The Syringe
The syringe is one of three essential components of the local anesthetic armamentarium (others include the needle and the cartridge). It is the vehicle whereby the contents of the anesthetic cartridge are delivered through the needle to the patient.
Types of Syringes
Eight types of syringes for local anesthetic administration are available for use in dentistry today. They represent a considerable improvement over the local anesthetic syringes formerly used. These various types of syringes are listed in Box 5-1.
Syringes that do not permit aspiration (i.e., nonaspirating syringes) are not discussed because their use unacceptably increases the risk of inadvertent intravascular drug administration. Use of aspirating dental syringes (capable of the aspiration of blood) represents the standard of care.
American Dental Association criteria for acceptance of local anesthetic syringes include the following1,2:
1. They must be durable and able to withstand repeated sterilization without damage. (If the unit is disposable, it should be packaged in a sterile container.)
2. They should be capable of accepting a wide variety of cartridges and needles of different manufacture, and should permit repeated use.
3. They should be inexpensive, self-contained, lightweight, and simple to use with one hand.
4. They should provide for effective aspiration and be constructed so that blood may be easily observed in the cartridge.
Nondisposable Syringes
Breech-Loading, Metallic, Cartridge-Type, Aspirating
The breech-loading, metallic, cartridge-type syringe (Fig. 5-1) is the most commonly used in dentistry. The term breech-loading implies that the cartridge is inserted into the syringe from the side of the barrel of the syringe. The needle is attached to the barrel of the syringe at the needle adaptor. The needle then passes into the barrel, where it penetrates the diaphragm of the local anesthetic cartridge. The needle adaptor (screw hub or convertible tip) is removable and sometimes is discarded inadvertently along with the disposable needle.
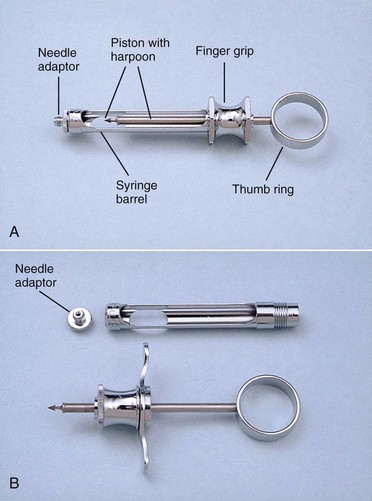
Figure 5-1 A, Breech-loading, metallic, cartridge-type syringe; assembled. B, Disassembled local anesthetic syringe.
The aspirating syringe has a device such as a sharp, hook-shaped end (often called the harpoon) attached to the piston that is used to penetrate the thick silicone rubber stopper (bung) at the opposite end of the cartridge (from the needle). Provided the needle is of adequate gauge, when negative pressure is exerted on the thumb ring by the administrator, blood will enter into the needle and will be visible in the cartridge if the needle tip rests within the lumen of a blood vessel. Positive pressure applied to the thumb ring forces local anesthetic into the needle lumen and the tissues wherever the needle tip lies. The thumb ring and finger grips give the administrator added control over the syringe. Almost all syringe manufacturers provide syringes with both “regular” and “small” thumb rings (Fig. 5-2). Most metallic, breech-loading, aspirating syringes are constructed of chrome-plated brass and stainless steel.
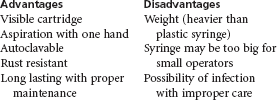
Advantages and disadvantages of the metallic, breech-loading, aspirating syringe are listed in Box 5-2.
Breech-Loading, Plastic, Cartridge-Type, Aspirating
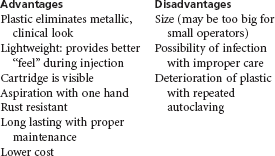
A plastic, reusable, dental aspirating syringe is available that is both autoclavable and chemically sterilizable. With proper care and handling, this syringe may be used for multiple anesthetic administrations before it is discarded. Advantages and disadvantages of the plastic, reusable, aspirating syringe are listed in Box 5-3.
Breech-Loading, Metallic, Cartridge-Type, Self-Aspirating
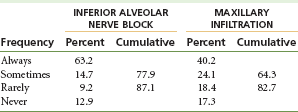
Potential hazards of intravascular administration of local anesthetics are great and are discussed more fully in Chapter 18. The incidence of positive aspiration may be as high as 10% to 15% with some injection techniques.3 It is accepted by the dental profession that an aspiration test before administration of a local anesthetic drug is of great importance. Unfortunately, it is abundantly clear that in actual clinical practice, too little attention is paid to this procedure (Table 5-1).
