Anesthetic Considerations in Dental Specialties
The techniques of local anesthesia described previously in this section are valuable to doctors in virtually all areas of dental practice. However, specific needs and problems are associated with pain control in particular areas of dentistry. This chapter discusses the dental specialties listed below and their peculiar needs in the area of pain control:
Endodontics
Effects of Inflammation on Local Anesthesia
Inflammation and infection lower tissue pH, altering the ability of a local anesthetic to provide clinically adequate pain control. As a review, local anesthetics are weak bases (pKa, 7.5 to 9.5) and are not water-soluble compounds. Combined with hydrochloric acid (HCl), local anesthetics are injected in their acid–salt form (e.g., lidocaine HCl), improving their water solubility and stability. The pH of a “plain” local anesthetic is approximately 6.5, and the pH of one containing a vasoconstrictor is approximately 3.5. In an acidic solution, hydrogen ions (H+) are “floating around.” If we abbreviate the anesthetic drug as RN (the un-ionized form of the local anesthetic), then some of these RNs will attach to an H+, forming the cationic form of the local anesthetic (RNH+). The more acidic the anesthetic solution, the greater the number of H+ ions available, and the greater the percentage of RNH+ found in the solution. Because only the RN ionic form is lipid soluble and is able to cross the lipid-rich nerve membrane, the lower the pH of the anesthetic solution and the tissue into which it is injected, the lower is the percentage of RN ions, the slower is the onset, and the less profound is the resultant anesthesia.
Once injected, the pH of the anesthetic solution is slowly increased toward the body’s normal pH of approximately 7.4 by tissue fluid buffers. As this conversion occurs, RNH+ ions lose H+, becoming un-ionized RN ions (according to the Henderson-Hasselbalch equation; see Chapter 1), which now are able to diffuse across the nerve membrane to the interior of the nerve.
Pulpal and periapical inflammation or infection can cause significant alterations in tissue pH in the affected region, including decreased pH (e.g., pus has a pH of 5.5 to 5.6) and increased vascularity. Increased acidity has several negative aspects.1 It severely limits the formation of RN, increasing the formation of RNH+. RNs that do diffuse into the nerve find a normal tissue pH of 7.4 within the nerve and re-equilibrate into both RN and RNH+ forms. These RNH+ forms are then able to enter into and block sodium channels, blocking nerve conduction. But with fewer total anesthetic molecules (RN’s and RNH+’s) diffusing into the nerve, there is a greater likelihood that incomplete anesthesia will develop. The overall effect of ion entrapment is to delay the onset of anesthesia and possibly interfere with nerve blockade.2 Ion entrapment changes the products of inflammation, so they inhibit anesthesia by directly affecting the nerve. Brown demonstrated that inflammatory exudates enhance nerve conduction by lowering the response threshold of the nerve,1 which may inhibit local anesthesia. This causes blood vessels in the region of inflammation to become unusually dilated, allowing more rapid removal of the anesthetic from the site of injection. This leads to an increased possibility that resultant local anesthetic blood levels will be elevated (from those seen in normal tissue).2
Although there are no magic bullets for attaining profound pain control in teeth requiring pulpal extirpation, several methods may increase the likelihood of success. First, administer the local anesthetic at a site distant from the area of inflammation. It is undesirable to inject anesthetic solutions into infected tissue because this may cause the infection to spread to uninvolved regions.3,4 Administration of local anesthetic solution into a site distant from the involved tooth is more likely to provide adequate pain control because of the existence of normal tissue conditions. Therefore, regional nerve block anesthesia is a major factor in pain control for the pulpally involved tooth. Second, use a buffered local anesthetic solution. Administration of a solution of local anesthetic with a pH in the range of 7.35 to 7.5 increases the percentage of RN ionic form approximately 6000-fold (lidocaine HCl with epinephrine [pH 3.5] = 0.004% of ionic forms RN; pH 7.4 = 24.03% RN). In studies with “normal” teeth, 71% of patients receiving a buffered local anesthetic achieved successful pulpal anesthesia within 2 minutes versus 5 minutes 17 seconds for unbuffered local anesthetic.5 Although at the time of this writing (January 2012), no clinical trials of buffered local anesthetics have been published, anecdotal reports from endodontists indicate that they have seen a considerably greater incidence of successful anesthesia on teeth requiring pulpal extirpation.6
Methods of Achieving Anesthesia
The following techniques are recommended for providing pain control in pulpally involved teeth: local infiltration, regional nerve block, intraosseous injection, intraseptal injection, periodontal ligament injection, and intrapulpal injection. The order in which these techniques are discussed is the typical sequence in which they are normally used to achieve pain control when one seeks to extirpate pulpal tissues.
Local Infiltration (Supraperiosteal Injection)
Local infiltration is commonly used to provide pulpal anesthesia in maxillary teeth. It is usually effective in endodontic procedures when severe inflammation or infection is not present. Local infiltration should not be attempted in a region where infection is obviously (clinically or radiographically) present because of the possible spread of infection to other regions and a greatly decreased rate of success. When infection is present, other techniques of pain control should be relied on. Infiltration anesthesia is often effective at subsequent endodontic visits, if adequate débridement and shaping of the canals have been previously accomplished.
Regional Nerve Block
Regional nerve block anesthesia is recommended in cases where infiltration anesthesia may be ineffective or contraindicated. These techniques are discussed in detail in Chapters 13 and 14. Regional nerve block is likely to be effective because the anesthetic solution is deposited at a distance from the inflammation, where tissue pH and other factors are more normal.
Intraosseous Injection
The intraosseous (IO) injection has experienced a resurgence of enthusiasm in recent years.7-15 IO injections can provide anesthesia profound enough to allow painless access into the pulp chamber for removal of pulpal tissue. IO technique is described in Chapter 15 and is reviewed here (Figs. 16-1 and 16-2):
1. Apply topical anesthetic at the site of the injection to anesthetize the soft tissue.
2. While holding the perforator perpendicular to the cortical plate, gently push it through the attached gingiva until its tip rests against bone.
3. Activate the handpiece and apply pressure on the perforator in a “pecking” motion until a sudden loss of resistance is felt.
4. Withdraw the perforator and dispose of it safely.
5. Insert the local anesthetic needle into the hole and deposit the volume of local anesthetic appropriate for the procedure (see charts in Chapter 15).
Cardiovascular absorption of the local anesthetic after IO injection is more rapid than after the other techniques described.16,17 Transient elevations in heart rate were noted in 67% (28/42) of healthy patients receiving 2% lidocaine with 1 : 100,000 epinephrine via IO injection. The heart rate returned to within 5 beats of normal within 4 minutes in 79% of patients. No significant increase was noted when 3% mepivacaine was injected IO in the same patients.17
The use of epinephrine-containing local anesthetics in the IO technique is not contraindicated in healthy, non–cardiovascular risk patients. However, where significant cardiovascular risk or other relative contraindications to administration of epinephrine exist, a “plain” local anesthetic is a good alternative for IO anesthesia, keeping in mind that neither the depth nor duration of anesthesia will be as good as expected in a non-pulpally involved tooth.
Intraseptal Injection
This is a variation of IO and periodontal ligament (PDL) injections and may be used as an alternative to these techniques. It is more successful in younger patients because of decreased bone density. Intraseptal anesthesia is described in Chapter 15 and proceeds as follows18:
1. Anesthetize the soft tissues at the injection site via local infiltration.
2. Insert a 27-gauge short needle into the intraseptal bone distal to the tooth to be anesthetized (Fig. 16-3).

Figure 16-3 For the intraseptal injection, a 27-gauge short needle is inserted into the intraseptal bone distal to the tooth to be anesthetized.
3. Advance the needle firmly into the cortical plate of bone.
Considerable resistance must be encountered as the anesthetic is being deposited. If administration of the anesthetic is easy, the needle tip is most likely in soft tissue, not in bone.
Periodontal Ligament Injection
The PDL injection may be an effective method of providing anesthesia in pulpally involved teeth if infection and severe inflammation are not present. This technique is discussed in Chapter 15. By way of review, a 27-gauge short needle is firmly placed between the interproximal bone and the tooth to be anesthetized. The bevel of the needle should face the tooth (although bevel orientation is not critical for success). It is appropriate to bend the needle if necessary to gain access. A small volume (0.2 mL) of local anesthetic is deposited under pressure for each root of the tooth. It may be necessary to repeat the PDL injection on all four sides of the tooth. Computer-controlled local anesthetic delivery (C-CLAD) devices enable the PDL injection to be administered more successfully and more comfortably than an injection given with a traditional dental local anesthetic syringe.
Intrapulpal Injection
The intrapulpal injection provides pain control both by the pharmacologic action of the local anesthetic and by applied pressure. This technique may be used once the pulp chamber is exposed surgically or pathologically. The technique is described in Chapter 15.
When intrapulpal injections are administered properly, a brief period of sensitivity, ranging from mild to severe, may accompany the injection. Clinical pain relief follows almost immediately, permitting instrumentation to proceed atraumatically.
Occasionally, the anesthetic needle does not fit snugly into the canal, preventing the increased pressure normally encountered in the intrapulpal injection. In this situation, the anesthetic can be deposited in the chamber or canal. Anesthesia is produced only by the pharmacologic action of the drug; there is no pressure anesthesia. Instrumentation may begin approximately 30 seconds after the drug is deposited.
With the growing popularity of IO anesthesia, the need for intrapulpal injection to provide profound pain control in cases of irreversible pulpitis has decreased.
Today there are but few occasions when all of the techniques discussed fail to provide clinically acceptable pain control, and intrapulpal anesthesia cannot be attempted until the pulp is exposed. The following sequence of treatment may be of value on these rare occasions:
1. Use slow-speed high-torque instrumentation (which usually is less traumatic than the high-speed low-torque option).
2. Use (minimal or moderate) sedation (which helps to decrease the patient’s response to painful stimuli). Nitrous oxide–oxygen inhalation sedation is a readily available, safe, and highly effective method of relaxing a patient and elevating his or her pain reaction threshold.
3. If, after steps 1 and 2, the pulp chamber is opened, administer direct intrapulpal anesthesia. This is usually effective despite the brief period of pain associated with intrapulpal administration.
4. If a high level of pain persists and it still is not possible to enter the pulp chamber, then the following sequence should be considered:
a. Place a cotton pellet saturated with local anesthetic loosely on the pulpal floor of the tooth.
b. Wait 30 seconds; then press the pellet more firmly into the dentinal tubules or the area of pulpal exposure. This area may be sensitive initially but should become insensitive within 2 to 3 minutes.
c. Remove the pellet and continue use of the slow-speed drill until pulpal access is gained; then perform direct injection into the pulp.
With most endodontic procedures, difficulty in providing adequate anesthesia occurs only at the first appointment. Once the pulp tissue has been extirpated, the need for pulpal anesthesia disappears. Soft tissue anesthesia may be necessary at ensuing appointments for comfortable placement of the rubber dam clamp, but if adequate tooth structure remains, this may not be necessary. Some patients respond unfavorably to instrumentation of their root canals, even when the canals have been thoroughly débrided. If this occurs, infiltration (in the maxillary or mandibular incisor region [with articaine HCl]), intrapulpal anesthesia, or topical anesthetic may be used. Apply a small amount of topical anesthetic ointment onto the file or reamer before inserting it into the canal. This helps to desensitize the periapical tissues during instrumentation of the canals. Patients may react to filling of the canals. Local anesthesia should be considered before this stage of treatment is started.
Pediatric Dentistry
Pain control is one of the most important aspects of behavioral management in children undergoing dental treatment. Unpleasant childhood experiences have made many adults acutely phobic with regard to dental treatment. Today, however, many local anesthetic drugs are available to make pain management relatively easy. Special concerns in pediatric dentistry relevant to local anesthetic include anesthetic overdose (toxic reaction), self-inflicted soft tissue injury related to the prolonged duration of soft tissue anesthesia, and technique variations related to the smaller skulls and differing anatomy of younger patients.
Local Anesthetic Overdose
Overdose from a drug occurs when its blood level in a target organ (e.g., brain and myocardium for local anesthetics) becomes excessive (see Chapter 18). Undesirable (toxic) effects may be caused by intravascular injection or administration of large volumes of the drug. Local anesthetic toxicity develops when the blood level of the drug in the brain or myocardium becomes too high. Therefore local anesthetic toxicity relates to the volume of drug reaching the cerebrovascular and cardiovascular systems and to the blood volume of the patient. Once the blood level of a drug reaches toxic levels, the drug exerts unwanted and possibly deleterious systemic actions that are consistent with its pharmacological properties. Local anesthetic toxicity produces central nervous system (CNS) and cardiovascular system (CVS) depression, with reactions ranging from mild tremor to tonic–clonic convulsions (CNS), or from a slight decrease in blood pressure and cardiac output to cardiac arrest (CVS).
Disproportionately high numbers of deaths and serious morbidities caused by local anesthetic overdose have occurred in children, leading to the assumption that local anesthetics are more toxic in children than in adults.19,20 This is untrue; it is the safety margin of local anesthetics in small children that is low. Given an equal dose (mg) of local anesthetic, a healthy adult patient with a larger body weight and greater blood volume will have a lower blood level of anesthetic than the child patient of lesser weight and smaller blood volume. Blood volume, to a large degree, relates to body weight: the greater the body weight, the greater the blood volume (except in cases of marked obesity).
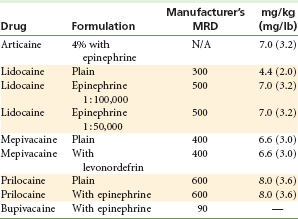
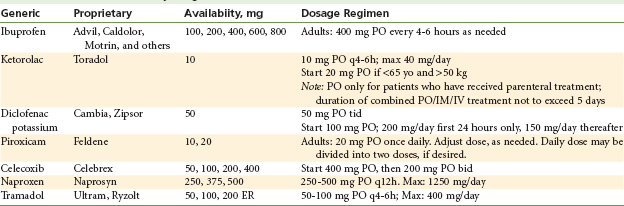
Maximum recommended doses (MRDs) of all drugs administered by injection should be calculated by body weight and should not be exceeded, unless it is absolutely essential to do so.20 For example, two cartridges of 3% mepivacaine (54 mg per cartridge) exceed the MRD for a 15-kg (33-lb) child of 66 mg. Unfortunately, lack of awareness of maximum doses has led to fatalities in children.21–25 The ease with which a lighter-weight child may be overdosed with local anesthetics is compounded by the practice of multiple-quadrant dentistry and the concomitant use of sedative drugs (especially opioids).19 When treating a smaller child, the dentist should maintain strict adherence to MRDs (Table 16-1) and should anesthetize only that quadrant that is currently being treated.
Cheatham and associates surveyed 117 dentists who regularly treated children about their local anesthetic usage.26 They found that the lighter the weight of the patient, the more likely the doctor was to administer an overly large dose of the local anesthetic, based on milligrams per kilogram of body weight. For example, a 13-kg patient should receive no more than 91 mg of lidocaine (based on an MRD of 7.0 mg/kg). The range of doses administered by dentists treating children was 0.9 to 19.3 mg/kg. As the patient’s weight increased, the number of milligrams per pound or kilogram reached lower and safer levels, the maximum mg/kg range falling to 12.6 mg/kg in the 20-kg patient and to 7.2 mg/kg in the 35-kg patient. The mean dose of local anesthetic also fell when the patient’s weight increased, from 5.4 mg/kg in the 13-kg patient to 4.8 mg/kg in the 20-kg patient to 3.8 mg/kg in the 35-kg patient (Table 16-2).
TABLE 16-2
Local Anesthetic Administration by Dentists Who Treat Children (n = 117)
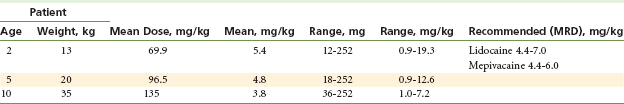
Modified from Cheatham BD, Primosch RE, Courts FJ: A survey of local anesthetic usage in pediatric patients by Florida dentists, J Dent Child 59:401–407, 1992.
Administration of large volumes of local anesthetic is not necessary when one is seeking to achieve pain control in younger patients. Because of differences in anatomy (see the following discussion of “Techniques of Local Anesthesia in Pediatric Dentistry”), smaller volumes of local anesthetics provide the depth and duration of pain control usually necessary to successfully complete planned dental treatment in younger patients.
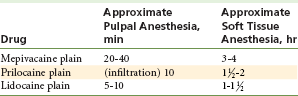
Because all injectable local anesthetics possess vasodilating properties, leading to more rapid vascular uptake and a shorter duration of adequate anesthesia, it is strongly recommended that a vasopressor be included in the local anesthetic solution unless there is a compelling reason for it to be excluded.27 Many treatment appointments in pediatric dentistry do not exceed 30 minutes in duration; therefore use of a local anesthetic containing a vasopressor is considered to be unnecessary and unwarranted. It is thought that increased duration of soft tissue anesthesia, especially after inferior alveolar nerve block, increases the risk of self-inflicted soft tissue injury. A non–vasopressor-containing local anesthetic is frequently used (most often, mepivacaine 3%). Providing 20 to 40 minutes of pulpal anesthesia, mepivacaine 3% is considered the appropriate drug for this group of patients; this is true, provided that treatment is limited to one quadrant per visit. However, when multiple quadrants are to be treated (and anesthetized) on a smaller, lighter-weight patient in a single visit, administration of a “plain” drug into multiple injection sites increases the potential risk of overdose. Use of a local anesthetic containing a vasopressor is strongly recommended whenever multiple quadrants are anesthetized in the smaller pediatric patient. Sixty-nine percent of doctors treating children administered lidocaine with epinephrine as their primary anesthetic (Table 16-3).26
TABLE 16-3
Local Anesthetic Choice by Dentists Who Treat Children (n = 117)
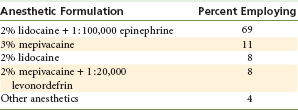
Adapted from Cheatham BD, Primosch RE, Courts FJ: A survey of local anesthetic usage in pediatric patients by Florida dentists, J Dent Child 59:401–407, 1992.
Factors increasing the risk of local anesthetic overdosage in younger patients are presented in Box 16-1.28
Complications of Local Anesthesia
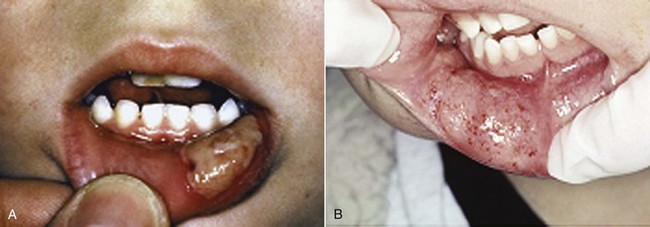
Self-inflicted soft tissue injury—accidental biting or chewing of the lip, tongue, or cheek—is a complication associated with residual soft tissue anesthesia (Fig. 16-4). Soft tissue anesthesia lasts considerably longer than pulpal anesthesia and may persist for 4 or more hours after local anesthetic administration. Fortunately, most patients do not encounter problems related to prolonged soft tissue anesthesia, but most of those who do are younger, oldest old (>85 years), or mentally or physically disabled. Problems related to soft tissue anesthesia most often involve the lower lip. Much less frequently, the tongue is injured, and rarely, the upper lip is involved.
College and associates reported an 18% incidence of self-inflicted soft tissue injury in patients younger than 4 years of age receiving inferior alveolar nerve block.29 From 4 to 7 years, the rate was 16%, from 8 to 11 years, 13%, and from 12 years on, 7%.
Several preventive measures can be implemented:
1. Select a local anesthetic with a duration of action that is appropriate for the length of the planned procedure. Some local anesthetics provide pulpal anesthesia of adequate duration (20 to 40 minutes) for restorative procedures in children, with a relatively short duration of soft tissue anesthesia (1 to 3 hours, instead of 4 or 5) (Table 16-4). It should be kept in mind, however, that investigators have not demonstrated a relationship between the use of plain local anesthetics and a reduction in soft tissue trauma. The clinician must consider the advisability of using a local anesthetic containing a vasopressor when treating multiple quadrants in view of the decreased margin of safety of local anesthetics in smaller children.
2. Administer phentolamine mesylate (Oraverse) at the conclusion of the traumatic portion of the dental procedure. Discussed more completely in Chapter 20, phentolamine mesylate is an alpha-adrenergic antagonist that, when injected into the site where local anesthetic with vasopressor was previously deposited, produces vasodilation, increasing blood flow through the area, thereby increasing the speed with which the local anesthetic drug diffuses out of the nerve. The duration of residual soft tissue anesthesia is significantly reduced. Phentolamine mesylate has been approved by the Food and Drug Administration (FDA) for use in patients 6 years of age and older and weighing more than 15 kg (33 lb).30,31
3. Advise both the patient and the accompanying adult about the possibility of injury if the patient bites, sucks, or chews on the lips, tongue, or cheeks, or ingests hot substances while anesthesia persists.
4. Some doctors reinforce the verbal warning to the patient and the adult by placing a cotton roll in the mucobuccal fold (held in position by dental floss through the teeth) if soft tissue anesthesia is still present at the time of the patient’s discharge. Warning stickers are available to help prevent soft tissue trauma.
Management of self-inflicted soft tissue trauma consists of reassuring the patient, allowing time for anesthetic effects to diminish, and coating the involved area with a lubricant (petroleum jelly) to help prevent drying, cracking, and pain.
Techniques of Local Anesthesia in Pediatric Dentistry
Local anesthetic techniques in children do not differ greatly from those used in adults. However, the skulls of children do have some anatomic differences from those of adults. For instance, maxillary and mandibular bone in children generally is less dense, which works to the dentist’s advantage (Fig. 16-5). Decreased bone density allows more rapid and complete diffusion of the anesthetic solution. Also, children are smaller; thus standard injection techniques usually can be completed with decreased depth of needle penetration.

Figure 16-5 Upper and lower jaws in a 4-year-old child with erupted primary teeth and unerupted permanent teeth. 1, First (central) incisor of primary dentition; 2, second (lateral) incisor of primary dentition; 3, canine of primary dentition; 4, first molar of primary dentition; 5, second molar of primary dentition; 6, first (central) incisor of permanent dentition; 7, second (lateral) incisor of permanent dentition; 8, canine of permanent dentition; 9, first premolar of permanent dentition; 10, second premolar of permanent dentition; 11, first molar of permanent dentition; 12, second molar of permanent dentition. (From Abrahams PH, Marks SC Jr, Hutchings RT: McMinn’s color atlas of human anatomy, ed 5, St Louis, 2003, Mosby.)
Maxillary Anesthesia
All primary teeth and permanent molars can be anesthetized by supraperiosteal infiltration in the mucobuccal fold. The posterior superior alveolar (PSA) nerve block is rarely necessary because of the effectiveness of infiltration in children. However, in some individuals, the morphology of the bone surrounding the apex of the permanent first molar does not permit effective infiltration of local anesthetic, because the zygomatic process lies closer to the alveolar bone in children. A PSA nerve block may be warranted in this clinical situation. A 27-gauge short dental needle should be used and the depth of needle penetration modified to meet the smaller dimensions of the pediatric patient, to minimize the risk of overinsertion leading to hematoma. As an alternative to the PSA, Rood32 has suggested using buccal infiltrations on both the mesial and the distal of the maxillary first molar to avoid a prominent zygomatic process. The anterior superior alveolar (ASA) nerve block also can be used in children, as long as it is realized that the depth of penetration is probably just slightly greater than with a supraperiosteal injection (because of the lower height of the maxillae in children). Generally, there are few indications for the PSA or ASA nerve block in children.
Occasionally, a maxillary tooth remains sensitive after a supraperiosteal injection because of accessory innervation from the palatal nerves33 or widely flared palatal roots. Palatal anesthesia can be attained in children through the nasopalatine and greater (anterior) palatine nerve blocks. The technique for a nasopalatine nerve block proceeds exactly as described in Chapter 13. That for a greater palatine nerve block is as follows: The administrator visualizes a line from the gingival border of the most posterior molar that has erupted to the midline. The needle is inserted from the opposite side of the mouth, distal to the last molar, bisecting this line. If the child has only primary dentition, the needle is inserted approximately 10 mm posterior to the distal surface of the second primary molar, bisecting the line drawn toward the midline.
An intrapapillary injection also can be used to achieve palatal anesthesia in young children. Once buccal anesthesia is effective, the needle (27-gauge short) is inserted horizontally into the buccal papilla just above the interdental septum. Local anesthetic is injected as the needle is advanced toward the palatal side. This should cause ischemia of the soft tissue.34
Mandibular Anesthesia
Supraperiosteal infiltration usually is effective in providing pain control in mandibular primary teeth.35,36 Sharaf reported that buccal infiltration in the mandible in 80 children (ages 3 to 9 years) was as effective as inferior alveolar nerve block (IANB) anesthesia in all situations, except when pulpotomy was performed on the primary second molar.35 This was the result of decreased density of bone in the mandible in younger children. The rate of success of mandibular infiltration anesthesia decreases somewhat for primary mandibular molars as the child increases in age. The technique of supraperiosteal infiltration in the mandible is the same as in the maxilla. The tip of the needle is directed toward the apex of the tooth, in the mucobuccal fold, and approximately one fourth to one third (0.45 to 0.6 mL) cartridge is slowly deposited.
The IANB has a greater success rate in children than in adults because of the location of the mandibular foramen. The mandibular foramen in children lies distal and more inferior to the occlusal plane. Benham37 demonstrated that the mandibular foramen lies at the height of the occlusal plane in children and extends an average of 7.4 mm above the occlusal plane in adults. He also found that there is no age-related difference as to the anteroposterior position of the foramen on the ramus.
The technique for an IANB is essentially identical for adults and children. The syringe barrel is placed in the corner of the mouth on the opposite side. The average depth of penetration to bone is approximately 15 mm, although this may vary significantly with the size of the mandible and the age of the patient. As with the adult, bone should be contacted before any solution is deposited. In general, the more inferior location of the mandibular foramen in children provides a greater opportunity for successful anesthesia. “Too low” injections are more likely to be successful. In clinical situations, the success rate for well-behaved children usually exceeds 90% to 95%.
Because of the decreased thickness of soft tissue overlying the inferior alveolar nerve (about 15 mm), a 25- or 27-gauge short needle may be recommended for the IANB in younger, smaller patients. This should be changed to a long needle once the patient is of sufficient size that a short needle does not reach the injection site without entering tissue almost to its hub.
The buccal nerve may be anesthetized if anesthesia of the buccal tissues in the permanent molar region is necessary. The needle tip is placed distal and buccal to the most posterior tooth in the arch. Approximately 0.3 mL of solution is deposited.
The Vazirani-Akinosi and Gow-Gates mandibular nerve blocks also can be used in children. Akinosi38 advocates the use of short needles with this technique in children. He states that the technique appears less reliable in children, which he relates to the difficulty of judging the depth of penetration necessary in a growing child. The Gow-Gates mandibular block can be used successfully in children.39 However, these injections are rarely necessary in pediatric dentistry because of the effectiveness of mandibular infiltration (when the dentition is composed entirely of primary teeth) and the relative ease with which one can achieve inferior alveolar and incisive nerve block anesthesia.
The incisive nerve block provides pulpal anesthesia to the five primary mandibular teeth in a quadrant. Deposition of anesthetic solution outside the mental foramen with application of finger pressure for 2 minutes provides a very high degree of success. The mental foramen usually is located between the two primary mandibular molars. A volume of 0.45 mL ( of a cartridge) is suggested.
of a cartridge) is suggested.
The PDL injection has been well accepted in pediatric dentistry and can be used as an alternative to supraperiosteal injection. It provides the doctor with the means to achieve anesthesia of proper depth and duration on one tooth, without unwanted residual soft tissue anesthesia. The PDL is also useful when a child has discrete carious lesions in multiple quadrants. See Chapter 15 for a complete discussion of technique for the PDL injection. It is recommended that the described technique be scrupulously adhered to, to avoid physiologic (pain) and psychological (fear) trauma to the patient. The PDL injection is not recommended for use on primary teeth because of the possibility of enamel hypoplasia occurring in the developing permanent tooth.40
Periodontics
Special requirements for local anesthesia in periodontal procedures center on the use of vasopressors to provide hemostasis and the use of long-duration local anesthetics for postoperative pain control. Postsurgical pain management, including the use of long-duration anesthesia, is discussed as a separate subject later in this chapter.
Soft tissue manipulation and surgical procedures are associated with hemorrhage, especially when the tissues involved are not healthy. Administration of local anesthetics without vasopressors proves to be counterproductive because the vasodilating property of the local anesthetic increases bleeding in the region of the injection.41 Vasopressors are added to counteract this undesirable property of local anesthetics.
The pharmacology of vasopressors is more completely discussed in Chapter 3. As a review, vasopressors produce arterial smooth muscle contraction through direct stimulation of α receptors located in the wall of the blood vessel. Consequently, it follows that local anesthetics with vasopressors used for hemostasis must be injected directly into the region where the bleeding is to occur.
Pain control for periodontal procedures should be achieved through nerve block techniques, including posterior superior alveolar, inferior alveolar, and infraorbital nerve blocks. Saadoun18 has shown that the intraseptal technique is very effective for periodontal flap surgical procedures. It decreases the total volume of administered anesthetic and the volume of blood lost during the procedure. Local anesthetic solutions used for nerve blocks should include a vasopressor in a concentration not greater than 1 : 100,000 epinephrine or 1 : 20,000 levonordefrin. An epinephrine concentration of 1 : 50,000 is not recommended for pain control because depth, duration, and success rates are no greater than those seen with anesthetics containing 1 : 100,000 or 1 : 200,000 epinephrine.
Epinephrine is the drug of choice for local hemostasis. Norepinephrine (which is not available in North America in dental local anesthetics) can produce marked tissue ischemia, which can lead to necrosis and sloughing and is not recommended for use in hemostasis.42,43 Epinephrine is most commonly used for hemostasis in a concentration of 1 : 50,000 (0.2 mg/mL). Generally, small volumes (not exceeding 0.1 mL) are deposited when used for hemostasis. Epinephrine also provides excellent hemostasis in a concentration of 1 : 100,000, although surgical bleeding is inversely proportional to the concentration of vasopressor administered. When plain local anesthetic is infiltrated (e.g., 3% mepivacaine) during periodontal surgery, blood loss is two to three times that noted when 2% lidocaine with 1 : 100,000 epinephrine is administered.44 Buckley and associates demonstrated that use of a 1 : 50,000 epinephrine concentration produced a 50% decrease in bleeding during periodontal surgery from that seen with a 1 : 100,000 concentration (with 2% lidocaine).45 However, epinephrine is not a drug without systemic effects and some undesirable local effects. Studies have shown that even the small volumes of epinephrine used in dentistry can significantly increase the concentrations of plasma catecholamine and can alter cardiac function.46 Therefore, it is prudent to administer the smallest volume of the least concentrated form of epinephrine that provides clinically effective hemostasis.
As tissue levels of epinephrine decrease after its injection for hemostasis, a rebound vasodilation develops. Sveen demonstrated that postsurgical bleeding (at 6 hours) occurred in 13 of 16 (81.25%) patients receiving 2% lidocaine with epinephrine for surgical removal of a third molar, whereas 0 of 16 patients who underwent surgery with 3% mepivacaine bled at 6 hours post surgery.44 Bleeding interfered with postoperative healing in 9 of 16 (56.25%) patients receiving lidocaine with epinephrine, compared with 25% of patients receiving no epinephrine. Evidence also suggests that the use of epinephrine in local anesthetics during surgery may produce an increase in postoperative pain.47
Many doctors use a 30-gauge short needle to deposit anesthetics for hemostasis. Their rationale is that the thinner needle produces a smaller defect (puncture) in the tissue. If a small puncture is important, then the 30-gauge needle should be used, but only for this purpose (hemostasis). The 30-gauge short needle should not be used if there is the possibility of positive aspiration of blood, or if any depth of soft tissue must be penetrated. Aspiration of blood through a 30-gauge needle is difficult (although possible). A 27-gauge needle can be used for local infiltration to achieve hemostasis when vascularity is a problem, or in any other area of the oral cavity without an increase in patient discomfort.
Oral and Maxillofacial Surgery
Pain control during surgical procedures is achieved through administration of local anesthetics, given alone or in combination with inhalation sedation, intravenous sedation, or general anesthesia. As is the case with periodontal surgery, long-duration local anesthetics play an important role in postoperative pain control and are discussed separately.
Local anesthetic techniques used in oral surgery do not differ from those employed in nonsurgical procedures. Therefore it should be expected that instances of partial or incomplete anesthesia will occur. Oral and maxillofacial surgeons frequently treat patients who have received intravenous sedation or general anesthesia before the start of surgery. These techniques act to modify the patient’s reaction to pain, leading to a decrease in the number of reported instances of inadequate local anesthesia.
Local anesthesia is administered almost routinely to patients for third molar extractions under general anesthesia. The reasons for this are as follows:
1. General anesthesia does not prevent pain. General anesthesia prevents the patient from responding outwardly to painful stimulation. Blood pressure (BP), heart rate (HR), and respiratory rate (RR) do respond to surgical stimulation (increases in BP, HR, and RR).
2. Pain control through local anesthetic administration during surgery permits lessened exposure to general anesthetic agents, allowing for a faster postanesthetic recovery period and minimizing drug-related complications.
3. Hemostasis is possible if a vasopressor is included.
4. Residual local anesthesia in the postoperative period aids in postsurgical pain control.
The volume of drug and the rate at which it is administered are important in all areas of dental practice, but probably are most important during extraction of teeth from multiple quadrants. When four third molars are extracted, effective pain control must be obtained in all four quadrants. This requires multiple injections of local anesthetics, which usually occur within a relatively short time. Four cartridges or more of local anesthetic are frequently used.* The rate at which these local anesthetics are administered must be closely monitored to lessen the occurrence of complications. Complications arising from rapid administration of local anesthetic include any of the following:
2. Greater possibility of a serious overdose reaction, if the local anesthetic is administered intravascularly (the speed of IV drug administration significantly affects the clinical manifestations of toxicity)
3. Postanesthetic pain caused by tissue trauma during the injection
These complications and their prevention, recognition, and management are discussed in greater detail in Chapters 17 and 18.
It should be noted that in some persons, the inferoposterior border of the mandible is not innervated by the trigeminal nerve. Any of the mandibular nerve blocks described in Chapter 14 provide only partial anesthesia in this situation. The PDL injection usually corrects the lack of pain control in this circumstance.
Fixed Prosthodontics
When preparing a tooth for full coverage (crown or bridge), it is necessary to place a provisional restoration over the prepared tooth. Although achieving pain control might not be difficult at the initial visit, it may be difficult at subsequent visits to adequately anesthetize the prepared tooth. The reason for this is probably the provisional restoration. Overly high restorations produce traumatic occlusion, which can lead to considerable sensitivity after about a day. Poorly adapted gingival margins develop microleakage, also causing sensitivity. Preparation of the tooth itself can cause sensitivity, through desiccation of tooth structure, possible pulpal involvement, and periodontal irritation. The longer these sources of irritation are present, the greater the trauma to the tooth is likely to be, and the more difficult it is to achieve adequate anesthesia. Usually a regional nerve block is effective. Supraperiosteal injections generally do not provide adequate pain control in these situations (depth may be adequate, but duration is considerably shorter than that usually expected from the drug).
Long-Duration Local Anesthesia
Prolonged Dental or Surgical Procedures
Several specialty areas of dental practice require longer than usual pulpal or soft tissue anesthesia. They include fixed prosthodontics, oral surgery, and periodontics. During longer procedures (2 or more hours), an adequate duration of pulpal anesthesia may be difficult to achieve with more commonly used anesthetics such as articaine, lidocaine, mepivacaine, and prilocaine. Bupivacaine is a long-acting local anesthetic that can then be used. It is discussed more completely in Chapter 4.
Bupivacaine, a homolog of mepivacaine, has a long duration of clinical effectiveness when used for regional nerve block. Its duration of action when administered by supraperiosteal injection, although still long, is somewhat shorter (shorter even than that of lidocaine with epinephrine).48 Its postoperative analgesic period lasts an average of 8 hours in the mandible and 5 hours in the maxilla.
Bupivacaine is available with a vasopressor (1 : 200,000 epinephrine). It is interesting to note that the addition of vasopressor to bupivacaine does not prolong its duration of action.49
Postsurgical Management of Pain
Frequently, after extensive surgical procedures, patients experience intense pain when the local anesthetic effect dissipates. It was, and still is in many cases, common practice to treat postoperative pain through the use of opioid analgesics. However, opioids have a high incidence of undesirable side effects such as nausea, vomiting, constipation, respiratory depression, and postural hypotension, especially in ambulatory patients.50 Additionally, opioid analgesics are not very effective in the management of pain following dental surgery.51
Long-acting local anesthetics administered to surgical patients offer a means of providing successful postoperative pain control with minimal risk of developing adverse reactions. An advantage of using long-duration local anesthetics is their longer postoperative analgesia, which leads to a reduced need for the administration of postoperative opioid analgesic drugs.52 Dentists often use an intermediate-acting local anesthetic such as articaine, lidocaine, mepivacaine, or prilocaine with a vasopressor for the surgical procedure, administering a long-acting local anesthetic just before the termination of surgery. Danielsson and associates compared bupivacaine, etidocaine, and lidocaine with regard to their effects on postoperative pain, and found that both bupivacaine and etidocaine were more effective in controlling postoperative pain when compared with lidocaine.48 They also reported that bupivacaine was more effective than etidocaine in providing postoperative analgesia, and that patients receiving bupivacaine used significantly fewer analgesics.
It is pertinent to note that there appears to be a difference between etidocaine and bupivacaine with respect to their ability to provide adequate hemostasis, even though they contain the same concentration of vasopressor (1 : 200,000). Danielsson and associates noted that bupivacaine and lidocaine provided adequate hemostasis in 90% and etidocaine in only 75% of procedures.49 It is possible that a higher concentration of local anesthetic may necessitate a higher concentration of vasopressor to provide comparable hemostasis. Also keep in mind the different vasodilating properties of the solutions.53 Etidocaine HCl is no longer available in dental cartridges in North America.
Protocol for Perioperative and Postoperative Pain Control in Surgical Patients
Postoperative pain associated with most uncomplicated dental surgical procedures is mild and is well managed by oral administration of nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen.51 Preoperative administration of NSAIDs appears to delay the onset of postoperative pain and to lessen its severity.52,54 When a patient is unable to tolerate aspirin or other NSAIDs, acetaminophen can provide acceptable analgesia.
Other dental surgical procedures, such as removal of bony impactions and osseous periodontal or endodontic surgery, are more traumatic and typically are associated with more intense and prolonged postoperative pain. The onset of such pain can be delayed by presurgical administration of an NSAID followed by administration of a long-acting local anesthetic (bupivacaine) at the completion of surgery.54
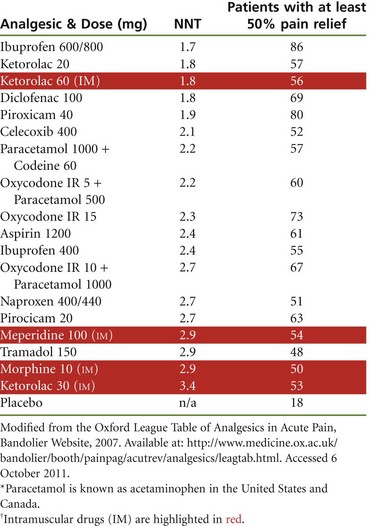
The Oxford League Table of Analgesic Efficacy presents a meta-analysis of randomized, double-blind, single-dose, placebo-controlled studies in patients with moderate to severe postoperative dental, orthopedic, gynecologic, and general surgical pain.51 Analgesic efficacy is expressed as number needed to treat (NNT), the number of patients who need to receive the active drug for one to achieve at least 50% relief of pain compared with placebo over a 4- to 6-hour treatment period.55 The most effective analgesics have an NNT of just over 2 (Table 16-5). Effective pain relief for dental surgery normally can be achieved with oral nonopioid, nonsteroidal anti-inflammatory drugs, coxibs, and combinations of acetaminophen (paracetamol) and codeine.51
As noted in Table 16-5, few, if any, analgesics are better than NSAIDs for acute pain. All NSAIDs on the League table have NNTs of 1.6 to 3.0. Alternative analgesics, such as codeine 60 mg and tramadol 50 mg, have NNTs of 16 and 8, respectively. Parenteral morphine 10 mg and meperidine 100 mg have NNTs of 2.9.51,56 Acetaminophen (paracetamol), administered orally at a dose of 1000 mg, has an NNT of almost 4. When combined with codeine 60 mg, its NNT improves to 2.2. Ibuprofen 400 mg at 2.4 and diclofenac 50 mg and rofecoxib 50 mg at about 2.3 are better. NSAIDs generally do well with lower (better) NNTs.51
For effective postsurgical pain management (i.e., no breakthrough pain), it is important to maintain a therapeutic blood level of the analgesic via time-based dosage administration of the appropriate oral analgesic. A therapeutic dose of the drug (e.g., ibuprofen 600 mg) should be administered every 4 to 6 hours. The drug package insert for ibuprofen states the following regarding its administration for mild to moderate dental pain57:
Despite the statement above regarding larger doses than 400 mg ibuprofen, the Oxford League clearly shows that ibuprofen 600 mg (NNT of 1.7) is more efficacious than ibuprofen 400 mg (NNT of 2.4).
Box 16-2 outlines a recommended protocol for the management of intraoperative and postoperative pain associated with dental surgical procedures.58 Common NSAIDs and their recommended doses are listed in Table 16-6.
Dental Hygiene
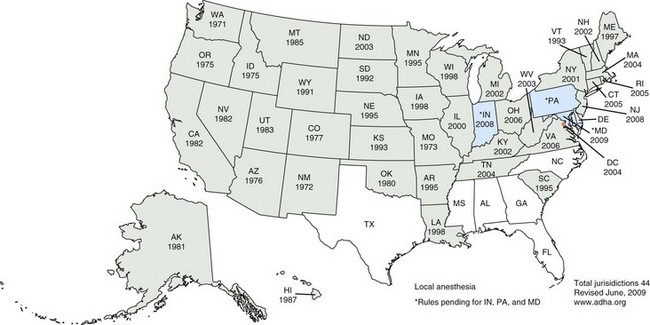
In 1997 when the fourth edition of this textbook was published, registered dental hygienists in 20 states in the United States and several provinces in Canada were permitted to administer local anesthesia to dental patients. This number increased to 32 in 2003 and today (2011) stands at 44 states (Fig. 16-6).59 Inclusion of this expanded function in the Dental Practice Act in these areas has proved of great benefit to the hygienist, doctor, and dental patient.60,61
Though not all patients need local anesthesia for scaling, root planing, and subgingival curettage, many do. The periodontal tissues being treated normally are sensitive to stimuli and are even more so when inflammation is present. Such is frequently the case when a patient is treated by the dental hygienist.
The hygienist who is permitted to administer local anesthetics to dental patients requires the same technique armamentarium as the doctor. Regional block anesthesia, especially in the maxilla (posterior superior or anterior superior alveolar nerve block), is an integral part of the hygienist’s anesthetic armamentarium because hygienists usually treat whole quadrants during a single appointment. The hygiene patient requires the same depth of anesthesia as is attained by the doctor doing restorative dentistry or surgery. Root planing without discomfort requires pulpal anesthesia, along with soft tissue and osseous anesthesia.60 More than 70% of respondents to a survey on dental hygiene patients’ need for pain control reported that their patients needed anesthesia but did not receive it.61
Feedback from dentists whose hygienists administer local anesthesia has been uniformly positive; negative comments have been extremely rare.62 Dental patients themselves are aware of the difference between local anesthesia administered by the dental hygienist and that administered by the dentist. They frequently comment on the lack of discomfort when the hygienist injects the local anesthetic. Be it a slower rate of administration, greater attention to the details of atraumatic injection technique, or greater empathy, it works.
References
1. Brown, RD. The failure of local anaesthesia in acute inflammation. Br Dent J. 1981;151:47–51.
2. Vandermeulen, E. Pain perception, mechanisms of action of local anesthetics and possible causes of failure. Rev Belge Medecine Dent. 2000;55:19–40.
3. Kitay, D, Ferraro, N, Sonis, ST. Lateral pharyngeal space abscess as a consequence of regional anesthesia. J Am Dent Assoc. 1991;122:56–59.
4. Connor, JP, Edelson, JG. Needle tract infection: a case report. Oral Surg. 1988;65:401–403.
5. Malamed SF: Buffering local aesthetics in dentistry, ADSA Pulse. In press.
6. Personal communication, Onpharma Inc., February 2011.
7. Coggins, R, Reader, A, Nist, R, et al. Anesthetic efficacy of the intraosseous injection in maxillary and mandibular teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont. 1996;81:634–641.
8. Reisman, D, Reader, A, Nist, R, et al. Anesthetic efficacy of the supplemental intraosseous injection of 3% mepivacaine in irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont. 1997;84:676–682.
9. Leonard, M. The efficacy of an intraosseous injection system of delivering local anesthetic. J Am Dent Assoc. 1995;126:11–86.
10. Coury, KA. Achieving profound anesthesia using the intraosseous technique. Tex Dent J. 1997;114:34–39.
11. Nusstein, J, Reader, A, Nist, R, et al. Anesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100,000 epinephrine in irreversible pulpitis. J Endodont. 1998;24:478–491.
12. Quinn, CL. Injection techniques to anesthetize the difficult tooth. J Calif Dent Assoc. 1998;26:665–667.
13. Parente, SA, Anderson, RW, Herman, WW, et al. Anesthetic efficacy of the supplemental intraosseous injection for teeth with irreversible pulpitis. J Endodont. 1998;24:826–828.
14. Brown, R. Intraosseous anesthesia: a review. J Calif Dent Assoc. 1999;27:785–792.
15. Weathers, AJr. Taking the mystery out of endodontics. Part 6. Painless anesthesia for the “hot” tooth. Dent Today. 1999;18:90–93.
16. Stabile, P, Reader, A, Gallatin, E, et al. Anesthetic efficacy and heart rate effects of the intraosseous injection of 1.5% etidocaine (1:200,000 epinephrine) after an inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont. 2000;89:407–411.
17. Replogle, K, Reader, A, Nist, R, et al. Cardiovascular effects of intraosseous injections of 2% lidocaine with 1:100,000 epinephrine and 3% mepivacaine. J Am Dent Assoc. 1999;130:549–657.
18. Saadoun, AP, Malamed, SF. Intraseptal anesthesia in periodontal surgery. J Am Dent Assoc. 1985;111:249–256.
19. Goodsen, JM, Moore, PA. Life-threatening reactions after pedodontic sedation: an assessment of narcotic, local anesthetic, and antiemetic drug interaction. J Am Dent Assoc. 1983;107:239–245.
20. Moore, PA. Preventing local anesthesia toxicity. J Am Dent Assoc. 1992;123:60–64.
21. Berquist, HC. The danger of mepivacaine 3% toxicity in children. Can Dent Assoc J. 1975;3:13.
22. Malamed, SF. Morbidity, mortality and local anesthesia. Prim Dent Care. 1999;6:11–15.
23. American Academy on Pediatric Dentistry Council on Clinical Affairs. Guideline on appropriate use of local anesthesia for pediatric dental patients. Pediatr Dent. 2008-2009;30(Suppl 7):134–139.
24. Meechan, JG, Rood, JP. Adverse effects of dental local anaesthesia. Dent Update. 1997;24:315–318.
25. Davis, MJ, Vogel, LD. Local anesthetic safety in pediatric patients. N Y State Dent J. 1996;62:22–35.
26. Cheatham, BD, Primosch, RE, Courts, FJ. A survey of local anesthetic usage in pediatric patients by Florida dentists. J Dent Child. 1992;59:401–407.
27. Yagiela, JA. Regional anesthesia for dental procedures. Int Anesthesiol Clin. 1989;27:28–82.
28. Malamed, SF. Allergic and toxic reactions to local anesthetics. Dent Today. April 2003;22:114–121.
29. College, C, Feigal, R, Wandera, A, et al. Bilateral versus unilateral mandibular block anesthesia in a pediatric population. Pediatr Dent. 2000;22:453–457.
30. FDA approves OraVerse. Available at www.drugs.com. [Accessed February 7, 2011].
31. Tavares, M, Goodson, JM, Studen-Pavlovich, D, et al. Reversal of soft tissue anesthesia with phentolamine mesylate in pediatric patients. The Local Anesthetic Reversal Group. J Am Dent Assoc. 2008;139:1095–1104.
32. Rood, JP. Notes on local analgesia for the child patient. Dent Update. 1981;8:377–381.
33. Kaufman, L, Sowray, JH, Rood, JP. General anaesthesia, local analgesia, and sedation in dentistry. Oxford, UK: Blackwell Scientific; 1982.
34. O’Sullivan, VR, Holland, T, O’Mullane, DM, et al. A review of current local anaesthetic techniques in dentistry for children. J Irish Dent Assoc. 1986;32:17–27.
35. Sharaf, AA. Evaluation of mandibular infiltration versus block anesthesia in pediatric dentistry. ASDC J Dent Child. 1997;64:276–281.
36. Oulis, CJ, Vadiakis, GP, Vasilopoulou, A. The effectiveness of mandibular infiltration compared to mandibular block anesthesia in treating primary molars in children. Pediatr Dent. 1996;18:301–305.
37. Benham, NR. The cephalometric position of the mandibular foramen with age. J Dent Child. 1976;43:233–237.
38. Akinosi, JO. A new approach to the mandibular nerve block. Br J Oral Surg. 1977;15:83–87.
39. Yamada, A, Jastak, JT. Clinical evaluation of the Gow-Gates block in children. Anesth Prog. 1981;28:106–109.
40. Brannstrom, M, Lindskog, S, Nordenvall, KJ. Enamel hypoplasia in permanent teeth induced by periodontal ligament anesthesia of primary teeth. J Am Dent Assoc. 1984;109:535–736.
41. Davenport, RE, Porcelli, RJ, Iacono, VJ, et al. Effects of anesthetics containing epinephrine on catecholamine levels during periodontal surgery. J Periodontol. 1990;61:553–558.
42. van der Bijl, P, Victor, AM. Adverse reactions associated with norepinephrine in dental local anesthesia. Anesth Prog. 1992;39:37–89.
43. Jakob, W. Local anaesthesia and vasoconstrictive additional components. Newslett Int Fed Dent Anesthesiol Soc. 1989;2:1.
44. Sveen, K. Effect of the addition of a vasoconstrictor to local anesthetic solution on operative and postoperative bleeding, analgesia and wound healing. Int J Oral Surg. 1979;8:301–306.
45. Buckley, JA, Ciancio, SG, McMullen, JA. Efficacy of epinephrine concentration in local anesthesia during periodontal surgery. J Periodontol. 1984;55:653–657.
46. Jastak, JT, Yagiela, JA. Vasoconstrictors and local anesthesia; a review and rationale for use. J Am Dent Assoc. 1983;107:623–630.
47. Skoglund, LA, Jorkjend, L. Postoperative pain experience after gingivectomies using different combinations of local anaesthetic agents and periodontal dressings. J Clin Periodontol. 1991;18:204–209.
48. Danielsson, K, Evers, H, Nordenram, A. Long-acting local anesthetics in oral surgery: an experimental evaluation of bupivacaine and etidocaine for oral infiltration anesthesia. Anesth Prog. 1985;32:65–68.
49. Danielsson, K, Evers, H, Holmlund, A, et al. Long-acting local anaesthetics in oral surgery. Int J Oral Maxillofac Surg. 1986;15:119–126.
50. , Goodman & Gilman’s the pharmacological basis of therapeutics. Hardman, JG, Limbird, LE, eds.. ed 10. McGraw-Hill: New York, 2001.
51. The Oxford League Table of Analgesics in Acute Pain, Bandolier Website, 2007. Available at http://www.medicine.ox.ac.uk/bandolier/booth/painpag/Acutrev/Analgesics/Leagtab.html. [Accessed October 6, 2011].
52. Jackson, DL, Moore, PA, Hargreaves, KM. Pre-operative nonsteroidal anti-inflammatory medication for the prevention of postoperative dental pain. J Am Dent Assoc. 1989;119:641–647.
53. Linden, ET, Abrams, H, Matheny, J, et al. A comparison of postoperative pain experience following periodontal surgery using two local anesthetic agents. J Periodontol. 1986;57:637–642.
54. Acute Pain Management Guideline Panel: Acute pain management: operative or medical procedures and trauma. Clinical practice guideline, AHCPR Pub. No. 92-0032, Rockville, Md, 1992, Agency for Health Care Policy and Research, Public Health Service, U.S. Department of Health and Human Services.
55. Cook, RJ, Sackett, DL. The number needed to treat: a clinically useful measure of treatment effect. BMJ. 1995;310:452–454.
56. Ong, CKS, Lirk, P, Tan, CH, et al. An evidence-based update on nonsteroidal anti-inflammatory drugs. Clin Med Res. 2007;5:19–34.
57. Ibuprofen monograph. Indications—Dosage. Available at www.mdconsult.com. [Updated August 16, 2010. Accessed October 6, 2011].
58. Malamed, SF. Local anesthetics: dentistry’s most important drugs. J Am Dent Assoc. 1994;125:1571–1576.
59. American Dental Hygienists Association. Available at www.adha.org. [January 2011. Accessed October 6, 2011].
60. Sisty-LePeau, N, Boyer, EM, Lutjen, D. Dental hygiene licensure specifications on pain control procedures. J Dent Hyg. 1990;64:179–185.
61. Sisty-LePeau, N, Nielson-Thompson, N, Lutjen, D. Use, need and desire for pain control procedures by Iowa hygienists. J Dent Hyg. 1992;66:137–146.
62. DeAngelis, S, Goral, V. Utilization of local anesthesia by Arkansas dental hygienists, and dentists’ delegation/satisfaction relative to this function. J Dent Hyg. 2000;74:196–204.
*Typical local anesthetic injections for extraction of four third molars include the following:
1. Right and left inferior alveolar nerve blocks, 1.8 mL each (3.6 mL)
2. Right and left posterior superior alveolar nerve blocks or supraperiosteal infiltration over each third molar, 1.3 to 1.8 mL each (2.6 to 3.6 mL)
3. Right and left palatal infiltration over the maxillary third molars, 0.45 mL each, or right and left greater palatine nerve block, 0.45 mL each (0.09 mL)
Total volume of local anesthetic: 8.1 mL or 162 mg or a 2% solution, 243 mg of a 3%, or 324 mg of a 4%.