CHAPTER 54 Chest wall and breast
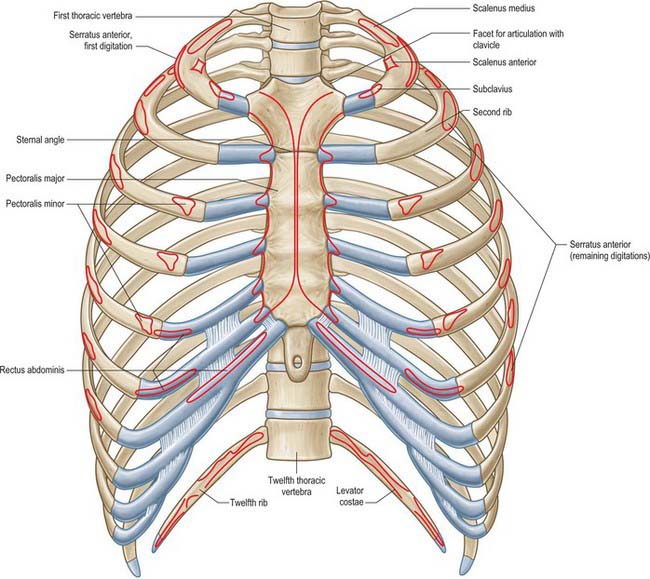
The chest wall surrounds the thoracic cavity. The skin and soft tissue cover a musculoskeletal frame consisting of 12 pairs of ribs which articulate with 12 thoracic vertebrae posteriorly, and (except for the last two pairs of ribs) with the sternum anteriorly, via their costal cartilages; intrinsic muscles and muscles which connect the chest wall with the upper limb and the vertebral column; numerous blood and lymphatic vessels and nerves which supply the components of the musculoskeletal frame and the overlying skin and breast tissue.
SKIN AND SOFT TISSUE
SKIN
Vascular supply
Arteries
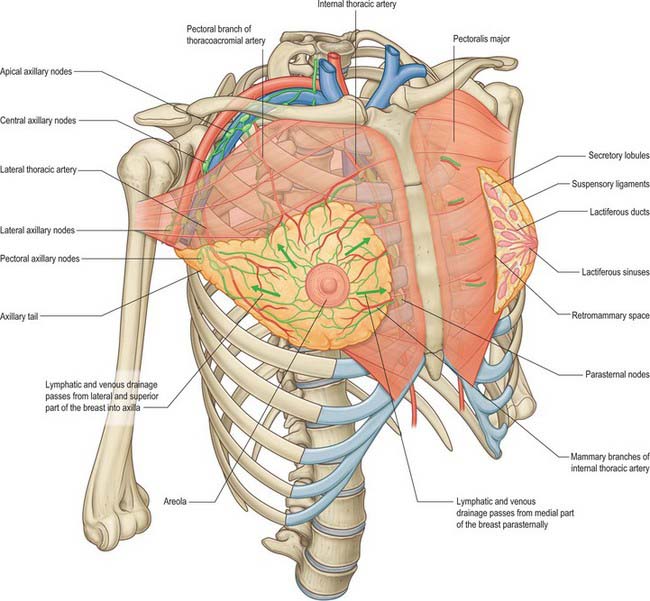
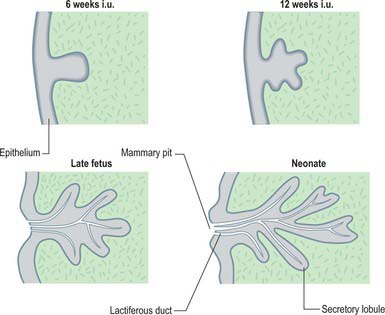
The skin of the thorax is supplied by a combination of direct cutaneous vessels and musculocutaneous perforators which reach the skin primarily via the intercostal muscles, pectoralis major, latissimus dorsi and trapezius. Branches from the thoracoacromial axis, lateral thoracic artery, internal thoracic artery, anterior and posterior intercostal arteries, thoracodorsal, transverse cervical/dorsal scapular and circumflex scapular arteries are the major contributing vessels (Figs 54.1, 54.2; see Fig. 42.4).
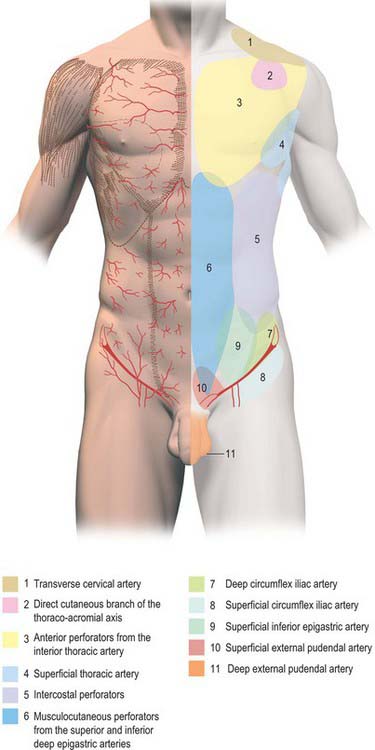
Fig. 54.1 Anatomical territories of cutaneous blood vessels on the anterior trunk.
(By permission from Cormack GC, Lamberty BGH 1994 The Arterial Anatomy of Skin Flaps, 2nd edn. Edinburgh: Churchill Livingstone.)
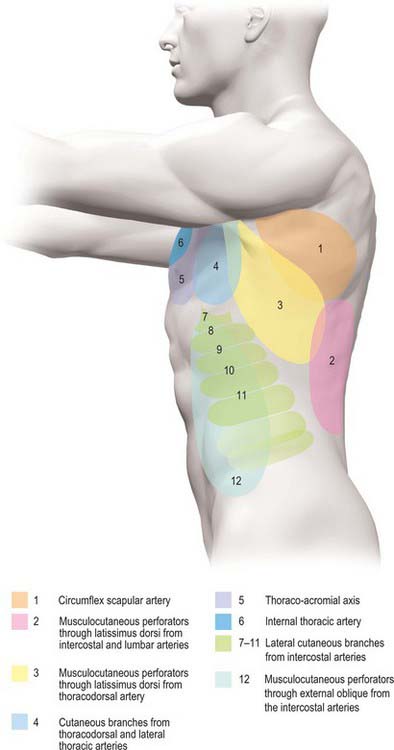
Fig. 54.2 Anatomical territories of cutaneous blood vessels on the lateral trunk.
(By permission from Cormack GC, Lamberty BGH 1994 The Arterial Anatomy of Skin Flaps, 2nd edn. Edinburgh: Churchill Livingstone.)
The anterior aspect of the thoracic skin is supplied by the thoracoacromial axis, the internal thoracic arteries, perforating branches from the intercostal arteries and branches from the lateral thoracic and superficial thoracic arteries. The thoracoacromial axis supplies the skin primarily via musculocutaneous perforators from its pectoral branch, which reach the skin through pectoralis major. In addition, direct cutaneous branches arise from the acromial and deltoid branches. The internal thoracic artery sends direct perforating branches to the skin of the upper six intercostal spaces, accompanied by the cutaneous branches of the anterior intercostal nerves. The branches reach the skin after passing through pectoralis major and travelling laterally in the subcutaneous fat as direct cutaneous vessels: the second intercostal perforator is usually the largest.
The lateral aspect of the thoracic skin is supplied by the lateral thoracic, superficial thoracic and lateral cutaneous branches of the intercostal arteries. The lateral thoracic artery gives off direct cutaneous branches to the lateral chest wall in addition to musculocutaneous branches that pass through pectoralis major.
The posterior aspect of the thoracic skin is supplied by the medial and lateral dorsal cutaneous branches of the posterior intercostal arteries (which reach the skin by passing through erector spinae and latissimus dorsi), musculocutaneous perforating branches from the superficial cervical artery and the transverse cervical/dorsal scapular artery (via trapezius), musculocutaneous perforating branches from the thoracodorsal artery and the intercostal arteries (via latissimus dorsi), and direct cutaneous branches from the circumflex scapular artery.
Veins
The intercostal veins accompany the similarly named arteries in the intercostal spaces (see Fig. 53.3). The small anterior intercostal veins are tributaries of the internal thoracic and musculophrenic veins; the internal thoracic veins drain into the appropriate brachiocephalic vein. The posterior intercostal veins drain backwards and most drain directly or indirectly into the azygos vein on the right and the hemiazygos or accessory hemiazygos veins on the left. The azygos veins exhibit great variation in their origin, course, tributaries, anastomoses and termination (see Ch. 55).
Lymphatic drainage
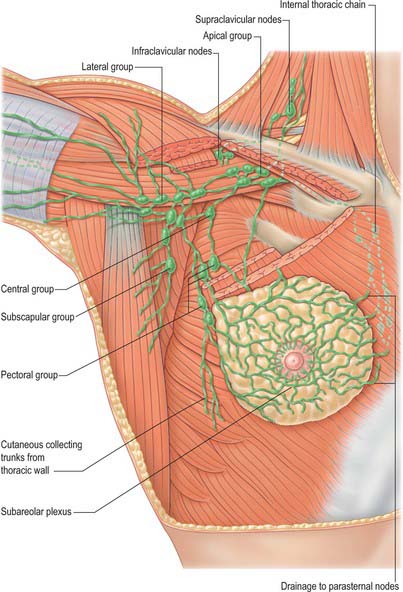
Superficial lymphatic vessels of the thoracic wall ramify subcutaneously and converge on the axillary nodes (see p. 928, Figs 54.19, 54.21). Lymph vessels from the deeper tissues of the thoracic walls drain mainly to the parasternal, intercostal and diaphragmatic lymphatic nodes.
Innervation
The skin of the thorax is supplied by cutaneous branches of cervical and thoracic nerves in consecutive, curved zones, the upper almost horizontal and the lower oblique. On the upper ventral thoracic aspect, the third and fourth cervical areas adjoin the first and second thoracic areas (Fig. 54.3; see Fig. 42.3) because the intervening nerves provide the sensory and motor supply to the upper limb. There is a similar, but less extensive, posterior ‘gap’: most of the skin of the back of the thorax is supplied by the dorsal rami of the thoracic nerves. The subcostal margin is supplied by the seventh thoracic nerve.
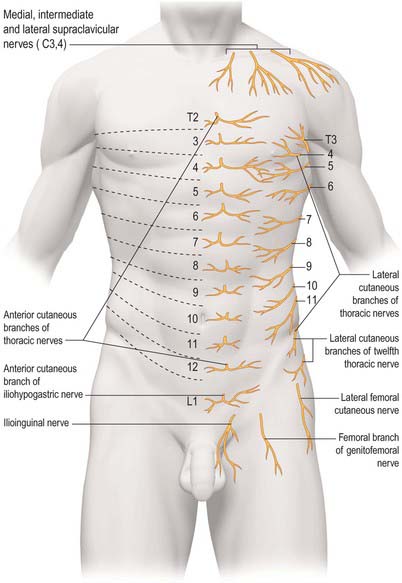
Fig. 54.3 The approximate segmental distribution of the cutaneous nerves on the front of the trunk. The contribution from the first thoracic spinal nerve is not shown and the considerable overlap that occurs between adjacent segments is not indicated.
The ventral rami of the first to the eleventh thoracic nerves pass into the intercostal spaces. Each intercostal nerve gives off a lateral cutaneous branch, which arises beyond the angle of the ribs and divides into anterior and posterior branches, and terminates near the sternum in an anterior cutaneous branch (see Fig. 54.18).
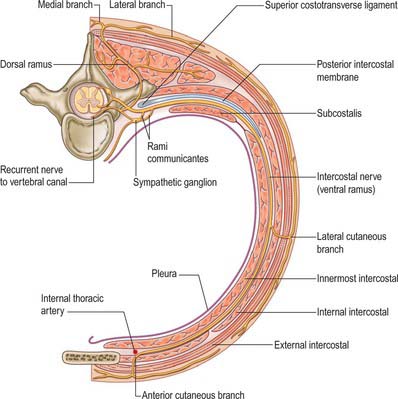
Fig. 54.18 The course of a typical intercostal nerve. The muscular and the collateral branches are not shown.
Branches of the supraclavicular nerve, which originates from the third and fourth cervical nerve roots, supply the skin in the upper pectoral region. Most of the first thoracic nerve joins the brachial plexus: it gives off a small inferior branch, which becomes the first intercostal nerve. The lateral cutaneous branch of the second intercostal nerve supplies the skin of the axilla and is known as the intercostobrachial nerve. The costal margin is supplied by a branch from the seventh thoracic nerve, and the tenth thoracic nerve supplies the skin of the abdomen at the level of the umbilicus. The seventh to eleventh thoracic nerves supply the skin of the thoracic wall as they pass anteriorly and inferiorly; they continue beyond the costal cartilages and supply the skin and subcutaneous tissues of the abdominal wall. The subcostal nerve follows the inferior border of the twelfth rib and supplies the skin of the lower abdominal wall (Fig. 54.3).
SOFT TISSUE
Superficial fascia
The superficial fascia lies below the skin. It consists primarily of fat and is only loosely attached to the skin, an arrangement that allows some movement of the underlying structures. Small blood vessels and nerves perforate the superficial fascia to supply the skin.
The breast lies within the superficial fascia and is described later in this chapter.
BONE AND CARTILAGE
The 12 thoracic vertebrae and their associated intervertebral discs are described in detail in Chapter 42.
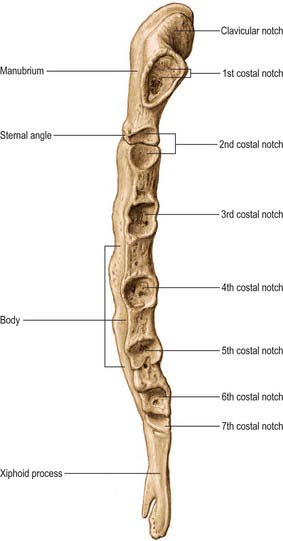
STERNUM
The sternum consists of a cranial manubrium, an intermediate body (mesosternum) and a caudal xiphoid process (Figs 54.4, 54.5). Until puberty, the mesosternum consists of four sternebrae, which, from their costal relations, appear to be intersegmental. The total length of the sternum is approximately 17 cm in males, less in females. The ratio between manubrial and mesosternal lengths differs between the sexes. Growth may continue beyond the third decade and possibly throughout life.
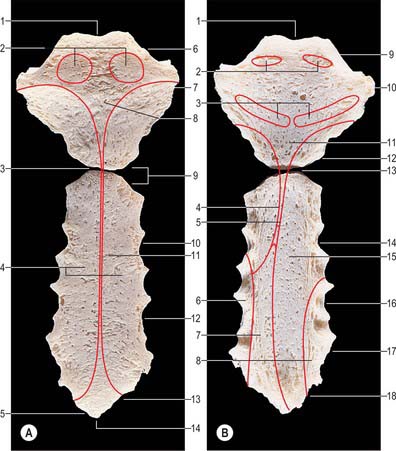
Fig. 54.4 The sternum. A, Anterior aspect. B, Posterior aspect.
Part A: 1. Jugular notch. 2. Attachment for sternocleidomastoid. 3. Sternal angle and manubriosternal joint. 4. Attachment for pectoralis major. 5. Notch for seventh costal cartilage. 6. Clavicular notch. 7. Notch for first costal cartilage 8. Manubrium. 9. Notch for second costal cartilage. 10. Notch for third costal cartilage. 11. Body of sternum. 12. Notch for fourth costal cartilage. 13. Notch for sixth costal cartilage. 14. Xiphisternal joint.
