Basic Concepts
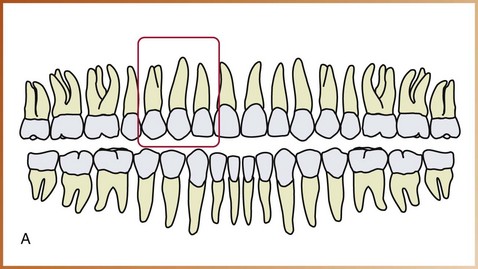
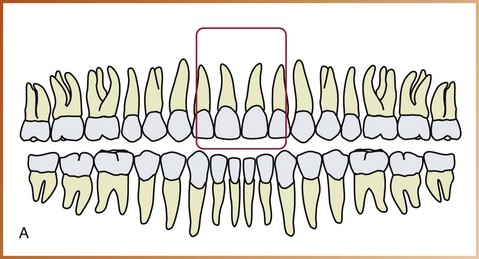
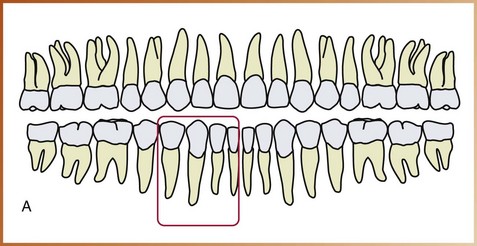
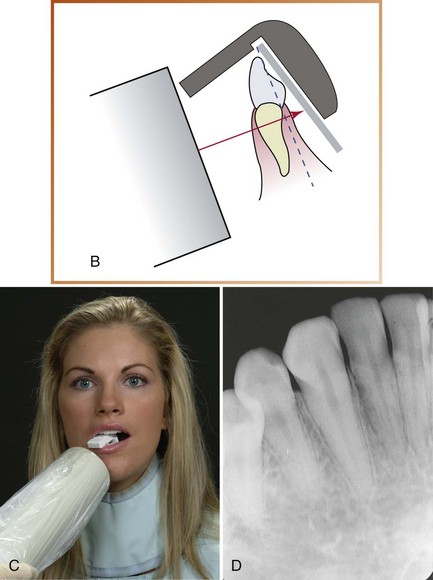
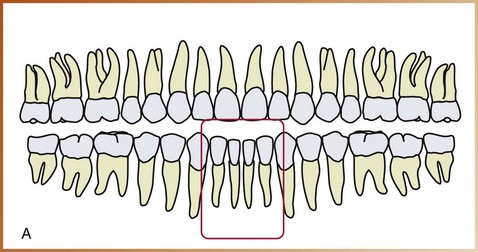
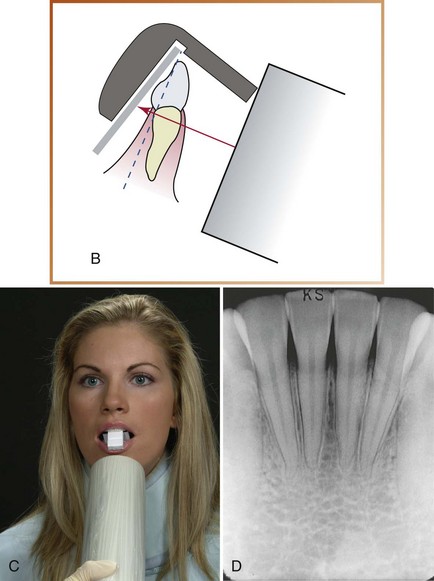
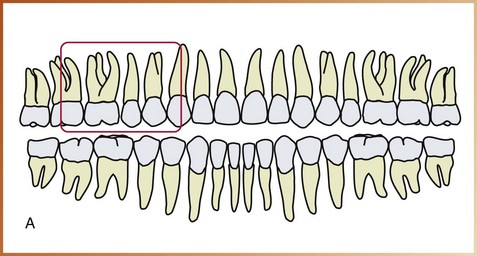
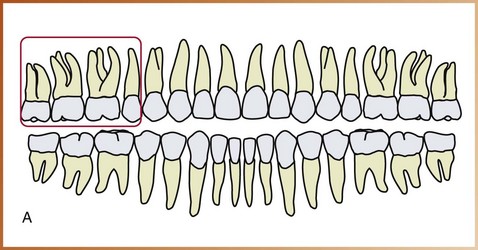
The bisecting technique (also known as the bisecting-angle technique or bisection-of-the-angle technique) is another method that can be used to expose periapical images.
