Imaging of Patients with Special Needs
After completion of this chapter, the student will be able to do the following:
• Define the key terms associated with patients who have special needs
• List the areas of the oral cavity that are most likely to elicit the gag reflex when stimulated
• List two precipitating factors responsible for initiating the gag reflex
• Describe how to control the gag reflex using operator attitude, patient and equipment preparations, exposure sequencing, and receptor placement and technique
• Describe common physical disabilities and what modifications in technique may be necessary during the imaging examination
• Describe common developmental disabilities and what modifications in technique may be necessary during the imaging examination
• List helpful hints that can be used when treating a person with a disability
• Describe the prescribing of dental images, patient and equipment preparations, recommended techniques, and patient management as they pertain to the pediatric dental patient
• Describe the use of receptor placement modifications, and recommended periapical technique during root canal procedures
• Describe the purposes of the imaging examination in the edentulous patient
• List and describe the three types of imaging examination that may be used for the edentulous patient
Not all dental imaging techniques can be successfully performed on all patients. Imaging examination techniques must often be modified to accommodate patients with special needs. The dental radiographer must be competent in altering the techniques to meet the specific diagnostic needs of individual patients.
The purpose of this chapter is to introduce the dental radiographer to the issues in dealing with patients with special needs. In addition, this chapter provides specific information on how to manage patients with a hypersensitive gag reflex, patients with physical or developmental disabilities, pediatric patients, endodontic patients, and edentulous patients.
Patients with Gag Reflex
The term gagging (also called retching) refers to the strong, involuntary effort to vomit. The gag reflex (also called the pharyngeal reflex) can be defined as retching that is elicited by stimulation of the sensitive tissues of the soft palate region. The gag reflex is a protective mechanism of the body that serves to clear the airway of obstruction. All patients have gag reflexes, although some are more sensitive than others. In dental imaging, a hypersensitive gag reflex is a problem that is commonly encountered.
The areas that are most likely to elicit the gag reflex when stimulated include the soft palate and the lateral posterior third of the tongue. Before the gag reflex is initiated, the following two reactions occur:
Precipitating factors for the initiation of the gag reflex include psychogenic stimuli (stimuli originating in the mind) and tactile stimuli (stimuli originating from touch). To suppress the gag reflex, the dental radiographer must eliminate or lessen these precipitating factors.
Patient Management
To effectively manage the patient with a hypersensitive gag reflex, the dental radiographer must be aware of the following:
Operator Attitude
To prevent the gag reflex, the dental radiographer must convey a confident attitude. The patient must be confident of the radiographer’s ability to perform imaging procedures and must be sure that the receptor will not slip and lodge in the throat. If the dental radiographer does not appear to be in complete control of the procedures, the patient interprets this as a lack of confidence. This lack of confidence may act as a psychogenic stimulus and elicit the gag reflex.
In addition, the dental radiographer must also convey patience, tolerance, and understanding. Every effort should be made to relax and reassure the patient with a hypersensitive gag reflex. The dental radiographer should explain the imaging procedures about to be performed and then compliment the patient as each exposure is completed. As the patient becomes comfortable with the imaging procedures, he or she becomes more confident and, as a result, is less likely to gag.
Patient and Equipment Preparations
Patient and equipment preparations can help prevent the gag reflex (see Chapters 17, 18, and 19). In the patient with a hypersensitive gag reflex, every effort should be made to limit the amount of time that a receptor remains in the mouth. The longer a receptor stays in the mouth, the more likely the patient is to gag. When patient and equipment preparations are completed before receptor placement, valuable time is saved, and the likelihood of stimulating the gag reflex is reduced.
Exposure Sequencing
Exposure sequencing plays an important role in preventing the gag reflex. As discussed in Chapters 17 to 19 , the dental radiographer should always begin with anterior exposures. Anterior receptors are easier for the patient to tolerate and are less likely to elicit the gag reflex. With posterior receptor placements, the dental radiographer should always expose the premolar receptor before the molar receptor. Of all receptor placements, the maxillary molar receptor is the most likely to elicit the gag reflex. In the patient with a hypersensitive gag reflex, the exposure sequence should be altered so that the maxillary molar receptors are exposed last.
