Blood-borne Pathogens
After completing this chapter, the student should be able to do the following:
 List the blood-borne pathogens important to the practice of dentistry.
List the blood-borne pathogens important to the practice of dentistry.
 Compare the five major types of viral hepatitis.
Compare the five major types of viral hepatitis.
 Describe the relative infectivity of blood-borne pathogens after an occupational exposure.
Describe the relative infectivity of blood-borne pathogens after an occupational exposure.
 Outline the clinical course of human immunodeficiency virus disease.
Outline the clinical course of human immunodeficiency virus disease.
 List and describe the three major routes of human immunodeficiency virus transmission.
List and describe the three major routes of human immunodeficiency virus transmission.
As described in Chapter 3, the patient’s oral cavity is the single most important source of potentially pathogenic microorganisms. Pathogenic agents may be present in the mouth as a result of four basic processes: blood-borne diseases, oral diseases, systemic diseases with oral lesions, and respiratory diseases. Blood-borne diseases are discussed in this chapter. Oral and respiratory diseases are presented in Chapter 7.
Blood-borne pathogens may infect different blood cells or other tissues of the body, but during infection the pathogens exist in or are released into the blood or other body fluids, which may include semen, vaginal secretion, intestinal secretions, tears, mother’s milk, synovial (joint) fluid, pericardial (around the heart) fluid, amniotic fluids (surround the developing fetus), and saliva. Because blood or other body fluids may contain these pathogens, the disease may be spread from one person to another by contact with the fluids. Thus the diseases are called blood-borne diseases. Blood-borne pathogens may enter the mouth during dental procedures that induce bleeding. Thus contact with saliva during such procedures may result in exposure to these pathogens if they are present. Because determining whether blood is actually present in saliva is difficult, saliva from all dental patients should be considered potentially infectious.
VIRAL HEPATITIS
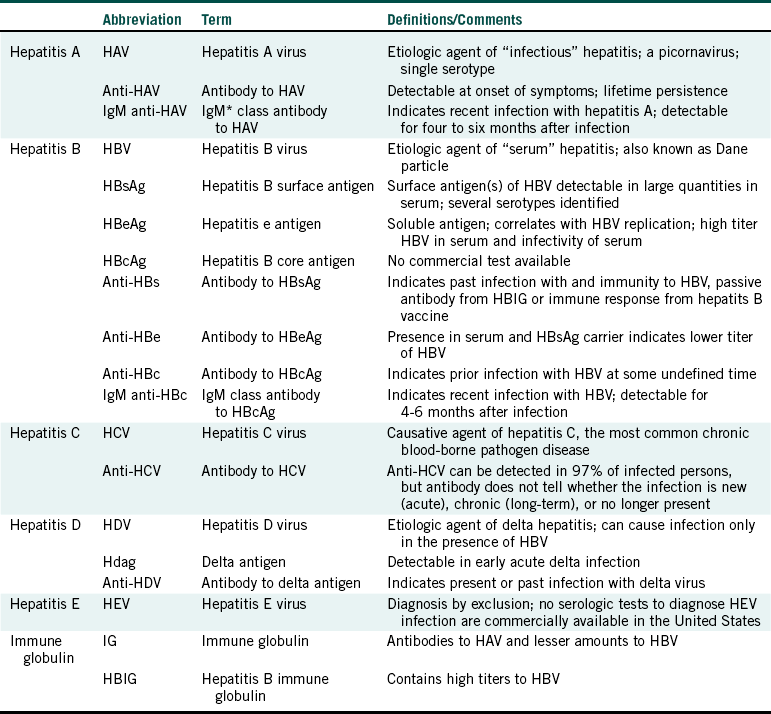
Five common hepatitis viruses cause clinically similar diseases: hepatitis A, B, C, D, and E (Table 6-1). Hepatitis A virus and hepatitis E virus are transmitted mainly through contaminated food and water (fecal-oral routes of spread), whereas hepatitis B virus (HBV), hepatitis C virus (HCV), and hepatitis D virus (HDV) are blood-borne diseases usually transmitted by direct or indirect contact with infected body fluids.
TABLE 6-1
Comparison of Hepatitis Viruses
Modified from Palenik CJ: Hepatitis C virus and dental personnel, Dent Today 23:56-59, 2004.
Hepatitis means an inflammation of the liver. Often the inflammation is virally related; however, hepatitis also may be caused by excessive alcohol consumption, exposure to some hazardous chemicals, and as a complication of other infections.
Hepatitis B
Hepatitis B is a major health problem in the United States and worldwide. Hepatitis B is endemic (occurs regularly) in many parts of the world. The number of new infections per year in the United States has declined from an estimated 260,000 in the 1980s to about 46,000 in 2006. About 8,000 persons with acute infections will require hospitalization. About 180 persons will die of fulminant hepatitis (an overwhelming and rapidly destructive form of the disease), whereas more than 3700 persons will become chronic carriers of the virus. About 5000 persons with chronic hepatitis B die each year. Current estimates by the Centers for Disease Control and Prevention (CDC) suggest that there are 1 million to 1.25 million HBV carriers in the United States. Each person has some potential to spread the virus to others. More than 200 million persons are estimated to be carriers worldwide. Hepatitis B virus accounts for 34% of all types of acute viral hepatitis.