Part B: 1. Jugular notch. 2. Attachment for sternohyoid. 3. Attachment for sternothyroid. 4. Edge of area covered by left pleura. 5. Edge of area covered by right pleura. 6. Attachment for transversus thoracis. 7. Area in contact with pericardium. 8. Attachment for transversus thoracis. 9. Clavicular notch. 10. Notch for first costal cartilage. 11. Manubrium. 12. Notch for second costal cartilage. 13. Sternal angle and manubriosternal joint. 14. Notch for third costal cartilage. 15. Body of sternum. 16. Notch for fourth costal cartilage. 17. Notch for fifth costal cartilage. 18. Notch for seventh costal cartilage.
In natural stance, the sternum slopes down and slightly forwards. It is convex in front, concave behind, and broadest at the junction with the first costal cartilages. It is narrow at the manubriosternal joint, below which it widens to its articulation with the fifth cartilages, and narrows again below this.
The sternum contains highly vascular trabecular bone enclosed by a compact layer that is thickest in the manubrium between the clavicular notches. Centrally, the bone is lightly constructed, whereas laterally the trabeculae are thicker and wider. The medulla contains haemopoietic bone marrow.
Manubrium
The manubrium is level with the third and fourth thoracic vertebrae. It is broad and thick above, and narrows to its junction with the body. The anterior surface is smooth, transversely convex and vertically concave, and the posterior surface is concave and smooth. The superior border is thick, and contains a central jugular (suprasternal) notch between two oval fossae, the clavicular notches, which are directed up and posterolaterally for articulation with the sternal ends of the clavicles. Fibres of the interclavicular ligament are attached to the jugular notch. The inferior border, oval and rough, carries a thin layer of cartilage for articulation with the body. The lateral borders are marked above by a depression for the first costal cartilage and below by a small articular demifacet, which articulates with part of the second costal cartilage. The narrow curved edge descends medially between these facets.
Unlike all the other sternocostal joints, the manubriocostal joint between the manubrium and the first costal cartilage is an unusual form of synarthrosis.
Body
The body is level with the fifth to ninth thoracic vertebrae. It is longer, narrower and thinner than the manubrium, and is broadest near its lower end. The anterior surface is nearly flat and faces slightly upwards. It bears three variable transverse ridges, which mark the levels of fusion of its four sternebrae. A sternal foramen, of varying size and form, may occur between the third and fourth sternebrae. The posterior surface, slightly concave, also displays three less distinct transverse lines. The oval upper end articulates with the manubrium at the level of the sternal angle (manubriosternal joint), which lies opposite the inferior border of the fourth vertebral body. The manubriosternal joint is marked by a posterior transverse groove and is palpable anteriorly as a ridge (Fig. 54.5).
The lower end of the body is narrow and continuous with the xiphoid process. On each lateral border, at its superior angle, a small notch articulates with part of the second costal cartilage (Fig. 54.4). Below this, four costal notches articulate with the third to sixth costal cartilages. The inferior angle bears a small facet which, together with the xiphoid process, articulates with the seventh costal cartilage. Between these articular depressions, a series of curved edges diminish in length downwards and form the anterior limits of the intercostal spaces.
Xiphoid process (xiphisternum)
The xiphoid process is in the epigastrium. It is the smallest and most variable sternal element, and may be broad and thin, pointed, bifid, perforated, curved or deflected. The xiphoid is cartilaginous in youth, but more or less ossified in adults. It is continuous with the lower end of the body at the xiphisternal joint. Anterior to its superolateral angles there are demifacets that articulate with parts of the seventh costal cartilages (Fig. 54.5).
The sternal ends of pectoralis major and sternocleidomastoid are attached to the anterior surface of the manubrium. Sternothyroid is attached to the posterior surface, opposite the first costal cartilage, and the most medial fibres of sternohyoid are attached above sternothyroid. The articular capsules of the sternocostal joints and sternal fibres of pectoralis major are attached to the anterior surface of the body. Transversus thoracis (sternocostalis) is attached to its posterior surface. The external intercostal membranes are attached to the borders of the body between the costal facets. The most medial fibres of rectus abdominis and the aponeuroses of external and internal oblique are attached to the anterior surface of the xiphoid. The linea alba is attached to its lower end, and the aponeuroses of internal oblique and transversus abdominis are attached to its borders. Slips of the diaphragm are attached to its posterior aspect, and the sternum is here related to the liver.
The internal thoracic artery provides the main blood supply for the sternum. A sternal network of vessels derived from the internal thoracic arteries provides a network of perforating arteries at the level of each intercostal space. An anterior network formed by anastomoses between anterior superior and anterior inferior sternal branches and laterosternal and anterosternal arches provides branches that go directly into the sternum. A similar network of vessels exists posteriorly and is formed by anastomoses between posterior superior and posterior inferior vessels and laterosternal and retrosternal arches. The posterior network is more highly developed than the anterior system; these networks are particularly developed at the level of the fourth and fifth intercostal spaces.
The venous network is less developed and formed mainly by large vessels. The inframedullary network of sinuses form a network in the bone and then drain into the venous system. They are transcortical veins, and drain either into the peripheral sternal networks or into the internal thoracic vein.
The manubrium is supplied by the anterior branch of the supraclavicular nerve and the anterior cutaneous branch of the first intercostal nerve, whereas the body of the sternum is supplied largely by anterior branches of the intercostal nerves. The anterior branch of the phrenic nerve runs anteromedially from the diaphragm and supplies the lower portion of the sternum with its contralateral counterpart.
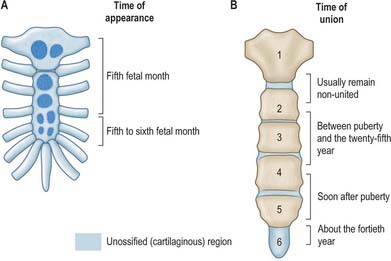
The sternum is formed by fusion of two cartilaginous sternal plates flanking the median plane. The arrangement and number of centres of ossification vary according to the level of completeness and time of fusion of the sternal plates, and to the width of the adult bone. Incomplete fusion leaves a sternal foramen. The manubrium is ossified from one to three centres appearing in the fifth fetal month. The first and second sternebrae usually ossify from single centres that appear at about the same time (Fig. 54.6A). Centres in the third and fourth sternebrae are commonly paired, and appear in the fifth and sixth months, respectively, but one of either pair may be delayed until the seventh or even eighth month, and the fourth sternebral centre may be absent. The xiphoid process begins to ossify in the third year or later. In some sterna, all centres are single and median; in others, the manubrial centre is single and the sternebral centres are all paired, symmetric or asymmetric. Union between mesosternal centres begins at puberty and proceeds from below upwards: by the age of 25 years, they are all united (Fig. 54.6B).
Suprasternal ossicles, paired or single, occur sometimes. They may fuse to the manubrium or articulate posteriorly at the lateral border of the jugular notch. When well formed, they are pyramidal, and their base is articular. The ossicles are cartilaginous at birth, and ossify during adolescence.
Pectus excavatum and carinatum
Pectus excavatum occurs to some extent in about 1 in 500 live births. It is a depression of the sternum and costal cartilage that results in a funnel-shaped chest. The lower costal cartilages and the body of the sternum are depressed and there is some asymmetric curving of the ribs posteriorly. There is frequently an abnormal posture with dorsal lordosis, and some patients also develop a scoliosis. The deformity is either found at birth or occurs early in life: the majority of affected individuals show signs of the abnormality in the first 12 months of life. The aetiology is unknown, but some cases are associated with conditions such as Marfan’s syndrome, in which the connective tissue is abnormal.
Pectus carinatum is the anterior protrusion of the sternum or a pigeon chest. The deformity is less common than pectus excavatum, and although present in early childhood, it usually progresses during adolescence and then remains the same from age 18 throughout adulthood.
RIBS
The ribs are 12 pairs of elastic arches (Fig. 54.7). They articulate posteriorly with the vertebral column and form the greater part of the thoracic skeleton. Their number may be increased by cervical or lumbar ribs or reduced by the absence of the twelfth pair. The first seven pairs are connected to the sternum by costal cartilages, and are referred to as the true ribs. The remaining five are the so-called false ribs: the cartilages of the eighth to tenth usually join the superjacent costal cartilage, whereas the eleventh and twelfth ribs, which are free at their anterior ends, are sometimes termed the ‘floating’ ribs. The tenth rib may also be a floating rib; the incidence varies from 35% to 70% in different races.
The ribs are separated by the intercostal spaces, which are deeper in front and between the upper ribs. The latter are less oblique than the lower ribs; obliquity is maximal at the ninth rib and decreases to the twelfth. Ribs increase in length from the first to seventh, and thereafter diminish to the twelfth. They decrease in breadth downwards; in the upper ten, the greatest breadth is anterior. The first two and last three ribs present special features, whereas the remainder conform to a common plan.
Ribs consist of highly vascular trabecular bone, enclosed in a thin layer of compact bone and containing large amounts of red marrow.
Typical rib
A typical rib has a shaft with anterior and posterior ends (Fig. 54.8). The anterior, costal, end has a small concave depression for the lateral end of its cartilage. The shaft has an external convexity and is grooved internally near its lower border, which is sharp, whereas its upper border is rounded. The posterior, vertebral, end has a head, neck and tubercle. The head presents two facets, separated by a transverse crest. The lower and larger facet articulates with the body of the corresponding vertebra, its crest attaching to the intervertebral disc above it. The neck is the flat part beyond the head, anterior to the corresponding transverse process. It is oblique, and faces anterosuperiorly. Its posteroinferior surface is rough and pierced by foramina. Its upper border is the sharp crest of the neck, its lower border rounded. The tubercle, which is more prominent in upper ribs, is posteroexternal at the junction of the neck and shaft and is divided into medial articular and lateral non-articular areas. The articular part bears a small, oval facet for the transverse process of the corresponding vertebra. The nonarticular area is roughened by ligaments. The shaft is thin and flat and has external and internal surfaces, and superior and inferior borders. It is curved, bent at the posterior angle (5–6 cm from the tubercle), and twisted about its long axis. The part behind the angle inclines superomedially, and so its external surface is posteroinferior. In front of the angle it faces slightly up. It is convex and smooth, and near the tubercle is crossed by a rough line, directed inferolaterally, towards the posterior angle. The smooth internal surface is marked by a costal groove, bounded below by the inferior border. The superior border of the groove continues behind the lower border of the neck, but terminates anteriorly at the junction of the middle and anterior thirds of the shaft, anterior to which the groove is absent.
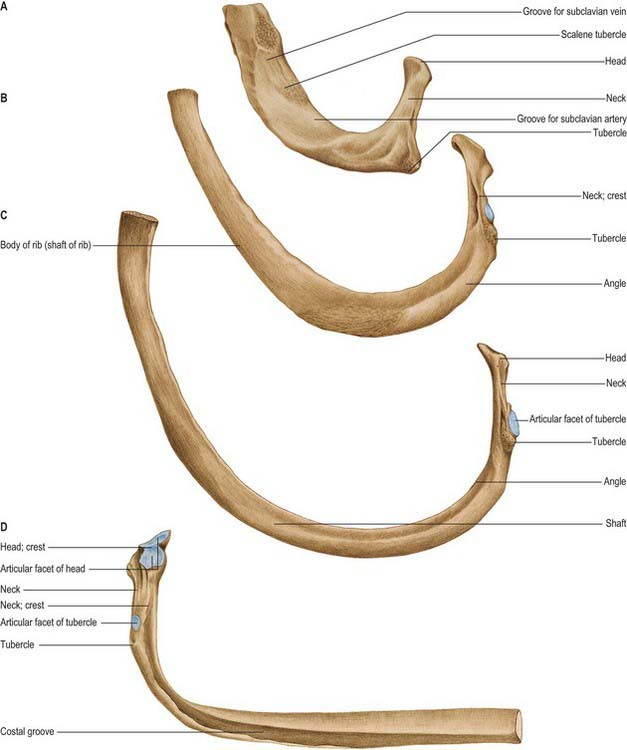
Fig. 54.8 Superior surfaces of a first rib (A) and of second (B) and third (C) ribs, and the inferior surface of an eighth (D) rib, left side.
(From Sobotta 2006.)
A radiate ligament is attached along the anterior border of the head and an intra-articular ligament is attached to the crest of the head. The anterior surface of the head is related to costal pleura and, in lower ribs, to the sympathetic trunk. The anterior surface of the neck is divided by a faint transverse ridge for the internal intercostal membrane and is continuous with the inner lip of the superior border of the shaft. The area above the ridge, which is more or less triangular, is separated from the membrane by fatty tissue. The lower, smooth area is covered by costal pleura. The posterior surface of the neck gives attachment to the costotransverse ligament and is pierced by vascular foramina. The superior costotransverse ligament is attached to the crest of the neck, which extends laterally into the outer lip of the superior border of the shaft. The rounded inferior border of the neck continues laterally into the upper border of the costal groove, and gives attachment to the internal intercostal membrane. The articular area of the tubercle in the upper six ribs is convex and faces posteromedially. In the succeeding three or four ribs it is almost flat, and faces down, back and slightly medially. The lateral costotransverse ligament is attached to the non-articular area.
The ridge on the external surface of the shaft (near its posterior angle) gives attachment to an upward continuation of the thoracolumbar fascia and lateral fibres of iliocostalis thoracis. From the second to the tenth ribs, the distance between angle and tubercle increases. Medial to the angle, the external surface gives attachment to a levator costae and is covered by erector spinae. Near the sternal end of this surface an indistinct oblique line, the anterior ‘angle’, separates the attachments of external oblique and serratus anterior (or latissimus dorsi, in the case of the ninth and tenth ribs). The internal intercostal muscle is attached to the costal groove on the internal surface, and separates the bone and the intercostal neurovascular bundle. At its vertebral end, the groove faces down, its borders in the same plane. The shaft broadens near the posterior angle, and the groove reaches its internal surface. The innermost intercostal is attached to the superior rim of the groove, and this attachment occasionally extends to the anterior quarter of the rib. Posteriorly, the superior rim meets the lower border of the neck. The external intercostal muscle is attached to the sharp inferior costal border. The superior border has two lips posteriorly: an inner and an outer lip. The internal intercostal muscles and the innermost intercostal muscles are attached to the inner lip. The external intercostal muscle is attached to the outer lip.
Vascular supply and innervation
Typical ribs receive their blood supply anteriorly via branches from the internal thoracic artery (first six intercostal spaces) or musculophrenic artery (subsequent spaces), and posteriorly from intercostal arteries derived directly from the aorta. Venous drainage is into the corresponding intercostal vein and then into the azygos system. Typical ribs are innervated segmentally by branches from the corresponding intercostal nerves.
Cervical rib
A cervical rib, the costal element of the seventh cervical vertebra, may be a mere epiphysis on its transverse process, but more often it has a head, neck and tubercle. When a shaft is present, it is of variable length, and extends anterolaterally into the posterior triangle of the neck, where it may end freely or join the first rib or costal cartilage, or even the sternum. A cervical rib may be partly fibrous, but its effects are not related to the size of its osseous part. If it is long enough, its relations are those of a first thoracic rib: the brachial plexus (usually lower trunk) and subclavian vessels are superior and apt to suffer compression in a narrow angle between the rib and scalenus anterior. Hence, cervical ribs may first be revealed by nervous and vascular symptoms, particularly those caused by pressure on the eighth cervical and first thoracic spinal nerves.
