CHAPTER 28 Neck
The neck extends from the base of the cranium and the inferior border of the mandible to the thoracic inlet.
SKIN
The skin in the neck is normally under tension. The direction in which this is greatest varies regionally; in the living face these lines often coincide with wrinkle lines. Lines of greatest tension have been termed ‘relaxed skin tension lines’, and surgical incisions made along these lines are said to heal with minimal postoperative scarring. Susceptible individuals are more prone to keloid scarring in the head and neck region.
Cutaneous vascular supply and lymphatic drainage
The blood vessels supplying the skin of the neck are derived principally from the facial, occipital, posterior auricular and subclavian arteries. They form a rich network within platysma and in the subdermal plexus, and account for the viability of the various skin flaps raised during block dissection of the neck, irrespective of whether they include platysma: the latter is usually elevated in extensive incisions.
The anterior cervical skin is supplied mainly by the superior thyroid artery and the transverse cervical branch of the subclavian artery. The posterior skin is supplied by branches from the occipital artery and the deep cervical and transverse cervical branches of the subclavian artery. The superior skin is supplied by the occipital artery and its upper sternocleidomastoid branch, and the submandibular and submental branches of the facial artery. Inferiorly, the skin is supplied by the transverse cervical and/or suprascapular branches of the subclavian artery.
The pattern of venous drainage of the skin of the neck mirrors the arterial supply: the veins drain into the jugular and facial veins.
Many lymphatic vessels draining the superficial cervical tissues skirt the borders of sternocleidomastoid to reach the superior or inferior deep cervical nodes. Some pass over sternocleidomastoid and the posterior triangle to drain into the superficial cervical and occipital nodes (see Fig. 28.15). Lymph from the superior region of the anterior triangle drains to the submandibular and submental nodes. Vessels from the anterior cervical skin inferior to the hyoid bone pass to the anterior cervical lymph nodes near the anterior jugular veins, and their efferents go to the deep cervical nodes of both sides, including the infrahyoid, prelaryngeal and pretracheal groups. An anterior cervical node often occupies the suprasternal space.
Cutaneous innervation
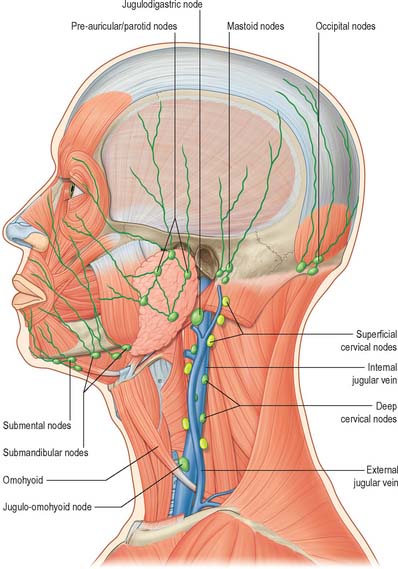
The cervical skin is innervated by branches of cervical spinal nerves, via both dorsal and ventral rami (see Fig. 43.6). The dorsal rami supply skin over the back of the neck and scalp, and the ventral rami supply skin covering the lateral and anterior portions of the neck, and the angle of the mandible (Fig. 28.1). The dorsal rami of the first, sixth, seventh and eighth cervical nerves have no cutaneous distribution in the neck. The greater occipital nerve mainly supplies the scalp; it comes from the medial branch of the dorsal ramus of the second cervical nerve. The medial branches of the dorsal rami of the third, fourth and fifth cervical nerves pierce trapezius to supply skin over the back of the neck sequentially. The ventral rami of the second, third and fourth cervical nerves supply named cutaneous branches (the lesser occipital, great auricular, transverse cutaneous and supraclavicular nerves), via the cervical plexus (Fig. 28.1) (see p. 456 for details of the motor branches of the cervical plexus).
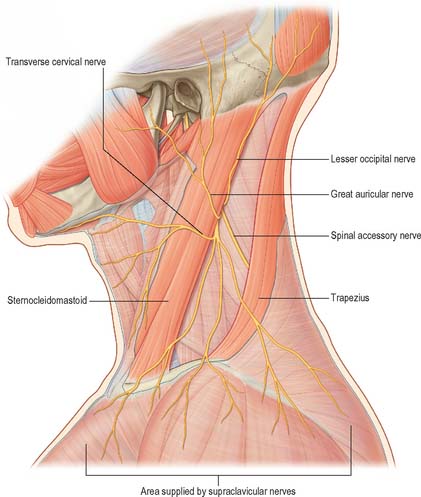
Fig. 28.1 The cutaneous branches of the cervical plexus. The spinal part of the accessory nerve that supplies trapezius is also shown as it crosses the posterior triangle. Note that the interval between the upper attachments of sternocleidomastoid and trapezius is not normally as extensive as shown here.
(Adapted from Drake, Vogl and Mitchell 2005.)
Lesser occipital nerve
The lesser occipital nerve is derived mainly from the second cervical nerve (although fibres from the third cervical nerve may sometimes contribute). It passes first anterior to the plane of the spinal accessory nerve before winding around it and becoming anterior to it. It next ascends along the posterior margin of sternocleidomastoid. Near the cranium it perforates the deep fascia and passes up onto the scalp behind the auricle to supply the skin and connect with the great auricular and greater occipital nerves and the auricular branch of the facial nerve. Its auricular branch supplies the skin on the upper third of the medial aspect of the auricle and connects with the posterior branch of the great auricular nerve. The auricular branch is occasionally derived from the greater occipital nerve. It has been suggested that compression or stretching of the lesser occipital nerve contributes to cervicogenic headache.
Great auricular nerve
The great auricular nerve is the largest ascending branch of the cervical plexus. It arises from the second and third cervical rami, encircles the posterior border of sternocleidomastoid, perforates the deep fascia and ascends on the muscle beneath platysma with the external jugular vein. On reaching the parotid gland, it divides into anterior and posterior branches. The anterior branch is distributed to the facial skin over the parotid gland and connects in the gland with the facial nerve. This cross innervation between somatic sensory supply (great auricular) and parasympathetic secretomotor fibres to the parotid is considered to be part of the anatomical basis for the phenomenon of gustatory sweating (Frey’s syndrome) seen after parotid surgery, when the nerve is at risk of injury. The posterior branch supplies the skin over the mastoid process and on the back of the auricle (except its upper part); a filament pierces the auricle to reach the lateral surface where it is distributed to the lobule and concha. The posterior branch communicates with the lesser occipital nerve, the auricular branch of the vagus and the posterior auricular branch of the facial nerve.
Transverse cervical cutaneous nerve
The transverse cervical cutaneous nerve arises from the second and third cervical rami. It curves round the posterior border of sternocleidomastoid near its midpoint and runs obliquely forwards, deep to the external jugular vein, to the anterior border of the muscle. It perforates the deep cervical fascia, and divides under platysma into ascending and descending branches that are distributed to the anterolateral areas of the neck. The ascending branches ascend to the submandibular region, forming a plexus with the cervical branch of the facial nerve beneath platysma. Some branches pierce platysma and are distributed to the skin of the upper anterior areas of the neck. The descending branches pierce platysma and are distributed anterolaterally to the skin of the neck, as low as the sternum.
Supraclavicular nerves
The supraclavicular nerves arise from a common trunk formed from rami from the third and fourth cervical nerves and emerge at the posterior border of sternocleidomastoid. Descending under platysma and the deep cervical fascia, the trunk divides into medial, intermediate and lateral (posterior) branches, which diverge to pierce the deep fascia a little above the clavicle. The medial supraclavicular nerves run inferomedially across the external jugular vein and the clavicular and sternal heads of sternocleidomastoid to supply the skin as far as the midline and as low as the second rib. They also supply the sternoclavicular joint. The intermediate supraclavicular nerves cross the clavicle to supply the skin over pectoralis major and deltoid down to the level of the second rib, next to the area of supply of the second thoracic nerve. Overlap between these nerves is minimal. The lateral supraclavicular nerves descend superficially across trapezius and the acromion, supplying the skin of the upper and posterior parts of the shoulder.
BONES, JOINTS AND CARTILAGES
The bones and cartilages of the neck are the cervical vertebrae and the hyoid bone, and the cartilages of the upper respiratory tract, including the larynx. The cervical vertebrae, occipital bone and the atlantooccipital and atlanto-axial joints are described in Chapter 42, and the laryngeal cartilages are described in Chapter 34.
HYOID BONE
The U-shaped hyoid bone (Fig. 28.2) is suspended from the tips of the styloid processes by the stylohyoid ligaments. It has a body, two greater and two lesser horns, or cornua.
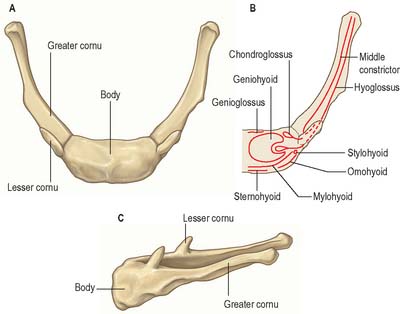
Fig. 28.2 The hyoid bone: A, B, anterosuperior aspect; C, lateral aspect. B shows the positions of muscular attachments.
The body is irregular, elongated and quadrilateral. Its anterior surface is convex, faces anterosuperiorly, and is crossed by a transverse ridge with a slight downward convexity. A vertical median ridge often bisects the upper part of the body, but rarely extends to the lower part. The posterior surface is smooth, concave, faces posteroinferiorly, and is separated from the epiglottis by the thyrohyoid membrane and loose areolar tissue. There is a bursa between the hyoid bone and the membrane.
Geniohyoid is attached to most of the anterior surface of the body, above and below the transverse ridge; the medial part of hyoglossus invades the lateral geniohyoid area. The lower anterior surface gives attachment to mylohyoid, the line of attachment lying above sternohyoid medially and omohyoid laterally. The lowest fibres of genioglossus, the hyoepiglottic ligament and (most posteriorly) the thyrohyoid membrane are all attached to the rounded superior border. Sternohyoid is attached to the inferior border medially and omohyoid is attached laterally. Occasionally the medial fibres of thyrohyoid and, when present, of levator glandulae thyroideae, are attached along the inferior border.
In early life, the greater cornua are connected to the body by cartilage, but after middle age they are usually united by bone. They project backwards (curving posterolaterally) from the lateral ends of the body. They are horizontally flattened, taper posteriorly, and each ends in a tubercle. When the throat is gripped between finger and thumb above the thyroid cartilage, the greater cornua can be identified and the bone can be moved from side to side.
The middle pharyngeal constrictor and, more laterally (i.e. superficially), hyoglossus, are attached along the whole length of the upper surface of each greater cornu. Stylohyoid is attached near the junction of the cornu with the body. The fibrous loop for the digastric tendon is attached lateral and a little posterior to hyoglossus. The thyrohyoid membrane is attached to the medial border and thyrohyoid is attached to the lateral border. The oblique inferior surface is separated from the thyrohyoid membrane by fibroareolar tissue.
The lesser cornua are two small conical projections at the junctions of the body and greater cornua. At its base, each is connected to the body by fibrous tissue and occasionally to the greater cornu by a synovial joint which occasionally becomes ankylosed.
The middle pharyngeal constrictors are attached to the posterior and lateral aspects of the lesser cornua. The stylohyoid ligaments are attached to their apices and are often partly calcified, and the chondroglossi are attached to the medial aspects of their bases.
The hyoid bone develops from cartilages of the second and third pharyngeal arches, the lesser cornua from the second, the greater cornua from the third and the body from the fused ventral ends of both. Chondrification begins in the fifth fetal week in these elements, and is completed in the third and fourth months. Ossification proceeds from six centres, i.e. a pair for the body and one for each cornu. Ossification begins in the greater cornua towards the end of intrauterine life, in the body shortly before or after birth, and in the lesser cornua around puberty. The greater cornual apices remain cartilaginous until the third decade and epiphyses may occur here. They fuse with the body. Synovial joints between the greater and lesser cornua may be obliterated by ossification in later decades.
TRIANGLES OF THE NECK
Anterolaterally the neck appears as a somewhat quadrilateral area, limited superiorly by the base of the mandible and a line continued from the angle of the mandible to the mastoid process, inferiorly by the upper border of the clavicle, anteriorly by the anterior median line, and posteriorly by the anterior margin of trapezius. This quadrilateral area can be further divided into anterior and posterior triangles by sternocleidomastoid, which passes obliquely from the sternum and clavicle to the mastoid process and occipital bone (Fig. 28.3). It is true that these triangles and their subdivisions are somewhat arbitrary, because many major structures – arteries, veins, lymphatics, nerves, and some viscera – transgress their boundaries without interruption, nevertheless they have a topographical value in description. Moreover, some of their subdivisions are easily identified by inspection and palpation and provide invaluable assistance in surface anatomical and clinical examination.
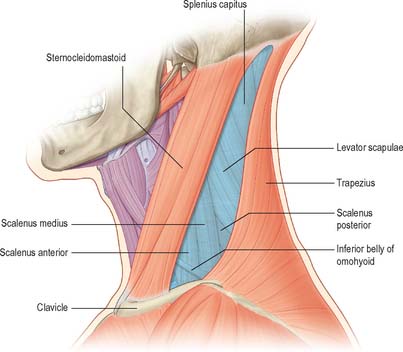
Fig. 28.3 The anterior and posterior triangles of the neck, left lateral aspect. See note in caption for Fig. 28.1
(Adapted from Drake, Vogl and Mitchell 2005.)
ANTERIOR TRIANGLE OF THE NECK
The anterior triangle of the neck is bounded anteriorly by the median line of the neck and posteriorly by the anterior margin of sternocleidomastoid. Its base is the inferior border of the mandible and its projection to the mastoid process, and its apex is at the manubrium sterni. It can be subdivided into suprahyoid and infrahyoid areas above and below the hyoid bone, and into digastric, submental, muscular and carotid triangles by the passage of digastric and omohyoid across the anterior triangle (see Fig. 28.5).
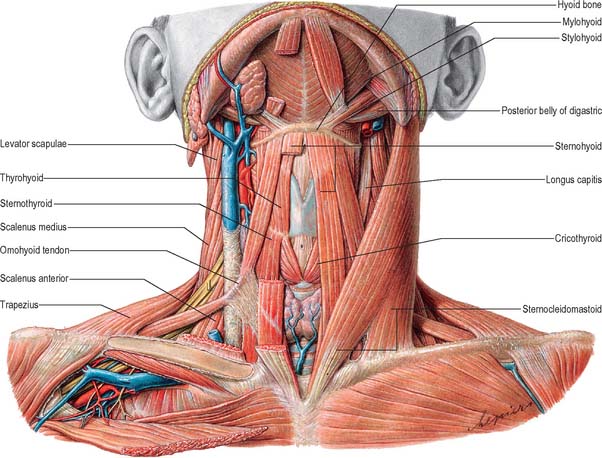
Fig. 28.5 Muscles of the neck: note that the head is slightly extended in order to expose the suprahyoid muscles.
(From Sobotta 2006.)
Digastric triangle
The digastric triangle is bordered above by the base of the mandible and its projection to the mastoid process, posteroinferiorly by the posterior belly of digastric and by stylohyoid, and anteroinferiorly by the anterior belly of digastric. It is covered by the skin, superficial fascia, platysma and deep fascia, which contain branches of the facial and transverse cutaneous cervical nerves. Its floor is formed by mylohyoid and hyoglossus. The anterior region of the digastric triangle contains the submandibular gland, which has the facial vein superficial to it and the facial artery deep to it. The submental and mylohyoid arteries and nerves lie on mylohyoid. The submandibular lymph nodes are variably related to the submandibular gland. The posterior region of the digastric triangle contains the lower part of the parotid gland. The external carotid artery, passing deep to stylohyoid, curves above the muscle, and overlaps its superficial surface as it ascends deep to the parotid gland before entering it. The internal carotid artery, internal jugular vein and vagus nerve lie deeper and are separated from the external carotid artery by styloglossus, stylopharyngeus and the glossopharyngeal nerve.
Submental triangle
The single submental triangle is demarcated by the anterior bellies of both digastric muscles. Its apex is at the chin, its base is the body of the hyoid bone and its floor is formed by both mylohyoid muscles. It contains lymph nodes and small veins that unite to form the anterior jugular vein. The structures within the digastric and submental triangles are described in more detail with the floor of the mouth (on p. 501).
Muscular triangle
The muscular triangle is bounded anteriorly by the median line of the neck from the hyoid bone to the sternum, inferoposteriorly by the anterior margin of sternocleidomastoid and posterosuperiorly by the superior belly of omohyoid. The triangle contains omohyoid, sternohyoid, sternothyroid and thyrohyoid.
Carotid triangle
The carotid triangle is limited posteriorly by sternocleidomastoid, anteroinferiorly by the superior belly of omohyoid and superiorly by stylohyoid and the posterior belly of digastric. In the living (except the obese) the triangle is usually a small visible triangular depression, sometimes best seen with the head and cervical vertebral column slightly extended and the head contralaterally rotated. The carotid triangle is covered by the skin, superficial fascia, platysma and deep fascia containing branches of the facial and cutaneous cervical nerves. The hyoid bone forms its anterior angle and adjacent floor and can be located on simple inspection, verified by palpation. Parts of thyrohyoid, hyoglossus and inferior and middle pharyngeal constrictor muscles form its floor. The carotid triangle contains the upper part of the common carotid artery and its division into external and internal carotid arteries. Overlapped by the anterior margin of sternocleidomastoid, the external carotid artery is first anteromedial, then anterior to the internal carotid artery. Branches of the external carotid artery are encountered in the carotid triangle. Thus the superior thyroid artery runs anteroinferiorly, the lingual artery anteriorly with a characteristic upward loop, the facial artery anterosuperiorly, the occipital artery posterosuperiorly and the ascending pharyngeal artery medial to the internal carotid artery. Arterial pulsation greets the examining finger. The superior thyroid, lingual, facial, ascending pharyngeal and sometimes the occipital, veins, correspond to the branches of the external carotid artery, and all drain into the internal jugular vein. The hypoglossal nerve crosses the external and internal carotid arteries. It curves round the origin of the lower sternocleidomastoid branch of the occipital artery, and at this point the superior root of the ansa cervicalis leaves it to descend anteriorly in the carotid sheath. The internal laryngeal nerve and, below it, the external laryngeal nerve, lie medial to the external carotid artery below the hyoid bone. Many structures in this region, such as all or part of the internal jugular vein, associated deep cervical lymph nodes, and the vagus nerve, may be variably obscured by sternocleidomastoid, and, pedantically, are thus ‘outside the triangle’.
POSTERIOR TRIANGLE OF THE NECK
The posterior triangle is delimited anteriorly by the posterior edge of sternocleidomastoid, posteriorly by the anterior edge of trapezius, and inferiorly by the middle third of the clavicle (Fig. 28.3). Its apex is between the attachments of sternocleidomastoid and trapezius to the occiput and is often blunted, so that the ‘triangle’ becomes quadrilateral. The roof of the posterior triangle is formed by the investing layer of the deep cervical fascia. The floor of the triangle is formed by the prevertebral fascia overlying splenius capitis, levator scapulae and the scalene muscles. It is crossed, approximately 2.5 cm above the clavicle, by the inferior belly of omohyoid, which subdivides it into occipital and supraclavicular triangles. The contents of the posterior triangle include fat, lymph nodes (level V – see later), spinal accessory nerve, cutaneous branches of the cervical plexus, inferior belly of omohyoid, branches of the thyrocervical trunk (transverse cervical and suprascapular arteries), the third part of the subclavian artery, and the external jugular vein. The anterior and lateral groups of prevertebral muscles form the floor of the posterior triangle.
Occipital triangle
The occipital triangle constitutes the upper and larger part of the posterior triangle, with which it shares the same borders, except that inferiorly it is limited by the inferior belly of omohyoid. Its floor, from above down, is formed by splenius capitis, levator scapulae, and scaleni medius and posterior; semispinalis capitis occasionally appears at the apex. The triangle is covered by skin, superficial and deep fasciae and inferiorly by platysma. The spinal accessory nerve pierces sternocleidomastoid and crosses levator scapulae obliquely downwards and backwards to reach the deep surface of trapezius. The surface marking of its course is in a line from the junction of the superior one-third and inferior two-thirds of sternocleidomastoid, to the junction of the inferior one-third and superior two-thirds of trapezius. Cutaneous and muscular branches of the cervical plexus emerge at the posterior border of sternocleidomastoid. Inferiorly, supraclavicular nerves, transverse cervical vessels and the uppermost part of the brachial plexus cross the triangle. Lymph nodes lie along the posterior border of sternocleidomastoid from the mastoid process to the root of the neck.
Supraclavicular triangle
The supraclavicular triangle is the lower and smaller division of the posterior triangle, with which it shares the same boundaries, except that superiorly it is limited by omohyoid. It corresponds in the living neck with the lower part of a deep, prominent hollow, namely, the greater supraclavicular fossa. Its floor contains the first rib, scalenus medius and the first slip of serratus anterior. Its size varies with the extent of the clavicular attachments of sternocleidomastoid and trapezius and also the level of the inferior belly of omohyoid. The triangle is covered by skin, superficial and deep fasciae and platysma and crossed by the supraclavicular nerves. Just above the clavicle, the third part of the subclavian artery curves inferolaterally from the lateral margin of scalenus anterior across the first rib to the axilla. The subclavian vein is behind the clavicle and is not usually in the triangle; but it may rise as high as the artery and even accompany it behind scalenus anterior. The brachial plexus is partly superior, and partly posterior to the artery and is always closely related to it. The trunks of the brachial plexus may easily be palpated here if the neck is contralaterally flexed and the examining finger is drawn across the trunks at right angles to their length. With the musculature relaxed, pulsation of the subclavian artery may be felt and the arterial flow can be controlled by retroclavicular compression against the first rib. The suprascapular vessels pass transversely behind the clavicle, below the transverse cervical artery and vein. The external jugular vein descends behind the posterior border of sternocleidomastoid to end in the subclavian vein. It receives the transverse cervical and suprascapular veins, which form a plexus in front of the third part of the subclavian artery; occasionally it is joined by a small vein that crosses the clavicle anteriorly from the cephalic vein. Other structures within the triangle include the nerve to subclavius, which crosses the triangle, and lymph nodes.
CERVICAL FASCIA
SUPERFICIAL CERVICAL FASCIA
The superficial cervical fascia is usually a thin lamina covering platysma and is hardly demonstrable as a separate layer. It may, however, contain considerable amounts of adipose tissue, especially in females. Like all superficial fascia it is not a separate stratum, but merely a zone of loose connective tissue between dermis and deep fascia, and is joined to both. In the lower cervical region, aponeurotic fibres of platysma gradually fan out in the superficial fascia: they either become skin ligaments or continue into the fascia covering pectoralis major and deltoid. These aponeurotic fibres cover the anterior and lateral cervical regions and often mimic the investing layer of deep cervical fascia, forming a tissue barrier (Nash et al 2005).
DEEP CERVICAL FASCIA
Descriptions of the organization of the deep cervical fascia are largely based on the classic work of Grodinsky & Holyoke in 1938. However recent anatomical studies using techniques such as sheet plastination and confocal microscopy have indicated that the arrangement of the deep cervical fascia is more complicated than was previously thought (Zhang & Lee 2002, Nash et al 2005) (Fig. 28.4).
