Chapter 52Thoracolumbar Spine
Back problems are a major cause of altered gait or performance (see Chapters 50, 51, and 97). Both identification and documentation of vertebral lesions are difficult in horses; therefore treating back pain is a challenge for the equine clinician. The equine back is a large area covered by thick muscles. Therefore assessment of the bony elements is limited. Every joint in the thoracolumbar region has restricted mobility; therefore detecting changes in restricted movement when the horse is working is difficult. Diagnostic imaging of the thoracolumbar region is also limited, and radiological assessment requires special equipment. Specific treatment of back pain can only be performed after complete identification of the site and nature of the lesions.
Anatomy and Function
Bones
The thoracolumbar spine is basically composed of 18 thoracic vertebrae (T1 to T18), six lumbar vertebrae (L1 to L6), and five fused sacral vertebrae (S1 to S5). Some horses have individual (congenital) variations at the cervicothoracic, thoracolumbar, and lumbosacral junctions. The most common is the sacralization of the last lumbar vertebra (sacralization of L6), which can be seen by ultrasonography. Transitional vertebrae, with a rib on one side and a transverse process on the other side, can be found at the thoracolumbar junction. Intervertebral ankylosis alters the biomechanical behavior of the involved part of the spine, especially at the lumbosacral junction, which in normal horses is the most mobile joint between T2 and S1. Ankylosis of this joint puts more stresses on the caudal lumbar intervertebral joints and may predispose to osteoarthritis (OA) of the facet joints and intervertebral disk lesions. Fusion of the lumbar transverse processes (see the following discussion) is also sometimes seen, and this has similar consequences on adjacent intervertebral joints, but the consequences are fewer because little movement usually occurs in these joints. Transitional transverse processes, or ribs that do not involve the vertebral body, have less biomechanical significance.
The first 10 thoracic vertebrae have long spinous processes. These have a dorsocaudal orientation and provide insertion for the strong but elastic supraspinous ligament. The anticlinal vertebra, the vertebra with a spinous process perpendicular to the vertebral axis, is usually T15. Caudal to the anticlinal vertebra the spinous processes are orientated obliquely dorsocranially. The spinous processes are higher between L2 and L5. Therefore lumbar muscular atrophy results in a kyphotic appearance of the lumbar area.
In most horses the spinous processes of L6 and S1 are divergent, allowing a range of flexion and extension movements at the lumbosacral joint. The transverse processes from L5 (sometimes L4) to S1 articulate through intertransverse synovial joints, which limit lateral flexion in this area. The lumbar vertebral bodies are bigger than the thoracic ones and have a ventral crest for the insertion of the diaphragm.
Joints
Stability of the thoracolumbar vertebrae is provided by the supraspinous and interspinous ligaments, the joints between the cranial and caudal articular processes (the facet joints), the joints between the vertebral bodies, and the dorsal and ventral longitudinal ligaments. Stability of the spinous processes is provided by the supraspinous and interspinous ligaments (Figure 52-1). These ligaments are wider and more elastic in the cranial and middle thoracic areas, permitting more movement than in the caudal thoracic and lumbar regions.
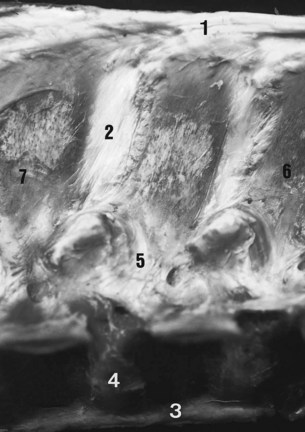
Fig. 52-1 Anatomical specimen showing the ligaments of the thoracolumbar spine. Cranial is to the right. 1, Supraspinous ligament; 2, interspinous ligament; 3, ventral longitudinal ligament; 4, fibrous superficial part of the intervertebral disk; 5, articular capsule of the synovial intervertebral joint; 6, first lumbar vertebra; 7, third lumbar vertebra.
The caudal and cranial articular processes articulate via synovial intervertebral articulations (the facet joints). At the base of the spinous processes these joints are symmetrically placed on each side of the median plane (Figure 52-2). These are typical synovial (diarthrodial) joints with articular cartilage, a closed synovial cavity containing synovial fluid, a synovial membrane, and a fibrous capsule. They have a single flat articular facet in the cranial thoracic area (up to T12) and two angulated articular facets between T12 and T16. From T17 to S1 the articular facets are congruent, with a cylindrical shape aligned on a paramedian axis. These regional variations are correlated with the limited mobility of the lumbar spine and the wider range of movement in the thoracic region, including flexion and extension in the median plane, lateral flexion in the horizontal plane, and rotation. The vertebral bodies are stabilized by joints composed of a fibrous intervertebral disk and two longitudinal ligaments. The ventral longitudinal ligament is replaced by the longissimus cervicis muscle in the cranial thoracic area. The dorsal longitudinal ligament is located in the vertebral canal and adherent to the dorsal border of each intervertebral disk.
Muscles
The vertebral column is moved by wide muscles (Figure 52-3). The strong epaxial muscles, located dorsal to the vertebral axis, have an extensor effect when contracted bilaterally. Unilateral contraction induces lateral flexion and contributes to rotation of the vertebral column. Electromyographic studies show that the epaxial muscles limit flexion and stabilize the vertebral column during the suspension phase at the trot.1,2
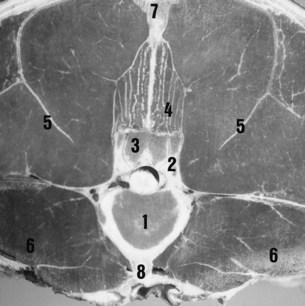
Fig. 52-3 Transverse anatomical section of the normal lumbar region of a 6-year-old Selle Français mare. 1, Vertebral head of third lumbar vertebra; 2, cranial articular process of third lumbar vertebra; 3, caudal articular process of second lumbar vertebra; 4, multifidus muscle; 5, erector spinae muscle; 6, psoas muscles; 7, supraspinous ligament; 8, ventral longitudinal ligament.
The epaxial muscles include the following:
The longissimus dorsi is the strongest muscle. The iliocostalis muscles are small but have a greater role in lateral flexion because of their eccentric location. Caudally, these muscles fuse to form the erector spinae muscle. The multifidus muscle lies under the spinosus muscle and is in close contact with the vertebrae (juxtavertebral muscle). This muscle plays a major role in the stability of the vertebrae and in the proprioceptive adjustment of the spine.
The hypaxial muscles, located ventral to the vertebral axis, have a flexor effect on the spine when contracted bilaterally. Unilateral contraction induces lateral flexion and contributes to rotation of the vertebral column. The hypaxial muscles include psoas minor and major, rectus abdominis, and rectus oblique.
