Chapter 13 Sports medicine and injuries
INTRODUCTION
Sports-related injuries have become a very common entity seen by the podiatrist. With the advent of exercise programmes, as well as amateur and professional sports, it is imperative that the practitioner has the knowledge to diagnose and treat many of the overuse and traumatic injuries seen in the foot and ankle. The continual and ever-expanding study of sports medicine now incorporates a total ‘sports medicine team’ consisting of the primary care physician, sports medicine subspecialist, physical medicine and rehabilitation specialist, orthopaedist, podiatrist, chiropractor, athletic trainer, physical therapist and massage therapist. The podiatrist is an integral part of this comprehensive, multidisciplinary team using his or her expertise of lower extremity biomechanics to offer conservative management and remedies to the injured athlete.
Many sports involve repetitive action of lower extremity joints and muscle groups, and thus overuse injuries are a common result. The recognition of the foot, ankle and lower extremity injuries, and their successful treatment, rely upon a proper history of the athlete (see Ch. 1) and a knowledge of the particular sport as well as the anatomical structures and biomechanics involved (see Ch. 15). In addition, a thorough physical examination, prudent clinical judgement and anatomically sound treatment, as well as an early and assertive physical and functional rehabilitation programme, are necessary.
ATHLETIC PROFILE AND HISTORY TAKING
When treating the athletic patient, the sports medicine practitioner should have a clear-cut understanding of the particular sport of that patient. In addition, it is imperative that the practitioner should also be cognisant of the unusual emotional, physiological, biomechanical and nutritional demands of the athletic patient. The podiatrist should have a working knowledge of the biomechanics and kinetics of that specific sport and the pattern of injury that can occur, as well as the rehabilitation exercises that the athlete should employ to return safely back to sporting activity. In addition, the practitioner should be aware of age-related injuries and their prevention and also general medical factors related to gender. For example, female triad is a term used to describe female athletes who have become too serious about exercise and sport (e.g. track stars, ballet dancers). Frequently they do not eat well and lose too much weight to maintain their perceived ‘image’ and consequently develop anorexia nervosa. As a result of eating poorly, they lose fat from their bodies and develop amenorrhoea, bone density loss, and osteoporosis.
The main focus of the podiatric sports medicine specialist should be to treat the athlete conservatively, avoid surgery whenever possible, and have the athlete return to sports competition healed, and in better condition than before the injury. Special attention should be directed towards improving the athlete’s strength, flexibility, proprioception, balance, alignment, power and biomechanical function. There should be good communication between the sports medicine specialist and the athlete, creating an awareness of the mechanism of injury and how that injury can be prevented in the future.
The following questions may be helpful in gaining a specific understanding of the athletic patient:
Box 13.1 suggests questions that should be asked when taking a history from an athletic patient.
Box 13.1 Taking the history of the sporting patient (after Boyd & Bogdan 1997)
Training history
Running shoe history
Injury-related history
Past treatment history
There are a variety of sports injuries that may be categorised as acute, chronic but improving (overuse) or chronic and not improving. An understanding of tissue response to trauma is helpful when creating an appropriate treatment plan and anticipating the eventual outcome (Frederson 1996). The aetiology behind the injury may be due to a number of factors: age, physiological preparedness, psychological dependency and, of course, biomechanical considerations.
An acute injury or traumatic injury occurs when an episode stresses tissue beyond its normal physiological limits. These injuries can affect a variety of tissues and anatomical sites, but they all share a common aetiology: repetitive trauma that overwhelms the tissue’s ability to repair itself (Herring & Nelson 1987). For example, a tendon ruptures when its tensile strength is exceeded. A ligament ruptures when the normal range of motion of a joint is exceeded. A sprain occurs when there is disruption of the ligamentous structures surrounding the joint. An inflammatory process that usually lasts 24 hours – and is characterised by vasodilatation, local necrosis of tissue, and the release of inflammatory cellular elements such as prostaglandin, serotonin and histamine (Subotnick & Sisney 1999) – follows acute injury. Factors in inflammation can be classified into three categories: vasoactive substances, chemotactic factors, and agents leading to cell and tissue damage (Rodman & Schumacher 1983). After acute injury, the initial inflammatory phase is best treated with the mnemonic RICE (Rest, Ice, Compression, Elevation).
Knowledge of how the patient treated the initial injury, and how that treatment may have affected the condition, is imperative. With early treatment, the practitioner and athlete can reduce the undesirable effects of the acute inflammatory phase. Applications of ice decreases pain and inflammation; this allows for early return to range of motion. After the initial vasoconstriction from the use of the ice, a secondary vasodilatation occurs. When combined with early range of motion, and decreased pain, a clearing of the inflammatory cellular elements occurs, thus leading to a decrease in local necrosis. Non-steroidal anti-inflammatory drugs (NSAIDs) are also helpful in decreasing the prostaglandin release, and allow for pain-free range of motion, providing for an early recovery (Aronoff 1982, Obel 1982, Weissman 1982).
CHRONIC OR OVERUSE INJURIES
Overuse injuries are common in serious athletes and the everyday aerobic exerciser. When analysing the biomechanical factors of aerobic sports, it is easy to see why damage to tissues from cyclic overloading occurs. It has been shown that 30–50% of all sports injuries are due to overuse (Orava 1980b, Renstrom & Johnson 1985). In overuse injuries the cumulative effects of repetitive force lead to microtrauma, which triggers the inflammatory process. Inflammation, although a necessary component in the healing process, can become a self-limiting entity, which can lead to chronic inflammation and eventual destruction of surrounding tissues. Therefore, it is essential to minimise the chronic inflammation so as to prevent repetitive overuse injury or new acute injuries.
When the patient ignores the signs and symptoms of overuse injury (stiffness, soreness, increased temperature of the affected area), and continues to participate in his or her sport despite the injury and advice against further activity, a more serious injury can develop. The concept at this point is to treat the patient aggressively with rest, ice, compression, elevation and cessation of the sport that caused the injury. This is followed by a combination of training and physical therapy to decrease the inflammation, and increase range of motion, while preventing further injury.
The tissue most commonly affected by overuse injuries is the musculotendinous unit. According to Barfred (1971) a tendon is most likely to be injured when:
During athletic sport participation, when maximum effort is attained, these conditions usually exist. In the case of tendons, the tendon sheath or paratendon may also be involved. As a result of chronic inflammation of the tendon, tenosynovitis, or tendinitis, can occur – leading to a local degeneration and even recurrent injury to the previously damaged tendon and resulting in a partial or even complete tendon rupture.
Bursae are located at sites of friction between tendon and bone, or skin and bone. When a bursa is subject to repetitive trauma due to overuse, it may become inflamed, thus causing effusion and thickening of the bursal wall. The latter is seen clearly in the retrocalcaneal bursitis that commonly develops from shoe irritation.
Bone, which has tremendous strength, is dependent on the forces placed upon it. Wolff’s law states that bone is laid down where needed and resorbed where not needed. Loads can be applied to bone in five different directions: tension, compression, bending, shear and torsion.
For the athlete, a stress fracture may be the result of the bone’s resorptive process exceeding its reparative process. When osteoclastic breakdown is greater than osteoblastic development weakness will occur, resulting in a stress fracture. In the athlete, the stress fracture is the epitome of an overuse injury and, as such, signals the need for an investigation into training habits, equipment and athletic techniques (De Lee et al 1983).
Bone may fracture as a result of a single, large force, or a number of repetitive, smaller forces. In endurance sports, such as running, which requires repetitive impact movement, the constant force on bone creates a remodelling process, which eventually results in increased bone strength in the direction in which that force is applied. The ability of the bone to withstand repetitive loading depends on the amount of the load, the number of repetitions, and the frequency of the loading. When the fatigue process outstrips the bone reparative process, a stress fracture will usually occur.
Physical factors
One theory, stated by Nordin and Frankel (1980), is that during continuous strenuous activity muscles fatigue. As the muscles tire they become less able to absorb energy and reduce the stress that is transmitted to the bone. This altered stress distribution allows abnormally high forces to be transmitted to bone, and a stress fracture may develop. A second theory, outlined by Stanitski et al (1978), is that the force of the muscles themselves acting on their attachments to the bone creates the repetitive stress that eventually leads to the failure of the bone. In 1855, Briethaupt, a Prussian military physician, first described swelling combined with foot pain in young military recruits unaccustomed to the rigours of basic training. These injuries were later described as ‘march fractures’ following their radiographic analysis (Markey 1987).
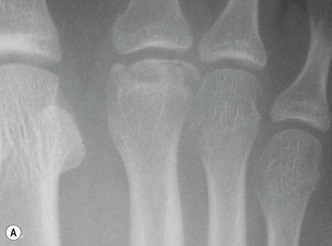
A stress fracture of the metatarsals is not evident for 2–3 weeks following the injury. The typical clinical picture will be that of swelling seen on the dorsum, redness, and discomfort overlying the involved metatarsal. There will usually be extreme pain elicited on direct digital pressure. Upon creating motion to the metatarsal, pain will be enhanced even further. As a general rule, when in doubt the clinician should suspect a stress fracture even without radiographic evidence until proven otherwise (see also Ch. 22).
Cartilage is composed of collagen, a proteoglycan gel, cells, and 60–80% water. In adults, cartilage contains no blood vessels, lymphatics or nerves. Because of its high metabolic activity, particularly in the production of proteoglycans, the ability of cartilage to repair itself is quite limited. After injury, rather than reproducing hyaline cartilage, the tissue that is synthesised is primarily fibrocartilage. Joint cartilage is normally lubricated and protected from injury by two different mechanisms (Rodman & Schumacher 1983). The hydrostatic mechanism prevails during high loads and at high speed. The second mechanism, the boundary surface phenomenon, occurs during low loads and at low speeds. Cancellous bone helps in the protection of the cartilage by its ability to deform in response to stress. However, when these mechanisms fail damage to the cartilage can occur.
Nerve tissue in the foot is also subject to overuse injury. Large-diameter myelinated peripheral fibres are at risk of compression. In the sporting patient, repetitive loading and motion direct trauma, decreased flexibility, and pathobiomechanics have all been involved in nerve entrapment. Particularly common in the runner, is tarsal tunnel syndrome, which may involve one, two or all three branches of the posterior tibial nerve.
Associated with equinus, or prolonged forefoot strike, intermetatarsal stress may result in perineurofibrosis, producing pain, tingling, numbness and burning from an interdigital neuroma.
With chronic overuse injuries, the question to be asked is: why has the condition not resolved, even when the patient has rested for a prolonged period of time? Factors leading to overuse injuries can be divided into intrinsic and extrinsic categories (Renstrom & Johnson 1985) (Box 13.2).
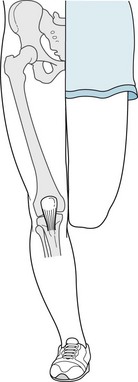
Combined with excessive repetition and impact, these intrinsic factors can lead to breakdown and injury. Malalignment, due to excessive pronation, tibial varum, genu valgum, underlying degenerative joint disease, and other structural abnormalities can lead to abnormal loads on joints, articular surfaces and soft tissue structures. Other intrinsic factors involved in the sports participant are muscle weakness and poor flexibility. As a result, atrophy of muscle groups can occur quite quickly and can be subject to re-injury unless those muscle groups are re-strengthened. When muscle tears or sprains take place scar tissue adhesions will be seen in the form of swelling and stiffness, and quite often instability and weakness. Other biomechanical factors, such as limb-length discrepancies, equinus and lack of flexibility associated with tight muscle groups, can also contribute to chronic recurrent injuries (Fig. 13.1).
Psychological factors
It has been considered that sports and exercise are endeavours for children, adolescents and young adults. However, with the exercise phenomenon explosion starting in the 1970s and 1980s, people from childhood to the age of senior citizens have discovered the physical and psychological benefits of exercise. And with the ‘addicted’ generation, attention now also focuses on psychological issues, such as exercise dependency, overtraining, motivation, injury acceptance, social factors, and burnout.
Studies have shown the positive effects from exercise on the mental status of athletes and those who exercise. Hughes (1984) reported that in more than 1000 studies exercise had a positive effect on the participants. A study by Steptoe et al (1989) indicated that moderate aerobic workouts alleviated psychological tension in both normal psychologically healthy people and in those who suffer from moderate anxiety – whereas non-aerobic exercise, such as weight or flexibility training, produced no such effect in either group.
On this evidence, the public should be highly motivated to participate in sports, and be exercisers; however, a study in 1986 showed that in the USA less than 20% of adults aged 18–65 years exercised at sufficient levels. By 1992, the level had increased to only 25% (Le Unes & Nation 1989). Practitioners can provide to the public a means to prevent injury, allowing the participant to continue to exercise injury-free and pain-free. The adult athlete must accept the fact that they will not be able to perform at a similar level as when they were young, and that exercise will continue to offer benefits, and help to increase longevity.
Fear of injury is one of the greatest concerns of most athletes. An estimated 17 million sports-related injuries occur yearly among American athletes (Heel 1993). It is imperative that the sports medicine practitioner or personal trainer helps people to understand that the physical and psychological benefits of activity far outweigh any risks to the body (Dulberg & Gueally 1999).
When injuries do occur the athlete must be able to deal with the physical injury, but also to cope on the psychological level. Once the participant is faced with a long-term injury there may be an initial emotional downturn which, if not recognised early, may eventually turn into a case of sport depression and withdrawal. After injury, the athlete goes through five stages, similar to the grieving process for a friend or relative (Heel 1993). Initially, the athlete experiences denial and disbelief over what has happened. Anger then sets in, followed by downplaying the severity of the injury, leading into the next stage, namely depression. Finally, the athlete comes to accept the true extent of the injury and at last the hope for a committed effort at rehabilitation will begin. Post-injury, fear and anxiety may be the major problem, even though physiologically the athlete is fine. The problem is a condition known as ‘phobic response to injury’, which can decrease performance and increase the risk of re-injury (Dulberg & Gueally 1999). Sports practitioners can offer support for athletic patients and help them to promote their return to active participation and prevent injuries.
Patient constraints
Once the sports participant has been injured the practitioner must create a treatment plan that is realistic, so that the patient will be compliant, and complete the treatment in the prescribed time period.
Rest is essential, to allow the healing process to begin and continue through the proper course. Occasionally, a non-impact cross-training regimen (swimming, water jogging, water aerobics, elliptical walker) may be prescribed to allow the participant to continue cardiovascular workout yet avoiding re-injury or further injury.
Nutrition is another important component for both the healthy participant and the injured exerciser. In addition to a balanced diet, nutritional supplements are important to support optimal function. Hydration is just as important to maintain tissue well-being. Water constitutes the majority of body tissue and is responsible for 60% of the average adult’s body weight. It is recommended that a typical adult should drink 8–12 glasses of water each day. A simple way to determine how much water should be ingested each day is to calculate two-thirds of body weight in pounds and drink that number of fluid ounces of water per day. As body weight increases, so does the fluid replacement requirement. Exercise generates oxidative stress via free radical toxins that can inflame and irritate tissues, and may increase potential for injury. After injury, damaged tissues under repair will have greater nutritional requirements and will need additional vitamin and antioxidant intake. Antioxidant supplement would include the regular use of vitamins C and E, β-carotene, zinc and selenium to the recommended daily dose.
To summarise, following diagnosis, a treatment plan (Box 13.3) is initiated, with a follow-up programme (consisting of weight training, cross-training, and rehabilitation). Attainable goals should be laid out for both the participant and the practitioner, with a reasonable timetable for return to activity. Finally, a prognosis is formulated. After the patient’s return, there are four possibilities for the patient’s condition:
Box 13.3 Treatment list (Boyd & Bogdan 1997)
If the patient is completely better, a gradual return to activity is essential.
RUNNING
The four phases of running
Subotnick (1999f) describes four phases of development that the majority of runners pass through:
 minutes/mile. The participant enjoys the sport and finds that it maintains weight control. They find they have more energy at the end of the day, a better mental attitude, and find that running gives them the benefits of aerobic fitness and makes them feel better in general.
minutes/mile. The participant enjoys the sport and finds that it maintains weight control. They find they have more energy at the end of the day, a better mental attitude, and find that running gives them the benefits of aerobic fitness and makes them feel better in general. -minute mile pace. They no longer have that great desire for serious competition but rather have matured into a more sensible competitive mode that helps to avoid injuries. These patients are very cooperative, and quite compliant post-injury, particularly during rehabilitation.
-minute mile pace. They no longer have that great desire for serious competition but rather have matured into a more sensible competitive mode that helps to avoid injuries. These patients are very cooperative, and quite compliant post-injury, particularly during rehabilitation.The walking–running cycle
Depending upon the sport in which the participant engages, they utilise either the entire walking and running cycle or parts of these cycles (see also Ch. 15). In the case of basketball, dribbling and driving to the basket may involve a quick sprinting run followed by a vertical leap. In alpine skiing, a down-weighting of the feet and legs, which is then followed by up-weighting, translates into a flatfoot on the skis (pronation) followed by a rolling outwards of the foot on the skis (supination). The repetitive action of the lower extremities that occurs during walking or running constitutes the gait cycle. Because the majority of sports require some form of running, it is essential that the practitioner interprets the gait cycle and how it affects the foot and lower extremity.
Walking gait differs from running gait in several ways. Walking is exhibited by a heel contact, midstance (flat foot) and propulsive phase (toe-off), with a base of gait approximately 5 cm between the malleoli (see Ch. 15). With slow walking speed there is a short period of swing phase; however, as walking speed increases there is an increase in swing phase. The duration of double support decreases as walking speed increases, and eventually is eliminated with the transition to running (Bates & Stergiou 1999b). As walking speed increases the contact phase shortens, and as the transition to running occurs the double support phase is eliminated completely, and is replaced by an airborne phase where neither foot is on the ground. It is estimated that the support phase varies from about 60% for slow runners, and 40% for fast runners. The non-support periods range from 40% and 60%, respectively. A single step concludes when the opposite limb makes contact with the ground about midway through the forward swing subphase at about 70–80% of the limb cycle.
To understand locomotion and the gait patterns of walking and running it may be observed that in walking gait the foot and lower limb is always in contact with the ground, whereas in running there is a period of time when the body is ‘airborne’ with both feet off the ground. In locomotion, there is a mechanical interaction between locomotor structures and an external force – that of gravity. The final product is forward physical movement, and postural stability. Thus, in running, at the heel contact phase the supporting foot must move beneath the centre of mass of the body for stability. In running, the body’s centre of gravity must travel in a more vertical direction than it does in walking. During the running heel contact, the base of gait is reduced, creating a varus attitude, thus, compelling the subtalar joint to increase pronation to allow the foot to plantar flex (Fig. 13.2). Locomotion comprises a number of important components; namely, stride length, stride frequency, and their resultant speed. It has been estimated that up to two to three times the body weight passes through the loaded limb during the contact phase of walking. In running, that figure can rise to as high as three to six times the body weight.
