Amputations and Prosthetics
Section 1: General Considerations of Upper and Lower Limb Amputations
Section 2: Upper Limb Amputations
After studying this chapter, the student or practitioner will be able to do the following:
1 List the common reasons for amputation.
2 Discuss the role of the occupational therapist in rehabilitation after limb amputation.
3 List the goals of amputation surgery.
4 Name two types of surgical procedures.
5 Name four factors that can interfere with prosthetic training.
6 Define neuroma, phantom limb, and phantom pain.
7 Describe the typical psychological consequences of amputation surgery.
8 Describe how the occupational therapist facilitates adjustment to amputation.
9 Describe the role of the occupational therapist in the rehabilitation of the individual with an upper limb amputation
10 Discuss the impact of the residual limb status on the success of fitting and operating an upper limb prosthesis.
11 Name the five components common to all body-powered prostheses.
12 List the motions used to operate the body-powered prosthesis.
13 Describe at least two techniques for donning the body-powered prosthesis.
14 Describe the importance of prepositioning the terminal device.
15 List the two phases of training in the use of an upper limb prosthesis.
16 Explain why it is optimal to introduce postprosthetic training on three levels.
17 Describe the basic operation of an electric prosthesis.
18 Discuss the primary function of any prosthesis in different daily tasks.
19 List the types and causes of lower extremity (LE) amputation (also known as lower limb amputation).
20 Describe the types of equipment that may be used by a person who has had a lower limb amputation.
21 Describe how lower limb amputation may affect a person’s occupational performance.
22 Identify the effects that lower limb amputation may have on client factors, performance skills, and performance patterns.
23 Discuss the potential psychosocial repercussions of lower limb amputation.
24 Describe the role of the occupational therapist in working with a person who has had a lower limb amputation.
25 Explain how context and activity demands can be altered to improve a client’s ability to participate in a given occupation.
26 Discuss additional concerns that may be present for an older person who has had a lower limb amputation.
Section 1: General Considerations of Upper and Lower Limb Amputations
Limb loss can result from disease, injury, or congenital causes. Individuals born with congenital limb deficiencies or whose amputations occur early in life usually grow and develop sensorimotor skills and self-image without the limb. The person who undergoes an amputation in adolescence or adulthood is confronted with the task of adjusting to the loss of a well-integrated part of the body scheme and self-image. These two populations present different problems for the rehabilitation worker.6,64,65
Among orthotists and prosthetists, terminology related to amputation has changed in the past few years to allow consistent communication with rehabilitation workers throughout the world. The International Society of Prosthetics and Orthotics (ISPO), the American Association of Orthotics and Prosthetics (AAOP), and national and international prosthetics and orthotics related bodies have agreed to follow the recommendations of the International Standards Organization regarding Prosthetics and Orthotics terminology. The term used for arms and legs and portions thereof is “limb.”76
The primary responsibility of the occupational therapist in the rehabilitation program consists of formulation and execution of the preprosthetic program and prosthetic training. During the preprosthetic phase, the treatment plan involves preparing the limb for a prosthesis; during the prosthetic phase, treatment involves increasing tolerance and function with the prosthesis. The rehabilitation program involves an individualized intervention plan that helps the client with physical and psychological adjustments. This program is designed so that the client may learn to accept the new body image and to function as independently as possible.6,64,65
Causes and Incidence of Amputation
Most amputations may result from trauma; peripheral vascular disease (PVD); peripheral vasospastic disease; chronic infection; chemical, thermal, or electrical injury; or malignant tumor. Elective upper limb amputations may occur as a result of a severe or complete brachial plexus injury9 or other medical conditions that limit the neuromuscular function of the limb.
Calculation of the number of individuals with limb amputations worldwide is difficult to complete because many countries do not keep records of these data. The U.S. National Limb Loss Information Center estimated 1.7 million Americans with upper limb loss in 2007, based on an unpublished study out of John Hopkins University. This number is projected to reach 3.6 million by 2050. Lower limb loss (80%) is more prevalent than upper limb loss (10%) or multiple limb loss (10%). Upper limb loss due to trauma is increased during times of active warfare.47a The incidence of amputation remains fairly constant between the ages of 1 and 15. From 21 to 64 years of age, however, a gradual increase in incidence occurs because of work-related injuries and highway accidents. Approximately 75% of upper limb amputations in adults are caused by trauma,1,34,43,43a as was the case for Roberto.
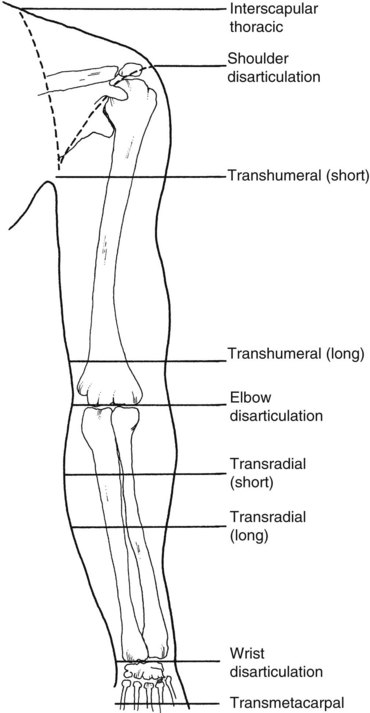
Previously, the level of amputation of the upper limb was referred to by its relationship to the elbow joint. For example, the terms above-elbow (AE) amputation and below-elbow (BE) amputation were universally used to clarify the level. This terminology has changed to reference the anatomy of the body when describing the level of limb loss. Terms now used include trans-radial, trans-humeral, and partial hand. See Figure 43-1.
The major cause of lower limb amputation is PVD, often associated with smoking and diabetes.36,39,56 Between 1988 and 1996, 82% of all lower limb amputations occurred as a result of vascular problems.15 Despite major improvements in noninvasive diagnosis, revascularization, and wound-healing techniques, 2% to 5% of individuals without diabetes but with PVD and 6% to 25% of those with both PVD and diabetes undergo amputation.28,29,41,45,68 Perioperative mortality rates of persons with lower limb amputation have been variously reported as between 7% and 13% and are usually associated with other medical problems, such as cardiac disease and stroke.22,28,29
The second leading cause of lower limb amputation, accounting for approximately 17% of amputations, is trauma,15 usually the result of motor vehicle accidents or gunshots. Individuals with traumatic amputation are usually young adults and more frequently are men.20,27 Improved imaging techniques, more effective chemotherapy, and better limb salvage procedures have reduced the incidence of amputation from osteogenic sarcoma. Tumor resection followed by limb reconstruction frequently provides an extremity that is as functional as a prosthesis and does not appear to affect the 5-year survival rate.30,38,61,67,75
Surgical Management
The surgeon is an important team member. Before performing surgery, the surgeon should consult with the health care team to maximize the functional outcome. The surgeon attempts to preserve as much length as possible and to provide a residual limb that has good soft tissue coverage and vascularization. Preservation of limb length directly affects the type of prosthesis that the limb can support; thus the surgeon and the prosthetist ideally communicate before surgical amputation or closure is performed. Conservation of residual limb length and uncomplicated wound healing are important. During and after surgery, the primary goal is to form a residual limb that maintains maximal function of the remaining tissue and allows maximal use of the prosthesis.6,34,64
Blood vessels and nerves are severed and are allowed to retract so that residual limb pain is minimized during prosthetic use. Bone beveling is a surgical procedure that smooths the rough edges and prevents the development of spurs (small projections of bone beyond the natural surface) on the remaining bone. Muscles are sutured to the bones distally by a surgical process called myodesis. The muscles involved in the function of the amputated limb are correspondingly affected by the loss.51
Surgical techniques vary with the level and cause of amputation.63,64 A closed or open surgical procedure may be performed. The open method allows drainage as the surgical site heals and minimizes the possibility of infection. The closed method reduces the period of hospitalization but also reduces free drainage and increases the risk of infection.64 The specific type of amputation performed is left to the discretion of the surgeon and is often determined by the status of the limb at the time of amputation. The surgery may be ablative (removal of devitalized tissues) only or reconstructive. In either case, the surgeon must remove the part of the limb that has to be eliminated and allow for primary or secondary wound healing. When the surgeon reconstructs a residual limb (sometimes referred to as a stump), this is done to achieve optimal prosthetic fitting and function. The residual limb that results should be strong and resilient.64
Client Social, Cultural, Personal, and Spiritual Contexts
Profound psychological shock and disbelief are likely to accompany amputation, particularly for those who experience a sudden trauma that causes or necessitates amputation.17,32,34 Seeing the residual limb for the first time can cause shock, panic, despair, self-pity, suicidal impulses, and even rage.49 Feelings of hopelessness, despondency, bitterness, and anger may ensue. Some individuals may mourn not only the lost limb but also the possible loss of a job or the ability to participate in favorite sports or activities.
The person may feel lonely, isolated, and an object of pity. Concerns about the future, body image and function, the responses of family and friends, and employment all affect the person’s emotional status.49 Reactions to amputation may be less severe in individuals who have had a chance to adjust before the surgery is performed.17,32,34 Older persons may demonstrate postoperative confusion, whereas younger persons may have a sense of mutilation, emasculation, or castration.17,32
The person’s personality; age; cultural background; and psychological, social, economic, and vocational resources influence the reaction to amputation. Ultimately, the individual must come to terms with the consequences of limb loss and the perception of diminished attractiveness. The person confronts discomfort, inconvenience, economic expense, loss of function, increased energy expenditure, and possible curtailment of favorite occupations. He or she may need to change employment because of social discrimination and to cope with resultant medical problems.17 Roberto expressed a strong desire to return to work. He recognized that his work capabilities had always been in the manual labor category. Roberto accepted consultation with a vocational counselor to assist him in the goal of returning to gainful employment as quickly as possible. He accepted the fact that some jobs identified by the counselor may be unfamiliar to him.
