Nervous System
1 Define and pronounce the key terms and anatomic terms in this chapter.
2 Describe the components of the nervous system and outline the actions of nerves.
3 Discuss the divisions of the central and peripheral nervous systems.
4 Identify and trace the routes of the cranial nerves on a diagram and skull.
5 Discuss the innervation of each of the cranial nerves.
6 Identify and trace the routes of the nerves to the oral cavity and associated structures of the head and neck on a diagram, skull, and patient.
7 Describe the tissue innervated by each of the nerves of the head and neck.
8 Discuss the nervous system pathology associated with the head and neck region.
9 Correctly complete the review questions and activities for this chapter.
10 Integrate an understanding of head and neck nerves into clinical dental practice.
Rapid depolarization of the cell membrane that results in propagation of the nerve impulse along the membrane.
(af-er-ent) Sensory nerve that carries information from the periphery of the body to the brain or spinal cord.
(ann-es-thee-zee-ah) Loss of feeling or sensation resulting from the use of certain drugs or gases that serve as inhibitory neurotransmitters.
(ef-er-ent) Motor nerve that carries information away from the brain or spinal cord to the periphery of the body.
(noor-on) Cellular component of the nervous system that is individually composed of a cell body and neural processes.
(nu-ro-tranz-mitt-er) Chemical agent from the neuron that is discharged with the arrival of the action potential, diffuses across the synapse, and binds to receptors on another cell’s membrane.
Bundle of neural processes outside the central nervous system; a part of the peripheral nervous system.
Extensive, intricate network of structures that activates, coordinates, and controls all functions of the body.
Charge difference between the fluid outside and inside a cell that results in differences in the distribution of ions.
Nervous System Overview
The nervous system is an extensive, intricate network of neural structures that activates, coordinates, and controls all functions of the body. The nervous system causes muscles to contract resulting in facial expressions and even joint movements, such as those involved in mastication and speech. The system stimulates glands to secrete and regulates many other systems of the body such as the vascular system and digestive system. The nervous system also allows sensation to be perceived, such as pain and touch during dental treatment.
Understanding the nervous system and its components is important to the dental professional as this system allows for the function of the muscles, the temporomandibular joint, and the glands of the head and neck (see Chapters 4, 5, 7). A thorough understanding of certain nerves is important in pain management that involves administering local anesthesia during dental treatment (see Chapter 9). Finally, nervous system pathology associated with the head and neck must be understood by the dental professional (discussed later).
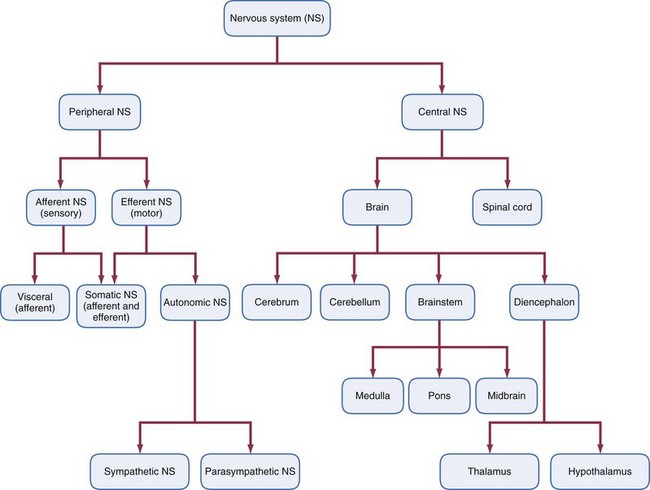
The nervous system has two main divisions: central and peripheral (Figures 8-1 and 8-2). These two divisions of the nervous system are constantly interacting. The neuron is the cellular component of the nervous system and is composed of a cell body and neural processes. A nerve is a bundle of neural processes outside the central nervous system and in the peripheral nervous system. A synapse is the junction between two neurons or between a neuron and an effector organ, where neural impulses are transmitted.
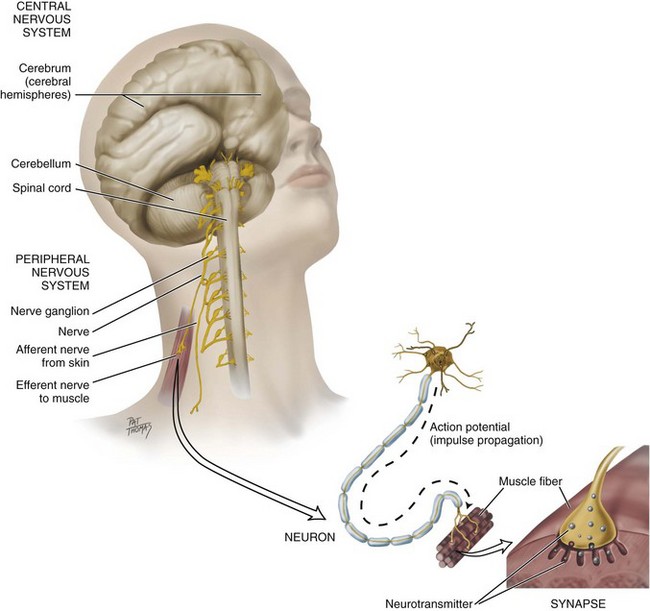
FIGURE 8-1 Nervous system with its two main divisions: central nervous and peripheral nervous systems.
In order to function, most tissue, structures, and organs have innervation, a supply of nerves to the body part. A nerve allows information to be carried to and from the brain, which is the central information center. An accumulation of neuron cell bodies outside the central nervous system is a ganglion (plural, ganglia).
Nerves are of two types: afferent and efferent (see Figure 8-1). An afferent nerve or sensory nerve carries information from the periphery of the body to the brain (or spinal cord). Thus an afferent nerve carries sensory information such as taste, pain, and proprioception to the brain. Proprioception is information concerning the movement and position of the body. This information is sent to the brain to be analyzed, acted on, associated with other information, and stored as memory.
An efferent nerve or motor nerve carries information away from the brain (or spinal cord) to the periphery of the body. Thus an efferent nerve carries information to the muscles in order to activate them, often in response to information received by way of the afferent nerves. One motor neuron with its branching process may control hundreds of muscle fibers.
The plasma membrane of a neuron, like all other cells, has an unequal distribution of ions and electric charges between the two sides of the membrane. The fluid outside of the membrane has a positive charge; the fluid inside has a negative charge. This charge difference is a resting potential and is measured in millivolts. Resting potential results in part from differences in the distribution of positively charged ions (sodium and potassium) and negatively charged ions in the cytoplasm and extracellular fluid. Sodium ions are more heavily concentrated outside the membrane, while potassium ions are more heavily concentrated inside the membrane. This imbalance is maintained by the active transport of ions against their concentration gradients by the sodium-potassium pump.
The rapid depolarization of the cell membrane results in an action potential, which then causes propagation of the nerve impulse along the membrane (see Figure 8-1). An action potential is a temporary reversal of the electric potential along the membrane for a brief period (less than a millisecond). Sodium gates suddenly open in the membrane to allow sodium ions to pour in, bringing their positive charge. At the height of the membrane potential reversal, sodium gates close and potassium channels open to allow potassium ions to pass to the outside of the membrane, reestablishing the resting potential. The changed ionic distributions must be reset by the continuously running sodium-potassium pump.
The action potential begins at one spot on the membrane but spreads to adjacent areas of the membrane, propagating the impulse along the length of the cell membrane. After passage of the action potential, there is a brief period—the refractory period—during which the membrane cannot be stimulated. This prevents the impulse from being transmitted backward along the membrane. By means of the action potential, nerve impulses travel the length of the neuron.
To have the impulse cross the synapse to another cell requires the actions of chemical agents or neurotransmitters from the neuron, which are discharged with the arrival of the action potential. Released neurotransmitters diffuse across the synapse and bind to receptors on the membrane of the other cell. Neurotransmitters cause ion channels to open or close in the second cell, prompting changes in the excitability of that cell’s membrane. Excitatory neurotransmitters such as acetylcholine and norepinephrine (in most organs) make it more likely that an action potential will be triggered in the second cell. Inhibitory neurotransmitters such as dopamine and serotonin make an action potential in the second cell less likely. Neurotransmitters are either destroyed by specific enzymes, diffuse away, or are reabsorbed by the neuron.
Neurotransmitters tend to be small molecules; some are even hormones. Some neurologic diseases (e.g., Parkinson disease, Huntington chorea, Alzheimer disease) are associated with imbalances of neurotransmitters. Some symptoms of Parkinson disease (e.g., rigidity) are due to a dopamine deficiency. Some symptoms of Huntington chorea may be caused by loss of a different inhibitory neurotransmitter. Alzheimer disease is accompanied by a loss of acetylcholine-producing neurons, which may explain the memory problems that result. In addition, depression can in some cases be linked to low levels of excitatory neurotransmitters in Alzheimer disease, with drug therapy for depression altering those levels. Among the drugs that affect neurotransmitter function is cocaine, which blocks the uptake of norepinephrine while stimulating the uptake of dopamine.
Special neurotransmitters involved with the sensation of pain in the central nervous system are endorphins, natural opioids that produce elation and reduction of pain, as do synthetic neurotransmitting chemicals such as opium and heroin. Many local anesthetic agents such as lidocaine, as used in dentistry, mimic inhibitory neurotransmitters by decreasing sensory neurons’ ability to generate an action potential, thus producing localized anesthesia. Anesthesia is the loss of feeling or sensation resulting from the use of certain drugs or gases that serve as inhibitory neurotransmitters. With damage to the nerves, there can be abnormal sensation or paresthesia to an area such as infection (see Chapter 12) or other trauma or agent toxicity (see Chapter 9).
Central Nervous System
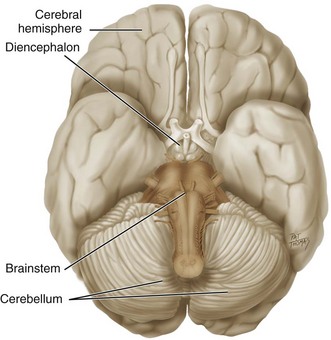
One of the major divisions of the nervous system, the central nervous system (CNS) includes both the brain and spinal cord (see Figures 8-2 and 8-4). The CNS is surrounded by bone, either the skull or vertebrae, and a system of membranes containing cerebrospinal fluid; both the bone and membranes serve to protect it. The system of membranes is the meninges (meh-nin-jez), which has three layers: dura mater, arachnoid mater, and pia mater. The dura mater also surrounds and supports the large venous channels (dural sinuses) carrying blood from the brain toward the heart (see Figure 6-12).
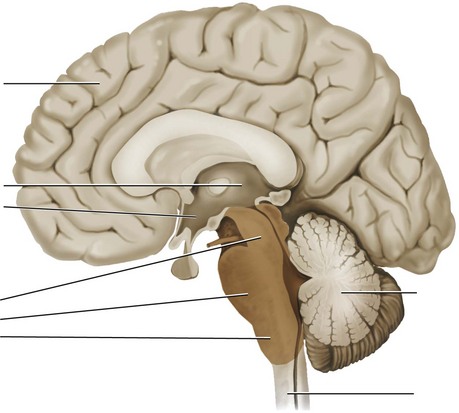
The major divisions of the brain include: the cerebrum, the cerebellum, the brainstem, and the diencephalon (Figure 8-3). The cerebrum (ser-e-brum) is the largest division of the brain and consists of two cerebral hemispheres. The cerebrum coordinates sensory data and motor functions and governs many aspects of intelligence and reasoning, learning, and memory. The cerebellum (ser-e-bel-um) is the second largest division of the brain, after the cerebrum. It functions to produce muscle coordination and maintains normal muscle tone and posture, as well as coordinating balance.