Receptor Placement and Technique
Receptor placement and technique also play an important role in preventing the gag reflex. To avoid stimulating the gag reflex, each receptor must be placed and exposed as quickly as possible. Placement and technique modifications include the following:
• Avoid the palate. When placing receptors in the maxillary posterior areas, do not slide the receptor along the palate. Sliding the receptor along the palate stimulates this sensitive area and causes the gag reflex. Instead, position the receptor lingual to the teeth, and then firmly bring the receptor into contact with the palatal tissues using one decisive motion.
• Demonstrate receptor placement. In the areas that are most likely to elicit the gag reflex, rub a finger along the tissues near the intended area of receptor placement while telling the patient, “This is where the receptor will be positioned.” Then place the receptor quickly. This technique demonstrates where the receptor will be placed and desensitizes the tissues in the area.
Extreme Cases of Gag Reflex
Occasionally the dental radiographer encounters a patient with a gag reflex that is uncontrollable. In such a patient, intraoral images are impossible to obtain. Instead, the dental radiographer must resort to extraoral images such as panoramic or lateral jaw images to obtain diagnostic information.
Helpful Hints
 NEVER suggest gagging. The dental radiographer must never bring up the subject of gagging or ask the patient such questions as “Are you a gagger?” or “Do you gag?” The power of suggestion can act as a strong psychogenic stimulus and can, in turn, elicit the gag reflex. When the patient brings up the subject of gagging, the dental radiographer must refrain from using the terms gag, gagging, and gagger; instead, the radiographer should refer to the gag reflex as “a tickle in the back of the throat” when discussing the topic with the patient.
NEVER suggest gagging. The dental radiographer must never bring up the subject of gagging or ask the patient such questions as “Are you a gagger?” or “Do you gag?” The power of suggestion can act as a strong psychogenic stimulus and can, in turn, elicit the gag reflex. When the patient brings up the subject of gagging, the dental radiographer must refrain from using the terms gag, gagging, and gagger; instead, the radiographer should refer to the gag reflex as “a tickle in the back of the throat” when discussing the topic with the patient.
 DO reassure the patient. If the patient gags, the dental radiographer must remove the receptor as quickly as possible and then reassure the patient. The patient with a hypersensitive gag reflex must be reassured that such a response is not unusual. Some patients are very embarrassed, and others may even cry. The dental radiographer must always maintain control of the situation while remaining calm and understanding.
DO reassure the patient. If the patient gags, the dental radiographer must remove the receptor as quickly as possible and then reassure the patient. The patient with a hypersensitive gag reflex must be reassured that such a response is not unusual. Some patients are very embarrassed, and others may even cry. The dental radiographer must always maintain control of the situation while remaining calm and understanding.
 DO suggest deep breathing. The dental radiographer should instruct the patient to “breathe deeply” through the nose during receptor placement and exposure. The breathing should be audible, and the dental radiographer should demonstrate it to the patient. As previously stated, respiration must cease for the gag reflex to occur; therefore, if the patient maintains breathing, the gag reflex cannot occur.
DO suggest deep breathing. The dental radiographer should instruct the patient to “breathe deeply” through the nose during receptor placement and exposure. The breathing should be audible, and the dental radiographer should demonstrate it to the patient. As previously stated, respiration must cease for the gag reflex to occur; therefore, if the patient maintains breathing, the gag reflex cannot occur.
 DO try to distract the patient. Distraction often helps suppress the gag reflex. The dental radiographer can instruct the patient to do one of the following during receptor placement and exposure: (1) bite as hard as possible on the bite-block or the tab or (2) position a leg or arm in the air. These acts help divert the patient’s attention and lessen the likelihood of the gag reflex being elicited.
DO try to distract the patient. Distraction often helps suppress the gag reflex. The dental radiographer can instruct the patient to do one of the following during receptor placement and exposure: (1) bite as hard as possible on the bite-block or the tab or (2) position a leg or arm in the air. These acts help divert the patient’s attention and lessen the likelihood of the gag reflex being elicited.
 DO try to reduce tactile stimuli. Reducing tactile stimuli helps prevent the gag reflex. The dental radiographer can try one of the following techniques before placing and exposing the receptor: (1) giving the patient a cup of ice water to drink or (2) placing a small amount of ordinary table salt on the tip of the tongue. These techniques help confuse the sensory nerve endings and lessen the likelihood of the gag reflex being stimulated.
