Clinical Reasoning for Splint Fabrication
1 Describe clinical reasoning approaches and how they apply to splinting.
2 Identify essential components of a splint referral.
3 Discuss reasons for the importance of communication with the physician about a splint referral.
4 Discuss diagnostic implications for splint provision.
5 List helpful hints regarding the hand evaluation.
6 Explain factors the therapist considers when selecting a splinting approach and design.
7 Describe what therapists problem solve during splint fabrication.
8 Describe areas that require monitoring after splint fabrication is completed.
9 Describe the reflection process of the therapist before, during, and after splint fabrication.
10 Discuss important considerations concerning a splint-wearing schedule.
11 Identify conditions that determine splint discontinuation.
12 Identify patient safety issues to consider when splinting errors occur
13 Discuss factors about splint cost and reimbursement.
14 Discuss how Health Insurance Portability and Accountability Act (HIPAA) regulations influence splint provision in a clinic.
Note: This chapter includes content from previous contributions from Sally E. Poole, MA, OTR, CHT and Joan L. Sullivan, MA, OTR, CHT.
In clinical practice there is no simple design or type of splint that applies to all diagnoses. Splint design and wearing protocols vary because each injury is unique. Clinical reasoning regarding which splint to fabricate involves considering the physician’s referral, the physician’s surgical and rehabilitation protocol, the therapist’s conceptual model, the therapist’s assessment of the person’s needs based on objective and subjective data gathered during the evaluation process, and knowledge about the reimbursement source.
Instructors sometimes teach students only one way to do something when in reality there may be multiple ways to achieve a goal. For example, this book emphasizes the typical methods that generalist clinicians use to fabricate common splints. Learning a foundation for splint fabrication is important. In clinical practice, however, the therapist should use a problem-solving approach and apply clinical reasoning to address each person who needs a splint. Clinical reasoning may include integration of knowledge of biomechanics, anatomy, kinesiology, psychology, conceptual models, pathology, splinting protocols and techniques, clinical experience, and awareness of the person’s motivation, compliance, and lifestyle (occupational) needs.
This chapter first overviews clinical reasoning models and then addresses approaches to clinical reasoning from the moment the therapist obtains a splint referral until the person’s discharge. This chapter also presents prime questions to facilitate the clinical reasoning process the therapist undertakes during treatment planning throughout the person’s course of therapy.
Clinical Reasoning Models
Clinical reasoning helps therapists deal with the complexities of clinical practice. It involves professional thinking during evaluation and treatment interventions [Neistadt 1998]. Professional thinking is the ability to distinctly and critically analyze the reasons for whatever actions therapists make and to reflect on the decisions afterward [Parham 1987]. Skilled therapists reflect throughout the entire splinting process (reflection in action), not solely after the splint is completed (reflection on action) [Schon 1987]. Clinical reasoning also entails understanding the meaning a disability, such as a hand injury, has for each person from the person’s perspective [Mattingly 1991]. Various approaches to clinical reasoning have been depicted in the literature, including interactive, narrative, pragmatic, conditional, and procedural reasoning. Although each of these approaches is distinctive, experienced therapists often shift from one type of thinking to another to critically analyze complex clinical problems [Fleming 1991] such as splinting.
Interactive reasoning involves getting to know the person as a human being so as to understand the impact the hand condition has had on the person’s life [Fleming 1991]. Understanding this can help identify the proper splint to fabricate. For example, for a person who is very sensitive about his or her appearance after a hand injury the therapist may select a skin-tone splinting material that blends with the skin and attracts less attention than a white splinting material.
With narrative reasoning, the therapist reflects on the person’s occupational story (or life history), taking into consideration activities, habits, and roles [Neistadt 1998]. For assessment and treatment, the therapist first takes a top-down approach [Trombly 1993] by considering the roles the person had prior to the hand condition and the meaning of occupations in the person’s life. The therapist also considers the person’s future and the impact the therapist and the person can have on it [Fleming 1991]. For example, through discussion or a formal assessment interview a therapist learns that continuation of work activities is important to a person with carpal tunnel syndrome. Therefore, the therapist fabricates a wrist immobilization splint positioned in neutral and has the person practice typing while wearing the splint.
With pragmatic reasoning, the therapist considers practical factors such as reimbursement, public policy regulations, documentation, availability of equipment, and the expected discharge environment. This type of reasoning includes the pragmatic considerations of the therapist’s values, knowledge, and skills [Schell and Cervero 1993, Neistadt 1998]. For example, a therapist may need to review the literature and research evidence if he or she does not know about a particular diagnosis that requires a splint. If a therapist does not have the expertise to splint a client with a complicated injury, he or she might consider referring the person to a therapist who does have the expertise.
In addition, a therapist may need to make an ethical decision such as whether to fabricate a splint for a terminally ill 98-year-old person. This ethical decision would involve the therapist’s values about age and terminal conditions. In today’s ever-changing health care environment, there is a trend toward cost containment. Budgetary shortages may require therapists to ration their clinical services. Prospective payment systems for reimbursing the costs of rehabilitation, such as in skilled nursing facilities (SNFs), are a reality. Therapists fabricate splints quickly and efficiently to save costs. The information provided throughout this book may assist with pragmatic reasoning.
With conditional reasoning, the therapist reflects on the person’s “whole condition” by considering the person’s life before the injury, the disease or trauma, current status, and possible future life status [Mattingly and Fleming 1994]. Reflection is multidimensional and includes the condition that requires splinting, the meaning of having the condition or dysfunction, and the social and physical environments in which the person lives [Fleming 1994]. The therapist then envisions how the person’s condition might change as a result of splint provision and therapy. Finally, the therapist realizes that success or failure of the treatment will ultimately depend on the person’s cooperation [Fleming 1991, Neistadt 1998]. Evaluation and treatment with this clinical reasoning model begin with a top-down approach, considering the meaning of having an injury in the context of a person’s life.