HEPATITIS B VIRUS
The HBV is an enveloped DNA virus that infects and multiplies in human liver cells. During the course of an infection, the virus and cells containing the virus are released in high numbers into the bloodstream and other body fluids, explaining its description as a blood-borne disease agent. A milliliter of blood from an infected person may contain as many as 100 million virus particles, meaning that only small amounts of blood or other body fluids are necessary to transmit the disease to others. The virus has three components that are important antigens; some components are on its surface (hepatitis B surface antigen, or HBsAg), and two are inside the virus (hepatitis B core antigen [HBcAg] and hepatitis B e antigen [HBeAg]) (Table 6-2). The hepatitis B vaccines consist of the HBsAg that is synthesized using yeast cells in a laboratory by genetic engineering techniques.
Hepatitis B virus has been shown to remain viable at room temperature for at least 1 month. The virus can be killed or inactivated by commonly used methods of sterilization and disinfection, including the steam autoclave, and a 10-minute exposure to 1:100 diluted bleach, 1:16 diluted phenolic glutaraldehyde, 75 ppm iodophor, and 70% isopropyl alcohol. Thus HBV is easy to kill when outside the body, provided the killing agent comes into direct contact with the virus. Hepatitis B virus is more easily killed than Mycobacterium tuberculosis and bacterial spores.
DISEASE STATES
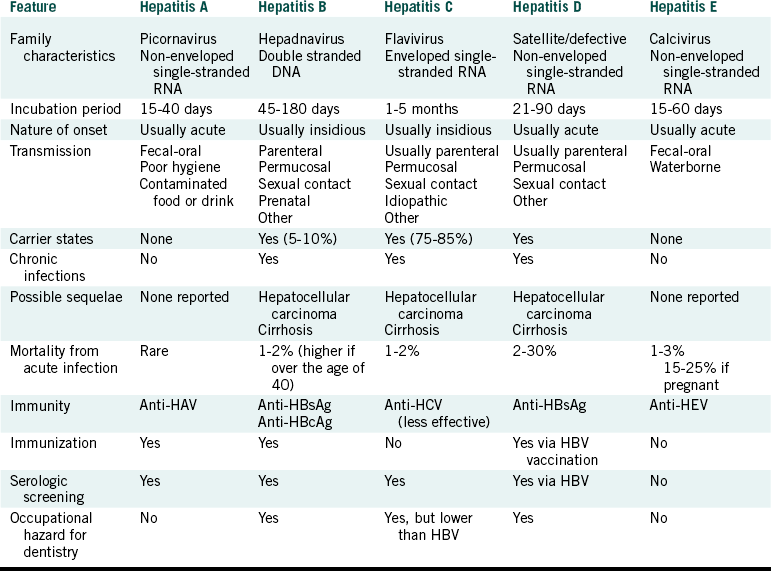
Human beings are the only known natural hosts of HBV. About 90% of those infected with HBV undergo complete recovery without developing a carrier state (Figure 6-1). About 2% to 10% become carriers of the virus, with about one half eliminating the virus from their bodies within 5 years. The other half become chronic carriers, and about 25% of these will develop chronic active hepatitis. Persons who have chronic active hepatitis have a 200 to 300 times greater chance of later developing liver cancer (hepatocellular carcinoma). Premature mortality from chronic liver disease occurs in about 15% to 25% of the chronically infected.
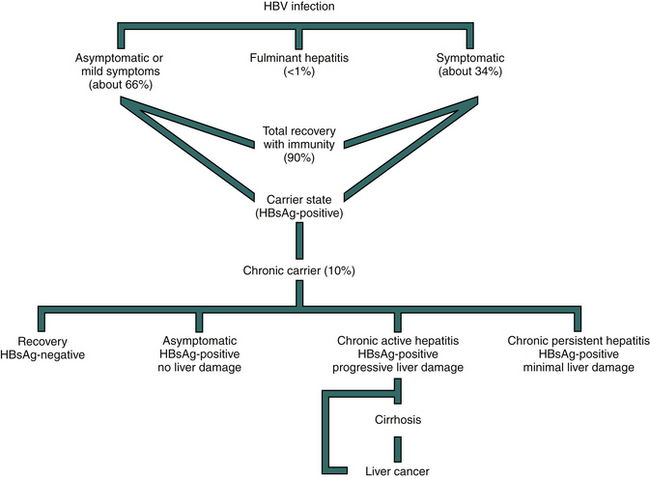
FIGURE 6-1 Hepatitis B outcomes. Hepatitis B virus infection may result in clinical symptoms in about one third of the cases and no symptoms or unrecognized symptoms in about two thirds of the cases. A rapidly progressive fulminant disease leading to death occurs in less than 1% of the cases. About 90% of all infected persons recover. The remaining 10% develop chronic infection and may carry the virus for up to 6 months and then have complete recovery. Others remain as chronic carriers, being asymptomatic, having chronic active hepatitis or having chronic persistent hepatitis.
