Equine Anesthesia
After completion of this chapter, the reader will be able to:
• Describe anesthetic techniques commonly used in equine practice.
• Explain the special anesthetic challenges resulting from patient temperament, large body size, and equine anatomy and physiology.
• List the causes of nasal congestion, atelectasis, neuropathy, and myopathy, and describe strategies to prevent these anesthetic complications.
• Describe the differences between anesthetic protocols and procedures used for field anesthesia and anesthesia in a clinic.
• Explain the indications for, the advantages of, and risks associated with standing chemical restraint.
• Describe anesthetic induction by intravenous injection and by inhalation via a nasotracheal tube.
• Prepare an equine patient, anesthetic equipment, and anesthetic agents and adjuncts for general anesthesia.
• Explain cautions and risks associated with each method of anesthetic induction, and strategies to maximize patient safety.
• Explain how to do each of the following: (1) select and prepare an endotracheal tube (ETT) for placement; (2) place an ETT in a horse; (3) check for proper placement; (4) inflate the cuff; (5) extubate a patient during anesthetic recovery.
• Describe maintenance of general anesthesia with an inhalant agent and with intravenous agents.
• List principles of providing appropriate patient positioning, comfort, and safety during anesthetic maintenance.
• Explain the significance of hypoventilation, hypoxemia, and hypotension in equine patients, as well as describe prevention and management strategies of these anesthetic complications.
• List factors that affect patient recovery from anesthesia, the signs of recovery, appropriate monitoring during recovery, and oxygen therapy during recovery.
• Describe general nursing care during the postanesthetic period.
The basic principles of anesthesia discussed in Chapter 8 apply to equine anesthesia. Horses present unique challenges to the anesthetist because of their temperament, size, anatomy, and physiology. The anesthetist should be aware of these concerns before anesthetizing equine patients.
Different breeds of horse, and even individuals within the same breed, can have varying temperaments ranging from calm and stoic to excitable and nervous. Also, because horses are “flight” animals (animals that tend to run away from stressful situations), even a normally calm, stoic horse can become excited in an unfamiliar environment such as a veterinary hospital. An excited horse may behave unpredictably and can cause injury to itself and veterinary personnel. A complete discussion of handling the equine patient is beyond the scope of this chapter; however, it is important to have a good understanding of how to catch, handle, and physically restrain a horse in order to minimize risk to the horse, the anesthetist, and other personnel. An aspect of equine behavior that differs from that of other species is that horses have an instinctive desire to stand shortly after awakening from anesthesia, a behavior that makes any equine anesthetic recovery relatively high risk. Ideally both induction and recovery from anesthesia should occur in a calm, quiet environment, with subdued lighting if possible.
The average adult horse weighs 350 to 500 kg, and some larger breed horses may weigh as much as 1000 kg. This necessitates having specialized equipment such as induction and recovery stalls, hoists, and special large animal surgery tables and anesthetic machines in addition to small animal machines and equipment, which are used for patients weighing less that 150 kg (foals, miniature horses). The equine anesthetist must be familiar with the operation of all related equipment in addition to anesthetic machines and monitors.
Anatomic concerns involve the respiratory, gastrointestinal, and musculoskeletal systems. Horses are obligate nasal breathers; thus anything that causes nasal obstruction, such as congestion (which develops when the head is below the withers during general anesthesia) or a horse pressing its nostrils against the recovery stall wall, can quickly lead to respiratory compromise and death without intervention. The large, heavy gastrointestinal tract places pressure on the lungs when horses are placed in dorsal or lateral recumbency, causing atelectasis (collapsed alveoli). Atelectatic lung tissue is not available for gas exchange; thus horses are prone to hypoxemia under anesthesia. Many anesthetic drugs affect the gastrointestinal tract (anticholinergics, opioids, alpha2-agonists), which must be taken into consideration when protocols are selected, as horses are susceptible to developing colic. Some superficial nerves (e.g., facial nerve, radial nerve) can become damaged (neuropathy) if intraoperative padding is not appropriate or if the halter is inadvertently left on during anesthesia. Muscle blood flow must be maintained during anesthesia in order to prevent myopathy, which manifests in recovery as muscle hardness, pain, and weakness and is commonly referred to using the lay term “tying up.” Insufficient padding can also lead to myopathy.
Because of these challenges, it is preferable, if the horse’s temperament and the surgical approach allow, to perform procedures on lightly or heavily sedated horses. Heavy sedation is often referred to as standing chemical restraint, and these terms are used interchangeably. Many diagnostic and surgical procedures can be performed with the patient under standing chemical restraint with the addition of local anesthetic nerve blocks (Box 9-1). Horses that are not cooperative after sedation and horses undergoing more complex procedures (e.g., abdominal surgery, arthroscopy) do, however, require general anesthesia. General anesthesia is frequently carried out at farms or stables and is referred to as field anesthesia. As the name implies, field anesthesia occurs away from the veterinary hospital in a relatively clean stall or paddock and is appropriate for short procedures (20 to 45 minutes). Procedures that will last longer than 60 minutes, those that are complex, and those involving compromised patients should be performed at a veterinary clinic where inhalant anesthetics and oxygen can be administered using an anesthetic machine and where anesthetic monitoring is available. As with small animal anesthesia, neuromuscular blockers are rarely used in general practice but are sometimes used to provide muscle relaxation for ocular and orthopedic procedures in veterinary schools and referral practices.
