CHAPTER 46 Pectoral girdle, shoulder region and axilla
SKIN AND SOFT TISSUE
SKIN
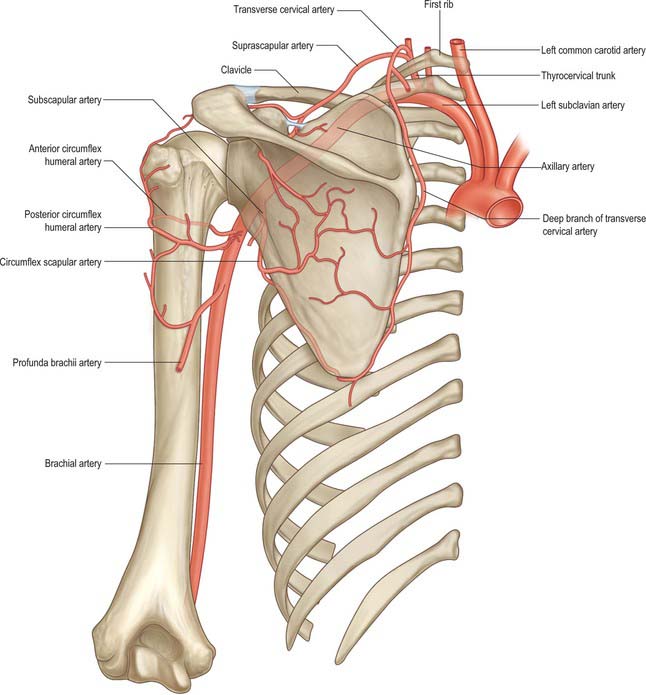
Cutaneous vascular supply
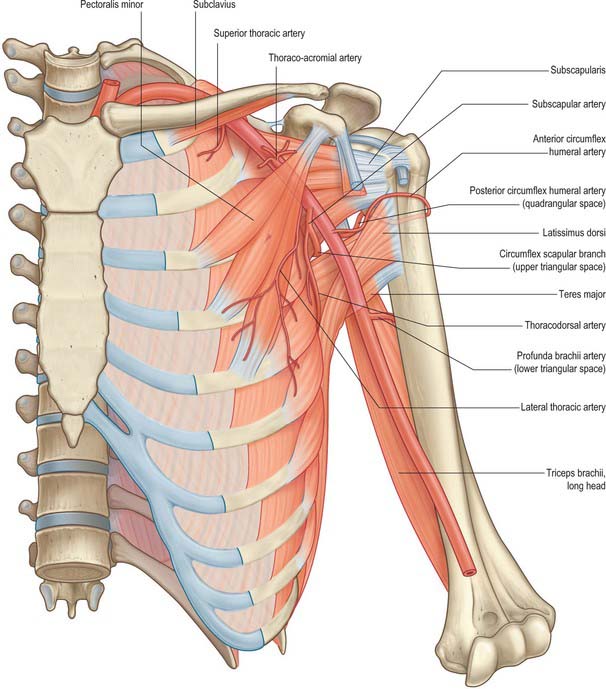
The area over the lateral end of the clavicle is supplied by the supraclavicular artery which pierces the deep fascia superior to the clavicle and anterior to trapezius (Fig. 45.4). In the majority of cases this artery arises from the superficial cervical/transverse cervical artery, but it occasionally arises from the suprascapular artery. The area over the deltoid is supplied by the anterior and posterior circumflex humeral arteries. The deltoid branch of the thoraco-acromial axis contributes to the blood supply of the anterior aspect of the shoulder via musculocutaneous perforators through deltoid. For details of the cutaneous supply to the anterior, lateral and posterior chest wall see page 915.
Cutaneous innervation
The segmental supply is described in Chapter 45, page 789. The cutaneous supply to the shoulder region comes from the supraclavicular nerves (p. 436, Fig. 45.15). The floor of the axilla together with part of the upper medial aspect of the arm is supplied by the intercostobrachial nerve (lateral branch of the second intercostal nerve). Occasionally the lateral branch of the third intercostal nerve contributes to the supply of skin in the floor of the axilla. The upper lateral cutaneous nerve of the arm supplies the skin over the inferolateral part of the shoulder.
SOFT TISSUE
Deep fascia
Fascia over deltoid
The deep fascia over deltoid sends numerous septa between its fasciculi and is continuous with the pectoral fascia in front and the thick and strong infraspinous fascia behind. Above it is attached to the clavicle, acromion and crest of the scapular spine; below it is continuous with the brachial fascia.
Subscapular fascia
The subscapular fascia is a thin aponeurosis attached to the entire circumference of the subscapular fossa; subscapularis itself is partly attached to its deep surface.
Supraspinous fascia
The supraspinous fascia completes the osseofibrous compartment in which supraspinatus is attached. It is thick medially, but thinner laterally under the coraco-acromial ligament. It is attached to the scapula around the boundaries of the attachment of supraspinatus.
Infraspinous fascia
The infraspinous fascia covers infraspinatus and is attached to the margins of the infraspinous fossa. The fascia is continuous with the deltoid fascia along the overlapping posterior border of deltoid.
Pectoral and axillary fascia
The pectoral fascia is a thin lamina which covers pectoralis major and extends between its fasciculi. It is attached medially to the sternum, above to the clavicle and is continuous inferolaterally with the fascia of the shoulder, axilla and thorax. Although thin over pectoralis major, it is thicker between this muscle and latissimus dorsi, and forms the floor of the axilla as the axillary fascia. The latter divides at the lateral margin of latissimus dorsi into two layers, which ensheathe the muscle and are attached behind to the spines of the thoracic vertebrae. As the fascia leaves the lower edge of pectoralis major to cross the axilla, a layer ascends under cover of the muscle and splits to envelop pectoralis minor: it becomes the clavipectoral fascia at the upper edge of pectoralis minor. The hollow of the armpit is produced mainly by the action of this fascia in tethering the skin to the floor of the axilla, and it is sometimes referred to as the suspensory ligament of the axilla. The axillary fascia is pierced by the tail of the breast (Ch. 54).
Clavipectoral fascia
The clavipectoral fascia is a strong fibrous sheet behind the clavicular part of pectoralis major. It fills the gap between pectoralis minor and subclavius, and covers the axillary vessels and nerves. It splits around subclavius and is attached to the clavicle both anterior and posterior to the groove for subclavius. The posterior layer fuses with the deep cervical fascia which connects omohyoid to the clavicle and with the sheath of the axillary vessels. Medially it blends with the fascia over the first two intercostal spaces and is attached to the first rib, medial to subclavius. Laterally, it is thick and dense, and is attached to the coracoid process, blending with the coracoclavicular ligament. Between the first rib and coracoid process the fascia often thickens to form a band, the costocoracoid ligament. Below this the fascia becomes thin, splits around pectoralis minor and descends to blend with the axillary fascia and laterally with the fascia over the short head of biceps. The cephalic vein, thoraco-acromial artery and vein, and lateral pectoral nerve pass through the fascia.
Spread of infection
When axillary suppuration occurs the local fascial arrangement affects the spread of pus. Suppuration may be superficial or deep to the clavipectoral fascia, either between the pectoral muscles or behind pectoralis minor. In the former, an abscess would appear at the edge of the anterior axillary fold or the groove between deltoid and pectoralis major; in the latter, pus would tend to surround vessels and nerves and ascend into the neck, the direction of least resistance. Pus may also track along vessels into the arm. When an axillary abscess is incised, the knife should enter the axillary ‘base’, midway between the anterior and posterior margins and near the thoracic side to avoid the lateral thoracic, subscapular and axillary vessels on the anterior, posterior and lateral walls respectively.
BONE
CLAVICLE
The clavicle lies almost horizontally at the root of the neck and is subcutaneous throughout its whole extent (Fig. 46.1). It acts as a prop which braces back the shoulder and enables the limb to swing clear of the trunk and transmits part of the weight of the limb to the axial skeleton. The lateral or acromial end of the bone is flattened and articulates with the medial side of the acromion, whereas the medial or sternal end is enlarged and articulates with the clavicular notch of the manubrium sterni and first costal cartilage. The shaft is gently curved and in shape resembles the italic letter f, being convex forwards in its medial two-thirds and concave forwards in its lateral third. The inferior aspect of the intermediate third is grooved in its long axis. The clavicle is trabecular internally, with a shell of much thicker compact bone in its shaft. Although elongated, the clavicle is unlike typical long bones in that it usually has no medullary cavity.
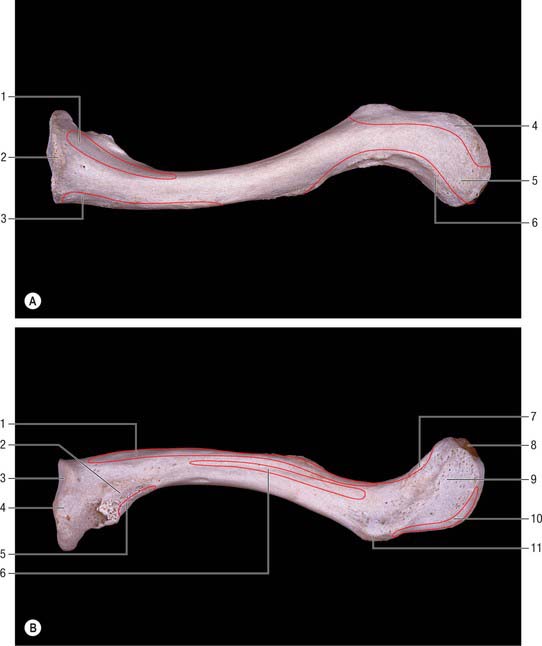
Fig. 46.1 A, Superior view of left clavicle. B, Inferior view of left clavicle. A: 1. Sternocleidomastoid (clavicular head). 2. Sternal end. 3. Pectoralis major. 4. Trapezius. 5. Acromial end. 6. Deltoid. B: 1. Pectoralis major. 2. For costoclavicular ligament. 3. For first costal cartilage. 4. For sternum. 5. Sternohyoid. 6. Subclavius. 7. Deltoid. 8. For acromion. 9. Trapezoid line. 10. Trapezius. 11. Conoid tubercle.
The female clavicle is shorter, thinner, less curved and smoother, and its acromial end is carried lower than the sternal in comparison with the male. In males the acromial end is on a level with, or slightly higher than, the sternal end when the arm is pendent. Midshaft circumference is the most reliable single indicator of sex: a combination of this measurement with weight and length yields better results. The clavicle is thicker and more curved in manual workers, and its ridges for muscular attachment are better marked.
Lateral third
The lateral third of the clavicle is flattened and has a superior and an inferior surface, limited by an anterior and a posterior border. The anterior border is concave, thin and roughened and may be marked by a small deltoid tubercle.
The posterior border, also roughened by muscular attachments, is convex backwards. The superior surface is roughened near its margins but is smooth centrally, where it can be felt through the skin. The inferior surface presents two obvious markings. Close to the posterior border, at the junction of the lateral fourth with the rest of the bone, there is a prominent conoid tubercle which gives attachment to the conoid part of the coracoclavicular ligament. A narrow, roughened strip, the trapezoid line, runs forwards and laterally from the lateral side of this tubercle, almost as far as the acromial end (Fig. 46.1B). The trapezoid part of the coracoclavicular ligament is attached to it. A small oval articular facet, for articulation with the medial aspect of the acromion, faces laterally and slightly downwards at the lateral end of the shaft.
Subclavius lies in a groove on the inferior surface (Fig. 46.1B). The clavipectoral fascia is attached to the edges of the groove; the posterior edge of the groove runs to the conoid tubercle, where fascia and conoid ligament merge. Lateral to the groove there is a laterally inclined nutrient foramen. Deltoid (anterior) and trapezius (posterior) are attached to the lateral third of the shaft: both muscles reach the superior surface. The coracoclavicular ligament, which is attached to the conoid tubercle and trapezoid line (Fig. 46.1B), transmits the weight of the upper limb to the clavicle, counteracted by trapezius which supports its lateral part. From the conoid tubercle this weight is transmitted through the medial two-thirds of the shaft to the axial skeleton.
The clavicle is often fractured, commonly by indirect forces, as a result of a violent impact to the hand or shoulder. The break is usually at the junction of the lateral and intermediate thirds, where the curvature changes, for this is the weakest part of the bone. A fracture medial to the conoid tubercle interrupts weight transmission from the arm to the axial skeleton. The resulting deformity is caused by the weight of the arm, which acts on the lateral fragment through the coracoclavicular ligament and draws it downwards. The medial fragment, as a rule, is a little displaced.
Medial two-thirds
The medial two-thirds of the shaft of the clavicle is cylindrical or prismoid in form and possesses four surfaces, but the inferior surface is often reduced to a mere ridge. The anterior surface is roughened over most of its extent but it is smooth and rounded at its lateral end, where it forms the upper boundary of the infraclavicular fossa. The upper surface is roughened in its medial part and smooth at its lateral end. The posterior surface is smooth and featureless. The inferior surface is marked, near the sternal end, by a roughened oval impression, which is often depressed below the surface. Its margins give attachment to the costoclavicular ligament, which connects the clavicle to the upper surface of the first rib and its cartilage. Rarely, this area is smooth or raised to form an eminence which may articulate with the upper surface of the first rib by means of a synovial joint. There is a groove in the long axis of the bone in the lateral half of the posterior surface.
The medial two-thirds provide attachment, anteriorly, for the clavicular head of pectoralis major: the area is usually clearly indicated on the bone. The clavicular head of sternocleidomastoid is attached to the medial half of the superior surface, but the marking on the bone is not very conspicuous. The smooth, posterior surface is devoid of muscular attachments except at its lower part immediately adjoining the sternal end, where the lateral fibres of sternohyoid are attached. Medially, this surface is related to the lower end of the internal jugular vein (from which it is separated by sternohyoid), the termination of the subclavian vein, and the start of the brachiocephalic vein. More laterally, it arches in front of the trunks of the brachial plexus and the third part of the subclavian artery. The suprascapular vessels are related to the upper part of this surface. The inferior surface gives insertion to subclavius in the subclavian groove: the clavipectoral fascia, which encloses subclavius, is attached to the edges of the groove. The posterior lip of the groove runs into the conoid tubercle and carries the fascia into continuity with the conoid ligament. A nutrient foramen is found in the lateral end of the groove, running in a lateral direction: the nutrient artery is derived from the suprascapular artery. The impression for the costoclavicular ligament is very variable in its character.
Sternal end
The sternal end of the clavicle is directed medially, and a little downwards and forwards, to articulate with the clavicular notch of the manubrium sterni. The sternal surface, usually irregular and pitted, is quadrangular (sometimes triangular). Its uppermost part is slightly roughened for attachment of the interclavicular ligament, sternoclavicular capsule and articular disc. Elsewhere the surface is smooth and articular and it extends onto the inferior surface for a short distance, where it articulates with the first costal cartilage. The sternal end of the clavicle projects upwards beyond the manubrium sterni and can be felt without difficulty and usually seen (a prominent clinical landmark), in the lateral wall of the jugular fossa.
Ossification
The clavicle begins to ossify before any other bone in the body, and is ossified from three centres. The shaft of the bone is ossified in condensed mesenchyme from two primary centres, medial and lateral, which appear between the fifth and sixth weeks of intrauterine life, and fuse about the 45th day. Cartilage then develops at both ends of the clavicle. The medial cartilaginous mass contributes more to growth in length than does the lateral mass: the two centres of ossification meet between the middle and lateral thirds of the clavicle. A secondary centre for the sternal end appears in late teens, or even early twenties, usually 2 years earlier in females (Fig. 46.2). Fusion is probably rapid but reliable data are lacking. An acromial secondary centre sometimes develops at around 18 to 20 years, but this epiphysis is always small and rudimentary and rapidly joins the shaft.
The clavicle does not ossify exclusively by intramembranous ossification. In 14 mm embryos the clavicle is a band of condensed mesenchyme between the acromion and apex of the first rib, which is continuous with the sternal rudiment. Medial and lateral zones of early cartilage transformation (‘precartilage’) occur within this band, and intramembranous centres of ossification appear, and soon fuse, in the mesenchyme between them. Sternal and acromial zones soon become true cartilage into which ossification extends from the shaft. Length increases by interstitial growth of these terminal cartilages; the latter develop zones of hypertrophy, calcification and advancing endochondral ossification like other growth cartilages. Diameter increases by subperichondral deposition in the extremities and subperiosteal deposition in the shaft. Epiphyses are endochondral and probably fuse in the same way as they do in long bones. Defects of ossification in the clavicle and those cranial bones which ossify by intramembranous ossification occasionally coincide, e.g. in cleidocranial dysostosis.
SCAPULA
The scapula is a large, flat, triangular bone which lies on the posterolateral aspect of the chest wall, covering parts of the second to seventh ribs (Fig. 46.3, Fig. 46.4). It has costal and dorsal surfaces, superior, lateral and medial borders, inferior, superior and lateral angles, and three processes, the spine, its continuation the acromion and the coracoid process. The lateral angle is truncated and bears the glenoid cavity for articulation with the head of the humerus. This part of the bone may be regarded as the head, and it is connected to the plate-like body by an inconspicuous neck. The long axis of the scapula is nearly vertical and the relatively featureless costal surface can easily be distinguished from the dorsal surface, which is interrupted by the shelf-like projection of the spine (Fig. 46.3A). The bone is very much thickened in the immediate neighbourhood of the lateral border, which runs from the inferior angle below, to the glenoid cavity above. The main processes, and thicker parts of the scapula, contain trabecular bone; the rest consists of a thin layer of compact bone. The central supraspinous fossa and the greater part of the infraspinous fossa are thin and even translucent; occasionally the bone in them is deficient, and the gaps are filled by fibrous tissue.
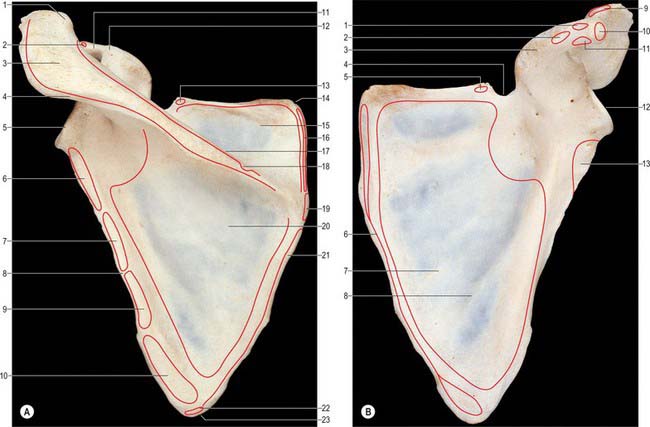
Fig. 46.3 A, Posterior aspect of left scapula. 1. Clavicular facet. 2. Biceps (short head). 3. Acromion. 4. Deltoid. 5. Glenoid fossa. 6. Triceps brachii (long head). 7 and 9. Teres minor. 8. Groove for circumflex scapular artery. 10. Teres major. 11. Conoid tubercle. 12. Coracoid process. 13. Omohyoid (inferior belly). 14. Superior angle. 15. Supraspinatus. 16. Levator scapulae. 17. Spine. 18. Trapezius. 19. Rhomboid minor. 20. Infraspinatus. 21. Rhomboid major. 22. Latissimus dorsi. 23. Inferior angle. B, Anterior aspect of left scapula. 1. Trapezoid ligament attachment. 2. Conoid ligament attachment. 3. Acromion process. 4. Suprascapular notch. 5. Omohyoid (inferior belly). 6. Serratus anterior. 7. Subscapularis. 8. Ridge for intermuscular tendon of subscapularis. 9. Deltoid. 10. Biceps (short head) and coracobrachialis. 11. Pectoralis minor. 12. Glenoid fossa. 13. Triceps (long head).