A cervical rib or pleurapophysis may show synostosis or diarthrosis with either the anterior (parapophysial) or posterior (diapophysial) ‘roots’ of the so-called seventh cervical transverse process or, more usually, with both.
First rib
Most acutely curved and usually shortest, the first rib is broad and flat, its surfaces are superior and inferior, and its borders are internal and external (Fig. 54.8). It slopes obliquely down and forwards to its sternal end. The obliquity of the first ribs accounts for the appearance of pulmonary and pleural apices in the neck.
The head of the first rib is small and round. It bears an almost circular facet, and articulates with the body of the first thoracic vertebra. The neck is rounded and ascends posterolaterally. The tubercle, wide and prominent, is directed up and backwards; medially, an oval facet articulates with the transverse process of the first thoracic vertebra. At the tubercle, the rib is bent, its head turned slightly down, and so the angle and tubercle coincide. The superior surface of the flattened shaft is crossed obliquely by two shallow grooves, separated by a slight ridge, which usually ends at the internal border as a small pointed projection, the scalene tubercle, to which scalenus anterior is attached. The groove anterior to the scalene tubercle forms a bed for the subclavian vein, and the rough area between this and the first costal cartilage gives attachment to the costoclavicular ligament and, more anteriorly, to subclavius. The subclavian artery and (usually) the lower trunk of the brachial plexus pass in the groove behind the tubercle. Behind this, scalenus medius is attached as far as the costal tubercle.
The external border is convex, thick posteriorly and thin anteriorly. It is covered behind by scalenus posterior descending to the second rib. The first digitation of serratus anterior is, in part, attached to it, behind the subclavian (arterial) groove. The internal border is concave and thin, and the scalene tubercle is near its midpoint. The suprapleural membrane, which covers the cervical dome of the pleura, is attached to the internal border. The inferior surface is smooth. The anterior end is larger than in any other rib.
Second rib
The second rib is twice the length of the first rib, and has a similar curvature. The non-articular area of the tubercle is small. The angle is slight and near the tubercle. The shaft is not twisted, but at the tubercle is convex upwards, as in the first rib, but less so. The external surface of the shaft is convex and superolaterally is marked centrally by a rough, muscular impression that continues posteromedially towards the tubercle as a narrow, roughened ridge. The internal surface, smooth and concave, faces inferomedially and there is a short costal groove posteriorly.
The lower parts of the first and second digitations of serratus anterior are attached to a rough prominence that extends from just behind the midpoint of the external surface (Fig. 54.8). The distinct lips of the upper border are widely separated behind; scalenus posterior and serratus posterior superior are attached to the outer lip in front of the angle.
Vascular supply and innervation
The blood supply of the second rib is the internal thoracic artery and the superior intercostal artery. Venous drainage is via the superior intercostal vein, which drains into the brachiocephalic vein, and the anterior intercostal veins, which drain into the internal thoracic vein. The bone is innervated by branches of the first intercostal nerve.
Tenth, eleventh and twelfth ribs
The tenth rib has a single facet on its head that may articulate with the intervertebral disc above, in addition to the upper border of the tenth thoracic vertebra near its pedicle. The ninth and tenth ribs are usually united anteriorly by a fibrous joint. However, the tenth rib may be free, in which case it is pointed like the eleventh and twelfth ribs.
The eleventh and twelfth ribs each have one large, articular facet on the head, but no neck or tubercle. Their pointed anterior ends are tipped with cartilage. The eleventh rib has a slight angle and shallow costal groove. The twelfth rib has neither, is much shorter and slopes cranially at its vertebral end. The internal surfaces of both ribs face slightly upwards, more so in the twelfth.
Numerous muscles and ligaments are attached to the twelfth rib (Fig. 54.9). Quadratus lumborum and its anterior covering layer of thoracolumbar fascia are attached to the lower part of its anterior surface in its medial one-half to two-thirds; the upper part is related to the costodiaphragmatic pleural recess. The internal intercostal muscle (medially) and the diaphragm (laterally) are attached at or near the upper border. The lower border gives attachment to the middle lamella of the thoracolumbar fascia and, lateral to quadratus lumborum, to the lateral arcuate ligament and posterior lamella of the thoracolumbar fascia. The lumbocostal ligament is attached posteriorly, close to the head, connecting it to the first lumbar transverse process. The lowest levator costae, longissimus thoracis and iliocostalis are attached to the medial half of the external surface, and serratus posterior inferior, latissimus dorsi and external oblique are attached to its lateral half. The external intercostal muscle is attached along the upper border. These attachments vary: those of the internal intercostal, levator costae and erector spinae merge and those of latissimus dorsi, diaphragm and external oblique may reach the costal cartilage. The lower limit of the pleural sac crosses in front of the rib, approximately at the point where it is crossed by the lateral border of iliocostalis. Its lateral end is usually below the line of costodiaphragmatic pleural reflection and is therefore not covered by pleura.
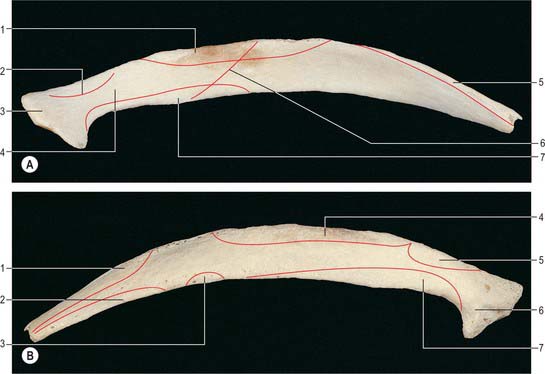
Fig. 54.9 The twelfth rib of the left side. A, Anterior aspect. B, Posterior aspect. A: 1. Attachment of internal intercostal muscle. 2. Attachment of costotransverse ligament. 3. Head. 4. Area covered by pleura. 5. Attachment of diaphragm. 6. Line of pleural reflection. 7. Attachment of quadratus lumborum. B: 1. Attachment of latissimus dorsi. 2. Attachment of external oblique. 3. Attachment of serratus posterior inferior. 4. Attachment of external intercostal muscle. 5. Attachment of levator costae. 6. Head. 7. Attachment of erector spinae.
Vascular supply and innervation
The tenth and eleventh ribs are supplied by the posterior intercostal artery and branches from the musculophrenic artery. The twelfth rib is supplied by the subcostal artery. Venous drainage is via the posterior intercostal and subcostal veins, which in turn drain into the azygos system. There is additional drainage via the anterior intercostal veins (branches of the musculophrenic vein). The tenth and eleventh ribs are innervated by the corresponding intercostal nerve, and the twelfth rib is innervated by the subcostal nerve.
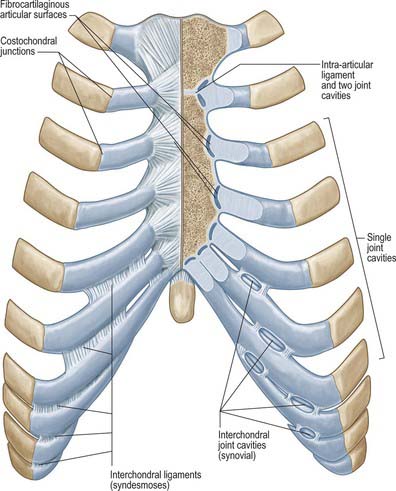
Costal cartilages
Costal cartilages are the persistent, unossified anterior parts of the cartilaginous models in which the ribs develop. They are flat bars of hyaline cartilage that extend from the anterior ends of the ribs, and contribute greatly to thoracic mobility and elasticity (Fig. 54.7). The upper seven pairs join the sternum; the eighth to tenth articulate with the lower border of the cartilage above; the lowest two have free, pointed ends in the abdominal wall. They increase in length from the first to the seventh, and then decrease to the twelfth. They diminish in breadth from first to last, like the intercostal spaces. The costal cartilages are broad at their costal continuity and taper as they pass forward. The first and second are of even breadth and the sixth to eighth enlarge where their margins are in contact. The first descends a little, the second is horizontal and the third ascends slightly; the others are angulated and incline up towards the sternum or cartilage above, a little anterior to their ribs.
Each costal cartilage has two surfaces, borders and ends. The anterior surface is convex, facing anterosuperiorly. The sternoclavicular articular disc, costoclavicular ligament and subclavius are attached to the first costal cartilage. Pectoralis major is attached to the medial aspect of the first six cartilages and the others are covered by the partial attachments of the anterior abdominal muscles. The posterior surface is concave, and really posteroinferior. Sternothyroid is attached to the first cartilage, transversus thoracis is attached to the second to sixth, and transversus abdominis is attached to the lower six. The internal intercostal muscles and external intercostal membranes are attached to the concave superior and convex inferior borders. The inferior borders of the fifth (sometimes), and sixth to ninth cartilages project at points of greatest convexity. Oblong facets on these projections articulate with facets on slight projections from the superior borders of subjacent cartilages. The lateral end of each cartilage is continuous with its rib. The medial end of the first is continuous with the sternum; those of the six succeeding cartilages are round and articulate with shallow costal notches on the lateral margins of the sternum; those of the eighth to tenth are pointed, each connected with the cartilage above; those of the eleventh and twelfth are pointed and free. With the exception of the synarthrosis between the first rib and sternum, all these articulations are synovial.
In old age the costal cartilages tend to ossify superficially, lose their pliability and become brittle.
Rib fractures
Elastic recoil of the ribs which suspend the sternum may explain the rarity of sternal fractures. Despite their pliability, the ribs are much more frequently broken, the middle ribs being the most vulnerable. Because traumatic stress is often the result of compression of the thorax, the usual site of fracture is just in front of the angle, which is the weakest point of the rib. Direct impact may fracture a rib at any point; the ends of the broken bone may be driven inwards, and potentially may injure thoracic or upper abdominal viscera.
JOINTS
MANUBRIOSTERNAL JOINT
The manubriosternal joint lies between the manubrium and sternal body, and is usually a symphysis. The bony surfaces are covered by hyaline cartilage and connected by a fibrocartilage, which may ossify in the aged. Sometimes, the central part of the disc is absorbed and the joint appears synovial. The manubriosternal joint is connected by a fibrous membrane enveloping the entire bone. In occasional individuals over the age of 30 years, the manubrium is joined to the sternal body by bone, but the intervening cartilage may be only superficially ossified; ossification becomes complete only in the aged. Early synostosis has been attributed to a persistent synchondrosis in place of a symphysis. In the newborn, union is by collagenous and elastic fibres, without chondrocytes.
The symphysis permits a small range of angulation between the longitudinal axes of the manubrium and body of the sternum, and also limited anteroposterior displacement. A study of these movements in 62 male athletes yielded (standing position) mean values of 162.7° (full inspiration) and 164.7° (full expiration) for the manubriosternal angle: both movements contribute to respiratory excursions of the sternum.
XIPHISTERNAL JOINT
The joint between the xiphoid process and the body of the sternum process is a symphysis. It is usually transformed to a synostosis by the fortieth year, but sometimes remains unchanged even in old age.
COSTOVERTEBRAL, STERNOCOSTAL AND INTERCHONDRAL JOINTS
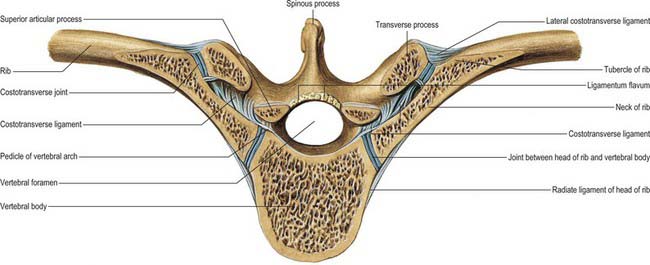
The heads of the ribs articulate with vertebral bodies (costocorporeal joints); their necks and tubercles articulate with transverse processes (costotransverse joints).
Joints of costal heads
Heads of typical ribs articulate with facets (often termed demifacets) on the margins of adjacent thoracic vertebral bodies and with the intervertebral discs between them (Fig. 54.10). The first and tenth to twelfth ribs articulate with a single vertebra by a simple synovial joint. In the others, an intra-articular ligament bisects the joint, producing a double synovial compartment, so the joint is classified as both compound and complex. Often inaccurately described as plane, their articular surfaces are slightly ovoid and the upper and lower synovial articulations are obtusely angled to each other. The ligaments are capsular, radiate and intra-articular.
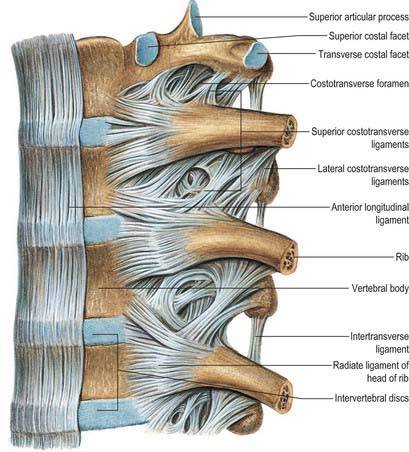
Fig. 54.10 Ligaments of the vertebral column and costovertebral joints, lateral parts of the anterior longitudinal ligament removed, left lateral aspect.
(From Sobotta 2006.)
The fibrous capsule connects the costal head to the circumference of the articular surface formed by an intervertebral disc and the demifacets of two adjacent vertebrae. Some of the upper fibres traverse their intervertebral foramina to blend with the posterior aspects of the intervertebral discs; the posterior fibres are continuous with the costotransverse ligaments.
Radiate ligaments connect the anterior parts of each costal head to the bodies of two vertebrae and their intervening intervertebral disc. Each is attached to the head just beyond its articular surface. Superior fibres ascend to the vertebral body above, inferior to the body below. Intermediate fibres, shortest and least distinct, are horizontal and attached to the disc. The radiate ligament associated with the first rib is attached to the seventh cervical and first thoracic vertebrae. In the joints of the tenth to twelfth ribs, which articulate with single vertebrae, the radiate ligament is attached to the numbered vertebra and the one above.
Costotransverse joints
The facet of a costal tubercle articulates reciprocally with the transverse process of its corresponding vertebra (Fig. 54.11). The eleventh and twelfth ribs lack this articulation. In the upper five or six joints, articular surfaces are reciprocally curved, but below this they are flatter (Fig. 54.12). Their ligaments are capsular, costotransverse, superior and lateral costotransverse, and accessory.
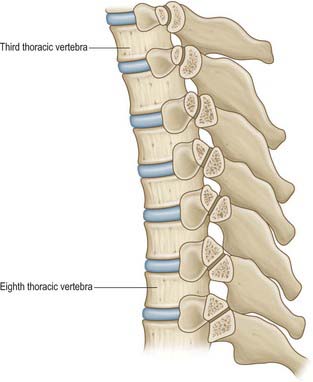
Fig. 54.12 Section through the costotransverse joints from the third to the ninth inclusive. Contrast the concave facets on the upper transverse processes with the less curved facets on the lower transverse processes.
