be used as an alternative for pain relief because it is less likely to cause histamine release (Powrie, 2006). Table 30-2 lists information on medications used in women with asthma during the intrapartum and postpartum periods.
TABLE 30-2
MEDICATIONS USED IN PREGNANCY IN WOMEN WITH ASTHMA
| STAGE/CONDITION OF PREGNANCY | PREFERRED MEDICATION | MEDICATION(S) TO AVOID (RATIONALE) |
| Labor | Continue asthma medications | |
| Induction | Prostaglandin E1 (Misoprostol [Cytotec])and E2 (Dinoprostone [Cervidil; Prepidil] may be used for cervical ripening) | 15-methyl prostaglandin F2α (Prostin/15m; Carboprost; Hemabate) (may cause bronchoconstriction or bronchospasm) |
| Oxytocin (Pitocin) | ||
| Pain relief | Fentanyl (Sublimaze) | Morphine and meperidine (Demerol) (release histamine) |
| Epidural anesthesia | ||
| Preterm labor | Magnesium sulfate | Beta-agonist (e.g., terbutaline [Brethine]) if woman is already taking one for her asthma (may cause respiratory distress) |
| Indomethacin (Indocin) may cause bronchospasm | ||
| NSAIDs (may exacerbate asthma) | ||
| Postpartum hemorrhage | Oxytocin | Methylergonovine (Methergine) and 15-methyl prostaglandin F2α Carboprost; Hemabate) (may worsen asthma) |
NSAIDs, Nonsteroidal antiinflammatory drugs.
Source: Whitty, J., & Dombrowski, M. (2009). Respiratory diseases in pregnancy. In R. Creasy, R. Resnik, J. Iams, C. Lockwood, & T. Moore (Eds.), Maternal-fetal medicine: Principles and practice (6th ed.). Philadelphia: Saunders.
During the postpartum period, women who have asthma are at increased risk for hemorrhage. If excessive bleeding occurs, oxytocin is the recommended drug (see Table 30-2). Asthma medications are usually safe for administration during the postpartum period and lactation. The woman usually returns to her prepregnancy asthma status within 3 months after giving birth.
Cystic Fibrosis
Cystic fibrosis is a common autosomal recessive genetic disorder in which the exocrine glands produce excessive viscous secretions, which causes problems with both respiratory and digestive functions. Most persons with cystic fibrosis have chronic obstructive pulmonary disease, pancreatic exocrine insufficiency, and elevated sweat electrolytes. Morbidity and mortality are usually caused by progressive chronic bronchial pulmonary disease (Whitty & Dombrowski, 2009).
Because the gene for cystic fibrosis was identified in 1989, data can be collected for the purposes of genetic counseling for couples regarding carrier status. In the United States, approximately 4% of the Caucasian population are carriers of the cystic fibrosis gene. Cystic fibrosis occurs in 1 in 3200 live Caucasian births (Whitty & Dombrowski, 2009). Persons with cystic fibrosis now live longer than they did in the past because
of earlier diagnosis of the disease and advances in antibiotic therapy and nutritional support. Men tend to live a little longer (median age of survival is 29.6 years) as compared with women, whose median age of survival is 27.3 years. Although most men with cystic fibrosis are infertile, women with the disease are often fertile and thus able to become pregnant (Whitty & Dombrowski, 2007).
Preconception counseling is essential for women with cystic fibrosis. Women should be advised of the risks of pregnancy, depending on their status. If possible, a woman should
lose or gain weight to be at 90% of her ideal body weight before conception (Cunningham et al., 2010; Whitty & Dombrowski, 2009).
Pulmonary function studies are the best predictor of both pregnancy and long term maternal outcome. Women with good nutrition, mild obstructive lung disease, and minimal lung impairment generally tolerate pregnancy well (Cunningham et al., 2010; Whitty & Dombrowski, 2009).
In women with severe disease, pregnancy is often complicated by chronic hypoxia and frequent pulmonary infections. Women with cystic fibrosis show a decrease in their residual volume during pregnancy, as do normal pregnant women, and are unable to maintain vital capacity. Presumably the pulmonary vasculature cannot accommodate the increased cardiac output of pregnancy. The result is decreased oxygen supply to the myocardium, decreased cardiac output, and increased hypoxemia. A pregnant woman with less than 50% of expected vital capacity usually has a difficult pregnancy. Increased maternal and perinatal mortality is related to severe pulmonary infection. There is an increased incidence of preterm birth, IUGR, and uteroplacental insufficiency (Cunningham et al., 2010; Whitty & Dombrowski, 2009).
In addition to respiratory problems, women with cystic fibrosis may also develop gestational diabetes and liver disease. Pancreatic insufficiency may put the woman at risk for malnutrition because she cannot meet the increased nutritional requirements of pregnancy. Fat-soluble vitamins may not be absorbed as well, resulting in deficiency in those nutrients. A weight gain of 11 to 12 kg is recommended during pregnancy. Women who are unable to achieve the recommended weight gain through oral supplements may require nasogastric tube feedings at night. If malnutrition is severe, parenteral hyperalimentation may be necessary (Whitty & Dombrowski, 2009).
Throughout pregnancy, frequent monitoring of the woman’s weight, blood glucose, hemoglobin, total protein, serum albumin, PT, and fat-soluble vitamins A and E is suggested. Her pancreatic enzyme prescription may need to be adjusted. Baseline pulmonary function tests should be completed before pregnancy ideally and repeated as necessary during pregnancy. Inhaled recombinant human deoxyribonuclease I may be given to improve lung function by decreasing sputum viscosity. Inhaled 7% saline is also beneficial in this regard (Cunningham et al., 2010). Early detection and treatment of infection are critical. Management of infection includes intravenous, inhaled, or oral antibiotics along with chest physiotherapy and bronchial drainage (Cunningham et al.; Whitty and Dombrowski, 2009).