Cultural factors are important in the reaction to amputation. In some social, cultural, or religious groups, amputation may be considered a means of punishment or atonement. Such beliefs and the general aversion of society to amputation can cause the affected person to adopt the same viewpoint or to perpetuate his or her own preexisting viewpoint. Similar attitudes can result in self-hatred and self-deprecation, which may affect the person’s reaction and adjustment to the disability.17
Depression and a sense of futility are considered a normal part of the adjustment process.17 If depression is severe and prolonged, psychological or psychiatric referral is indicated. Medication may be necessary to reduce depression.17 The preexisting personality of the person determines the severity and duration of the reaction, and ultimately the adjustment to the amputation and to prosthetic use.16,17 Roberto acknowledged his depression, reported that it was decreasing (6 months after the amputation), and said that he was actively involved in planning his life and attaining his goals for the future.
Psychosocial Contexts Influencing Adjustment to Amputation
Psychosocial adjustment depends on various factors: the individual’s character and essence, the quality of the social support systems available, the sociocultural reactions to amputation, and the team’s management of rehabilitation.17 Social, personal, and spiritual contexts may be significantly altered for those who have experienced amputation. Through the interview with Roberto, the therapist identifies successful adaptation and coping strategies already in place and does not note a significant change in his spiritual self.
The process of adjustment to amputation is analogous to the grieving process. The client experiences identifiable stages of denial, anger, depression, coping, and acceptance.17 Some clients move through these stages and ultimately adapt to the loss. The cause of the amputation may contribute significantly to the person’s response. For example, if the amputation was caused by negligence on the part of the affected person or others, self-blame, guilt, or anger at others may be noted.
During any phase, clients may react with hostility toward themselves and the medical team. Often, overt solicitousness and friendliness may mask such hostility. Caregivers should make allowances for such behavior rather than respond in kind. Positive reinforcement through involvement in the rehabilitation process and contact with people who experienced similar amputations may help the client solve the problem of returning to former life roles.17
The client may be afraid to return to family, social, vocational, and sexual roles. Frequent discussions of fears and solutions to real or imagined problems (if possible, with a similar, successfully rehabilitated client) are important for facilitating adjustment.17
After a mourning period, the client may minimize the significance of the amputation and actually joke about it. When this phase of adjustment has subsided, the client begins seriously to consider the future. At this point, the therapist may discuss social, vocational, and educational plans with the client.17
Loss of a portion of the body necessitates revision and acceptance of the body image. Problems with acceptance of the change in body image may cause difficulties in prosthetic training.64,65 Fostering acceptance of the prosthesis is a crucial way to promote the client’s adjustment. Establishing a training program that presents the prosthesis in a manner that meets the client’s needs and goals has a beneficial effect in integrating the prosthesis into the body scheme. The prosthesis must become part of the self before it can be used most effectively. The prosthesis contributes to what society regards as a normal appearance, which may in turn help the client continue to identify with able-bodied individuals. Thus, the client may reconnect more quickly with his or her former image, leaving the door open for reconfiguration of that image to include the newly changed body.17,64,65
Long-term adjustment depends on the person’s basic personality structure; sense of accomplishment; and place in the family, community, and world. Generally, individuals who have had an amputation may dream of themselves as not being amputated. This image may be so vivid that persons with lower extremity amputation fall as they get up at night and attempt to walk to the bathroom without a prosthesis.49
Rehabilitation team members can help the client understand the importance of the prosthetic training program. Use of new prosthetic technology that addresses different lifestyles promotes participation in meaningful occupation and enhances normal appearance. The person’s preferred body image should be stressed.
Postsurgical Physical Client Factors and Performance Skills
Several factors and potential problems can affect the outcome of rehabilitation. Length of the residual limb, skin integrity, edema, sensation, pain, time for healing, infection, and allergic reaction to the prosthesis are among the physical factors that affect rehabilitation potential.37
Skin
Skin complications account for most postsurgical problems. These complications may occur in the preprosthetic or the prosthetic phase. Delayed healing and extensive skin grafting are complications in the preprosthetic phase. Skin breakdown, ulcers, infected sebaceous cysts, and allergic reactions can occur in the prosthetic phase. Residual limb edema can occur in either phase. Delayed healing of the incision site is one of the earliest preprosthetic complications, resulting in postponed prosthetic fitting. Necrotic areas may develop, requiring surgical intervention.7
To achieve a residual limb length suitable for prosthetic use, the surgeon may perform extensive skin grafting. If the skin graft adheres to bone, the area may ulcerate, requiring medical attention.7 Daily gentle massage by the individual, family members, or the therapist decreases the likelihood of skin graft adherence to bone and the associated complications.
Immediately after surgery, the residual limb is normally edematous as a result of fluid that collects within the soft tissues, especially in its distal portion. Compression wrapping, that is, wearing a prosthetic sock or a rigid dressing, helps decrease the edema.8,23,34
During the postprosthetic phase, an ill-fitting socket or wrinkles in the prosthetic sock may cause skin breakdown or scar adhesions.24 Residual limb ulceration is associated with ischemia and pressure exerted by the prosthesis on the limb. The physician should see the client in this case, and the prosthesis should not be worn until the area heals. The prosthetist should also examine the prosthesis to determine whether the socket requires adjustment. If problems persist, surgical revision of the limb may be necessary before rehabilitation can continue.51
Torque forces between the socket and the residual limb cause a predisposition to the development of sebaceous cysts. Treatment involves the application of moist heat. When the cyst becomes infected, drainage ensues and enucleation of the cyst wall may be required.7
Development of residual limb edema during the postprosthetic phase usually indicates an ill-fitting socket. Proximal tightness of the socket may result in distal edema, which may require a new, well-fitted socket.7
Sensation
Loss of sensory feedback from the amputated limb is a major problem for clients. This loss of sensation is especially significant for the person with an upper limb amputation because sensory feedback from the hand, so essential for function, is lost. Residual limb hyperesthesia, neuroma, and phantom sensations are problems that interfere with functional use of the limb with or without the prosthesis.
Residual limb hyperesthesia, or an overly sensitive limb, limits functional use and causes discomfort. Desensitization consists of texture stimulation, tapping, and massage, all of which help to decrease the discomfort.6,24 Sympathetic nerve blocks may be used medically to manage residual limb hypersensitivity.55
The residual limb may have areas of absent or impaired sensation requiring education and special attention when the prosthesis is worn. The person must rely on visual and proprioceptive feedback because sensation is functionally lost when the prosthesis is on the residual limb. The client must adjust to new sensations, such as the pressure of the residual limb inside the socket and the feel of the harness system, if used.64
Neuroma: Severed peripheral nerves may form neuromas in the residual limb.39,44 A neuroma is a small ball of nerve tissue that develops when growing axons attempt to reach the distal end of the residual limb. As the axons grow, they turn back on themselves, producing a ball of nerve tissue. If the neuroma adheres to scar tissue or skin subject to repetitive pressure, it can be painful when pressed. Diagnosis is made by palpating the neuroma.8 Most neuromas occur 1 to 2 inches (2.5 to 5 cm) proximal to the end of the residual limb and are not troublesome.7
So that pain will not interfere with prosthetic wear, the neuroma must be well surrounded by soft tissue. During surgery, the surgeon identifies the major nerves, pulls them down under some tension, cuts them clearly and sharply, and allows them to retract into soft tissue of the residual limb. Neuromas that form close to scar tissue or bone generally cause pain.39,44
Treatment for painful neuroma involves local anesthetic injections or ultrasound. Both treatments should be followed by massage and stretching. Surgical intervention may be necessary. Surgical options are to (1) redirect the nerve more proximally into a padded area, (2) tie the nerve ending into a proximal wound bed to protect it, or (3) tie two nerve ends to each other to prevent neuroma development. In addition, the residual limb socket may be fabricated or modified to accommodate the neuroma.6,71,72
Phantom Limb: Most individuals who have had an amputation experience phantom limb. In its simplest form, the phantom is the sensation of the limb that is no longer there. The phantom usually occurs initially immediately after surgery. The distal part of the limb is most frequently felt, although sometimes the person feels the whole extremity. Sensation is influenced by external stimuli such as bandaging or rigid dressing. It may dissipate over time, or the person may experience the phantom sensation throughout life. Phantom sensation that is not painful does not usually interfere with prosthetic rehabilitation. The client should be assured that the feeling is quite normal.63,72
Education, supportive counseling, and early use of the residual limb with a preparatory or permanent prosthesis are effective measures for dealing with phantom limb.64 In many cases it is best not to dwell on the discussion of phantom limb, but rather to focus on prosthetic training and the return to a former lifestyle.