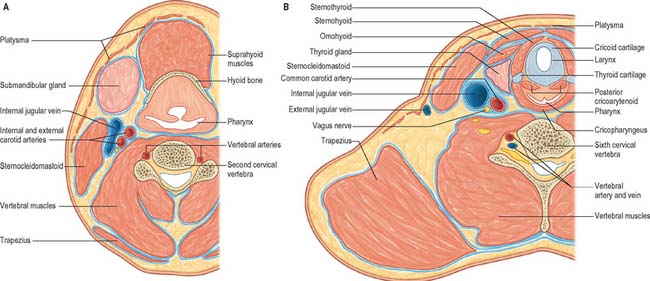
Fig. 28.4 Transverse sections through the neck at the levels of the second (A) and sixth (B) cervical vertebrae, showing the arrangement of the deep cervical fascia, much of which has been coloured blue. Diagrams are based on plastinated sections: note that many muscles have not been individually delineated.
(By courtesy of Dr M Zhang and Mr Robbie McPhee.)
Deep fascia in the neck is conventionally divided into an investing layer, pretracheal fascia, and prevertebral fascia.
Investing layer
The investing layer of the deep cervical fascia is continuous posteriorly with the corresponding fascia from the opposite side. It forms a thin covering for trapezius and encloses sternocleidomastoid. The portions between trapezius and sternocleidomastoid and in the anterior triangle of the neck are formed of areolar tissue, indistinguishable from that in the superficial cervical fascia and deep potential tissue spaces. Superiorly, the deep fascia fuses with periosteum along the superior nuchal line of the occipital bone, over the mastoid process and along the entire base of the mandible. Between the angle of the mandible and the anterior edge of sternocleidomastoid it is particularly strong. Between the mandible and the mastoid process it is related to the parotid gland, extending beneath it to become attached to the zygomatic arch. From this region the strong stylomandibular ligament ascends to the styloid process. Inferiorly, along trapezius and sternocleidomastoid, the investing layer of the deep cervical fascia is attached to the acromion, clavicle and manubrium sterni, fusing with their periostea. A short distance above the manubrium, the investing layer interweaves with aponeurotic fibres of platysma and the fascia investing the strap muscles. It is organized into superficial and deep layers which are attached to the anterior border of the manubrium, and to the posterior border and the interclavicular ligament respectively. Between these two layers a slit-like interval, the suprasternal space, contains a small amount of areolar tissue, the lower parts of the anterior jugular veins and the jugular venous arch, the sternal heads of the sternocleidomastoid muscles and sometimes a lymph node.
Pretracheal fascia
The pretracheal layer of the deep cervical fascia is very thin. It provides fascial sheaths for the thyroid gland, larynx, pharynx, trachea, oesophagus and the infrahyoid strap muscles. Superiorly, it is attached to the hyoid bone; inferiorly, it continues into the superior mediastinum along the great vessels and merges with the fibrous pericardium; laterally, it merges with the investing layer of deep cervical fascia and with the carotid sheath.
Prevertebral fascia
The prevertebral layer of the deep cervical fascia covers the anterior vertebral muscles and extends laterally on scalenus anterior, scalenus medius and levator scapulae, forming a fascial floor for the posterior triangle of the neck. As the subclavian artery and the brachial plexus emerge from behind scalenus anterior they carry the prevertebral fascia downwards and laterally behind the clavicle as the axillary sheath.
The prevertebral fascia is particularly prominent in front of the vertebral column, where there may be two distinct layers of fascia. The space created by the splitting of the anterior prevertebral fascia, the danger space, is a part of the prevertebral space. Traced laterally, the prevertebral fascia becomes thin and areolar. Superiorly it is attached to the base of the skull. Inferiorly it descends in front of longus colli into the superior mediastinum, where it blends with the anterior longitudinal ligament. Anteriorly the prevertebral fascia is separated from the pharynx and its covering buccopharyngeal fascia by a loose areolar zone, the retropharyngeal space. Laterally this loose tissue connects the prevertebral fascia to the carotid sheath and the fascia on the deep surface of sternocleidomastoid. All the ventral rami of the cervical nerves are initially behind the prevertebral fascia. The nerves to the rhomboids and serratus anterior and the phrenic nerve retain this position throughout their course in the neck, but the accessory nerve lies superficial to the prevertebral fascia.
Carotid sheath
The carotid sheath is a condensation of deep cervical fascia around the common and internal carotid arteries, the internal jugular vein, the vagus nerve and the constituents of the ansa cervicalis. It is thicker around the arteries than the vein, an arrangement that allows the vein to expand. Peripherally the carotid sheath is connected to adjacent fascial layers by loose areolar tissue.
Tissue spaces and the spread of infection and injectate
The fascial layers of the neck define a number of potential tissue ‘spaces’ above and below the hyoid bone. In health, the tissues within these spaces are closely applied to each other or are filled with relatively loose connective tissue. However, infections arising superiorly, such as dental, tonsillar, vertebral or intervertebral disc-related infections, can alter these relationships. The organisms responsible are often betahaemolytic streptococci or a variety of anaerobes. Streptococci produce proteolytic enzymes which digest the loose connective tissue and so open up the tissue spaces. Since there are no tissue barriers running horizontally in the neck, infections which are not treated promptly can rapidly spread from the infratemporal fossa down to the mediastinum below (see Ch. 55), cross the midline through the sublingual and submental spaces and even track into the axilla.
Understanding the configuration of the cervical fasciae and spaces is essential for the placement of local anaesthetic cervical plexus blocks in the neck to facilitate operations such as thyroidectomy, parathyroidectomy and carotid endarterectomy (Pandit et al 2000). For example, injection of local anaesthetic either in the superficial fascial plane or under the investing fascia of the posterior triangle can provide a similarly effective cervical plexus block (Pandit et al 2003), presumably because the investing fascia between sternocleidomastoid and trapezius is not a well-defined fascial sheet and is indistinguishable from the surrounding loose connective tissue (Zhang & Lee 2002).
The tissue spaces above the hyoid bone are the submandibular and submental spaces beneath the inferior border of the mandible; the pharyngeal spaces; and the prevertebral space near the base of the skull. These spaces are described on pages 524 and 568. Tissue spaces around the larynx are described on page 584.
Tissue spaces below the hyoid bone are the pretracheal and retrovisceral tissue spaces in the visceral compartment of the neck; the prevertebral space in front of the vertebral column; and a space associated with the carotid sheath.
The pretracheal tissue space lies behind the pretracheal fascia and the strap muscles, and in front of the anterior wall of the oesophagus, and therefore immediately surrounds the trachea. It is bounded superiorly by the attachments of the strap muscles to the thyroid cartilage of the larynx. Inferiorly, it extends down into the anterior portion of the superior mediastinum. Infection usually spreads into the pretracheal space either by perforating the anterior wall of the oesophagus or from the retrovisceral space.
Radiologically, the portion of the pretracheal space between the strap fascia and the fascia of the thyroid gland is referred as the anterior cervical space. The posterolateral border of the space is the carotid sheath or the fascia of sternocleidomastoid. The anterior cervical space often provides a symmetric landmark on transverse imaging (Smoker & Harnsberger 1991).
The retrovisceral space is continuous superiorly with the retropharyngeal space. It is situated between the posterior wall of the oesophagus and the prevertebral fascia. Inferiorly, the retrovisceral space extends into the superior mediastinum. Should the prevertebral fascia merge with the connective tissue on the posterior surface of the oesophagus – usually at the level of the fourth thoracic vertebra – the retrovisceral space then has a distinct inferior boundary.
The prevertebral tissue space has been variously described as the potential space lying between the prevertebral fascia and the vertebral column, and as the space between the two layers of the prevertebral fascia, the so-called danger space. Infection usually spreads into the space via its fascial walls from the retrovisceral area because it is closed superiorly and laterally. Inferiorly, it extends into the posterior mediastinum. Clinically, however, the danger space and the retropharyngeal or retrovisceral space are often considered together because they cannot be differentiated radiologically.
The carotid sheath is a layer of loose connective tissue demarcated by adjacent portions of the investing layer of deep cervical fascia, the pretracheal fascia, and the prevertebral fascia. It delineates a potential space into which infections from the visceral spaces may track. Infections around the carotid sheath may be restricted because superiorly (near the hyoid bone) and inferiorly (near the root of the neck) the connective tissues adhere to the vessels.
The main cause of cellulitis of the neck is infection arising from the region of the mandibular molar teeth. Several fascial spaces are accessible from this area, and several anatomical factors contribute to the spread of infection. Thus, the apices of the second and, more especially, the third, mandibular molar teeth are often close to the lingual surface of the mandible. The apices of the roots of the third mandibular molars are usually, and the second molars are often below the attachment of mylohyoid on the inner aspect of the mandible and so drain directly into the submandibular tissue space. The posterior free border of mylohyoid is close to the sockets of the third mandibular molars, and at this point, the floor of the mouth consists only of mucous membrane covering part of the submandibular salivary gland. Any virulent periapical infection of the mandibular third molar teeth may therefore penetrate the lingual plate of the mandible and is then at the entrance to the submandibular and sublingual spaces anteriorly, and the parapharyngeal and pterygoid spaces posteriorly. Infection in this area may also spread from an acute pericoronitis, particularly when the deeper tissues are opened to infection by extraction of the tooth during the acute phase.
In general, cellulitis around the jaw is only likely to develop when the tissues are infected by virulent and invasive organisms at a point where there is access to the fascial spaces: the predisposing causes do not often coincide, and cellulitis is therefore uncommon. Cellulitis in the region of the maxilla is even more uncommon, but fascial space infections may develop in various sites as the result of infected local anaesthetic needles. Since there are no barriers running horizontally with respect to the tissue spaces in the neck, infection entering in this site can rapidly spread more or less unhindered down the neck and may enter the mediastinum (see Ch. 55).
All forms of cellulitides of the neck or deep neck space infections are potentially serious. Narrowing of the upper airway can occur as a result of inflammation and oedema, leading to dyspnoea or obstruction of the upper airway (with stridor) and reduced oxygenation of the lungs. This situation can be extremely difficult to manage by conventional techniques. The increased rigidity and reduced compliance of the tissues mean that manoeuvres such as manual anterior jaw thrust or laryngoscopy may fail to re-open the airway. Specialized techniques, e.g. flexible fibreoptic-assisted tracheal intubation or surgical tracheostomy under local anaesthesia, may be required to provide general anaesthesia to facilitate the surgical drainage and treatment of the cellulitis or deep space abscess.
MUSCLES
The superficial muscles of the neck are platysma, which lies in the subcutaneous tissue of the neck, and sternocleidomastoid and trapezius. Sternocleidomastoid is a key landmark because it divides the neck into anterior and lateral regions (anterior and posterior triangles respectively); the anterior region may be further subdivided into several smaller named triangles (see above). Muscles in the anterior region are organized into supra- and infra-hyoid groups, and with one exception are all attached to the hyoid bone. The supra-hyoid muscles, which connect the hyoid bone to the mandible and the base of the skull, include mylohyoid, geniohyoid, stylohyoid and digastric. The infrahyoid (strap) muscles, which connect the hyoid, sternum, clavicle and scapula, are arranged in two planes, a superficial plane consisting of sternohyoid and omohyoid and a deep plane consisting of sternothyroid and thyrohyoid.
The muscles that form part of the musculoskeletal column in the neck are described in Chapter 42. They can be considered in three groups, anterior, lateral and posterior; very broadly speaking, the muscles in these groups lie anterior, lateral or posterior to the cervical vertebrae. The anterior and lateral groups include longi colli and capitis; recti capitis anterior and lateralis; scaleni anterior, medius, posterior and minimi (when present). The posterior muscle group is composed of the cervical components of the intrinsic muscles of the back, overlaid by some of the extrinsic ‘immigrant’ muscles of the back that run between the upper limb and the axial skeleton (trapezius, levator scapulae, see Ch. 42). The intrinsic muscles are arranged in superficial and deep layers. The superficial layer contains splenius capitis and cervicis. The deeper layers include the transversospinal group (semispinales cervicis and capitis, multifidus and rotatores cervicis), interspinales and intertransversarii, and the suboccipital group (recti capitis posterior major and minor and obliquus capitis superior and inferior).
The muscles associated with the pharynx and larynx are described in Chapters 33 and 34 respectively.
Platysma
Platysma is a broad sheet of muscle of varying prominence which arises from the fascia covering the upper parts of pectoralis major and deltoid. Its fibres cross the clavicle and ascend medially in the side of the neck. Anterior fibres interlace across the midline with the fibres of the contralateral muscle, below and behind the symphysis menti. Other fibres attach to the lower border of the mandible or to the lower lip or cross the mandible to attach to skin and subcutaneous tissue of the lower face. Careful elevation of a myocutaneous flap in the subplatysmal plane as part of a neck dissection will include this muscle and its associated blood supply, thereby minimizing the risk of skin necrosis and wound breakdown.
Platysma is supplied by the submental branch of the facial artery and by the suprascapular artery (from the thyrocervical trunk of the subclavian artery).
Platysma is innervated by the cervical branch of the facial nerve which descends on the deep surface of the muscle close to the angle of the mandible.
Contraction diminishes the concavity between the jaw and the side of the neck and produces tense oblique ridges in the skin of the neck. Platysma may assist in depressing the mandible, and via its labial and modiolar attachments it can draw down the lower lip and corners of the mouth in expressions of horror or surprise.
Sternocleidomastoid
Sternocleidomastoid (Fig. 28.5) descends obliquely across the side of the neck and forms a prominent surface landmark, especially when contracted. It is thick and narrow centrally, and broader and thinner at each end. The muscle is attached inferiorly by two heads. The medial or sternal head is rounded and tendinous, arises from the upper part of the anterior surface of the manubrium and sterni and ascends posterolaterally. The lateral or clavicular head, which is variable in width and contains muscular and fibrous elements, ascends almost vertically from the superior surface of the medial third of the clavicle. The two heads are separated near their attachments by a triangular interval which corresponds to a surface depression, the lesser supraclavicular fossa. As they ascend, the clavicular head spirals behind the sternal head and blends with its deep surface below the middle of the neck, forming a thick, rounded belly. Sternocleidomastoid inserts superiorly by a strong tendon into the lateral surface of the mastoid process from its apex to its superior border, and by a thin aponeurosis into the lateral half of the superior nuchal line. The clavicular fibres are directed mainly to the mastoid process; the sternal fibres are more oblique and superficial, and extend to the occiput. The direction of pull of the two heads is therefore different, and the muscle may be classed as ‘cruciate’ and slightly ‘spiralized’.
The superficial surface of sternocleidomastoid is covered by skin and platysma, between which lie the external jugular vein, the great auricular and transverse cervical nerves and the superficial lamina of the deep cervical fascia. Near its insertion the muscle is overlapped by a small part of the parotid gland. The deep surface of the muscle near its origin is related to the sternoclavicular joint and sternohyoid, sternothyroid and omohyoid. The anterior jugular vein crosses deep to it, but superficial to the infrahyoid muscles, immediately above the clavicle. The carotid sheath and the subclavian artery are deep to these muscles. Between omohyoid and the posterior belly of digastric, the anterior part of sternocleidomastoid lies superficial to the common, internal and external carotid arteries, the internal jugular, facial and lingual veins, the deep cervical lymph nodes, the vagus nerve and the rami of the ansa cervicalis. The sternocleidomastoid branch of the superior thyroid artery crosses deep to the muscle at the upper border of omohyoid. The posterior part of sternocleidomastoid is related on its internal surface to splenius capitis, levator scapulae and the scalene muscles, the cervical plexus, the upper part of the brachial plexus, the phrenic nerve and the transverse cervical and suprascapular arteries. The occipital artery crosses deep to the muscle at, or under cover of, the lower border of the posterior belly of digastric. At this point the accessory nerve passes deep to sternocleidomastoid, then pierces and supplies the muscle, before it reappears just above the middle of the posterior border. At its insertion the muscle lies superficial to the mastoid process, splenius capitis, longissimus capitis and the posterior belly of digastric.
Sternocleidomastoid receives its blood supply from branches of the occipital and posterior auricular arteries (upper part of muscle), the superior thyroid artery (middle part of muscle), and the suprascapular artery (lower part of muscle). A superiorly based flap can be raised on sternocleidomastoid to include a paddle of skin supplied by perforator vessels. This flap has been used to reconstruct the lips, floor of mouth and inner aspect of the cheeks, however its use has been superseded by microvascular free transfer flaps or by conventional myocutaneous flaps such as the pectoralis major flap.
Sternocleidomastoid is supplied by the spinal part of the accessory nerve. Branches from the ventral rami of the second, third, and sometimes fourth, cervical spinal nerves also enter the muscle. Although these cervical rami were believed to be solely proprioceptive, clinical evidence suggests that some of their fibres are motor.
Acting alone, each sternocleidomastoid will tilt the head towards the ipsilateral shoulder, simultaneously rotating the head so as to turn the face towards the opposite side. This movement occurs in an upward, sideways glance. A more common visual movement is a level rotation from side to side, and this probably represents the most frequent use of the sternocleidomastoids. Acting together from below, the muscles draw the head forwards and so help longi colli to flex the cervical part of the vertebral column, which is a common movement in feeding. The two sternocleidomastoids are also used to raise the head when the body is supine, and when the head is fixed, they help to elevate the thorax in forced inspiration.
Branchial cysts usually present in the upper neck in early adulthood as fluctuant swellings at the junction of the upper and middle thirds of the anterior border of sternocleidomastoid. The cyst typically passes backwards and upwards through the carotid bifurcation and ends at the pharyngeal constrictor muscles, a course which brings it into intimate association with the hypoglossal, glossopharyngeal and spinal accessory nerves. Great care must be taken to avoid damage to these nerves during surgical removal of a branchial cyst.
Branchial fistulae represent a persistent connection between the second branchial pouch and the cervical sinus. The fistula typically presents as a small pit adjacent to the anterior border of the lower third of sternocleidomastoid, which may weep saliva and become intermittently infected. Excision involves following the tract of the fistula up the neck – often through the carotid bifurcation – and into the distal tonsillar fossa where it opens into the pharynx.
Branchial cysts, sinuses and fistulae are thought to arise from inclusions of salivary gland tissue in lymph nodes: they may also occur around the parotid gland.
MUSCLES OF THE ANTERIOR TRIANGLE OF THE NECK
Apart from the superficial neck muscles already described, the anterior triangle contains two of the suprahyoid muscles, namely digastric and stylohyoid, and the four infrahyoid strap muscles (Fig. 28.5). The other suprahyoid muscles, namely mylohyoid and geniohyoid, are described with the floor of the mouth on page 501.
Digastric
Digastric has two bellies and lies below the mandible, extending from the mastoid process to the chin (Fig. 28.5). The posterior belly, which is longer than the anterior, is attached in the mastoid notch of the temporal bone, and passes downwards and forwards. The anterior belly is attached to the digastric fossa on the base of the mandible near the midline, and slopes downwards and backwards. The two bellies meet in an intermediate tendon which perforates stylohyoid and runs in a fibrous sling attached to the body and greater cornu of the hyoid bone and is sometimes lined by a synovial sheath. The two bellies of digastric mark out the borders of the submandibular triangle.
Digastric may lack the intermediate tendon and is then attached midway along the body of the mandible. The posterior belly may be augmented by a slip from the styloid process or arise wholly from it. The anterior belly may cross the midline and it is not uncommon for it to fuse with mylohyoid.
Superficial to digastric are platysma, sternocleidomastoid, splenius capitis, longissimus capitis and stylohyoid, the mastoid process, the retromandibular vein and the parotid and submandibular salivary glands. Mylohyoid is medial to the anterior belly, and hyoglossus, superior oblique and rectus capitis lateralis, the transverse process of the atlas vertebra, the accessory nerve, internal jugular vein, occipital artery, hypoglossal nerve, internal and external carotid, facial and lingual arteries are all medial to the posterior belly.
The posterior belly is supplied by the posterior auricular and occipital arteries. The anterior belly of digastric receives its blood supply chiefly from the submental branch of the facial artery.
Stylohyoid
Stylohyoid arises by a small tendon from the posterior surface of the styloid process, near its base. Passing downwards and forwards, it inserts into the body of the hyoid bone at its junction with the greater cornu (and just above the attachment of the superior belly of omohyoid). It is perforated near its insertion by the intermediate tendon of digastric (Fig. 28.5). The muscle may be absent or double. It may lie medial to the external carotid artery and may end in the suprahyoid or infrahyoid muscles.
Stylohyoid ligament
The stylohyoid ligament is a fibrous cord extending from the tip of the styloid process to the lesser cornu of the hyoid bone. It gives attachment to the highest fibres of the middle pharyngeal constrictor and is intimately related to the lateral wall of the oropharynx. Below, it is overlapped by hyoglossus. The ligament is derived from the cartilage of the second branchial arch, and may be partially calcified.
INFRAHYOID MUSCLES
The infrahyoid muscles are organized so that sternohyoid and omohyoid lie superficially and sternothyroid and thyrohyoid lie more deeply (Fig. 28.5). The muscles are involved in movements of the hyoid bone and thyroid cartilage during vocalization, swallowing and mastication and are mainly innervated from the ansa cervicalis.
Sternohyoid
Sternohyoid is a thin, narrow strap muscle that arises from the posterior surface of the medial end of the clavicle, the posterior sternoclavicular ligament and the upper posterior aspect of the manubrium (Fig. 28.5). It ascends medially and is attached to the inferior border of the body of the hyoid bone. Inferiorly, there is a considerable gap between the muscle and its contralateral fellow, but the two usually come together in the middle of their course, and are contiguous above this. Sternohyoid may be absent or double, augmented by a clavicular slip (cleidohyoid), or interrupted by a tendinous intersection.
Omohyoid
Omohyoid consists of two bellies united at an angle by an intermediate tendon (Fig. 28.5). The inferior belly is a flat, narrow band, which inclines forwards and slightly upwards across the lower part of the neck. It arises from the upper border of the scapula, near the scapular notch, and occasionally from the superior transverse scapular ligament. It then passes behind sternocleidomastoid and ends there in the intermediate tendon. The superior belly begins at the intermediate tendon, passes almost vertically upwards near the lateral border of sternohyoid and is attached to the lower border of the body of the hyoid bone lateral to the insertion of sternohyoid. The length and form of the intermediate tendon varies, although it usually lies adjacent to the internal jugular vein at the level of the arch of the cricoid cartilage. The angulated course of the muscle is maintained by a band of deep cervical fascia, attached below to the clavicle and the first rib, which ensheathes the tendon. A variable amount of skeletal muscle may be present in the fascial band; either belly may be absent or double; the inferior belly may be attached directly to the clavicle and the superior is sometimes fused with sternohyoid.
Sternothyroid
Sternothyroid is shorter and wider than sternohyoid, and lies deep and partly medial to it (Fig. 28.5). It arises from the posterior surface of the manubrium sterni inferior to the origin of sternohyoid and from the posterior edge of the cartilage of the first rib. It is attached above to the oblique line on the lamina of the thyroid cartilage, where it delineates the upward extent of the thyroid gland. In the lower part of the neck the muscle is in contact with its contralateral fellow, but the two diverge as they ascend.
Thyrohyoid
Thyrohyoid is a small, quadrilateral muscle that may be regarded as an upward continuation of sternothyroid (Fig. 28.5). It arises from the oblique line on the lamina of the thyroid cartilage, and passes upwards to attach to the lower border of the greater cornu and adjacent part of the body of the hyoid bone.
ANTERIOR VERTEBRAL MUSCLES
The anterior vertebral group of muscles are longi colli and capitis, and recti capitis anterior and lateralis (Fig. 28.6), all of which are flexors of the head and neck to varying degrees. Together with the lateral vertebral muscles they form the prevertebral muscle group.