Fetal assessment is essential, given that the fetus is at risk for uteroplacental insufficiency, which can result in IUGR. Maternal nutritional status and weight gain during pregnancy significantly affect fetal growth. Fundal height should be measured routinely and ultrasound examinations performed to evaluate fetal growth and amniotic fluid volume. Fetal movement counts are often recommended, starting at 28 weeks of gestation. Nonstress tests should be initiated at 32 weeks of gestation or sooner if there is evidence of fetal compromise (see Chapter 26) (Whitty & Dombrowski, 2009).
During labor, monitoring for fluid and electrolyte balance is required. Increased cardiac output could lead to cardiopulmonary failure in the woman with pulmonary hypertension or cor pulmonale. The amount of sodium lost through sweat can be significant, and hypovolemia can occur. Conversely, if any degree of cor pulmonale is present, fluid overload is a concern. Oxygen is given by nonrebreather face mask during labor, and monitoring by pulse oximetry is recommended. Diuretics may be prescribed for fluid overload. Epidural or local analgesia is the preferred analgesic for birth, with vaginal birth recommended. Cesarean birth should be reserved for obstetric indications.
Breastfeeding appears to be safe as long as the sodium content of the milk is not abnormal (Lawrence & Lawrence, 2005). Pumping and discarding the milk are done until the sodium content has been determined. Milk samples should be tested periodically for sodium, chloride, and total fat, and the infant’s growth pattern should be monitored.
Acute Respiratory Distress Syndrome
Acute respiratory distress syndrome (ARDS), or shock lung, occurs when the lungs are unable to maintain levels of oxygen and carbon dioxide within normal limits. Severe hypoxemia, in spite of high levels of inspired oxygen, is accompanied by an increase in pulmonary capillary permeability, a decrease in lung volume, and shunting of blood.
ARDS is not specific to pregnancy; it also can result from trauma, pneumonia, sepsis, aspiration of gastric contents, fat emboli, acute pancreatitis, and drug overdose. When ARDS is associated with pregnancy, the precipitating factors can also be amniotic fluid embolism, air embolism, tocolytic therapy, asthma, thromboembolism, disseminated intravascular coagulopathy, pyelonephritis, preeclampsia, eclampsia, severe hemorrhage, blood transfusion reactions, or peripartum cardiomyopathy (Curran, 2006). An initial intervention is to find and correct the underlying cause, if possible. To provide the best fetal environment, early intubation and mechanical ventilation are recommended. With severe lung injury, positive end-expiratory pressure (PEEP) may be necessary. Sedatives may be prescribed for intubation and ventilation. The administration of vasoactive agents, inotropic agents, and corticosteroids may be necessary. Maintaining fluid balance is a challenge and a key component of management. For the woman who is hypovolemic, administration of blood may help increase cardiac output. For the woman who is hypervolemic, diuretics may be necessary to maintain adequate cardiac output. Whether birth of the fetus improves maternal oxygenation remains controversial (Cunningham et al., 2010).
The postpartum incidence of ARDS is affected not by the method of birth but by the amount of trauma occurring during pregnancy and birth. ARDS can also occur after miscarriage or therapeutic abortion.
Laboratory results are important in identifying the origin of acute pulmonary problems. Chest radiographs can indicate the presence of infiltrates in the lungs, and ABGs identify the status of acid-base balance. The priority assessments are vital signs, oxygen saturation levels, and signs and symptoms of thrombophlebitis and hemorrhage. During the postpartum period, apprehension, distended neck veins, cyanosis, diaphoresis, or pallor may indicate hypoxemia. Mental confusion or disorientation also may be noted.
The pulse rate increases to compensate for respiratory insufficiency of any origin. The severity of the pulmonary problem increases as the pulse rate increases. An initial increase in blood pressure occurs as cardiac output increases in an attempt to supply the tissue with oxygen. When lung damage is severe, blood pressure decreases.
Respiratory changes are the most important indicators of ARDS. The rate and depth of respirations, respiratory pattern, symmetry of chest movement, and use of accessory muscles should be noted; therefore, observation of respiratory characteristics after activity is important.
On auscultation, crackles, rhonchi, wheezes, or a pleural friction rub should be reported, especially when they are present after an earlier assessment with normal findings. The pregnant woman should be positioned for breathing comfort. Oxygen and emergency equipment should be available. The woman should be reassured and coached in relaxation techniques to lessen her anxiety.
Although they are usually younger and healthier than most adults who develop ARDS, pregnant women with this condition still experience mortality rates of 25% to 40%. With pulmonary injury, the clinical condition is determined by the degree of damage, the ability to compensate for it, and the stage of the disease. Ideally, lung injury will be detected at an early stage and the underlying disease process promptly identified and treated. The long-term prognosis for pulmonary function in survivors is surprisingly good, even for women who experienced severe lung damage (Cunningham et al., 2010).
Integumentary Disorders
Dermatologic disorders induced by pregnancy include melasma (chloasma), vascular “spiders,” palmar erythema, and striae gravidarum. A number of chronic skin disorders may complicate pregnancy. These disorders may be present prior to pregnancy or appear for the first time during pregnancy. The course of these disorders varies during pregnancy. Acne, for example, may improve. Psoriasis improves in 40% of women, remains unchanged in 40% of women, and worsens in 20% of women during pregnancy. Lesions from neurofibromatosis may increase in size and number during pregnancy (Cunningham et al., 2010). Explanation, reassurance, and commonsense measures should suffice for normal skin changes. In contrast, disease processes during and soon after pregnancy may be extremely difficult to diagnose and treat.
Pruritus is a major symptom in several pregnancy-related skin diseases. Pruritus gravidarum, generalized itching without the presence of a rash, develops in up to 14% of pregnant women. It is often limited to the abdomen and is usually caused by skin distention and development of striae. Pruritus gravidarum is not associated with poor perinatal outcomes. It is treated symptomatically with skin lubrication, topical antipruritics, and oral antihistamines. Ultraviolet light and careful exposure to sunlight decrease itching. Pruritus gravidarum usually disappears shortly after birth but can recur in approximately half of all subsequent pregnancies (Rapini, 2009).