The psoas minor and major muscles insert on the ventral aspect of the lumbar and caudal three thoracic vertebrae (juxtavertebral muscles). They act mainly at the lumbosacral junction but are also able to flex the thoracolumbar junction and the lumbar spine. The rectus abdominis muscle is an effective flexor of the complete thoracolumbar spine because of its eccentric insertions on the pubis, sternum, and ventral part of the ribs. The oblique muscles can create lateral flexion and rotation of the thoracolumbar spine because of eccentric insertions on the tubera coxae and ribs. Electromyographic studies show that the rectus abdominis muscles act to limit extension and stabilize the vertebral column during each diagonal stance phase at the trot.1,2
Diagnosis of Back Pain
The objectives of clinical examination of the horse’s back3-7 are to determine whether back pain is present, the site or sites of pain, and the potential lesions responsible for the pain. Acute back pain can arise after traumatic injuries, such as a fall, or after an awkward jump. Acute pain and muscle spasm may be identified and may be the primary lesion, but a complete radiographic examination of the thoracolumbar spine may be indicated to assess for vertebral fractures or long-standing bony lesions that may be responsible for the accident. These lesions may become clinically significant because of overstress on the intervertebral structures. For example, a long-standing spondylosis lesion may cause acute pain on landing after a jump.
A poor rider or an ill-fitting saddle may cause back pain, but correction of these problems may not be easy. It is important to manage these causes of back pain before proceeding with more advanced imaging techniques.
Back pain may also be manifest by abnormal behavior, for example, bucking (see page 992).
Physical Examination
Physical examination is essential in diagnosing back pain. Only the main criteria for each step or procedure are discussed. It is obviously important to perform a comprehensive evaluation of the whole horse to identify any other potential problems that may contribute to gait abnormalities or poor performance.
Inspection
The most commonly described abnormal curvatures of the back are lumbar kyphosis and thoracic lordosis. These can be seen in the same horse. Atrophy of the epaxial muscles in the lumbosacral regions results in prominence of the normal summits of the spinous processes and apparent kyphosis of the lumbar spine. Detection of atrophy of the epaxial muscles is a key finding in a horse with potential back pain because atrophy reflects the reduction of movement in the painful areas. The finding can help provide information on the possible location of the lesions. However, one should bear in mind that muscular development also reflects the horse’s previous work history, and if the horse has never worked properly through its back, the epaxial muscles will be poorly developed.
Thoracic lordosis may be seen in clinically normal horses and does not necessarily imply the presence of back pain. However, a short coupled horse with lordosis is more likely to have impinging spinous processes, a reflection of the horse’s normal conformation.
Abnormal swellings in the saddle area or abnormal hair loss may reflect a poorly fitting saddle or the position and balance of the rider. A rider who sits crookedly predisposes to excessive movement of the saddle and asymmetrical hair loss. However, it should be noted that hindlimb lameness may also induce abnormal movement of the saddle.
The stance of the horse may also be important; some horses with back pain may stand either camped out or camped under. However, a normal stance certainly does not preclude thoracolumbar region pain.
Palpation
Palpation of the thoracolumbar region should be performed with the horse standing quietly, bearing weight evenly on all limbs. Time should be spent getting the horse accustomed to the clinician’s presence, especially with an apprehensive horse, so that the horse’s true reactions to pain and pressure can be assessed. Unless approached quietly a thin-skinned Thoroughbred (TB) type may give a false impression of guarding the back and having protective spasm of the epaxial muscles.
Palpation of the superficial structures of the thoracolumbar region helps to identify supraspinous desmopathy and deformation or malalignment of the spinous processes. Identification of localized muscle tension can be a key feature in establishing the presence of a clinically significant lesion. The thickness of the epaxial muscles prohibits accurate assessment of deeper structures.
Pressure
Pressure on the superficial structures, such as the supraspinous ligament and the epaxial muscles, is useful to assess pain. Reliably assessing the response to pressure applied to deeper structures, such as the epaxial synovial intervertebral articulation complexes, is not possible.
Mobilization
Stimulation of movement of the thoracolumbar spine (Figure 52-4) is important to assess the amount of movement tolerated by the horse and any signs of pain, such as flexion of the limbs, alteration of facial expression, tension of the back muscles, movement of the tail, and alteration of behavior (kicking, rearing, bucking, and grunting).
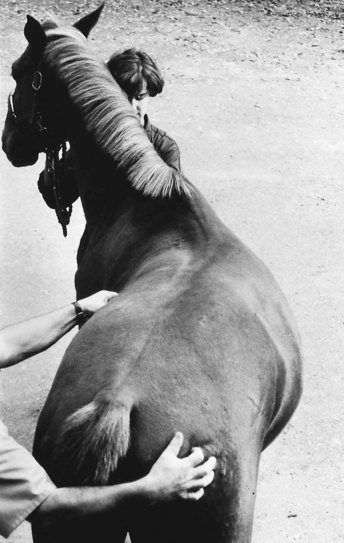
Fig. 52-4 Physical examination by left lateral flexion of the thoracolumbar spine. The two main criteria evaluated are the amount of movement and manifestations of pain.
The following protocol is recommended:
The clinician should try to determine which movements are restricted or not tolerated so as to determine potential sources of pain. These movements can be induced by skin stimulation of the dorsal and lateral aspects of the trunk and hindquarters. Although some horses respond to soft digital stimulation, in others a stronger stimulus is required, for example, using the tips of a pair of artery forceps. Firm stroking with a hard instrument displaced craniocaudally and inducing spectacular wide extension and flexion movements may lack sensitivity and specificity in determining the site of back pain, but firm stroking may be necessary in extremely stoical cob-type horses to induce any movement. A normal, relaxed horse is able to flex and extend the thoracolumbar spine smoothly and repeatedly. The degree of movement reflects in part the type of horse. Cob-type horses naturally tend to have much more restricted movement than TBs or Warmbloods. The clinician will find it useful to keep one hand resting on the midback region during these maneuvers to detect induced muscle spasm or abnormal cracking of the muscles or ligaments (a crepitus-like feeling as the epaxial muscles or ligaments contract and relax). Further descriptions of assessment of thoracolumbar movement are provided in Chapter 51. Pressure algometry has been used to more objectively quantify back pain.8,9
Examination during Movement
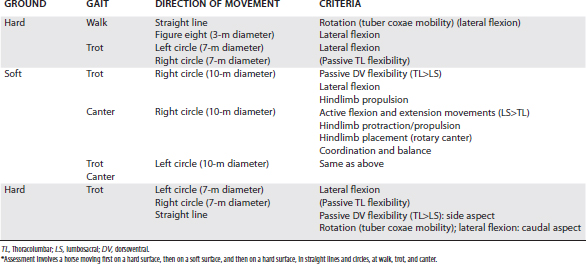
Evaluation of the horse moving at walk, trot, and canter is essential to assess whether pain is present and to identify functional disorders, such as limitation of regional intervertebral mobility (Figure 52-5). The clinician should always bear in mind that impinging spinous processes can be present asymptomatically. Therefore the clinical significance of impinging spinous processes should not be overinterpreted, unless clinical signs of back pain are evident. The horse should be assessed moving in straight lines and in small circles at a walk and trot on a hard surface and moving at a trot and canter on the lunge to determine whether any reduction of back mobility is apparent (Table 52-1).