Phantom Sensation: Phantom sensations are different from phantom limb in that they are detailed sensations of the limb. Individuals may describe these as cramping, squeezing, relaxed, numb, tingling, painful, moving, stuck, shooting, burning, cold, hot, or achy. Phantom sensations are described as constant or intermittent. Some individuals report a variety of sensations occurring simultaneously, especially in the hand itself. For example, they may feel the second through fifth digits cramped tightly into flexion and may describe the absence of thumb sensation, as was the case with Roberto. Alternatively, an individual may describe a painful wrist that feels stuck in one position, although the phantom forearm rotates easily with no pain. Pain is one phantom sensation. The therapist must be careful when describing or questioning the client about phantom sensations to avoid using the term “phantom pain.” This phrase is most often interpreted by clients as the absence of true pain; their psychological responses to this concept may include fear, anger, distrust in the practitioner’s knowledge or support, or confusion. Pain may diminish over time or may remain a permanent and sometimes disabling condition.
No treatment protocol has been established for the pain associated with phantom sensation. Isometric exercises of the phantom and residual limb initiated 5 to 7 days after the amputation and performed several times throughout the day may help to minimize pain. Active movement of muscles associated with the phantom limb can be beneficial, especially when the sensations are described as stuck, cramped, or tight. Mirror therapy has been eliciting some positive results in decreasing the pain of the phantom limb.64a,64b Biofeedback, transcutaneous electrical nerve stimulation (TENS), ultrasound, progressive relaxation exercises, and controlled breathing exercises may reduce the pain. Activities such as massaging, tapping, and applying pressure to the residual limb may be beneficial. A physician may treat the pain by prescribing oral medications, injecting anesthetics into a specific soft tissue area, or performing sympathetic nerve blocks. Surgical revision of the residual limb is sometimes necessary to alleviate the pain.6,13,71 An individual may take nonpharmaceutical oral supplements to decrease the pain. A client’s excessive concern with phantom sensations requires the intervention of the team. The therapist can allay the client’s fears about these phenomena by offering support, information, reassurance, and contact with other prosthesis wearers.
Bone
The formation of bone spurs is another complication that may occur during the preprosthetic phase. Because most bone spurs are not palpable, an X-ray examination is necessary to confirm their presence or absence. Bone spurs that cause pain or result in persistent drainage require surgical excision.
Wound Healing
For clients with LE amputation, delayed wound healing and excessive skin grafting are potential complications during the preprosthetic phase.
Many factors may affect normal wound healing. Postoperative infection from external or internal sources is a major concern. Clients with wounds contaminated from injury, infected foot ulcers, or wounds with other causes are at greater risk for infection. Research indicates that smoking is a major deterrent to wound healing because it diminishes or restricts circulation to the distal extremities. One study reported that individuals who smoke are approximately 2.5 times more likely to have higher rates of infection and reamputation than nonsmokers.15,37 Evidence suggests that failure of limb revascularization may negatively influence healing at below-knee levels. Other factors that influence wound healing include the severity of the vascular problems, diabetes, renal disease, and other medical conditions such as cardiac disease.14,39,68,70
Section 2: Upper Limb Amputations
Body-Powered Prostheses
Information regarding prostheses and the rehabilitation program should be provided before the amputation, if possible, because subsequent pain medication and anxiety may interfere with the client’s ability to process new information. Team discussion is vital for determining whether to generate a prosthetic prescription and, if so, which components to include, or, alternatively, whether a prosthesis is inappropriate. The client’s age, medical status, amputation level, skin coverage, skin condition, cognitive status, and desire for a prosthesis are important factors in making the decision.
Levels of Amputation and Functional Losses in the Upper Limb
The higher the level of amputation, the greater is the functional loss of the limb. Greater functional loss necessitates a more complex prosthesis and more extensive training in operation and use of the prosthesis (see Figure 43-1).27 Table 43-1 provides an outline of progressively higher upper limb amputations, associated loss of function, and appropriate components required for a functional body-powered prosthesis.22,27 Partial hand amputations are commonly seen. When surgical replantation is not feasible, the focus is placed on reconstruction of the remaining hand. Successful fit of a partial hand prosthesis can preserve the general function of the hand or provide improved cosmesis (Figure 43-2).
TABLE 43-1
Amputation Levels, Functional Losses, and Suggested Prosthetic Components
| Level of Amputation | Loss of Function | Suggested Functional Prosthetic Components |
| Partial hand | Some or all grip functions | Dependent on cosmesis and functional loss |
| Wrist disarticulation | Hand and wrist function; about 50% of pronation and supination | Harness, control cable, socket, flexible elbow hinges |
| Long trans-radial | Hand and wrist function; most pronation and supination | Same as for wrist disarticulation but circular wrist unit |
| Short trans-radial | Hand and wrist function; all pronation and supination; half cuff, wrist unit, and terminal device | Harness, control cable, self-suspending socket or traditional socket with rigid elbow hinge, wrist unit, and terminal device extension |
| Elbow disarticulation | Hand and wrist function; all pronation and supination; elbow flexion and extension | Harness, dual-control cables, socket, externally locking elbow, forearm shell, wrist unit, and terminal device |
| Long trans-humeral | Hand and wrist function; all pronation and supination; most shoulder internal and external rotation, elbow flexion and extension | Harness, dual-control cables, socket, internally locking elbow, lift assist, turntable, forearm shell, wrist unit, and terminal device |
| Short trans-humeral | All of the above; shoulder internal and external rotation | Same as for long transhumeral, but socket may partially cover shoulder, restricting its function |
| Shoulder disarticulation | Loss of all arm and hand functions | Same as for long trans-humeral, but socket covers much of the chest wall shoulder; chest strap; shoulder unit; upper arm shell; chin-operated nudge control for elbow unit |
| Interscapular thoracic | Loss of all arm and hand functions; partial or complete loss of clavicle and scapula | May be same as above but with lightweight materials; when minimal function is attainable, endoskeletal cosmetic prosthesis sometimes preferred |
| Bilateral amputation | Dependent on levels of amputation | Appropriate to level of amputation, plus wrist flexion unit and cable-operated wrist rotator |
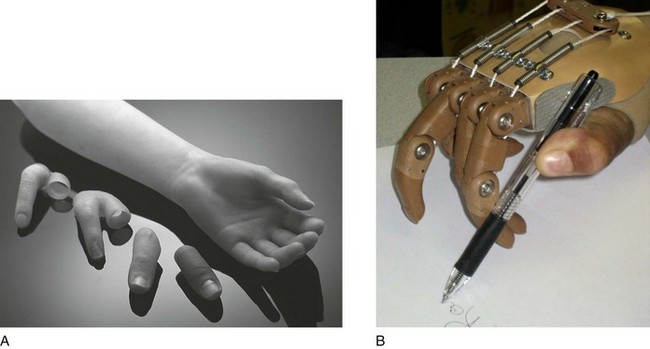
FIGURE 43-2 Prostheses for a partial hand amputation. (A, Courtesy Otto Bock HealthCare, Minneapolis, MN; B, Available from Liberating Technologies, Ltd. www.liberatingtech.com.)
Component Parts of the Upper Limb Body-Powered Prosthesis
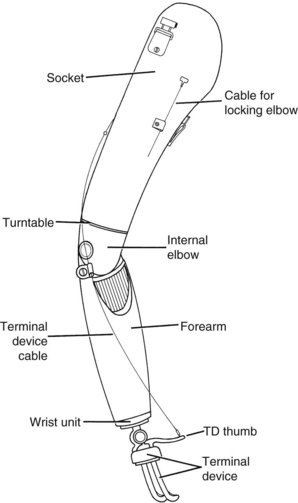
Various prosthetic components are available for each level of amputation (Figure 43-3). Each prosthesis is prescribed according to the client’s needs and lifestyle and is custom made and individually fitted. The prosthesis can be a functional prosthesis or a passive prosthesis. Passive does not mean nonfunctional; the prosthesis provides postural balance and can assist the individual in securing items for the functional limb.
The first five prosthetic components described in the following sections are common to all body-powered prostheses prescribed for wrist disarticulation and higher levels. They are the socket, harness, cable, terminal device (TD), and wrist unit. Many people with upper limb amputations wear a prosthetic sock between the residual limb and the prosthesis.62
Prosthetic Sock: A prosthetic sock of knit wool, cotton, or Orlon Lycra is worn between the prosthesis and the limb (Figure 43-4). Silipos makes Silo-Line, which assists in minimizing hypertrophic scarring and may be worn as the prosthetic sock or covered with an additional sock. The function of the prosthetic sock is to absorb perspiration and protect against irritation that can result from direct contact of the skin with the socket. The sock compensates for volume change in the residual limb and contributes to fit and comfort in the socket.62,74
Socket: The socket is the fundamental component to which the remaining components are attached. A cast molding of the residual limb is used to construct the socket to optimize fit, comfort, and function. It fits snugly over the limb and extends as far as the wrist unit with a trans-radial prosthesis or to the elbow unit with a trans-humeral prosthesis. It should cover enough of the residual limb to be stable but not so much that it unnecessarily restricts movement. Uneven pressure distribution may lead to skin problems.62,72
The length of the residual limb determines whether a socket is of single- or double-wall construction. The single wall is most commonly used with a wrist disarticulation or elbow disarticulation level of amputation. The single-wall socket requires no shaping over the residual limb. Most sockets have a double wall. This construction involves an inner socket with an outer shape created in foam or wax, covered with an outer shell that is laminated to it. The two shells, inner and outer, become one. The outer wall provides a structurally cosmetic surface. The inner wall maintains total contact with the skin surface of the residual limb to distribute socket pressure evenly. Recently, flexible frame-type sockets have been favored. The inner socket is flexible and is covered with a rigid outer frame that carries the hardware. This type of socket allows for volume and contour changes that occur when muscles contract and relax. Wearers report that this type of socket is cooler than conventional alternatives.3 The Utah Dynamic Socket has a unique socket design that provides mediolateral and rotational stability through shaping of the shoulder region.3
Harness and Control System: The prosthetic control system functions through the interaction of a Dacron harness and stainless-steel cable. The figure-of-eight harness is commonly used, although others are available. The harness is worn across the back and shoulders or around the chest and fastens to the socket to secure the prosthesis. When the amputation level is higher, the harnessing system becomes more complex.