Another common pregnancy-specific cause of pruritus is pruritic urticarial papules and plaques of pregnancy (PUPPP) (Fig. 30-2), also known as polymorphic eruption of pregnancy. PUPPP classically appears in primigravidas during the third trimester. The abdomen is usually affected, but lesions can spread to the arms, the thighs, the back, and the buttocks. PUPPP almost always causes pruritus, and the itching is severe in 80% of cases. It is not, however, associated with poor maternal or fetal outcomes. Therefore, the goal of therapy is simply to relieve maternal discomfort. Antipruritic topical medications, topical steroids, and oral antihistamines usually provide relief. Women with severe symptoms may require oral prednisone. PUPPP usually resolves before birth or within several weeks after birth. Rarely, however, it may persist or even begin after birth. PUPPP does not usually recur in subsequent pregnancies (Papoutsis & Kroumpouzos, 2007; Rapini, 2009).

FIG. 30-2 Woman with pruritic urticarial papules and plaques of pregnancy. Lesions also are present on her arms, back, abdomen, and buttocks. (Courtesy Shannon Perry, Phoenix, AZ.)
Intrahepatic cholestasis of pregnancy (ICP) is a liver disorder unique to pregnancy that is characterized by generalized pruritus. The itching commonly affects the palms and soles but can occur on any part of the body. No skin lesions are present. Women with ICP have elevated serum bile acids and elevated liver function tests. Jaundice may or may not be present. Up to one half of women with ICP develop dark urine and light-colored stools. The cause of ICP is unknown, but approximately half of women have a family history of the disorder. ICP occurs more frequently during the winter months. A geographic variance in the prevalence of the disease also occurs. ICP occurs most often in Southeast Asia, Chile, Bolivia, and Scandinavia, although it is seen less frequently now in Chile and in Scandinavia than in the past (Cappell, 2007; Williamson & Mackillop, 2009).
The major risks associated with ICP are meconium staining, stillbirth, and preterm birth. The cause of these complications is likely related to increased levels of fetal serum bile levels. Treatment consists of giving ursodeoxycholic acid, which effectively controls the pruritus and laboratory abnormalities associated with ICP, and continued monitoring of liver function tests and bile acids (Cappell, 2007; Williamson & Mackillop, 2009). Antepartum fetal testing is essential. If liver function tests do not improve, induction of labor is considered at 36 to 37 weeks of gestation if the fetal lungs are mature. Symptoms usually disappear and laboratory abnormalities resolve within 2 to 4 weeks postpartum. ICP can recur in subsequent pregnancies, however, or with oral contraceptive use (Cappell).
Neurologic Disorders
The pregnant woman with a neurologic disorder must deal with potential teratogenic effects of prescribed medications, changes of mobility during pregnancy, and impaired ability to care for the baby. The nurse should be aware of all drugs the woman is taking and the associated potential for producing congenital anomalies. As the pregnancy progresses, the woman’s center of gravity shifts and causes balance and gait changes. The nurse should advise the woman of these expected changes and suggest safety measures as appropriate. Family and community resources may be needed to assist in providing infant care for the neurologically impaired woman.
Epilepsy
Epilepsy (often called seizure disorder) is a disorder of the brain that causes recurrent seizures and is the most common major neurologic disorder accompanying pregnancy. Less than 1% of all pregnant women have a seizure disorder (Aminoff, 2009). Seizure disorders are either acquired (less than 15% of all cases) or idiopathic (more than 85% of all cases), which means that a specific cause for the seizures cannot be identified. The majority of women with a seizure disorder who become pregnant have an uneventful pregnancy with an excellent outcome (Samuels & Niebyl, 2007).
Women with epilepsy should receive preconception counseling if at all possible. A detailed history of medication use and seizure frequency should be obtained. If the woman has frequent seizures before conception, she is likely to continue this pattern during pregnancy; therefore, achieving effective seizure control is extremely important before conception, even if changing medications is required. Many studies have reported an increased incidence of congenital anomalies, including cleft lip and palate, congenital heart disease, and neural tube defects (NTDs), in infants born to women taking anticonvulsant medications.
Several new anticonvulsant medications have been developed for use within the last decade. More information is needed regarding the fetal effects of these medications. Any anticonvulsant medication required to achieve good seizure control in a woman with epilepsy should be used, however, regardless of the increased risk of fetal anomalies because the most important goal during pregnancy is the prevention of seizures (Samuels & Niebyl, 2007).
Pregnant women with epilepsy are advised to take a folic acid supplement of 4 mg daily, which may decrease the incidence of NTDs. They are also encouraged to take a prenatal vitamin containing vitamin D daily because anticonvulsant medications can interfere with production of the active form of this vitamin (Cunningham et al., 2010; Samuels & Niebyl, 2007).
During pregnancy, only one anticonvulsant medication—at the lowest dose level that is effective at keeping the woman seizure free—should be prescribed. The increase in plasma volume that is a normal pregnancy change can affect drug metabolism and distribution. Therefore, blood levels of anticonvulsant medications should be checked and drug dosages adjusted as necessary. With client cooperation and close monitoring, most women with epilepsy should experience no change or even have fewer seizures during pregnancy. An increase in seizure frequency is usually related either to noncompliance with taking prescribed anticonvulsant medications or with sleep deprivation (Samuels & Niebyl, 2007). If an increase in seizure activity does occur during pregnancy, it is usually in women who had frequent seizures (more than one per month) before pregnancy (Aminoff, 2009).
In addition to congenital anomalies, the fetus of a woman with epilepsy is also at risk for IUGR. Determining an accurate gestational age as early as possible is important. This information will decrease any confusion later in pregnancy in regard to fetal growth issues. Maternal serum screening around 16 weeks of gestation and ultrasound examination at 18 to 22 weeks of gestation should be performed to assess for the presence of an NTD or other fetal anomalies. Nonstress testing later in pregnancy is not necessary, unless the woman has other medical or obstetric factors that increase the risk for stillbirth (Samuels & Niebyl, 2007).
Management of anticonvulsant therapy during prolonged labor is challenging. During labor, absorption of medications given orally is unpredictable, especially if vomiting occurs. Women who are maintained on phenytoin (Dilantin) or phenobarbital may be given these medications parenterally during labor. No parenteral form of carbamazepine has been developed; therefore, women maintained on this medication may be given phenytoin intravenously instead to carry them through labor. Vaginal birth is preferred (Samuels & Niebyl, 2007).