The brainstem has a number of divisions including the medulla, pons, and midbrain (Figure 8-4). The medulla (me-dul-ah) is closest to the spinal cord and is involved with the regulation of heartbeat, breathing, vasoconstriction (blood pressure), and reflex centers for vomiting, coughing, sneezing, swallowing, and hiccupping. The cell bodies of the motor neurons for the tongue are located in the medulla. The pons (ponz) connects the medulla with the cerebellum and with higher brain centers. Cell bodies for cranial nerves V and VII are found in the pons. The midbrain includes relay stations for hearing, vision, and motor pathways.
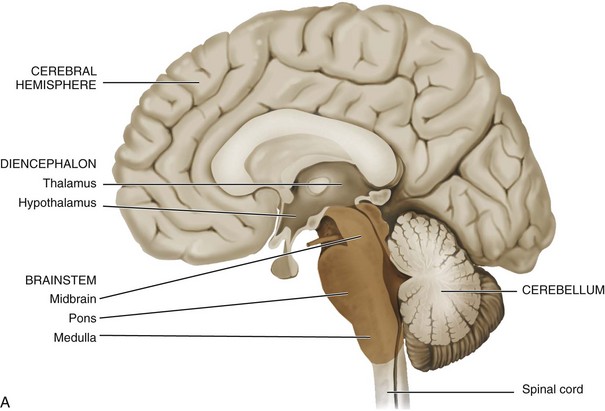
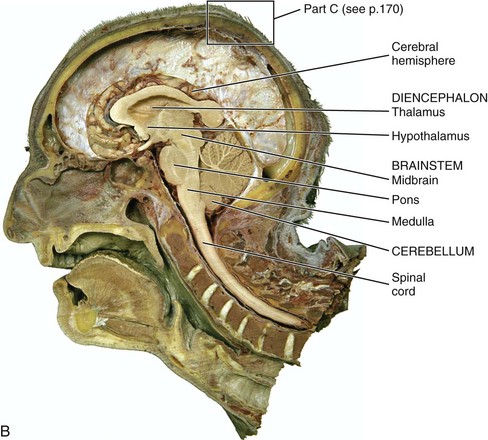
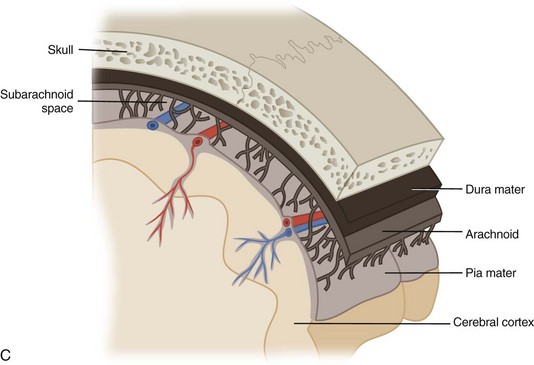
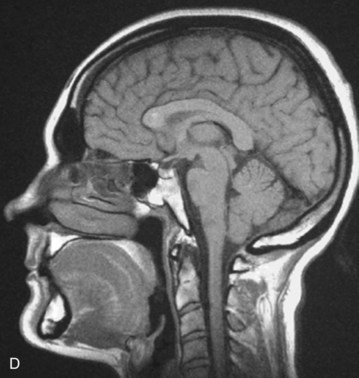
FIGURE 8-4 Sagittal sections of the brain. A, Brainstem highlighted. B, Dissection. C, Layers of meninges. D, MRI. (B and D, From Reynolds PA, Abrahams PH: McMinn’s interactive clinical anatomy: head and neck, ed 2, London, 2001, Mosby Ltd.)
Superior to the brainstem, the diencephalon (di-en-sef-a-lon) primarily includes the thalamus and hypothalamus (see Figure 8-4). The thalamus (thal-a-mus) serves as a central relay point for incoming nerve impulses. The hypothalamus (hi-po-thal-a-mus) regulates homeostasis; it has regulatory areas for thirst, hunger, body temperature, water balance, and blood pressure, linking the nervous system to the endocrine system.
The other component of the CNS, the spinal cord, runs along the dorsal side of the body and links the brain to the rest of the body (see Figure 8-4). The spinal cord in adults is encased in a series of bony vertebrae that make up the vertebral column and is made up of two types of brain substance: gray and white. The gray matter of the spinal cord consists mostly of unmyelinized cell bodies and dendrites. The surrounding white matter is made up of tracts of axons, insulated in sheaths of myelin, formed from a combination of lipids and proteins. Some tracts are ascending (carrying messages to the brain), and others are descending (carrying messages from the brain). The spinal cord is also involved in reflexes that do not immediately involve the brain.
Peripheral Nervous System
The other major division of the nervous system, the peripheral nervous system (PNS), is composed of all the nerves stretching their pathways among the CNS and the receptors, muscles, and glands of the body (see Figure 8-2). The PNS is further divided into the afferent nervous system or sensory nervous system, which carries information from receptors to the brain or spinal cord, and the efferent nervous system or motor nervous system, which carries information from the brain or spinal cord to muscles or glands. A nerve cell leading from the eye to the brain and carrying visual information is a part of the afferent nervous system. A nerve cell leading from the brain to the muscles controlling the eye’s movement is a part of the efferent nervous system. The efferent division of the PNS is further subdivided into the somatic nervous system and the autonomic nervous system.
Somatic Nervous System
The somatic nervous system (SNS) (sow-mat-ik) is a subdivision of the efferent division of the peripheral nervous system and includes all nerves controlling the muscular system and external sensory receptors. The SNS involves both receptors and effectors. External sense organs (including skin) are receptors; muscle fibers and gland cells are effectors. Sensory input from the PNS is first processed by the CNS, and then responses are sent by the PNS from the CNS to the organs of the body. The motor neurons of the somatic system are distinct from those of the autonomic system. Inhibitory signals cannot be sent through the motor neurons of the somatic system.
Autonomic Nervous System
The autonomic nervous system (ANS) (awt-o-nom-ik) is the other subdivision of the efferent division of the peripheral nervous system. This system operates without any conscious control as the caretaker of the body. Autonomic fibers are efferent nerves, and they always occur in two-nerve chains: the first nerve carries autonomic fibers to a ganglion, where they terminate near the cell bodies of the second nerve. The ANS itself has two nervous system subdivisions: sympathetic and parasympathetic. Most tissue, structures, and organs of the body are supplied by both divisions of the ANS. However, the sympathetic and parasympathetic systems generally work in opposition to each other: one stimulates an organ, as the other inhibits it.
The sympathetic nervous system (sim-pah-thet-ik) is involved in “fight-or-flight responses” such as the shutdown of salivary gland secretion with certain medications. Thus such a response by the sympathetic system leads to the reduced level of saliva with hyposalivation, which can cause dry mouth (xerostomia) (see Chapter 7). Sympathetic nerves arise in the spinal cord and relay in ganglia arranged like a chain running up the neck close to the vertebral column on both sides. Therefore all the sympathetic neurons in the head have already relayed in a ganglion. Sympathetic fibers reach the cranial tissue they supply by traveling with the arteries.
The parasympathetic nervous system (pare-ah-sim-pah-thet-ik) is involved in “rest-or-digest” responses such as the stimulation of salivary gland secretions, the exact opposite of the earlier discussion of medication-induced hyposalivation. Thus such a response by the parasympathetic system leads to the natural salivary flow to aid in digestion when being stimulated by food.
Parasympathetic fibers associated with the glands of the head and neck region are carried within various cranial nerves and are briefly described here, as well as in greater detail later. Their ganglia are located in the head, and therefore parasympathetic neurons in this region may be either preganglionic neurons (before relaying in the ganglion) or postganglionic neurons (after relaying in the ganglion).
The principal parasympathetic outflow for glands in the head and neck is carried within the seventh and ninth cranial nerves. The seventh cranial or facial nerve has two branches involved in glandular secretion. The greater petrosal nerve is associated with the pterygopalatine ganglion, and the lacrimal gland is the major target organ. The chorda tympani nerve is associated with the submandibular ganglion, and the target organs are the submandibular and sublingual salivary glands. The lesser petrosal nerve, a branch of the ninth cranial or glossopharyngeal nerve, is associated with the otic ganglion, and the target organ is the parotid salivary gland.
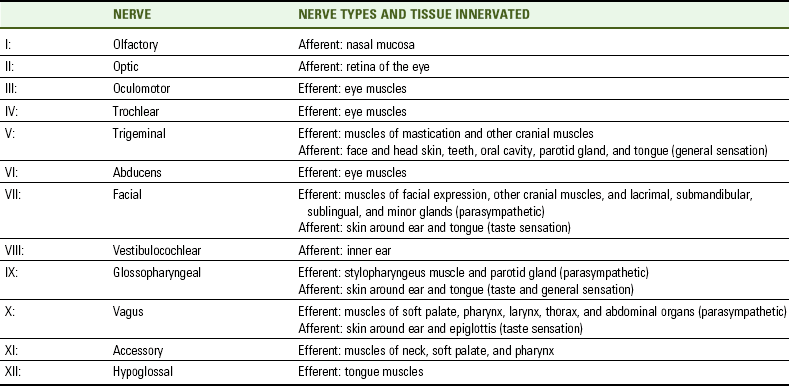
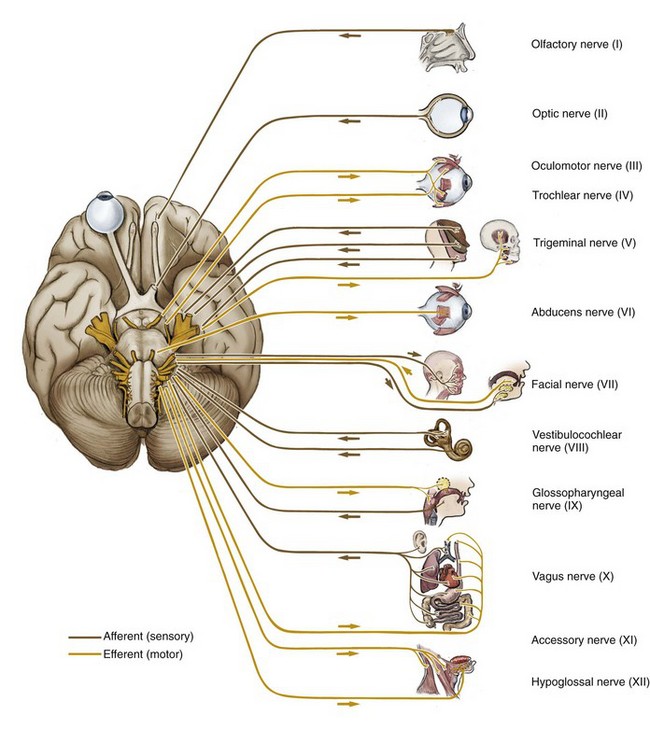
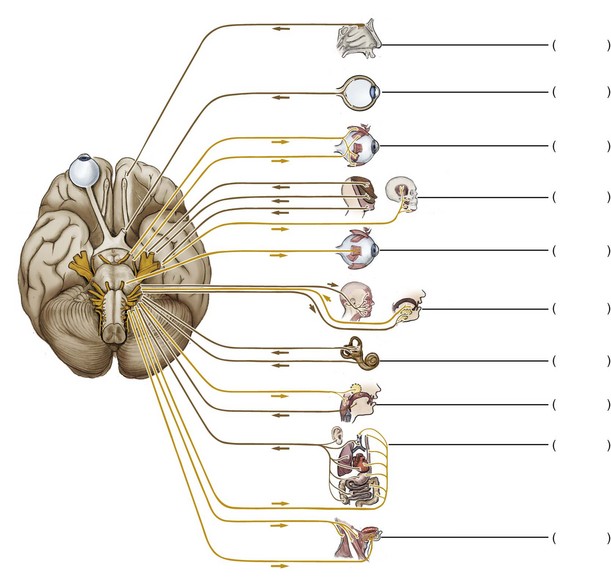
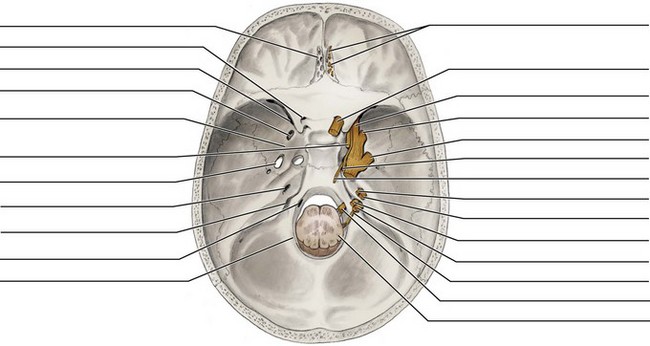
Cranial Nerves
The cranial nerves (kray-nee-al) are an important part of the PNS. All twelve paired cranial nerves are connected to the brain at its base and pass through the skull by way of fissures or foramina (Figures 8-5 and 8-6 and Table 8-1 and see Chapter 3 and Table 3-3). All the cranial nerves serve to innervate structures in the head or neck. In addition, the tenth cranial or vagus nerve descends through the neck and into the thorax and abdomen where it innervates viscera.
