Chapter 50Lumbosacral and Pelvic Injuries in Sports and Pleasure Horses
Anatomical Considerations
Detailed anatomy of the ilium, ischium, pubis, sacrum, coxofemoral joint, sacroiliac joints, nerves, and major vessels is described elsewhere (see Chapters 49, page 564, and 51, page 583). The lumbosacral joint comprises five separate joints: the intercentral joint between the caudal aspect of the vertebral body of the sixth lumbar vertebra and the sacrum, between which is an intervertebral disk; two intertransverse joints; and two synovial intervertebral articulations between the articular processes of the sixth lumbar vertebra and the cranial articular processes of the sacrum. Movement is principally restricted to flexion and extension because of the large transverse processes.1 Congenital variations in anatomy can be seen, including fusion of the fifth and sixth lumbar vertebrae or sacralization of the sixth lumbar vertebra resulting in lumbosacral ankylosis. These result in stress concentration on adjacent joints. The biomechanical stresses of movement of the lumbosacral joint place particular compression and traction forces on the intervertebral disk, which may predispose to disk degeneration.
Clinical Signs
History
Pelvic injury in a mature athletic horse is a comparatively unusual cause of lameness, except as the result of trauma from a fall, rearing and falling over backward, becoming cast in the stable, or sustaining an injury during transport. When the horse has no history of trauma, diagnosis can be difficult, and excluding all possible sources of pain in the distal aspect of the limb is frequently necessary before focusing on the pelvic region.
Horses with clinically significant pathological conditions of the lumbosacral or sacroiliac joints frequently have a history of progressive reduction in performance, difficulty engaging the hindlimbs, and poor hindlimb impulsion, especially when ridden.2,3
Clinical Examination
Clinical assessment of individual structures of the pelvic region by visual examination and palpation is not easy, especially in Warmblood and draft breeds, because of the large muscle mass of the hindquarters. Frequently, only the tubera coxae and tubera sacrale can be palpated. Large muscle mass may prohibit palpation of the greater trochanter of the femur. Atrophy of the hindquarter musculature is nonspecific and can reflect disuse because of pain arising anywhere in the limb, although atrophy of the muscles around the tail head often reflects injury to the tuber ischium or local nerve damage. Asymmetry of the height of the tubera sacrale is a common finding in horses in full work, free from lameness, although it may be seen along with poor performance or alterations in hindlimb gait. Apparent asymmetry may actually reflect differences in size of the dorsal sacroiliac ligaments. Alteration in muscle mass in the proximity of the tubera sacrale superficially can give a false impression of asymmetry of the tubera sacrale. Asymmetry of the tubera coxae may reflect a previous injury unassociated with ongoing pain. Poor muscle development in the lumbar region and over the hindquarters may make the tubera sacrale and the summits of the dorsal spinous processes of the lumbar vertebrae appear abnormally prominent. This should alert the clinician to the possibility of thoracolumbar or pelvic pain; however, this finding is nonspecific and may reflect the horse’s work history.
The pelvic region should be appraised visually and palpated systematically, and although preliminary assessment is usually best performed in the stable, for accurate evaluation of symmetry of the musculature and bony elements of the pelvic region the horse should be standing completely squarely behind on a firm, level surface with the horse looking straight ahead. In a horse with severe lameness this may not be possible because the horse may be unwilling to load the lame limb fully. Careful differentiation should be made between muscular and bony asymmetry. Muscle atrophy can make accurate assessment of symmetry of the pelvic bones difficult. To evaluate accurately the levelness of the tubera coxae, two assistants each must place an index finger on the craniodorsal aspect of each tuber coxae and extend the finger horizontally, or the tubera coxae should be marked using tape. Elevation of the tail may be necessary to identify muscle atrophy around the tail head, which may be seen along with nerve damage, or injuries of the ipsilateral tuber ischium.
Assessment of symmetry when the horse is unwilling to bear weight evenly on both hindlimbs is not easy, but particular attention should be paid to the way in which the limb is positioned. An abnormally straight limb may reflect luxation of the coxofemoral joint and secondary upward fixation of the patella. The greater trochanter of the femur of the lame limb may appear higher than that of the contralateral limb.
The muscles of the lumbar and pelvic regions should be assessed carefully to identify any area of abnormal muscle tension, pain on palpation, or unusual firmness. Firm stroking of the muscles first with a finger and then with a blunt-ended object (e.g., artery forceps) is useful to determine whether muscle spasm or muscle fasciculation is induced. Palpation of the caudal muscles of the thigh is also important because abnormal pain or tension can reflect primary muscle injury or an injury of the ipsilateral tuber ischium.
Firm pressure should be applied to the bony prominences to see whether pain or an abnormal reaction, such as sinking on the hindlimbs when pressure is applied to the tubera sacrale, can be induced. Both tubera coxae should be grasped simultaneously and the horse rocked from side to side to determine whether crepitus can be detected by palpation or auscultation, bearing in mind that the absence of crepitus does not preclude a fracture. Pull the tail while holding one hand over the coxofemoral joint; palpable crepitus may reflect a fracture, severe osteoarthritis (OA), or subluxation of the joint.
Careful, systematic examination of the pelvic canal region per rectum is also indicated to assess the aorta and iliac arteries, psoas musculature, the lumbosacral joint, the caudal aspect of the ilial shaft, and the pubis and ischium.
Pelvic injuries should also be considered when a clinician examines a recumbent horse that has fallen over a fence. Palpation of the pelvic region is even more difficult in these circumstances. Even with a severe fracture, palpating any abnormality may be impossible. The clinician should bear in mind that in the acute phase, local reflexes such as the patellar reflex and the withdrawal reflex may be suppressed, which does not necessarily reflect a spinal cord injury. Major fractures may be associated with rupture of one or more large vessels, resulting in potentially fatal internal hemorrhage. Thus it is important to assess the recumbent horse as a whole, monitoring pulse rate, color of mucous membranes, and capillary refill time. Increased pulse rate and progressive pallor of the mucous membranes are good indicators of major vessel rupture, such as laceration of the iliac artery after fracture of the ilial shaft.
Manipulation of the limb may be resented if pain is associated with the coxofemoral joint, but generally the responses to flexion of the limb, protraction, retraction, and abduction are rather nonspecific. A horse with pain associated with the sacroiliac joints or a coxofemoral joint may be reluctant to stand on one limb, with the other limb raised, and may behave awkwardly in anticipation of discomfort. However, the reaction is nonspecific, and one must bear in mind that some horses present difficulties in picking up the hindlimbs in the absence of any sign of lameness or poor performance. Difficulties in picking up hindlimbs may be caused by reluctance to accentuate weight bearing on the lamest limb, reluctance to flex the lame limb, or may be psychological. If the horse is a shiverer, unilaterally or bilaterally, the response to hindlimb flexion can be difficult to assess.