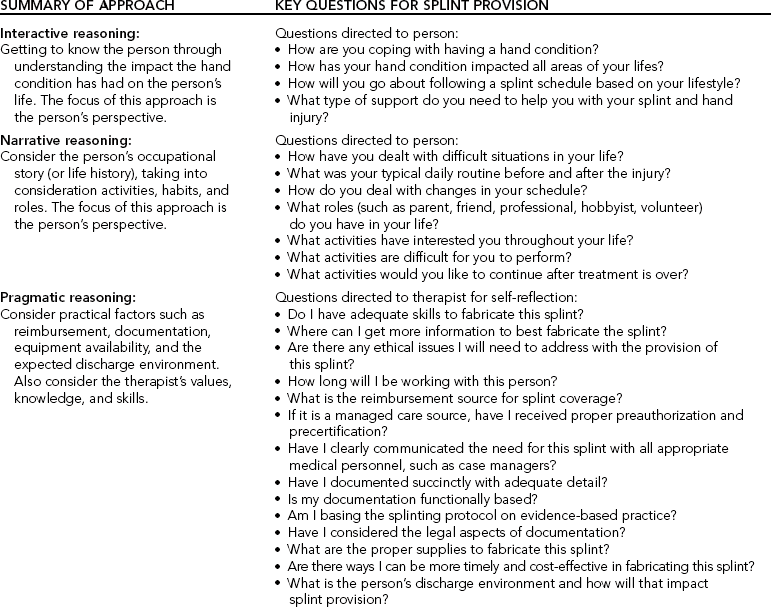
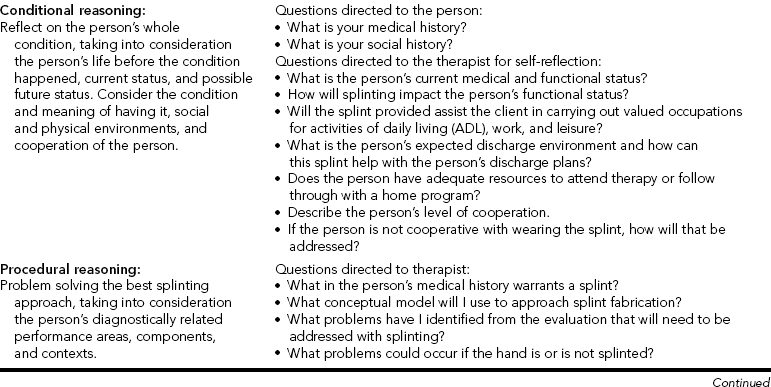
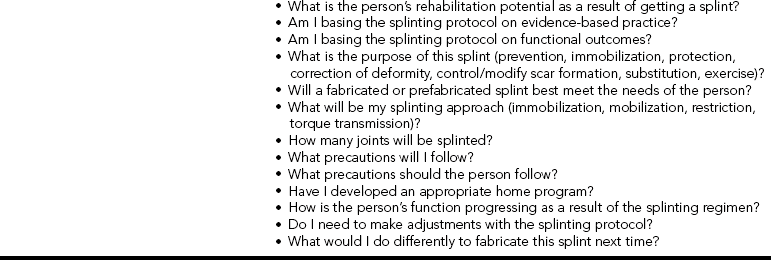
Procedural reasoning involves finding the best splinting approach to improve functional performance, taking into consideration the person’s diagnostically related performance areas, components, and contexts [Fleming 1991, 1994; Neistadt 1998]. Much of the material in this chapter, which summarizes the treatment process from referral to discontinuation of a splint, can be used with procedural reasoning. To demonstrate clinical reasoning,Table 6-1 summarizes each approach and includes questions for the therapist to either ask the person or reflect on during splint provision and fabrication. As stated at the beginning of this discussion, each approach is explained separately. However, experienced therapists combine these approaches, moving easily from one to another [Mattingly and Fleming 1994].
Clinical Reasoning Throughout the Treatment Process
The following information assists with pragmatic and procedural reasoning.
Essentials of Splint Referral
The first step in the problem-solving process is consideration of the splint referral. The ideal situation is to receive the splint referral from the physician’s office early to allow ample time for preparation. In reality, however, the first time the therapist sees the referral is often when the person arrives for the appointment. In these situations the therapist makes quick clinical decisions. Aside from client demographics, Fess et al. [2005] suggest that therapists also need or should determine the following information.
Therapist/Physician Communication About Splint Referral
A problem that many therapists encounter is an incomplete splint referral that lacks a clear diagnosis. Even an experienced therapist becomes frustrated upon receiving a referral that states “Splint.” Splint what? For what purpose? For how long? An open line of communication between the physician and the therapist is essential for good splint selection and fabrication. Most physicians welcome calls from the treating therapist when those calls are specific. If the physician’s splint referral does not contain the pertinent information, the therapist is responsible for requesting this information. The therapist prepares a list of questions before calling, and if the physician is not available the therapist conveys the list to the physician’s secretary or nurse and agrees on a specific time to call again. Sometimes the secretary or nurse can read the chart notes or fax an operative report to the therapist. The therapist must never rely solely on the client’s perception of the diagnosis and splint requirements.
In some cases, the physician expects the therapist to have the clinical reasoning skills to select the appropriate splint for the specific clinical diagnosis. Sometimes a therapist receives a physician’s order for an inappropriate splint, a nontherapeutic wearing schedule, or a less than optimal material. It is the therapist’s responsibility to always scrutinize each physician referral. If the referral is inappropriate, the therapist should apply clinical reasoning skills to determine the appropriate splinting approach. The therapist makes successful independent decisions with a knowledge base about the fundamentals of splinting and with the ability to locate additional information. Then the therapist calls the physician’s office and diplomatically explains the problem with the referral and suggests a better splinting approach and rationale. See Boxes 6-1 and 6-2 for examples of complete and incomplete splinting referrals. Reflect on what you would do if you received the incomplete splint referral.
Diagnostic Implications for Splint Provision
The therapist identifies the person’s diagnosis after reviewing the splint order. Often, the therapist can begin the clinical reasoning process by using a categorical splinting approach according to the diagnosis. The first category involves chronic conditions, such as hemiplegia. In such a situation, a splint may prevent skin maceration or contracture. The second category involves a traumatic or acute condition that may encompass surgical or nonsurgical intervention. For example, the person may have tendinitis and require a nonsurgical splint intervention for the affected extremity.
Regardless of whether the condition is acute or chronic, it is very important that the therapist have an adequate knowledge of diagnostic protocols. By knowing protocols, therapists are aware of any precautions for splinting. For example, for a person with carpal tunnel syndrome the therapist knows to splint the wrist in a neutral position. If the therapist splinted the wrist in a functional position of 30 degrees of extension it could actually harm the person by putting too much pressure on the median nerve. Therapists should keep abreast of current treatment trends through literature, continuing education, and communication with physicians. In all cases, the splint provision approach is individually tailored to each client, beginning with categorization by diagnosis and then adapting the approach according to the client’s performance, cognition, and physical environment.
Factors Influencing the Splint Approach
The sections that follow offer specific hints that elaborate on areas of the splinting evaluation the therapist can use with clinical reasoning. (See Chapter 5 for essential components to include in a thorough hand evaluation.)
Age
The person’s age is important for many reasons. Barring other problems, most children, adolescents, and adults can wear splints according to the respective protocol. An infant or toddler, however, can usually get out of any splint at any time or place. Extraordinary and creative methods are often necessary to keep splints on these youngsters [Armstrong 2005]. Older persons, especially those with diminished functional capacities, may require careful monitoring by the caregiver to ensure a proper fit and compliance with the wearing schedule.
Occupation
From the interview with the person, family, and caregiver (and from the medical record review), the therapist obtains information about the impact a splint may have on occupational function, economic status, and social well-being. The therapist should carefully consider the meaning the condition has for the person, how the person has dealt with medical conditions in the past, how the person’s condition may change as a result of the splint provision, and the person’s social environment. Thus, when choosing the splint design and material the therapist considers the person’s lifestyle needs. The following are some specific questions to reflect on when determining lifestyle needs.
• What valued occupations, such as work or sports, will the person engage in while wearing the splint?
• Do special considerations exist because of rules and regulations for work or sports?
• In what type of environment will the person wear the splint? For example, will the splint be used in extreme temperatures? Will the splint get wet?
• Will the splint impede a hand function necessary to the person’s job or home activities?
• What is the person’s normal schedule and how will wearing a splint impact that schedule?
If a physician refers a person for a wrist immobilization splint because of wrist strain, the therapist might contemplate the following question: Is the person a construction worker who does heavy manual work or a computer operator who does light, repetitious work? A construction worker may require a splint of stronger material with extremely secure strapping. The computer operator may benefit from lighter, thinner splint material with wide soft straps. In some situations the person may best benefit from a prefabricated splint.