After birth the levels of anticonvulsant medications must be monitored frequently for the first few weeks because they can rise rapidly. If medication dose levels were increased during pregnancy, they will need to be decreased quickly to prepregnancy levels. All of the major anticonvulsant medications are found in breast milk, but the use of these medications is not a contraindication to breastfeeding. Neonatal sedation may be a side effect of carbamazepine, primidone (Mysoline), and phenobarbital (Samuels & Niebyl, 2007).
During the neonatal period infants can have a hemorrhagic disorder associated with exposure to anticonvulsant medications in utero, which causes vitamin K deficiency. Some authorities recommend giving vitamin K daily during the last few weeks of pregnancy to women taking anticonvulsant medications, but this practice is not considered the standard of care (Samuels & Niebyl, 2007).
All methods of contraception can be used by women with an idiopathic seizure disorder. Commonly prescribed anticonvulsant medications such as carbamazepine, primidone, phenobarbital, and phenytoin, however, reduce the effectiveness of oral contraceptives. Women taking low-dose oral contraceptives especially may have more breakthrough bleeding and be at risk for an unplanned pregnancy (Cunningham et al., 2010; Samuels & Niebyl, 2007). Valproic acid and the newer anticonvulsant medications have not been reported to cause oral contraceptive failure (Aminoff, 2009). In terms of planning for future childbearing, couples should be informed that children born to women with a seizure disorder of unknown cause have a four times greater chance of developing an idiopathic seizure disorder compared with the general population. Epilepsy in the father does not appear to increase a child’s risk for developing a seizure disorder (Samuels & Niebyl).
Multiple Sclerosis
Multiple sclerosis (MS), a patchy demyelinization of the spinal cord and CNS, may be a viral disorder. MS occurs equally in men and women. Onset of symptoms, which include weakness of one or both lower extremities, visual complaints, and loss of coordination, is subtle and usually occurs between the ages of 20 and 40 years. The disease is characterized by exacerbations and remissions. Pregnancy does not seem to worsen the disease (Samuels & Niebyl, 2007).
Remissions during pregnancy are common. If an exacerbation occurs, it is more likely to do so during the third trimester of pregnancy or postpartum. Treatment may include corticosteroids and immunosuppressive agents. Several new drugs and biopharmaceuticals are available for treating MS. These agents should be used during pregnancy only if the benefits clearly appear to outweigh the potential risks, as their effects on pregnancy and the fetus are unknown (Samuels & Niebyl, 2007).
Women who have become paraplegic or have lumbosacral lesions as a result of MS may have little pain during labor. Determining when labor begins may be difficult for them. Uterine contractions occur normally, but these women may have difficulty pushing effectively during the second stage of labor. Therefore, vacuum- or forceps-assisted birth may be necessary (Samuels & Niebyl, 2007). Breastfeeding is encouraged.
Bell Palsy
Bell palsy is an acute idiopathic facial paralysis. The cause is unknown, but it may be related to the reactivation of herpesvirus infection or acute human immunodeficiency virus type 1 (HIV-1) retroviral infections. Bell palsy occurs fairly often, especially in women of reproductive age. Women are affected two to four times more often than men (Cunningham et al., 2010). An association between Bell palsy and pregnancy was first cited by Bell in 1830. Pregnant women are affected three to four times more often than nonpregnant women. The incidence usually peaks during the third trimester and the puerperium. Women who develop Bell palsy during pregnancy have an increased risk for gestational hypertension as well (Cunningham et al.).
The clinical manifestations of Bell palsy include the sudden development of a unilateral facial weakness, with maximal weakness within 48 hours after onset, pain surrounding the ear, difficulty closing the eye on the affected side, hyperacusis (abnormal acuteness of the sense of hearing), and occasionally a loss of taste (Aminoff, 2009; Cunningham et al., 2010).
No effects of maternal Bell palsy have been observed in infants. Maternal outcome is generally good unless a complete block in nerve conduction occurs. Steroid therapy may improve outcome, although its benefits have not always been proven in past research studies. To be effective, steroids should be administered within the first 5 to 6 days after the paralysis develops (Aminoff, 2009). Supportive care includes prevention of injury to the constantly exposed cornea, facial muscle massage, careful chewing and manual removal of food from inside the affected cheek, and reassurance. Although 80% of affected men and nonpregnant women recover to a satisfactory level within a year, only approximately half of women who develop the disorder during pregnancy do so (Cunningham et al., 2010).
Autoimmune Disorders
Autoimmune disorders make up a large group of diseases that disrupt the function of the immune system of the body. In these types of disorders the body’s immune system is unable to distinguish “self” from “nonself.” As a result, antibodies develop that attack its normally present antigens, causing tissue damage. Autoimmune disorders can occur during pregnancy because a large percentage of women with an autoimmune disease are women of childbearing age (Gilbert, 2011). Common autoimmune diseases include systemic lupus erythematosus, myasthenia gravis, antiphospholipid syndrome, rheumatoid arthritis, and systemic sclerosis (Cunningham et al., 2010; Holmgren & Branch, 2007).
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a chronic, multisystem inflammatory disease that affects the skin, joints, kidneys, lungs, nervous system, liver, and other body organs. The exact cause is unknown but probably involves the interaction of several factors, including immunologic, environmental, hormonal, and genetic factors. SLE is the most common serious autoimmune disease affecting women of reproductive age. It occurs 2 to 4 times more often in African-American and Hispanic women than in Caucasian women and is 10 times more common in women than in men. Most cases of SLE occur in adolescence or young adulthood (Gilbert, 2011; Holmgren & Branch, 2007).
The most common presenting symptoms of SLE include fatigue, weight loss, arthralgias, arthritis, and myalgias. Although a diagnosis of SLE is suspected based on clinical signs and symptoms, it is confirmed by laboratory testing that demonstrates the presence of circulating autoantibodies. As is the case with other autoimmune diseases, SLE is characterized by a series of exacerbations (flares) and remissions (Holmgren & Branch, 2007).