The carrier state is defined as being HBsAg-positive on at least two occasions when tested at least 2 months apart or being HBsAg-positive and immunoglobulin M anti–HBc-negative at a single test. Anyone who is positive for HBsAg has a potential to spread the disease to others. Those who are also HBeAg-positive have high concentrations of the virus in their blood and therefore are considered as being highly infectious.
TRANSMISSION
Hepatitis B virus is spread percutaneously (through the skin) or permucosally (through mucous membranes) by contact with infected body fluids, for example, at birth, during sexual activities, or with contaminated needles or other sharp objects. Perinatal transmission of the virus to infants at birth is efficient. If the mother is positive for HBsAg and HBeAg, the infant has a 70% to 90% chance of being infected. If the mother is only HBsAg-positive, the risk to the infant drops to 20%. Up to 90% of infected infants become chronic carriers. When infection occurs between 1 and 5 years of age, 30% of children become chronic carriers. Above the age of 5 years the rate drops to about 6%.
The virus also may be spread in environments involving frequent close contact with an infected person, as in households or institutions for developmentally disabled children. This latter route of spread likely involves unnoticed contact of infected body fluids with skin lesions or mucosal surfaces.
Infection occurs when blood or body fluids from an infected person enter the body of a person who is not immune to HBV. High-risk behaviors for acquiring hepatitis B include the following:
• Sharing of contaminated needles during intravenous drug abuse
• Sexual intercourse with an infected person without using a condom
Spread of HBV through transfused blood or blood products is now rare because of routine testing of blood for HBsAg and donor screening. A fecal-oral route of transmission does not occur commonly. No transmission appears to occur through tears, sweat, stool, urine, or droplet infection.
SYMPTOMS
If symptoms develop after infection, they begin to appear 45 to 180 days (average of 60 to 90 days) after exposure. Roughly one third of those infected (see Figure 6-1) exhibit the more easily recognizable symptoms of yellowing of the skin (jaundice) and whites of the eyes, light-colored stools, dark urine, joint pain, fever, a rash, and itching. Clinical illness is more common among infected individuals above 5 years of age. About another one third of those infected develop less descript mild symptoms that may include malaise (“not feeling good”), loss of appetite, nausea, and abdominal pain. The remaining one third develop no symptoms at all. Thus two thirds of all those infected develop no symptoms or mild nondescript symptoms that often are unrecognized as being related to hepatitis. Yet symptomatic and asymptomatic carriers can spread the virus to others. This unrecognizable infection with HBV and with other viruses (such as human immunodeficiency virus, HIV, described later) serves as the basis for universal and standard precautions—applying infection control procedures during care for all patients, not just those who are considered infectious.
Development of a hepatitis B chronic carrier state may occur more commonly in those who are asymptomatic and is more likely to occur in the young. Women who are pregnant should seek the advice of their personal physician about being tested for HBV, so that, if infected, proper procedures can be instituted to protect the newborn. One could be infected unknowingly with HBV, not develop any recognizable symptoms, become a chronic carrier, unknowingly spread the virus to others, and die years later of HBV liver damage. Hepatitis B is obviously an insidious disease.
RISK FOR THE DENTAL TEAM
Several blood testing surveys of dental workers conducted between 1975 and 1982 attempted to determine how many of the different types of dental workers had been infected with HBV. Although some of the studies involved only small groups of workers, the results suggested that about 13% of dental assistants, 17% of dental hygienists, 14% of dental laboratory technicians, and 9% to 25% of dentists had been infected. At that time, about 5% of the general population was estimated to have been infected. Thus unvaccinated members of the dental team are at least 2 to 5 times more likely to become infected with HBV than the general population.
In the early to mid-1980s, 10,000 to 12,000 cases of HBV infection (about 4% of all cases) occurred annually in persons who had an occupational risk for exposure to body fluids. In 1994 this number dropped to about 1000 cases, showing about a 90% decrease in HBV among health care workers. This decrease can be related to the development of a protective vaccine and the increased application of better engineering and work practice controls and personal protective equipment. However, exposure still can occur readily through injuries with contaminated sharp instruments and needles. Thus hepatitis B still remains the most important occupationally acquired disease for dental professionals.
The greatest dental occupational risks for exposure are the following:
DENTIST-TO-PATIENT SPREAD OF HEPATITIS B
The chances of a patient acquiring any disease in a dental office are low. In the past, HBV has been spread from dentists to patients, as documented in 11 separate instances. In each instance, the dentist was highly infectious (HBeAg-positive) and apparently did not wear gloves routinely. These instances occurred between 1974 and 1987, with none, as yet, being reported since. The drop in the spread of HBV from dentists to patients coincides with the time (around 1984) when infection control in dentistry was reemphasized as a result of the advent of acquired immunodeficiency syndrome (AIDS).