Terminology
An understanding of the following basic terms is necessary before describing the bisecting technique:
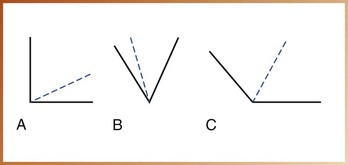
Angle: In geometry, a figure formed by two lines diverging from a common point (Figure 18-1, A).
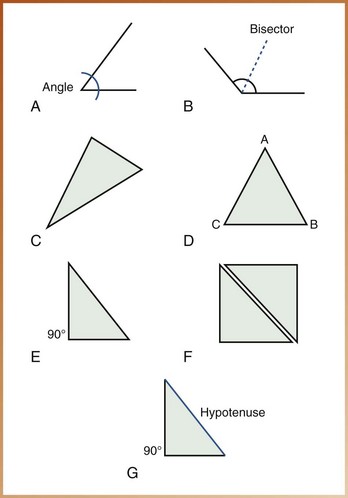
FIGURE 18-1 A, An angle is formed by two lines that diverge from a common point. B, A bisector divides an angle into equal angles. C, A triangle. D, An equilateral triangle has three equal sides (AB = BC = CA). E, A right triangle has one 90-degree angle. F, Congruent triangles are identical. G, The hypotenuse is the side of a right triangle opposite the right angle.
Bisect: To divide into two equal parts (noun, bisector) (Figure 18-1, B).
Triangle: In geometry, a figure formed by connecting three points not in a straight line by three straight-line segments (Figure 18-1, C). A triangle has three angles.
Triangle, equilateral: In geometry, a triangle with three equal sides (Figure 18-1, D).
Triangle, right: In geometry, a triangle with one 90-degree angle (right angle) (Figure 18-1, E).
Triangles, congruent: Triangles that are identical and correspond exactly when superimposed (Figure 18-1, F).
Hypotenuse: In geometry, the side of a right triangle opposite the right angle (Figure 18-1, G).
Isometry: Equality of measurement.
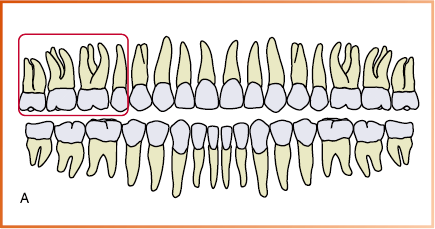
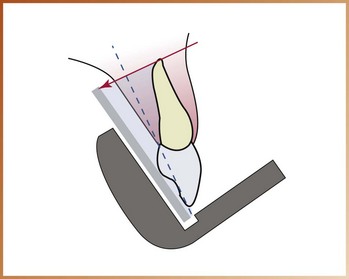
Long axis of the tooth: An imaginary line that divides the tooth longitudinally into two equal halves (Figure 18-2).
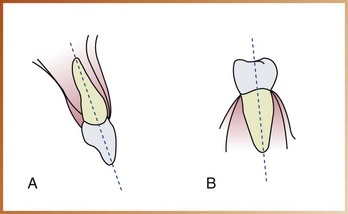
FIGURE 18-2 A, The long axis of the maxillary incisor divides the tooth into two equal halves. B, The long axis of a mandibular premolar divides the tooth into two equal halves.
Central ray: The central portion of the primary beam of x-radiation.
