Basic Concepts
The paralleling technique (also known as the extension cone paralleling [XCP] technique, right-angle technique, and long-cone technique) is one method that can be used to expose periapical and bite-wing image receptors. Before the dental radiographer can competently perform the paralleling technique, a thorough understanding of the terminology, principles, and basic rules governing this technique is necessary. Knowledge of the beam alignment devices and receptors used with the paralleling technique is also required.
Terminology
An understanding of the following basic terms is necessary before describing the paralleling technique:
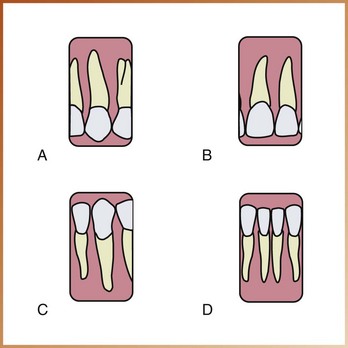
Parallel: Moving or lying in the same plane, always separated by the same distance and not intersecting (Figure 17-1, A)
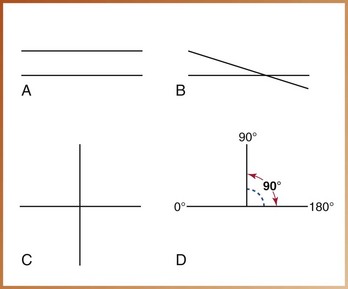
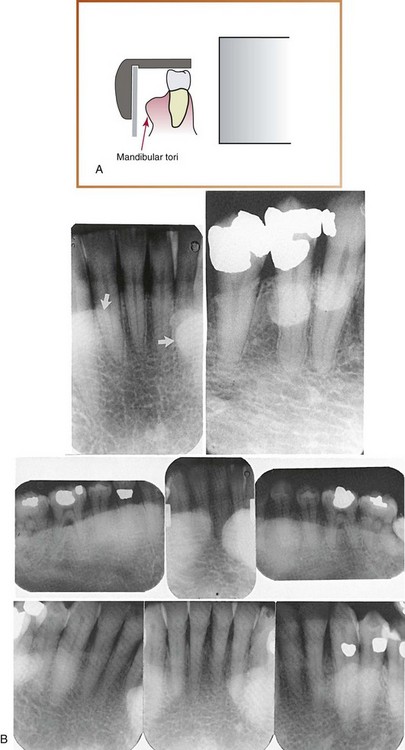
FIGURE 17-1 A, Parallel lines are always separated by the same distance and do not intersect. B, Intersecting lines cross one another. C, Perpendicular lines intersect one another to form right angles. D, A right angle measures 90 degrees and is formed by two perpendicular lines.
Intersecting: To cut across or through (Figure 17-1, B)
Perpendicular: Intersecting at or forming a right angle (Figure 17-1, C)
Right angle: An angle of 90 degrees formed by two lines perpendicular to each other (Figure 17-1, D)
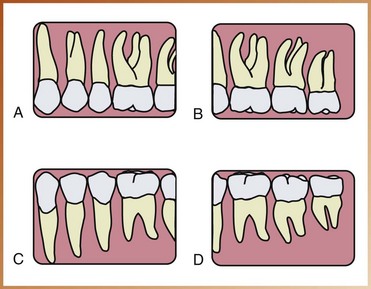
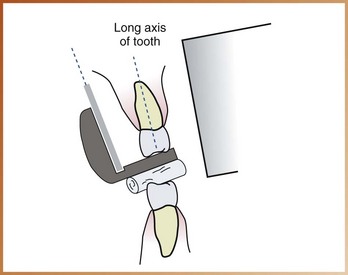
Long axis of the tooth: An imaginary line that divides the tooth longitudinally into two equal halves (Figure 17-2)
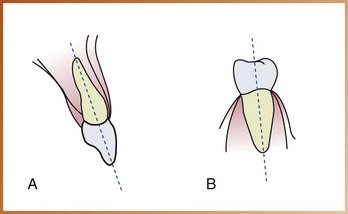
FIGURE 17-2 A, The long axis of the maxillary incisor divides the tooth into two equal halves. B, The long axis of a mandibular premolar divides the tooth into two equal halves.