The costotransverse ligament fills the costotransverse foramen between the neck of the rib and its adjacent corresponding transverse process. Its numerous short fibres extend back from the posterior rough surface on the neck to the anterior surface of the transverse process. A costotransverse ligament is rudimentary or absent in the eleventh and twelfth ribs.
Superior costotransverse ligament
The superior costotransverse ligament has anterior and posterior layers. The anterior layer is attached between the crest of the costal neck and lower aspect of the transverse process above, and blends laterally with the internal intercostal membrane; it is crossed by the intercostal vessels and nerve. The posterior layer is attached posteriorly on the costal neck, ascending posteromedially to the transverse process above, and blends laterally with the external intercostal muscle. The first rib has no such ligament. The shaft of the twelfth rib, near its head, is connected to the base of the first lumbar transverse process by a lumbocostal ligament in series with the superior costotransverse ligaments.
An accessory ligament is usually present. It lies medial to the superior costotransverse ligament, and is separated from it by the dorsal ramus of a thoracic spinal nerve and accompanying vessels. These bands are variable in their attachments, but usually pass from a depression medial to a costal tubercle to the inferior articular process immediately above. Some fibres also pass to the base of the transverse process.
Lateral costotransverse ligament
The lateral costotransverse ligament is short, thick and strong and passes obliquely from the apex of the transverse process to the rough non-articular part of the adjacent costal tubercle. The ligaments of upper ribs ascend from their transverse processes, and are shorter and more oblique than those of the lower ribs, which descend.
Costal heads are so firmly tied to vertebral bodies by radiate and intra-articular ligaments that only slight gliding can occur. Strong ligaments binding costal necks and tubercles to transverse processes also limit movements at costotransverse joints to slight gliding, guided by the shape and direction of the articular surfaces (Fig. 54.12). The facets on the tubercles of the upper six ribs are oval and vertically convex, and fit corresponding concavities on the anterior surfaces of transverse processes; consequently, up and down movements of tubercles involve rotation of costal necks about their long axes. The facets on the seventh to tenth tubercles are almost flat, and face down, medially and backwards; their opposing surfaces are on the upper aspects of transverse processes, and so when these tubercles ascend they also move posteromedially. Both sets of joints move simultaneously and in the same directions: the costal neck therefore moves as if at a single joint in which the two articulations form its ends.
In the upper six ribs, the neck moves slightly up and down but its chief movement is one of rotation about its long axis, which means that downward rotation of its anterior aspect is associated with depression, and upward rotation with elevation, of the shaft and anterior end of the rib. In the seventh to tenth ribs, the neck ascends posteromedially or descends anterolaterally, increasing or diminishing the infrasternal angle respectively; slight rotation accompanies these movements.
Sternocostal joints
Costal cartilages articulate with small concavities on the lateral sternal borders (chondrosternal articulations) (Fig. 54.13). Perichondrium and periosteum are continuous. The first sternocostal joint is an unusual variety of synarthrosis, and is often inaccurately called a synchondrosis. The second to seventh costal cartilages articulate by synovial joints, although articular cavities are often absent, particularly in the lower joints. Fibrocartilage covers the articular surfaces and also unites the costal cartilages and the sternum in those joints where cavities are absent. The seventh costosternal joint may be synovial or ‘symphysial’. Ligaments involved are capsular, radiate sternocostal, intra-articular and costoxiphoid.
Fibrous capsules surround the second to seventh sternocostal joints. They are thin, blended with the sternocostal ligaments and are strengthened above and below by fibres that connect the costal cartilages to the sternum.
Radiate sternocostal ligaments
The radiate sternocostal ligaments are broad, thin bands which radiate from the anterior and posterior surfaces of the sternal ends of the costal cartilages of the true ribs to the corresponding sternal surfaces. Their superficial fibres intermingle with adjacent ligaments above and below, with those of the opposite side and with tendinous fibres of pectoralis major; collectively, these tissues form a thick fibrous membrane around the sternum that is more marked inferiorly.
Intra-articular ligaments are constant only between the second costal cartilages and sternum. The ligament associated with the second costal cartilage extends from the costal cartilage to the fibrocartilage uniting the manubrium and sternal body and is therefore intra-articular. Occasionally, the third sternal cartilage is connected with the first and second sternal segments by a similar ligament. Fibrocartilaginous strands may occur in the third and lower joints. Articular cavities may be absent at any age.
Interchondral joints
Contiguous borders of the sixth to ninth costal cartilages articulate by apposition of small oblong facets. Each articulation is enclosed in a thin fibrous capsule, lined by synovial membrane, with lateral and medial interchondral ligaments. Sometimes the fifth cartilage, and less commonly the ninth cartilage, articulate at their inferior borders with adjoining cartilages; this connection is usually effected by ligamentous fibres. Articulation between the ninth and tenth cartilages is never synovial and sometimes absent.
Costochondral junctions
Artificially separated from its rib, a costal cartilage has a rounded end that fits a reciprocal depression in the rib. Periosteum and perichondrium are continuous across the costochondral junctions, and the collagen of the osseous and cartilaginous matrices blend. No movement occurs at costochondral junctions.
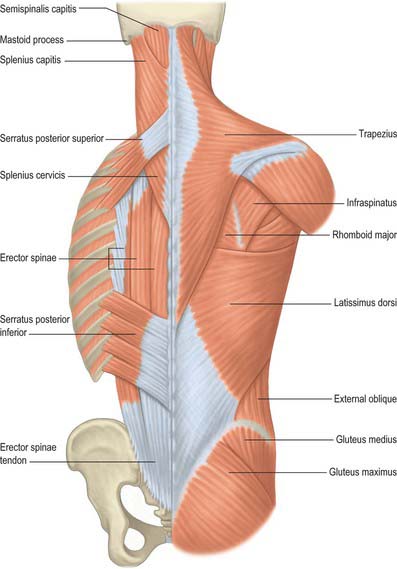
MUSCLES
The intrinsic muscles of the chest wall are the intercostals, subcostales, transversus thoracis, levatores costarum and serratus posterior. Scapular muscles and muscles connecting the upper limb, chest wall and vertebrae, i.e. trapezius, latissimus dorsi, rhomboids major and minor, levator scapulae, pectorales major and minor, subclavius, supra- and infraspinatus, teres major and teres minor, are described in detail in Chapter 46.
INTRINSIC CHEST WALL MUSCLES
Intercostal muscles
The intercostal muscles are thin multiple layers of muscular and tendinous fibres that occupy the intercostal spaces; their names are derived from their spatial relationship, i.e. the external, internal and innermost intercostals (Fig. 54.14).
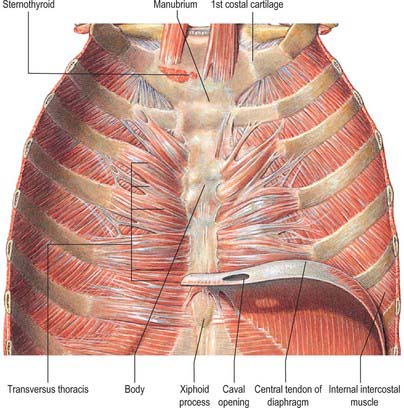
Fig. 54.14 The left transversus thoracis, exposed and viewed from its posterior aspect. Note that the lower border of transversus thoracis is in contact with the upper border of transversus abdominis in the interval between the sternal and costal origins of the diaphragm.
(From Sobotta 2006.)
External intercostals
Eleven pairs of external intercostals extend from the tubercles of the ribs, where they blend with the posterior fibres of the superior costotransverse ligaments, almost to the costal cartilages, where each continues forwards to the sternum as an aponeurotic layer, the external intercostal membrane. Each muscle passes from the lower border of one rib to the upper border of the rib below: their fibres are directed obliquely downwards and laterally at the back of the thorax, and downwards, forwards and medially at the front. In the upper two or three spaces, they do not quite reach the ends of the rib, and in the lower two spaces they extend to the free ends of the costal cartilages. The external intercostals are thicker than the internal intercostals.
Internal intercostals
Eleven pairs of internal intercostals begin anteriorly at the sternum, in the interspaces between the cartilages of the true ribs, and at the anterior extremities of the cartilages of the ‘false’ ribs. Their greatest thickness lies in this intercartilaginous or parasternal part. They continue back as far as the posterior costal angles, where each is replaced by an aponeurotic layer, the internal intercostal membrane, that is continuous posteriorly with the anterior fibres of a superior costotransverse ligament, and anteriorly with the fascia between the internal and external intercostal muscles. Each muscle descends from the floor of a costal groove and adjacent costal cartilage, and inserts into the upper border of the rib below: their fibres are directed obliquely, nearly at right angles to those of the external intercostal muscles.
Innermost intercostals
The innermost intercostals were once regarded as internal laminae of the internal intercostal muscles, and fibres in the two layers do coincide in direction. Each muscle is attached to the internal aspects of two adjoining ribs. They are insignificant, and sometimes absent, at highest thoracic levels, but become progressively more substantial below this, typically extending through the middle two quarters of the lower intercostal spaces. Posteriorly, the innermost intercostals, in those spaces where they are well developed, may come together with the corresponding subcostales. The innermost intercostals are related internally to the endothoracic fascia and parietal pleura, and externally to the intercostal nerves and vessels.
Subcostales
Subcostales consist of muscular and aponeurotic fasciculi, and are usually well developed only in the lower part of the thorax. Each descends from the internal surface of one rib, near its angle, to the internal surface of the second or third rib below. Their fibres run parallel to those of the internal intercostals and, like the innermost intercostals, they lie between the intercostal vessels and nerves and the pleura.
Transversus thoracis
Transversus thoracis (triangularis sternae, sternocostalis) spreads over the internal surface of the anterior thoracic wall (Fig. 54.14). It arises from the lower one-third of the posterior surface of the sternum, the xiphoid process and the costal cartilages of the lower three or four true ribs near their sternal ends. The fibres diverge and ascend laterally as slips that pass into the lower borders and inner surfaces of the costal cartilages of the second, third, fourth, fifth and sixth ribs. The lowest fibres are horizontal, and are contiguous with the highest fibres of transversus abdominis, the intermediate fibres are oblique, and the highest are almost vertical. Transversus thoracis varies in its attachments, not only between individuals but even on opposite sides of the same individual. Like the innermost intercostals and subcostales, transversus thoracis separates the intercostal nerves from the pleura.
Levatores costarum
Levatores costarum are strong bundles, 12 on each side, that arise from the tips of the transverse processes of the seventh cervical and first to eleventh thoracic vertebrae. They pass obliquely downwards and laterally, parallel with the posterior borders of the external intercostals. Each is attached to the upper edge and external surface of the rib immediately below the vertebra from which it takes origin, between the tubercle and the angle (levatores costarum breves). Each of the four lower muscles divides into two fasciculi: one is attached as already described, and the other descends to the second rib below its origin (levatores costarum longi).
Serratus posterior
Serratus posterior superior
Serratus posterior superior (Fig. 54.15) is a thin quadrilateral muscle, external to the upper posterior part of the thorax. It arises by a thin aponeurosis from the lower part of the nuchal ligament, the spines of the seventh cervical and upper two or three thoracic vertebrae and their supraspinous ligaments. It descends laterally, and ends in four digitations attached to the upper borders and external surfaces of the second, third, fourth and fifth ribs, just lateral to their angles. It is superficial to the thoracic part of the thoracolumbar fascia and deep to the rhomboids. The number of digitations can vary from three to six, and the muscle may even be absent.
Serratus posterior inferior
Serratus posterior inferior is a thin, irregularly quadrilateral muscle at the junction of the thoracic and lumbar regions. It arises from the spines of the lower two thoracic and upper two or three lumbar vertebrae and their supraspinous ligaments by a thin aponeurosis that blends with the lumbar part of the thoracolumbar fascia. It ascends laterally, and its four digitations pass into the inferior borders and outer surfaces of the lower four ribs, a little lateral to their angles. There may be fewer digitations and in rare cases the entire muscle may be absent.
Mechanism of thoracic cage movement
Breathing involves changing the thoracic volume by altering the vertical, transverse and anteroposterior dimensions of the thorax (see Ch. 58). The diaphragm is the key muscle in this process. Its muscle fibres descend from their relatively ‘high’ anterior sternocostal attachments steeply to the central tendon and obliquely to their complex ‘low’ posterior attachments (see Fig. 58.1). The central tendon is fixed: when the diaphragm contracts, it allows the lower ribcage to move inferiorly and anteriorly without any change to the curvature of the diaphragm. The intercostal muscles maintain the rigidity of the chest wall. The external and internal intercostals, transversus thoracis, subcostales, levatores costarum, serratus posterior superior and serratus posterior inferior can elevate or depress the ribs, and hence can act as accessory muscles of ventilation.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE OF THE CHEST WALL
ARTERIES
Muscles of the thoracic wall receive their blood supply from the internal thoracic artery, either directly or via the musculophrenic artery, the superior intercostal artery, descending thoracic aorta, and the subcostal and superior thoracic arteries. Additional contributions come from vessels that supply the proximal muscles of the upper limb, namely the suprascapular, superficial cervical, thoracoacromial, lateral thoracic and subscapular arteries.
Internal thoracic artery
The internal thoracic artery arises inferiorly from the first part of the subclavian artery, approximately 2 cm above the sternal end of the clavicle, opposite the root of the thyrocervical trunk (see Figs 53.2, 53.3). It descends behind the first six costal cartilages 1 cm from the lateral sternal border and divides at the level of the sixth intercostal space into musculophrenic and superior epigastric branches.
At first, the internal thoracic artery descends anteromedially behind the sternal end of the clavicle, the internal jugular and brachiocephalic veins and the first costal cartilage. As it enters the thorax, the phrenic nerve crosses it obliquely from its lateral side, usually in front. The artery then descends almost vertically to its bifurcation, lying behind pectoralis major, the first six costal cartilages, external intercostal membranes, internal intercostals and terminations of the upper six intercostal nerves. It is separated from the pleura, down to the second or third cartilage, by a strong layer of fascia, and below this by transversus thoracis. The artery is accompanied by a chain of lymph nodes and by venae comitantes that unite at about the third costal cartilage into a single vein medial to the artery. Its intermediate branches are sternal, anterior intercostal and perforating.
Sternal branches are distributed to transversus thoracis, the periosteum of the posterior sternal surface and the sternal red bone marrow. These branches, together with small branches of the pericardiacophrenic artery, anastomose with branches of the posterior intercostal and bronchial arteries to form a subpleural mediastinal plexus.
Anterior intercostal arteries are distributed to the upper six intercostal spaces. They pass laterally along the borders of the space and anastomose with the posterior intercostal arteries and their collateral branches. The anterior intercostals usually arise from the internal thoracic artery as single vessels that promptly divide into two branches, one passing to the superior, and one to the inferior, part of each intercostal space. Occasionally, one branch passes to the space above, and one to the space below. (The anterior intercostals may sometimes arise as two separate branches from the internal thoracic artery.) The arteries lie at first between the pleura and the internal intercostals, then between the innermost and the internal intercostals. They supply the intercostal muscles and send branches through them to the pectoral muscles, breast and skin.