With commonly used breech-loading, metallic, cartridge-type syringes, an aspiration test must be carried out purposefully by the administrator before or during drug deposition. The key word here is purposefully. However, as demonstrated in Table 5-1, many dentists do not purposefully perform an aspiration test before injection of the anesthetic drug.4
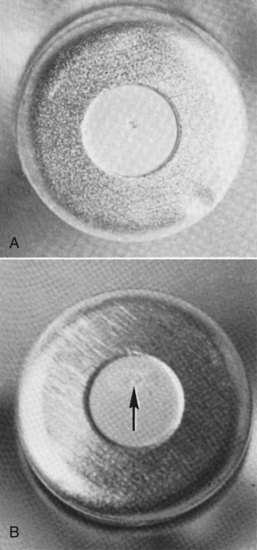
To increase the ease of aspiration, self-aspirating syringes have been developed (Fig. 5-3). These syringes use the elasticity of the rubber diaphragm in the anesthetic cartridge to obtain the necessary negative pressure for aspiration. The diaphragm rests on a metal projection inside the syringe that directs the needle into the cartridge (Fig. 5-4). Pressure acting directly on the cartridge through the thumb disc (Fig. 5-5) or indirectly through the plunger shaft distorts (stretches) the rubber diaphragm, producing positive pressure within the anesthetic cartridge. When that pressure is released, sufficient negative pressure develops within the cartridge to permit aspiration. The thumb ring produces twice as much negative pressure as the plunger shaft. The use of a self-aspirating dental syringe permits easy performance of multiple aspirations throughout the period of local anesthetic deposition.
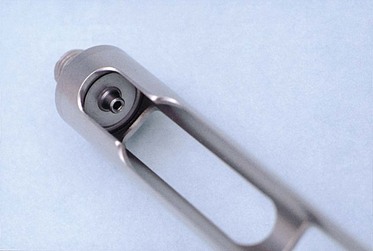
Figure 5-4 A metal projection within the barrel depresses the diaphragm of the local anesthetic cartridge.
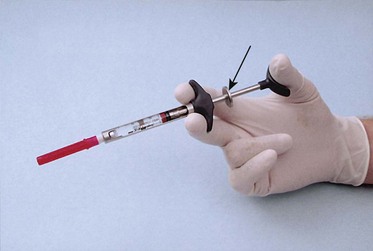
Figure 5-5 Pressure on the thumb disc (arrow) increases pressure within the cartridge. Release of pressure on the thumb disc produces the self-aspiration test.
The self-aspirating syringe was introduced into the United States in 1981. After an initial period of enthusiasm, the popularity of this syringe decreased. Some dentists believed that the self-aspirating syringe did not provide the same reliable degree of aspiration that was possible with the harpoon-aspirating syringe. It has been demonstrated, however, that this syringe does in fact aspirate as reliably as the harpoon-aspirating syringe.5-7 The notion can occur that aspiration may not be as reliable with the self-aspirating syringe because the administrator simply has to depress and release the thumb ring to aspirate, rather than pulling back on the thumb ring. Moving the thumb off the thumb ring and onto the thumb disc for aspiration has been mentioned by many dentists as uncomfortable for them. Although this is the preferred means of obtaining a satisfactory aspiration test with these syringes, pressure adequate for aspiration may be obtained by simply releasing the pressure of the thumb on the thumb ring. Second-generation self-aspirating syringes have eliminated the thumb disc.
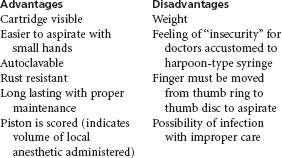
The major factor influencing ability to aspirate blood is not the syringe, but the gauge of the needle being used.7 In addition, most doctors using the harpoon-aspirating syringe tend to overaspirate, that is, they retract the thumb ring back too far and with excessive force (and, on occasion, disengage the harpoon from the stopper). These doctors feel more insecure with the self-aspirating syringe. Proper technique of aspiration is discussed in Chapter 11. Advantages and disadvantages of the metallic, self-aspirating syringe are listed in Box 5-4.
Pressure Syringes
Introduced in the late 1970s, pressure syringes brought about a renewed interest in the periodontal ligament (PDL) injection (also known as the intraligamentary injection [ILI]). Discussed in Chapter 16, the PDL injection, although usable for any tooth, helped make it possible to achieve more reliable pulpal anesthesia of one isolated tooth in the mandible where, in the past, nerve block anesthesia (e.g., inferior alveolar nerve block [IANB], Gow-Gates mandibular nerve block), with its attendant prolonged soft tissue (e.g., lingual) anesthesia, was necessary.
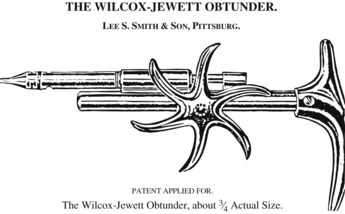
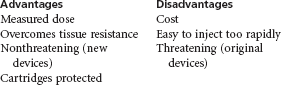
The original pressure devices, Peripress (Universal Dental Implements, Edison, NJ) and Ligmaject (IMA Associates, Bloomington, Ind) (Fig. 5-6), were modeled after a device that was available in dentistry in 1905—the Wilcox-Jewett obtunder (Fig. 5-7). These first-generation devices, using a pistol grip, are somewhat larger than the newer, pen-grip devices (Fig. 5-8). Although “special” syringes such as these are not necessary for a successful PDL injection, several advantages are associated with their use, not the least of which is the mechanical advantage they provide the administrator, making the local anesthetic easier to administer. This same mechanical advantage, however, makes the injection somewhat “too easy” to administer, leading to “too rapid” injection of the anesthetic solution and patient discomfort both during the injection and later, when the anesthetic has worn off. However, when used slowly, as recommended by manufacturers, pressure syringes are of some benefit in administration of this valuable technique of anesthesia.

