Evaluation of Motor Control
Linda Anderson Preston*
Muscle tone assessment/reflexes
Guidelines for muscle tone assessment
Manual rating scales for spasticity and hypertonicity
Mechanical and computer rating systems for spasticity and hypertonicity
Range-of-motion assessment in evaluation of tone
Other considerations in tone assessment
After studying this chapter, the student or practitioner will be able to do the following:
1 Differentiate between upper and lower motor neuron pathologic conditions.
2 List the components of motor control.
4 Differentiate between motor control and neuroplasticity.
5 Compare and contrast spasticity and hypertonia.
6 Recognize four types of rigidity.
7 Differentiate between spinal and cerebral hypertonus.
8 Identify all categories of the Ashworth Scale.
9 List standardized assessments designed for evaluating function after cerebrovascular accident.
10 Describe normal muscle tone.
11 List and describe at least four different states of abnormal tone.
12 Describe how to assess muscle tone.
13 List the components of the postural mechanism.
14 List and describe at least four types of cerebellar disorders.
15 List and describe at least four extrapyramidal disorders.
16 Describe how to assess coordination.
17 Identify impairments that are contributing to functional limitations.
18 Describe the principles of neuroplasticity.
19 Link functional training and neuroplasticity.
20 Name several current medical and surgical treatment options for the management of hypertonia.
21 List at least three conservative occupational therapy interventions for hypertonia.
Motor control is the ability to make dynamic postural adjustments and direct body and limb movement in purposeful activity.97 Components necessary for motor control include normal muscle tone, normal postural tone and postural mechanisms, selective movement, and coordination. Complex neurologic systems (i.e., the cerebral cortex, basal ganglia, and cerebellum) collaborate to make motor control possible. A neurologic insult such as a cerebrovascular accident (stroke or brain attack), brain injury, or a disease such as multiple sclerosis or Parkinson’s disease affects motor control. Functional recovery depends on the initial amount of neurologic damage, prompt access to medical treatment that limits the extent of neurologic damage,86 the nature of the neurologic damage, whether it is static or progressive, and therapeutic intervention that can facilitate motor recovery.
Plasticity is an important concept in neurologic rehabilitation because it helps to explain why recovery is possible after brain injury or lesion. Neuroplasticity is defined as “anatomic[al] and electrophysiologic[al] changes in the central nervous system.”97
In some instances, the central nervous system (CNS) is able to reorganize and adapt to functional demands after injury.18 Motor relearning can occur through the use of existing neural pathways (unmasking) or through the development of new neural connections (sprouting).75 In the case of unmasking, it is believed that seldom-used pathways become more active after the primary pathway has been injured. Adjacent nerves take over the functions of damaged nerves. In the case of sprouting, dendrites from one nerve form a new attachment or synapse with another (Figure 19-1).24 It has also been demonstrated that new axonal processes develop in sprouting.75
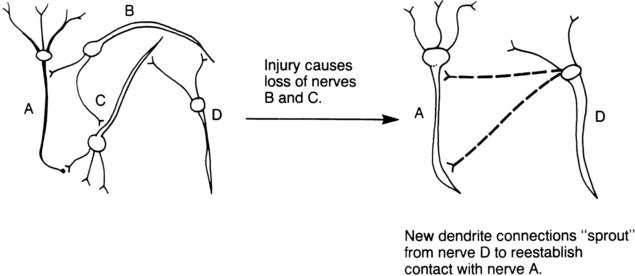
FIGURE 19-1 Sprouting theory of nerve cell replacement. Injury causes loss of nerves B and C. New dendrite connections “sprout” from nerve D to re-establish contact with nerve A. (From DeBoskey DS, et al: Educating families of the head injured, Rockville, Md, 1991, Aspen Publishers.)
Observing movements during occupational performance is a way to assess motor control. Following evaluation of occupational performance, it may be necessary to evaluate the specific components that underlie motor control. These components include muscle tone, postural tone and the postural mechanism, reflexes, selective movement, and coordination.
This chapter focuses on the functional effects of lesions in the upper motor neuron system (UMNS). The UMNS includes any nerve cell body or nerve fiber in the spinal cord (other than the anterior horn cells) and all superior structures. These structures include descending nerve tracts and brain cells of both gray and white matter that subserve motor function.
The lower motor neuron system includes the anterior horn cells of the spinal cord, the spinal nerves, the nuclei and axons of cranial nerves III through X, and the peripheral nerves. Lower motor neuron dysfunction results in diminished or absent deep tendon reflexes and muscle flaccidity. Figure 19-2 illustrates the influence of the upper motor neuron system on the lower motor neuron system.66

FIGURE 19-2 Control of movement is comparable with a chariot driver with a team of horses. The upper motor neuron system facilitates or inhibits the lower motor neuron system. The driver is like the brain, the reins are like the upper motor neurons, and the horses are like lower motor neurons and muscles. (From DeBoskey DS, et al: Educating families of the head injured, Rockville, Md, 1991, Aspen Publishers).
Performance Assessments
The occupational therapist has the challenge of maximizing the client’s ability to return to purposeful and meaningful occupation within his or her physical, cultural, and social environment.93 Therefore, evaluating functional performance is primary in helping clients to set realistic goals. The Canadian Occupational Performance Measure60 is an assessment tool that ensures client-centered therapy. This tool helps prioritize the client’s functional activity goals in the areas of self-care, leisure, and productivity.60
The occupational therapist (OT) can observe the client for motor control dysfunction during assessment of basic activities of daily living (BADLs) and instrumental activities of daily living (IADLs), along with productive and leisure activities. The therapist must observe how problems in motor control affect occupational performance. The therapist must also consider the client’s sensation, perception, cognition, and medical status.
Many activity of daily living (ADL) tests are available to assess occupational performance and are useful in observing motor control. The Test d’Évaluation des Membres Supérieurs de Personnes Âgées (TEMPA) is an upper extremity functional activity performance test for clients. This test was developed to help therapists distinguish between “normal and pathologic[al] aging in upper extremity performance.”26 Test items include picking up and moving a jar, writing on an envelope, tying a scarf, and handling coins, among others.26
Several assessments have been designed to assess function after cerebrovascular accident (CVA). These can be used to observe for motor control problems.
1. The Graded Wolf Motor Function Test (GWMFT) is a new assessment developed to measure functional gains after a hemiparetic event from cerebrovascular accident or traumatic brain injury.72 This test was based on the Wolf Motor Function Test.9 It is called “Graded” because there are two levels of difficulty for each task: level A is more advanced, and level B is easier (Figure 19-3). Gorman38 investigated the interreliability and intrareliability of the GWMFT with a sample of eight physical therapist investigators and three subjects. Intrarater and interrater reliability was .935 on the timing scores. Intrarater reliability was .897 and interrater reliability was .879 on the functional ability scores. This is a very useful test that can be used on a wide variety of clients with hemiparesis with varying degrees of motor recovery. More research is needed to confirm the validity and reliability of this test.

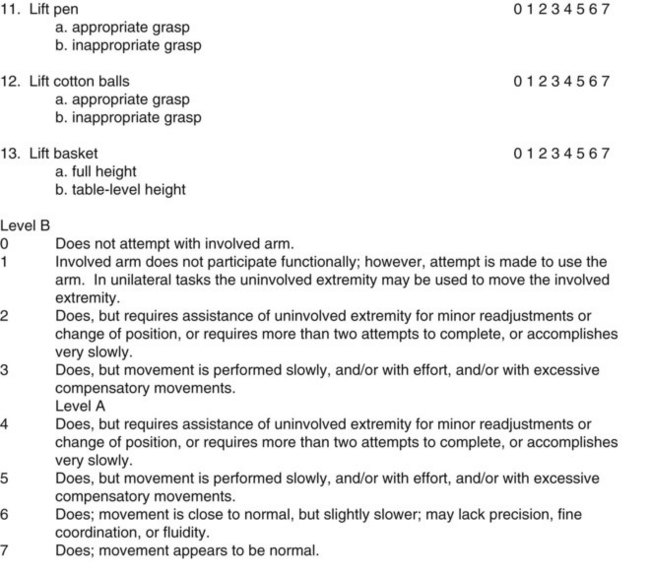
FIGURE 19-3 Graded Wolf Motor Function Test. (From Morris DM, et al: Graded Wolf Motor Function Test. Dr. Edward Taub, Department of Psychology, University of Alabama at Birmingham, Birmingham, Ala, revision date May 6, 2002.)
In the aforementioned case study, Juan’s mean functional ability score was 5.5 (see Figure 19-3). He performed the test items slowly, with effort and lack of precision.
2. The Wolf Motor Function Test (WMFT) has been used to quantify the motor abilities of chronic clients from a population with high upper extremity function following CVA or traumatic brain injury. It has an interrater reliability range of .95 to .97.9
3. The Functional Test for the Hemiplegic/Paretic Upper Extremity103 assesses the client’s ability to use the involved arm for purposeful tasks. This test provides objective documentation of functional improvement and includes tasks ranging from those that involve basic stabilization to more difficult tasks requiring fine manipulation and proximal stabilization. Examples include holding a pouch, stabilizing a jar, wringing a rag, hooking and zipping a zipper, folding a sheet, and putting in a light bulb overhead.103
4. The Fugl-Meyer55 assessment is based on the natural progression of neurologic recovery after CVA. Low scores on the Fugl-Meyer have been closely correlated with the presence of severe spasticity. Fugl-Meyer and associates developed a quantitative assessment of motor function following stroke by measuring such parameters as range of motion (ROM), pain, sensation, and balance. Scores on the Fugl-Meyer assessment correlate with ADL performance.55
5. The Arm Motor Ability Test (AMAT)58 is a functional assessment of upper extremity function. Cutting meat, making a sandwich, opening a jar, and putting on a T-shirt are some of the tasks included in this test. This test has high interrater and test-retest reliability.58
6. The Motricity Index (MI)21 is a valid and reliable test of motor impairment that can be performed quickly. The test assesses pinching a cube with the index finger and thumb, as well as elbow flexion, shoulder abduction, ankle dorsiflexion, knee extension, and hip flexion.21
7. The Assessment of Motor and Process Skills (AMPS)7 is a standardized test that assesses motor and process skills in IADLs. The test was created by occupational therapists. Although this test is not diagnosis specific, it has been widely used with clients who have had a CVA. Occupational therapy practitioners are eligible to become certified in the use of this test upon completion of a 5-day training course.7
After observing functional performance, the occupational therapist usually will find it necessary to assess the performance components that underlie motor control: muscle tone (normal/abnormal), the postural mechanism, muscle tone assessment/reflexes, sensation, and coordination.
Normal Muscle Tone
Normal muscle tone, a component of the normal postural mechanism, is a continuous state of mild contraction, or a state of preparedness in the muscle.87 Tone is the resistance felt by the examiner as he or she passively moves a client’s limb. It is dependent on the integrity of peripheral and CNS mechanisms and the properties of muscle. When normal muscle tone is present, tension between the origin and the insertion of a muscle is felt as resistance by the therapist when passively manipulating the limb. It is high enough to resist gravity, yet low enough to allow movement. The tension is determined in part by mechanical factors such as connective tissue and viscoelastic properties of muscle, and in part by the degree of motor unit activity. When passively stretched, normal muscle offers a small amount of involuntary resistance.
Normal muscle tone relies on normal function of the cerebellum, motor cortex, basal ganglia, midbrain, vestibular system, spinal cord, and neuromuscular system (including the mechanical-elastic features of the muscle and connective tissues),54 and on a normally functioning stretch reflex. The stretch reflex is mediated by the muscle spindle, a sophisticated sensory receptor that continuously reports sensory information from muscles to the CNS.