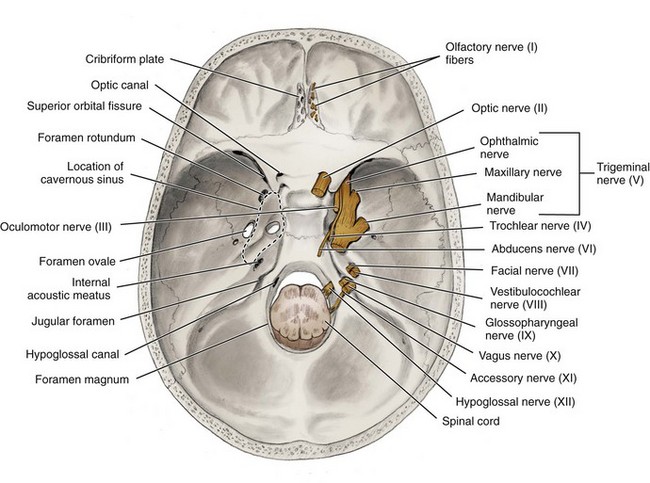
FIGURE 8-6 Superior view of the internal skull showing cranial nerves exiting or entering the skull.
Some cranial nerves are either afferent or efferent, and others have both types of neural processes. A general background of all 12 cranial nerves is discussed next. Both Roman numerals (I to XII) and anatomic terms are used to designate the cranial nerves within this chapter.
Cranial Nerve I
The first (I) cranial or olfactory nerve (ol-fak-ter-ee) transmits smell from the nasal mucosa to the brain and thus functions as an afferent nerve. The nerve enters the skull through the perforations in the cribriform plate of the ethmoid bone to join the olfactory bulb in the brain (see Figures 3-36 and 9-24 ).
Cranial Nerve II
The second (II) cranial or optic nerve (op-tik) transmits sight from the retina of the eye to the brain and thus functions as an afferent nerve. The nerve enters the skull through the optic canal of the sphenoid bone on its way from the retina (see Figure 3-19). In the skull, both the right and left optic nerves join at the optic chiasma, where many of the fibers cross to the contralateral side before continuing into the brain as the optic tracts.
Cranial Nerve III
The third (III) cranial or oculomotor nerve (ok-yule-oh-mote-er) serves as an efferent nerve to some of the eye muscles that move the eyeball. The nerve also carries preganglionic parasympathetic fibers to the ciliary ganglion near the eyeball. The postganglionic fibers innervate small muscles inside the eyeball. The nerve lies in the lateral wall of the cavernous sinus and exits the skull through the superior orbital fissure of the sphenoid bone on its way to the orbit (see Figure 3-19).
Cranial Nerve IV
The small fourth (IV) cranial or trochlear nerve (trok-lere) also serves as an efferent nerve for one eye muscle, as well as proprioception, similar to the oculomotor nerve but without any parasympathetic fibers. Similar to the oculomotor nerve, the trochlear nerve runs in the lateral wall of the cavernous sinus and exits the skull through the superior orbital fissure of the sphenoid bone on its way to the orbit (see Figure 3-19).
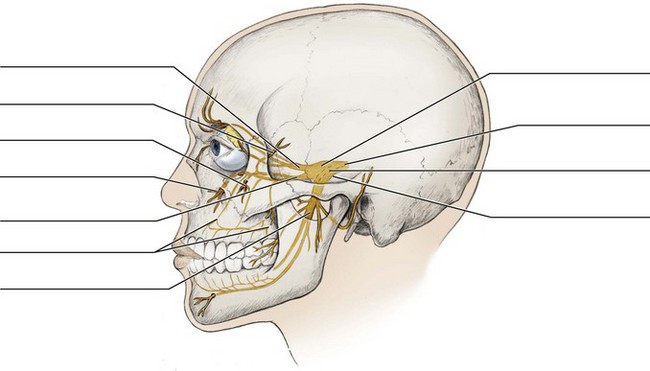
Cranial Nerve V
The fifth (V) cranial or trigeminal nerve (try-jem-i-nal) has both an efferent component for the muscles of mastication, as well as some other cranial muscles, and an afferent component for the teeth, tongue, and oral cavity, as well as most of the skin of the face and head. Although the trigeminal nerve has no preganglionic parasympathetic fibers, many postganglionic parasympathetic fibers travel along with its branches.
The trigeminal nerve is the largest cranial nerve and has two roots: sensory and motor (see Figures 8-5 and 8-6). The sensory root of the trigeminal nerve has three nerve divisions: ophthalmic, maxillary, and mandibular (Figure 8-7). The ophthalmic nerve (division) provides sensation to the upper face and scalp. The maxillary and mandibular nerves (divisions) provide sensation to the middle and lower face, respectively.
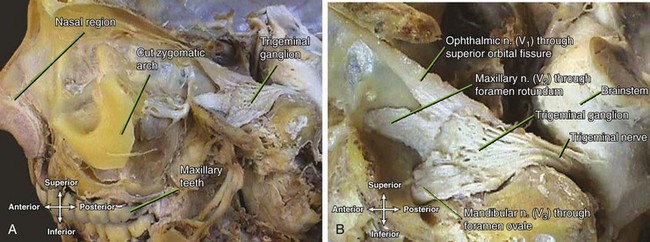
FIGURE 8-7 Dissection of the trigeminal ganglion (A) and its three nerves or divisions (B). (Reprinted with permission of Jeremy S. Melker, MD.)
Each of the three nerves or divisions of the sensory root of the trigeminal nerve enters the skull in one of three different locations in the sphenoid bone (Figure 8-7). The ophthalmic nerve or division enters through the superior orbital fissure. The maxillary nerve or division enters by way of the foramen rotundum. The mandibular nerve or division passes through the skull by way of the foramen ovale.
The motor root of the trigeminal nerve accompanies the mandibular nerve of the sensory root and also exits the skull through the foramen ovale of the sphenoid bone.
The trigeminal nerve is the most important cranial nerve to the dental professional because it innervates relevant tissue, structures, and organs of the head and neck (Table 8-2). The trigeminal nerve is discussed in greater detail later in this chapter, and local anesthesia of its nerve branches is discussed in Chapter 9.
TABLE 8-2
| HEAD AND NECK STRUCTURES | NERVES AND TYPE |
| Maxillary anterior lingual gingiva and anterior hard palate | Nasopalatine of V2: afferent |
| Maxillary posterior lingual gingiva and posterior hard palate | Greater palatine of V2: afferent |
| Soft palate and palatine tonsils | Lesser palatine of V2, glossopharyngeal (IX); afferent branches of V3, accessory (XI), and vagus (X): efferent |
| Maxillary anterior teeth, maxillary anterior facial gingiva | ASA of V2: afferent and anterior labial mucosa |
| Maxillary posterior teeth, maxillary posterior buccal gingiva, posterior labial mucosa, and maxillary sinus | MSA and PSA of V2: afferent |
| Mandibular teeth and facial gingiva of mandibular anterior teeth and premolars | IA of V3: afferent |
| Mandibular buccal gingiva and buccal mucosa | Buccal of V3: afferent |
| Mandibular labial mucosa | Mental of V3: afferent |
| Floor of mouth and mandibular lingual gingiva | Lingual of V3: afferent |
| Tongue muscles | Hypoglossal (XII): efferent |
| Tongue—general sensation | Body, lingual of V3; Base, glossopharyngeal (IX): afferent |
| Tongue—taste sensation | Body, chorda tympani of facial (VII); Base, glossopharyngeal (IX): afferent |
| Parotid salivary gland | Otic ganglion Lesser petrosal of glossopharyngeal (IX) (parasympathetic) via auriculotemporal of V3: efferent |
| Submandibular and sublingual salivary glands | Submandibular ganglion Chorda tympani of facial (VII) (parasympathetic) via lingual nerve of V3: efferent |
| Muscles of facial expression | Branches of facial (VII): efferent |
| Muscles of mastication | Medial pterygoid, deep temporal, masseteric, and lateral pterygoid of V3: efferent |
| Trapezius and sternocleidomastoid muscles | Accessory (XI): efferent |
ASA, Anterior superior alveolar; IA, inferior alveolar; MSA, middle superior alveolar; PSA, posterior superior alveolar; V2, maxillary nerve; V3, mandibular nerve.
Cranial Nerve VI
The sixth (VI) cranial or abducens nerve (ab-doo-senz) or abducent nerve serves as an efferent nerve to one of the muscles that moves the eyeball, similar to the oculomotor and trochlear nerves. Similar to both of those cranial nerves, the nerve exits the skull through the superior orbital fissure of the sphenoid bone on its way to the orbit (see Figure 3-19).
However, the nerve has a somewhat different intracranial course. Rather than lying in the wall of the cavernous sinus, the nerve runs through the sinus, close to the internal carotid artery, and is often the first nerve affected by infection of the sinus (see Chapter 12).
Cranial Nerve VII
The seventh (VII) cranial or facial nerve carries both efferent and afferent components. The nerve carries an efferent component for the muscles of facial expression and for the preganglionic parasympathetic innervation of the lacrimal gland (relaying in the pterygopalatine ganglion) as well as the submandibular and sublingual salivary glands (relaying in the submandibular ganglion) (see Figures 8-5 and 8-6). The afferent component serves a tiny patch of skin behind the ear, taste sensation, and the body of the tongue.
The facial nerve leaves the cranial cavity by passing through the internal acoustic meatus, which leads to the facial canal inside the temporal bone (see Figure 3-18). Finally, the nerve exits the skull by way of the stylomastoid foramen of the temporal bone. The facial nerve is also important to dental professionals because it innervates relevant tissue of the head and neck (see Table 8-2) and it travels through the parotid salivary gland. Thus the facial nerve can also be involved in complications with the administration of local anesthesia (see Chapters 7 and 9). The facial nerve is discussed in greater detail later.