Loss of muscle power and range of motion (ROM) may necessitate variations in the harness design. A properly fitted harness is important for both comfort and function.58,62,72
A flexible stainless-steel cable, contained in Teflon housing, attaches to the harness on one end via a T-bar or hanger fitting and attaches to a functional component of the prosthesis on the other end. Spectra fiber, an extremely strong material, has been used recently instead of the stainless-steel cable because it glides through the housing with less friction. A trans-radial prosthesis uses one cable to operate the TD, which is connected by a ball swivel. A trans-humeral prosthesis uses a second cable to lock and unlock the elbow unit. Specific upper body movements create tension on the cables, thereby operating the prosthesis. A properly fitted control system maximizes prosthetic control while minimizing body movements and exertion.2,58,72
Terminal Device: The terminal device, the most distal component, functions to stabilize or hold an object. When choosing the most appropriate TD for a prosthesis, team members consider the client’s age and life roles.
Two styles of TDs are commonly prescribed: the hook and the hand. Many TDs and prosthetic hands have the same shaft size at their base, which allows them to be interchangeable. Hooks are of two basic designs: canted or lyre shaped.18 They may be voluntary opening (VO) or voluntary closing (VC).46
The VO TD opens when the wearer exerts tension on the control cable that connects to the “thumb” of the TD. When tension is released, rubber bands or springs close the fingers of the TD. The number of rubber bands or springs determines the holding force of the TD.
VC TDs close by tension applied to the control cable. The tension may also lock the TD and maintain the grasp on the object. The VC TD automatically opens by spring operation when the cable is relaxed. The VO TD was commonly prescribed in the past. Since World War II, more modern alternatives have become available (Figure 43-5).2,3,10

FIGURE 43-5 Hosmer-Dorrance hook terminal devices are available in a variety of materials, shapes, and sizes that can be matched to the particular functional needs of a child or adult. (Courtesy Hosmer-Dorrance Corp., Campbell, CA.)
VO TDs have several options to better suit the wearer’s lifestyle. The option chosen depends on the desired durability, weight, or grip of the TD.
Stainless-steel TDs are prescribed for activities requiring a durable TD, such as yard work or construction. Aluminum TDs are recommended for lighter work and to reduce the total weight of the prosthesis for a person with a higher-level amputation. Most TDs have a neoprene lining or a serrated grid between their fingers. The neoprene lining increases the holding friction and minimizes damage when holding objects. Neoprene is a high-density rubber that wears out faster than the stainless-steel grid and disintegrates if it comes in excessive contact with some chemical solutions. The TD must be sent back to the manufacturer for neoprene replacement.
A variation of the standard VO TD is the heavy duty model. This model is made of stainless steel and has a serrated grid between its fingers. The heavy duty model is designed to hold tools, nails, and long-handled instruments such as a broom or shovel.
A prosthetic hand is also available as a TD. It attaches to the wrist unit and is passively operated or cable operated. The passive hand has cosmetic and lightweight appeal, but it is also functional because it is used to push, pull, and stabilize objects. The same control cable that operates the hook activates the functional prosthetic hand. It comes in VO and VC styles. As with the hook-style TD, the VO hand is preferred and prescribed more often than the VC hand. A flesh-colored rubber glove fits over the prosthetic hand for protection and a more realistic appearance.62
The client’s lifestyle and activities determine the most appropriate TDs. It is important to provide the wearer with certain information regarding the differences between hook- and hand-style TDs. The hook TD is lighter and provides better visibility when grasping objects. It is more durable and functional than prosthetic hands. Hook VO TDs are mechanically simpler than both VC TDs and functional prosthetic hands. Prosthetic hands are more cosmetically appealing than prosthetic hook TDs. However, the cosmetic glove that covers the hand stains easily, wears out quickly, and disintegrates if it comes in contact with certain cleaning solutions and chemicals. Many individuals with amputations choose an interchangeable hand for social occasions in addition to a hook TD for daily activities.18
Wrist Unit: The wrist unit connects the TD to the forearm socket and serves as the unit for interchange and to pronate and supinate the TD for prepositioning purposes. The wearer rotates the TD by turning it with the sound hand, by pushing the TD against an object or surface, or by stabilizing the TD between the knees and using the arm to rotate it. With bilateral amputations, TD rotation in the wrist unit may be accomplished by cable operation. Five basic types of wrist units are available, and the unit for a particular patient must be chosen according to its ability to meet the person’s needs in daily living and vocational activities: the friction-held unit, the locking unit, the wrist flexion unit, the oval unit, and the ball-and-socket unit.
Friction-held wrist units hold the TD in place by friction provided by a rubber washer or setscrews. Tightening the washer or screws increases friction. Friction is sufficient to hold the TD against moderate loads. Friction-held units are mechanically simple but are not as strong as locking units.
The locking wrist unit allows the TD to be manually positioned and locked into place. The quick-disconnect locking wrist unit is most common. An adapter is permanently attached to the base of the TD. The unit has a button on its side that locks, unlocks, and ejects the TD. Inserting the TD into the wrist unit locks it into place. Another style of TD with the same adapter type on its base may be locked into place. Friction and locking wrist units allow the TD to be rotated up and down but not deviated in toward the body.
The wrist flexion unit allows the TD to be manually flexed and locked into position. It is generally used on the dominant side of a person with bilateral amputations to facilitate midline activities close to the body, such as dressing and toileting.2,46,62,72,74
The oval unit, which conforms to the shape of the wrist, is used on the wrist disarticulation prosthesis. It is thinner than the other wrist units, so the prosthesis may more closely match the length of the sound arm.
A ball-and-socket wrist unit is also available (Figure 43-6). This unit is unique in that it allows prepositioning in multiple wrist positions. It has constant friction, and the magnitude of the loading is adjustable.18
The socket, harness, control system, TD, and wrist unit are components common to all body-powered prostheses. Remaining body-powered prosthetic components maximize function at specific levels of amputation. These components are the elbow hinges for trans-radial prostheses, elbow units for trans-humeral prostheses, and shoulder units designed for shoulder prostheses.
Trans-Radial Hinges: A trans-radial prosthesis employs two hinges, one on each side of the elbow, that attach to the socket below the elbow and to a pad or cuff above the elbow. These hinges stabilize and align the trans-radial prosthesis on the residual limb. When properly aligned, the hinges help distribute the stress of the prosthesis on the limb.
Two hinge styles, flexible and rigid, are available for the prosthesis. Flexible hinges are used on wrist amputation and long trans-radial prostheses. They usually are made of Dacron and connect the socket to a triceps pad positioned over the triceps muscle. The flexibility permits some forearm rotation, decreasing the need to rotate the TD manually in the wrist.
Medium to short trans-radial prostheses may have a socket that covers most of the residual limb below the elbow and rigid or flexible hinges to provide stability. Rigid hinges usually are made of steel and attached to a laminated Dacron biceps half-cuff positioned behind the arm, which is sturdier and provides more support than the triceps pad. They are used less frequently now and have been replaced by a design using a self-suspending socket, where supercondylar flares mimic some of the function of the hinges and triceps pad. Team members consider the amount of residual function and the length of the limb when choosing the appropriate hinge style for the trans-radial prosthesis.46
Elbow Units for Trans-Humeral Prostheses: A prosthetic elbow unit is prescribed for the person who has had an amputation through the level of the elbow or higher. The elbow unit allows 5 to 135 degrees of elbow flexion and locks in various positions. The two main types of elbow units are internally and externally locking units. The more durable internally locking unit is prescribed for a person who has had an amputation 2 inches or more above the elbow. This unit connects the trans-humeral socket to the prosthetic forearm. The locking mechanism is contained within the unit and attaches to a control cable. A lift assist, which consists of a tightly coiled spring attached to the elbow unit and forearm shell, helps reduce the amount of energy required to lift the forearm shell. The lift assist also allows a slight bounce in the forearm when walking with the elbow unlocked, which enhances the appearance of a natural arm swing.
A friction-held turntable positioned on top of the elbow unit allows the prosthetic forearm to be rotated manually toward or away from the body. Lateral and medial aspects of a trans-humeral prosthesis are shown in Figure 43-7. The internally locking unit is 2 inches long and therefore does not fit on a person who has had an amputation close to the elbow.
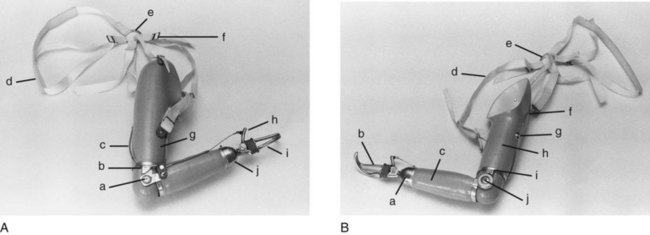
FIGURE 43-7 A, Lateral side of trans-humeral prosthesis: a, elbow unit; b, turntable; c, control cable; d, adjustable axilla loop; e, harness ring; f, figure-of-eight harness; g, elbow lock cable; h, terminal device (TD) thumb; i, hook TD; j, wrist flexion unit. B, Medial side of transhumeral prosthesis: a, wrist unit; b, hook TD; c, forearm; d, harness; e, harness ring; f, control cable; g, baseplate and retainer; h, socket; i, turntable; j, spring-loading device.