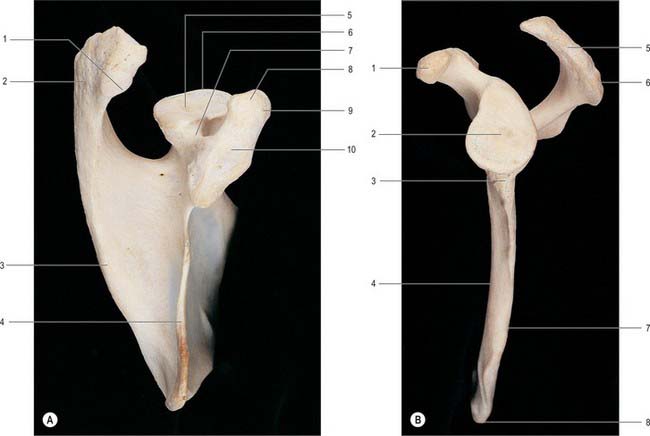
Fig. 46.4 A, Superior aspect of left scapula. 1. Facet for clavicle. 2. Acromial process. 3. Spine. 4. Superior border. 5. Head. 6. Glenoid fossa. 7. Neck. 8. Conoid tubercle (for conoid ligament). 9. Coracoid process. 10. Trapezoid ligament attachment. B, Lateral aspect of left scapula. 1. Coracoid process. 2. Glenoid fossa. 3. Infraglenoid tubercle for long head of triceps. 4. Ventral surface. 5. Acromion. 6. Acromial angle. 7. Lateral border. 8. Inferior angle.
The inferior angle lies over the seventh rib, or over the seventh intercostal space. It can be felt through the skin and the muscles which cover it and, when the arm is raised above the head, it can be seen to pass forwards round the chest wall. The superior angle is placed at the junction of the superior and medial borders, and is obscured by the muscles which cover it. The lateral angle is truncated and broadened. It constitutes the head of the bone. On its free surface it bears the glenoid cavity for articulation with the head of the humerus in the shoulder joint. Very gently hollowed out, the glenoid forms a poor socket for the humeral head. It is narrow above and wider below, and is pear-shaped in outline. Immediately above the glenoid cavity a small, roughened area encroaches on the root of the coracoid process and is termed the supraglenoid tubercle. The neck of the scapula is the constriction immediately adjoining the head. It can be identified most easily on its inferior and dorsal aspects. Ventrally, it can be regarded as extending between the infraglenoid tubercle and the anterior margin of the suprascapular notch.
Costal surface
The costal surface, which is directed medially and forwards when the arm is by the side, is slightly hollowed out, especially in its upper part (Fig. 46.3B).
Near the lateral border there is a longitudinal rounded ridge, prominent near the neck, but less so below, which is separated from the lateral border by a narrow grooved area.
Subscapularis arises from nearly the whole of the costal surface, including the grooved area immediately adjoining the lateral border, but excluding the area next to the neck of the bone. Small intramuscular tendons are attached to the roughened ridges which subdivide this surface incompletely into a number of smooth areas. The anterior aspect of the neck is separated from subscapularis by a bursal protrusion of the synovial membrane of the shoulder joint (subscapular ‘bursa’). The lower five or six digitations of serratus anterior are attached to an oval area near the inferior angle. The remainder of the muscle is inserted into a narrow strip along the ventral aspect of the medial border, which is wider above, where it receives the large first digitation. The longitudinal thickening of the bone near the lateral border provides a lever of the necessary strength to withstand the pull of serratus anterior on the inferior angle during lateral scapular rotation, when the glenoid cavity is turned to face more directly upwards as the arm is raised from the side and carried above the head against gravity.
Dorsal surface
The dorsal surface is divided by the shelf-like spine of the scapula into a small upper and a large lower area, which are confluent at the spinoglenoid notch between the lateral border of the spine and the dorsal aspect of the neck (Fig. 46.3A).
Supraspinatus is attached to the medial two-thirds of the supraspinous fossa on the dorsal surface: the fascia which covers the muscle is attached to the margins of the fossa. Teres minor is attached to the upper two-thirds of a flattened strip which adjoins the lateral border. The strip is grooved near its upper end by the circumflex scapular vessels, which pass between teres minor and the bone as they enter the infraspinous fossa. The lower limit of the attachment of teres minor is indicated by an oblique ridge, which runs from the lateral border to the neighbourhood of the inferior angle and cuts off a somewhat oval area where teres major is attached. The dorsal aspect of the inferior angle may give origin to a small slip which joins the deep surface of latissimus dorsi. The infraspinous fossa is hollowed out laterally but is convex medially. Infraspinatus is attached to the infraspinous fossa, with the exception of an area near the neck of the bone. The strong infraspinatus fascia passes onto teres minor and teres major, and sends fascial partitions between them which reach the bone along the ridges which mark the limits of their attachments.
Superior border
The superior border, thin and sharp, is the shortest. At its anterolateral end it is separated from the root of the coracoid process by the suprascapular notch (Fig. 46.3B). Near the suprascapular notch it gives origin to the inferior belly of omohyoid. The notch is bridged by the superior transverse ligament which is attached laterally to the root of the coracoid process and medially to the limit of the notch. The ligament is sometimes ossified. The foramen, thus completed, transmits the suprascapular nerve to the supraspinous fossa, whereas the suprascapular vessels pass backwards above the ligament.
Lateral border
The lateral border of the scapula forms a clearly defined, sharp, roughened ridge, which runs sinuously from the inferior angle to the glenoid cavity. At its upper end it widens into a rough, somewhat triangular area, which is termed the infraglenoid tubercle (Fig. 46.4B). The lateral border separates the attachments of subscapularis and teres minor and major. These muscles project beyond the bone and, with latissimus dorsi, cover it so completely that it cannot be felt through the skin. The long head of triceps is attached to the infraglenoid tubercle.
The grooved part of the costal surface, the narrow flat lateral strip of the dorsal surface and the adjacent thickened ridge (Fig. 46.4B), are often included in the ‘lateral border’ during clinical examination.
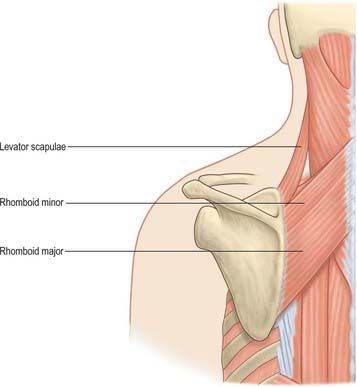
Medial border
The medial border of the scapula extends from the inferior to the superior angle. In its lower two-thirds this border can easily be felt through the skin, but its upper third is more deeply placed and cannot be palpated. It is thin and often angled opposite the root of the spine. Levator scapulae is attached to a narrow strip, extending from the superior angle to the root of the spine, and rhomboid minor is attached below this, opposite the root of the spine. Rhomboid major is attached to the remainder of the border.
Scapular angles
The inferior angle overlies the seventh rib or intercostal space. Palpable through the skin and covering muscles, it is also visible as it advances round the thoracic wall when the arm is raised. It is covered on its dorsal aspect by the upper border of latissimus dorsi, a small slip from which is frequently attached to the inferior angle. The superior angle, at the junction of the superior and medial borders, is obscured by the upper part of trapezius. The lateral angle, truncated and broad, bears the glenoid cavity which articulates with the head of the humerus at the glenohumeral joint. It provides a shallow, and limited, socket for the humeral head. Its outline is piriform, narrower above (Fig. 46.4B). The glenohumeral ligaments are attached to its anterior margin. When the arm is by the side, the cavity is directed forwards, laterally and slightly upwards. When the arm is raised above the head it is directed almost straight upwards. Just above it a small rough supraglenoid tubercle encroaches on the root of the coracoid process. The anatomical neck, the constriction adjoining the rim of the glenoid cavity, is most distinct at its inferior and dorsal aspects. Anteriorly and posteriorly it extends between the infraglenoid and supraglenoid tubercles, passing lateral to the root of the coracoid process. The long head of biceps brachii is attached to the supraglenoid tubercle, and the long head of triceps brachii is attached to the infraglenoid tubercle.
Spine of the scapula
The spine of the scapula forms a shelf-like projection on the upper part of the dorsal surface of the bone, and is triangular in shape (Fig. 46.3A). Its lateral border is free, thick and rounded and helps to bound the spinoglenoid notch, which lies between it and the dorsal surface of the neck of the bone. Its anterior border joins the dorsal surface of the scapula along a line which runs laterally and slightly upwards from the junction of the upper and middle thirds of the medial border. The plate-like body of the bone is bent along this line, which accounts for the concavity of the upper part of the costal surface. The dorsal border is the crest of the spine, and is subcutaneous throughout nearly its whole extent. At its medial end the crest expands into a smooth, triangular area. Elsewhere the upper and lower edges and the surface of the crest are roughened for muscular attachments. The upper surface of the spine widens as it is traced laterally, and is slightly hollowed out. Together with the upper area of the dorsal surface of the bone, the upper surface of the spine forms the supraspinous fossa. The lower surface is overhung by the crest at its medial, narrow end, but is gently convex in its wider, lateral portion. Together with the lower area of the dorsal surface of the bone, the lower surface of the spine forms the infraspinous fossa, which communicates with the supraspinous fossa through the spinoglenoid notch.
Supra- and infraspinatus are attached to the upper and lower surfaces of the spine of the scapula, respectively. The flattened triangular area at its root lies opposite the spine of the third thoracic vertebra and is covered by the tendon of trapezius; a bursa intervenes to enable the tendon to play over this part of the bone. The posterior fibres of deltoid are attached to the lower border of the crest. The middle fibres of trapezius are attached to the upper border of the crest, and the lowest fibres of trapezius terminate in a flat triangular tendon which glides over the smooth area at the base of the spine and inserts into a rough prominence, erroneously called the deltoid tubercle, on the dorsal or subcutaneous aspect of the spine near its medial end.
Acromion
The acromion projects forwards, almost at right angles, from the lateral end of the spine, with which it is continuous. The lower border of the crest of the spine becomes continuous with the lateral border of the acromion at the acromial angle, which forms a subcutaneous, bony landmark. The medial border of the acromion is short and is marked anteriorly by a small, oval facet, directed upwards and medially, for articulation with the lateral end of the clavicle. The lateral border, tip and upper surface of the acromion can all be felt through the skin without difficulty. There may be an accessory articular facet on the inferior surface of the acromion.
The acromion is subcutaneous over its dorsal surface, being covered only by the skin and superficial fascia. The lateral border, which is thick and irregular, and the tip of the process, as far round as the clavicular facet, give origin to the middle fibres of deltoid. The medial aspect of the tip gives attachment, below deltoid, to the lateral end of the coraco-acromial ligament. The articular capsule of the acromioclavicular joint is attached around the margins of the clavicular facet. Behind the facet, the medial border of the acromion gives insertion to the horizontal fibres of trapezius. The inferior aspect of the acromion is relatively smooth, and together with the coraco-acromial ligament and the coracoid process forms a protective arch over the shoulder joint. The tendon of supraspinatus passes below the overhanging acromion and is separated from it and from deltoid by the subacromial bursa.
Coracoid process
The coracoid process arises from the upper border of the head of the scapula and is bent sharply so as to project forwards and slightly laterally (Fig. 46.3B, Fig. 46.4A). When the arm is by the side, the coracoid process points almost straight forwards and its slightly enlarged tip can be felt through the skin, although it is covered by the anterior fibres of deltoid. The supraglenoid tubercle marks the root of the coracoid process where it adjoins the upper part of the glenoid cavity. There is another impression on the dorsal aspect of the coracoid process at the point where it changes direction: it gives attachment to the conoid part of the coracoclavicular ligament.
The coracoid process lies about 2.5 cm below the clavicle at the junction of the lateral fourth with the rest of the bone and is connected to its under surface by the coracoclavicular ligament. It is covered by the anterior fibres of deltoid and can be identified only on deep pressure through the lateral border of the infraclavicular fossa. The attachment of the conoid part of the ligament has already been considered: the trapezoid part is attached to the upper aspect of the horizontal part of the process. Pectoralis minor is attached to the superior aspect of the coracoid process. The wider, medial end of the coraco-acromial ligament and, below that, the coracohumeral ligament, are attached to the lateral border. Coracobrachialis is attached to the medial side of the tip of the process, and the short head of biceps is attached to the lateral side of the tip. The inferior aspect of the process is smooth and helps to complete the coraco-acromial arch.
Ligaments
The main scapular ligaments are the coracoacromial and superior transverse scapular; there may also be a weaker, variable inferior transverse scapular (spinoglenoid) ligament (see below Fig. 46.13, see below Fig. 46.14).
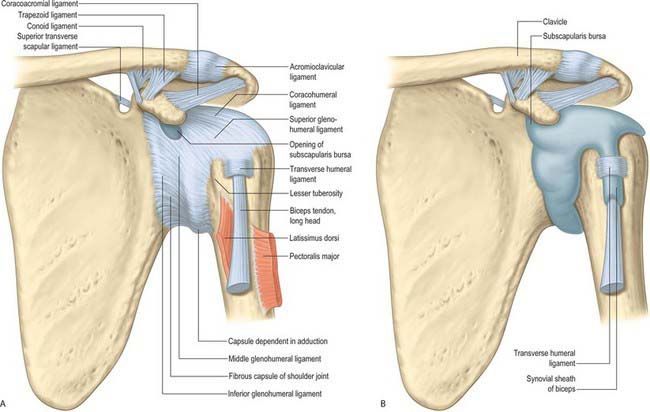
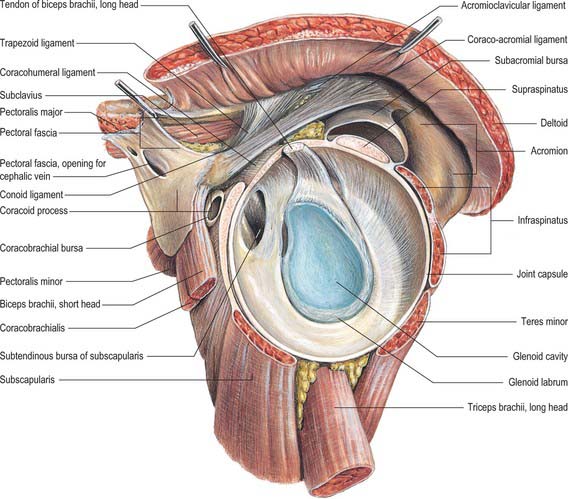
Fig. 46.14 A, The anterior aspect of the left shoulder. B, A deeper view of the anterior aspect than in (A), showing the subscapularis bursa.
The coracoacromial ligament is a strong triangular band between the coracoid process and acromion. It is attached apically to the acromion anterior to its clavicular articular surface and by its base along the whole lateral border of the coracoid. Together with the coracoid process and acromion it completes an arch above the humeral head. It may be composed of two strong marginal bands with a thinner centre; when pectoralis minor is inserted into the humeral capsule instead of the coracoid process, which happens occasionally, its tendon passes between the bands. The subacromial bursa facilitates movement between the coracoacromial arch and the subjacent supraspinatus and shoulder joint, functioning as a secondary synovial articulation.
Superior transverse scapular (suprascapular) ligament
The superior transverse scapular (suprascapular) ligament converts the scapular notch into a foramen: it is sometimes ossified. A flat fasciculus, it narrows towards its attachments to the base of the coracoid process and medial side of the scapular notch. The suprascapular nerve traverses the foramen and the suprascapular vessels cross above the ligament.
Inferior transverse scapular (spinoglenoid) ligament
When present, the inferior transverse scapular ligament is a membranous ligament which may stretch from the lateral border of the spine of the scapula to the glenoid margin. It forms an arch over the suprascapular nerve and vessels entering the infraspinous fossa.
Ossification
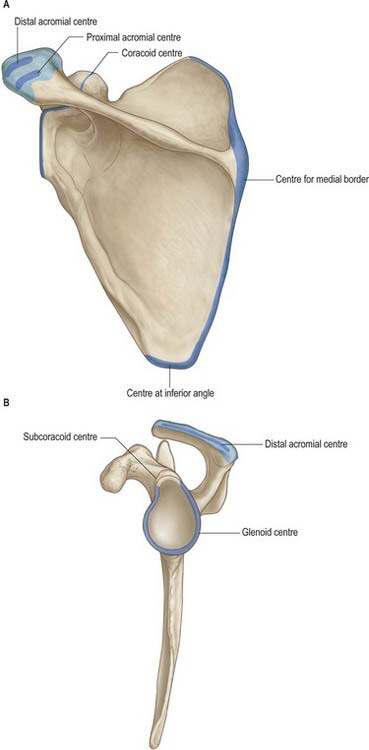
The cartilaginous scapula is ossified from eight or more centres: one in the body, two each in the coracoid process and the acromion, one each in the medial border, inferior angle and lower part of the rim of the glenoid cavity (Fig. 46.5). The centre for the body appears in the eighth intrauterine week. Ossification begins in the middle of the coracoid process in the first year or in a small proportion of individuals before birth and the process joins the rest of the bone about the 15th year. At or soon after puberty centres of ossification occur in the rest of the coracoid process (subcoracoid centre), in the rim of the lower part of the glenoid cavity, frequently at the tip of the coracoid process, in the acromion, in the inferior angle and contiguous part of the medial border and in the medial border. A variable area of the upper part of the glenoid cavity, usually the upper third, is ossified from the subcoracoid centre; it unites with the rest of the bone in the 14th year in the female and the 17th year in the male. A horse-shoe shaped epiphysis appears for the rim of the lower part of the glenoid cavity; thicker at its peripheral than at its central margin, it converts the flat glenoid cavity of the child into the gently concave fossa of the adult. The base of the acromion is formed by an extension from the spine; the rest of the acromion is ossified from two centres which unite and then join the extension from the spine. The various epiphyses of the scapula have all joined the bone by about the 20th year.
HUMERUS
The humerus, the longest and largest bone in the upper limb, has expanded ends and a shaft (Fig. 46.6, Fig. 46.7, Fig. 46.8). The rounded head occupies the proximal and medial part of the upper end of the bone and forms an enarthrodial articulation with the glenoid cavity of the scapula. The lesser tubercle projects from the front of the shaft, close to the head, and is limited on its lateral side by a well-marked groove. The distal end, loosely termed ‘condylar’, is adapted to the forearm bones at the elbow joint.
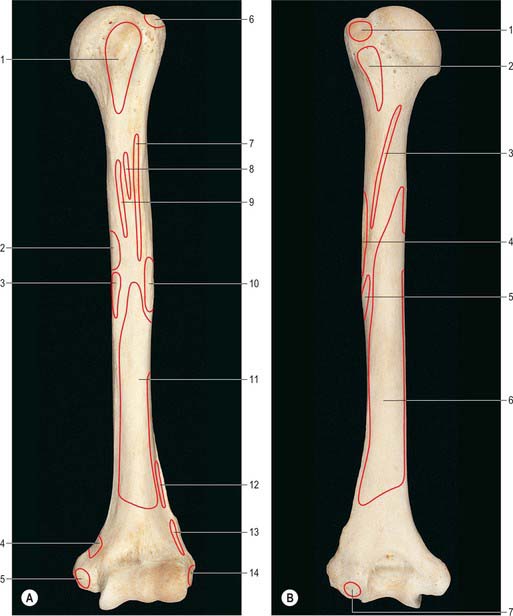
Fig. 46.6 Left humerus showing muscular attachments. A, Anterior aspect. B, Posterior aspect. A: 1. Subscapularis. 2. Triceps (medial head). 3. Coracobrachialis. 4. Pronator teres (humeral head). 5. Common flexor origin. 6. Supraspinatus. 7. Pectoralis major. 8. Latissimus dorsi. 9. Teres major. 10. Deltoid. 11. Brachialis. 12. Brachioradialis. 13. Extensor carpi radialis longus. 14. Common extensor origin. B: 1. Infraspinatus. 2. Teres minor. 3. Triceps (lateral head). 4. Deltoid. 5. Brachialis. 6. Triceps (medial head). 7. Anconeus.

Fig. 46.7 A, Anterior aspect of proximal end of left humerus. B, Posterior aspect of proximal end of left humerus. A: 1. Head. 2. Anatomical neck. 3. Surgical neck. 4. Greater tubercle. 5. Lesser tubercle. 6. Intertubercular sulcus. 7. Shaft. B: 1. Greater tubercle. 2. Surgical neck. 3. Shaft. 4. Radial groove. 5. Head. 6. Anatomical neck.