Cranial Nerve VIII
The eighth (VIII) cranial or vestibulocochlear nerve (ves-tib-you-lo-kok-lere) serves as an afferent nerve for hearing and balance. This nerve conveys signals from the inner ear to the brain. The inner ear is located within the temporal bone. The nerve enters the cranial cavity through the internal acoustic meatus of the temporal bone (see Figure 3-19).
The nerve supplies the two major parts of the inner ear: the cochlea and semicircular canals. The first part, the cochlea, serves the function of hearing and is supplied by the cochlear part of the vestibulocochlear nerve. The second part, the semicircular canals, serves the function of balance and is supplied by the vestibular part of the semicircular canals.
Cranial Nerve IX
The ninth (IX) cranial or glossopharyngeal nerve (gloss-oh-fah-rin-je-al) carries an efferent component for the pharyngeal muscle, the stylopharyngeus muscle, and the preganglionic gland parasympathetic innervation for the parotid salivary gland (relaying the otic ganglion). The nerve also carries an afferent component for the oropharynx and for taste and general sensation from the base of the tongue, and thus is the afferent limb of the gag reflex.
The nerve passes through the skull by way of the jugular foramen, between the occipital and temporal bones (see Figure 3-19). The tympanic branch, with sensory fibers for the middle ear and preganglionic parasympathetic fibers for the parotid gland, arises here and reenters the skull.
After supplying the ear, parasympathetic fibers leave the skull through the foramen ovale of the sphenoid bone as the lesser petrosal nerve (peh-troh-sil) (see Figure 3-32). These preganglionic fibers then terminate in the otic ganglion (ot-ik) (see Figure 8-20). The otic ganglion is located near the medial surface of the mandibular nerve of the trigeminal or fifth cranial nerve, just inferior to the foramen ovale. Inferior branches of the nerve supply the carotid artery, oropharynx, and base of the tongue (afferent component), as well as the stylopharyngeus muscle. The glossopharyngeal nerve is important to dental professionals because it innervates relevant tissue of the head and neck (see Table 8-2).
Cranial Nerve X
The tenth (X) cranial or vagus nerve (vay-gus) carries a large efferent component for the muscles of the soft palate, pharynx, and larynx and for parasympathetic fibers to many organs in the thorax and abdomen including the thymus gland, heart, and stomach. The nerve carries a smaller afferent component for a small amount of skin around the ear and for taste sensation for the epiglottis.
The nerve passes through the skull by way of the jugular foramen, between the occipital and temporal bones (see Figure 3-19). The vagus nerve is important to dental professionals because it innervates relevant tissue of the head and neck (see Table 8-2).
Cranial Nerve XI
The eleventh (XI) cranial or accessory nerve functions as an efferent nerve for the trapezius and sternocleidomastoid muscles as well as for muscles of the soft palate and pharynx (see Figures 4-29 and 4-30 ). This nerve is only partly a cranial nerve and consists of two roots: one from the brain and one from the spinal cord. The accessory nerve exits the skull through the jugular foramen, between the occipital and temporal bones (see Figure 3-19). The accessory nerve is important to dental professionals because it innervates relevant tissue of the head and neck (see Table 8-2).
Cranial Nerve XII
The twelfth (XII) cranial or hypoglossal nerve (hi-poh-gloss-al) functions as an efferent nerve for both the intrinsic and extrinsic muscles of the tongue (see Figure 4-28). The nerve exits the skull through the hypoglossal canal in the occipital bone (see Figure 3-19). The hypoglossal nerve is important to dental professionals because it innervates the tongue (see Table 8-2).
Nerves to Oral Cavity and Associated Structures
The dental professional must understand the basic components of the nervous system, as well as the location of the major nerve supply of the head and neck because it adds to the general background of certain pathology involving head and neck muscles (discussed later), the temporomandibular joint, and the salivary glands (see Chapters 5 and 7).
The management of dental pain using local anesthetic agents is an important tool in dentistry. The dental professional involved in the administration of local anesthesia in the oral cavity must have a sufficient understanding of the nervous system of the head and neck (see Chapter 9).
The two cranial nerves that primarily affect the head and neck structures, the trigeminal nerve and facial nerve, are discussed in greater detail in this chapter, with the stronger emphasis on the trigeminal nerve.
Trigeminal Nerve
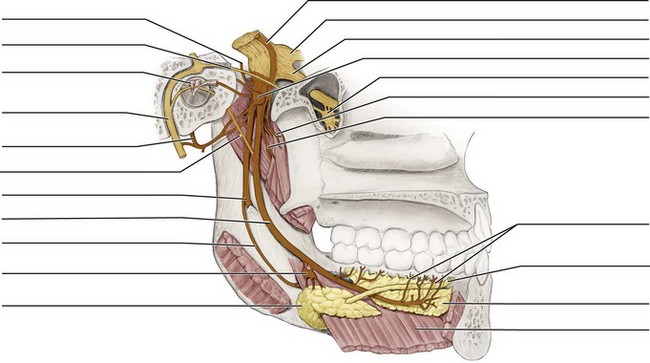
The dental professional must have a thorough understanding of the fifth (V) cranial or trigeminal nerve. Each trigeminal nerve is a short nerve trunk composed of two closely adapted roots (Figures 8-7 and 8-8). These roots of the nerve consist of a thicker sensory root and thinner motor root.
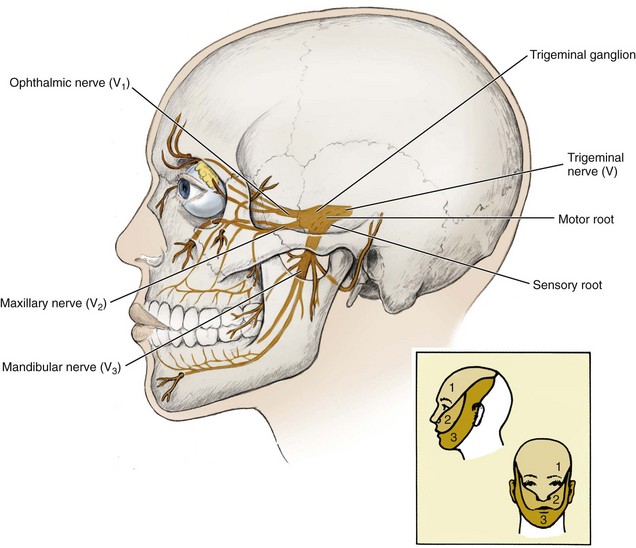
FIGURE 8-8 General pathway of the trigeminal or fifth cranial nerve and its motor and sensory roots and three nerves or divisions (inset shows innervation coverage for each nerve division).
Within the skull, a bulge can be noted in the sensory root of the trigeminal nerve. This bulge is the trigeminal ganglion (semilunar or gasserian ganglion), which is located on the anterior surface of the petrous part of the temporal bone (see Figure 3-31). Anterior to the trigeminal ganglion, the sensory root arises from three nerves or divisions that pass into the skull by way of three different fissures or foramina.
As mentioned earlier and detailed later, these three nerves or divisions of the sensory root are the ophthalmic, maxillary, and mandibular nerves. The ophthalmic nerve and maxillary nerve of the sensory root carry only afferent nerves. In contrast, the mandibular nerve of the sensory root runs together with the motor root and thus carries both afferent and efferent nerves. Important to note is that the commonly used terms “V1,” “V2,” and “V3” (pronounced “vee one,” “vee two,” and “vee three”) are simply shorthand notation for these nerves or divisions of the fifth cranial (V being the Roman numeral five) or trigeminal nerve.
The motor root of the trigeminal nerve supplies the efferent nerves for the muscles of mastication. The motor root exits the skull at the foramen ovale of the sphenoid bone and then travels with the mandibular nerve of the sensory root of the trigeminal nerve.
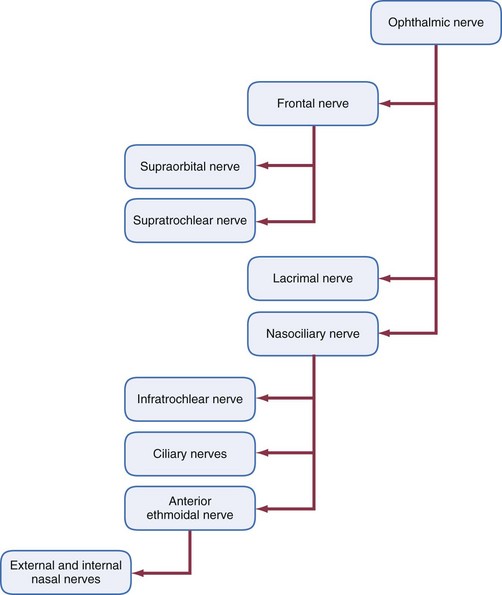
Ophthalmic Nerve
The first (V1) nerve division of the sensory root of the trigeminal nerve is the ophthalmic nerve (of-thal-mik) (Figures 8-9 and 8-10). This smallest division serves as an afferent nerve for the conjunctiva, cornea, eyeball, orbit, forehead, and ethmoidal and frontal sinuses, plus a part of the dura mater.
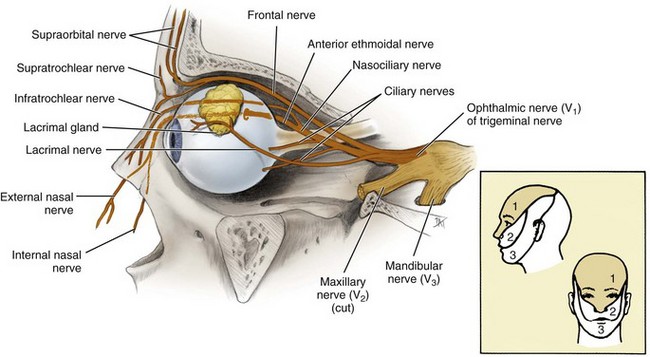
FIGURE 8-9 Lateral view of the cut-away orbit with the pathway of the ophthalmic nerve or division of the trigeminal nerve highlighted (inset shows innervation coverage).
The nerve carries this sensory information toward the brain by way of the superior orbital fissure of the sphenoid bone (see Figure 3-19). Other nerves that traverse this fissure include the third, fourth, and sixth cranial nerves. The ophthalmic nerve arises from three major nerves: the frontal, lacrimal, and nasociliary nerves.
Frontal Nerve.: The frontal nerve is an afferent nerve located in the orbit and is composed of a merger of the supraorbital nerve (soo-prah-or-bit-al) from the forehead and anterior scalp and the supratrochlear nerve (soo-prah-trok-lere) from the bridge of the nose and medial parts of the upper eyelid and forehead. The nerve courses along the roof of the orbit toward the superior orbital fissure of the sphenoid bone where it is joined by the lacrimal and nasociliary nerves to form V1 (see Figure 3-25).
Lacrimal Nerve.: The lacrimal nerve (lak-ri-mal) serves as an afferent nerve for the lateral part of the upper eyelid, conjunctiva, and lacrimal gland. The nerve also delivers the postganglionic parasympathetic nerves to the lacrimal gland. These nerves are responsible for the production of lacrimal fluid or tears. The nerve runs posteriorly along the lateral roof of the orbit and then joins the frontal and nasociliary nerves near the superior orbital fissure of the sphenoid bone to form V1 (see Figure 3-25).