DO try to reduce tactile stimuli. Reducing tactile stimuli helps prevent the gag reflex. The dental radiographer can try one of the following techniques before placing and exposing the receptor: (1) giving the patient a cup of ice water to drink or (2) placing a small amount of ordinary table salt on the tip of the tongue. These techniques help confuse the sensory nerve endings and lessen the likelihood of the gag reflex being stimulated.
 DO use a topical anesthetic. In the patient with a severe hypersensitive gag reflex, a topical anesthetic spray may be used. The spray is used to numb the areas that elicit the gag reflex. The dental radiographer should instruct the patient to exhale while the anesthetic is sprayed on the soft palate and posterior tongue. Caution must be used to ensure that the patient does not inhale the spray, which may cause inflammation of the lungs. The topical anesthetic spray takes effect after 1 minute and lasts for approximately 20 minutes. Topical anesthetic sprays should not be used in patients who are allergic to benzocaine.
DO use a topical anesthetic. In the patient with a severe hypersensitive gag reflex, a topical anesthetic spray may be used. The spray is used to numb the areas that elicit the gag reflex. The dental radiographer should instruct the patient to exhale while the anesthetic is sprayed on the soft palate and posterior tongue. Caution must be used to ensure that the patient does not inhale the spray, which may cause inflammation of the lungs. The topical anesthetic spray takes effect after 1 minute and lasts for approximately 20 minutes. Topical anesthetic sprays should not be used in patients who are allergic to benzocaine.
Patients with Disabilities
A disability can be defined as a “physical or mental impairment that substantially limits one or more of an individual’s major life activities.” In the dental office, persons with both physical and developmental disabilities are encountered. The dental radiographer must be prepared to modify imaging techniques to accommodate persons with disabilities.
Physical Disabilities
A person with a physical disability may have problems with vision, hearing, or mobility. The dental radiographer must make every effort to meet the individual needs of such patients. The person with a physical disability often is accompanied to the dental office by a family member or other caregiver. Caregivers can be asked to assist the dental radiographer with communication or with the patient’s physical needs. The dental radiographer must be aware of the common physical disabilities involving vision, hearing, and mobility and the necessary modifications to the procedure for patients who have such problems.
Vision Impairment
If a person is blind or visually impaired, the dental radiographer must communicate using clear verbal explanations. The dental radiographer must keep the patient informed of what is being done and explain each step of the procedure before performing it. The dental radiographer must never gesture to another person in the presence of a person who is blind. Blind persons are sensitive to this type of communication and perceive this as the dental radiographer “talking behind their backs.”
Hearing Impairment
With regard to a person is deaf or hearing impaired, the dental radiographer has several options. The radiographer may ask the caregiver to act as an interpreter, use gestures or sign language, or use written instructions. When the patient can read lips, the dental radiographer must face the patient and speak clearly and slowly.
Mobility Impairment
If a person is in a wheelchair and does not have use of the lower limbs, the dental radiographer should initially ask the patient how he or she would prefer to transfer to the dental chair. The dental radiographer may offer to assist the patient in transferring to the dental chair or ask the caregiver to assist in the transfer. If a transfer is not possible, the dental radiographer may attempt to perform the necessary imaging procedures with the patient seated in the wheelchair.
If a person does not have use of the upper limbs and a beam alignment device cannot be used to stabilize receptor placement, the dental radiographer may ask the caregiver to assist with the holding of the receptor. In such cases, the caregiver must wear a lead apron and thyroid collar during exposure of the receptors. In addition, the caregiver must be given specific instructions on how to hold the receptor for the patient. As stated in previous chapters, the dental radiographer must never hold a receptor for a patient during an x-ray exposure.
Developmental Disabilities
A developmental disability is “a substantial impairment of mental or physical functioning that occurs before the age of 22 and is of indefinite duration.” Examples include autism, cerebral palsy, epilepsy and other neuropathies, and mental retardation. The dental radiographer must make every effort to meet the individual needs of the patient with a developmental disability.
A person with a developmental disability may have problems with coordination or with comprehension of instructions. As a result, the dental radiographer may experience difficulties in obtaining intraoral images. If coordination is a problem, mild sedation may be useful. If comprehension is a problem, the caregiver may be asked to assist with the holding of the receptor.