The therapist determines the person’s activity status, including when the person is wearing a splint that does not allow for function or movement (such as a positioning splint). If the person must return to work immediately, albeit in a limited capacity, the splint must always be secure. Proper instructions regarding appropriate care of the limb and the splint are necessary. This care may involve elevation of the affected extremity, wound management, and periodic range-of-motion exercises while the person is working.
When the person plans to continue in a sports program (professional, school, or community based), the therapist checks the rules and regulations governing that particular sport. Rules and regulations usually prevent athletes from wearing hard splint material during participation in the sport, unless the splint design includes exterior and interior padding. Therapists need to communicate with the coach or referee to determine appropriateness of a splint [Wright and Rettig 2005].
Expected Environment
The therapist must consider the person’s discharge environment. Some persons return to their own homes and have families and friends who can lend assistance if necessary. For those persons returning to inpatient units or nursing homes, therapists consider instructing the staff in the care and use of the splints. If persons return to psychiatric units or prison wards, therapists consider whether supervision is necessary so that persons cannot use their splints as potential weapons to harm themselves or others.
Activities of Daily Living Responsibilities
The therapist considers the following question: Is the person able to successfully complete all activities of daily living (ADL) and instrumental activities of daily living (IADL) if a splint needs to be worn? For example, the therapist may consider how a person can successfully prepare a meal wearing a splint that immobilizes one extremity. In that case, the therapist may address one-handed meal-preparation techniques.
Person Motivation and Compliance
There has been a limited amount of research investigating compliance issues with splint provision. Only recently have experts considered compliance as it relates to persons with hand injuries [Groth and Wilder 1994, Kirwan et al. 2002]. Many considerations affect compliance with a treatment regimen, including such external factors as socioeconomic status and family support (and such internal factors as the person’s perception of the severity of the condition). Knowledge, beliefs, and attitudes about the condition also influence compliance [Bower 1985, Groth and Wulf 1995].
Another factor addressed in research is the psychosocial construct of locus of control, which proposes a relationship between a person’s perception of control over treatment outcomes and the likelihood the person will comply with treatment. This perception of control can be internally or externally based [Bower 1985]. For example, an internally motivated person would follow a splint schedule on his or her own motivation. An externally motivated person may need encouragement from the therapist or caregiver to follow a splint-wearing schedule. Often not discussed with compliance are organizational variables and clinic environment issues such as transportation problems, interference with daily schedule, wait time, differing therapists, and clinic location [Kirwan et al. 2002].
The therapist can positively influence the person’s compliance and motivation to wear a splint. Establishing goals together may help invest the person in the treatment. Perhaps doing an occupation-focused assessment such as the Canadian Occupational Performance Measure (COPM) can help invest the client in wearing the splint [Law et al. 1998]. If the goals determined by the COPM are improvement of hand function, the therapist discusses how the splint will meet this goal. Furthermore, it is important for the therapist to examine her own treatment goals in relation to the client’s goals because there might be disparity between them [Kirwan et al. 2002]. Sometimes the client will have input about the splint design, which should be considered seriously by the therapist. Therapists should convey to clients that success with rehabilitation and splints involves shared responsibility. To attain the splint goal, the therapist must always clarify the person’s responsibilities in the treatment plans.
In addition, the therapist should perceive the person as a whole individual with a lifestyle beyond the clinic, not just as a person with an injury. Paramount to compliance is education about the medical necessity of wearing splints, in which the therapist should consider the person’s perspectives on the ways the splints would affect his or her lifestyle. Education should be repetitive throughout the time the person wears the splint [Southam and Dunbar 1987, Groth and Wulf 1995]. When the therapist and the physician communicate clearly about the type of splint necessary, the person receives consistent information regarding the rationale for wearing the splint. Showing the way the splint works and explaining the goal of the splint enhance client compliance.
Rather than labeling the person as noncompliant or uncooperative, trained personnel must make a serious attempt to help the person better cope with the injury. The therapist should be an empathetic listener as the person learns to adjust to the diagnosis and to the splint. Compliance also involves both therapist and client [Kirwan et al. 2002].Box 6-3 presents some of the many factors that may influence compliance with splint wear.Box 6-4 provides some suggested questions that may assist the therapist in eliciting pertinent information from clients about splint compliance, fit, and follow-up.
Others can also have an impact on client compliance. Sometimes a peer wearing a splint can be a role model to help a person who is noncompliant. A supportive spouse or caregiver encourages compliance, and physician support influences compliance. Sometimes a person may need more structured psychosocial support from mental health personnel.
Selection of an appropriate design may alleviate a person’s difficulty in adjusting to an injury and wearing a splint. Therapists should ask themselves many questions as they consider the best design. (See the questions listed in the section on procedural reasoning inTable 6-1.)
In addition to splint design, material selection (e.g., soft instead of hard) may influence satisfaction with a splint [Callinan and Mathiowetz 1996]. People with rheumatoid arthritis who wear a soft prefabricated splint consider comfort and ease of use when involved in activities important factors for splint satisfaction [Stern et al. 1997]. (See the discussion of advantages and disadvantages of prefabricated soft splints in Chapter 5.)
Making the splint aesthetically pleasing helps with a person’s compliance. A person is less likely to wear a splint that is messy or sloppy. This is especially true of children and adolescents, for whom personal appearance is often an important issue.
Splint and strapping materials are now available in a variety of colors. Persons, both children and adults, who are coping successfully with the injury may want to have fun with the splint and select one or more colors. However, a person who is having a difficult time adjusting to the injury may not want to wear a splint in public at all, let alone a splint with a color that draws more attention.
Finally, fabrication of a correct-fitting splint on the first attempt eases a person’s anxiety. The therapist is responsible for listening to the person’s complaints and adjusting the splint. A therapist’s attitude about splint adjustments makes a difference. If the therapist seems relaxed, the person may consider adjustment time a normal part of the splintmaking process. Encouraging effective communication with the person facilitates understanding and satisfaction about splint provision.
Cognitive Status
When a person is unable to attend the therapy program and follow the splinting regimen because of his or her cognitive status, the therapist must educate the family, caregiver, or staff members. Education includes medical reasons for the splint provision, wearing schedule, home program, splint precautions, and splint cleaning. This leads to better cooperation. Sometimes the therapist chooses designs and techniques to maximize the person’s independence. For example, instructions are written directly on the splint. Such symbols as suns and moons to represent the time of day can be used in written instructions [personal communication, K. Schultz-Johnson, March 1999]. Simple communication strategies such as showing the client a sheet with a smiley face, neutral face, or frowning face can be used to determine how the client feels about splint comfort.
Splinting Approach and Design Considerations
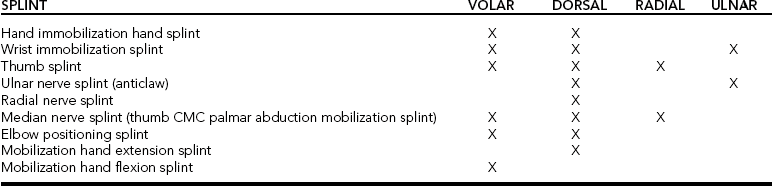
The five approaches to splint design are dorsal, palmar, radial, ulnar, and circumferential. The therapist must determine the type of splint to fabricate, such as a mobilization splint or immobilization splint. Understanding the purpose of the splint clarifies these decisions. For example, when working with a person who has a radial nerve injury the therapist may choose to fabricate a dorsal torque transmission splint (wrist flexion: index-small finger MP extension/index-small finger MP flexion, wrist extension torque transmission splint, ASHT, 1992) to substitute for the loss of motor function in the wrist and MCP extensors. On the basis of clinical reasoning, the therapist may choose in addition to fabricate a palmar-based wrist extension immobilization splint once the person regains function of the MCP extensors. The wrist splint allows the person to engage in functional activities.