Energy transfer takes place when there is a change in frequency of the foot impact, as well as the stride length. It has been shown that at lower or higher speeds greater energy per strike is necessary compared to an intermediate speed. In Rolston’s (1993) article on the energetics of human walking, he showed that plotting the energy expenditure versus speed in walking would result in a parabola. The parabolic function demonstrates that there is an optimal minimum at which walking is more efficient than the participant’s preferred speed. There is a period immediately after the transition from walking to running, in which energy expenditure will fall to an optimal minimum where frequency and stride length work in harmony to the body’s best advantage (Hreljac 1993).
In running, deceleration occurs every time the foot makes contact with the ground. Immediately after contact the forward velocity of the body decreases during a ‘breaking phase’ of action. In running, this critical phase causes the centre of gravity to be elevated, creating additional potential energy, thus a greater vertical velocity at contact, with even higher kinetic energy. Thus, a braking action of the limb occurs in addition to the impact occurrence of the body in regard to ground reactive forces. Therefore, running is a combination of actions of the lower extremity that involves maintaining forward motion while simultaneously accentuating the centre of gravity against internal and external resistance. In addition, the lower extremities must also support the body’s weight and absorb the impact forces that transcend up the leg during the contact phase. As the speed of the runner increases, energy production and usage increases due to increased forward propulsion and, in addition, muscle contraction that must decelerate the body while simultaneously diffusing impact forces.
Shock occurs after immediate impact of the heel striking the ground as the stance phase of gait begins. As mentioned before, at heel strike ground reaction forces are transmitted into the heel as shock. This shock is usually absorbed and dissipated by the normal motion of the foot and lower limb. It is when that motion is restricted within certain joints of the lower extremity that abnormal degrees of shock are transmitted through the foot and leg and directly into the trunk. One of the key functions of the subtalar joint is to absorb shock at heel contact. The subtalar joint pronates quickly to absorb some of this shock directly. Again at heel strike, additional shock is absorbed by knee flexion. However, the knee cannot flex rapidly unless the tibia can internally rotate faster and farther than the femur. Subtalar joint pronation allows the tibia to rotate faster and farther than the femur, thus unlocking the knee so that it can flex and assist in shock absorption (Steindler 1955). Thus, the subtalar joint is the main means of shock absorption for the foot and lower limb at heel strike. In the runner, who demonstrates increased stride and greater acceleration, additional ground reactive forces will be transmitted through the heel as it hits the ground. The subtalar joint will demonstrate increased pronation, thus increasing the ability of the foot and limb to absorb this increased amount of shock. Therefore, adequate shock absorption cannot occur at heel strike unless subtalar joint pronation can take place (Root et al 1977).
In addition, muscle function is also influenced by the action of the subtalar joint. When subtalar joint motion is limited, a ripple effect of abnormal muscle function can occur. This will impede knee flexion, creating increased impact shock into the lower leg and knee. The action of the posterior tibial muscle at heel contact is to decelerate subtalar joint pronation. However, when the foot and subtalar joint are completely pronated, the posterior tibial muscle will contract with its effect more proximally, rather than distally. Therefore, the knee will remain extended, limiting both its ability to flex and to act in shock absorption. In running, the knee flexes through 35–40° at contact, compared with only 15° when walking.
Subtalar joint pronation lasts longer in the running gait cycle, and readjustment of the foot into supination occurs much later – approximately 70% of the support phase. When the foot demonstrates abnormal pronation of the subtalar joint, pathological shock will develop. The runner or walker experiences increased impact shock up the limb, through the pelvis, and into the spine. This can be prevented when the participant shortens his or her stride, and utilises a flattened foot to eliminate the heel strike, and the remainder of the contact phase. For the foot to become a rigid structure for propulsion it has to function in an adaptive manner longer in the gait cycle, and resupination must occur much sooner.
During propulsion, the centre of gravity must be transferred toward the opposite foot. During transference, force is diminished while motion is maximised. At the end of propulsion, weight is transferred completely to the opposite foot. In walking, the centre of gravity moves over the support limb, whereas in running the limbs move beneath the centre of gravity, thus cancelling out any transference.
In addition to visual observation of walking and running gait, computerised force data sensor systems can be used to measure the distribution of pressure at specific areas on the plantar aspect of the foot. Henning and Milani (1995) used a discrete pressure sensor system in conjunction with a force platform to examine the effects of shoes on ground reactive forces. With computerised pressure technology, the clinician can evaluate the participant’s gait in any type of environment. In addition, specific areas of pressure can be determined, including the specific point of heel strike, adaptation and propulsion. This information can be helpful in determining whether the participant is in need of an orthotic device and, when worn, obtain data on the device relative to the foot and/or shoe.
Often, walking and running disorders can be identified using a simple video system. An inexpensive, high-quality digital video camera, in conjunction with a computer and appropriate software can be used to record the participant’s gait pattern. The subject can be evaluated in slow motion or freeze-frame to analyse any potential faults in the gait pattern such as leg-length discrepancy, shoulder drop, internal or external femoral rotation, high degrees of tibial varum, or excessive pronation or supination. With slow motion, and having the capability to freeze frame the subject, the clinician can determine specifically when the heel strikes the ground, or whether there is an excessive propulsive phase (equinus) and/or a functional hallux limitus. The recording can also be used to measure stride length, the position of the foot at heel contact, base of gait, and position of the foot during toe-off. This can be performed either on a treadmill, or simply by walking or running down a corridor. This system can be extremely helpful in the education of the patient, in pointing out specific areas of concern, and when walking or running styles can be altered or corrected. In addition, it is a great tool for determining whether an orthotic device might be necessary, while simultaneously educating the patient as to its need and use.
Marathon running
The marathon is a gruelling 26.2-mile endurance race. As one of the original Olympic events, it continues to rank as one of the most challenging of all track events. The popularity of the marathon has transcended from the elite athlete to the ‘weekend warrior’. Men and women of all ages have focused in on the marathon as the ultimate challenge to compete in and to complete.
During the training period, or before, during or after the marathon, many runners suffer from some type of overuse injury. Some of these runners never even make it to the starting line due to overtraining, running on hard concrete surfaces, worn-out shoes (Fig. 13.3), poor biomechanics, lack of flexibility or recurrent injury.
Many of the overuse injuries that have been mentioned previously will now be examined individually.
CASE STUDY 13.1
INSERTIONAL CALCIFIC TENDINOSIS FRACTURE
A 57-year-old male runner first presented with shooting, burning, pulling pains on the posterior aspect of his right heel of 2 months duration. The patient was training for the Houston Marathon in January but was unable to participate in the race because of the pain and took time off, resuming running in March, starting with 3 miles/day. He again experienced soreness in the same region and took 6 weeks off from running. However, when he resumed running the pain started again. His first steps in the morning were painful.
The patient has been running for approximately 5 years and has completed two marathons in 5.5–6 hours.
The patient also indicated that he had suffered from other chronic injuries along the right lower extremity ranging from piriformis syndrome to plantar fasciitis, a groin pull and ankle pain. All of these have been resolved.
The patient had prescription orthotics fabricated 2 years ago to help correct a right out-toeing. He goes to the gym 6 days a week to cross-train, runs two times a week and also does weight lifting.
Impression. Achilles tendinitis on the right foot. There is also a limb-length discrepancy, with the right leg being longer than the left, and a collapsing pes plano valgus foot type.
The patient was re-casted for new orthotic devices to treat the chronic left heel pain and prescribed a night splint, NSAIDs and ice massage.
BIOMECHANICAL EVALUATION
Vascular and neurological examination – all seemed normal.
Hip range of motion 90° external, 45° internal, equal and symmetrical, bilateral.
There was significant limb-length discrepancy, the right leg being 2 cm longer than the left leg. His gait was abducted with significant medial column prolapse in both stance and gait but he denied pain on the posterior central portion of the calcaneus and in the plantar fascia. There was no pain in the midbody of the Achilles tendon.
ONE YEAR LATER
The insertional Achilles tendinitis flared again. The patient has run three previous marathons, and recently ran the Great Wall of China Marathon. He experienced no pain during the run but now complains of pain during his first steps in the morning and when he steps out of a car. The pain diminishes after one minute of walking. There is pain along the medial–posterior right heel.
Bilateral lateral-projection radiographs revealed a right fracture insertional calcific Achilles tendinosis ‘spur’, with fragmentation. There was an infracalcaneal exostosis, and a possible previous fracture.
On the left foot there was a retrocalcaneal insertional calcinosis ‘spur’ but no fracture.
CASE STUDY 13.2
RUPTURED ACHILLES TENDON
A 69–year-old woman complained of retrocalcaneal insertional calcific Achilles tendinosis. The patient had run/walked numerous marathons, and was participating in the Alaskan Marathon when she began to experience excruciating pain. One month ago, after the race, she stepped off a kerb and began to experience swelling along the posterior tibial and flexor hallucis longus tendons of the right foot, and a strain of the gastrocnemius–soleus. She has been receiving physical therapy and describes pain and tenderness along the posterior tibial and flexor hallucis longus tendons, and the gastrocnemius–soleus muscle group. She also described pain at the posteromedial aspect of the insertion of the Achilles tendon in her right foot.
MEDICAL HISTORY
The patient had hypertension, arthritis, seasonal allergies, hypercholesterolaemia and gout.
Past lower extremity history. Posterior tibial tendinitis, tarsal tunnel syndrome, plantar fasciitis, metatarsalgia and sciatica, on the left foot. She was taking a number of systemic medications: Allopurinol, Avapro, Lopid, Clarityn, Zyrtec, Aleve.
Social history. A retired nurse who enjoys walking and jogging for fitness. Denies smoking.
PHYSICAL EXAMINATION
There was pain at the insertion of Achilles tendon and a palpable exostosis on the retrocalcaneal region of the right foot. There was some weakness and pain upon dorsiflexion of the right foot. There was oedema along the posteromedial aspect of the calcaneus and along the medial aspect of the right ankle. The gastrocnemius–soleus muscle group was tight and there was pain along the course of the posterior tibial and flexor hallucis longus tendons. The patient was unable to perform a single heel-raise test.
LOWER EXTREMITY PHYSICAL EXAMINATION
The patient is 5 feet (152 cm) tall and weighs 124 pounds (56 kg).
Vascular examination. The dorsalis pedis and posterior tibial pulses were recorded as +2/4 bilaterally; the capillary filling time was 3 seconds, the toes were warm and the colour was normal; there were no varicosities.
Neurological examination. There was mild tingling along the posterior tibial nerve on the left foot; sensation was good, equal and symmetrical; Achilles and patellar deep tendon reflexes were normal; the plantar response was normal.
LOWER EXTREMITY BIOMECHANICAL EXAMINATION
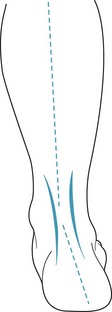
There was bilateral tibial varum, some collapse of the midtarsal joint and the longitudinal arch with medial column prolapse and talonavicular prolapse.
The foot type was pes planus, the first ray was hypermobile, and ankle joint dorsiflexion was normal. The stance position showed mild abduction with calcaneal eversion.
| Subtalar inversion: | R18°;L 30° |
| Subtalar eversion: | R8°;L 7° |
| Subtalar neutral: | R3°;L 3° |
| Forefoot: | R2°;L 2° |
X-RAY EXAMINATION
Insertional calcific Achilles tendinosis with bone cystic changes, posterosuperior aspect, and right calcaneus.
Loose body bone fragments, with spur formation at the insertional level of the Achilles tendon.
MRI FOOT AND ANKLE
Presence of focal swelling, with partial disruption of the distal portion of the Achilles tendon near the attachment of the tendon to the posterior aspect of the calcaneus.
No joint effusion. The fibular (peroneal)s, extensor and flexor tendons were normal, with no evidence of inflammatory changes or disruption.
SURGICAL INTERVENTION
Resection of insertional calcific Achilles tendinosis
Resection of posterosuperior ‘step’ of the calcaneus
Repair of partial rupture insertion of Achilles tendon
Reattachment with absorbable anchor screw with absorbable suture
Non-weight-bearing posterior splint cast was applied, and with crutches the patient was able to be ambulant postoperatively.
CHILD AND ADOLESCENT SPORTS
It is estimated that 30 million children and adolescents in the USA participate in organised sports. With this change of focus of children in sport, the number of overuse injuries has increased. Children participate in a particular sport not just for one season but often for many seasons – and in some cases all year round. It is not uncommon to see youngsters and adolescents engaged in a variety of sports (e.g. soccer, football, rugby in the autumn; basketball, swimming, indoor track, hockey, volleyball, gymnastics in the winter; baseball, lacrosse, soccer, cross-country-track in the spring; and swimming, soccer, baseball and running in the summer). Some children who excel in a particular sport may participate in that activity all year round, as seen in gymnastics, ballet dancing, basketball, soccer and baseball. One of the main questions that parents have to ask is: is my child ready to participate in organised sports? There are two aspects to a child’s readiness: motivational readiness and maturity or cognitive readiness (Dulberg 1999). Many times the child may be physically ready to master the skills of the sport but may not be intellectually prepared to participate. Determining the right age for the child to participate in a particular sport can often be difficult. Physical-contact sports suitable for one young person who is more physically mature may not be right for another. Similarly, choosing to go on point for one young ballet dancer may be deleterious for another young ballet dancer.
With the increased participation of younger athletes in organised athletic and competitive sporting programmes, there has been a change in the pattern of injuries observed (Maffulli et al 1992, Sterling et al 1991) as well as an increasing number of injuries (Kannus et al 1988, Micheli 198, 1987, Micheli & Ireland 1987, Micheli & Smith 1982). These include microtrauma overuse injuries as well as acute macrotrauma injuries.
Overuse injuries are not only common in adult athletes. With the volume of training and repetition now being undertaken by many young athletes, normal repetitive processes are eventually overwhelmed, leading to tissue inflammation (Herring & Nelson 1987). In addition to tissue areas that are subject to overuse injuries (i.e. tendons, bones, tendon–bone junctions), other areas in the young athlete also vulnerable to overuse injury include growing tissues. Growth cartilage, found in the youngster at the epiphyseal plate, the articular cartilage of the joint surface, as well as the apophyses at the insertion of the muscle tendon unit, are at risk of overuse injuries. The traction apophysitises involve growing tissue and are particularly evident during the rapid growth during adolescence (Micheli & Fehlandt 1992). Injuries at the traction apophyses may be the result of an acute macrotrauma, creating an avulsion of a portion of the apophysis. The repetitive microtrauma to the youngster will present with pain, swelling, as well as ‘apophysitis’ where bony or cartilaginous overgrowth occurs. Osgood–Schlatter’s disease of the tibial tubercle apophysis is probably one of the most commonly recognised of these injuries in youngsters. Sever’s disease or calcaneal apophysitis is another common complaint seen in the child and adolescent. It is usually seen between the ages of 10 and 12 years in boys and girls, occurring more frequently in boys.
A significant amount of growth takes place between the ages of 11 and 15 years, and this is quite often rapid and in spurts. Bone is undeveloped and is not completely ossified until 18–21 years of age. The immature bone can be stressed when muscles are relatively overdeveloped through excessive activity (Ch. 12). A frequent site of injuries in children is where muscles and ligaments attach to bone. Because bone grows faster than the soft-tissue structures mature, frequently there will be restriction in motion as well as muscle imbalances for periods of time while soft tissues adapt to the additional bone development. During puberty, the growth plates are especially soft and weak, and are subject to injury at the end of the growing period as they become more rigid. As the youngster matures, the body changes shape, muscles become bigger, bones become longer and weight increases. Adaptation to these changes, as well as a change in coordination, also takes place as the young athlete matures.
The patient complains of pain located in the posterior medial aspect of the heel which is exacerbated by sports activities where running and high impact are involved (e.g. soccer, basketball, baseball, football and tennis). Hard surfaces can also contribute to the impact shock, and contribute to the complaint. Aetiological factors that are often seen include repetitive microtrauma, a sudden adolescent growth spurt, a tight gastrocnemius–soleus muscle group, a tight Achilles tendon and weak dorsiflexors. Biomechanical factors are also contributory; for example, genu valgum, excessive pronation of the subtalar joint and forefoot varus. It is difficult to make a clear-cut diagnosis of Sever’s disease because radiographs show only increased density and a maturing apophysis that may reveal lines that could mimic fractures (see also Ch. 4). Treatment usually begins with rest from the affected sport for a period of time until pain has subsided significantly. In addition, treatment should include exercises for the plantar flexors to improve dorsiflexion of the ankle as well as strengthening exercises for the dorsiflexors of the ankle.
A stretching programme involving the gastrocnemius complex, Achilles tendon and hamstrings is also advised. For children whose feet pronate excessively, and who have tight Achilles tendons, prescription orthotic devices and heel lifts are also helpful, particularly in the pes plano valgus individual. In severe situations where conservative treatment has been exhausted, lower-leg cast immobilisation may be necessary to rest the inflamed apophysis. Another injury to the apophysis that has been described in youngsters is at the base of the fifth metatarsal (Lehman et al 1986).
Another site for traction apophysitis is the tarsal accessory navicular. It is suggested that the formation of the accessory navicular may be the result of an apophyseal separation, similar in nature to Osgood–Schlatter’s disease, at the insertion site of the tibialis posterior tendon–muscle unit. Children who suffer from painful accessory navicular bones experience inflammatory traction apophysitis at the insertion site of the posterior tibial tendon into the accessory navicular and the navicular. These children usually demonstrate severe pronation, secondary to a pes planus or flat foot. In cases where there is a hypertrophied navicular, mechanical irritation over the bony prominence may be the cause. With pain associated with traction apophysitis, biomechanical correction, and support of the longitudinal arch and tendon with the use of prescription orthotic devices has proven to be very successful. In addition to anti-inflammatory medications, strength and flexibility exercises directed towards the tibialis posterior muscle–tendon unit, as well as heel walking, are also helpful. For the youngster who suffers from mechanical irritation of the navicular bone, as in skiers, skaters, snow-boarders and horseback riders, a tight-fitting, unrelenting boot is often responsible. The use of accommodative felt oval cavity pads (Ch. 16), or those made from ethyl vinyl acetate (EVA) or polyurethane (Ch. 17), as well as boot modification (Ch. 18), can be very helpful.