PATIENT PREPARATION
The reader is referred to Chapters 2 and 8 for a detailed discussion of the essentials of patient preparation before anesthesia. See Procedure 9-1, p. 279, for additional tasks pertinent to preparation of the equine patient undergoing general anesthesia. In addition, the anesthetist should be familiar with operation of additional equipment such as surgical tables and hoists that will be used during the anesthetic episode.
SELECTING A PROTOCOL
A suitable protocol takes into account the minimum patient database, the patient’s physical status class, and the type and duration of the procedure to be performed. Location also plays a role; field anesthesia is most commonly performed under total intravenous anesthesia (TIVA) whereas in a veterinary clinic the anesthetic protocol may be TIVA, or induction with an injectable drug followed by maintenance with an inhalant agent.
Regardless of the protocol, the correct drugs and amounts must be prepared. Box 8-2 shows the steps required to calculate the doses of most injectable drugs, and Box 9-2 shows an example of drug calculations for a horse. Ill, geriatric, pediatric, or otherwise compromised patients (physical status class P3 to P5) require use of modified protocols based on the patient’s primary condition. Management of these cases can be quite challenging and requires customization of the anesthetic protocol by the veterinarian-in-charge (VIC).
SUMMARY OF A GENERAL ANESTHETIC PROCEDURE
The dynamics for the commonly used protocols in equine anesthesia are similar to those for small animal (see Chapter 8), with the exception that induction with an intramuscular (IM) agent is not done in clinical practice, although it is used for capture of feral horses.
EQUIPMENT PREPARATION
During a typical anesthetic induction, many events occur in rapid succession. Anesthetic agents are administered, the patient becomes unconscious and recumbent, and the endotracheal tube is placed, secured, and cuffed. The horse is then hoisted onto the surgery table, the halter is removed, and the endotracheal tube is connected to the anesthetic machine and the anesthetic gas level is adjusted, all within the first few minutes. Because these events follow one another so rapidly, the technician does not have the luxury of leaving the patient to locate equipment. For this reason, all equipment must be carefully gathered, checked, and organized before commencement of the procedure.
Equine patients weighing more than 150 kg are usually placed on a large animal anesthetic machine (Figure 9-1). Most large animal anesthetic machines incorporate a ventilator (Figure 9-1, D). Both the circle system and the ventilator of the machine should be checked before use. Smaller horses, ponies, and foals weighing less than 150 kg
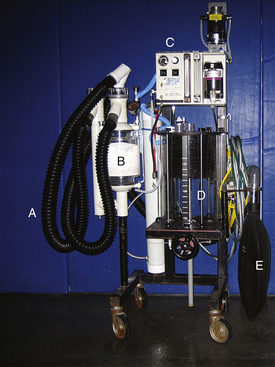
FIGURE 9-1 Large animal anesthetic machine (Drager). A, Large animal breathing tubes and Y-piece. B, CO2 absorber canister. C, Ventilator control panel, flow meters, and vaporizers. D, Ventilator bellows and housing. E, 35-L reservoir bag.
can be placed on a small animal anesthetic machine. Hypothermia is uncommon in anesthetized adult horses; however, methods such as forced air warming and warm water circulating blankets can be used in smaller horses and foals. A crash cart containing emergency equipment and drugs should also always be available.
PREMEDICATION OR SEDATION
Premedication refers to the administration of anesthetic agents and adjuncts to calm and prepare the patient for anesthetic induction. Preanesthetic medications are chosen specifically to produce a set of desired effects such as sedation, analgesia, and muscle relaxation. Tranquilizers, alpha2-agonists, and opioids are commonly used as preanesthetic medications and are given via the IM or intravenous (IV) route. Anticholinergic drugs are not used to premedicate horses because they reduce gastrointestinal motility, which may result in colic. This class of drugs is therefore reserved for treatment of arrhythmias and for cardiopulmonary resuscitation (CPR) in this species.
The preanesthetic procedure in horses differs slightly from that used for small animals. After appropriate patient assessment, the first step is placement of an IV catheter (4 to 6 inch, 14 to 16 gauge), almost always in one of the jugular veins. Some horses object to venipuncture and must be sedated first. Such horses may be premedicated at this time (Protocol 9-1). Alternatively, a low dose of xylazine (0.2 to 0.5 mg/kg IV) may be sufficient to achieve catheter placement. Once the horse is cooperative, a small bleb of local anesthetic is administered over the proposed site of catheterization to desensitize the skin.