Normal muscle tone varies from one individual to another. Within the range that is considered normal, the degree of normal tone depends on such factors as age, sex, and occupation. Normal muscle tone is characterized by the following:
1. Effective coactivation (stabilization) at axial and proximal joints
2. Ability to move against gravity and resistance
3. Ability to maintain the position of the limb if it is placed passively by the examiner and then released
4. Balanced tone between agonistic and antagonistic muscles
5. Ease of ability to shift from stability to mobility and to reverse as needed
6. Ability to use muscles in groups or selectively with normal timing and coordination
7. Resilience or slight resistance in response to passive movement
Hypertonicity (increased tone) interferes with the performance of normal selective movement because it affects the timing and smoothness of agonist and antagonist muscles groups. Normalization of muscle tone and amelioration of paresis (slight or incomplete paralysis/weakness) are desirable when striving for selective motor control. Some function can be achieved even though tone may not be normal.83
Abnormal Muscle Tone
Abnormal muscle tone usually is described with the following terms: flaccidity, hypotonus, hypertonus, spasticity, and rigidity. To plan appropriate treatment interventions, the therapist must recognize the differences among these tone states and must identify them during the clinical assessment, to plan the appropriate intervention.
Flaccidity
Flaccidity refers to the absence of tone. The client will have absent deep tendon reflexes. Active movement is absent as well. Flaccidity can result from spinal or cerebral shock immediately after a spinal or cerebral insult. In traumatic upper motor neuron lesions of cerebral or spinal origin, flaccidity usually is present initially and then changes to hypertonicity within a few weeks.63
Flaccidity also can result from lower motor neuron dysfunction, such as peripheral nerve injury or disruption of the reflex arc at the alpha motor neuron level. The muscles feel soft and offer no resistance to passive movement. If the flaccid limb is moved passively, it will feel heavy. If moved to a given position and released, the limb will drop because the muscles are unable to resist the pull of gravity.96
Hypotonus
Hypotonus is considered by many to be a decrease in normal muscle tone (i.e., low tone). Deep tendon reflexes are diminished or absent. Van der Meche and Van der Gijn100 suggested that hypotonus could be an erroneous clinical concept. They performed electromyography (EMG) analysis on the quadriceps muscles in “hypotonic” clients (e.g., peripheral neuropathy, cerebral infarction, other diagnoses) and in relaxed normal subjects in a lower leg free-fall test. They concluded in their study that if a client’s limb feels hypotonic or flaccid, this is the result of weakness, not of long-latency stretch reflexes.100
Hypertonus
Hypertonus is increased muscle tone. Hypertonicity can occur when a lesion is present in the premotor cortex, the basal ganglia, or descending pathways. Damage to upper motor neuron systems increases stimulation of the lower motor neurons, with resultant increased alpha motor activity. Any neurologic condition that changes the upper motor neuron pathways that directly or indirectly facilitate alpha motor neuron activity may result in hypertonicity. Other spinal or brainstem reflexes may become hyperactive, which leads to hypertonus patterns such as the flexor withdrawal or the re-emergence of tonic neck reflexes.63
Hypertonicity often occurs in a synergistic neuromuscular pattern, particularly when seen after CVA or traumatic brain injury. Synergies are defined as patterned movement characterized by co-contraction of flexors and extensors. A typical synergy seen in the upper extremity after CVA or traumatic brain injury is a flexion synergy.62 In contrast, an extension synergy is seen in the lower extremity.
The energy cost in moving against hypertonicity is considerable. It takes a great deal of effort for clients with moderate to severe hypertonicity to move against this drawing force. Antagonist power may be insufficient to overcome the spastic agonist muscle groups. Even clients with mild hypertonicity report frustration during functional activities. Loss of reciprocal inhibition is noted between spastic agonists and antagonists. Clients are unable to rapidly turn off their muscles. The client with an upper motor neuron lesion will have dysfunction in spatial and temporal timing of movement. This makes his/her movements very uncoordinated.104 This frustration, coupled with the fatigue, decreased dexterity, and paresis associated with UMNS, can influence therapy participation.80 Furthermore, the architecture of hypertonic muscles changes over time. The muscles lose their ability to lengthen and shorten because of viscoelastic changes that result from the hypertonia.18,54
The abnormal timing of Juan’s distal upper extremity muscles, particularly between the finger flexors and extensors, impaired his coordination so much that he could not play the keyboard with his left hand.
Hypertonicity can increase as a result of painful or noxious stimuli. These stimuli often can be reduced with good medical care. Stimuli that can increase tone include pressure sores, ingrown toenails, tight elastic straps on a urine collection leg bag, tight clothing, an obstructed catheter, urinary tract infection, constipation, and fecal impaction.29,51 Other triggering factors include fear, anxiety, environmental temperature extremes, heterotopic ossification, and sensory overload. These factors are true for both cerebral and spinal hypertonicity; however, they are more pronounced in spinal hypertonia. Therapeutic intervention should be designed to reduce, eliminate, or cope with these extrinsic factors.
Clients with hypertonicity often have difficulty initiating movement, especially rapid movement.54 Although hypertonic muscles appear to be able to take a lot of resistance, they do not function as normal, strong muscles do. Through the mechanism of reciprocal inhibition, hypertonic muscles inhibit the activity of their antagonists and thus can mask potentially good or normal function of antagonists.83,97 Four types of hypertonia are described in the following paragraphs.
Cerebral Hypertonia
Cerebral hypertonia is caused by traumatic brain injury, stroke, anoxia, neoplasms (brain tumors), metabolic disorders, cerebral palsy, and diseases of the brain. In multiple sclerosis, hypertonia is produced from both spinal and cerebral lesions. Tone fluctuates continuously in response to extrinsic and intrinsic factors. Cerebral hypertonia usually occurs in definite patterns of flexion or extension, causing the limb to be pulled in one direction (Figure 19-4). Typically, these patterns occur in the antigravity muscles of the upper and lower extremities (e.g., flexors of the upper extremities, extensors of the lower extremities).
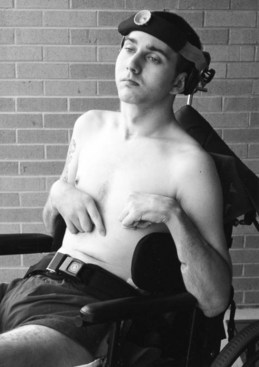
FIGURE 19-4 A client with right upper extremity dystonic posturing of the wrist and finger extensors. His left wrist shows severe hypertonicity. Tone abnormalities are the result of a traumatic brain injury.
The re-emergence of primitive reflexes and associated reactions alters postural tone. When an individual is lying supine, muscle tone is less than when the individual is sitting or standing. The tone is at its highest during ambulation. Thus, attention to postural tone is important when positioning a client for splinting or casting. A cast or splint fabricated on a client in a supine position may not fit when the client is sitting up because of the influence of gravity and posture on increasing muscle tone.83
Spinal Hypertonia
Spinal hypertonia results from injuries and diseases of the spinal cord. In slow-onset spinal disease (e.g., spinal stenosis, tumor), there is no period of spinal shock. In traumatic spinal cord injury, spinal shock occurs and is characterized by initial flaccidity. Over time (weeks or months), the flaccidity diminishes and hypertonus develops. The affected extremities first develop flexor and adductor tone.105 Over time, extensor tone develops and becomes predominant in the lower extremities. Spinal hypertonia can lead to muscle spasms severe enough to cause an individual to fall out of a wheelchair, off a gurney, or out of bed. The degree of hypertonicity in incomplete spinal lesions varies, depending on the degree of damage to the spinal cord. The tone tends to be more severe in incomplete spinal cord lesions than in complete lesions.83
Spasticity
Much controversy in recent years has surrounded the difference between spasticity and hypertonia. Lance’s59 definition of spasticity is still accepted by many physicians and therapists. He defined spasticity as “a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon jerks resulting from hyperexcitability of the stretch reflex as one component of the upper motor neuron syndrome.”59
Little and Massagli62,63 believe that pure spasticity is a subset of hypertonia. It is possible that Lance’s definition does not adequately distinguish between the presence of phasic and tonic stretch reflexes, which present different clinical scenarios. This chapter attempts to clarify the differences using current physiatry literature.
Spasticity has three characteristics:
1. Hyperactivity of the muscle spindle’s phasic stretch reflex with hyperactive firing of the Ia afferent nerve.
2. Velocity dependence, meaning that the stretch reflex is elicited only by the examiner’s rapid passive stretch.62,63
3. The “clasp-knife” phenomenon. This means that when the examiner takes the extremity through a quick passive stretch, a sudden catch or resistance is felt, followed by a release of the resistance. What actually happens is that the initial high resistance of spasticity is suddenly inhibited.54
One of the main systems affected when spasticity is present is the pyramidal system, which consists of the corticospinal and corticobulbar tracts. The corticospinal tract controls goal-directed, voluntary movement by influencing the lower motor neuron. The corticobulbar tract influences the voluntary action of the cranial nerves.18
Therapists often confuse hypertonia with spasticity. These two conditions are similar because both pull the limb into a unilateral direction.
Hypertonia is different from spasticity in two ways:
1. Hypertonia typically is not velocity dependent, that is, rapid movement does not evoke it; rather, slow joint movement elicits hypertonia. Hypertonus persists as long as the muscle stretch is maintained because of the firing of group II muscle spindle afferents (tonic stretch reflex).62,63
2. During passive movement, no catch is felt with hypertonia, as is felt with the clasp-knife phenomenon of spasticity. This is objectively measurable with EMG.55
Clonus
Clonus is a specific type of spasticity. This condition often is present in clients with moderate to severe spasticity. Clonus is characterized by repetitive contractions in the antagonistic muscles in response to rapid stretch. Recurrent bursts of Ia afferent activity result in a cyclic oscillation of phasic stretch reflexes.54,63 Clonus is seen most commonly in the finger flexors and ankle plantar flexors.63 The occurrence of clonus can interfere with participation in purposeful activity, transfers, and mobility. Therapists should educate clients and their families about how to bear weight actively because this usually will stop the clonus. Therapists and physicians record clonus by counting the number of beats.54 A three-beat clonus can be rated as mild and is less likely to interfere with ADLs than a clonus that is 10 beats or more. Clonus may be elicited during quick stretch tone evaluation or may become apparent during assessment of occupation (e.g., grasping, ambulation). If clonus greatly interferes with ADLs, the client may be a candidate for a referral to a physiatrist or neurologist for oral medication, Botox12 injection, Myobloc73 injection, or alcohol or phenol motor point block.80
Rigidity
Rigidity is a simultaneous increase in muscle tone of agonist and antagonist muscles (i.e., muscles on both sides of the joint). Both groups of muscles contract steadily, leading to increased resistance to passive movement in any direction and throughout the ROM. Rigidity signals involvement of the extrapyramidal pathways in the circuitry of the basal ganglia, diencephalon, and brainstem. It occurs in isolated forms in disorders such as Parkinson’s disease, traumatic brain injury, some degenerative diseases, encephalitis, and tumors,25 and after poisoning from certain toxins and carbon monoxide. Rigidity also is seen in conjunction with spasticity in those with stroke and traumatic brain injury. Rigidity is not velocity dependent.96
Rigidity is evaluated during muscle tone evaluation (see Figure 19-4). Four types of rigidity are commonly seen:
Both lead pipe and cogwheel rigidity can occur in Parkinson’s disease. In lead pipe rigidity, constant resistance is felt throughout the ROM when the part is moved slowly and passively in any direction. This rigidity feels similar to the feeling of bending solder or a lead pipe, thus its name. In cogwheel rigidity, a rhythmic give in resistance occurs throughout the ROM, much like the feeling of turning a cogwheel. It is thought that cogwheel rigidity is lead pipe rigidity with concomitant tremor, which results in the ratchety pattern.70 Deep tendon reflexes are normal or are only mildly increased in Parkinson’s rigidity.
Decerebrate and decorticate rigidity can occur after severe traumatic brain injury with diffuse cerebral damage or anoxia. These abnormal postures occur immediately after injury and can last a few days or weeks if recovery occurs, or can persist indefinitely if there is little or no recovery.
