Glandular Tissue
1 Define and pronounce the key terms and anatomic terms in this chapter.
2 Locate and identify the glands and associated structures in the head and neck on a diagram, skull, and patient.
3 Discuss the glandular pathology associated with the head and neck.
4 Correctly complete the review questions and activities for this chapter.
5 Integrate an understanding of the head and neck glands during clinical dental practice.
(en-dah-krin) Type of gland without a duct, with the secretion being poured directly into the vascular system, which then carries the secretion to the region in which it is to be used.
(ek-sah-krin) Type of gland with an associated duct that serves as a passageway for the secretion so that it can be emptied directly into the location where the secretion is to be used.
Glandular Tissue Overview
The glandular tissue in the head and neck area includes the lacrimal, salivary, thyroid, parathyroid, and thymus glands. A gland is a structure that produces a chemical secretion necessary for normal body functioning. An exocrine gland is a gland that has a duct associated with it. A duct is a passageway that allows the secretion to be emptied directly into the location where the secretion is to be used. An endocrine gland is a ductless gland, with the secretion being poured directly into the vascular system, which then carries the secretion to the region in which it is to be used. Motor nerves associated with both types of glands help regulate the flow of the secretion, and sensory nerves are also present.
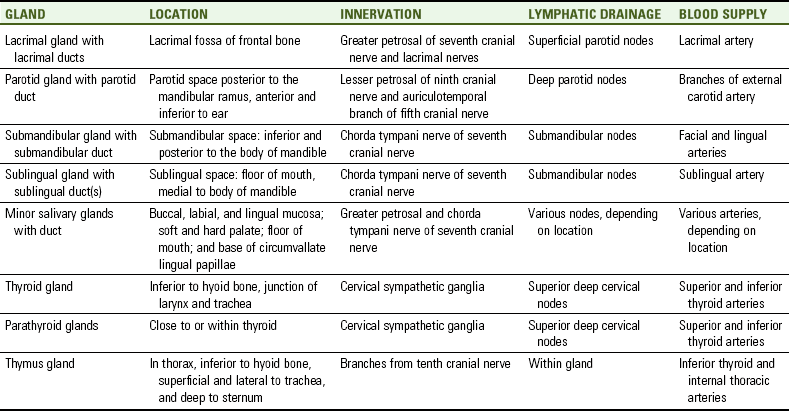
A dental professional needs to be able to locate and identify these glands and their innervation, lymphatic drainage, and vascular supply as well as examine them extraorally and possibly intraorally (Table 7-1 and see Appendix B). This information will help the dental professional determine if the glands are involved in a disease process and, if so, the extent of the involvement.
Lacrimal Glands
The lacrimal glands are paired exocrine glands that secrete lacrimal fluid or tears (see Figure 2-6). Lacrimal fluid is a watery fluid that lubricates the conjunctiva lining the inside of the eyelids and the front of the eyeball. The gland is divided into two parts: the palpebral part and the orbital part. The smaller palpebral part lies close to the eye, along the inner surface of the eyelid; if the upper eyelid is everted, the palpebral part can be seen.
The larger orbital part of the gland contains the lacrimal ducts (lak-ri-mal). At first, fine interlobular ducts unite to form three to five main excretory ducts, which then join five to seven ducts in the palpebral part before the secreted fluid may enter on the surface of the eye. Tears secreted collect in the fornix conjunctiva of the upper lid, and pass over the eye surface to the lacrimal puncta (punk-tah), small holes found at each medial canthus.
Any lacrimal fluid that passes over the eye surface ends up in the nasolacrimal sac (nay-so-lak-rim-al), a thin-walled structure behind each medial canthus. From the nasolacrimal sac, the lacrimal fluid continues into the nasolacrimal duct, ultimately draining into the inferior nasal meatus. This connection of eyes to nose explains why crying leads to a runny nose.
Location
Each gland is located in the lacrimal fossa of the frontal bone (see Figure 3-25). The lacrimal fossa is located just inside the lateral part of the supraorbital ridge inside the orbit. The nasolacrimal duct is formed at the junction of the lacrimal and maxillary bones.
Innervation
The glands are innervated by parasympathetic fibers from the greater petrosal nerve, a branch of the seventh cranial or facial nerve. These preganglionic fibers synapse at the pterygopalatine ganglion, and postganglionic fibers reach the gland through branches of the trigeminal nerve. The lacrimal nerve serves as an afferent nerve for it.