Correspondingly, the externally locking elbow unit is prescribed for a person who has an elbow disarticulation or an amputation within 2 inches above the elbow. This unit, which consists of a pair of hinges positioned on either side of the prosthesis, attaches the socket to the forearm. The cable attaches to one of the hinges, which locks and unlocks the unit.
Shoulder Units: A person with an amputation at the shoulder requires a prosthesis with a shoulder unit in addition to the TD, wrist unit, forearm shell, elbow unit, socket, harness, and cables. Because of the high level of amputation, however, shoulder and back movements are not sufficient to use a cable-operated shoulder unit. Thus, most shoulder units are manually operated and friction held. The TD and elbow units may still be cable operated.
Two shoulder unit styles that are often prescribed are the flexion-abduction unit and the locking shoulder joint. The flexion-abduction (or double-axis) unit provides manual prosthetic positioning in flexion and abduction and is friction held (Figure 43-8).18 The locking unit allows the prosthesis to be locked in various degrees of shoulder flexion. This feature is helpful because the prosthesis is heavy and the friction style may not be strong enough.


FIGURE 43-8 Hosmer-Dorrance flexion/abduction shoulder joint, shown attached to a shoulder disarticulation-type prosthesis, provides passive mechanical range of motion in flexion to 90 degrees and abduction to 135 degrees. An extension stop is provided to restrict extension. (From Hunter JM, Mackin EJ, Callahan AD: Rehabilitation of the hand: surgery and therapy, ed 4, St Louis, 1995, Mosby.)
With an interscapular thoracic amputation, all or a portion of the scapula and clavicle is removed with the arm. If standard prosthetic components were used, the prosthesis might be too heavy for practical use. Therefore, an endoskeletal prosthesis, made from lightweight materials such as a single aluminum alloy surrounded by a soft foam shape, is often prescribed to decrease its weight. The system provides its own style of prosthetic joints, which will not withstand heavy duty usage. An endoskeletal prosthesis with a lightweight cosmetic cover is commonly prescribed as an aesthetic prosthesis with limited functional value.
Upper Limb Preprosthetic Program
The preprosthetic program begins when the decision to perform an amputation is made, or when a client is evaluated after a traumatic amputation.34 Education regarding prosthesis options, relaxation techniques, the phantom limb phenomenon, and general conditioning may begin in some cases before the surgical amputation. During the period between amputation and fitting of the prosthesis, the client participates in a program designed to prepare the residual limb for a prosthesis, facilitate adjustment to his or her loss, and achieve maximal independence in self-care.50,72 The occupational therapist is the primary person who will be coordinating this program. It is also important for the team to assist the client in securing the financial resources necessary to complete rehabilitation and obtain a prosthesis if desired.
Preprosthetic Evaluation: To establish an individualized intervention plan, the therapist must complete a thorough evaluation, which includes assessments of the client’s medical history; body functions (mental, sensory, movement, skin); motor skills (posture, coordination, strength and effort, energy); process skills (adaptation, organizing space and objects); activities of daily living (ADLs); instrumental activities of daily living (IADLs); education; work; leisure; and rest and sleep and social participation.1 The therapist will also consider the values, beliefs, and spirituality of the person. A statement of the client’s goals is important for orienting treatment toward meeting these goals and for determining the client’s understanding of the program and prosthesis functions.6 The interview portion of Roberto’s evaluation was essential in establishing his desires, goals, and concerns and is necessary in developing the most appropriate intervention for him.
Preprosthetic Treatment: The intervention plan is based on evaluation results. Most plans include the interventions for body functions, body structures, and performance skills that are listed in Box 43-1.
Depending on the level of amputation, medical conditions, and ADL status, the decision is made whether to complete the preprosthetic program on an inpatient or outpatient basis. In most cases in which the client has undergone a unilateral amputation, therapy services are offered on an outpatient basis. When an individual loses a dominant hand, which is often the case with unilateral amputation, minimal training in one-handed activity completion may take place. The focus of this training is on problem-solving approaches to task completion with new hand dominance and on encouraging the client to practice completing activities independently. A person with bilateral limb amputations may need to be admitted to a facility because of the significant amount of therapy and assistance required. In the case of bilateral upper limb loss, the client has significant issues with functional independence to address, as well as emotional issues related to a severe life change that affects emotions, finances, life goals, body image, and relationships. The complexity of the issues is best addressed in an inpatient setting. A client who has had both upper limbs amputated will appreciate being introduced to other persons who are using one or two prostheses to function. The team closely monitors the residual limbs and reports problems to the physician. If the client is followed on an outpatient basis, frequent medical visits may be necessary to monitor progress. Early fit of a prosthesis has been shown to significantly enhance functional prosthetic use.53 Fitting clients with a preparatory prosthesis before they become “one-handed” facilitates their success with prosthetic function.
Body Image, Self-Image, Psychosocial Adjustment: Facilitating the client’s engagement in occupations in response to altered activity demands and restoring family, occupational, and social relationships are the primary focus of occupational therapy intervention. The therapist helps the client integrate the physical loss into his or her life. It is essential that the therapist validate the client’s right to be in control of his or her life. The person’s values, beliefs spirituality, and well-being direct the occupational therapist’s interventions. Roberto’s strong work ethic and goal of returning to work as quickly as possible to fulfill his role identity must be honored. It is not uncommon for individuals who have undergone an amputation to experience a physical shock to their body, as well as an emotional shock to their spirit. Fear, confusion, anger or frustration, emotional swings, introspectiveness, and dependence are common responses following loss. Allow the client to experience and express these feelings during therapy sessions, and promote recognition by family members and the client of the common nature of these feelings.1
Assist the client in describing which of his or her features are pleasing. Encourage the client to continue with useful habits to maintain a normal routine. Give positive feedback for every accomplishment reported or observed.
Once the person’s level of social participation before the amputation is explored, facilitate opportunities to engage in similar events. The client may be encouraged to participate in one event monthly or weekly, initially in the company of a family member or friend. Introduce the client to others who have suffered a similar limb loss to allow communication with a peer. Provide adaptive equipment that allows the client to resume leisure activities and increase his or her participation in life. Some clients are uncomfortable with the changes in fashion and clothing style that are recommended to ease the dressing process. Recommend a tailoring service, or help the client identify a family member, friend, or neighbor who would be willing to modify some of the clothing.
Activities of Daily Living: During the preprosthetic period, the client with a unilateral amputation is encouraged to use the sound arm to perform ADLs. If the dominant arm was amputated, training may be required for the nondominant limb to assume the dominant role. In the author’s experience, most clients change dominance to the sound extremity automatically as a result of the adaptive process, and minimal intervention is necessary for this to occur. Some clients need support and a few sessions of practice performing meaningful activities with the nondominant hand to understand and accept their ability to perform and create new habits. The focus of performance is on problem-solving techniques and adaptations that will allow clients to modify multiple activities in their daily lives. Some adaptive equipment is appropriate for increasing independence with bilateral activities. Practice in writing and activities requiring dexterity and coordination may be helpful in the retraining process.50,62,72 The importance of early fitting of a prosthesis cannot be minimized. Early fit programs are very successful in helping the client with an amputation to incorporate the new extremity more rapidly into his or her daily activities.2
In the case of bilateral amputations, adaptive equipment should be introduced as soon as possible to increase the client’s level of independence. The equipment may include a utensil cuff secured by elastic or Velcro to the residual limb to aid in eating, writing, and hygiene; a dressing tree with hooks to hold articles of clothing in a position conducive to donning them, to improve dressing independence; and loops added to items such as socks and towels. Individuals with bilateral amputations can learn to complete activities using foot skills, such as holding items between the toes in a functional pinch for dressing, eating, and turning pages, and using the toes to push buttons on a keyboard or telephone pad.
Wound Healing: When the surgical dressing is removed, the residual limb is massaged to discourage scar adhesions, increase circulation, aid in desensitization, and reduce swelling. Massage of the limb also helps the client overcome fear of touching or moving the residual limb. Massage over the incision site begins once the incision has stabilized.6 Initially, light massage over healed areas is performed, followed by deeper pressures, as tolerated by the client. If skin grafts have been placed, the therapist must confer with the surgeon to determine tissue status before performing any scar remodeling techniques.