The degree and character of lameness depend on the underlying cause. Fracture or luxation of the coxofemoral joint results in acute-onset severe lameness. Lameness associated with other lesions in the pelvic region may vary in degree, not only among horses with similar lesions but also within and between examination periods. Pain from the coxofemoral joint frequently results in the horse moving on three tracks, with the nonlame limb being placed between the two forelimbs. On the lunge the horse may be inclined to break to canter rather than move with adequate hindlimb impulsion, but this is not specific for pelvic pain and is typical of many horses with hindlimb lameness. Pain associated with the coxofemoral joint or the greater trochanter of the femur sometimes results in the horse carrying the lame limb in canter. Lesions associated with the sacroiliac joints frequently result in the horse crossing over each hindlimb at the trot (i.e., plaiting), but this is not pathognomonic, and some horses move with a base-wide hindlimb gait![]() .2 The horse may move with reduced hindlimb impulsion rather than overt lameness. Although acute fractures of the tuber ischium invariably cause lameness, chronic injuries may result in loss of performance (e.g., jumping to the right) rather than overt lameness.
.2 The horse may move with reduced hindlimb impulsion rather than overt lameness. Although acute fractures of the tuber ischium invariably cause lameness, chronic injuries may result in loss of performance (e.g., jumping to the right) rather than overt lameness.
The response to flexion tests is nonspecific. The clinician should bear in mind that increased weight bearing on one limb, caused by flexing the contralateral limb, may accentuate lameness in the weight-bearing limb. Turning the horse in small circles, inducing rotational forces on the coxofemoral joint, may accentuate lameness associated with the coxofemoral joint.
Ridden exercise is invaluable in horses with a history of poor performance, reduced hindlimb impulsion, or low-grade lameness because frequently the lameness or restriction in hindlimb gait is accentuated. This may be most obvious in deep footing. Some horses with sacroiliac joint region pain or lumbosacral region pain show extreme reluctance to go forward freely. Affected horses may feel to the rider much worse than they appear to a trained observer. However, care must be taken to differentiate these horses from those with bilateral hindlimb lameness, thoracolumbar pain, or recurrent low-grade exertional rhabdomyolysis and those performing poorly because of the rider (see Chapter 97), previous poor schooling, or a combination of boredom and an unwilling temperament.
Analgesic Techniques
In horses with chronic lameness, reduced hindlimb impulsion, or poor performance, excluding the distal aspect of the limb as a source of pain by performing perineural analgesia of the fibular and tibial nerves and intraarticular analgesia of the three compartments of the stifle joint may first be necessary. If the response is negative, intraarticular analgesia of the coxofemoral joint may be indicated. This is relatively straightforward to perform if the horse is not well muscled and the greater trochanter of the femur is readily palpable. However, in the majority of heavily muscled, mature competition horses, needle placement must be guided by ultrasonography.4 Even if the needle is accurately positioned, retrieval of synovial fluid may be difficult. Extraarticular deposition of local anesthetic solution may result in transient paralysis of the obturator nerve and instability of the limb. The technique is described in Chapter 10.
Intraarticular injection of the sacroiliac joint cannot be achieved; however, infiltration of local anesthetic solution around the sacroiliac joint region may result in dramatic clinical improvement, presumably by alleviation of pain associated with the joint and periarticular structures. It cannot be considered an entirely specific technique and potentially could also influence pain from the lumbosacral joint and local nerve roots. The techniques are described on page 589. Infiltration of local anesthetic solution around the sacroiliac joint regions resulted in significant improvement in 95 of 108 horses with clinical signs suggestive of sacroiliac joint pain.5 Horses were reassessed ridden 15 minutes after injection. If local anesthetic solution is placed too far caudally there is the possibility of inducing sciatic nerve paralysis either unilaterally or bilaterally. In my experience, this is extremely rare (<2%), but if bilateral, the horse will become recumbent and may remain so for up to 3 hours before returning to normality.5
Serum Muscle Enzyme Concentration
Measuring serum concentration of creatine kinase (CK) and aspartate transaminase (AST) is invaluable for diagnosing horses with acute and chronic rhabdomyolysis (tying up). In horses with chronic tying up, comparing resting levels with concentrations reached after maximum exercise may be necessary. Peak levels of CK are likely to occur 3 hours after exercise. If a horse has had a tying-up episode within the past 4 or 5 days, AST levels almost invariably will be increased. Some horses with chronic recurrent problems have constantly elevated levels of CK and AST. The degree of elevation of muscle enzyme concentrations may show a poor correlation with the severity of clinical signs.
Diagnostic Imaging
Radiography
Radiographic examination of the pelvic region of a horse, anesthetized and positioned in dorsal recumbency or in the standing position, is described in depth elsewhere.6 Since the advent of nuclear scintigraphy and diagnostic ultrasonography the indications for radiographic examination have decreased. If the source of pain has been localized to the coxofemoral joint, radiographic examination is indicated to determine the nature of the pathological condition and hence prognosis. High-quality radiographs can only be obtained with the horse positioned in dorsal recumbency under general anesthesia. Evaluation of the sacroiliac joints can be difficult because of the superimposition of abdominal viscera. Identification of new bone formation on the caudal aspect of the joint and irregular joint space width are poor prognostic indicators. Nuclear scintigraphic examination gives accurate information about bone turnover, but anatomical detail is less well defined. Therefore radiography of a horse with a suspected acetabular fracture may be indicated at least 6 weeks after the onset of lameness to determine whether a suspected fracture involves the coxofemoral joint, which merits an extremely guarded prognosis for return to full athletic function in a mature horse.
Radiographs of the coxofemoral joint, caudal aspect of the ilial shaft, and the ischium obtained in the standing position may be satisfactory for confirmation of luxation or major fractures of the joint.6 A dorsal 50° proximal medial–ventrodistal lateral oblique image can be used to assess the integrity of the tubera coxae in a standing horse.7
Ultrasonography
Diagnostic ultrasonography of the pelvic region can be performed transcutaneously or per rectum.8,9 The choice of transducer frequency depends on the structures to be imaged. Transcutaneous evaluation of the bony elements of the pelvis and the deep musculature requires a 5- or 3.5-MHz transducer, depending on the size of the horse, whereas evaluation of the dorsal sacroiliac ligaments, sublumbar musculature, ventral aspect of the lumbar and sacral vertebrae, and aorta and iliac arteries is better performed using a 5- or 10-MHz transducer. Evaluation of nerve roots per rectum may be best achieved using a 10- to 12-MHz transducer.
Diagnostic ultrasonography is useful in evaluating fractures (see Chapter 49, page 564), assessing muscles (see Chapter 83) and the sacroiliac ligaments (see page 578), determining blood vessel patency (see page 581), assessing the lumbar vertebrae and articulations, and evaluating nerve roots.