For youngsters who suffer from consistent painful accessory navicular bones, aggressive conservative treatment with cast immobilisation is very helpful in relieving pain. Once the cast has been removed, stretching and strengthening exercises are resumed and orthotic devices employed. For those children who have not responded well to conservative management, surgical intervention is recommended. This takes the form of resection of the hypertrophied navicular, with excision of the accessory navicular when present, combined with a transposition of the tibialis posterior tendon in a more mechanically efficient location inferior to the navicular, as described by Kidner (1929). It is not uncommon for a child to be out of sports training and/or competition for up to 6–9 months postoperatively.
When traction apophysitises are recognised early, and the clinician institutes rest, therapeutic exercises and biomechanical correction, these overuse apophyseal injuries can be managed conservatively, allowing the youngster to return to his or her full sports programme. However, in cases where these complaints are neglected, or treated minimally, symptoms, deformity and disability can continue into adulthood.
Some youngsters, as with their adult counterparts, are at high risk of injury. These young athletes, due to morphological difficulties, may break down even with minor trauma. Some of these participants may truly be ‘accident-prone’ (Lysens et al 1989, Standish 1995, Stanitski 1989). The well-trained young athlete, compared to the novice, is generally more resilient to an equivalent trauma. Standish (1995) states, that any tissue (whether bone, ligament or tendon) will disrupt only when it faces a force greater than its inherent strength.
In the child athlete eight main causative factors for injury have been identified (Betz & Klimt 1992, Boyd & Bogdan 1997):
Underlying biomechanical imbalances and weaknesses can play an important role in the onset of overuse injuries in the child or adolescent athlete. As described, excessive pronation due to rearfoot, knee or leg structural abnormality can lead to undue amounts of stress upon tissues and disturb normal alignment, thus reducing shock-absorbing mechanisms. Conservative intervention with antipronatory devices can often solve a simple biomechanically induced overuse injury. These biomechanically corrective appliances can often restore normal alignment and function to the feet and lower extremities. The common overuse injuries occurring in the young athlete include traction apophysitis (Sever’s disease), sinus tarsi syndrome, chondromalacia patellae and patellofemoral joint syndrome (where articular cartilage of the joint is damaged), osteochondritis dissicans, stress fractures, avulsion injuries, spondylosis and spondylothesis.
FOOTBALL – SOCCER
Football is known internationally, but in the USA it is referred to as soccer. Due to the popularity of the sport, the number of football injuries is high. Whereas running involves a unidirectional movement, football, like other sports, requires multidirectional movements in addition to running. In football, manoeuvring and manipulating the ball with the foot, as well as tackling to gain the ball, requires a number of motions of the foot (subtalar joint, midtarsal joint, Lisfranc joint) as well as the ankle. Flexibility is a key component due to the sprinting and changes in direction involved in this sport. Strengthening and conditioning are integral components in soccer. Thus weight training may improve the strength and endurance of the participant, but at the cost of flexibility. It is imperative that the coach or trainer supervises properly to avoid a loss of flexibility in muscle groups.
There are a number of common football injuries incurred from the youth league age to the professional. These injuries include traction apophysitis, which is commonly seen in the active, growing child. Injuries at the traction apophyses may be a result of macrotrauma, in which avulsion of a portion of the apophysis takes place, or an effect of repetitive microtrauma (soccer cleats, hard soccer fields, increased training and running).
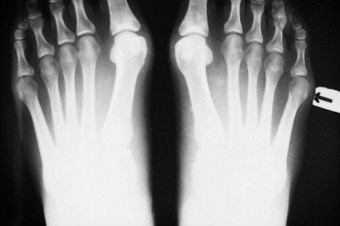
Commonly seen in football are injuries to the nail and nail plate, as well as ingrown toenails, blisters and tinea pedis (athlete’s foot) infections. Severely involuted nails can be due to a tight toe box in a soccer cleat. In many cases a patient who pronates excessively and who has hallux abductus will develop a close approximation to the adjacent second digit, and with forefoot shoe pressure can also develop an involuted tibial or fibular border of the hallux nail. On occasion these involuted nail borders, complicated by paronychia, may require partial avulsion with or without matricectomy (see Ch. 23).
Plantar fasciitis is a common chronic overuse injury resulting from microtrauma and microinflammation of the plantar fascia. It is located at the calcaneal origin and is usually involved with the medial band of the plantar fascia. In football, due to the stop and run motion, chronic repetitive stress can occur, and this can lead to chronic irritation and inflammation of the plantar fascia. After sudden, violent or ‘explosive’ movement partial rupture of the plantar fascia can also occur. After repetitive microtrauma, eventual heel spur development may occur. Plantar fasciitis is commonly brought on in football by prolonged training sessions and playing numerous games. Another contributing factor is that the typical football cleat does not have adequate arch support and does not have good shock-absorbing properties for the heel. Football fields may also contribute to the problem, because hard, unrelenting ground surfaces can add increased impact shock to the heel, particularly in the young football player.
Other common injuries seen in soccer play involve stress fractures of the lesser metatarsals (Davis & Alexander 1990, Stanitski et al 1978). There is no age that is immune from this overuse injury. Jones fractures and avulsion fractures at the base of the fifth metatarsal, due to traction of the fibularis (peroneus) brevis tendon, are also seen. Strains of the hamstrings and quadriceps are quite common as a result of continual contraction during play. In youngsters during their growth years, enthesitis at the attachment of these muscles to bone can also occur, particularly in shin splint areas of the tibialis anterior or posterior muscle groups, such as the soleus. Painful inflammation along the lower third of the medial tibia is often seen as a result of Sharpey’s fibres being torn away. Chronic shin splints, if left untreated, could eventually lead to medial stress fractures of the tibia as well. A direct blow to the lower leg from an opponent can lead to increased pressure of either the anterior, lateral or posterior medial compartment, and eventual compartment syndrome. Running on uneven surfaces, being kicked by an opponent, or tripping over another player, can easily lead to ankle injury. Most frequently seen is the inversion mechanism sprain as a result of supination of the rearfoot, and plantar flexion of the forefoot. Occasionally, when attempting to block a kick, and sliding the foot and leg towards the ball and ground, a medial, eversion mechanism ankle sprain can occur. Os trigonum fractures of the talus can occur as a result of the player striking the ground, in a hyper-plantar-flexing motion, with the posterior, lateral process wedged between the posterior tibial malleolus and calcaneus. Flexion of the flexor hallucis longus tendon will elicit painful symptoms at the region of the os trigonum. Achilles tendinitis, another common overuse soccer injury, is seen as a result of tight posterior muscle groups and a short/tight Achilles tendon, with a lack of flexibility and inadequate stretching. In youngsters, traction of the Achilles tendon can occur, and in adults insertional calcific tendinosis may also occur. Excessive pronation, and flat football shoes without sufficient cushioning, can also cause and aggravate the condition (Clark et al 1983, Scioli 1994, Talloway et al 1992). Patellofemoral joint syndrome is quite frequently seen in footballers, as is internal derangement of the knee ligaments. Chondromalacia may develop due to the distance run, running on hard ground surfaces, increased Q-angles and excessive pronation, all of which can lead to this overuse syndrome. Women football players with genu valgum and increased Q-angles are highly subject to this injury. Hip injuries are frequently seen, with bursitis, contusions and hip dysfunction being the typical complaints. Groin pain may actually emanate from the hip, lower abdomen and lumbosacral region, or from the groin itself (Renstrom & Peterson 1980, Taylor et al 1991).
Prevention of football injuries can be accomplished with proper supervision and capable coaching in a properly designed training programme (Erstrand & Gillquist 1983a,b). With the preponderance of youth football leagues, careful attention should be given to growing children, as well as to the intensity and duration of the training sessions. Proper football cleat selection, a pre-season training programme as well as a flexibility and stretching programme can dramatically reduce the occurrence of football injuries. Some other helpful means of preventing injuries include proper equipment (shin guards), correct training habits, proper footwear with biomechanical balanced insoles/orthotics, and pre-activity ankle-taping for those with a chronically unstable ankle. It is also important to have a certified trainer and/or sports medicine healthcare professional, and optimal field conditions (dry, level, no divots or cracks).
GYMNASTICS
Gymnastics is another sport that has seen an increase in interest in the past decade, particularly due to exposure in the amateur and Olympic ranks. About 500 BC, the Spartans gave meaning to the word gymnastics, which translates as ‘to perform exercises while naked’.
Facets of gymnastic safety include: pre-assessment of the gymnast; proper warm-up and stretching; physical, psychological and emotional preparedness of both the gymnast and the coach; and proper gymnasium design. The coaches, parents, gymnast and team physicians are all involved in the overall safety of the gymnastic participant.
There are many causes of gymnastic accidents (Wettstone 1982): horse play, failure to spot a slippery area, shoes, aggressive coaching, fatigue, lack of strength and flexibility, lack of kinaesthetic awareness, overexertion, bones, lack of fundamentals and defective equipment.
Plyometrics are dynamic exercises designed to develop power for running, jumping and throwing. These drills include hops, bounds, depth jumps, and jumping with weights and medicine balls (Dyatch Rov 1969, Miller 1980). Plyometrics are based on the principle of the stretch reflex mechanism – that a muscle contracts faster and with more force from a prestretched position than from a relaxed state. Gymnastics has specific strength and power demands, and plyometric exercises are specifically designed to meet these needs (coupled development).
Injuries to the lower extremities in gymnastics can occur on a variety of equipment, and during various movements. It has been shown that nearly all beam injuries to the non-team-level gymnasts (preparation level) occur on the high balance beam (Weider & Ganim 1982). Dismounting from the balance beam, pommel horse or rings can easily result in acute injuries such as a stress fracture, periostitis of the calcaneus, plantar fascia strains or inversion mechanism sprains to the ankle. Proper care and maintenance of these pieces of equipment can help avoid unnecessary injury. The fact that gymnasts train and perform barefooted (except when wearing ankle or foot braces) adds to the high risk of injury that these athletes face.
BASKETBALL
Basketball is physically demanding, and there is the risk of high-intensity trauma to the lower extremities. Although technically a non-contact sport, basketball could be compared to hockey or football. Quite frequently, physical contact between players, as well as between players and the court, can result in spontaneous acute traumatic injury. Overuse injuries can be the result of poor lower extremity biomechanics, shoes, practice deficiencies and other factors.
Due to the tremendous stresses on the musculoskeletal system of the lower extremity, a basketball player’s feet, ankles and knees must absorb high levels of impact shock. These muscles, tendons and ligaments are subject to constant loading forces, and the hamstring and gastrocnemius–soleus muscle groups must activate and ‘spring into action’ with every vertical leap.
Even the lower back is at risk from hyperextension during shooting and rebounding. Effective recognition and management of acute and overuse injuries will help to increase the effectiveness of later treatment and promote early return to play.
The vast majority of musculoskeletal injuries sustained by basketball players are to the lower extremity (Henry et al 1982, Messina et al 1999, National Basketball Athletic Trainers’ Association 1989–90, Ray et al 1991). As in adult players, a 1999 study of Texas high-school basketball players found that ankles were the most common sites of injury in both boys and girls. After the ankles, the next most frequent areas to be injured are the knee and groin. Injuries to the hip and lower back also occur with high frequency.
The fundamental treatment plan for basketball injuries should include the following: proper diagnosis, with early intervention, followed by aggressive treatment that will guard the basketball player from further injury, permit return to activity as quickly as possible and prevent recurrent injury. A basic treatment plan can be divided into three steps:
At the side of the court, sprains and strains are treated according to the recognised mnemonic RICE (Rest, Ice, Compression, Elevation) (see Ch. 16). Immediate application of ice will help to reduce swelling and the ensuing inflammation. Compression may be by means of a simple elastic bandage, taping, an Air Splint, an ankle brace, or a posterior splint to immobilise the injured site. Elevating the extremity will also help to minimise the swelling and reduce discomfort. By reducing the onset and extent of the swelling, recovery time can be reduced, and this also helps promote early rehabilitation.
One of the more common injuries that basketball players suffer from is toenail injury. Due to rapid acceleration and deceleration, and with twisting and changing of direction, the foot will slide forward in the basketball shoe and cause a jamming of the nail against both the upper of the shoe and the toe box. It is not uncommon for players to be stepped on during a game, and suffer from a typical subungual haematoma fracture of the distal phalanx. Injuries to the nails include ingrown toenails and subungual exostosis secondary to trauma (see Ch. 2).
Blisters are another typical problem in basketball players, usually at the beginning of the season due to friction and shearing forces on the toes and plantar aspect of the foot. Initial treatment should include draining of the blister, while leaving the blister roof in place.
Products such as Second Skin can be used for players who have sensitive skin and a predilection for abrasion and blister formation. Duct tape, which fanatical marathon runners use to prevent blisters, is another remedy that can be employed. To reduce shearing and rubbing, insoles such as Spenco, Superfeet and Sorbothane can be very beneficial. If a biomechanical problem is present wherein abnormal pronation and abduction (pivoting) of the hallux takes place, a soft prescription orthotic covered with the anti-friction insoles can provide even greater defence against blister formation. Marathon runners often apply Vaseline to the skin to reduce friction, and this has also been shown to be helpful.
Other common basketball injuries include: stress fractures of the metatarsals, sesamoids, calcaneus and tibia/fibula; fractures of the os trigonum; avulsion fractures of the navicular and of the base of the fifth metatarsal; cuboid subluxation; heel bursitis; plantar fasciitis–heel spur syndrome; anterior ankle impingement; painful accessory navicular; and ankle sprains. Other acute injuries include Achilles tendon ruptures, knee injuries, contusions to the quadriceps, and muscle pulls and tears, particularly of the gastrocnemius–soleus, fibular (peroneal) and posterior tibial tendons. Frequent overuse injuries seen in basketball include contusions and bursitis of the sesamoid bones, sesamoiditis, hallux rigidus, bunions, interdigital neuromas, Achilles tendinitis, insertional Achilles tendinitis and calcinosis formation, posterior tibial tendinitis, fibularis (peroneus) longus, brevis tendinitis and flexor hallucis longus tendinitis.
With the high incidence of injuries to basketball players, trainers and team physicians have a responsibility to prevent these injuries. Measures include proper training to take into account the fact that a National Basketball Association or college season runs for 6–9 months and that players practise continually – both during the season and in the off-season – for about 11–12 months. The amount of mental and physical stress, in addition to the physical pounding that the players experience during the game itself, can lead to injury. Other means of reducing the incidence of injuries include diet and nutrition, strengthening programmes, travel schedules (jet lag), proper equipment, and a well-designed stretching and flexibility programme.
BOWLING
It may not generally be expected that bowling would be a sport with frequent injuries. However, the movement of the bowler toward the foul line may lead to injury due to lurching or a heavy awkward gait (Wysocki 1999). When a foot does not track straight ahead with approximately 10° of abduction, balanced flexion at the metatarsophalangeal joint (MTPJ) cannot occur. As a result, the ankle changes the direction needed by this movement. Stress occurs to the foot and ankle, and eventually compensation begins, leading to overuse injuries such as medial band plantar fasciitis, posterior tibial tendinitis, ankle strain, medial knee pain, and hip and lower back strain.
TENNIS
Tennis is multidirectional, involving both forward and reverse as well as side-to-side motion. As in other court sports, many of the acute injuries in tennis involve a sudden, violent movement from a stationary position, and they usually occur when the player comes to a sudden stop to hit the ball. This can be seen in the movements of rushing to the net, covering the sidelines or retreating to cover the baseline. These multidirectional movements can lead to both acute and overuse injuries. Many of the injuries incurred in tennis involve overuse inflammatory processes; however, traumatic fractures and dislocations, as well as tears and ruptures of ligamentous and tendon structures, are often seen (Ross 1999c). Grand slam exposure, worldwide ranking, junior play, and high school and intercollegiate play have all contributed to the increase in popularity of tennis since the 1960s. Tennis is a sport that demonstrates technique, athletic ability, stamina and agility, and to this end there have been great advances in flexibility, strength training and conditioning (Hageman & Lehman 1988).
Tennis injuries of the lower leg and foot can be divided into two basic categories: acute and chronic. Most of the lower-leg injuries that occur in competitive tennis are chronic in nature and develop from repetitive stress (Leach 1988, Levisohn & Simon 1984, O’Connor et al 1992). The overuse syndrome injury that is seen in tennis, as in other sports, has a common aetiology: a repetitive trauma that eventually interferes with a tissue’s ability to repair itself (Herring & Nelson 1987). Microtrauma occurs with overuse, triggering events that ultimately can lead to tissue degeneration (Galloway et al 1992, Greenfield 1990, O’Connor et al 1992). These muscles and tendons are subject to repeated stretching and traction. As a result, a degenerative process develops, wherein the rate of tissue breakdown is faster than the rate of tissue repair. This continual stretching during play can cause fatigue, as is often seen in overuse syndrome. Because of the poor blood supply directed to tendons, repeated subintimal injury and delayed healing are very common. According to Clancy (1982), the Achilles is the tendon most commonly injured in sports.
Overuse injuries suffered by tennis players include tendon injuries, chronic Achilles tendinitis, Haglund’s deformity, with chronic bursitis, posterior tibial and fibular (peroneal) tendinitis, posterior and anterior shin splints, compartment syndromes, interdigital neuromas, chronic plantar fasciitis, hallux limitus/rigidus of the first metatarsal phalangeal joint, acute and chronic sesamoiditis, as well as subungual exostosis, with nail deformities. These overuse injuries occur as the musculoskeletal system becomes more and more fatigued due to increased and repeated loads of stress, followed by failure.
In tennis, overuse injuries that may not force the player out of competitive play but will affect performance can be categorised as the ‘lesser injuries’. These entities develop as a result of excessive pressures on bony prominent areas, or as a result of the foot or toe(s) jamming against the shoe or toe box – ‘tennis toe’ or a subungual haematoma. This is one of the reasons why it is so important for the tennis shoe to have adequate room and toe space. Keeping the nails short and trimming them properly will help to delay the onset of ‘tennis toe’. Repeated pressure on the sole of the foot or against the digits can lead to blisters, corns and calluses, and these often develop in a competitive game of tennis or when breaking in a new pair of tennis shoes.