Desensitization: The person’s residual limb may be hypersensitive after surgery, requiring a technique known as desensitization. By overstimulating a hypersensitive peripheral area with nonharmful stimuli, the central nervous system learns to accept these stimuli as nonharmful and to minimize aversive responses to them. Massage is one method of desensitization. Other methods are tapping, vibration, constant pressure, and rubbing of various textures on the limb, such as terry cloth, silk, and cotton. The therapist introduces the tissue to soft, lightweight, smooth textures and progresses to rough, hard, uneven, heavier textures as the client is able to tolerate them. A therapist with a thorough understanding of nerve anatomy and hierarchy of response to stimuli should be consulted, and the intervening therapist must understand this information before subjecting the client’s tissues to a desensitization program. As the techniques are performed, the therapist teaches them to the client and his or her family members or caregivers to facilitate completion at home.6,24
Wrapping: Shrinking and shaping the residual limb are necessary to form a tapered limb that will tolerate a snug-fitting socket. Compression using an elastic bandage, a tubular bandage, or a shrinker sock applied to the residual limb aids in the shrinking and shaping process. When an elastic bandage is applied to the limb, a figure-of-eight method is used—not a circumferential method in which the bandage is wrapped around the limb spirally. Care must be taken to apply the bandage smoothly, evenly, and not too tightly from the distal to the proximal end of the residual limb. Care must also be taken to avoid wrapping skin-grafted areas too tightly or without an inner nonadherent dressing applied, so that the graft is not compromised. A limb that is wrapped incorrectly may take longer to shrink and shape. A limb with a trans-radial amputation should be wrapped up to or above the elbow. A limb with a trans-humeral amputation should be wrapped up to or above the shoulder. Short trans-humeral amputations usually must be wrapped around the chest to help stabilize the wrap.62,72 The elastic bandage should be changed several times a day and the skin checked between wrappings. Several compression wraps are required, so that the limb can be wrapped in a clean bandage at all times, except when bathing. Wraps should be washed often with a mild soap, rinsed well, and allowed to dry thoroughly while lying flat. For longer life, bandages should not be wrung out after washing.6
Shrinker socks generally are preferred over elastic bandage wrapping because the client can more independently don the sock, and because changing the sock is much quicker than changing the wrap. Compression tubing sewed closed or with a knot tied at one end is commonly used. The tubing may be attached to a chest strap if necessary. Occupational therapists collaborate with prosthetists to identify options available or recommended for the client’s limb.
Circumference Measurements: Circumference measurements of the residual limb are taken often and in the same area to determine when the person is ready to be casted for a prosthesis. The therapist uses a tape measure to establish baseline and subsequent measurements (Figure 43-9). When edema is gone and circumference measurements have stabilized, the limb is ready to be casted.
Skin Hygiene: Instruction in proper residual limb hygiene is an important aspect of the preprosthetic program. The limb should be washed daily using a mild soap, rinsed thoroughly, and patted dry. The limb should dry completely before the wrap or sock is reapplied.5
Insensate Skin: The client with an upper limb amputation requires instruction regarding the care and safety of a residual limb that lacks all or partial sensation. The client is taught to inspect the limb when removing the wrap and washing the limb. Problems should be reported to the therapist or physician. The client also learns to visually track a sensory-impaired residual limb when completing activities, such as wearing protective clothing while engaged in yard work or recreational activities, adjusting the position of the limb when seated in a chair and reading to prevent stretch or compression injury to the tissues, and refraining from using the limb for sensory input, such as testing water temperature.
Upper Extremity Range of Motion, Strength, and Endurance: Motor skills are promoted once medical approval is provided. The client begins exercises designed to maintain and increase range of motion (ROM) and to strengthen upper quadrant and trunk muscles. Depending on the level of amputation, the client performs specific exercises that mimic the movements required to operate the prosthesis. The therapist manually positions and holds the residual limb in the desired posture and asks the client to resist the hold, facilitating increased strength of the appropriate muscles. In the case of a trans-radial amputation, it is important to strengthen the muscles of the shoulder, elbow, and scapula. Pronation and supination movements are also important for long trans-radial amputations. Trans-humeral amputation strengthening may include a movement combining shoulder depression, extension, and abduction that mimics the operation of the body-powered prosthesis. Isometric exercises enable the client to engage in a strengthening program without equipment. Exercises may be completed with rubber tubing, elastic band, or strap-on weights. It may be appropriate to guide the client in the modified use of home or gym equipment to complete exercises. Chest expansion capability is important for higher-level amputations, and when the harness wraps around the chest. A tape measure positioned around the chest helps in the documentation of increased chest expansion.
The occupational therapist prepares a home program containing exercises for general strengthening and body conditioning, as well as specific movements taught during therapy. (Figure 43-10).
Prosthetic Information and Prescription
During the preprosthetic period, the client consults with a prosthetist to learn information about the benefits and limitations of a variety of prostheses. The prosthetist generally provides information regarding specific prosthetic options, and the therapist promotes the client’s understanding of the options as they relate to the client’s performance in areas of occupation. Through collaboration and evaluation, the therapist understands the values, beliefs, and spirituality of the client. What do the amputation and the prosthesis mean to the client at this stage, and what are the client’s future goals? Roberto verbalized his desires for return to gainful and fulfilling employment to provide for his family. In selecting prosthetic components, the therapist must consider whether the client’s primary desire is function or cosmesis, and which style is most appropriate for the client’s needs and choices. Prosthetic components can be introduced in several ways: through slides, videotapes, photographs, interaction with a person with a similar amputation wearing a prosthesis, practice in handling a prosthesis, and a collaborative visit to the prosthetist.
Prosthetic Program
The amount of training each client needs depends on how quickly he or she is able to understand the body structures and mechanics required to operate the prosthesis and on the client’s current motor, sensory, cognitive, and emotional regulation skills. These affect the cueing needed by the client to include the prosthesis in an activity and the carryover of motor skill between activities. When a long period has elapsed between the amputation and fit of the prosthesis, the client may require more cueing because he or she has become adept at one-handed activities. Some clients arrive at therapy already able to operate their prosthesis, whereas others require extensive training.
Ideally, the prosthetist and the therapist coordinate fitting of the prosthesis and initiation of therapy. The therapist may arrange to be present for the final fitting session with the prosthetist and the client. Communication between the wearer, therapist, and prosthetist is essential to ensure that the prosthesis fits and functions optimally. It is common that the prosthesis requires adjustments, and the therapist initiates consultation with the prosthetist when these needs become evident.
The prosthesis will not be as functional as a normal arm, and training for the client with a unilateral amputation should stress that the prosthesis functions primarily as an assist or helper to the sound arm. If the prosthesis is presented in this manner, the wearer may experience less difficulty when incorporating it into daily occupations. In training the person with bilateral amputations to function with prostheses, the likelihood of success with one prosthesis is high, as the wearer instantly recognizes the benefit of the prosthesis to independent function.
The prosthetic program begins after the final fitting of the prosthesis. This final fitting may be done with a preparatory prosthesis rather than a definitive prosthesis, incomplete in its cosmetic form. The occupational therapy intervention is occupation-based and includes purposeful activity and preparatory methods to facilitate therapeutic goals. These include the following:
• Promote positive body image and self-image
• Establish successful adaptation and problem-solving skills
• Promote proper residual limb and prosthetic sock hygiene
• Promote recognition of prosthesis terminology and function
• Promote proper care of the prosthesis
• Establish a prosthesis-wearing schedule and routines
• Promote control of the prosthesis (control training)
• Promote use of the prosthesis in activity (use training)
• Promote independent ADL and IADL function with the prosthesis (functional training)
• Promote driving modifications and ability
• Recommend a home activity program
• Restore upper extremity muscle strength necessary for operation of the prosthesis
Prosthesis checkout, control training, use, and functional training are individualized according to the client’s level of amputation.
Body Image and Self-image: The interview process reveals the client’s lifestyle, habits, routines, rituals, primary roles, and social and personal relationships. The occupational therapist is the professional who investigates and responds to the spiritual essence of the client. Expanding the interview with questions about the client’s interests, social activities, style of dress and appearance, and self-concept is necessary to establish the client’s preinjury behaviors and skills. The therapist observes the client’s body language. Is the residual limb hidden? Does the client use the residual hand and arm to communicate? Is the client visually attentive and engaged in the interview or intervention? What does this tell you about the client’s self-image and body image? Provide opportunities for the client to verbalize his or her accomplishments and skills. Ask the client to describe those parts of the body with which he or she is most pleased. Create therapy sessions that facilitate the client’s ability to style hair, apply jewelry, fasten a tie, apply makeup, resume general physical activity and recreation, drive independently, and manage a briefcase or personal electronic equipment.
Residual Limb and Prosthetic Sock Hygiene: The client is instructed in residual limb hygiene and care of the prosthetic sock in the early phase of prosthetic training. The residual limb and armpit should be inspected, washed, and patted dry, and deodorant should be applied daily. If the client wears a prosthetic sock, he or she should own several so that a clean one may be worn daily to decrease the incidence of skin problems. The socks should be hand washed, gently squeezed, and placed on a flat surface to dry in their original dimensions. Wearing an undergarment under the harness is often recommended because it will absorb perspiration and protect the axilla and back from irritation. It may be necessary to change prosthetic socks and undergarments twice daily in hot weather.72,74 To minimize sweating, educate the client in the application of antiperspirant to the portion of the extremity within the socket.
