Chapter 8 Respiratory system
The function of the respiratory system is to conduct inspired air containing oxygen along the respiratory passages to the areas where gaseous exchange takes place and to conduct the expired air containing carbon dioxide out of the body.
Respiration is the gaseous exchange between an organism and its environment. All animals require oxygen to carry out the chemical processes that are essential for life: oxygen is needed by the cells to obtain energy from raw materials derived from food. This process involves the oxidation of glucose to yield energy in the form of adenosine triphosphate (ATP) (see Ch. 1). Water and carbon dioxide are produced as byproducts of this reaction. Respiration can be considered to occur in two stages:
The respiratory system consists of:
Structure and function
Nose
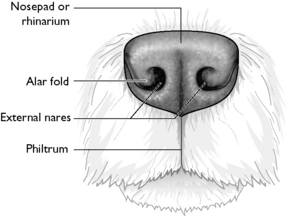
Inspired air enters the respiratory system through the nostrils or external nares leading into the nasal cavity, which is divided by a cartilaginous septum into the right and left nasal chambers. The entrance to the nasal cavity is protected by a hairless pad of epidermis consisting of a thick layer of stratified squamous epithelium, which is heavily pigmented and well supplied with mucous and sweat glands – this is known as the rhinarium and it is penetrated by the two curved nares (Fig. 8.1). The epidermis on a dog’s nose has a unique patterning that is much like a human ‘fingerprint’.
The right and left nasal chambers are filled with fine scrolls of bone called turbinates or conchae (Fig. 8.2). The chambers and the turbinates are covered by a ciliated mucous epithelium, which is well supplied with blood capillaries. The turbinates arising from the ventral part of the nasal cavity end rostrally in a small bulbous swelling visible through the nostril – the alar fold.
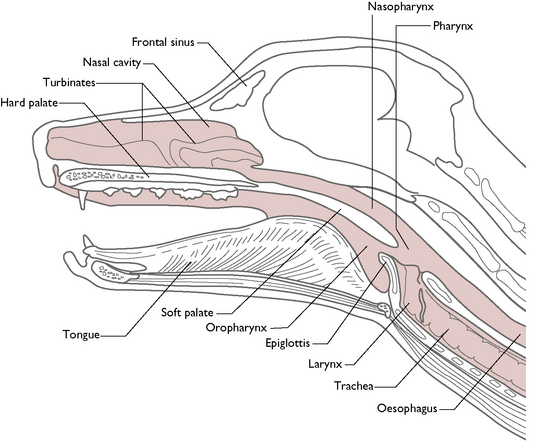
Fig. 8.2 Longitudinal section to illustrate the upper respiratory tract of the dog.
(With permission from Colville T, Bassett JM 2001 Clinical anatomy and physiology for veterinary technicians. Mosby, St Louis, MO, p 222.)
Towards the back of the nasal chambers, the mucous epithelium covering the turbinates has a rich supply of sensory nerve endings that are responsive to smell – this is the olfactory region. These nerve fibres pass through the cribriform plate of the ethmoid bone to reach the olfactory bulbs of the forebrain (see Ch. 5). The remainder of the mucous membrane is the respiratory region.
The function of the turbinates and their ciliated mucous epithelium covering is to warm and moisten the incoming air as it passes over them. The cilia and mucus help to trap any particles that are present in the inspired air and waft them to the back of the nasal cavity where they pass to the pharynx and are swallowed. The inspired air is therefore warm, damp and free from harmful particles, protecting the lungs from any form of damage.
Paranasal sinuses
A sinus is an air-filled cavity within a bone. Within the respiratory system, they are referred to as the paranasal sinuses and lie within the facial bones of the skull (Fig. 8.2). They are lined with ciliated mucous epithelium and communicate with the nasal cavity through narrow openings.
It is thought that the function of the paranasal sinuses is to lighten the weight of the skull, allowing the areas of the skull used for muscle attachment to be larger. This is evident in those species that have large, heavy skulls, such as the horse, which has numerous large paranasal sinuses. The paranasal sinuses also act as areas for heat exchange and as sites for mucus secretion.
Pharynx
From the nasal cavity, the inspired air passes into the pharynx, a region at the back of the mouth that is shared by the respiratory and digestive systems. The pharynx is divided into the dorsal nasopharynx and the ventral oropharynx by a musculomembranous partition called the soft palate (Fig. 8.2). The soft palate extends caudally from the hard palate and prevents food from entering the nasal chambers when an animal swallows (see Ch. 9). The oropharynx conducts food from the oral cavity to the oesophagus; the nasopharynx conducts inspired air from the nasal cavity to the larynx, but air can also reach the respiratory passages from the mouth, e.g. during ‘mouth breathing’.