PATIENT-TO-PATIENT SPREAD OF HEPATITIS B
After a lull of 14 years, HBV raised its ugly head again in 2001 as the cause of an infection in a dental patient as reported by Redd et al. in May of 2007. Hepatitis B was spread from one patient to another patient on the same day in 2001 in an oral surgery practice. The source patient was a 36-year-old chronic carrier positive for HBsAg and HBeAg, the latter indicating high communicability. She had some teeth extracted on the day of the incident but did not tell anyone in the office that she was an HBV carrier. A little over 2.5 hours after her teeth were extracted, the same oral surgeon and staff extracted 7 teeth from a 61-year-old woman who later developed hepatitis B, but recovered. Molecular epidemiologic techniques determined that the same virus caused hepatitis B in both women. Fourteen of the 15 employees in the practice were tested and showed evidence of HBV vaccination, and none showed any evidence of previous HBV infection. Testing of 25 of the 27 patients seen after the source patient that week in the practice revealed that 19 of them were immune to hepatitis B. This included 3 of the 5 patients seen after the source patient on the same day. CDC investigators visited the practice after the incident and determined that the office was clean, that standard precautions were being practiced, and that appropriate infection control procedures were in place at that time.
Since no clear-cut mode of viral spread was identified in this case, the CDC investigators could only speculate on the mechanism of transmission involved. One possibility mentioned was the spread of the virus from a contaminated environmental surface. HBV is known to survive for several days in dried blood, and maybe a contaminated surface was not properly managed after treatment of the source patient.
This case alerts us to the continued importance of the potential spread of HBV in dentistry and the importance of HBV vaccination. The spread of this virus in this case was likely limited by the high incidence of HBV immunity in the staff and patients.
HEPATITIS B VACCINE
The availability of safe and effective vaccines for hepatitis B is fortunate. Because no successful medical treatment exists to cure this disease, prevention is of paramount importance. Chapter 9 presents details on the vaccines and the vaccination series. The vaccines are strongly recommended for all members of the dental team. The Occupational Safety and Health Administration of the U.S. Department of Labor actually requires dentist-employers to offer the hepatitis B vaccine series free of charge to office staff who may have any potential for exposure to blood or saliva. The requirement applies to employers in all health care and other professions in which body fluid exposure is possible. Also, in late 1991 the CDC recommended hepatitis B vaccination for all newborns, and in 1995 the CDC recommended vaccination for 12 year olds who were not vaccinated previously. In 2006 CDC recommended vaccination for all unvaccinated adults at risk for HBV infection and for all adults requesting protection from HBV infection. They also stated that acknowledgment of a specific risk factor should not be a requirement for vaccination. Because no vaccine is 100% effective, the CDC does recommend testing for immunity (anti-HBsAg antibody) 1 to 2 months after one receives the third inoculation of the vaccine series.
Hepatitis C
Hepatitis C virus previously was called parenterally transmitted non-A, non-B hepatitis (see Table 6-2). Hepatitis C virus is thought to cause about 30% of acute viral hepatitis cases in the United States and is a blood-borne disease. About 19,000 persons in the United States are estimated to become infected with HCV every year, but only about 20% of those infected have any (generally mild) recognizable symptoms.
About 50% of hepatitis C cases are associated with intravenous drug abuse, 10% with sexual activity, 3% with blood transfusions, and 1% with occupational exposure in health care workers. The remaining cases have unidentified routes of transmission. Hepatitis C virus has been transmitted to medical health care workers through needlestick injuries.
An alarming fact about hepatitis C is that 75% to 85% of those infected apparently become chronic carriers, and 20% develop chronic liver disease. An estimated 3.2 million persons have chronic infection with HCV, and deaths from cirrhosis may occur in 1% to 5% of all those infected.
Until recently, HCV was diagnosed by indirect means showing that the patient did not have type A or type B hepatitis. The causative virus was first isolated in 1989, and a blood test for antibodies to HCV was designed in 1991. This test aids in diagnosing the disease, identifying those who are or have been infected, and in screening potential blood donors. As yet, no vaccine is available for hepatitis C, but development of the badly needed test for HCV is leading to firmer information on modes of spread of this virus. Those at the highest risk are injection drug users and recipients of clotting factors made before 1987. Those at intermediate risk include hemodialysis patients, recipients of blood and/or solid organs before 1992, people with undiagnosed liver problems, and infants born to infected mothers. Those with low risk include health care and public safety workers, people having sex with multiple partners, and people having sex with an infected steady partner. Neither the hepatitis A nor the hepatitis B vaccine provides any protection against hepatitis C.
Hepatitis D
Infection with hepatitis D virus, previously known as the delta agent, apparently can be regarded as a complication of hepatitis B (see Table 6-1). This virus may cause infection only in the presence of an active HBV infection. Hepatitis D virus is a defective virus that needs a part of the HBV to complete its life cycle.
Infection with HDV may occur as a coinfection with HBV (HDV and HBV infect simultaneously) or as a superinfection of HDV in an HBV carrier. Both instances usually result in clinical acute hepatitis, and coinfection usually resolves, whereas superinfection frequently causes chronic HDV infection and chronic active hepatitis. Routes similar to those of HBV transmit the hepatitis D virus. Outbreaks of hepatitis D have been reported in the United States. Thus those who are susceptible to HBV infection, occupationally or otherwise, are also susceptible to HDV infection. Successful vaccination against hepatitis B also should prevent hepatitis D.