If the diagnosis has been established and the woman desires a child, she is advised to wait until she has been in remission for at least 6 months before attempting to become pregnant (Gilbert, 2011). A lupus flare occurs during pregnancy or postpartum in 15% to 60% of women with SLE. In addition to an exacerbation, other maternal risks include an increased rate of miscarriage, nephritis, preeclampsia, possible need to give birth at a preterm gestation, and an increased risk of cesarean birth. Fetal risks include stillbirth, IUGR, and preterm birth (Holmgren & Branch, 2007).
Medical therapy during pregnancy is kept to a minimum in women who are in remission or who have a mild form of SLE. Immunosuppressive medications should be discontinued before conception. Nonsteroidal antiinflammatory drugs and aspirin are ordinarily the most commonly used antiinflammatory drugs, but they are not recommended for use during pregnancy. Aspirin should not be used after 24 weeks of gestation because of an increased risk of premature closure of the fetal ductus arteriosus (Cunningham et al., 2010). Maintenance therapy with hydroxychloroquine or low doses of glucocorticoids can continue. Hydroxychloroquine, an antimalarial drug, may be the best medication for maintenance SLE therapy during pregnancy because it significantly reduces SLE disease activity but appears to cause no adverse effects on the fetus (Holmgren & Branch, 2007).
Prenatal care otherwise focuses on close monitoring to detect common pregnancy complications, such as hypertension, proteinuria, and IUGR. Ultrasound examinations are performed frequently to monitor fetal growth. Fetal assessment tests, including daily fetal movement counts, nonstress tests, and amniotic fluid volume assessment, will likely begin at 30 to 32 weeks of gestation (see Chapter 26). More frequent ultrasound examinations and fetal testing are necessary if the woman develops a SLE flare, hypertension, proteinuria, or evidence of IUGR (Holmgren & Branch, 2007).
Women with SLE can develop an exacerbation during labor. Even if a flare does not occur, all women who have received chronic steroid therapy within the year will need larger (stress) doses of steroids during labor (Holmgren & Branch, 2007). Vaginal birth is preferred, but cesarean birth is common because of maternal and fetal complications.
Because determining which, if any, women are at risk for a SLE flare after birth is difficult, close follow-up with all of these women during the postpartum period is necessary. Any maintenance medications that were discontinued during the intrapartum period should be restarted immediately at doses similar to those used during pregnancy (Holmgren & Branch, 2007).
Women with SLE and chronic vascular or renal disease should limit their number of pregnancies because of maternal complications associated with the illness, as well as increased adverse perinatal outcomes (Cunningham et al., 2010). If desired, the safest time for tubal sterilization is during the postpartum period or when the disease is in remission. Estrogen-containing oral contraceptives may increase the risk of thromboembolism (Gilbert, 2011). Progestin-only implants and injections provide effective contraception with no known effects on lupus flares (Cunningham et al.). Barrier methods, in addition to progestin-only contraceptive options, are the least risky forms of contraception for women with SLE (Gilbert). Evidence does not support concerns regarding an increased risk of infection when IUDs are prescribed for women receiving immunosuppressive therapy (Cunningham et al.).
Myasthenia Gravis
Myasthenia gravis (MG), an autoimmune motor (muscle) end-plate disorder that involves acetylcholine use, affects the motor function at the myoneural junction. Muscle weakness results, particularly of the eyes, the face, the tongue, the neck, the limbs, and the respiratory muscles. In addition, women may experience ptosis, diplopia, and dysphagia. Women are affected twice as often as men, and the incidence peaks between the ages of 20 and 30 years (Porter & Branch, 2006). Because the greatest period of risk is during the first year after diagnosis, pregnancy should probably be avoided until symptomatic improvement occurs (Cunningham et al., 2010). The response of women with MG to pregnancy is unpredictable; remission, exacerbation, or continued stability during pregnancy can occur.
Pregnancy does not appear to affect the overall course of MG, but as the uterus enlarges respirations may be compromised. Also the normal fatigue experienced by many pregnant women may be tolerated poorly by those with MG (Cunningham et al., 2010). Treatment during pregnancy is the same as for nonpregnant women. Usual medications include glucocorticoids and acetylcholinesterase inhibitors. Monitoring blood glucose values is important because hyperglycemia may result from corticosteroid therapy. Thymectomy may result in remission of the disease but is best performed before or after pregnancy, if at all possible. For severe weakness, plasmapheresis or intravenous (IV) immunoglobulin therapy may be needed.
Because MG does not affect smooth muscle, most women usually tolerate labor well. Vaginal birth is desired, but vacuum or forceps assistance may be required because of muscle weakness. Oxytocin may be given, but all medications that cause muscular relaxation should be avoided if at all possible. Magnesium sulfate should not be administered to these women because it inhibits the release of acetylcholine and can trigger myasthenic crisis. Narcotics must be used cautiously because they may cause respiratory depression, and women with MG are already at risk for respiratory muscle weakness. Regional analgesia is preferred (Aminoff, 2009; Cunningham et al., 2010). After birth, women must be carefully supervised because relapses often occur during the puerperium.
Approximately 10% to 15% of neonates born to women with MG develop neonatal myasthenia. This transient disorder results from the transfer of maternal antibody against acetylcholine receptors across the placenta. Symptoms, including a poor cry, respiratory difficulties, weakness in suckling, a weak Moro reflex, and feeble limb movements, usually appear within the first 72 hours after birth. Neonatal myasthenia can be treated with anticholinesterase medications and usually resolves by 6 weeks after birth (Aminoff, 2009).
Gastrointestinal Disorders
Compromise of gastrointestinal (GI) function during pregnancy is a concern. Obvious physiologic alterations, such as the greatly enlarged uterus, and less apparent changes, such as hormonal differences and hypochlorhydria (deficiency of hydrochloric acid in the stomach’s gastric juice), require understanding for proper diagnosis and treatment. Gallbladder disease and inflammatory bowel disease are examples of GI disorders that may occur during pregnancy.