Salivary Glands
The salivary glands (sal-i-ver-ee) produce saliva (sah-li-vah), which is part of the immune system as well as the digestive system. Saliva lubricates and cleanses the oral cavity and helps in digestion. These glands are controlled by the autonomic nervous system (see Chapter 8). The glands are divided by size into major and minor glands. Both the major and minor salivary glands are exocrine glands and thus have ducts associated with them. These ducts help drain the saliva directly into the oral cavity, where the saliva can function. The salivary glands should be palpated during an extraoral examination (see Appendix B). Salivary biomarkers for many systemic, and even periodontal, diseases are now being effectively used.
Major Salivary Glands
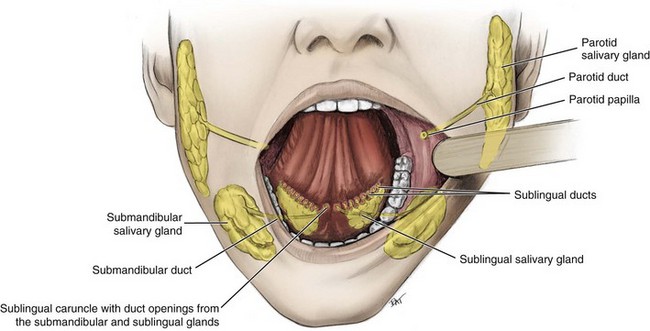
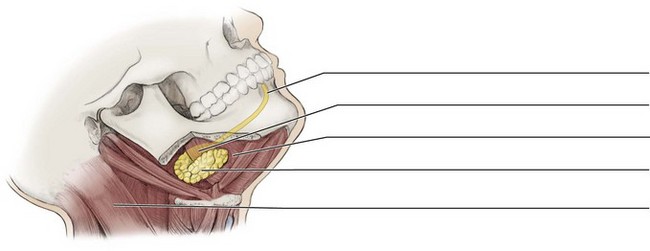
The major salivary glands are large paired glands and have named ducts associated with them. The three major salivary glands include the parotid, submandibular, and sublingual glands (Figure 7-1).
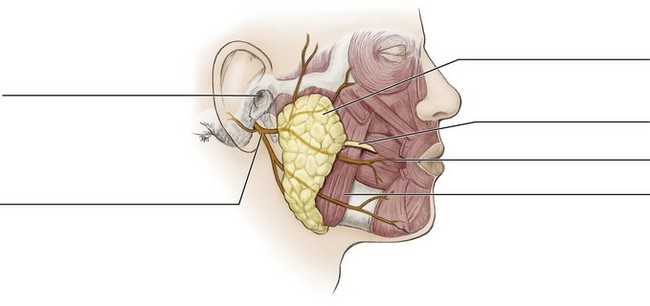
Parotid Salivary Gland
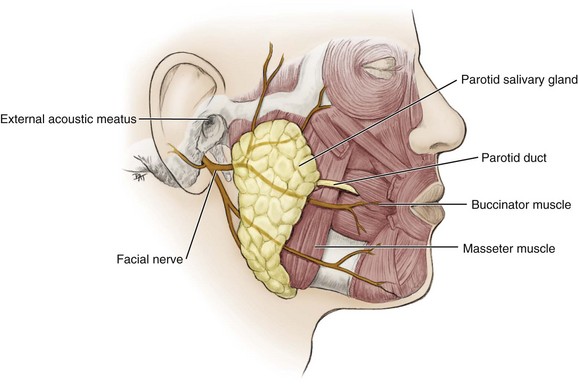
The parotid salivary gland (pah-rot-id) is the largest encapsulated major salivary gland but provides only 25% of the total salivary volume. The salivary product from the parotid is mainly a serous type of secretion. The gland is divided into two lobes: superficial and deep.
Location.: The parotid salivary gland occupies the parotid fascial space, an area posterior to the mandibular ramus, anterior and inferior to the ear (Figure 7-2, see Figures 7-1 and 11-6). It extends irregularly from the zygomatic arch to the angle of the mandible. This gland is effectively palpated bilaterally. Start anterior to each ear, move to the cheek area, and then inferior to the angle of the mandible (Figure 7-3).
Ducts.: The duct associated with the parotid salivary gland is the parotid duct or Stensen duct. This long duct emerges from the anterior border of the gland, superficial to the masseter muscle. The duct pierces the buccinator muscle, then opening up into the oral cavity on the inner surface of the cheek, usually opposite the maxillary second molar. The parotid papilla is a small elevation of tissue that marks the opening of the parotid duct on the inner surface of the cheek (see Figure 2-12).