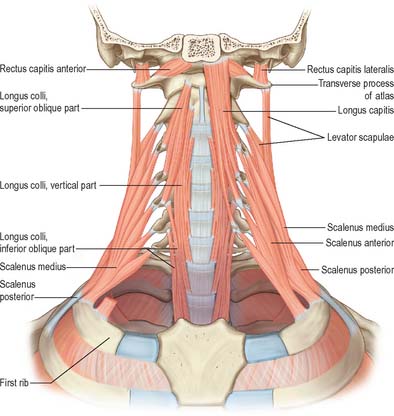
Fig. 28.6 The anterior and lateral vertebral muscles. Scalenus anterior and longus capitis have been removed on the right side.
Rectus capitis anterior
Rectus capitis anterior is a short, flat muscle situated behind the upper part of longus capitis. It arises from the anterior surface of the lateral mass of the atlas and the root of its transverse process, and ascends almost vertically to the inferior surface of the basilar part of the occipital bone immediately anterior to the occipital condyle.
Rectus capitis lateralis
Rectus capitis lateralis is a short, flat muscle that arises from the upper surface of the transverse process of the atlas and inserts into the inferior surface of the jugular process of the occipital bone. In view of its attachments and its relation to the ventral ramus of the first spinal nerve, rectus capitis lateralis is regarded as homologous with the posterior intertransverse muscles.
Longus capitis
Longus capitis (Fig. 28.6) has a narrow origin from tendinous slips from the anterior tubercles of the transverse processes of the third, fourth, fifth and sixth cervical vertebrae and becomes broad and thick above, where it is inserted into the inferior surface of the basilar part of the occipital bone.
Longus colli
Longus colli (Fig. 28.6) is applied to the anterior surface of the vertebral column, between the atlas and the third thoracic vertebra. It can be divided into three parts which all arise by tendinous slips. The inferior oblique part is the smallest, running upwards and laterally from the fronts of the bodies of the first two or three thoracic vertebrae to the anterior tubercles of the transverse processes of the fifth and sixth cervical vertebrae. The superior oblique part passes upwards and medially from the anterior tubercles of the transverse processes of the third, fourth and fifth cervical vertebrae to be attached by a narrow tendon to the anterolateral surface of the tubercle on the anterior arch of the atlas. The vertical intermediate part ascends from the fronts of the bodies of the upper three thoracic and lower three cervical vertebrae to the fronts of the bodies of the second, third and fourth cervical vertebrae.
LATERAL VERTEBRAL MUSCLES
Scaleni anterior, medius and posterior extend obliquely between the upper two ribs and the cervical transverse processes. Scalenus minimus (pleuralis) is associated with the suprapleural membrane and cervical pleura, and is described in Chapter 57.
Scalenus anterior
Scalenus anterior lies at the side of the neck deep (posteromedial) to sternocleidomastoid (Fig. 28.5; see also Fig. 28.18). Above, it is attached by musculotendinous fascicles to the anterior tubercles of the transverse processes of the third, fourth, fifth and sixth cervical vertebrae. These converge, blend and descend almost vertically, to be attached by a narrow, flat tendon to the scalene tubercle on the inner border of the first rib, and to a ridge on the upper surface of the rib anterior to the groove for the subclavian artery.
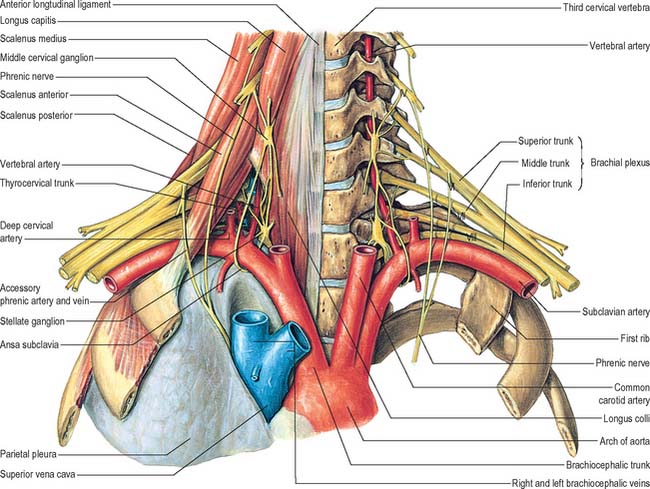
Fig. 28.18 The root of the neck. Note the sympathetic chain, the middle and inferior cervical sympathetic ganglia, the trunks of the brachial plexus, the phrenic nerve and the vertebral artery.
(From Sobotta 2006.)
Scalenus anterior forms an important landmark in the root of the neck, because the phrenic nerve passes anterior to it, the subclavian artery posterior to it, and the brachial plexus lies at its lateral border. The clavicle, subclavius, sternocleidomastoid and omohyoid, lateral part of the carotid sheath, transverse cervical, suprascapular and ascending cervical arteries, subclavian vein, prevertebral fascia and phrenic nerve are all anterior to scalenus anterior. Posteriorly are the suprapleural membrane, pleura, roots of the brachial plexus and the subclavian artery: the latter two separate scalenus anterior from scalenus medius. The proximity of the muscle to the brachial plexus, subclavian artery and vein can give rise to compression syndromes. Below its attachment to the sixth cervical vertebra, the medial border of the muscle is separated from longus colli by an angular interval in which the vertebral artery and vein pass to and from the foramen transversarium of the sixth cervical vertebra. The inferior thyroid artery crosses this interval from the lateral to the medial side near its apex. The sympathetic trunk and its cervicothoracic ganglion are closely related to the posteromedial side of this part of the vertebral artery. On the left side the thoracic duct crosses the triangular interval at the level of the seventh cervical vertebra and usually comes into contact with the medial edge of scalenus anterior. The musculotendinous attachments of scalenus anterior to anterior tubercles are separated from those of longus capitis by the ascending cervical branch of the inferior thyroid artery.
Scalenus medius
Scalenus medius, the largest and longest of the scaleni, is attached above to the transverse process of the axis and the front of the posterior tubercles of the transverse processes of the lower five cervical vertebrae (Fig. 28.6). It frequently extends upwards to the transverse process of the atlas. Below it is attached to the upper surface of the first rib between the tubercle of the rib and the groove for the subclavian artery.
The anterolateral surface of the muscle is related to sternocleidomastoid (Fig. 28.5). It is crossed anteriorly by the clavicle and omohyoid, and it is separated from scalenus anterior by the subclavian artery and ventral rami of the cervical spinal nerves. Levator scapulae and scalenus posterior lie posterolateral to it. The upper two roots of the nerve to serratus anterior and the dorsal scapular nerve (to the rhomboids) pierce the muscle and appear on its lateral surface.
Scalenus posterior
Scalenus posterior is the smallest and most deeply situated of the scalene muscles (Fig. 28.6). It passes from the posterior tubercles of the transverse processes of the fourth, fifth, and sixth cervical vertebrae to the outer surface of the second rib, behind the tubercle for serratus anterior, where it is attached by a thin tendon.
Scalenus posterior is occasionally blended with scalenus medius. The scalene muscles vary a little in the number of vertebrae to which they are attached, in their degree of separation, and their segmental innervation.
All the scalene muscles are chiefly supplied by the ascending cervical branch of the inferior thyroid artery. Scalenus posterior receives an additional supply from the superficial cervical artery.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
ARTERIES OF THE NECK
The common carotid, internal carotid, and external carotid arteries provide the major source of blood to the head and neck (Figs 28.7A, 28.8). Additional arteries arise from branches of the subclavian artery, particularly the vertebral artery.
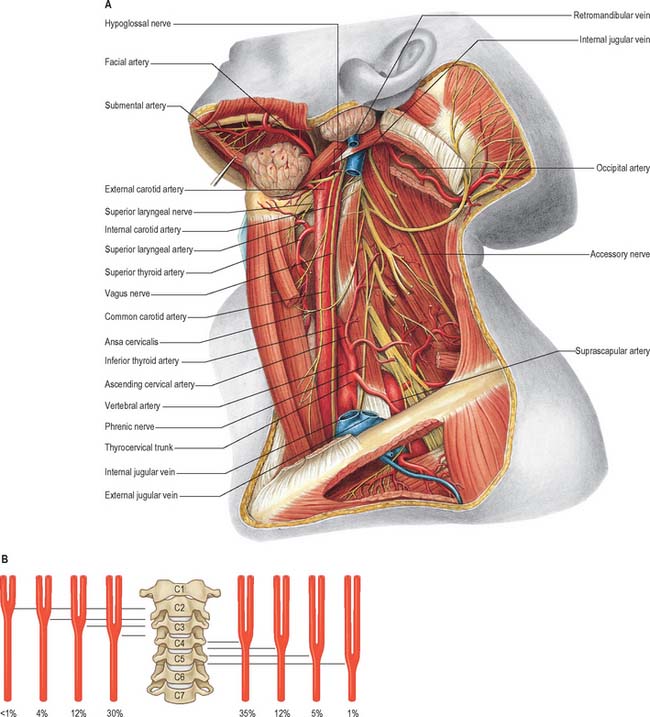
Fig. 28.7 A, Vessels and nerves of the neck, left lateral view: sternocleidomastoid and the greater part of omohyoid and the internal jugular vein have been removed. Compare with Fig. 28.17, which shows a deeper level of dissection. B, Variation in levels of bifurcation of the common carotid artery, related to the cervical vertebrae.
(A, From Sobotta 2006.) (Redrawn with permission from Sobatta 2006.)
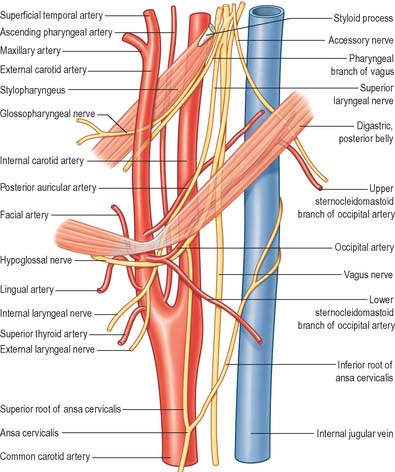
Fig. 28.8 The branches of the external carotid artery. Note the structures that either cross the internal jugular vein and the carotid arteries or intervene between the external and internal carotid arteries.
The common, internal and external carotid arteries and accompanying veins and nerves, all lie in a cleft that is bound posteriorly by the transverse processes of cervical vertebrae and attached muscles, medially by the trachea, oesophagus, thyroid gland, larynx and pharyngeal constrictors, and anterolaterally by sternocleidomastoid and, at different levels, omohyoid, sternohyoid, sternothyroid, digastric and stylohyoid muscles. The common and internal carotid arteries lie within the carotid sheath, accompanied by the internal jugular vein and the vagus nerve.
Common carotid artery
The common carotid arteries differ on the right and left sides with respect to their origins. On the right, the common carotid arises from the brachiocephalic artery as it passes behind the sternoclavicular joint. On the left, the common carotid artery comes directly from the arch of the aorta in the superior mediastinum. The right common carotid has, therefore, only a cervical part whereas the left common carotid has cervical and thoracic parts. Following a similar course on both sides, the common carotid artery ascends, diverging laterally from behind the sternoclavicular joint to the level of the upper border of the thyroid cartilage of the larynx (C3–4 junction), where it divides into external and internal carotid arteries. This bifurcation can sometimes be at a higher level. The artery may be compressed against the prominent transverse process of the sixth cervical vertebra (Chassaignac’s tubercle), and above this level it is superficial and its pulsation can be easily felt.
In the lower part of the neck the common carotid arteries are separated by a narrow gap which contains the trachea. Above this, the arteries are separated by the thyroid gland, larynx and pharynx. Each artery is contained within the carotid sheath of deep cervical fascia, which also encloses the internal jugular vein and vagus nerve. The vein lies lateral to the artery, and the nerve lies between them and posterior to both.
The artery is crossed anterolaterally, at the level of the cricoid cartilage, by the intermediate tendon – sometimes the superior belly – of omohyoid. Below omohyoid it is sited deeply, covered by skin, superficial fascia, platysma, deep cervical fascia, and sternocleidomastoid, sternohyoid and sternothyroid. Above omohyoid it is more superficial, covered merely by skin, superficial fascia, platysma, deep cervical fascia and the medial margin of sternocleidomastoid, and it is crossed obliquely from its medial to lateral side by the sternocleidomastoid branch of the superior thyroid artery. The superior root of the ansa cervicalis, joined by its inferior root from the second and third cervical spinal nerves, lies anterior to, or embedded within, the carotid sheath as it crosses it obliquely. The superior thyroid vein usually crosses near the upper border of the thyroid cartilage, and the middle thyroid vein crosses a little below the level of the cricoid cartilage. The anterior jugular vein crosses the common carotid artery above the clavicle, separated from it by sternohyoid and sternothyroid. Posterior to the carotid sheath are the transverse processes of the fourth to sixth cervical vertebrae, to which are attached longus colli, longus capitis and tendinous slips of scalenus anterior. The sympathetic trunk and ascending cervical branch of the inferior thyroid artery lie between the common carotid artery and the muscles. Below the level of the sixth cervical vertebra the artery is in an angle between scalenus anterior and longus colli, anterior to the vertebral vessels, inferior thyroid and subclavian arteries, sympathetic trunk and, on the left, the thoracic duct. The oesophagus, trachea, inferior thyroid artery and recurrent laryngeal nerve and, at a higher level, the larynx and pharynx are medial to the sheath and its contents. The thyroid gland overlaps it anteromedially. The internal jugular vein lies lateral, and, in the lower neck also anterior, to the artery, while the vagus nerve lies posterolaterally in the angle between artery and vein.
On the right side, low in the neck, the recurrent laryngeal nerve crosses obliquely behind the artery. The right internal jugular vein diverges from it below but the left vein approaches and often overlaps its artery.
In 12% of cases the right common carotid artery arises above the level of the sternoclavicular joint, or it may be a separate branch from the aorta. The left common carotid artery varies in origin more than the right and may arise with the brachiocephalic artery. Division of the common carotid may occur higher, near the level of the hyoid bone, or, more rarely, at a lower level alongside the larynx. Very rarely it ascends without division, so that either the external or internal carotid is absent, or it may be replaced by separate external and internal carotid arteries which arise directly from the aorta, on one side, or bilaterally.
Although the common carotid artery usually has no branches, it may occasionally give rise to the vertebral, superior thyroid, superior laryngeal, ascending pharyngeal, inferior thyroid or occipital arteries.
External carotid artery
The external carotid artery (Figs 28.7A, 28.8) begins lateral to the upper border of the thyroid cartilage, level with the intervertebral disc between the third and fourth cervical vertebrae. A little curved and with a gentle spiral, it first ascends slightly forwards and then inclines backwards and a little laterally, to pass midway between the tip of the mastoid process and the angle of the mandible. Here, in the substance of the parotid gland behind the neck of the mandible, it divides into its terminal branches, the superficial temporal and maxillary arteries. As it ascends, it gives off several large branches, and diminishes rapidly in calibre. In children the external carotid is smaller than the internal carotid, but in adults the two are of almost equal size. At its origin, it is in the carotid triangle and lies anteromedial to the internal carotid artery. It later becomes anterior, then lateral, to the internal carotid as it ascends. At mandibular levels the styloid process and its attached structures intervene between the vessels: the internal carotid is deep, and the external carotid superficial, to the styloid process. A fingertip placed in the carotid triangle perceives a powerful arterial pulsation, which represents the termination of the common carotid, the origins of external and internal carotids and the stems of the initial branches of the external carotid.
The skin and superficial fascia, the loop between the cervical branch of the facial nerve and the transverse cutaneous nerve of the neck, the deep cervical fascia and the anterior margin of sternocleidomastoid all lie superficial to the external carotid artery in the carotid triangle. The artery is crossed by the hypoglossal nerve and its vena comitans and by the lingual, facial and, sometimes, the superior thyroid veins. Leaving the carotid triangle, the external carotid artery is crossed by the posterior belly of digastric and by stylohyoid, and ascends between these muscles and the posteromedial surface of the parotid gland, which it next enters. Within the parotid, the artery lies medial to the facial nerve and the junction of the superficial temporal and maxillary veins. The pharyngeal wall, superior laryngeal nerve and ascending pharyngeal artery are the initial medial relations of the artery. At a higher level, it is separated from the internal carotid artery by the styloid process, styloglossus and stylopharyngeus, glossopharyngeal nerve, pharyngeal branch of vagus nerve and part of the parotid gland. The artery is equally likely to lie medial to the parotid gland, or within it.
The external carotid artery has eight named branches distributed to the head and neck. The superior thyroid, lingual and facial arteries arise from its anterior surface, the occipital and posterior auricular arteries arise from its posterior surface and the ascending pharyngeal artery arises from its medial surface. The maxillary and superficial temporal arteries are its terminal branches within the parotid gland.
Superior thyroid artery
The superior thyroid artery is the first branch of the external carotid artery, and arises from the anterior surface of the external carotid just below the level of the greater cornu of the hyoid bone (Figs 28.7A, 28.8). It descends along the lateral border of thyrohyoid to reach the apex of the lobe of the thyroid gland. Lying medially are the inferior constrictor muscle and the external laryngeal nerve: the nerve is often posteromedial, and therefore at risk when the artery is being ligatured. Occasionally it may issue directly from the common carotid.
Branches
The superior thyroid artery supplies the thyroid gland and some adjacent skin. Glandular branches are: anterior, which runs along the medial side of the upper pole of the lateral lobe to supply mainly the anterior surface; a branch which crosses above the isthmus to anastomose with its fellow of the opposite side; and posterior, which descends on the posterior border to supply the medial and lateral surfaces and anastomoses with the inferior thyroid artery. Sometimes a lateral branch supplies the lateral surface. The artery also has the following named branches: infrahyoid, superior laryngeal, sternocleidomastoid and cricothyroid.
The infrahyoid artery is a small branch which runs along the lower border of the hyoid bone deep to thyrohyoid and anastomoses with its fellow of the opposite side to supply the infrahyoid strap muscles.
The superior laryngeal artery accompanies the internal laryngeal nerve. Deep to thyrohyoid it pierces the lower part of the thyrohyoid membrane to supply the tissues of the upper part of the larynx. It anastomoses with its fellow of the opposite side and with the inferior laryngeal branch of the inferior thyroid artery.
Ascending pharyngeal artery
The ascending pharyngeal artery is the smallest branch of the external carotid. It is a long, slender vessel which arises from the medial (deep) surface of the external carotid artery near the origin of that artery. It ascends between the internal carotid artery and the pharynx to the base of the cranium. The ascending pharyngeal artery is crossed by styloglossus and stylopharyngeus, and longus capitis lies posterior to it. It gives off numerous small branches to supply longus capitis and longus colli, the sympathetic trunk, the hypoglossal, glossopharyngeal and vagus nerves and some of the cervical lymph nodes. It anastomoses with the ascending palatine branch of the facial artery and the ascending cervical branch of the vertebral artery. Its named branches are the pharyngeal, inferior tympanic and meningeal arteries.
The pharyngeal artery gives off three or four branches to supply the constrictor muscles of the pharynx and stylopharyngeus. A variable ramus supplies the palate, and may replace the ascending palatine branch of the facial artery. The artery descends forwards between the superior border of the superior constrictor and levator veli palatini to the soft palate, and also supplies a branch to the palatine tonsil and the pharyngotympanic tube.
The inferior tympanic artery is a small branch which traverses the temporal canaliculus with the tympanic branch of the glossopharyngeal nerve and supplies the medial wall of the tympanic cavity.
The meningeal branches are small vessels which supply the nerves that traverse the foramen lacerum, jugular foramen and hypoglossal canal, and the associated dura mater and adjoining bone. One branch, the posterior meningeal artery, reaches the cerebellar fossa via the jugular foramen, and is usually regarded as the terminal branch of the ascending pharyngeal artery.
Lingual artery
The lingual artery provides the chief blood supply to the tongue and the floor of the mouth (Fig. 28.8; see Ch. 30). It arises anteromedially from the external carotid artery opposite the tip of the greater cornu of the hyoid bone, between the superior thyroid and facial arteries. It often arises with the facial or, less often, with the superior thyroid artery. It may be replaced by a ramus of the maxillary artery. Ascending medially at first, it loops down and forwards, passes medial to the posterior border of hyoglossus and then runs horizontally forwards deep to it. The lingual artery next ascends again almost vertically, and courses sinuously forwards on the inferior surface of the tongue as far as its tip. The further course of the lingual artery is described on page 505.
Its relationship to hyoglossus naturally divides the lingual artery into descriptive ‘thirds’. In its first part the lingual artery is in the carotid triangle. Skin, fascia and platysma are superficial to it, while the middle pharyngeal constrictor muscle is medial. The artery ascends a little medially, then descends to the level of the hyoid bone, and the loop so formed is crossed externally by the hypoglossal nerve. The second part passes along the upper border of the hyoid bone, deep to hyoglossus, the tendons of digastric and stylohyoid, the lower part of the submandibular gland and the posterior part of mylohyoid. Hyoglossus separates it from the hypoglossal nerve and its vena comitans. Here its medial aspect adjoins the middle constrictor muscle and it crosses the stylohyoid ligament accompanied by lingual veins. The third part is the arteria profunda linguae which turns upward near the anterior border of hyoglossus and then passes forwards close to the inferior lingual surface near the frenulum, accompanied by the lingual nerve. Genioglossus is a medial relation, and the inferior longitudinal muscle of the tongue lies lateral to it below the lingual mucous membrane. Near the tip of the tongue the lingual artery anastomoses with its fellow of the opposite side. Its named branches are the suprahyoid, dorsal lingual and sublingual arteries.
Suprahyoid artery
The suprahyoid artery is a small branch which runs along the upper border of the hyoid bone to anastomose with the contralateral artery. It supplies adjacent structures.
Facial artery
The facial artery (Figs 28.7, 28.8; see Figs 29.13, 29.18) arises anteriorly from the external carotid in the carotid triangle, above the lingual artery and immediately above the greater cornu of the hyoid bone. In the neck, at its origin, it is covered only by the skin, platysma, fasciae and often by the hypoglossal nerve. It runs up and forwards, deep to digastric and stylohyoid. At first on the middle pharyngeal constrictor, it may reach the lateral surface of styloglossus, separated there from the palatine tonsil only by this muscle and the lingual fibres of the superior constrictor. Medial to the mandibular ramus it arches upwards and grooves the posterior aspect of the submandibular gland. It then turns down and descends to the lower border of the mandible in a lateral groove on the submandibular gland, between the gland and medial pterygoid. Reaching the surface of the mandible, the facial artery curves round its inferior border, anterior to masseter, to enter the face: its further course is described on page 490. The artery is very sinuous throughout its extent. In the neck this may be so that the artery is able to adapt to the movements of the pharynx during deglutition, and similarly on the face, so that the artery can adapt to movements of the mandible, lips and cheeks. Facial artery pulsation is most palpable where the artery crosses the mandibular base, and again near the corner of the mouth. Its branches in the neck are the ascending palatine, tonsillar, submental and glandular arteries.
The ascending palatine artery arises close to the origin of the facial artery. It passes up between styloglossus and stylopharyngeus to reach the side of the pharynx, along which it ascends between the superior constrictor of the pharynx and medial pterygoid towards the cranial base. It bifurcates near levator veli palatini. One branch follows this muscle, winding over the upper border of the superior constrictor of the pharynx to supply the soft palate and to anastomose with its fellow of the opposite side and the greater palatine branch of the maxillary artery. The other branch pierces the superior constrictor muscle to supply the tonsil and pharyngotympanic tube and to anastomose with the tonsillar and ascending pharyngeal arteries.