In addition to the information the therapist obtains from a thorough evaluation, other factors dictate splint choice. To determine the most efficient and effective splint choice, the therapist must consider the physician’s orders, the diagnosis, the therapist’s judgment, the reimbursement source, and the person’s function.
Physician’s Orders
Physicians often predetermine the splint-application approach on the basis of their training, surgical technique, and restriction/torque transmission splint with the ring and little fingers in the anticlaw position of MCP flexion (ring-small finger MP extension restriction/ring-small finger IP extension torque transmission splint, ASHT, 1992). However, a spring wire splint to hold the MCPs in flexion may be ordered if that is the physician’s preference. Sometimes the therapist may apply clinical reasoning to determine a different splint design or material than what was ordered. In that case, the therapist calls the physician.
Diagnosis
Frequently, the diagnosis mandates the approach to splint design. The diagnosis determines the number of joints the therapist must splint. The least number of joints possible should be restricted while allowing the splint to accomplish its purpose. Diagnosis also determines positioning and whether the splint should be of the mobilization or immobilization type. For example, using an early mobilization protocol for a flexor tendon repair, the therapist places the base of the splint on the dorsum of the forearm and hand to protect the tendon and to allow for rubber band traction. The wrist and MCPs should be in a flexed position (alternatively, some physicians now prefer a neutral position to block extension). These splints protect the repair and allow early tendon glide. In this example, the repaired structures and the need to begin tendon gliding guide the approach. (See Chapter 11 for more information on mobilization splint fabrication with tendon repairs.)
Therapist’s Judgment
The therapist can also determine the splint design and type on the basis of knowledge and experience. For example, when dealing with elective carpal tunnel release the therapist can place a wrist immobilization splint dorsally or volarly directly over the surgical site. As an advocate of early scar management, the therapist chooses a palmar splint and adds silicone elastomer or Otoform to the splint.
Person’s Function
The person’s primary task responsibilities may influence splint choice. A construction worker’s wrist has different demands placed on it than the wrist of a computer operator with the same diagnosis. Not only does the therapist choose different materials for each client but the design approach may be different. A thumb-hole volar wrist immobilization splint decreases the risk of the splint migrating up the arm during the construction worker’s activities, as it tightly conforms to the hand. The computer operator may prefer a dorsal wrist immobilization splint to allow adequate sensory feedback and unimpeded flexibility of the digits during keyboard use. (See Chapter 7 for patterns of wrist splints.)
Table 6-2 outlines a variety of positioning choices for splint design. However, therapists should not view these suggestions as strict rules. For example, a skin condition may necessitate that a mobilization extension splint be volarly based rather than dorsally based.
Clinical Reasoning Considerations for Designing and Planning the Splint
The splint designing and planning process involves many clinical decisions about materials and techniques the therapist can use. (Refer to chapters throughout this book for more specifics on materials and techniques.) Initial considerations are often related to infection control procedures.
Infection-Control Procedures
The therapist considers whether dressing changes are necessary. If so, the therapist follows universal precautions and maintains a sterile environment. The therapist should be aware that skin maceration under a splint can more easily occur in the presence of a draining wound. In this situation the therapist first carefully applies a dressing that will absorb the fluid.
Splint fabrication should take place over the dressing, and the therapist should instruct the person in how to apply new dressings at appropriate intervals [Skotak and Stockdell 1988]. Before the application of the splinting material, the therapist can place a stockinette over the person’s bandages. This action prevents the thermoplastic material from sticking to the bandages.
If the person has a draining or infected wound, the therapist does not use regular strapping material to hold the splint in place. Strapping material can absorb bacteria. Instead, the therapist uses gauze bandages that are replaced at each dressing change. If a person is unwilling or unable to change a dressing, the therapist can instruct a family member or friend to do so. If this is not possible, the person may need to visit the therapist more frequently.
Time Allotment for Splint Fabrication and Person and Nursing or Caregiver Education
The therapist also considers the time required for splint fabrication and education. Splint fabrication time varies according to splint complexity and the person’s ability to comply with the splinting process. For example, squirmy babies and people with spasticity are more difficult to splint and require more time. In these cases, it may be beneficial to have additional staff or a caregiver to help position the person.
Splint fabrication time is also dependent on the therapist’s experience. If possible, a beginning therapist should schedule a large block of time for splint fabrication. As therapists gain clinical experience, they require less time to fabricate splints. With any splint application, the therapist should allow enough time for educating the person, family, and caregiver about the wear schedule, precautions, and their responsibility in the rehabilitation process. As discussed, education helps with compliance.
Batteson [1997] found that in an institutional setting a nurse training program developed by the occupational therapist that addressed splinting was very helpful in increasing compliance with a splint-wearing schedule. This program included splint rationale, common splint care questions, and familiarization with splinting materials. A nurse liaison was identified to deal specifically with the client’s splint concerns. In addition, a splint resource file developed by the therapist was made available to the nurses.
Post-fabrication Monitoring
The therapist uses clinical reasoning skills to thoroughly evaluate and monitor the fabricated splint. In particular, the therapist must be aware of pressure areas and edema.
Monitoring Pressure
Regardless of its purpose or design, the splint requires monitoring to determine its effect on the skin. The therapist must remember that a person wearing a splint is superimposing a hard lever system on an existing lever system that is covered by skin, a living tissue that requires an adequate blood supply. The therapist must therefore follow mechanical principles during splint fabrication to avoid excessive pressure on the skin. With fabrication, therapists have to weigh the pros and cons of the amount of splint coverage. With minimal coverage from a splint, there is increased mobility. Increased coverage by a splint allows for more protection and better pressure distribution. To reduce pressure, the therapist should design a splint that covers a larger surface area [Fess et al. 2005]. Warning signs of an ill-fitting splint are red marks and ulcerations on the skin.
A well-fitting splint, after its removal, may leave a red area on the person’s skin. This normal response to the pressure of the splint disappears within seconds. When a splint has applied too much pressure on one area, which usually occurs over a bony prominence, the redness may last longer. For persons with dark skin, in whom redness is not easily visible, the therapist may lightly touch the skin to determine the presence of hot spots or warmer skin. Another way to check skin temperature is with a thermometer. With any splint, the therapist checks the skin after 20 to 30 minutes of wearing time before the person leaves the clinic. If red areas are present after 20 to 30 minutes of wearing the splint, adjustments need to be made.
A person with intact sensibility who has an ill-fitting splint usually requests an adjustment or simply discards the splint because it is not comfortable. For a condition in which sensation is absent, vigorous splint monitoring is critical [Brand and Hollister 1993, Fess et al. 2005]. The therapist teaches the person and the family to remove the splint every one to two hours to check the skin so as to avoid skin breakdown.
Monitoring for Skin Maceration
Wet, white, macerated skin can occur when the skin under a splint holds too much moisture. This can occur for many reasons, such as a child drooling on a splint. When this happens to a person with intact skin who has simply forgotten to remove the splint, the therapist can easily correct the problem by washing and drying the area. Educating the person about proper care of the hand and providing a polypropylene stockinette to absorb moisture should resolve this situation.