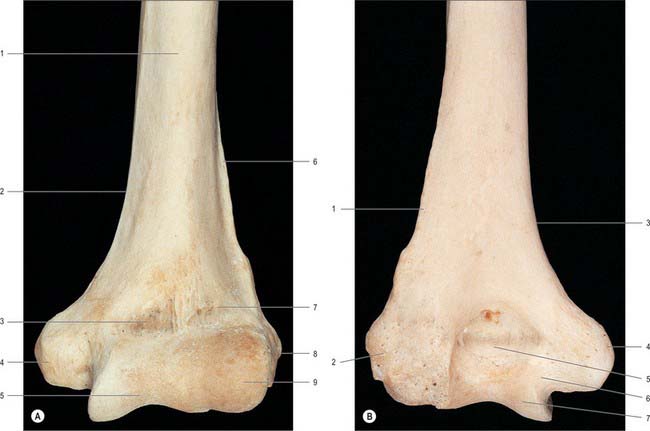
Fig. 46.8 A, Anterior aspect of distal end of left humerus. B, Posterior aspect of distal end of left humerus. A: 1. Shaft. 2. Medial supracondylar ridge. 3. Coronoid fossa. 4. Medial epicondyle. 5. Trochlea. 6. Lateral supracondylar ridge. 7. Radial fossa. 8. Lateral epicondyle. 9. Capitulum. B: 1. Lateral supracondylar ridge. 2. Lateral epicondyle. 3. Medial supracondylar ridge. 4. Medial epicondyle. 5. Olecranon fossa. 6. Sulcus for ulnar nerve. 7. Trochlea.
The capsular ligament of the elbow joint is attached anteriorly to the upper limits of the radial and coronoid fossae, so that both these bony depressions are intracapsular and therefore lined with synovial membrane. Medially it is attached to the medial non-articular aspect of the projecting lip of the trochlea and to the root of the medial epicondyle. Posteriorly it ascends to, or almost to, the upper margin of the olecranon fossa, which is therefore intracapsular and covered with synovial membrane. Laterally it skirts the lateral borders of the trochlea and capitulum, lying medial to the lateral epicondyle.
With the arm by the side, the medial epicondyle lies on a plane which is posterior to that of the lateral epicondyle, so that the humerus appears to be rotated medially. In this position the head of the humerus is directed almost equally backwards and medially, and the posterior surface of the shaft faces posterolaterally. Since the glenoid fossa of the scapula faces anterolaterally, the humerus is not rotated medially relative to the scapula in this position of rest, but it is so rotated relative to the conventional anatomical position. This position of the bone must be remembered when movements of the arm and forearm are considered.
Proximal end
The proximal end of the humerus consists of the head, anatomical neck and the greater and lesser tubercles. It joins the shaft at an ill-defined ‘surgical neck’, which is closely related on its medial side to the axillary nerve and posterior humeral circumflex artery (Fig. 46.7).
Head
The head of the humerus forms rather less than half a spheroid; in sectional profile it is spheroidal (strictly ovoidal) (Fig. 46.7). Its smooth articular surface is covered with hyaline cartilage, which is thicker centrally. When the arm is at rest by the side, it is directed medially, backwards and upwards to articulate with the glenoid cavity of the scapula. The humeral articular surface is much more extensive than the glenoid cavity, and only a portion of it is in contact with the cavity in any one position of the arm.
Anatomical neck
The anatomical neck of the humerus immediately adjoins the margin of the head and forms a slight constriction, which is least apparent in the neighbourhood of the greater tubercle, and superiorly, and for some distance anteriorly and posteriorly: it indicates the line of capsular attachment of the shoulder joint (Fig. 46.7), other than at the intertubercular sulcus, where the long tendon of biceps emerges. Medially, the capsular attachment diverges from the anatomical neck and descends 1 cm or more onto the shaft.
Lesser tubercle
The lesser tubercle is anterior to and just beyond the anatomical neck. It has a smooth, muscular impression on its upper part palpable through the thickness of deltoid 3 cm below the acromial apex. The bony prominence slips away from the examining finger when the humerus is rotated. The lateral edge of the lesser tubercle is sharp and forms the medial border of the intertubercular sulcus. Subscapularis is attached to the lesser tubercle (Fig. 46.6A), and the transverse ligament of the shoulder joint is attached to the lateral margin.
Greater tubercle
The greater tubercle is the most lateral part of the proximal end of the humerus. It projects beyond the lateral border of the acromion. Its posterosuperior aspect, near the anatomical neck, bears three smooth flattened impressions for the attachment of supraspinatus (uppermost), infraspinatus (middle) and teres minor (lowest and placed on the posterior surface of the tubercle) (Fig. 46.6). The attachments of subscapularis and teres minor are not confined to their respective tubercles, but extend for varying distances on to the adjacent metaphysis. The projecting lateral surface of the tubercle presents numerous vascular foramina and is covered by the thick, fleshy deltoid, which produces the normal rounded contour of the shoulder. A part of the subacromial bursa may cover the upper part of this area and separate it from deltoid.
The intertubercular sulcus (bicipital groove) lies between the tubercles. It contains the long tendon of biceps, its synovial sheath, and an ascending branch from the anterior circumflex humeral artery. The rough lateral lip of the groove is marked by the bilaminar tendon of pectoralis major, its floor by the tendon of latissimus dorsi and its medial lip by the tendon of teres major; the attachment of pectoralis major extends beyond that of teres major, that of latissimus dorsi is least extensive.
Shaft
The shaft of the humerus is almost cylindrical in its proximal half but is triangular on section in its distal half, which is compressed in an anteroposterior direction. It can be identified when the arm is grasped firmly, but its outline is obscured by the strong muscles which surround it. It has three surfaces and three borders – which are not everywhere equally obvious.
Anterior border
The anterior border starts on the front of the greater tubercle and runs downwards almost to the lower end of the bone. Its proximal third forms the lateral lip of the intertuberculous sulcus and is roughened for muscular attachments. The succeeding portion is also roughened and forms the anterior limit of the deltoid tubercle; the lower half of the border is smooth and rounded.
Lateral border
The lateral border is conspicuous at the lower end of the bone, where it is thickened to form the lateral supracondylar ridge and its sharp edge is roughened along its anterior aspect. In its middle and upper thirds the border is barely discernible, but in a well-marked bone it can be traced upwards to the posterior surface of the greater tubercle. A little above its middle it is marked by a V-shaped roughened area, the deltoid tubercle. The limbs of the V are broad: the groove for the radial nerve runs downwards behind the posterior limb and fades away on the lower part of the surface.
Medial border
The medial border, although rounded, can be identified without difficulty in the lower half of the shaft, where it becomes the medial supracondylar ridge. In the proximal third the medial border is indistinct until it reappears as the medial lip of the intertubercular sulcus, where it is again rough and reaches the lesser tubercle. In its middle third, the border is interrupted by a wide, shallow groove, the radial or spiral groove, which crosses the bone obliquely, passing downwards and forwards from its posterior to its anterior surface.
Surfaces
The anterolateral surface is bounded by the anterior and lateral borders and is smooth and featureless in its upper part, which is covered by deltoid. About, or a little above, the middle of this surface, deltoid is inserted into the deltoid tubercle; further distally the surface gives origin to the lateral fibres of brachialis, which extend upwards into the floor of the lower end of the groove for the radial nerve (Fig. 46.6). Brachioradialis is attached to the proximal two-thirds of the roughened anterior aspect of the lateral supracondylar ridge, and extensor carpi radialis longus is attached to its distal third. Behind these muscles, the ridge gives attachment to the lateral intermuscular septum of the arm.
The anteromedial surface is bounded by the anterior and medial borders. Rather less than its upper third forms the rough floor of the intertubercular sulcus; the rest of the surface is smooth. Distal to the intertubercular sulcus a small area of the anteromedial surface is devoid of muscular attachment, but its lower half is occupied by the medial part of brachialis (Fig. 46.6A). Coracobrachialis is attached to a roughened strip on the middle of the medial border. The humeral head of pronator teres is attached to a narrow area close to the lowest part of the medial supracondylar ridge, and the ridge itself gives attachment to the medial intermuscular septum of the arm.
A little below its midpoint, the nutrient foramen, which is directed downwards, opens close to the medial border. A hook-shaped process of bone, the supracondylar process, from 2 to 20 mm in length, occasionally projects from the anteromedial surface of the shaft, approximately 5 cm proximal to the medial epicondyle. It is curved downwards and forwards, and its pointed apex is connected to the medial border, just above the epicondyle, by a fibrous band to which part of pronator teres is attached. The foramen completed by this fibrous band usually transmits the median nerve and brachial artery, but sometimes encloses only the nerve, or the nerve plus the ulnar artery (in cases of high division of the brachial artery). A groove which lodges the artery and nerve usually exists behind the process, and may protect the nerve and artery from compression by muscles.
The posterior surface, between the medial and lateral borders, is the most extensive surface and is occupied mostly by the medial head of triceps. A ridge, sometimes rough, descends obliquely and laterally across its proximal third, and gives attachment to the lateral head of triceps. Above triceps, the axillary nerve and the posterior circumflex humeral vessels wind round this aspect of the bone under cover of deltoid. Below and medial to the attachment of the lateral head of triceps, a shallow groove which contains the radial nerve and the profunda brachii vessels, runs downwards and laterally to gain the anterolateral surface of the shaft. The area for the origin of the fleshy medial head of triceps includes a very large part of the posterior surface of the bone. It covers an elongated triangular area, the apex of which is placed on the medial part of the posterior surface above the level of the lower limit of the insertion of teres major. The area widens below and covers the whole surface almost down to the lower end of the bone.
Fractures of the humeral shaft
Fractures of the humerus are comparatively common and may occur at almost any level. The humerus is fractured by muscular action probably more frequently than any other long bone: usually the shaft is broken below the attachment of deltoid. The radial nerve may be injured in its groove or may very rarely become involved later in the growth of callus. Fractures at the proximal end of the humerus may rarely damage the axillary nerve, and similarly fractures of the medial epicondyle may be complicated by damage to the ulnar nerve. Supracondylar fractures are relatively common in children: the end of the proximal fragment can sometimes injure the brachial artery or median nerve. In adults, non-union is more common in the humerus than in any other long bone, although contemporary management of humeral fractures has rendered non-union rare: the incidence of scaphoid non-union is similar, if not greater.
Distal end
The distal end of the humerus is a modified condyle: it is wider transversely and has articular and non-articular parts (Fig. 46.8, Fig. 46.9). The articular part is curved forwards, so that its anterior and posterior surfaces lie in front of the corresponding surfaces of the shaft. It articulates with the radius and the ulna at the elbow joint, and is divided by a faint groove into a lateral capitulum, and a medial trochlea.

Fig. 46.9 Inferior aspect of distal end of left humerus. 1. Trochlea. 2. Capitulum. 3. Medial epicondyle. 4. Sulcus for ulnar nerve. 5. Lateral epicondyle.
The capitulum is a rounded, convex projection, considerably less than half a sphere, which covers the anterior and inferior surfaces of the lateral part of the condyle of the humerus but does not extend onto its posterior surface. It articulates with the discoid head of the radius, which lies in contact with its inferior surface in full extension of the elbow but slides onto its anterior surface during flexion. The groove of the trochlea winds backwards and laterally as it is traced from the anterior to the posterior surface of the bone, and it is wider, deeper and more symmetrical posteriorly. Anteriorly, the medial flange of the pulley is much longer than the lateral, and the surface adjoining its projecting medial margin is convex to accommodate itself to the medial part of the upper surface of the coronoid process of the ulna. These asymmetries entail varying angulation between the humeral and ulnar axes, together with some conjunct rotation. The non-articular part of the condyle includes the medial and lateral epicondyles, olecranon and coronoid and radial fossae.
Trochlea
The trochlea is a pulley-shaped surface that covers the anterior, inferior and posterior surfaces of the condyle of the humerus medially. It articulates with the trochlear notch of the ulna. On its lateral side it is separated from the capitulum by a faint groove; its medial margin projects distally beyond the rest of the bone. When the elbow is extended the inferior and posterior aspects of the trochlea are in contact with the ulna, but, as the joint is flexed, the trochlear notch slides on to the anterior aspect and the posterior aspect is then left uncovered. The downward projection of the medial edge of the trochlea is the principal factor in determining the angulation between the long axis of the humerus and the long axis of the supinated forearm when the elbow is extended.
Medial epicondyle
The medial border of the humerus ends by turning slightly backwards as the medial epicondyle, which forms a conspicuous, blunt projection on the medial side of the condyle. It is subcutaneous and usually visible, especially in passive flexion of the elbow. Its posterior surface is smooth and is crossed by the ulnar nerve, which lies in a shallow sulcus as it enters the forearm. In this situation the nerve can be felt and rolled against the bone, and if it is jarred against the epicondyle, characteristic tingling sensations result. The lower part of the anterior surface of the medial epicondyle is marked by the attachment of the superficial group of forearm flexors. They arise from the epiphysis for the epicondyle, but are entirely extracapsular.
Lateral epicondyle
The lateral border of the humerus terminates at the lateral epicondyle, and its lower portion constitutes the lateral supracondylar ridge. The lateral epicondyle occupies the lateral part of the non-articular portion of the condyle, but does not project beyond the lateral supracondylar ridge. It turns slightly forwards, unlike the medial epicondyle, which turns slightly backwards. Its lateral and anterior surfaces show a well-marked impression for the superficial group of the extensor muscles of the forearm (Fig. 46.6B), which arise from the lateral side of the lower humeral epiphysis, and, like the flexors, are situated outside the articular capsule. The posterior surface, which is very slightly convex, is easily felt in a depression visible behind the extended elbow. A small area on the posterior surface gives origin to anconeus.
Olecranon, coronoid and radial fossae
The olecranon fossa is a deep hollow on the posterior surface of the condyle, immediately above the trochlea, that lodges the tip of the olecranon of the ulna when the elbow is extended. The floor of the fossa is always thin and may be partially deficient. A similar but smaller hollow lies immediately above the trochlea on the anterior surface of the condyle and is termed the coronoid fossa. It accommodates the anterior margin of the coronoid process of the ulna during flexion of the elbow. A very slight depression lies above the capitulum on the lateral side of the coronoid fossa. It is termed the radial fossa, since it is related to the margin of the head of the radius in full flexion of the elbow.
Ossification
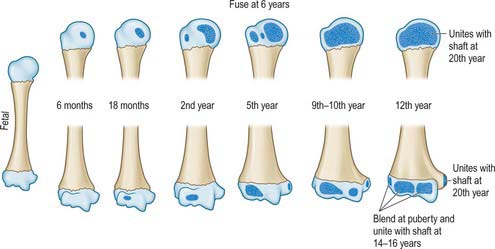
The humerus is ossified from eight centres, in the shaft, head, greater and lesser tubercles, capitulum with the lateral part of the trochlea, the medial part of the trochlea, and one for each epicondyle (Fig. 46.10). The centre for the shaft appears near its middle in the eighth week of intrauterine life, and gradually extends towards the ends. Before birth (20%), or in the first six months afterwards, ossification begins in the head, during the first year in females and second year in males in the greater tubercle, and about the fifth in the lesser tubercle. The existence of a centre in the lesser tubercle is often questioned, perhaps because it is often obscured in the usual anteroposterior radiological views (Fig. 46.11).

Fig. 46.11 Anteroposterior radiograph of the left shoulder in a boy aged 11. Note the conical junction of the humeral epiphysis with the diaphysis. 1. Clavicle. 2. Spine of scapula. 3. Coracoid process. 4. Glenoid cavity. 5. Acromion. 6. Proximal humeral epiphysis. 7. Proximal humeral growth plate.
By the sixth year the centres for the head and tubercles have joined to form a single large epiphysis, which is hollowed out on its inferior surface to adapt it to the somewhat conical upper end of the metaphysis. It fuses with the shaft of the humerus about the twentieth year in males, two years earlier in females. The lower end is ossified as follows. During the first year ossification begins in the capitulum and extends medially to form the chief part of the articular surface; the centre for the medial part of the trochlea appears in the ninth year in females and tenth year in males.
Ossification begins in the medial epicondyle in the fourth year in females, sixth in males, and in the lateral epicondyle about the 12th year. The centres for the lateral epicondyle, capitulum and trochlea fuse around puberty and the composite epiphysis unites with the shaft in the fourteenth year in females, sixteenth in males. The centre for the medial epicondyle forms a separate epiphysis, which is entirely extracapsular and is placed on the posteromedial aspect of the epicondyle. It is separated from the rest of the lower epiphysis by a downgrowth from the shaft, with which it unites about the 20th year.
Amputation of the humerus in youth
The proximal epiphysis joins the humeral shaft later than the distal, which means that growth in length is mainly attributable to growth from the proximal epiphysial plate. After amputation through the arm in youth, the humerus continues to grow and its lower end progressively moulds the surrounding soft tissues so that the stump becomes conical.
JOINTS
STERNOCLAVICULAR JOINT
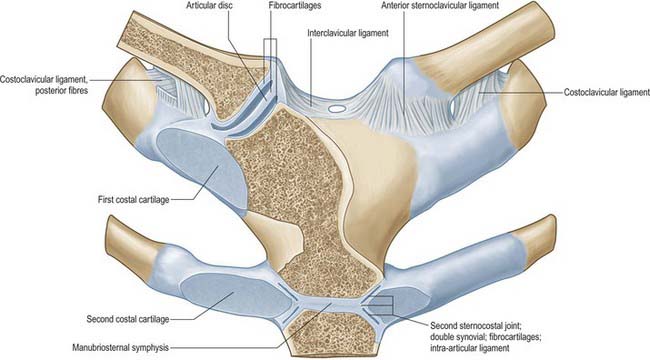
The sternoclavicular joint is a synovial sellar joint and represents the only skeletal articulation between the upper limb and the axial skeleton.
The articulating surfaces are the sternal end of the clavicle and the clavicular notch of the sternum, together with the adjacent superior surface of the first costal cartilage (Fig. 46.12). The larger clavicular articular surface is covered by fibrocartilage, which is thicker than the fibrocartilaginous lamina on the sternum. The joint is convex vertically but slightly concave anteroposteriorly, and is therefore sellar; the clavicular notch of the sternum is reciprocally curved, but the two surfaces are not fully congruent. An articular disc completely divides the joint.
The capsule is thickened in front and behind, but above, and especially below, it is little more than loose areolar tissue.
The ligaments are the anterior and posterior sternoclavicular and the costoclavicular on each side, and the midline interclavicular.
Anterior sternoclavicular ligament
The anterior sternoclavicular ligament is broad and attached above to the anterosuperior aspect of the sternal end of the clavicle. It passes inferomedially to the upper anterior aspect of the manubrium, spreading onto the first costal cartilage.
Posterior sternoclavicular ligament
The posterior sternoclavicular ligament is a weaker band posterior to the joint. It descends inferomedially from the back of the sternal end of the clavicle to the back of the upper manubrium.
The interclavicular ligament is continuous above with deep cervical fascia, and unites the superior aspect of the sternal ends of both clavicles; some fibres are attached to the superior manubrial margin.
The costoclavicular ligament is like an inverted cone, but short and flattened. It has anterior and posterior laminae which are attached to the upper surface of the first rib and costal cartilage, and ascends to the margins of an impression on the inferior clavicular surface at its medial end. Fibres of the anterior lamina ascend laterally and those of the posterior lamina (which are shorter) ascend medially (Fig. 46.12); they fuse laterally and merge medially with the capsule.
The articular disc is flat and almost circular, between the sternal and clavicular surfaces. It is attached above to the posterosuperior border of the articular surface of the clavicle, below to the first costal cartilage near its sternal junction, and by the rest of its circumference to the capsule. It is thicker peripherally, especially in its superoposterior part and a smaller inferomedial one. The capsule around the former is more lax: movements between the clavicle and the disc are more extensive than those between the disc and sternum. The sellar shape of the articular surfaces permits movement in approximately anteroposterior and vertical planes, and some rotation about the long axis of the clavicle. Close-packing probably coincides with maximum posterior rotation associated with full scapular rotation. Some anteroposterior translation also occurs.
The sternoclavicular joint is supplied by branches from the internal thoracic and suprascapular arteries.
The sternoclavicular joint is innervated by branches from the medial supraclavicular nerve and the nerve to subclavius.