Nuclear Scintigraphy
Nuclear scintigraphic evaluation of the pelvic region is useful for identifying fractures, stress reactions in bone, increased bone modeling associated with OA and other bony lesions, and evidence of rhabdomyolysis; for evaluating blood flow in the aorta, iliac, and femoral arteries; and for assessing the sacroiliac joints.10 Sensitivity of the technique in part depends on the angle of the gamma camera to the area of interest and the degree of overlying muscle mass. It is important to recognize that some lesions may be bilateral; therefore recognition of the normal scintigraphic appearance of the region in horses of different ages and different disciplines is important. The clinician should bear in mind that superficial bony structures such as the tubera coxae and tubera sacrale always have apparently greater radiopharmaceutical uptake (RU) than deeper structures. Unilateral muscle atrophy and shape of the pelvis may also confound interpretation.10-14
Radioactive urine in the bladder may complicate interpretation; therefore the judicious use of furosemide to induce urination before examination is essential.
Complete evaluation of the pelvic region requires dorsal images of the sacroiliac joints, oblique images of the ilial wings, caudodorsal and caudal images of the tubera ischii, and lateral and caudolateral images of the coxofemoral joints. Care must be taken in interpreting the appearance of the sacroiliac joints because age-related changes occur in normal horses.10-15 Swaying movement of the horse during image acquisition can result in images that mimic abnormalities, and using motion correction software is invaluable.
Differential Diagnosis
Fractures
Clinical features, diagnosis, and treatment of fractures of the pelvis in the young Thoroughbred (TB) racehorse have been dealt with in depth (see Chapter 49), and this section focuses on differences in mature athletic horses. The incidence of stress or fatigue fractures of the pelvic region in the mature horse is low, except in horses that race over fences, which have a substantial incidence of ilial stress fractures. The clinical features are similar to those in the young racehorse (see Chapter 49), although there is a higher prevalence of horses with fractures extending into the ilial shaft that have a guarded prognosis. The majority of other fractures result from external trauma.
Tuber Ischium
Trauma to or fractures of the tubera ischii sometimes occur in event horses that fall when jumping up onto a bank, may also occur in any horses as a result of a fall on the flat, and also have been recognized in horses from other disciplines with no known history of trauma.17-19 Lameness is usually acute in onset and severe. Mild localized swelling is easily overlooked unless the tuber ischium is suspected as a site of injury. The ipsilateral semimembranosus and semitendinosus muscles are usually sore to palpation. Atrophy of the muscles around the tail head often develops within 7 to 10 days. Usually crepitus is not palpable. In horses with chronic lameness, pain on palpation may not be evident, although the tubera ischii may appear asymmetrical, and the lameness may be only mild or moderate.
Diagnosis of a fracture of the tuber ischium can be confirmed using nuclear scintigraphy (Figure 50-1). Dorsal oblique and caudal images are useful. Usually increased radiopharmaceutical uptake (IRU) and an abnormal pattern of uptake are apparent.16 In some horses determining whether the fracture is complete and whether it has become substantially displaced may be possible. It is important to recognize that IRU may persist for many years after injury, and therefore the results of scintigraphic examination must be carefully correlated with the results of clinical examination.19 Discontinuity of the bone outline may also be confirmed using diagnostic ultrasonography. Limited radiographic examination can be performed in a standing horse, but it is most easily and safely done with the horse under general anesthesia. Less commonly there is entheseous reaction with IRU in both the tuber ischium and the ipsilateral semimembranosus and/or semitendinosus muscles. Ultrasonographic examination may demonstrate irregularity of the tuber ischium and decreased or increased echogenicity of the injured muscles depending on the acuteness or chronicity of injury.
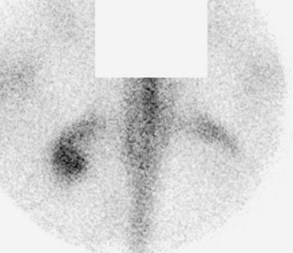
Fig. 50-1 Caudal scintigraphic image of a 7-year-old part Shire riding horse with acute-onset left hindlimb lameness after falling over while being shod. There was no response to tibial and fibular nerve blocks or to intraarticular analgesia of all three compartments of the stifle joint. There is an abnormal pattern of radiopharmaceutical uptake and increased radiopharmaceutical uptake in the left tuber ischium consistent with a displaced fracture of the tuber ischium, which was confirmed using ultrasonography.
Treatment by restriction to box rest usually results in a satisfactory outcome, although occasionally sequestration of the fracture fragment occurs, necessitating surgical removal.
Occasionally a horse shows no obvious lameness, but it has reduced performance and a tendency to jump drifting consistently to one side because of pushing off unevenly with each hindlimb. This symptom is associated with reduced muscle development over one of the tubera and IRU in the tuber ischium (see Figure 12-4). The outline of the tuber ischium appears irregular in an ultrasonographic image.
Ilial Wing and/or Shaft
Fractures of the ilial wing and/or shaft are unusual in mature sports horses and are almost invariably the result of a heavy fall when jumping and may be catastrophic if the fracture(s) becomes displaced and results in laceration of the iliac artery and fatal hemorrhage. Initial diagnosis is challenging because the horse is invariably recumbent and may mimic a severely winded horse, which may remain down for 30 to 45 minutes. There may be remarkably few signs of pain considering the severity of injury. If the horse is in lateral recumbency with the affected limb down, the horse may be unable to make any attempt to get up. Examination per rectum may facilitate a diagnosis. In my experience, most of such fractures have been fatal. Monitoring pulse and respiratory rates and color of the mucous membranes is the best method of diagnosing potentially fatal hemorrhage.
Tuber Coxae
Fractures of a tuber coxae in sports and pleasure horses have little difference to those in racehorses (see Chapter 49). The prognosis is usually favorable, with 27 of 29 horses (93%) returning to full athletic function.7 Horses with partial fractures of the cranial or caudolateral aspects of a tuber coxae returned to use more quickly than horses with complete transverse, longitudinal, or oblique fractures (mean 3 months vs. 6.5 months).
Greater Trochanter of the Femur
Fracture of the greater trochanter of the femur is an unusual injury causing severe lameness. The fracture fragment is often displaced cranially because of the pull of the attachments of the deep and middle gluteal muscles.
Usually no localizing clinical signs are apparent unless the horse is poorly muscled and the greater trochanter is readily palpable. The diagnosis is based on nuclear scintigraphic examination, with or without diagnostic ultrasonography. The prognosis for return to athletic function with conservative treatment is guarded.
Sacrum
Fractures of the sacrum may be complete or incomplete and result in bilateral hindlimb lameness. If the fracture is complete, the contour of the hindquarters when viewed from the side changes, so that the rump has abnormal angulation (Figure 50-2). Associated neurological signs include flaccid paralysis of the tail, reduced sensation around the tail head, urine dribbling in a mare, and loss of anal tone. The onset of neurological signs may be delayed for several weeks after the primary fracture. The fracture may be palpable per rectum. The fracture may be confirmed radiologically and using diagnostic ultrasonography per rectum. The prognosis for return to athletic function is guarded, although horses with more caudal fractures have made a complete functional recovery. Fractures of the femur are considered in Chapter 47.