Cholelithiasis and Cholecystitis
Cholelithiasis (the presence of gallstones in the gallbladder) occurs more often in women than in men. Its incidence increases during pregnancy, probably because of increased hormone levels, along with pressure from the enlarged uterus that interferes with the normal circulation and drainage of the gallbladder. In fact, the second most common nonobstetric condition requiring surgery during pregnancy is symptomatic cholelithiasis, occurring in 1 of 1600 pregnancies (Blackburn, 2007; Lu & Curet, 2007).
Cholecystitis (inflammation of the gallbladder), although rare, also occurs more often during pregnancy and the postpartum period. The incidence of acute cholecystitis is about 4 cases per 10,000 pregnancies. It most often occurs in multiparous women who have a history of previous attacks. Acute cholecystitis is the third most common indication for nonobstetric surgical intervention in pregnancy (Blackburn, 2007; Cappell, 2007). Women with acute cholecystitis usually have fatty food intolerance along with colicky abdominal pain radiating to the back or shoulder, nausea, and vomiting. Fever may also be present. Ultrasound is often used to detect the presence of stones or dilation of the common bile duct (Lu & Curet, 2007).
Often gallbladder surgery is postponed until the puerperium. The woman can usually be managed conservatively for the remainder of the pregnancy. Initial therapy generally includes intravenous hydration, bowel rest with nasogastric suction and no oral intake, and narcotics. Morphine should not be used as an analgesic because it may cause ductal spasm. Antibiotics are given if evidence of cholecystitis or infection exists (Lu & Curet, 2007). See the Teaching for Self-Management box: Nutritional Counseling for the Pregnant Woman with Cholecystitis or Cholelithiasis for diet suggestions once the woman is able to resume oral intake. Currently, however, cholecystitis is increasingly being managed surgically during pregnancy. If cholecystitis is treated conservatively, there is a high risk for recurrent problems during the pregnancy. Also if cholecystitis recurs later in pregnancy, preterm labor is more likely, and if surgery is necessary it is technically more difficult to perform (Cunningham et al., 2010).
Women with obstructive jaundice, gallstone pancreatitis, suspected peritonitis or those for whom conservative (medical) management has not been successful should be treated surgically with cholecystectomy or cholecystotomy (Lu & Curet, 2007). Although the second trimester has traditionally been considered the safest time for this surgery, it is increasingly performed at any time during pregnancy because of improved
surgical outcomes. Both laparoscopic and open cholecystectomy procedures are acceptable during pregnancy (Cappell, 2007; Cunningham et al., 2010). Preoperative care includes IV fluids, discontinuing oral intake, analgesia, and administration of antibiotics.
Inflammatory Bowel Disease
Inflammatory bowel disease, particularly ulcerative colitis and Crohn disease, is relatively common in young women, so these disorders are seen during pregnancy. The incidence of an inflammatory bowel disease flare is not increased in pregnancy and no evidence suggests that pregnancy significantly affects either ulcerative colitis or Crohn disease (Cunningham et al., 2010). Women with ulcerative colitis and Crohn disease usually have healthy babies at the same rate as the general population, although some studies have suggested a higher risk for preterm birth and low-birth-weight infants (Kelly & Savides, 2009). Active disease early in pregnancy increases the risk for a poor pregnancy outcome (Cunningham et al.).
Treatment of inflammatory bowel disease is usually the same for the pregnant woman as it is for the nonpregnant woman. Sulfasalazine, 5-aminosalicylate drugs, and corticosteroids are often prescribed for treatment of inflammatory bowel disease. These drugs appear to be safe for use during pregnancy (Kelly & Savides, 2009). Fat-soluble vitamin and folic acid supplementation is especially important because of problems with intestinal malabsorption. Calcium supplementation is also necessary because osteoporosis is common. Some women may require parenteral nutrition. With complications, such as hemorrhage, or if there is no response to medical therapy, surgery may be indicated (Cunningham et al., 2010).
Urinary Tract Infections
Urinary tract infections (UTIs) are a common medical complication of pregnancy, occurring in approximately 20% of all pregnancies. They are also responsible for 10% of all hospitalizations during pregnancy (Duff, Sweet, & Edwards, 2009). UTIs include asymptomatic bacteriuria, cystitis, and pyelonephritis. UTIs are usually caused by coliform organisms that are a normal part of the perineal flora. By far the most common cause is Escherichia coli, a gram-negative bacteria responsible for 85% of cases. Another gram-negative bacterium that causes UTIs is Klebsiella pneumoniae. The gram-positive organisms group B streptococci, enterococci, and staphylococci account for approximately 3% to 7% of all infections (Gilbert, 2011).
Asymptomatic Bacteriuria
Asymptomatic bacteriuria refers to the persistent presence of bacteria within the urinary tract of women who have no symptoms. A clean-voided urine specimen containing more than 100,000 organisms per ml is diagnostic. If asymptomatic bacteriuria is not treated, up to 40% of infected women will subsequently develop symptomatic infection during the pregnancy (Colombo & Samuels, 2007). Therefore, the ACOG recommends that all women be screened for asymptomatic bacteriuria at their first prenatal visit (Colombo & Samuels). Asymptomatic bacteriuria has been associated with preterm birth and low-birth-weight infants (American Academy of Pediatrics [AAP] & ACOG, 2007; Cunningham et al., 2010).
Asymptomatic bacteriuria should be treated with an antibiotic. Antibiotics that are often prescribed include amoxicillin, ampicillin, cephalexin (Keflex), ciprofloxacin (Cipro), levofloxacin (Levaquin), nitrofurantoin (Macrodantin), and trimethoprim-sulfamethoxazole (Bactrim DS). Several different regimens, including single dose, 3-, 7-, and 10-day treatment may be used (Cunningham et al., 2010). A repeat urine culture is usually ordered 1 to 2 weeks after completing therapy because approximately 15% of women will not respond to therapy or will have a reinfection (Colombo & Samuels, 2007). Women who have persistent or frequent recurrences of bacteriuria may be placed on suppressive therapy, often nitrofurantoin each night at bedtime, for the remainder of the pregnancy (Cunningham et al.).