Hepatitis A and E
Hepatitis A does not pose a particular occupational risk to dental workers or patients, because this form of hepatitis is spread primarily by the fecal-oral route involving consumption of contaminated food or water (see Table 6-1). A vaccine is available for hepatitis A; vaccination is recommended for persons who may travel to countries with poor sanitation systems. Isolated instances of hepatitis A spread by contact with body fluids other than feces have been reported.
Hepatitis E also is spread by contaminated food or water, and only a handful of cases have been reported in the United States. In contrast, hepatitis E is a problem in the Middle Eastern countries.
HUMAN IMMUNODEFICIENCY VIRUS DISEASE
The human immunodeficiency virus (HIV) causes HIV disease, which involves HIV infection and progresses to a final phase called acquired immunodeficiency syndrome. In the summer of 1981 AIDS was reported as a new clinical disease, and the CDC now estimates that about 1.25 million persons in the United States have been infected with HIV. Worldwide, HIV is thought to have infected about 42 million persons. At the end of 2003, an estimated 1,039,000 to 1,185,000 persons in the United States were living with HIV/AIDS, with 24% to 27% undiagnosed and unaware of their HIV infection. In 2006, 35,314 new cases of HIV/AIDS in adults, adolescents, and children were diagnosed in the 33 states with long-term, confidential name–based HIV reporting.
Human immunodeficiency virus disease involves destruction of the immune system of the body, making an individual susceptible to life-threatening opportunistic infections and cancers. Progression from the initial phase of the disease (HIV infection) to the terminal phase of the disease (AIDS) has been lengthened significantly through the combined use of antiviral drugs. Effective therapy in the United States has made HIV disease a manageable affliction. Life after infection now can be expected to approach 25 years.
Human Immunodeficiency Virus
The human immunodeficiency virus is a member of a group of single-stranded RNA viruses called retroviruses. Human immunodeficiency virus type 1 (HIV or HIV-1) is the most common worldwide cause of HIV disease. Human immunodeficiency virus type 2 causes another less aggressive immunodeficiency syndrome, especially in Western Africa. Infection with HIV-2 in the United States is uncommon, with most cases occurring in immigrants from Africa and among injection drug abusers.
Human immunodeficiency virus primarily infects T4 lymphocytes but also can infect macrophages and a few other cell types. These special lymphocytes are the cells that regulate the immune response. Human immunodeficiency virus selectively attaches to and enters T4 lymphocytes (also called CD4 lymphocytes). The viral RNA is converted quickly into viral DNA, which then is incorporated as viral genes into the chromosomes of the host lymphocyte. Thus the lymphocyte and its succeeding generations of cells are infected permanently with the HIV-1 genes. These genes may remain latent (delayed) for prolonged periods, but they induce the production of new virus particles within the lymphocytes. This virus production occurs throughout HIV disease but at widely different rates in different patients.
Virus production destroys lymphocytes and yields more viruses that can infect and destroy even more lymphocytes. This process eventually depletes the body of T4 cells. Thus HIV produces a seemingly latent infection in which the infected person usually remains asymptomatic until the level of T4 lymphocytes becomes critically low.
Human immunodeficiency virus undergoes mutations that produce several different genetic forms as the virus replicates inside lymphocytes and other cells. This genetic variation may explain the difference in the course of HIV disease in different individuals, with some strains of HIV being more virulent than others. This genetic variation also is one reason why a vaccine for prevention has not yet been developed. A vaccine made against one HIV strain may not protect against other strains.
Although an approach to kill HIV after it is in the body is not known, HIV can be killed easily when outside the body. All forms of heat and gas sterilization readily kill it. The virus also is killed by commonly used liquid sterilants and surface disinfectants, provided the killing agent comes into direct contact with the virus. Human immunodeficiency virus is killed much more easily on instruments and surfaces than Mycobacterium tuberculosis and bacterial spores.
Disease States and Symptoms
HUMAN IMMUNODEFICIENCY VIRUS INFECTION
About 4 weeks after the initial infection with HIV, many persons experience a sore throat, fever, swollen glands, diarrhea, joint pain, and fatigue. This condition is called acute retroviral syndrome, which signifies an acute HIV infection. This process commonly occurs soon after many viral infections. Symptoms may be slight or even may go unnoticed. Antibodies to HIV usually develop within 6 to 12 weeks after initial infection, and, by 6 months, 95% of those infected have developed antibodies (seroconverted). Unfortunately, these antibodies do not protect against the disease; however, they do provide a means to diagnose HIV disease. A person with antibodies to HIV is referred to as being “HIV-positive,” indicating that the person is infected with the virus.
After acute HIV infection has occurred, most persons have no further clinical symptoms until months or years later, when the killing of T4 lymphocytes or other cells becomes prominent. Nevertheless, persons with asymptomatic HIV infection still can transmit the virus to others. Some HIV-positive persons experience persistent swollen glands under the arms and in the groin but are otherwise asymptomatic. The condition is referred to as generalized lymphadenopathy.