Nasociliary Nerve.: Several afferent nerve branches converge to form the nasociliary nerve (nay-zo-sil-ee-a-re). These branches include the infratrochlear nerve (in-frah-trok-lere) from the skin of the medial part of the eyelids and the side of the nose, ciliary nerves (sil-ee-a-re) to and from the eyeball, and anterior ethmoidal nerve (eth-moy-dal) from the nasal cavity and paranasal sinuses (see Figures 3-8 and 3-9 ). The anterior ethmoidal nerve is formed by the external nasal nerve (nay-zil) from the skin of the ala and apex of the nose and the internal nasal nerves from the anterior part of the nasal septum and lateral wall of the nasal cavity.
The nasociliary nerve is an afferent nerve that runs within the orbit, superior to the second cranial or optic nerve, to join the frontal and lacrimal nerves near the superior orbital fissure of the sphenoid bone to form V1.
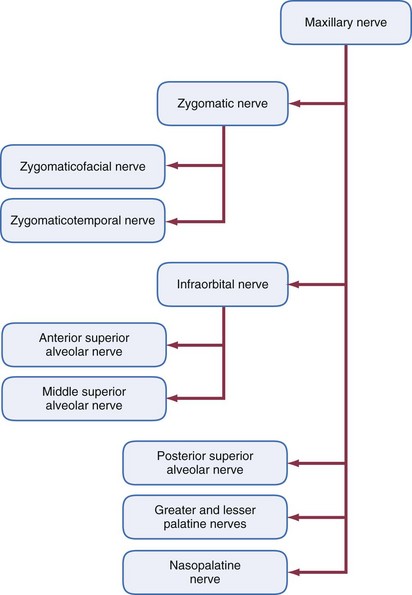
Maxillary Nerve
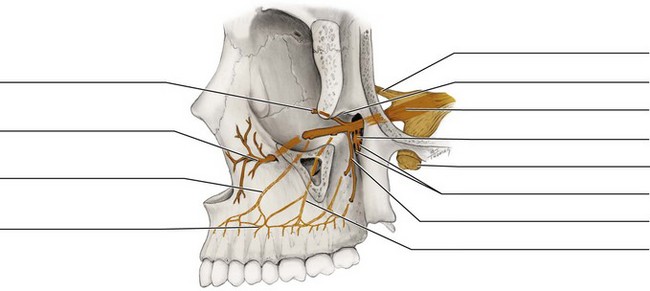
The second nerve division (V2) from the sensory root of the trigeminal nerve is the maxillary nerve (mak-sil-ar-ee) (Figures 8-11 and 8-12). The afferent nerve branches of the maxillary nerve carry sensory information for the maxillae and overlying skin, maxillary sinuses, nasal cavity, palate, nasopharynx, and part of the dura mater. The maxillary nerve is intermediate both in position and size between the ophthalmic nerve and the mandibular nerve.
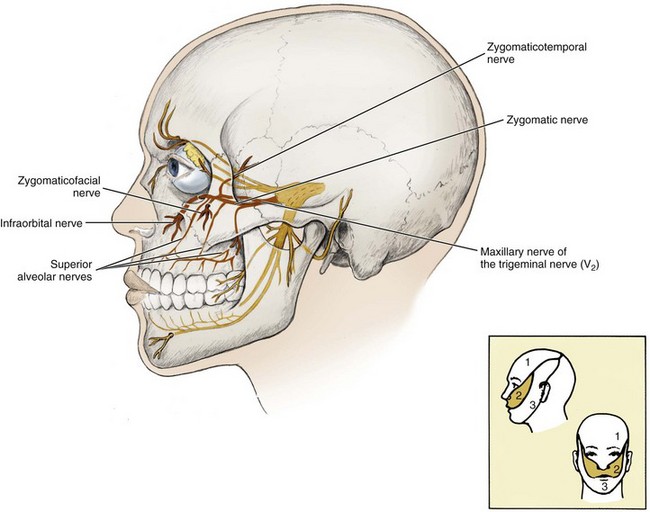
FIGURE 8-11 Pathway of the maxillary nerve or division of the trigeminal nerve is highlighted (inset shows innervation coverage).
The maxillary nerve is a nerve trunk formed in the pterygopalatine fossa by the convergence of many nerves (see Figure 3-61). The largest contributor is the infraorbital nerve. Tributaries of the infraorbital nerve or maxillary nerve trunk include: the zygomatic, the anterior, middle and posterior superior alveolar, the greater and lesser palatine, and the nasopalatine nerves.
After all these branches come together in the pterygopalatine fossa to form the maxillary nerve, the nerve enters the skull through the foramen rotundum of the sphenoid bone (see Figure 3-33). Small afferent meningeal branches from parts of the dura mater join the maxillary nerve as it enters the trigeminal ganglion.
Another ganglion, the pterygopalatine ganglion (ter-i-go-pal-ah-tine), lies just inferior to the maxillary nerve in the pterygopalatine fossa. This ganglion serves as a relay station for parasympathetic nerves that arise within the facial nerve (described later). Fibers from the ganglion (postganglionic) are then distributed to various types of tissue such as the minor salivary glands by the nerves of V2. Because the pterygopalatine ganglion lies between the maxillary nerve and its tributaries from the palate, the sensory fibers actually pass through the ganglion. However, unlike the parasympathetic fibers just discussed, the sensory fibers do not synapse within the ganglion.
Zygomatic Nerve.: The zygomatic nerve (zy-go-mat-ik) is an afferent nerve composed of the merger of the zygomaticofacial nerve and the zygomaticotemporal nerve in the orbit (see Figure 8-11). This nerve also conveys the postganglionic parasympathetic fibers for the lacrimal gland to the lacrimal nerve. The zygomatic nerve courses posteriorly along the lateral orbit floor; enters the pterygopalatine fossa through the inferior orbital fissure, between the sphenoid bone and maxilla; and finally joins V2 (see Figure 3-47).
The rather small zygomaticofacial nerve (zygo-mat-i-ko-fay-shal) serves as an afferent nerve for the skin of the cheek. This nerve pierces the frontal process of the zygomatic bone at the zygomaticofacial foramen and enters the orbit through its lateral wall (see Figure 3-42). The zygomaticofacial nerve then turns posteriorly to join with the zygomaticotemporal nerve.
The other nerve, the zygomaticotemporal nerve (zy-go-mat-i-ko-tem-poh-ral), serves as an afferent nerve for the skin of the temporal region, pierces the temporal surface of the zygomatic bone at the zygomaticotemporal foramen. The zygomaticotemporal then traverses the lateral wall of the orbit to join the zygomaticofacial nerve, forming the zygomatic nerve.
Infraorbital Nerve.: The infraorbital nerve (in-frah-or-bit-al) or IO nerve is an afferent nerve formed from the merger of cutaneous branches from the upper lip, the medial part of the cheek, the lower eyelid, and the side of the nose (Figure 8-13). The IO nerve then passes into the infraorbital foramen of the maxilla, which is a landmark for the infraorbital block, which when given, anesthetizes the IO nerve as well as both the anterior and middle superior alveolar nerves (see Figures 9-15 and 9-18 ). Then the IO nerve travels posteriorly through the infraorbital canal, along with the infraorbital blood vessels where it is joined by the anterior superior alveolar nerve (see Figures 3-45 to 3-47 ).
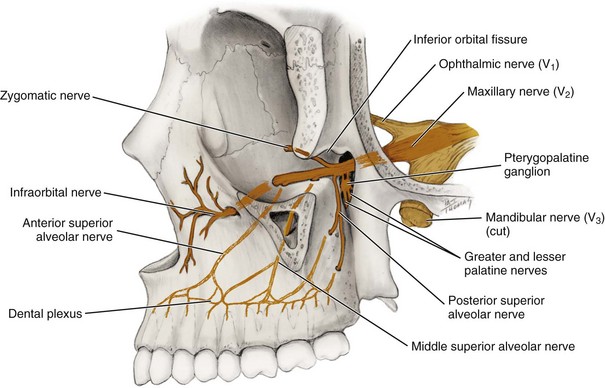
FIGURE 8-13 Lateral view of the skull (part of lateral wall of orbit has been removed) with the branches of the maxillary nerve highlighted.
From the infraorbital canal and groove, the IO nerve passes into the pterygopalatine fossa through the inferior orbital fissure. After it leaves the infraorbital groove and within the pterygopalatine fossa, the IO nerve receives the posterior superior alveolar nerve.
Anterior Superior Alveolar Nerve.: The anterior superior alveolar nerve (al-vee-o-lar) or ASA nerve serves as an afferent nerve of sensation (including pain) for the maxillary central incisors, lateral incisors, and canine, as well as their associated tissue.
The ASA nerve originates from dental branches in the pulp of these teeth that exit through the apical foramina (see Figure 8-13). The ASA nerve also receives interdental branches from the surrounding periodontium, forming a dental plexus or nerve network in the maxilla for the region, which is a landmark for the anterior superior alveolar block that anesthetizes the ASA nerve (see Figures 9-12 and 9-14 ). The ASA nerve also innervates the overlying facial gingiva.
The ASA nerve then ascends along the anterior wall of the maxillary sinus to join the IO nerve within the infraorbital canal (see Figure 3-45). Thus the ASA nerve can be anesthetized by either the anterior superior alveolar block at this site as discussed, or along with the MSA nerve, the infraorbital block (discussed earlier), as well as with the use of the anterior middle superior alveolar block along with other maxillary nerve branches using a palatal technique.
Many times the ASA nerve also provides crossover-innervation to the contralateral side in a patient. Crossover-innervation is the overlap of terminal nerve fibers from the contralateral side of the dental arch. This is important to consider when administering local anesthesia for the maxillary anterior teeth and associated tissue (see Chapter 9).
Middle Superior Alveolar Nerve.: The middle superior alveolar nerve or MSA nerve serves as an afferent nerve of sensation (including pain), usually for the maxillary premolar teeth and mesiobuccal root of the maxillary first molar and their associated periodontium and overlying buccal gingiva.
The MSA nerve originates from dental branches in the pulp that exit the teeth through the apical foramina, as well as interdental and interradicular branches from the periodontium (see Figure 8-13). The MSA nerve, like the posterior superior alveolar and ASA nerves, forms the dental plexus or nerve network in the maxilla, which is a landmark for the middle superior alveolar block which anesthetizes the MSA nerve (see Figures 9-8, 9-9, and 9-11).
The MSA nerve then ascends to join the IO nerve by running in the lateral wall of the maxillary sinus. Thus the MSA nerve can be anesthetized by either the middle superior alveolar block at this site as discussed, or along with the ASA nerve, the infraorbital block (discussed earlier), as well as with the use of the anterior middle superior alveolar block along with other maxillary nerve branches using a palatal technique.
It is important to note that the MSA nerve is not present in all patients. If this nerve is not present, the area is innervated by both the ASA and posterior superior alveolar nerves, but mainly by the ASA nerve. If the MSA nerve is present, there is communication between the MSA nerve and both the ASA and posterior superior alveolar nerves. These considerations are important when administering local anesthesia for the maxillary posterior teeth and associated tissue; the administration of both the posterior superior alveolar block as well as the middle superior alveolar block will provide complete coverage to the maxillary premolar region at the site (see Chapter 9).
Posterior Superior Alveolar Nerve.: The posterior superior alveolar nerve or PSA nerve joins the IO nerve (or maxillary nerve directly in some cases) in the pterygopalatine fossa (see Figure 8-13). The PSA nerve serves as an afferent nerve of sensation (including pain) for most parts of the maxillary molar teeth and their periodontium and buccal gingiva, as well as the maxillary sinus.