Prosthesis Terminology and Function: The wearer should learn the terminology and function of each prosthetic component. This task allows the client to communicate with the rehabilitation team, using terminology understood by all, regarding operation of the prosthesis and difficulties with or repairs needed to the prosthesis.5,72,74
Care of the Prosthesis: Instructions regarding care of the prosthesis are provided and reviewed. Generally, the prosthetist educates the person in this area and the therapist reviews the information with the wearer. The socket should be cleaned daily. Cleaning at night is recommended to allow the prosthesis to dry completely. Wearing the prosthesis when the socket is wet may lead to skin problems. Components should be cleaned and maintained according to the manufacturer’s or prosthetist’s specifications. Daily inspection of the prosthesis will help prevent unnecessary problems.5
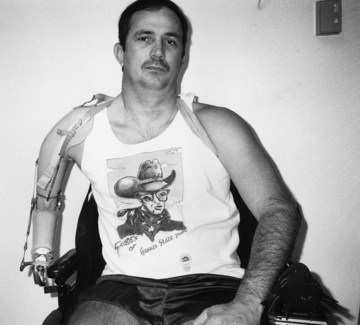
Prosthesis-Wearing Schedule: A prosthesis-wearing schedule is established and reviewed during the first training session. The client initially wears the prosthesis 15 to 30 minutes three times a day. The skin must be closely monitored, and wearing time is increased only if the skin remains in good condition. If there are no skin problems, the three scheduled wearing periods may be increased by 30 minutes each day. By the end of the first week, the client may be wearing the prosthesis all day, as was the case with Roberto. If skin problems occur, the therapist, prosthetist, or physician must be notified. The prosthesis should not be worn until the skin problem has cleared. Restarting the initial wearing schedule may be necessary to decrease the risk of additional skin problems.5
As the person’s wearing tolerance increases, the number of rubber bands on the TD can be increased. Each rubber band added to the TD increases the pinch force by approximately 1 pound. It is best to wait several days after adding one rubber band before adding another to allow the residual limb’s skin and strength to acclimate. If the addition of a rubber band substantially increases limb pain or skin irritation, it should be removed until the pain diminishes and skin tolerance increases.
Checkout of the Prosthesis: When the prosthesis is received, team members check it to ensure that it meets prescription requirements, is functioning efficiently, and is mechanically sound. The prosthesis is checked for fit and function against specific mechanical standards developed from actual tests on prostheses worn by individuals. Tests performed are comparative ROM with the prosthesis on and off; control system function and efficiency; TD opening in various arm positions; amount of socket slippage on the residual limb under various degrees of load or tension; compression fit and comfort; and force required to flex the forearm or open/close the TD.2,58,72 Communication between the wearer, therapist, and prosthetist is essential to ensure an efficiently operating and comfortable prosthesis. The following methods and standards for prosthesis checkout were adapted primarily from Wellerson.72 Step-by-step instructions for prosthetic checkout are available in Wellerson72 and Santschi.58 The prosthesis checkout is primarily performed by the prosthetist. Understanding the process allows the occupational therapist to recognize fit problems that interfere with a client’s engagement in activities.
Trans-radial Prosthesis: The therapist measures elbow flexion with the trans-radial prosthesis on and off the wearer. ROM should not differ by more than 10 degrees, except when there are joint or muscle limitations. Pronation and supination of a wrist disarticulation or a long trans-radial residual limb with the prosthesis on should not be less than 50% of the rotation possible without the prosthesis.
With the elbow flexed at 90 degrees, the client should be able to open the TD fully. The TD is also opened near the mouth (elbow fully flexed) and again near the zipper of the trousers (elbow extended). From 70% to 100% of TD opening should be achieved in these two positions.
Trans-humeral and Shoulder Prosthesis: With the trans-humeral prosthesis on and the elbow locked, the client is instructed to move the residual limb (humerus) into shoulder flexion, extension, abduction, and internal and external rotation. The ROM of each of these is measured. Minimal standards for shoulder ROM with the prosthesis on are as follows: 90-degree flexion, 30-degree extension, 90-degree abduction, and 45-degree rotation. The previous part of the checkout is not applicable for the shoulder prosthesis.
With the elbow unlocked, the client is instructed to flex the shoulder slowly, which flexes the mechanical elbow. Elbow ROM should be about 10 to 135 degrees. The therapist measures the amount of shoulder flexion, which should not exceed 45 degrees, that is required to fully flex the mechanical elbow. The client should also be able to abduct the prosthesis to 60 degrees without locking of the elbow.
The client flexes the elbow to 90 degrees, locks the elbow, and then activates the TD. Full TD opening should be attained in this position. The TD is then opened in full elbow flexion with elbow locked (Figure 43-11) and extension with elbow locked (TD at fly of trousers). At least 50% of full TD opening should be obtained.

FIGURE 43-11 Trans-humeral prosthesis checkout: opening terminal device at mouth with elbow locked in full flexion.
With the elbow unlocked, the client is asked to walk and practice swinging the prosthesis without locking the elbow. This action mimics a normal arm swing during gait.
The client flexes the elbow to 90 degrees, locks the elbow, abducts the residual limb to 60 degrees, and then rotates the humerus. The client should be able to control the prosthesis during this motion. The socket should not slip around the residual limb, and the client should not feel pain or discomfort during these maneuvers. When the prosthesis is removed, the residual limb should not appear discolored or irritated.
Prosthesis checkout also includes technical inspection of the prosthesis to determine correct length, fit, and mechanical function of all parts. Various forms have been devised to record all information for complete checkout of the prosthesis. The initial checkout is performed before prosthetic training begins, and the final checkout is done after prosthetic revisions and adjustments and during or after training.5,58
Donning and Doffing the Prosthesis: Two common methods of donning and doffing the body-powered prosthesis are the coat method and the sweater method. Either method can be used by a person with unilateral or bilateral amputations. The method used depends on the client’s ease of use. Whichever the method, the harness and cables must not be kinked or twisted around the prosthesis before starting. When the prosthesis is removed, it should be placed on a surface so it is ready for the person to don again.
Coat Method: The coat method is similar to placing one arm in the coat sleeve and manipulating the coat to a position where the other arm can reach the sleeve. The coat method has two variants. In the first method, the person places the prosthesis on a table or bed and pushes the residual limb between the control cable and the Y-strap from the medial side into the socket. By raising the residual limb or leaning sideways, the person places the harness across the shoulder on the amputated side and dangles the harness down the back. The sound hand reaches around the back and slips into the axilla loop. The person then slips into the harness as if putting on a coat. The shoulders are shrugged to shift the harness forward and into the correct position.
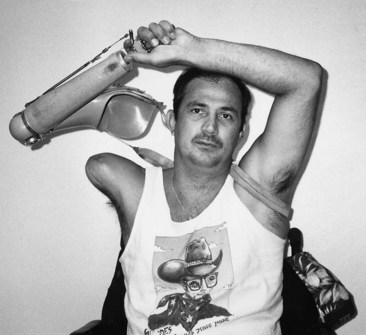
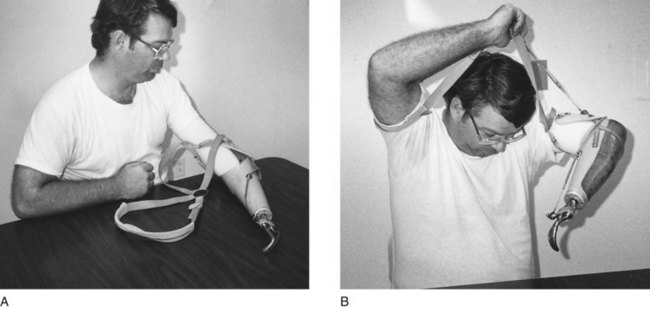
The second approach works by placing the axilla loop of the harness on the sound arm first. For example, if the client has a trans-humeral amputation, it might be easier to lock the elbow at 90 degrees; position the axilla loop on the sound arm above the elbow; grasp the prosthetic forearm; and raise the prosthesis over the head, allowing the harness to position itself across the back. By raising the residual limb, the person positions it in the socket (Figure 43-12).
To remove the prosthesis, the person uses the TD to slip the axilla loop off the sound side and then slips the shoulder strap off the amputated side. The harness is slipped off like a coat.2,58,72
The person with bilateral amputations can use the coat method by placing the prostheses face up on a surface, placing the longer residual limb into the socket, and elevating the prosthesis, allowing the other prosthesis to hang across the back. The person then leans to the side and places the shorter limb in the prosthesis.58,74 To remove the prosthesis, the person shrugs the harness off the shoulders and removes the prosthesis from the shorter side first. Before removing the prosthesis on the longer side, the person should position the prostheses somewhere convenient for the next donning.
Sweater Method: The sweater method (Figure 43-13) is equivalent to entering both sleeves at the same time and then raising both arms up, out, and up to don the sweater. To apply a unilateral prosthesis using the sweater method, the person places the prosthesis on a surface face up, positions the residual limb in the socket under the Y-strap, and places the opposite arm in the harness. The person then raises both arms above the head, allowing the axilla loop to slide down to the axilla and the harness to be properly positioned across the back and on the shoulders. To remove the prosthesis, the person raises both arms above the head and grasps and removes the prosthesis with the sound arm, while allowing the axilla loop to slide off the arm.58
A person with bilateral amputations dons the prostheses using the sweater method by placing the prostheses on a surface, face up. With the longer limb stabilizing the socket, the shorter residual limb is then positioned under the harness and in the socket. The longer limb is positioned similarly under the harness in the socket, and the arms are raised, allowing the harness to flip over the head and across the back and shoulders. The person removes the prostheses by shrugging the shoulders to bring the harness up, grasping it with one TD, and pulling it over the head, while allowing the residual limbs to come out of their sockets.
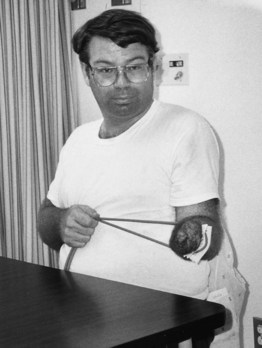
Control Training: Control training may be accomplished in front of a mirror to help the client learn the minimal motions necessary to operate the prosthesis while maintaining proper body mechanics (Figure 43-14).