Mouth breathing may occur during strenuous exercise to enable a greater volume of air to enter the lungs. It may also be seen in conditions that impair the flow of air through the nasal chambers, e.g. foreign bodies, tumours; or if the lung capacity is reduced, e.g. pneumothorax, haemothorax, pneumonia.
A pair of Eustachian or auditory tubes also opens into the pharynx and connects the pharynx to each of the middle ears (see Ch. 5). The function of the Eustachian tubes is to equalise the air pressure on either side of the ear drum.
Larynx
The inspired air enters the larynx, which lies caudal to the pharynx in the space between the two halves of the mandible (Fig. 8.2). The function of the larynx is to regulate the flow of gases into the respiratory tract and to prevent anything other than gases from entering the respiratory tract.
The root of the tongue is attached to one side of the hyoid apparatus and the larynx to the other. When intubating a dog or cat, pulling the tongue forward will also pull the larynx forward and the epiglottis will fall downwards, opening the glottis so that the tube can be placed correctly.
The larynx is suspended from the skull by the hyoid apparatus (see Ch. 3), which allows it to swing backwards and forwards (Fig. 8.3). The hyoid apparatus is a hollow, box-like structure consisting of a number of cartilages connected by muscle and connective tissue. The most rostral of these cartilages, the epiglottis, is composed of elastic cartilage and is responsible for sealing off the entrance to the larynx or glottis when an animal swallows. This prevents saliva or food from entering the respiratory tract, causing the animal to choke. When the larynx returns to its resting position after swallowing the epiglottis falls forward, opening the glottis and thus allowing the passage of air to resume.
Fig. 8.3 Lateral view of dog’s laryngeal area, showing the cartilages of the hyoid apparatus as they appear on X-ray.
Laryngeal paralysis is a condition seen in older dogs, often of larger breeds, e.g. Labradors. The vocal folds hang within the lumen of the larynx and are unable to move out of the flow of air. This results in interference with the passage of air down the larynx and trachea, which could result in asphyxiation during exercise. It also causes a constant ‘roaring’ sound as the dog breathes.
Within the larynx is a pair of vocal ligaments. The mucous membrane covering the inner surface of the vocal ligaments forms the vocal folds, which project bilaterally into the lumen of the larynx. When air moves past the vocal folds they vibrate and sound is produced. These sounds can be modified by factors such as the size of the glottis and the tension of the vocal folds, resulting in a characteristic range of sounds, e.g. growling, barking, purring.
Trachea
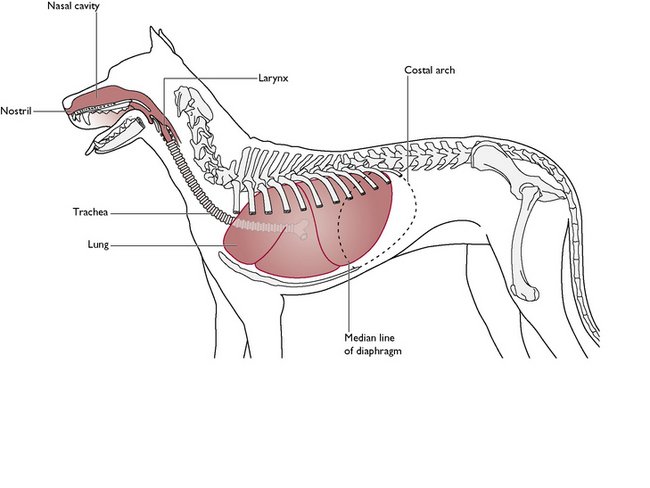
From the larynx, air enters the trachea. This is a permanently open tube attached to the caudal border of the laryngeal cartilages (Fig. 8.4). It lies on the ventral aspect of the neck, i.e. below the oesophagus and slightly to the right of it, and extends the length of the neck, passing through the cranial thoracic inlet. In the thoracic cavity it enters the mediastinum and terminates at a bifurcation above the heart.
The lumen of the trachea is kept open by a series of C-shaped rings of hyaline cartilage. These prevent the trachea from collapsing when the thoracic pressure falls and the incomplete rings allow food boluses to pass down the oesophagus unimpeded by the tracheal cartilages. The structure of the trachea is flexible to allow movement of the head and neck. The cartilage rings are connected by fibrous tissue and smooth muscle fibres.