Monitoring Edema
A therapist frequently needs to splint an edematous extremity. Edema is often present after surgery, in the presence of infection, with severe trauma (e.g., from a burn), or with vascular or lymphatic compromise. A well-designed, well-fitting splint can reduce edema and prevent the sequelae of tissue damage and joint contracture. A poorly designed or ill-fitting splint can contribute to the damaging results of persistent edema. Generally, the design and fit principles already discussed in this text apply.
The therapist also considers the method used to hold the splint in place. Soft, wide straps accommodate increases in edema and are better able to distribute pressure than rigid, non-yielding Velcro straps [Cannon et al. 1985]. When too tight, strapping can contribute to pitting edema as a result of hampered lymphatic flow [Colditz 2002]. For severe edema, the therapist may gently apply a wide elastic wrap to keep the splint in place. The continuous contact of the wrap helps reduce edema [Colditz 2002]. Therapists should be cautioned that straps applied at intervals may further restrict circulation and cause “windowpane” edema distally and between the straps. When using Ace wraps or compressive gauze, the therapist must apply them in a figure-of-eight pattern and use gradient distal-to-proximal pressure. The therapist must properly monitor the splint and wrap to ensure that the wrap does not roll or bunch [Mackin et al. 2002]. Pressure created by rolling or bunching could cause constriction and further edema and stiffness.
If the lymphatic system is not damaged, edema reduction usually begins relatively quickly with appropriate wound healing (i.e., no infection), proper elevation, and gentle active exercises as permitted. As edema resolves, the therapist remolds the splint to fit the new configuration of the extremity. The therapist asks the person with severe edema to return to the clinic daily for monitoring and treatment. When the edema appears to be within the normal postoperative range, the therapist asks the person to return to the clinic in three to five days for a splint check. Helping the person understand the frequency and purpose of the splint adjustments is also important. Again, education is an important part of the edema-reduction regimen [Mackin et al. 2002].
Monitoring Physical and Functional Status
When a person’s physical or functional status changes, a splint adjustment is often necessary. If a person is receiving treatment for a specific injury and it is effective, the splint requires adjustments in conjunction with improvement. For example, if a person has a median nerve injury in which the thumb has an adduction contracture the therapist fabricates a thumb CMC palmar abduction mobilization splint [ASHT 1992] to gradually widen the tight web space. As treatment progresses and thumb motions increase, the therapist adjusts the splint to accommodate the gains in motion [Reynolds 1995].
Evaluation and Adjustment of Splints
After fabricating the splint, the splintmaker carefully evaluates the design to determine fit and necessary adjustments. The therapist looks carefully at the splint when the person is and is not wearing it and considers whether the splint serves its purpose. The splint should be functional for the person and should accomplish the goals for which it was intended. It should also have a design that uses correct biomechanical principles and should be cosmetically appealing. (Refer to specific chapters in this book for hints and splint-evaluation forms.)
Therapists learn from self-reflection before, during, and after each splint is made. This helps fine-tune professional thinking skills. The following are reflective questions the therapist can consider after splint fabrication.
• Did the splint accomplish the purpose for which it was intended?
• Is it correctly fitted according to biomechanical principles?
• Did I select the best materials for the splint?
• Did I take into consideration fluctuating edema?
• Is it cosmetically appealing?
• Is it comfortable for the person and free of pressure areas?
• Have I addressed how splinting impacts the person’s valued occupations?
• Have I addressed functional considerations?
• What would I do differently if I were to refabricate this splint?
If major adjustments are required, the therapist should avoid using a heat gun except to smooth splint edges. If the therapist has selected the appropriate simple splint design and has used a thermoplastic product that is easily reheatable and remoldable, the water-immersion method is the best way to adjust the splint. Years of experience demonstrate that reheating the entire splint in water and reshaping it is more efficient than spot heating. The activity of the therapist reheating and adjusting one spot often affects the adjacent area, thereby producing another area requiring adjustment. This cycle may not end until the splint is useless. When possible, the therapist should use a splint product that is reheatable in water and easily reshapable to obtain a proper fit for the client.
Splint-Wearing Schedule Factors
Development of a splint-wearing schedule for a person is sometimes extremely frustrating for a beginning splintmaker because there are no magic numbers or formulas for each type of splint or diagnostic population. The therapist tailors and customizes the wearing schedule to the individual and exercises clinical judgment. Only general guidelines for splint-wearing schedules exist.
In the case of joint limitation, the therapist increases the wearing frequency and time as much as the person can tolerate. Alternatively, the therapist adjusts the treatment plan to try a different splint. If motion is increasing steadily, the therapist may decrease the splint-wearing time, allowing the person to engage in function by using the limited joint or joints. If the splint improves function or the extremity requires protection, the person wears the splint when necessary. The following are questions to consider when determining a wearing schedule.
• What is the purpose of the splint?
• Does the therapist anticipate that the person will be compliant with a splint-wearing schedule?
• Does the person have any medical contraindications or precautions for removing the splint?
• Which variables may affect the person’s tolerance of the splint?
• Does the person need assistance to apply or remove the splint?
• Is the splint for day or night use, or both?
• Does the person need to apply or remove the splint for any functions?
• How often does the person need to perform exercises and hygiene tasks?
Answers to these questions should guide the development of a wearing schedule. The therapist should keep in mind that the wearing schedule may require adjustment as the person’s condition progresses. In any situation, the therapist should discuss the wearing schedule with the person and caregiver.Box 6-5 shows a sample wearing schedule the therapist can post in a person’s room or give to the person to take home.
Discontinuation of a Splint
No distinct rules exist concerning a splint’s discontinuation. Sometimes the physician makes the decision to discontinue a splint. Other times the physician defers to the clinical judgment of the therapist to determine when a splint is no longer beneficial. Sometimes specific protocols, such as for a flexor tendon repair, indicate when a splint should be discontinued. In such cases, the therapist should contact the physician for a splint-discharge order. Sometimes physicians order a splint to be discontinued “cold turkey.” If the therapist clinically reasons that the person would benefit from being weaned off the splint, the physician should be contacted. The therapist should communicate the rationale for the weaning and ask for approval. The following are questions to consider when making the clinical decision to discontinue a splint.
• Have the person and the caregivers been compliant with the splint-wearing schedule? If not, why?
• What are the original objectives for the splint’s provision, and has the person accomplished them?
• Will the same objectives be compromised or accomplished without a splint?
The compliance of the person and the caregiver is essential for success with a splint-wearing regimen. If the person is not wearing the splint, the therapist first uses clinical reasoning to identify the reasons for noncompliance. For example, the noncompliance of an older person in an institutional setting could be the result of one or more of the following factors: (1) poor communication among the staff about the splint-wearing schedule, (2) poor staff follow-through with the splint-wearing schedule, (3) the elder’s lack of understanding about the splint’s purpose, (4) discomfort of the splint, (5) the elder’s fear of hidden costs associated with the splint, and (6) the elder’s dislike of the splint’s cosmetic appearance. Reasons for noncompliance could be beyond this list and it would be up to the therapist to ascertain the problem. After identifying the reason or reasons for noncompliance, the therapist can work on possible solutions.