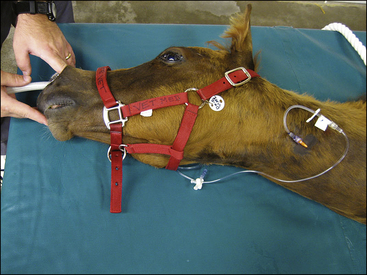
After catheterization, the horse’s mouth should be washed out with a large syringe (Figure 9-2) to flush out any feed material. This prevents aspiration of the material during intubation or in recovery. Feet should be cleaned before sedation, and then shoes should be removed or wrapped. Just before or immediately after premedication, the horse is positioned in an induction area or placed adjacent to a tilt table. Some breeds generally require higher doses of sedatives than others—for example, Arabians and thoroughbreds, particularly those in training—whereas draught horses typically require lower doses. See Protocol 9-1 for preanesthetic and sedative protocols in horses.

FIGURE 9-2 Preparing a horse for general anesthesia. Flushing a horse’s mouth with water using a large dosing syringe. The nozzle of the syringe is inserted between the horse’s cheek and teeth. This is done on both sides of the mouth to flush out feed material.
Standing Chemical Restraint
Standing chemical restraint is essentially a continuation or extension of sedation. The patient is prepared as if it were having surgery, with placement of an IV catheter and extension set. The patient is usually secured in stocks for the procedure (Figure 9-3). If the level of sedation required for the procedure is inadequate, additional drugs are given intravenously. See Protocol 9-2 for standing chemical restraint protocols in horses. The dynamics of standing chemical restraint differ because general anesthesia is not the goal; the horse remains standing. The horse’s level of consciousness may change from light to heavy sedation, which can be gauged based on the horse’s level of interest in the environment, head position, and stance. On rare occasions general anesthesia may be required after or during standing restraint. If a horse becomes oversedated or becomes excited and falls
in the stocks, or if the veterinarian cannot perform the procedure because of inadequate sedation or surgical access, the anesthetist should be prepared to anesthetize the horse under instructions from the VIC. If the procedure lasts for a considerable period of time, the horse may develop nasal congestion, which could lead to respiratory obstruction. To avoid this, the head should be held up in a neutral position. If the horse is placed in stocks, cross-ties can be used for this purpose.
Signs of appropriate sedation before anesthetic induction or for standing restraint include lowering of the head and neck, drooping of the lower lip, a reluctance to move, a wide-based stance, and a lack of interest in the surrounding activity. Some horses remain sensitive to sudden loud noises and movements. This can be diminished by ensuring the work area of the induction stall is quiet, by covering the horse’s eyes, or by placing cotton in the horse’s ears. Moving a horse into position behind a squeeze gate or into stocks may cause brief excitement or loss of sedation. Waiting for a few minutes will usually allow the horse to settle down. It may also be necessary to give additional sedative drug if the horse is not adequately sedated. It is also possible that external stimuli in an environment unfamiliar to the horse may result in the excitement, even if the horse initially appeared to be adequately sedated with acepromazine or an alpha2-agonist. If this occurs, the horse should be given time to calm down (decrease external stimuli, refrain from trying to move the horse into the induction area) before proceeding. Again, additional sedation may also be required. Once the patient is adequately sedated, anesthetic induction should immediately follow, or, as an alternative, these protocols can be used alone to provide sedation for diagnostic and therapeutic procedures.
ANESTHETIC INDUCTION
Anesthetic induction is the process by which an animal loses consciousness and enters surgical anesthesia. In addition to the goals set out for induction in Chapter 8, an additional goal for equine anesthetic induction is to render the horse unconscious as quickly as possible so that its transition from standing to lateral recumbency occurs with minimal risk of injury to the horse or personnel. In healthy horses induction drugs are therefore given as rapid bolus injections, rather than “to effect.” Induction is most commonly accomplished by IV administration of injectable agents, typically ketamine alone or in combination with other agents. Inhalant induction is reserved for foals that can be nasotracheally intubated while still awake; foals that will tolerate this are typically compromised and will require careful anesthetic management. What follows is a description of specific techniques used to induce anesthesia. (See Protocol 9-3 for IV induction protocols in horses, and Procedure 9-2, p. 279, for the sequence of events.)
Intravenous Induction
Unless it occurs in the field, induction typically occurs in a special induction stall that has padded walls and often a padded floor. Induction may be done “free fall” or behind
a gate that restrains the horse (Figure 9-4). Sometimes the induction stall is also used for recovery. In comparison to small animals, in which IV induction is given to effect, the goal of induction in horses is to rapidly take the horse from standing (sedated) to lateral recumbency (unconscious) so as to minimize excitement, which can lead to the horse’s injuring itself or personnel. All drugs are therefore given as a bolus, with the exception of the muscle relaxant guaifenesin, which is administered rapidly intravenously to effect by placing it in a pressure bag (Figure 9-5). Once the horse shows signs of ataxia, typically knuckling of the forelimbs at the carpi and/or fetlocks, the induction agent is given as a bolus.

FIGURE 9-4 Equine anesthetic induction gate. Premedicated horse restrained behind a gate before induction. The purpose of the rope (which is looped through a ring in the wall of the induction stall) is to prevent the horse from moving forward during induction and potentially injuring itself or personnel. One person controls the rope, and an assistant should always be present to control the head of the horse.