Principles of Bisecting Technique
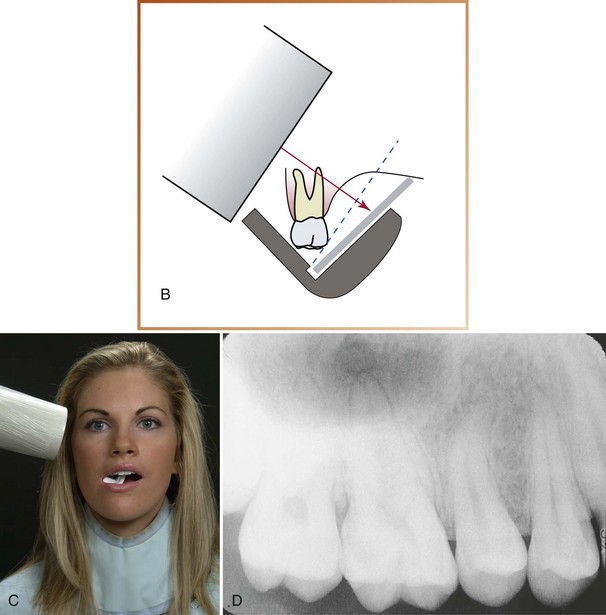
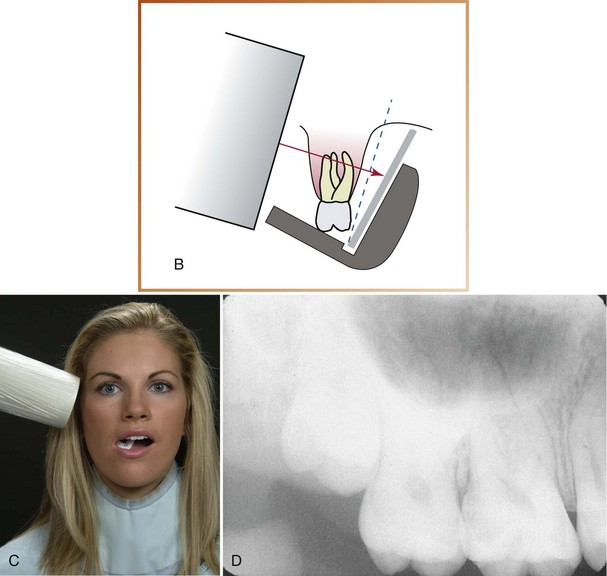
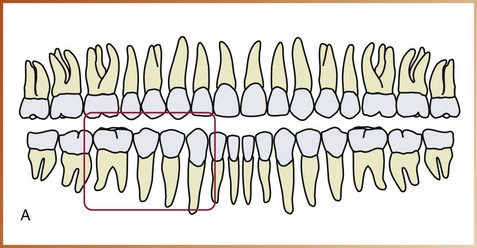
The bisecting technique is based on a simple geometric principle known as the rule of isometry. The rule of isometry states that two triangles are equal if they have two equal angles and share a common side (Figure 18-3). In dental imaging, this geometric principle is applied to the bisecting technique to form two imaginary equal triangles (Figure 18-4). The bisecting technique can be described as follows:
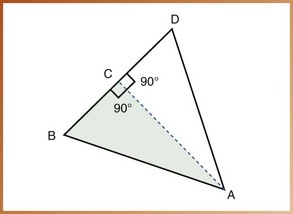
FIGURE 18-3 Angle A is bisected by line AC. Line AC is perpendicular to line BD. Angle BAC is equal to angle DAC. Angle ACB is equal to angle ACD. According to the rule of isometry, triangle BAC (shaded) is equal to triangle DAC.