In vivo kinematic studies have quantified dorsoventral flexibility of the back in sound horses trotting10,11 and at various gaits on the treadmill.12 Horses with vertebral lesions showed a reduction of passive flexibility of the back at trot,13-15 with reduced flexion and extension, lateral flexion, and rotation. Thus the horse may appear to hold its back rather stiffly. This can be caused by mechanical problems (partial or complete ankylosis) or pain. Back pain may also influence stride length and limb flight, resulting in a more restricted and less animated gait. On the lunge the horse may show loss of balance and a tendency to lean the body rather than bend the trunk toward the direction of circle. However, such clinical signs may also be seen in association with lameness, which, if bilateral, may not be obvious.
Examination of the Horse Being Ridden or in Harness
The presence and the degree of back pain may be underestimated unless the horse is evaluated under its normal working conditions, that is, ridden or in harness. The influence of a rider on mobility of the horse’s back has recently been quantified.16 The clinician should watch carefully as the tack or harness is applied, particularly as the girth is tightened. However, the clinician should bear in mind that cold-back behavior (see Chapter 97) is not necessarily a reflection of back pain, although it may be. The fit of the saddle for the horse and the rider should be evaluated. Back mobility,3 the movements that the horse finds difficult, and the horse’s attitude toward work should all be assessed (see Chapter 97). The clinician should pay attention also to the observations of the rider because the horse may feel considerably worse than it appears. The rider may describe lack of hindlimb power, lateral stiffness of the back to the left or right, unwillingness of the horse properly to take the bit, or loss of fluidity in the paces. The rider may complain of back pain induced by riding the horse.
Examination of the horse while it is ridden also gives the clinician the opportunity to assess the rider because back pain is readily induced by poor riding, a situation that may not be easy to handle diplomatically.
Local Analgesia
Diagnostic infiltration of local anesthetic solution may be useful to assess the clinical significance of impingement of spinous processes, where only the bones, ligaments, and adjacent muscles are affected by the analgesia. If impingement is severe, local anesthetic solution can only be deposited around the spinous processes and not between them. The volume of local anesthetic solution required depends on the number of spinous processes involved. Sixty to 80 mL of mepivacaine is injected at several sites using 4-cm needles if four or five impinging spinous processes exist. The response is assessed in 15 to 20 minutes and is most accurately evaluated by observing the horse while it is ridden and by the rider’s feel. If kissing spines is the only clinically significant lesion, then substantial improvement should be anticipated, but if other lesions are contributing to pain, the response is limited.
If deeper injections are performed in the region of the epaxial synovial intervertebral articulations, interpretation may be confounded because the injections are effectively intramuscular injections, and the local anesthetic solution may readily diffuse to affect sites on the dorsal and ventral rami of the spinal nerves. Thus local analgesia has potentially limited value for the assessment of the clinical significance of OA of the synovial intervertebral articulations and little value for assessment of intervertebral disk disease and spondylosis.
Imaging
Radiography and ultrasonography are essential to determine potential causes of pain or mechanical restriction. Nuclear scintigraphy is also a useful tool to detect abnormal bone activity and to help establish the clinical significance of radiological findings.
Radiography
Indications for radiographic examination of the thoracolumbar spine include owner complaints of a back problem in their horse, abnormal clinical findings, poor performance, or as part of the assessment of an obscure lameness.
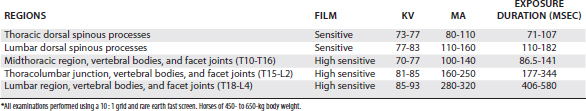
The horse should stand squarely on all limbs.17 Sedation may be necessary using detomidine (3 to 7 mg) or romifidine (12 to 25 mg). A high-output x-ray machine is necessary, with a rotating anode and an 80-kW power generator, for example.
Imaging plates or cassettes (20- × 40-cm format) with fast screens and sensitive or high-sensitive films are used to provide highly sensitive film-screen combinations. The cassettes should be placed in a vertically orientated ceiling or wall-mounted cassette holder, which can be aligned with the x-ray machine. The cassette should be placed as close to the trunk of the horse as possible. A 10 : 1 ratio focused grid is used to reduce radiation scatter. The focus-film distance varies between 1.15 and 1.30 m. The x-ray beam is directed perpendicular to the vertebral column axis. At least five exposures are required (Figure 52-6) to obtain a complete evaluation of the thoracolumbar spine between T10 and L4. In some horses L5 or L6 may also be imaged. The exposure parameters are summarized in Table 52-2. Additional horizontal 20° ventral oblique radiographic images are useful to assess the left and right thoracic synovial intervertebral articulations.6 To reduce motion, the exposure is performed during the last part of expiration.
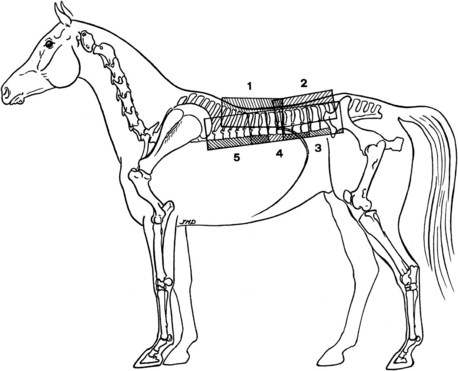
Fig. 52-6 Position of the imaging plates for radiographic examination of the thoracolumbar spine. 1, Thoracic spinous processes; 2, lumbar spinous processes; 3, lumbar vertebral bodies and synovial intervertebral articulation; 4, thoracolumbar vertebral bodies and synovial intervertebral articulation; 5, thoracic vertebral bodies and synovial intervertebral articulation.