FIGURE 9-5 Guaifenesin in a pressure bag. Guaifenesin is administered as a rapid infusion using a pressure bag. Note that the induction drug (in this case ketamine) is attached to the three-way stopcock so that once the desired level of muscle relaxation has been reached, anesthesia can be induced.
Once anesthesia has been induced, the vital signs should be briefly checked. The horse is then intubated.
In some practices the floor of the induction stall forms part of the surgery table, but in many the horse must be hoisted onto a table (Figure 9-6). It is important to understand how the hoist functions so that the horse can be transported safely and any problems can be resolved rapidly.

FIGURE 9-6 Hoisting a horse after induction. A, Hobbles are placed distal to the fetlock joints of the front and hindlimbs and attached to the hook of a hoist. B, The horse is then hoisted so that a large animal surgery table can be positioned underneath it. The hoist can then be used to facilitate correct positioning on the table. The anesthetist controls and supports the head while an assistant controls the tail.
It is important to ensure that muscles and prominent nerves are protected when a horse is placed on a surgical table or surface. The anesthetist should make sure that muscle groups are well supported and do not rest on hard surfaces to prevent myopathy (“tying up”) and that the facial and radial nerves are protected. Horses in lateral recumbency should have the forelimb closest to the table pulled forward if possible to decrease the pressure placed on it by the chest and opposite limb, and the hindlimbs should be separated by padding so that they are in a neutral position (Figure 9-7).
Agents commonly used to induce general anesthesia in horses by IV injection include (1) ketamine as a bolus injection, (2) a mixture of either ketamine and diazepam or midazolam as a bolus injection, and (3) guaifenesin infused under pressure to effect followed by ketamine as a bolus injection.
After induction with the commonly used IV injectable agents, the duration of anesthesia varies but is usually no more than 10 to 20 minutes. If a period longer than 20 minutes is required, anesthesia is maintained with inhalation anesthetics or administration of repeat boluses or a constant rate infusion (CRI) of ketamine. Occasionally horses will be too lightly anesthetized to intubate or place on the hoist after the induction dose. If this is the case, a bolus dose of ketamine at 0.4 mg/kg (one fifth of the induction dose) or thiopental at 0.5 mg/kg is given intravenously. See Procedure 9-3, p. 279, for IV induction in horses.
Inhalation Induction via Nasotracheal Tube
This technique is limited to use in young foals, particularly those that are sick or those that will tolerate nasotracheal intubation. The anatomy of the horse’s nasal passages and nasopharynx is such that an endotracheal tube passed from the nostril into the ventral nasal meatus will emerge in the nasopharynx in a position that favors entry into the larynx. Once the nasotracheal tube has been placed and the cuff inflated, the tube is connected to the breathing system of a small animal machine. Oxygen and inhalant are then administered. (See Protocol 9-4 for inhalant induction protocols in foals and Procedure 9-4, p. 280, for the technique.)
This technique has the same risks as mask induction in small animals (see Chapter 8). The placement of the nasotracheal tube has the advantage of having few, if any, leaks compared with mask induction; thus induction should be faster and can occur at lower vaporizer settings, and causes far less environmental pollution.
Foals that require general anesthesia and are amenable to nasotracheal intubation without sedation are often compromised. Care should be taken during inhalant induction in these patients because anesthesia may become deep relatively quickly compared with anesthesia in their healthy counterparts.
ENDOTRACHEAL INTUBATION
After induction of general anesthesia, an endotracheal tube is usually placed. The advantages of intubation are discussed in Chapter 4, p. 97 and Chapter 8, p. 245.
Equipment for Endotracheal Intubation
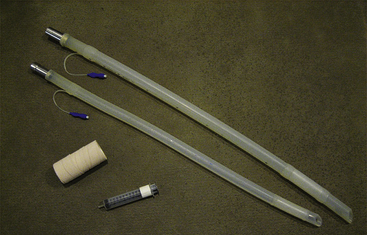
The following equipment is required to perform endotracheal intubation (Figure 9-8):
Selecting an Endotracheal Tube
The general principles for selecting an endotracheal tube are discussed in Chapter 8. Adult horses typically require a 22-mm, 26-mm, or 30-mm diameter cuffed tube. Because of head and neck length in horses, endobronchial intubation is rarely of concern. Typically two tube sizes are selected for intubation—the anticipated size and one size smaller. Foals require smaller tubes, but rarely smaller than 10 mm in diameter. Longer tubes of smaller diameter may be required for successful nasotracheal intubation in foals.
Endotracheal tubes are further discussed in Chapter 4.
Preparing the Tube
Before an endotracheal tube is used, it must be checked for integrity. It should be clean, sanitized, and free of blockages, holes, deterioration, or other damage. The connector must be securely attached, and the cuff must inflate and hold pressure after the syringe is detached from the valve. The tube may be lubricated with a small amount of sterile water-soluble lubricant, although this is not essential in most horses.
Intubation Procedure
Intubation in the horse is performed blindly. This means that the anesthetist does not directly visualize the larynx but instead passes the tube more by feel. The oral and oropharyngeal anatomy of the horse make blind intubation relatively easy. Unlike in other species, it is uncommon for the tube to pass into the esophagus.