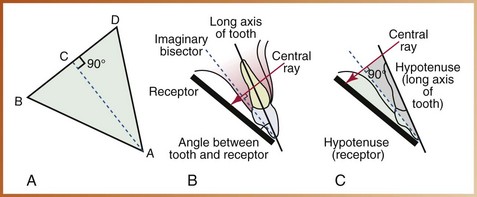
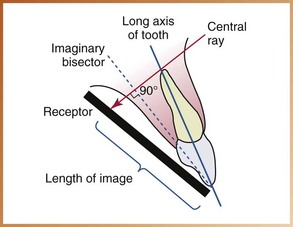
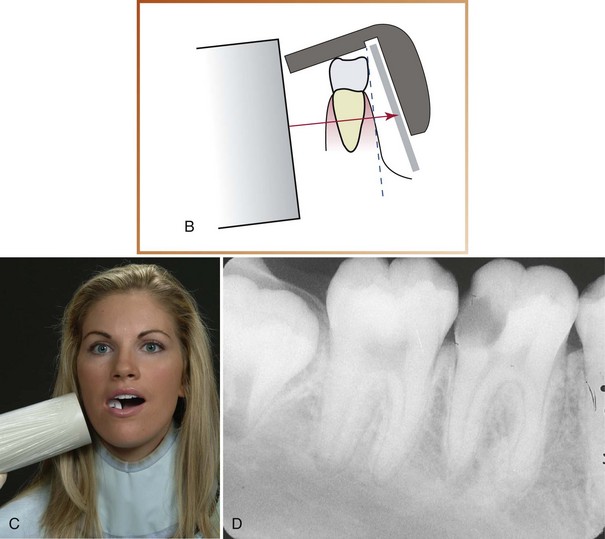
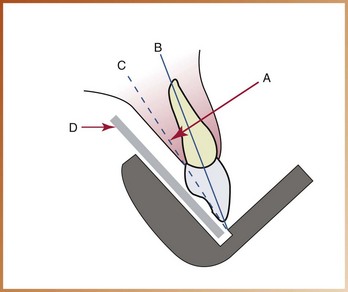
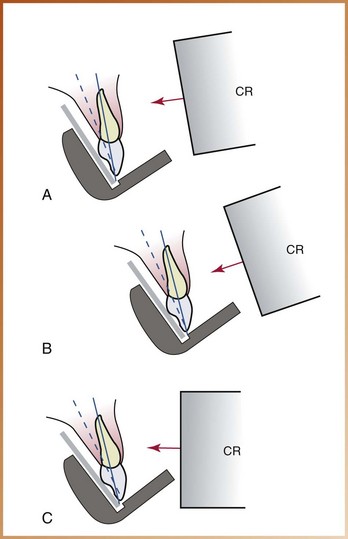
FIGURE 18-4 A, The receptor (line BA) is placed along the lingual surface of the tooth. At the point where the receptor contacts the tooth, the plane of the receptor and the long axis of the tooth (DA) form an angle (BAD). The imaginary bisector divides this angle into two equal angles (BAC and DAC). The central ray (BD) is directed perpendicular to the imaginary bisector and completes the third sides (BC and CD) of the two triangles. B, The central ray is directed at a right angle to the imaginary bisector. C, The two imaginary triangles that result are right triangles and congruent. The hypotenuse of each triangle is represented by the long axis of the tooth and the plane of the receptor.
1. The receptor must be placed along the lingual surface of the tooth.
2. At the point where the receptor contacts the tooth, the plane of the receptor and the long axis of the tooth form an angle.
3. The dental radiographer must visualize a plane that divides in half, or bisects, the angle formed by the receptor and the long axis of the tooth. This plane is termed the imaginary bisector. The imaginary bisector creates two equal angles and provides a common side for the two imaginary equal triangles.
4. The dental radiographer must then direct the central ray of the x-ray beam perpendicular to the imaginary bisector. When the central ray is directed at an angle of 90 degrees to the imaginary bisector, two imaginary equal triangles are formed.
5. The two imaginary triangles that result are right triangles and are congruent. The hypotenuse of one imaginary triangle is represented by the long axis of the tooth; the other hypotenuse is represented by the plane of the receptor.