Acute injuries to the lower leg, ankle and foot in tennis are also quite common. Racquet sports place an undue amount of stress on the lower leg and the supporting soft-tissue structures. The reason for this increased stress, and potential for acute injury, is the amount of time players spend on the balls of their feet, the extreme ranges of motion that foot and ankle must move through, and the violent nature of these movements (Levisohn & Simon 1984). Two of the more common acute injuries incurred in tennis are spontaneous rupture of the Achilles tendon and of the gastrocnemius muscle. As in basketball, tennis involves a ballistic start from a standing position, which can impose a large force on the Achilles tendon. Barfred (1971) stated that the tendon is subject to injury when (1) tension is applied quickly, (2) the tendon is under tension before loading, and (3) the tendon is weak compared to the muscle. Recurrent injury to the Achilles or any other tendon can cause partial or complete rupture. A tear of the medial head of the gastrocnemius (‘tennis leg’), usually occurs in a younger population than those suffering from acute Achilles tendon ruptures. This is the most common injury occurring in male tennis players (Arner & Lindholm 1958, Leach 1988) and is often misdiagnosed as a rupture of the plantaris muscle (Anouche et al 1987, Froimson 1969). This injury often occurs while the player’s foot is in plantar flexion with simultaneous supination. This creates tension on the medial head of the gastrocnemius, while relaxing the plantaris and lateral head of the gastrocnemius.
Other acute traumatic injuries include spontaneous rupture of the posterior tibial and fibularis (peroneus) tendons, dislocation or subluxation of the fibularis (peroneus) tendons, and acute compartment syndrome. The most common fractures in tennis are stress fractures of the metatarsals and calcaneal fractures, which occur particularly when landing hard on the court from an overhead jump shot, service or net play. Another stress fracture site due to forced dorsiflexion, during the same shots, is the tibial plateau or distal shaft of the tibia. Occasionally, fractures to the styloid process or os trigonum of the posterior aspect of the talus occur due to a sudden violent movement of the rearfoot when in plantar flexion and inversion, with the posterior process impinged on the tibia.
Ankle sprains are often seen in tennis, particularly in the net game, or when running hard laterally, and attempting to stop quickly to set up to return the shot. The lateral ankle injury is the most frequent, usually affecting the anterior talofibular ligament, followed by the calcaneal fibular ligament, and lastly the posterior talofibular ligament. Another acute trauma to the ankle involves an eversion–plantar flexion and abduction mechanism sprain, affecting the deltoid ligament. If severe enough, this can lead to fracture of the medial malleolus, as in a lateral injury, resulting in avulsions of the fibular apex. Styloid process fractures (Jones) of the base of the fifth metatarsal are also seen in tennis players who have experienced an inversion, lateral ankle sprain. A proximal fifth metatarsal fracture can be categorised into two specific types: (1) a fracture of the tuberosity, and (2) a fracture of the metatarsal shaft within 1.5 cm of the tuberosity (Ross 1999b).
Tennis court surfaces are another factor to consider. The various surfaces can be divided into clay, composition, hard court, wood, carpet and grass. The harder the court surface the greater the stress incurred by the tennis player’s feet and lower extremities, while the softer surfaces dampen shock and impart less stress to the knees, ankles and feet. For the older player who suffers from degenerative joint disease, with concomitant foot pathology, a softer surface should be chosen to avoid excessive amounts of stress and shock to the feet and legs. After a player has been injured, it is recommended that softer surfaces be used to allow for rehabilitation, and then to resume play later on harder surfaces.
GOLF
Foot and lower extremity function is one of the keys to a proper golf swing. To transfer weight and produce an efficient swing proper biomechanical balance of the foot is essential. Most professional golf injuries involve the lower back, followed by injuries to the left wrist and shoulder. Whereas, in male amateur golfers the lower back was the most commonly injured area, followed by the elbow, hand or wrist, shoulder and knee, among female amateur golfers the elbow was the most commonly injured site, followed by the back, shoulder, hand or wrist, and knee (McCarroll & Gioe 1982).
Approximately 10–12% of golf injuries occur in the lower extremity (McCarrol et al 1990). Acute foot injuries in golf are not common. One study showed that in 584 golf-related injuries, 2.1% were foot-related (Cavanaugh & Williams 1983). However, walking the course, pre-existing foot injuries are complicated by repetitive weight transference during swing, and improperly fitting shoes can contribute to foot complaints during golf play.
As recognised by Cavanaugh and Williams (1983), foot function, ground reaction forces and centre-of-pressure position are critical for a proper golf swing. It was shown that the right and left foot function in an entirely different manner, and with no symmetry. During the swing, the right foot begins a rocking movement, and by the end of the swing the golfer begins to apply pressure to the medial border of the hallux, concluding at the distal aspect of the hallux.
The left foot functions asymmetrically by beginning with a pronatory effect on the medial edge and then supinating to the lateral edge of the foot and ankle.
There are numerous foot conditions that the golfer may suffer from, particularly from the shoes they wear; for example, hallux abducto valgus can be a source of irritation in shoes. Hallux limitus/rigidus with dorsal osteophytic lipping of the first metatarsal head can create degenerative joint disease and synovitis. This can cause limitation of motion and stiffness, and prohibit normal pivoting and toe-off during the golf swing. Irritation from the counter of the golf shoe against the posterior aspect of the heel can cause exacerbation of a Haglund’s deformity, or retrocalcaneal bursitis. Occasionally, Achilles tendinitis can be a problem, particularly in a middle-aged or older golfer.
Aetiological factors such as excessive pronation, tight Achilles tendon and posterior muscle groups, equinus, combined with uneven terrain and uphill lies, can create additional stretch and torque of the tendon and contribute to the tendinitis. Plantar fasciitis, one of the more common overuse injuries seen in sports, particularly in golfers who walk the course, is due to chronic traction and irritation of the origin of the plantar fascia on the medial plantar condyle of the calcaneus. If left untreated, an enthesopathy will eventually develop, due to hyperpronation, with resulting heel spur formation. Old golf shoes and poor foot biomechanics can lead to this overuse injury. Ankle sprains are not uncommon.
Golfers who walk on undulating fairways, attempt to swing from an uneven or uphill lie, or have excessive supination of the ankle in the follow-through of the swing may suffer from an acute ankle sprain. Morton’s neuroma, usually in the third inter-space, is quite common, particularly if walking a great deal or wearing tight-fitting golf shoes with little toe box room. Other conditions that golfers suffer from are blisters, corns tinea pedis, dryness of the skin, heel fissuring and onychomycotic nails.
Golf shoes are important because they act as a base of support for the golf swing by reducing foot slippage and offering lateral stability (Furman 1999). They are found in three basic styles: (1) welted shoes, the classic-appearing shoe, with a leather upper and stitched leather sole; (2) athletic-style shoes, similar to the characteristic athletic shoe; and (3) comfort classic shoes, which are similar to the classic welted shoe, but lighter and with more cushioning.
AMERICAN FOOTBALL
American football is a contact sport, and more acute injuries occur in this sport than any other (Meewwisse & Fowler 1988, Pritchett 1980). The study by Pritchett revealed that one-third of the injures involved the lower extremities and accounted for one-half of the cost (Welch 1996). It was also noted that nearly half of the injuries reported involved sprains and strains of the ankle, knee and back, as well as contusions of the lower extremity (Kune et al 1980, McCarthy 1989). Other aetiological variables that play a part in American football injuries include the surface of the field (grass versus artificial turf), the size of opponents, speed, style of play and conditioning of the athlete (Skovrm et al 1990). The question of whether artificial surfaces cause more injuries than natural grass, particularly to the knees, ankles, foot and hallux, is continually being explored; however, there is some evidence to support this assertion (McCarthy 1989, Skovrm et al 1990).
One of the more common problems incurred involves the medial and intermediate dorsal cutaneous nerves. As a result of direct trauma, and being ‘cleated’ (stepped on) by another player, a neuropraxia of these nerves can occur. Another factor in this condition is chronic irritation on the dorsum of the foot due to taping and from the laces of the shoe being too tight. Such neuropraxia is seen quite frequently in American football players who have a cavus foot type with a metatarsal–cuneiform exostosis (instep). Radiating pain extending from the medial dorsal cutaneous nerve will extend to the medial branch of the saphenous nerve, and to the hallux (McNerney 1990, 1999). Another nerve injury that occurs commonly in American football is interdigital neuroma with entrapment and degenerative fibrosis. This occurs as a result of being on the ball of the foot for a prolonged period of time and a strong propulsive push-off. Tight-fitting shoes are another reason for compression of the nerve, and can create other symptoms. Occasionally, tarsal tunnel syndrome may develop from excessive pronation, traction of the posterior tibial nerve, and direct and indirect trauma to the deltoid ligament region or the nerve itself.
Other traumatic and overuse injuries include turf toe, a traumatic injury to the first MTPJ and the metatarsal–cuneiform joint, which occurs more frequently on artificial surfaces (Clanton et al 1986, Dollar 1978). The term ‘turf toe’ refers to a hyperextension or a hyperflexion of the joint, creating a capsular or ligamentous sprain of the MTPJ. Other injuries that can be categorised as turf toe are dislocation and subluxation of the joint, rupture of the intersesamoidal ligament, sesamoiditis, fracture of the sesamoids and capsulitis of the joint (Fig. 13.4). Rodeo et al (1990) evaluated a number of professional American football players and found that 57 of those surveyed had reported symptoms of turf toe. It should be noted that this figure was similar to that for players from other teams who played on a natural grass surface; however, 84% of the players in the series reported that their initial injury occurred on artificial turf. Some of the aetiologies that predispose an American football player to this type of injury include the number of years in professional American football (Rodeo et al 1990), pes planus, decreased pre-injury MTPJ range of motion (Clanton et al 1986), decreased pre-injury ankle range of motion, and shoes too flexible at the shank. Although turf toe is a common injury in football it can occur in any sport that is played on artificial turf (Underwood 1985).
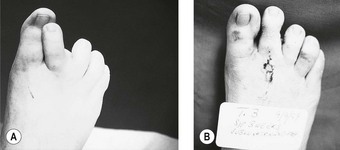
Figure 13.4 (A) Spontaneous subluxation of the second metatarsophalangeal joint (MTPJ); (B) postoperative repair of spontaneous subluxation of the second metatarsophalangeal joint.
Other injuries commonly seen in American football include Lisfranc’s joint injuries, which are also common on artificial turf surfaces, causing pain and swelling of the metatarsal–cuneiform joint. In some cases of violent hyperextension, Lisfranc dislocations and fractures may occur. Ankle sprains, common in all sports, are reported to be the second most common injury in American football, with knee injuries being the most common (Meewwisse & Fowler 1988, Pritchett 1980). Lateral ankle sprains make up the majority of these injuries, involving the anterior talofibular and calcaneal fibular ligaments. Injuries to the tibiofibular syndesmosis are associated with a high morbidity, limiting the player’s early return to normal activity (Hopkison et al 1990). Deltoid sprains occur very infrequently, but can be just as serious and disabling. Overuse injuries seen often in American football include intracalcaneal pain, which in younger athletes (described in the younger athlete section) is quite often due to calcaneal apophysis (Sever’s disease). Heel spur syndrome and plantar fasciitis are other frequent overuse injuries in American football. Chronic Achilles tendinitis, insertional tendinosis, shin splints, myositis, bursitis of the foot, ankle and lower leg, and exertional compartment syndromes are typical in this game.
Recommendations for the reduction of overuse injuries in American football are pre-season flexibility and strength exercise programmes, physical therapy, proper selection of stable and motion-control cleats, flexible arch supports, prescription orthotics to control poor biomechanics, anti-inflammatory medication and, when safe, injection therapy.
Skin disorders are prevalent. Thick socks and perspiration can lead to tinea pedis and, with trauma to the nails due to the cleated shoe and constant forefoot push-off, this can cause subsequent onychomycosis. Other skin lesions such as blisters, corns, calluses, intractable plantar keratomas and verrucae may also develop. Conservative management of these disorders in the American football athlete is desirable, except when trauma or conservative measures have failed, when surgical intervention may be necessary.
RUGBY
A contact sport, historically the forerunner of American football, rugby is played without any protective gear. Injuries to the head, upper extremities and lower extremities are prevalent. The sport requires upper body strength and lower body power.
This sport also requires great athleticism, where speed is needed during sprint running. In addition to running skills, the player must pass and catch the ball, requiring balance and coordination. The training for such an explosive sport is designed to improve stamina and speed.
The training methods in rugby have not necessarily paid sufficient attention to pre-season conditioning, strengthening and flexibility. As a result, tight muscle groups and poor flexibility lead to many acute and overuse injuries such as gastrocnemius–soleus muscle pulls and tears, ruptures of the Achilles tendon, and chronic Achilles tendinitis, plantar fascia strains and chronic plantar fasciitis. Due to biomechanical imbalances, posterior tibial and fibular (peroneal) tendinitis, shin splints and turf toe injuries are seen. Direct trauma to the lower extremity can result in knee injuries, ankle sprains, fractures and compartment syndromes. Tackling on grass, compared to artificial turf, reduces the chances of injuries (as discussed in the section on American football); however, playing rugby often leads to injury. Field conditions (dry versus wet) as well as footwear can have an impact on the incidence of injury in this highly physical, combative, traditional sport.
STEP/BENCH AEROBICS
Step and bench aerobics as an ‘exercise dance’ was developed from the high-impact aerobic dance form, which led to an abundance of lower extremity injuries, as a safer form of low-impact dance. By reducing impact shock on the lower extremities the number of injuries seen by the sports medicine practitioner has been dramatically reduced. However, step and bench aerobics can still cause overuse injuries.
Approximately 18 years ago aerobic dance matured into a new form utilising a ‘bench’ platform and creating a new way to exercise with less impact, while simultaneously allowing for the same, if not better, cardiovascular workout. The exercise routine is centred on a ‘step’ that is just 43 inches long by 16 inches wide by a minimum of 4 inches high (109 cm × 40 cm × 10 cm). It was thought in the early stages that the higher the step the harder and more vigorous a workout. However, with the elevations of one-, two- and three-block increments the risk of overuse injury is increased.
The development of aerobic shoes has had a great deal of impact on the sport. Over the years, technological advances in design have led to a much more stable, as well as a high-performance, aerobic shoe. Further design changes have led to a new breed of ‘cross-trainers’. This popular shoe can be used for aerobic dance and for short-distance running, and it is a favourite among aerobic instructors. With increased running incorporated in the routines, and with dance movements, including lateral movements as well as back peddling, the cross-trainer shoe has proved to be an asset.
Injury prevention, as in all sports, begins with good observation and correction. Most aerobic instructors agree that technique is very important in the avoidance of injuries, and that repetition is dangerous. It has been shown that if an aerobic dance routine is performed at a cadence that is too fast (over 128 beats/minute) participants cannot secure their entire foot on the bench, resulting in strain or pulling of the Achilles tendon, posterior tibial tendon or fibularis (peroneus) tendons. This can also lead to strain of the long plantar fascia or the intrinsic musculature of the plantar aspect of the foot (Ross 1999a). In addition, an over-quick step off the bench can lead to sesamoiditis, stress fractures of the lesser metatarsals as well as the tibia and fibula, tarsal tunnel syndrome and the formation of interdigital neuroma. It has been shown that extending too far back off the bench can lead to a hyperextension of the ankle, with concomitant traction of the Achilles tendon. If left undetected, this overuse injury could eventually develop into a chronic Achilles tenosynovitis and/or insertional calcinosis. It is imperative that instructors observe carefully the participant’s knee alignment in relationship to the lower leg, as well as their foot placement on the bench. It has also been shown that striking the floor from the bench with repeated impact can result in overuse patellofemoral joint syndrome or shin splints. It is important that the instructor survey the class before the initial workout to help determine whether any of the participants has a pre-existing overuse injury or a high potential for developing a new injury.
Prevention of injuries should be of paramount importance to the sports medicine specialist, particularly for aerobic enthusiasts who train at high intensity levels and ignore the potential for injury. Quite often aerobic dance participants may have psychological or physiological disorders (e.g. anorexia nervosa, amenorrhoea and osteoporosis). Any one of these conditions can have serious consequences when participating seriously in this sport. The sports medicine specialist should be on alert when interviewing the patient during the history taking, because any one of these diagnoses can render clues regarding the underlying injury. Extreme weight loss and/or stress fractures (particularly in the young female) should alert the sports medicine practitioner to look beyond the easily definable diagnosis and consider referral.
In a preliminary study by Ross (1999a) of 329 participants, 153 claimed that they had suffered some discomfort or pain due to step/bench aerobics, whereas 163 claimed that they were symptom-free. The most common sites for the incidence of injury were the knee, calf, Achilles tendon, foot and shin.
There were a number of recommendations made by the instructors to help prevent some of the typical injuries:
BALLET AND DANCE
Classical ballet had its origins in the Italian Court in the 15th and 16th centuries. The practice of dancing ‘en pointe’, or on the tips of the toes, was popularised in the early 1830s, and is one of the aetiological factors in the development of foot deformities. Yet it is a ballet form that is practised by young girls and women all over the world. In addition to classical ballet, other forms of dance are also popular. Each form of dance has its own intrinsic character and injury incidence.
Ballet is an elegant and very athletic art form, and ballet dancers can be regarded as elite aesthetic athletes. The athletic artiste must master solitary body positions and specific repetitive movements that are incorporated into a choreographed programme. Dance has a unique set of biomechanical considerations specific to this art form, and with a whole group of distinct injuries connected to the biomechanical demands of the activity.
The sports medicine specialist must be attuned to the high demands and mechanics of the sport as well as the potential for injury and recurrent injury. Quirk (1994) described four main causes of injury in ballet:
What makes ballet so unusual is the ‘turnout’ of the feet, or extreme external rotation of the hips. The dancer trains daily by exercising the anterior musculature of the hip to achieve the classic position, referred to as ‘well turned out’. The ideal position is that in which the hips and feet are laterally rotated 180° from each other, and where the heel is facing the opposite heel, and the toes are facing in opposite directions. Kravitz and Murgia (1999) suggest that dancers attempt to create the illusion of the desired foot position by tilting the pelvis forward, by laterally rotating the tibia at the knee, or by applying an abductory force to the pedal segment. The pelvic tilt can produce excessive compressive forces on the posterior aspect of the vertebral bodies and discs of the lumbar spine, and can result in lumbar strain injuries.
The rotation of the knee produces excessive strain of the capsule and medial collateral ligament, and can produce medial knee pain. The abductory force created on the foot will then lead to subtalar joint and midtarsal joint pronation, as well as prolapsing of the longitudinal arch. For the pronated dancer, with a collapsed longitudinal arch, difficulty in maintaining position can create pain and a ‘rolled in at the ankle’ appearance.