Decerebrate rigidity results from lesions in the bilateral hemispheres of the diencephalon and midbrain. It appears as rigid extension posturing of all limbs and the neck. Bilateral cortical lesions can result in decorticate rigidity, which appears as flexion hypertonus in the upper extremities and as extension tone in the lower extremities. Supine positioning increases the abnormal tone, and with either type of rigidity it may be extremely difficult to position clients in a sitting position.63
Muscle Tone Assessment
Objective assessment of muscle tone in the client with cerebral spasticity is difficult because the tone fluctuates continuously in response to extrinsic and intrinsic factors. The postural reflex mechanism, the position of the body and head in space, the position of the head in relation to the body, and stereotypical reflexes and associated reactions all influence the degree and distribution of abnormal muscle tone.87
Guidelines for Muscle Tone Assessment
The following steps describe correct procedures for assessing muscle tone.
It is helpful to rate spasticity and hypertonia with the client in the same position, preferably at the same time of day, to enhance reliability, because body and head position influence cerebral hypertonus. The client’s upper extremity muscle tone usually is evaluated with the client sitting on a mat table when possible. Remember that the client’s trunk posture (e.g., the seated client bearing weight symmetrically vs. slumped or leaning to one side) will affect the results of the tone evaluation. Tone fluctuates from hour to hour and from day to day because of intrinsic and extrinsic factors that influence it. This fluctuation makes accurate measurement difficult, particularly for cerebral hypertonia. Rating tone is still worthwhile, especially in the managed care environment, in which objective measures of progress are needed to justify the continuation of therapy.
Grasp the client’s limb proximal and distal to the joint to be tested and move the joint slowly through its range to determine the free and easy ROM available. Note the presence and location of pain. If there is no active movement and if the limb feels heavy, record that the limb is flaccid or “0” in strength. If the limb has some active movement and no evidence of increased tone, the affected muscle or muscle group may be labeled “paretic” instead of “hypotonic.” The paretic antagonist muscle can then be graded in strength (usually the strength grade will fall between 1 and 4−). Grading the paretic antagonist muscles provides more objective clinical information than merely labeling the muscles as hypotonic. Strength grading antagonists can help the occupational therapist to triage phenol block and botulinum toxin type A or B injection candidates who have the potential to improve function; for example, a client with an elbow extension strength grade of 2− (in the presence of elbow flexor tone) would be a better block candidate than a client with a triceps strength grade of 0.
Juan did not have sufficient strength in his supinators (4−/5) or in his finger extensors (extrinsic 3−/5, intrinsic 2−/5) to counteract the pull of moderate finger flexor and pronator hypertonia.
Hold the limb on the lateral aspects to avoid giving tactile stimulation to the muscle belly of the muscle being tested.
Clinical assessment of spasticity involves holding the client’s limb as just described and moving it rapidly through its full range while the client is relaxed. Label the tone “mild,” “moderate,” or “severe.” (Refer to tone rating scales defined in the next section.)
Clinical assessment of rigidity and hypertonia involves moving the limb slowly during the range, noting the location of first tone or resistance to movement in degrees and labeling it “mild,” “moderate,” or “severe.” Some physicians find goniometric measuring of the location of the first tone helpful before and after long-acting nerve block. Others find documentation of the limb’s resting position helpful before and after injection.65
Manual Rating Scales for Spasticity and Hypertonicity
The Ashworth Scale4 (Box 19-1) and the Modified Ashworth Scale10 (MAS) are the two scales most widely used to manually rate spasticity.75,89 These scales were not designed to differentiate between pure spasticity and hypertonic stretch reflexes. They are used to quantify the degree of hypertonus. Controversy can be found in the literature about the validity and reliability of these scales. Brashear and associates concluded that in upper limb spasticity, the Ashworth Scale had good intrarater and interrater reliability when used by trained medical professionals.14 However, Seghal and McGuire88 believed that the Ashworth scale lacks reliability. Pandyan and colleagues76,78 noted that the Ashworth Scale and the Modified Ashworth Scale should be used as an ordinal scale of resistance to passive movement; however, they are not valid for assessing spasticity. Preston believes that both scales should be considered nominal because the last stage of each scale is describing rigidity, not spasticity. Rigidity is an extrapyramidal phenomenon and spasticity is pyramidal; therefore the two should not be measured on the same scale.81
Three studies have demonstrated that the MAS is a reliable scale for assessment of spasticity.10,40,41 Four studies have reported that it is not reliable.3,8,31,62 Therapists familiar with the Ashworth Scale can help physicians evaluate candidates for neurosurgical procedures. For example, some of the selection criteria for the Synchromed Intrathecal Baclofen Pump (ITB)69 implantation are based on the presence of a two-point reduction on the Ashworth Scale after the test dose of medication is given.83 Resistance encountered during passive muscle stretching is described in Box 19-1.
Tardieu Scale
Both the Modified Tardieu Scale (MTS)13 and the Tardieu Scale43 measure spasticity.34 The Tardieu Scale is written in French and was not reviewed. The MTS had an interrater reliability coefficient of .7 and was shown to be more reliable than the aforementioned MAS.39
Mild-Moderate-Severe Spasticity Scale
Some therapists and physicians find a mild-moderate-severe scale easier to use than the aforementioned scales. The scale in Box 19-2 is suggested as a guide for estimating the degree of spasticity.30
Preston’s Hypertonicity Scale
Some therapists and physicians find a mild-moderate-severe hypertonia scale easier to use. The scales in Box 19-3 are suggested as a guide for estimating the degree of hypertonicity.
One of the reasons why Juan could not keyboard with his left hand was the presence of moderate hypertonia in his finger flexors. He could not retrieve change in his left hand from the drive-through window cashier because moderate hypertonia in his forearm pronators limited full active supination. One needs to have close to normal supination and functional grasp/release to obtain change from a drive-through cashier.
Mechanical and Computer Rating Systems for Spasticity and Hypertonicity
Mechanically determined parameters of assessing hypertonia may be more reliable than the aforementioned manual methods. McCrea and coworkers67 concluded that using a linear spring damper model to assess the hypertonic elbow was reliable and valid. This model is not widely used in clinical practice, nor even in research practice, because of time constraints and difficulty accessing certain muscle groups (e.g., it is easier to set up and measure elbow hypertonia than hip hypertonia in a mechanical tone rating device).
Leonard and associates investigated the construct validity of the Myotonometer (Neurogenic Technologies, Inc., Missoula, Mont), a newly developed computerized, electronic device with a probe (that looks similar to an ultrasound transducer) that is placed on top of the skin over the muscle belly. Measurements were taken over the biceps brachii at rest and during maximum voluntary muscle contraction. They revealed a significant difference between affected and unaffected extremities in subjects with upper motor neuron spasticity. The authors concluded that the Myotonometer could provide objective data about the tone reduction efficacy of various tone reducing procedures.61
Clearly, more research is needed in the areas of manual, mechanical, and computer rating systems for assessment of hypertonia. Sehgal and McGuire summed up the controversy over hypertonia/spasticity rating scales quite well: “A uniformly acceptable, reliable and practical measure of spasticity continues to elude the clinician.”88
Range-of-Motion Assessment in Evaluation of Tone
Passive ROM (PROM) assessment supplements and often correlates with tone assessment. For example, if a client with acute CVA (1 month after onset) has a wrist ROM measurement of 20 degrees extension (normal, 70 degrees), and if orthopedic causes (e.g., arthritis, fixed contracture) have been ruled out, the therapist should assess the tone in the wrist flexors and the extrinsic finger flexors. Hypertonicity of any of these muscles can prohibit full wrist extension. Assessment of PROM can reveal possible signs of joint changes (e.g., subluxation, dislocation, contracture) that have occurred from chronic hypertonus, such as proximal interphalangeal joints (PIPs) that measure −45 to 125 degrees instead of 0 to 100 degrees. Some physicians find PROM measurements useful in documenting the location of the first tone, or resting position, before and after Botox12 or Myobloc73 injections.
Juan had only 20 degrees of active supination. His passive range of motion was not limited. He has a soft tissue limitation of active supination as the result of paresis of the supinator and hypertonicity of the pronators; 20 degrees of supination is not enough to orient his hand palm up to hold coins.
Other Considerations in Tone Assessment
Changes in bone or other peripheral structures can lead to ROM limitations. For example, the presence of heterotopic ossification can limit joint ROM. Heterotopic ossification is the formation of new bone in soft tissue or joints, which can lead to joint ankylosis. Heterotopic ossification can occur in individuals with traumatic brain injury and spinal cord injury, along with severe spasticity, or with other types of severe injuries.11,53,102 Conversely, the presence of fixed contractures may be incorrectly labeled as hypertonus. Physiatrists and other physician specialists can aid in the diagnosis of contractures with the use of diagnostic short-term nerve blocks, EMG, and/or X-rays.83
Incidentally, Juan had no passive range-of-motion deficits, so he did not have contractures.
Assessing Movement and Control
Along with the assessment of muscle tone previously described, the occupational therapist performs an assessment of upper extremity movement and control. The therapist identifies where and how much the client’s motor control is dominated by synergies, and where selective, isolated movement is present. The degree to which abnormal tone interferes with selective control is identified. Also, identifying in which direction of movement hypertonicity occurs and how it affects function helps in determining the need for intervention.
Manual muscle testing usually is not appropriate for clients who exhibit moderate to severe hypertonicity or rigidity, because the relative tone and strength of the muscles are not normal, and movement is not voluntary or selective. Tone and strength are influenced by the position of the head and body in space, as well as by abnormal contraction, deficits in tactile and proprioceptive sensation, and impaired reciprocal inhibition.104 However, if hypertonia is mild and selective movements are possible, it is helpful to grade the strength of the antagonists to measure progress objectively.83
Position change, spinal reflexes, the reticular formation, and supraspinal reflexes influence muscle tone and motor control. Because the level and distribution of muscle tone change as the position of the head in space and of the head in relation to the body changes, tone cannot be assessed in isolation from postural mechanisms, motor function, synergies present, task specificity, and other factors related to motor control.48
Sensation
The following sensibility tests are recommended for clients with damage to the central nervous system: static two-point discrimination, kinesthesia, proprioception, pain, and light touch using the Semmes-Weinstein monofilament test.5 The therapist can assess light touch more accurately with the Semmes-Weinstein monofilaments because they provide better pressure control than a cotton ball. (Chapter 23 discusses procedures for administration of these sensory tests.)
Medical Assessment of Muscle Tone
Physiatrists, orthopedic surgeons, and neurologists are some of the physicians who may specialize in assessment of muscle tone. They may use static or dynamic surface or percutaneous (needle) EMG. Multiple channels are used in dynamic EMG to evaluate the hypertonicity of many contributing muscles.62 EMG helps the physician determine abnormal, excessive electrical activity in muscles. EMG can help physiatrists and neurologists plan and implement short- and long-acting nerve blocks to treat hypertonia. Clients who have local muscle wasting, flaccidity, numbness, or unexplained paresis should undergo EMG assessment to rule out peripheral neuropathy.102
Normal Postural Mechanism
The normal postural mechanism is composed of automatic movements that provide an appropriate level of stability and mobility. These automatic reactions develop in the early years of life and allow for trunk control and mobility, head control, midline orientation of self, weight bearing and weight shifting in all directions, dynamic balance, and controlled voluntary limb movement. Components of the normal postural mechanism include normal postural tone and control, integration of primitive reflexes and mass movement patterns, righting reactions, equilibrium and protective reactions, and selective movement.
In clients who have suffered UMNS damage, the normal postural mechanism is disrupted. Abnormal tone and mass patterns of movement dominate clients’ movements, and these clients have impaired balance and stability. Movements are slow and uncoordinated. Therapists must assess the extent of damage to the postural mechanism in clients with CNS trauma or disease.
Normal postural tone allows automatic and continuous postural adjustment to movement. Postural control is the ability to control or regulate specific postural outputs. It is important to assess the following automatic reactions, which are part of the postural mechanism, in clients with CNS trauma or disease.