There is relatively little bony articular congruence at the sternoclavicular joint. However, the strength of its associated ligaments, and especially its articular disc, actually make it very stable. These factors, and the usual transmission of forces along the clavicle, make dislocation rare: fracture along the clavicular shaft is far more common.
ACROMIOCLAVICULAR JOINT
The acromioclavicular joint is a synovial plane joint.
The articulating surfaces are between the acromial end of the clavicle and the medial acromial margin (Fig. 46.13). The joint is approximately plane, but either surface may be slightly convex, the other being reciprocally concave, and both are covered by fibrocartilage. The clavicular surface is a narrow, oval area which faces inferolaterally and overlaps a corresponding facet on the medial acromial border. The long axis is anteroposterior.
The capsule completely surrounds the articular margins and is strengthened above by the acromioclavicular ligament. The capsule is lined by synovial membrane.
The acromio- and coraco-clavicular ligaments run between the clavicle and the acromion and coracoid processes respectively.
The acromioclavicular ligament is quadrilateral. It extends between the upper aspects of the lateral end of the clavicle and the adjoining acromion. Its parallel fibres interlace with the aponeuroses of trapezius and deltoid.
The coracoclavicular ligament connects the clavicle and the coracoid process of the scapula (Fig. 46.14). Though separate from the acromioclavicular joint, it is a most efficient accessory ligament, and maintains the apposition of the clavicle to the acromion. The trapezoid and conoid parts of the ligament, usually separated by fat or, frequently, by a bursa, connect the medial horizontal part of the coracoid process and lateral end of the subclavian groove of the clavicle; these adjacent areas may even be covered by cartilage to form a coracoclavicular joint.
The trapezoid part is anterolateral and is broad, thin and quadrilateral, ascending slightly from the upper coracoid surface to the trapezoid line on the inferior clavicular surface. It is almost horizontal, its anterior border is free, and its posterior border is joined to the conoid part, forming an angle which projects backwards.
The conoid part is posteromedial and is a dense, almost vertical triangular band. Its base is attached to the conoid tubercle of the clavicle and its inferior apex is attached posteromedially to the root of the coracoid process in front of the scapular notch.
The articular disc often occurs in the upper part of the joint, partially separating the articular surfaces: occasionally it completely divides the joint.
The acromioclavicular joint receives its arterial supply from branches from the suprascapular and thoracoacromial arteries.
The acromioclavicular joint is innervated by branches from the suprascapular and lateral pectoral nerves.
The coracoclavicular ligament stabilizes the acromioclavicular joint. In acromioclavicular dislocation, the ligament is torn and the scapula falls away from the clavicle, which may be slightly elevated by the unopposed pull of trapezius. Dislocation can occur because of the flatness and orientation of the joint surfaces; once the acromioclavicular joint dislocates it never reduces.
Movements at the joint are like those of the sternoclavicular joint. These are passive, i.e. no muscle directly moves the joint, but muscles which move the scapula indirectly move the clavicle. Axial rotation of the clavicle is about 30°, the two joints together therefore, permit about 60° of scapular rotation. Angulation with the scapula occurs in any direction.
MOVEMENTS OF THE PECTORAL (SHOULDER) GIRDLE
Clavicular movements at the sternoclavicular and acromioclavicular joints are inevitably associated with movements of the scapula, and these are usually accompanied by movements of the humerus. The acromioclavicular joint allows anteroposterior gliding and rotation of the acromion, and hence the scapula, on the clavicle: scapular range is increased by movements at the sternoclavicular joint. The sternoclavicular and the acromioclavicular joints, in combination with the fascial space between the scapula and underlying chest wall, are collectively known as the scapulothoracic articulation.
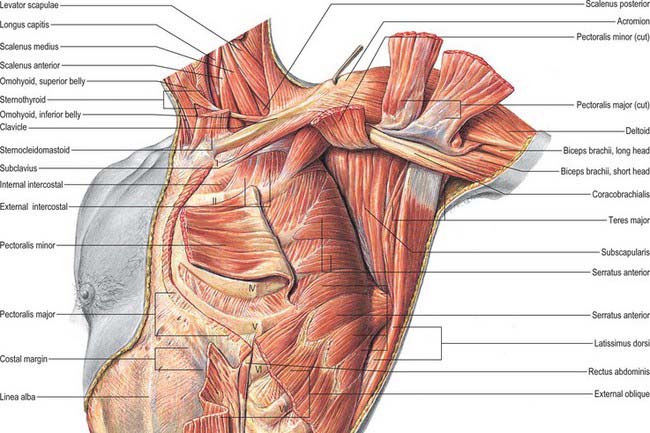
In all scapular movements, it is assumed that subclavius probably steadies the clavicle by drawing it medially and downwards, although its inaccessibility for electromyographic analysis makes its role uncertain. Scapular movements on the thoracic wall are facilitated by areolar tissue between subscapularis, serratus anterior and the chest wall. With the arm by the side, the normal posture of the shoulder girdle relative to the trunk involves moderate activity in trapezius and serratus anterior, and this increases when the limb is loaded.
The following account should be read together with the description of movements of the glenohumeral joint.
Elevation and depression
Scapular elevation and depression, as in ‘shrugging the shoulders’, do not necessarily imply movement at the shoulder joint. In elevation, slight angulation or swing occurs at the acromioclavicular joint. The sternal end of the clavicle, rotating about an anteroposterior axis through the bone above the medial attachment of the costoclavicular ligament, slides down over the articular disc (translation). This is checked by antagonist muscles and tension in the costoclavicular ligament and lower capsule. It is produced by the upper part of trapezius and levator scapulae, and since these tend to rotate the scapula in opposite directions, pure elevation can occur. In depression, slight angulation occurs at the acromioclavicular joint, and the clavicle slides up on the disc at the sternoclavicular joint. The movements are checked by antagonist muscles, the interclavicular and sternoclavicular ligaments and the articular disc. Usually gravity alone is sufficient: when necessary, the lowest part of serratus anterior and pectoralis minor are active depressors.
Protraction and retraction
Protraction (forward movement) round the thoracic wall occurs in pushing, thrusting and reaching movements, usually with some lateral rotation. The acromion advances over the clavicular facet to the limit, and the shoulder is simultaneously advanced by forward movement of the lateral end of the clavicle and posterior translation of its sternal end over the sternal facet, carrying the disc with it. Antagonist muscles, together with the anterior sternoclavicular ligament and posterior lamina of the costoclavicular ligament, check backward slide of the sternal end. Serratus anterior and pectoralis minor are prime movers and maintain continuous apposition of the scapula, especially its medial border, in smooth gliding on the thoracic wall. The upper part of latissimus dorsi also acts like a strap across the inferior scapular angle in protraction and lateral rotation.
In scapular retraction, i.e. bracing back the shoulders, these movements are reversed and checked at the sternoclavicular joint by the posterior sternoclavicular ligament and anterior lamina of the costoclavicular ligament. Trapezius and the rhomboids are prime movers, but gravity may also produce retraction when the weight of the trunk is taken by the arms in leaning forwards, which is to a degree controlled by protractive musculature.
When force is applied at the end of an outstretched arm, e.g. in a fall on the hand, pressure transmitted to the glenoid fossa tends to drive the sloping acromial facet below the acromial end of the clavicle. It also tenses the trapezoid ligament, which resists the displacement.
Lateral and medial rotation
Lateral (upward) rotation of the scapula increases the range of humeral elevation by turning the glenoid cavity to face almost directly up, e.g. raising an arm above the head. This movement is always associated with some humeral elevation and with protraction of the scapula. Scapular rotation requires movement at both sternoclavicular and acromioclavicular joints: the sternoclavicular joint permits elevation of the lateral end of the clavicle, a movement which is almost complete when the arm is abducted to 90°. The acromioclavicular joint moves in the first 30° of abduction, when the conoid ligament becomes taut, and is subsequently accompanied by clavicular rotation at the sternoclavicular joint around the longitudinal axis of the bone. The medial end is depressed further as the lateral end continues to rise. Some acromioclavicular movement also occurs in the final stages of humeral abduction. Trapezius (upper part) and serratus anterior (lower part) are prime movers.
Medial (downward) rotation is usually effected by gravity: gradual active lengthening of trapezius and serratus anterior is sufficient to control it. When more force is needed, levator scapulae, the rhomboids and, in the initial stages, pectoralis minor, are prime movers in returning the scapula to a position of rest.
Muscles which are antagonists in one movement may combine as prime movers in another. Movements, not muscles, are represented in cerebral motor areas. Muscles are not grouped unalterably in nervous control but can be variably combined as demands dictate. Thus serratus anterior and trapezius are opposed in scapular movement round the thorax, but combine as prime movers in lateral rotation of the scapula.
GLENOHUMERAL (SHOULDER) JOINT
The glenohumeral joint is a synovial multiaxial spheroidal joint between the roughly hemispherical head of the humerus and the shallow glenoid fossa of the scapula (Fig. 46.15). Notable for its relative lack of bony constraint, the joint possesses three degrees of freedom. Its static and dynamic stability depends on the surrounding muscular and soft tissue envelope more than on its shape and ligaments: effective function is achieved by a complex interaction between the articular and soft tissue restraints. It is the most mobile joint in the body and the most frequently dislocated.
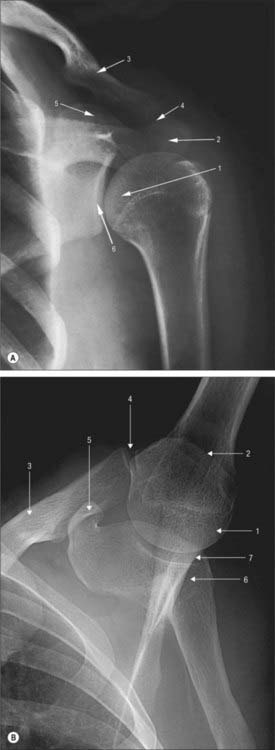
Fig. 46.15 Radiographs of the left shoulder of an 18 year old female in anteroposterior view (A) and axillary view with the arm abducted (B). 1. Head of humerus. 2. Acromion. 3. Clavicle. 4. Acromioclavicular joint. 5. Coracoid. 6. Glenoid. 7. Glenohumeral articulation.
The articular surfaces are reciprocally curved and are really ovoids. (Here, as in the hip, where ovoid surfaces are almost spherical they are often termed spheroidal.) The area of the humeral convexity exceeds that of the glenoid concavity such that only a small portion opposes the glenoid in any position (Fig. 46.16). The remaining capitular articular surface is in contact with the capsule, so that contact on the glenoid fossa is much more uniformly distributed over its entire articular surface. The radius of curvature of the glenoid fossa in the coronal plane is greater than that of the humeral head, and is deepened by a fibrocartilaginous rim, the glenoid labrum (Fig. 46.13, Fig. 46.17). Both articular surfaces are covered by hyaline cartilage, which is thickest centrally and thinner peripherally over the humerus, and the reverse in the glenoid cavity. In most positions, their curvatures are not fully congruent, and the joint is loose-packed. Close packing (full congruence) is reached with the humerus abducted and laterally rotated (Fig. 5.61).
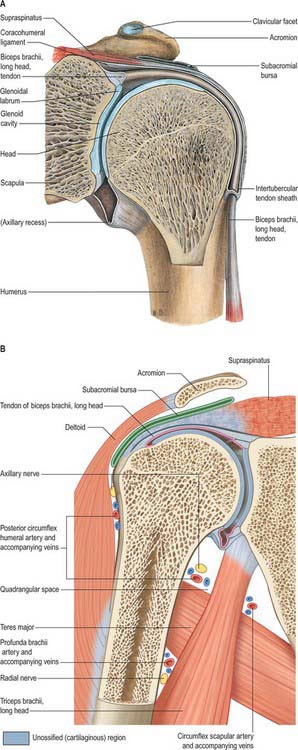
Fig. 46.16 Coronal sections through the left shoulder joint viewed from the posterior aspect. A, Anteriorly placed coronal section to show tendon of biceps, long head. B, Posteriorly placed coronal section to show subacromial bursa and contents of quadrangular space.
(From Sobotta 2006.)
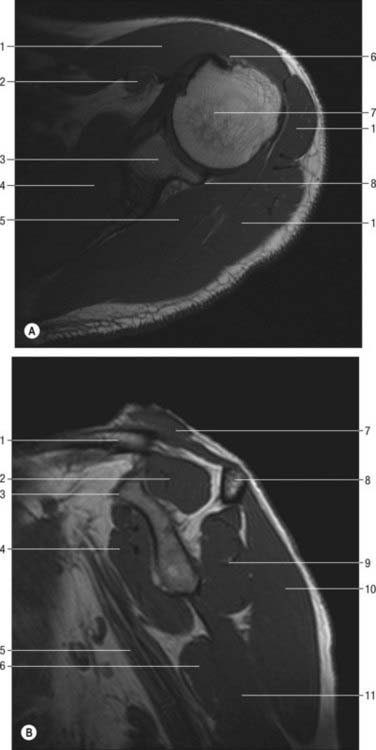
Fig. 46.17 MRI of shoulder. A, Axial image. B, Median sagittal oblique image at base of coracoid. A: 1. Deltoid. 2. Coracobrachialis. 3. Glenoid. 4. Subscapularis. 5. Infraspinatus. 6. Tendon of the long head of biceps. 7. Head of humerus. 8. Posterior labrum. B: 1. Clavicle. 2. Supraspinatus. 3. Coracoid. 4. Subscapularis. 5. Axillary nerve. 6. Latissimus dorsi. 7. Trapezius. 8. Scapular spine. 9. Infraspinatus. 10. Deltoid. 11. Triceps. Compare A with Fig. 46.23.
The glenoid labrum is a fibrocartilaginous rim around the glenoid fossa. It is triangular in section and varies in size and thickness; its base is attached to the margin of the fossa and its free inner edge projects as a continuation of the curve of the glenoid. It blends above with two fasciculi from the long tendon of biceps. The labrum deepens the cavity, may protect the bone, and probably assists lubrication. Its attachment is sometimes partly deficient anterosuperiorly, in which case synovial membrane may protrude through the gaps.
A fibrous capsule envelops the joint (Fig. 46.14, Fig. 46.16). It is attached medially to the glenoid neck outside the glenoid labrum, and encroaches on the coracoid process to include the attachment of the long head of biceps. The capsule often extends and attaches to the base of the coracoid and to the body of the scapula, forming anterior and posterior recesses. Laterally, it is attached to the anatomical neck of the humerus, i.e. near the articular margin, except inferomedially, where it descends more than 1 cm on the humeral shaft. It is so lax that the bones can be distracted for 2 or 3 cm, which accords with the very wide range of movement possible at the glenohumeral joint. However, such unnatural separation requires relaxation of the upper capsule by abduction.
The fibrous capsule is supported by the tendons of supraspinatus (above), infraspinatus and teres minor (behind), subscapularis (in front) and by the long head of triceps (below). The rotator interval is a medially based triangular area of uncovered capsule between the superior edge of subscapularis and the anterior edge of supraspinatus as these tendons pass on either side of the base of the coracoid: it may represent an area of weakness that increases instability in some shoulders. Triceps is separated from the capsule by the axillary nerve and posterior circumflex humeral vessels as they pass back from the axilla (Fig. 46.14). The capsule is least supported inferiorly, and subjected to the greatest strain in full abduction, when it is stretched tightly across the humeral head. It is strengthened anteriorly by extensions from the tendons of pectoralis major and teres major.
There are usually two or three openings in the capsule: below the coracoid process, connecting the joint to a bursa behind the tendon of subscapularis (anterior); between the humeral tubercles, transmitting the long tendon of biceps and its synovial sheath; connecting the joint to a bursa under the tendon of infraspinatus (posterior and inconstant).
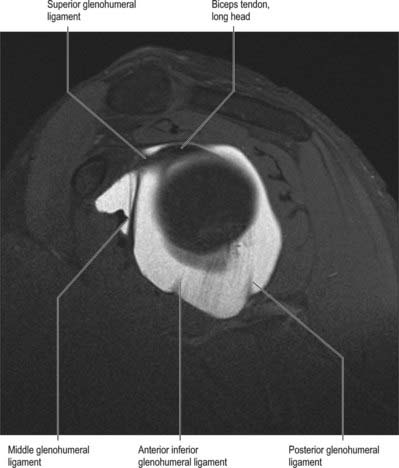
The ligaments associated with the glenohumeral joint are the glenohumeral (superior, middle and inferior), coracohumeral and transverse humeral.
Three glenohumeral ligaments, only visible from within the joint, reinforce the capsule anteriorly and inferiorly (Fig. 46.18). They do not act as traditional ligaments (which carry a pure tensile force along their length), but become taut at varying positions of abduction and humeral rotation, acting as ‘check-reins’. Moreover, they do not have the strength characteristics of the ligaments at the knee. The superior glenohumeral ligament passes from the supraglenoid tubercle, just anterior to the origin of the long head of biceps, to the humerus near the proximal tip of the lesser tubercle on the medial ridge of the intertuberculous groove, the fovea capitis. It forms an anterior cover around the long head of biceps, and is part of the rotator interval. Together with the coracohumeral ligament it is an important stabilizer in the inferior direction, helping to keep the humeral head suspended (the coracohumeral ligament is more robust than the superior glenohumeral ligament). The middle glenohumeral ligament arises from a wide attachment below the superior glenohumeral ligament, along the anterior glenoid margin as far as the inferior third of the rim, and passes obliquely inferolaterally, enlarging as it does, to attach to the lesser tubercle deep to the tendon of subscapularis, with which it blends. The width and thickness of this ligament may be as much as 2 cm and 4 mm respectively. It provides anterior stability at 45° and 60° abduction. The thicker and longer inferior glenohumeral ligament complex is a hammock-like structure with anchor points on the anterior and posterior sides of the glenoid. It arises from the anterior, middle and posterior margins of the glenoid labrum, below the epiphysial line, and passes anteroinferiorly to the inferior and medial aspects of the neck of the humerus. The anterior, superior edge of the inferior ligament is thickened as the superior band, and the diffuse thickening of the anterior part of the capsule to which it is attached is known as the axillary pouch. The anterior band of the inferior glenohumeral ligament is thought to be the primary static anterior stabilizer of the abducted and externally rotated glenohumeral joint. (For further details consult Burkart & Debski 2002.)
The coracohumeral ligament is attached to the dorsolateral base of the coracoid process and extends as two bands, which blend with the capsule, to the greater and lesser tubercles (Fig. 46.14). Portions of the coracohumeral ligament form a tunnel for the biceps tendon on the anterior side of the joint. The rotator interval is reinforced by the coracohumeral ligament. It also blends inferiorly with the superior glenohumeral ligament.
The transverse humeral ligament is a broad band which passes between the humeral tubercles, and is attached superior to the epiphysial line (Fig. 46.14). It converts the intertubercular sulcus into a canal, and acts as a retinaculum for the long tendon of biceps.
The synovial membrane lines the capsule and covers parts of the anatomical neck. The long tendon of biceps traverses the joint in a synovial sheath which continues into the intertubercular sulcus as far as the surgical neck of the humerus (Fig. 46.14, Fig. 46.16).
Bursae Many bursae adjoin the shoulder joint.
They are usually found between the tendon of subscapularis and the capsule, communicating with the joint between the superior and middle glenohumeral ligaments; on the superior acromial aspect; between the coracoid process and capsule; between teres major and the long head of triceps: anterior and posterior to the tendon of latissimus dorsi. The subacromial bursa, between deltoid and the capsule, does not communicate with the joint cavity but is prolonged under the acromion and coracoacromial ligament, and between them and supraspinatus: it appears to be attached, together with the subdeltoid fascia, to the acromion. Bursae sometimes occur behind coracobrachialis and between the tendon of infraspinatus and the capsule, occasionally opening into the joint.
The glenohumeral joint is supplied by branches from the anterior and posterior circumflex humeral, suprascapular and circumflex scapular vessels.
The glenohumeral joint is innervated mainly from the posterior cord of the brachial plexus. The capsule is supplied by the suprascapular nerve (posterior and superior parts), axillary nerve (anteroinferior) and the lateral pectoral nerve (anterosuperior).