Central ray: The central portion of the primary beam of x-radiation
Principles of Paralleling Technique
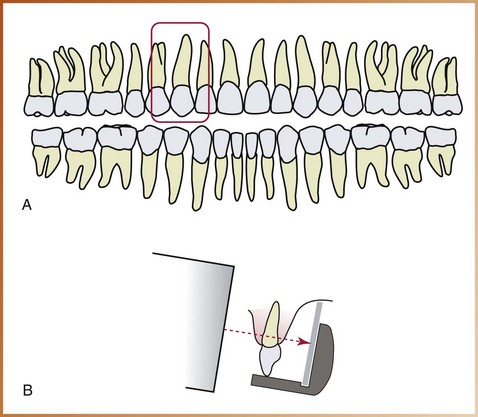
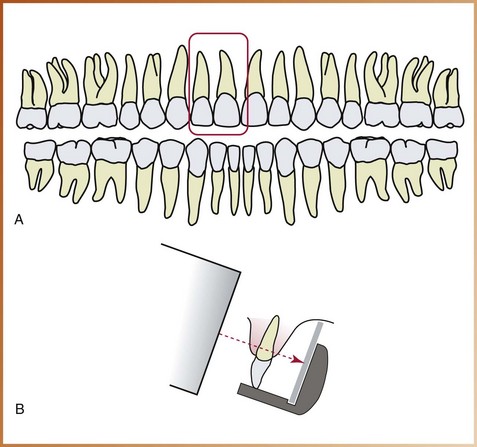
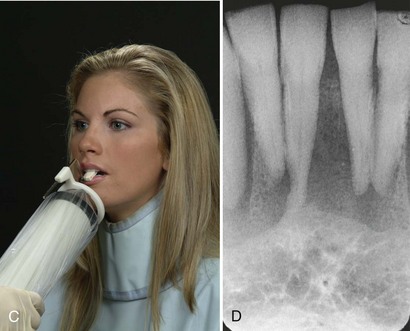
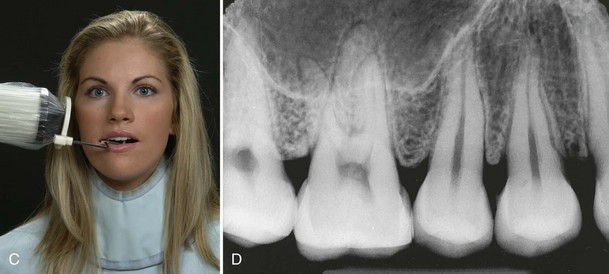
As the term paralleling indicates, this technique is based on the concept of parallelism. The basic principles of the paralleling technique can be described as follows (Figure 17-3):
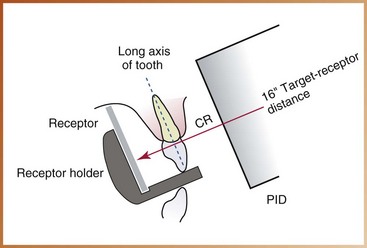
FIGURE 17-3 Positions of the receptor, teeth, and central ray (CR) of the x-ray beam in the paralleling technique. The receptor and the long axis of the tooth are parallel. The central ray is perpendicular to the tooth and the receptor. An increased target–receptor distance (16 inches) is required. PID, position-indicating device.
1. The receptor is placed in the mouth parallel to the long axis of the tooth being radiographed.
2. The central ray of the x-ray beam is directed perpendicular (at a right angle) to the receptor and the long axis of the tooth.
3. A beam alignment device must be used to keep the receptor parallel with the long axis of the tooth. The patient cannot hold the receptor in this manner.