Some branches of the PSA nerve remain external to the posterior surface of the maxilla. These external branches provide afferent innervation for the buccal gingiva that overlies the maxillary molars.
Other afferent nerve branches of the PSA nerve originate from dental branches in the pulp of each of the maxillary molar teeth that exit the teeth by way of the apical foramina. These dental branches are then joined by interdental branches and interradicular branches from the periodontium, forming a dental plexus or a nerve network in the maxilla for the region.
All these internal branches of the PSA nerve exit from several posterior superior alveolar foramina on the maxillary tuberosity of the maxilla. The posterior superior alveolar arteries (from the maxillary artery) enter the maxillary tuberosity through these same foramina (see Figure 3-47). The foramina are landmarks for the posterior superior alveolar block (see Figures 9-2, 9-4, and 9-7).
Both the external and internal branches of the PSA nerve then move superiorly together along the maxillary tuberosity, which forms the posterolateral wall of the maxillary sinus, to join either the IO nerve or maxillary nerve. The PSA nerve usually provides afferent innervation for the maxillary second and third molars and the palatal and distal buccal root of the maxillary first molar, as well as the mucous membranes of the maxillary sinus.
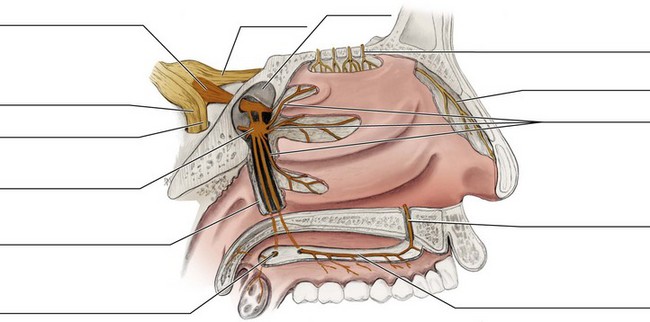
Greater and Lesser Palatine Nerves.: Both palatine nerves join with the maxillary nerve from the palate (Figure 8-14). The greater palatine nerve (pal-ah-tine) or GP nerve or anterior palatine nerve is located between the mucoperiosteum and bone of the posterior hard palate (see Figures 3-16 and 3-44 ). This nerve serves as an afferent nerve for the posterior hard palate and posterior lingual gingiva. Communication occurs with the terminal fibers of the nasopalatine nerve in the anterior hard palate, lingual to the maxillary canines.
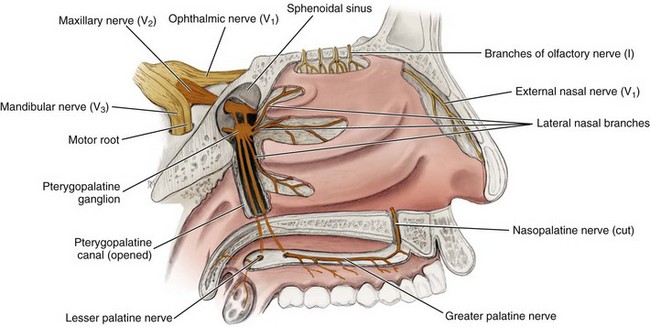
FIGURE 8-14 Medial view of the lateral nasal wall and opened pterygopalatine canal highlighting the maxillary nerve and its palatine branches. The nasal septum has been removed, thus severing the nasopalatine nerve.
Posteriorly, the GP nerve enters the greater palatine foramen in the horizontal plate of palatine bone near the maxillary second or third molar to travel within the pterygopalatine canal, along with the greater palatine blood vessels. This is a landmark for the greater palatine block (see Figures 9-19, 9-20, and 9-22).
The lesser palatine nerve or posterior palatine nerve, serves as an afferent nerve for the soft palate and palatine tonsils. The lesser palatine nerve enters the lesser palatine foramen in the palatine bone near its junction with the pterygoid process of the sphenoid bone, along with the lesser palatine blood vessels (see Figure 8-14). The lesser palatine nerve then joins the GP nerve within the pterygopalatine canal.
Both palatine nerves move superiorly through the pterygopalatine canal, toward the maxillary nerve in the pterygopalatine fossa. On the way, the palatine nerves are joined by lateral nasal branches, which are afferent nerves from the posterior nasal cavity.
Nasopalatine Nerve.: The nasopalatine nerve (nay-zo-pal-ah-tine) or NP nerve originates in the mucosa of the anterior hard palate, lingual to the maxillary anterior teeth, the maxillary central incisors (see Figure 8-14). Both the right and left NP nerves enter the incisive canal by way of the incisive foramen, deep to the incisive papilla, thus exiting the oral cavity (see Figures 2-15 and 3-48 ). This is a landmark for the nasopalatine block (see Figures 9-23 and 9-24 ).
The nerve then travels along the nasal septum. The NP nerve serves as an afferent nerve for the anterior hard palate and the lingual gingiva of the maxillary anterior teeth, as well as the nasal septal tissue. Communication also occurs with the GP nerve in the area that is located lingual to the maxillary canines.
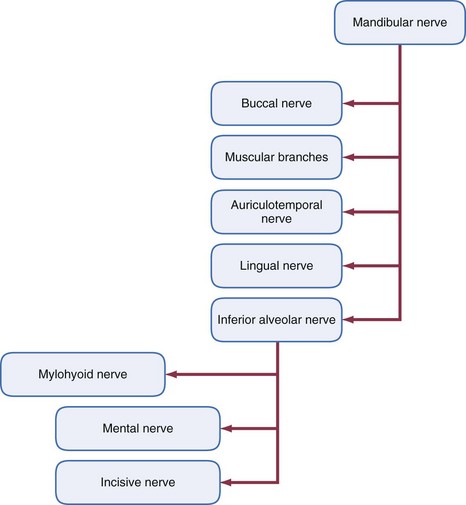
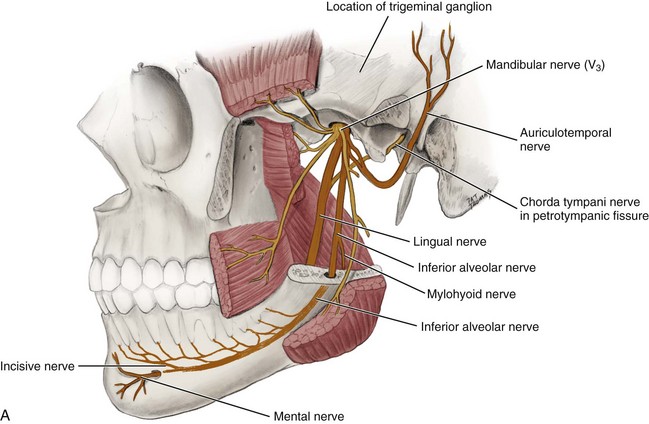
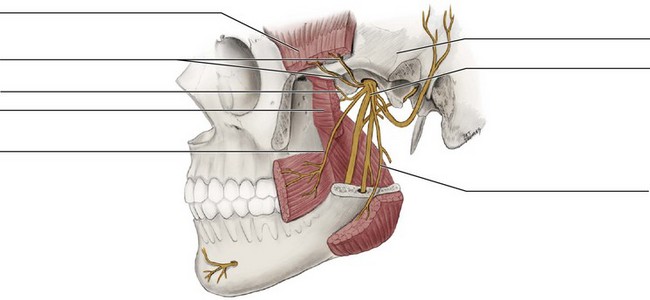
Mandibular Nerve
The third nerve division (V3) of the trigeminal nerve is the mandibular nerve (man-dib-you-lar), which is a short main trunk formed by the merger of a smaller anterior trunk and a larger posterior trunk within the infratemporal fossa deep to the base of the skull, before the nerve passes through the foramen ovale of the sphenoid bone (Figures 8-15, 8-16, and 8-17 and see Figure 3-32). The mandibular nerve then joins with the ophthalmic nerve and maxillary nerve to form the trigeminal ganglion of the trigeminal nerve. The mandibular nerve is the largest of the three nerve divisions that form the trigeminal nerve; the mandibular nerve is also a mixed nerve with both afferent and efferent nerves. Additionally, it contains the entire efferent part of the trigeminal nerve.
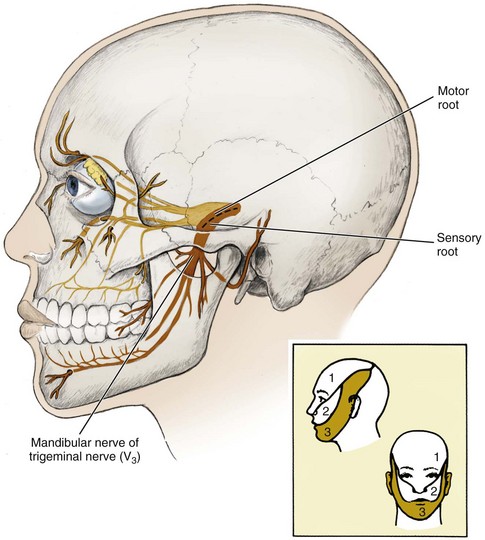
FIGURE 8-15 Pathway of the mandibular nerve or division of the trigeminal nerve is highlighted (inset shows innervation coverage).
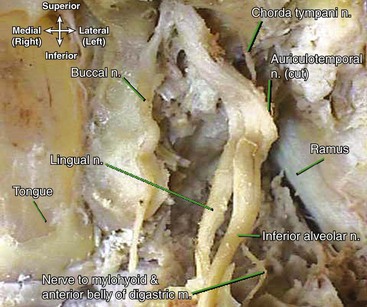
FIGURE 8-16 Dissection of the mandibular nerve of the trigeminal nerve. (Reprinted with permission of Jeremy S. Melker, MD.)
A few small branches arise from the V3 trunk before its separation into the anterior and posterior trunks (see Figure 8-20). These branches from the undivided mandibular nerve include the meningeal branches (me-nin-je-al), which are afferent nerves for parts of the dura mater. Also from the undivided mandibular nerve are muscular branches, which are efferent nerves for the medial pterygoid, tensor tympani, and tensor veli palatini muscles (see Figure 4-23).
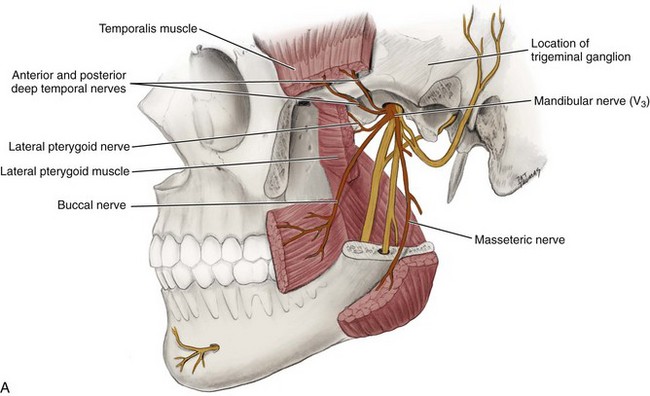
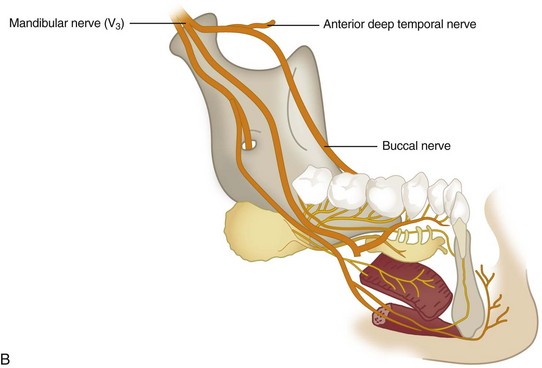
Anterior Trunk of Mandibular Nerve.: The anterior trunk, or anterior division of the mandibular nerve, is formed by the merger of the buccal nerve and additional muscular nerve branches (Figure 8-18). The anterior trunk has both afferent and efferent nerves.