The articulation between the relatively large humeral head and the shallow glenoid fossa allow a wide range of movement at the expense of providing an unstable bony complex. The anterior joint capsule is strong but lax. A variety of additional factors help to increase the stability of the joint: the glenoid labrum deepens the concavity of the articulating glenoid, the glenohumeral ligaments act as static stabilizers in certain positions, and there is a negative pressure within the joint. The coracoacromial arch (coracoid, acromion and coracoacromial ligament) prevents upward dislocation of the humerus. The tendons of subscapularis, supraspinatus, infraspinatus and teres minor fuse with the lateral part of the joint capsule to form the ‘rotator cuff’. These short muscles collectively produce a compressive force during active glenohumeral movements which maintains congruent contact between the head of the humerus and the glenoid fossa, helps to resist skid, and checks excessive translation. The rotator cuff also provides strong lateral stability and prevents this part of the lax capsule from being nipped during joint movements. The long head of biceps offers additional superior support. The long head of triceps offers inferior support which is particularly important when the shoulder is abducted. However, the glenohumeral joint is least stabile inferiorly when the shoulder is fully abducted.
Movements at the shoulder (glenohumeral) joint
The shoulder is capable of any combination of swing and spin over a very wide range. Laxity of the capsule, and a humeral head which is large relative to a shallow glenoid fossa, afford a wider range of movement than at any other joint. Flexion–extension, abduction–adduction, circumduction and medial and lateral rotation all occur at the shoulder. Although the majority of the movement of the shoulder occurs at the glenohumeral joint, there is a varying contribution from the scapulothoracic articulation in most directions, most significantly in abduction, and excluding lateral rotation.
In analysis of shoulder movements it is preferable to refer humeral movement to the scapula, rather than to conventional anatomical planes (Fig. 46.19). When the arm hangs at rest the glenoid fossa faces almost equally forwards and laterally, and the humeral capitular and scapular (topographical) axes correspond, although the humerus, relative to the anatomical position, is medially rotated. Flexion carries the arm anteromedially on an axis through the humeral head orthogonal to the glenoid fossa at its centre. Abduction and adduction occur in a vertical plane orthogonal to that of flexion–extension; the axis is horizontal, through the humeral head, parallel with the glenoid plane. Pure abduction raises the arm anterolaterally in the plane of the scapula. However, when referred to the trunk, flexion and extension occur in the paramedian plane, and abduction and adduction in the coronal plane. In this sense, raising the arm vertically from flexion or raising it from abduction are both accompanied by humeral rotation in opposite directions. Whether ‘scapular’ or any other plane of abduction is described, these are selections from an infinite series. In scapular abduction points on the humeral surface pursue vertical cords but in rotation they are horizontal. In ‘pure’ flexion–extension, in a plane orthogonal to the scapula the axis of movement, and the notional ‘mechanical axis’, are regarded as projected from the centre of the glenoid cavity.
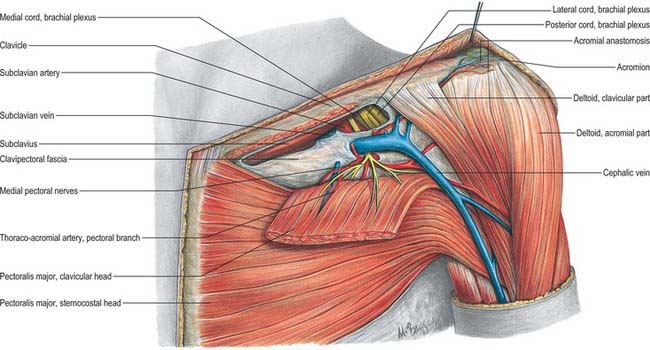
Fig. 46.19 Left deltopectoral groove showing clavipectoral fascia and thoracoacromial axis.
(From Sobotta 2006.)
Glenohumeral abduction is approximately 90°, but angles up to 120° have been reported. Some 60° further abduction occurs at the sterno- and acromioclavicular articulations. Contralateral vertebral flexion also aids in bringing the arm to the vertical. During active elevation, movements at the glenohumeral and acromioclavicular joints are simultaneous, except in the initial few degrees, when most, often all, movement is glenohumeral. For every 15° of elevation, glenohumeral movement is said to be 10° and scapular movement 5°. During the initial stages of abduction, subscapularis, infraspinatus and teres minor counteract the strong upward component of pull of deltoid, which would otherwise cause the humeral head to slide up; the additive turning moments exerted by deltoid and supraspinatus about the shoulder joint can then abduct the arm.
In flexion, the humerus swings at right angles to the scapular plane and scapular rotation cannot increase the elevation (120°) obtainable in full flexion. If the fully flexed humerus is also abducted, elevation increases pro rata until, when the humerus reaches the scapular plane, i.e. when true abduction is reached, 180° of elevation becomes possible. In medial or lateral rotation, the humerus revolves about one-quarter of a circle around a vertical axis; the range is greatest when the arm is pendent, and least when it is vertical. When assessing the rotational range at the glenohumeral joint, the forearm should be flexed to a right angle at the elbow: this will prevent the effects of superadded pronation or supination in the pendent limb. In circumduction, which is a succession of the foregoing movements, the distal end of the humerus describes the base of a cone, its apex at the humeral head. This glenohumeral movement can be much increased by scapular movements, e.g. in acts of slinging objects with force.
The peculiar relation of the long head of biceps to the shoulder joint may serve several purposes. By its connection with both the shoulder and elbow, the muscle harmonizes their actions as an elastic ligament during all their movements. It helps to prevent the humeral head impinging on the acromion when deltoid contracts and to steady it in movements of the arm. In paralysis of supraspinatus it may also help initiate abduction of the arm, particularly when the humerus is laterally rotated.
The muscles which produce movements at the glenohumeral joint are principally deltoid, pectoralis major, latissimus dorsi and teres major. These long muscles all converge on the humerus, acting at mechanical advantage on a joint which, as a result of glenoid shallowness and capsular laxity, is relatively unstable. The long muscles are counteracted by the rotator cuff, a group of short muscles (subscapularis, supraspinatus, infraspinatus and teres minor) which are attached nearer to the joint, and which centre the head of the humerus in the glenoid fossa through the midrange of motion, when the capsuloligamentous structures are lax.
Pectoralis major (clavicular part), deltoid (anterior fibres) and coracobrachialis assisted by biceps. The sternocostal part of pectoralis major is a major force in flexion forwards to the coronal plane from full extension.
Deltoid (posterior fibres) and teres major, from the dependent position. When the fully flexed arm is extended against resistance, latissimus dorsi and the sternocostal part of pectoralis major act powerfully until the arm reaches the coronal plane.
Deltoid. Initially its effect is mainly upward and, unless opposed, this would displace the humerus upwards. Subscapularis, infraspinatus and teres minor exert downward traction and so apply an opposing force: together with deltoid they constitute a ‘couple’ to produce abduction in the scapular plane. Supraspinatus assists in effecting and maintaining this movement, but its precise role is controversial.
The subacromial space is defined inferiorly by the humeral head, and superiorly by the anterior edge and inferior surface of the anterior third of the acromion, coracoacromial ligament and acromioclavicular joint, forming the coracoacromial arch. It is occupied by the supraspinatus tendon, subacromial bursa, tendon of the long head of biceps brachii, and the capsule of the shoulder joint. Rotator cuff disease is a painful condition with a multifactorial aetiology in which severe or chronic impingement of the rotator cuff tendons on the undersurface of the coracacromial arch is often a significant factor. The cuff normally impinges against the coracoacromial arch when the humerus is abducted, flexed and internally rotated. This is known as the impingement position. The supraspinatus tendon is anatomically affected most by the impingement, which interestingly also coincides with an area of reduced vascularity in this tendon. Severe impingement can be caused by thickening of the coracoacromial arch, by inflammation of the cuff from disorders such as rheumatoid arthritis, or as a result of prolonged overuse in the impingement position, e.g. in cleaning windows. When associated with a tendinopathy from age-related degenerative changes within the tendon, impingement may be associated with partial or complete tears of the cuff. Clinically, this condition causes tenderness over the anterior portion of the acromion, and pain which typically occurs on abducting the shoulder between 60° and 120° (the painful arc).
Glenohumeral joint dislocations
The glenohumeral joint is the most frequently dislocated joint in the body. It is most unstable anteroinferiorly, which explains why the vast majority of dislocations are anterior, and occur when the arm is forced backwards when it is in abduction, external rotation and extension. Clinically, a dislocated shoulder loses its normal contour, and the acromion process, rather than the greater tubercle, becomes the most lateral bony structure. The axillary nerve and artery may be injured during dislocation, and this can lead to inability to abduct the shoulder as a result of paralysis of deltoid together with an area of anaesthesia over the distal part of the muscle (sometimes referred to as the ‘badge area’ of skin), as well as ischaemic changes in the limb. Posterior dislocation is rare and typically occurs when violent movements produce marked internal rotation and adduction, e.g. in epileptic seizures or electric shock.
MUSCLES
Pectoralis major
Pectoralis major (Fig. 46.19) is a thick, fan-shaped muscle. It arises from the anterior surface of the sternal half of the clavicle; half the breadth of the anterior surface of the sternum down to the level of the sixth or seventh costal cartilage; the first to the seventh costal cartilages (first and seventh often omitted); the sternal end of the sixth rib; and the aponeurosis of external oblique. The clavicular fibres are usually separated from the sternal fibres by a slight cleft. The muscle converges to a flat tendon, approximately 5 cm across, which is attached to the lateral lip of the intertubercular sulcus of the humerus. The tendon is bilaminar. The thicker anterior lamina is formed by fibres from the manubrium, which are joined superficially by clavicular fibres and deeply by fibres from the sternal margin and the second to fifth costal cartilages. Clavicular fibres may be prolonged into the deltoid tendon. The posterior lamina receives fibres from the sixth (and often seventh) costal cartilages, sixth rib, sternum, and aponeurosis of the external oblique. Costal fibres join the lamina without twisting. Fibres from the sternum and aponeurosis curve around the lower border, turning successively behind those above them, which means that this part of the muscle is twisted so that the fibres that are lowest at their medial origin are highest at their insertion on the humerus. The posterior lamina reaches higher on the humerus than the anterior, and gives off an expansion which covers the intertubercular sulcus and blends with the capsular ligament of the shoulder joint. An expansion from the deepest part of the lamina lines the intertubercular sulcus at its linear insertion; from its lower border another expansion descends into the deep fascia of the upper arm.
The rounded lower border of the muscle forms the anterior axillary fold, and becomes conspicuous in abduction against resistance.
The abdominal slip from the aponeurosis of the external oblique is sometimes absent. The number of costal attachments and the extent to which the clavicular and costal parts are separated vary. Right and left muscles may decussate across the sternum. A superficial vertical slip, or slips, may ascend from the lower costal cartilages and rectus sheath to blend with sternocleidomastoid or to attach to the upper sternum or costal cartilages. This is sternalis (rectus sternalis). The muscle may be partially or completely absent.
Skin, superficial fascia, platysma, medial and intermediate supraclavicular nerves, breast, and deep fascia are all anterior. The sternum, ribs and costal cartilages, clavipectoral fascia, subclavius, pectoralis minor, serratus anterior, external intercostal muscles and membranes are all posterior. Pectoralis major forms the superficial layer of the anterior axillary wall, and hence lies anterior to the axillary vessels and nerves and the upper parts of biceps and coracobrachialis. Its upper border is separated from deltoid by the infraclavicular fossa, which contains the cephalic vein and deltoid branch of the thoraco-acromial artery. Its lower border forms the anterior axillary fold. Pectoralis major is separated from latissimus dorsi on the medial axillary wall, but the two muscles converge as they approach the lateral axillary wall: the floor of the intertuberculous sulcus lies between their attachments.
Pectoralis major is supplied by one dominant vascular pedicle from the pectoral branch of the thoraco-acromial axis, supplemented by several smaller secondary segmental vessels from the deltoid and clavicular branches of the thoraco-acromial axis, and perforating branches of the internal thoracic arteries and superior and lateral thoracic arteries.
The presence of a dominant vascular pedicle (together with its musculocutaneous perforators) means that a musculocutaneous flap in this region can be surgically raised solely on the pectoral branch (the pectoralis major musculocutaneous flap). This flap can be used to reconstruct areas of missing tissue following head and neck cancer resections.
Pectoralis major is supplied through the medial and lateral pectoral nerves. Fibres for the clavicular part are from C5 and 6; those for the sternocostal part are from C6, 7, 8, and T1.
The two parts of the muscle can act separately or together. The whole muscle assists adduction and medial rotation of the humerus against resistance. It swings the extended arm forwards and medially, its clavicular part acting with the anterior fibres of deltoid and coracobrachialis: the sternocostal part is relaxed. The opposite movement is usually aided by gravity. When it is resisted, the sternocostal part acts together with latissimus dorsi, teres major and the posterior fibres of deltoid: the clavicular part is relaxed. With the raised arms fixed, e.g. gripping a branch, the same combination of muscles draws the trunk up and forwards. Pectoralis major is active in deep inspiration. Electromyography suggests that the clavicular part acts alone in medial rotation.
To test the clavicular head, the abducted arm is flexed against resistance. To test the sternocostal head, the arm is adducted against resistance.
Poland syndrome is a rare congenital anomaly where there is hypoplasia of the thoracic chest wall muscles and ipsilateral hypoplasia of the arm and hand. It occurs in approximately 1 : 50,000 live births. The major clinical features are that the sternocostal head of pectoralis major and all of pectoralis minor are absent. In addition, there may be hypoplasia of latissimus dorsi, serratus anterior, external oblique, supraspinatus, infraspinatus, deltoid and the intercostal muscles, and hypoplasia of the hemithorax and ribs. There may be ipsilateral breast hypoplasia and absent nipple-areolar-complex (Ch. 55).
Hypoplasia affecting the arm ranges from syndactyly to symbrachydactyly and ectrodactyly. The second, third and fourth fingers are the most affected; the wrist, forearm, upper arm and scapula are variably involved.
The aetiology is unclear. It has been suggested that the condition is caused by disruption of the arterial blood supply to the subclavian vessels during the sixth and seventh week of embryonic life, or by disruption of lateral plate mesoderm 2–4 weeks after fertilization.
Pectoralis minor
Pectoralis minor is a thin, triangular muscle lying posterior (deep) to pectoralis major (Fig. 46.20). It arises from the upper margins and outer surfaces of the third to fifth ribs (frequently second to fourth), near their cartilages, and from the fascia over the adjoining external intercostal muscles. Its fibres ascend laterally under cover of pectoralis major, converging in a flat tendon which is attached to the medial border and upper surface of the coracoid process of the scapula. Part or all of the tendon may cross the coracoid process into the coraco-acromial ligament, or even beyond to the coracohumeral ligament, thereby gaining attachment to the humerus.
Slips of the muscle are sometimes separated and vary in number and level. In rare cases, one passes from the first rib to the coracoid (pectoralis minimus). The costal attachments can be 2nd to 5th ribs; 3rd to 5th; 2nd to 4th; 3rd to 4th. The muscle can be present or absent when the pectoralis major is absent.
Pectoralis major, the lateral pectoral nerve and pectoral branches of the thoraco-acromial artery are anterior. The ribs, external intercostals, serratus anterior, the axilla, axillary vessels, lymphatics and brachial plexus are all posterior. The upper border of pectoralis minor is separated from the clavicle by a triangular gap which is filled by the clavipectoral fascia, behind which are the axillary vessels, lymphatics and nerves. The lateral thoracic artery follows the lower border of the muscle. The medial pectoral nerves pierce and partly supply the muscle.
Pectoralis minor is supplied by pectoral and deltoid branches of the thoraco-acromial and superior and lateral thoracic arteries.
Pectoralis minor is innervated by branches of the medial and lateral pectoral nerves, C5, 6, 7, 8 and T1.
Pectoralis minor assists serratus anterior in drawing the scapula forwards around the chest wall. With levator scapulae and the rhomboids it rotates the scapula, depressing the point of the shoulder. Both pectoral muscles are electromyographically quiescent in normal inspiration, but are active in forced inspiration.
Subclavius
Subclavius is a small, triangular muscle tucked between the clavicle and the first rib (Fig. 46.20). It arises from the junction of the first rib and its costal cartilage by a thick tendon, prolonged at its inferior margin and anterior to the costoclavicular ligament. It passes upwards and laterally to a groove on the under surface of the middle third of the clavicle, where it is attached by muscular fibres.
Subclavius may be attached to the coracoid process or the upper border of the scapula as well as, or instead of, the clavicle.
Posteriorly subclavius is separated from the first rib by the subclavian vessels and brachial plexus, and anteriorly it is separated from pectoralis major by the anterior lamina of the clavipectoral fascia.
Subclavius is supplied by the clavicular branch of the thoraco-acromial artery and the suprascapular artery.
Subclavius is supplied by the subclavian branch of the brachial plexus, which contains fibres from C5 and 6.
Subclavius probably pulls the point of the shoulder down and forwards and braces the clavicle against the articular disc of the sternoclavicular joint: however it is inaccessible to palpation, and difficult to investigate by electromyography. It ‘protects’ the subclavian vessels in fractures of the clavicle, which rarely involve these vessels.
Trapezius
Trapezius is a flat, triangular muscle which extends over the back of the neck and upper thorax (Fig. 54.15). The paired trapezius muscles form a diamond shape, from which the name is derived: the lateral angles occur at the shoulder tips, the superior angle at the occipital protuberance and superior nuchal lines, and the inferior angle at the spine of the twelfth thoracic vertebra. On either side, the muscle is attached to the medial third of the superior nuchal line, external occipital protuberance, ligamentum nuchae, and apices of the spinous processes and their supraspinous ligaments from C7 to T12. Superior fibres descend, inferior fibres ascend, and the fibres between them proceed horizontally: all converge laterally on the shoulder. The superior fibres are attached to the posterior border of the lateral third of the clavicle; the middle fibres to the medial acromial margin and superior lip of the crest of the scapular spine; and the inferior fibres pass into an aponeurosis which glides over a smooth triangular surface at the medial end of the scapular spine and is attached to a tubercle at its lateral apex. The occipital attachment is by a fibrous lamina, which is also adherent to the skin. The spinal attachment is by a broad triangular aponeurosis from the sixth cervical to the third thoracic vertebrae, and by short tendinous fibres below this.
The clavicular attachment of trapezius varies in extent, sometimes reaching mid-clavicle, and occasionally blending with sternocleidomastoid. The vertebral attachment sometimes stops at the eighth thoracic spine. The occipital attachment may be absent. Cervical and dorsal parts are occasionally separate.
The upper third of trapezius is supplied by a transverse muscular branch which arises from the occipital artery at the level of the mastoid process. It enters the muscle on its deep surface and gives off several musculocutaneous perforators to the overlying skin.
The middle portion of trapezius, together with an area of overlying skin, is supplied by the superficial cervical artery or by a superficial branch of the transverse cervical artery, via musculocutaneous perforators.
The lower third of trapezius is supplied by a muscular branch from the dorsal scapular artery, passing medial to the medial border of the scapula. It reaches the deep surface of the muscle either by piercing the rhomboids or by passing between rhomboid major and minor at the level of the base of the spine of the scapula. It anastomoses with the medial and lateral perforating branches of the posterior intercostal arteries.
The presence of these three discrete vascular pedicles means that musculocutaneous flaps can be surgically raised based on these individual arteries and their accompanying venae comitantes. These flaps can be used for reconstructing areas in the posterior head and neck.
Trapezius is innervated by the spinal part of the accessory nerve. Sensory (proprioceptive) branches are derived from the ventral rami of C3 and C4.
Trapezius cooperates with other muscles in steadying the scapula, controlling it during movements of the arm, and maintaining the level and poise of the shoulder. Electromyographic activity is minimal in the unloaded arm, and heavy loads can be suspended with a small contribution from the upper part. Acting with levator scapulae, the upper fibres elevate the scapula and with it the point of the shoulder; acting with serratus anterior, trapezius rotates the scapula forward (upwards) so that the arm can be raised above the head; and acting with the rhomboids, it retracts the scapula, bracing back the shoulder. With the shoulder fixed, trapezius may bend the head and neck backwards and laterally. Trapezius, levator scapulae, rhomboids and serratus anterior combine in producing a variety of scapular rotations (p. 803).