When the rule of isometry is followed strictly, the dental image of the tooth will be accurate. When the angle formed by the plane of the receptor and the long axis of the tooth is bisected, and the x-ray beam is directed at a right angle to the imaginary bisector, the actual tooth and the dental image of the tooth will be of the same length (Figure 18-5).
Receptor Stabilization
In the bisecting technique, beam alignment devices may be used to position and stabilize the receptor.
Beam Alignment Devices
Beam alignment devices are used to position an intraoral receptor in the mouth and maintain it in position during exposure (see Chapter 6). Examples of commercially available intraoral beam alignment devices that can be used with the bisecting technique include the following:
• Rinn BAI instruments (Dentsply, Rinn Corporation, Elgin, IL). The bisecting angle instrument (BAI) includes plastic bite-blocks, plastic aiming rings, and metal indicator arms. To reduce the amount of radiation received by the patient, snap-on ring collimators can be added to the plastic aiming rings. BAIs have been designed to aid in the determination of horizontal and vertical angulations, minimize distortion from film bending, and prevent cone-cuts (Figure 18-6, A).
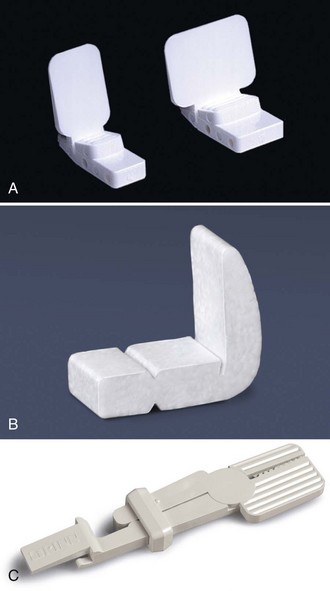
FIGURE 18-6 A, Rinn bisecting angle bite-blocks used with the bisecting technique. B, Stabe disposable film holders (bite-blocks). C, EEZEE-Grip (Snap-A-Ray) intraoral receptor holder.
• Stabe bite-block (Rinn). This device can be used with the paralleling technique or the bisecting technique. For use with the bisecting technique, the scored front section is removed, and the receptor is placed as close to the teeth as possible (Figure 18-6, B).
• EEZEE-Grip receptor holder (Rinn). Formerly known as Snap-A-Ray, this device is used to stabilize a receptor in either the paralleling technique or the bisecting technique (Figure 18-6, C).
The Stabe bite-block is disposable and is designed for one-time use only. BAIs and the EEZEE-Grip film holder are reusable and must be sterilized after each use.
BAIs with collimators are the recommended devices for the bisecting technique because (1) aiming rings are included that aid in the alignment of the position-indicating device (PID), and (2) collimators significantly reduce the amount of patient exposure to x-radiation. BAIs are simple to assemble and position. For information about the use of BAIs or other devices available for the bisecting technique, the dental radiographer should refer to the manufacturer’s instructions.
Receptors Used in Bisecting Technique
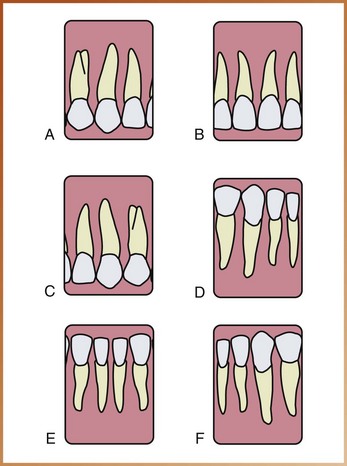
Traditionally, a size 2 intraoral receptor is used with the bisecting technique. In the anterior regions, a size 2 receptor is always placed with the long portion of the receptor in a vertical (upright) direction. In the posterior regions, a size 2 receptor is always placed with the long portion of the receptor in a horizontal (sideways) direction.