Buccal Nerve.: The buccal nerve or long buccal nerve serves as an afferent nerve for the skin of the cheek, buccal mucous membranes, and buccal gingiva of the mandibular posterior teeth. The nerve is located on the surface of the buccinator muscle (see Figures 8-17 and 4-11). The buccal nerve then travels posteriorly in the cheek, deep to the masseter muscle.
At the level of the occlusal plane of the most distal molar of the mandibular arch, the nerve crosses anteriorly to the anterior border of the ramus and goes between the two heads of the lateral pterygoid muscle to join the anterior trunk of V3 (see Figure 8-18). This is a landmark for the buccal block (see Figures 9-39 and 9-41 ). This nerve must not be confused with the buccal nerve, which innervates the buccinator muscle and is an efferent nerve branch from the facial nerve.
Muscular Branches.: Several muscular branches are part of the anterior trunk of V3 (see Figures 8-17 and 8-18). They arise from the motor root of the trigeminal nerve. The deep temporal nerves (tem-poh-ral), usually two, anterior and posterior, are efferent nerves that pass between the sphenoid bone and the superior border of the lateral pterygoid muscle and turn around the infratemporal crest of the sphenoid bone to terminate in the deep surface of the temporalis muscle that they innervate (see Figure 4-22). The posterior temporal nerve may arise in common with the masseteric nerve, and the anterior temporal nerve may be associated at its origin with the buccal nerve.
The masseteric nerve (mass-et-tehr-ik) is also an efferent nerve that passes between the sphenoid bone and the superior border of the lateral pterygoid muscle. The nerve then accompanies the masseteric blood vessels through the mandibular notch to innervate the masseter muscle (see Figure 4-19). A small sensory branch also goes to the temporomandibular joint. The lateral pterygoid nerve (teh-ri-goid), after a short course, enters the deep surface of the lateral pterygoid muscle between the muscle’s two heads of origin and serves as an efferent nerve for that muscle (see Figure 4-22).
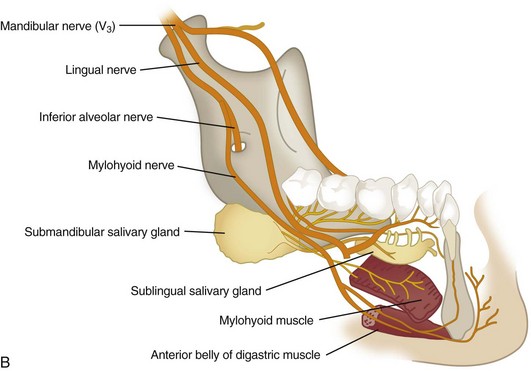
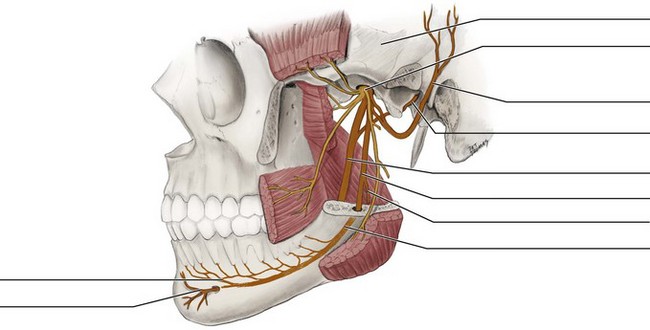
Posterior Trunk of Mandibular Nerve.: The posterior trunk, or posterior division of the mandibular nerve, is formed by the merger of the auriculotemporal, lingual, and inferior alveolar nerves (Figure 8-19). The posterior trunk has both afferent and efferent nerves.
Auriculotemporal Nerve.: The auriculotemporal nerve (aw-rik-yule-lo-tem-poh-ral) travels with the superficial temporal artery and vein and serves as an afferent nerve for the external ear and scalp (Figure 8-20; see Figure 8-19). The nerve also carries postganglionic parasympathetic nerve fibers to the parotid salivary gland. Important to note is that these parasympathetic fibers arise from the lesser petrosal branch of the glossopharyngeal or ninth cranial nerve, joining the auriculotemporal nerve only after relaying in the otic ganglion near the foramen ovale.
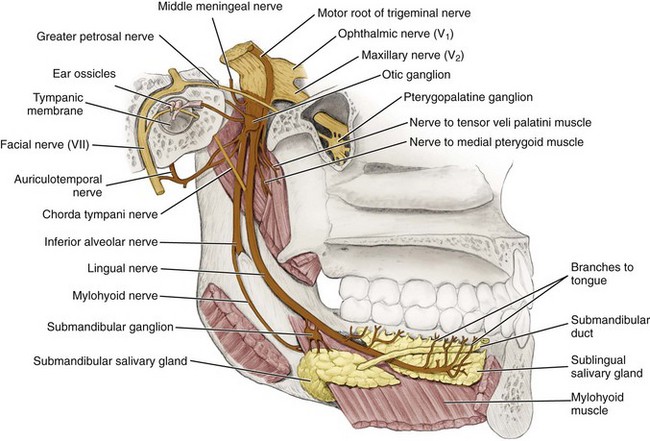
FIGURE 8-20 Medial view of the mandible with the motor and sensory branches of the mandibular nerve or division highlighted.
Communication of the auriculotemporal nerve with the facial nerve near the ear also occurs. The nerve courses deep to the lateral pterygoid muscle and neck of the mandible, then splits to encircle the middle meningeal artery, and finally joins the posterior trunk of V3. The auriculotemporal nerve is anesthetized with the Gow-Gates mandibular block and also accidentally in some cases with the inferior alveolar block due to its proximity (see Figures 9-31 and 9-47 ).
Lingual Nerve.: The lingual nerve is formed from afferent branches from the body of the tongue that travel along the lateral surface of the tongue (see Figures 8-16, 8-17, 8-19, and 8-20). The nerve then passes posteriorly, passing from the medial to the lateral side of the duct of the submandibular salivary gland by going inferior to the duct.
The lingual nerve communicates with the submandibular ganglion (sub-man-dib-you-lar) located superior to the deep lobe of the submandibular salivary gland (Figure 8-21 and see Figure 7-5). The submandibular ganglion is part of the parasympathetic system. Parasympathetic efferent innervation for the sublingual and submandibular salivary glands arises from the facial nerve (more specifically, the branch of the facial nerve, chorda tympani, which is discussed later) but travel along with the lingual nerve (see Figure 8-21).
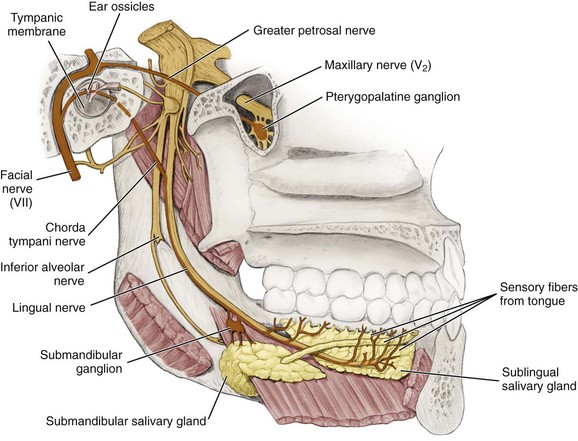
FIGURE 8-21 Pathway of the trunk of the facial nerve, greater petrosal nerve, and chorda tympani nerve highlighted (note relationship with lingual nerve).
At the base of the tongue, the lingual nerve ascends and runs between the medial pterygoid muscle and the mandible, anterior and slightly medial to the inferior alveolar nerve. Thus the lingual nerve is also anesthetized when administering an inferior alveolar block through diffusion of the local anesthetic agent (see Figures 9-31, 9-34, and 9-38).
Because the lingual nerve is only a short distance posterior to the roots of the most distal mandibular molar tooth and can be covered by only by a thin layer of oral mucosa, its location is can be visible in the oral cavity. Thus the lingual nerve can be endangered by dental procedures in this region such as the extraction of permanent mandibular third molars. In addition, the Gow-Gates mandibular block can be used to anesthetize the lingual nerve along with other branches of the mandibular nerve (see Figure 9-47).
The lingual nerve then continues to travel superiorly to join the posterior trunk of V3. Thus the lingual nerve serves as an afferent nerve for general sensation for the body of the tongue, the floor of the mouth, and the lingual gingiva of the mandibular teeth.
Inferior Alveolar Nerve.: The inferior alveolar nerve or IA nerve is an afferent nerve formed from the merger of the mental and incisive nerves (see Figures 8-17 and 8-19). The mental and incisive nerves are discussed later in this section.
After forming, the IA nerve continues to travel posteriorly through the mandibular canal, along with the inferior alveolar artery and vein (see Figures 3-52 and 3-54 ). The IA nerve is joined by dental branches such as both interdental and interradicular branches from the mandibular posterior teeth, forming a dental plexus or nerve network in the region. The IA nerve then exits the mandible through the mandibular foramen where it is joined by the mylohyoid nerve (discussed later). The mandibular foramen is an opening of the mandibular canal on the medial surface of the ramus, three fourths the distance from the coronoid notch to the posterior border of the ramus, within the pterygomandibular space (see Figure 11-8). This is a landmark for the inferior alveolar block (see Figures 9-32, and 9-34 to 9-38).
The IA nerve then travels lateral to the medial pterygoid muscle, between the sphenomandibular ligament and ramus of the mandible. This is posterior and slightly lateral to the lingual nerve. The IA nerve then joins the posterior trunk of V3 (see Figures 8-16, 8-19, and 8-20). The IA nerve carries afferent innervation for the mandibular teeth. The IA nerve along with the lingual nerve is anesthetized by the inferior alveolar block at this site (see Figure 9-30). In addition, the Gow-Gates mandibular block can be used to anesthetize the IA nerve along with other branches of the mandibular nerve (see Figure 9-47).
In some cases there are two nerves present on the unilateral side, creating bifid IA nerves. This situation can occur unilaterally or bilaterally and can be detected on a radiograph by the presence of a double mandibular canal. As discussed in Chapter 3, there can be more than one mandibular foramen, usually inferiorly placed, either unilaterally or bilaterally, along with the bifid IA nerves. These considerations must be kept in mind when administering local anesthesia for the mandibular teeth and associated tissue (see Chapter 9).
Mental Nerve.: The mental nerve (ment-il) is composed of external branches that serve as an afferent nerve for the chin, lower lip, and labial mucosa of the mandibular premolars and anterior teeth (see Figure 8-19). The mental nerve then enters the mental foramen on the lateral surface of the mandible, usually between the apices of the mandibular first and second premolars. The mental nerve is anesthetized by the mental block at this site. The incisive block can also be administered at the same site along with anesthesia of the deeper incisive nerve due to using more local anesthetic agent (see Figures 9-42, 9-43, and 9-45). In addition, either the inferior alveolar block or Gow-Gates mandibular block can be used to anesthetize the mental nerve along with other branches of the mandibular nerve from other target injection sites (see Figure 9-47).
After entering via the mental foramen and traveling a distance within the mandibular canal, the mental nerve merges with the incisive nerve to form the IA nerve within the mandibular canal and before the IA nerve exits the mandibular nerve (see Figures 3-52 and 3-54 ).