Perforating branches traverse the upper five or six intercostal spaces with the anterior cutaneous branches of the corresponding intercostal nerves. They pierce and supply pectoralis major, and then curve laterally to become direct cutaneous vessels that supply the skin. These cutaneous vessels provide the anatomical basis for surgically raising a skin flap in this region, the deltopectoral flap, that is used for reconstructing areas of missing tissue in the head and neck. The second to fourth branches supply the breast, and become enlarged during lactation.
The musculophrenic artery passes inferolaterally behind the seventh to ninth costal cartilages, traverses the diaphragm near the ninth, and ends near the last intercostal space. It anastomoses with the inferior phrenic and lower two posterior intercostal arteries and ascending branches of the deep circumflex iliac arteries. Two anterior intercostal arteries branch from it for each of the seventh to ninth intercostal spaces, and are distributed similarly to their counterparts in the higher spaces. The musculophrenic artery also supplies the lower part of the pericardium and the abdominal muscles.
Superior intercostal artery
The superior intercostal artery arises from the costocervical trunk. It descends between the pleura and the necks of the first and second ribs and anastomoses with the third posterior intercostal artery. Crossing the neck of the first rib, it lies medial to the ventral branch of the first thoracic spinal nerve, which it crosses at a lower level, and lateral to the stellate ganglion. In the first space it gives off the first posterior intercostal artery, which has a similar distribution to the lower posterior intercostal arteries. It descends to become the second posterior intercostal artery, usually joining a branch from the third. The artery is not constant, and is more common on the right; when absent, it is replaced by a direct branch from the aorta.
Posterior intercostal arteries
There are usually nine pairs of posterior intercostal arteries (Fig. 54.16). They arise from the posterior aspect of the descending thoracic aorta and are distributed to the lower nine intercostal spaces. Right posterior intercostal arteries are longer, because the aorta deviates to the left: they cross the vertebral bodies behind the oesophagus, thoracic duct and azygos vein, right lung and pleura. Left posterior intercostal arteries turn backwards on the vertebral bodies in contact with the left lung and pleura; the upper two are crossed by the left superior intercostal vein, and the lower by the hemiazygos and accessory hemiazygos veins. The further course of the arteries is the same on both sides. The sympathetic trunk lies anterior to all of the arteries, and the splanchnic nerves descend in front of the lower arteries.
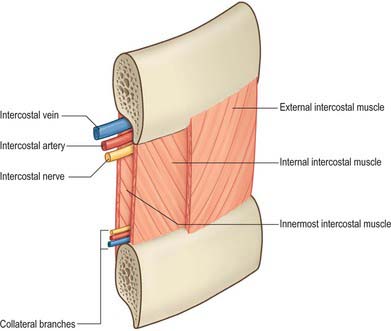
Fig. 54.16 Dissection of part of an intercostal space, showing the position of the intercostal vessels and nerve relative to the intercostal muscles.
Each artery crosses its intercostal space obliquely towards the angle of the rib above and continues forward in its costal groove. At first between the pleura and internal intercostal membrane as far as the costal angle, it passes between the internal intercostal and innermost intercostal muscles (Fig. 54.17), anastomosing with an anterior intercostal branch from either the internal thoracic or musculophrenic artery. Each artery has a vein above and a nerve below, except in the upper spaces, where the nerve at first lies above the artery. The third posterior intercostal artery anastomoses with the superior intercostal artery and may provide the major supply to the second space. The lower two arteries continue anteriorly into the abdominal wall, where they anastomose with the subcostal, superior epigastric and lumbar arteries. Each posterior intercostal artery has dorsal, collateral, muscular and cutaneous branches.
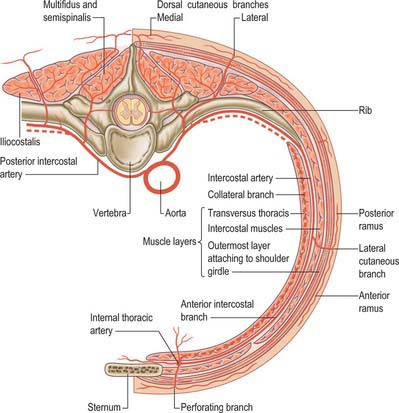
Fig. 54.17 Schematic transverse section through one half of a lower intercostal space to show the branches of a typical intercostal artery. The usual branching arrangement of the dorsal cutaneous branch is shown to the right of the spine and a common variant is shown to the left.
(By permission from Cormack GC, Lamberty BGH 1994 The Arterial Anatomy of Skin Flaps, 2nd edn. Edinburgh: Churchill Livingstone.)
Each dorsal branch runs dorsally between the necks of adjoining ribs; a vertebral body and superior costotransverse ligament lie medial and lateral, respectively. Each dorsal branch gives off a spinal branch which enters the vertebral canal via the intervertebral foramen and supplies the vertebrae, spinal cord and meninges, and anastomoses with the spinal arteries above and below and with its contralateral fellow. It then divides into a medial and a lateral dorsal musculocutaneous branch (occasionally these arise separately from the posterior intercostal artery rather than from a common trunk). The medial branch crosses a transverse process with the medial dorsal branch of a thoracic spinal nerve to supply spinalis and longissimus thoracis and an area of overlying skin. The lateral branch supplies longissimus thoracis and iliocostalis, and the medial aspects of latissimus dorsi and trapezius, in addition to an area of overlying skin.
A collateral intercostal branch arises near the costal angle and descends to the upper border of the subjacent rib, along which it courses to anastomose with an anterior intercostal branch of the internal thoracic or musculophrenic artery.
Muscular branches supply intercostal and pectoral muscles and serratus anterior, and anastomose with the superior and lateral thoracic branches of the axillary artery. Lateral cutaneous branches accompany the same branches of the thoracic spinal nerves. Mammary branches from the vessels in the second to fourth spaces supply the pectoral muscles, breast tissue and skin: they enlarge during lactation.
The lateral cutaneous branch is given off in the posterior part of the intercostal space and travels anteriorly for a few centimetres with an accompanying vein and the lateral cutaneous branch of the equivalent intercostal nerve. This neurovascular bundle pierces the intercostal muscles and emerges lower down between the interdigitations of serratus anterior and external oblique. It divides into anterior and posterior rami, which contribute to the blood supply of the skin of the lateral trunk; these vessels are less significant in the upper three intercostal spaces.
VEINS
Internal thoracic veins
The internal thoracic veins are venae comitantes of the inferior half of the internal thoracic artery. Near the third costal cartilages, the veins unite and ascend medial to the artery to end in their appropriate brachiocephalic vein (see Fig. 28.14). Tributaries correspond to branches of the artery, and include a pericardiacophrenic vein. The internal thoracic veins have several valves.
Left superior intercostal vein
The left superior intercostal vein drains the second and third (sometimes fourth) left posterior intercostal veins. It ascends obliquely forwards across the left aspect of the aortic arch, lateral to the left vagus and medial to the left phrenic nerve, to open into the left brachiocephalic vein (see Fig. 28.14). It usually receives the left bronchial veins, sometimes the left pericardiacophrenic vein, and connects inferiorly with the accessory hemiazygos vein.
Posterior intercostal veins
The posterior intercostal veins accompany their arteries in 11 pairs. Approaching the vertebral column, each vein receives a posterior tributary that returns blood from the dorsal muscles and skin and the vertebral venous plexuses (see Fig. 55.4A,B). On both sides, the first posterior intercostal vein ascends anterior to the neck of the first rib, arching forward above the pleural dome to end in the ipsilateral brachiocephalic or vertebral vein. On the right side, the second, third and often fourth veins form a right superior intercostal vein that joins the arch of the azygos vein. Veins from the lower spaces drain directly to the azygos. On the left side, the second, third and sometimes fourth veins form a left superior intercostal vein. Veins from the fourth or fifth to eighth intercostal spaces end in the accessory hemiazygos vein, and veins from the ninth to the eleventh intercostal spaces end in the hemiazygos vein.
Posterior intercostal veins are so called to distinguish them from small anterior intercostal veins, which are tributaries of the internal thoracic and musculophrenic veins.
LYMPHATIC DRAINAGE
Superficial lymphatic vessels of the thoracic wall ramify subcutaneously and converge on the axillary nodes (see Fig. 54.19). Those superficial to trapezius and latissimus dorsi unite to form 10 or 12 trunks which end in the subscapular nodes. Those in the pectoral region, including vessels from the skin covering the periphery of the breast and its subareolar plexus, run back, collecting those superficial to serratus anterior, to reach the pectoral nodes. Vessels near the lateral sternal margin pass between the costal cartilages to the parasternal nodes, but also anastomose across the sternum. A few vessels from the upper pectoral region ascend over the clavicle to the inferior deep cervical nodes. Lymph from the deeper tissues of the thoracic walls drains mainly to the parasternal, intercostal or diaphragmatic nodes.
Parasternal (internal thoracic) nodes
There are four or five parasternal nodes along each internal thoracic artery, at the anterior ends of the intercostal spaces. They drain afferents from the breast, deeper structures of the supraumbilical anterior abdominal wall, the superior hepatic surface (through a small group of nodes behind the xiphoid process) and deeper parts of the anterior thoracic wall. Their efferents usually unite with those from the tracheobronchial and brachiocephalic nodes to form the bronchomediastinal trunk. The latter may open, on either side, directly into the jugulosubclavian junction or into either great vein near the junction or may join the right subclavian trunk or right lymphatic duct, or the thoracic duct on the left.
Intercostal nodes
Intercostal nodes occupy the intercostal spaces near the heads and necks of the ribs. They receive deep lymph vessels from the posterolateral aspects of the chest and the breast, some of which are interrupted by small lateral intercostal nodes. Efferents of nodes in the lower four to seven spaces unite into a trunk that descends to the abdominal confluence of lymph trunks or to the start of the thoracic duct. Efferents of nodes in the left upper spaces end in the thoracic duct; those of the right upper spaces end in one of the right lymph trunks.
Diaphragmatic nodes
Located on the thoracic surface of the diaphragm, these nodes are arranged in anterior, right and left lateral, and posterior groups.
The anterior group consists of two or three small nodes behind the base of the xiphoid process, draining the convex hepatic surface, and one or two nodes on each side near the junction of the seventh rib and cartilage, which receive anterior lymph vessels from the diaphragm. The anterior group drains to the parasternal nodes.
The lateral groups each contain two or three nodes, and lie close to the point where the phrenic nerves enter the diaphragm. On the right, some nodes lie within the fibrous pericardium anterior to the intrathoracic end of the inferior vena cava. Their afferents drain the central diaphragm; those on the right also drain the convex surface of the liver, and their efferents pass to the posterior mediastinal, parasternal and brachiocephalic nodes.
Lymphatic drainage of deeper tissues
Collecting vessels of the deeper thoracic tissues include lymphatics that drain the muscles attached to the ribs. Most end in axillary nodes, and some from pectoralis major also drain to the parasternal nodes. Intercostal vessels drain the intercostal muscles and parietal pleura; those from the anterior thoracic wall and pleura end in the parasternal nodes, and their posterior counterparts drain to intercostal nodes.
Vessels from the diaphragm form two plexuses, thoracic and abdominal, which anastomose freely, especially in areas covered by pleurae and peritoneum respectively. The thoracic plexus unites with lymph vessels draining the costal and mediastinal pleura. Its efferents are anterior, draining to the anterior diaphragmatic nodes near the junctions of the seventh ribs and cartilages; middle, draining to nodes on the oesophagus and around the end of the inferior vena cava; posterior, draining to nodes around the aorta at the point where it leaves the thorax. The abdominal plexus anastomoses with the hepatic lymphatics and peripherally with those of the subperitoneal tissue. Efferents from its right half end in a group of nodes on the inferior phrenic artery, or in the right lateral aortic nodes. Those from the left half of the abdominal diaphragmatic plexus pass to the pre-aortic and lateral aortic nodes and to nodes near the terminal oesophagus.
INNERVATION OF THE CHEST WALL
THORACIC VENTRAL SPINAL RAMI
There are 12 pairs of thoracic ventral rami. The upper 11 lie between the ribs (intercostal nerves), and the twelfth lies below the last rib (subcostal nerve) (Figs 54.3, 54.18). Each is connected with the adjoining ganglion of the sympathetic trunk by grey and white rami communicantes; the grey ramus joins the nerve proximal to the point at which the white ramus leaves it. Intercostal nerves are distributed primarily to the thoracic and abdominal walls. The first two nerves supply fibres to the upper limb in addition to their thoracic branches, the next four supply only the thoracic wall, and the lower five supply both thoracic and abdominal walls. The subcostal nerve is distributed to the abdominal wall and the gluteal skin. Communicating branches link the intercostal nerves posteriorly in the intercostal spaces, and the lower five nerves communicate freely in the abdominal wall.
First to sixth thoracic ventral rami
The first thoracic ventral ramus divides unequally. A large branch ascends across the neck of the first rib, lateral to the superior intercostal artery, and enters the brachial plexus. The smaller branch is the first intercostal nerve; it runs in the first intercostal space and ends on the front of the chest as the first anterior cutaneous nerve of the thorax. It gives off a lateral cutaneous branch, which pierces the chest wall in front of serratus anterior and supplies the axillary skin; it may communicate with the intercostobrachial nerve and sometimes joins the medial cutaneous nerve of the arm. The first thoracic ramus often receives a connecting ramus from the second, which ascends in front of the neck of the second rib.
The second to sixth thoracic ventral rami pass forwards in their intercostal spaces below the intercostal vessels. Posteriorly they lie between the pleura and external intercostal membranes, but in most of their course they run between the internal intercostals and the subcostales and innermost intercostals. Near the sternum, they cross anterior to the internal thoracic vessels and transversus thoracis, pierce the internal intercostals, the external intercostal membranes and pectoralis major, and end as the anterior cutaneous nerves of the thorax, supplying the skin on the anterior chest wall. The second anterior cutaneous nerve may be connected to the medial supraclavicular nerves of the cervical plexus, and twigs from the sixth intercostal nerve supply abdominal skin in the upper part of the infrasternal angle.
Numerous slender muscular filaments supply the intercostals, serratus posterior superior and transversus thoracis. Anteriorly, some cross the costal cartilages from one intercostal space to another.
Each intercostal nerve gives off a collateral and a lateral cutaneous branch before it reaches the angle of the adjoining ribs (Fig. 54.18). The collateral branch follows the inferior border of its space in the same intermuscular place as the main nerve, which it may rejoin before it is distributed as an additional anterior cutaneous nerve. The lateral cutaneous branch accompanies the main nerve a little way and then pierces the intercostal muscles obliquely. With the exception of the lateral cutaneous branches of the first and second intercostal nerves, each divides into anterior and posterior rami that subsequently pierce serratus anterior. Anterior branches run forwards over the border of pectoralis major to supply the overlying skin; those of the fifth and sixth also supply twigs to a variable number of upper digitations of external oblique. Posterior branches run backwards and supply the skin over the scapula and latissimus dorsi.
The lateral cutaneous branch of the second intercostal nerve is the intercostobrachial nerve (see Fig. 46.30). It crosses the axilla to gain the medial side of the arm and joins a branch of the medial cutaneous nerve of the arm. It then pierces the deep fascia of the arm, and supplies the skin of the upper half of the posterior and medial parts of the arm, communicating with the posterior cutaneous branch of the radial nerve. Its size is in inverse proportion to the size of the medial cutaneous nerve. A second intercostobrachial nerve often branches off from the anterior part of the third lateral cutaneous nerve and sends filaments to the axilla and the medial side of the arm.