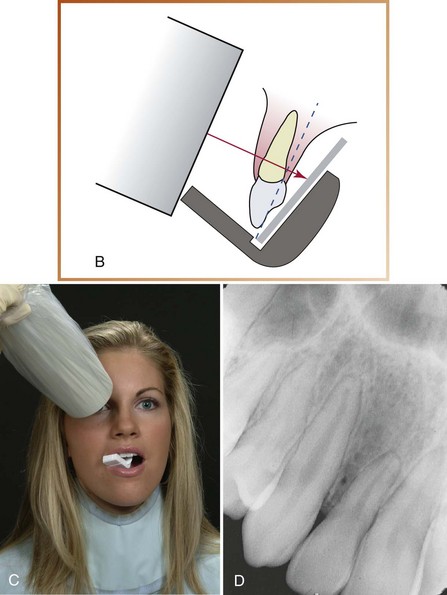
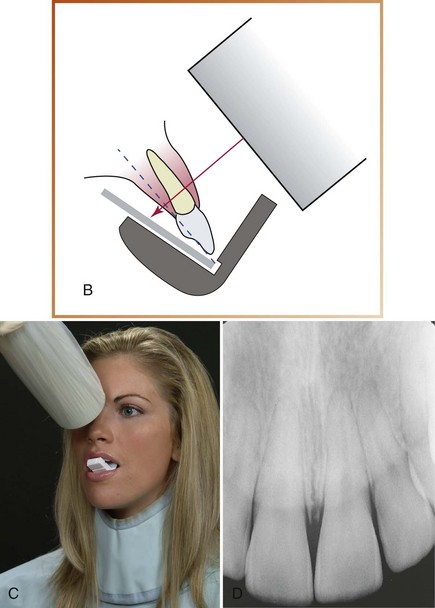
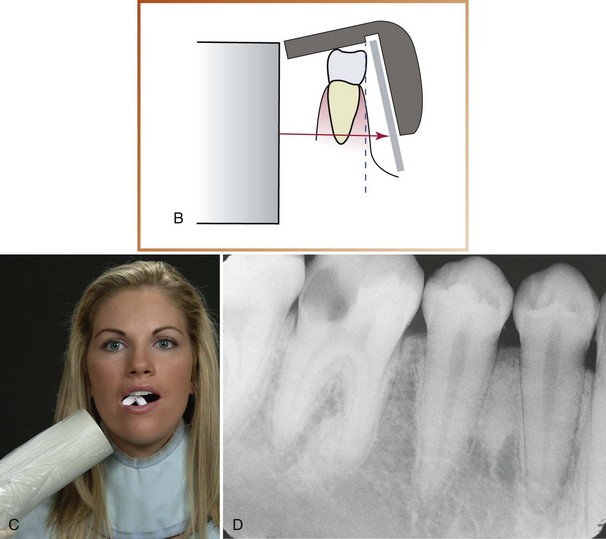
Position-Indicating Device Angulation
In the bisecting technique, the angulation of the PID is critical. Angulation is a term used to describe the alignment of the central ray of the x-ray beam in horizontal and vertical planes. Angulation can be varied by moving the PID in either a horizontal direction or a vertical direction. The use of BAIs with aiming rings dictates the proper PID angulation. However, when a bite-block or other device without an aiming ring is employed, the dental radiographer must determine both horizontal and vertical angulations.
Horizontal Angulation
Horizontal angulation refers to the positioning of the PID and the direction of the central ray in a horizontal, or side-to-side, plane (Figure 18-7). The horizontal angulation does not differ according to the technique used; paralleling, bisecting, and bite-wing techniques all use the same principles of horizontal angulation.