Ultrasonography
Ultrasonographic examination of all the epaxial structures is possible.18-20 Imaging of the spinous processes and associated ligaments is performed with 7.5- or 10-MHz probes. A standoff pad is used to improve detection of the superficial structures. Imaging of the articular and transverse processes can be performed with 5- to 2.5-MHz probes. Longitudinal median and paramedian scans and transverse scans are combined to image all dorsal vertebral structures. For ultrasonographic examination the hair on the median plane over the spinous processes is removed with a No. 40 clipper blade, and the skin is cleaned. The skin is never shaved. When the hair is short (during the summer time), wetting the hair and skin with hot water for several minutes allows examination without clipping. Aqueous contact transmission gel is applied to the wet skin to couple the transducer to the skin to avoid air interference and artifacts. The lumbosacral and intertransverse lumbar and lumbosacral articulations can be assessed per rectum.21
Nuclear Scintigraphy
Patterns of radiopharmaceutical uptake (RU) in clinically normal riding horses have been described and compared with radiological findings.22,23 In a retrospective study of 50 horses with back pain, the most common abnormal finding was increased radiopharmaceutical uptake (IRU) in the spinous processes between T12 and L2, identified in 48 horses.24 Three horses had abnormal RU in the vertebral bodies of L3 to L6 and T11 to T14. Patterns of RU associated with OA of the synovial intervertebral articulations25 and spondylosis26 have been described. However, normal RU does not preclude the presence of clinically significant osseous pathology.25,26
Lateral or slightly oblique lateral images give the most information. Scattered radiation is a problem because of the large muscle mass overlying the vertebrae, so use of a high-resolution collimator is preferred. This requires longer acquisition times to obtain an adequate number of counts to give adequate image quality. Slight swaying movement of the horse during image acquisition and the movement of breathing detract from image quality unless motion correction software is used. The gamma camera may need to be angled slightly to avoid the kidneys being superimposed over the caudal thoracic vertebrae. At least three images are required to evaluate the entire length of the thoracolumbar spine, and comparable images from the left and right sides can be useful. If images are acquired from only one side, the right side is best because of the position of the kidney. Dorsal images are occasionally useful to clarify the anatomical position of a focus of IRU identified in a lateral image. The summits of the spinous processes in the withers region, the caudoproximal aspect of the scapula, and the kidneys may all have greater normal RU than the rest of the thoracolumbar spine and may effectively conceal lesions (Figure 52-7). Masking these areas out after image acquisition potentially results in more information. Using a high-frequency filter can also yield additional information, making a subtle focus of IRU more obvious, and facilitating anatomical localization of IRU. Image resolution in fat horses may be compromised by scattered radiation in the soft tissues.
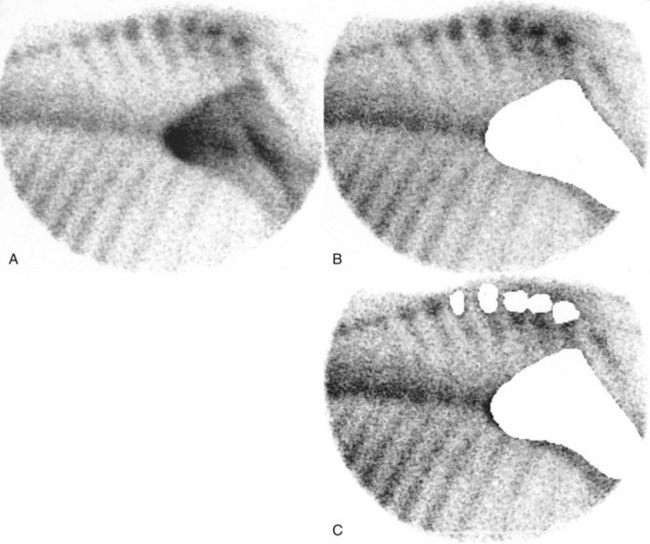
Fig. 52-7 A, Motion-corrected scintigraphic image of the cranial thoracic vertebrae without a filter. There is greater radiopharmaceutical uptake (RU) in the summits of the spinous processes in the withers region and the scapula than elsewhere. B, The same image as A after masking the scapula. C, The same image as A after masking the summits of the spinous processes at the withers and the caudal aspect of the scapula. Masking increases the information available. These images show normal patterns of RU.
Thermography
Normal thermographic patterns of the thoracolumbar region have been described.27 Thermography may be useful in identifying acute superficial muscle injuries or demonstrating to an owner the impact of a poorly fitting saddle or a rider sitting crookedly. However, in horses with chronic back pain, thermography does not usually add useful information and lacks sensitivity and specificity.
Lesions
Spinal Processes and Associated Ligaments
Impingement of the Dorsal Spinous Processes: Kissing Spines and Overriding Spinous Processes
Impingement of the summits of the spinous processes, or kissing spines, is a well-known pathological entity of the horse’s back28; however, it is important to recognize that lesions may not be restricted to the summits, and the entire length of the spinous processes must be evaluated. The most common location of these lesions is the vertebral segment between T10 and T18 (Figure 52-8), although lesions also occur between L1 and L6.17 Modeling of the dorsal aspect of a spinous process or an avulsion fracture reflects an insertional lesion of the supraspinous ligament. We grade impingement of the dorsal part of the spinous processes as follows:

Fig. 52-8 Lateral radiographic image of the spinous processes of the twelfth to sixteenth thoracic vertebrae. Cranial is to the left. There are radiological signs of impingement of the spinous processes between the eleventh and sixteenth thoracic vertebrae, with clinically significant marginal bone remodeling. T14, Fourteenth thoracic vertebra.
Overriding of spinous processes is a congenital condition with abnormal orientation of the spinous processes and similar changes in the margins of adjacent spinous processes. Other congenital abnormalities include complete fusion of two adjacent spinous processes or “webs” of spinous processes, or bony bridges between one or more adjacent spinous processes. The contour of the middle part of a spinous process may be altered because of enthesophyte formation at the insertion of the interspinous ligaments. Kissing lesions may also be seen at the ventral part of a spinous process with type 4 lesions of the epaxial synovial intervertebral articulation (see page 601). Generally speaking, the more severe and extensive the radiological abnormalities, the more likely they are to be of clinical significance; however, two close spinous processes may be associated with pain in a horse with a low pain threshold.
Ultrasonographic examination can easily demonstrate contact or modeling between two adjacent spinous processes, transverse thickening of the processes, and abnormal alignment. However, ultrasonography is more useful to assess concomitant supraspinous ligament lesions, including insertion desmopathies (enthesopathies) on the summits of the spinous processes.