The externally rotated position is seen in the five basic positions in ballet. Essential basic movements in ballet comprise the plié, relevé and pointe. The plié exercise consists of deep knee flexion while maintaining the ‘toe-out’. Again, the hips are rotated laterally at 180° to each other. Plié is a flexed-knee position. In demi-plié the dancer lowers herself, upper body erect with the knees bent, and with the heels in full contact with the floor. Demi-plié is an important movement used in preparation for a propulsive action phase, as well as in the landing stage when impact forces are being reduced, or at the end of movements such as jumps, turns or leaps. In grand plié, the dancer lowers herself even further, again with the upper body erect, with greater bending of the knees, and as the heels come off the floor weight is transferred to the ball of the foot. In relevé the dancer assumes an erect upper body stance, with the knees extended, and the weight shifted to the balls of the feet. The next position is referred to in French as ‘sur les pointes’ or ‘en pointe’. In going en pointe the dancer assumes a stance position on the toes. Pointe shoes are identical between the right and left. The pointe shoe is constructed of a leather sole with an upper made of canvas, cotton and silk, with a stiffened toe cap made of fabric, glue and stiffened paper (Whiteside 1986). A stiffened shank made of board material is found plantarly to help secure the longitudinal arch. Ribbons are used to hold the shoe on the foot, wrapped around the ankle, and tied at the back. Their half-life can be very short and, once broken, they have to be discarded immediately. In some cases soft, flexible orthotics can be used for additional support and to attempt to achieve neutral control.
When the dancer is en pointe, weight is shifted onto the distal and medial aspects of the first and second rays as the foot is supported by the toe box, the shank, the musculature of the dancer and the intrinsic bony architecture of the foot and ankle (Denton 1997). The demi-pointe attitude is a position in which the dancer stands on the metatarsal heads while the ankle is fully plantar flexed and the MTPJs are maximally dorsiflexed. A forced arch attitude is the same as demi-pointe, with the addition of the knee being flexed.
Overuse injuries in ballet are a common entity. The injuries are specific particularly to dancers, and are not seen in other athletic sports. Specific movements combined with repetitive biomechanical demands on the lower extremities frequently lead to these overuse injuries.
Tendinitis
Due to the repetitive nature of ballet, tendinitis conditions are common overuse injuries. Flexor hallucis longus tendinitis is a very common injury (Hamilton 1982b). This type of injury frequently occurs as a result of the strain created on the hallux tendon antagonistic to hallux hyperextension while en pointe. The foot is plantar flexed or pointed, with the hallux in maximum plantar flexion. When jumping, leaping or push-off is required, the great toe flexor is required for the completion of this propulsive phase. The flexor hallucis longus is then maximally stretched, followed by contracture along with the other plantar flexors. Repetitive movement, and jumps with the foot en pointe can lead to fatigue, tendinitis, peritendinitis, tenosynovitis and, if severe and long-lasting, the flexor hallucis longus can spontaneously rupture. Pain and crepitus can be elicited around the medial malleolus. The second most commonly affected tendon is the Achilles tendon, with pain elicited at the distal portion of the tendon and at its insertion. Crepitus upon movement as well as thickening of the tendon and distortion of the surrounding tissues may develop. There are various aetiologies for the onset of Achilles tendinitis. One such mechanism is the repetitive jumping involved in ballet, where a concentric tension is created at push-off, followed by an eccentric force on the posterior muscles and Achilles during the completion of the movement. Not getting the heel down to the floor (as in running equinus injuries) can also lead to this overuse injury. Another interesting entity is that of the dancer who ties her ankle ribbons too tightly around the back of the ankle, and the knot presses directly on the Achilles tendon, thus irritating during these leaping manoeuvres. Extensor tendinitis occurs as a result of overuse of the extensor digitorum longus, and in some cases the tibialis anterior tendons. This is usually seen with increased external rotation and turnout of the foot. Due to excessive pronation, and plantar flexion to achieve additional external rotation and turnout, fibular (peroneal) tendinitis may develop.
Plantar fasciitis is another entity due to a weak arch, barefooted practices, repetitive jumping and landing, as well as attempting to further toe-out with additional pronation. The dancer will often attempt to compensate for this chronic injury, and may develop other areas of injury, such as posterior tibial tendinitis, fibular (peroneal) tendinitis, shin splints, iliotibial band syndrome, as well as hip and lower back pain.
Posterior and anterior impingement syndrome of the ankle
Posterior impingement of the ankle or talar compression syndrome (Quirk 1982) is much more common in dancers than in athletes. It is seen with maximal plantar flexion of the ankle joint, and occurs with the en pointe position. Pain may be elicited at the posterior aspect of the ankle when the toe is pointed, and is caused by compression of the posterior tubercle of the talus on the posterior distal tibia when the ankle is maximally plantar flexed.
This process can fracture and irritate against the flexor hallucis longus tendon. Flexing or extending the hallux will precipitate a painful response. This usually requires cast immobilisation and, on occasion, may necessitate surgical excision of the bone fragment. Another aetiology is the os trigonum (being separate from the main body of the talus in about 10% of ankles), which may become entrapped and compress the surrounding soft-tissue structures (Quirk 1982, 1994). Anterior tibiotalar impingement syndrome is another complaint experienced when the ankle joint is dorsiflexed. The aetiology of this syndrome may be an exostosis of either the anterior distal tibia or the dorsal neck of the talus. In either scenario, a bony block occurs when an attempt is made to maximally dorsiflex the ankle.
Shin splints
These are usually seen with pain in the anterior lower third of the tibia, involving the posterior tibial and anterior tibial tendons. Fibularis (peroneus) tendons may also become involved, particularly the fibularis (peroneus) longus, which plantar flexes the first ray and ankle joint. As in any sport with the commencement of conditioning, tendons and muscles that have been inactive initially become ‘overused’ and inflammation develops. For ballet dancers who are pronators, or who have a pes planus foot type and force the ‘turn-out’, shin splints can be a recurring problem.
Ankle sprains and toe sprains
The ankle sprain is the most common traumatic injury seen in ballet. When a dancer performs a leap or jump and lands incorrectly, or on a previously injured ankle, a typical lateral inversion mechanism sprain may occur. When the ballet performer has to place the ankle in a plantar-flexed position during performance or participation, ankle sprains become a common entity (Hamilton 1982a). Lateral ankle injuries usually affect the anterior talofibular ligament, sometimes with or without injury to the calcaneal–fibular ligament. The posterior talofibular ligament is rarely involved, except in severe ankle sprain cases. With dancers who over-pointe, stretching of the ankle collateral ligaments and capsular tissues may occur. This can often lead to symptoms of a sinus tarsi syndrome, rather than a typical ankle sprain. Toe sprains, as in footballers with turf-toe, can also be a frequent occurrence, particularly with dancers en pointe, and who rehearse and perform barefooted (modern dance). A sprain of the collateral ligaments and/or the sesamoid apparatus may occur.
Stress fractures
This is another common entity for the ballet dancer, again as a result of overuse. With the dancer en pointe, the first and second rays are where weight impact is focused. In the demi-pointe dancer, the entire weight of the body rests on the second metatarsal. As a result, most dancers have a marked hypertrophy of the second metatarsal bones (Quirk 1994). The most frequent site for fractures of the second metatarsal is at the neck, but fractures at the base are also not uncommon. Other areas where stress fractures may occur in the ballerina are the other metatarsals, the lower third of the fibula, and occasionally the talus, calcaneus and navicular.
Fractures of the sesamoids are another injury to suspect, particularly with the dancer who performs a great deal on demi-pointe.
Hallux limitus
With narrowing of the joint space, metatarsus primus elevatus, osteophytic changes of the first metatarsal head and base of the proximal phalanx, hallux limitus can be a disabling condition for a ballet dancer. Due to increased stress on the first metatarsal phalangeal joint en pointe and in the demi-pointe stance, ‘jamming’ of the joint occurs, with subsequent stiffness and capsulitis. Surgical intervention may be necessary in cases where there is decreased range of motion and where hypertrophic bone and ‘spurs’ cause further destruction of articular cartilage. Simple cheilectomy may be all that is needed; however, even plantar-flexor osteotomies may not provide enough dorsiflexion of the joint to provide total relief and normal range of motion.
Bunion deformities
Although bunion deformities are common among ballet dancers, a normal foot type does not necessarily mean that the dancer will have a predisposition towards developing a bunion. However, the pronated, pes planus, flexible fore-footed dancer will have a greater tendency towards developing a hallux abducto valgus deformity. Ballet, and dancing en pointe, contribute to further deterioration of the joint and a more extensive deformity. Surgery should be an absolute last option for the ballet dancer; however, when symptoms are consistent, and performing dance has become impossible, surgical correction with a distal metatarsal head osteotomy, that is an Austin procedure (Chevron – see also Ch. 23), is a desirable.
Neuromas
Due to being en pointe and performing in a toe shoe with a rigid toe box, compression of the intermetatarsal nerves can develop, creating irritation and fibrosis of the nerve. Once again, surgery should be reserved for the dancer who suffers from consistent pain and an inability to perform after conservative measures have failed.
Nail problems
With the dancer’s en pointe stance, and the focus of the weight directed to the distal aspect of the hallux, pressure on the nail can be tremendous, and subungual haematoma is a common entity. In addition, formation of a subungual exostosis may cause further irritation of the hallux nail and develop into a thickened, sometimes onychomycotic, nail. The nail may even begin to involute, causing an ingrown nail with paronychia formation. On occasion, when pain is persistent, the ingrown nail, or the thickened nail or spur may have to be removed (see Ch. 21).
BASEBALL
Although injuries to the throwing arm are quite common in baseball (Magnusson et al 1994, Timmerman & Andrews 1994), lower extremity injuries can be just as unrelenting. Baseball is a throwing, catching, batting and running sport. Injuries to the lower extremity can be categorised by specific injury, and by the position that is played. Typical injuries include muscle pulls and strains, ankle injuries, contusions and fractures by being struck by the ball, either by the pitcher or by being ‘fouled-off’ by the bat. Runners sliding into the bases or the home plate are predisposed to injury because of a sprinting action creating hamstring pulls, ankle sprains, knee injuries, turf-toe or being ‘cleated’ by the opposition player.
Many overuse injuries can also develop during the conditioning ‘spring-training’ season. Due to the running involved, and taking into account the biomechanical lower extremity factors of the player (i.e. genu valgum, tibial varum, pes planus, cavus foot, etc.) common overuse injuries such as chronic Achilles tendinitis, plantar fasciitis, heel spur formation, posterior/anterior shin splints, iliotibial band syndrome, anterior/posterior tibial tendinitis, retrocalcaneal exostosis with bursitis, patellofemoral joint syndrome and hip dysfunction are found.
As in football, basketball, soccer and hockey, strength and conditioning coaches are a key element to the training of these amateur and professional athletes. Running is a key element in the preparation for, and the maintenance of, conditioning during the baseball season. As in most sports, the three training factors involved with preparation and injury prevention are flexibility (range of motion of joints), function and strength. Speed work and interval training are an integral part of the training and conditioning process for the baseball athlete. This is what affords the player the ability to accelerate from home plate to first base, after hitting the ball, or when attempting to steal a base. Running style, gait, stride, limb-length discrepancies and foot type are all part of the evaluation of the baseball player that should be performed by the trainer and/or team podiatrist or sports medicine specialist. When needed, biomechanical correction with soft insoles, or prescription orthotics within the baseball spikes, may be a great asset in the correction of lower leg and foot imbalances.
Special consideration for injury prevention begins with the individual player, and the position played. Pitchers, when delivering the pitch, have a particular set of biomechanical considerations. Technique, leg extension, rotation, weight balanced on one foot, stride and foot plant during delivery are all important factors that can cause faulty mechanics or injury at any time. Slow- and fast-pitch softball pitching have different sets of mechanics, yet they can also be subject to repeated overuse injury. Particular injuries include blister formation on the medial hallux and forefoot, as well as subungual haematoma from the hallux striking the end of the shoe at the end of the delivery of the pitch. For pitchers with excessive pronation on the stance leg, medial knee pain may develop.
Catchers are high-risk players for foot, ankle and lower leg injuries. The catcher, constantly in a crouched position, places his or her entire body weight on the forefoot, creating a great deal of forefoot pressure which can translate into neuroma formation. For a pes planus foot type, or in the case of a pronated catcher, subtalar joint pronation can result in posterior tibial tendinitis, deltoid ligament strain and, combined with the rocking and stretching of the longitudinal arch, plantar fasciitis will often develop. Stretching of the posterior muscle groups, Achilles and plantar fascia is essential for catchers. Catchers are constantly being hit by foul balls off the bat and onto the toes, first MTPJ and beneath the instep protector on the dorsum of the foot.
Batters must have good foot mechanics and position to transfer weight efficiently from one foot to the other when attempting to hit the ball. Batting is a sequence of coordinated muscle activity, beginning with the hip, followed by the trunk and terminating with the arms (Shaffer et al 1993). For a right-handed batter, the right foot (back) is stable in relation to the ground, with the foot supinated and the leg externally rotated. Until the swing is attempted, the left foot is virtually unweighted. As the swing begins, weight transference from the right foot to the left begins. Once the bat is in motion, and has begun to swing forward, the forefoot and hips begin to pivot, further transferring weight from the right foot and leg to the left foot and leg. At the conclusion of the swing, and at the time of contact with the ball, both feet should be pointed forward to the pitcher. Batters, as well as their counterparts behind the plate, are frequently being struck on the foot directly, or by the ball ricocheting off the ground. Often, the ball will strike the instep, medial arch, shin or the great toe, possibly resulting in a painful contusion or haematoma.
Infielders are subject to injuries from sliding runners, spiking them as they slide into base or step across the base. Runners are at risk of hamstring strains as they sprint to the next base, as well as inversion ankle sprains as their foot connects with the base as they slide.
Baseball shoes vary according to level of play and the surfaces being played on. High-school players use rubber cleats, while college and professional baseball players wear metal ones. Rubber cleats are also worn on artificial turf. The configuration of the cleats is three on the forefoot and three on the heel. Baseball shoes should have a strong counter for stability, a rigid shank for longitudinal arch support, a deep toe box to prevent toe irritation, and a flexible sole to allow for quick running speed.
SKIING
Alpine or downhill skiing is a complex skill that requires controlled pronation, setting the foot, ankle and lower extremity on the inside ski edge. Pronation sets the inside edge of the downhill (control) ski, and allows for the skier to lean inward against the ski, which holds a skidless arc throughout the turn. While balanced on a beam of flexible composite 6.3 cm wide, the skier drives the shin forward against the stiff boot cuff and swings the hips to the opposite direction. The ski rolls onto its sharp steel edge and bites the snow, creating an arc across the hill (Ross & Subotnick 1999). Skiing is like ballet on snow, and the skier encounters many centrifugal and g-forces, as turns are created, while simultaneously attempting to keep the centre of gravity in line over the centre of the ski. Any variation in normal lower extremity biomechanical balance can alter the skier’s ability to develop a controlled turn, thus predisposing the skier to injury if the abnormality is great enough. The three factors that are important in a skier’s conditioning and performance are flexibility, strength and proper range of motion. Variable factors such as structural biomechanical deformity, functional deformity or dynamic imbalance of muscle groups can also influence the performance of the skier and help to predict potential injury. When skiers have pre-existing injuries, creating weakness in muscle groups, decreased flexibility and limited range of motion of the involved lower leg joints, the skier’s ability to ski efficiently and safely will be significantly diminished. As a result of these compromised factors, an increased muscular effort is required, resulting in skier fatigue. Fatigue has been shown to be one of the main factors in the incidence of downhill skiing injuries (Ross & Subotnick 1999). Skiers will compensate for biomechanical abnormalities by obtaining the use of pronatory forces from other joints (i.e. hips and knees) in order to ski properly. Ross (1985), utilising the electrodynogram (EDG), showed that forces are transmitted from both the forefoot and the rearfoot, which is essential in up-and-down weighting, as well as in the completion of proper turns. Abnormalities such as excessive foot pronation, shortened heel contact and excessive propulsive phase on the toes, extreme forward lean of the boot, including asymmetry between the two feet, were all observed, affecting the skier’s effectiveness and performance. Skiers can overcome some of these lower extremity abnormalities, including poor skiing style, poor edge control and foot imbalances, by using various orthotic controls in their ski boots. It has also been shown that custom insoles for mild foot and lower leg imbalances, as well as prescription orthoses for the more severe rearfoot and forefoot abnormalities, could be valuable in helping to provide proper foot bed balance and to improve ski performance and efficiency (Ross & Cohn 1984). It has become widely accepted to use easy-to-customise liners and removable full-length soft support systems within them; custom insoles or prescription orthoses may be substituted for the pre-existing insole.
It is imperative that the foot specialist or sports medicine specialist has a basic understanding of both boot design and skiing performance, in addition to a working relationship with the boot shop and ski boot fitter. The sports medicine specialist can help in the selection of the correct boot by determining foot type and targeting existing areas of biomechanical weakness or physiological defects. The specialist can diagnose bony deformities, stress areas of the foot, biomechanical imbalances, areas of friction and irritation, poor circulation, nerve entrapments and metabolic disorders. With these factors taken into consideration, the boot fitter can help to decide whether the skier will require a boot designed for a wide foot, a flat or high-arched foot, a volume boot, a pure forward entry boot, a hybrid boot (with both overlap and rear entry design), a narrow heel pocket or a thin, thick or adaptable liner.
Tibia varum is a biomechanical abnormality that has a great effect on a skier’s ability to ski normally. Tibia varum is a result of an uncompensated varus deformity of the tibia, which transmits instantaneously to the ski–snow interface and causes the skier to ride excessively on the outside edge of the ski. When a skier has more than 8–10° of tibia varum deformity, he or she will have a great deal of difficulty initiating a parallel turn without ‘catching’ the outside edge of the ski. Skiing on the outside edge is often associated with tips being crossed, which eventually leads to sudden falls (Ross & Subotnick 1999). Today, most high-performance boots provide a boot cuff adjustment to accommodate varying degrees of tibia varum and create a flat ski surface. One of the easiest and most reliable methods of treating tibia varum is to use a full-length, canted, in-boot foot orthosis. This method has the advantage of providing for total foot contact within the boot, thus correcting for biomechanical imbalances within the foot and lower leg. It also has the effect of reducing the friction of the foot against the boot while at the same time affording a comfortable, dependable, balanced foot bed that helps to provide effectual edge control. Other lower-leg and foot abnormalities that can contribute to a skier’s difficulty in edge control and performance are tibia valgum, subtalar varus, forefoot varum, forefoot valgum, transverse plane asymmetry and leg-length discrepancies.