Innervation.: The parotid salivary gland is innervated by the motor or efferent (parasympathetic) nerves of the otic ganglion of the ninth cranial or glossopharyngeal nerve, as well as by the afferent nerves from the auriculotemporal branch of the fifth cranial or trigeminal nerve. However, the seventh cranial or facial nerve and its branches travel through the gland between its superficial and deep lobes to serve as a divider but are not involved in its innervation.
Submandibular Salivary Gland
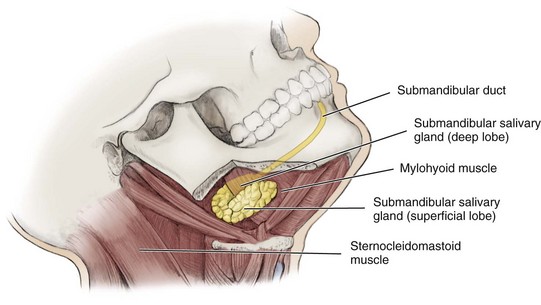
The submandibular salivary gland (sub-man-dib-you-lar) is the second largest encapsulated major salivary gland yet provides 60% to 65% of total salivary volume. The saliva from the submandibular gland is a mixed salivary product that has both serous and mucous secretions.
Location.: The submandibular salivary gland occupies the submandibular fossa in the submandibular fascial space, mainly in its posterior part (Figure 7-5, see Figures 3-54 and 11-12). Most of the gland is a larger lobe superficial to the mylohyoid muscle, but a smaller and deeper lobe wraps around the posterior border of the muscle. The submandibular gland is posterior to the sublingual gland. The gland is effectively bilaterally palpated inferior and posterior to the body of the mandible, moving inward from the inferior border of the mandible near its angle as the patient lowers the head (Figures 7-6).
Ducts.: The duct associated with this gland is the submandibular duct or Wharton duct. This long duct travels along the anterior floor of the mouth then opens into the oral cavity at the sublingual caruncle, a small papilla near the midline of the mouth floor on each side of the lingual frenum (see Figure 2-19). The duct’s tortuous travel for a considerable upward distance may be the reason the gland is the most common salivary gland to be involved in salivary stone formation as well as its mucous salivary product (see later discussion).
The submandibular duct arises from the deep lobe of the gland and remains medial to the mylohyoid muscle. The duct lies close to the large lingual nerve, a branch of the fifth cranial or trigeminal nerve, which can be injured in surgery performed to remove salivary stones from the duct.
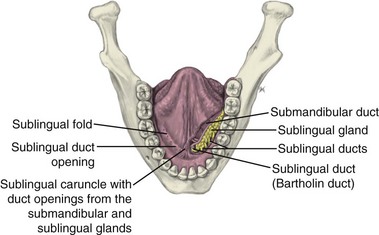
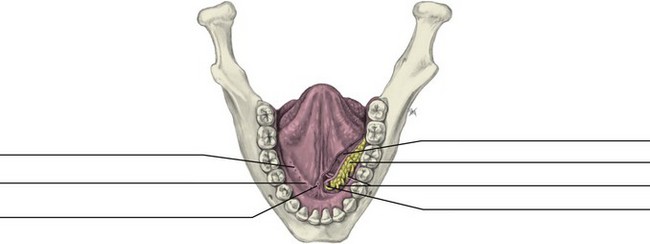
Sublingual Salivary Gland
The sublingual salivary gland (sub-ling-gwal) is the smallest, most diffuse, and only unencapsulated major salivary gland, providing only 10% of the total salivary volume. The saliva from the sublingual gland is a mixed salivary product, but with the mucous secretion predominating.
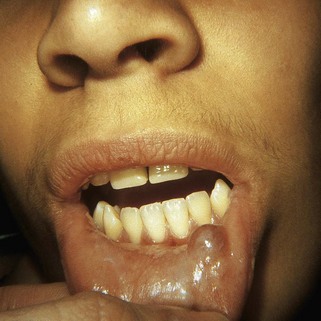
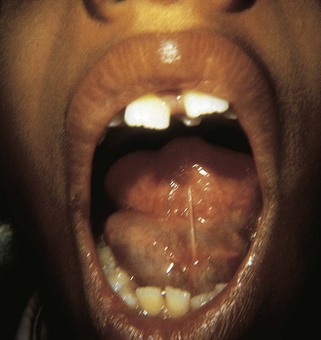
Location.: This gland occupies the sublingual fossa in the sublingual fascial space at the floor of the mouth (Figure 7-7, see Figures 3-54 and 11-12). This gland is superior to the mylohyoid muscle and medial to the body of the mandible. The sublingual gland is also located anterior to the submandibular gland. The gland is effectively palpated on the floor of the mouth posterior to each mandibular canine. Placing one index finger intraorally and the fingertips of the opposite hand extraorally, the compressed gland is manually palpated between the inner and outer fingers (Figure 7-8).