Righting Reactions
Righting reactions direct the head to an upright position. Righting reactions help one assume a position. Automatic reactions maintain and restore the normal position of the head in space and the normal relationship of the head to the trunk, as well as the normal alignment of the trunk and limbs. Without effective righting reactions, the client will have difficulty getting up from the floor, getting out of bed, sitting up, and kneeling.92
Equilibrium Reactions
Equilibrium reactions help one sustain or keep a position. They are the “first line of defense against falling.”87 Equilibrium reactions, which are elicited by stimulation of the labyrinths within the inner ear, are used to maintain and regain balance in all activities. These reactions ensure sufficient postural alignment when the body’s center of gravity is altered by a change in the supporting surface.52 Without equilibrium reactions, the client will have difficulty maintaining and recovering balance in all positions and activities.
Protective Reactions
Protective reactions are the second line of defense against falling if the equilibrium reactions cannot correct a balance perturbation. They consist of protective extension of the arms and hands, which is used to protect the head and face when one is falling. Stepping and hopping are examples of lower extremity protective reactions. Without protective reactions, the client may fall or may be reluctant to bear weight on the affected side during normal bilateral activities.87
Assessment of Righting, Equilibrium, Protective Reactions, and Balance
Formal testing of these reactions may be difficult because of the cognitive and physical limitations of the client or time constraints of the therapist. The therapist can evaluate righting reactions, however, during transfers and ADLs. Equilibrium and protective reactions can be observed when the client shifts farther out of midline than necessary during functional activities, such as lower extremity dressing.
Balance depends on normal equilibrium and protective reactions. Balance is “the ability to maintain the center of gravity over the base of support, usually while in an upright position.”56 Balance involves a complex interaction between many systems, including the vestibular, proprioceptive, and visual systems, and motor modulation from the cerebellum, basal ganglia, and cerebral cortex. Occupational and physical therapists must also observe the client’s ankle, hip, and step strategies and note areas of breakdown in the kinetic chain.28,96
When assessing a client with CNS dysfunction, the therapist should assess the client’s static and dynamic balance before leaving the client unattended on a mat table, in a wheelchair, or during ambulatory ADLs. Dynamic balance involves maintaining balance while moving, and static balance involves maintaining equilibrium while stationary.
The Physical Performance Test assesses physical function during activity. Seven of the nine tested items involve static and dynamic balance.101 The test takes only 10 minutes to complete.85 Figure 19-5 shows the test form and test protocol. Two other noteworthy balance assessments are the Tinetti Balance Test of the Performance-Oriented Assessment of Mobility Problems94 and the Berg Balance Scale.6
Primitive Reflexes
The dominance of primitive reflex movement patterns can interfere with the client’s occupational performance. Difficulties that may be encountered are described in the following paragraphs. Observation of these motor behaviors is a way of evaluating for the presence of primitive reflexes.
Brainstem Level Reflexes
Asymmetric Tonic Neck Reflex (ATNR): The ATNR is tested with the client positioned supine or sitting.
Stimulus: actively or passively turn the client’s head 90 degrees to one side.
Response: an increase in extensor tone of the limb on the face side and an increase in flexor tone on the skull side of the limb.37
The client with an asymmetric tonic neck reflex may have difficulty maintaining the head in midline while moving the eyes toward or past midline. The client may be unable to (1) extend an arm without turning the head, or (2) flex the arm without turning the head the other way. The client may be unable to move either or both arms to midline, especially when in the supine position, because movement of the arms is dependent on head positioning. This positioning causes asymmetry in the arms. Thus, this reflex makes it difficult or impossible to bring an object to the mouth, hold an object in both hands, or grasp an object in front of the body while looking at it.
Symmetric Tonic Neck Reflex (STNR): The STNR is tested with the client positioned sitting or quadruped.
Stimulus 1: flex the client’s head and bring his/her chin toward the chest.
Response: flexion of the upper extremities and extension of the lower extremities.
Stimulus 2: extend the client’s head.
Response: extension of the upper extremities and flexion of the lower extremities.57
The client with the STNR will be unable to support the body weight on hands and knees, to maintain balance in a quadruped position, or to crawl normally without fixating the head. The client will have difficulty moving from lying to sitting because when the head is lifted to initiate the task, increased hip extension resists the movement. As he or she struggles to sit up, increased leg extension can interfere. The client will have difficulty with transfers from bed to wheelchair and from wheelchair to bed, because as the arms and neck are extended to initiate the transfer, one or both legs may show increased flexion, which may cause the client to slide under the bed or wheelchair. Additionally, the affected leg may actually lift off the floor, causing an inability to bear weight on that extremity.23
Tonic Labyrinthine Reflex (TLR): The TLR can be tested with the client supine with his or her head in midposition. The stimulus is the test position. The response is an increase in extension tone or extension of the extremities. The TLR can also be tested with the client prone with the head in midposition; again, the test position is the stimulus. The response is an increase in flexor tone or flexion of the extremities. The client who exhibits a poorly integrated tonic labyrinthine reflex will be severely limited in the ability to move. Functional limitations include an inability to lift the head in the supine position, to initiate flexion to sit up independently from the supine position, to roll over, or to sit in a wheelchair for long periods. In attempts to move from a supine to a sitting position, extensor tone will dominate until the client is halfway up, when flexor tone begins to take over. Flexor tone continues until full sitting is reached, causing the head to fall forward, the spine to flex, and the client to fall forward. Sitting in a wheelchair for extended periods can lead to increased extensor tone as the client hyperextends the head to view the environment. The knee is extended, the foot is pushed forward off the wheelchair footrest, and eventually the client may slip or remain in a half-lying asymmetric position.57
Positive Supporting Reaction: The positive supporting reaction is caused by pressure on the ball of the foot. This stimulus elicits the following response: rigid extension of the lower extremities due to co-contraction of the flexors and extensors of the knee and hip joints.57 One may also see internal rotation of the hip, ankle plantar flexion, and foot inversion. The client with a positive supporting reaction will have difficulty placing the heel on the ground for standing, putting the heel down first in walking, and having normal body weight transference in walking. The client will have difficulty getting up from a chair, sitting in a chair, or walking down steps, because the leg remains in rigid extension and it is not possible to move the joints while weight bearing. The rigid leg can carry the client’s body weight but is unable to contribute to any balance reactions. All balance reactions therefore are compensated for by other parts of the body.57
Spinal Level Reflexes
Spinal reflexes can occur after an upper motor neuron lesion. They appear because of lack of integration with higher centers. Some examples of exaggerated spinal reflexes are hyperactive deep tendon reflexes, the Babinski sign, flexor withdrawal reflex, crossed extension, and grasp reflex.50 Three spinal reflexes are reviewed.57
Crossed Extension Reflex: The crossed extension reflex causes increased extensor tone in one leg when the other leg is flexed. Therefore, if the client with hemiplegia who is influenced by this reflex flexes the unaffected leg for walking, a strong extensor hypertonicity occurs in the affected leg and interferes with the normal pattern of ambulation. By the same token, the client can bridge (lift buttocks) in bed with the weight supported by both legs. If the unaffected leg is lifted (with hip flexed), however, a total extension pattern occurs in the affected leg and the bridge cannot be maintained.57
Flexor Withdrawal: The client with flexor withdrawal will exhibit flexion of the ankle, knee, and hip when the sole of the foot is touched (swiped heel to ball of foot). This reflex clearly interferes with gait pattern and transfers.57
Grasp Reflex: The client with a grasp reflex will not be able to release objects placed in the hand, even if active finger extension is present. The reflexes just discussed are rarely seen in isolation.51
Trunk Control Assessment
Collin and Wade21 designed a quick and easily administered test of trunk control that is valid and reliable in clients with a diagnosis of CVA. It involves four timed tests: (1) rolling to the weak side, (2) rolling to the sound side, (3) moving from supine to sitting, and (4) sitting on the side of the bed with feet off the floor for 30 seconds.21
To accurately assess trunk control, the therapist must evaluate strength and control in the following muscle groups: trunk flexors, extensors, lateral flexors, and rotators. The client should be sitting upright on a mat table with the feet supported for all tests. Again, the client should not be left unattended on the mat table until the therapist determines that the client has adequate trunk control and sitting balance. The procedures described in the following sections are condensed from Gillen’s Stroke Rehabilitation: A Function-Based Approach.36
Trunk Flexors
The examiner asks the client to sit upright, to slowly move his or her shoulders behind the hips (eccentric control), and to hold the end-range posture (isometric control) (Figure 19-6, A). The client then is asked to move forward (concentric control) to resume the initial upright posture (Figure 19-6, B).
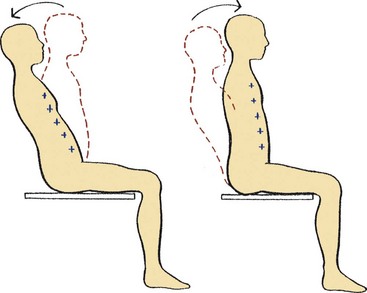
FIGURE 19-6 Trunk flexor control. Dotted lines indicate trunk starting position, solid lines indicate trunk final position, arrows indicate movement direction, and plus symbols indicate muscle groups primarily responsible for control of the pattern. (Skeletal muscle activity occurs on both sides of the trunk [reciprocal innervation].) (From Gillen G, Burkhardt A: Stroke rehabilitation: a function-based approach, ed 2, St Louis, Mo, 2004, Elsevier Mosby.)
The examiner should observe for evidence of unilateral weakness, potential for falls, and symmetry of weight shift. A functional test for trunk flexor control is to observe the client move from supine to sitting.
Trunk Extensors
Test 1: The client is sitting in a position of spinal flexion with a posterior pelvic tilt and moves into trunk extension while simultaneously moving the pelvis into neutral or into a slight anterior tilt. This test assesses concentric trunk extensor control, which is a prerequisite for lower extremity dressing and forward reach (Figure 19-7, A).
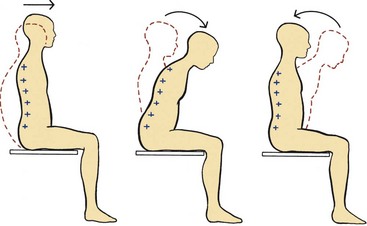
FIGURE 19-7 Trunk extensor control. Dotted lines indicate trunk starting position, solid lines indicate trunk final position, arrows indicate movement direction, and plus symbols indicate muscle groups primarily responsible for control of the pattern. (Skeletal muscle activity occurs on both sides of the trunk [reciprocal innervation].) (From Gillen G, Burkhardt A: Stroke rehabilitation: a function-based approach, ed 2, St Louis, Mo, 2004, Elsevier Mosby.)
Test 2: The client is seated in an upright posture. The examiner asks the client to maintain an erect spine and lean forward. This test evaluates eccentric trunk extensor control (Figure 19-7, B). For both trunk extensor tests, the examiner should observe signs of unilateral weakness and note end-range control.
Test 3: The client is asked to move his or her shoulders back to assume a seated, aligned, upright position. The trunk extensors are contracting concentrically (Figure 19-7, C).
Lateral Flexors
The client sits in an upright posture. The pelvis is stationary, and the upper trunk laterally flexes toward the mat table. Figure 19-8, A, shows eccentric contraction of the left side and muscle shortening of the right side. The client is asked to return to the original test position (concentric control of the left side) (Figure 19-8, B).
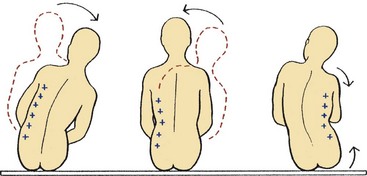
FIGURE 19-8 Lateral flexor control. Dotted lines indicate trunk starting position, solid lines indicate trunk final position, arrows indicate movement direction, and plus symbols indicate muscle groups primarily responsible for control of pattern. (Skeletal muscle activity occurs on both sides of the trunk [reciprocal innervation].) (From Gillen G, Burkhardt A: Stroke rehabilitation: a function-based approach, ed 2, St Louis, Mo, 2004, Elsevier Mosby.)