Figure 5-6 Original design of pressure syringe for periodontal ligament (PDL) injection or intraligamentary (ILI) injection.
Pressure syringes offer advantages over the conventional syringe when used for PDL injections because their trigger delivers a measured dose of local anesthetic and enables a relatively physically weak administrator to overcome the significant tissue resistance encountered when the technique is administered properly. This mechanical advantage may also prove to be detrimental if the administrator deposits the anesthetic solution too quickly (<20 sec/0.2 mL dose). All pressure syringes completely encase the glass dental cartridge with plastic or metal, thereby protecting the patient in the unlikely event that the glass cartridge cracks or shatters during injection. The original pressure syringes looked somewhat threatening, having the appearance of a gun (see Fig. 5-6). Newer devices are smaller and are much less intimidating.
Probably the greatest disadvantage of using the pressure syringe is its cost; most are priced at considerably more than US $200 (November 2011). For this reason among others, it is recommended that pressure devices be considered for use only after the PDL injection has been found to be ineffective after several attempts with a conventional syringe and needle. Box 5-5 lists the advantages and disadvantages of the pressure syringe.
Jet Injector
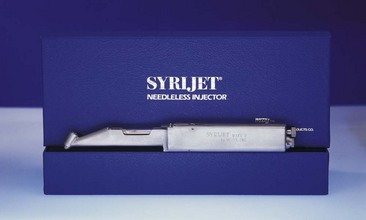
In 1947 Figge and Scherer introduced a new approach to parenteral injection—the jet or needle-less injection.8 This represented the first fundamental change in the basic principles of injection since 1853, when Alexander Wood introduced the hypodermic syringe. The first report of the use of jet injections in dentistry was published in 1958 by Margetis and associates.9 Jet injection is based on the principle that liquids forced through very small openings, called jets, at very high pressure can penetrate intact skin or mucous membrane (visualize water flowing through a garden hose that is being crimped). The most frequently used jet injectors in dentistry are the SyriJet Mark II (Mizzy Inc., Cherry Hill, NJ) (Fig. 5-9) and the MadaJet (Mada Medical Products Incorporated, Carlstadt, NJ) (Fig. 5-10). The SyriJet holds any 1.8-mL dental cartridge of local anesthetic. It is calibrated to deliver 0.05 to 0.2 mL of solution at 2000 psi.
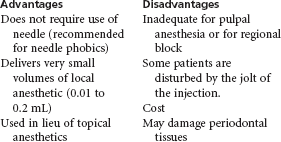
The primary purpose of the jet injector is to obtain topical anesthesia before insertion of a needle. In addition, it may be used to obtain mucosal anesthesia of the palate. Regional nerve blocks or supraperiosteal injections are still necessary for complete anesthesia. The jet injector is not an adequate substitute for the more traditional needle and syringe in obtaining pulpal or regional block anesthesia. Additionally, many patients dislike the feeling that accompanies use of the jet injector, as well as the possible postinjection soreness of soft tissue that may develop even with proper use of the device. Topical anesthetics, applied properly, serve the same purpose as jet injectors at a fraction of the cost (SyriJet Mark II, US $1950 [November 2011]*; MadaJet XL Dental, US $600 [November 2011]) and with minimum risk. Advantages and disadvantages of jet injectors are listed in Box 5-6.
Disposable Syringes
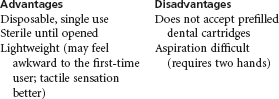
Plastic disposable syringes are available in a variety of sizes with an assortment of needle gauges. Most often they are used for intramuscular or intravenous drug administration, but they also may be used for intraoral injection (Fig. 5-11).
These syringes contain a Luer-Lok screw-on needle attachment with no aspirating tip. Aspiration can be accomplished by pulling back on the plunger of the syringe before or during injection. Because there is no thumb ring, aspiration with the plastic disposable syringe requires the use of both hands. In addition, these syringes do not accept dental cartridges. The needle, attached to the syringe, must be inserted into a vial or cartridge of local anesthetic drug and an appropriate volume of solution withdrawn. Care must be taken to avoid contaminating the multi-use vial during this procedure. Two- and 3-mL syringes with 25- or 27-gauge needles are recommended when the system is used for intraoral local anesthetic administration.
The plastic, disposable, non–cartridge-containing syringe is not recommended for routine use. Its use should be considered only when a traditional syringe is not available or cannot be used. This system is also practical when diphenhydramine HCl is used as a local anesthetic in cases of presumed local anesthetic allergy (see Chapter 18). Box 5-7 lists the advantages and disadvantages of the disposable syringe.
Safety Syringes
Recent years have seen a move toward the development and introduction of safety syringes in both medicine and dentistry. Safety syringes minimize the risk of an accidental needle-stick injury occurring to a dental health provider with a contaminated needle after administration of a local anesthetic. These syringes possess a sheath that “locks” over the needle when it is removed from the patient’s tissues, preventing accidental needle-stick.