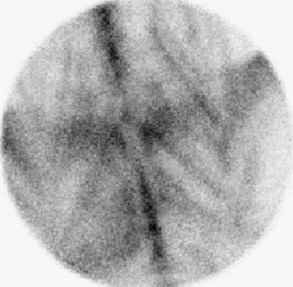
Fig. 50-2 Dorsal bone phase scintigraphic image of the pelvic region of a 12-year-old Thoroughbred mare, a former winner of the European Three Day Event Championships. The mare had shown slight but clinically significant loss of performance with no overt lameness. She had never shown any signs typical of classical tying up. There are linear stripes of abnormal radiopharmaceutical uptake in the gluteal muscles, which also were seen in the psoas, biceps femoris, and semitendinosus and semimembranosus muscles. This is compatible with recurrent exertional rhabdomyolysis and was associated with persistently elevated levels of creatine kinase and aspartate transaminase.
Equine Rhabdomyolysis (Tying Up)
Equine rhabdomyolysis is considered in depth elsewhere (see Chapter 83). This section focuses on aspects of diagnosis and differential diagnosis of lameness associated with the hindquarters and pelvic injuries in sports horses used for different disciplines and is restricted to recurrent exertional rhabdomyolysis (RER).
The spectrum of clinical signs associated with RER is enormous. A horse may have mild bilateral hindlimb stiffness or loss of freedom of action that may deteriorate slightly with work, without the horse becoming unduly distressed, but the horse sometimes requires a prolonged recovery period after work. Such horses may have no palpable firmness of the hindquarter musculature or pain induced by firm palpation and a normal pattern of sweating. The horse may be able to compete but performs below expectations. These clinical signs are not unique to exertional rhabdomyolysis and may be seen in horses with severe thoracolumbar discomfort associated with impinging dorsal spinous processes, pain associated with the sacroiliac joints, or bilateral hindlimb lameness. Some horses show progressive agitation during ridden exercise and awkwardness to ride, without recognition of a gait abnormality. Careful clinical evaluation usually reveals a progressive shortening of stride.
Alternatively, a horse may start to jump poorly during, for example, the cross-country phase of a Three Day Event and pull up with a unilateral hindlimb lameness, with no localizing clinical signs, that resolves within 24 hours. In contrast, a different horse may have recurrent acute-onset, severe episodes—often provoked by competition, for example, during the cross-country phase of a Three Day Event—that may be so bad as to result in recumbency. An endurance horse may demonstrate unilateral or bilateral hindlimb lameness at the final vet gate but show no typical signs of tying up.
The incidence of RER depends to some extent on the discipline in which the horse is involved, occurring most commonly in racehorses (see Chapters 83, 106, and 107), endurance horses (see Chapter 118), and event horses (see Chapter 117). RER is unusual in show jumpers and dressage horses but occasionally occurs in competitive TB-type ponies. In all these horses, the results of muscle biopsies usually indicate no evidence of abnormal glycogen metabolism as in polysaccharide storage myopathy, which occurs more commonly in draft and draft crossbreeds and Quarter Horses. In the TB, evidence indicates that RER may be a heritable condition, as an autosomal recessive trait with variable expression.20 A familial trait has also been observed in some part-TB event horses. However, RER in many event and endurance horses does not become apparent until the horse is middle aged, or even older. The condition is manifest more frequently in mares than in stallions or geldings.
Diagnosis is based on measuring elevated serum muscle enzymes (CK and AST) after exercise (see page 573). The degree of muscle enzyme elevation frequently does not correlate with the severity of clinical signs. Interpretation is not always straightforward because asymptomatic endurance horses frequently have extremely high levels of CK and AST during and after a ride. Horses with low-grade RER, which occurs daily, often have constantly elevated levels of CK and AST, even if rested.
Nuclear scintigraphy can be useful in horses with low-grade hindlimb stiffness and poor performance to validate a diagnosis of suspected RER,10,21 to evaluate blood flow to the hindlimb musculature,22 and to exclude any other concurrent musculoskeletal lesions. In association with RER in some but not all horses, abnormal uptake of 99mTc–methylene diphosphonate occurs in the affected muscles in the bone phase of the scan, appearing usually as linear streaking (see Figure 50-2), but in horses with more severe, long-standing RER, affected muscles may show large areas of intense IRU. Lesions are not restricted to the gluteal muscle mass, but they may also affect quadriceps, biceps femoris, semitendinosus, semimembranosus, psoas, and longissimus dorsi muscles. Lesions may be symmetrical or asymmetrical. However, normal RU does not exclude RER.
Muscle biopsy is used to determine whether any evidence exists of polysaccharide storage myopathy. Feeding horses a high-fat and low-carbohydrate diet may reduce the frequency and severity of attacks after a period of 3 to 6 months.23
Measuring fractional excretion of electrolytes (sodium, potassium, calcium phosphorus, and chloride) can be useful to identify those horses that seem unable to absorb or to use normally specific dietary electrolytes and that might benefit from dietary supplementation.24,25 For accurate interpretation of results, it is important that the horse is consuming its normal diet and has recovered from any recent acute attack of exertional rhabdomyolysis when blood and urine samples are collected. A midstream urine sample should be collected, preferably freely voided rather than by catheterization. Results are only valid if serum creatinine is within the normal range and the fractional excretion of creatinine is normal. Results should be compared with the normal ranges for a horse on a similar diet because results for horses eating an oat- and hay-based diet are different than for those on a cube-based diet or a diet high in alfalfa. Fractional excretion ratios for potassium tend to be high if the horse is allowed access to pasture. Low values for fractional excretion ratios for sodium or calcium indicate that the diet should be supplemented with sodium chloride or either calcium carbonate or calcium gluconate, respectively. Appropriate dietary supplementation may help to prevent further attacks.
Management practices may also help to prevent attacks in some horses. These include daily work, with a long, slow warm-up period, turnout as much as possible, and avoiding undue stress, especially in highly strung, nervous individuals. However, some horses, especially those with daily low-grade clinical signs that are not stress provoked, prove intractable to successful management.
Muscle Injury
Muscle soreness is frequently unassociated with any recognizable histopathological changes within the muscle and is often secondary to some other cause of lameness because of the altered way in which the horse is moving. Muscle soreness can often be induced by overuse of an undertrained muscle and can result in localized soreness and stiffness for several days. Focal intense muscle spasm and pain can cause sudden-onset reduction in performance and, if primary, are usually alleviated by manipulation to relieve the muscle spasm, producing rapid amelioration of clinical signs.
Focal muscle soreness associated with localized swelling may be caused by intramuscular hemorrhage, muscle fiber tearing, or exertional rhabdomyolysis. Diagnosis of the cause may be determined by measuring serum muscle enzyme concentrations and by ultrasonographic evaluation (Figure 50-3). Hemorrhage results in an area of diffuse increase in echogenicity within the muscle. This should be differentiated from hyperechogenic regions that result from chronic muscle fibrosis. Serum muscle enzyme concentrations are usually not elevated in those horses with hemorrhage, muscle fiber tearing, or fibrosis.

Fig. 50-3 Ultrasonographic image of the semimembranosus muscle of a 6-year-old Thoroughbred with acute-onset, severe left hindlimb lameness. The horse had palpable enlargement of the muscle and localized soreness. The increased echogenicity reflects hemorrhage.