Deltoid
Deltoid is a thick, curved triangle of muscle. It arises from the anterior border and superior surface of the lateral third of the clavicle, the lateral margin and superior surface of the acromion, and the lower edge of the crest of the scapular spine (other than its smooth medial triangular surface) (Fig. 46.19). The fibres converge inferiorly to a short, substantial tendon which is attached to the deltoid tubercle on the lateral aspect of the midshaft of the humerus. Anterior and posterior fibres converge directly to this tendon. The intermediate part is multipennate: four intramuscular septa descend from the acromion to interdigitate with three septa ascending from the deltoid tubercle. The septa are connected by short muscle fibres, which provide powerful traction. The fasciculi are large, producing a coarse longitudinal striation. The muscle surrounds the glenohumeral articulation on all sides except inferomedially, lending the shoulder its rounded profile. In contraction its borders are easily seen and felt. The tendon gives off an expansion into the brachial deep fascia which may reach the forearm.
Deltoid may fuse with pectoralis major or may receive additional slips from trapezius, the infraspinous fascia or the lateral scapular border.
The skin, superficial and deep fasciae, platysma, lateral supraclavicular and upper lateral brachial cutaneous nerves are all superficial. The coracoid process, coraco-acromial ligament, subacromial bursa, tendons of pectoralis minor, coracobrachialis, both heads of biceps, pectoralis major, subscapularis, supraspinatus, infraspinatus, teres minor, long and lateral heads of triceps, the circumflex humeral vessels, axillary nerve, and the surgical neck and upper shaft of the humerus, including both tubercles, all lie deep to deltoid. The anterior border of the muscle is separated proximally from pectoralis major by the infraclavicular fossa, which contains the cephalic vein and deltoid branches of the thoraco-acromial artery. Distally, the muscles are in contact, and their tendons are usually united. The posterior border overlies infraspinatus and triceps.
Deltoid is supplied by acromial and deltoid branches of the thoraco-acromial artery; the anterior and posterior circumflex humeral arteries; subscapular artery; and the deltoid branch of profunda brachii.
Different parts of the muscle can act independently as well as together. Anterior fibres assist pectoralis major in drawing the arm forwards and rotating it medially. Posterior fibres act with latissimus dorsi and teres major in drawing the arm backwards and rotating it laterally. The multipennate acromial part of deltoid is a strong abductor: aided by supraspinatus it abducts the arm until the joint capsule is tense below. Movement takes place in the plane of the body of the scapula, which is the only way that scapular rotation can be fully effective in raising the arm above the head. In true abduction (Fig. 46.19), acromial fibres contract strongly, while clavicular and posterior fibres prevent departure from the plane of motion. In the early stages of abduction, traction by the deltoid is upward, but the humeral head is prevented from translating upward by the synergistic downward pull of subscapularis, infraspinatus and teres minor. Electromyography suggests that deltoid contributes little to medial or lateral rotation but confirms that it takes part in most other shoulder movements. It may also aid supraspinatus in resisting the downward drag of a loaded arm. A common action of the deltoid is arm-swinging while walking.
Levator scapulae
Levator scapulae is a slender muscle attached by tendinous slips to the transverse processes of the atlas and axis, and to the posterior tubercles of the transverse processes of the third and fourth cervical vertebrae (Fig. 28.6, see below Fig. 46.21). It descends diagonally to approach the medial scapular border between its superior angle and the triangular smooth surface at the medial end of the scapular spine.
Levator scapulae varies considerably in its vertebral attachments and the extent to which it separates into slips. There may be accessory attachments to the mastoid process, occipital bone, first or second rib, scaleni, trapezius, and serratus muscles.
Levator scapulae receives its arterial supply mainly from the transverse cervical and ascending cervical arteries. The vertebral extremity of the muscle is supplied by branches from the vertebral artery.
Levator scapulae is innervated directly by branches of the third and fourth cervical spinal nerves, and from the fifth cervical nerve via the dorsal scapular nerve.
The levator scapulae and the rhomboids assist other scapular muscles in controlling the position and movement of the scapula. Acting with trapezius, rhomboids retract the scapula, bracing back the shoulder; with levator scapulae and pectoralis minor they rotate the scapula, depressing the point of the shoulder. With the cervical vertebral column fixed, levator scapulae acts with trapezius to elevate the scapula or to sustain a weight carried on the shoulder; with the shoulder fixed, the muscle inclines the neck to the same side.
Rhomboid major
Rhomboid major is a quadrilateral sheet of muscle which arises by tendinous fibres from the spines and supraspinous ligaments of the second to fifth thoracic vertebrae, and descends laterally to the medial border of the scapula between the root of the spine and the inferior angle (Fig. 46.21). Most of its fibres usually end in a tendinous band between these two points, joined to the medial border by a thin membrane. Occasionally this is incomplete, in which case some muscular fibres are attached directly into the scapula. The attachments of rhomboid major – and also those of rhomboid minor, levator scapulae and serratus anterior – can be more extensive, with ‘folds’ or extensions passing to both dorsal and costal aspects of the scapula adjacent to its medial margin.
Rhomboid minor
Rhomboid minor is a small, cylindrical muscle. It runs from the lower ligamentum nuchae and the spines of the seventh cervical and first thoracic vertebrae to the base of a smooth triangular surface at the medial end of the spine of the scapula, where dorsal and ventral layers enclose the inferior border of levator scapulae (Fig. 46.21). The dorsal layer of rhomboid minor is attached to the rim of the triangular surface, dorsolateral to and below levator scapulae. The ventral layer is strong and wide, extending 2–3 cm medial to and below levator scapulae; here the fasciae of rhomboid minor and serratus anterior are tightly fused. Rhomboid minor is usually separate from rhomboid major, but the muscles overlap and are occasionally united.
There is some variability in the vertebral and scapular attachments of rhomboids major and minor. A slip of muscle may extend from the upper border of rhomboid minor to reach the occipital bone (rhomboid occipitalis).
Vascular supply of the rhomboids
Rhomboids major and minor are supplied by the dorsal scapular artery or deep branch of the transverse cervical artery and by dorsal perforating branches from the upper five or six posterior intercostal arteries.
Latissimus dorsi
Latissimus dorsi is a large, flat, triangular muscle that sweeps over the lumbar region and lower thorax and converges to a narrow tendon (Fig. 46.22, Fig. 54.15). It arises by tendinous fibres from the spines of the lower six thoracic vertebrae anterior to trapezius; from the posterior layer of thoracolumbar fascia, by which it is attached to the spines and supraspinous ligaments of the lumbar and sacral vertebrae; and from the posterior part of the iliac crest. It also springs by muscular fibres from the posterior part (outer lip) of the iliac crest lateral to erector spinae, and by fleshy slips from the three or four lower ribs, interdigitating with external oblique (Fig. 61.9). From this extensive attachment, fibres pass laterally with different degrees of obliquity (the upper fibres are nearly horizontal, the middle oblique, and the lower almost vertical) to form a sheet approximately 12 or 13 mm thick that overlaps the inferior scapular angle. The muscle curves around the inferolateral border of teres major to gain its anterior surface. Here it ends as a flattened tendon, approximately 7 cm long, in front of the tendon of teres major. It is attached to the floor of the intertubercular sulcus of the humerus, with an expansion to the deep fascia. The attachment extends higher on the humerus than that of teres major. As the muscle curves round teres major, the fasciculi rotate around each other, so that fibres that originate lowest at the midline insert highest on the humerus, and fibres that originate highest at the midline insert lowest on the humerus. A bursa sometimes occurs between the muscle and the inferior scapular angle. The tendons of latissimus dorsi and teres major are united at their lower borders: they are separated by a bursa near their humeral attachments.
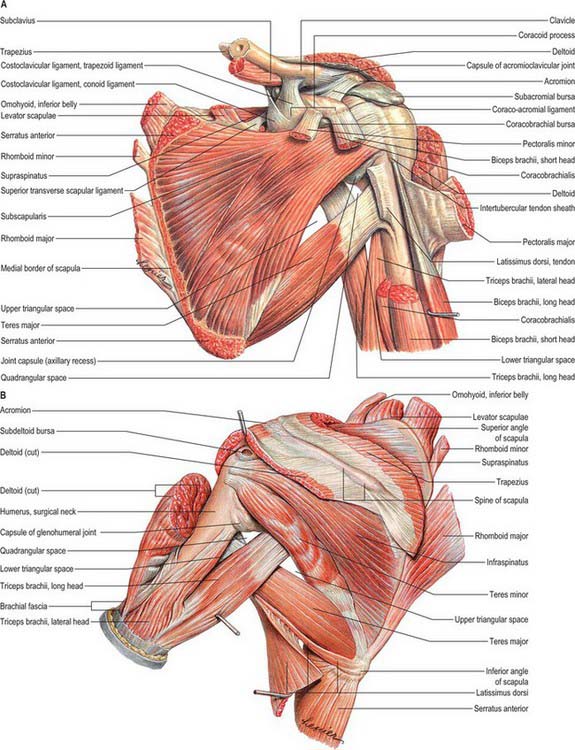
Fig. 46.22 Deep muscles of the left shoulder girdle. A, Anterior aspect after removal of several superficial muscles. B, Posterior aspect.
(From Sobotta 2006.)
Latissimus dorsi and teres major together form the posterior axillary fold. When the arm is adducted against resistance, this fold is accentuated, and the whole inferolateral border of latissimus dorsi can then be traced to its attachment to the iliac crest.
The lower, lateral margin of the muscle is usually separated from the posterior border of external oblique by the lumbar triangle; the base of this small triangle is the iliac crest and its floor the internal oblique. It should not be confused with the triangle of auscultation, which is medial to the scapula, and is bounded above by the trapezius, below by latissimus dorsi and laterally by the medial border of the scapula; part of rhomboid major is exposed in the triangle. If the scapulae are drawn forwards, by folding the arms across the chest, and the trunk is bent forwards, parts of the sixth and seventh ribs and the interspace between them (overlying the apex of the lower pulmonary lobe) become subcutaneous.
Latissimus dorsi commonly receives some additional fibres from the scapula as it crosses the inferior scapular angle. A muscular axillary arch, 7–10 cm in length and 5–15 mm in breadth, may sometimes be present: it crosses from the edge of latissimus dorsi, midway in the posterior fold, over the front of the axillary vessels and nerves to join the tendons of pectoralis major, coracobrachialis or the fascia over the biceps. The vertebral and costal attachments of latissimus dorsi may be reduced or, in rare cases, increased. A fibrous slip usually passes from the tendon, near its humeral insertion, to the long head of triceps.
Latissimus dorsi is supplied by a single dominant vascular pedicle, the thoracodorsal artery, itself a continuation of the subscapular artery (p. 817). The thoracodorsal artery (and its accompanying venae comitantes) enters the muscle at a single neurovascular hilum on its costal surface, 6–12 cm from the subscapular artery and 1–4 cm medial to the lateral border of the muscle. The artery gives off one to three large branches to serratus anterior before dividing at, or even before, the hilum to supply latissimus dorsi itself. The basic pattern of branching is a bifurcation into lateral and medial branches. The larger lateral branch follows a course parallel to, and 1–4 cm from, the upper border of the muscle; the smaller branch diverges at an angle of 45° and travels medially. In a small number of cases the artery trifurcates: this usually yields a small recurrent branch which returns to supply the proximal part of the muscle, but in some cases it provides a third major branch which supplies the distal part of the muscle. Occasionally the lateral branch gives off a further collateral to serratus anterior. The major branches give off 5–9 longitudinal branches which travel distally, parallel with the muscle fibres. Musculocutaneous perforators arising from these vessels supply the overlying skin.
In addition to the dominant vascular pedicle, latissimus dorsi is supplied inferiorly by several smaller secondary segmental vascular pedicles. These are dorsal perforating arteries derived from the 9th, 10th and 11th posterior intercostal and 1st, 2nd and 3rd lumbar arteries, and they all enter the muscle on its deep surface. They anastomose within the muscle with branches of the thoracodorsal artery.
The blood supply of latissimus dorsi is particularly important because of its applications in plastic and reconstructive surgery. The presence of the dominant vascular pedicle provides the anatomical basis for raising the muscle either alone, or together with an overlying paddle of skin in the form of a musculocutaneous flap based solely on the thoracodorsal artery and its accompanying venae comitantes. These flaps can be used in a pedicle fashion, e.g. in reconstructing a breast following a mastectomy, or used as free tissue transfer to cover large areas of tissue loss anywhere in the body.
Latissimus dorsi is supplied by the thoracodorsal nerve, from the posterior cord of the brachial plexus, C6, 7 and 8. This nerve runs in the neurovascular pedicle and divides approximately 1.3 cm proximal to the point of bifurcation or trifurcation of the thoracodorsal artery. The pattern of branching follows that of the artery closely, and the neural and vascular branches travel together.
Latissimus dorsi is active in adduction, extension and especially in medial rotation of the humerus. Humeral adduction and extension are most powerful when the initial position of the arm is one of partial abduction, flexion or a combination of the two. With the sternocostal part of pectoralis major and teres major it adducts the raised arm against resistance. It assists backward swinging of the arm, as in walking and many athletic pursuits. When the arms are raised above the head, as in climbing, it pulls the trunk upwards and forwards. It takes part in all violent expiratory efforts, such as coughing or sneezing: this is readily confirmed by palpation. Electromyography suggests that it aids deep inspiration, but it is also active towards the end of forcible expiration, e.g. when blowing a sustained note on a musical instrument. When the arm is elevated, the stretched fibres of latissimus dorsi press on the inferior scapular angle, keeping it in contact with the chest wall. Despite this range of actions, surgical transposition of the muscle does not produce any serious restriction of normal activity.
Serratus anterior
Serratus anterior is a large muscular sheet which curves around the thorax. It arises from an extensive costal attachment and inserts on the scapula (Fig. 46.19, Fig. 46.20). Fleshy digitations spring anteriorly from the outer surfaces and superior borders of the upper eight, nine or even ten ribs, and from fasciae which cover the intervening intercostals. They lie on a long, slightly curved, line which passes inferolaterally across the thorax. The first digitations spring from the first and second ribs and intercostal fascia, the others from a single rib, and the lower four interdigitate with the upper five slips of external oblique. The muscle follows the contour of the chest wall closely. It passes ventral to the scapula and reaches the medial border of the scapula in the following way. The first digitation encloses, and is attached to, a triangular area of both the costal and dorsal surfaces of the superior scapular angle. The next two or three digitations form a triangular sheet which is attached to the costal surface along almost its entire medial border. The lower four or five digitations converge to be attached by musculotendinous fibres to a triangular impression on the costal surface of the inferior angle: they enclose the inferior angle and are also attached to a smaller triangular part of its dorsal surface near its tip.
Digitations may be absent, particularly the first and eighth, and sometimes also the intermediate part. Serratus anterior may be partly fused with levator scapulae, adjacent external intercostals or external oblique.
Serratus anterior is supplied by superior and lateral thoracic arteries, and branches from the thoracodorsal artery before (occasionally after) it divides in latissimus dorsi.
Serratus anterior is innervated by the long thoracic nerve, C5, 6 and 7, which descends on the external surface of the muscle.
With pectoralis minor, serratus anterior protracts (draws forward) the scapula, as a prime mover in all reaching and pushing movements. The upper part, with levator scapulae and upper fibres of trapezius, suspends the scapula, but slight activity is sufficient to support the unloaded arm. The heavier insertion lower down pulls the inferior scapular angle forwards around the thorax, assisting trapezius in upward rotation of the bone, an action that is essential to raising the arm above the head. In the initial stages of abduction, serratus anterior helps other muscles to fix the scapula, so that deltoid acts effectively on the humerus, and not the scapula. While deltoid is raising the arm to a right angle with the scapula, serratus anterior and trapezius are simultaneously rotating the scapula: the combination allows the arm to be raised to the vertical. To effect this upward rotation of the scapula, forward pull on the inferior angle by the lower digitations of serratus anterior is coupled with an upward and medial pull on the lateral end of the clavicle and acromion by the upper fibres of trapezius, and a downward pull on the base of the scapular spine by the lower fibres of trapezius. Conversely, slow downward scapular rotation assisted by gravity is achieved by controlled lengthening of these muscles. More powerful downward rotation requires balanced contraction of the upper fibres of serratus anterior, levator scapulae, rhomboids, pectoralis minor and the middle part of trapezius. When weights are carried in front of the body, serratus anterior prevents backward rotation of the scapula. Electromyography shows that serratus anterior is not active in normal human respiration. This may not apply to laboured respiration, e.g. when asthmatics and athletes may be observed to fix the scapula by grasping a rail or other support.
The muscular digitations of serratus anterior can be seen and felt when the outstretched hand pushes against resistance.
When serratus anterior is paralysed, the medial border of the scapula, and especially its lower angle, stand out prominently. The arm cannot be raised fully. Pushing is ineffective, indeed attempts to do so produce further projection, known as ‘winging’ of the scapula.
Supraspinatus
Supraspinatus arises from the medial two-thirds of the supraspinous fossa and from the supraspinous fascia (Fig. 46.22). The fibres converge, under the acromion, into a tendon which crosses above the shoulder joint and is attached to the highest facet of the greater tubercle of the humerus. The tendon blends into the articular capsule and may give a slip to the tendon of pectoralis major. Fibrocartilage has been described at the tendinous insertion, as in other tendons attached to epiphysial bone.
The conventional view is that supraspinatus initiates abduction of the shoulder and assists deltoid in abduction thereafter. However, there is evidence that both supraspinatus and deltoid are involved throughout the range of abduction, including initiation of the movement. As part of the rotator cuff, supraspinatus helps to stabilize the head of the humerus in the glenoid fossa during movements of the glenohumeral joint. With the arm dependent, even when moderately loaded, supraspinatus and tension in the upper capsule prevent downward displacement of the humerus.
Supraspinatus can be palpated deep to trapezius when the arm is abducted at the shoulder joint against resistance.
The tendon of supraspinatus is separated from the coraco-acromial ligament, acromion and deltoid by the large subacromial bursa; when this is inflamed, abduction of the shoulder joint is painful. The tendon is the most frequently torn element of the musculotendinous cuff around the shoulder joint.
Infraspinatus
Infraspinatus is a thick triangular muscle which occupies most of the infraspinous fossa (Fig. 46.22). It arises by muscular fibres from the medial two-thirds of the fossa, by tendinous fibres from ridges on its surface and from the deep surface of the infraspinous fascia, which separates it from teres major and minor. Its fibres converge to a tendon which glides under the lateral border of the spine of the scapula, and then passes across the posterior aspect of the capsule of the shoulder joint to be attached to the middle facet on the greater tubercle of the humerus. The tendon is sometimes separated from the capsule by a bursa, which may communicate with the joint cavity. Infraspinatus is sometimes fused with teres minor.
Infraspinatus is a lateral rotator of the humerus. Together with supraspinatus, subscapularis and teres minor, it helps to stabilize the head of the humerus in the glenoid fossa during shoulder movements (p. 806).
Subscapularis
Subscapularis is a bulky, triangular muscle which fills the subscapular fossa (Fig. 46.20). In its medial two-thirds, the fibres are attached to the periosteum of the costal surface of the scapula. Other fibres arise from tendinous intramuscular septa, which are attached to ridges on the bone, and from the aponeurosis which covers the muscle and separates it from teres major and the long head of triceps. The fibres converge laterally into a broad tendon which is attached to the lesser tubercle of the humerus and the front of the articular capsule. The tendon is separated from the neck of the scapula by the large subscapular bursa, which communicates with the shoulder joint.
Variation is unusual. A separate slip may pass from the medial border of the scapula to the glenohumeral capsule or to the periosteum medial to the intertuberculous sulcus of the humerus.
Subscapularis forms much of the posterior axillary wall. Its anterior surface is apposed inferomedially to serratus anterior, and superolaterally to coracobrachialis and biceps, the axillary vessels, brachial plexus and subscapular vessels and nerves. Its posterior surface is attached to the scapula and glenohumeral capsule. Its lower border contacts teres major and latissimus dorsi.
Subscapularis is supplied by small branches from the suprascapular, axillary and subscapular arteries.
Subscapularis is a medial rotator of the humerus. Together with supraspinatus, infraspinatus and teres minor, it helps to stabilize the head of the humerus in the glenoid fossa during shoulder movements (p. 806).