Skiers frequently complain that their feet hurt and that they are cold, tight and irritating. Over the years, ski boots have advanced in technological design and performance, and have become quite biomechanically sophisticated. Some of the adjustable features include internal versus external canting systems, adjustable ‘spoilers’ or shaft-angle adjustments, boot flex, forward lean, internal/external heaters and custom heat-mouldable liners made of EVA. Most ski boots have removable foot beds that may be replaced with custom-made orthoses. Some ski shop devices can be made readily by using an apparatus that places the foot in a semi-weight-bearing neutral position, with knee stabiliser apparatus built into the platform to accurately align the knee over the foot for complete lower leg correction. The traditional orthotic, made from an in-boot cast while the skier assumes a neutral ski stance position, will function much better than the custom insole because it can provide additional correction and stability in the rearfoot, subtalar joint, midtarsal joint and forefoot. It has been shown that control of excessive pronation/supination and locking of the midtarsal joint (stability) will result in better edging and higher performance. The five areas of concern in a boot are:
The sports podiatrist or specialist should be cognisant of the numerous problems that skiers face, whether they be biomechanical imbalances leading to poor ski technique or performance problems related to foot or boot-fit discomfort. It is imperative to understand the lower extremity biomechanics related to skiing, boot design, boot fitting, and the interrelationship between a ski orthosis and the boot in which it sits.
Cross-country skiing
Cross-country skiing compared to alpine skiing has a totally different technique and application. In downhill skiing the heel and lower leg are locked in a rigid boot, affording more control to the skier’s rearfoot complex. The body’s centre of mass is located directly over the rearfoot complex (subtalar joint); with properly aligned joint compressional forces, rearfoot neutrality is maintained. By comparison, cross-country skiing involves a heel that is repeatedly lifted within the shoe from the ski surface and lowered again, allowing for more skier imbalance. Cross-country skiing employs a technique referred to as a ‘swing kick and glide’. Using the poles to create upper body stability and propulsion, the heel is kicked upward to maintain forward motion with a forefoot propulsion on the ski. Diagonal stride is created by alternating the opposite arm and leg forward; a ski gait is created similar to walking and jogging (Parks 1989).
Cross-country boots are an intermediary between backcountry and racing boots in both design and support. Compared to the alpine ski boot, the cross-country touring boot has much more freedom of movement, at the expense of much less support. Because sagittal plane motion is the predominant direction of foot and leg action, it is not essential for the touring skier to require stability in the shoe for exaggerated turns because moderate curves are usually the only ones encountered.
Similar biomechanical considerations for the cross-country skier as for the alpine skier are essential. The patella should be properly aligned over the skis in a bent-knee skiing position. A lighter, flexible orthosis than the bulkier alpine device is preferred. Keeping the devices as thin as possible will provide more room for the foot and toes to function.
SNOWBOARDING
This relatively new sport is popular with participants of all ages. This winter version of skateboard surfing has its risks, as does alpine skiing. Of the injuries incurred in snowboarding 40% involve the upper extremity while 43% involve the lower extremity. The most common site of injury is the wrist (trauma and fracture), followed by the knee (sprains) and then the ankle (fractures) (Ganong et al 1992). The snowboarder lacks the freedom of individual leg movement, and thus the chance for recovery is much less than in downhill skiing. Unlike alpine skiing, which uses the integration of foot, knee and hip motion, the short pivoting turns involved in snowboarding concentrate the energy on the hips and knees.
Snowboarding boots are quite different from their alpine skiing counterparts. Earlier designs incorporated a soft type of boot, whereas the full hard shell and half-shell are the more recent designs. The soft boot allows for more motion of the foot, so that more injuries are incurred than with the harder designs. The most common injury seen with the soft boot is at the ankle, whereas the rigid full-shell boots protect the ankle but allow for more forces to be transmitted to the knees. This has resulted in a higher frequency of knee injuries.
FOREFOOT INJURIES
Athletic injuries can be classified by the area in which they occur: the forefoot, midfoot or rearfoot. Forefoot injuries to the athlete can be attributed to the high levels of stress that the ball of the foot has to withstand. These injuries can range from nagging to disabling, depending on the site and the repeated impact to the area. We can further divide the forefoot into medial, lateral and central sections to specify the exact location of the injury. The following is a list of potential differential diagnoses based on mechanical considerations:
The plantar aspect of the foot is subject to friction and shearing forces that create plantar keratomas under the metatarsal heads. Thickened subcutaneous tissue beneath the metatarsal heads offers a protective layer to dampen the shock that is transmitted to the forefoot bones.
Plantar keratomas vary from simple calluses to deep, intractable plantar keratomas, which can be both painful and incapacitating to the athlete.
Metatarsalgia
Athletes who have equinus deformity or protracted propulsive phases may develop changes in the forefoot – the metatarsal heads change position, becoming plantar flexed and prominent on the plantar aspect of the foot. Metatarsalgia occurs when these protuberant metatarsal heads become painful, and may be either acute or chronic. One of the primary reasons for this painful debilitating injury is that there is loss of the transverse arch, with increased metatarsal stress. As the metatarsal bones begin to sublux in a plantar-grade direction, plantar interdigital nerves are subject to irritation from prominent metatarsal heads. When the metatarsalgia, along with the plantar callus, is due to a pes planus as well as a hypermobile first ray, a more rigid orthotic device would be more advantageous than a softer, accommodative, shock-absorbing device. Metatarsalgia can also result from a rupture of the plantar (volar) plates of the MTPJs, or may possibly be due to a synovial cyst plantar to the MTPJ. This type of injury is seen quite often in martial arts and hard-landing sports such as basketball, tennis and volleyball. Lastly, stress fractures may produce symptoms of metatarsalgia, particularly in the metatarsal shaft regions and the sesamoids.
Capsulitis
The capsule of the first MTPJ, as well as the lesser MTPJs, may develop inflammation as a result of repeated trauma. This may occur in any of the sports outlined earlier. Typical examples are turf toe involving the first MTPJ in football, capsulitis of the first MTPJ due to pointe stance in ballet, vertical landing on the first MTPJ in basketball, hyperextension inflammation in track sprinting and step aerobics, and direct trauma to the first MTPJ in striking a ball in soccer.
Bursa formation and bursitis
As a consequence of constant pounding of the second, third or fourth MTPJ, chronic irritation of the periarticular structures can lead to the development of a submetatarsal bursa. This can occur naturally (anatomically) or adventitiously (in response to superficial external irritation) in the subcutaneous tissues. These anatomical bursae are nature’s response to a functional need to reduce both friction and shearing. The adventitious bursa will develop in response to soft-tissue structures that are constantly being subjected to great shearing forces. Pain and swelling will usually develop as a result of an inflamed bursa due to mechanical trauma. Chronic irritation may cause the bursa to distend due to the accumulation of synovial fluid within the bursa sac. The sac may be either fixed (attached to fascia or to the capsule) or freely moveable.
In any case, the larger the bursa the greater the chance of irritation and painful symptoms. The abnormal shearing forces may be secondary to hypermobility of the forefoot, of the first and fifth rays, or from the foot sliding forward in the athletic shoes due to improper fit. These conditions can lead to increased friction, inflammation of the plantar tissues, formation of plantar keratomas and, if severe and consistent enough, bursa formation anterior and plantar to the metatarsal heads. Conservative treatment, such as protective padding and/or accommodation incorporated into the forefoot extension of a sport prescription orthotic device, will help to reduce the chronic friction and shearing forces affecting the chronic adventitious bursa.
Sesamoiditis and fracture
The sesamoid bones of the plantar surface of the first MTPJ are now recognised for their importance in relation to symptoms of pain, gait biomechanics (functional and structural hallux limitus), the particular sport in which the athlete participates, and the footwear that is worn.
The sesamoid bones are isolated bones that lie within the flexor tendons; they have a dorsal concavity and a plantar convexity. The larger and longer tibial sesamoid lies more distally than the smaller, more rounded fibular sesamoid. Both sesamoids lie plantar and within each respective tendinous expansion of the medial and lateral heads of the flexor hallucis brevis muscle (Bojsen-Moller & Flagstad 1976). It has been shown that 10–33% of feet have either a bipartite or multipartite sesamoid (Jahss 1981). The sesamoids have articular cartilage that lies within the tendon and is subject to injury. The sesamoid provides protection and shock absorption for both the joint and tendon. In addition, like any pulley, they increase the musculotendinous mechanical advantage for the first MTPJ, particularly during the propulsive phase of gait. In court sports, as well as in running and other high-impact sports, the high ground reactive forces act on the first MTPJ. Together with constant ‘push-off’ and pronatory ‘pivoting’ of the hallux, the sesamoids act by assisting gait, and provide additional flexor strength. It has been shown that forces three times the body weight pass through the sesamoids during weight shift in a normal gait cycle (Drez 1982). Forces are greater beneath the tibial sesamoid, which explains why the tibial sesamoid is involved in more injuries than the fibular sesamoid.
In cases of hallux abducto valgus a lateral shift of the tibial sesamoid will occur, creating a situation in which the medial sesamoid is susceptible to increased forces beneath the first metatarsal head. With the sesamoid vulnerable to these excessive forces, subchondral erosion and/or fracture can occur. In cases of hallux limitus, with a semi-rigid or rigid plantar-flexed first ray, it is not unusual to see sesamoiditis or injury to the sesamoid apparatus.
When injury to the sesamoid does occur, there will be limited movement and pain upon dorsiflexion of the first MTPJ. Routine radiographs with comparison views of the contralateral foot can often determine whether there is an actual fracture or whether it is a bipartite or tripartite sesamoid. An axial ‘sesamoidal’ view radiograph can aid in determining whether there is deviation of the sesamoids. It can also help to identify whether the tibial sesamoid is more plantargrade, and whether upon weight bearing the standing forces are greater than normal. Additional investigative studies, such as bone scans and computerised tomography (CT) scans, can help determine whether or not a fracture is present.
There are five categories of injury to the sesamoid apparatus. The injuries can be either of the acute nature, such as avulsion fractures, or of the chronic type, involving repetitive stress to the sesamoids or the medial and lateral support structures.
CASE STUDY 13.3
SESAMOID FRACTURE
A 39-year-old woman presented with a chief complaint of severe pain of 4 months’ duration under the ball of her left foot, and directly beneath the first metatarsophalangeal joint. Some years ago a cyst overlying the extensor hallucis longus tendon was excised, with scar tissue formation and possible recurrence. The patient described the previous injury as having broken the base of the fifth metatarsal of her left foot stepping off a pavement. Over 4 months ago she suffered an injury to the tibial sesamoid. Radiographs revealed a stress fracture to the tibial sesamoid.
The patient is a runner who, until the injury, ran on a treadmill for 3 miles two or three times a week, and used a recumbent bicycle and elliptical trainer two times a week. Since the injury the patient has attempted to exercise by walking and running on a treadmill for 3 miles twice a week. However, she continues to experience pain and discomfort. She has begun to exercise with the stair-stepper and walks to work in comfortable dress-heel shoes. She experiences pain when wearing her shoes.
A Cam-walker removable cast boot was applied for 2 months, and prescription orthotics and NSAIDs were prescribed. The patient continued to have pain and discomfort in the region of the plantar first metatarsal head.
A repeat radiograph (anteroposterior/medial oblique) revealed a stress fracture distal to the tibial sesamoid of the left foot with mild distal migration and lateral deviation.
Past medical history. Non-contributory to condition (mitral valve prolapse and hay fever).
PHYSICAL EXAMINATION
Cavus foot type, semiflexible, plantar flexed to normal first ray. Hallux dorsiflexion normal to semirigid. Supinated subtalar joint. Ankle joint dorsiflexion – normal, tibial varum; subtalar joint range of motion – normal.
Gait analysis. Right foot abducted. Supinated heel strike, right foot pronates significantly more than the left foot at midstance to toe-off. Circumvention of right foot, left stays rectus, with functional hallux limitus, and plantar-flexing first ray.
ORTHOTICS AND TREATMENT
The patient’s sport orthotics required modification. They were uncomfortable and created too much pressure under the first metatarsal head. In addition, her dress-shoe orthotics required reducing in size to fit properly into her shoes. A dancer’s pad was created with accommodation for the tibial sesamoid and first metatarsal head.
It was recommended that the patient cease all impact physical activities to allow bone healing of the fractured sesamoid. A bone stimulator was prescribed for the fractured tibial sesamoid.
ONE-YEAR FOLLOW-UP
The dress-shoe orthotics required refurbishing as the rearfoot posts had worn down. A metatarsal pad was put on the sport orthotics, creating too much pressure under the tibial sesamoid. There was a contusion fracture of the distal phalanx (fifth digit, left foot).
A radiograph showed a healing fracture of the tibial sesamoid of the left foot. There was no displacement or further migration. There was reduced but continued intermittent pain. A therapeutic steroid injection with vitamin B12 was administered to the capsular joint tissues below the tibial sesamoid. Physical therapy was given. A Cox-2 NSAID was prescribed for 7 days. Bone stimulation was continued.
Metatarsal stress fractures
Stress fractures are common injuries among athletes (Devas 1958, Drez et al 1980, Jones et al 1978, Markey 1987, Ting & Yocum 1988). A stress fracture occurs as a result of repetitive cyclic loading with lower forces than those necessary to produce acute fracture (Gilad et al 1985). The term ‘fatigue fracture’ has also been used to demonstrate the result of mild forces or stress with eventual alteration or disruption of a material, such as bone (Morris & Blickenstaff 1967). Therefore, a stress fracture is not the result of a single occurrence but rather an ongoing process. The end result may be a fracture, but in actuality it is the product of continued applied forces on the bone creating a defect (weakness) by reabsorbing bone in advance of the laying down of new bone (Ross 1999b). Johnson (1964) describes it as a disease process that never involves any strange or new reactions, but only altered relationships in normal reactions. For the athlete, constant change in levels of stress, training methods and environmental factors can create an alteration in the relationship between growth and repair. For the runner, forces of three to six times the body weight occur at heel strike, with an estimated 800-foot strikes impacted on each foot per mile. It is estimated that stress fractures comprise 6% of all injuries to runners (Mann 1986).
There are various stresses that are transferred to bone which ultimately develop into a stress fracture. Devas (1975) has described several types, including:
Stress fractures occur most often in the central region of the forefoot; however, they may occur in any location depending on the forces. In high-impact sports, stress fractures usually result from repetitive pounding and impact through both the soft tissues surrounding the bone (muscle, tendons and periosteum) and the bone itself. There are many aetiologies for the development of stress fractures. Biomechanical abnormalities, such as excessive pronation (Fig. 13.5), hypersupination, lower extremity malalignment (tibia varum, genu valgum, external or internal femoral rotation) and limb-length discrepancy, can all lead to alteration in normal gait, which can then lead to stress fractures. A second tier of aetiology is the training methods of the athlete. The runner who runs in worn-out shoes, on crowned roads or hard running surfaces, or who inadequately prepares for long-distance events or overtrains, is at high risk of developing a stress fracture. In addition to the metatarsals (third, second, fourth), other areas of the foot and lower leg that are subject to increased stress and fracture are the distal tibia, distal and proximal fibula, navicular, calcaneus, cuboid and sesamoids (Fig. 13.6).
An athlete will present with erythema and oedema overlying the involved metatarsal.
After such an injury, extreme pain upon palpation of the area will usually determine the site of the fatigue fracture. Pain will be elicited upon motion, as well as with the use of a tuning fork overlying the involved bone. Keep in mind that bone callus formation will usually not be evident on a radiograph for at least 2–3 weeks after injury. After radiographic evaluation, the standard special procedure for early detection is the technetium-99m diphosphonate three-phase or single-phase bone scan. This investigative study can help to detect a fracture within days of the injury. When the athlete presents clinically, it is important to determine from the history the exact mechanism of occurrence of the injury. This can often help to differentiate a stress fracture from another type of injury. When combining the history and the clinical findings, even without radiographic or nuclear study evidence, if there is suspicion of a stress fracture, assume that it is a fracture until proved otherwise.
The treatment of a stress fracture depends on the time at which the diagnosis was made. The clinician should take into account the severity of the stress fracture. In cases of a fresh injury, an Unna boot (soft compression cast) with overlying elastic tape and a postoperative shoe is usually indicated for at least 3 weeks. Ice, elevation and anti-inflammatory medication are also very helpful in reducing symptoms. Follow-up physical therapy treatments of heat (warm gentle whirlpool) and fluidotherapy (dry whirlpool) are helpful in increasing blood flow to the area, which can help to accelerate bone healing. When the fracture is pronounced, cast immobilisation and non-weight-bearing for 4–6 weeks may be necessary. In cases where delayed union (after 6 weeks) is evident, the use of a bone stimulator may be advantageous. When displacement of the fracture is seen, particularly in midshaft fractures, or if angulation takes place, then closed or open reduction with internal fixation is indicated.
Rest, immobilisation and refraining from participation in impact sports for at least 4–8 weeks post-injury is necessary. Metaphyseal stress fractures take the least time to heal, while intra-articular, cortical fractures take the longest. When the athlete is pain-free, he or she is ready to begin rehabilitation, but not necessarily ready to return to sports activity. The athlete must have a full range of motion in the joints in the involved injured extremity, and must have redeveloped the flexibility of the muscles of that limb, and developed strength, endurance, proprioception, agility and cardiovascular reserve before returning to full competition. A good training programme will help to lower the incidence of recurrent injury. Cycling between vigorous activity and periods of rest are essential. The use of proper shoes, impact surfaces and orthotics can be important preventive measures in avoiding the recurrence of stress fractures in the athlete.
Osteochondritis dissicans – Freiberg’s infraction
Freiberg’s disease (see also Ch. 4) is a sequel to injury of the lesser MTPJs. It is a dorsal trabecular stress injury of the lesser metatarsal heads (Kinnard & Lirette 1989). An osteochondrosis develops as a result of trauma or vascular embarrassment that changes enchondral ossification and ultimately results in an incongruity of the articular cartilage. Freiberg’s infraction is such a case where, due to repetitive stress on a long second metatarsal bone, overuse injury to the articular surface occurs.
Examples of sports where there is a high probability of developing such an injury include running sports and impact jumping. The condition can lead to chronic pain and limited function when participating in sport activity.
Smillie (1955) developed a staging classification correlating the physical and radiographic findings, and described various stages of the injury:
There are various theories as to the aetiology of Freiberg’s disease. Freiberg (1914) originally concluded that the condition was due to trauma, whereas Kohler (1961) disputed that theory. Smillie (1955) also reported that trauma was the underlying cause, and postulated that the condition was due to a weak foot, with a short, hypermobile first ray. Others have reported a vascular deficiency that can cause necrosis of the metatarsal head (Wiley & Thurston 1981), while other investigators have argued that the epiphysis was underdeveloped for unknown reasons, although mechanical stress to the abnormal epiphysis eventually caused the final injury (Duthii & Haughton 1981) (see also Ch. 4).