Nuclear scintigraphy can help identify evidence of active bone modeling of the spinous processes and other potential lesions. However, one must bear in mind that active bone modeling is not synonymous with pain. Increased modeling of the dorsal aspects of the spinous processes may reflect impingement or insertional desmopathy of the supraspinous ligament (Figure 52-9). The degree of IRU does not always appear to be well correlated with the severity of the clinical signs or the radiological abnormalities (see Figure 52-9, A). Obvious focal IRU can be seen in horses with neither back pain nor radiological abnormality, whereas some horses with back pain associated with impinging spinous processes have only mild IRU. Mechanical limitations may contribute to back stiffness, which may predispose to the development of other lesions.
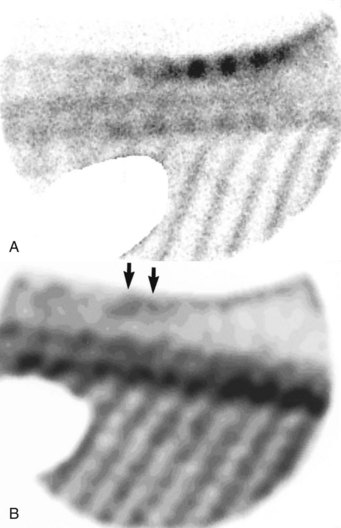
Fig. 52-9 A, Lateral nuclear scintigraphic image of the thoracolumbar region of a 10-year-old Grand Prix dressage horse with loss of action.There is increased radiopharmaceutical uptake (IRU) in the dorsal aspects of six adjacent spinous processes. The horse showed clinical signs of restricted mobility of the back. Radiographic examination revealed impinging spinous processes. The horse’s gait was dramatically improved by infiltration of local anesthetic solution around the affected spinous processes. B, Lateral nuclear scintigraphic image of the thoracic region of an 8-year-old show jumper gelding with stiffness of the thoracolumbar region and poor hindlimb impulsion. A high-resolution filter has been applied to the image. There is mild IRU in the summits of two spinous processes in the caudal thoracic region (arrows). However, five adjacent spinous processes were impinging, and infiltration of local anesthetic solution produced a profound clinical improvement. No soft tissue lesions were identified by ultrasonography.
Kissing spines can be found in performance horses with no clinical manifestations of back pain. Therefore the clinical significance of kissing spines must be carefully assessed. Kissing spines may also be present with another vertebral lesion, which may have a greater influence on prognosis; therefore a comprehensive evaluation of all structures should be performed, even if kissing spines have been identified. Radiological findings should be carefully correlated with the results of the physical examination and preferably with nuclear scintigraphic examination and the response to local analgesia.
Desmopathies: Supraspinous Ligament Injuries
Injuries of the supraspinous ligament occur most commonly between T15 and L3 and may be associated with palpable localized thickening and pain. Lesions are identified best by ultrasonography18,19; however, it is important to recognize that regions of altered echogenicity can be seen in some clinically normal horses.30
Thickening of the supraspinous ligament induces a local deformation (bump) of the dorsal profile of the thoracolumbar area, which can be measured by ultrasonography and compared with two adjacent equivalent locations. Lesions usually occur at a spinous process, sometimes extending between two adjacent spinous processes. The normal supraspinous ligament is uniformly echogenic (Figure 52-10). Hypoechogenic lesions in the deep and intermediate part of the supraspinous ligament (Figure 52-11) are compatible with recent or chronic desmopathies of the supraspinous ligament. Hyperechogenic foci, with or without acoustic shadows, may be seen in the supraspinous ligament. They reflect chronic or old desmopathy. Insertion desmopathy (enthesopathy) of the supraspinous ligament can be identified by irregularity of the surface of the spinous process, with a thicker appearance. Alteration of echogenicity and fiber orientation occurs in the supraspinous ligament.
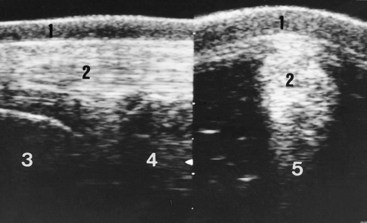
Fig. 52-10 Median (left) and transverse (right) ultrasonographic images of the normal supraspinous ligament in the lumbar area. 1, Skin; 2, supraspinous ligament; 3, second lumbar vertebra; 4, third lumbar vertebra; 5, interspinous ligament.
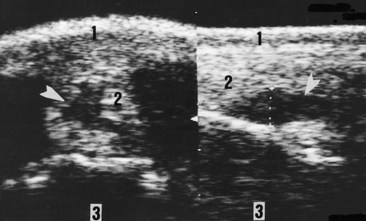
Fig. 52-11 Transverse (left) and median (right) ultrasonographic images indicate supraspinous desmopathy. The ligament is thickened and presents a central hypoechogenic zone (arrowheads). 1, Skin; 2, supraspinous ligament; 3, seventeenth thoracic spinous process.
With low-exposure radiographs, the soft tissue thickening and some focal radiopacities may be seen in horses with long-standing injuries. Avulsion fractures or bone modeling and increased opacity of the dorsal surface of the spinous processes may also be noted.29
Nuclear scintigraphic examination may reveal IRU in the summit of one or more spinous processes in association with insertional lesions of the supraspinous ligament.
Fractures of Spinous Processes
Fractures of the spinous processes usually occur in the withers region as the result of the horse falling over backwards. However, other traumatic episodes, such as the horse getting stuck under a dividing rail between two compartments of a trailer or lorry (van), may result in fractures of more caudally located spinous processes. Fractures of the withers are often displaced, resulting in a change in conformation. There is generally focal pain and swelling, as well as marked back stiffness. An affected horse moves in a restricted fashion, often plaiting the forelimbs. Diagnosis is confirmed by radiographic or scintigraphic examination. Although the radiological abnormalities may be dramatic, the prognosis is generally favorable with conservative management. A purpose-fitted saddle may be required to accommodate the change in the horse’s shape.
Articular Processes: Synovial Intervertebral Articulations
Normal Anatomy
The articular processes’ synovial intervertebral articulation complex is located dorsal to the vertebral canal and is composed of the caudal articular process of one vertebra, the joint space, and the cranial articular process of the following vertebra (Figures 52-12 through 52-14).17
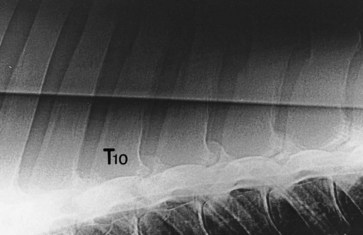
Fig. 52-12 Normal radiological appearance of the synovial intervertebral articulations in the midthoracic area. Cranial is to the left. T10, Tenth thoracic vertebra.