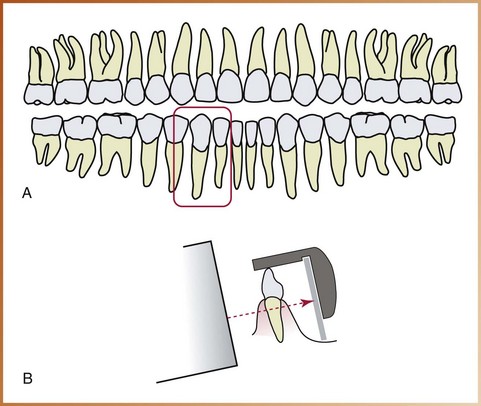
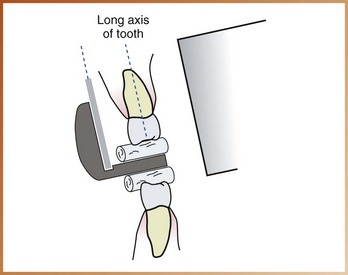
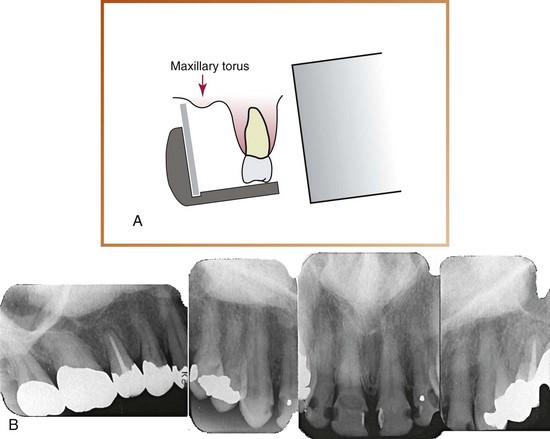
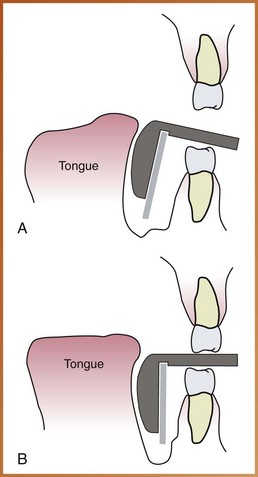
To achieve parallelism between the receptor and the tooth, the receptor must be placed away from the tooth and toward the middle of the oral cavity. Because of the anatomic configuration of the oral cavity (e.g., curvature of palate), the object–receptor distance (distance between receptor and tooth) must be increased to keep the receptor parallel with the long axis of the tooth (Figure 17-4). Because the receptor is placed away from the tooth, image magnification and loss of definition result. As discussed in Chapter 8, increased object–receptor distance results in increased image magnification.
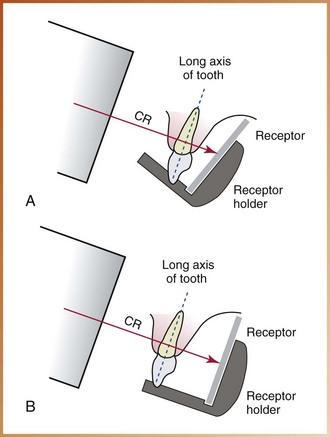
FIGURE 17-4 A, The receptor is placed close to the tooth and is not parallel to the long axis of the tooth. B, Increased object–receptor distance. The receptor is placed away from the tooth and is now parallel with the long axis of the tooth. CR, central ray.