Damage to deep muscles of the hindquarters is difficult to identify because localizing clinical signs are frequently not apparent to alert the clinician to the possible site of damage. Thermographic evaluation can be useful to help identify superficial muscle injury.
Some horses with reduced performance have pain on palpation of the psoas muscles per rectum. Pain may be primary or secondary to pathological conditions of the lumbosacral or sacroiliac regions and is an indication for nuclear scintigraphic evaluation of the pelvic region and ultrasonographic examination of the lumbosacral vertebrae.
Sacroiliac Joint Injury
See Chapter 51 for further discussion of sacroiliac joint injury. Detailed anatomy of the sacroiliac joints is discussed elsewhere (see page 583).
The diagnosis of sacroiliac joint disease has tended historically to be a dustbin diagnosis, frequently made by exclusion when the clinical signs could not be explained by any other condition. The high incidence of pathological degenerative lesions found in the sacroiliac joints of TB racehorses26 and in mixed-breed horses27 indicates that degenerative disease of the sacroiliac joint is likely to be a clinically significant problem, but definitive diagnosis remains difficult. In a study of 74 horses with sacroiliac joint pain, affected horses were older than the normal clinic population, and there was a high proportion of Warmblood horses.2 Horses used for dressage or show jumping predominated. Affected horses were also of great body weight and height. However, the condition is seen in horses used for all sports disciplines and has been recognized in competition ponies.
I recognize six clinical manifestations of sacroiliac joint region pain5: an acute onset of unwillingness to go forward when ridden; sudden onset of bucking and kicking out with one or both hindlimbs when ridden; insidious onset of reduced hindlimb impulsion and engagement; sacroiliac joint region pain in association with primary thoracolumbar region pain; unilateral or bilateral hindlimb lameness and secondary sacroiliac joint region pain; and sacroiliac region pain secondary to a previous ilial stress fracture.
Pathological changes of the sacroiliac joint include lipping, cortical buttressing, and osteophyte formation, together with enlargement of the joint surfaces. These signs are thought to be a response to chronic instability of the joints, although no evidence of ligamentous laxity has been identified.27,28 Erosion of the articular cartilage may also occur, but joint ankylosis has not been documented. A positive association has been recognized between the severity of the impingement of thoracolumbar dorsal spinous processes and lumbar transverse processes and the severity of sacroiliac lesions and also between the severity of articular process degeneration and the degree of pathological conditions of the sacroiliac region.
A separate entity of enthesophyte formation at the site of attachment of the sacroiliac ligaments has been described unassociated with pathological conditions of the sacroiliac joints.29 The clinical significance of this finding has not been well defined.
Subluxation of the sacroiliac joint is comparatively rare29,30 and results from acute, traumatic disruption of the dorsal sacroiliac ligament and the sacroiliac joint capsule. Subluxation should be differentiated from an acute ilial wing fracture resulting in depression of the ipsilateral tuber sacrale (see pages 564 and 567).
The prominence of the tubera sacrale and lumbar dorsal spinous processes varies between horses and in part reflects the conformation of the back and hindlimbs and the fitness of the horse. They may appear extremely prominent in a lean, fit event or endurance horse; however, this would be unusual in a normal dressage or show jumping horse. However, abnormal prominence could also result from poor development of the epaxial muscles in the lumbar region caused by the horse not using its back and hindlimbs properly. Poor muscle development may be a reflection of pain or of the horse’s previous training: if the horse has never been asked to engage the hindlimbs properly and work through its back, these muscles will not be well developed.
Many apparently clinically normal horses have some degree of asymmetry of the height and/or shape of each tuber sacrale and the overlying soft tissues. Careful clinical appraisal of a small proportion of these horses may reveal subtle hindlimb gait abnormalities and mild discomfort induced by pressure applied over the tubera sacrale or by picking up one hindlimb and swaying the horse on the other. These findings are more likely to be detected in horses that are not fully fit and are often ameliorated when the horse is fitter and has greater muscle support. They may reflect mild instability of the sacroiliac joints but are not necessarily synonymous with degenerative change. Mild secondary sacroiliac joint region pain is often seen in association with hindlimb proximal suspensory desmitis.
Pain associated with the sacroiliac joints may be present despite symmetry of the tubera sacrale, is usually a bilateral condition, and is rarely associated with unilateral hindlimb lameness.2 Pain often manifests as reduced performance, failure properly to engage the hindlimbs, and back stiffness. Signs are often greatly accentuated when the horse is ridden. In horses with mild clinical signs, the loss of hindlimb power and lack of suppleness through the horse’s back may be much easier for the rider to feel than for an observer to appreciate. The rider may feel that he or she is being thrown forward in trot. Gait irregularities may be most apparent as the horse changes direction through a tight circle. Specific lateral movements such as half pass or sequence flying changes may be difficult. The quality of the canter is often worse than the trot. The horse may become progressively more unwilling to work under saddle and start to resist.
A comprehensive clinical evaluation is essential to preclude other conditions that may present similarly, such as bilateral distal hock joint pain. Precluding the hindlimbs as a potential source of pain by performing perineural analgesia of the tibial and fibular nerves and intraarticular anesthesia of the femorotibial and femoropatellar joints of one hindlimb may be necessary to see whether lameness becomes apparent in the contralateral limb.
Using a 15-cm needle inserted on the midline at the lumbosacral space and directed approximately 20 degrees caudally, local anesthetic solution (up to 20 mL/side) can be infiltrated in the direction of the sacroiliac joints (see page 589)![]() . This may improve clinical signs in some horses and resulted in clinically significant change in 95 of 108 horses with suspected sacroiliac pain in which local analgesia was performed.5 However, false-negative results do occur.
. This may improve clinical signs in some horses and resulted in clinically significant change in 95 of 108 horses with suspected sacroiliac pain in which local analgesia was performed.5 However, false-negative results do occur.
Nuclear scintigraphic examination may facilitate diagnosis by helping to preclude the presence of other clinically significant causes of poor hindlimb action and by giving a positive indication of abnormalities of the sacroiliac joints.10-15,31,32 Profile analysis and quantitative evaluation using regions of interest are required for accurate diagnosis. The results ideally should be compared with horses of similar age and work history because of apparent significant age-related variability between clinically normal horses.11 Considerable overlap in ratios of RU between each sacroiliac joint region and a standard reference site also occurs in clinically normal horses, horses with lameness unrelated to the sacroiliac joint, and horses with clinical signs compatible with sacroiliac joint disease.32 However, RU is bilaterally symmetrical in a normal horse. Excessive motion during image acquisition can result in images that are not of diagnostic quality and may mimic abnormalities; therefore images ideally should be acquired dynamically, and motion correction software should be used.11 Residual radiopharmaceutical in the bladder may also confound interpretation. Abnormalities are recognized as abnormal patterns of RU (Figure 50-4) and asymmetrical ratios of RU between the left and right sacroiliac joint regions.28 Care must be taken to differentiate between uptake in the tubera sacrale and uptake associated with the region of the sacroiliac joints.