Seventh to eleventh thoracic ventral rami
The ventral rami of the seventh to eleventh thoracic nerves are continued anteriorly from the intercostal spaces into the abdominal wall; their further course is described in Chapter 62.
Lesions of the intercostal nerves
Subluxation of the interchondral joints between the lower costal cartilages may trap the intercostal nerves, causing referred abdominal pain. The dorsal cutaneous branch of an intercostal nerve can become entrapped as it penetrates the fascia of erector spinae. This produces an area of numbness, usually with painful paraesthesiae, which extends approximately 10 cm from the midline laterally and 10 cm in length (notalgia paraesthetica); the area between the medial edge of the scapula and the spine is commonly affected. The anterior cutaneous branches of the intercostal nerves can become entrapped as they penetrate the fascia of rectus abdominis, and this produces an area of numbness on the abdomen, usually with painful paraesthesiae, which extends from the midline laterally 10 or 12 cm (rectus abdominis syndrome).
Twelfth thoracic ventral ramus (subcostal nerve)
The ventral ramus of the twelfth thoracic nerve (subcostal nerve) is larger than the others and gives a communicating branch to the first lumbar ventral ramus (sometimes termed the dorsolumbar nerve). Like the intercostal nerves, it soon gives off a collateral branch and then accompanies the subcostal vessels along the inferior border of the twelfth rib, passing behind the lateral arcuate ligament and kidney and in front of the upper part of quadratus lumborum. It perforates the aponeurosis of the origin of transversus abdominis and passes forwards between that muscle and internal oblique, to be distributed in the same manner as the lower intercostal nerves. The subcostal nerve connects with the iliohypogastric nerve of the lumbar plexus and sends a branch to pyramidalis. Its lateral cutaneous branch pierces the internal and external oblique muscles and supplies the lowest slip of the latter. It usually descends over the iliac crest 5 cm behind the anterior superior iliac spine (see Fig. 61.4) and is distributed to the anterior gluteal skin; some filaments reach as low as the greater trochanter of the femur.
THORACIC DORSAL SPINAL RAMI
Thoracic dorsal rami pass backwards close to the vertebral zygapophysial joints and divide into medial and lateral branches. The medial branch emerges between the joint and the medial edge of the superior costotransverse ligament and intertransverse muscle. The lateral branch runs in the interval between the ligament and the muscle before inclining posteriorly on the medial side of levator costae.
Medial branches of the upper six thoracic dorsal rami pass between and supply semispinalis thoracis and multifidus; they then pierce the rhomboids and trapezius, and reach the skin near the vertebral spines (see Fig. 43.6). Medial branches of the lower six thoracic dorsal rami are distributed mainly to multifidus and longissimus thoracis; occasionally they give filaments to the skin in the median region. Lateral branches increase in size from above downwards. They run through or deep to longissimus thoracis to the interval between it and iliocostalis cervicis, and supply these muscles and levatores costarum; the lower five or six also give off cutaneous branches, which pierce serratus posterior inferior and latissimus dorsi in line with the costal angles (see Fig. 43.6). The lateral branches of a variable number of the upper thoracic rami also supply the skin. The lateral branch of the twelfth sends a filament medially along the iliac crest, then passes down to the skin of the anterior part of the gluteal region.
Medial cutaneous branches of the thoracic dorsal rami descend for some distance close to the vertebral spines before reaching the skin. Lateral branches descend for a considerable distance, which may be as much as the breadth of four ribs, before they become superficial, e.g. the branch of the twelfth thoracic ramus reaches the skin only a little way above the iliac crest.
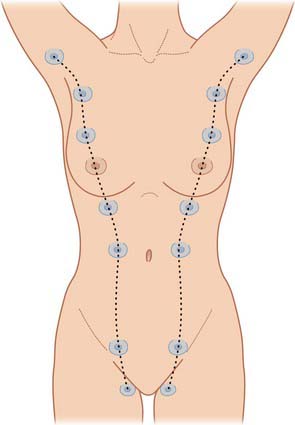
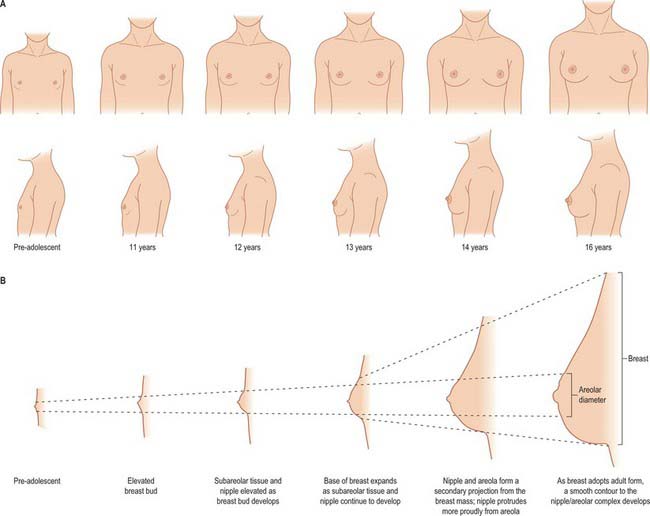
BREAST
The breasts form a secondary sexual feature of females and are the source of nutrition for the neonate. They are also present in a rudimentary form in males. The breasts are the site of malignant change in as many as one in ten women. For reviews of normal breast structure, consult Ellis et al (1993).
In young adult females, each breast is a rounded eminence lying within the superficial fascia, largely anterior to the upper thorax but spreading laterally to a variable extent (Figs 54.19, 54.20B). Breast shape and size depend upon genetic, racial and dietary factors, and the age, parity and menopausal status of the individual. Breasts may be hemispherical, conical, variably pendulous, piriform or thin and flattened. In the adult female, the base of the breast, i.e. its attached surface, extends vertically from the second or third to the sixth rib, and in the transverse plane from the sternal edge medially almost to the midaxillary line laterally. The superolateral quadrant is prolonged towards the axilla along the inferolateral edge of pectoralis major, from which it projects a little, and may extend through the deep fascia up to the apex of the axilla (the axillary tail of Spence). The trunk superficial fascial system splits to enclose the breast to form the anterior and posterior lamellae. Posterior extensions of the superficial fascial system connect the breast to the pectoralis fascia, part of the deep fascial system. The inframammary crease is a zone of adherence of the superficial fascial system to the underlying chest wall at the inferior crescent of the breast.
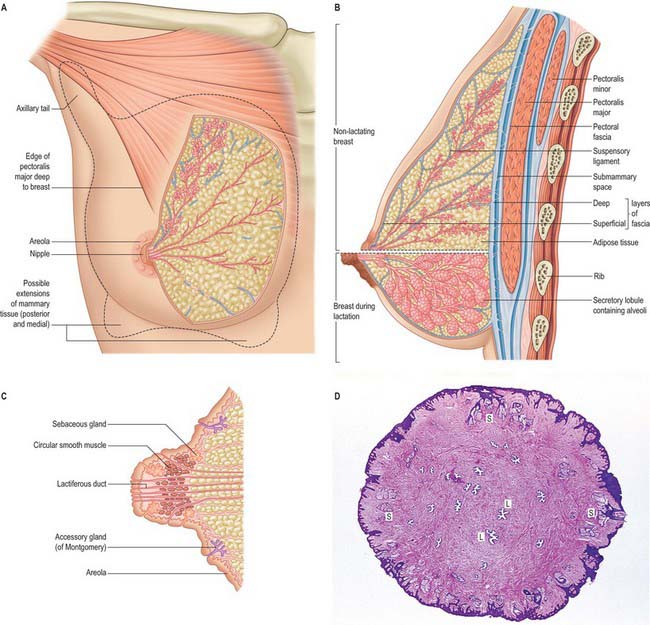
Fig. 54.20 A, Structure of the breast. B, Changes in the breast during lactation. C, Section of the nipple. D, Cross-section of the nipple. There is a corrugated layer of stratified squamous keratinized epithelium over the nipple surface; 20 or more lactiferous ducts (L) open onto the surface; sebaceous glands (S) are deep to the epidermis.
(D, By permission from Dr JB Kerr, Monash University, from Kerr JB 1999 Atlas of Functional Histology. London: Mosby.)
The breast lies upon the deep pectoral fascia, which in turn overlies pectoralis major and serratus anterior superiorly and external oblique and its aponeurosis (as the latter forms the anterior wall of the sheath of rectus abdominis) inferiorly. Between the breast and the deep fascia the loose connective tissue in the ‘submammary space’ allows the breast some degree of movement on the deep pectoral fascia. Advanced mammary carcinoma may, by invasion, cause tethering or fixation of the breast to the underlying musculature. Occasionally, small projections of glandular tissue may pass through the deep fascia into the underlying muscle in normal subjects.
The nipple projects from the centre of the breast anteriorly (Fig. 54.20C,D). Its shape and projection varies from cylindrical and rounded at the top, to hemispherical, to flattened, depending on nervous, hormonal, developmental and other factors. The level of the nipple varies widely. In females, its site is dependent on the size and shape of the breasts, but it overlies the fourth intercostal space in most young women. In the male, the nipple is usually sited in the fourth intercostal space in the midclavicular line. In the young adult of either sex, the nipples are usually positioned 20–23 cm from the suprasternal notch in the midclavicular line and 20–23 cm apart in the horizontal plane. With increasing age and parity, female breasts adopt a more ptotic shape and the nipple position drops either to the level of the inframammary crease or lies below this surface landmark. In the nulliparous, it is pink, light brown or darker, depending on the general melanization of the body. Occasionally, the nipple may not evert during prenatal development, in which case it remains permanently retracted and so causes difficulty in suckling.
NIPPLE AND AREOLA
The skin covering the nipple and the surrounding areola (the disc of skin that circles the base of the nipple) has a convoluted surface (Fig. 54.20C). It contains numerous sweat and sebaceous glands which open directly onto the skin surface. The oily secretion of these specialized sebaceous glands acts as a protective lubricant and facilitates latching of the neonate during lactation: the glands are often visible in parous women, arranged circumferentially as small elevations, Montgomery’s tubercles, around the areola close to the margin. Other areolar glands, which are intermediate in structure between mammary and sweat glands, become enlarged in pregnancy and lactation as subcutaneous tubercles. The sebaceous glands of the areola usually lack hair follicles. The skin of the nipple and areola is rich in melanocytes and is therefore typically darker than the skin covering the remainder of the breast: further darkening occurs during the second month of pregnancy, and subsequently persists to a variable degree.
SOFT TISSUE
The breasts are composed of lobes which contain a network of glandular tissue consisting of branching ducts and terminal secretory lobules in a connective tissue stroma (see Fig. 54.26A). The terminal duct lobular unit is the functional milk secretory component of the breast and pathologically gives rise to primary malignant lesions within the breast. Although the lobes are usually described as discrete territories, they intertwine in three dimensions and merge at their edges; they cannot be distinguished during surgery. The connective tissue stroma that surrounds the lobules is dense and fibrocollagenous, whereas intralobular connective tissue has a loose texture that allows the rapid expansion of secretory tissue during pregnancy (see Fig. 54.26B). Fibrous strands or sheets consisting of condensations of connective tissue extend between the layer of deep fascia that covers the muscles of the anterior chest wall and the dermis. These suspensory ligaments (of Astley Cooper) are often well developed in the upper part of the breast and support the breast tissue, helping to maintain its non-ptotic form. Elsewhere in the normal breast, fibrous tissue surrounds the glandular components and extends to the skin and nipple, assisting the mechanical coherence of the gland. The interlobar stroma contains variable amounts of adipose tissue which is responsible for much of the increase in breast size at puberty.
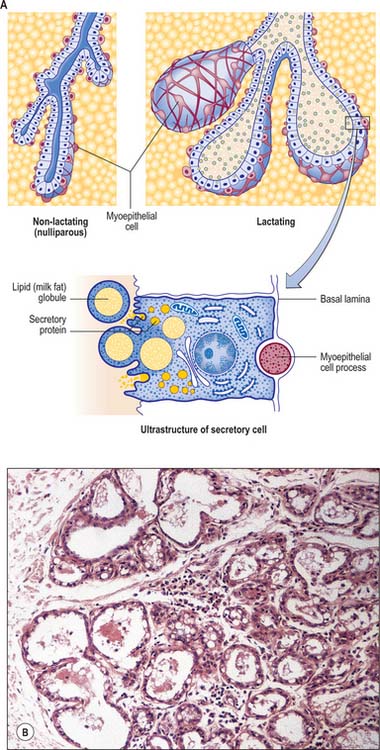
Fig. 54.26 Microstructure of breast epithelium. A, Note that the myoepithelial process is actually about half the relative size shown in the lower diagram. B, The peripheral part of a lactating breast lobule enclosed by a connective tissue septum (left). The alveoli are distended by milk secretion. Milk protein appears as eosinophilic material in the lumen and milk fat as pale cytoplasmic vacuoles in the flattened alveolar epithelium. Intralobular connective tissue between the alveoli contains a prominent lymphocytic infiltration, including plasma cells secreting IgA.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
Arteries
The breasts are supplied by branches of the axillary artery, the internal thoracic artery, and some intercostal arteries. The axillary artery supplies blood via the superior thoracic artery, the pectoral branches of the thoracoacromial artery, the lateral thoracic artery (via branches which curve around the lateral border of pectoralis major to supply the lateral aspect of the breast) and the subscapular artery. The internal thoracic artery supplies perforating branches to the anteromedial part of the breast. The second to fourth anterior intercostal arteries supply perforating branches more laterally in the anterior thorax: the second perforating artery is usually the largest, and supplies the upper region of the breast, and the nipple, areola and adjacent breast tissue.
Veins
Blood drains from the circular venous plexus around the areola and from the glandular tissue of the breast into the axillary, internal thoracic and intercostal veins via veins that accompany the corresponding arteries. Individual variation is common.
Lymphatic drainage
The lymphatic flow of the breast is of great clinical significance because metastatic dissemination occurs principally by the lymphatic routes. The dominant lymphatic drainage of the breast is derived from the dermal network. The breast lymphatics branch extensively and do not contain valves: lymphatic blockage through tumour occlusion may therefore result in reverse blood flow through the lymphatic channels. The direction of lymphatic flow within the breast parallels the major venous tributaries and enters the regional lymph nodes via the extensive periductal and perilobular network of lymphatic channels. Most of these lymphatics drain into the axillary group of regional lymph nodes either directly or through the retroareolar lymphatic plexus (see Fig. 46.28). Dermal lymphatics also penetrate pectoralis major to join channels that drain the deeper parenchymal tissues, and then follow the vascular channels to terminate in the subclavicular lymph nodes. Lymphatics from the left breast ultimately terminate in the thoracic duct and subsequently the left subclavian vein. On the right, the lymphatics ultimately drain into the right subclavian vein near its junction with the internal jugular vein. Part of the medial side of the right breast drains towards the internal thoracic group of lymph nodes. The internal thoracic chain may drain inferiorly via the superior and inferior epigastric lymphatic routes to the groin. Connecting lymphatics across the midline may provide access of lymphatic flow to the opposite axilla.