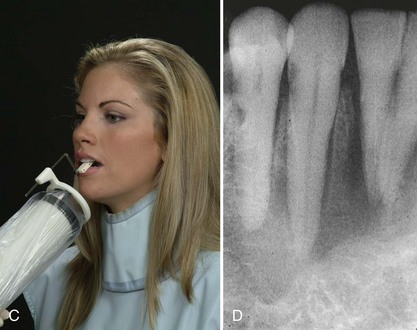
To compensate for image magnification, the target–receptor distance (distance between source of x-rays and receptor) must also be increased to ensure that only the most parallel rays will be directed at the tooth and the receptor. As a result, a long (16-inch) target–receptor distance must be used with the paralleling technique. The paralleling technique is sometimes referred to as the “long-cone technique”; long refers to the length of the cone, or position-indicating device (PID), that is used. The use of a long target–receptor distance in the paralleling technique results in less image magnification and increased definition.
The American Dental Association (ADA) and the American Academy of Oral and Maxillofacial Radiology recommend the use of a rectangular collimator to reduce the amount of radiation the patient receives. Limiting the size of the x-ray beam not only reduces the amount of skin that is exposed but also results in a significant reduction of radiation to the patient, by as much as 70%. The receptor placement procedures are illustrated with a rectangular collimator attached to the end of the PID.
Beam Alignment Devices
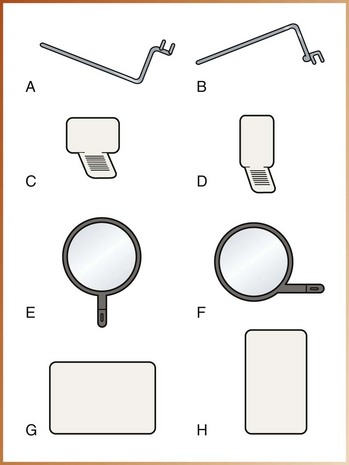
The paralleling technique requires the use of a beam alignment instrument to position the receptor parallel to the long axis of the tooth. Beam alignment devices are used to position an intraoral receptor in the mouth and maintain the receptor in position during exposure (see Chapter 6). Examples of commercially available intraoral beam alignment devices include the following:
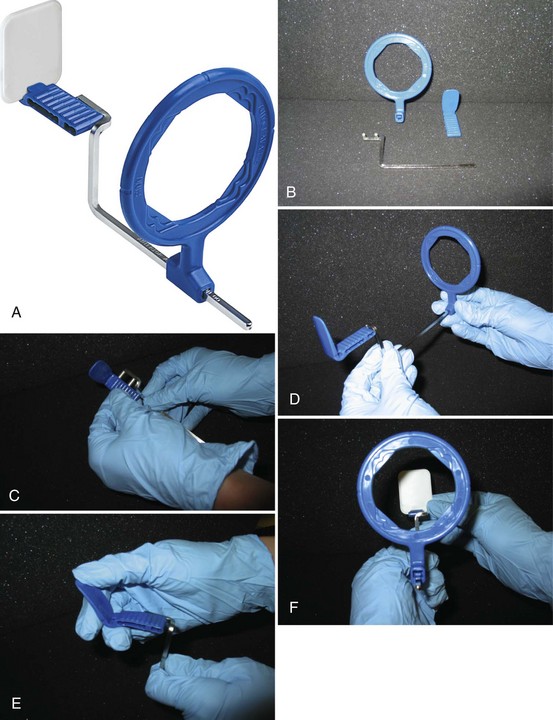
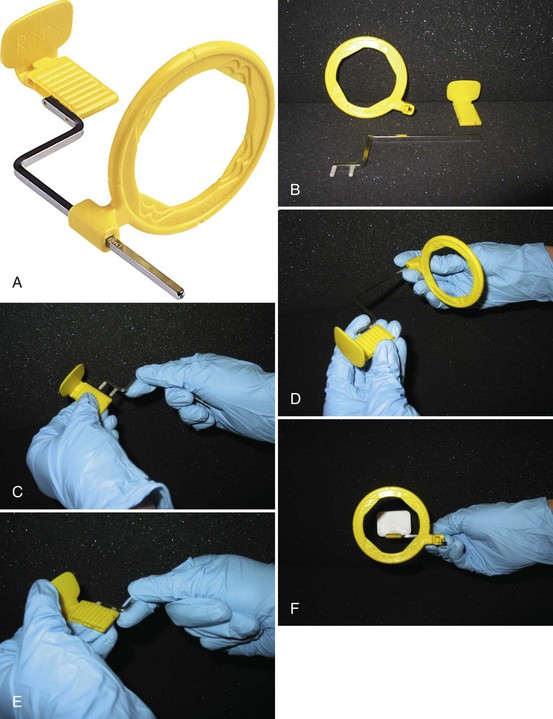
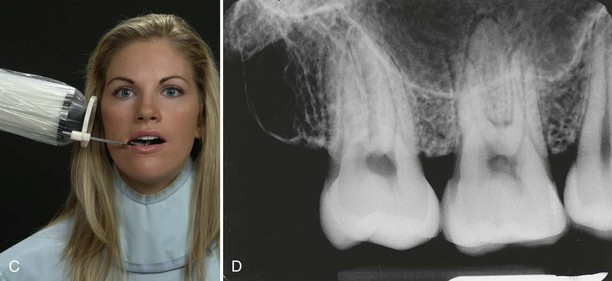
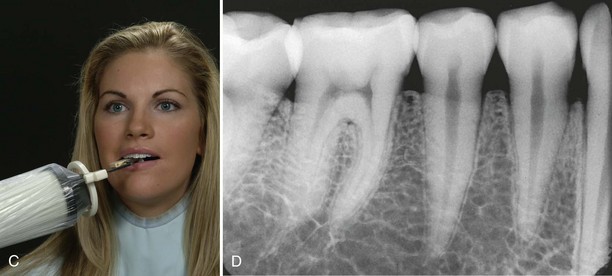
• Rinn XCP instruments (Dentsply Rinn Corporation, Elgin, IL). The XCP (extension cone paralleling) instruments include plastic bite-blocks, plastic aiming rings, and metal indicator arms (Figure 17-5, A). The plastic bite-blocks and aiming rings are color-coded to aid in assembly: blue instruments are used in the anterior regions, yellow instruments are used in the posterior regions, red instruments are used for bite-wing projections, and torquoise instruments are used in endodontic procedures. To reduce the amount of radiation the patient receives, a snap-on ring collimator can be added to the plastic aiming ring.
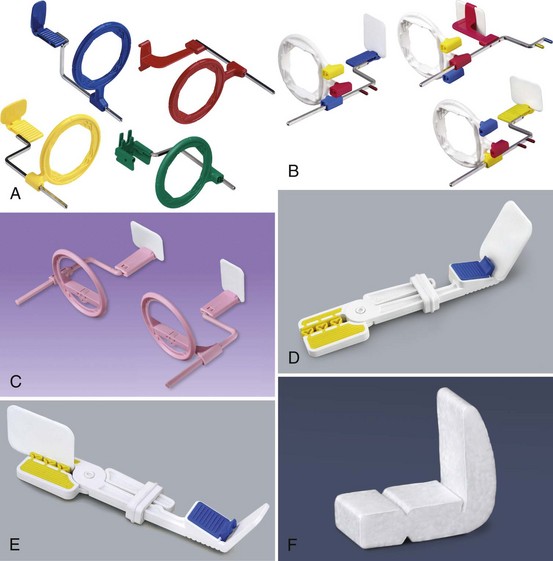
FIGURE 17-5 Beam alignment devices. A, XCP instruments: blue instruments are used in the anterior region, yellow instruments are used in the posterior region, red instruments are used in the bite-wing technique, and torquoise instruments are used for endodontic procedures. B, Rinn XCP-ORA beam alignment devices provide accurate positioning in a system with one ring and one arm for anterior, posterior, and bite-wing projections. C, The Rinn Flip-Ray system uses a rotating bite-block and ring to eliminate multiple beam alignment devices. D, E, The EEZEE Grip (formerly Snap-A-Ray) Xtra intraoral receptor holder is color coded for the anterior and posterior regions. F, An example of a disposable Stabe bite-block. (A, D, E, Courtesy Dentsply Rinn Corporation, Elgin IL.)