The trachea is lined with ciliated mucous epithelium. The surface layer of mucus traps any foreign particles and the cilia ‘sweep’ the particles and mucus upwards to the pharynx, where they are spat out or swallowed. In some cases, such as in a dusty or smoky atmosphere, the production of mucus may increase. This mucus irritates the tracheal lining and causes the animal to cough. The coughing reflex serves to expel substances such as excess mucus and dust particles from the respiratory tract, preventing them from entering the lungs and is part of the animal’s primary defence system.
Tracheal collapse may be seen in some small breeds of dog, e.g. Yorkshire Terriers, and causes a chronic ‘honking’ cough. There is a risk that during strenuous exercise the trachea may flatten, preventing the flow of inspired air. This causes the dog to collapse suddenly. During the period of unconsciousness, the trachea relaxes, air begins to flow again and the dog recovers.
Bronchi and bronchioles
The trachea divides (or bifurcates) into the right and left bronchi (sing. bronchus), entering each of the lungs respectively. As they enter the lung tissue the bronchi divide into smaller and smaller branches, like a tree. This arrangement is therefore known as the bronchial tree. The point at which each bronchus enters the lung is known as the root of the lung.
The bronchi are supported by complete rings of cartilage but, as the branches become smaller, the cartilaginous support gradually diminishes, and then disappears completely, at which point the passages are called bronchioles. The bronchioles continue to branch into smaller passages throughout the lungs. Finally, the smallest diameter branches are known as the alveolar ducts and lead to the alveoli.
The walls of the bronchi and bronchioles contain smooth muscle, which is under the control of the autonomic nervous system. The respiratory passages are able to dilate to enable a greater volume of air to reach the lungs, e.g. during exercise, or constrict to their original size during ‘normal’ breathing.
Alveoli
The alveolar ducts end as the alveolar sacs, which resemble bunches of grapes. Each alveolar sac consists of a large number of alveoli, which are small, thin-walled sacs surrounded by capillary networks (Fig. 8.5). The epithelial lining of the alveolus is called the pulmonary membrane, and is very thin to allow gaseous exchange with the blood to take place. Oxygen in the inspired air diffuses across the pulmonary membrane of the alveolus into the blood within the capillaries of the pulmonary circulation. Simultaneously, it is exchanged for carbon dioxide in the blood, which is to be excreted in the expired air from the lungs (Fig. 8.6). There are millions of alveoli in each lung, providing a large surface area for gaseous exchange.
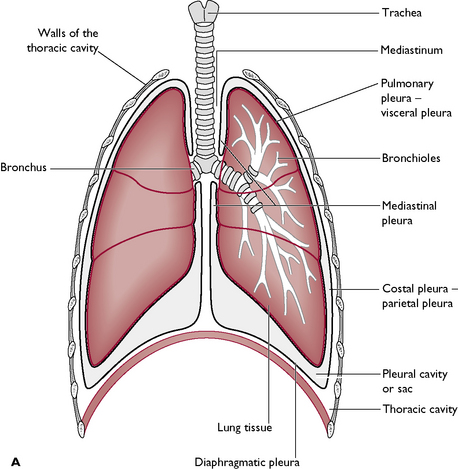
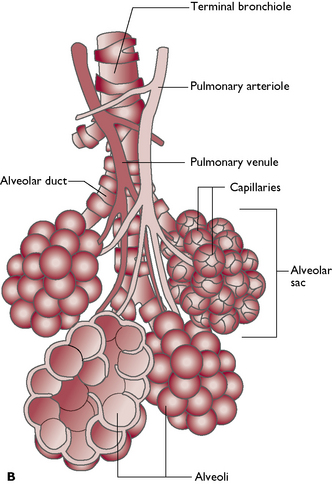
Fig. 8.5 The lungs within the thoracic cavity. A The pleural membranes. B The terminal air passages.
(Part B with permission from Colville T, Bassett JM 2001 Clinical anatomy and physiology for veterinary technicians. Mosby, St Louis, MO, p 227.)
Fig. 8.6 The exchange of gases within the alveoli. A Inspiration: the air contains high levels of oxygen and low levels of carbon dioxide. Blood entering the alveolar capillary contains low levels of oxygen and high levels of carbon dioxide. B Gas exchange occurs: oxygen diffuses from air in the alveolus, where its level is high, into blood in the alveolar capillary, where its level is low. Carbon dioxide does the reverse, diffusing from alveolar capillaries into the alveolus. C Expiration: exhaled air contains less oxygen and more carbon dioxide than are present in room air. Next breath brings in a fresh supply of high oxygen air.