The tonsillar artery provides the main blood supply to the palatine tonsil. It ascends between medial pterygoid and styloglossus, penetrates the superior constrictor of the pharynx at the upper border of styloglossus, and enters the inferior pole of the tonsil. Its branches ramify in the tonsil and in the musculature of the posterior part of the tongue. The tonsillar artery may sometimes arise from the ascending palatine artery.
The submental artery is the largest cervical branch of the facial artery (Fig. 28.7). It arises as the facial artery separates from the submandibular gland and turns forwards on mylohyoid below the mandible. It supplies the overlying skin and muscles, and anastomoses with a sublingual branch of the lingual and mylohyoid branch of the inferior alveolar artery. At the chin it ascends over the mandible, and divides into superficial and deep branches, which anastomose with the inferior labial and mental arteries to supply the chin and lower lip.
Occipital artery
The occipital artery arises posteriorly from the external carotid artery, approximately 2 cm from its origin (Figs 28.7A, 28.8). At its origin, the artery is crossed superficially by the hypoglossal nerve, which winds round it from behind. The artery next passes backwards, up and deep to the posterior belly of digastric, and crosses the internal carotid artery, internal jugular vein, hypoglossal, vagus and accessory nerves. Between the transverse process of the atlas and the mastoid process, the occipital artery reaches the lateral border of rectus capitis lateralis. It then runs in the occipital groove of the temporal bone, medial to the mastoid process and attachments of sternocleidomastoid, splenius capitis, longissimus capitis and digastric, and lies successively on rectus capitis lateralis, obliquus superior and semispinalis capitis. Finally, accompanied by the greater occipital nerve, it turns upwards to pierce the investing layer of the deep cervical fascia connecting the cranial attachments of trapezius and sternocleidomastoid, and ascends tortuously in the dense superficial fascia of the scalp where it divides into many branches.
The occipital artery has two main branches (upper and lower) to the upper part of sternocleidomastoid in the neck. The lower branch arises near the origin of the occipital artery, and may sometimes arise directly from the external carotid artery. It descends backwards over the hypoglossal nerve and internal jugular vein, enters sternocleidomastoid and anastomoses with the sternocleidomastoid branch of the superior thyroid artery. The upper branch arises as the occipital artery crosses the accessory nerve, and runs down and backwards superficial to the internal jugular vein. It enters the deep surface of sternocleidomastoid with the accessory nerve.
Posterior auricular artery
The posterior auricular artery is a small vessel which branches posteriorly from the external carotid just above digastric and stylohyoid. It ascends between the parotid gland and the styloid process to the groove between the auricular cartilage and mastoid process, and divides into auricular and occipital branches which are described with the face on page 491. In the neck, it provides branches to supply digastric, stylohyoid, sternocleidomastoid and the parotid gland. It also gives origin to the stylomastoid artery – described as an indirect branch of the posterior auricular artery in about a third of subjects – which enters the stylomastoid foramen to supply the facial nerve, tympanic cavity, mastoid antrum air cells and semicircular canals. In the young, its posterior tympanic ramus forms a circular anastomosis with the anterior tympanic branch of the maxillary artery.
Internal carotid artery
The internal carotid artery supplies most of the ipsilateral cerebral hemisphere, eye and accessory organs, forehead and, in part, the nose. From its origin at the carotid bifurcation (Fig. 28.8) (where it usually has a carotid sinus), it ascends in front of the transverse processes of the upper three cervical vertebrae to the inferior aperture of the carotid canal in the petrous part of the temporal bone. Here it enters the cranial cavity and turns anteriorly through the cavernous sinus in the carotid groove on the side of the body of the sphenoid bone. It terminates below the anterior perforated substance by division into the anterior and middle cerebral arteries. It may be divided conveniently into cervical, petrous, cavernous and cerebral parts.
The internal carotid artery is initially superficial in the carotid triangle, then passes deeper, medial to the posterior belly of digastric. Except near the skull, the internal jugular vein and vagus nerve are lateral to it within the carotid sheath. The external carotid artery is first anteromedial, but then curves back to lie superficial. Posteriorly the internal carotid adjoins longus capitis, and the superior cervical sympathetic ganglion lies between them. The superior laryngeal nerve crosses obliquely behind it. The pharyngeal wall lies medial to the artery, which is separated by fat and pharyngeal veins from the ascending pharyngeal artery and superior laryngeal nerve. Anterolaterally the internal carotid artery is covered by sternocleidomastoid. Below the posterior belly of digastric, the hypoglossal nerve and superior root of the ansa cervicalis and the lingual and facial veins are superficial to the artery. At the level of the digastric, the internal carotid is crossed by stylohyoid and the occipital and posterior auricular arteries. Above the digastric it is separated from the external carotid artery by the styloid process, styloglossus and stylopharyngeus, the glossopharyngeal nerve and the pharyngeal branch of the vagus, and the deeper part of the parotid gland. At the base of the skull the glossopharyngeal, vagus, accessory and hypoglossal nerves lies between the internal carotid artery and the internal jugular vein, which here has become posterior. The length of the artery varies with the length of the neck and the point of the carotid bifurcation. It may arise from the aortic arch in which case it lies medial to the external carotid as far as the larynx, where it crosses behind it. The cervical portion is normally straight but may be very tortuous, when it lies closer to the pharynx than usual, very near the tonsil. The internal carotid artery enters the cranium without giving off any branches. It may occasionally be absent.
Occlusive atherosclerotic disease within either the internal carotid or common carotid artery may cause strokes or transient ischaemic attacks (TIAs) characterized by weakness of the contralateral side. It may also result in visual disturbances characterized classically as a ‘curtain’ falling down over the visual field (amaurosis fugax). These episodes will be experienced in the ipsilateral eye.
Carotid sinus and carotid body
The common carotid artery shows two specialized organs near its bifurcation, the carotid sinus and the carotid body. They relay information concerning the pressure and chemical composition of the arterial blood respectively, and are innervated principally by carotid branch(es) of the glossopharyngeal nerve, with small contributions from the cervical sympathetic trunk and the vagus nerve.
The carotid sinus usually appears as a dilation of the lower end of the internal carotid, and functions as a baroreceptor.
The carotid body is a reddish-brown, oval structure, 5–7 mm in height and 2.5–4 mm in width. It lies either posterior to the carotid bifurcation or between its branches, and is attached to, or sometimes partly embedded in, their adventitia. Occasionally it takes the form of a group of separate nodules. Aberrant miniature carotid bodies, microstructurally similar but with diameters of 600 μm or less, may appear in the adventitia and adipose tissue near the carotid sinus.
The carotid body is surrounded by a fibrous capsule from which septa divide the enclosed tissue into lobules. Each lobule contains glomus (type I) cells which are separated from an extensive network of fenestrated sinusoids by sustentacular (type II) cells (Fig. 28.9). Glomus cells store a number of peptides, particularly enkephalins, bombesin and neurotensin, and amines including dopamine, serotonin, adrenaline (epinephrine) and noradrenaline (norepinephrine), and are therefore regarded as paraneurones. Unmyelinated axons lie in a collagenous matrix between the sustentacular cells and the sinusoidal endothelium, and many synapse on the glomus cells. They are visceral afferents which travel in the carotid sinus nerve to join the glossopharyngeal nerve. Preganglionic sympathetic axons and fibres from the carotid sinus synapse on parasympathetic and sympathetic ganglion cells, which lie either in isolation or in small groups near the surface of each carotid body. Postganglionic axons travel to local blood vessels: the parasympathetic efferent fibres are probably vasodilatory and the sympathetic ones are vasoconstrictor.
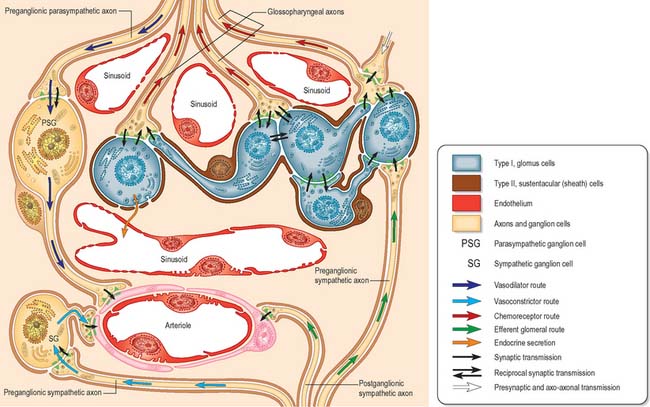
Fig. 28.9 The cellular, neural and vascular architecture of the carotid body: functional pathways are indicated.
The carotid body receives a rich blood supply from branches of the adjacent external carotid artery, which is consistent with its role as an arterial chemoreceptor. When stimulated by hypoxia, hypercapnia or increased hydrogen ion concentration (low pH) in the blood flowing through it, it elicits reflex increases in the rate and volume of ventilation via connections with brain stem respiratory centres. The bodies are most prominent in children and normally involute in older age, when they are infiltrated by lymphocytes and fibrous tissue. Individuals with chronic hypoxia, or who live at high altitude or suffer from lung disease, may have enlarged carotid bodies as a result of hyperplasia.
Other small bodies, resembling carotid bodies, and also considered to be chemoreceptors, occur near the arteries of the fourth and sixth pharyngeal arches and hence are found near the aortic arch, ligamentum arteriosum and right subclavian artery, and are supplied by the vagus nerve.
Subclavian artery
The right subclavian artery arises from the brachiocephalic trunk, the left from the aortic arch (see Figs 28.14, 28.18). For description, each is divided into a first part, from its origin to the medial border of scalenus anterior, a second part behind this muscle and a third part from the lateral margin of scalenus anterior to the outer border of the first rib, where the artery becomes the axillary artery. Each subclavian artery arches over the cervical pleura and pulmonary apex. Their first parts differ, whereas the second and third parts are almost identical.
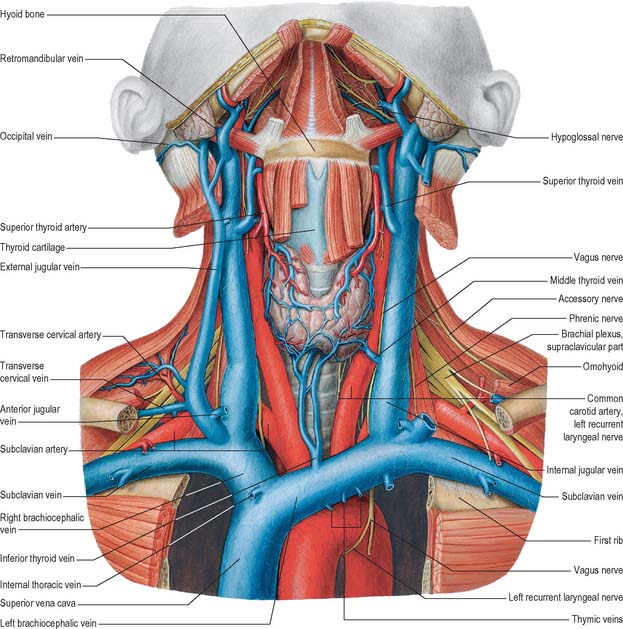
Fig. 28.14 The veins of the neck, seen from the front and at a deeper level than Fig. 28.13. Both sternocleidomastoids have been removed and additional dissection has exposed the thyroid gland and some of the structures that pass through the upper thoracic aperture.
(From Sobotta 2006.)
Parts of the subclavian arteries
First part of right subclavian artery
The right subclavian artery branches from the brachiocephalic trunk behind the upper border of the right sternoclavicular joint, and passes superolaterally to the medial margin of scalenus anterior. It usually ascends 2 cm above the clavicle, but this varies.
The artery is deep to the skin, superficial fascia, platysma, supraclavicular nerves, deep fascia, clavicular attachment of sternocleidomastoid, sternohyoid and sternothyroid. It is at first behind the origin of the right common carotid artery; more laterally it is crossed by the vagus nerve, the cardiac branches of the vagus and the sympathetic chain and by internal jugular and vertebral veins; the subclavian sympathetic loop encircles it. The anterior jugular vein diverges laterally in front of it, separated by sternohyoid and sternothyroid. Below and behind the artery are the pleura and pulmonary apex: they are separated from the artery by the suprapleural membrane, the ansa subclavia, a small accessory vertebral vein and the right recurrent laryngeal nerve which winds round the lower and posterior part of the vessel.
First part of left subclavian artery
The first part of the left subclavian artery springs from the aortic arch, behind the left common carotid, level with the disc between the third and fourth thoracic vertebrae. It ascends into the neck, then arches laterally to the medial border of scalenus anterior.
In the neck, near the medial border of scalenus anterior, the artery is crossed anteriorly by the left phrenic nerve and the termination of the thoracic duct. Otherwise anterior relations are the same as those of the first part of the right subclavian artery. Posteriorly and inferiorly, the relations of both vessels are identical but the left recurrent laryngeal nerve, medial to the left subclavian artery in the thorax, is not directly related to its cervical part.
Second part of subclavian artery
The second part of the subclavian artery lies behind scalenus anterior; it is short and the highest part of the vessel (see Fig. 28.18).
The skin, superficial fascia, platysma, deep cervical fascia, sternocleidomastoid and scalenus anterior are anterior. The right phrenic nerve is often described as being separated from the second part of the subclavian artery by scalenus anterior, whereas it crosses the first part of the left subclavian artery. However, both nerves may sometimes lie anterior to the muscle. The suprapleural membrane, pleura and lung and the lower trunk of the brachial plexus are posteroinferior; the upper and middle trunks of the plexus are superior; the subclavian vein is anteroinferior, separated by scalenus anterior.
Third part of subclavian artery
The third part of the subclavian artery descends laterally from the lateral margin of scalenus anterior to the outer border of the first rib, where it becomes the axillary artery. It is the most superficial part of the artery and lies partly in the supraclavicular triangle, where its pulsations may be felt and it may be compressed. The third part of the subclavian artery is the most accessible segment of the artery. Since the line of the posterior border of sternocleidomastoid approximates to the (deeper) lateral border of scalenus anterior, the artery can be felt in the anteroinferior angle of the posterior triangle. It can only be effectively compressed against the first rib: with the shoulder depressed, pressure is exerted down, back and medially in the angle between sternocleidomastoid and the clavicle. The palpable trunks of the brachial plexus may be injected with local anaesthetic allowing major surgical procedures to the arm.
The skin, superficial fascia, platysma, supraclavicular nerves and deep cervical fascia are anterior. The external jugular vein crosses its medial end and here receives the suprascapular, transverse cervical and anterior jugular veins, which collectively often form a venous plexus. The nerve to subclavius descends between the veins and the artery; the latter is terminally behind the clavicle and subclavius, where it is crossed by the suprascapular vessels. The subclavian vein is anteroinferior and the lower trunk of the brachial plexus is posteroinferior, between the subclavian artery and the scalenus medius (and on the first rib). The upper and middle trunks of the brachial plexus (which are palpable here) and the inferior belly of omohyoid are superolateral. The first rib is inferior.
The right subclavian artery may arise above or below sternoclavicular level; it may be a separate aortic branch and be the first or last branch of the arch. When it is the first branch, it is in the position of a brachiocephalic trunk. When it is the last branch, it arises from the left end of the arch, and ascends obliquely to the right behind the trachea, oesophagus and right common carotid to the first rib. When this occurs, the right recurrent laryngeal nerve hooks round the common carotid artery. Sometimes, when the right subclavian artery is the last aortic branch, it passes between the trachea and oesophagus and can cause dysphagia, a condition known as dysphagia lusoria. It may perforate scalenus anterior, and very rarely may pass anterior to it. Sometimes the subclavian vein accompanies the artery behind scalenus anterior. The artery may ascend as high as 4 cm above the clavicle or it may reach only its upper border. The left subclavian artery is occasionally combined at its origin with the left common carotid artery.
Vertebral artery
The vertebral artery arises from the superoposterior aspect of the first part of the subclavian artery. It passes through the foramina in the transverse processes of all of the cervical vertebrae except the seventh, curves medially behind the lateral mass of the atlas and enters the cranium via the foramen magnum (Fig. 28.11). At the lower pontine border it joins its fellow to form the basilar artery. Occasionally it may enter the cervical vertebral column via the fourth, fifth or seventh cervical vertebra (Fig. 28.10).
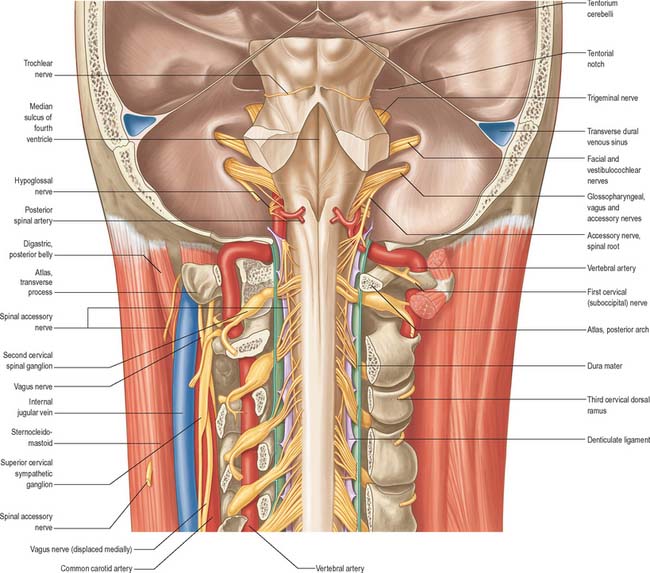
Fig. 28.11 A dissection of the brain stem and the upper part of the spinal cord after removal of large portions of the occipital and parietal bones, the cerebellum and the roof of the fourth ventricle. On the left side, the foramina transversaria of the atlas and the third, fourth and fifth cervical vertebrae have been opened to expose the vertebral artery. On the right side the posterior arch of the atlas and the laminae of the succeeding cervical vertebrae have been divided and have been removed together with the vertebral spines and the contralateral laminae. The tentorium cerebelli and the transverse sinuses have been divided and their posterior portions removed.
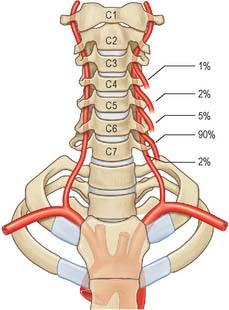
Fig. 28.10 The level of entry of the vertebral artery into the foramina transversaria of the cervical vertebrae. Note that 90% enter at the level of the sixth cervical vertebra.
(Redrawn with permission from Sobotta 2006.)
The first part passes back and upwards between longus colli and scalenus anterior, behind the common carotid artery and the vertebral vein. It is crossed by the inferior thyroid artery, and by the thoracic duct on the left side and the right lymphatic duct on the right side. The seventh cervical transverse process, the inferior cervical ganglion and ventral rami of the seventh and eighth cervical spinal nerves lie posterior to the artery. The second part ascends through the transverse foramina of the remaining cervical vertebrae, accompanied by a large branch from the inferior cervical ganglion and a plexus of veins which form the vertebral vein low in the neck. It lies anterior to the ventral rami of the cervical spinal nerves (C.2–C.6), and ascends almost vertically to pass through the transverse process of the axis, where it turns laterally to gain access to the transverse foramen of the atlas (Fig. 28.11). The third part issues medial to rectus capitis lateralis, and curves backwards and medially behind the lateral mass of the atlas, with the first cervical ventral spinal ramus lying on its medial side. In this position it lies in a groove on the upper surface of the posterior arch of the atlas, and it enters the vertebral canal below the inferior border of the posterior atlanto-occipital membrane. This part of the artery, covered by semispinalis capitis, lies in the suboccipital triangle. The first cervical dorsal spinal ramus separates the artery from the posterior arch. The fourth part pierces the dura and arachnoid mater, and ascends anterior to the hypoglossal roots. It inclines anterior to the medulla oblongata and unites with its contralateral fellow to form the midline basilar artery at the lower border of the pons.
Cervical branches of the vertebral artery
The spinal branches enter the vertebral canal via the intervertebral foramina, and supply the spinal cord and its membranes. They fork into ascending and descending rami, which unite with those above and below, to form two lateral anastomotic chains on the posterior surfaces of the vertebral bodies near the attachment of their pedicles. Branches from these chains supply the periosteum and vertebral bodies, and others communicate with similar branches across the midline; from these connections small rami join similar ones above and below, to form a median anastomotic chain on the posterior surfaces of the vertebral bodies.
Internal thoracic artery
The internal thoracic artery arises inferiorly from the first part of the subclavian artery, 2 cm above the sternal end of the clavicle, opposite the root of the thyrocervical trunk.
Thyrocervical trunk
The thyrocervical trunk is a short wide artery which arises from the front of the first part of the subclavian artery near the medial border of scalenus anterior, and divides almost at once into the inferior thyroid, suprascapular and superficial cervical arteries.
Inferior thyroid artery
The inferior thyroid artery loops upwards anterior to the medial border of the scalenus anterior, turns medially just below the sixth cervical transverse process, then descends on longus colli to the lower border of the thyroid gland (Figs 28.7A, 28.17). It passes anterior to the vertebral vessels and posterior to the carotid sheath and its contents (and usually the sympathetic trunk, whose middle cervical ganglion frequently adjoins the vessel). On the left, near its origin, the artery is crossed anteriorly by the thoracic duct as the latter curves inferolaterally to its termination. Relations between the terminal branches of the artery and recurrent laryngeal nerve are very variable and of considerable surgical importance. The artery usually passes behind the nerve as it nears the gland. However, very close to the gland, the right nerve is equally likely to be anterior, posterior or amongst, the branches of the artery, and the left nerve is usually posterior. The artery is not accompanied by the inferior thyroid vein.
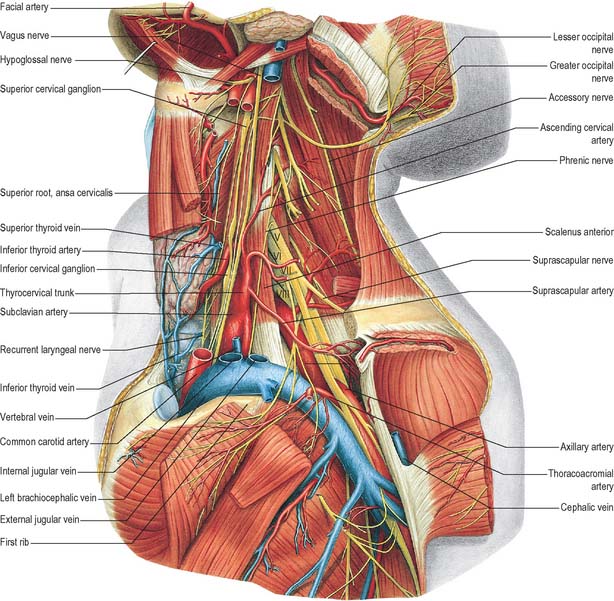
Fig. 28.17 Vessels and nerves of the neck, left lateral view. The left sternocleidomastoid, the greater part of the infrahyoid group of muscles and numerous vessels have been removed in order to expose deeper structures. Compare with Fig. 28.7A, which shows a more superficial level of dissection. V, VI, VII, VIII refer to the anterior primary rami of C5, C6, C7, and C8, respectively.
(From Sobotta 2006.)
These supply the infrahyoid muscles, longus colli, scalenus anterior and the inferior pharyngeal constrictor.
The ascending cervical artery is a small branch which arises as the inferior thyroid turns medially behind the carotid sheath and ascends on the anterior tubercles of the cervical transverse processes between scalenus anterior and longus capitis. It supplies the adjacent muscles and gives off one or two spinal branches which enter the vertebral canal through the intervertebral foramina to supply the spinal cord and membranes and vertebral bodies, and thereby supplement the spinal branches of the vertebral artery. The ascending cervical artery anastomoses with the vertebral, ascending pharyngeal, occipital and deep cervical arteries.