Devices such as the UltraSafety Plus XL* and the 1 Shot Safety Syringe† were available as of January 2011. The UltraSafety Plus XL aspirating syringe system contains a syringe body assembly and a plunger assembly (Fig. 5-12, A). Once the syringe is properly assembled and the injection administered, the syringe may be made “safe” with one hand by gently moving the index and middle fingers against the front collar of the guard (Fig. 5-12, B). Once “guarded,” the now contaminated needle is “safe,” so that it is virtually impossible for dental health providers to be injured with the needle. Upon completion of the injection, the entire syringe is discarded into the proper receptacle (e.g., sharps container).

Figure 5-12 A, UltraSafety Plus XL aspirating syringe, ready for injection. B, UltraSafety Plus XL aspirating syringe; needle sheathed to prevent needle-stick injury.
Dental safety syringes are designed as single-use items, although they permit reinjection. Reloading the syringe with a second anesthetic cartridge and reinjecting with the same syringe is discouraged because this obviates the important safety aspect of the device.
In 2000, Cuny and associates evaluated four dental safety syringe systems—Safe-Mate needle system (Septodont Inc.), Safety Plus syringe (Septodont Inc.), UltraSafe syringe (Septodont Inc.), and Hypo Safety syringe (Dentsply MPL Technologies, Franklin Park, Ill)—over a 1-year period at a U.S. dental school.10 Their finding was that using these Food and Drug Administration (FDA)-approved devices resulted in an initial increase in needle-stick injuries. They stated that hands-on training, monitoring, and follow-up reminders appeared to be effective in reducing injuries associated with the change from traditional to safety needles.
Advantages and disadvantages of the safety syringe are listed in Box 5-8.
Computer-Controlled Local Anesthetic Delivery (C-CLAD) Systems
The standard dental syringe described previously is a simple mechanical instrument that dates back to 1853, when Charles Pravaz patented the first syringe.11 The dental syringe is a drug delivery device requiring that the operator simultaneously attempt to control the variables of drug infusion and the movement of a penetrating needle. The operator’s inability to precisely control both of these activities during an injection can compromise an injection technique. In addition, a traditional syringe is handled with a palm-thumb grasp, which is not designed for ideal ergonomics or needle control during the injection. For certain practitioners—those with small hands—just holding a syringe with a full cartridge of anesthetic may be difficult.
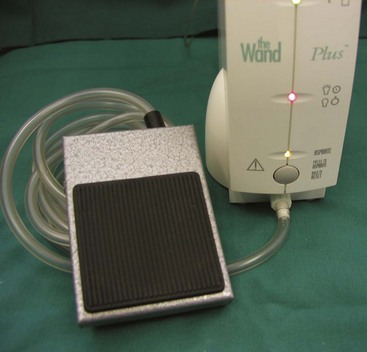
In 1997 the first computer-controlled local anesthetic delivery (C-CLAD) system was introduced into dentistry. The Wand (Milestone Scientific Inc., Livingston, NJ) was designed to improve on the ergonomics and precision of the dental syringe (Fig. 5-13). This system enabled a dentist or hygienist to accurately manipulate needle placement with fingertip accuracy and deliver the local anesthetic with a foot-activated control (Fig. 5-14). A lightweight handpiece (Fig. 5-15), held in a penlike grasp, provides increased tactile sensation and control compared with the traditional syringe. Available flow rates of local anesthetic delivery are computer controlled and thus remain consistent from one injection to the next. C-CLAD systems represent a significant change in the manner in which a local anesthetic injection is administered. The operator is now able to focus attention on needle insertion and positioning, allowing the motor in the device to administer the drug at a preprogrammed rate of flow. It is likely that greater ergonomic control coupled with fixed flow rates is responsible for the improved injection experience demonstrated in many clinical studies conducted with these devices in dentistry.12-16 Several clinical trials in medicine have demonstrated measurable benefits of this technology.17,18

Figure 5-15 The Wand has a lightweight handpiece that provides improved tactile sensation and control.
Hochman and colleagues were the first to demonstrate a marked reduction in pain perception with injections using C-CLADs.11 Fifty blindfolded dentists participated (they received the injection) in a controlled clinical study comparing the standard manual syringe with The Wand/CompuDent System for palatal injection. Forty-eight (96%) preferred injections with the C-CLADs. Overall pain perception was reduced two- to threefold when compared with the standard manual syringe.
Nicholson and associates conducted a randomized clinical study using two operators administering four different types of dental injections to compare C-CLADs with the standard syringe.13 Mean injection discomfort ratings were found to be consistently lower when C-CLADs were used compared with the manual syringe. Two thirds of patients preferred that future dental injections be performed with a C-CLAD system. Investigators in the study increasingly preferred to perform all injections with C-CLAD technology.