(With permission from Colville T, Bassett JM 2001 Clinical anatomy and physiology for veterinary technicians. Mosby, St Louis, MO, p 233.)
The parts of the respiratory tract that are not involved in gaseous exchange, i.e. all but the alveoli, are referred to as the dead space. Their function is to conduct gases to and from the area of gaseous exchange.
Lungs
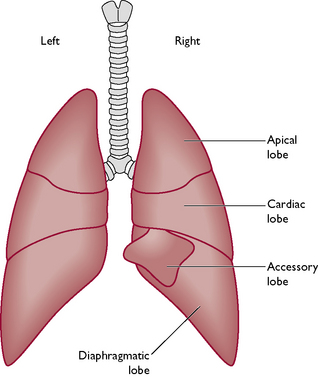
The right and left lungs lie within the thoracic cavity on either side of the double layer of connective tissue known as the mediastinum (Figs 8.7, 8.8). Each lung consists of the air passages (only the most proximal parts of the bronchi are outside of the lung), blood vessels and surrounding connective tissue, all enclosed within a membrane called the pulmonary pleura (Fig. 8.5A).
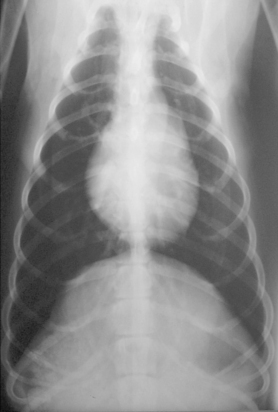
Fig. 8.7 Ventrodorsal radiograph of a dog’s thorax. The lungs are full of air and appear dark on the X-ray.
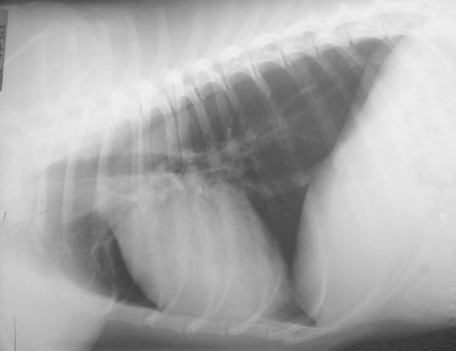
Fig. 8.8 Lateral radiograph of a dog’s thorax. The lungs appear dark on the X-ray due to air, and allow the other structures to be visualised.
The lungs are divided into well-defined lobes by deep fissures (Fig. 8.9). The left lung is divided into three lobes; the right lung has four lobes. The lobes are referred to as the cranial or apical, middle or cardiac, and caudal or diaphragmatic. The fourth lobe of the right lung is the accessory lobe; this is small and lies on the medial surface of the caudal lobe of the right lung.
Thoracic cavity
The thoracic cavity or thorax is divided into the right and left pleural cavities by a double layer of pleura known as the mediastinum. Each pleural cavity is lined by a single layer of serous membrane, the pleural membrane (Fig. 8.5). This secretes a small amount of serous or watery fluid whose function is to reduce friction between the pleural surfaces as the lungs move during respiration.
If the pleural cavity becomes occupied by anything other than a vacuum, e.g. air (pneumothorax), blood (haemothorax) or pus (pyothorax), the ability of the lung to inflate fully will be impaired and the animal will show signs of respiratory distress (dyspnoea).
All the structures lying in the pleural cavities are covered in the pleural membrane and it is named according to the structures it is covering. The pleural cavity lies between the two layers of pleural membranes and contains a vacuum and a small volume of pleural fluid (Fig. 8.5A).
| Type of pleura | Structures covered |
|---|---|
| Diaphragmatic | Cranial aspect of the diaphragm |
| Pulmonary or visceral | Right and left lungs – outlines each lobe |
| Costal or parietal | Inner side of the ribs |
| Mediastinal | Mediastinum |
Most of the organs in the thorax lie in the space between the two layers of mediastinal pleura, i.e. the heart and its associated blood vessels, trachea and oesophagus (Fig. 8.10). The mediastinum of the dog and cat is quite tough and forms a complete barrier between the two pleural cavities. If one side is damaged or becomes infected then, providing that the mediastinum remains intact, the effect is limited to that side and the other lung can continue to function normally.