The inferior laryngeal artery ascends on the trachea with the recurrent laryngeal nerve, enters the larynx at the lower border of the inferior constrictor and supplies the laryngeal muscles and mucosa. It anastomoses with its contralateral fellow, and with the superior laryngeal branch of the superior thyroid artery.
These supply the lower part of the pharynx. Tracheal branches supply the trachea and anastomose with the bronchial arteries; oesophageal branches supply the oesophagus and anastomose with the oesophageal branches of the thoracic aorta; inferior and ascending glandular branches supply the posterior and inferior regions of the thyroid gland, and anastomose with the contralateral inferior and ipsilateral superior thyroid arteries. The ascending branch also supplies the parathyroid glands.
Suprascapular artery
The suprascapular artery descends laterally across scalenus anterior and the phrenic nerve, posterior to the internal jugular vein and sternocleidomastoid (Fig. 28.7A). It then crosses anterior to the subclavian artery and brachial plexus, posterior to, and parallel with, the clavicle, subclavius and the inferior belly of omohyoid, to reach the superior scapular border.
Superficial cervical artery
The superficial cervical artery is given off at a higher level than the suprascapular artery. It crosses anterior to the phrenic nerve, scalenus anterior and the brachial plexus and is covered by the internal jugular vein, sternocleidomastoid and platysma. It crosses the floor of the posterior triangle to reach the anterior margin of levator scapulae, and ascends deep to the anterior part of the trapezius, which it supplies, together with the adjoining muscles and the cervical lymph nodes. It anastomoses with the superficial ramus of the descending branch of the occipital artery. About a third of the superficial cervical and dorsal scapular arteries arise in common from the thyrocervical trunk, with a superficial (superficial cervical artery) and a deep (dorsal scapular artery) branch (see Figs 25.1, 25.2 and 46.26). The latter passes laterally anterior to the brachial plexus and then posterior to levator scapulae.
Costocervical trunk
On the right, this short vessel arises posteriorly from the second part of the subclavian artery, and, on the left, from its first part. It arches back above the cervical pleura to the neck of the first rib, where it divides into superior intercostal and deep cervical branches.
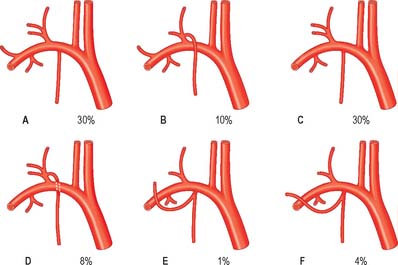
Fig. 28.12 Variations in the origins of the inferior thyroid, suprascapular, transverse cervical and internal thoracic arteries.
(Redrawn with permission from Sobotta 2006.)
Deep cervical artery
The deep cervical artery usually arises from the costocervical trunk (see Fig. 25.1). It is analogous in its first segment to a posterior branch of a posterior intercostal artery, and occasionally is a separate branch of the subclavian artery. It passes back above the eighth cervical spinal nerve between the transverse process of the seventh cervical vertebra and the neck of the first rib (sometimes between the transverse processes of the sixth and seventh cervical vertebrae). It then ascends between semispinales capitis and cervicis to the level of the second cervical vertebra. It supplies adjacent muscles and anastomoses with the deep branch of the descending branch of the occipital artery and branches of the vertebral artery. A spinal branch enters the vertebral canal between the seventh cervical and first thoracic vertebrae.
Dorsal scapular artery
The dorsal scapular artery arises from the third, or less often the second, part of the subclavian artery. It gives off a small branch (which sometimes arises directly from the subclavian artery), to scalenus anterior. It passes laterally through the brachial plexus in front of scalenus medius and then deep to levator scapulae to the superior scapular angle.
VEINS OF THE NECK
Veins in the neck show considerable variation. They are superficial or deep to the deep fascia but are not entirely separate systems. Superficial veins are tributaries, some with specific names, given below, of the anterior, external and posterior jugular veins (Figs 28.13, 28.14). They drain a much smaller volume of tissue than the deep veins. The latter drain all but the subcutaneous structures, mostly into the internal jugular vein and also into the subclavian vein.
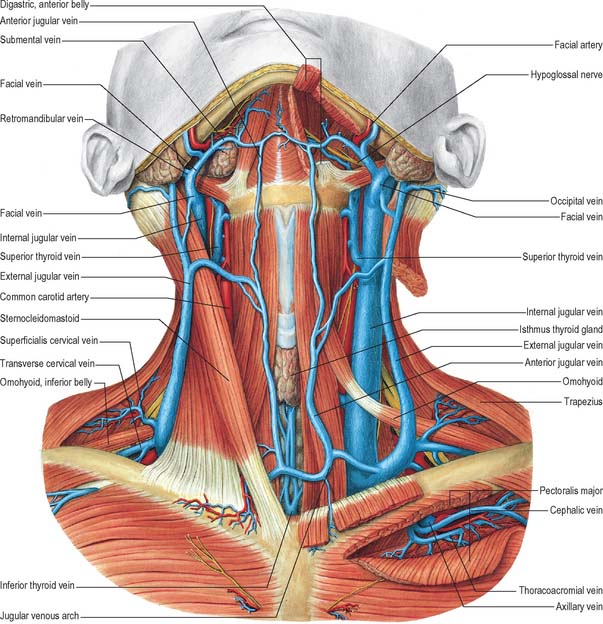
Fig. 28.13 The veins of the neck, seen from the front. The greater part of sternocleidomastoid has been removed on the left side and the cut lower edges have been reflected over the clavicle.
(From Sobotta 2006.)
External jugular vein
The external jugular vein mainly drains the scalp and face, although it also drains some deeper parts. The vein is formed by the union of the posterior division of the retromandibular vein with the posterior auricular vein and begins near the mandibular angle just below or in the parotid gland (see Fig. 25.3). It descends from the angle to the midclavicle, running obliquely, superficial to sternocleidomastoid, to the root of the neck. Here it crosses the deep fascia and ends in the subclavian vein, lateral or anterior to scalenus anterior. There are valves at its entrance into the subclavian, but they do not prevent regurgitation. Its wall is adherent to the rim of the fascial opening. It is covered by platysma, superficial fascia and skin, and is separated from sternocleidomastoid by deep cervical fascia. The vein crosses the transverse cutaneous nerve and lies parallel with the great auricular nerve, posterior to its upper half. In size the external jugular vein is inversely proportional to the other veins in the neck, and may be double. Between the entrance into the subclavian vein and a point approximately 4 cm above the clavicle, the vein is often dilated, producing a so-called sinus.
In addition to formative tributaries, the external jugular receives the posterior external jugular and, near its end, transverse cervical, suprascapular and anterior jugular veins. In the parotid gland it is often joined by a branch from the internal jugular. The occipital vein occasionally joins it.
Posterior external jugular vein
The posterior external jugular vein begins in the occipital scalp, and drains the skin and the superficial muscles which lie posterosuperior in the neck. It usually joins the middle part of the external jugular vein.
Anterior jugular vein
The anterior jugular vein arises near the hyoid bone from the confluence of the superficial submandibular veins. It descends between the midline and the anterior border of sternocleidomastoid. Turning laterally, low in the neck, deep to sternocleidomastoid but superficial to the infrahyoid strap muscles, it joins either the end of the external jugular vein or may enter the subclavian vein directly. In size it is usually inverse to the external jugular vein. It communicates with the internal jugular vein, and receives the laryngeal veins and sometimes a small thyroid vein. There are usually two anterior jugular veins, united just above the manubrium by a large transverse jugular arch, receiving the inferior thyroid tributaries. They have no valves and may be replaced by a midline trunk.
Internal jugular vein
The internal jugular vein collects blood from the skull, brain, superficial parts of face and much of the neck. It begins at the cranial base in the posterior compartment of the jugular foramen, where it is continuous with the sigmoid sinus. At its origin it is dilated as the superior bulb, which lies below the posterior part of the tympanic floor. The internal jugular vein descends in the carotid sheath, and unites with the subclavian vein, posterior to the sternal end of the clavicle, to form the brachiocephalic vein (Fig. 28.14). Near its termination the vein dilates into the inferior bulb, above which is a pair of valves.
From above, rectus capitis lateralis, the transverse process of the atlas, levator scapulae, scalenus medius, scalenus anterior, the cervical plexus, the phrenic nerve, thyrocervical trunk, vertebral vein and the first part of the subclavian artery all lie posterior to the vein. On the left, the internal jugular crosses anterior to the thoracic duct. The internal and common carotid arteries and the vagus nerve are medial to the vein: the nerve lies between vein and arteries but posterior to them. Superficially the internal jugular vein is overlapped above, then covered below, by sternocleidomastoid and is crossed by the posterior belly of digastric and the superior belly of omohyoid. Superior to digastric the parotid gland, styloid process, accessory nerve, and posterior auricular and occipital arteries cross the vein. Between digastric and omohyoid, the sternocleidomastoid arteries and inferior root of the ansa cervicalis cross it, although the nerve often passes between the vein and the common carotid artery. Below omohyoid, the vein is covered by the infrahyoid muscles and sternocleidomastoid and is crossed by the anterior jugular vein. Deep cervical lymph nodes lie along the internal jugular, mainly on its superficial aspect. At the root of the neck the right internal jugular vein is separated from the common carotid artery, but the left usually overlaps its artery. At the base of the skull the internal carotid artery is anterior to the vein, separated from it by the ninth to 12th cranial nerves.
The inferior petrosal sinus, facial, lingual, pharyngeal, superior and middle thyroid veins, and occasionally the occipital vein, are all tributaries of the internal jugular vein. The internal jugular vein may communicate with the external jugular vein. The thoracic duct opens near the union of the left subclavian and internal jugular veins, and the right lymphatic duct opens at the same site on the right.
Inferior petrosal sinus
The inferior petrosal sinus leaves the skull through the anterior part of the jugular foramen, crosses lateral or medial to the ninth to eleventh cranial nerves and joins the superior jugular bulb.
Facial vein
The initial part of the facial vein as it lies on the face is described on page 492. From the face it passes over the surface of masseter, crosses the body of the mandible and enters the neck where it runs obliquely back under platysma. Here it lies superficial to the submandibular gland, digastric and stylohyoid (Fig. 28.14). Just anteroinferior to the mandibular angle it is joined by the anterior division of the retromandibular vein, and then descends superficial to the loop of the lingual artery, the hypoglossal nerve and external and internal carotid arteries, to enter the internal jugular near the greater cornu of the hyoid bone, i.e. in the upper angle of the carotid triangle. Near its end a large branch often descends along the anterior border of sternocleidomastoid to the anterior jugular vein. Its uppermost segment, above its junction with the superior labial vein, is often termed the angular vein.
Lingual vein
The lingual veins follow two routes. The dorsal lingual veins drain the dorsum and sides of the tongue, join the lingual veins accompanying the lingual artery between hyoglossus and genioglossus and enter the internal jugular near the greater cornu of the hyoid bone. The deep lingual vein begins near the tip of the tongue and runs back, lying near the mucous membrane on the inferior surface of the tongue. Near the anterior border of hyoglossus it joins a sublingual vein, from the sublingual salivary gland, to form the vena comitans nervi hypoglossi which runs back between mylohyoid and hyoglossus with the hypoglossal nerve to join the facial, internal jugular or lingual vein.
Pharyngeal veins
The pharyngeal veins begin in a pharyngeal plexus external to the pharynx. They receive meningeal veins and a vein from the pterygoid canal, and usually end in the internal jugular vein, but may sometimes end in the facial, lingual or superior thyroid vein.
Superior thyroid vein
The superior thyroid vein is formed by deep and superficial tributaries corresponding to the arterial branches in the upper part of the thyroid gland (Figs 28.13, 28.14). It accompanies the superior thyroid artery, receives the superior laryngeal and cricothyroid veins, and ends in the internal jugular or facial vein.
Middle thyroid vein
The middle thyroid vein drains the lower part of the gland and also receives veins from the larynx and trachea. It crosses anterior to the common carotid artery to join the internal jugular vein behind the superior belly of omohyoid.
Tympanic body
The tympanic body (glomus jugulare) is ovoid, 0.5 mm long and 0.25 mm broad, and lies in the adventitia of the upper part of the superior bulb of the internal jugular vein. It is similar in structure to the carotid body and is presumed to have a similar function. The predominant cell type has morphological similarities to adrenal chromaffin cells, and is derived from the neural crest. Cells obtained from glomus jugulare paragangliomas show spontaneous neurite outgrowth in culture, and have vasoactive intestinal peptide (VIP)-like activity. The tympanic body may be present as two or more parts near the tympanic branch of the glossopharyngeal nerve or the auricular branch of the vagus as they lie within their canals in the petrous part of the temporal bone. Tumours of tympanic bodies may involve the adjacent cranial nerves and the middle ear.
Subclavian vein
The subclavian vein is a continuation of the axillary vein and extends from the outer border of the first rib to the medial border of scalenus anterior, where it joins the internal jugular vein to form the brachiocephalic vein (Fig. 28.14). The clavicle and subclavius lie anterior to it, the subclavian artery is posterosuperior, separated by scalenus anterior and the phrenic nerve, and the first rib and pleura are inferior. The vein usually has a pair of valves 2 cm from its end. Its tributaries are the external jugular, dorsal scapular and sometimes the anterior jugular vein. At its junction with the internal jugular, the left subclavian vein receives the thoracic duct, and the right subclavian vein receives the right lymphatic duct.
Vertebral vein
Numerous small tributaries from internal vertebral plexuses leave the vertebral canal above the posterior arch of the atlas and join small veins from local deep muscles in the suboccipital triangle. Their union produces a vessel which enters the foramen in the transverse process of the atlas and forms a plexus around the vertebral artery. It descends through successive transverse foramina and ends as the vertebral vein. The vein emerges from the sixth cervical transverse foramen, whence it descends, at first anterior, then anterolateral, to the vertebral artery, to open superoposteriorly into the brachiocephalic vein: the opening has a paired valve. As it descends it passes behind the internal jugular vein and in front of the first part of the subclavian artery. A small accessory vertebral vein usually descends from the vertebral plexus, traverses the seventh cervical transverse foramen and turns forwards between the subclavian artery and the cervical pleura to join the brachiocephalic vein.
The vertebral vein connects with the sigmoid sinus by a vessel in the posterior condylar canal, when this exists. It also receives branches from the occipital vein, prevertebral muscles, internal and external vertebral plexuses. It is joined by anterior vertebral and deep cervical veins (see below) and, sometimes near its end, by the first intercostal vein.
Anterior vertebral vein
The anterior vertebral vein starts in a plexus around the upper cervical transverse processes, descends near the ascending cervical artery between attachments of scalenus anterior and longus capitis, and opens into the end of the vertebral vein.
Deep cervical vein
The deep cervical vein accompanies its artery between semispinales capitis and cervicis. It is formed in the suboccipital region by the union of communicating branches of the occipital vein; veins from suboccipital muscles; and veins from plexuses around the cervical spines. It passes forwards between the seventh cervical transverse process and the neck of the first rib to end in the lower part of the vertebral vein.
Central venous access
Central venous cannulation permits monitoring of the central venous pressure and the administration of drugs directly into the central circulation.
Internal jugular vein cannulation
The patient is placed in the supine position with the head turned slightly towards the contralateral side. The key anatomical landmarks are the two inferior heads of sternocleidomastoid, which form two sides of a triangle with the clavicle as its base. The internal jugular vein lies between the two heads of the muscle, slightly lateral and anterior to the common carotid artery. After the skin has been prepared, local anaesthetic is injected around the apex of the triangle. With one hand palpating the carotid artery, the physician inserts a needle at the apex of the triangle and the tip is directed lateral to the midpoint of the triangle, with a downward angulation of 30°. From a high internal jugular approach, the needle is inserted at the midpoint of the medial border of sternocleidomastoid and directed towards the ipsilateral nipple with a downward angulation of 30–45°. When the left internal jugular vein is cannulated, additional care must be taken to avoid the thoracic duct and the cupula of the pleura, which is higher than on the right side, an arrangement which increases the risk of accidental pneumothorax. The left internal jugular vein is often smaller in diameter than the right.
Subclavian vein cannulation
Subclavian vein cannulation is performed with the patient supine, the head turned slightly to the opposite side, and the arms placed by the side. The bed is tilted down by 10° and a small bedroll may be placed between the shoulder blades in order to ensure that the infraclavicular area is more prominent. The skin is cleaned and local anaesthetic injected into the skin 3 cm lateral to the midpoint of the clavicle. The central venous needle is then inserted from the inferior edge of the clavicle towards the suprasternal notch. The needle is directed so that it passes just below the posterior border of the clavicle; care must be taken to avoid downward direction of the needle, which may cause a pneumothorax. Gentle aspiration of the syringe is performed whilst the needle is being advanced until the subclavian vein is punctured.
CERVICAL GROUPS OF LYMPH NODES
Lymph nodes in the head and neck are distributed in terminal and outlying groups (Fig. 28.15; see Fig. 25.5). The terminal group is related to the carotid sheath and the nodes it contains are the deep cervical lymph nodes. All lymph vessels of the head and neck drain into this group, either directly from tissues or indirectly through nodes in the outlying groups. Efferents of the deep cervical nodes form the jugular trunk. The right jugular trunk collects lymph from the right arm and right half of the thorax and the right head and neck and may end in the jugulosubclavian junction or the right lymphatic duct. The left jugular trunk usually enters the thoracic duct, but it may join the internal jugular or subclavian vein.
Lymphatic drainage of the neck
Many vessels draining the superficial cervical tissues skirt the borders of sternocleidomastoid to reach the superior or inferior deep cervical nodes. Others pass to the superficial cervical and occipital nodes. Lymph from the superior region of the anterior triangle drains to the submandibular and submental nodes. Vessels from the anterior cervical skin inferior to the hyoid bone pass to the anterior cervical lymph nodes near the anterior jugular veins. Their efferents go to the deep cervical nodes of both sides, including the infrahyoid, prelaryngeal and pretracheal groups. An anterior cervical node often occupies the suprasternal space. Lymph from tissues of the head and neck internal to the deep fascia drains to the deep cervical nodes directly or through outlying groups that include the retropharyngeal, paratracheal, lingual, infrahyoid, prelaryngeal and pretracheal groups. The lymphatic drainage associated with the nasal region, larynx and oral cavity is described in the appropriate regions. The deep cervical lymphatic nodes lie alongside the carotid sheath, and form superior and inferior groups.
The superior deep cervical nodes adjoin the upper part of the internal jugular vein. Most are deep to sternocleidomastoid, but a few extend beyond it. One subgroup, consisting of one large and several small nodes, is in a triangular region bounded by the posterior belly of digastric and the facial and internal jugular veins, and is known as the jugulodigastric group. It is concerned specially with drainage of the tongue. Efferents from the upper deep cervical nodes drain either to the lower group or direct to the jugular trunk.
The inferior deep cervical nodes are partly deep to the sternocleidomastoid, and are particularly related to the lower part of the internal jugular vein. Some are closely related to the brachial plexus and subclavian vessels. The jugulo-omohyoid node lies on, or just above, the intermediate tendon of omohyoid, and is concerned especially with lymphatic drainage from the tongue. Efferents from this lower group join the jugular lymph trunk.
Retropharyngeal nodes lie between the pharyngeal and prevertebral fasciae and form a median and two lateral groups, the latter anterior to the lateral masses of the atlas along the lateral borders of longus capitis. The nodes receive afferents from the nasopharynx, pharyngotympanic tube and atlanto-occipital and atlanto-axial joints and drain to the upper deep cervical nodes.
The paratracheal nodes flank both trachea and oesophagus along the recurrent laryngeal nerves. Efferents pass to the corresponding deep cervical nodes.
Infrahyoid, prelaryngeal and pretracheal nodes
The infrahyoid, prelaryngeal and pretracheal nodes lie beneath the deep cervical fascia. They drain afferents from the anterior cervical nodes, and their efferents join the deep cervical nodes. Infrahyoid nodes are anterior to the thyrohyoid membrane, prelaryngeal nodes lie on the cricovocal membrane, and pretracheal nodes lie anterior to the trachea near the inferior thyroid veins.
Spread of malignant disease in the neck
Cancers arising in the head and neck from regions such as the thyroid gland, larynx, oral cavity and oropharynx, nasopharynx and paranasal sinuses have predictable patterns of spread through the chains of lymph nodes in the neck. When operating on malignant disease in this region it is vitally important to understand these patterns of spread so that for any individual cancer the appropriate operation is undertaken. Clinical experience has shown that the lymph nodes in the neck fall into five distinct groups (see Fig. 25.5). Level I nodes lie in the submandibular triangle bounded by the anterior and posterior bellies of digastric and the lower border of the mandible above. Level II (upper jugular) nodes lie around the upper portion of the internal jugular vein and the upper part of the spinal accessory nerve. They extend from the skull base to the bifurcation of the common carotid artery or the hyoid bone. Level III (middle jugular) nodes lie around the middle third of the internal jugular vein from the inferior border of level II to the superior belly of omohyoid or cricothyroid membrane. Level IV (lower jugular) nodes lie around the lower third of the internal jugular vein from the inferior border of level III to the clavicle. The anterior and posterior borders for levels II, III and IV are the lateral border of sternohyoid and the posterior border of sternocleidomastoid respectively. Level V (posterior triangle) nodes lie around the lower part of the spinal accessory nerve and the transverse cervical vessels.
Knowing which levels of nodes are likely to be involved in the metastatic spread of a particular cancer arising in the head and neck means that appropriate nodal clearance can be undertaken. The classic radical neck dissection first described by Crile in 1906 involves a thorough clearance of levels I to V including the sacrifice of sternocleidomastoid, the internal jugular vein and the spinal accessory nerve. Modified radical neck dissections (so-called functional neck dissections) still remove level I to V nodes, but spare either or all of sternocleidomastoid, the internal jugular vein and the spinal accessory. Selective neck dissections remove selected groups of nodes, e.g. the supraomohyoid neck dissection removes level I to III nodes, the lateral neck dissection removes level II to IV nodes, and the posterolateral neck dissection removes level II to V nodes.
Cervical lymphovenous portals
Lymph is returned to the systemic venous circulation via right and left lymphovenous portals sited at, or near, the junctions of the internal jugular and subclavian veins (Fig. 28.16). The arrangement of these terminations is variable. Usually, three small lymph trunks converge towards their venous junctions on either side of the body, and they are joined, on the left side only, by the larger thoracic duct.
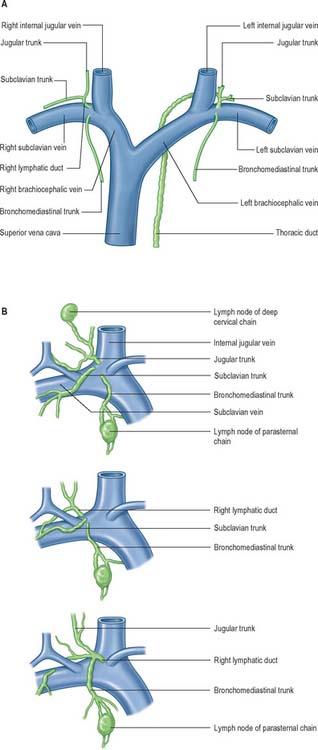
Fig. 28.16 A, The termination of the right lymphatic trunk and the thoracic duct.
(From Drake, Vogl and Mitchell 2005.) B, Variations in the terminal lymphatic trunks nodes of the right side.