Perry and Loomer presented data from a single-blind crossover study comparing C-CLADs with traditional syringe delivery of local anesthetic for quadrant scaling and root planing. Twenty subjects received the anterior middle superior alveolar nerve block (AMSA) injection (described in Chapter 13). Scores for AMSA computer-controlled injection revealed highly significant differences in favor of the computer-controlled device (P <.0001).14
Fukayama and associates conducted a controlled clinical study to evaluate the pain perception of a C-CLAD device. Seventeen of 20 subjects reported a slight- or no-pain rating on a visual analog scale (VAS) for palatal injections administered with C-CLADs. Investigators concluded, “The new system provides comfortable anesthesia for patients and can be a good alternative for conventional manual syringe injection.”15
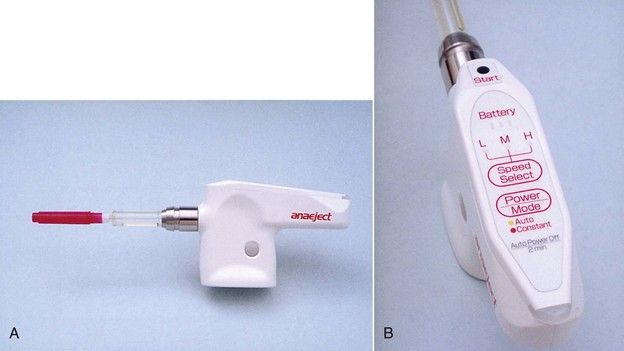
At present, three C-CLADs are available in the North American market: The Wand/CompuDent System, The Wand/STA System, and the Comfort Control Syringe. Another system, the QuickSleeper, is marketed in Europe. Similar devices, such as the Anaeject, are marketed in Japan (Fig. 5-16).
The Wand/STA System
The STA-Single Tooth Anesthesia System (Milestone Scientific Inc., Livingston, NJ) represents a significant advance in C-CLAD technology (Fig. 5-17). The STA System was introduced in 2007. This third-generation C-CLAD instrument represents a new and meaningful innovation for subcutaneous injections performed both in dentistry and in medicine.19 The technological advancement is related to the development of what is called dynamic pressure-sensing technology (DPS technology).20 DPS technology enables the precise monitoring and control of fluid pressure at the needle tip when a subcutaneous injection is performed. Fluid exit-pressure at the needle tip is used to identify a given anatomic location and/or a specific tissue type based on this repeatable finding.21 Exit-pressure information is provided to the clinician on a continuous basis in the form of spoken and/or audible sounds and visual indicators emitted from the STA instrument, thus providing continuous real-time feedback while a dental injection is performed (Fig. 5-18, A through C).22

Figure 5-18 Dynamic Pressure Sensing (DPS) on the STA Single Tooth Anesthesia C-CLAD device provides both visual and audible feedback regarding placement of the needle tip during the periodontal ligament (PDL) injection. Horizontal color bars indicate pressure at the tip of the needle. A, Red—pressure is too low. B, Orange and dark yellow—increasing pressure but not yet adequate. C, Light yellow—correct pressure for PDL injection. At this point (C) the STA unit will also provide an audible clue “PDL, PDL, PDL” that the needle tip is properly situated.
The STA System instrument can perform all traditional injections, as well as several newer dental injection techniques as previously described with The Wand and CompuDent System instruments. In addition, the STA System offer a unique approach for performing PDL (intraligamentary) injection using DPS technology.22 The instrument has been designed to accurately identify the precise anatomic location for the intraligamentary (PDL) injection.23 The STA System audibly and visually “guides” placement of the needle tip into the anatomic entrance of the periodontal ligament space through DPS technology. Important to the success of the PDL injection is proper needle placement into its the PDL space. Use of a traditional syringe provides little or no information as to correct needle-tip location, so this can be considered a “blinded” approach to PDL injection. In contrast, using the DPS technology of the STA System informs the clinician of the status of needle position based on real-time information. This transforms the PDL injection technique into a “guided” technique that can be easily and accurately performed. Additionally, the STA instrument is capable of generating precise fluid pressures in ranges that are much lower in comparison with other injection devices. This ability to maintain lower pressures permits the absorption of greater volumes of anesthetic solution safely and effectively through the intraligamentary tissues—another benefit of this technology.24 Allowing a greater volume of anesthetic to be safely administered results in a longer duration of anesthesia produced by the STA intraligamentary injection compared with intraligamentary (PDL) injection performed using high-pressure syringes and/or other delivery instruments.25
Ferrari and coworkers published data on 60 patients receiving the intraligamentary (PDL) injection; they compared the STA System versus two other delivery instruments: a high-pressure mechanical syringe (Ligmaject, IMA Associates) and a conventional dental syringe.25 Electrical pulp testing was performed on all teeth at regular intervals to determine success or failure when these different instruments are used. In addition, patient subjective pain responses were recorded post treatment. This study found the STA System to have a success rate of 100% in achieving effective pulpal anesthesia, as well as more rapid onset of anesthesia. The PDL injection in this study was performed as a primary injection for restorative dental care in mandibular teeth. The study also found subjective pain responses of “minimal or no pain” observed in all patients receiving PDL injections with the STA System. In contrast, PDL injections performed with the other two systems were found to have generally higher pain scores throughout testing. Investigators concluded that the STA instrument provided a more predictable, more reliable, and more comfortable PDL injection than a high-pressure mechanical syringe or a conventional dental syringe.