An important factor in determining when to discontinue the splint is a careful review of the splint’s objectives. For example, a therapist fabricates a mobilization splint for a person who has a proximal interphalangeal (PIP) soft-tissue flexion contracture of the middle finger. The splint’s objective is mobilization of the PIP joint to help correct the flexion deformity. Gradually, the splint lengthens the restricting structures and extension is restored. By monitoring range of motion (ROM) and evaluating the splint’s line of pull, the therapist determines that the splint has maximally helped the person and that the original treatment objectives were accomplished. At this time, the therapist calls the physician for an order to discontinue the splint.
The therapist must consider whether accomplishment of the objectives is possible without the splint. Timely discontinuation of any splint is important. The therapist should keep in mind that inappropriately provided or poorly fabricated splints can restrict movement, make postural compromises by causing atrophy in one muscle group and overuse in another, and injure other parts of the anatomy. In addition, preventing the person’s dependence on a splint is important. When the person has the functional capabilities, the therapist should adjust the splint-wearing schedule to gradually wean the person away from the splint [Pascarelli and Quilter 1994].
Cost and Reimbursement Issues
Two issues exist regarding the cost of splints. First, how does the therapist arrive at the price of a splint? Second, how does the therapist receive payment for a splint? To calculate the price of a splint, the therapist totals the direct and indirect costs. Direct costs include such items as the thermoplastic material, strapping material, stockinette, rivets, shipping cost, tax, and so on. A hospital or clinic purchases supplies at wholesale cost. However, a percentage markup may appear on the cost. (This assists with replenishing the inventory.) Indirect costs include nondisposable supplies such as scissors and fry pans, the time required for the average therapist to make the splint, and overhead costs such as rent and electricity. SeeTable 6-3 for examples of how to figure out direct and indirect costs.
Table 6-3
Hints for Determining Direct and Indirect Costs
• Lighting, space, fry pan, hydrocollator, scissors, heat gun, shipping, handling, and storage charges for materials.
• Indirect costs are usually figured in a percentage mark-up of the direct costs of a splint (for example, a 10% mark-up cost).
• Estimate how much of the sheet you used
• Determine cost (¼ sheet used)
• Charge for number of inches used
• Charge for number of square inches used
Chemicals (cold spray, glue, solvent, and so on)
• Usually a small set amount is charged whenever chemicals are used
Other materials (finger loops, outrigger kitsss, D-rings, and so on)
As a result of tighter control of the health-care dollar in managed care and prospective payment systems, many therapists are finding that reimbursement for splints is becoming increasingly difficult. It is important that when necessary the therapist take an active role in the outcome of a reimbursement policy of an insurance plan regarding splints. This may help obtain reimbursement for the splint. For example, knowing that a splint is reimbursed from a health maintenance organization (HMO), the therapist gets preauthorization to qualify the fabrication of a splint. The therapist will also get precertification to observe the person for a specified amount of time.
The therapist must remember, however, that the plan belongs to the person, not to the therapist. If a particular insurance plan reimburses costs partially or not at all, the therapist should inform the client of the responsibility for paying the balance of the cost. Some facilities make accommodations for people who are uninsured or underinsured and need splint provision, or there might be a pro-bono clinic available in the area. In addition, the therapist should provide specific documentation to insurance companies about the affected extremity and the type of splint and purpose of the splint [personal communication, R. B. Evans, February 7, 1995].
It is important that therapists know how to effectively navigate the system to receive reimbursement for splint fabrication. If a splint is ordered, it needs to be made. The therapist and the client should work out financial aspects with the facility. Communication with the appropriate persons in the facility.
For some persons with upper extremity problems that occurred on the job, rehabilitation is reimbursed from the Worker’s Compensation System. Therapists must keep in mind that in every state the Worker’s Compensation law is interpreted differently. Therefore, it is important to familiarize oneself with the state guidelines. Most state worker compensation plans cover medical costs related to the injury, such as medical care (including receiving a splint), vocational rehabilitation, and temporary disability (the amount varies from state to state) [Bailey 1998]. Many states have adopted a managed care system. If case managers are involved in the person’s care, the therapist should provide consistent and clear communication about the person’s progress.
Some insurance companies simply refuse to pay for splints, and others ask for so much documentation that more time is required to prepare the bill than to make the splint. For example, some insurance companies ask therapists for original invoices for the purchase of thermoplastic and strapping materials. Developing outcome studies or finding outcome data in the literature may help with reimbursement from insurers, especially managed care organizations (MCOs). Giving these outcomes to insurers will increase their understanding of the importance of splinting in its relation to function. The American Society of Hand Therapists (1992) published Splint Classification Systems, a book on naming and designing splints. This book helps with terminology becoming more uniform [American Society of Hand Therapists 1992].
Policy Regulations: The Health Insurance Portability and Accountability Act
This broad health legislation enacted in 1996 covers many areas with Title II, or Administrative Simplification, influencing therapy practice. Title II includes three main parts: Transaction Rule, Privacy Rule, and Security Rule.
The first part, Transaction Rule, affects billing procedures. It mandates uniform national requirements for formats and codes for electronic transmission [Wilson 2004].
Privacy Rule is another major component of Administrative Simplification and directly influences clinical practice. These rules involve protection of client-identifying or confidential information and client rights about their health information. It regulates how protected health information (PHI) or any client-identifying information is presented in written, verbal, or electronic format [U.S. Department of Health and Human Services 2003]. Therapists should obtain the client’s consent prior to using PHI for treatment, payment, or health care operations. However, if a client objects or fails to provide consent therapists are permitted to use PHI for treatment, payment, or health care operations without the client’s consent. In most other circumstances, with very few exceptions, therapists may not disclose PHI without the client’s written authorization to do so [U.S. Department of Health and Human Services 2004].
Numerous privacy rights with respect to the client’s health information are written into the regulations. For example, clients have a right to request to see their medical record. SeeBox 6-6 for a listing of client protections. Therapy clinics should have policies in place to protect the privacy of client information. Requiring working charts to be kept in a locked cabinet with the documents shredded after treatment completion is an example of an internal policy protecting privacy [Costa and Whitehouse 2003]. Some areas of client information are excluded from the law, such as allowing clients to sign in for treatment, calling out a client’s name to go into the splint fabrication room, or sharing information with another health professional about the splint [Costa and Whitehouse 2003, Sullivan 2004]. However, reasonable efforts to avoid these types of disclosures should be taken. For instance, instead of calling out “Mr. Edward Jones, the therapist will see you now to customize your resting hand splint,” a better approach would be “Edward, the therapist will see you now.”
Incidental disclosures (information that is heard with reasonable efforts to not be overheard) or sharing information that is limited are not considered in violation of the HIPAA law [Sullivan 2004]. An example of an incidental disclosure is an occupational therapist discussing information about a splint bill with the secretary in the waiting room. These disclosures are not considered liable under the law as long as there are no other reasonable options (i.e., no other area for individual privacy to discuss the bill) [personal communication, J. M. Sullivan, October 12, 2004]. Because therapy often takes place in an open area with several people involved in conversations, some of which potentially involve sharing of PHI, it needs to be clear in the consent form about the clinic setup [Murer 2002].
Therapists working in such clinics can employ simple strategies to allow more privacy, such as partitioning off a private area or using a private room available for treatment, communicating with lower voices, and being careful with leaving sensitive messages on answering machines [York 2003]. As York [2003, p. 45] states, “creating a culture of privacy and maintaining good rapport with patients will go a long way to preventing HIPAA complaints as well as other types of legal problems.”