Cystitis
Cystitis (bladder infection) is characterized by dysuria, urgency, and frequency, along with lower abdominal or suprapubic pain. Usually white blood cells, as well as bacteria, will be found in the urine. Microscopic or gross hematuria may also be present. Typically, symptoms are confined to the bladder rather than becoming systemic. Cystitis is usually uncomplicated, but it may lead to ascending UTI if untreated. Approximately 40% of pregnant women with pyelonephritis experienced symptoms of bladder infection before developing pyelonephritis (Cunningham et al., 2010).
Cystitis is often treated with a 3-day course of antibiotic therapy, which is usually 90% effective in curing the infection. Antibiotics often prescribed include amoxicillin, ampicillin, cephalexin (Keflex), ciprofloxacin (Cipro), levofloxacin (Levaquin), nitrofurantoin (Macrodantin), and trimethoprim-sulfamethoxazole (Bactrim DS) (Cunningham et al., 2010). Phenazopyridine (Pyridium), a urinary analgesic, is often prescribed along with an antibiotic for relief of symptoms caused by irritation of the urinary tract. Although phenazopyridine is effective at relieving dysuria, urgency, and frequency, women should be taught that the medication colors urine and tears orange. Therefore, they should be instructed to avoid wearing contact lenses while taking this medication and warned that it will stain underwear.
Pyelonephritis
Renal infection (pyelonephritis) is a common serious medical complication of pregnancy and the second most common nondelivery reason for hospitalization (Cunningham et al., 2010). The most common maternal complications associated with pyelonephritis include anemia, septicemia, transient renal dysfunction, and pulmonary insufficiency. Women with pyelonephritis can develop urosepsis, sepsis syndrome, and renal dysfunction. In addition, pulmonary injury resembling ARDS can occur in pregnant women with acute pyelonephritis, most likely the result of damage to alveolar tissue caused by the release of endotoxins from gram-negative bacteria (Colombo & Samuels, 2007; Cunningham et al.). Recurrent pyelonephritis is thought to cause fetal death and IUGR. Acute pyelonephritis is associated with preterm labor (Colombo & Samuels).
Pyelonephritis develops most often during the second trimester of pregnancy and is usually caused by the E. coli organism. Infection develops only in the right kidney in more than half of all cases. The onset of pyelonephritis is often abrupt, with fever, shaking chills, and aching in the lumbar area of the back. Anorexia and nausea and vomiting also can be present. Usually one or both costovertebral angles will be tender to palpation.
Women diagnosed with pyelonephritis are admitted to the hospital immediately. Treatment with IV antibiotics is started as soon as urine and blood samples for culture and sensitivity have been collected. Ampicillin, gentamicin, cefazolin (Ancef), or ceftriaxone (Rocephin) are often ordered initially because they are broad-spectrum antibiotics that are usually effective. The woman must be monitored closely for the possible development of sepsis (Cunningham et al., 2010).
Clinical symptoms generally resolve within a couple of days after antibiotic therapy is begun. The antibiotic may need to be changed based on the results of the initial culture and sensitivity testing, or if the woman has not responded to therapy within 48 hours (Gilbert, 2011). Most women become afebrile within 72 hours. If no clinical improvement is seen within 48 to 72 hours, an ultrasound should be performed to assess for a urinary tract obstruction. Once the woman is afebrile, she will be changed from IV to oral antibiotics (Cunningham et al., 2010).
Usually antibiotic therapy is continued for 7 to 14 days after the woman is discharged from the hospital. A urine culture will likely be repeated 1 to 2 weeks after antibiotic therapy has been completed. Recurrent infection develops in 30% to 40% of women after completion of treatment for pyelonephritis. Therefore, urine cultures should be obtained each trimester for the remainder of the pregnancy. Many women are maintained on a prophylactic antibiotic (often nitrofurantoin once or twice daily) for the remainder of the pregnancy (Colombo & Samuels, 2007; Cunningham et al., 2010).
Client Education
Nurses are often responsible for teaching pregnant women about taking medications safely and effectively. This education is especially important in regard to antibiotics because this type of medication is so often misused by the general public. The woman should be instructed to finish the entire course of prescribed antibiotic therapy rather than stopping the medication as soon as she feels better. Failure to do so can lead to the creation of additional drug-resistant organisms. Antibiotics should
be taken on time and around the clock so that medication levels in the body remain constant. Finally, many women will develop a yeast infection while taking antibiotics because the medication kills normal flora in the genitourinary tract, as well as pathologic organisms. Therefore, they should be encouraged to include yogurt, cheese, or milk containing active acidophilus cultures in their diet while on antibiotics.
Woman should also be taught simple ways to prevent urinary tract infections. See the Teaching for Self-Management box: Prevention of Urinary Tract Infections for several suggestions.
Surgery During Pregnancy
The need for abdominal surgery occurs as frequently among pregnant women as among nonpregnant women of comparable age. However, pregnancy may make the diagnosis more difficult. An enlarged uterus and displaced internal organs may make abdominal palpation more difficult, alter the position of an affected organ, and/or change the usual signs and symptoms associated with a particular disorder. The most common nongynecologic condition necessitating abdominal surgery during pregnancy is appendicitis.
Appendicitis
Appendicitis occurs approximately once in 1000 pregnancies. The incidence is 30%, 45%, and 25% in the first, second, and third trimesters, respectively (Mahomed, 2006). The diagnosis of appendicitis is often delayed because the usual signs and symptoms mimic some normal changes of pregnancy such as nausea and vomiting and increased white blood cell (WBC) count. As pregnancy progresses, the appendix is pushed upward and to the right from its usual anatomic location (see Fig. 13-14) (Cunningham et al., 2010). Because of these changes, rupture of the appendix and the subsequent development of peritonitis occur two to three times more often in pregnant women than in nonpregnant women.