On the right side, the three trunks are the right jugular, right subclavian and right bronchomediastinal. The right jugular trunk extends from the terminal lower deep cervical nodes along the ventrolateral aspect of the internal jugular vein, and conveys all the lymph from the right half of the head and neck. The right subclavian trunk drains from the terminal apical axillary group. It extends along the axillary and subclavian veins, and conveys lymph from the right upper limb and superficial tissues of the right half of the thoracoabdominal wall, down to the umbilicus anteriorly and iliac crest posteriorly (and includes much of the breast). The right bronchomediastinal trunk, ascends over the trachea towards the lymphovenous portal and conveys lymph from the thoracic walls, the right cupola of the diaphragm and subjacent liver, the right lung, bronchi and trachea, the greater part of the ‘right heart’ – of clinical parlance, not the geometric right half – and a proportionately small drainage from the thoracic oesophagus.
The three right lymphatic trunks usually open independently (Fig. 28.16B). Their orifices are clustered either on the ventral aspect of the jugulo/subclavian junction, or in the nearby wall of either of the great veins. Sometimes one or more of the trunks may bifurcate (or even trifurcate) preterminally and then terminate via multiple orifices. Rarely, the three trunks fuse to form a short, single, right lymphatic duct (about 1 cm long) that inclines across the medial border of scalenus anterior at the root of the neck to reach the ventral aspect of the venous junction, where its orifice is guarded by a bicuspid semilunar valve. An incomplete right lymphatic duct may be present if the subclavian and jugular trunks, or any combination of their terminals, are fused. When this occurs, the bronchomediastinal trunk almost invariably opens separately.
On the left, the four trunks that converge on the left lymphovenous portal are the left jugular and left subclavian trunks, which have a disposition corresponding to that of their counterparts on the right; the left bronchomediastinal trunk, which has a drainage similar to the right trunk, but which drains more of the heart – the ‘left’ and part of the ‘right’ hearts of clinical parlance – and more of the oesophagus; and the thoracic duct, which drains all of the rest of the body (Fig. 28.16A).
INNERVATION
The skin, joints, viscera and muscles of the neck are innervated by branches of the glossopharyngeal, vagus and spinal accessory nerves, the cervical spinal nerves and the cervical sympathetic trunk.
The first and second cervical dorsal root ganglia lie on the vertebral arches of the atlas and axis respectively. The first cervical ganglion may be absent. Smaller aberrant ganglia sometimes occur on the upper cervical dorsal roots between the ganglia and cord. The upper four cervical roots are small, the lower four are large. In general, cervical dorsal roots have a thickness ratio to the ventral roots of three to one, which is greater than is seen in other regions. The first dorsal root is an exception, being smaller than the ventral, and in 8% cases it is absent. The first and second cervical roots are short, and run almost horizontally to their exit from the vertebral canal. From the third to the eighth cervical they slope obliquely down. Obliquity and length increase successively, however the distance between spinal attachment and vertebral exit never exceeds the height of one vertebra.
CERVICAL VENTRAL RAMI
Cervical ventral rami, except the first, appear between the anterior and posterior intertransverse muscles. The upper four form the cervical plexus, and the lower four, together with most of the first thoracic ventral ramus, form the brachial plexus. Each receives at least one grey ramus communicans, the upper four from the superior cervical sympathetic ganglion, the fifth and sixth from the middle ganglion and the seventh and eighth from the cervicothoracic ganglion.
The first cervical ventral ramus, the suboccipital nerve, emerges above the posterior arch of the atlas, passes forwards lateral to its lateral mass and medial to the vertebral artery. It supplies rectus capitis lateralis, emerges medial to it, descends anterior to the transverse process of the atlas and posterior to the internal jugular vein and joins the ascending branch of the second cervical ventral ramus.
The second cervical ventral ramus issues between the vertebral arches of the atlas and axis. It ascends between their transverse processes, passes anterior to the first posterior intertransverse muscle and emerges lateral to the vertebral artery generally between longus capitis and levator scapulae. The ramus divides into an ascending branch which joins the first cervical nerve and a descending branch which joins the ascending branch of the third cervical ventral ramus.
The third cervical ventral ramus appears between longus capitis and scalenus medius. The remaining ventral rami emerge between scalenus anterior and the scalenus medius.
Cervical plexus
The cervical plexus is formed by the ventral rami of the upper four cervical nerves, and supplies some neck muscles and the diaphragm, and areas of skin on the head, neck and chest (Fig. 28.1). It is situated in the neck opposite a line drawn down the side of the neck from the root of the auricle to the level of the upper border of the thyroid cartilage. It lies deep to the internal jugular vein, the deep fascia and sternocleidomastoid, and anterior to scalenus medius and levator scapulae. Each ramus, except the first, divides into ascending and descending parts, which unite in communicating loops. From the first loop (C2 and 3) superficial branches supply the head and neck; cutaneous nerves of the shoulder and chest arise from the second loop (C3 and 4). Muscular and communicating branches arise from the same nerves. The branches are superficial or deep. The superficial branches perforate the cervical fascia to supply the skin while the deep branches in general supply muscles. The superficial branches either ascend (the lesser occipital, great auricular and the transverse cutaneous nerves) or descend (supraclavicular nerves). These nerves are described in detail in this chapter on page 435. The deep branches form medial and lateral series.
Deep branches – medial series
Communicating branches pass from the loop between the first and second cervical rami to the vagus and hypoglossal nerves and to the sympathetic trunk. The hypoglossal branch later leaves the hypoglossal nerve as a series of branches, viz. the meningeal, superior root of ansa cervicalis, nerves to thyrohyoid and to geniohyoid. A branch also connects the fourth and fifth cervical rami. The first four cervical ventral rami each receive a grey ramus communicans from the superior cervical sympathetic ganglion.
The superior root of the ansa cervicalis (descendens hypoglossi) (Figs 28.7A, 28.8) leaves the hypoglossal nerve where it curves round the occipital artery and then descends anterior to or in the carotid sheath. It contains only fibres from the first cervical spinal nerve. After giving a branch to the superior belly of omohyoid, it is joined by the inferior root of the ansa from the second and third cervical spinal nerves. The two roots form the ansa cervicalis (ansa hypoglossi), from which branches supply sternohyoid, sternothyroid and the inferior belly of omohyoid. Another branch is said to descend anterior to the vessels into the thorax to join the cardiac and phrenic nerves.
Muscular branches supply rectus capitis lateralis (C1), rectus capitis anterior (C1, 2), longus capitis (C1–3) and longus colli (C2–4). The inferior root of the ansa cervicalis and the phrenic nerve are additional muscular branches.
The inferior root of the ansa cervicalis (nervus descendens cervicalis) (Figs 28.7A, 28.8) is formed by the union of a branch from the second with another from the third cervical ramus. It descends on the lateral side of the internal jugular vein, crosses it a little below the middle of the neck, and continues forwards to join the superior root anterior to the common carotid artery, forming the ansa cervicalis (ansa hypoglossi), from which all infrahyoid muscles except thyrohyoid are supplied. The inferior root comes from the second and third cervical ventral rami in 75% cases, from the second to fourth in 15%, from the third alone in 5%. Occasionally it may be derived from either the second alone or from the first to third.
The phrenic nerve arises chiefly from the fourth cervical ventral ramus, but also has contributions from the third and fifth. It is formed at the upper part of the lateral border of scalenus anterior and descends almost vertically across its anterior surface behind the prevertebral fascia (Figs 28.7A, 28.17, 28.18). It descends posterior to sternocleidomastoid, the inferior belly of omohyoid (near its intermediate tendon), the internal jugular vein, transverse cervical and suprascapular arteries and, on the left, the thoracic duct. At the root of the neck, it runs anterior to the second part of the subclavian artery, from which it is separated by the scalenus anterior (some accounts state that on the left side the nerve passes anterior to the first part of the subclavian artery), and posterior to the subclavian vein. The phrenic nerve enters the thorax by crossing medially in front of the internal thoracic artery.
In the neck, each nerve receives variable filaments from the cervical sympathetic ganglia or their branches and may also connect with internal thoracic sympathetic plexuses.
The accessory phrenic nerve is composed of fibres from the fifth cervical ventral ramus which run in a branch of the nerve to subclavius. This lies lateral to the phrenic nerve and descends posterior (occasionally anterior) to the subclavian vein. The accessory phrenic nerve usually joins the phrenic nerve near the first rib, but may not do so until near the pulmonary hilum or beyond. The accessory phrenic nerve may be derived from the fourth or sixth cervical ventral rami or from the ansa cervicalis.
Brachial plexus
The brachial plexus is formed by the union of the ventral rami of the lower four cervical nerves and the greater part of the ventral ramus of the first thoracic ventral ramus. It may also receive contributions from the fourth cervical and second thoracic spinal nerves. As its name suggests, its branches supply the muscles, joints and skin of the upper limb. The relations and distribution of the brachial plexus are described in detail in Section 6. However, it is also mentioned here because, at its origin, the brachial plexus lies in the posterior triangle of the neck, in the angle between the clavicle and the lower posterior border of sternocleidomastoid. It emerges between the scaleni anterior and medius, superior to the third part of the subclavian artery, and is covered by platysma, deep fascia and skin, through which it is palpable (Fig. 28.17). It is crossed by the supraclavicular nerves, the nerve to subclavius, the inferior belly of omohyoid, the external jugular vein and the superficial ramus of the transverse cervical artery. The plexus passes posterior to the medial two-thirds of the clavicle, subclavius and the suprascapular vessels, and lies on the first digitation of serratus anterior and on subscapularis.
CERVICAL DORSAL RAMI
Each cervical spinal dorsal ramus except the first divides into medial and lateral branches, and all innervate muscles. In general, only medial branches of the second to fourth, and usually the fifth, supply skin. Except for the first (sometimes called the suboccipital nerve) and second, each dorsal ramus passes back medial to a posterior intertransverse muscle, curving round the articular process into the interval between semispinalis capitis and semispinalis cervicis. The cervical dorsal rami are described in detail on pages 755–756.
CRANIAL NERVES
Glossopharyngeal nerve
The glossopharyngeal nerve (Figs 28.8, 28.11, 28.19) supplies motor fibres to stylopharyngeus, parasympathetic secretomotor fibres to the parotid gland (derived from the inferior salivatory nucleus), sensory fibres to the tympanic cavity, pharyngotympanic tube, fauces, tonsils, nasopharynx, uvula and posterior (postsulcal) third of the tongue, and gustatory fibres for the postsulcal part of the tongue.
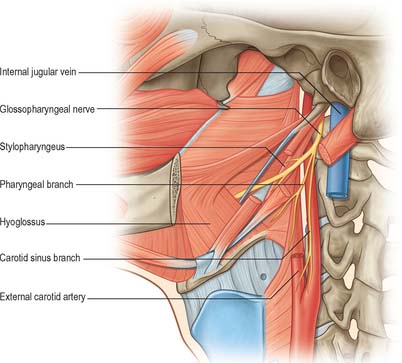
Fig. 28.19 Glossopharyngeal nerve in the anterior triangle of the neck.
(From Drake, Vogl and Mitchell 2005.)
The nerve leaves the skull through the anteromedial part of the jugular foramen, anterior to the vagus and accessory nerves, and in a separate dural sheath. In the foramen it is lodged in a deep groove leading from the cochlear aqueductal depression, and is separated by the inferior petrosal sinus from the vagus and accessory nerves. The groove is bridged by fibrous tissue, which is calcified in 25% of skulls. After leaving the foramen, the nerve passes forwards between the internal jugular vein and internal carotid artery and then descends anterior to the latter, deep to the styloid process and its attached muscles, to reach the posterior border of stylopharyngeus. It curves forwards on stylopharyngeus and either pierces the lower fibres of the superior pharyngeal constrictor or passes between it and the middle constrictor to be distributed to the tonsil, the mucosae of the pharynx and postsulcal part of the tongue, the vallate papillae, and oral mucous glands.
Two ganglia, superior and inferior, are situated on the glossopharyngeal nerve as it traverses the jugular foramen. The superior ganglion is in the upper part of the groove occupied by the nerve in the jugular foramen. It is small, has no branches and is usually regarded as a detached part of the inferior ganglion. The inferior ganglion is larger and lies in a notch in the lower border of the petrous part of the temporal bone. Its cells are typical unipolar neurones, whose peripheral branches convey gustatory and tactile signals from the mucosa of the tongue (posterior third including the sulcus terminalis and vallate papillae) and general sensation from the oropharynx, where it is responsible for initiating the gag reflex.
Communicating branches
The glossopharyngeal nerve communicates with the sympathetic trunk, vagus and facial nerves. Its inferior ganglion is connected with the superior cervical sympathetic ganglion. Two filaments from the inferior ganglion pass to the vagus, one to its auricular branch and the other to its superior ganglion. A branch to the facial nerve arises from the glossopharyngeal nerve below the inferior ganglion, and perforates the posterior belly of digastric to join the facial nerve near the stylomastoid foramen.
Branches of distribution
The glossopharyngeal nerve has tympanic, carotid, pharyngeal, muscular, tonsillar and lingual branches.
The tympanic nerve leaves the inferior ganglion, ascends to the tympanic cavity through the inferior tympanic canaliculus and divides into branches that contribute to the tympanic plexus. The lesser petrosal nerve is derived from the tympanic plexus.
The carotid branch is often double. It arises just below the jugular foramen and descends on the internal carotid artery to the wall of the carotid sinus and to the carotid body. The nerve contains primary afferent fibres from chemoreceptors in the carotid body and from the baroreceptors lying in the carotid sinus wall. It may communicate with the inferior ganglion of the vagus, or with one of its branches, and with a sympathetic branch from the superior cervical ganglion.
The pharyngeal branches are three or four filaments which unite with the pharyngeal branch of the vagus and the layngopharyngeal branches of the sympathetic trunk to form the pharyngeal plexus near the middle pharyngeal constrictor. They constitute the route by which the glossopharyngeal nerve supplies sensory fibres to the mucosa of the pharynx.
Lesions of the glossopharyngeal nerve
Damage to the glossopharyngeal nerve rarely occurs without involvement of other lower cranial nerves. Transient or sustained hypertension may follow surgical section of the nerve, and indicates involvement of the carotid branch. Isolated lesions of the glossopharyngeal nerve lead to loss of sensation over the ipsilateral soft palate, fauces, pharynx and posterior third of the tongue, although this is difficult to assess clinically and confirmation requires galvanic stimulation. The palatal and pharyngeal (gag) reflexes are reduced or absent and salivary secretion from the parotid gland may also be reduced. Weakness of stylopharyngeus cannot be tested individually. Glossopharyngeal neuralgia consists of episodic brief but severe pain, often precipitated by swallowing, and experienced in the throat, behind the angle of the jaw and within the ear. Superior jugular bulb thromboses (e.g. in otitis media) and jugular foramen syndrome (associated with nasopharyngeal carcinoma or a glomus tumour) may cause lesions of the adjacent glossopharyngeal, vagus and accessory nerves, with associated weakness in the muscles supplied in the pharynx and larynx.
Vagus nerve
The vagus is a large mixed nerve. It has a more extensive course and distribution than any other cranial nerve, and runs through the neck, thorax and abdomen. Its central connections are described in Chapter 19.
The vagus exits the skull through the jugular foramen accompanied by the accessory nerve, with which it shares an arachnoid and a dural sheath. Both nerves lie anterior to a fibrous septum that separates them from the glossopharyngeal nerve. The vagus descends vertically in the neck in the carotid sheath, between the internal jugular vein and the internal carotid artery, to the upper border of the thyroid cartilage, and then passes between the vein and the common carotid artery to the root of the neck. Its relationships in this part of its course are therefore similar to those described for these structures (Figs 28.7A, 28.8, 28.17). Its further course differs on the two sides. The right vagus descends posterior to the internal jugular vein to cross the first part of the subclavian artery and enter the thorax. The left vagus enters the thorax between the left common carotid and subclavian arteries and behind the left brachiocephalic vein.
After emerging from the jugular foramen, the vagus bears two marked enlargements, a small, round, superior ganglion and a larger inferior ganglion.
Superior (jugular) ganglion
The superior ganglion is greyish, spherical and approximately 4 mm in diameter. It is connected to the cranial root of the accessory nerve, the inferior glossopharyngeal ganglion, and the sympathetic trunk, the latter by a filament from the superior cervical ganglion. The significance of these connections is not entirely clear, but the first probably contains aberrant motor fibres from the nucleus ambiguus which issue in the accessory nerve, to be distributed to the palatal, pharyngeal, laryngeal and upper oesophageal musculature via the vagus.
Inferior (nodose) ganglion
The inferior or nodose ganglion is larger than the superior ganglion, and is elongated and cylindrical in shape with a length of 25 mm and a maximum breadth of 5 mm. It is connected with the hypoglossal nerve, the loop between the first and second cervical spinal nerves, and with the superior cervical sympathetic ganglion. Just above the ganglion the cranial accessory blends with the vagus nerve, its fibres being distributed mainly in pharyngeal and recurrent laryngeal vagal branches. Most visceral afferent fibres have their cell bodies in the nodose ganglion.
Both vagal ganglia are exclusively sensory, and contain somatic, special visceral and general visceral afferent neurones. The superior ganglion is chiefly somatic, and most of its neurones enter the auricular nerve, whilst neurones in the inferior ganglion are concerned with visceral sensation from the heart, larynx, lungs and the alimentary tract from the pharynx to the transverse colon. Some fibres transmit impulses from taste endings in the vallecula and epiglottis. Large afferent fibres are derived from muscle spindles in the laryngeal muscles. Vagal sensory neurones in the nodose ganglion may show some somatotopic organization. Both ganglia are traversed by parasympathetic, and perhaps some sympathetic fibres, but there is no evidence that vagal parasympathetic components relay in the inferior ganglion. Preganglionic motor fibres from the dorsal vagal nucleus and the special visceral efferents from the nucleus ambiguus, which descend to the inferior vagal ganglion, commonly form a visible band, skirting the ganglion in some mammals. These larger fibres probably provide motor innervation to the larynx in the recurrent laryngeal nerve, together with some contribution to the superior laryngeal nerve supplying cricothyroid.
Branches in the neck
The branches of the vagus in the neck are the meningeal, auricular, pharyngeal, carotid body, superior and recurrent laryngeal nerves and cardiac branches.
Meningeal branches appear to start from the superior vagal ganglion and pass through the jugular foramen to be distributed to the dura mater in the posterior cranial fossa.
The auricular branch arises from the superior vagal ganglion and is joined by a branch from the inferior ganglion of the glossopharyngeal nerve. It passes behind the internal jugular vein and enters the mastoid canaliculus on the lateral wall of the jugular fossa. Traversing the temporal bone, it crosses the facial canal approximately 4 mm above the stylomastoid foramen and here supplies an ascending branch to the facial nerve. Fibres of the nervus intermedius may pass to the auricular branch at this point, which may explain the cutaneous vesiculation in the auricle that sometimes accompanies geniculate herpes. The auricular branch then traverses the tympanomastoid fissure, and divides into two rami. One ramus joins the posterior auricular nerve and the other is distributed to the skin of part of the ear and to the external acoustic meatus.
The pharyngeal branch of the vagus is the main motor nerve of the pharynx. It emerges from the upper part of the inferior vagal ganglion and consists chiefly of filaments from the cranial accessory nerve. It passes between the external and internal carotid arteries to the upper border of the middle pharyngeal constrictor, and divides into numerous filaments which join rami of the sympathetic trunk and glossopharyngeal nerve to form a pharyngeal plexus. A minute filament, the ramus lingualis vagi, joins the hypoglossal nerve as it curves round the occipital artery.
Branches to the carotid body are variable in number. They may arise from the inferior ganglion or travel in the pharyngeal branch, and sometimes in the superior laryngeal nerve. They form a plexus with the glossopharyngeal rami and branches of the cervical sympathetic trunk.
The superior laryngeal nerve is larger than the pharyngeal branch, and issues from the middle of the inferior vagal ganglion. It receives a branch from the superior cervical sympathetic ganglion and descends alongside the pharynx, at first posterior, then medial, to the internal carotid artery, and divides into the internal and external laryngeal nerves.
The internal laryngeal nerve is sensory to the laryngeal mucosa down to the level of the vocal folds. It also carries afferent fibres from the laryngeal neuromuscular spindles and other stretch receptors. It descends to the thyrohyoid membrane, pierces it above the superior laryngeal artery and divides into an upper and lower branch. The upper branch is horizontal and supplies the mucosa of the pharynx, the epiglottis, vallecula and laryngeal vestibule. The lower branch descends in the medial wall of the piriform recess, supplies the aryepiglottic fold, the mucosa on the back of the arytenoid cartilage and one or two branches to transverse arytenoid (the latter unite with twigs from the recurrent laryngeal to supply the same muscle). The internal laryngeal nerve ends by piercing the inferior pharyngeal constrictor to unite with an ascending branch from the recurrent laryngeal nerve. As it ascends in the neck it supplies branches, more numerous on the left, to the mucosa and tunica muscularis of the oesophagus and trachea and to the inferior constrictor.
The external laryngeal nerve, smaller than the internal, descends behind sternohyoid with the superior thyroid artery, but on a deeper plane. It lies first on the inferior pharyngeal constrictor, then pierces it to curve round the inferior thyroid tubercle and reach cricothyroid, which it supplies. The nerve also gives branches to the pharyngeal plexus and the inferior constrictor. Behind the common carotid artery, the external laryngeal nerve communicates with the superior cardiac nerve and superior cervical sympathetic ganglion.
The recurrent laryngeal nerve differs, in origin and course, on the two sides. On the right it arises from the vagus anterior to the first part of the subclavian artery, and curves backwards below and then behind it to ascend obliquely to the side of the trachea behind the common carotid artery. Near the lower pole of the lateral lobe of the thyroid gland it is closely related to the inferior thyroid artery, and crosses either in front of, behind, or between, its branches. On the left, the nerve arises from the vagus on the left of the aortic arch, curves below it immediately behind the attachment of the ligamentum arteriosum to the concavity of the aortic arch and ascends to the side of the trachea. As the recurrent laryngeal nerve curves round the subclavian artery, or the aortic arch, it gives cardiac filaments to the deep cardiac plexus. On both sides the recurrent laryngeal nerve ascends in or near a groove between the trachea and oesophagus. It is closely related to the medial surface of the thyroid gland before it passes under the lower border of the inferior constrictor, and it enters the larynx behind the articulation of the inferior thyroid cornu with the cricoid cartilage. The recurrent laryngeal nerve supplies all laryngeal muscles, except the cricothyroid, and it communicates with the internal laryngeal nerve, supplying sensory filaments to the laryngeal mucosa below the vocal folds. It also carries afferent fibres from laryngeal stretch receptors. The recurrent laryngeal nerve is described further with the larynx (p. 589).
Accessory nerve
The accessory nerve (Figs 28.7A, 28.11, 28.17) is conventionally described as a single entity, even though its two components, which join for a relatively short part of its course, are of quite separate origin.
Cranial root
The cranial root of the accessory nerve is smaller than the spinal root. It exits the skull through the jugular foramen, and unites for a short distance with the spinal root. It is also connected to the superior vagal ganglion. After traversing the foramen, the cranial root separates from the spinal part and immediately joins the vagus nerve superior to the inferior vagal ganglion. Those of its fibres that are distributed in the pharyngeal branches of the vagus are derived from the nucleus ambiguus, and probably innervate the pharyngeal and palatal muscles except tensor veli palatini. Other fibres enter the recurrent laryngeal nerve to supply the adductor muscles of the vocal cords, thyroarytenoid and lateral cricoarytenoid.