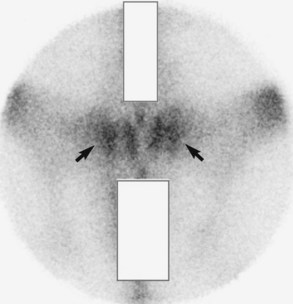
Fig. 50-4 Dorsal delayed (bone) phase scintigraphic image of a 9-year-old Warmblood dressage horse with clinical signs compatible with chronic sacroiliac joint disease. The horse’s performance was markedly improved by periarticular infiltration of local anesthetic solution around the sacroiliac joints. There is increased radiopharmaceutical uptake in the region of both the left and right sacroiliac joints. The horse failed to respond to treatment, and a diagnosis of osteoarthritis of the sacroiliac joints was confirmed post mortem.
Radiographic examination requires general anesthesia and can be frustrating because superimposition of abdominal viscera can preclude evaluation of the sacroiliac joints.6,33 However, detection of joint space irregularities and spur formation on the caudal aspect of the joints are poor prognostic indicators.
Ultrasonographic examination should be performed transcutaneously to evaluate the dorsal sacroiliac ligaments8,9,34,35 and per rectum2,8 to assess the sacroiliac joints and to eliminate as potential diagnoses pathological conditions of the lumbosacral vertebrae. Irregularities of the caudal aspect of the sacroiliac joint may be identified.
Management is essentially palliative, and prognosis is generally inversely correlated with the severity of clinical signs. Local infiltration33 of a phenol-based sclerosing agent, P2G (phenol, glucose, glycerin), or a combination of corticosteroids (methylprednisolone acetate, 200 mg) and Sarapin (High Chemical Company, Levittown, Pennsylvania, United States) appears to provide relief in some horses. Some horses benefit from treatment with nonsteroidal antiinflammatory drugs (NSAIDs), which provide partial pain relief, enabling the horse to work better and develop increased muscle strength. Daily work on the lunge using side reins, a Pessoa or a chambon, together with exercise in a cage horse walker in which the horse is free and not tied, and no ridden exercise for several weeks may be of substantial benefit. Acupuncture therapy helps some horses. Affected horses should be maintained in work at all times to maintain muscular fitness. Horses with acute problems respond best.
Sacroiliac joint disease may occur with other conditions; therefore careful appraisal of the whole horse is essential if a successful management strategy is to be achieved.2,5 Nuclear scintigraphic evaluation should include the thoracolumbar region. Concurrent impingement of dorsal spinous processes in the midthoracic, caudal thoracic, or cranial lumbar regions may occur with or without associated pain (see page 598). Infiltration of local anesthetic solution between or around the impinging dorsal spinous processes may be necessary to determine their contribution to the clinical problem. Careful evaluation of the synovial intervertebral articulations, especially close to the thoracolumbar junction, is also important. Occasionally sacroiliac disease has been seen together with OA of the coxofemoral joints. This warrants a guarded prognosis.
Desmitis of the Dorsal Sacroiliac Ligament
Desmitis of the dorsal sacroiliac ligament has been recognized in horses that have back pain, with or without focal pain on palpation.31,32 Usually lesions have been restricted to one side and have been characterized by ultrasonography as enlargements of the ligament and disruption of normal architecture, with hypoechoic regions in transverse images and loss of parallel alignment of echoes in longitudinal images. Enthesophyte formation may occur on the tuber sacrale. Such lesions have been seen alone or with other causes of back pain.
New Bone on the Caudal Aspect of the Wing of the Sacrum
A few mature competition horses used for dressage or show jumping have insidious onset loss of hindlimb action, progressing to unwillingness to maintain a proper trot. These horses have appeared considerably worse when ridden compared with evaluation in hand or on the lunge. The horses have shown abnormal sensitivity to palpation in the general areas of the sacroiliac joints. However, careful analysis of nuclear scintigraphic images has shown relatively normal radiopharmaceutical uptake in the region of the joints themselves but increased uptake abaxial to the joints. The horses have responded poorly to treatment with NSAIDs or other analgesic drugs. Post mortem examination has revealed spurs of new bone on the wings of the sacrum just caudal to the auricular surface but not involving the sacroiliac joint itself.26,27 This has been seen in association with fusion of the transverse processes of caudal lumbar vertebrae and osseous proliferation involving intervertebral foramina or synovial articulations.
Lumbosacral Joint
The clinical signs referable to lumbosacral pathology are difficult to differentiate from those associated with sacroiliac joint region pain and lesions in the thoracolumbar region. Moreover, lumbosacral pathology may coexist with sacroiliac or thoracolumbar lesions; therefore systematic radiographic, scintigraphic, and ultrasonographic evaluation of all areas should be performed. Lesions of the lumbosacral joint may be present in asymptomatic horses26; thus determination of the potential clinical significance of abnormalities is not always easy. Radiographic examination of the lumbosacral joint is only possible with the horse in dorsal recumbency under general anesthesia. Lesions of the intertransverse joints are not uncommon, but their clinical significance is unclear. Nuclear scintigraphy is not particularly sensitive for detection of lesions of the lumbosacral joint largely because of the large overlying muscle mass resulting in shielding.
The lumbosacral joint and the intertransverse joints are evaluated ultrasonographically per rectum (Figure 50-5). The transrectal ultrasonographic appearance of the lumbosacral joint was assessed in 43 horses with no history or clinical evidence of back pain or hindlimb lameness.36 In the majority of horses (34/43, 79.1%) the lumbosacral disk had uniform or mildly heterogeneous echogenicity. Variations included hyperechogenic regions within the lumbosacral disk with or without an acoustic shadow, and mild or moderate irregularity of the opposing surfaces of the last lumbar and the first sacral vertebral bodies. Marked irregularity of the bony surfaces or marked disruption of the lumbosacral disk was not seen in any horse. The mean distance between the ventral aspects of the last lumbar and first sacral vertebrae was 14.2 mm (range: 7.1 to 26.5 mm). The degree of protrusion of the ventral aspect of the lumbosacral disk ranged from 0 to 5 mm (mean: 1.32 mm). The mean angle between the ventral surfaces of the last lumbar and first sacral vertebrae was 147 degrees (range: 118 to 165 degrees). There was no significant effect of the age, breed, gender, or size of the horses on either subjective findings in the lumbosacral joint or objective measurements.
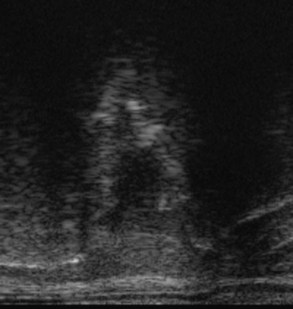
Fig. 50-5 Ultrasonographic image of the lumbosacral joint of a 10-year-old show jumper with a history of loss of performance. Dorsal is to the top and cranial to the right. The margins of the lumbosacral joint are poorly defined, and there is a large area of reduced echogenicity within the intervertebral disk. There are also focal hyperechogenic foci. This is consistent with intervertebral disk degeneration.