Axillary nodes receive more than 75% of the lymph from the breast (Fig. 54.21). There are 20–40 nodes, grouped artificially as pectoral (anterior), subscapular (posterior), central and apical. Surgically, the nodes are described in relation to pectoralis minor. Those lying below pectoralis minor are the low nodes (level 1), those behind the muscle are the middle group (level 2), while the nodes between the upper border of pectoralis minor and the lower border of the clavicle are the upper or apical nodes (level 3). There may be one or two other nodes between pectoralis minor and major; this interpectoral group of nodes are also known as Rotter’s nodes. Efferent vessels directly from the breast pass round the anterior axillary border through the axillary fascia to the pectoral lymph nodes; some may pass directly to the subscapular nodes. A few vessels pass from the superior part of the breast to the apical axillary nodes, sometimes interrupted by the infraclavicular nodes or by small, inconstant, interpectoral nodes. Most of the remainder drains to parasternal nodes from the medial and lateral parts of the breast; they accompany perforating branches of the internal thoracic artery. Lymphatic vessels occasionally follow lateral cutaneous branches of the posterior intercostal arteries to the intercostal nodes.
Axillary surgery in breast cancer
Axillary lymph node dissection may be performed because the presence of metastases within axillary lymph nodes has strong prognostic significance and might influence decisions on adjuvant therapy. However, axillary lymph node dissection can lead to chronic postoperative problems such as pain, seroma formation, reduced mobility of the arm, impaired sensation and lymphoedema The vessels and nerves have to be carefully identified at surgery as anatomical landmarks.
Lymphatic drainage in breast cancer and role of sentinel lymph node biopsy
Lymphatic mapping with sentinel lymph node biopsy has become an important technique in the staging of patients with early breast cancer. A radiolabelled colloid is injected into either the subareolar tissue of the index quadrant of the breast or the peritumoural tissue and intradermal tissue overlying the primary breast cancer. At the time of surgery, a vital blue dye is injected after general anaesthesia is established. The combination of radioisotope and dye provides the most accurate means of localizing the sentinel node (Rubio & Klimberg 2001, Tanis et al 2001). The sentinel node represents the first draining node of the axilla and is surgically removed for careful histopathological analysis to detect the presence of metastases. The sentinel node procedure seeks to identify this first draining node, and, if negative for cancer metastases, avoids more radical surgery in women who have no cancer spread, thus reducing morbidity associated with axillary dissection. In women who are found to have metastases to the axillary node, selective treatment to the axilla by completion axillary dissection or radiotherapy is offered. The majority of sentinel nodes are found in the low axilla within the level I group of nodes but can sometimes be found in higher echelon axillary nodes. This occurs in 5–10% of cases; the nodes are termed skip-metastases. Occasionally, the sentinel node is identified in an extra-axillary position, either within the breast parenchyma in an intramammary lymph node, the internal thoracic lymph node chain, or in the supraclavicular fossa.
INNERVATION
The breast is innervated by anterior and lateral branches of the fourth to sixth intercostal nerves, which carry sensory and sympathetic efferent fibres. The nipple is supplied from the anterior branch of the lateral cutaneous branch of T4 which forms an extensive plexus within the nipple; its sensory fibres terminate close to the epithelium as free endings, Meissner corpuscles and Merkel disc endings. These are essential in signalling suckling to the central nervous system. Secretory activities of the gland are largely controlled by ovarian and hypophysial hormones rather than by efferent motor fibres. The areola has fewer sensory endings.
MICROSTRUCTURE
The microstructure of breast tissue varies with age, time in the menstrual cycle, pregnancy and lactation. The following description relates to the mature, resting breast. For most of their lengths, the ducts are lined by columnar epithelium (Fig. 54.22). In the larger ducts, this is two cells thick, but, in the smaller ones, only a single layer of columnar or cuboidal cells is present. The bases of these cells are in close contact with numerous myoepithelial cells of ectodermal origin, similar to those of certain other glandular epithelia (see Figs 2.3, 54.26A). Myoepithelial cells are so numerous that they form a distinct layer surrounding the ducts and presumptive alveoli and give the epithelium a bilayered appearance.
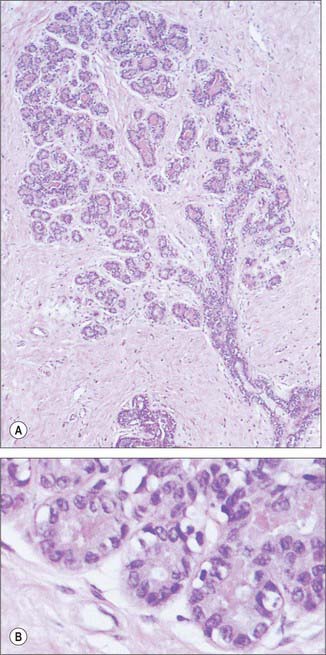
Fig. 54.22 A, A glandular lobule surrounded by collagenous interlobular connective tissue in the mature resting breast. A terminal duct (bottom right) branches extensively to terminate in rudimentary acini, which are shown at higher magnification in the lower panel (B).
(By permission from Young B, Heath JW 2000 Wheater’s Functional Histology. Edinburgh: Churchill Livingstone.)
Lactiferous ducts draining each lobe of the breast pass through the nipple and open onto its tip as 15–20 orifices. Near its orifice, each of these ducts is slightly expanded as a lactiferous sinus, which, in the lactating breast, is further dilated by the presence of milk. Each lactiferous duct is therefore connected to a system of ducts and lobules, surrounded by connective tissue stroma, collectively forming a lobe of the breast. Lobules consist of the portions of the glands that have secretory potential. Their structure varies according to hormonal status. In the mature resting breast, each lobule consists of a cluster of blind-ended, branched ductules whose termini lack terminal alveoli (acini), which are the sites of milk secretion in the lactating breast (see Fig. 54.26B). The stratified cuboidal lining is replaced by keratinized stratified squamous epithelium, continuous with the epidermis, close to the openings of the lactiferous ducts on the nipple. Shed squames may sometimes block the duct apertures in the non-pregnant breast.
Internally, the nipple is composed mostly of collagenous dense connective tissue and contains numerous elastic fibres which wrinkle the overlying skin. Deep to the nipple and areola, bundles of smooth muscle cells are arranged radially and circumferentially within the connective tissue. Their contraction, induced by cold or tactile stimuli (e.g. in suckling), causes erection of the nipple and wrinkling of the surrounding areola.
BREAST CANCER
Breast cancer is a common disease, particularly in postmenopausal women (see Fentiman 1993). Each year in the United Kingdom, there are approximately 40,000 new cases diagnosed and 14,000 deaths. Male breast cancers make up 1% of all mammary malignancies and may include tissue beyond the areolar boundary.
Breast cancers arise within the epithelia of lobules or ducts. As they increase in size and infiltrate the stroma they often lead to a fibrous tissue reaction. Breast lumps may be classified as benign or malignant masses. Malignant breast lumps may have the clinical signs of infiltrating adjacent structures, leading to a hard and irregular mass with skin-tethering, muscle fixation, skin infiltration or oedema of the overlying skin (peau d’orange). Standard radiological imaging investigations of the breast include mammography and ultrasonography. Mammography is useful in detecting the presence of malignant masses as a stellate opacity with architectural distortion of the surrounding parenchyma. Early stages of preinvasive breast cancer, ductal cancer in situ, may appear as microcalcification on the mammogram. An ultrasound scan of the breast is helpful to distinguish solid from cystic (or fluid-filled) masses, and can also aid in the distinction of breast cancer from benign lumps by the different attenuation characteristics of the ultrasound waves and blood flow patterns. Magnetic resonance imaging is also useful in diagnosis, particularly in women with younger, more dense breasts, achieving higher sensitivity of breast cancer detection but with lower specificity. A cytological diagnosis of a breast lump can be achieved using fine needle aspiration (FNA) to evaluate the cellular component of a lump. FNA is also useful to drain symptomatic breast cysts. A wide bore needle biopsy is a procedure performed under local anaesthetic to obtain several pieces of specimen for a histological diagnosis with the tissue architecture maintained. This permits distinction between in situ and invasive cancer and provides an indication of tumour subtype by evaluation of the pathological characteristics. Vacuum-assisted mammotome biopsies based on the wide bore needle enables some benign and indeterminate lesions to be excised for full histological analysis and in some patients can avoid the need for conventional open surgery.
If a breast lump has to be surgically removed, the incision should be based, whenever possible, in the relaxed skin tension lines, for the best cosmetic results. In women with sizeable malignant lesions where breast conservation surgery is to be attempted, the skin incision should be planned with consideration of the possible requirement of the need for a subsequent mastectomy if the margins of excision are incompletely excised by pathological criteria. Most women with single breast cancers up to 4 cm in diameter are treated by breast conservation rather than mastectomy. This is a combination of surgery (tumour excision and axillary lymph node sampling or clearance) together with external beam radiotherapy. Patients with larger tumours are treated by modified radical mastectomy with axillary lymph node clearance. During axillary dissection to clear the axillary lymph nodes, the nerve to serratus anterior, the thoracodorsal vessels, the nerve to latissimus dorsi, and the medial and lateral pectoral nerves are all identified and carefully preserved. The boundaries of the axillary dissection are the nerve to serratus anterior medially, the thoracodorsal pedicle laterally and the axillary vein superiorly (see Fig. 46.30). The posterior limit of the dissection is the ventral surface of subscapularis. The superomedial limit of a level I axillary dissection extends to the lateral border of pectoralis minor at the apex of the axilla, a level II dissection extends to the medial border of pectoralis minor, and a level III dissection extends beyond the medial border until it reaches the point where the axilla is limited by the first rib (the latter is easily distinguished by its flat lateral surface, easily palpable at surgery). Failure to preserve the nerve to serratus anterior will result in winging of the scapula. The intercostobrachial nerve is often sacrificed in an axillary lymph node clearance operation, and this may result in anaesthesia of a narrow strip of sensation in the upper medial border of the arm.
Reconstructive surgery for breast cancer disease
Breast reconstruction may be performed at the time of mastectomy for breast cancer, or at a later stage (Serletti & Moran 2000). During a mastectomy where an immediate breast reconstruction is planned, the glandular breast tissue is removed either through a conventional mastectomy skin incision or in association with preservation of the native breast skin, a form of mastectomy termed a skin-sparing mastectomy. Patient selection is important to minimize risks of breast cancer recurrence in the skin of the reconstructed breast mound or associated lymph nodes. In an implant-based immediate breast reconstruction, a tissue expander is placed beneath the submusculofascial plane consisting of pectoralis major, in continuity laterally under serratus anterior with the intervening fascia, and the abdominal fascia inferiorly. The lower fibres of the attachment of pectoralis major to the sixth rib need to be detached, otherwise the implant will be placed too high on the chest wall. The tissue expander has to stretch the potential space below this musculofascial plane to match the space created by the removed breast beneath the subcutaneous plane and the deep fascia overlying pectoralis major. The tissue expander is subsequently replaced by a silicone or saline breast implant.
The skin and volume component of the breast can also be replaced by the latissimus dorsi musculocutaneous flap with or without an underlying silicone or saline breast implant. Latissimus dorsi and an overlying paddle of skin is raised on its dominant vascular pedicle, namely the thoracodorsal artery and vein, which enter the muscle on its deep surface and send perforating branches through the muscle to the overlying skin. The flap is transferred in an arc from the back to the front of the chest and fashioned to make a new breast. An implant is usually required to provide additional volume replacement, in which case it is placed beneath the flap. The donor defect on the back is directly sutured and there is minimal functional disability following transfer of latissimus dorsi. In suitable women, subcutaneous fat harvested in conjunction with the latissimus dorsi muscle may contain sufficient material to avoid the need for an implant as an autologous tissue breast reconstruction.
The skin and volume component of the breast can be replaced by a pedicled transverse rectus abdominis musculocutaneous flap (TRAM flap). In a pedicled TRAM flap, rectus abdominis and a transverse ellipse of skin from the lower abdomen are raised on the superior epigastric artery, which enters the deep surface of the muscle below the costal cartilage. Women suitable for an abdominal-based procedure have a sufficient abdominal panniculus to form the donor tissue in order to recreate the breast mound without an implant. Microvascular surgical techniques now permit the free transfer of the lower abdominal panniculous skin and subcutaneous fat based upon the cutaneous supply of the deep inferior epigastric artery with minimal disruption to rectus abdominis. Cutaneous perforators near the level of the umbilicus pass to the skin in two rows (a medial and a lateral row). If the superior epigastric artery is used as the pedicle for the flap, the deep inferior epigastric artery is ligated and the flap is swung on the pedicle and tunnelled up into the chest where it is fashioned into a new breast. If the deep inferior epigastric artery is used as the pedicle, the superficial epigastric artery is divided and the flap is transferred as a free flap; the deep inferior epigastric artery and vein are anastomosed to recipient vessels either in the chest (usually the internal thoracic vessels, accessed by removing the third costal cartilage) or to the dominant anterior intercostal perforator in the second (or third) intercostal space. A deep inferior epigastric artery perforator flap (DIEP flap) can be raised by dissecting a single cutaneous perforator through rectus abdominus to its origin from the deep inferior epigastric artery, a procedure that obviates the need to sacrifice the muscle.
The advantage of the TRAM flap over the latissimus dorsi flap is that there is sufficient volume to reconstruct even a large breast without the need for an implant. The donor defect in the abdominal wall is sutured directly; where the muscle has been harvested in the pedicled TRAM flap, a mesh may be incorporated into the repair of the rectus sheath to reduce the potential risk of muscle weakness caused by surgical disruption of rectus abdominis, which could produce a bulge of the abdominal contents or a hernia.
DEVELOPMENT
The epithelial/mesenchymal interactions that will give rise to the glandular tissue of the breast, in both sexes, can first be seen at about the fifth or sixth week, when two ventral bands of thickened ectoderm, the mammary ridges or milk lines, extend from the axilla to the inguinal region. Usually, invagination of the thoracic mammary bud occurs by day 49, and the remaining mammary line involutes.
The thoracic ectodermal ingrowths branch into 15–20 solid buds of ectoderm which will become the lactiferous ducts and their associated lobes of alveoli in the fully formed gland. They are surrounded by somatopleuric mesenchyme which forms the connective tissue, fat and vasculature which is invaded by the mammary nerves. Continued cell proliferation, elongation and further branching produces the alveoli and defines the duct system. Nipple formation begins at day 56, primitive ducts (mammary sprouts) develop at 84 days and canalization occurs at about the 150th day. During the last 2 months of gestation the ducts become canalized; the epidermis at the point of original development of the gland forms a small mammary pit, into which the lactiferous tubules open (Fig. 54.23). Perinatally the nipple is formed by mesenchymal proliferation. Should this process fail, the ducts open into shallow pits. Rarely, the nipple may not develop (athelia), a phenomenon that occurs more commonly in accessory breast tissue.
At birth the breasts have reached a similar developmental stage in both sexes: the combination of fetal prolactin and maternal oestrogen may give rise to transient hyperplasia and secretion of ‘witch’s milk’. In males, the breasts normally remain undeveloped, whereas in females at puberty, in late pregnancy and during the period of lactation, they undergo further, hormone-dependent, developmental changes. The female breast is a unique organ in that it remains in a rudimentary (i.e. fetal) form until puberty, at which time its development continues under the influence of sex hormones. The adult form is reached in late adolescence, i.e. the breast is then able to function as a milk-producing organ. At menopause, the breast involutes into a predominantly fatty organ with minimal glandular parenchyma.