• Rinn XCP-ORA instruments have a universal ring and arm positioning system to accommodate anterior, posterior and bitewing projections (Figure 17-5, B).
• The Rinn Flip-Ray system uses a rotating bite-block and ring to eliminate multiple positioning parts.
• EEZEE-Grip receptor holder, formerly known as the Snap-A-Ray. This receptor-holding device can be used in both anterior and posterior areas (Figures 17-5, D and E).
• Stable bite blocks. The Stable bite block is a disposable receptor holder, and is designed for one time use only (Figure 17-5, F).
Some film holders are disposable (e.g., Stabe bite-block) and are designed for one-time use only. Other film holders are reusable (e.g., XCP instruments, Precision film holders, EEZEE-Grip film holder, hemostat with bite-block) and must be sterilized after each use. Additional beam alignment devices for use with imaging receptors will be discussed in Chapter 25, Digital Imaging).
Of all the film holders listed, the Rinn XCP beam alignment instruments with snap-on ring collimators and the Precision film holders are recommended for exposure of periapical receptors. These beam alignment devices are recommended because both include aiming rings that aid in the alignment of the PID with the receptor, and both significantly reduce the amount of patient exposure to radiation. These instruments are simple to position and easy to sterilize. Although only the Rinn XCP beam alignment instruments are illustrated in this text, the same principles apply to all the film holders listed.
Receptors Used for Paralleling Technique
The size of the intraoral receptor used with the paralleling technique depends on the teeth being radiographed, as follows:
• In the anterior regions, size 1 receptor is used; this narrow size is needed to permit placement high in the palate without bending or curving. Size 1 is always positioned with the long portion of the receptor in a vertical (upright) direction.