Ducts.: The short ducts associated with the gland in some cases combine to form the sublingual duct or Bartholin duct. The sublingual duct then opens directly into the oral cavity through the same opening as the submandibular duct, the sublingual caruncle. The sublingual caruncle is a small papilla near the midline of the floor of the mouth on each side of the lingual frenum. Other small ducts of the gland open along the sublingual fold, a fold of tissue on each side of the floor of the mouth (see Figure 2-19).
Minor Salivary Glands
The minor salivary glands are smaller than the larger major salivary glands but are more numerous.
Location
The minor salivary glands are scattered in the tissue of the buccal, labial, and lingual mucosa, the soft palate, the lateral parts of the hard palate, and the floor of the mouth. In addition, minor salivary glands, von Ebner glands (eeb-ners), are associated with the base of the large circumvallate lingual papillae on the posterior part of the tongue’s dorsal surface (see Figure 2-17). Most minor salivary glands secrete a mainly mucous type of salivary product, with some serous secretion. The exception is von Ebner glands, which secrete only a serous type of salivary product.
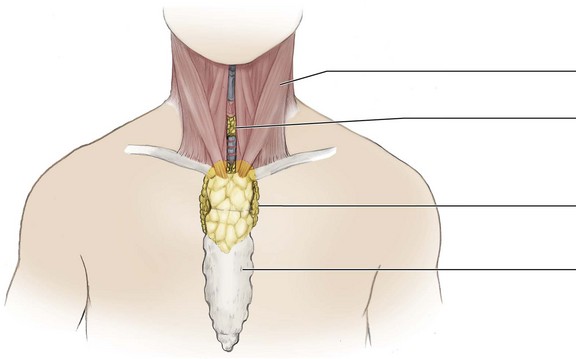
Thyroid Gland
The thyroid gland (thy-roid) is the largest endocrine gland. Because it is ductless, the gland produces and secretes thyroxine (thy-rok-sin) directly into the vascular system. Thyroxine is a hormone that stimulates the metabolic rate. The gland consists of two lateral lobes, right and left, connected anteriorly by an isthmus.
Location
The thyroid gland is located in the anterior and lateral regions of the neck. It is inferior to the thyroid cartilage, at the junction between the larynx and trachea (Figure 7-11 and see Figure 2-24). The gland is encased in previsceral fascia, which is firmly adherent to the upper part of the trachea (see Figure 11-14).
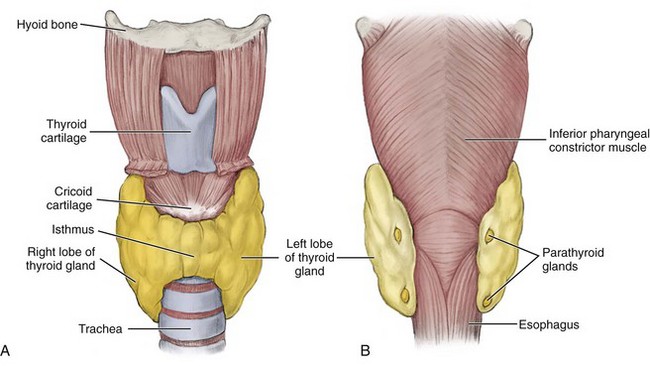
FIGURE 7-11 Thyroid gland and associated structures. A, Anterior view. B, Posterior view with parathyroid glands noted.
In a healthy patient the gland is not visible yet can be palpated as a soft mass. Examination of the thyroid gland is carried out by locating the thyroid cartilage and passing the fingers up and down, examining for abnormal masses and overall thyroid size. Then, place one hand on each of the trachea and gently displace the thyroid tissue to the contralateral side of the neck for both sides while the other hand manually palpates the displaced gland tissue; having the patient flex the neck slightly to the side when being palpated may help in this examination (Figure 7-12).

FIGURE 7-12 Palpating thyroid gland during extraoral examination by placing one hand on one side of trachea and gently displacing thyroid tissue to the contralateral side of the neck, while the other hand palpates displaced gland tissue.