The athlete requires a full range of motion at the MTPJ and, due to this type of deformity, foot function is greatly impaired. The condition resembles that of a second metatarsal stress fracture and compels the clinician to radiograph the foot to differentiate between the two. Conservative management includes rest, cast immobilisation and, in some cases, non-weight bearing with crutches for walking. This is followed by a slow phased return to sports activity, with the use of biodynamic orthoses, with a metatarsal pad or a metatarsal bar (over metatarsals 2–4) to diminish pressure on the second metatarsal head. In some cases, the capsulitis can be treated with injections of corticosteroid with local anaesthetic. Alternatively, homeopathic intra-articular injections of Traumeel or Ruta Graveolens may be used safely, without further weakening the periarticular structures (Subotnick & Sisney 1999).
When conservative measures have failed, surgical intervention is usually required, with many and various procedures advocated. Some include abrasion arthroplasty, with removal of the osteophytes and loose bone bodies and remodelling of the metatarsal head. Others include dorsiflexory metatarsal osteotomies at the metatarsal head, metatarsal head resection and MTPJ replacement with a lesser total joint hinged implant. Orthotic therapy in all cases is also strongly advised.
CASE STUDY 13.4
FREIBERG’S INFRACTION
A 14-year-old female cross-country runner presented with pain of 2 weeks duration in her right foot, and 4 months duration in her second toe. She experiences pain when running, with pain in the arch and extending to the ball of the foot. She states that she experiences pain during her track workouts, but had no pain during her workout yesterday. The foot hurts at night, but there is no swelling. She has been applying ice, and did not run for one weekend 2 weeks ago.
The patient has been running since her fifth grade at school. In seventh grade she ran track and cross-country. As a freshman in high school she runs 3200 metres, 2 miles, 1 mile and cross-country. She has run a number of 5-km races. After running 800 metres on her last track workout she began to experience pain. She admitted to experiencing pain after a cross-country. The pain did not persist from the previous day’s workout, but pain appears during a track workout.
TREATMENT
Two weeks after the initial visit a walking and running gait analysis was performed. The capsulitis in the second metatarsal area was improved. Temporary insoles were supplied, followed by biomechanical evaluation and casting for prescription orthotics. A Cox-2 NSAID was prescribed to be taken every day with meals. Rest from all running activities was advised, with no impact sports to be carried out.
Five weeks later the pain had improved. Repeat radiographs showed no further changes (Fig. A). With walking exercise and short-distance running the patient continues to experience pain. The patient was advised to undertake no further running and no impact exercise, and to return in 4 weeks.
After 9 weeks radiographs showed more flattening of the metatarsal head, and more impaction and narrowing of the second metatarsophalangeal joint space (Fig. B). The patient has continued to walk and occasionally sprint. All running and impact activities were stopped, as was the taking of the Cox-2 NSAID. The patient was now wearing orthotics and running shoes. The patient was asked to return in 5 weeks.
Fourteen weeks after the trauma the patient was wearing the orthotics continuously. Radiographs showed no further changes. The second metatarsophalangeal joint was no longer inflamed and the swelling was reduced, with much less discomfort. The patient has been compliant and had ceased running and impact activity. A bone scan was ordered to determine the level of osteoblastic/osteoclastic activity, and a bone stimulator was prescribed.
Morton’s neuroma
One of the most common nerve disorders is the interdigital (Morton’s) neuroma (see also Ch. 4), which affects the third intermetatarsal and interdigital space, but which can also affect the second intermetatarsal and interdigital space. It is less commonly seen in the first interspace and is occasionally seen in the fourth interspace. Morton’s neuroma was described by T. G. Morton in 1876. Distinctive pathological changes such as oedema of the endoneureum, perineural fibrosis, fibrinoid degeneration, demyelination and endoneural fibrosis are often seen.
The athlete will complain of pain, as well as a burning and tingling sensation that radiates distally into the adjacent digits. They will experience symptoms more often after wearing a tight athletic shoe that compresses the metatarsal heads together against the nerve. In running, and particularly in skiing, it is not unusual for the athlete to describe a numbness of the toes and forefoot, with a cramping and occasional shooting pain as well. Occasionally, the athlete will say that they feel a fullness or swelling in the forefoot. They will often be forced to remove their shoe to massage the foot to relieve the numbness and burning pain. The pain often begins as an intermittent soreness and is related to increased athletic activity. If left untreated, the neuroma pain symptoms will become more persistent as well as more severe. It is not uncommon for the pain to be associated with certain shoes.
This condition is manifest during sports activity, particularly during the propulsive phase of gait, when toe-off begins. This is seen in running sports, ballet, aerobic dance, stair steppers and skiing. It is often seen postoperatively following bunion correction, when the patient compensates to the lateral aspect of the forefoot due to a hallux that is functionally limited. It is also seen with athletes who demonstrate a high degree of pronation combined with a forefoot varus (Fig. 13.7). It may also be seen in athletes who have suffered hyperextension injury of the second or third MTPJ, particularly when rupture of the collateral ligaments has occurred. For runners and dancers who suffer recurrent metatarsalgia and capsulitis of the second MTPJ, oedema surrounding the joint will lead to compression of the nerve and a greater incidence of metatarsal head irritation. An abnormal metatarsal parabola can cause impingement (Hoadley 1893), as well as nerve ischaemia (Nissen 1948), trauma and stretching of the nerve.
On physical examination pain will be elicited upon direct pressure to the indicated interspace. Squeezing of the metatarsal heads with the use of medial and lateral compression, together with direct push-up pressure of the nerve in the interspace, will produce a palpable click, known as a positive Mulder’s sign, and will often induce symptoms. This is usually pathognomonic for a neuroma within the interspace. Pain may be elicited both distally to the toes and proximally to the tarsal tunnel region. Therefore, the clinician should trace the nerve from the web space to the tarsal tunnel to rule out an impingement or compression of the nerve outside the web space. It is imperative to rule out other possible diagnoses such as stress fractures, neuropathy and lesions within the spaces as well as bone and joint lesions.
Conservative treatment is always recommended, with a variety of injection therapies described. The author uses a combination of long- and slow-acting corticosteroids (dexamethasone acetate and phosphate), a total of 1 ml in combination with 1 ml of 1% lidocaine (lignocaine) plain, 1 ml 0.5% bupivacaine plain, 0.2 ml Wydase and 0.5 ml of vitamin B12 with a 27-gauge needle. After the injection, the use of nerve stimulation, ultrasound, and later iontophoresis, in combination with NSAIDs, the application of ice, change of footwear, massage and prescription orthotic use with a metatarsal pad and/or a ‘peanut’ to spread apart the metatarsal heads has proven very successful. Subotnick (1999b) has reported a 70% success rate using both cortisone and homeopathic injection mixtures. The use of orthotic devices has proven successful in controlling abnormal pronation and excessive transverse plane motion of the forefoot, particularly in the midstance to toe-off phases of gait.
After all conservative measures have been exhausted, surgical excision of the neuroma may be necessary. Excision of the nerve proved successful in 76% of the cases reported by Gaynor et al (1989) and 80% of the cases reported by Miller (1987), with a 7% recurrence rate according to Subotnick (1999b). The author has also found that, by using a CO2 laser, bleeding and fibrosis are reduced, and there is a reduction in postoperative pain and recurrence. However, athletes should be forewarned that a stump neuroma can develop, and this can present an entirely new set of problems. Some surgeons advocate release of the intermetatarsal ligament when the nerve appears compressed, as seen via the endoscopic procedure. In all cases, however, it is strongly suggested to the athletic surgical patient that an orthotic device with a metatarsal pad be worn to prevent recurrence and to prevent the development of a neuroma in an adjacent interspace.
There are many other nerve entrapment disorders of the foot involving nerves – such as the tarsal tunnel – proximally involving the tibial nerve and distally involving divisions of the tibial nerve, medial, calcaneal lateral and the first branch of the lateral plantar nerve. Other nerves involved include the medial plantar nerve, lateral plantar nerve, the higher tibial nerve in the leg or popliteal fossa, deep fibular (peroneal) nerve, superficial fibular (peroneal) nerve, saphenous nerve, sural nerve and the medial common hallucal nerve. All these entities can cause symptoms similar to the interdigital nerve and can result from a variety of sports activities. Proper identification of the involved nerve and early conservative management can often help to prevent unwarranted surgical intervention.
CASE STUDY 13.5
SURAL NERVE ENTRAPMENT
A 53-year-old, white man presented with pain and numbness in his left leg and foot. He was preparing for the Amsterdam Marathon, and 2 months ago ran 23 miles in Huntsville Texas. At mile 15 his calf muscle went into cramp up to 4 inches (10 cm) above the heel. He completed the 23 miles and next day there was no pain. On the following Wednesday he ran 6.5 miles. There was no problem for the first 3 miles but he experienced pain during the last 3.5 miles.
The following Sunday he attempted a 10-mile run. Over the first 3 miles there was no pain, but the next 3 miles he ran slowly and walked the last 4 miles in pain. That afternoon numbness developed in his left foot. The patient began applying ice and taking ibuprofen. Ten days later he began massage therapy.
Forty-two days later the patient was continuing with massage therapy twice a week, as well as applying ice and taking 6 tablets/day of ibuprofen 200 mg. The left foot continued to be numb and tingled when touched on the rear 4 inches of the leg above the heel. He attempted slow running and experienced no pain. At day 35 pain began in the left ankle, independently of running. Forty days later the patient ceased all running. The numbness decreased, but the pain increased.
PHYSICAL EXAMINATION
Vascular. DP/PT pulses palpable bilaterally. Capillary filling time within normal limits. Skin temperature and colour within normal limits.
Neurological. Deep tendon reflexes within normal limits. Fine touch sensation within normal limits. Plantar response normal, clonus-negative. Numbness along the lateral aspect the left foot, along the course of innervation of the sural nerve. No tingling recreated with percussion of the sural nerve. Mild pain experienced posterior to the lateral malleolus.
Dermatological. Skin texture and swelling within normal limits.
Musculoskeletal. Muscle strength 5/5 bilaterally. Pain on palpation of the base of the fifth metatarsal of the left foot.
CONSULTATION FINDINGS
Sports Medicine Physical Medicine Assessment. Nerve entrapment, left lateral cutaneous nerve-branch sural nerve.
Ruled out compartment syndrome – condition too focal, pain worse with rest. Hyperaesthesia rather than numbness. No evidence of muscular involvement. Area of injury localises to the superficial posterior compartment rather than the deep posterior compartment. Positive Tinel sign
PHYSICAL MEDICAL CONSULTATION
A/P. Possible muscle tear, some type of stretch injury, resulted in compression of this branch of the sural nerve.
Recommended. Limited surgical exploration and decompression of sural nerve. After decompression patient might have full recovery over course of months.
NEUROLOGY CONSULTATION
Neurological examination. Thickened left sural nerve at the ankle.
Positive Tinel sign with palpation below the lateral malleolus. Reduced superficial pain sensation over left ankle and foot. No lower extremity motor or reflex deficits present.
SURGERY (5 MONTHS 3 WEEKS)
Procedure. Decompression with neurolysis of adhesions sural nerve left lower leg.
Lysis of adhesions, scar tissue formation gastrocnemius/Achilles tendon 14 cm proximal to tip fibular malleolus.
Skin incision 6 cm length. Lysis, decompression 4–6 cm proximally and distally. 4 mg Decadon. Jones compression dressing.
POSTOPERATIVE COURSE OF EVENTS
2 weeks. Less discomfort distal to nerve and posterior to lateral malleolus. Continued numbness and sensitivity from lateral branch of sural nerve to base fifth metatarsal. Cast boot removed – physical therapy twice a week begun.
4 weeks. Continued improvement, physical therapy, biomechanical evaluation for orthotics.
6 weeks. Physical therapy completed (continued in office on follow-up visits). At times states he is 50% improved. Walking 1 mile. Swimming. Mild pain lateral heel. Numbness still present in lateral midfoot.
8 weeks. Mild superficial numbness of dorsum/lateral foot. Ambulating/exercising.
4 months. Continued improvement. Less paraesthesia, decreased hyperaesthesia posterior inferior aspect lateral malleolus. No pain along course to base fifth metatarsal. Increased sensation in dorsal lateral aspect. Running  miles/week; 8 min/mile.
miles/week; 8 min/mile.
6 months. Feeling much better. Ran 9 miles/week for 6 weeks. To run 12 miles this week. Mild numbness of lateral third, fourth, fifth digits. Mild numbness of dorsum and lateral aspect of foot. No complaints re. posterior heel. No complaints of pain in fibular (peroneal) groove. No complaints along incision line.
Hallux limitus and rigidus
In hallux limitus and rigidus (see also Ch. 4), a condition seen frequently in the athletic patient, a limited range of motion of the first MTPJ occurs, creating pain during propulsion. It was first described in 1887 by Davies-Colley as a progressive, degenerative, arthritic condition of the first MTPJ and termed ‘hallux flexus’. In 1888, Cotterill proposed the term ‘hallux rigidus’ to describe this same condition. There are two forms of hallux limitus/rigidus, with various levels of pain. They include a structural hallux limitus and a functional hallux limitus (Root et al 1977). In structural hallux limitus/rigidus a degenerative process of the first MTPJ occurs, which impairs joint motion, leading to ankylosis.
Primary motion of the first MTPJ is in the sagittal plane, where the minimum dorsiflexion range of motion for normal propulsion is about 65–75°. In running sports this figure may actually be greater, because in running there is a prolonged propulsive phase and an elongated stride. To achieve this dorsiflexion, the first metatarsal must plantar flex. With a limitation of plantar flexion of the first ray, the hallux may be able to dorsiflex only 25–30°.
During the propulsive phase the hallux must be stable against the ground, and then act as a rigid lever arm to push off the ground. While the hallux remains stable against the ground, the first metatarsal plantar flexes as the heel lifts off the ground. As the metatarsal head glides over the sesamoid apparatus, the sesamoids begin to migrate distally to the metatarsal head. When the first metatarsal is restricted, and unable to glide along the dorsal aspect of the sesamoid apparatus, the development of a hallux limitus or rigidus will be accelerated. Some examples of these sesamoid conditions include chondromalacia or degeneration of the sesamoids, degenerative breakdown of the articular surfaces of the metatarsal head, and ankylosis of the sesamoid apparatus to the plantar articular condyles of the metatarsal head.
As noted earlier, the first ray must be able to plantar flex for the hallux to ride dorsally over the metatarsal head and dorsiflex. When the metatarsal head is limited in its ability to plantar flex during propulsion, the shift of the first metatarsal in the transverse axis of motion will be inhibited, thus preventing the hallux from dorsiflexing and creating a jamming of the MTPJ dorsally.
There are a number of aetiological, mechanical factors that lead to dorsiflexion of the first metatarsal. Root et al (1977) described several mechanical factors that cause a dysfunctional first ray. Some of these include excessive subtalar joint pronation, a long first metatarsal, hypermobility of the first ray, a dorsiflexed position of the first ray (structural metatarsus primus elevatus) and functional metatarsus primus elevatus.
Dananberg (1986) described how abnormal biomechanical function of the first MTPJ can restrict the body’s peak power for forward motion (as may be seen in walking as well as running) over the stance foot. This will lead to compensation occurring at various sites, minimising forward thrust and finally resulting in a decrease in forward momentum. For the athlete, normal range of motion with unrestricted dorsiflexion of the first MTPJ is essential. For sports involving quick acceleration (track, football, soccer), vertical leaping (basketball, volleyball), jumping (aerobics, dance, gymnastics) and quick changes of direction (tennis, court sports, football, soccer) the athlete relies on normal function of the first MTPJ. Certain sports require maximum dorsiflexion of the first MTPJ, such as in step aerobics, to step rapidly on and off the bench from a certain height, and the ballet dancer who must assume the demi-pointe position before going en pointe. The athlete who is limited in that dorsiflexory range of motion will develop dorsal lipping of both the first metatarsal head and the base of the proximal phalanx. In addition, the athlete may begin to compensate for the hallux limitus or rigidus deformity with hyperextension of the hallux interphalangeal joint, external rotation of the lower extremity, or increasing forefoot varus, all of which may lead to increased stress and loads to the foot and lower legs, leading to acute or chronic overuse injuries.
The athlete may present with either non-painful functional or painful structural hallux limitus. In the case of the functional hallux limitus, the patient will demonstrate a normal range of motion of the first MTPJ in weight bearing; however, during gait or running, when the first MTPJ is loaded, a limited range of motion is observed. Kravitz et al (1994) referred to the functional hallux limitus as a ‘pre-hallux limitus, which is entirely functional, related to the biomechanical abnormality of hyperpronation syndrome causing unlocking, and metatarsus primus elevatus, where the participant either relates minimal pain or no pain at all. In the case of the structural hallux limitus there is limitation of motion of the first MTPJ, in both the unloaded and loaded state, due to the fact that the first ray is fixed in a dorsiflexed position, or due to a structural metatarsus primus elevatus.
The athlete may present to the clinician with pain and stiffness of the first MTPJ. Many will complain that they are having difficulty pushing off during running and jumping gait. They will often relate that the shoe is beginning to rub a joint that now has become swollen or becoming physically larger. Various sports and the physical demands of these activities may cause increased symptoms, particularly when the first MTPJ is ‘pushed’ to its limits. As the degenerative disease process begins, further dorsal jamming of the first MTPJ will occur and a ‘dorsal bunion bump’ will appear. This is followed by a narrowing of the joint space and development of subchondral erosion of the articular surfaces. As a result, greater impingement during push off, fracturing of the dorsal exostosis or lipping may occur, creating loose bone body fragments either floating in the joint or becoming attached via synchondrosis. The athlete will often relate that they feel a painful popping or grinding sensation in the joint during their athletic activities. During the final stages, when ankylosis and joint destruction takes place (Fig. 13.8), as well as fusion of the sesamoid apparatus, consistent pain and swelling will be described. Due to the prominence of bone and/or bursa formation overlying the first MTPJ, an increase in the width and depth of the foot will occur. This will significantly reduce the space available in the shoe, creating additional pressure on the joint. This, in turn, will often lead to compensation, with increased weight bearing to the lesser metatarsals and a reduced loading of the first metatarsal, resulting in metatarsalgia capsulitis and callus formation plantar to the second metatarsal head. Another typical compensatory effect will be the formation of a hallux elevatus or hyperextension of the distal phalanx, which will cause rubbing and irritation of the hallux nail against the toe box of the athletic shoe. This constant pressure on the distal phalanx and nail may cause proliferation of the bone, resulting in a subungual exostosis and a dystrophic nail. Frequently, runners and other athletes will present with subungual haematoma as a result of this distal hallux jamming against the shoe. Evaluation of the shoe and observing wear patterns in both the toe box and the outer-sole of the forefoot will help identify these pathologies.