• In the posterior regions, size 2 receptor is used. Size 2 is always placed with the long portion of the receptor in a horizontal (sideways) direction.
Rules for Paralleling Technique
Five basic rules should be followed when using the paralleling technique.
1. Receptor placement. The receptor must be positioned to cover the prescribed area of teeth to be examined. Specific placements are detailed in the Procedures sections of this chapter.
2. Receptor position. The receptor must be positioned parallel to the long axis of the tooth. The receptor and beam alignment device must be placed away from the teeth and toward the middle of the oral cavity (see Figure 17-3).
3. Vertical angulation. The central ray of the x-ray beam must be directed perpendicular (at a right angle) to the receptor and the long axis of the tooth (see Figure 17-3).
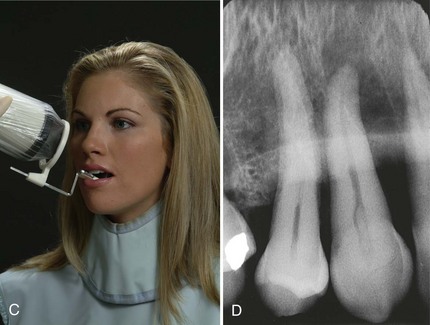
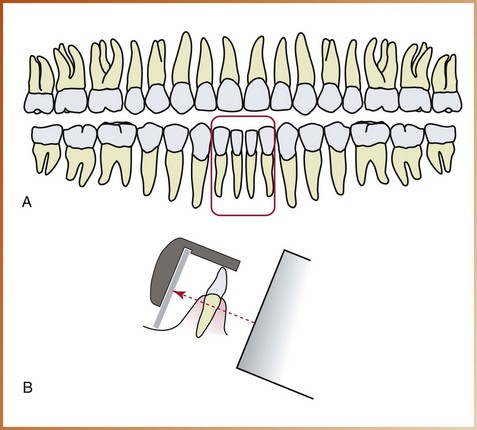
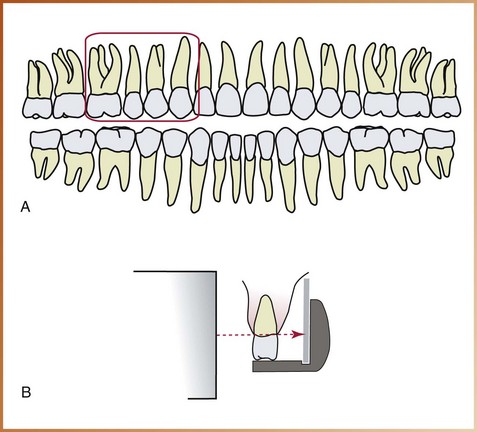
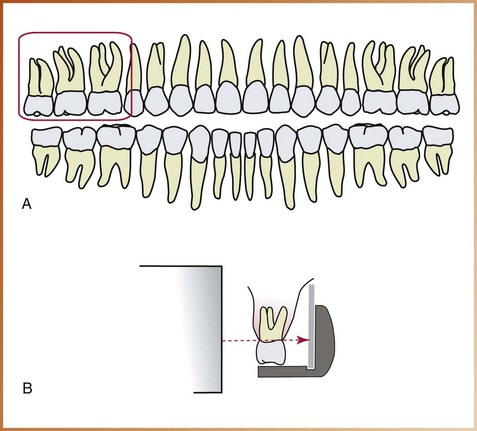
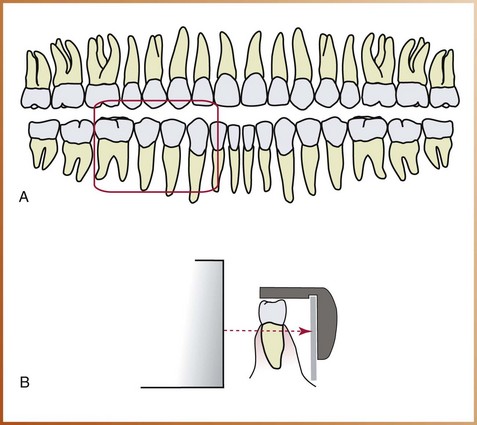
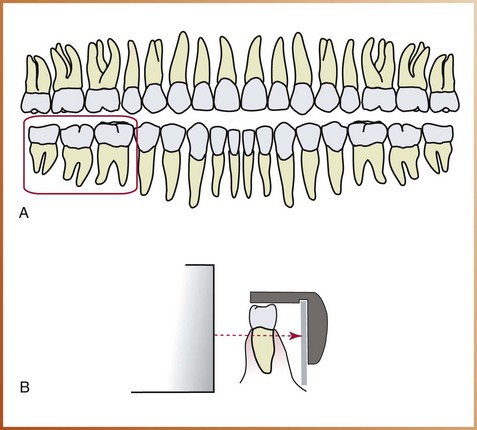
4. Horizontal angulation. The central ray of the x-ray beam must be directed through the contact areas between teeth (Figure 17-6).
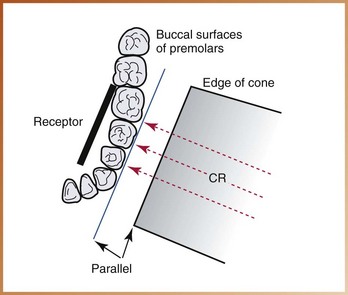
FIGURE 17-6 In this diagram, x-rays pass through the contact areas of the premolars because the central ray (CR) is directed through the contacts and perpendicular to the receptor. If the central ray is not directed through the contacts, overlap of the premolar contacts occurs.
5. Film receptor exposure. The x-ray beam must be centered on the receptor to ensure that all areas are exposed. Failure to center the x-ray beam results in a partial image on the receptor or a “cone-cut.” Cone-cuts can be produced with either a round PID or a rectangular PID. (Figure 17-7). Cone-cuts are discussed in Chapter 20.