The most common symptom of appendicitis in pregnant women is right lower quadrant abdominal pain, regardless of gestational age. Nausea and vomiting are often present, but loss of appetite is not a reliable indicator of appendicitis. Fever, tachycardia, a dry tongue, and localized abdominal tenderness are commonly found in nonpregnant persons with appendicitis, but they are less likely indicators for the disorder in pregnant women. Because of the physiologic increase in WBCs that occurs in pregnancy, this test is not helpful in making the diagnosis. A urinalysis and a chest x-ray should be performed to rule out UTI and right lower lobe pneumonia, given that both of these conditions can cause lower abdominal pain (Kelly & Savides, 2009). Appendicitis can also be confused with other disorders such as cholecystitis, preterm labor, pyelonephritis, or placental abruption (abruptio placentae) (Cunningham et al., 2010).
Ultrasound is useful during the first and second trimesters of pregnancy for diagnosing appendicitis. It is less accurate during the third trimester than earlier in pregnancy because it is technically more difficult to perform. In the third trimester of pregnancy, helical CT scanning may be more useful than other imaging modalities (Lu & Curet, 2007). MRI may be used if appendicitis has not been confirmed by other imaging techniques (Kelly & Savides, 2009).
Prompt surgical intervention to remove the appendix is still the standard treatment (Kelly & Savides, 2009). Appendectomy before rupture usually does not require either antibiotic or tocolytic therapy. If surgery is delayed until after rupture, multiple antibiotics are ordered. Rupture is likely to result in preterm labor and perhaps fetal loss.
Care Management
Initial assessment of the pregnant woman requiring surgery focuses on her presenting signs and symptoms. A thorough history and physical examination are performed. Laboratory testing includes, at a minimum, a complete blood count with differential and a urinalysis. Additional laboratory and other diagnostic tests may be necessary to reach a diagnosis. In addition, fetal heart rate (FHR) and activity, along with uterine activity, should be monitored, and constant vigilance for symptoms of impending obstetric complications maintained. The extent of presurgery assessment is determined by the immediacy of surgical intervention and the specific disorder that requires surgery.
Hospital Care
When surgery becomes necessary during pregnancy, the woman and her family are concerned about the effects of the procedure and medication on fetal well-being and the course of pregnancy. An important aspect of preoperative nursing care is encouraging the woman to express her fears, concerns, and questions.
Preoperative care for a pregnant woman differs from that for a nonpregnant woman in one significant aspect: the presence of at least one other person, the fetus. Continuous FHR and uterine contraction monitoring should be performed if the fetus is considered viable. Procedures such as preparation of the operative site and time of insertion of IV lines and urinary retention catheters vary with the physician and the facility. However, in every instance, there is a total restriction of solid foods and liquids or a clear specification of the type, amount, and time at which clear liquids may be taken before surgery. Some bowel preparation such as clear liquids and laxatives may be required before surgery. Food by mouth is restricted for several hours before a scheduled procedure. Even if she has had nothing by mouth—but more important, if surgery is unexpected—the woman is in danger of vomiting and aspirating, and special precautions are taken before anesthetic is administered (e.g., administering an antacid).
Intraoperatively, perinatal nurses may collaborate with the surgical staff to increase their knowledge about the special needs of pregnant women undergoing surgery. One intervention to improve fetal oxygenation is positioning the woman on the operating table with a lateral tilt to avoid compression of the maternal vena cava. Continuous fetal and uterine monitoring during the procedure is recommended because of the risk for preterm labor. Monitoring may be accomplished by using sterile aquasonic gel and a sterile sleeve for the transducer. During abdominal surgery, uterine contractions may be manually palpated.
In the immediate recovery period, general observations and care pertinent to postoperative recovery are initiated. Frequent assessments are carried out for several hours after surgery. Whether the woman is cared for in the surgical postanesthesia recovery area or in a labor and birth unit, continuous fetal and uterine monitoring will likely be initiated or resumed because of the potential risk for preterm labor. Tocolysis may be necessary if preterm labor occurs (see Chapter 33).
Home Care
Plans for the woman’s return home and for convalescent care should be completed as early as possible before discharge. Depending on her insurance coverage, nursing care may be provided through a home health agency. If not, the woman and other support persons must be taught necessary skills and procedures, such as wound care. Ideally the woman and other caregivers should have opportunities for supervised practice before discharge so that they can feel comfortable with their knowledge and ability before being totally responsible for providing care. Box 30-3 lists information that should be included in discharge teaching for the postoperative client. The woman also may need referrals to various community agencies for evaluation of the home situation, child care, home health care, and financial or other assistance.
KEY POINTS
• The normal hemodynamic values are significantly altered as a result of pregnancy.
• The stress of the normal maternal adaptations to pregnancy on a heart whose function is already taxed may cause cardiac decompensation.
• Maternal morbidity and mortality are significant risks in a pregnancy complicated by mitral stenosis.
• In the case of a cardiac arrest in a pregnant woman, the standard advanced cardiac life support guidelines should be implemented with a few slight modifications: the uterus must be displaced laterally, and the defibrillation paddles should be placed one rib interspace higher.
• Anemia, a common medical disorder of pregnancy, affects at least 20% of pregnant women.
• Asthma is a common medical condition to complicate pregnancy, and the prevalence and morbidity from this disorder are increasing.
• Pruritus is a common symptom in pregnancy-specific inflammatory skin diseases.
• A pregnant woman with epilepsy should take only one anticonvulsant medication at the lowest dose level that is effective at keeping her seizure-free.
• Autoimmune disorders can occur during pregnancy because a large percentage of persons with an autoimmune disorder are women of childbearing age. Common autoimmune diseases include SLE and MG.
• Cholecystitis and cholelithiasis are common GI problems in pregnancy.
• UTIs are a common medical complication of pregnancy.
• Pyelonephritis is a very serious medical complication of pregnancy and the second most common nondelivery reason for hospitalization.
• In the pregnant woman, an enlarged uterus, displaced internal organs, and altered laboratory values may confuse diagnosis when the need for immediate abdominal surgery occurs.
• Perioperative care for a pregnant woman differs from that for a nonpregnant woman in one significant aspect: the presence of at least one other person, the fetus.
![]() Audio Chapter Summaries Access an audio summary of the Key Points on
Audio Chapter Summaries Access an audio summary of the Key Points on ![]()