Abnormalities that may be of clinical significance include:
Lesions of the lumbosacral joint are treated by deep paramedian injection3,35,37,38 of corticosteroids with Sarapin (High Chemical Company) or local anesthetic solution under ultrasound guidance. The needle is inserted 4 cm from the median plane on a line connecting the cranial aspects of the tubera coxae. The needle is directed obliquely caudally and is inserted under the ilial wing until contact is made with bone in the vicinity of the axial aspect of the lumbosacral intertransverse joint. This is repeated on the left and right sides. Success of treatment is highly variable, but is often transient. Modification of the work program as discussed in Chapter 52 (see page 605) is also important.
Aortoiliacofemoral Thrombosis
Aortoiliacofemoral thrombosis is a relatively uncommon cause of exercise-induced hindlimb lameness of variable severity.39 Clinical signs may be sudden and severe in onset or subtle initially and slowly progressive. Horses of all ages may be affected. The incidence is higher in male horses than mares. The pathogenesis is unknown.
Clinical signs vary depending on the site(s) of thrombus formation, its size, and the degree of vessel occlusion![]() . Lesions occur most commonly at the terminal aspect of the aorta, but they may also involve the internal and external iliac arteries and the femoral arteries, unilaterally or bilaterally. Lesions restricted to the femoral artery have not been documented. With mild lesions, the horse may show poor performance, early fatigue, or slight loss of hindlimb action during a work period. If the lesion(s) is predominantly unilateral, the horse may show episodic hindlimb lameness induced by work. With more advanced lesions, progressive shortening of hindlimb stride may occur with exercise, followed by development of distress and sweating, except over the hindlimbs (Figure 50-6, A). If the horse is allowed to stop, it may repeatedly flex its hindlimbs and stamp the feet to the ground. The affected limbs feel cool, and delayed filling of the saphenous veins may be seen (see Figure 50-6, B), with reduced pulse amplitudes in the dorsal metatarsal artery. Clinical signs usually resolve if the horse is allowed to stand still for a few minutes.
. Lesions occur most commonly at the terminal aspect of the aorta, but they may also involve the internal and external iliac arteries and the femoral arteries, unilaterally or bilaterally. Lesions restricted to the femoral artery have not been documented. With mild lesions, the horse may show poor performance, early fatigue, or slight loss of hindlimb action during a work period. If the lesion(s) is predominantly unilateral, the horse may show episodic hindlimb lameness induced by work. With more advanced lesions, progressive shortening of hindlimb stride may occur with exercise, followed by development of distress and sweating, except over the hindlimbs (Figure 50-6, A). If the horse is allowed to stop, it may repeatedly flex its hindlimbs and stamp the feet to the ground. The affected limbs feel cool, and delayed filling of the saphenous veins may be seen (see Figure 50-6, B), with reduced pulse amplitudes in the dorsal metatarsal artery. Clinical signs usually resolve if the horse is allowed to stand still for a few minutes.
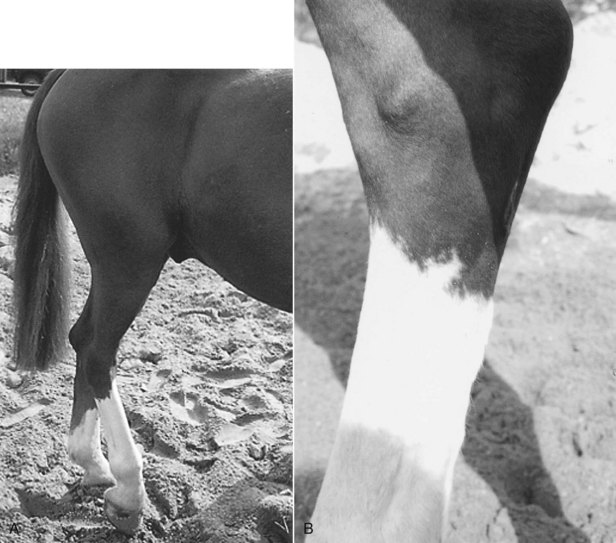
Fig. 50-6 A 9-year-old gelding with aortoiliac thrombosis. Clinical signs were provoked by just 5 minutes of lunging exercise. A, The horse repeatedly flexed each hindlimb, stamping it to the ground. No evidence of sweating over the hindquarters was apparent, but the horse was sweating profusely over the neck and flanks. B, The saphenous vein cannot be seen because of delayed filling.
In horses with advanced thromboembolism, it is usually possible to palpate a thrombus per rectum in the terminal aspect of the aorta, which feels abnormally firm. Pulses in the iliac arteries may be reduced or absent. With less advanced lesions, diagnostic ultrasonography is required for identification of the lesion (Figure 50-7). Ultrasonography is also useful to determine the extent of the lesions.40 Examination of part of the femoral artery can be performed transcutaneously on the medial aspect of the crus,3,41 and the use of Doppler ultrasonography to measure blood flow characteristics should help to determine whether a more proximal site of obstruction exists.40,42
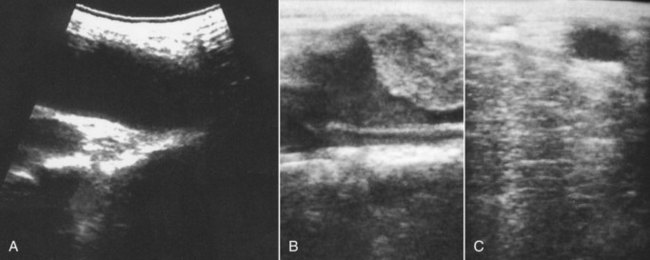
Fig. 50-7 Longitudinal ultrasonographic images of the terminal aorta of a normal horse (A) and a horse with aortoiliac thrombosis (B). Cranial is to the left. There is a large echogenic mass in the aorta of the clinically affected horse. C, Transverse ultrasonographic image of the right external iliac artery. This appears normal, but an extensive thrombus was identified farther distally at post mortem examination.
First-pass radionuclide angiography can be used to determine blood flow in the aorta and iliac arteries22,43 and also the femoral arteries. However, the sensitivity of the technique for detecting subtle lesions has yet to be determined.
The aims of treatment are to try to prevent further thrombus formation and to promote the development of a collateral blood supply for adequate perfusion. No drugs are available that alter a preformed thrombus. Treatment rationale has been based on pain relief and the use of antiinflammatory drugs, platelet inhibitors, anthelmintics, fibrinolytic agents, and anticoagulant drugs. Those most commonly used include phenylbutazone (2.2 mg/kg twice daily for 2 months), aspirin (5 mg/kg daily for several months), and isoxsuprine (1 mg/kg twice daily for 3 months). Successful treatment presumably is based on development of an effective collateral blood supply.