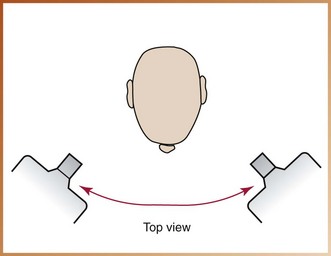
FIGURE 18-7 Horizontal angulation of the position-indicating device (PID) refers to PID placement in a side-to-side (ear-to-ear) direction. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
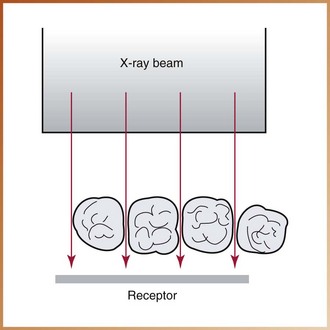
Correct Horizontal Angulation: With correct horizontal angulation, the central ray is directed perpendicular to the curvature of the arch and through the contact areas of the teeth (Figure 18-8). As a result, the contact areas on the dental image appear “opened.”
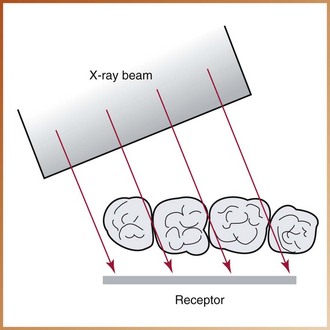
Incorrect Horizontal Angulation: Incorrect horizontal angulation results in overlapped (“unopened”) contact areas (Figure 18-9). An image with overlapped interproximal contact areas cannot be used to examine the interproximal areas of the teeth and is thus nondiagnostic (Figure 18-10).
Vertical Angulation
Vertical angulation refers to the positioning of the PID in a vertical, or up-and-down, plane (Figure 18-11). Vertical angulation is measured in degrees and is registered on the outside of the tubehead. The vertical angulation differs according to the imaging technique used, as follows:
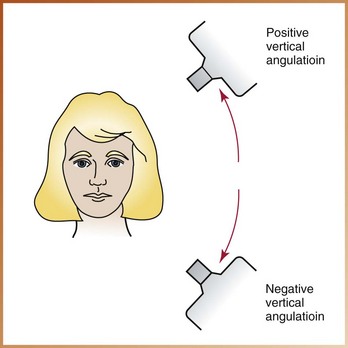
FIGURE 18-11 Vertical angulation of the position-indicating device (PID) refers to PID placement in an up-and-down (head-to-toe) direction. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
• With the paralleling technique, the vertical angulation of the central ray is directed perpendicular to the receptor and the long axis of the tooth (see Chapter 17).
• With the bisecting technique, the vertical angulation is determined by the imaginary bisector; the central ray is directed perpendicular to the imaginary bisector.
• With the bite-wing technique, the vertical angulation is predetermined; the central ray is directed at +10 degrees to the occlusal plane (see Chapter 19).
Correct Vertical Angulation: Correct vertical angulation results in a dental image that is of the same length as that of the tooth. Table 18-1 lists recommended vertical angulation ranges for the bisecting technique.
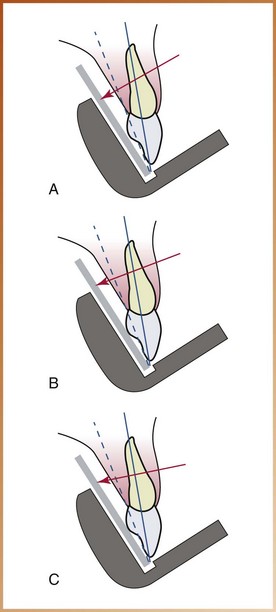
Incorrect Vertical Angulation: Incorrect vertical angulation results in a radiographic image that is not of the same length as that of the tooth; instead, the image appears longer or shorter. Elongated or foreshortened images are not diagnostic.