It is important that the dental radiographer recognize situations in which the patient cannot tolerate intraoral exposures. In such cases, no intraoral exposures must be done; such exposures result only in nondiagnostic images and needless radiation exposure of the patient. In these patients, extraoral exposures (e.g., lateral jaw and panoramic) may be used.
Helpful Hints
For treating a patient with a disability:
 DO NOT ask personal questions about a disability; such questions are inappropriate in the dental setting.
DO NOT ask personal questions about a disability; such questions are inappropriate in the dental setting.
 DO offer assistance to a person with a disability. For example, offer to push a wheelchair or to guide a person who is blind. The person with a disability will indicate whether help is needed or not and is often specific about how the assistance should be provided. For example, a person who is blind may prefer to hold the arm of a person offering guidance rather than having an arm held.
DO offer assistance to a person with a disability. For example, offer to push a wheelchair or to guide a person who is blind. The person with a disability will indicate whether help is needed or not and is often specific about how the assistance should be provided. For example, a person who is blind may prefer to hold the arm of a person offering guidance rather than having an arm held.
 DO talk directly to the person with a disability. It is inappropriate to talk to the caregiver instead of talking to the patient; for example, instead of asking the caretaker, “Can he [or she] transfer out of the wheelchair?” the radiographer should speak directly to the patient in the wheelchair. In addition, it is inappropriate to talk to the caregiver about a person with a disability as if that person were not present; the same is also true when an interpreter accompanies a deaf person.
DO talk directly to the person with a disability. It is inappropriate to talk to the caregiver instead of talking to the patient; for example, instead of asking the caretaker, “Can he [or she] transfer out of the wheelchair?” the radiographer should speak directly to the patient in the wheelchair. In addition, it is inappropriate to talk to the caregiver about a person with a disability as if that person were not present; the same is also true when an interpreter accompanies a deaf person.
Patients with Specific Dental Needs
Different patients have different diagnostic dental requirements based on specific needs. Dental imaging examination techniques must often be modified to accommodate patients with specific dental needs, including pediatric, endodontic, and edentulous patients.
Pediatric Patients
A pediatric patient is a child; the term pediatric is derived from the Greek word pedia meaning child. Pediatrics is the branch of dentistry dealing with the diagnosis and treatment of dental diseases in children. In children, dental images are useful for detecting lesions as well as conditions of teeth and bones, for showing changes secondary to caries and trauma, and for evaluating growth and development. When treating pediatric patients, the dental radiographer must be aware of the following:
Prescribing of Dental Images
As described in Chapter 5, the prescribing of dental images is based on individual needs of patients. The Guidelines for Prescribing Dental Radiographs include recommendations for both children and adults (see Table 5-1). For the pediatric patient, the prescribed number and type of dental images depend not only on the individual needs of the child but also on the age of the child and his or her ability to cooperate during the procedures.
Patient and Equipment Preparations
Patient and equipment preparations for the pediatric patient are identical to those described for the adult patient (see Chapters 17 to 19). With the pediatric patient, however, special attention must be devoted to the following preparations:
• Explanation of procedure. The imaging procedures that are to be performed must be explained to the child in terms that are easily understood by the child. For example, the dental radiographer can refer to the tubehead as a “camera,” the lead apron as a “coat,” and the image as a “picture.”
• Lead apron. The growing tissues of a child are particularly vulnerable to the effects of ionizing radiation and must be protected. As a result, a lead apron and thyroid collar must be placed on a child before radiographic exposure.
• Exposure factors. Exposure factors (milliamperage, kilovoltage, time) must be reduced because of the size of the pediatric patient. A reduced exposure time is preferred; the shorter exposure time will reduce the chance of a blurred image should the child move. All exposure factors should be set according to the recommendations of the receptor manufacturer.
• Receptor size. As described in Chapter 7, size 0 receptor is recommended for use in the pediatric patient with a primary dentition because of the small mouth size. In the child with a transitional dentition, size 1 or 2 receptor is recommended. As described in Chapter 21, a size 2 receptor is preferred for maxillary and mandibular occlusal exposures in children.