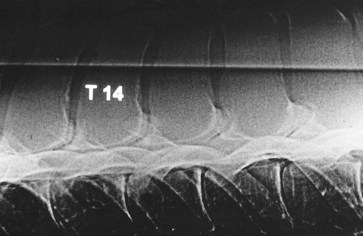
Fig. 52-13 Normal radiological appearance of the synovial intervertebral articulations in the caudal thoracic area. Cranial is to the left. T14, Fourteenth thoracic vertebra.
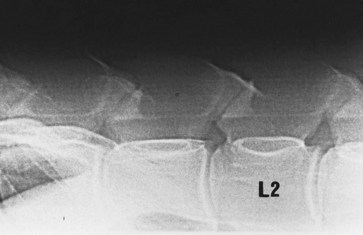
Fig. 52-14 Normal radiological appearance of the synovial intervertebral articulations in the lumbar area. Cranial is to the left. L2, Second lumbar vertebra.
On lateral radiographic images, in the middle of the film, the left and right synovial intervertebral articulations are superimposed. On the extremities of the film, the images of the left and right synovial intervertebral articulations are progressively dissociated because of the divergent x-ray beam. In some horses the ribs are extremely convex dorsally and are superimposed over the thoracic and the first lumbar synovial intervertebral articulations, prohibiting assessment. Oblique radiographic images from left to right and right to left permit evaluation of the left and right synovial intervertebral articulations independently.6 The radiolucent cartilaginous joint space is thin and more clearly defined in the thoracic areas, where the articular facets are flat (see Figure 52-12), than in the lumbar area because of the condylar shape. Between T12 and T16 the joint space is a wide V shape, with a cranial oblique branch and a shorter vertical caudal branch (see Figure 52-13). At the thoracolumbar junction and in the lumbar region the joint space is less well defined. Usually, the joint space is linear and makes a 40-degree angle with the horizontal (see Figure 52-14). The caudal articular process is dorsal to the corresponding intervertebral foramen and is triangular with a caudal apex in the lumbar region. The thickness of the dense subchondral bone of the cranial articular process increases caudally. The cranial articular process is extended dorsocranially by a mammillary process, which is larger in the thoracic area than in the lumbar area.
On transverse ultrasonographic images obtained using 2.5- to 5-MHz probes, the synovial intervertebral articulations can be imaged (Figure 52-15). On each side the joint space separating the cranial (lateral) and caudal (medial) articular process can be identified.19 This joint space is limited dorsally by a thin articular capsule. Comparison of the left and right synovial intervertebral articulations of the same intervertebral joint is helpful to assess size and shape.
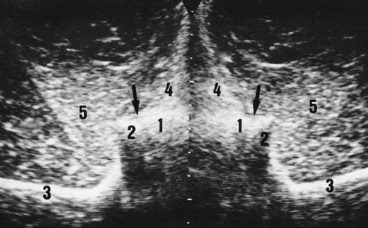
Fig. 52-15 Transverse ultrasonographic image of the synovial intervertebral articulations between the first and second lumbar vertebrae shows normal appearance (compare with Figure 52-3). 1, Caudal articular process of first lumbar vertebra; 2, cranial articular process of second lumbar vertebra; 3, transverse process of second lumbar vertebra; 4, multifidus muscle; 5, longissimus muscle; arrow, joint space of the epaxial synovial intervertebral articulation.
Abnormal Findings
Eight types of abnormal radiological findings associated with OA have been identified in the synovial intervertebral articulations of the equine thoracolumbar spine6,17 (Table 52-3). These findings were mainly present at the thoracolumbar junction and in the lumbar area. Types 2, 4, and 6 (Figures 52-16 to 52-19) were mainly found between T16 and L3. Types 5 and 7 have mainly been found in the lumbar area. However, lesions may occur anywhere from T9 to L5.6 Abnormalities have been found in mature riding horses and immature racehorses.
TABLE 52-3 Types of Radiographic Lesions of the Thoracolumbar Synovial Intervertebral Articulations
| TYPES | GENERAL CRITERIA | RADIOLOGICAL SIGNS |
|---|---|---|
| 1 | Asymmetry | No clear joint space; double joint space |
| 2 | Modification of opacity of the articular process | Increased radiopacity of the subchondral bone |
| Increased opacity of the synovial intervertebral articulations | ||
| 3 | Radiolucent areas in the subchondral bone | |
| Increased opacity of the articular process | ||
| 4 | Periarticular proliferation | Dorsal periarticular proliferation |
| Increased size of the synovial intervertebral articulations | ||
| Often associated with alteration in opacity of subchondral bone | ||
| 5 | Ventral periarticular proliferation | |
| 6 | Ankylosis | Dorsal bridge between two adjacent vertebrae |
| 7 | Osteolysis of the synovial intervertebral articulations | |
| No joint space | ||
| 8 | Fracture | Radiolucent line on the caudal (or cranial) articular process |
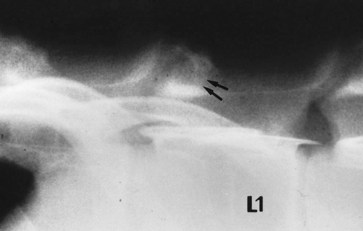
Fig. 52-16 Lateral radiographic image of the thoracolumbar junction. Cranial is to the left. There are type 2 lesions (arrows) of the synovial intervertebral articulations between the eighteenth thoracic and first lumbar vertebrae in this 5-year-old French trotter male. Compare with the opacity of the cranial articular processes in Figure 52-14. L1, First lumbar vertebra.
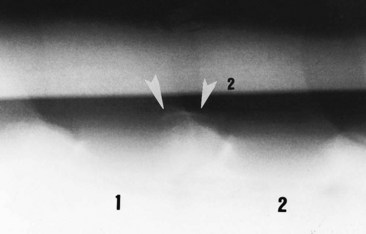
Fig. 52-17 Lateral radiographic image of the cranial lumbar vertebrae. Cranial is to the left. There is a mild (grade 1) type 4 lesion of the synovial intervertebral articulation complex between the first (1) and second (2) lumbar vertebrae in this 8-year-old mare.
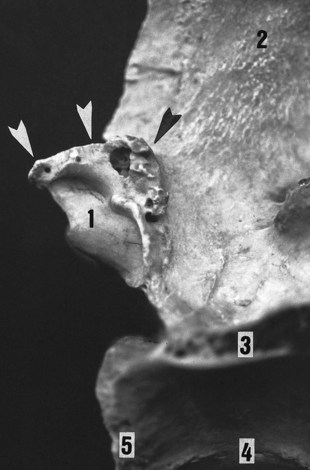
Fig. 52-18 Bone specimen showing a moderate (grade 2) type 4 lesion (arrowheads) of the caudal articular process of the third lumbar vertebra. 1, Caudal articular process; 2, dorsal spinous process; 3, transverse process; 4, vertebral body; 5, vertebral fossa.