The STA System has two basic components: the STA Wand handpiece and the STA drive unit. The STA Wand handpiece is a single-use (per patient visit) lightweight handpiece (weighing less than 10 g) (Fig. 5-19, A and B). It provides excellent tactile control and use of a more desirable ergonomic grasp (Fig. 5-20). Clinicians have reported that a C-CLAD instrument, such as the STA System, is more comfortable to use and produces fewer musculoskeletal problems over the long term.26
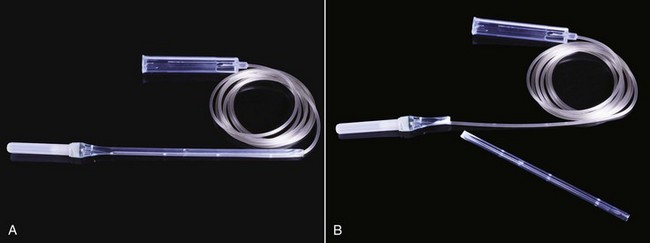
Figure 5-19 STA Wand handpiece is lightweight (less than 10 grams) (A) and can easily be shortened to aid in administration of some injections (B), such as the AMSA or other palatal techniques.

Figure 5-20 The STA Wand handpiece is held in an instrument grasp permitting the administrator greater tactile sensitivity during the injection.
STA Wand handpieces are available with many standard dental needle sizes: 30-gauge  inch, 27-gauge
inch, 27-gauge  inch, 30-gauge 1 inch, and 27-gauge
inch, 30-gauge 1 inch, and 27-gauge  inch needle lengths. The STA Wand handpiece is a single-use sterilized handpiece (Fig. 5-21) that is available in two forms: one in which the handpiece has a preattached needle, and one in which a needle needs to be attached at the time of treatment. When the STA intraligamentary (PDL) injection is performed, it is suggested that a preattached needle handpiece be used. The STA Wand handpiece provides the general benefit of being easier and lighter to hold, allowing for greater access and ease of use as compared with the conventional syringe. Additionally, the STA Wand handpiece can be modified to different lengths for greater versatility of use (see Fig. 5-19, B).
inch needle lengths. The STA Wand handpiece is a single-use sterilized handpiece (Fig. 5-21) that is available in two forms: one in which the handpiece has a preattached needle, and one in which a needle needs to be attached at the time of treatment. When the STA intraligamentary (PDL) injection is performed, it is suggested that a preattached needle handpiece be used. The STA Wand handpiece provides the general benefit of being easier and lighter to hold, allowing for greater access and ease of use as compared with the conventional syringe. Additionally, the STA Wand handpiece can be modified to different lengths for greater versatility of use (see Fig. 5-19, B).
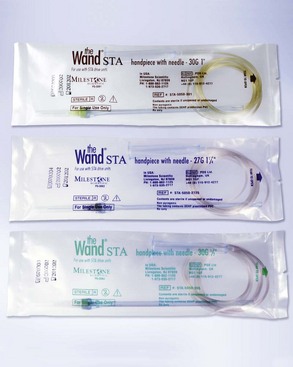
Figure 5-21 The STA Wand handpiece is presterilized, single-use and is available in a variety of needle gauge and lengths. Other Luer-Lok needles can also be sued on this handpiece.
The second component of the STA System is the drive unit itself. The drive unit integrates two cap holders into the base of the unit, thus allowing single-handed recapping of the needle from either side of the unit (see Fig. 5-17). New features not previously available with earlier versions of this C-CLAD device (Wand, CompuDent) include automatic purging of anesthetic solution that primes the handpiece before use, automatic plunger retraction after completion of use, and a multicartridge feature that reduces anesthetic waste when more than one anesthetic cartridge is used. The STA System also has a Training Mode feature that provides clinicians with spoken instructional guidance on its use, thereby minimizing the learning curve when the system is used for the first time.
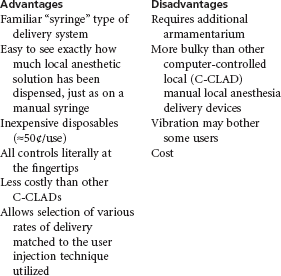
Advantages and disadvantages of The Wand/STA System are listed in Box 5-9.
Comfort Control Syringe
Introduced several years after The Wand, the Comfort Control Syringe (CCS) System attempts to improve on the C-CLAD concept. The CCS System is an electronic, preprogrammed delivery device that provides the operator with the control needed to make the patient’s local anesthetic injection experience as pleasant as possible (Fig. 5-22). As with other C-CLADs, this is achieved by depositing the local anesthetic more slowly and consistently than is possible manually. The CCS has a two-stage delivery system. Injection begins at an extremely slow rate to avoid the pain associated with rapid anesthetic delivery. After 10 seconds, the CCS automatically increases speed to a preprogrammed injection rate for the technique selected. Five preprogrammed injection rates are available for specific injections: Block, Infiltration, PDL, AMSA/palatal anterior superior alveolar nerve block (P-ASA), and Lingual Infiltration.
The handpiece controls are shown in Figure 5-23.
• The front button with the arrow and square controls the “Start/Stop” functions by initiating or terminating the selected program.
• The middle button activates the “Aspiration” function by slightly retracting the plunger.
• The rear button initiates “Double Rate” and operates in the same manner as the Double Rate button on the unit. It doubles the preprogrammed injection rate. Re-selecting it restores the preprogrammed speed.
Standard dental local anesthetic cartridges and dental needles may be used in the CCS. Box 5-10 lists advantages and disadvantages of the CCS.
C-CLADs allow local anesthetics to be administered comfortably to the patient in virtually all areas of the oral cavity. This is of greatest importance in the palate, where the level of patient discomfort can be significant. The nasopalatine nerve block, as well as other palatal injections (e.g., AMSA,27 P-ASA28), can be administered atraumatically in most patients. It is reasonable to conclude that any injection technique that has even a remote possibility of being uncomfortable for the patient can be delivered more comfortably using a C-CLAD device.
Care And Handling of Syringes
When properly maintained, metal and plastic reusable syringes are designed to provide long-term service. Following is a summary of manufacturers’ recommendations concerning care of these syringes:
1. After each use, the syringe should be thoroughly washed and rinsed so as to be free of any local anesthetic solution, saliva, or other foreign matter. The syringe should be autoclaved in the same manner as other surgical instruments.
2. After every five autoclavings, the syringe should be dismantled and all threaded joints and the area where the piston contacts the thumb ring and the guide bearing should be lightly lubricated.
3. The harpoon should be cleaned with a brush after each use.
4. Although the harpoon is designed for long-term use, prolonged use will result in decreased sharpness and failure to remain embedded within the stopper of the cartridge. Replacement pistons and harpoons are readily available at low cost.
Problems
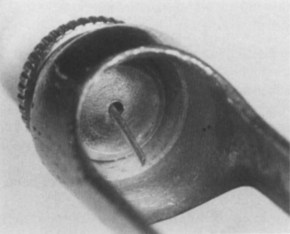
When a syringe is reloaded with a second local anesthetic cartridge and a needle is already in place, care must be taken to ensure that the needle penetrates the center of the rubber diaphragm. An off-center perforation produces an ovoid puncture of the diaphragm, allowing leakage of the anesthetic solution around the outside of the metal needle and into the patient’s mouth (Fig. 5-24). (For further information, see Chapter 7.)
Broken Cartridge
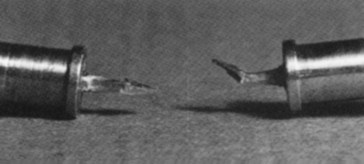
A badly worn syringe may damage the cartridge, leading to breakage. This also can result from a bent harpoon. A needle that is bent at its proximal end (Fig. 5-25) may not perforate the diaphragm on the cartridge. Positive pressure on the thumb ring increases pressure within the cartridge, which may cause the cartridge to break.
Bent Harpoon
The harpoon must be sharp and straight (Fig. 5-26). A bent harpoon produces an off-center puncture of the silicone rubber plunger, causing the plunger to rotate as it moves down the glass cartridge. This may result in cartridge breakage.
Disengagement of the Harpoon from the Plunger During Aspiration
Disengagement occurs if the harpoon is dull or if the administrator applies too much pressure to the thumb ring during aspiration. If this happens, the harpoon should be cleansed and sharpened or replaced with a new sharp harpoon. Disengagement is most likely to occur when a 30-gauge dental needle is being used because significant resistance is produced within the needle lumen as aspiration is attempted. A very gentle backward motion of the plunger is all that is necessary for successful aspiration. Forceful action is not necessary. (See the discussion in Chapter 11.)
Recommendations
No conclusive evidence indicates that any manufacturer’s syringe is superior. Therefore the ultimate decision in selection of a syringe must be left to the discretion of the buyer. It is recommended, however, that before purchasing any syringe, the buyer place a full dental cartridge into it and pick up the syringe as if to use it. It should be noted whether the fingers (thumb to other fingers) are stretched maximally, because to aspirate with a harpoon-type syringe, one must be able to pull the thumb ring back several millimeters. If one is not able to do so, reliable aspiration is not possible. Although all syringes available today are of roughly the same dimensions, some variation is noted. Manufacturers market syringes with smaller thumb rings or shorter pistons. These modifications make aspiration easier to accomplish for persons with smaller hands.
Following are additional recommendations:
1. A safety syringe, minimizing the risk of accidental needle-stick injury, is recommended for use during all local anesthetic injections.
2. A self-aspirating syringe is recommended for practitioners with small hands.
3. Any syringe system used must be capable of aspiration. Nonaspirating syringes should never be used for local anesthetic injections.
4. All reusable syringes must be capable of being sterilized.
References
1. Council on Dental Materials and Devices. New American National Standards Institute/American Dental Association specification no. 34 for dental aspirating syringes. J Am Dent Assoc. 1978;97:236–238.
2. Council on Dental Materials, Instruments, and Equipment. Addendum to American National Standards Institute/American Dental Association specification no. 34 for dental aspirating syringes. J Am Dent Assoc. 1982;104:69–70.
3. Bartlett, SZ. Clinical observations on the effects of injections of local anesthetic preceded by aspiration. Oral Surg. 1972;33:520.
4. Malamed, SF. Handbook of local anesthesia. St Louis: Mosby; 1980.
5. Meechan, JG, Blair, GS, McCabe, JF. Local anaesthesia in dental practice. II. A laboratory investigation of a self-aspirating system. Br Dent J. 1985;159:109–113.
6. Meechan, JG. A comparison of three different automatic aspirating dental cartridge syringes. J Dent. 1988;16:40–43.
7. Peterson, JK. Efficacy of a self-aspirating syringe. Int J Oral Maxillofac Surg. 1987;16:241–244.
8. Figge, FHJ, Scherer, RP. Anatomical studies on jet penetration of human skin for subcutaneous medication without the use of needles. Anat Rec. 1947;97:335. [(abstract)].
9. Margetis, PM, Quarantillo, EP, Lindberg, RB. Jet injection local anesthesia in dentistry: a report of 66 cases. US Armed Forces Med J. 1958;9:625–634.
10. Hoffmann-Axthelm, W. History of dentistry. Chicago: Quintessence; 1981. [p 339].
11. Hochman, MN, Chiarello, D, Hochman, CB, et al. Computerized local anesthesia delivery vs. traditional syringe technique. NY State Dent J. 1997;63:24–29.
12. Gibson, RS, Allen, K, Hutfless, S, et al. The Wand vs. traditional injection: a comparison of pain related behaviors. Pediatr Dent. 2000;22:458–462.
13. Nicholson, JW, Berry, TG, Summitt, JB, et al. Pain perception and utility: a comparison of the syringe and computerized local injection techniques. Gen Dent. 2001;49:167–172.
14. Perry, DA, Loomer, PM. Maximizing pain control: the AMSA injection can provide anesthesia with few injections and less pain. Dimensions Dent Hyg. 2003;1:28–33.
15. Fukayama, H, Yoshikawa, F, Kohase, H, et al. Efficacy of anterior and middle superior alveolar (AMSA) anesthesia using a new injection system: The Wand. Quint Int. 2003;34:737–741.
16. Tan, PY, Vukasin, P, Chin, ID, et al. The Wand local anesthetic delivery system. Dis Colon Rectum. 2001;44:686–689.
17. Landsman, A, DeFronzo, D, Hedman, J, McDonald, J. A new system for decreasing the level of injection pain associated with local anesthesia of a toe, (abstract). Annual Meeting of the American Academy of Podiatric Medicine. 2001.
18. Friedman, MJ, Hochman, MN. 21st century computerized injection for local pain control. Compend Contin Educ Dent. 1997;18:995–1003.
19. Kudo, M, Ohke, H, Katagiri, K, et al. The shape of local anesthetic injection syringes with less discomfort and anxiety: evaluation of discomfort and anxiety caused by various types of local anesthetic injection syringes in high level trait-anxiety people. J Jpn Dent Soc Anesthesiol. 2001;29:173–178.
20. Hochman, MN, Friedman, MJ. In vitro study of needle deflection: a linear insertion technique versus a bi-directional rotation insertion technique. Quint Int. 2000;31:737–743.
21. Hochman, MN, Friedman, MJ. An in vitro study of needle force penetration comparing a standard linear insertion to the new bidirectional rotation insertion technique. Quint Int. 2001;32:789–796.
22. Pashley, EL, Nelson, R, Pashley, DH. Pressures created by dental injections. J Dent Res. 1981;60:1742–1748.
23. Fuhs, QM, Walker, WA, Gouigh, RW, et al. The periodontal ligament injection: histological effects on the periodontium in dogs. J Endodont. 1983;9:411–415.
24. Galili, D, Kaufman, E, Garfunkel, AA, et al. Intraligamentary anesthesia: a histological study. Int J Oral Surg. 1984;12:511–516.
25. Albers, DD, Ellinger, RF. Histologic effects of high- pressure intraligamental injections on the periodontal ligament. Quint Int. 1988;19:361–363.
26. Froum, SJ, Tarnow, D, Caiazzo, A, et al. Histologic response to intraligament injections using a computerized local anesthetic delivery system: a pilot study in Mini-Swine. J Periodont. 2000;71:1453–1459.
27. Friedman, MJ, Hochman, MN. The AMSA injection: a new concept for local anesthesia of maxillary teeth using a computer-controlled injection system. Quint Int. 1998;29:297–303.
28. Friedman, MJ, Hochman, MN. P-ASA block injection: a new palatal technique to anesthetize maxillary anterior teeth. J Esthet Dent. 1999;11:23–71.
*Mizzy Inc., 616 Hollywood Ave., Cherry Hill, NJ 08002; 1-800-663-4700; www.keystoneind.com.
*UltraSafety Plus XL, Septodont Inc., 245C Quigley Blvd., New Castle, DE 19720; 1-800-872-8305; www.septodontinc.com.
†1 Shot Safety Syringe, Sultan Chemists, Englewood, NJ; 1-800-637-8582; www.sultanintl.com.