ACQUIRED IMMUNODEFICIENCY SYNDROME
Replication of HIV in T4 lymphocytes kills the lymphocytes, and, as more and more cells are killed, the immune system becomes progressively weaker. This immunodeficiency results in increased susceptibility to opportunistic infections that normally do not cause infections or cause less severe infections in those with healthy immune systems. When an HIV-positive patient experiences one or more of these indicator opportunistic infections or a cancer, the patient is diagnosed as having AIDS. The symptoms experienced depend on the type of infection or cancer that occurs. Eventually, one of these diseases causes death. The infectious diseases may be caused by bacterial, viral, fungal, or protozoal agents. The leading cause of death in an AIDS patient is Pneumocystis jiroveci pneumonia, a fungal infection.
Oral Manifestations of Acquired Immunodeficiency Syndrome
In many instances, early manifestations of AIDS occur as oral lesions. Oral manifestations include fungal diseases such as candidiasis (thrush), histoplasmosis, geotrichosis, or cryptococcosis; viral diseases such as warts, hairy leukoplakia, or human herpesvirus type 1 (herpes simplex) infection; bacterial diseases such as rapidly progressing periodontitis or gingivitis; and cancerous diseases such as Kaposi’s sarcoma (recently associated with human herpesvirus type 8) and non-Hodgkin’s lymphoma.
Transmission
Human immunodeficiency virus is transmitted primarily from an infected person through the following routes:
• Intimate sexual contact (vaginal, anal, oral) involving contact or exchange of semen or vaginal secretions
• Exposure to blood, blood-contaminated body fluids, or blood products (e.g., sharing intravenous drug paraphernalia)
Other exposures resulting in HIV-infection are variations of these three basic modes of transmission. Human immunodeficiency virus infection is not spread by casual contact. Table 6-3 lists risk factors for acquiring AIDS. Note the overall increase in percent of heterosexual contacts involving an infected partner as a risk factor.
TABLE 6-3
Estimated AIDS Cases by Exposure Category in the United States: through 1993, 2001 and 2006
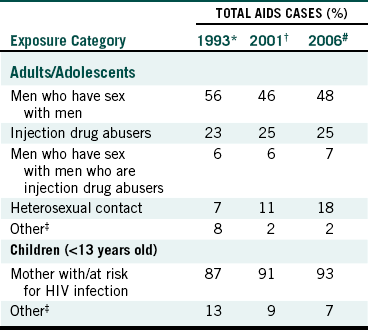
∗Based on 289,320 cases of AIDS. Centers for Disease Control and Prevention: HIV/AIDS surveillance report 5:1-19, 1993.
†Based on 816,149 cases of AIDS. Centers for Disease Control and Prevention: HIV/AIDS surveillance report 13(2):1-48, 2001.
#Based on 973,352 cases of AIDS. Centers for Disease Control and Prevention. HIV/AIDS statistics and surveillance: Basis statistics. Accessed May 2008 at: http://www.cdc.gov/hiv/topics/surveillance/basic.htm#exposure.
‡Includes hemophilia/coagulation disorder, transfusion, and risk not reported or identified.
SEXUAL CONTACT
Nationwide, unprotected sex has resulted in the greatest number of AIDS cases. The risk of exposure to HIV is present when unprotected genital or anal intercourse is performed with individuals whose HIV status is not known, be it homosexual, bisexual, or heterosexual contact. Having multiple sex partners of unknown HIV status increases this risk even further. Clearly, HIV disease is a sexually transmitted disease, as are genital herpes, gonorrhea, syphilis, nongonococcal urethritis, genital warts, and several other conditions. The presence of a sexually transmitted disease, particularly herpes, syphilis, or chancroid, increases the chance of acquiring HIV infection 100 to 200 times if one is exposed.
As of 2006, 48% of AIDS cases have involved men who have sex with men, whereas heterosexual contact has accounted for 18% of cases. The latter is an increase of 7% since 2001 (see Table 6-3).
EXPOSURE TO BLOOD
Intravenous drug abuse is a high-risk behavior when users share injection needles, allowing the transfer of blood remaining in the used needles from one person to another. Twenty-five percent of cases involve injecting drug use. Men who have sex with men who inject drugs have been associated with 7% of AIDS cases in the United States (see Table 6-3).
Injection of infected blood directly into the bloodstream is an efficient route of transmission. Percutaneous (through the skin) injuries with contaminated needles or other sharp objects and contamination of skin or mucous membranes containing small cuts or abrasions or dermatitis are variations of this “shared needles” mode of transmission.
Administration of infected blood products (e.g., to those with bleeding disorders such as hemophilia) or transfusions with infected blood have caused about 3% of the total reported cases of AIDS. In 1985, however, tests were developed that detect HIV-infected blood, and since then these modes of transmission essentially have been eliminated.
Human immunodeficiency virus has been isolated from numerous body fluids, including blood, semen, vaginal and cervical secretions, cerebrospinal fluid, synovial fluid, amniotic fluid, pericardial fluid, saliva, tears, breast milk, and urine.
Although HIV has been isolated from saliva, so far this route in casual or household contacts has not resulted in any documented cases of transmission. Transmission also was shown not to occur in a 2.5-year follow-up study of 198 health care workers, 30 of whom were bitten or scratched by an HIV-infected patient. The low risk for transmission through saliva may be attributable to the low concentration of the virus in the saliva of infected persons. A proteinaceous factor in human saliva also has been shown to interfere with the HIV infection process. Nevertheless, “saliva in dentistry” still is considered potentially infectious because of the intimate contact with the patient’s mouth during dental care and because most dental procedures result in varying degrees of bleeding into the mouth. Some natural bleeding also may occur in the mouths of dental patients who have gingivitis or other oral soft tissue lesions. Thus “saliva in dentistry” commonly contains blood.