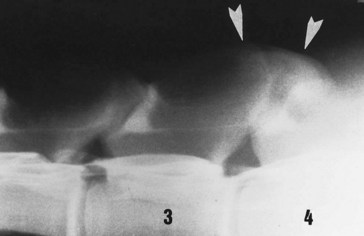
Fig. 52-19 Lateral radiographic image of the midlumbar vertebrae. Cranial is to the left. There is a severe (grade 3) type 4 lesion (arrowheads) of the synovial intervertebral articulation between the third (3) and fourth (4) lumbar vertebrae in this 12-year-old mare.
Dorsal periarticular proliferation (types 4 and 6) can be imaged with ultrasonography, and with this procedure determining whether the proliferation is symmetrical or, if not, which side is the most affected is possible (Figure 52-20).
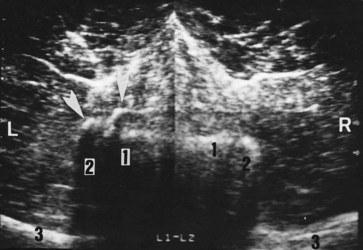
Fig. 52-20 Transverse ultrasonographic image of the synovial intervertebral articulation between the first and second lumbar vertebrae in a 5-year-old French trotter mare: on the left side (L) a dorsal periarticular osteophyte is present (arrowheads). 1, Caudal articular process of first lumbar vertebra; 2, cranial articular process of second lumbar vertebra; 3, transverse process of second lumbar vertebra.
Nuclear scintigraphy can be helpful in identifying evidence of abnormal bone modeling in the region of synovial intervertebral articulations, especially in horses where radiological appraisal is limited by the ribs. There was a strong association between the presence of moderate or intense IRU and radiological abnormalities in a study of 65 horses with back pain and radiological evidence of OA, whereas in 31 horses with no evidence of back pain RU was generally normal.25
In our experience, synovial intervertebral articulation lesions are much more consistently associated with back pain than are kissing spines. However, in a series of 644 horses with thoracolumbar region pain, only 77 (12%) had OA of the synovial intervertebral articulations, 47 of which had concurrent impinging or overriding dorsal spinous processes.6
Vertebral Bodies and Disks of the Thoracolumbar Region
Lesions of the vertebral bodies are less commonly found in horses28 and cannot be imaged by ultrasonography in the thoracolumbar area (except caudal to L4 with a transrectal approach). These lesions include the following17,28,31,32:
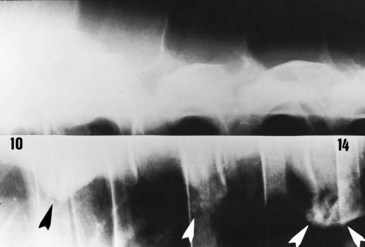
Fig. 52-21 Lateral radiographic image of the vertebral bodies of the caudal thoracic vertebrae. Cranial is to the left. There is extensive ventral spondylosis (arrowheads) between the tenth (10) and fourteenth (14) thoracic vertebrae in this 13-year-old international show jumper stallion.
These lesions have been found in horses with a history or clinical manifestations of back pain—acute, intermittent, and chronic—and are considered to be of likely clinical significance. However, spondylosis also is an incidental finding in low-level performance horses with no history or clinical manifestations of back pain. Spondylosis was identified in 23 of 670 (3.3%) horses with back pain, usually occurring between T10 and T14.26 There was a range of one to five lesions (mean 2.3). However, only nine of the 23 horses had spondylosis as the sole osseous lesion; the remainder also had impingement of the dorsal spinous processes and/or OA of the synovial intervertebral articulations. Nuclear scintigraphy may help to identify spondylosis and to elucidate the clinical significance of these findings in horses with back pain; however, not all lesions have IRU. In 17 of 23 horses with spondylosis that underwent scintigraphic evaluation, 64.7% had IRU associated with spondylosis, but only 33.3% of horses with lesions identified radiologically had IRU.26 Extensive spondylosis may potentially limit back mobility, despite the absence of IRU.
Fracture and/or subluxation of a thoracolumbar vertebral body normally results in neurological abnormalities, but occasionally horses have acute severe back pain, with rapid atrophy of the epaxial musculature, but no evidence of ataxia.
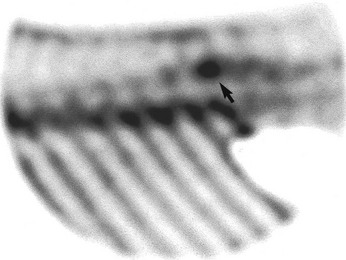
Vertebral laminar stress fractures have been identified using nuclear scintigraphy in young TB flat race horses with loss of performance and clinical evidence of back pain (Figure 52-22). They have been seen most commonly at the thoracolumbar junction and in the lumbar vertebrae. In a post mortem sample of TB race horses, 18 (50%) of 36 specimens had evidence of vertebral stress fractures.33
The Lumbosacral Joint
The lumbosacral joint (see also Chapter 50) and the intertransverse joints are evaluated ultrasonographically per rectum. Clinically significant abnormalities include21:
Prognosis
The prognosis for horses with any back lesion depends on a number of factors, including the individual pain tolerance of the horse, the skill of the rider and trainer, the discipline in which the horse is involved, and the type, number, and severity of lesions. Vertebral lesions are tolerated better by flat race horses than by Three Day Event horses, show jumpers, and dressage horses. Racing trotters tolerate vertebral lesions poorly. The prognosis for each lesion is not influenced by the level of work but more by the rider’s or trainer’s ability to exploit the horse despite its problems. A horse with an acute isolated supraspinous ligament injury has a good long-term prognosis, whereas horses with restricted mobility of the back caused by extensive kissing spines or type 6 or 7 synovial intervertebral articulation lesions have a poor prognosis. Horses with grades 3 and 4 dorsal kissing spines have a guarded prognosis, as do those with ventral kissing spine lesions. The prognosis for horses with synovial intervertebral articulation lesions depends on severity and the number of joints affected. Horse tolerance of ventral thoracic spondylosis seems to vary more, but generally the larger the number of vertebrae affected, the poorer the prognosis.
Specific Management
The general aims of management of back problems are to remove pain and to make the horse as comfortable as possible, as soon as possible, to allow it to be exercised to avoid further muscle loss and to promote muscle function and strength. Medical treatment aims to remove pain and muscle spasm.