The status of the cranial root of the accessory nerve continues to excite debate. Cadaveric dissection studies have revealed wide variation in the patterns of anastomosis between the intracranial branches of the lower four cranial nerves (glossopharyngeal, vagus, accessory and hypoglossal) in the posterior cranial fossa: a separate cranial root of the accessory cannot always be demonstrated.
Spinal root
The spinal root arises from an elongated nucleus of motor cells situated in the lateral aspect of the ventral horn which extends from the junction of the spinal cord and medulla to the sixth cervical segment (Fig. 28.11). Some rootlets emerge directly, others turn cranially before exiting. Their line of exit is irregular rather than linear, and the spinal root usually passes through the first cervical dorsal root ganglion. The rootlets form a trunk which ascends between the ligamentum denticulatum and the dorsal roots of the spinal nerves and enters the skull via the foramen magnum, behind the vertebral artery. It then turns upwards and passes laterally to reach the jugular foramen, which it traverses in a common dural sheath with the vagus, but separated from that nerve by a fold of arachnoid mater. As the spinal root exits the jugular foramen it runs posterolaterally and passes either medial or lateral to the internal jugular vein. Occasionally it passes through the vein. The nerve then crosses the transverse process of the atlas and is itself crossed by the occipital artery. It descends obliquely, medial to the styloid process, stylohyoid and the posterior belly of the digastric. Running with the superior sternocleidomastoid branch of the occipital artery, it reaches the upper part of sternocleidomastoid and enters its deep surface, to form an anastomosis with fibres from C2 alone, C3 alone, or C2 and C3, the ansa of Maubrac. It may also communicate with the anterior root of the first cervical nerve (McKenzie branch).
The accessory nerve occasionally terminates in sternocleidomastoid. More commonly it emerges a little above the midpoint of the posterior border of sternocleidomastoid, generally above the emergence of the great auricular nerve (usually within 2 cm of it) and between 4–6 cm from the tip of the mastoid process. However, the point of emergence is very variable. The nerve then crosses the posterior triangle on levator scapulae (Fig. 28.7A), separated from it by the prevertebral layer of deep cervical fascia and adipose tissue. Here the nerve is relatively superficial and related to the superficial cervical lymph nodes. About 3–5 cm above the clavicle it passes behind the anterior border of trapezius, often dividing to form a plexus on its deep surface which receives contributions from C3 and C4, or C4 alone. It then enters the deep surface of the muscle.
The cervical course of the nerve follows a line from the lower anterior part of the tragus to the tip of the transverse process of the atlas and then across the sternocleidomastoid and the posterior triangle to a point on the anterior border of the trapezius 3–5 cm above the clavicle.
Conventionally, the spinal root is thought to provide the sole motor supply to sternocleidomastoid, and the second and third cervical nerves are believed to carry proprioceptive fibres from it. The supranuclear pathway of fibres destined for sternocleidomastoid is not simple: fibres may undergo a double decussation in the brainstem and/or there may be a bilateral projection to the muscle from each hemisphere. The motor supply to the upper and middle portions of trapezius is primarily from the spinal accessory nerve. However, the lower two-thirds of the muscle, in 75% of subjects, receives an innervation from the cervical plexus. On the basis of the incomplete denervation of the muscle that sometimes occurs following sacrifice of both the accessory nerve and the cervical plexus, it has been suggested that the trapezius receives a partial motor supply from other sources, possibly via thoracic roots. In addition to their motor contribution, C3 and 4 carry proprioceptive fibres from trapezius. In 25% of subjects the spinal accessory nerve receives no fibres from the cervical plexus. (For a detailed review of the applied surgical anatomy of the spinal accessory nerve plexus, see Brown 2002.)
Sensory ganglia have been described along the course of the spinal root.
Lesions affecting the accessory nerve
Lesions of the accessory nerve may occur centrally; at its exit from the skull; in the neck. The supranuclear fibres which influence motor neurones innervating sternocleidomastoid decussate twice, therefore a lesion of the pyramidal system above the pons produces weakness of the ipsilateral sternocleidomastoid and contralateral trapezius. Episodic contraction of sternocleidomastoid and trapezius, often accompanied by contraction of other muscle groups, e.g. splenius capitis, occurs in spasmodic torticollis, a focal dystonia. In jugular foramen syndrome, caused by pathologies including nasopharyngeal carcinoma or a glomus tumour, lesions of the glossopharyngeal, vagus and accessory nerves coexist. The accessory nerve can be injured more distally in the neck by trauma or by surgical exploration in the posterior triangle. If the accessory nerve is sacrificed as part of a radical neck dissection, and the innervation of trapezius is lost, the patient develops intractable neuralgia due to traction on the brachial plexus caused by the unsupported weight of the shoulder and arm.
Hypoglossal nerve
The hypoglossal nerve is motor to all the muscles of the tongue, except palatoglossus. The hypoglossal rootlets run laterally behind the vertebral artery, collected into two bundles which perforate the dura mater separately opposite the hypoglossal canal in the occipital bone, and unite after traversing it. The canal is sometimes divided by a spicule of bone. The nerve emerges from the canal in a plane medial to the internal jugular vein, internal carotid artery, ninth, tenth and eleventh cranial nerves, and passes inferolaterally behind the internal carotid artery and glossopharyngeal and vagus nerves to the interval between the artery and the internal jugular vein (Fig. 28.8). Here it makes a half-spiral turn round the inferior vagal ganglion, and is united with it by connective tissue. It then descends almost vertically between the vessels and anterior to the vagus to a point level with the angle of the mandible, becoming superficial below the posterior belly of digastric and emerging between the internal jugular vein and internal carotid artery. It loops round the inferior sternocleidomastoid branch of the occipital artery, crosses lateral to both internal and external carotid arteries and the loop of the lingual artery a little above the tip of the greater cornu of the hyoid, and is itself crossed by the facial vein (Figs 28.7A, 28.8, 28.17). Its course is described further on page 506.
Communications
The hypoglossal nerve communicates with the sympathetic trunk, vagus, first and second cervical nerves and lingual nerve. Near the atlas it is joined by branches from the superior cervical sympathetic ganglion and by a filament from the loop between the first and second cervical nerves which leaves the hypoglossal as the upper root of the ansa cervicalis. The vagal connections occur close to the skull, and numerous filaments pass between the hypoglossal nerve and the inferior vagal ganglion in the connective tissue uniting them. As the hypoglossal nerve curves round the occipital artery it receives the ramus lingualis vagi from the pharyngeal plexus. Near the anterior border of hyoglossus it is connected with the lingual nerve by many filaments which ascend on the muscle.
Branches of distribution
The branches of distribution of the hypoglossal nerve are meningeal, descending, thyrohyoid and muscular nerves.
Meningeal branches leave the nerve in the hypoglossal canal and return through it to supply the diploë of the occipital bone, the dural walls of the occipital and inferior petrosal sinuses and much of the floor of the anterior wall of the posterior cranial fossa, probably through pathways other than that of the hypoglossal nerve, e.g. upper cervical spinal nerves.
The descending branch (descendens hypoglossi) contains fibres from the first cervical spinal nerve. It leaves the hypoglossal nerve when it curves around the occipital artery, and runs down on the carotid sheath. It provides a branch to the superior belly of omohyoid before joining with the descendens cervicalis to form the ansa cervicalis (Figs 28.7A, 28.8).
Lesions of the hypoglossal nerve
The hypoglossal nerve may be damaged during neck dissection. Complete hypoglossal division causes unilateral lingual paralysis and eventual hemiatrophy; the protruded tongue deviates to the paralysed side, and, on retraction, the wasted and paralysed side rises higher than the unaffected side. The larynx may deviate towards the active side in swallowing, due to unilateral paralysis of the hyoid depressors associated with loss of the first cervical spinal nerve which runs with the hypoglossal nerve. If paralysis is bilateral, the tongue is motionless. Taste and tactile sensibility are unaffected but articulation is slow and swallowing very difficult.
CERVICAL SYMPATHETIC TRUNK
The cervical sympathetic trunk lies on the prevertebral fascia behind the carotid sheath and contains three interconnected ganglia, the superior, middle and inferior (stellate or cervicothoracic) (Figs 28.17, 28.18). However there may occasionally be two or four ganglia. The cervical sympathetic ganglia send grey rami communicantes to all the cervical spinal nerves but receive no white rami communicantes from them. Their spinal preganglionic fibres emerge in the white rami communicantes of the upper five thoracic spinal nerves (mainly the upper three), and ascend in the sympathetic trunk to synapse in the cervical ganglia. In their course, the grey rami communicantes may pierce longus capitis or scalenus anterior.
Superior cervical ganglion
The superior cervical ganglion is the largest of the three ganglia (Fig. 28.17). It lies on the transverse processes of the second and third cervical vertebrae and is probably formed from four fused ganglia judging by its grey rami to C1–4. The internal carotid artery within the carotid sheath is anterior, and longus capitis is posterior. The lower end of the ganglion is united by a connecting trunk to the middle cervical ganglion. Postganglionic branches are distributed in the internal carotid nerve, which ascends with the internal carotid artery into the carotid canal to enter the cranial cavity, and in lateral, medial and anterior branches. They supply vasoconstrictor and sudomotor nerves to the face and neck, dilator pupillae and smooth muscle in the eyelids and orbitalis.
The lateral branches are grey rami communicantes to the upper four cervical spinal nerves and to some of the cranial nerves. Branches pass to the inferior vagal ganglion, the hypoglossal nerve, the superior jugular bulb and associated jugular glomus or glomera, and to the meninges in the posterior cranial fossa. Another branch, the jugular nerve, ascends to the cranial base and divides into two; one part joins the inferior glossopharyngeal ganglion and the other joins the superior vagal ganglion.
The medial branches of the superior cervical ganglion are the laryngopharyngeal and cardiac. The laryngopharyngeal branches supply the carotid body and pass to the side of the pharynx, joining glossopharyngeal and vagal rami to form the pharyngeal plexus. A cardiac branch arises by two or more filaments from the lower part of the superior cervical ganglion and occasionally receives a twig from the trunk between the superior and middle cervical ganglia. It is thought to contain only efferent fibres, the preganglionic outflow being from the upper thoracic segments of the spinal cord, and to be devoid of pain fibres from the heart. It descends behind the common carotid artery, in front of longus colli, and crosses anterior to the inferior thyroid artery and recurrent laryngeal nerve. The courses on the two sides then differ. The right cardiac branch usually passes behind, but sometimes in front of, the subclavian artery and runs posterolateral to the brachiocephalic trunk to join the deep (dorsal) part of the cardiac plexus behind the aortic arch. It has other sympathetic connections. About midneck it receives filaments from the external laryngeal nerve. Inferiorly, one or two vagal cardiac branches join it. As it enters the thorax it is joined by a filament from the recurrent laryngeal nerve. Filaments from the nerve also communicate with the thyroid branches of the middle cervical ganglion. The left cardiac branch, in the thorax, is anterior to the left common carotid artery and crosses in front of the left side of the aortic arch to reach the superficial (ventral) part of the cardiac plexus. Sometimes it descends on the right of the aorta to end in the deep (dorsal) part of the cardiac plexus. It communicates with the cardiac branches of the middle and inferior cervical sympathetic ganglia and sometimes with the inferior cervical cardiac branches of the left vagus, and branches from these mixed nerves form a plexus on the ascending aorta.
The anterior branches of the superior cervical ganglion ramify on the common and external carotid arteries and the branches of the external carotid, and form a delicate plexus around each in which small ganglia are occasionally found. The plexus around the facial artery supplies a filament to the submandibular ganglion; the plexus on the middle meningeal artery sends one ramus to the otic ganglion and another, the external petrosal nerve, to the facial ganglion. Many of the fibres coursing along the external carotid and its branches ultimately leave them to travel to facial sweat glands via branches of the trigeminal nerve.
Middle cervical ganglion
The middle cervical ganglion is the smallest of the three, and is occasionally absent, in which case it may be replaced by minute ganglia in the sympathetic trunk or may be fused with the superior ganglion. It is usually found at the level of the sixth cervical vertebra, anterior or just superior to the inferior thyroid artery, or it may adjoin the inferior cervical ganglion. It probably represents a coalescence of the ganglia of the fifth and sixth cervical segments, judging by its postganglionic rami, which join the fifth and sixth cervical spinal nerves (but sometimes also the fourth and seventh). It is connected to the inferior cervical ganglion by two or more very variable cords. The posterior cord usually splits to enclose the vertebral artery, while the anterior cord loops down anterior to, and then below, the first part of the subclavian artery, medial to the origin of its internal thoracic branch, and supplies rami to it. This loop is the ansa subclavia and is frequently multiple, lies closely in contact with the cervical pleura and typically connects with the phrenic nerve, and sometimes with the vagus (Fig. 28.18).
The middle cervical ganglion gives off thyroid and cardiac branches. The thyroid branches accompany the inferior thyroid artery to the thyroid gland. They communicate with the superior cardiac, external laryngeal and recurrent laryngeal nerves, and send branches to the parathyroid glands. Fibres to both glands are largely vasomotor but some reach the secretory cells. The cardiac branch, the largest sympathetic cardiac nerve, either arises from the ganglion itself or more often from the sympathetic trunk cranial or caudal to it. On the right side it descends behind the common carotid artery, in front of or behind the subclavian artery, to the trachea where it receives a few filaments from the recurrent laryngeal nerve before joining the right half of the deep (dorsal) part of the cardiac plexus. In the neck, it connects with the superior cardiac and recurrent laryngeal nerves. On the left side the cardiac nerve enters the thorax between the left common carotid and subclavian arteries to join the left half of the deep (dorsal) part of the cardiac plexus. Fine branches from the middle cervical ganglion also pass to the trachea and oesophagus.
Inferior (or cervicothoracic/stellate) ganglion
The inferior cervical ganglion (cervicothoracic/stellate) is irregular in shape and much larger than the middle cervical ganglion (Fig. 28.18). It is probably formed by a fusion of the lower two cervical and first thoracic segmental ganglia, sometimes including the second and even third and fourth thoracic ganglia. The first thoracic ganglion may be separate, leaving an inferior cervical ganglion above it. The sympathetic trunk turns backwards at the junction of the neck and thorax and so the long axis of the cervicothoracic ganglion becomes almost anteroposterior. The ganglion lies on or just lateral to the lateral border of longus colli between the base of the seventh cervical transverse process and the neck of the first rib (which are both posterior to it). The vertebral vessels are anterior, and the ganglion is separated from the posterior aspect of the cervical pleura inferiorly by the suprapleural membrane. The costocervical trunk of the subclavian artery branches near the lower pole of the ganglion, and the superior intercostal artery is lateral.
A small vertebral ganglion may be present on the sympathetic trunk anterior or anteromedial to the origin of the vertebral artery and directly above the subclavian artery. When present, it may provide the ansa subclavia and is also joined to the inferior cervical ganglion by fibres enclosing the vertebral artery. It is usually regarded as a detached part of the middle cervical or inferior cervical ganglion. Like the middle cervical ganglion it may supply grey rami communicantes to the fourth and fifth cervical spinal nerves. The inferior cervical ganglion sends grey rami communicantes to the seventh and eighth cervical and first thoracic spinal nerves, and gives off a cardiac branch, branches to nearby vessels and sometimes a branch to the vagus nerve.
The grey rami communicantes to the seventh cervical spinal nerve vary from one to five (two being the usual number). A third often ascends medial to the vertebral artery in front of the seventh cervical transverse process. It connects with the seventh cervical nerve, and sends a filament upwards through the sixth cervical transverse foramen in company with the vertebral vessels to join the sixth cervical spinal nerve as it emerges from the intervertebral foramen. An inconstant ramus may traverse the seventh cervical transverse foramen. Grey rami to the eighth cervical spinal nerve vary from three to six in number.
The cardiac branch descends behind the subclavian artery and along the front of the trachea to the deep cardiac plexus. Behind the artery it connects with the recurrent laryngeal nerve and the cardiac branch of the middle cervical ganglion (the latter is often replaced by fine branches of the inferior cervical ganglion and ansa subclavia).
The branches to blood vessels form plexuses on the subclavian artery and its branches. The subclavian supply is derived from the inferior cervical ganglion and ansa subclavia, and typically extends to the first part of the axillary artery, although a few fibres may extend further. An extension of the subclavian plexus to the internal thoracic artery may be joined by a branch of the phrenic nerve.
Within the foramina transversaria and intertransverse spaces, the cervical grey rami communicantes form intersegmental arcades as they communicate with one another and the ventral rami of the upper five or six cervical spinal nerves. These arcades accompany the second part of the vertebral artery and create the appearance of a long nerve known as the vertebral nerve. Fine filaments from this nerve and the grey rami communicantes form the vertebral plexus on the surface of the vertebral artery. This plexus contains not only sympathetic efferent fibres but also somatic sensory fibres from the adventitia of the artery, whose cell bodies are located in the cervical dorsal root ganglia. The vertebral nerve sends filaments to the posterolateral corners of the cervical intervertebral discs (Bogduk et al 1988), and gives rise to the meningeal branches (sinuvertebral nerves) at each cervical segment. The vertebral plexus, which contains some neuronal cell bodies, continues into the skull along the vertebral and basilar arteries and their branches as far as the posterior cerebral artery, where it meets a plexus from the internal carotid artery. The plexus on the inferior thyroid artery reaches the thyroid gland, and connects with the recurrent and external laryngeal nerves, the cardiac branch of the superior cervical ganglion, and the common carotid plexus.
Horner’s syndrome
Any condition or injury that destroys the sympathetic trunk ascending from the thorax through the neck into the face results in Horner’s syndrome, characterized by a drooping eyelid (ptosis), sunken globe (enophthalmos), narrow palpebral fissure, contracted pupil (meiosis), vasodilatation and lack of thermal sweating (anhydrosis) on the affected side. This occurs classically when a bronchial carcinoma invades the sympathetic trunk. It also occurs as a complication of cervical sympathectomy or a radical neck dissection. Avulsion of the first thoracic nerve from the spinal cord may be diagnosed by development of the syndrome after closed traction lesion of the supraclavicular brachial plexus.
VISCERA
The main cervical viscera are the submandibular salivary glands, the thyroid and parathyroid glands and the cervical portions of the trachea and oesophagus.
SUBMANDIBULAR SALIVARY GLAND
Each submandibular salivary gland is situated behind and below the ramus of the mandible, in the region of the submandibular triangle, between the anterior and posterior bellies of digastric (Fig. 28.7A). The gland is described in detail on page 520.
THYROID GLAND
The thyroid gland, brownish-red and highly vascular, is placed anteriorly in the lower neck, level with the fifth cervical to the first thoracic vertebrae (Figs 28.4, 28.17). It is ensheathed by the pretracheal layer of deep cervical fascia and consists of right and left lobes connected by a narrow, median isthmus. It usually weighs 25 g, but this varies. The gland is slightly heavier in females, and enlarges during menstruation and pregnancy. Estimation of the size of the thyroid gland is clinically important in the evaluation and management of thyroid disorders and can be achieved non-invasively by means of diagnostic ultrasound. No significant difference in thyroid gland volume has been observed between males and females from 8 months to 15 years.
The lobes of the thyroid gland are approximately conical. Their ascending apices diverge laterally to the level of the oblique lines on the laminae of the thyroid cartilage, and their bases are level with the fourth or fifth tracheal cartilages. Each lobe is usually 5 cm long, its greatest transverse and anteroposterior extents being 3 cm and 2 cm respectively. The posteromedial aspects of the lobes are attached to the side of the cricoid cartilage by a lateral thyroid ligament.
The isthmus connects the lower parts of the two lobes, although occasionally it may be absent. It measures 1.25 cm transversely and vertically, and is usually anterior to the second and third tracheal cartilages, though often higher or sometimes lower because its site and size vary greatly.
A conical pyramidal lobe often ascends towards the hyoid bone from the isthmus or the adjacent part of either lobe (more often the left). It is occasionally detached or in two or more parts. A fibrous or fibromuscular band, the levator of the thyroid gland, musculus levator glandulae thyroideae, sometimes descends from the body of the hyoid to the isthmus or pyramidal lobe. Small detached masses of thyroid tissue may occur above the lobes or isthmus as accessory thyroid glands. Vestiges of the thyroglossal duct may persist between the isthmus and the foramen caecum of the tongue, sometimes as accessory nodules or cysts of thyroid tissue near the midline or even in the tongue.
Surfaces and relations
The convex lateral (superficial) surface is covered by sternothyroid, whose attachment to the oblique thyroid line prevents the upper pole of the gland from extending on to thyrohyoid. More anteriorly lie sternohyoid and the superior belly of omohyoid, overlapped inferiorly by the anterior border of sternocleidomastoid. The medial surface of the gland is adapted to the larynx and trachea; its superior pole contacts the inferior pharyngeal constrictor and the posterior part of cricothyroid, which separate it from the posterior part of the thyroid lamina and the side of the cricoid cartilage. The external laryngeal nerve is medial to this part of the gland as it passes to supply cricothyroid. Inferiorly, the trachea and, more posteriorly, the recurrent laryngeal nerve and oesophagus (which is closer on the left), are medial relations. The posterolateral surface of the thyroid gland is close to the carotid sheath, and overlaps the common carotid artery.
The anterior border of the gland is thin, and near the anterior branch of the superior thyroid artery it slants down medially. The posterior border is rounded and related inferiorly to the inferior thyroid artery and its anastomosis with the posterior branch of the superior thyroid artery. On the left side, the lower end of the posterior border lies near the thoracic duct. The parathyroid glands are usually related to the posterior border.
The isthmus is covered by sternothyoid, from which it is separated by pretracheal fascia. More superficially it is covered by sternohyoid, the anterior jugular veins, fascia and skin. The superior thyroid arteries anastomose along its upper border and the inferior thyroid veins leave the gland at its lower border.
Vascular supply and lymphatic drainage
Arteries
The thyroid gland is supplied by the superior and inferior thyroid arteries and sometimes by an arteria thyroidea ima from the brachiocephalic trunk or aortic arch (Figs 28.14, 28.17). The arteries are large and their branches anastomose frequently both on and in the gland, ipsilaterally and contralaterally. The superior thyroid artery, which is closely related to the external laryngeal nerve, pierces the thyroid fascia and then divides into anterior and posterior branches. The anterior branch supplies the anterior surface of the gland, and the posterior branch supplies the lateral and medial surfaces. The inferior thyroid artery approaches the base of the thyroid gland and divides into superior (ascending) and inferior thyroid branches to supply the inferior and posterior surfaces of the gland. The superior branch also supplies the parathyroid glands. The relationship between the inferior thyroid artery and the recurrent laryngeal nerve is highly variable and of considerable clinical importance: iatrogenic injury to the nerves that supply the larynx represents a major complication of thyroid surgery (Yalcxin 2006). The recurrent laryngeal nerve is usually related to the posterior branch of the inferior thyroid artery, which may be replaced by a vascular network (Moreau et al 1998).
Veins
The venous drainage of the thyroid gland is usually via superior, middle, and inferior thyroid veins (Figs 28.13, 28.14). The superior thyroid vein emerges from the upper part of the gland and runs with the superior thyroid artery towards the carotid sheath: it drains into the internal jugular vein. The middle thyroid vein collects blood from the lower part of the gland: it emerges from the lateral surface of the gland and drains into the internal jugular vein. The inferior thyroid veins arise in a glandular venous plexus, which also connects with the middle and superior thyroid veins. These veins form a pretracheal plexus, from which the left inferior vein descends to join the left brachiocephalic vein and the right descends obliquely across the brachiocephalic artery to join the right brachiocephalic vein at its junction with the superior vena cava. The inferior thyroid veins often open via a common trunk into the superior vena cava or left brachiocephalic vein. They drain the oesophageal, tracheal and inferior laryngeal veins and have valves at their terminations.