Recommended Techniques
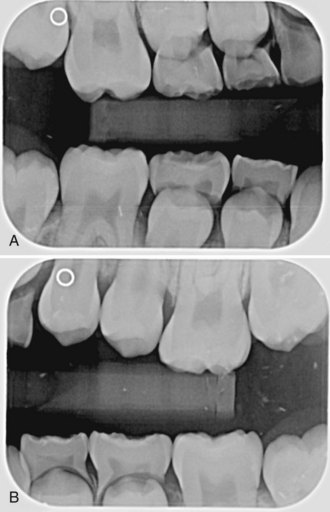
The techniques used to expose intraoral projections in pediatric patients are basically the same as those used in adults. With periapical projections, either the bisecting technique or the paralleling technique can be used (see Chapters 17 and 18 ). In children with primary or transitional dentition, the bisecting technique is preferred because the small size of the mouth precludes the placement of a receptor beyond the apical regions of teeth. The bite-wing and occlusal techniques are also used in pediatric patients (see Chapters 19 and 21). Typical examinations of primary and transitional dentitions using these techniques are described in Table 24-1. Figures 24-1 through 24-5 provide examples of occlusal, bite-wing, and panoramic pediatric dental images.
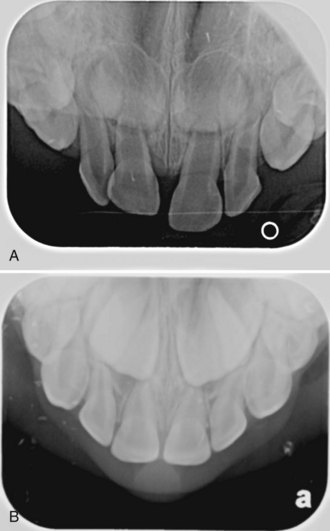
FIGURE 24-1 A & B, Examples of maxillary pediatric occlusal projections, each patient exposed with size 2 intraoral receptors. (Courtesy of Cary Pediatric Dentistry, Cary, NC.)
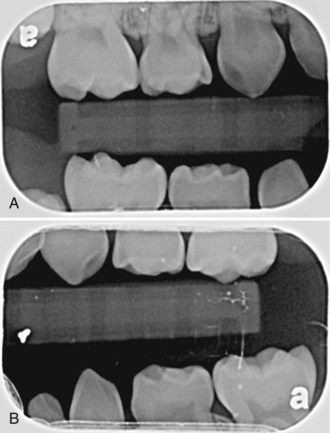
FIGURE 24-2 A & B, Right and left bite-wing images from a 5-year-old patient. (Courtesy of Cary Pediatric Dentistry, Cary, NC.)
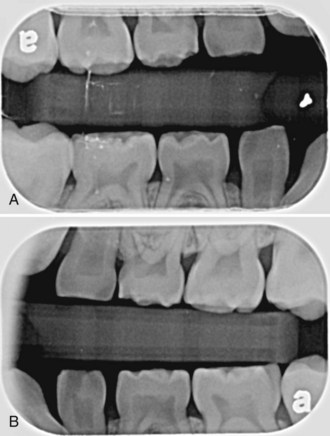
FIGURE 24-3 A & B, Right and left bite-wing images from a  -year-old patient. (Courtesy of Cary Pediatric Dentistry, Cary, NC.)
-year-old patient. (Courtesy of Cary Pediatric Dentistry, Cary, NC.)
Helpful Hints
For managing a pediatric patient:
 BE CONFIDENT. Most children react favorably to the authority of a confident and capable operator. The dental radiographer must secure the child’s confidence, trust, and cooperation. In addition, the dental radiographer must be patient and must not rush the imaging procedures.
BE CONFIDENT. Most children react favorably to the authority of a confident and capable operator. The dental radiographer must secure the child’s confidence, trust, and cooperation. In addition, the dental radiographer must be patient and must not rush the imaging procedures.
 SHOW AND TELL. The typical child is curious. The dental radiographer can use a “show and tell” approach to prepare the patient for imaging procedures. Before beginning any exposures, the dental radiographer can show the child the equipment and materials that will be used and then describe to the child what will happen. The child should be encouraged to touch the tubehead, receptor, beam alignment device, and lead apron.
SHOW AND TELL. The typical child is curious. The dental radiographer can use a “show and tell” approach to prepare the patient for imaging procedures. Before beginning any exposures, the dental radiographer can show the child the equipment and materials that will be used and then describe to the child what will happen. The child should be encouraged to touch the tubehead, receptor, beam alignment device, and lead apron.
 REASSURE THE PATIENT. The typical child has a fear of the unknown. Because a frightened child is not cooperative, the dental radiographer must reassure the child and allay any fears about the procedures.