The third main part of Administrative Simplification, the Security Rule, involves the policies and procedures a facility has in place to protect the PHI through “administrative, technical and physical safeguards” [Wilson 2004, p. 132]. It mainly focuses on “electronic protected health information” [Wilson 2004, p. 133] such as who has access to computer data in a clinic. Finally, therapists must keep abreast of their state privacy laws. If they are stricter, they take priority over the HIPAA regulations [York 2003].
Documentation
Splint application must be well documented. Documentation assists in third-party reimbursement and communication with other health care providers, helps ascertain the medical-legal necessity, and demonstrates the efficacy of the intervention.
Splint documentation should be specific and should include several elements, such as the onset of the medical condition that warrants a splint; the medical necessity for the splint; the level of function before the splint; the person’s rehabilitation potential with the splint; and type, purpose, and anatomical location of the splint. Therapists should also document that they have communicated with the person an oral and written schedule and have had discussions about precautions. Any input the person provides to the treatment plan, such as mutual goal setting, should be documented.
Splint documentation, including goal setting, should be related to function. It is not sufficient to document that a person’s ROM has improved to a certain level as a result of wearing a splint. The therapist should specifically document how the improved ROM has helped the person perform specific functional activities. For example, the therapist may document that because of improved wrist motion from wearing a splint the person is able to write at work.
As with any documentation, the therapist should consider legal implications. Documentation should be thorough, complete, and objective. The therapist should always remember, “If it wasn’t documented it didn’t happen.” For example, the therapist should document the specific measurements by which the hand is splinted for a person who has de Quervain’s tenosynovitis. Also for example, if the person has a reddened area as a result of wearing a splint the specific location and size of the reddened area as well as any splint adjustments made should be documented. Any communication or advice about the splint from the physician should be documented, with the time and date of the call [Ekelman-Ranke 1998].
Documentation for follow-up visits should include the date and time the person is supposed to return and a notation that the date and time had been discussed with the person. This helps protect the therapist if there are claims of negligence with follow-up care [Ekelman-Ranke 1998]. Documentation for follow-up visits should also include any changes in the splint’s design and wearing schedule. In addition, the therapist should note whether problems with compliance are apparent. Documenting evidence of compliance includes documenting instructions provided and objective person’s or caregiver’s behavior that contradicts instructions. For example, the therapist might document that the person stated that he or she did not follow the splint-wearing schedule.
Also for example, for a person in a skilled nursing facility the therapist bases documentation on objective observations of dates and times the splint-wearing schedule is not being followed. The therapist in this case may then further educate the caregivers and note when and what type of education was completed. If the caregivers still do not properly follow the schedule, the therapist should come up with another plan and involve the caregivers in the decision-making process to ensure compliance. Another objective observation for a person followed in any setting is notation of signs of wear, such as scratching, light soil, or strap wear. In documentation, it is inappropriate to criticize other health care professionals, such as documenting that contractures developed in a person as a result of the nursing staff’s not having applied a splint [Ekelman-Ranke 1998].
The therapist should perform splint reassessments regularly until completion of the person’s weaning from the splint or discharge from services. Documentation after the reassessments should be timely and based on guidelines from the insurer [Ekelman-Ranke 1998]. Finally, the therapist should keep in mind that different facilities use different methods to document, and the therapist should be familiar with the routine method of the facility. (See Examples 6-1 and 6-2 for illustrations, respectively, of a narrative and a SOAP note for a splint.)
Splinting Error and Client Safety Issues
Splinting errors occur in occupational therapy [Scheirton et al. 2003]. Examples of these errors include fabricating the wrong type of splint for the condition or failure to follow through with the splint-wearing schedule. Either of these errors could cause client harm such as severe pain or breakdown of the skin. Although many errors are the direct result of individual failure, most errors are caused by system problems. System errors may occur due to diagnostic error, equipment/product failure, or miscommunication of medical orders, to name a few. Splinting errors can easily result from incorrect or inadequate communication. A physician, for example, may order a right hand splint when it is meant for the left hand. If the therapist fails to question the physician order, a splint may be fabricated for the wrong site.
According to data collected by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), team miscommunication is at the root of a great proportion of all errors made in health care [Joint Commission on Accreditation of Healthcare Organizations 2005a, 2005b]. Occupational therapists often lack assertiveness when communicating with physicians, and this failure to adequately communicate can result in patient harm [Lohman et al. 2004]. Understanding the nature of hierarchic organizational structures and the need for coordination of care through “interdisciplinary care management” and “coordinated communication” are vital to client safety [Joint Commission on Accreditation of Healthcare Organizations 2005a, p. 161].
To create this culture of safety, occupational therapists must debunk or dispel the myth of performance perfection. To err is human! After all, health care delivery is a very complex system. In complex systems, errors are inevitable regardless of how well trained, well intentioned, or ultra-careful the individual therapist may be. In the case of the therapist acting on the physician’s wrong order, it would be unjust to simply require the last treating practitioner to be fully accountable for the error. In this situation, blaming and sanctioning would only encourage the therapist and/or physician to hide the error rather than disclose and report it.
Today’s undisclosed near miss or minor error can become tomorrow’s egregiously harmful error. Only by acknowledging error can we individually and collectively learn from that error and make individual and system practice changes to prevent errors in the future. Furthermore, truthful disclosure of error to clients by the therapist or a disclosure team is not only an ethical obligation but is now dictated by JCAHO standards as well as varied institutional policies [Joint Commission on Accreditation of Healthcare Organizations 2001, Minneapolis Children’s Hospital and Clinics 2001, Dana-Farber Cancer Institute 2004]. Ultimately, creating an environment where practitioners are encouraged and supported for promoting safety and reporting errors and disclosing them to clients is everyone’s goal. This practice safety goal for practice should always be a guidepost for clinical reasoning when splint fabrication failures occur.
1. How would a therapist apply the various clinical reasoning models to splint provision?
2. What does a splint referral include?
3. How can the therapist facilitate communication with the physician’s office about the splint referral?
4. Why is knowing the person’s age important to the therapist when fabricating a splint?
5. Which lifestyle needs of the person must the therapist consider with splint provision?
6. How can the therapist enhance the compliance of a person wearing a splint?
7. What are the infection-control procedures a therapist should follow with splint provision?
8. What should therapists monitor when providing a splint for a person during the following conditions: pressure, edema, and physical status of a person?
9. What are the four directions of splint design?
10. What are some helpful hints for making adjustments after splint fabrication?
11. What are the factors the therapist should consider when establishing a person on a splint-wearing schedule?
12. What are the factors a therapist should consider for splint discontinuation?
13. What are the cost and reimbursement issues the therapist must keep in mind?
14. How might the HIPAA influence communication with clients about splints in a clinical setting?
15. What documentation issues should the therapist be aware of with splinting?
References
American Society of Hand Therapists. Splint Classification Systems. Garner, NJ: The American Society of Hand Therapists, 1992.
Armstong, J. Splinting the pediatric patient. In: Fess EE, Gettle KS, Philips CA, Janson JR, eds. Hand and Upper Extremity Splinting: Principles and Methods. Third Edition. St. Louis: Elsevier Mosby; 2005:480–516.
Bailey, DM. Legislative and reimbursement influences on occupational therapy: Changing opportunities. In: Neistadt ME, Crepaeau EB, eds. Willard & Spackman’s Occupational Therapy. Ninth Edition. Philadelphia: Lippincott; 1998:763–772.
Batteson, R. A strategy to improve nurse/occupational therapist communication for managing persons with splints. British Journal of Occupational Therapy. 1997;60:451–454.