The horse’s head is extended, the tongue is gently pulled to the side of the mouth, and a mouth gag or speculum is placed. Mouth gags can be proprietary, or homemade from polyvinyl chloride (PVC) piping. The endotracheal tube is then passed through the mouth gag, over the base of the tongue, and into the larynx. If the anesthetist meets resistance at the level of the laryngopharynx, he or she should withdraw the tube 1 to 2 inches, rotate it 90 degrees, and advance it again (Figure 9-9 and Procedure 9-5, p. 280).
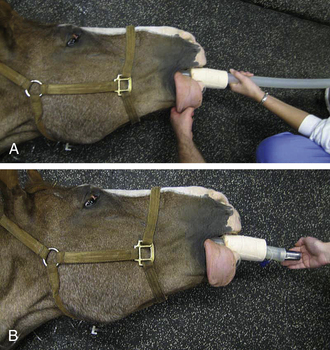
FIGURE 9-9 Intubation of the horse. A, The anesthetist advances the endotracheal tube blindly through a speculum in the mouth into the larynx with the head extended. B, The anesthetist feels for movement of air when the horse breathes out to confirm correct placement of the tube in the trachea.
Advancement of the tube without resistance indicates successful placement in the trachea. Intubation is confirmed by feeling air move when the horse exhales, or when an assistant pushes on the thoracic wall. The endotracheal tube in horses is either tied to the mouth speculum or taped to the horse’s muzzle. In the event that a tube will not pass into the larynx, changing the angle of the head slightly, changing the angle of the tube slightly, or trying with a smaller tube usually results in success. If there is any resistance, it is important not to force the tube, as this may damage the larynx.
The cuff is inflated as for small animal intubation (see Chapter 8). Often it is partially inflated before hoisting, then, once the patient is connected to the anesthetic machine, the cuff is checked for proper inflation in the same way as for a small animal patient.
Nasotracheal intubation may be preferred over orotracheal intubation in horses undergoing some surgeries of the head and neck (e.g., sinus surgery, dental surgery). Nasotracheal intubation is performed by passing a well-lubricated tube, one size smaller than will likely pass orotracheally, into the ventral nasal meatus with the head in the same position as for orotracheal intubation. The tube should be passed very gently in order to avoid damaging the nasal mucosa and turbinates and causing epistaxis (nosebleed).
Complications of Intubation
Complications are similar to those in small animal anesthesia. Additional concerns include the following:
• Epistaxis may occur as a result of nasal intubation.
• Animals with abnormal anatomy (miniature horses, horses with diseases of the oral and nasal cavity, horses with laryngeal paralysis) may be difficult or impossible to intubate. These patients may require endoscopy-assisted intubation, in which an endoscope is passed through the tube and into the larynx, then the tube is threaded off the endoscope. In some cases placement of an endotracheal tube through a tracheostomy incision may be indicated.
Because healthy horses do not regurgitate under anesthesia, when horses are undergoing intraoral surgery, and for reasons of convenience, not all horses undergo endotracheal intubation during anesthesia. This is particularly true of field anesthesia. When oxygen is available, it is recommended that anesthetized horses be intubated and allowed to breathe oxygen.
MAINTENANCE OF ANESTHESIA
After anesthetic induction and endotracheal intubation, patients that are in a light plane of anesthesia must be brought into surgical anesthesia. When the patient reaches the desired anesthetic depth, general anesthesia is maintained with injectable anesthetics (using TIVA), inhalant anesthetics delivered via an anesthetic machine, or a combination thereof. See Protocol 9-5 for maintenance protocols in horses.
Maintenance with an Inhalant Agent
Maintenance of anesthesia with an inhalant agent is similar to that in a small animal patient, with the exception that sudden unexpected movement can occur without any change in signs of depth. Because of the large breathing circuit volume and patient size, response to changes in inhalant anesthetic and oxygen flow rates occur too slowly to return the patient to surgical anesthesia simply by altering machine settings. A syringe of thiopental or ketamine is typically drawn up before anesthesia and either attached to a three-way stopcock in the fluid administration line or kept close to the IV port for this purpose. Approximately one fifth of the IV induction dose is administered to the horse to return it to surgical anesthesia, which corresponds to 0.4 mg of ketamine per kilogram intravenously or 0.5 mg of thiopental per kilogram intravenously. See Procedure 9-6, p. 281.
Compared with other species, horses are more likely to develop hypoxemia, hypoventilation, and hypotension during maintenance of anesthesia, particularly when inhalant agents are used.
In order to monitor blood pressure more accurately and to obtain arterial blood gas values, it is recommended that horses anesthetized with inhalant anesthetics for procedures lasting longer than 1 hour have an arterial catheter placed in a peripheral artery (facial, transverse facial, dorsal pedal) (Figure 9-10). Blood gas samples should be taken every 30 to 60 minutes, or more frequently if the situation warrants.

FIGURE 9-10 Direct blood pressure monitoring in the anesthetized horse. A, Catheter placed in the facial artery. B, Catheter placed in the transverse facial artery. C, Catheter placed in the dorsal metatarsal artery.