Next, the two lobes of the gland should be compared for size and texture using visual inspection, as well as manual or bimanual palpation. Finally, ask the patient to swallow to check for mobility of the gland; many clinicians find that having the patient swallow water helps this part of the examination. In a healthy state, the gland is mobile when swallowing occurs due its fascial encasement. Thus when the patient swallows, the gland moves superiorly, as does the whole larynx. With pathology, the thyroid gland can lose this mobility and become fixated (see discussion next).
Parathyroid Glands
The parathyroid glands (par-ah-thy-roid) usually consist of four small endocrine glands, two on each side. Because the glands are ductless, they produce and secrete parathyroid hormone directly into the vascular system to regulate calcium and phosphorus levels. In addition, the parathyroid glands may alter the function of the thyroid gland if they are involved in a disease process.
Location
The parathyroid glands are usually adjacent to or within the thyroid gland on its posterior surface (see Figure 7-11, B). Thus the parathyroid glands are not visible or palpable during extraoral examination of a patient.
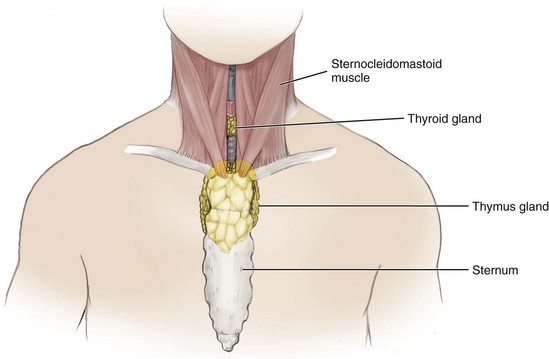
Thymus Gland
The thymus gland (thy-mus) is an endocrine gland and therefore ductless. It is part of the immune system that fights disease processes; the T-cell lymphocytes, white blood cells of the immune system, mature in the gland in response to stimulation by thymus hormones. The gland grows from birth to puberty while performing this task. After puberty, the gland stops growing and starts to shrink, undergoing involution. Thus by adulthood, the gland has almost disappeared and returned to its low birth weight, making it mainly a temporary structure. The adult gland consists of two lateral lobes, right and left, connected by an isthmus at the midline.
Location
The thymus gland is located in the thorax and the anterior region of the base of the neck, inferior to the thyroid gland (Figure 7-14). The gland is superficial and lateral to the trachea and deep to the sternum and the sternohyoid and sternothyroid muscles. The gland is not easily palpated.
Innervation
This gland is innervated by branches of the tenth cranial or vagus nerve and cervical nerves.
Lymphatic Drainage
Its lymphatic system arises within the substance of the gland and terminates in the internal jugular vein.
1. The sublingual salivary gland is located
A anterior to the submandibular gland.
B inferior to the mylohyoid muscle.
2. Which of the following glands has BOTH a superficial and deep lobe?
3. Which of the following nerves innervates BOTH the submandibular and sublingual salivary glands?
4. Which of the following nerves travels through the parotid salivary gland but is NOT involved in its innervation?
5. Which of the following glands shrinks in size as a person matures?
6. Which of the following glands has a duct that usually opens on the inner surface of the cheek, opposite the maxillary second molar?
7. Which oral landmark marks the opening of the submandibular duct?
8. The thyroid gland as part of the endocrine system is located
9. Which of the following blood vessels supplies the parotid salivary gland?
10. As endocrine glands, the parathyroid glands are known to
11. The lacrimal gland ultimately drains into the
12. Which of the following can block the drainage of saliva from the duct?
13. Which of the following statements concerning minor salivary glands is CORRECT?
A Minor glands are smaller and less numerous than the major glands
B Minor glands secrete only mucous saliva
C Minor glands have longer ducts than major glands
D Minor glands are located in the buccal, labial, and lingual mucosa
14. In a healthy patient, the thyroid gland is known to
A consist of two lobes that are connected by an isthmus.
B not move with the thyroid cartilage when swallowing.
15. When examining the thyroid gland on a patient, it is important to
16. Into which structure does the lacrimal fluid initially drain into after passing over the eyelid?
17. Which of the following is a significant feature noted with the thymus gland?
A Maturation of immune system T-cells
B Regulation of calcium and phosphorus levels
18. Which of the following oral tissue contain minor salivary glands?
19. Which of the following lesions is due to an enlarged thyroid gland?
20. The primary lymphatic drainage of the sublingual salivary gland is by the