Figure 19-8, C, shows assessment of trunk and pelvis lateral flexion, where movement is initiated from the lower trunk and pelvis. The end position is one of trunk elongation on the weight-bearing side and shortening on the non–weight-bearing side, which involves concentric contraction of the right side.
Lateral flexion is needed for fall prevention when a client is reaching to the side (e.g., shutting a car door).36
Trunk Rotation
The primary muscles responsible for rotation are the obliques. When a person rotates the trunk to the left, the right external and the left internal obliques are recruited. Rotational control is a prerequisite for upper extremity dressing and reaching across the midline. The following three movement patterns are evaluated:
1. The client sits upright and the pelvis is in a neutral, stable position. The client reaches with his or her right arm, across the body, in the direction of the floor. This motion helps in assessment of concurrent flexion and rotation. The motion tests concentric control of the obliques and the back extensors (particularly the thoracic region). Both sides need to be tested.
2. The second movement pattern involves trunk extension with rotation. The upper trunk remains stable, and the lower trunk and pelvis move forward on one side (i.e., shifting forward). Again, both sides are tested.
3. The client is positioned supine for the third movement. The client initiates a “segmental roll by lifting the shoulders from the support surface and toward the opposite side of the body. This pattern is controlled by a concentric contraction of the abdominals (obliques).”36
Coordination
Coordination is the ability to produce accurate, controlled movement. Characteristics of coordinated movement include smoothness, rhythm, appropriate speed, refinement to the minimum number of muscle groups needed, and appropriate muscle tension, postural tone, and equilibrium. Coordination of muscle action is under the control of the cerebellum and is influenced by the extrapyramidal system.
For coordinated movement, all elements of the neuromuscular mechanism must be intact. Coordinated movement depends on contraction of the correct agonist muscles with simultaneous relaxation of the correct antagonist muscles, together with contraction of the joint fixator and synergist muscles. In addition, proprioception, body scheme, and the ability to judge space accurately and to direct body parts through space with correct timing to the desired target must be intact.
Incoordination
Many types of lesions can produce disturbances in coordination. Disturbances in coordination often stem from cerebellar and extrapyramidal disorders. Noncerebellar causes include diseases and injuries of muscles and peripheral nerves, lesions of the posterior columns of the spinal cord, and lesions of the frontal and post-central cerebral cortex. Paralysis of the limbs caused by a peripheral nervous system lesion prevents testing for coordination, even though CNS mechanisms are intact.
Cerebellar Disorders
Cerebellar dysfunction can cause incoordination that may affect any body region and cause a variety of clinical symptoms. For example, the client may have postural difficulties that include slouching or leaning positions (caused by bilateral lesions) or spinal curvature (caused by unilateral lesions) and wide-based standing. Eye movements, both voluntary and reflexive, may be affected, as well as the resting position of the eye. The following are common signs of cerebellar dysfunction that the therapist may encounter.98
Ataxia
Ataxia is manifested as delayed initiation of movement responses, errors in range and force of movement, and errors in the rate and regularity of movement. Poor coordination is noted between the agonist and antagonist muscle groups. This results in jerky, poorly controlled movements. When a client with ataxia reaches for an object, it is apparent that the shortest distance between the client and the object is not a straight line. The client with gait ataxia has a staggering, wide-based gait with reduced or no arm swing. Step length may be uneven, and the client may have a tendency to fall. The client with cerebellar dysfunction isolated to one cerebellar hemisphere will have a tendency to fall on the side of the lesion or dysfunction because of the ipsilateral influence of the cerebellum on the lower motor neurons. Ataxia will result in poor postural stability.28,70
Adiadochokinesis
Adiadochokinesis is an inability to perform rapid alternating movements such as pronation and supination or elbow flexion and extension. Preston tests this by counting how many cycles a client can perform in a 10-second time frame. A cycle consists of one full repetition of supination and pronation. It is best to test the unaffected (or lesser affected) side first. The affected side is then compared with the unaffected side.80
Dysmetria
Dysmetria is an inability to estimate the ROM necessary to reach the target of movement. Two types of dysmetria are known. Hypermetria involves the limb overshooting the target. Conversely, hypometria involves the limb undershooting the target.70
Dyssynergia
Literally, dyssynergia is a “decomposition of movement” in which voluntary movements are broken up into their component parts and appear jerky. Dyssynergia can also cause problems in articulation and phonation.25,70
Rebound Phenomenon of Holmes
The rebound phenomenon of Holmes is the lack of a check reflex, that is, the inability to stop a motion quickly to avoid striking something. For example, if the client’s arm is flexed against the resistance of the examiner and the resistance is released suddenly, the client’s hand will hit the client’s face or body.25
Nystagmus
Nystagmus is an involuntary movement of the eyeballs in an up-and-down, back-and-forth, or rotating direction. It interferes with head control and fine adjustments required for balance. Nystagmus can occur as a result of vestibular system, brainstem, or cerebellar lesions.25
Dysarthria
Dysarthria is explosive or slurred speech caused by incoordination of the speech mechanism. The client’s speech may also vary in pitch or may seem nasal and tremulous, or both.25
Extrapyramidal Disorders
Extrapyramidal disorders are characterized by hypokinesia or hyperkinesia. Parkinson’s disease is characterized by hypokinesia (bradykinesia), cogwheel and lead pipe rigidity, a decrease in or loss of postural mechanisms, and a resting, pill-rolling tremor.27
Parkinson’s plus is the name given to a group of movement disorders that have signs of Parkinson’s disease with concomitant neurologic deficits. Progressive supranuclear palsy (PSP) is one such disease.50 Clients affected with PSP have “loss of vertical ocular gaze, rigidity of the neck and trunk muscles, dementia, and parkinsonian signs,”49 usually in the absence of tremor. Life expectancy is shorter than in Parkinson’s disease. Death often occurs within 6 to 10 years.49
Chorea
Chorea is irregular, purposeless, involuntary, coarse, quick, jerky, and dysrhythmic movements of variable distribution. These movements may occur during sleep.25 Two diagnoses often presenting with chorea are tardive dyskinesia and Huntington’s disease. Tardive dyskinesia is a drug-induced disorder, often associated with neuroleptic drug use. Occupational therapists most often see clients who have tardive dyskinesia in psychiatric settings. Huntington’s disease is an inherited, autosomal dominant disease. Clients with Huntington’s disease have an ataxic gait with choreoathetoid movements. As the disease progresses, rigidity develops. Choreiform movements are faster than athetoid movements.50
Athetoid Movements
Athetoid movements are continuous, slow, wormlike, arrhythmic movements that primarily affect the distal portions of the extremities. These movements occur in the same patterns in the same individual and are not present during sleep.25 Adult athetosis can occur after cerebral anoxia and Wilson’s disease. Movement patterns include alternating “extension and flexion of the arm, supination and pronation of the forearm, and flexion and extension of the fingers.”49 Athetosis that occurs with chorea is termed choreoathetosis.50
Dystonia
Dystonia results in persistent posturing of the extremities (e.g., in hyperextension or hyperflexion of the wrist and fingers), often with concurrent torsion of the spine and associated twisting of the trunk.1 Dystonic movements are often continuous and are often seen in conjunction with spasticity. Figure 19-9 shows a client with a traumatic brain injury, with his right wrist and fingers exhibiting dystonia. Dystonia can be primary or secondary, the latter occurring with other CNS disorders (e.g., hypoxic brain injury, tumor). Segmental dystonia involves two or more adjacent body parts. Generalized and multifocal types of dystonia also exist. Focal dystonia involves only one limb, as seen in writer’s cramp, musician’s cramp, and spasmodic torticollis.49
Ballism
Ballism is a rare symptom that is produced by continuous, abrupt contractions of the axial and proximal musculature of the extremity. Ballism causes the limb to fly out suddenly. It occurs on one side of the body (hemiballism) and is caused by lesions of the opposite subthalamic nucleus.25,70
Tremor
The following are three common types of tremor:
1. Intention tremor, associated with cerebellar disease, occurs during voluntary movement. It is intensified at the termination of the movement and is often seen in multiple sclerosis. The client with intention tremor may have trouble performing tasks that require accuracy and precision of limb placement (e.g., drinking from a cup, inserting a key in a lock).
2. Resting tremor occurs at rest and subsides when voluntary movement is attempted. It occurs as a result of damage or disease of the basal ganglia and is seen in Parkinson’s disease.
3. Essential familial tremor is inherited as an autosomal dominant trait. It is most visible when the client is carrying out a fine precision task.49
Assessment of Coordination
Medical Assessment of Coordination
Incoordination consists of errors in rate, rhythm, range, direction, and force of movement.35 Therefore, observation is an important element of the clinical examination. The neurologic examination for incoordination may include the nose-finger-nose test, the finger-nose test, the heel-knee test, the knee pat (pronation-supination) test, hand pat and foot pat tests, finger wiggling, and drawing a spiral. Such tests can reveal dysmetria, dyssynergia, adiadochokinesis, tremors, and ataxia. Usually the neurologist or the physiatrist performs these examinations. Magnetic resonance imaging and computed tomography scans also may be ordered. Tremors are frequency rated with EMG, which helps the physician accurately diagnose tremor type.49
Occupational Therapy Assessment of Coordination
Selected activities and specific performance tests can reveal the effects of incoordination on function. The occupational therapist can observe for coordination difficulties during ADL assessment. The therapist can prepare simulated tasks that require coordinated muscle function, such as writing, opening containers, tossing and catching a bean bag or ball, or playing a board game.90 The therapist should observe for irregularity in the rate of movement and for sudden, corrective movements in an attempt to compensate for incoordination. Movement during the performance of various activities may appear irregular and jerky and may overreach the mark. The following general guidelines and questions can be used when evaluating incoordination:
1. Assess muscle tone and joint mobility first in a sitting position.
2. Observe for ataxia, proximal to distal, during functional upper extremity movement. Are movements away from or toward the body more difficult for the client? Where, within the ROM, is ataxia most prevalent?
3. Stabilize joints proximally to distally during the functional task, and note differences in client performance as compared with performance without stabilization. (Stabilization can be attained by splinting or stabilizing the affected body part against a wall.) Weighted cuffs may be applied to the extremity during task performance to determine whether weighting or resistance decreases the tremor (use caution). Note the amount of resistance provided. Observe whether the weights make the coordination worse. Sometimes the use of weights increases tremor.
4. Observe for tremor. Are the eyes and speech affected?
5. Does the client’s emotional status affect coordination?
6. How do the client’s ataxia and coordination problems affect participation in occupation?
7. Perform an occupational profile, as well as a performance patterns interview, to ask about the client’s roles, routines, goals, and environment to determine which functions are important for the client.
Numerous standardized tests of motor function and manual dexterity are available and can be administered to evaluate coordination. These tests include the Purdue Pegboard,84 the Minnesota Rate of Manipulation Test,71 the Pennsylvania Bimanual Work Sample,79 the Crawford Small Parts Dexterity Test,22 the Jebsen-Taylor Hand Function Test,51 and the 9-Hole Peg Test.64 Standardized functional assessments for CVA (e.g., the GWMFT) mentioned earlier in this chapter may be useful for measuring the efficacy of occupational therapy intervention for impaired coordination.72
Occupational Therapy Intervention
Intervention for Hypertonicity and Spasticity
Hypertonicity is only one part of the UMNS. It is very important to treat other performance deficits of the UMNS such as paresis, fatigue, and decreased dexterity. These deficits can impede function to a greater extent than hypertonia.14
Before treating hypertonus, the therapist and the physician need to closely evaluate the function of the tone. Hypertonicity can have beneficial effects, such as aiding in standing and transfers, maintaining muscle bulk, and preventing deep vein thrombosis, osteoporosis, and edema. Intervention is necessary when spasticity interferes with ADLs, gait, sleep, or wheelchair positioning, or when it causes severe pain and limits hygiene (e.g., the client is unable to wash hand or axilla) or leads to contractures or decubitus ulcers. Hypertonicity or spasticity may be treated with conservative therapeutic interventions, pharmacologic agents, or surgery.83
Conservative Treatment Approaches
Weight Bearing: For hypertonicity reduction and paresis remediation in the upper extremity, therapists have been using weight-bearing skills/activities for many years when treating clients with upper motor neuron lesions, but evidence of treatment efficacy has not been fully established.