Hypoventilation is so common in anesthetized horses, particularly those placed in dorsal recumbency, that a ventilator is often used to maintain normal ventilation. See Chapter 6 for a discussion of mechanical ventilation.
Hypotension (mean arterial blood pressure <70 mm Hg) has been shown to contribute to myopathy, so treatment with drugs is frequently indicated if increased IV fluid rate, decreased anesthetic depth, and surgical stimulation do not increase blood pressure. The most common drug used to support blood pressure is the positive inotrope dobutamine (commonly administered via a syringe pump). Dobutamine and many other positive inotropes may cause arrhythmias, so it is important to monitor the electrocardiogram (ECG) closely when an infusion is being administered. See Procedure 9-7, p. 281, for preparation and administration of dobutamine.
Hypoxemia, usually defined as a Pao2 lower than 80 mm Hg, can occur in any horse, regardless of the physical status class. It is more common in horses that are obese, are pregnant, have torsed intestines, or are placed in dorsal recumbency. Hypoxemia has several possible causes, including hypoventilation, ventilation-perfusion mismatch, lung disease, and low cardiac output. Wherever possible the cause should be investigated and corrected.
Maintenance with Intravenous Agents (Total Intravenous Anesthesia)
IV maintenance of anesthesia in horses is generally reserved for shorter procedures (less than 1 hour) in healthy patients, and for procedures done away from a veterinary clinic (“field anesthesia”). TIVA is generally characterized by higher blood pressure, less respiratory depression, and more active palpebral reflexes than inhalant anesthesia. When used for procedures lasting less than 1 hour, TIVA is associated with recoveries of good quality.
Anesthesia can be extended by administering additional doses of an alpha2-agonist and ketamine. Typically half the amount of each drug used to sedate and induce anesthesia in the horse is administered intravenously to prolong anesthesia. The mainstay of TIVA in horses is, however, a combination commonly referred to as “triple drip.” As its name suggests, this is a combination of three drugs: guaifenesin, ketamine, and xylazine (or any other alpha2-agonist). Ketamine and xylazine are added to the guaifenesin and infused together to maintain anesthesia (see Procedure 9-8, p. 281, for preparation and administration of “triple drip”).
Maintenance with Injectable and Inhalant Agents
As an alternative, inhalant and injectable agents can be used in combination to maintain anesthesia. In equine anesthesia triple drip can be infused at a very slow rate (with a 10-gtt/mL administration set, 1 drop every 5 to 10 seconds is delivered to an adult horse), which will allow some reduction in the amount of inhalant required as well as providing muscle relaxation and analgesia. Lidocaine or detomidine infusions are also commonly administered to decrease inhalant requirements in horses and to produce analgesia.
PATIENT POSITIONING, COMFORT, AND SAFETY
During anesthetic induction and maintenance, a number of considerations must be observed to ensure that the patient is not harmed. Many of the same principles of small animal anesthesia apply to equine anesthesia (see Chapter 8). Additional concerns are as follows:
• Take care to physically control the head to protect the eyes during gate inductions; horses will tend to fall against the wall or the gate, which leaves their eyes vulnerable to corneal scrapes.
• When hoisting horses, ensure that hobbles are correctly applied so that the horse cannot fall from the hoist or be injured by hobble placement.
• Correct positioning and padding on the surgery table are paramount to prevent neuropathies and myopathies.
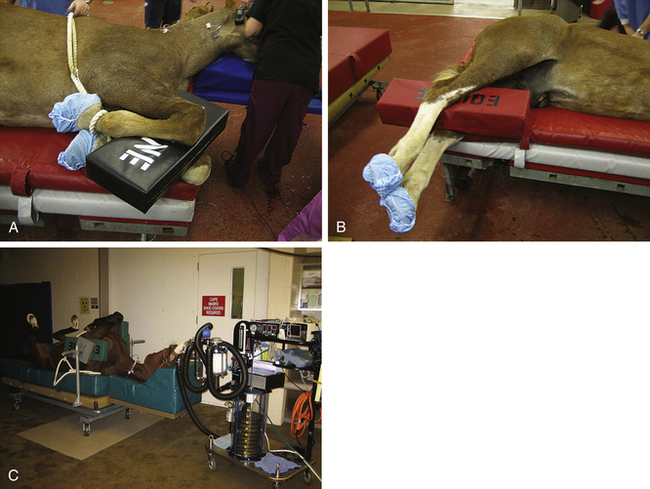
ANESTHETIC RECOVERY
Horses have a psychologic need to stand up shortly after awakening from anesthesia, and it is this that makes recovery particularly dangerous. Some steps can be taken to minimize injury to the horse and anesthetist, but there is a high incidence of complications from anesthetic recovery in horses, and clients should be informed of the risks. In veterinary clinics and hospitals, specific padded areas or rooms are dedicated as recovery stalls. In some clinics the induction stall is also used for recovery. Depending on the facilities and personnel available, horses may be left to recover unassisted after extubation, or may have ropes attached to the halter and tail with which personnel can assist the horse as it attempts to stand (Figure 9-11). Under field conditions the anesthetist typically restrains the horse by kneeling on its neck until the anesthetist believes the horse is ready to make a successful attempt to stand (see later for signs of recovery) (Figure 9-12). Personnel then typically hold the head and tail until the horse is able to stand unassisted.