MOTHER TO CHILD
Many infants who have HIV-positive mothers are infected before birth by passage of the virus across the placenta, at the time of birth by contact with mother’s blood during delivery, or less commonly through breast milk. Effective drug therapy during pregnancy can reduce the chances of mother-to-child transmission by close to 90%. About 0.9% of all reported AIDS cases in the United States have occurred in children younger than age 13 years (pediatric AIDS cases), and 93% of these occurred by spread from infected mothers, with the remainder involving hemophilia, transfusion, or unidentified risks (see Table 6-3).
Risk for the Dental Team
The risk of HIV disease transmission from dental patients to members of the dental team is low. Nevertheless, some small potential exists for this to occur. Through June 2003 the CDC received reports of 57 health care workers in the United States with documented, occupationally acquired HIV infections and an additional 138 with possible occupationally acquired HIV infections (Table 6-4). Since June 2001 no new documented cases and only one new case of possible occupational transmission have been reported. No documented cases of occupationally related AIDS transmission have occurred among dental personnel. However, six possible cases have been noted.
TABLE 6-4
Occupational Risk of HIV Infection for Health-Care Workers∗
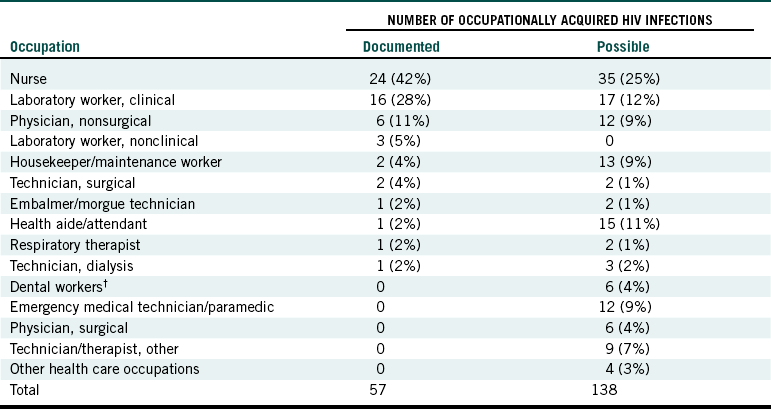
∗CDC. Surveillance of healthcare personnel with HIV/AIDS, as of December 2002. Accessed May 2008 at: http://www.cdc.gov/ncidod/dhqp/bp_hiv_hp_with.html.
†3 dentists, 1 oral surgeon, 2 dental assistants.
A “documented” case involves seroconversion (HIV-negative at the time of exposure, later becoming HIV-positive) following a percutaneous or mucocutaneous (mucous membrane and skin) occupational exposure to blood, body fluids, or tissues. A “possible” case involves persons with no determined behavioral or transfusion risks who reported past percutaneous or mucocutaneous occupational exposure to blood, other body fluids, or tissues but did not have a documented seroconversion. This means that they became HIV-positive; but, since they did not get tested at the time of exposure, it is possible that they were already positive at that time. Although no documented cases exist of occupational spread to dental workers, in six cases this may have occurred (see Table 6-4). Three of these were dentists, one was an oral surgeon, and two were dental assistants.
Of the cases shown in Table 6-4, 48 (84%) of the health care workers sustained a percutaneous (puncture/cut injury) exposure. Two had percutaneous and mucocutaneous exposures, whereas 6 had mucocutaneous exposures only. Risk of transmission increases when hollow bore needles are involved, especially if the needles are obviously soiled with blood, have been inserted into an artery or vein, or have caused a deep tissue injury. Another important factor is whether the source patient dies within 2 months of the exposure. Generally, the greatest concentration of HIV in blood (viral load) occurs soon after infection (acute retroviral syndrome) and during the AIDS stage of HIV disease.
Risk for Dental Patients
The risk for a dental patient of acquiring HIV disease in the office from a member of the dental team must be low. Although the blood-borne HBV has been spread in rare instances from dentist to patient, spread of HIV is suggested in only one instance in dentistry. Apparently, a dentist with HIV infected six of his patients being treated in his Florida dental office during the years 1987 to 1990. The investigation of this case involved a comparison of the HIV from the dentist with the viruses isolated from the infected patients, and this demonstrated significant similarity in the viruses. Unfortunately, the investigation did not discover the mode of virus spread from the dentist to the six patients, but the final conclusion by the investigators from the CDC and the Florida Department of Health suggested that direct spread from the dentist to the patients was most likely, rather than spread from contaminated instruments, equipment, or surfaces.