Bower, KA. Compliance as a patient education issue. In: Woldum KM, Ryan-Morrell V, Towson MC, Bower KA, Zander K, eds. Patient Education: Foundations of Practice. Rockville, MD: Aspen Publications; 1985:45–111.
Brand, PW, Hollister, A. Clinical Mechanics of the Hand, Second Edition. St. Louis: Mosby, 1993.
Callinan, NJ, Mathiowetz, V. Soft versus hard resting hand splints in rheumatoid arthritis: Pain relief, preference, and compliance. American Journal of Occupational Therapy. 1996;50:347–354.
Cannon, NM, Foltz, RW, Koepfer, JM, Lauck, MR, Simpson, DM, Bromley, RS. Manual of Hand Splinting. New York: Churchill Livingstone, 1985.
Colditz, JC. Therapist’s management of the still hand. In: Mackin EJ, Callahan AD, Skirven TM, Schneider LH, Osterman AL, eds. Rehabilitation of the Hand and Upper Extremity. Fifth Edition. St. Louis: Mosby; 2002:1021–1049.
Costa, DM, Whitehouse, D. HIPAA and fieldwork. OTPractice. 2003;8(17):23–24.
Dana Farber Cancer Institute (2004). Policy for disclosing medical errors to patients and families. Approved 7/12/01, reviewed 7/17/01 and 7/04.
Ekelman-Ranke, BR. Documentation in the age of litigation. OT Practice. 1998;3(3):20–24.
Fess, EE, Gettle, KS, Philips, CA, Janson, JR. Hand and Upper Extremity Splinting: Principles and Methods, Third Edition. St. Louis: Elsevier Mosby, 2005.
Fleming, MH. Conditional reasoning: Creating meaningful experiences. In: Mattingly C, Fleming MH, eds. Clinical Reasoning: Forms of Inquiry in a Therapeutic Practice. Philadelphia: F. A. Davis; 1994:197–235.
Fleming, MH. The therapists with the three-track mind. American Journal of Occupational Therapy. 1991;45:1007–1014.
Groth, GN, Wilder, DM. The impact of compliance of rehabilitation of persons with mallet finger injuries. Journal of Hand Therapy. 1994;7(1):21–24.
Groth, GN, Wulf, MB. Compliance with hand rehabilitation: Health beliefs and strategies. Journal of Hand Therapy. 1995;8:18–22.
Joint Commission on Accreditation of Healthcare Organizations (2001). Hospital Accreditation Standards RI.1.2.2, July 1
Joint Commission on Accreditation of Health Care Organizations. Patient Safety: Essentials for Healthcare, Third Edition. Oakbrook, IL: Joint Commission Resources, 2005.
Joint Commission on Accreditation of Healthcare Organizations. Sentinel Event Statistics, 1995-2004. http://www.jcaho.org/accredited+organizations/sentinel+events/sentinel+events+statistics.htm 2005.
Kirwan, T, Tooth, L, Harkin, C. Compliance with hand therapy programs: Therapists’ and patients’ perceptions. Journal of Hand Therapy. 2002;15(1):31–40.
Law, M, Baptiste, S, Carswell, A, McCall, MA, Polatajko, H, Pollock, N. Canadian Occupational Performance Measure, Third Edition. Ottawa, ON: CAOT Publications, 1998.
Lohman, H, Mu, K, Scheirton, L. Occupational therapists perspectives on practice errors in geriatric settings. Physical and Occupational Therapy in Geriatrics. 21(4), 2004.
Mackin EJ, Callahan AD, Skirven TM, Schneider LH, Osterman AL, eds. Rehabilitation of the Hand and Upper Extremity, Fifth Edition, St. Louis: Mosby, 2002.
Malick, MH. Manual on Static Splinting. Hamarville, PA: Harmarville Rehabilitation Center, 1972.
Mattingly, C. The narrative nature of clinical reasoning. American Journal of Occupational Therapy. 1991;45:998–1005.
Mattingly, C, Fleming, MH. Clinical Reasoning: Forms of Inquiry in a Therapeutic Practice. Philadelphia: F. A. Davis, 1994.
Minneapolis Children’s Hospital and Clinics. Policy 703.00. Medical accidents, reporting, and disclosure, including sentinel events. Originally effective 28 July 1999, revised 1 October 2001.
Murer, CG. Trends and issues: Protecting patient privacy. Rehab Management. 2002;15(3):46–47.
Neistadt, ME. Teaching clinical reasoning as a thinking frame. American Journal of Occupational Therapy. 1998;52:211–229.
Parham, D. Towards professionalism: The reflective therapist. American Journal of Occupational Therapy. 1987;41:555–560.
Pascarelli, E, Quilter, D. Repetitive Strain Injury. New York: John Wiley & Sons, 1994.
Reynolds, CC. Preoperative and postoperative management of tendon transfers after radial nerve injury. In: Hunter JM, Mackin EJ, Callahan AD, eds. Rehabilitation of the Hand. Fourth Edition. St. Louis: Mosby; 1995:753–763.
Scheirton, LS, Mu, K, Lohman, H. Occupational therapists’ responses to practice errors in physical rehabilitation. American Journal of Occupational Therapy. 57(3), 2003.
Schell, BA, Cervero, RM. Clinical reasoning in occupational therapy: An integrated review. American Journal of Occupational Therapy. 1993;47:605–610.
Schon, DA. Educating the Reflective Practitioner. San Francisco: Jossey-Bass, 1987.
Skotak, CH, Stockdell, SM. Wound management in hand therapy. In: Cromwell FS, Bear-Lehman J, eds. Hand Rehabilitation in Occupational Therapy. Binghamton, NY: Haworth Press; 1988:17–35.
Southam, MA, Dunbar, JM. Integration of adherence problems. In: Meichenbaum D, Turk DC, eds. Facilitating Treatment Adherence. New York: Plenum Publishing, 1987.
Stern, EB, Ytterberg, SR, Krug, HE, Larson, LM, Portoghese, CP, Kratz, WNR, et al. Commercial wrist extensor orthoses: A descriptive study of use and preference in patients with rheumatoid arthritis. Arthritis Care and Research. 1997;10:27–35.
Sullivan, JM. The OT’s Guide to HIPAA: The Impact of Privacy Laws on the Practice of Occupational Therapy. Minneapolis, MN: The American Occupational Therapy Association, 2004.
Trombly, C. Anticipating the future: Assessment of occupational function. American Journal of Occupational Therapy. 1993;47:253–257.
United States Department of Health and Human Services. Fact sheet: Protecting the privacy of patients’ health information. http://www.hhs.gov/news/facts/privacy.html 2003.
United States Department of Health and Human Services. What is the difference between ‘consent’ and ‘authorization’ under the HIPAA Privacy Rule? Retrieved on October 12, 2004, from http://answers.hhs.gov/cgi-bin/hhs.cfg/php/enduser/std 2004.
Wilson, HP. HIPAA: The big picture for home care and hospice. Home-Health-Care-Mangement-and Practice. 2004;16(2):127–137.
Wright, HH, Rettig, A. Management of common sports injuries. In: Mackin EJ, Callahan AD, Skirven TM, Schneider LH, eds. Rehabilitation of the Hand and Upper Extremity. Fifth Edition. St. Louis: Mosby; 2005:2076–2109.
York, AM. HIPAA smarts: Top 10 privacy musts. Rehab Management. 2003;16(2):44–45.