Brouwer and Ambury concluded that corticospinal facilitation of motor units occurred during upper extremity weight bearing. They believed that afferent input from weight bearing increased motor cortical excitability.15 Chakerain and Larson studied the effects of upper extremity weight bearing on hand opening and prehension in children with spastic cerebral palsy. Computer calculations of clients’ hand surface area were performed. An increase in surface area was noted after weight bearing, along with an increase in the maturity of movement components needed for prehension.19 McIlroy and Maki demonstrated that if the affected arm is used when weight bearing, postural responses occur throughout the weight-bearing extremity, as well as during other perturbations of posture.68
Despite the fact that few well-controlled studies document how and why weight bearing works physiologically, it certainly is a requirement for improving functional performance. Clients need upper extremity postural support when reaching to the floor to pick up an object while seated, to prevent falling. When standing, upper extremity weight bearing is needed to reach into a high cabinet to facilitate balance.36
Traditional Sensorimotor Approaches
Proprioceptive neuromuscular facilitation (PNF; see Chapter 31) has been shown to be effective in gaining motor control for a variety of diagnoses.91 According to the Neuro-Developmental Treatment (NDT) Association,74 therapists who follow an NDT approach:
• “Utilize an in-depth analysis of the intricacies of movement and how the details relate to the whole to allow for functional movement in a wide variety of environments.
• Believe that control of movement is based on a complex interaction of many body systems, which are plastic and adaptable, as well as on the tasks presented and the environments in which the tasks are performed. Therefore, function can be altered by changing one or more of these elements.
• Utilize an understanding of the development of atypical movement, as well as the compensations, to help minimize the impact of CNS pathology and prevent the emergence of contractures and deformities which contribute to the functional problems.”74
Another occupational therapy objective is to have the client manage muscle tone to engage in and complete basic and instrumental activities of daily living. Positioning and movement in patterns opposite to hypertonic or synergistic patterns are important to expand the motor repertoire and develop movement that is as close to normal as possible. At times it is appropriate to facilitate synergistic movements in the client with chronic disease (or if the client does not recover beyond Modified Brunnstrom’s stage 3) (see Table 19-1). The synergy patterns can be facilitated to improve lateral pinch or elbow flexion function. The client should be taught how to modulate the abnormal tone or how to instruct others to do so. The client should also be taught how to incorporate the affected upper extremity as much as possible into all ADLs. ADLs, crafts, games, and work activities can be used to teach incorporation of the extremities for a total approach to treatment.95 Refer to Chapter 30 for a more detailed review of traditional sensorimotor treatment strategies.
Juan was recovering from an acute CVA. His Modified Brunnstrom Stages of Motor Recovery Score was 4 (see Table 19-1). He had good rehabilitation potential to restore the client factors needed for ADL tasks. The therapist will work with him on acquiring full finger extension and dexterity for keyboarding, as well as on supination activities for opening doors and holding change.
Even when motor control is adequate for participation in occupation, the sensory, cognitive, and perceptual abilities of the client may affect the achievement of functional goals. Perceptual dysfunction may alter the client’s abilities, requiring the therapist to focus on perceptual training as well.7
Casting: In some cases, unilateral hypertonicity is severe enough to necessitate serial inhibitive casting or splinting (see Chapter 29). Casting in inhibitive postures has been shown to be effective in tone reduction.44,105 The beneficial effect of casting on hypertonia and upper extremity contractures has been well documented in the literature.8,30,32
Casting in inhibitive postures is effective because it provides neutral warmth, maintained pressure, and constant joint positioning with static lengthening of muscle.47 Serial casting is most successful when a contracture has been present for less than 6 months. The cast may be bivalved (cut in half) and worn as a splint. This helps protect the skin and allows the therapist to work with the extremity out of the cast. However, many clinicians believe that a nonbivalved cast is more effective and actually causes less skin breakdown. A dropout cast, which can be used as part of the serial casting process, includes a cutout area, allowing movement of the joint in the desired direction. For example, for an elbow that has flexor hypertonicity, the dorsal upper arm portion of a long arm cast can be cut out to allow the triceps to be facilitated to extend the arm.
Serial casting should cease when the desired position is achieved and tone is manageable with the last cast or splint. If no evidence is found of increased passive ROM after two to three casts are removed, serial casting must cease; however, the last cast should be kept, bivalved, and used as a “retainer” splint to prevent additional contractures, similar to retainer use in orthodontics. Many innovations have occurred in commercially available spasticity reduction splints that are used to place the wrist and hand in inhibitive postures. The client and the family need to be educated on continuing to incorporate the extremity in occupation, and on bearing weight on the extremity as much as possible to retain the ROM gains achieved during casting.83
Physical Agent Modalities
Physical agent modalities such as cold, superficial heat, ultrasound, and neuromuscular electrical stimulation can be used as preparation for, or in conjunction with, purposeful activity and muscle re-education, provided the therapist has the appropriate training and can prove competency. Ultrasound can help inhibit or reduce hypertonicity temporarily and can increase tendon and muscle extensibility. It is helpful to provide concurrent stretch during the ultrasound procedure.83 Neuromuscular electrical stimulation has been shown to strengthen paretic muscles.17,45
Juan actually did gain strength and range of motion in his finger extensors with the help of neuromuscular electrical stimulation to the extensor digitorum communis muscle group—the extrinsic finger extensors. His extrinsic strength improved from 3−/5 to 4/5 within 1 month.
Distal-to-Proximal Approach
The Functional Tone Management (FTM) Arm Training Program was developed by Saebo Inc. (Charlotte, NC) to address the weaknesses of therapeutic interventions currently applied to the neurologically impaired upper extremity (UE) and hand. The occupational therapists who founded Saebo theorized that because grasp and release capabilities are pivotal to reintegrating the UE into daily activities, a paradigm shift for UE neurologic rehabilitation was needed. Although traditional therapeutic interventions such as Bobath-based programs are based on a proximal-to-distal recovery pattern, Saebo developed the FTM Arm Training Program on the basis of a distal activation model, which focused on the key point of early initiation of UE movements that incorporate grasp and release. To incorporate the hand into the FTM Arm Training Program, Saebo developed a dynamic orthosis for the hand, called the SaeboFlex (Figure 19-10).
The SaeboFlex orthosis assists an individual who exhibits hypertonia in the hand to place the hand in an open, functional position. This positioning is accomplished by means of a fixed wrist support and a finger and thumb spring system of variable strength. Once the hand is open, the client can begin to retrain the finger flexors for improved motor control of the hand. While wearing the SaeboFlex, the client relearns to produce a graded muscle contraction of the finger flexors to grasp an object. The finger and thumb spring system, coupled with the client’s own efforts to relax muscle activation, allows the hand to open enough for the object held in the hand to be released.
Once the client is comfortable using the SaeboFlex, the FTM Arm Training Program can begin. The FTM program combines high-repetition grasp and release with task-specific arm training drills to progress the client toward a functional goal. A significant body of research supports the FTM Arm Training Program16,33,99; however, this program does not require the wrist or finger extension typically needed for participation in a constraint-induced program. Clinically observed improvements with the FTM Arm Training Program include increased AROM at the shoulder elbow and wrist, improved UE Fugl-Meyer scores, and decreased Modified Ashworth scores.31 Clients as far as 20 years post insult have shown improvements. Independent research studies using the SaeboFlex and the FTM Arm Training Program are under way.
Pharmacologic Agents
Pharmacologic agents prescribed and administered by physicians include oral medications, short-term nerve blocks, and long-term blocks.
Clients with severe hypertonicity accompanied by severe pain may need evaluation to determine the cause of the pain. Drug therapy and other pain management techniques may be part of the treatment approach. The four commonly used oral medications for spasticity of UMN origin are diazepam, baclofen, dantrolene sodium, and tizanidine. Dantrolene sodium acts at the skeletal muscle. Dantrolene sodium is preferred in cerebral spasticity because it is less apt to cause sedation. However, it can cause weakness and liver damage. Side effects of diazepam include drowsiness, fatigue, and possible addiction. Baclofen is more effective with spinal cord injuries than with cerebral injuries. Its potential side effects include confusion, drowsiness, and hallucinations. Neither diazepam nor baclofen can be discontinued suddenly because to do so may cause seizures. Tizanidine HCl is labeled for spasticity reduction in multiple sclerosis and spinal cord injury. Its side effects may include hypotension, sedation, and visual hallucinations. No matter which drug is used, it is crucial for the occupational therapist to communicate to the medical staff any noted side effects that may interfere with the client’s overall function.83
Nerve blocks and motor point blocks consist of injections of a chemical agent to diminish or obliterate tone. Short- and long-term blocks may be used. Short-term blocks are injections of an anesthetic (e.g., bupivacaine) to temporarily reduce pain and muscle tone. Short-term blocks help the physician to differentiate between hypertonus and contracture.82 Short-term blocks last from 1 to 7 hours, depending on which anesthetic is used.
Long-term blocks, which usually consist of injections of phenol or botulinum toxin type A (Botox) or botulinum toxin type B (Myobloc), generally last several months. Botox lasts for 2 to 5 months with spastic hypertonia. Botulinum toxin type B has been shown to quell cervical dystonia for 12 to 16 weeks.2 Phenol blocks last from 2 to 8 months, depending on whether the motor points (2 to 3 months) or the motor branch (8 months) is injected. Phenol and the botulinum toxins type A and B have different mechanisms of action. Botulinum toxins type A and B exert their effects via chemical denervation, and phenol works via motor point or motor branch neurolysis. Both blocks can be used to diminish or obliterate hypertonicity in the agonist. These blocks help to prevent contractures and render the hypertonic muscle weak or flaccid.20,42,77 The effect and time interval of the long-term block provide therapists the opportunity to increase antagonistic strength and function. A combination of long-acting blocks and casting or splinting is often used to treat hypertonicity. Long-term blocks in the upper extremities are commonly used in the subscapularis, brachioradialis, and flexor digitorum superficialis.83
Surgical Methods
Surgery to control hypertonicity is an option. Dynamic EMG can help orthopedic surgeons plan surgery. Orthopedic surgical intervention can improve function or release contractures. Examples of upper extremity functional surgery include lengthening of the biceps tendon to reduce elbow flexion and to gain elbow extension, thumb-in-palm release, and transfer of the flexor carpi ulnaris tendon to the extensor carpi radialis longus or brevis tendon to decrease the deforming force of wrist flexion while simultaneously augmenting wrist extension.80 An example of a contracture release procedure is the flexor digitorum superficialis-to-profundus transfer to gain length in the extrinsic finger flexors.46
Therapists will encounter clients with severe spasticity who have undergone a neurosurgical procedure called intrathecal baclofen pump (ITB) implantation. This procedure enables baclofen to enter the body at the spinal level and avoids the centrally mediated side effects of oral baclofen. The ITB provides baclofen, a spasticity-reducing medication, directly into the intrathecal (subarachnoid) space via a catheter attached to a subcutaneous implantable pump in the abdomen. The client must undergo a lumbar puncture test dose of intrathecal baclofen to determine candidacy before pump implantation.69
ITB has been shown to be very effective in the reduction of severe spinal spasticity and spasticity associated with multiple sclerosis and is also effective for cerebral spasticity. For additional details on medical and surgical treatments and their relation to occupational therapy, the reader is referred to Preston and Hecht’s Spasticity Management: Rehabilitation Strategies.83
Treatment of Rigidity
Decerebrate and decorticate rigidity can wax and wane. When rigidity is waning, it is recommended that the client be transferred to a wheelchair or a reclining chair because rigidity decreases in sitting. Rigidity is worse during episodes of agitation.57 Parkinson’s rigidity responds temporarily to heat, massage, stretching, and ROM exercises. Rocking back and forth before standing can aid in the transition.62 See Chapter 35 for a discussion of Parkinson’s disease and additional treatment strategies for rigidity.