Systemic Treatment
Treatment of horses with back pain with nonsteroidal antiinflammatory drugs (NSAIDs) usually has disappointing results. Many horses are brought in for in-depth investigation of the cause of back pain because of lack of response to treatment with phenylbutazone or other NSAIDs. Treatment of muscle spasm with myorelaxants is indicated and sometimes useful; for example, thiocolchicoside (2 to 4 mg/100 kg twice weekly for 4 weeks) and methocarbamol (10 mg/kg intravenously). Repeated treatments may be necessary.
Intravenous infusion of tiludronate has resulted in improvement in clinical signs associated with OA of the synovial intervertebral articulations37 and may also be indicated for treatment of osseous abnormalities associated with the lumbosacral joint.
Local Injections
Local perispinal or interspinal injections of corticosteroids, sometimes in association with myorelaxants or Sarapin (High Chemical Company, Levittown, Pennsylvania, United States), are used to treat horses with kissing spines: flumethasone (0.5 to 1 mg/injection site with a maximum total dose of 4 mg); dexamethasone (isonicotinate, 1.5 to 2.5 mg/injection site, with a maximum total dose of 10 mg); or methylprednisolone acetate (40 to 60 mg/injection site, with a maximum total dose of 200 mg).
Horses with OA of the synovial intervertebral articulations are treated by deep paramedian injections of corticosteroids (see the previous discussion) into the multifidus muscle on each side at the level of the lesion, 2 cm apart from the median plane, using 9- to 11-cm needles. These local injections are best performed using ultrasonographic guidance (Figure 52-23). Injections are made into the multifidus muscles that provide proprioceptive information on intervertebral movements. Therefore we suggest that the use of Sarapin is contraindicated in this situation. Local infiltrations can be performed alone or with mesotherapy.
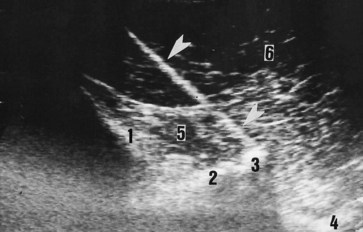
Fig. 52-23 Transverse ultrasonographic image showing an ultrasound-guided periarticular injection for the treatment of synovial intervertebral articulation arthropathies. The probe is placed on a paramedian position; thus the image is slightly oblique. 1, Spinous process; 2, caudal articular process of first lumbar vertebra; 3, cranial articular process of second lumbar vertebra; 4, transverse process; 5, multifidus muscle; 6, longissimus muscle; arrowheads, needle.
Horses with lesions of the lumbosacral joint are treated by deep paramedian injection of corticosteroids with Sarapin or local anesthetic solution under ultrasound guidance.21 The needle is inserted 4 cm from the median plane on a line connecting the cranial aspects of the tubera coxae. The needle is directed obliquely caudally and is inserted under the ilial wing until contact is made with bone in the vicinity of the axial aspect of the lumbosacral intertransverse joint. This is repeated on the left and right sides.
Mesotherapy
Mesotherapy is a technique that has been used for more than 40 years in France and consists of intradermal injections with short and thin needles (5 mm long) in the dermatomes corresponding to the site(s) of the lesion(s).
The principle is based on the theory of the gait control of pain, which takes place in the dorsal horn of the spinal cord. According to this theory, which is currently controversial, type I and II nerve fibers coming from the skin have collateral fibers that can inhibit the conduction of information in the spinothalamic fasciculus, transmitting painful information from deep structures of the same spinal segment to the thalamus and cerebrum.
After aseptic preparation of the skin, mesotherapeutic injections are usually made using a local anesthetic solution (lidocaine, 140 mg), a short-acting corticosteroid (dexamethasone, 15 mg), and a myorelaxant (thiocolchicoside, 20 mg). Injection with only saline solution may also have beneficial effects. Because most horses are sensitive to the procedure, the horse is placed in stocks, and the use of a twitch and sedation are recommended. A multiinjector (Coveto, Montaigu, France) is used. These intradermal injections are performed at the level of the lesion and caudal to it, taking into account the caudal orientation of the segmental nerves. For example, if one is treating kissing spines between T10 and T15, the treated region extends from T10 to L1. If the lesions involve the synovial intervertebral articulation between T17 and L2, the treated area should extend between T17 and the lumbosacral junction. If lesions are at the lumbosacral junction, the treated area should extend caudally to the croup. Two to three rows of injections are made on each side of the median plane.
After local injections or mesotherapy, the horse is restricted to light work on the lunge, without a surcingle, for 3 days. Normal training is progressively resumed over 5 days. A substantial improvement is anticipated within 7 to 14 days. If improvement is limited, mesotherapy should be repeated 2 to 3 weeks after the first treatment. The expected duration of action varies between 3 and more than 12 months. In horses with chronic pain, ideally a maximum of two local infiltrations should be performed each year with, or alternately with, mesotherapy.
Acupuncture
Acupuncture can be useful for treating chronic pain in some horses (see Chapter 92); however, relief of clinical signs may only be short term.34
Training Management
With the medical treatment to reduce pain, modification of the training program is an essential part of the management of back problems.35 The aims of the exercise management are to avoid further muscle atrophy and to develop the back proprioceptive control and intervertebral stability. Rest is contraindicated, except in untreatable horses that are not improved by any kind of treatment and management. The general recommendations include the following:
Some physical exercises, such as lowering of the neck (flexion of the cervicothoracic junction), may have a therapeutic value because they induce an associated thoracic flexion, which provides more support to the weight of the rider. A separation of the spinous processes reduces the contact between them.35,36 An elongation of the strong epaxial muscles reduces muscle contraction.35
Exercises to increase hypaxial muscle strength may also be of clinically significant benefit.
Alternative Medicines
Much interest exists in using alternative therapeutic techniques to manage back pain in horses. Once a clear diagnosis is established, alternative techniques, if appropriately applied and objectively assessed for each pathological entity, may be useful adjunctively in managing horses with back pain (see Chapters 93 through 96). Collaboration with a specialized physiotherapist or chiropractor may be of major benefit.
Surgery
Surgical treatment of kissing spines by resection of the summit of one or more spinous processes has been successful in some horses that had not responded to conservative management.39-42 Case selection is important and should be restricted to horses with lesions only involving the dorsal aspect of the spinous processes, without other clinically significant osseous abnormalities. A postoperative convalescent period of 6 months is generally required. Twenty-seven of 50 Warmblood horses (54%) used for dressage or show jumping returned to full athletic function at the previous level of performance.39 One hundred fifty of 209 horses (72%) used for various disciplines returned to full work after removal of the summits of one to six dorsal spinous processes, although the level of work was not specified.40 There was no significant difference between the number of spines removed and the outcome; however, in the authors’ experience, the greater the number of spinous processes affected, the more guarded the prognosis for return to full athletic function as a sports horse.