FIGURE 9-11 Rope placement for assisted recovery in a horse. One rope is attached to the halter, and the other is attached to the tail.

FIGURE 9-12 Anesthetist restraining a horse. The anesthetist can restrain a horse by kneeling on the horse’s neck and lifting the muzzle slightly off the ground. Once the horse is awake enough to “lift” the anesthetist off its neck, the anesthetist may leave the recovery area and allow the horse to make an attempt to stand. This technique is useful in any size horse—in this case, a miniature horse.
Preparation for Recovery
Replace the halter. Place a nasopharyngeal tube before movement if nasal congestion or edema is present (Figure 9-13). On completion of the procedure, turn off the inhalant and transfer the horse to a padded recovery stall, where it can be extubated and monitored. Horses are often placed on thick foam or air mattresses, although a padded floor may also give enough support. If possible, and particularly if the horse was hypoxemic during anesthesia, provide oxygen support using a demand valve (Figure 9-14) or insufflation (5 to 10 L/min nasally or through the endotracheal tube) until the horse is extubated or anesthesia is too light for the horse to tolerate an insufflation hose. A demand valve provides oxygen at a very high flow rate (160 to 280 L/min). An assisted breath can be given as follows: remove the endotracheal tube connector from the tube; connect the demand valve to the endotracheal tube of the intubated horse; and manually depress the button while observing the chest wall (oxygen should flow into the patient’s lungs and expand the chest). Once an adequate chest expansion is observed, release the button and disconnect the demand valve from the endotracheal tube to allow complete exhalation. Insufflation is the passive provision of oxygen: a tube that is able to fit inside the endotracheal tube, nasopharyngeal tube, or nostril is advanced to at least the level of the oropharynx; oxygen flow is set at 10 L/min.

FIGURE 9-13 Nasopharyngeal tube placed for recovery. Through use of the same technique as for nasotracheal tube placement, a nasopharyngeal tube can be placed for recovery and secured to the halter. The tube is gently removed after the horse stands.

FIGURE 9-14 Oxygen demand valve. A, An oxygen demand valve showing A, the demand valve and B, the quick-release connector, which is inserted into the hospital oxygen supply hose. B, Close up view of the demand valve showing A, manual button and B, connector for endotracheal tube. C, Demand valve connected to endotracheal tube (it is usually easier to remove the endotracheal tube connector when the demand valve is used).
If the recovery is to be assisted by ropes, a head rope should be attached to the halter and another rope tied to the tail (see Figure 9-11). See Procedure 9-9, p. 281, for the sequence of events for preparing a horse for recovery.
Monitoring during Recovery
During recovery it is ideal to watch the horse on a continual basis so that it can be assisted or sedated if necessary. While the horse is lying quietly the anesthetist should watch respirations to make sure the horse is breathing normally, take the pulse (facial artery) every 5 to 10 minutes, and assess the eye for depth of anesthesia. The anesthetist stays close to the head of the horse in order to monitor the pulse, to be ready for extubation, and to control the horse if it attempts to stand too soon.
Signs of Recovery
As the patient recovers, it will progress back through the stages and planes of anesthesia. Many horses develop nystagmus during recovery, and rapid nystagmus accompanied by ‘paddling’ of the limbs generally means that a horse will try to get up too soon and will have a ‘rough’ recovery. In this event it may be prudent to sedate the horse with 0.1 to 0.2 mg of xylazine per kilogram intravenously and/or 0.01 to 0.03 mg of acepromazine per kilogram intravenously. Generally, maintaining control of the head by sitting on the neck or holding the head up off the floor will provide some control over the horse. However, once the horse is strong enough to lift an anesthetist off its neck, the anesthetist should retreat to a safe distance to observe the remainder of recovery. Other signs that a horse is recovering and may be close to extubation are chewing, swallowing, and purposeful ear, limb, or tail movement.
Extubation
To prepare the patient for extubation, deflate the cuff by drawing out all the air until the pilot balloon is empty. Both before and after removal, keep the neck in a natural but extended position to protect the airway. Remove the endotracheal tube gently when the swallowing reflex returns, using a slow, steady motion. You may also remove it when signs of imminent arousal are present such as voluntary movement of the limbs or head, movement of the tongue, or chewing. Check to make sure the horse can breathe without obstruction. Horses can breathe only through their noses and will become distressed and compromised if they are unable to. If a nasopharyngeal tube has not been placed and the nasal passages are or become obstructed, one must be placed immediately. In the event that a nasopharyngeal tube does not alleviate the obstruction, a tracheostomy must be performed by the veterinarian, so materials for performing one must be close to the recovery stall at all times.