Teres major
Teres major is a thick, flat muscle which arises from the oval area on the dorsal surface of the inferior scapular angle, and from the fibrous septa interposed between the muscle and teres minor and infraspinatus (Fig. 46.22). Its fibres ascend laterally and end in a flat tendon, approximately 5 cm long, which is attached to the medial lip of the intertubercular sulcus of the humerus. The tendon lies behind that of latissimus dorsi, from which it is separated by a bursa; the tendons are united along their lower borders for a short distance.
Teres major may be fused with the scapular part of latissimus dorsi, and it may send a slip to join the long head of triceps or the brachial fascia.
Teres major is supplied by the thoracodorsal branch of the subscapular artery on its way to latissimus dorsi and by the posterior circumflex humeral artery.
Despite its name, teres major has a nerve supply and action that is distinct from teres minor. Teres major draws the humerus backwards and rotates it medially. Electromyographic studies are equivocal about its major role in movement, but its involvement as a contributor to static posture and arm-swinging is not contested.
Teres minor
Teres minor is a narrow elongated muscle which arises from the upper two-thirds of a flattened strip on the dorsal surface of the scapula adjoining its lateral border, and from two aponeurotic laminae which separate it from infraspinatus and teres major (Fig. 46.22). It runs upwards and laterally. The upper fibres end in a tendon attached to the lowest facet on the greater tubercle of the humerus. The lower fibres are attached directly into the humerus distal to this facet and above the origin of the lateral head of triceps. The tendon passes across, and blends with, the lower posterior surface of the capsule of the shoulder joint.
Teres minor is supplied by the circumflex scapular artery, which pierces the origin of the muscle as it turns upward in the infraspinous fossa, and by the posterior circumflex humeral artery.
Teres minor acts as a lateral rotator and weak adductor of the humerus. Together with supraspinatus, infraspinatus and subscapularis, it helps stabilize the head of the humerus in the glenoid fossa during shoulder movements (p. 803).
The quadrangular and triangular spaces
Anteriorly, the quadrangular space is bounded by subscapularis, the capsule of the shoulder joint and teres minor above, teres major below, the long head of triceps medially, and the surgical neck of the humerus laterally. Posteriorly, the quadrangular space is bounded above by teres minor. The axillary nerve and the posterior circumflex artery and vein pass through the space (Fig. 46.22).
There are two triangular spaces (Fig. 46.22). The upper triangular space is bounded above by subscapularis anteriorly, teres minor posteriorly, teres major below, and the long head of triceps laterally. The circumflex scapular artery passes through this space. The lower triangular space (triangular interval) is bounded above by subscapularis anteriorly and teres major posteriorly; the long head of triceps medially and the humerus laterally. The radial nerve and the profunda brachii vessels pass through this space.
AXILLA
BOUNDARIES
The axilla is a pyramidal region between the upper thoracic wall and the arm (Fig. 46.23, Fig. 46.24). Its blunt apex continues into the root of the neck (cervico-axillary canal) between the external border of the first rib, superior border of the scapula, posterior surface of the clavicle and the medial aspect of the coracoid process. Its base, which is virtual, can be imagined as facing downwards: it is broad at the chest and narrow at the arm, and corresponds to the skin and a thick layer of axillary fascia between the inferior borders of pectoralis major anteriorly and latissimus dorsi posteriorly. It is convex upwards, conforming to the concavity of the armpit.
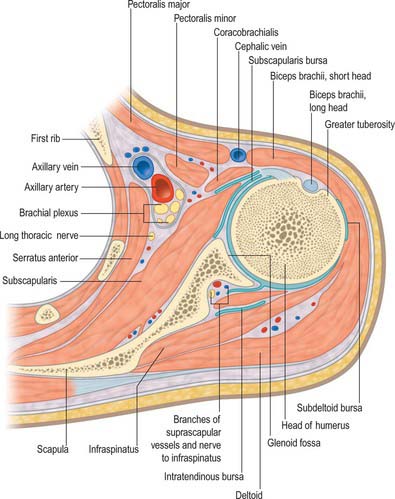
Fig. 46.23 Transverse section through left shoulder joint and axilla, viewed from below. Compare with Fig. 46.17A.
The anterior wall is formed by pectorales major and minor, the former covering the whole wall, the latter its intermediate part. The interval between the upper border of pectoralis minor and clavicle is occupied by the clavipectoral fascia. The posterior wall is formed by subscapularis above, and teres major and latissimus dorsi below. The medial ‘wall’ is convex laterally and is composed of the first four ribs and their associated intercostal muscles, together with the upper part of serratus anterior. The anterior and posterior walls converge laterally: the ‘wall’ is narrow and consists of the humeral intertubercular sulcus. The lateral angle lodges coracobrachialis and biceps.
CONTENTS
The axilla contains the axillary vessels, the infraclavicular part of the brachial plexus and its branches, lateral branches of some intercostal nerves, many lymph nodes and vessels, loose adipose areolar tissue and, in many instances, the ‘axillary tail’ of the breast. The axillary vessels and brachial plexus run from the apex to the base along the lateral wall, nearer to the anterior wall: the axillary vein is anteromedial to the artery. The obliquity of the upper ribs means that the neurovascular bundle, after it emerges from behind the clavicle, crosses the first intercostal space: its relations are therefore different at upper and lower levels. Thoracic branches of the axillary artery are in contact with the pectoral muscles; the lateral thoracic artery reaches the thoracic wall along the lateral margin of pectoralis minor. Subscapular vessels descend on the posterior wall at the lower margin of subscapularis. The subscapular and thoracodorsal nerves cross the anterior surface of latissimus dorsi at different inclinations. Circumflex scapular vessels wind round the lateral border of the scapula; posterior circumflex humeral vessels and the axillary nerve curve back and laterally around the surgical neck of the humerus.
No large vessel lies on the medial ‘wall’, which is crossed proximally only by small branches of the superior thoracic artery. The long thoracic nerve descends on serratus anterior and the intercostobrachial nerve perforates the upper anterior part of this wall, crossing the axilla to its lateral ‘wall’.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
ARTERIES
Suprascapular artery
The suprascapular artery usually arises from the thyrocervical trunk of the subclavian artery, although it may arise from the third part of the subclavian artery (Fig. 28.7). It first descends laterally across scalenus anterior and the phrenic nerve, posterior to the internal jugular vein and sternocleidomastoid, then crosses anterior to the subclavian artery and brachial plexus, posterior and parallel with the clavicle and subclavius and the inferior belly of omohyoid, to reach the superior border of the scapula. Here it passes above (sometimes under) the superior transverse ligament, separating it from the suprascapular nerve, and enters the supraspinous fossa (Fig. 46.25), where it lies on the bone, and supplies supraspinatus. It descends behind the scapular neck, and passes through the spinoglenoid notch deep to the inferior transverse ligament to gain the deep surface of infraspinatus, where it anastomoses with the circumflex scapular and deep branch of the transverse cervical artery. Its muscular branches supply sternocleidomastoid, subclavius and infraspinatus. It also gives off a suprasternal branch which crosses the sternal end of the clavicle to supply the skin of the upper thorax, and an acromial branch which pierces trapezius to supply the skin over the shoulder. This last branch anastomoses with the thoraco-acromial and posterior circumflex humeral arteries.
As the suprascapular artery passes over the superior transverse ligament, it gives off a branch which enters the subscapular fossa beneath subscapularis and anastomoses with the subscapular artery and the deep branch of the transverse cervical artery. It also supplies the acromioclavicular and glenohumeral joints, the clavicle and the scapula.
Dorsal scapular artery
In the majority of cases, the dorsal scapular artery arises from the third, or less often the second, part of the subclavian artery. It passes laterally through the trunks of the brachial plexus in front of scalenus medius and then deep to levator scapulae to reach the superior scapular angle. Here it descends with the dorsal scapular nerve under the rhomboids along the medial border of the scapula to the inferior angle (Fig. 46.25). It supplies the rhomboids, latissimus dorsi and the inferior portion of trapezius. It supplies the skin over the inferomedial aspect of trapezius via musculocutaneous perforators. It anastomoses with the suprascapular and subscapular and with posterior branches of some posterior intercostal arteries. It sends a small branch to scalenus anterior: sometimes this arises directly from the subclavian artery.
About a third of the superficial cervical and dorsal scapular arteries arise in common from the thyrocervical trunk as a transverse cervical artery, together with a superficial and a deep branch (superficial cervical and dorsal scapular arteries respectively). In this case the dorsal scapular artery arises near the superior border of the scapula: it passes laterally, anterior to the brachial plexus and then posterior to levator scapulae (Fig. 46.26).
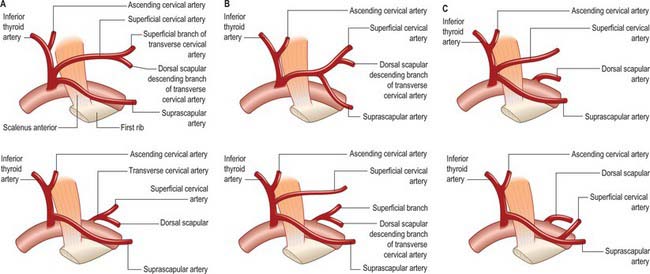
Fig. 46.26 A–F, Variations in origin and branches of the thyrocervical trunk. The superficial cervical artery is the distinct vessel arising from the thyrocervical trunk (C and E) or from the suprascapular artery (D), which supplies the territory of the superficial branch of the (absent) transverse cervical artery.
(By permission from Cormack GC, Lamberty BGH 1994 The Arterial Anatomy of Skin Flaps, 2nd edn. Edinburgh: Churchill Livingstone.)
Supraclavicular artery
This small vessel arises from either the transverse cervical or superficial cervical artery. It pierces the deep fascia just superior to the clavicle and anterior to trapezius and supplies an area of skin over the lateral end of the clavicle.
Axillary artery
The axillary artery, a continuation of the subclavian artery, begins at the outer border of the first rib, and ends nominally at the inferior border of teres major where it becomes the brachial artery. Its direction varies with the position of the limb: it is almost straight when the arm is raised at right angles, concave upwards when the arm is elevated above this, and convex upwards and laterally when the arm is by the side. At first deep, it subsequently becomes superficial, when it is covered only by the skin and fasciae. Pectoralis minor crosses it and so divides it into three parts which are proximal, posterior and distal to the muscle.
Relations of the first part
The skin, superficial fascia, platysma, supraclavicular nerves, deep fascia, clavicular fibres of pectoralis major and the clavipectoral fascia, lateral pectoral nerve and the loop of communication between the lateral and medial pectoral nerves, and the thoraco-acromial and cephalic veins are all anterior. The first intercostal space and external intercostal, first and second digitations of serratus anterior, long thoracic and medial pectoral nerves and the medial cord of the brachial plexus are all posterior. The posterior cord of the brachial plexus is lateral and the axillary vein is anteromedial. The first part is enclosed with the axillary vein and brachial plexus in a fibrous axillary sheath, which is continuous with the prevertebral layer of the deep cervical fascia.
Relations of the second part
The skin, superficial and deep fascia, and pectorales major and minor are all anterior. The posterior cord of the brachial plexus and the areolar tissue between it and subscapularis are posterior. The axillary vein is medial, separated from the artery by the medial cord of the brachial plexus and the medial pectoral nerve. The lateral cord of the brachial plexus is lateral, separating the artery from coracobrachialis. The cords of the brachial plexus thus surround the second part on three sides, with the dispositions implied by their names, and separate it from the vein and adjacent muscles.
Relations of the third part
Pectoralis major, and, distal to the muscle, skin and fasciae, are anterior. The lower part of subscapularis and the tendons of latissimus dorsi and teres major are posterior. Coracobrachialis is lateral and the axillary vein is medial. Branches of the brachial plexus are arranged as follows: laterally, the lateral root and then trunk of the median nerve and, for a short distance, the musculocutaneous nerve; medially, the medial cutaneous nerve of the forearm between the axillary artery and vein anteriorly, and the ulnar nerve between these vessels posteriorly; anteriorly, the medial root of the median nerve; posteriorly, the radial and axillary nerves, the latter only to the distal border of subscapularis.
Branches
The branches of the axillary artery are superior thoracic, thoracoacromial, lateral thoracic, subscapular, anterior and posterior circumflex humeral.
Superior thoracic artery
The superior thoracic artery is a small vessel which arises from the first part of the axillary artery near the lower border of subclavius: it sometimes arises from the thoraco-acromial artery (Fig. 46.24). It runs anteromedially above the medial border of pectoralis minor, then passes between it and pectoralis major to gain the thoracic wall. It supplies these muscles and the thoracic wall, and anastomoses with the internal thoracic and upper intercostal arteries.
Thoraco-acromial (acromio-thoracic) artery
The thoraco-acromial artery is a short branch which arises from the second part of the axillary artery (Fig. 28.7, Fig. 46.19). It is at first overlapped by pectoralis minor; skirting its medial border, next pierces the clavipectoral fascia and divides into pectoral, acromial, clavicular and deltoid branches, which supply pectoralis major and minor, an area of skin over the clavipectoral fascia and the anterior portion of deltoid.
The pectoral branch is the largest branch. It descends between the pectoral muscles, gives a branch to pectoralis minor, and then continues on the deep surface of pectoralis major. It enters the muscle and anastomoses with the intercostal branches of the internal thoracic and lateral thoracic arteries. It gives off perforating branches to the breast, and musculocutaneous perforators to the skin over pectoralis major.
The acromial branch crosses the coracoid process under deltoid, which it supplies, pierces the muscle and ends on the acromion. It anastomoses with branches of the suprascapular artery, the deltoid branch of the thoraco-acromial artery and the posterior circumflex humeral arteries.
Lateral thoracic artery
The lateral thoracic artery arises from the second part of the axillary artery. Following the lateral border of pectoralis minor, it passes to the deep surface of pectoralis major as far distally as the fifth intercostal space. It supplies serratus anterior and the pectoral muscles, the axillary lymph nodes and subscapularis. It anastomoses with the internal thoracic, subscapular, and intercostal arteries and with the pectoral branch of the thoraco-acromial artery. In females it is large and has lateral mammary branches, which curve round the lateral border of pectoralis major to the breast. In both males and females, it gives off cutaneous branches which pass around the lateral border of pectoralis major to supply the skin in this region.
Subscapular artery
The subscapular artery is the largest branch of the axillary artery (Fig. 46.24, Fig. 46.25). It usually arises from the third part of the axillary artery at the distal (inferior) border of subscapularis, which it follows to the inferior scapular angle, where it anastomoses with the lateral thoracic and intercostal arteries and the deep branch of the transverse cervical artery. It supplies adjacent muscles and the thoracic wall. It is accompanied distally by the nerve to latissimus dorsi. Approximately 4 cm from its origin the subscapular artery divides into the circumflex scapular and thoracodorsal arteries.
Circumflex scapular artery
The circumflex scapular artery, the larger of the two terminal branches of the subscapular artery, curves backwards around the lateral border of the scapula, traversing a triangular space between subscapularis above and teres major below and the long head of the triceps laterally. It enters the infraspinous fossa under teres minor and then divides. One branch (infrascapular) enters the subscapular fossa deep to subscapularis, and anastomoses with the suprascapular and dorsal scapular arteries (or deep branch of the transverse cervical artery). The other branch continues along the lateral border of the scapula between teres major and minor and, dorsal to the inferior angle, anastomoses with the dorsal scapular artery. Small branches supply the posterior part of deltoid and the long head of triceps, and anastomose with an ascending branch of the profunda brachii artery.
Two significant cutaneous branches arise from the circumflex scapular artery as it emerges through the upper triangular space. The superior, or horizontal, branch is a direct cutaneous artery which passes medially at the level of the deep fascia parallel with the spine of the scapula: it supplies a band of skin overlying the spine of the scapula. The lower branch (parascapular branch) is also a direct cutaneous vessel which passes in an inferomedial direction, again at the level of the deep fascia, and supplies an area of skin overlying the lateral border of the scapula. Both these cutaneous vessels provide the anatomical basis of skin flaps which can be surgically raised in this region (scapular flap based on the horizontal branch and parascapular flap based on the lower, parascapular branch) to reconstruct areas of missing tissue elsewhere in the body.
Thoracodorsal artery
The other terminal branch of the subscapular artery, the thoracodorsal artery, follows the lateral margin of the scapula, posterior to the lateral thoracic artery, between latissimus dorsi and serratus anterior. Before entering the deep surface of latissimus dorsi, it supplies teres major and the intercostals and sends one or two branches to serratus anterior. It enters latissimus dorsi muscle with the thoracodorsal nerve: this constitutes the principle neurovascular pedicle to the muscle. It provides numerous musculocutaneous perforators which supply the skin over the superior part of latissimus dorsi. The intramuscular portion of the artery anastomoses with intercostal arteries and lumbar perforating arteries.
Anterior circumflex humeral artery
The anterior circumflex humeral artery arises from the lateral side of the axillary artery at the distal border of subscapularis. It runs horizontally behind coracobrachialis and the short head of biceps, anterior to the surgical neck of the humerus. Reaching the intertubercular sulcus, it sends an ascending branch to supply the humeral head and shoulder joint. It continues laterally under the long head of biceps and deltoid, and anastomoses with the posterior circumflex humeral artery.
Posterior circumflex humeral artery
The posterior circumflex humeral artery is larger than the anterior (Fig. 46.25, Fig. 46.27). It branches from the third part of the axillary artery at the distal border of subscapularis and runs backwards with the axillary nerve through a quadrangular space which is bounded by subscapularis, the capsule of the shoulder joint and teres minor above, teres major below, the long head of triceps medially, and the surgical neck of the humerus laterally. It curves round the humeral neck and supplies the shoulder joint, deltoid, teres major and minor, and long and lateral heads of triceps. It gives off a descending branch which anastomoses with the deltoid branch of the profunda brachii artery and with the anterior circumflex humeral and acromial branches of the suprascapular and thoraco-acromial arteries.
Variants
Branches exhibit considerable variation. An alar thoracic artery, often from the second part, may supply fat and lymph nodes in the axilla. The lateral thoracic artery may be absent, in which case it is replaced by lateral perforating branches of the intercostal arteries, alternatively, it may become, or give off, a direct cutaneous vessel (named the superficial thoracic artery by some sources) which supplies the skin over the lateral border of pectoralis major. In up to 30% of cases, the subscapular artery can arise from a common trunk with the posterior circumflex humeral artery. Occasionally the subscapular, circumflex humeral and profunda brachii arteries arise in common, in which case, branches of the brachial plexus surround this common vessel instead of the axillary artery. The posterior circumflex humeral artery may arise from the profunda brachii artery, and pass back below teres major instead of passing through the quadrangular space. Sometimes the axillary divides into radial and ulnar arteries (anomalous ‘high division’), and is occasionally the source of the anterior interosseous artery.
VEINS
Axillary vein
The axillary vein is the continuation of the basilic vein. It begins at the lower border of teres major, and ascends to the outer border of the first rib, where it becomes the subclavian vein. It is joined by the brachial vein near subscapularis, and by the cephalic vein near its costal end; other tributaries follow the axillary arterial branches. It lies medial to the axillary artery, which it partly overlaps. The medial pectoral nerve, medial cord of the brachial plexus, ulnar nerve and medial cutaneous nerve of the forearm lie between the artery and the vein. The medial cutaneous nerve of the arm is medial to the vein; the lateral group of axillary lymph nodes is posteromedial. There are a pair of valves near its distal end, and valves also occur near the ends of the cephalic and subscapular veins.
Subclavian vein
The subclavian vein is a continuation of the axillary vein. It extends from the outer border of the first rib to the medial border of scalenus anterior, where it joins the internal jugular to form the brachiocephalic vein. The clavicle and subclavius are anterior, the subclavian artery is posterosuperior, separated by scalenus anterior and the phrenic nerve, and the first rib and pleura are inferior. The vein usually has a pair of valves about 2cm from its end. Its tributaries are the external jugular, dorsal scapular and (sometimes) anterior jugular veins, and occasionally a small branch from the cephalic vein which ascends anterior to the clavicle. At its junction with the internal jugular vein, the left subclavian receives the thoracic duct: the right subclavian vein receives the right lymphatic duct.