I have successfully managed some mildly affected horses with long-term aspirin therapy, but horses with more severe lesions are usually refractory to treatment. Only two of 29 horses returned to former athletic function, with resolution of clinical signs, following medical treatment.38 Surgical removal is feasible,44,45 although the rate of complications is high. Surgery was successful in 53% of 17 horses, but four horses had postoperative myopathy, two of which were humanely destroyed, and a fifth horse sustained a fatal femoral fracture during recovery from anesthesia.45 Reocclusion of the treated vessels may occur.
Coxofemoral Joint
The coxofemoral joint is rarely a source of pain causing lameness in the horse.
Dysplasia
Dysplasia of the coxofemoral joint is rare, usually occurs bilaterally, and predisposes relatively young horses to develop OA. The prognosis for athletic function is poor. Dysplasia may be a heritable condition in the Norwegian Dole.
Osseous Cystlike Lesions
An osseous cystlike lesion occasionally has been identified in young horses and associated with lameness.46 The lesions have resulted in chronic lameness.
Osteoarthritis
OA of the coxofemoral joint is an unusual cause of hindlimb lameness in the horse, usually occurring unilaterally but occasionally bilaterally. OA may occur secondary to dysplasia, rupture of the teres ligament (see page 582), or trauma.
Lameness varies from moderate to severe. The horse resents flexion of the limb and is unwilling to stand on the limb for long periods with the contralateral limb picked up. The degree of gluteal muscle disuse atrophy may be more than that from pain in the more distal part of the limb. Lameness may be characterized by a tendency for the horse to move on three tracks.
Intraarticular analgesia usually, but not always, improves lameness, but it is rarely alleviated fully.
Nuclear scintigraphic evaluation may help in highlighting the coxofemoral joint as abnormal, especially if the results of intraarticular analgesia are equivocal. However, it is important to be aware that loss of muscle over the hindquarter of the lame limb may confound image interpretation. I have found it useful to evaluate ratios of RU in the region of the coxofemoral joint and another standardized location and compare this with values for normal horses. Caudal oblique images can be helpful. The clinician should be aware that RU associated with a normal coxofemoral joint is much less than that of the cranial and caudal parts of the greater trochanter of the femur.
Definitive diagnosis of OA requires radiographic examination, and high-quality radiographs can only be achieved with the horse in dorsal recumbency under general anesthesia. Abnormalities include periarticular osteophyte formation, new bone formation along the femoral neck, lucent zones in the subchondral bone of the acetabulum or femoral head, and loss of congruity between the acetabulum and femoral head (Figure 50-8). Care should be taken not to confuse the depression in the femoral head and underlying radiolucent zone at the site of insertion of the teres ligament as a lesion.
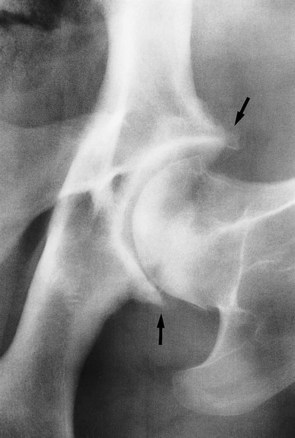
Fig. 50-8 Ventrodorsal radiographic image of the left coxofemoral joint of a 9-year-old steeplechaser with osteoarthritis. The horse had raced successfully the previous season, but it now showed moderate left hindlimb lameness at trot and carried the left hindlimb at canter. Note the marked periarticular osteophyte formation on the pelvic acetabulum (arrows) and the irregular subchondral bone opacity.
Intraarticular medication of a coxofemoral joint with radiological abnormalities has yielded disappointing results. The prognosis for return to athletic function is guarded.
Trochanteric Bursitis
Trochanteric bursitis has been described in the older literature, but the Editors have not recognized this condition. The condition is discussed elsewhere (page 552).
Luxation with or without Secondary Upward Fixation of the Patella
Luxation or subluxation of the coxofemoral joint is an unusual injury and can occur as a primary injury or secondary to an unstable fracture of the ilial shaft. The trauma causing luxation also can result in articular fractures of the acetabulum. Permanent upward fixation of the patella may develop as a sequela because of displacement of the femur. The femur is displaced proximally; therefore the greater trochanter of the femur appears higher on the lame limb. However, this can be difficult to assess because the horse is usually reluctant to bear weight on the limb. Upward fixation of the patella results in an abnormally straight hindlimb stance and an inability to flex the limb. The diagnosis can be confirmed radiologically, and with high-output x-ray machines, diagnostic radiographs can be obtained with the horse standing; however, determining whether concurrent fractures exist may be difficult. Ultrasonography can also be used to verify the presence of subluxation.47 The prognosis for athletic function is hopeless.
Rupture of the Teres Ligament
Rupture of the teres ligament results from trauma. It has been seen in a horse that tried to get up prematurely from general anesthesia while the limbs were still restrained in hobbles, and in other circumstances in which a hindlimb has become trapped. Lameness is severe, with the horse being unwilling to bear weight on the limb. Secondary OA rapidly ensues. Definitive diagnosis is only possible post mortem. The prognosis for athletic function is hopeless.
Fracture (or Enthesopathy) of the Third Trochanter of the Femur
Fracture of the third trochanter of the femur is a relatively unusual injury, resulting in acute-onset severe lameness that often improves rapidly with box rest. In a lean, poorly muscled horse, eliciting pain by palpation may be possible, but in a well-muscled Warmblood type, eliciting pain is usually not possible, even in acute injuries. No particular gait characteristics are apparent. Nuclear scintigraphy is particularly valuable for tentative diagnosis of a fracture10,16 characterized by IRU (Figure 50-9) and sometimes a change in the pattern of uptake. Diagnosis may be confirmed radiologically, but good-quality radiographs in large horses can only be achieved under general anesthesia. Oblique radiographic images can be acquired standing in small horses. Fractures are often longitudinal, occurring at the base of the trochanter, but horizontal fractures have been seen.6,16 Displacement is usually minimal. Diagnostic ultrasonography is sometimes useful to confirm a fracture and to exclude abnormalities of the superficial gluteal muscle, which inserts on the third trochanter. Insertional tears of this muscle may be associated with a similar scintigraphic appearance. Treatment is box rest for 2 months, followed by walking exercise for another month. Healing may occur by osseous or fibrous union. Prognosis is good.
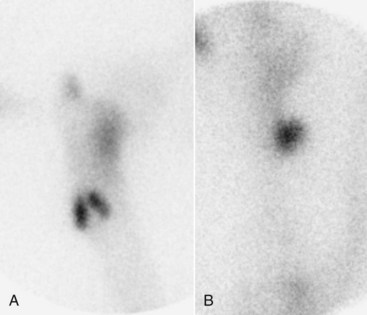
Fig. 50-9 Lateral (A) and caudal (B) scintigraphic images of the right femur of a 7-year-old Warmblood dressage horse with sudden onset of severe right hindlimb lameness. In the lateral image (A), there are two areas of focal intense increased radiopharmaceutical uptake (IRU) in the region of the third trochanter of the femur; IRU is seen within the third trochanter in the caudal image. This is consistent with a fracture of the third trochanter of the femur.