Incisive Nerve.: The incisive nerve (in-sy-ziv) is an afferent nerve composed of dental branches from the mandibular premolar and anterior teeth that originate in the pulp, exit the teeth through the apical foramina, and join with interdental branches from the surrounding periodontium, forming a dental plexus in the region (see Figure 8-19). The incisive nerve serves as an afferent nerve for the mandibular premolars and anterior teeth. The incisive nerve then merges with the mental nerve, just posterior to the mental foramen. The incisive nerve is anesthetized by the incisive local block at this site, or with the inferior alveolar block or Gow-Gates mandibular block along with other branches of the mandibular nerve (see Figures 9-43, 9-45, 9-46, and 9-47). The incisive nerve will go on next to form the IA nerve within the mandibular canal before it exits the mandibular canal (see Figures 3-52 and 3-54 ).
To complicate matters, crossover-innervation from the contralateral incisive nerve can also occur, which is an important consideration when administering local anesthesia for the mandibular premolars and anterior teeth and associated tissue (see Chapter 9).
Mylohyoid Nerve.: After the inferior alveolar nerve exits the mandibular foramen, a small branch occurs, the mylohyoid nerve (my-lo-hi-oid) (see Figures 8-16, 8-17, 8-19, 8-20 and 4-25). This nerve pierces the sphenomandibular ligament and runs inferiorly and anteriorly in the mylohyoid groove and then onto the inferior surface of the mylohyoid muscle. The mylohyoid nerve serves as an efferent nerve to the mylohyoid muscle and anterior belly of the digastric muscle (the posterior belly of the digastric muscle is innervated by a branch from the facial nerve).
The mylohyoid nerve may in some cases also serve as an afferent nerve for the mandibular first molar, which needs to be considered when the inferior alveolar block fails (see Chapter 9). If there is concern, the mylohyoid nerve can be additionally anesthetized by giving a supraperiosteal injection at the apex of the mesial root of the mandibular first molar on the medial surface of the mandible. The mylohyoid nerve is also anesthetized by the Gow-Gates mandibular block, along with other branches of the mandibular nerve (see Figure 9-47).
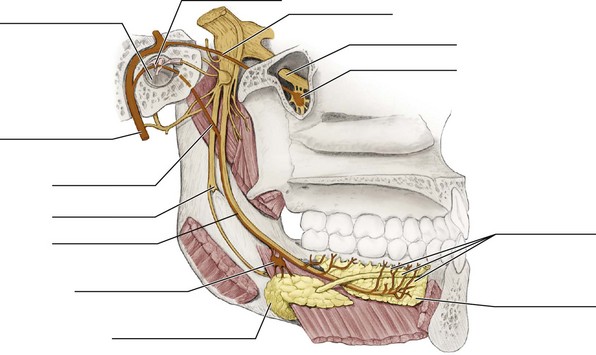
Facial Nerve
The dental professional must also have an understanding of the seventh (VII) cranial or facial nerve. It carries both efferent and afferent nerves. The facial nerve emerges from the brain and enters the internal acoustic meatus in the petrous part of the temporal bone (see Figure 3-19). Within the bone, the nerve gives off a small efferent branch to the muscle in the middle ear (stapedius) and two larger branches, the greater petrosal and chorda tympani nerves, both of which carry parasympathetic fibers (see Figure 8-21).
The main trunk of the nerve emerges from the skull through the stylomastoid foramen of the temporal bone and gives off two branches, the posterior auricular nerve and a branch to the posterior belly of the digastric and stylohyoid muscles (Figure 8-22 and see Figure 3-31, A). The facial nerve then passes into the parotid salivary gland and divides into numerous branches to supply the muscles of facial expression, but not the parotid salivary gland itself (see Figure 7-2). Avoiding anesthesia of this nerve at this location is important when administering an inferior alveolar block because it may result in transient facial paralysis if given incorrectly (discussed later, see Figure 9-37). In addition, a neoplastic growth in the parotid salivary gland may be painful due to the presence of this nerve (see Chapter 7).
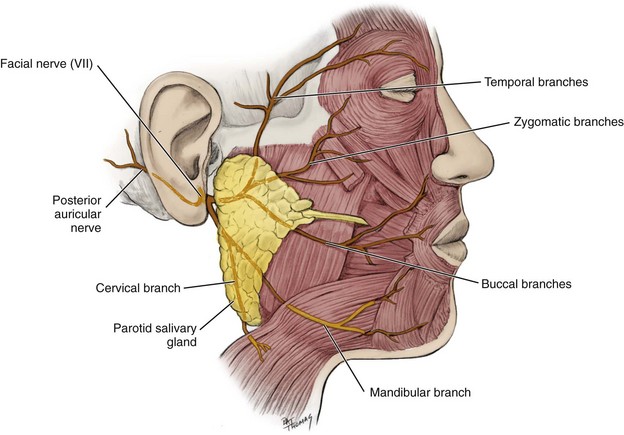
FIGURE 8-22 Pathway of the branches of the facial nerve to the muscles of facial expression highlighted.
Greater Petrosal Nerve
The greater petrosal nerve (peh-troh-sil) is a branch off the facial nerve before it exits the skull (see Figure 8-21). The greater petrosal nerve carries efferent nerve fibers; preganglionic parasympathetic fibers to the pterygopalatine ganglion in the pterygopalatine fossa (see Figure 3-61).
The postganglionic fibers arising in the pterygopalatine ganglion then join with branches of the maxillary nerve of the trigeminal nerve to be carried to the lacrimal gland (via the zygomatic and lacrimal nerves), nasal cavity, and minor salivary glands of the hard and soft palate. The greater petrosal nerve also carries afferent nerve fibers for taste sensation in the palate.
Chorda Tympani Nerve
This small branch of the facial nerve, the chorda tympani nerve (kor-dah tim-pan-ee), is a parasympathetic efferent nerve for the submandibular and sublingual salivary glands and also serves as an afferent nerve for taste sensation for the body of the tongue.
After branching off the facial nerve within the petrous part of the temporal bone, the chorda tympani nerve crosses the medial surface of the tympanic membrane (eardrum) (see Figures 8-19, 8-20, and 8-21), which thereby exits the skull by the petrotympanic fissure, located immediately posterior to the temporomandibular joint (see Figure 3-30). The chorda tympani nerve then travels with the lingual nerve along the floor of the mouth in the same nerve bundle.
In the submandibular triangle, the chorda tympani nerve, appearing as part of the lingual nerve, has communication with the submandibular ganglion. The submandibular ganglion is located superior to the deep lobe of the submandibular salivary gland, for which it supplies parasympathetic efferent innervation (see Figures 8-21 and 7-5).
Posterior Auricular, Stylohyoid, And Posterior Digastric Nerves
The posterior auricular nerve (aw-rik-you-lar), stylohyoid nerve (sty-lo-hi-oid), and posterior digastric nerve (di-gas-trik) are branches of the facial nerve after it exits the stylomastoid foramen. All are efferent nerves. The posterior auricular nerve supplies the occipital belly of the epicranial muscle (see Figure 8-22). The other two nerves supply the stylohyoid muscle and the posterior belly of the digastric muscle, respectively.
Branches To Muscles Of Facial Expression
Additional efferent nerve branches of the facial nerve originate within the parotid salivary gland and pass to the muscles they innervate (see Figures 8-22 and 4-5). These branches to the muscles of facial expression include: the temporal, zygomatic, buccal, (marginal) mandibular, and cervical branches. However, these branches are rarely seen as five independent nerves; they may vary in number and connect irregularly. However, for convenience when studying, they are described as five simple branches.
The temporal branches supply the muscles anterior to the ear, frontal belly of the epicranial muscle, superior part of the orbicularis oculi muscle, and corrugator supercilii muscle.
The zygomatic branches supply the inferior part of the orbicularis oculi muscle and zygomatic major and minor muscles. The buccal branches supply the muscles of the upper lip and nose and buccinator, risorius, and orbicularis oris muscles. The zygomatic and buccal branches are usually closely associated, exchanging many fibers.
The (marginal) mandibular branch supplies the muscles of the lower lip and mentalis muscle. The mandibular branch should not be confused with the mandibular nerve or V3. The cervical branch runs inferior to the mandible to supply the platysma muscle.
Identification Exercises
Identify the structures on the following diagrams by filling in each blank with the correct anatomic term. You can check your answers by looking back at the figure indicated in parentheses for each identification diagram.
1. (Figure 8-4, A)
2. (Figure 8-5)
3. (Figure 8-6)
4. (Figures 8-8 and 8-11)
5. (Figure 8-13)
6. (Figure 8-14)
7. (Figure 8-18, A)
8. (Figure 8-19, A)
9. (Figure 8-20)
10. (Figure 8-21)
1. The brainstem of the central nervous system consists of which structures?
2. The central nervous system consists of which two of the following structures?
3. Which of the following is a CORRECT statement concerning neurotransmitters within the nervous system?
A Discharged with the arrival of the action potential
B Bind to red blood cells so as to prompt transmission of impulses
C Can initiate an action potential in an adjacent cell if inhibitory
D Destroyed by specific white blood cells while still active
4. To what division of the nervous system does a nerve cell belong if it leads from the eye to the brain carrying visual information?
5. An efferent nerve with the nervous system is known to carry information
A from the periphery of the body to the brain (or spinal cord).
B such as taste or pain to the spinal cord.
C such as proprioception to the brain.
D away from the brain (or spinal cord) to the periphery of the body.
6. To which of the following structures does the posterior superior alveolar nerve and its branches supply?
7. Through which of the following foramina does the facial nerve pass through the skull?
8. Which of the following cranial nerves is directly involved in Bell palsy?
9. Which of the following nerve and muscle pairs is a CORRECT match?
A Long buccal nerve, buccinator muscle
B Accessory nerve, platysma muscle
10. Which of the following nerve and innervation pairs is a CORRECT match?
A Facial nerve, parotid salivary gland
B Chorda tympani, sublingual salivary gland
11. Which of the following cranial nerves has fibers that provide crossover-innervation to the contralateral side in the skull before continuing into the brain?
12. Which of the following cranial nerves carries taste sensation for the base of the tongue?
13. In which of the following regions of the head and neck is the trigeminal ganglion located?
A Superior to the deep lobe of the submandibular salivary gland
B Anterior surface of the petrous part of the temporal bone
C Posterior surface of the maxillary tuberosity of the maxilla
14. Sensory information is supplied for the soft palate by which of the following?
15. The posterior belly of the digastric muscle is innervated by branches from which of the following nerves?
16. Which of the following nerves within the head and neck may show crossover-innervation from the contralateral side in a patient?
17. Which of the following nerves listed below is considered part of the ophthalmic nerve?
18. Which of the following anatomic names is also used for cranial nerve X?
19. Which of the following nerves is located within the mandibular canal?
20. Which of the following nerves exits the foramen ovale of the sphenoid bone?
A Chorda tympani of the facial nerve
B Greater petrosal nerve of the facial nerve
21. Which of the following cranial nerves and its motor function is involved when a patient protrudes the tongue and a deviation to the right side is noted?
22. Which of the following nerves exits the skull through the foramen ovale?
23. Which of the following nerves serves the pulp of the mandibular molars?
24. Which of the following is considered the loss of feeling or sensation resulting from the use of certain drugs or gases that serve as inhibitory neurotransmitters?
25. Which nerve may in some cases also serve as an afferent nerve for the mandibular first molar, which needs to be considered when there is failure of the inferior alveolar local anesthetic block?