REASSURE THE PATIENT. The typical child has a fear of the unknown. Because a frightened child is not cooperative, the dental radiographer must reassure the child and allay any fears about the procedures.
 DEMONSTRATE BEHAVIOR. With the pediatric patient, the dental radiographer can demonstrate the desired behavior to show the child exactly what to do. For example, the radiographer can demonstrate “how to hold still” and then ask the child to do the same thing.
DEMONSTRATE BEHAVIOR. With the pediatric patient, the dental radiographer can demonstrate the desired behavior to show the child exactly what to do. For example, the radiographer can demonstrate “how to hold still” and then ask the child to do the same thing.
 REQUEST ASSISTANCE. If a child cannot hold still or stabilize the receptor, the dental radiographer can ask the parent or accompanying adult to provide assistance. The adult should wear a lead apron and thyroid collar and hold the receptor or the child during the x-ray exposure.
REQUEST ASSISTANCE. If a child cannot hold still or stabilize the receptor, the dental radiographer can ask the parent or accompanying adult to provide assistance. The adult should wear a lead apron and thyroid collar and hold the receptor or the child during the x-ray exposure.
 POSTPONE THE EXAMINATION. Only in emergencies should a child be forced to undergo dental imaging. It is much better to postpone the examination until the second or third visit rather than instill in the child a fear of visiting the dental office.
POSTPONE THE EXAMINATION. Only in emergencies should a child be forced to undergo dental imaging. It is much better to postpone the examination until the second or third visit rather than instill in the child a fear of visiting the dental office.
Endodontic Patients
The term endodontic is derived from two Greek words, endon, meaning “within,” and odontos, meaning “tooth.” Endodontics is the branch of dentistry concerned with the diagnosis and treatment of diseases of the dental pulp within the tooth. Endodontic treatment usually involves removal of the dental pulp (nerve tissue) from the pulp chamber and canals within the tooth, then filling the empty pulp chamber and canals with a material such as gutta percha or silver points. This treatment is often referred to as a root canal procedure or root canal therapy. The endodontic patient is one who has undergone root canal therapy.
The dental image is indispensable during root canal procedures and essential for diagnosing and managing pulpal problems. During a root canal procedure, a series of exposures is typically obtained of the same tooth; these exposures are used to evaluate the tooth before, during, and after treatment.
Receptor Placement
The dental radiographer must modify the receptor placement method for the endodontic patient. During a root canal procedure, receptor placement is difficult because of poor visualization of the tooth. The equipment used during a root canal procedure makes it difficult for the dental radiographer to visualize the area well in order to position and stabilize the receptor. Equipment used during a root canal procedure includes a rubber dam, rubber dam clamp, root canal instruments (files, reamers, broaches), and filling materials (gutta percha and silver points).
The EndoRay film holder (see Chapter 6) can be used as an aid in positioning the receptor during a root canal procedure; this holder fits around a rubber dam clamp and allows space for root canal instruments and filling materials to protrude from the tooth. A hemostat or a wooden tongue depressor may also be used to hold the receptor.
Recommended Technique
During a root canal procedure, the length of the pulp canals must be accurately measured without distortion (elongation or foreshortening). To avoid distortion, the paralleling technique (see Chapter 17) should be used whenever possible; the use of the bisecting technique (see Chapter 18) may result in elongated or foreshortened images. With the paralleling technique, the use of a beam alignment device (e.g., EndoRay) is strongly recommended.
Edentulous Patients
Edentulous means “without teeth.” The edentulous patient, or patient without teeth, requires a dental imaging examination for the following reasons:
• To detect the presence of root tips, impacted teeth, and lesions (cysts, tumors)
• To identify objects embedded in bone
• To establish the position of normal anatomic landmarks (e.g., mental foramen) relative to the crest of the alveolar ridge
• To observe the quantity and quality of bone that is present
The dental imaging examination of the edentulous patient may include the following projections: panoramic, periapical, or a combination of occlusal and periapical.