Until recently, this Florida dentist case was the only known instance in all of dentistry and medicine of possible spread of HIV disease from a health care worker to patients. The case still remains the only known instance in dentistry, but in February 1997 the French government reported that a woman patient contracted HIV disease from a physician in France in 1992. All of the details are not available, but evidence released so far supporting this transmission (comparing the viruses from the patient and the physician) is compelling. The available information suggests that the physician (an orthopedic surgeon) may have contracted the disease from a patient in 1983 but was not tested for HIV status until 1994. The physician performed an orthopedic procedure of some 10 hours in length on the woman patient in 1993; this is the time when the transmission is assumed to have occurred. To date, 968 of this physician’s surgery patients have been tested and only the one woman has been found to be HIV-positive. Further attempts have been made to identify and define the low risk of spread from health care workers to patients by performing HIV testing on patients who have been cared for by other HIV-positive health care workers. Of about 28,000 medical and dental patients tested so far, none has shown to have acquired HIV diseases from any of the 63 infected dentists or physicians involved. Nevertheless, maintenance of proper infection control during care for all patients is important.
Prevention
Recommendations for preventing the spread of HIV through sexual contact include abstinence or limiting sexual activities to one partner who is not infected and who does not have any other sex partners. A lesser level of protection is offered by safer sex practices such as the use of condoms to eliminate or minimize contact of each partner with body fluids that may contain HIV.
BLOOD CONTACT
Injection drug abusers must not use blood-contaminated needles. Continued screening for HIV-infectivity of blood for transfusion and of blood products began in June 1985 and must continue. All members of the dental team and other health care workers must protect themselves from exposure to blood, saliva in dentistry, and other potentially infectious body fluids. Contaminated sharps must be handled and disposed of properly. Gloves, mask, and protective eyewear and clothing must be used during the care of all patients and in other instances to prevent direct or indirect contact with body fluids. All health care workers also must prevent their blood or body fluids from coming into contact with the patients being treated, and instruments and equipment used on more than one patient must be decontaminated properly before reuse. The infection control procedures involved in these approaches to disease prevention are described in Chapter 8 and in Chapters 10 to 15.
PERINATAL
Monotherapy or combined drug treatment has been shown to reduce perinatal transmission of HIV significantly. Side effects of treatment commonly develop in the mothers. The overall safety of the combination therapy still is being investigated. The rate of congenital abnormalities appears to be similar between groups of infected women who did and did not receive drug therapy while pregnant.
Centers for Disease Control and Prevention: A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States. Accessed May 2008 at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5516a1.htm?s_cid=rr5516a1_e.
Centers for Disease Control and Prevention. National Institute for Occupational Safety and Health: Alert: preventing needlestick injuries in health care settings. Cincinnati: US Department of Health and Human Services, Public Health Services; 1999. CDC, DHHS (NIOSH) Pub No 2000-198
Centers for Disease Control and Prevention: Preventing occupational HIV transmission to health-care personnel (fact sheet). Accessed May 2008 at: http://www.cdc.gov/hiv/pubs/facts/hcwprev.htm.
Centers for Disease Control and Prevention. Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. MMWR. 1998;47(RR-19):1–38.
Centers for Disease Control and Prevention. Recommended infection control practices for dentistry, 2003. MMWR. 2003;52(RR-17):1–66.
Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in healthcare settings. MMWR. 2006;55(RR-14):1–24.
Centers for Disease Control and Prevention. Surveillance for acute viral hepatitis—United States 2006. MMWR. 2008;57(SS-2):1–28.
Centers for Disease Control and Prevention. Updated US Public Health Service guidelines for the management of occupational exposures to HBV, HCV and HIV and recommendations for postexposure prophylaxis. MMWR. 2001;50(RR-11):1–43.
Centers for Disease Control and Prevention: Viral hepatitis. Accessed May 2008 at: http://www.cdc.gov/ncidod/diseases/hepatitis.
Cottone, J.A., Puttaiah, R. Hepatitis B virus infection: current status in dentistry. Dent Clin North Am. 1996;40:293–307.
Glick, M. The role of the dentist in the era of AIDS. Dent Clin North Am. 1996;40:343–357.
Palenik CJ, Zunt SA: Managing the HIV positive patient in the dental office, Chicago, 2003, American Dental Assisting Association.
Redd, J.T., et al. Patient-to-patient transmission of hepatitis B virus associated with oral surgery. J Infect Dis. 2007;195:1311–1314.
Review Questions
______1. Which is a correct statement about hepatitis B?
a. Only about one third of those infected have recognizable symptoms.
b. Most dental assistants who have been working for more than 5 years get hepatitis B.
c. Most persons who get hepatitis B die.
d. Hepatitis b is usually spread through drinking contaminated water.
______2. How does HIV cause AIDS?
b. It destroys the body’s defenses against diseases.
______3. The vaccine for hepatitis B protects against:
______4. The risk of getting AIDS as a dental assistant is:
______5. About how many persons in the world have been infected with HIV?
______6. All of the following types of viral hepatitis are blood-borne except
______7. Occupationally, acquired hepatitis B in health care workers is most commonly contracted:
______8. The best way for one to avoid contracting a blood-borne disease in the office is:
______9. A hepatitis B carrier is:
______10. Which of the following is not a mode of spread of HIV disease?
______11. Most persons who develop HIV disease become HIV-positive within __________ after exposure.
______12. What percent of persons infected with hepatitis C virus become chronic carriers of the disease?