Treatment of Flaccidity
Flaccidity stemming from upper motor neuron dysfunction (e.g., recovering from spinal or cerebral shock resulting from acute CNS insult) is treated with facilitation techniques such as weight bearing, high-frequency vibration, tapping, quick stretch, bed positioning with weight on the flaccid side most of the time, and functional neuromuscular electrical stimulation. Splinting of the hand and wrist may be indicated for support. Therapists should closely supervise splinting because contractures can result from excessive splint wear. Passive ROM exercises also are indicated. The arm can be passively positioned as normally as possible during ADL tasks to provide sensory and proprioceptive feedback. When the client is eating, have him or her place his or her arm on the dining room table, resting on top of a piece of Dycem.29 Client and family education on proper positioning and joint protection is important to prevent overlengthening of soft tissues and trauma (e.g., having his or her arm fall off of the lap and bump the wheel of the wheelchair).83
Treatment of Incoordination
Treatment of incoordination is difficult. Activities graded on the basis of motor learning and control may be helpful for attaining proximal stability and then mobility. Therapy directed toward the modulation of reflexes and abnormal synergy patterns and the enhancement of postural control mechanisms, such as the righting and equilibrium reactions, can help to improve coordination. Weight bearing, joint approximation, placing and holding techniques, and fixed points of stability (having the client stabilize his elbow or wrist on the tabletop) can be helpful.
It is critical that the therapist encourage the client to use his or her vision to help direct upper extremity movements. The therapist should begin with small ranges of movement and gradually increase them as the client progresses. Initially, work is done in the plane and direction of movement that are easiest for the client, then work progresses toward more difficult areas. Some of the involuntary movements of cerebellar or extrapyramidal origin, particularly primary movement disorders, are difficult to manage or change. Therapists have greater influence over movement disorders that are associated with traumatic brain injury and stroke.
Methods and devices to compensate for incoordination may be necessary to make BADLs and IADLs safer, more possible, and more satisfying. Obtaining a thorough occupational profile is necessary to make appropriate activity and equipment choices and to determine adaptive strategies that the client can carry over to the home environment. The physician may employ pharmacologic agents or surgical intervention in an effort to dampen tremors or other involuntary movement patterns.70
Surgical Intervention for Movement Disorders
Neurosurgical intervention for movement disorders may include stereotactic thalatomy for ballismus, chorea (Huntington’s), Parkinson’s disease, essential tremor, and athetosis. Surgical treatment for dystonia may include rhizotomy, neurectomy, cryothalotomy, or ITB implantation.49 Deep brain stimulation has been effective in tremor reduction in essential tremor and Parkinson’s disease.70,93
Because of the current managed care system, occupational therapists are receiving more referrals than ever before from primary care physicians. Occupational therapists who have a basic knowledge of medical and surgical options in ameliorating motor control problems can play a triage role in suggesting referral to physician specialists.
Summary
As one can determine from reading the aforementioned case study, the presence of abnormal elements of motor control affects the quality of movement and the ability to perform in areas of occupation. The occupational therapist assesses muscle tone, upper extremity recovery, and coordination, using standardized tests and observation of movement during occupational performance. Results of the motor control assessment can help the client and the therapist collaborate on appropriate intervention. Ameliorating motor control can be a rewarding experience for the client and the therapist.
2. When would a physician recommend a long-term nerve block or a motor point block?
3. Describe the characteristics of rigidity.
4. Compare and contrast spasticity and hypertonia.
5. Why should the assessment of muscle tone be performed in conjunction with evaluation of the client’s overall motor function?
6. Demonstrate how to perform an upper extremity muscle tone evaluation.
7. Describe equilibrium reactions and the functional implications of their presence in motor control.
8. Describe functional difficulties encountered when the asymmetric tonic neck reflex is present.
9. Compare and contrast chorea and athetosis.
11. Compare and contrast the following tremors: essential, resting, and intention.
References
1. Adams RD, Victor M, eds. Principles of neurology, ed 5, New York, NY: McGraw-Hill, 1993.
2. Albany, K. Physical and occupational therapy considerations in adult patients receiving botulinum toxin injections for spasticity. In: Mayer NH, Simpson DM, eds. Spasticity: etiology, evaluation, management and the role of botulinum toxin. New York, NY: We Move, 2002.
3. Allison, SC, Abraham, LD, Petersen, CL. Reliability of the Modified Ashworth Scale in the assessment of plantar-flexor muscle spasticity in patients with traumatic brain injury. Int J Rehabil Res. 1996;19:67–78.
4. Ashworth, B. Preliminary trial of carisoprodol in multiple sclerosis. Practitioner. 1964;192:540–542.
5. Bell-Krotoski, JA, Fess, EE, Figarola, JH, Hiltz, D. Threshold detection and Semmes-Weinstein monofilaments. J Hand Ther. 1995;8:155–162.
6. Berg, KO, Wood-Dauphinee, SL, Williams, JI, et al. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–311.
7. Bernspång, B, Fisher, AG. Differences between persons with right or left CVA on the Assessment of Motor and Process Skills. Arch Phys Med Rehabil. 1995;76:1114–1151.
8. Blackburn, M, van Vliet, P, Mockett, SP. Reliability of measurements obtained with the modified Ashworth scale in the lower extremity of people with stroke. Phys Ther. 2002;82:25–34.
9. Blanton, S, Wolf, S. An application of upper-extremity constraint-induced movement therapy in a patient with subacute stroke. Phys Ther. 1999;79:847–853.
10. Bohannon, RW, Smith, MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67:206–207.
11. Bontke, CF, Boake, C. Principles of brain injury rehabilitation. In: Braddom R, ed. Physical medicine and rehabilitation. Philadelphia, Pa: WB Saunders, 1996.
12. Botox package insert, Irvine, Calif, Allergan Pharmaceuticals, Inc.
13. Boyd, R, Graham, H. Objective measurement of clinical findings in the use of botulinum toxin for the management of children with cerebral palsy. Eur J Neurol. 1999;6:S23–S36.
14. Brashear, A, Zafonte, R, Corcoran, M, et al. Inter- and intrarater reliability of the Ashworth Scale and the Disability Assessment Scale in patients with upper limb poststroke spasticity. Arch Phys Med Rehabil. 2002;83:1349–1354.
15. Brouwer, BJ, Ambury, P. Upper extremity weight-bearing effect on corticospinal excitability following stroke. Arch Phys Med Rehabil. 1994;75:861–866.
16. Bütefisch, C, Hummelsheim, H, Denzler, P, Mauritz, KH. Repetitive training of isolated movements improves the outcome of motor rehabilitation of centrally paretic hand. J Neurol Sci. 1995;130:59–68.
17. Carmick, J. Clinical use of neuromuscular electrical stimulation for children with cerebral palsy, part 2, upper extremity. Phys Ther. 1993;73:514–522.
18. Carr, JH, Shepherd, RB. Neurological rehabilitation: optimizing motor performance. Oxford, United Kingdom: Butterworth-Heinemann; 1998.
19. Chakerian, DL, Larson, MA. Effects of upper-extremity weight bearing on hand-opening and prehension patterns in children with cerebral palsy. Dev Med Child Neurol. 1993;35:216–229.
20. Chironna, RL, Hecht, JS. Subscapularis motor point block for the painful hemiplegic shoulder. Arch Phys Med Rehabil. 1990;71:428–429.
21. Collin, C, Wade, D. Assessing motor impairment after a stroke: a pilot reliability study. J Neurol Neurosurg Psychiatry. 1990;53:576–579.
22. Crawford, J, Crawford, D. Crawford small parts dexterity test. New York, NY: Psychological Corporation; 1956.
23. Cruickshank, DA, O’Neill, DL. Upper-extremity inhibitive casting in a boy with spastic quadriplegia. Am J Occup Ther. 1990;44:552–555.
24. DeBoskey, DS, Hecht, JS, Club, CJ. Educating families of the head injured: a guide to medical, cognitive, and social issues. Gaithersburg, Md: Aspen Publishers; 1991.
25. deGroot, J. Correlative neuroanatomy, ed 21. Norwalk, Conn: Appleton & Lange; 1991.
26. Desrosiers, J, Hébert, R, Bravo, G, Dutil, E. Upper extremity performance test for the elderly (TEMPA): normative data and correlates with sensorimotor parameters. Arch Phys Med Rehabil. 1995;76:1125–1129.
27. Dombovy, ML. Rehabilitation concerns in degenerative movement disorders of the central nervous system. In: Braddom RL, ed. Physical medicine and rehabilitation. Philadelphia, Pa: WB Saunders, 1996.
28. Donato, S, Pulaski, KH. Overview of balance impairments: functional implications. In: Gillen G, Burkhardt A, eds. Stroke rehabilitation: a function-based approach. St Louis, Mo: Mosby, 1998.
29. Dycem package insert, Bolingbrook, Ill, Sammons Preston Roylan.
30. Farber, S. Neurorehabilitation: a multisensory approach. Philadelphia, Pa: WB Saunders; 1982.
31. Farrell, JF, Hoffman, HB, Snyder, JL, et al. Orthotic aided training of the paretic limb in chronic stroke: results of a phase 1 trial. Neurorehabilitation. 2007;22:99–103.
32. Feldman, PA. Upper extremity casting and splinting. In: Glenn MB, White J, eds. The practical management of spasticity in children and adults. Philadelphia, Pa: Lea & Febiger, 1990.
33. Feys, H, De Weerdt, W, Verbeke, G, et al. Early and repetitive stimulation of the arm can substantially improve the long-term outcome after stroke: a 5-year follow-up study of a randomized trial. Stroke. 2004;35:924–929.
34. Fosang, AL, Galea, MP, McCoy, AT, et al. Measures of muscle and joint performance in lower limbs of children with cerebral palsy. Dev Med Child Neurol. 2003;45:664–670.
35. Ghez, C, Thach, WT. The cerebellum. In Kandel ER, Schwartz JH, Jessel TM, eds.: Principles of neural science, ed 4, New York: McGraw-Hill, 2000.
36. Gillen, G. Trunk control: supporting functional independence. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Elsevier Mosby, 2011.
37. Goldberg, C, VanSant, A. Normal motor development. In Tecklin JS, ed.: Pediatric physical therapy, ed 3, Philadelphia, Pa: Lippincott Williams & Wilkins, 1999.
38. Gorman IG: personal communication, June 2004.
39. Gracies, JM, Marosszeky, JE, Renton, R, et al. Short-term effects of dynamic lycra splints on upper limb in hemiplegic patients. Arch Phys Med Rehabil. 2000;81:1547–1555.
40. Gregson, JM, Leathley, MJ, Moore, AP, et al. Reliability of measurements of muscle tone and muscle powering in stroke patients. Age Ageing. 2000;29:223–228.
41. Gregson, JM, Leathley, M, Moore, AM, et al. Reliability of the Tone Assessment Scale and the Modified Ashworth Scale as clinical tools for assessing poststroke spasticity. Arch Phys Med Rehabil. 1999;80:1013–1016.
42. Hecht, JS. Subscapular nerve block in the painful hemiplegic shoulder. Arch Phys Med Rehabil. 1992;73:1036–1039.
43. Held, JP, Pierrot-Deseilligny, E. Reeducation motrice des affections neurologiques. Paris, France: Bailliere; 1969.
44. Hill, J. The effects of casting on upper extremity motor disorders after brain injury. Am J Occup Ther. 1994;48:219–224.