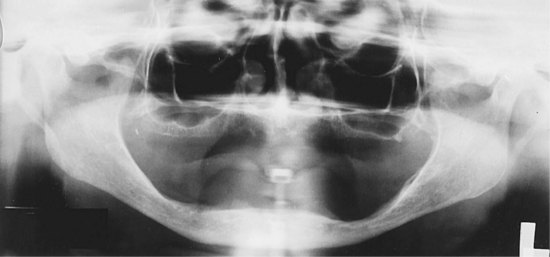
Panoramic Examination
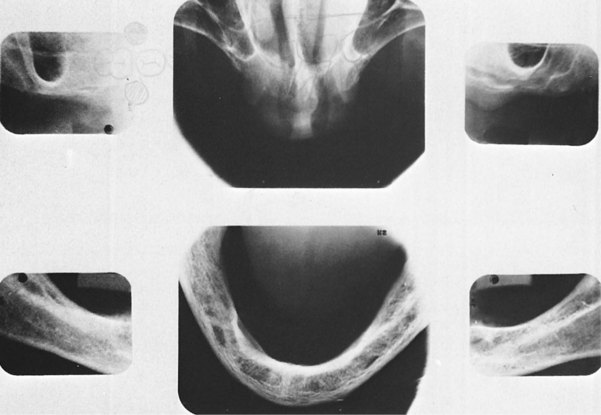
A panoramic image (see Chapter 22) is the most common way of examining the edentulous jaw (Figure 24-6). The panoramic examination is quick and easy for the patient and requires only one exposure. If a panoramic image reveals any root tips, impacted teeth, foreign bodies, or lesions in the jaws, a periapical projection of that specific area must be exposed. The periapical image has more definition and permits the area in question to be examined in greater detail.
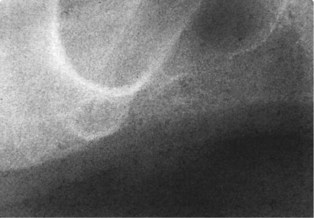
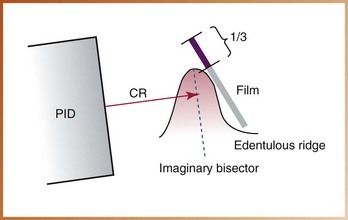
Periapical Examination
If a panoramic x-ray machine is not available, 14 periapical projections (6 anterior and 8 posterior) can be used to examine the edentulous arches (Figure 24-7). A size 2 receptor is typically used for the edentulous examination. Either the paralleling technique (see Chapter 17) or the bisecting technique (see Chapter 18) can be used for this periapical examination. If the paralleling technique is used, cotton rolls must be placed on both sides of the bite-block in place of the missing teeth. If the bisecting technique is used, the edentulous ridge and the receptor form the angle to be bisected (Figure 24-8). The receptor should be positioned such that approximately one third of it extends beyond the edentulous ridge. If the alveolar ridges of the patient are severely resorbed, the bisecting technique is recommended.
Occlusal–Periapical Examination
Some practitioners prefer to use both occlusal and periapical projections to examine the edentulous patient. The combined occlusal and periapical examination consists of a total of 6 exposures (Figure 24-9): 1 maxillary topographic occlusal projection (size 4 receptor), 1 mandibular cross-sectional occlusal projection (size 4 receptor), and 4 standard molar periapical exposures (size 2 receptor). As with the panoramic image, if an object is identified on an occlusal projection, a periapical projection of that specific area should be exposed.
Summary
• Imaging techniques must often be modified to accommodate patients with special needs, including patients with a hypersensitive gag reflex, patients with physical or developmental disabilities, pediatric patients, endodontic patients, and edentulous patients.
• In dental imaging, the hypersensitive gag reflex is a commonly encountered problem. The areas most likely to elicit the gag reflex when stimulated include the soft palate and the posterior third of the tongue.
• The dental radiographer can effectively manage the patient with a hypersensitive gag reflex by conveying a confident attitude, completing all patient and equipment preparations before receptor placement, using proper exposure sequencing, placing and exposing receptors as quickly as possible, and using modifications in technique as necessary.
• Helpful strategies to prevent gagging include never suggesting gagging, reassuring the patient, suggesting breathing, distracting the patient, reducing tactile stimuli, and using a topical anesthetic.
• If the patient has an uncontrollable gag reflex, extraoral projections (e.g., panoramic or lateral jaw) can be used to obtain diagnostic information.
• The dental radiographer must be aware of the common physical disabilities (e.g., problems with vision, hearing, or mobility) and know the necessary modifications in technique to accommodate a person with a disability.