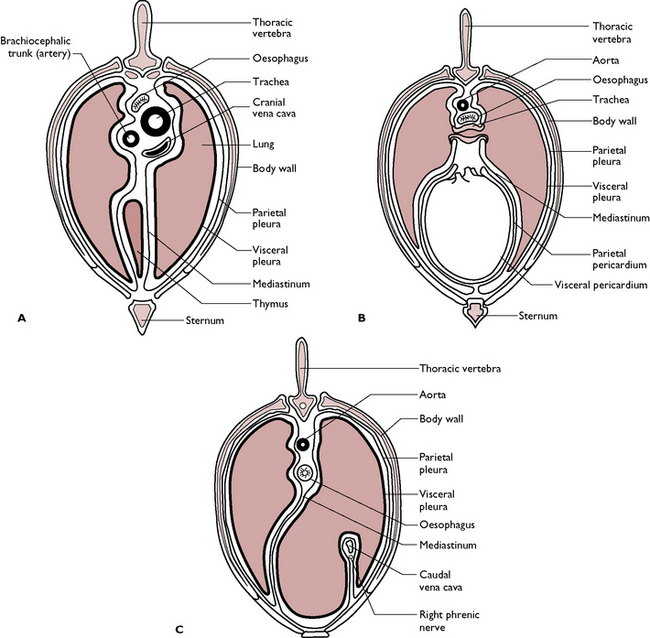
Fig. 8.10 Cross-section of the thorax at three different levels, showing the positions of major structures. A Section taken cranial to the heart. B Section taken through the heart. C Section taken caudal to the heart.
(With permission from Colville T, Bassett JM 2001 Clinical anatomy and physiology for veterinary technicians. Mosby, St Louis, MO, p 230.)
The mechanics of respiration
Respiration, which may also be referred to as breathing or pulmonary ventilation, is achieved by a coordinated series of actions carried out by muscles. This brings about the alternate expansion and reduction in the volume of the thoracic cavity.
The lungs are suspended within the thoracic cavity, which is divided into the right and left pleural cavities by the pleural membranes. The pleural cavities contain a vacuum and, as they are totally enclosed, any increase in their volume will result in negative pressure and air will be sucked into the lung tissue. Conversely, if the volume of the pleural cavity decreases, the increase in pressure will push air out. This is the principle behind inspiration and expiration.
Three sets of muscles are responsible for respiration:
Control of respiration
During normal life, the changing metabolic needs of the body make demands on the respiratory system. As the tissues are remote from the organs involved in the intake and expulsion of gases, a complex system of control of respiration has evolved.
Within the pons and medulla of the hindbrain there are respiratory centres responsible for the control of inspiration and expiration. They are the pneumotaxic and apneustic centres, which control expiration, and the inspiratory centre, which controls inspiration. Impulses from the inspiratory centre travel to the diaphragm via the phrenic nerve and to the intercostal muscles via the intercostal nerves and bring about inspiration. Expiration is mainly passive but impulses from the expiratory centres may assist in expiration. These centres inhibit each other and cannot work simultaneously. They are responsible for the basic rhythm of respiration.
The rate and depth of respiration is controlled by receptors within the body:
Both types of chemoreceptor monitor the levels of oxygen and the pH of the blood, e.g. high levels of carbon dioxide in the blood lower the pH, i.e. the blood becomes more acidic. This change in pH is detected by the chemoreceptors, which stimulate an increase in the rate and depth of respiration. The carbon dioxide is expelled and the pH returns to normal.
The interrelationship between the control centres in the brain and the chemoreceptors in the peripheral circulation enable the respiratory system to respond rapidly to the changing state of the body.
Respiratory definitions
When an animal is breathing normally (at rest), the amount of air that passes into and out of the lungs during each respiration is called the tidal volume. However, this is only a fraction of the actual lung capacity and more air can be inhaled during forced inspiration – this is the inspiratory reserve volume. Conversely, it is possible to forcibly exhale more air than is expired during normal respiration – this additional amount of air is called the expiratory reserve volume. However, even after the most forced exhalation there is always some air left in the lungs and airways (otherwise they would collapse) – this is called the residual volume.
The total amount of air that can be expired after a maximum inspiration is called the vital capacity. The amount of air that is left in the lungs after normal expiration is called the functional residual capacity and it is this that allows gaseous exchange to take place during expiration. The total lung capacity is the sum of the residual volume, expiratory reserve volume, tidal volume and inspiratory reserve volume. Much of the air drawn in at each breath is exhaled again before it reaches the alveoli (i.e. it is not involved in gaseous exchange) – this is equal to the volume of the conducting system and is called the dead space.