Standing after Regaining Consciousness
The ideal recovery to standing is one in which the horse, after it is extubated, rolls smoothly from lateral to sternal recumbency. After lying in sternal recumbency for several minutes, the horse ideally makes a coordinated, strong attempt to stand and is successful on its first try. Head and tail ropes are used to assist the horse each time it attempts to stand (Figure 9-15). Unfortunately many horses, particularly those anesthetized for several hours with inhalant anesthesia, do not have ideal recoveries. With experience the anesthetist will learn when it is appropriate to provide additional sedation, analgesia, or physical assistance in the recovery stall to minimize injury to the horse. There is always the possibility that a horse may experience a catastrophic event during recovery, such as a fractured long bone (femur, tibia, humerus, radius). In such an event the VIC should assist the anesthetist in immediately reanesthetizing the horse to assess the situation.
POSTANESTHETIC PERIOD
Once the horse is standing and able to walk steadily, it can be returned to its stall. This can be assessed by walking the horse in a circle inside the recovery stall. Once back in its own stall, the horse should be muzzled for 1 to 3 hours but should have free access to water. The horse should also be observed for any signs of neuropathy (e.g., facial nerve paralysis—drooping eyelid and lip on the affected side; radial nerve paralysis—inability to fully extend affected forelimb), myopathy (hard, swollen muscles, stiff and painful gait), or colic (rolling, kicking at the abdomen) in the postanesthetic period.
KEY POINTS
1. Horses present unique challenges to the anesthetist because of their size, physiology, and temperament. Horses also seem to have a psychologic need to stand after anesthesia, making recovery from anesthesia challenging and potentially dangerous to horse and anesthetist.
2. Horses are susceptible to hypoventilation, nasal congestion, atelectasis, and hypoxemia during general anesthesia.
3. Superficial nerves are susceptible to pressure injury leading to neuropathy, and muscles are prone to injury if blood flow to them is inadequate during anesthesia. Attention must be paid to positioning and padding on the surgery table and in recovery.
4. Standing chemical restraint may be used to perform many surgical and medical procedures in horses, instead of general anesthesia, which is fraught with risks to the patient. The head should be supported in a neutral position in a standing sedated horse in order to minimize nasal congestion.
5. A horse should always be appropriately sedated before induction of general anesthesia.
6. Induction of anesthesia is typically done by injecting a rapid bolus of injectable anesthetic intravenously. This provides a smooth transition from standing to lateral recumbency with minimal risk of injury to the horse and anesthetist.
7. Maintenance of anesthesia in the field and for short procedures (<1 hour in duration) is typically accomplished using total intravenous anesthesia (TIVA). The most common drug combination used for this is a co-infusion of guaifenesin, ketamine, and xylazine, known as “triple drip.”
8. Foals that are easily restrained may be nasotracheally intubated after sedation. The nasotracheal tube can then be attached to an anesthetic machine, and anesthesia can be induced using an inhalant anesthetic.
9. Intubation in equine patients is a blind procedure that is facilitated by extending the horse’s head and neck.
10. Common problems encountered during maintenance of anesthesia are hypoventilation, hypoxemia, and hypotension. These problems are more common when anesthesia is maintained with inhalant anesthetics and in horses positioned in dorsal recumbency.
11. Recovery is the most challenging part of equine anesthesia. Various strategies can be employed to minimize injury to the horse and personnel; however, it is possible for any horse to have a recovery that is not ideal.
12. After general anesthesia horses should be monitored for signs of neuropathy, myopathy, pain, and colic.
REVIEW QUESTIONS
1. Which of the following is true regarding use of standing chemical restraint for performing surgery on a horse?
a. Horses must be endotracheally intubated for standing chemical restraint.
b. Risk of myopathy or neuropathy is higher with standing chemical restraint.
c. The head must be supported in a normal position to avoid nasal congestion.
d. Hypoxemia is a common complication of standing chemical restraint.
2. If a horse becomes excited after it has been premedicated with xylazine intravenously before general anesthesia, the next step the anesthetist should take is to:
a. Allow the horse time to calm down before proceeding
b. Physically restrain the horse using ropes
3. Appropriate positioning and padding of the horse on the surgery table is essential to prevent:
4. What is the main reason for including guaifenesin in an induction protocol in horses?
5. An inhalant induction via nasotracheal tube placement is appropriate for which of the following patients?
a. A 2-year-old Arabian stallion undergoing arthroscopy
b. A 25-year-old thoroughbred mare undergoing sinus surgery
6. Which of the following statements best describes endotracheal intubation in the horse?
a. Intubation is performed blindly with the head and neck extended.
b. Intubation can be performed only with the patient in lateral recumbency.
c. A laryngoscope is useful for visualization of the larynx.
7. The most common complications during maintenance of anesthesia in horses with inhalant anesthetics are:
a. Hypoxemia, hypertension, and bradycardia
b. Hypoxemia, hypotension, and bradycardia
8. Which drug is used to treat hypotension in the anesthetized horse?
9. Of all phases of anesthesia, recovery poses the highest risk to the horse and is the phase over which the anesthetist has the least control.
10. A horse has recovered from anesthesia for arthroscopy and shows the following symptoms: hard, swollen gluteal muscles, stiff gait, and reluctance to walk. The most likely diagnosis is: