The Needle
Types
The needle is the vehicle that permits local anesthetic solution to travel from the dental cartridge into the tissues surrounding the needle tip. Most needles used in dentistry are stainless steel and disposable. Needles manufactured for dental intraoral injections are presterilized and disposable.
Reusable needles should not be used for injections.
Because the needle represents the most dangerous component of the armamentarium, the one most likely to produce injury to patient or doctor, safety needles are being developed.1,2 Although these needles are not yet used to any appreciable degree in dentistry in the United States, it is likely that at some point in the not too distant future their use will become commonplace, if not mandatory.
Anatomy of A Needle
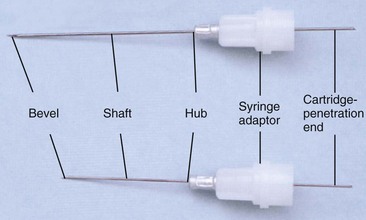
The needle is composed of a single piece of tubular metal around which is placed a plastic or metal syringe adaptor and the needle hub (Fig. 6-1).
All needles have the following components in common: the bevel, the shaft, the hub, and the cartridge-penetrating end (Fig. 6-2).
The bevel defines the point or tip of the needle. Bevels are described by manufacturers as long, medium, and short. Several authors have confirmed that the greater the angle of the bevel with the long axis of the needle, the greater will be the degree of deflection as the needle passes through hydrocolloid (or the soft tissues of the mouth) (Fig. 6-3).3-6 A needle whose point is centered on the long axis (e.g., the Huber point, the Truject needle; Fig. 6-4, A) will deflect to a lesser extent than a beveled-point needle, whose point is eccentric (Fig. 6-4, B) (Table 6-1).
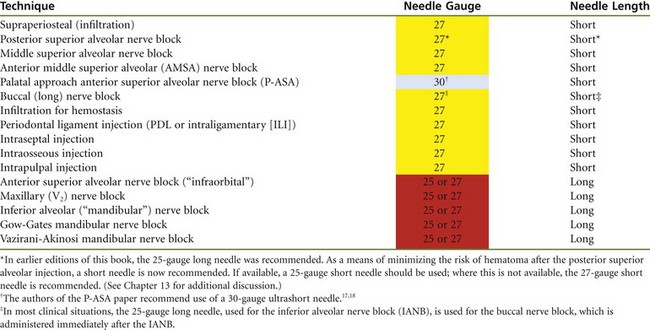
TABLE 6-1
Deflection of Needles Inserted in Hydrocolloid Tubes to Their Hubs
| Length (mm, Tip to Hub) |
Maximum Tip Deflection (mm, ± SD) |
|
| 25-Gauge long (conventional) | 35 | 7.1 ± 0.81* |
| 27-Gauge long (conventional) | 36 | 8.4 ± 1.2* |
| 27-Gauge short (conventional) | 26 | 4.6 ± 0.97† |
| 28-Gauge long (nondeflecting) | 31 | 1.1 ± 0.82 |
| 28-Gauge short (nondeflecting) | 22 | 0.8 ± 0.91 |
*A statistically significant difference from the nondeflecting long needle (P < .01); n = 10 needles in each group.
†A statistically significant difference from the nondeflecting short needle (P < .01); n = 10 needles in each group.
Data modified from Jeske AH, Boshart BF: Deflection of conventional versus non-deflecting dental needles in vitro, Anesth Prog 32:62-64, 1985.

Figure 6-3 Radiograph demonstrating varying degrees of needle deflection with different gauges (left to right, 30-, 27-, and 25-). (From Robison SF, Mayhew RB, Cowan RD, et al: Comparative study of deflection characteristics and fragility of 25-, 27-, and 30-gauge short dental needles, J Am Dent Assoc 109:920-924, 1984.)
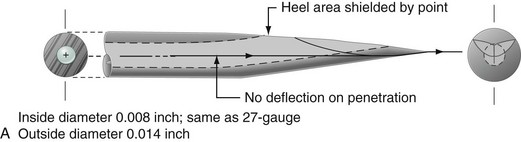
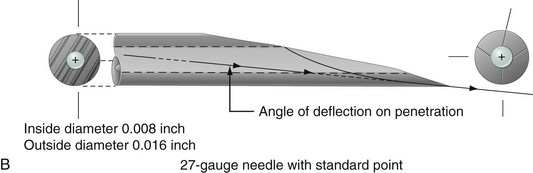
Figure 6-4 A, The tip of a nondeflecting needle is located in the center of the shaft, thereby minimizing deflection as the needle penetrates soft tissues. B, Conventional dental needle. The needle tip lies at the lower edge of the needle shaft, thereby producing deflection as the needle passes through soft tissue.
Several manufacturers of dental needles have placed indicators on the plastic or metal hub to help orient the doctor to the position of the bevel during needle insertion and injection of the drug.
The shaft of the needle is one long piece of tubular metal running from the tip of the needle through the hub, and continuing to the piece that penetrates the cartridge (see Fig. 6-1). Two factors to be considered about this component of the needle are the diameter of its lumen (e.g., the needle gauge) and the length of the shaft from point to hub.
The hub is a plastic or metal piece through which the needle attaches to the syringe. The interior surface of metal-hubbed needles is prethreaded, as are most but not all plastic-hubbed needles.
The cartridge-penetrating end of the dental needle extends through the needle adaptor and perforates the diaphragm of the local anesthetic cartridge. Its blunt end rests within the cartridge.
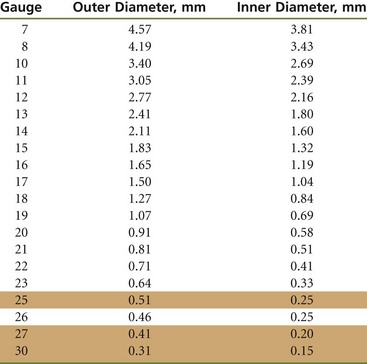
When needles are selected for use in various injection techniques, two factors that must be considered are gauge and length.
Gauge
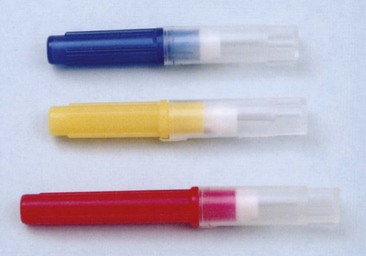
Gauge refers to the diameter of the lumen of the needle: the smaller the number, the greater the diameter of the lumen. A 30-gauge needle has a smaller internal diameter than a 25-gauge needle. In the United States, needles are color-coded by gauge (Fig. 6-5).
There is a growing trend toward the use of smaller-diameter (higher-number gauge) needles, based on the assumption that they are less traumatic to the patient than needles with larger diameters (Table 6-2). This assumption is unwarranted.7 Hamburg8 demonstrated as far back as 1972 that patients cannot differentiate among 23-, 25-, 27-, and 30-gauge needles. Others have confirmed this finding.9,10 A clinical experiment demonstrates this point:
TABLE 6-2
Needle Purchases, U.S. Dentistry, 2006
From Malamed SF, Reed KL, Poorsattar S: Needle breakage: incidence and prevention, Dent Clin North Am 54:745-756, 2010.
1. Three needles—25-, 27-, and 30-gauge—are selected.
2. The buccal mucosa over the maxillary anterior teeth should be dried.
3. No topical anesthetic should be used.
5. The mucosa should be gently penetrated (about 2 to 3 mm) with each of the three needles without revealing to the patient which needle is being used. A different site should be selected for each penetration.
6. Question the patient about his or her “feelings”: Which one was felt the most? Which one the least?
In literally hundreds of clinical demonstrations, no patient was able to correctly determine the gauge of each needle. The usual response has been that he or she could not discern any difference.
Larger-gauge needles (e.g., 25-gauge, 27-gauge) have distinct advantages over smaller ones (30-gauge) (Box 6-1): less deflection occurs as the needle passes through tissues (see Table 6-1 and Fig. 6-3). This leads to greater accuracy during needle insertion (it goes in a straighter line) and, it is hoped, to increased success rates, especially for techniques in which the depth of soft tissue penetrated is significant (e.g., inferior alveolar, Gow-Gates mandibular, Akinosi-Vazirani mandibular, anterior superior alveolar [ASA; infraorbital] nerve blocks). Needle breakage, although rare today with the use of disposable needles, is even less likely to occur with a larger needle. Numerous authors11-14 have demonstrated that aspiration of blood is easier and more reliable through a larger lumen. Foldes and McNall11 reported the following findings based on an unpublished study by Monheim:
1. One hundred percent positive aspirations were achieved from blood vessels with 25-gauge needles.
2. Eighty-seven percent positive aspirations were achieved from blood vessels with 27-gauge needles.
3. Two percent positive aspirations were achieved from blood vessels with 30-gauge needles.
Trapp and Davies15 reported that in vivo human blood may be aspirated through 23-, 25-, 27-, and 30-gauge needles without a clinically significant difference in resistance to flow.
Despite this ambiguity concerning ability to aspirate blood through needles of various gauges, the use of larger needles (e.g., 25-gauge, 27-gauge) is recommended for any injection technique used in a highly vascular area, or when needle deflection through soft tissue would be a factor. Although blood may be aspirated through all 23- through 30-gauge needles, resistance to aspiration is greater when smaller-gauge needles are used, increasing the likelihood that the metal harpoon will become dislodged from the rubber plunger during aspiration, making the aspiration attempt futile.
Industry standards for needle gauge have been in place for years (Table 6-3); however, variations in internal diameter do exist between needle manufacturers. Larger-gauge needles (e.g., 25-gauge, 27-gauge) should be used when the risk of positive aspiration is increased, as during an inferior alveolar, posterior superior alveolar, or mental or incisive nerve block.
The most commonly used (e.g., most often purchased) needles in dentistry are the 30-gauge short and the 27-gauge long.16 The 25-gauge (long or short) remains the preferred needle for all injections presenting a high risk of positive aspiration. The 27-gauge can be used for all other injection techniques, provided the aspiration percentage is low and tissue penetration depth is not great (increased deflection with this thinner needle). The 30-gauge needle is not specifically recommended for any injection, although it may be used in instances of localized infiltration, as when hemostasis is attained during periodontal therapy.
Deflection of the needle is a consideration when a needle must penetrate a greater thickness of soft tissue. On the standard dental needle (see Fig. 6-4, B), the tip of the point is located eccentrically. As the needle shaft penetrates soft tissue, the point of the needle is deflected by the tissue through which it passes. The greater the angle of the bevel, the greater is the degree of needle deflection. Every decade or so, a needle is introduced on which the tip of the point is located in the center of the lumen, thereby minimizing deflection as the needle passes through soft tissue (see Fig. 6-4, A). Jeske and Boshart4 demonstrated the effectiveness of this “nondeflecting” needle (see Table 6-1). However, it needs to be demonstrated clinically that a lesser degree of needle deflection occurring as the needle passes through soft tissues actually results in an increased rate of successful anesthesia compared with that observed with standard needles. Over years of use, dentists become accustomed to the deflecting needles they use and gradually modify their injection techniques to accommodate this deflection (they “learn” to make the injections work even with deflection). Changing to a nondeflecting needle might initially lead to lower success rates.
Minimizing Needle Deflection: Bi-Rotational Insertion Technique (BRIT)
A new approach to reducing needle deflection has been described.17 Rotational insertion (described as bi-rotational insertion technique [BRIT]), a technique in which the operator rotates the handpiece or needle in a back-and-forth rotational movement while advancing the needle through soft tissue, is similar to techniques used for acupuncture or endodontic instrumentation. Hochman and Friedman demonstrated that needle deflection could be virtually eliminated by using a rotational insertion technique during needle advancement.17 An in-vitro study of 60 needle insertions into a tissue-like medium was performed with needles of three different gauges to compare rotational insertion versus the traditional linear nonrotating insertion technique. Investigators demonstrated that deflectional bending of a needle could be minimized or eliminated, regardless of the length or gauge of a needle, as long as the insertion was performed using the bi-rotational insertion technique.
Deflection of a needle is a consequence of resultant forces acting on the needle bevel during tissue penetration and advancement. An eccentric pointed beveled needle generates several different forces that act on it during insertion when a nonrotating linear insertion technique is used. A linear insertion technique is the conventional technique used with the traditional dental syringe, which is typically held with a palm-thumb grasp (Fig. 6-6). During this type of insertion, a force perpendicular to the forward directional movement (vector) acts on the surface of the beveled needle, causing the needle to bend (or deflect) in a direction opposite to which the bevel faces (e.g., if the bevel faces “up,” the advancing movement causes a beveled needle to deflect “downward”). The longer the needle length, the more exaggerated the bending or deflection becomes as a result of the greater distance traveled along the deflecting path. The smaller the diameter of the needle, the more exaggerated the bending or deflection, because a smaller-gauge needle is less capable of resisting the deflection or bending force on the surface of the beveled needle tip.
When the BRIT is used during needle insertion, the perpendicular force that causes deflection is eliminated or “neutralized” from the constant changing of bevel orientation as it is rotated (Fig. 6-7).17 This allows eccentrically beveled needles to travel in a straight path. The traditional handheld syringe requires a palm-thumb grasp (see Fig. 6-6) that does not permit such a technique. A computer-controlled local anesthetic delivery (C-CLAD) device such as The Wand/CompuDent/STA (Milestone Scientific Inc., Livingston, NJ; discussed in Chapter 5) employs a lightweight handpiece that is held with a “penlike” or “dart” grasp that is easily rotated.
A subsequent study by the same authors demonstrated that the BRIT offers the added benefit of reducing the force necessary for needle penetration and advancement through tissues.18 This is explained as follows. With rotational insertion, all resultant forces are directed toward the forward path of insertion because the deflecting or bending forces have been eliminated from the rotational insertion technique, as described earlier. This allows forward movement of the needle to occur more efficiently and with less effort (e.g., less force). In addition, rotation of the beveled needle allows the sharp cutting edge to contact the full circumference of the tissue surface, contributing to the reduction in force that is necessary during penetration and advancement. This is not unlike the rotational effect that a surgical drill bit has as it is boring through tissue or bone.
The BRIT, or bi-rotational insertion technique has been demonstrated to improve injection techniques because the deflection of a standard needle during insertion is minimized.19
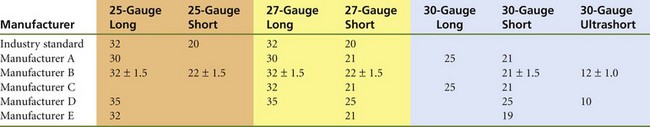
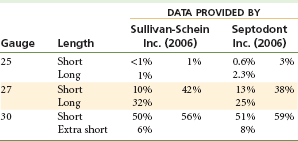
Length
Dental needles are available in three lengths: long, short and ultrashort. Ultrashort needles are available only as 30-gauge needles. Despite the claim for uniformity of length by manufacturers, significant differences are found (Table 6-4).
The length of a short needle is between 20 and 25 mm (measured hub to tip) with a standard of about 20 mm, and is 30 to 35 mm for the long dental needle, with a standard of about 32 mm (Fig. 6-8).
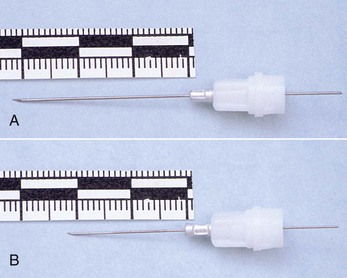
Figure 6-8 A, Long dental needle: length approximately 32 mm. B, Short dental needle: length approximately 20 mm.
Needles should not be inserted into tissues all the way to their hubs unless this is absolutely necessary for the success of the injection. This statement has appeared in “standard” local anesthesia textbooks since the early to mid 1900s.20-24 One reason for this precaution is needle breakage, which, although rare, does occur. The weakest portion of the needle (the most rigid, the part receiving the greatest stress during needle advancement through tissues) is at the hub, which is where needle breakage happens. When a needle that is inserted into the soft tissues to its hub breaks, the elastic properties of the tissues permit them to rebound and cover (bury) the needle remnant entirely. Retrieval is usually difficult (as discussed in Chapter 17). If even a small portion (5 mm or more) of the broken needle shaft remains visible within the oral cavity, it can usually be retrieved easily with a hemostat or pickup forceps.
A long needle is preferred for all injection techniques for which penetration of significant thicknesses of soft tissue (e.g., inferior alveolar, Gow-Gates mandibular, Akinosi mandibular, infraorbital, maxillary [V2] nerve blocks) is required. Short needles may be used for any injection in any patient who does not require penetration of significant depths of soft tissue (e.g., close to or beyond 20 mm).
Care And Handling of Needles
Needles available to the dental profession today are presterilized and disposable. With proper care and handling, they should not be the cause of significant difficulties.
1. Needles must never be used on more than one patient.
2. Needles should be changed after several (three or four) tissue penetrations in the same patient.
a. After three or four insertions, stainless steel disposable needles become dulled. Tissue penetration becomes increasingly traumatic with each insertion, producing pain on insertion and soreness when sensation returns after the procedure.
3. Needles should be covered with a protective sheath when not being used to prevent accidental needle-stick with a contaminated needle. (See the discussion in Chapter 9.)
4. Attention should always be paid to the position of the uncovered needle tip, whether inside or outside the patient’s mouth. This minimizes the risk of potential injury to the patient and the administrator.
5. Needles must be properly disposed of after use to prevent possible injury or reuse by unauthorized individuals. Needles can be destroyed in any of the following ways:
a. Contaminated needles (as well as all other items contaminated with blood or saliva, such as cartridges) should be disposed of in special “contaminated” or “sharps” containers (Fig. 6-9).
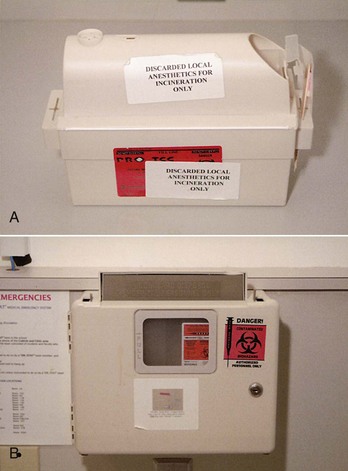
Figure 6-9 A, Container for disposal of discarded local anesthetic cartridges. B, “Sharps” container for disposal of contaminated needles.
b. Proper use of a self-sheathing (“safety” needle) needle or syringe unit (as discussed in Chapter 5) minimizes risk of accidental needle-stick.
c. When needles are to be reused for subsequent injections (a practice unique to the dental profession vs. medicine or other health care professions, where second injections are rarely administered), recapping is accomplished using the “scoop” technique or a needle holder (Fig. 6-10).
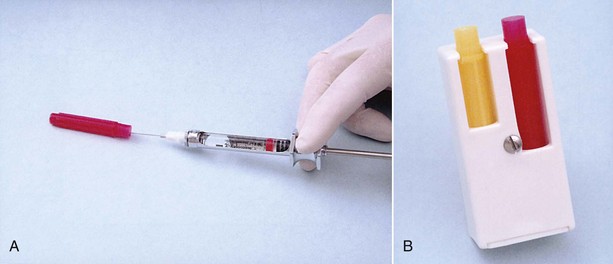
Figure 6-10 A, “Scoop” technique for recapping contaminated local anesthetic needle. B, Plastic needle cap holder.
d. Contaminated needles should never be discarded into open trash containers.
In summary, in actual fact, only one local anesthetic needle is necessary in the dental office, the 25-gauge long, which can be used for all anesthetic techniques discussed in this text. It provides a rigidity that is not available with higher-gauge (smaller-diameter) needles and is necessary in the periodontal ligament (PDL) and for intraseptal injections; it deflects to a lesser degree than smaller needles and seemingly provides easier and more reliable aspiration. Because patient sensitivity is not increased with the 25-gauge long needle, its value is increased still further. In reality, however, it is practical to have a second needle available—the 25- or 27-gauge short needle—for use in injections in which the thickness of soft tissue to be penetrated is less than 20 mm, and where the risk of positive aspiration is minimal, as well as in areas of the oral cavity where stabilization of a long needle might prove difficult (e.g., maxillary anterior teeth, the palate).
Problems With Needles
Use of a dull needle can lead to pain on initial penetration of the mucosa. This pain may be prevented by using sharp, new, disposable needles and applying a topical anesthetic at the penetration site. The needle should be changed after three or four penetrations of mucosa if multiple insertions are necessary.
Breakage
Bending weakens needles, making them more likely to break on subsequent contact with hard tissues such as bone. Needles should not be bent if they are to be inserted into soft tissue to a depth greater than 5 mm. No injection technique used in dentistry (in which the needle enters into soft tissue) requires a needle to be bent for success of the injection. Most often, needles are bent by doctors administering an inferior alveolar nerve block (IANB), a posterior superior alveolar (PSA) nerve block, an intrapulpal injection, an injection into the PDL, or an intraosseous injection. The two nerve blocks mentioned (IANB, PSA) can be easily administered successfully with a straight (unbent) needle (see Chapters 13 and 14). The PDL and intrapulpal injections usually can be administered without bending the needle; however, occasions arise, such as at the distal root of a mandibular second molar (PDL), with root canals in posterior teeth (intrapulpal), or with injection into bone distal to a second molar (intraosseous), in which the injection site is not accessible with a straight needle. In these cases, bending of the needle is essential to success. Because the needle does not enter into soft tissue farther than 2 to 4 mm (PDL), or at all (intrapulpal), there is little danger of the needle being nonretrievable in the unlikely event that it breaks (Figs. 6-11 and 6-12).

Figure 6-12 Remainder of retained local anesthetic needle shown in Figure 6-11.
No attempt should be made to change the direction of a needle when it is embedded in tissue. If the direction of a needle must be changed, the needle should first be withdrawn almost completely from the tissue and then its direction altered.
No attempts should be made to force a needle against resistance (needles are not designed to penetrate bone). Smaller (30- and 27-gauge) needles are more likely to break than larger (25-gauge) needles. Of 105 broken needle cases this author has examined, 100 involved a 30-gauge short or ultrashort needle (95.23%). The remaining five needles were 27-gauge short.99
Needles recommended for specific injection techniques are presented in the following “Recommendations” section.
Pain on Withdrawal
Pain on withdrawal of the needle from tissue can be produced by “fishhook” barbs on the tip. Fishhook barbs may be produced during the manufacturing process, but it is much more likely that they will develop when the needle tip forcefully contacts a hard surface, such as bone. A needle should never be forced against resistance. If in doubt about the presence of barbs, change the needle between insertions.
Injury to the Patient or Administrator
Penetration of, with resultant injury to, areas of the body with the needle can occur unintentionally. A major cause is inattention by the administrator, although sudden unexpected movement by the patient is also a frequent cause. The needle should remain capped until it is to be used and should be made safe (sheathed or recapped) immediately after withdrawal from the mouth.
Recommendations
1. Sterile disposable needles should be used.
2. If multiple injections are to be administered, needles should be changed after three or four insertions in a single patient.
3. Needles must never be used on more than one patient.
4. Needles should not be inserted into tissue to their hub unless this is absolutely necessary for success of the injection.
5. The direction of a needle should not be changed while it is still in tissue.
6. A needle should never be forced against resistance.
7. Needles should remain capped until used and should be made safe immediately when withdrawn.
8. Needles should be discarded and destroyed after use to prevent injury or reuse by unauthorized persons.
9. The injection techniques presented in Table 6-5 are listed with their recommended needles (for the adult of average size).