45. Hines, AE, Crago, PE, Billian, C. Functional electrical stimulation for the reduction of spasticity in the hemiplegic hand. Biomed Sci Instrum. 1993;29:259–266.
46. Hisey, MS, Keenan, MAE. Orthopedic management of upper extremity dysfunction following stroke or brain injury. In Green DP, Hotchkiss RN, Pederson WC, eds.: Operative hand surgery, ed 4, New York, NY: Churchill Livingstone, 1999.
47. Hylton, N. Dynamic casting and orthotics. In: Glenn MB, Whyte J, eds. The practical management of spasticity in children and adults. Philadelphia, Pa: Lea & Febiger, 1990.
48. Iyer, MB, Mitz, AR, Winstein, C. Motor 1: lower centers. In Cohen H, ed.: Neuroscience for rehabilitation, ed 2, Philadelphia, Pa: Lippincott Williams & Wilkins, 1999.
49. Jain, SS, Francisco, GE. Parkinson’s disease and other movement disorders. In DeLisa JA, Gans BM, eds.: Rehabilitation medicine: principles and practice, ed 3, Philadelphia, Pa: Lippincott-Raven, 1998.
50. Jain, SS, Kirshblum, SC. Movement disorders, including tremors. In Delisa JA, ed.: Rehabilitation medicine: principles and practice, ed 2, Philadelphia, Pa: JB Lippincott, 1993.
51. Jebsen, RH, Taylor, N, Trieschmann, RB, et al. An objective and standardized test of hand function. Arch Phys Med Rehabil. 1969;50:311–319.
52. Jewell, MJ. Overview of the structure and function of the central nervous system. In Umphred DA, ed.: Neurological rehabilitation, ed 2, St Louis, Mo: Mosby, 1990.
53. Jordan, CL, Allely, RR. Burns and burn rehabilitation. In Pedretti LW, ed.: Occupational therapy: practice skills for physical dysfunction, ed 4, St Louis, Mo: Mosby, 1996.
54. Katz, RT. Management of spasticity. In: Braddom RL, ed. Physical medicine and rehabilitation. Philadelphia, Pa: WB Saunders, 1996.
55. Katz, RT, Rovai, GP, Brait, C, Rymer, WZ. Objective quantification of spastic hypertonia: correlation with clinical findings. Arch Phys Med Rehabil. 1992;73:339–347.
56. Kisner, C, Colby, LA. Therapeutic exercise foundations and techniques, ed 3. Philadelphia, Pa: FA Davis; 1996.
57. Kohlmeyer, K. Evaluation of performance skills and client factors. In Crepaeau EB, Cohn ES, Boyt-Shell BA, eds.: Willard and Spackman’s occupational therapy, ed 10, Philadelphia, Pa: Lippincott Williams & Wilkins, 2003.
58. Kopp, B, Kunkel, A, Flor, H, et al. The Arm Motor Ability Test: reliability, validity, and sensitivity to change of an instrument for assessing disabilities in activities of daily living. Arch Phys Med Rehabil. 1997;78:615–620.
59. Lance, JW. Symposium synopsis. In: Feldman RG, Young RR, Koella WP, eds. Spasticity: disordered motor control. Chicago, Ill: Year Book, 1980.
60. Law, M, Baptiste, S, Carswell, A, et al. Canadian occupational performance measure, ed 3. Ottawa, Ontario, Canada: Canadian Association of Occupational Therapists; 1998.
61. Leonard, CT, Stephens, JU, Stroppel, SL. Assessing the spastic condition of individuals with the upper motoneuron involvement: validity of the myotonometer. Arch Phys Med Rehabil. 2001;82:1416–1420.
62. Little, JW, Massagli, TL. Spasticity and associated abnormalities of muscle tone. In Delisa JB, ed.: Rehabilitation medicine: principles and practice, ed 2, Philadelphia, Pa: JB Lippincott, 1993.
63. Little, JW, Massagli, TL. Spasticity and associated abnormalities of muscle tone. In Delisa JA, Gans BM, eds.: Rehabilitation medicine: principles and practice, ed 3, Philadelphia, Pa: Lippincott-Raven, 1998.
64. Mathiowetz, V, Weber, K, Kashman, N, Volland, G. Adult norms for the nine hole peg test of finger dexterity. Occup Ther J Res. 1985;5:24–38.
65. Mayer NH, Simpson DM, eds. Spasticity: etiology, evaluation, management and the role of botulinum toxin. New York, NY: We Move, 2002.
66. McCormack, G, Pedretti, LW. Motor unit dysfunction. In Pedretti LW, ed.: Occupational therapy practice skills for physical dysfunction, ed 4, St Louis, Mo: Mosby, 1996.
67. McCrea, PH, Eng, JJ, Hodgson, AJ. Linear spring-damper model of the hypertonic elbow: reliability and validity. J Neurosci Methods. 2003;128:121–128.
68. McIlroy, WE, Maki, BE. Early activation of arm muscles follows external perturbation of upright stance. Neurosci Lett. 1995;184:177–180.
69. Medtronic ITB Therapy, Minneapolis, Minn, Medtronic Neurological.
70. Melnick, ME, Oremland, B. Movement dysfunction associated with cerebellar problems. In Umphred DA, ed.: Neurological rehabilitation, ed 4, St Louis, Mo: Mosby, 2001.
71. Minnesota Rate of Manipulation Test, Circle Pines, Minn, American Guidance Service.
72. Morris DM, et al: Graded Wolf Motor Function Test. Dr. Edward Taub, Department of Psychology, University of Alabama at Birmingham, Birmingham, Ala, revision date May 6, 2002.
73. Myobloc, San Diego, Calif, Elan Pharmaceuticals.
74. Howle, JM. Neurodevelopmental treatment approach: theoretical foundations and principles of clinical practice. Laguna Beach, Calif.: Neurodevelopmental Treatment Association; 2002.
75. Nudo, RJ, Wise, BM, SiFuentes, F, Milliken, GW. Neural substrates for the effects of rehabilitative training on motor recovery after ischemic infarct. Science. 1996;272:1791–1794.
76. Pandyan, AD, Johnson, GR, Price, CI, et al. A review of the properties and limitations of the Ashworth and Modified Ashworth scales as a measure of spasticity. Clin Rehabil. 1999;13:373–383.
77. Pandyan, AD, Price, CI, Barnes, MP, Johnson, GR. A biomechanical investigation into the validity of the modified Ashworth Scale as a measure of elbow spasticity. Clin Rehabil. 2003;17:290–293.
78. Pandyan, AD, Price, CI, Rodgers, H, et al. Biomechanical examination of a commonly used measure of spasticity. Clin Biomech. 2001;16:859–865.
79. Pennsylvania Bi-Manual Work Sample, Educational Test Bureau, Circle Pines, Minn, American Guidance Service.
80. Preston, LA, Effects of botulinum toxin type B on shoulder pain. Master’s thesis, Nashville Tenn, Belmont University, 2003.
81. Preston, LA. Interdisciplinary upper-extremity spasticity management. Physical Disabilities Special Interest Section Quarterly. 2004;27:1.
82. Preston, LA. OT’s role in enhancing nerve blocks for spasticity. OT Practice. 1998;3:29–35.
83. Preston, LA, Hecht, JS. Spasticity management: rehabilitation strategies. Bethesda, Md: American Occupational Therapy Association; 1999.
84. Purdue Pegboard, Chicago, Ill, Science Research Associates, Inc,
85. Reuben, DB, Siu, AL. An objective measure of physical function of elderly outpatients. J Am Geriatr Soc. 1990;38:1105–1112.
86. Roth, EJ, Harvey, RL. Rehabilitation of stroke syndromes. In: Braddom RL, ed. Physical medicine and rehabilitation. Philadelphia, Pa: WB Saunders, 1996.
87. Ryerson, SD. Hemiplegia. In Umphred DA, ed.: Neurological rehabilitation, ed 5, St Louis, Mo: Mosby, 2007.
88. Sehgal, N, McGuire, JR. Beyond Ashworth: electrophysiologic quantification of spasticity. Phys Med Rehabil Clin N Am. 1998;9:949–979.
89. Sköld, C, Harms-Ringdahl, K, Hultling, C, et al. Simultaneous Ashworth measurements and electromyographic recordings in tetraplegic patients. Arch Phys Med Rehabil. 1998;79:959–965.
90. Smith, HD. Occupational therapy assessment and treatment. In Hopkins HL, Smith HD, eds.: Willard & Spackman’s occupational therapy, ed 8, Philadelphia, Pa: JB Lippincott, 1997.
91. St. John, K, Stephenson, J. PNF I: the functional approach to proprioceptive neuromuscular facilitation. Steamboat Springs, Colo: The Institute of Physical Art, Inc; 2002.
92. Szklut, SE, Breath, DM. Learning disabilities. In Umphred DA, ed.: Neurological rehabilitation, ed 4, St Louis, Mo: Mosby, 2001.
93. Tasker, RR. Deep brain stimulation is preferable to thalamotomy for tremor suppression. Surg Neurol. 1998;49:145–153.
94. Tinetti, ME. Performance oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–126.
95. Tomas, ES, et al. Nonsurgical management of upper extremity deformities after traumatic brain injury. Phys Med Rehabil. 7, October 1993.
96. Umphred, DA. Classification of treatment techniques based on primary input systems. In Umphred DA, ed.: Neurological rehabilitation, ed 3, St Louis, Mo: Mosby, 1995.
97. Umphred, DA. Neurological rehabilitation, ed 3. St Louis, Mo: Mosby; 1995.
98. Urbscheit, NL. Cerebellar dysfunction. In: Umphred DA, ed. Neurological rehabilitation. St Louis, Mo: Mosby, 1990.
99. Van der Lee, JH, Snels, IAK, Beckerman, H, et al. Exercise therapy for arm function in stroke patients: a systemic review of randomized controlled trials. Clin Rehabil. 2001;15:20–31.
100. Van der Meche, F, Van der Gijn, J. Hypotonia: an erroneous clinical concept? Brain. 1986;109(pt 6):1169–1178.
101. Whitney, SL, Poole, JL, Cass, SP. A review of balance instruments for older adults. Am J Occup Ther. 1998;52:666–671.
102. Whyte, J, Rosenthal, M. Rehabilitation of the patient with traumatic brain injury. In DeLisa JA, ed.: Rehabilitation medicine: principles and practice, ed 2, Philadelphia, Pa: JB Lippincott, 1993.
103. Wilson, DJ, Baker, LL, Craddock, JA. Functional test for the hemiplegic/paretic upper extremity. Downey, Calif: Los Amigos Research and Education Institute; 1984.
104. Winkler, PA. Traumatic brain injury. In Umphred DA, ed.: Neurological rehabilitation, ed 4, St Louis, Mo: Mosby, 2001.
105. Young, RR. Spasticity: a review. Neurology. 1994;44(11 suppl 9):S12–S20.
*The author would like to thank Crystal Edwards, OTR/L, and Jessica Dye, OTR/L.



 full,
full,  full, then
full, then  full. Occupational therapists trained in neuromuscular electrical stimulation can expedite recovery of range of motion and strength by placing electrodes on the wrist extensors and extensor digitorum communis while the client actively performs composite wrist and finger extension. Another suggested electrode placement would be on the biceps and supinator muscle. For the latter placement, the negative electrode would be placed on the supinator and the positive on the biceps. (An asymmetric waveform would be utilized.) Again, active recruitment of the supination motion would be encouraged.
full. Occupational therapists trained in neuromuscular electrical stimulation can expedite recovery of range of motion and strength by placing electrodes on the wrist extensors and extensor digitorum communis while the client actively performs composite wrist and finger extension. Another suggested electrode placement would be on the biceps and supinator muscle. For the latter placement, the negative electrode would be placed on the supinator and the positive on the biceps. (An asymmetric waveform would be utilized.) Again, active recruitment of the supination motion would be encouraged.