AXILLARY LYMPH NODES
There are between 20 to 30 axillary nodes, which may be divided into five not wholly distinct groups, namely, lateral, anterior (pectoral), posterior (subscapular), central and apical (Fig. 54.21, Fig. 45.6, Fig. 46.28). Four of the groups are intermediary, and only the apical group is terminal. Collectively they drain the entire upper limb, breast and trunk above the umbilicus.
The lateral group of four to six nodes is posteromedial to the axillary vein, its afferents drain the whole limb except the vessels accompanying the cephalic vein (Fig. 54.21, Fig. 45.6, Fig. 46.28). Efferent vessels pass partly to the central and apical axillary groups, and partly to the inferior deep cervical nodes. The anterior group of four or five nodes spreads along the inferior border of pectoralis minor near the lateral thoracic vessels. Their afferents drain the skin and muscles of the supraumbilical anterolateral body wall and breast, and efferents pass partly to the central and partly to the apical axillary nodes. The posterior group of six or seven nodes lie on the inferior margin of the posterior axillary wall, along the subscapular vessels. Their afferents drain the skin and superficial muscles of the inferior posterior region of the neck and the dorsal aspect of the trunk down to the iliac crest, and efferents pass to the apical and central axillary nodes. A central group of three or four large nodes embedded in axillary fat receives afferents from all preceding groups, and their efferents drain to the apical nodes. An apical group of six to twelve nodes is partly posterior to the superior part of pectoralis minor and partly above its superior border, extending to the apex of the axilla medial to the axillary vein. The only direct territorial afferents are those which accompany the cephalic vein or some which drain the upper peripheral region of the breast: the group drains all the other axillary nodes. Their efferents unite as the subclavian trunk and drain directly to the jugulosubclavian venous junction, or the subclavian vein, or jugular lymphatic trunk or (occasionally) to a right lymphatic duct; the left trunk usually ends in the thoracic duct. A few efferents from apical nodes usually reach the inferior deep cervical nodes.
One or two infraclavicular nodes appear beside the cephalic vein, in the groove between pectoralis major and deltoid, just inferior to the clavicle. Their efferents pass through the clavipectoral fascia to the apical axillary nodes. Occasionally some pass anterior to the clavicle to the inferior deep cervical (supraclavicular) nodes.
INNERVATION
BRACHIAL PLEXUS
For an overview of the brachial plexus see page 779 and Fig. 45.7.
In the axilla, the lateral and posterior cords of the brachial plexus are lateral to the first part of the axillary artery, and the medial cord is behind the artery. The cords surround the second part of the artery, their names indicating their relationship. In the lower axilla the cords divide into nerves that supply the upper limb (Fig. 46.29). Other than the medial root of the median nerve, these nerves are related to the third part of the artery in the same way as their cords are related to the second part, i.e. branches of the lateral cord are lateral to the artery, branches of the medial cord are medial, and branches of the posterior cord are posterior.
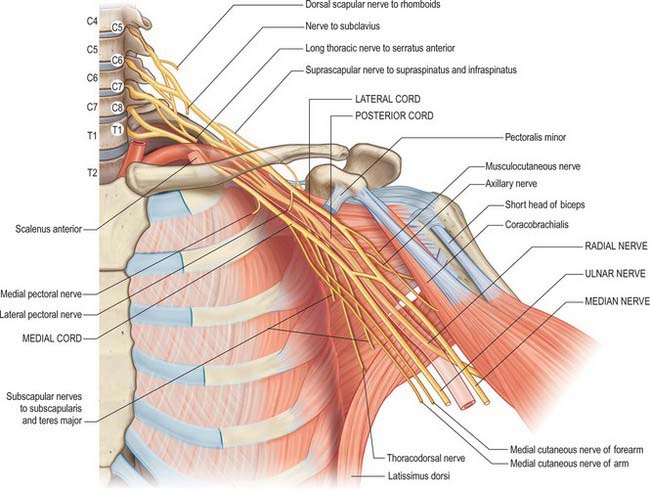
Fig. 46.29 The brachial plexus, its branches and the muscles which they supply. The axillary artery, shown in red outline, runs anterior to the radial nerve. The vertebral levels are labelled C4–T2. The nerve roots are labelled C5–T1 (white circles).
Branches of the brachial plexus may be described as supraclavicular and infraclavicular.
Supraclavicular branches
Supraclavicular branches arise from roots or from trunks as follows:
| From roots | 1. Nerves to scaleni and longus colli | C5, 6, 7, 8 |
| 2. Branch to phrenic nerve | C5 | |
| 3. Dorsal scapular nerve | C5 | |
| 4. Long thoracic nerve | C5, 6 (7) | |
| From trunks | 1. Nerve to subclavius | C5, 6 |
| 2. Suprascapular nerve | C5, 6 |
Branches to the scaleni and longus colli arise from the lower cervical ventral rami near their exit from the intervertebral foramina. The phrenic nerve is joined by a branch from the fifth cervical ramus anterior to scalenus anterior.
Dorsal scapular nerve
The dorsal scapular nerve comes from the fifth cervical ventral ramus, pierces scalenus medius, passes behind levator scapulae, which it occasionally supplies, and runs with the deep branch of the dorsal scapular artery to the rhomboids, which it supplies.
Long thoracic nerve
The long thoracic nerve is usually formed by roots from the fifth to the seventh cervical rami, although the last ramus may be absent (Fig. 46.30). The upper two roots pierce scalenus medius obliquely, uniting in or lateral to it. The nerve descends dorsal to the brachial plexus and the first part of the axillary artery and crosses the superior border of serratus anterior to reach its lateral surface. It may be joined by the root from C7, which emerges between scalenus anterior and scalenus medius, and descends on the lateral surface of medius. The nerve continues downwards to the lower border of serratus anterior, and supplies branches to each of its digitations.
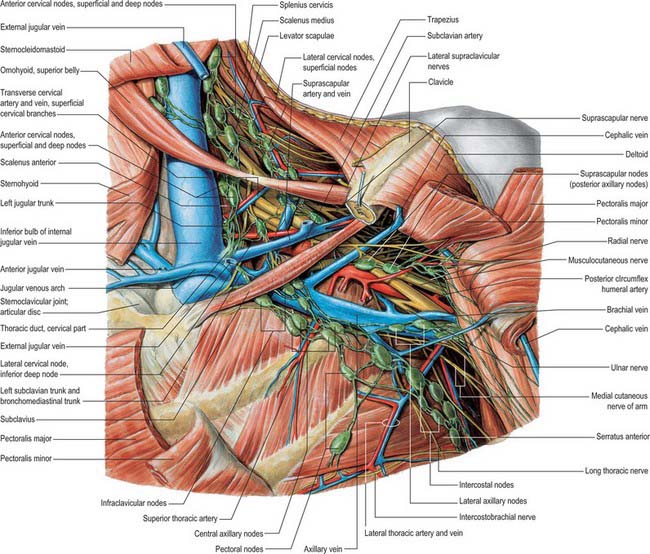
Fig. 46.30 Anterior aspect of left axillary fossa and deep aspect of thoracic inlet. The clavicle has been partially removed and the pectoral muscles have been reflected.
(From Sobotta 2006.)
The long thoracic nerve is the most common nerve to be affected by neuralgic amyotrophy. Winging of the scapula may be the only clinical manifestation: it is best demonstrated by asking the patient to push against resistance with the arm extended at the elbow and flexed to 90° at the shoulder.
Nerve to subclavius
The nerve to subclavius is small and arises near the junction of the fifth and sixth cervical ventral rami. It descends anterior to the plexus and the third part of the subclavian artery and is usually connected to the phrenic nerve. It passes above the subclavian vein to supply subclavius.
Suprascapular nerve
The suprascapular nerve is a large branch of the superior trunk (Fig. 28.17). It runs laterally, deep to trapezius and omohyoid and enters the supraspinous fossa through the suprascapular notch inferior to the superior transverse scapular ligament. It runs deep to supraspinatus, supplies it, and curves round the lateral border of the spine of the scapula with the suprascapular artery to reach the infraspinous fossa, where it gives two branches to infraspinatus and articular rami to the shoulder and acromioclavicular joints. The suprascapular nerve rarely has a cutaneous branch. When present, it pierces deltoid close to the tip of the acromion and supplies the skin of the proximal third of the arm within the territory of the axillary nerve.
Lesions of the suprascapular nerve
The commonest cause involving the suprascapular nerve is neuralgic amyotrophy. An entrapment neuropathy may occur in the scapular notch, often related to a degenerate cyst originating from the posterior glenoid labrum, or the nerve may be damaged by trauma to the scapula and shoulder. There is pain in the shoulder and wasting and weakness of supraspinatus and infraspinatus.
Infraclavicular branches
Infraclavicular branches come from the cords, but their axons may be traced back to the spinal nerves detailed in the box below.
| Lateral cord | Lateral pectoral | C5, 6, 7 |
| Musculocutaneous | C5, 6 7 | |
| Lateral root of median | C(5), 6, 7 | |
| Medial cord | Medial pectoral | C8, T1 |
| Medial cutaneous of forearm | C8, T1 | |
| Medial cutaneous of arm | C8, T1 | |
| Ulnar | C(7), 8, T1 | |
| Medial root of median | C8, T1 | |
| Posterior cord | Upper subscapular | C5, 6 |
| Thoracodorsal | C6, 7,8 | |
| Lower subscapular | C5, 6 | |
| Axillary | C5, 6 | |
| Radial | C5, 6, 7, 8, (T1) |
Lateral pectoral nerve
The lateral pectoral nerve is larger than the medial, and may arise from the anterior divisions of the upper and middle trunks, or by a single root from the lateral cord. Its axons are from the fifth to seventh cervical rami. It crosses anterior to the axillary artery and vein, pierces the clavipectoral fascia and supplies the deep surface of pectoralis major. It sends a branch to the medial pectoral nerve, forming a loop in front of the first part of the axillary artery (Fig. 46.30), to supply some fibres to pectoralis minor.
Medial pectoral nerve
The medial pectoral nerve is derived from the eighth cervical and first thoracic ventral rami and branches from the medial cord while the latter lies posterior to the axillary artery. It curves forwards between the axillary artery and vein. Anterior to the artery it joins a ramus of the lateral pectoral nerve, and enters the deep surface of pectoralis minor, which it supplies. Two or three branches pierce pectoralis minor and others may pass round its inferior border to end in pectoralis major.
Upper (superior) subscapular nerve
The superior subscapular nerve is smaller than the inferior. It arises from the posterior cord (C5 and 6), enters subscapularis at a high level, and is frequently double.
Lower (inferior) subscapular nerve
The inferior subscapular nerve arises from the posterior cord (C5 and 6). It supplies the lower part of subscapularis, and ends in teres major, which is sometimes supplied by a separate branch.
Thoracodorsal nerve
The thoracodorsal nerve arises from the posterior cord (C6 to 8) between the subscapular nerves. It accompanies the subscapular artery along the posterior axillary wall and supplies latissimus dorsi, reaching its distal border.
Axillary nerve
The axillary nerve arises from the posterior cord (C5, 6) (Fig. 46.22). It is at first lateral to the radial nerve, posterior to the axillary artery and anterior to subscapularis. At the lower border of subscapularis it curves back inferior to the humeroscapular articular capsule and, with the posterior circumflex humeral vessels, traverses a quadrangular space bounded above by subscapularis (anterior) and teres minor (posterior), below by teres major, medially by the long head of triceps, and laterally by the surgical neck of the humerus. It divides in the space into anterior and posterior branches. The anterior branch curves round the neck of the humerus with the posterior circumflex humeral vessels, deep to deltoid. It reaches the anterior border of the muscle and supplies it, and gives off a few small cutaneous branches which pierce deltoid and ramify in the skin over its lower part. The posterior branch courses medially and posteriorly along the attachment of the lateral head of triceps, inferior to the glenoid rim. It usually lies medial to the anterior branch in the quadrangular space. It gives off the nerve to teres minor and the upper lateral cutaneous nerve of the arm at the lateral edge of the origin of the long head of triceps. The nerve to teres minor enters the muscle on its inferior surface. The posterior branch frequently supplies the posterior aspect of deltoid, usually via a separate branch from the main stem, occasionally from the superior lateral cutaneous nerve of the arm. However, the posterior part of deltoid has a more consistent supply from the anterior branch of the axillary nerve, which should be remembered when performing a posterior deltoid-splitting approach to the shoulder. The upper lateral cutaneous nerve of the arm pierces the deep fascia at the medial border of the posterior aspect of deltoid and supplies the skin over the lower part of deltoid and the upper part of the long head of triceps. The posterior branch is intimately related to the inferior aspects of the glenoid and shoulder joint capsule, which may place it at particular risk during capsular plication or thermal shrinkage procedures (Ball et al 2003). There is often an enlargement or pseudoganglion on the branch to teres minor. The axillary trunk supplies a branch to the shoulder joint below subscapularis.
The commonest causes of axillary nerve lesions are trauma (dislocation of the shoulder, fracture of the surgical neck of the humerus), and neuralgic amyotrophy. There is wasting and weakness of deltoid, which is usually clinically evident, and a patch of sensory loss on the outer aspect of the arm. This can be differentiated from a C5 root lesion by finding normal function in the distribution of the suprascapular nerve.
Musculocutaneous nerve
The musculocutaneous nerve arises from the lateral cord (C5–7), opposite the lower border of pectoralis minor (Fig. 46.30). It pierces coracobrachialis and descends laterally between biceps and brachialis to the lateral side of the arm. Just below the elbow it pierces the deep fascia lateral to the tendon of biceps, and continues as the lateral cutaneous nerve of the forearm. A line drawn from the lateral side of the third part of the axillary artery across coracobrachialis and biceps to the lateral side of the biceps tendon is a surface projection for the nerve (but this varies according to its point of entry into coracobrachialis). It supplies coracobrachialis, both heads of biceps and most of brachialis. The branch to coracobrachialis is given off before the musculocutaneous nerve enters the muscle: its fibres are from the seventh cervical ramus and may branch directly from the lateral cord. Branches to biceps and brachialis leave after the musculocutaneous has pierced coracobrachialis: the branch to brachialis also supplies the elbow joint. The musculocutaneous nerve supplies a small branch to the humerus, which enters the shaft with the nutrient artery.
Lesions of the musculocutaneous nerve
An isolated lesion of the musculocutaneous nerve is rare, but may occur in injuries to the upper arm and shoulder, e.g. fracture of the humerus, and in patients with neuralgic amyotrophy. There is marked weakness of elbow flexion, because biceps brachii and much of brachialis are paralysed, and sensory impairment on the extensor aspect of the forearm in the distribution of the lateral cutaneous nerve of the forearm. Pain and paraesthesiae may be aggravated by elbow extension.
Medial cutaneous nerve of arm
The medial cutaneous nerve of the arm is the smallest and most medial branch of the brachial plexus, and arises from the medial cord (C8, T1). It crosses the axilla, either anterior or posterior to the axillary vein, then passes medial to the axillary vein, communicates with the intercostobrachial nerve, and descends medial to the brachial artery and basilic vein. It pierces the deep fascia at the midpoint of the upper arm to supply the skin over the medial aspect of the distal third of the upper arm.
Medial cutaneous nerve of forearm
The medial cutaneous nerve of the forearm arises from the medial cord (C8, T1). It is described further on pages 830 and 856.
Median nerve
The median nerve has two roots from the lateral (C5, 6, 7) and medial (C8, T1) cords, which embrace the third part of the axillary artery, and unite anterior or lateral to it (Fig. 46.30). Some fibres from C7 often leave the lateral root in the lower part of the axilla and pass distomedially posterior to the medial root, and usually anterior to the axillary artery, to join the ulnar nerve. They may branch from the seventh cervical ventral ramus. Clinically they are believed to be mainly motor and to supply flexor carpi ulnaris. If the lateral root is small, the musculocutaneous nerve (C5, 6, 7) connects with the median nerve in the arm.
Ulnar nerve
The ulnar nerve arises from the medial cord (C8, T1) but often receives fibres from the ventral ramus of C7 (Fig. 46.30). It runs distally through the axilla medial to the axillary artery, between it and the vein. It is described further on page 827.
Radial nerve
The radial nerve is the largest branch of the brachial plexus. It arises from the posterior cord (C5, 6, 7, 8, (T1)) (Fig. 46.22), and descends behind the third part of the axillary artery and the upper part of the brachial artery, anterior to subscapularis and the tendons of latissimus dorsi and teres major. With the profunda brachii artery it inclines dorsally, and passes through the triangular space below the lower border of teres major, between the long head of triceps and the humerus. It is described further on page 827.
Brachial plexus lesions
Lesions of the brachial plexus commonly affect either the upper part of the plexus, i.e. C5 and C6 roots and the upper trunk, or the lower part of the plexus, i.e. C8 and T1 roots and the lower trunk. Lesions affecting the upper part are usually traumatic, whereas those affecting the lower part may be caused by trauma but may also be produced by malignant infiltration or a thoracic outlet syndrome. Severe trauma may affect the whole plexus.
Upper plexus palsies
Downward traction of an infant’s arm during birth, or, in adults, a severe fall on the side of the head and the shoulder, forcing the two apart, as frequently occurs in motor cycle injuries, may tear the roots of C5 and C6. This will result in paralysis of deltoid, the short muscles of the shoulder, and of brachialis and biceps. The last two are both elbow flexors, and biceps is also a powerful supinator of the superior radio-ulnar joint. The arm therefore hangs by the side, with the forearm pronated and the palm facing backwards, like a waiter hinting for a tip (Erb–Duchenne paralysis). There is sensory loss over the lateral aspect of the upper arm.
Lower plexus palsies
Upward traction on the arm, e.g. in a forcible breech delivery, may tear the lowest root, T1, which provides the segmental supply to the intrinsic muscles of the hand. The hand assumes a clawed appearance reflecting the unopposed action of the long flexors and extensors of the fingers (Klumpke’s paralysis). There is sensory loss along the medial aspect of the forearm and there is often an associated Horner’s syndrome (ptosis and constriction of the pupil) which occurs as a result of traction on the cervical sympathetic chain.
Malignant infiltration of the brachial plexus may result from extension of an apical lung carcinoma (Pancoast tumour) or from metastatic spread, often from carcinoma of the breast. There is slowly progressive weakness which usually starts in the small muscles of the hand (T1) and spreads to involve the finger flexors (C8). This is usually a painful condition, and the pain may be severe. There is sensory loss on the medial aspect of the forearm (T1) extending into the medial side of the hand and to the little finger (C8). A Horner’s syndrome may occur if there is involvement of the cervical sympathetic ganglia. A similar syndrome may occur following radiotherapy for breast carcinoma, but this is usually painless. Thoracic surgery involving a sternal split may cause traction on the brachial plexus and usually affects the lower part of the plexus.
The lower trunk of the brachial plexus (C8, T1), together with the subclavian artery, may be angulated over a cervical rib (thoracic outlet syndrome). Patients may present with vascular symptoms as a result of kinking of the subclavian artery (this is more likely to occur with large bony ribs), or they may present with neurological deficit (this is more likely in patients with small rudimentary ribs which extend into a fibrous band which joins the first rib anteriorly). Cervical ribs are quite common and are rarely associated with symptoms. There is a slow insidious onset of wasting of the small muscles of the hand, which often starts on the lateral side with involvement of the thenar eminence and first dorsal interosseous. There is pain and paraesthesiae in the medial aspect of the forearm extending to the little finger, and this is often aggravated by carrying shopping or suitcases. A bruit may be heard over the subclavian artery, and the radial pulse may be easily obliterated by movements of the arm, particularly with the arm extended and abducted at the shoulder.
Ball CM, Steger T, Galatz LM, Yamaguchi K. The posterior branch of the axillary nerve: an anatomic study. J Bone Joint Surg. 2003;85:1497-1501.
Burkart AC, Debski RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthopaed Related Res. 2002;400:32-39.
Michael Salmon: Anatomic Studies. In: Taylor GI, Razaboni RM. Book 1, Arteries of the Muscles of the Extremities and the Trunk, Book 2, Arterial anastomotic pathways of the extremities. St Louis: Quality Medical Publishing, 1994.
Contains the translated work of Dr Michel Salmon and describes the blood supply to muscle as well as the anastomotic pathways in the limbs..