Figure 13.8 Hallux rigidus of the first metatarsophalangeal joint showing the level of degeneration.
Radiographic evaluation of the involved foot and joint in the anteroposterior view will reveal typical narrowing of the first MTPJ space, and broadening and flattening of the articular surfaces of both the metatarsal head and the base of the proximal phalanx. In the severe stages osteochondral defects, osteophytic changes of the metatarsal head, subchondral cystic formation and loose bone bodies will be seen. On weight-bearing lateral views, dorsal lipping of the first metatarsal head and base of the proximal phalanx is characteristic. The first metatarsal may appear dorsiflexed when compared to the contralateral side. To further illustrate the deformity, and to demonstrate the restriction of joint function, it is recommended that the clinician perform a stress lateral radiograph (see also Ch. 22). In this image, the patient is asked to raise the heel and stand on the ball of the foot maximally with the hallux stabilised on the surface, similar to a demi-pointe position. The radiograph will now reveal the degree of dorsal impingement and plantar joint distraction of the joint. Comparing the two views may help to determine just how restricted the joint has become during the midstance to propulsive phase of gait. This may also help to determine whether the athlete is suffering from a functional or a structural hallux limitus.
For athletes with hallux limitus or rigidus deformity, conservative care is always indicated initially. Because the condition is a degenerative as well as a progressive process, conservative management is designed to reduce the biomechanical metatarsus primus elevatus, as well as the dorsiflexory jamming of the first MTPJ. Conservative treatment will offer relief of symptoms, particularly in the early stages, in which minimal degenerative changes of the articular surfaces and joint are seen. However, this treatment plan only diminishes the damage to the joint. It does not alter the progressive nature of the deformity, nor does it restore normal range of motion to the joint.
To begin with, altering shoe selection is advised. A stiffer-soled shoe will help to reduce painful dorsiflexion of the first MTPJ. A rocker-bottom shoe or a metatarsal bar (rocker) proximal to the metatarsal heads will also help to reduce dorsiflexion of the first MTPJ. Again, a shoe with greater toe box room will help to avoid chronic rubbing of the hallux and reduce the pressure on the enlarged first MTPJ. Laces, seams and the tongue of the athletic shoe should also be checked prior to wear to avoid direct pressure and irritation.
In addition to shoe modifications, conservative treatment may consist of NSAIDs, intra-articular steroid or homeopathic injections, physical therapy modalities, with active/passive range of motion exercises and functional orthotic control. The orthosis will help to address the aetiology of the hallux limitus/rigidus development, such as hypermobility of the first ray, metatarsus primus elevatus and increased pronation of the foot. A Morton’s extension placed distally plantar to the hallux has been used quite successfully by equalising the height of the hallux and the first metatarsal. This extension can be incorporated in the orthotic device, occasionally with a dancer’s pad accommodation for the first metatarsal head, resembling ‘kinetic wedge’ described by Dananberg (1986).
As in all cases where conservative measures have been exhausted and the athlete continues to have pain, surgical intervention is indicated. There are five types of surgical procedure that can be performed, each classified according to the particular region of the MTPJ where the surgery takes place:
There is no ‘perfect procedure’ for cases of hallux limitus and rigidus. However, when treating the athlete or active patient, joint preservation and attempting to achieve maximum motion of the first MTPJ should be the surgeon’s goal. Cheilectomy is an excellent procedure when the biomechanics of the first ray are correct; however, decompression and plantar-flexor osteotomies are desired to reduce dorsiflexion stress and jamming of the joint.
For patients who are less demanding in terms of athletic activity, joint fusion can be a consideration.
When degenerative joint disease changes are great, and the older non-competitive participant wants to improve the range of motion and maintain hallux length without placing high stresses on the joint, implant replacement surgery is a viable option. In cases where the total joint prosthesis fails, arthrodesis may be the only remaining viable option.
Bunion deformity in the athlete
For the athlete, a symptomatic bunion deformity can limit function, reduce performance and be extremely frustrating. Associated with metatarsus primus varus are excessive pronation, hypermobility of the first ray, equinus, hyperelasticity, metatarsus adductus and a strong family history, which are more common in the female population. Even the mention of bunion surgery drives fear into the heart of any athlete. Therefore, the clinician is prudent to consider all conservative measures first before entering any discussion about surgical correction.
The clinician must take into account a number of factors first before considering the surgical option (Baxter 1994b, Pagliano 1997, Subotnick 1999g):
In the mildly compensated bunion deformity, with a low intermetatarsal angle (less than 11°) and a low hallux abductus angle (less than 20°), only intermittent symptoms may be present, particularly in sports activity. Neuritis of the saphenous and superficial medial dorsal cutaneous nerve, as well as capsulitis and bursitis, may also be present. With a functional fibular sesamoid in an acceptable position (at least 50% covered by the metatarsal head) and the first MTPJ articulation congruent, the positional compensated bunion deformity should be treated conservatively. The goal for this athlete should be to prevent further progression of the bunion deformity, by proper athletic shoe selection (wide forefoot with adequate toe box room). In addition, the athlete should use a prescription orthosis to limit excessive subtalar joint pronation and hypermobility of the first ray, and also undertake a good stretching programme when equinus of the gastrocnemius or Achilles tendon is identified. As long as the athlete is performing at a normal level and symptoms are controllable, surgery should be avoided, with the clinician reviewing the bunion deformity radiologically (Fig.13.9) at least once a year.

Figure 13.9 Hallux abducto valgus deformity showing the extent of dislocation of the sesamoids from the articular surface.
When the athlete presents with an uncompensated symptomatic bunion deformity, a rapid deterioration of the deformity will often be seen. As a result of excessive pronation and excessive medial column prolapse and instability, retrograde forces upon the hallux and first MTPJ cause further deviation of both the first ray and hallux. Pain will ensue, particularly during the propulsive phase of gait, which is the most important phase for the athlete. With a hypermobile first ray, instability of the joint region will occur. In the uncompensated bunion, the first metatarsal head will further increase adduction, dorsiflexion and inversion, as the sesamoid apparatus becomes subluxated laterally and the joint becomes incongruous. The joint becomes unstable and dysfunctional, and as a result other compensatory events occur, such as the development of neuromas, stress fractures, plantar-flexed second metatarsals with plantar lesions, varus rotated fifth digits, with hyperkeratotic lesions, tailor’s bunions of the fifth metatarsals, as well as compensatory ankle and lower leg pain.
When the symptomatic hallux abducto valgus deformity becomes consistently painful, both in athletic as well as in everyday shoes, and after orthotic use, altering of shoes and all conservative measures have failed, surgical correction should be considered (Fig. 13.10). The surgical procedures to be considered are of two types: the soft-tissue procedures; and the bone procedures, consisting of osteotomies and fusions. For the athlete, the simpler procedures are always recommended over the fusions, Lapidus procedures, Keller arthroplasties and implant procedures. Whenever possible, unilateral correction of the bunion deformity of the athlete is advised, particularly in cases of bilateral osteotomies.

Figure 13.10 Postoperative view of a repair to a hallux abducto valgus with total joint replacement.
The V-transpositional (Austin – see also Ch. 23) osteotomy (Austin & Leiventhen 1981) has shown to be for the athlete one of the simplest, most consistent procedures with the least complications. There have been a number of modifications to the Chevron (Austin) transpositional osteotomy, with various types of cuts of the first metatarsal head. Fixation of the osteotomy can be accomplished with a variety of techniques, including K-wire, screw, Steinman pin, Biofix (absorbable) and Orthosorb (absorbable) pins. For the athlete, the use of a biodegradable pin, when indicated, is preferable to screws that may need to be removed at a later time. The short Scarf Z-plasty is another excellent procedure for higher intermetatarsal angles. In cases where the proximal or distal articular set angle is high, or where hallux interphalangeus is present, proximal or distal osteotomies of the hallux (Akin) may be performed to correct the deformity.
For the athletic bunion patient, 6–8 weeks of postoperative progressive care is required before return to activity, with most distal osteotomies. With proper fixation, early return to activity may be permitted with surgical shoes, and assistance with crutches. After 3–4 weeks, stationary bicycling, as well as swimming and water jogging rehabilitation is strongly encouraged. Physical therapy, with active/passive range of motion of the first MTPJ and or hallux interphalangeal joint, is essential for restoration of function. This will help the athlete to return to the athletic sport without previous symptoms, but now with normal function.
Tailor’s bunion
In cases where the athlete has a cavus foot type and high degree of forefoot varus with splaying of the forefoot, it is not uncommon to see a tailor’s bunion develop. Both clinical and radiographic evaluation of the deformity to determine the extent of the bowing and rotation of the fifth metatarsal head are required (Fig. 13.11). The lateral bowing or concavity of the fifth metatarsal is a radiographic positional observation secondary to eversion and abduction of the fifth ray (Schepsis et al 1991). For the athlete who has a prominent lateral fifth metatarsal head, irritation due to unyielding athletic shoes (e.g. roller blade boots, ski boots, cycling shoes) can produce an adventitious bursa, entrapment of the lateral dorsal cutaneous nerve or enlargement of the styloid process. If the transverse plane separation between the fourth and fifth metatarsals is minor, and there is a low lateral metatarsal deviation angle, the clinician may choose a simple resection of the lateral prominence of the metatarsal head, with remodelling both laterally and dorsally if necessary. If a plantar lesion is present secondary to hypertrophy of the plantar condyles, the surgeon may decide to resect concomitantly the hypertrophied plantar condyles during the remodelling procedure. For the athlete, this simple procedure can afford an early return to activity because no osteotomy is involved.
However, in cases where there is a great deal of bowing with a high transverse plane separation of the fourth and fifth metatarsal heads, a distal osteotomy should be considered.
Evaluation of the separation should be planned preoperatively to determine whether adequate reduction of the fifth metatarsal deformity can be achieved with a distal osteotomy (Fallet 1990).
There are a number of procedures the surgeon can choose for correction of this deformity, including: oblique sliding osteotomy at the neck (Sponsel 1976), the transverse V (Throchmorton & Bradlee 1978), the medial closing wedge and the Hohmann displacement osteotomy (Hohmann 1951). Various fixation techniques are available, including 0.045- and 0.062-gauge K-wire fixation and 2.0-mm screw fixation. One preferred by the author employs, in conjunction with the transverse V osteotomy, the Orthosorb (half) absorbable pin from dorsal distally (just proximal to the articular surface) to plantar proximally, crossing the osteotomy site. If a second pin (half) is needed it can be utilised from dorsal proximally to plantar distally (opposite direction). When the symptomatic tailor’s bunion deformity is a result of significant splaying of the fifth metatarsal, a proximal basal wedge osteotomy may be chosen as the corrective procedure. Postoperative care and rehabilitation is similar in nature to the bunionectomy with osteotomy procedures.
REARFOOT INJURIES
Infracalcaneal heel pain
Infracalcaneal heel pain is one of the most common overuse injuries seen by the sports medicine practitioner on a daily basis. It comprises over 12% of the overuse injuries in the foot, and is seen in runners as well as middle-aged walkers who, after a fairly sedentary lifestyle, embark upon a fitness walking programme without commensurate preparation. As in most overuse injuries, underlying causes include improper shoe selection or worn-out shoes, poor biomechanics associated with excessive pronation, increased level of activity and intensity, and atrophy of the plantar fat pad as the athlete begins to age. It is estimated that the fat pad absorbs 20–30% of the heel force at heel strike (Paul et al 1978).
A runner or other athlete will describe pain at the beginning of a run or activity that quickly dissipates as the activity continues. The pain is often described as deep and aching, occasionally described as a burning sensation, or shooting pain down the foot, or up to the ankle. After the so-called ‘cooling down’ period when the participant has been off his or her feet, pain on the plantar aspect of the heel is once again encountered. The next day, upon rising, the first steps can result in excruciating, hobbling pain until the intrinsic soft-tissue structures of the plantar aspect of the feet have adapted to the floor and stretched out adequately. (Dog owners will have observed their pets arise in the morning and see how instinctively they stretch before they begin to walk.) This type of pain is referred to as post-static dyskinesia and is pathognomonic in the diagnosis of heel spur syndrome (Agostinelli & Ross 1977).
Plantar fasciitis is inflammation of the plantar fascia as well as the surrounding perfascial structures. The most commonly described painful region is the plantar medial calcaneal eminence, the origin of the plantar fascia. The plantar fascia is a multilayered fibrous aponeurosis, consisting of three bands, the medial, central and lateral, which fan out from the medial plantar calcaneal eminence into each of the plantar toe areas.
The dominant central band originates on the plantar surface of the posteromedial calcaneal tuberosity. The medial component of the fascia covers the abductor hallucis, while the lateral band covers the origin of the abductor digiti quinti, and extends to the plantar plate of the fourth and fifth digits. Passive dorsiflexion of the toes causes tightening of the fascia and allows the medial band to bowstring and become easily visible. Occasionally, a subcalcaneal bursa may form, and may be another cause of the heel pain in the athlete. The bursal sac develops often as a result of acute or chronic trauma, often related to the athlete’s heel landing hard on the floor or ground (volleyball, basketball), or repetitive striking of the ground (running, aerobics, martial arts). In addition, the nerve supply is as important in this syndrome.
The aetiological and biomechanical factors involved in heel spur syndrome are of great value in making a diagnosis (Agostinelli & Ross 1977):
The plantar fascia tightens by passive extension of the digits, which then raises the arch. As the plantar fascia is maximally elongated by digital plantar flexion, the longitudinal arch will be greatly depressed. As the plantar fascia is shortened at the time of MTPJ dorsiflexion, the longitudinal arch is then elevated. Hicks (1954) compared the function of the plantar fascia during the propulsive phase of gait to that of a windlass. There are many abnormal foot conditions that can lead to plantar fasciitis, such as pes planus foot, with a decrease in the calcaneal inclination angle, and with excessive subtalar joint pronation, cavus foot, external femoral rotation, inadequate dorsiflexion (equinus), a forefoot varus, or flexible forefoot valgus, and weakness of the plantar intrinsic musculature, which can alter normal biomechanics and lead to heel spur syndrome (Malay & Duggan 1987, Schepsis et al 1991, Ubler et al 1991).
When attempting to define the aetiology of plantar fasciitis the clinician should consider the three major categories: mechanical, degenerative and systemic (Bordelon 1983, Leach et al 1983). Athletes who develop plantar fasciitis as a result of chronic inflammation will develop pain that will extend distally along the entire course of the fascia, with concomitant thickening, and even nodular formation of the fascia. Their heel pain, or calcaneodynia, falls into the mechanical overuse category. The older active patient who develops atrophy of the plantar fat pad will also develop increased pronation with age as the medial longitudinal arch begins to prolapse and weaken. The younger athlete with the same foot type may not suffer symptoms due to the compensatory ability of the foot to maintain intrinsic support. However, as age takes its toll, the foot may weaken and become unable to compensate for the additional loads placed upon it. This is a degenerative process that results in an increased level of stress to the plantar fascia and perifascial structures. The result will be pain due to the inability to accommodate for these increased loads.
Repetitive traction of the plantar fascia and surrounding soft-tissue structures, particularly the ligamentous tissues, has been implicated in the development of a symptomatic heel. This repetitive stress will lead to development of chronic irritation of the plantar fascia or, in some cases, an acute traumatic incident can lead to a partial rupture of the fascia. Generally it is not the spur that is the underlying cause of the heel pain but rather the inflammation process of the fascia due to the extreme tension and traction. The ‘sharpy fibres’ that attach ligaments to bone are stretched in heel spur syndrome, hence the term enthesopathy for the micropathology of the associated heel spur syndrome (Agostinelli & Ross 1977). However, the actual spur can be a source of pain, particularly in the older patient who has begun to suffer from atrophy of the plantar fat pad, or even in younger athletes where repeated steroid injections have been employed. In cases of large infracalcaneal heel spurs, any rotation of the calcaneus (i.e. everted rearfoot) can cause increased irritation to the calcaneal tuberosity and make the spur more prominent and subject to trauma. Both conditions can be conservatively treated with Spenco or Sorbethane heel pads or cups, as well as protective shock-absorbing and heel-countered athletic shoes. The use of orthotic devices can also furnish rearfoot balance and cushioning to protect the calcaneus and spur against unwarranted trauma.
A number of other differential diagnoses that need to be ruled out when considering the diagnosis of heel spur syndrome are listed in Box 13.4.
On physical examination some patients may exhibit mild oedema surrounding the plantar fascia attachment at the medial calcaneal tubercle. Deep palpation of the medial band of the plantar fascia, as well as the medial calcaneal tubercle, will elicit a sharp pain, which is typical of heel spur syndrome. When cupping the posterior-inferior portions of the calcaneus with compression, a non-painful test is usually indicative of a possible stress fracture of the calcaneus, rather than heel spur syndrome. A tight plantar fascia will again elicit pain at the attachment at the calcaneus upon passive dorsiflexion of the digits. Midarch plantar fasciitis can be recognised as a separate entity from heel spur syndrome that displays more proximal symptoms. Quite often in long-distance running and in track and field events requiring violent bursts of effort, particularly sprinting, long jump and high jump, as well as basketball and other jumping and landing sports, partial ruptures of the plantar fascia can occur due to overuse and weakening of the collagen tissue. The athlete will present with pain, oedema and ecchymosis. Chronic partial ruptures will develop thickened scar tissue formation surrounding the injury. As a result of the chronic strain, tension and partial tears of the plantar fascia, the resulting scar tissue may organise and become solidified and develop into a singular or multiple plantar fibromas.
After physical examination, a dynamic gait analysis is often very helpful in determining any compensatory action of the symptomatic foot, such as an early heel-off or diminished propulsive phase. The clinician may observe an antalgic gait due to tenderness in the heel region upon heel contact, and may observe excessive pronation in the midstance phase that could be contributing to the traction on the plantar fascia.
Conservative treatment is geared towards both short-term relief of the inflammatory process of the plantar fascia and long-term relief involving correction of biomechanical imbalances. By only treating the initial complaint, and not directing attention to the underlying causes, the patient is doomed to repeated bouts of the overuse injury. The key to treatment of chronic plantar fasciitis is the recognition of aetiology and prevention of recurrent injury. Some of the various factors that should be investigated also involve choice of shoes as well as the discarding of old shoes. Shoes with proper shock absorption, and motion control and stability, can be very helpful in preventing this particular injury. In addition, the surfaces on which the participants play should be evaluated, as hard surfaces contribute to the incidence of injury. Conservative care has been shown to be effective after all measures have been employed. Baxter (1994a) studied 200 patients for over 2 years and found that 95% of them recovered and did not require surgery. Most authors have recommended that 6–12 months of conservative treatment be employed before considering surgical intervention (Box 13.5).