• The dental radiographer must also be aware of patients with specific dental needs, including pediatric patients, endodontic patients, and edentulous patients, and know the necessary modifications in technique to accommodate such patients.
• With the pediatric patient, special attention must be paid to the prescription of dental images, patient and equipment preparations, recommended techniques, and patient management.
• With the endodontic patient, the dental radiographer must be able to modify receptor placement and, at the same time, provide accurate images that measure the length of the pulp canals without distortion.
• With the edentulous patient also, the dental radiographer must be able to modify intraoral placements. Imaging is used in the edentulous patient to detect lesions, root tips, impacted teeth, and objects embedded in bone and to observe the quantity of bone present.
Frommer, HH, Savage-Stabulas, JJ, Patient management and special problems. Radiology for the dental professional, ed 9, St. Louis, Mosby, 2011.
Johnson, ON, McNally, MA, Essay, CE, Managing patients with special needs. Essentials of dental radiography for dental assistants and hygienists, ed 8, Upper Saddle River, NY, Pearson Education, Inc, 2009.
Johnson, ON, McNally, MA, Essay, CE, Radiography for children. Essentials of dental radiography for dental assistants and hygienists, ed 8, Upper Saddle River, NY, Pearson Education, Inc, 2009.
Miles, DA, Van Dis, ML, Jensen, CW, Williamson, GF, Accessory radiographic techniques and patient management. Radiographic imaging for dental auxiliaries, ed 4, St. Louis, Saunders, 2009.
Miles, DA, Van Dis, ML, Razmus, TF. Intraoral radiographic techniques. In: Basic principles of oral and maxillofacial radiology. Philadelphia: Saunders; 1992.
Ohio Governor’s Council on People with Disabilities. Ten do’s and don’t’s when you meet a person with a disability. Catalog No G-16, Columbus, Ohio, 1990 http://gcpd.ohio.gov/index.asp. accessed October 2010
White, SC, Pharoah, MJ, Intraoral radiographic examinations. Oral radiology: Principles of interpretation, ed 6, St. Louis, Mosby, 2009.
True or False
________ 1. The area of the oral cavity that is most likely to elicit the gag reflex when stimulated is the anterior third of the tongue.
________ 2. Breathing takes place simultaneously with the gag reflex.
________ 3. Psychogenic and tactile stimuli are precipitating factors for the gag reflex.
________ 4. Lack of operator confidence may act as a psychogenic stimulus and contribute to the gag reflex.
________ 5. The longer a receptor stays in the mouth, the more likely the patient is to gag.
________ 6. Exposure sequence does not play a role in preventing the gag reflex.
________ 7. Posterior periapical projections are always exposed before anterior periapical projections.
________ 8. The mandibular molar periapical projection is most likely to elicit the gag reflex.
________ 9. A receptor that is dragged along the palatal tissues may stimulate the gag reflex.
________ 10. The dental radiographer should ask the patient, “Are you a gagger?”
________ 11. If a patient gags, the dental radiographer should remove the receptor as quickly as possible and reassure the patient.
________ 12. If a patient is breathing during receptor placement and exposure, the gag reflex will not occur.
________ 13. Distracting the patient often helps suppress the gag reflex.
________ 14. Increasing tactile stimuli helps prevent the gag reflex.
________ 15. The patient with a hypersensitive gag reflex should be instructed to inhale during the application of topical anesthetic spray.
________ 16. It is appropriate for the dental radiographer to gesture to another person in the presence of a person who is blind.
________ 17. In the case of a person with a disability, it is appropriate for the dental radiographer to hold a receptor during x-ray exposure.
________ 18. If the dental radiographer determines that a person cannot tolerate intraoral projections, no intraoral receptors should be exposed.
________ 19. It is appropriate for the dental radiographer to question a patient about a disability.
________ 20. The dental radiographer should talk to the caregiver of a patient with a disability instead of talking directly to the patient.
________ 21. With the pediatric patient, the dental radiographer does not need to alter patient management techniques.
________ 22. The radiographic examination should be performed on the pediatric patient regardless of the cooperation of the patient.
________ 23. During an endodontic procedure, receptor placement is difficult because of poor visualization of the tooth.
________ 24. The bisecting technique is recommended for the endodontic patient.
________ 24. The panoramic examination is the imaging examination most often used in edentulous patients.