Accessory breast tissue and nipples
Polymastia (supernumerary breasts) and polythelia (supernumerary nipples) may develop in males and females anywhere along the length of the mammary ridges (milk lines; Fig. 54.24). Conversely, breast tissue may not develop at all (amastia) or there may be nipple development but no breast tissue (amazia). Supernumerary breast development occurs in most cases in the thoracic region, just inferior to the normal breast (90%), but may also occur in the axillary (5%) and abdominal regions (5%). Polythelia occurs along the same mammary line but no underlying glandular tissue develops. About 1% of the female population has this condition, but it is more common in males, where the accessory nipple may be mistaken for a mole.
Congenital inversion of nipple
Congenital inversion of the nipples occurs in about 3% of the female population. The condition is almost always bilateral. The majority of the cases are umbilicated, i.e. the nipple can be easily pulled forward from its depressed position underneath the areolar surface. The condition is thought to be due to failure of proliferation of the mesenchymal tissue, which fails to push the nipple out. The remaining cases are due to invagination of the nipple. Apart from psychological implications, inversion of the nipple may cause recurrent mastitis and difficulty with breast feeding. The abnormality may be corrected surgically.
AGE-RELATED CHANGES
Prepuberty
The neonatal breast contains lactiferous ducts but no alveoli. Until puberty, little branching of the ducts occurs, and any slight mammary enlargement reflects the growth of fibrous stroma and fat.
Puberty
In the postpubertal female, the ducts, stimulated by ovarian oestrogens, become branched. The ends of the branches form solid, spheroidal masses of granular polyhedral cells, the potential alveoli. Oestrogens also promote adipocyte differentiation from mesenchymal cells in the interlobar stroma: breast enlargement at puberty is largely a consequence of lipid accumulation by these adipocytes.
From puberty onwards, externally recognizable breast development (thelarche) can be divided into five separate phases (Fig. 54.25): elevation of the breast bud (phase I); glandular subareolar tissue is present and both nipple and breast project from the chest wall as a single mass (phase II); the areola increases in diameter and becomes pigmented, and there is proliferation of palpable breast tissue (phase III); further pigmentation and enlargement occurs in the areola, so that the nipple and areola form a secondary mass anterior to the main part of the breast (phase IV); a smooth contour to the breast develops (phase V).
Changes during the menstrual cycle
Changes occur in the breast tissues in the menstrual cycle. In the follicular phase (days 3–14), the stroma becomes less dense. Various changes including luminal expansion take place in the ducts; there are occasional mitoses but no secretion. In the luteal phase (days 15–28), there is a progressive increase in stromal density and the ducts have an open lumen that contains secretion, associated with flattening of the epithelial cells. Cell proliferation is maximal on day 26 and thereafter the ductal system undergoes reduction; epithelial cell apoptosis is greatest on day 28 of the cycle. There are also changes in blood flow, which are greatest at midcycle, and an increase in the water content of the stroma in the second half of the menstrual cycle.
Postmenopausal
Progressive atrophy of lobules and ducts occurs after the menopause, and there is fatty replacement of glandular breast tissue. A few ducts may remain. The stroma becomes much less cellular and collagenous fibres decrease. The amount of adipose tissue varies widely between individuals, and the breast may return to a condition similar to the prepubertal state.
CHANGES ASSOCIATED WITH PREGNANCY AND LACTATION
Pregnancy
As the output of oestrogen and progesterone produced first by the corpus luteum and later by the placenta rises during pregnancy, the intralobular ductal epithelium proliferates and the cells increase in size: the number and length of the ductal branches therefore increase. Alveoli develop at their termini and expand as their cells and lumina fill with newly synthesized and secreted milk. The myoepithelial cells, which are initially spindle-shaped, become highly branched stellate cells, especially around the alveoli. Adjacent myoepithelial cells intermesh to form a basket-like network around the alveoli and ducts, interposed between the basal lamina and the luminal cells. Their cytoplasm contains actin and myosin filaments and they are contractile. There is a concomitant reduction in adipose tissue in the stroma. The numbers of lymphocytes, including plasma cells, and eosinophils increase greatly. Blood flow through the breast increases.
Secretory activity in the alveolar cells rises progressively in the latter half of pregnancy. In late pregnancy, and for a few days after parturition, their product is different from later milk and is known as colostrum, which is low in lipid but rich in protein and immunoglobulins. Colostrum confers a measure of passive immunity to the neonatal alimentary tract; it also has laxative properties. Proliferation of the glandular breast parenchyma results in an overall increase in breast size through gestation.
Lactation
True milk secretion begins a few days after parturition as a result of a reduction in circulating oestrogen and progesterone, a change which appears to stimulate production of prolactin by the anterior hypophysis.
Milk distends the alveoli so that the cells flatten as secretion increases (Figs 54.20B, 54.26B,C). The alveolar cell cytoplasm accumulates membrane-bound granules of casein and other milk proteins, and these are released from the apical plasma membrane by membrane fusion (merocrine secretion; see Ch. 2). Lipid vacuoles are formed directly in the apical cytoplasm as small lipid droplets which fuse with each other to create large ‘milk vacuoles’ up to 10 μm across, that frequently protrude from the cell surface. These are released as intact lipid droplets with a thin surround of apical plasma membrane and adjacent cytoplasm (apocrine secretion). On hormonal stimulation by oxytocin, myoepithelial cells contract to expel alveolar secretions into the ductal system in readiness for suckling.
After the onset of lactation there is a gradual reduction in the numbers of lymphocytes and eosinophils in the stroma, although plasma cells continue to synthesize IgA for secretion into the milk. Alveolar cells take up IgA synthesized by adjacent plasma cells by endocytosis at their basal surfaces and secrete it apically, as dimers complexed to epithelial secretory component.
Postlactation
When lactation ceases, which may be as long as 3½ years, or even longer if frequent suckling is maintained, the secretory tissue undergoes some involution, but the ducts and alveoli never return completely to the pre-pregnant state. Two major processes are responsible for the regression of the alveolar–ductal system: a reduction in epithelial cell size and a reduction in cell numbers mediated via apoptosis (see Ch. 1). Gradually the breast tissue reverts to its resting state. If another pregnancy occurs, the resting glandular tissue is reactivated, and the process outlined above recurs. Up to the age of 50 years, increasing amounts of elastic tissue tend to be laid down around vessels and ducts (elastosis), and also in the stroma. Elastosis does not normally continue into later life.
MALE BREAST
The male breast remains rudimentary throughout life. It is formed of small ducts (without lobules or alveoli) or solid cellular cords and a little supporting fibroadipose tissue (see Ellis et al 1993). Slight temporary enlargement may occur in the newborn, reflecting the influence of maternal hormones, and again at puberty. The areola is well developed, although limited in area, and the nipple is relatively small. It is usually stated that the ducts do not extend beyond the areola in a male breast, but glandular tissue can be more extensive.
Gynaecomastia
Gynaecomastia is a benign proliferation of subareolar breast tissue or excessive growth of breast tissue. It is usually bilateral but may be unilateral, and is commonly associated with pain or tenderness, which is thought to be due to accumulation of fluid in the glandular ducts. Histological changes are fibrosis, followed by hyalinization. It is sometimes due to a biochemical imbalance in the ratio of free oestrogens, androgens and sex hormone-binding globulin. Hence it is commonly seen after antiandrogen therapy for conditions such as prostatic cancer, but other drugs such as spironolactone, cimetidine, anabolic steroids and cannabinoids have been implicated. Gynaecomastia may have a hormonal basis during puberty and senescence, or in liver failure where normal hepatic function is associated with sex steroid hormone metabolism. However, the majority of cases have no known cause and are termed idiopathic gynaecomastia.
SURGICAL ACCESS TO THORACIC VISCERA
Thoracocentesis (pleural aspiration)
Thoracocentesis or pleural aspiration is an essential step in the assessment of pleural effusions. A chest radiograph will confirm the location and extent of the effusion and clinical examination will identify the best position for aspiration: the posterior midscapular line is a common site. The skin of the desired interspace is cleaned and anaesthetized, and the aspiration needle is inserted at the lower margin of the interspace. The needle is not inserted in the middle of the interspace because the intercostal vessels run along the middle of the interspace posteriorly, and from the axilla forwards onto the anterior chest wall they are protected only by the lower border of the rib. After appropriate local analgesia has been applied, the needle is carefully advanced in a perpendicular direction in the lower portion of the interspace until it enters the pleural space. More complex or small effusions should be aspirated under ultrasound guidance.
Needle thoracocentesis is performed in patients in whom a life-threatening tension pneumothorax is suspected. A needle is inserted into the second intercostal space in the midclavicular line on the side of the tension pneumothorax, with the patient in an upright position. A sudden escape of air is heard when the needle enters the parietal pleura. A chest tube must be inserted after this procedure.
The insertion site for a chest drain is usually the fifth intercostal space, just anterior to the midaxillary line on the affected side. A 2 cm horizontal incision is followed by blunt dissection through the subcutaneous tissues to the top of the rib. The parietal pleura is punctured with the tip of a clamp and a gloved finger inserted into the pleural space to free up any adhesions. The chest drain (thoracostomy tube) is then inserted into the pleural space and attached to an underwater sealed container placed below the level of the lungs: the water level rises and falls in the tube with ventilation.
Pericardiocentesis is performed to aspirate a pericardial effusion or, in an emergency, to decompress a cardiac tamponade, where pressure from blood in the pericardial space prevents the heart chambers from filling during the cardiac cycle, and seriously impairs cardiac output.
Pericardial puncture can be performed in either the fifth or sixth left intercostal space near the sternum (to avoid the internal thoracic artery), or at the left costoxiphoid angle. The needle is passed 1–2 cm to the left of the costoxiphoid angle at 45° to the skin, and then up and backwards towards the tip of the scapula until it enters the pericardial sac.
Placement of electrocardiograph leads
The 12-lead electrocardiograph (ECG) provides three-dimensional information on the electrical activity of the heart. The limb leads provide information about the electrical activity in the frontal plane. They are placed on the left and right wrists, and the left foot, with the right foot acting as a neutral grounding point. The chest leads provide information about the electrical activity in the horizontal plane. They are placed as follows: V1, right fourth intercostal space, parasternal position; V2, left fourth intercostal space, parasternal position; V3, midpoint of V2 and V4 on the left; V4, fifth intercostal space, midclavicular line on the left; V5, fifth intercostal space, anterior axillary line on the left; V6, fifth intercostal space, midaxillary line on the left.
Thoracotomy incisions may be posterolateral, anterolateral or involve a transverse thoracosternotomy.
A posterolateral incision is most commonly used in thoracic surgery for unilateral pulmonary resections, bullectomy, unilateral lung volume reduction surgery, chest wall resection and oesophageal surgery (Fry 2000). The patient is placed in a lateral decubitus position with adequate support of the elbow, axilla and knee with padding. The standard approach is via an incision from the anterior axillary line which curves about 4 cm below the tip of the scapula and then vertically between the posterior midline and medial edge of the scapula. The incision is usually extended to the level of the spine of scapula. Overall, the incision forms an S-shape in the fifth intercostal space. The sixth or seventh intercostal space is used in oesophageal surgery.
The lower portions of trapezius and latissimus dorsi are divided. Serratus anterior is retracted, and may be divided in a high thoracotomy. The costal muscle and pleura are dissected along the inferior margin of the intercostal space to avoid damaging the neurovascular bundle. A small section of rib is removed at the costovertebral angle to reduce the risk of fracture, particularly in patients older than 40 years. This technique provides good access to the thoracic contents; the main problem is postoperative pain as a consequence of intraoperative musculoskeletal traction.
Using an anterolateral approach, the patient is placed in the supine position with their arms by their sides. A roll is placed vertically under the back and hips so as to raise the operative side by approximately 45°. The incision is from the midaxillary line over the fifth intercostal space along the inframammary fold, and curves upwards parasternally. The pectoral muscles are divided, and subsequent access to the thorax is similar to that used in the posterolateral approach. However, access is limited, and may be improved by dividing costal cartilages.
The transverse thoracosternotomy is known as the ‘clam shell’ incision. It provides excellent exposure to both sides of the chest and is therefore used in bilateral lung transplantation and in lung volume reduction surgery with bilateral lung resections. The patient is placed in the supine position with a roll vertically along the upper thoracic spine. Bilateral anterolateral incisions are made in the inframammary fold, and the sternum is transected. This allows the upper portion of the thorax to be displaced upwards with a rib-spreader, hence the name clam shell. The main disadvantage of the clam shell procedure is the need to transect the sternum: even after careful repair with sternal wires, there is a risk of sternal instability.
Sternotomy is commonly needed in cardiac surgery. The patient is placed in the supine position with both arms extended by the side. A vertical incision is made in the midline from the suprasternal notch to a point just below the xiphoid process. The tissues around the manubrium and the xiphoid process are mobilized. The pectoral fascia in the midline is incised and the sternum is split and its two edges retracted. The sternum is closed using interosseous wire sutures.
The patient is placed in the lateral decubitus position, with arms abducted at 90° and supported on an arm rest. The incision is based along the desired intercostal space, which, for upper thoracic lesions, is the second or third space. Latissimus dorsi is elevated and retracted, whereas serratus anterior is divided in the direction of its fibres. The anterior aspect of serratus anterior is divided to expose the intercostal muscles, which are divided in turn. The overall size of the incision is limited and it provides good access to the upper thorax. Postoperative pain is less than with some other approaches, but the long thoracic nerve (nerve of Bell) may be damaged if serratus anterior is divided too posteriorly.
Occasionally, video-assisted thoracoscopic surgery is required to assess the mediastinum. The thoracoscope is usually introduced via the fifth intercostal space in the midclavicular line, with additional ports at the third and sixth intercostal spaces to assess the anterior mediastinum. To assess the posterior mediastinum, the thoracoscope is inserted into the seventh intercostal space in the midclavicular line.
Ellis H, Colborn GL, Skandalakis JE. Surgical embryology and anatomy of the breast and its related anatomic structures. Surg Clin North Am. 1993;73:611-632.
Fentiman IS. Detection and Treatment of Early Breast Cancer. London: Martin Dunitz, 1993.
Fry WA. Thoracic incisions. Shields TW, LoCicero JIII, Ponn RB. General Thoracic Surgery. 5th edn.. Philadelphia: Lippincott Williams & Wilkins; 2000:367-374.
Kurihara Y, Yakushiji YK, Matsumoto J, Ishikawa T, Hirata K. The ribs: anatomic and radiologic considerations. Radiographics. 1999;19:105-119.
Includes some chest wall and ribcage abnormalities..
Rubio IT, Klimberg S. Techniques of sentinel lymph node biopsy. Semin Surg Oncol. 2001;20:214-223.
Serletti JM, Moran SL. Microvascular reconstruction of the breast. Semin Surg Oncol. 2000;19:264-271.
Tanis PJ, Nieweg OE, Valdes Olmos RA, Kroon BB. Anatomy and physiology of lymphatic drainage of the breast from the perspective of sentinel node biopsy. J Am Coll Surg. 2001;192:399-409.
Yap LH, Whiten SC, Forster A, Stevenson JH. The anatomical and neurophysiological basis of the sensate free TRAM and DIEP flaps. Br J Plast Surg. 2002;55:35-45.