References
1. Cuny, EJ, Fredekind, R, Budenz, AW. Safety needles: new requirements of the Occupational Safety and Health Administration bloodborne pathogens rule. J Calif Dent Assoc. 1999;27:525–530.
2. Cuny, E, Fredekind, RE, Budenz, AW. Dental sefety needles “effectiveness”: results of a one-year evaluation. J Am Dent Assoc. 2000;131:1143–1148.
3. Aldous, JA. Needle deflection: a factor in the administration of local anesthetics. J Am Dent Assoc. 1968;77:602–604.
4. Jeske, AH, Boshart, BF. Deflection of conventional versus non-deflecting dental needles in vitro. Anesth Prog. 1985;32:62–64.
5. Robison, SF, Mayhew, RB, Cowan, RD, et al. Comparative study of deflection characteristics and fragility of 25-, 27-, and 30-gauge short dental needles. J Am Dent Assoc. 1984;109:920–924.
6. Delgado-Molina, E, Tamarit-Borras, M, Berini-Aytes, L, et al. Comparative study of two needle models in terms of deflection during inferior alveolar nerve block. Med Oral Patol Oral Cir Bucal. 2009;14:440–444.
7. Jeske, AH, Blanton, PL. Misconceptions involving dental local anesthesia. Part 2. Pharmacology. Tex Dent J. 2002;119:310–314.
8. Hamburg, HL. Preliminary study of patient reaction to needle gauge. NY State Dent J. 1972;38:425–426.
9. Farsakian, LR, Weine, FS. The significance of needle gauge in dental injections. Compendium. 1991;12:264–268.
10. Flanagan, T, Wahl, MI, Schmitt, MM, et al. Size doesn’t matter: needle gauge and injection pain. Gen Dent. 2007;55:216–217.
11. Foldes, FF, McNall, PG. Toxicity of local anesthetics in man. Dent Clin North Am. 1961;5:257–258.
12. Harris, S. Aspirations before injection of dental local anesthetics. J Oral Surg. 1957;25:299–303.
13. Kramer, H, Mitton, V. Dental emergencies. Dent Clin North Am. 1973;17:443–460.
14. McClure, DB. Local anesthesia for the preschool child. J Dent Child. 1968;35:441–448.
15. Trapp, LD, Davies, RO. Aspiration as a function of hypodermic needle internal diameter in the in-vivo human upper limb. Anesth Prog. 1980;27:49–51.
16. Malamed, SF. Septodont Inc: Newark, Del, April 2006.
17. Hochman, MN, Friedman, MJ. In vitro study of needle deflection: a linear insertion technique versus a bi-directional rotation insertion technique. Quint Int. 2000;31:737–743.
18. Hochman, MN, Friedman, MJ. An in vitro study of needle force penetration comparing a standard linear insertion to the new bidirectional rotation insertion technique. Quint Int. 2001;32:789–796.
19. Aboushala A, Kugel G, Efthimiadis N, Krochak M: Efficacy of a computer-controlled injection system of local anesthesia in vivo, IADR Annual Meeting, 2000, Abstract 2775.
20. Cook-Waite Laboratories Inc. Manual of local anesthesia in general dentistry. New York: Rensselaer & Springville; 1936. [p 38].
21. Local anesthesia and pain control in dental practice. St Louis: CV Mosby, 1957. [p 184].
22. Allen, GD. Dental anesthesia and analgesia (local and general), ed 2. Baltimore, Md: Williams & Wilkins; 1979. [p 133].
23. Yagiela, JA, Jastack, JT. Regional anesthesia of the oral cavity. St Louis: CV Mosby; 1981. [p 105].
24. Malamed, SF, Needles. Handbook of local anesthesia, ed 5. . CV Mosby: St Louis, 2004. [p 103].
25. Malamed, SF, Reed, KL, Poorsattar, S. Needle breakage: incidence and prevention. Dent Clin North Am. 2010;54:745–756.