Lymphatics
Thyroid lymphatic vessels communicate with the tracheal plexus, and pass to the prelaryngeal nodes just above the thyroid isthmus and to the pretracheal and paratracheal nodes; some may also drain into the brachiocephalic nodes related to the thymus in the superior mediastinum. Laterally the gland is drained by vessels lying along the superior thyroid veins to the deep cervical nodes. Thyroid lymphatics may drain directly, with no intervening node, to the thoracic duct.
Innervation
The thyroid gland receives its innervation from the superior, middle and inferior cervical sympathetic ganglia. Postganglionic fibres from the inferior cervical ganglion form a plexus on the inferior thyroid artery which accompanies the artery to the thyroid gland, and communicates with the recurrent and external laryngeal nerves, with the superior cardiac nerve, and with the plexus on the common carotid artery.
Imaging
The follicular nature of the thyroid gland is not resolved by current imaging techniques and thus presents a homogeneous texture on cross-sectional imaging (US, CT, MRI). Its superficial location makes the thyroid an ideal organ for sonographic examination (Fig. 28.20). The thyroid gland is highly vascular and demonstrates intense contrast enhancement and increased signal on T2-weighted MRI (Fig. 28.21). Radionuclide imaging of the thyroid may be performed with technetium (Tc99m) pertechnetate. This readily available radionuclide is trapped by the thyroid in the same way as iodine, but is not organified. It yields morphological information and will reveal the presence of ectopic thyroid tissue. Functional data can be obtained with the use of 131iodine which is trapped and organified.
Microstructure
The thyroid gland has a thin capsule of connective tissue, which extends into the glandular parenchyma and divides each lobe into irregularly shaped and sized lobules. The functional units of the thyroid are follicles, which are spherical and cyst-like, between 0.02 and 0.9 mm in diameter. Follicles consist of a central colloid core surrounded by a single-layered epithelium resting on a basal lamina (Fig. 28.22). Colloid consists almost entirely of an iodinated glycoprotein, iodothyroglobulin, which is the inactive, stored form of the active thyroid hormones, tri-iodothyronine (T3) and tetraiodothyronine or thyroxine (T4), and is produced by the follicular epithelial cells. Sufficient iodothyroglobulin is stored extracellularly within follicles to regulate the metabolic activity of the body for up to three months. Follicles are surrounded by a delicate connective tissue stroma, containing dense plexuses of fenestrated capillaries, extensive lymphatic networks and sympathetic nerve fibres which supply the arterioles and capillaries. Some nerve fibres end close to the follicular epithelial cells.
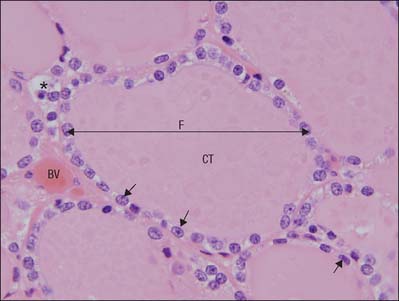
Fig. 28.22 A section through parts of several human thyroid follicles, one of which is labelled (F), showing the follicular epithelium (arrows) enclosing a lumen filled with colloidal thyroglobulin (CT). Calcitonin-secreting C cells are not readily identifiable in routine preparations of human tissue, where they appear as poorly-staining (clear) cells within follicles; an example is indicated by the asterisk. A network of blood vessels (BV) within connective tissue septa surrounds the follicles.
(By courtesy of Mr Peter Helliwell and Dr Joseph Mathew, Department of Histopathology, Royal Cornwall Hospitals Trust, UK.)
Follicular cells vary from squamous or low cuboidal to columnar, depending on their level of activity, which is controlled mainly by circulating hypophysial thyroid-stimulating hormone (TSH, thyrotropin). Resting follicles are large and lined by squamous or low cuboidal epithelium with abundant luminal colloid. Apical microvilli are short in resting cells, but elongate and often branch on stimulation by TSH. Follicles showing differing levels of activity may co-exist.
Active follicular cells are highly polarized functionally. The secretion of TSH leads to endocytosis of colloidal droplets at the luminal epithelium (Fig. 28.22). The hormone provokes the cells to extend cytoplasmic processes into the luminal colloid and sequester droplets of colloid. The iodinated thyroglobulin in the intracellular colloid droplets is then degraded by follicular cell lysosomes, liberating T3 and T4 which pass to the base of the cell, where they are released. They are exported from the thyroid mainly via the blood capillaries and lymphatics. Prolonged high levels of circulating TSH induce follicular cell hypertrophy, progressive resorption of colloid and increased stromal vascularity.
Thyroid parenchyma also contains C (clear) cells, so-called because they have pale-staining cytoplasm, which is more pronounced in some species than in the human thyroid. C cells are members of the amine precursor uptake and decarboxylation (APUD) system of dispersed neuroendocrine cells. They produce the peptide hormone calcitonin (thyrocalcitonin) which lowers blood calcium by inhibiting bone resorption and calcium recovery from renal tubule ultrafiltrate. C cells populate the middle third of each lateral lobe of the thyroid and are typically found scattered within thyroid follicles, lying inside the basal lamina but not reaching the follicle lumen. Occasionally they occur in clusters in the interfollicular stroma, which is why they are also called parafollicular cells.
Thyroidectomy
Apart from variable enlargement during menstruation and pregnancy, any thyroid swelling is a goitre, which may press on related structures. Symptoms most commonly are the consequence of pressure on the trachea or on the recurrent laryngeal nerves, and there may also be venous engorgement. During thyroidectomy, care must be taken when tying off the superior and inferior thyroid arteries to avoid damage to adjacent nerves. The external laryngeal nerve runs close to the superior thyroid artery and the recurrent laryngeal nerve runs close to the inferior thyroid artery. Partial thyroidectomy is often necessary in the treatment of hyperthyroidism and thyroid enlargement: the posterior parts of both lobes are left intact to preserve the parathyroid glands.
PARATHYROID GLANDS
The parathyroid glands are small, yellowish-brown, ovoid or lentiform structures, usually lying between the posterior lobar borders of the thyroid gland and its capsule. They are commonly 6 mm long, 3–4 mm across, and 1–2 mm from back to front, each weighing about 50 mg. Typically there are two on each side, superior and inferior, but there may be more or there may be only three or many minute parathyroid islands scattered in connective tissue near the usual sites. Very occasionally an occult gland may follow a blood vessel into a groove on the surface of the thyroid. Normally the inferior parathyroids migrate only to the inferior thyroid poles, but they may descend with the thymus into the thorax or they may be sessile and remain above their normal level near the carotid bifurcation. The anastomotic connection between the superior and inferior thyroid arteries that occurs along the posterior border of the thyroid gland usually passes very close to the parathyroids, and is a useful aid to their identification.
The superior parathyroid glands are more constant in location than the inferior and are usually to be found midway along the posterior borders of the thyroid gland, although they may be higher. The inferior pair are more variably situated (related to their embryological development) and may be within the fascial thyroid sheath, below the inferior thyroid arteries and near the inferior lobar poles; or outside the sheath, immediately above an inferior thyroid artery; or in the thyroid gland near its inferior pole. These variations are surgically important (Fig. 28.23). A tumour of the inferior parathyroid situated within the fascial thyroid sheath may descend along the inferior thyroid veins anterior to the trachea into the superior mediastinum, whereas if it is outside the sheath it may extend posteroinferiorly behind the oesophagus into the posterior mediastinum. The superior parathyroids are usually dorsal, and the inferior parathyroids ventral, to the recurrent laryngeal nerves.
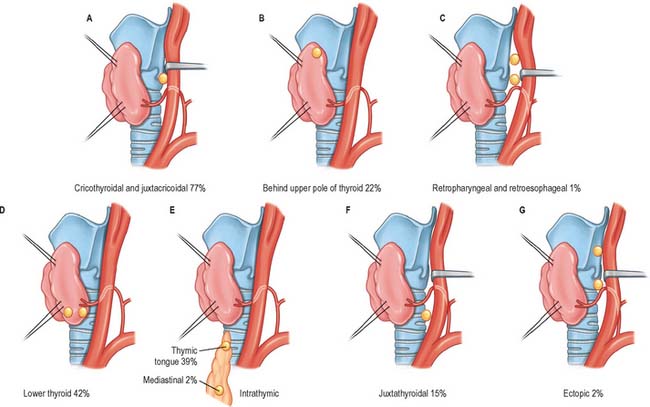
Fig. 28.23 Distribution of superior (A–C) and inferior (D–G) parathyroid glands. A, Cricothyroidal and juxtathyroidal; B, Behind upper pole of thyroid; C, Retropharyngeal and retroesophageal; D, Lower thyroid; E, Intrathymic; F, Juxtathyroidal; G, Ectopic.
The parathyroid glands are very flattened in cross-section and are not normally visible by current imaging methods, including scintigraphy.
Vascular supply and lymphatic drainage
Both superior and inferior parathyroid glands are usually supplied by the inferior thyroid arteries; the superior thyroid may be supplied by the superior thyroid artery or from anastomoses between the superior and inferior thyroid arteries in 10–15% cases. The glands drain into the plexus of veins on the anterior surface of the thyroid. Lymph vessels are numerous and associated with those of the thyroid and thymus glands.
Innervation
The nerve supply is sympathetic, either direct from the superior or middle cervical ganglia or via a plexus in the fascia on the posterior lobar aspects. Parathyroid activity is controlled by variations in blood calcium level: it is inhibited by a rise and stimulated by a fall. The nerves are believed to be vasomotor but not secretomotor.
Microstructure
Each parathyroid gland has a thin connective tissue capsule with intraglandular septa but lacks distinct lobules. The parathyroids synthesize and secrete parathyroid hormone (PTH, parathormone), a single-chain polypeptide of 84 amino-acid residues concerned with the control of the level and distribution of calcium and phosphorus. In childhood, the gland consists of wide, irregular, interconnecting columns of chief or principal cells separated by a dense plexus of fenestrated sinusoidal capillaries. After puberty, adipose tissue accumulates in the stroma and typically accounts for about one third of the adult tissue mass, increasing further with age.
Chief cells differ ultrastructurally according to their level of activity: active chief cells have large Golgi complexes with numerous vesicles and small membrane-bound granules. Glycogen granules are most abundant in inactive cells, which have few of the cytoplasmic features of synthetic or secretory activity, and appear histologically as ‘clear’ cells. In normal human parathyroid glands, inactive chief cells outnumber active cells in a ratio of 3–5 : 1 (Fig. 28.24). In contrast to the thyroid, where the activities of adjacent follicular cells are coordinated, individual chief cells of the parathyroid glands go through cycles of secretory activity and rest independently, according to serum calcium levels.
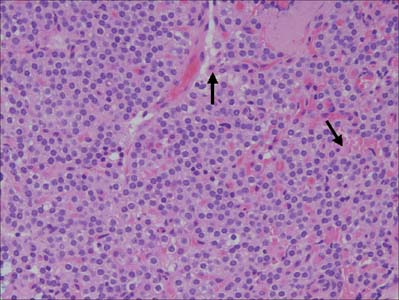
Fig. 28.24 Parathyroid gland, showing clusters and cords of small, tightly packed chief cells surrounded by vascular sinusoids. Scattered oxyphil cells (arrowed) are generally larger and more eosinophilic.
(By courtesy of Mr Peter Helliwell and Dr Joseph Mathew, Department of Histopathology, Royal Cornwall Hospitals Trust, UK.)
A second cell type, the oxyphil (eosinophil) cell, appears just before puberty and increases in number with age. Oxyphil cells are larger than chief cells and contain more cytoplasm, which stains deeply with eosin. Their nuclei are smaller and more darkly staining than those of chief cells, and their cytoplasm is unusually rich in mitochondria. The functional significance of oxyphil cells and their relationship to chief cells are uncertain.
ROOT OF THE NECK
The root of the neck is a zone of transition between four discrete anatomical spaces: the neck, the thorax and both upper limbs (Fig. 28.18). It contains the subclavian vessels; common carotid artery; trunks of the brachial plexus; sympathetic trunk; phrenic, vagus and recurrent laryngeal nerves (all bilaterally); the terminal portion of the thoracic duct (on the left side only); the terminal portion of the right lymphatic duct (on the right side only); and the oesophagus and trachea (in the midline). The brachiocephalic veins are formed by the union of the internal jugular and subclavian veins at the junction of the neck and thorax, behind the head of the clavicle.
The essential anatomical landmark in orienting and understanding the root of the neck is scalenus anterior, covered by the prevertebral layer of deep cervical fascia. Anteriorly lie sternocleidomastoid and subclavius, the intermediate tendon of omohyoid, the subclavian vein, branches from the thyrocervical trunk of the first part of the subclavian artery (transverse cervical, suprascapular and ascending cervical arteries), and the phrenic nerve. The nerve lies on the surface of scalenus anterior in the root of the neck, before passing between it and the subclavian vein to enter the superior mediastinum, and is the anatomical key to identifying the muscle intra-operatively. Posteriorly, the roots of the brachial plexus and the second part of the subclavian artery separate scalenus anterior from scalenus medius. Pathologies that cause impingement upon either brachial plexus or subclavian artery may present clinically as an upper limb compression syndrome. The suprapleural membrane and pleura are intimate posterior relations of scalenus anterior. On each side, the apical (cervical) pleura and the apex of the lung bulge up into the root of the neck. The height to which the apical pleura rises – with reference to the first pair of ribs and costal cartilages – varies in different individuals according to the obliquity of the thoracic inlet. Posteriorly, the apical pleura typically reaches the level of the neck of the first rib; it forms a domed roof over each side of the thoracic cavity that is strengthened by the suprapleural membrane. Scalenus anterior covers the anterolateral part of the dome of the pleura, and separates it from the subclavian vein. The subclavian artery crosses the dome below its summit, immediately above the vein. The costocervical trunk arches backwards from the subclavian artery and crosses the summit of the dome: its superior intercostal branch descends behind the dome, between the first intercostal nerve laterally and the first thoracic sympathetic ganglion medially.
Medial relations of scalenus anterior are longus colli and the inferior thyroid artery. The two muscles are separated by an angular interval through which the vertebral artery and vein pass to gain access to the foramen transversarium of the sixth cervical vertebra, and more anteriorly the inferior thyroid artery arches from lateral to medial on its way to the thyroid gland. The cervical sympathetic chain and the inferior cervical ganglion lie close to the posteromedial aspect of the vertebral artery here. The internal thoracic artery descends from the first part of the subclavian artery: it passes behind the brachiocephalic vein and, on the right side, is crossed by the phrenic nerve. The vagus descends anterior to the first part of the subclavian artery; on the right side only its recurrent laryngeal branch usually turns around the lower border of the artery. The terminal portions of the thoracic duct and the right lymphatic duct, on the left and right sides respectively, cross the triangular interval at the level of the seventh cervical vertebra, coming into contact with the medial edge of scalenus anterior.
The axillary sheath, an extension of the prevertebral fascia that accompanies the axillary artery and trunks of the brachial plexus, lies lateral to scalenus anterior.
Cervical rib
A small extra rib (cervical rib) may develop in the root of the neck in association with the seventh cervical vertebra. It is often fibrous in nature, although in some cases it may have undergone ossification. A cervical rib may cause compression of the subclavian artery and the lower roots of the brachial plexus. Should this occur, affected individuals will complain of pain, paraesthesia and even pallor of the affected upper limb, a condition known as thoracic outlet syndrome.
OESOPHAGUS – CERVICAL PORTION
The oesophagus is a muscular tube approximately 25 cm long, connecting the pharynx to the stomach. It begins in the neck, level with the lower border of the cricoid cartilage and the sixth cervical vertebra. It descends, largely anterior to the vertebral column, into the superior mediastinum. Generally vertical and median, it inclines to the left as far as the root of the neck, and also bends in an anteroposterior plane to follow the cervical curvature of the vertebral column.
The trachea lies anterior to the oesophagus, attached to it by loose connective tissue. The vertebral column, longus colli and prevertebral layer of deep cervical fascia are posterior, and the common carotid artery and posterior part of the thyroid gland are lateral on each side. In the lower neck, where the oesophagus deviates to the left, it becomes closer to the left carotid sheath and thyroid gland than it is on the right. The thoracic duct ascends for a short distance along its left side. The recurrent laryngeal nerves ascend on each side in or near the groove between the trachea and the oesophagus.
TRACHEA – CERVICAL PORTION
The trachea is a tube 10–11 cm long, formed of cartilage and fibromuscular membrane. It descends from the larynx, and extends from the level of the sixth cervical vertebra to the upper border of the fifth thoracic vertebra (Figs 28.14, 28.17). It lies approximately in the sagittal plane but its point of bifurcation is usually a little to the right. The trachea is flexible and can rapidly alter in length. It is flattened posteriorly so that in transverse section it is shaped, with some individual variation, like a letter D. Its external transverse diameter is 2 cm in adult males, and 1.5 cm in adult females. The lumen in live adults is 1.2 cm in transverse diameter. In children the trachea is smaller, more deeply placed and more mobile. Tracheal diameter does not exceed 3 mm in the first postnatal year: during later childhood its diameter in millimetres is about equal to age in years.
The relationships of the trachea to other cervical structures is of clinical significance: tracheostomy is not an uncommon clinical procedure (see below). Anteriorly the cervical part of the trachea is crossed by skin and by the superficial and deep fasciae. It is also crossed by the jugular arch and overlapped by sternohyoid and sternothyroid. The second to fourth tracheal cartilages are crossed by the isthmus of the thyroid gland, above which an anastomotic artery connects the bilateral superior thyroid arteries. Below and in front are the pretracheal fascia, inferior thyroid veins, thymic remnants and the arteria thyroidea ima (when it exists). In children the brachiocephalic artery crosses obliquely in front of the trachea at or a little above the upper border of the manubrium. The left brachiocephalic vein may also rise a little above this level. The oesophagus lies posterior to the trachea, and separates it from the vertebral column. The paired lobes of the thyroid gland, which descend to the fifth or sixth tracheal cartilage, and the common carotid and inferior thyroid arteries, all lie lateral to the trachea. The recurrent laryngeal nerves ascend on each side, in or near the grooves between the sides of the trachea and oesophagus.
Vascular supply and lymphatic drainage
The cervical part of the trachea is mainly supplied by branches from the inferior thyroid arteries. The tracheal veins drain into the bracheocephalic veins via the inferior thyroid plexus, and lymphatic vessels drain into the pretracheal and paratracheal nodes.
The trachea is innervated by branches from the vagi, recurrent laryngeal nerves and sympathetic trunks.
The trachea may be accessed directly in the neck via cricothyroidotomy or tracheostomy. There are numerous indications for performing an elective tracheostomy. They include: the need to provide prolonged intubation, manage acute airway obstruction from supraglottic or glottic pathology or trauma (for example, midface, mandibular or laryngeal fractures).
For detailed descriptions of the operative procedures, appropriate surgical texts should be consulted. However, it is worth emphasizing here the importance of understanding the relevant regional anatomy. In creating a surgical airway, potential hazards can be avoided by dissecting in the midline. Dissections that stray laterally, which are a real risk in pediatric patients or in those who are obese, can result in pneumothorax, pneumomediastinum and damage to paratracheal structures (the carotid sheath and its contents, and the recurrent laryngeal nerves and inferior thyroid veins lying in the tracheo-oesophageal groove). In the midline, the isthmus of the thyroid gland, which overlies the 2nd and 3rd tracheal rings, must be divided. Careful haemostasis of the divided stumps, and secure transfixion of the thyroidea ima artery and inferior thyroid vein, minimize the risk of catastrophic post-operative bleeding. A high bifurcation of the brachiocephalic trunk, or aberrant anterior jugular veins (which usually lie between the midline and anterior border of sternocleidomastoid), are additional anatomical complications.
Cricothyroidotomy endangers the cricothyroid artery (a branch of the superior thyroid artery), which is usually found close to the midline, and which reaches the median cricothyroid ligament close to the thyroid cartilage.
Berkovitz BKB, Kirsch C, Moxham BJ, Alusi G, Cheeseman T. Interactive Head and Neck. London: Primal Pictures, 2002.
Bogduk N, Windsor M, Inglis A. The innervation of the cervical intervertebral discs. Spine. 1988;13:2-8.
Brown H. Anatomy of the spinal accessory nerve plexus: relevance to head and neck cancer and atherosclerosis. Exp Biol Med. 2002;227:570-578.
Cady B, Rossi RL. Surgery of the Thyroid and Parathyroid Glands. Philadelphia: Saunders, 1991.
Crile G. Excision of cancer of the head and neck with special reference to the plan of dissection based on one hundred and thirty two operations. J Am Med Assoc. 1906;47:1780-1786.
Seminal paper which considers the surgical anatomy of radical neck dissection..
Froes LB, De Tolosa EMC, Camargo RDC, Pompeu E, Liberti EA. Blood supply to the human sternocleidomastoid muscle by the sternocleidomastoid branch of the occipital artery. Clin Anat. 1999;12:412-416.
Ger R, Evans JT. Tracheostomy: an anatomico-clinical review. Clin Anat. 1993;6:337-341.
Jarvis JF. Displaced brachiocephalic artery: a potential hazard in tracheostomy. S Afr Med J. 1966;40:396-397.
Kapandji IA. The Physiology of Joints. Ediburgh: Churchill Livingstone, 1975.
Lingeman RE. Surgical anatomy. Cummings CW, et al, editors. Otolaryngology, Head and Neck Surgery, 3rd edn., vol. 2. St Louis: Mosby, 1998;1673-1685.
Lucas GDA, Laudanna A, Chopard RP, Raffaelli EJr. Anatomy of the lesser occipital nerve in relation to cervicogenic headache. Clin Anat. 1994;7:90-96.
Matthers LHJr, Smith DW, Frankel L. Anatomical considerations in placement of central venous catheters. Clin Anat. 1992;5:89-106.
Moreau S, de Rugy MG, Babin E, Salame E, Delmas P, Valdazo A. The recurrent laryngeal nerve: related vascular anatomy. Laryngoscope. 1998;108:1351-1355.
Nash L, Nicholson HD, Zhang M. Does the investing layer of the deep cervical fascia exist? Anesthesiology. 2005;103:962-968.
Pandit JJ, Dutta D, Morris JF. Spread of injectate with superficial cervical plexus block in humans: an anatomical study. Br J Anaesth. 2003;91:733-735.
Racic G, Matulic J, Roje Z, Dogas Z, Vilovic K. Abnormally high bifurcation of the brachiocephalic trunk as a potential operative hazard: case report. Otolaryngol Head Neck Surg. 2005;133:811-813.
Robbins KT. Neck dissection. Cummings CW, et al, editors. Otolaryngology, Head and Neck Surgery, 3rd edn., vol. 2. St Louis: Mosby, 1998;1787-1819.
Shah JP, Patel SJ. Cervical lymph nodes. In Head and Neck Surgery and Oncology, 3rd edn., Edinburgh: Mosby; 2003:353-394.
Smoker WRK, Harnsberger HR. Differential diagnosis of head and neck lesions based on their space of origin. 2. The infrahyoid portion of the neck. Am J Roentgenol. 1991;157:155-159.
Wilson-Pauwels L, Akesson EJ, Stewart PA. Cranial Nerves: Anatomy and Clinical Comments. Toronto: Decker, 1998.
Yalcxin B. Anatomic configurations of the recurrent laryngeal nerve and inferior thyroid artery. Surgery. 2006;139:181-187.
Zhang M, Lee ASJ. The investing layer of the deep cervical fascia does not exist between the sternocleidomastoid and trapezius muscles. Otolaryngol Head Neck Surg. 2002;127:452-457.