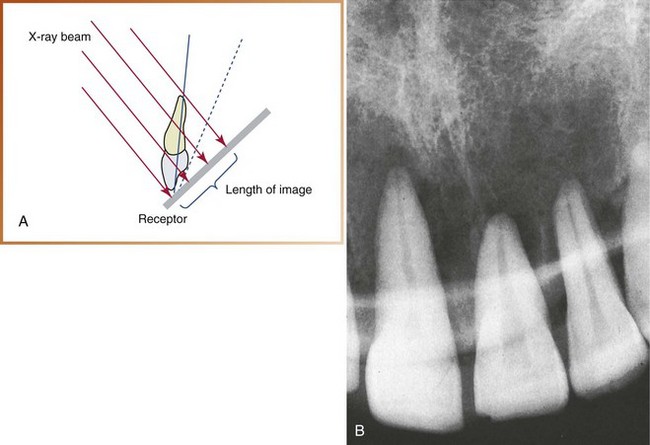
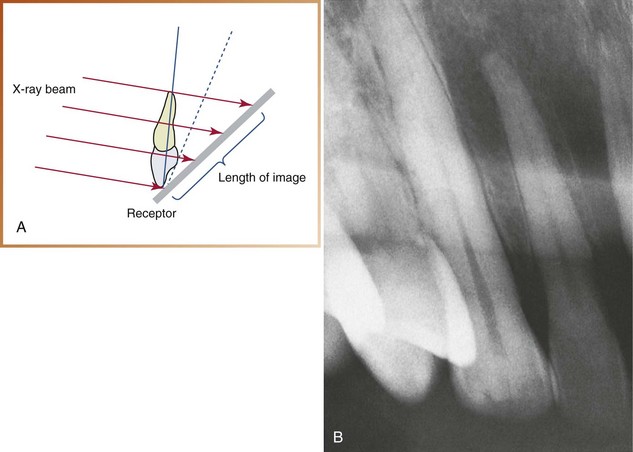
Foreshortened Images: Foreshortened images refer to radiographic images that appear shortened. Foreshortening of images results from excessive vertical angulation. When the vertical angulation is too steep, the image of the tooth appears shorter than the actual tooth (Figure 18-12). Foreshortening also occurs if the central ray is directed perpendicular to the plane of the receptor rather than to the imaginary bisector.
Elongated Images: Elongated images refer to images of the teeth that appear too long. Elongation of images results from insufficient vertical angulation. When the vertical angulation is too flat, the image of the tooth appears longer than the actual tooth (Figure 18-13). Elongation also occurs if the central ray is directed perpendicular to the long axis of the tooth rather than to the imaginary bisector.
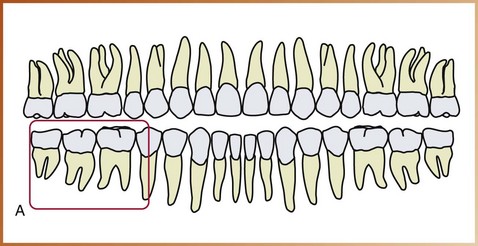
Rules of Bisecting Technique
Five basic rules should be followed when using the bisecting technique.
1. Receptor placement. The receptor must be positioned to cover the prescribed area of the tooth to be examined. Specific placements are described in the procedures.
2. Receptor position. The receptor must be placed against the lingual surface of the tooth. The occlusal end of the receptor must extend approximately one eighth of an inch beyond the incisal or occlusal surfaces (Figure 18-14). The apical end of the receptor must rest against the palatal or alveolar tissues.
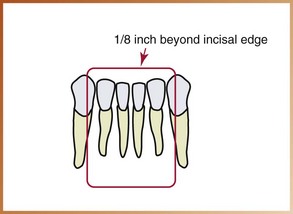
FIGURE 18-14 Approximately one eighth of an inch of the receptor must appear beyond the incisal edges of the teeth.
3. Vertical angulation. The central ray of the x-ray beam must be directed perpendicular (at a right angle) to the imaginary bisector that divides the angle formed by the receptor and the long axis of the tooth.
4. Horizontal angulation. The central ray of the x-ray beam must be directed through the contact areas between teeth.
5. Receptor exposure. The x-ray beam must be centered on the receptor to ensure that all areas of the receptor are exposed. Failure to center the x-ray beam results in a partial image or a cone-cut.