Acquiring skill in the operation of the prosthesis is emphasized in control training. The therapist educates the wearer on the importance of the practice drills that will ensure more successful function with the prosthesis in daily activities. Joint protection, energy conservation, and work simplification principles and techniques should be stressed during this phase of training. Each prosthetic component should be reviewed separately and understood before the components are combined into functional activities. Such movements as elbow flexion and TD opening are cable operated. Other movements, such as TD or elbow rotation, are passively positioned using the sound hand or an item in the environment. Emphasizing external assists from the environment is an important part of this training process. A client preparing to cut vegetables at the counter may be instructed to use the countertop to rotate the TD in the best position to stabilize the vegetable while the sound hand holds a knife.
Control Training for the Unilateral Trans-Radial Prosthesis:
Terminal Device Control: Scapula abduction and glenohumeral flexion are the motions necessary to open and close the TD. The client is instructed to operate the TD first, by flexing the humerus on the amputated side, then by scapula abduction while the humerus remains at the body’s side. The therapist instructs the client to operate the TD with the arm in various positions in space, such as overhead and leaning over toward the floor.74
Pronation and Supination: If the residual limb is long enough for flexible hinges to be prescribed on the prosthesis, pronation and supination should be practiced. The therapist asks the client to stabilize the elbow at 90 degrees and to pronate and supinate the forearm. If rigid hinges were prescribed, the TD is manually rotated in the wrist unit to achieve pronation and supination. Using the opposite hand or stabilizing the TD between the knees and turning the forearm or shoulder accomplishes manual TD rotation.
Exchanging Terminal Devices: The client learns to exchange the TD in the wrist unit if more than one TD is prescribed. Cable slack is necessary to release the cable from the TD. To obtain enough slack in the cable, it may be necessary to place an item between the fingers of the hook or hand. The TD is then removed according to the specifications of the prescribed wrist unit. When the TD has been removed, another TD style may then be positioned in the wrist unit and the cable attached to it.
To complete control training with a below elbow (BE) prosthesis, the therapist instructs the client to repeat the motions required to position and operate the TD until they are performed in one continuous smooth and natural sequence in both sitting and standing positions.72 Once control training is completed, use training may begin to improve the client’s application of the prosthesis in a variety of the person’s customary daily occupations.
Control Training for the Unilateral Trans-Humeral Prosthesis: Most trans-humeral prostheses operate through the use of a dual-control cable system. When tension is applied on the cable attached to the elbow unit, it locks and unlocks. When the elbow unit is unlocked, tension on the second cable attached to the TD raises the prosthetic forearm (flexes the elbow). A spring assist helps reduce the amount of effort required to raise the forearm, and gravity assists in lowering it. When the elbow unit is locked, tension on the second cable is used to operate the TD. The client learns to operate each component separately.
Internal and External Rotation: Many internally locking elbow units have a manually operated turntable located between the elbow unit and the socket that allows internal and external forearm rotation. The person operates the turntable, first with the elbow at 90 degrees, by manually rotating the forearm medially (toward the body) or laterally (away from the body).
Elbow Flexion and Extension: Flexion and extension of the mechanical elbow are the next steps in the training process. The therapist should protect the client’s face when teaching elbow flexion control. This precaution is important because initially the client may have poor control over elbow flexion, which could cause the TD to hit the face.2
The therapist makes sure that the elbow unit is unlocked. Then the therapist asks the client to flex the humerus slowly and to simultaneously abduct the scapula to accomplish elbow flexion, and to slowly extend the shoulder to achieve elbow extension. This movement is repeated until the client gains sufficient control to accomplish elbow flexion and extension smoothly and easily.2,74
Elbow Locking: The elbow unit operation has an audible two-click cycle. Both clicks must be heard each time the unit is locked or unlocked. The same body movement both locks and unlocks the unit. The client is instructed to operate the elbow unit by moving the shoulder into a combination of hyperextension, abduction, and scapula depression. This movement places tension on the cable that attaches the harness to the elbow unit and may be difficult to master. The reminder “down, out, and away” may be repeated until the client develops a proprioceptive memory. The client is then asked to practice locking and unlocking the elbow in various ranges of elbow flexion and extension (Figure 43-15).2,5,74
Terminal Device Control: The same motions of shoulder flexion and scapula abduction that flex the forearm with the elbow unlocked control the TD when the elbow is locked. The person is instructed to lock the elbow, first at 90 degrees, and to perform the motions to operate the TD. Care must be taken not to unlock the elbow by placing tension on the cable that operates the elbow unit. The sequence of elbow positioning, elbow locking, TD operation, elbow unlocking, elbow repositioning, and locking is repeated at various points in elbow ROM from full extension to full flexion.2,74
The person then learns how to rotate the TD manually in the wrist unit and to exchange TDs in the same manner as described previously for the trans-radial prosthesis. Once the trans-humeral prosthesis controls are performed in a smooth manner, use training begins.
Control Training for the Shoulder Disarticulation Prosthesis: A prosthesis prescribed for a client with a shoulder disarticulation may have different components and methods of operation than those of the trans-humeral prosthesis. The prosthesis may have a manually operated, friction-held shoulder unit that the client pre-positions using the sound arm or a table’s edge. Chin-operated nudge control may be used to operate the elbow unit if the client does not have the shoulder movements needed to lock and unlock the elbow (Figure 43-16). A cable connects the nudge control to the elbow unit. The client still learns the two-click cycle and dual-cable system of operation described previously for the trans-humeral prosthesis. The elbow turntable is also available for a shoulder prosthesis.
A chest harness may be needed to secure the prosthesis on the client. It can also assist TD operation by using chest expansion to increase tension on the TD cable. Shoulder flexion and scapula abduction on the opposite side also assist in TD operation. Wrist operation is the same as explained for the trans-radial prosthesis.
Control Training for Bilateral Prostheses: A client with bilateral amputations usually receives two prostheses that are attached to one harness (Figure 43-17, A). Operating one of the prostheses may transmit tension through the harness to the other prosthesis, causing it to operate also. The client must learn to operate each prosthetic component without affecting the components on either side. This skill is called separation of controls, and the client may need extensive practice to master it. Each prosthesis operates according to the level of amputation, as described in the previous sections, with special attention given to relaxing the opposite side (Figure 43-17, B).
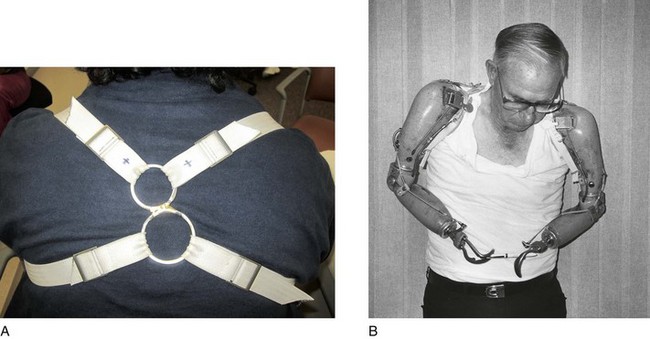
FIGURE 43-17 A, Single harness for bilateral prostheses. B, Passing a pen from one prosthesis to the other to practice separation of controls.
Two components not generally used on unilateral prostheses may be prescribed on bilateral prostheses to improve the client’s functional independence. These components are the wrist flexion unit and a cable-operated wrist rotation unit. The wrist flexion unit assists in the completion of midline activities and is prescribed for both prostheses or for the dominant side. The ability to achieve midline is important for completing activities such as dressing, grooming, and eating. Depressing the unit’s control button and creating tension on the TD cable operate the flexion unit. The opposite TD—a surface edge, the knee, or another surface—can depress the button. The TD cable must be medial to the flexion axis of the unit to pull the TD into flexion. A spring in the flexion unit repositions the TD in extension when the button is depressed and slack is provided in the TD cable.
Wrist rotation may be achieved in several ways. One is by using the wrist units mentioned earlier and rotating the TD by placing it between the knees or by pulling on the thumb of one hook with the other. Another method consists of use of a button on the medial side of the forearm, which controls a cable attached inside the forearm to a wrist-locking device. The wrist is locked and unlocked by pressing the button against the side of the body. When the wrist is unlocked, tension on the TD cable rotates the TD to the desired position.
Use Training: Use training begins after the client understands how to operate and control the prosthetic components. This training applies the mechanics of operation to activities. Repetition is important for the wearer to gain an understanding of how to pre-position the prosthesis and the objects, and how to use the environment to help pre-position them. Along with pre-positioning, prehension training begins.
Pre-positioning: Pre-positioning involves moving the prosthetic units in their optimal position to grasp an object or perform a given activity. All prosthetic components must be pre-positioned in a proximal-to-distal order. Thus, the client with the trans-radial prosthesis rotates the TD into the desired degree of pronation or supination to accomplish an activity. With a trans-humeral prosthesis, the client flexes and locks the elbow and rotates the turntable before pre-positioning the TD. The client with a shoulder disarticulation pre-positions the shoulder unit before the elbow and wrist components. The client with bilateral prostheses must still pre-position all components in the same fashion. The goal of pre-positioning is to allow the person to approach the object or activity as one would with a normal hand or in the most efficient manner and thereby avoid awkward body movements used to compensate for poor pre-positioning.58
Prehension Training: The prosthesis should be regarded as an assistive arm and not as the dominant arm.72 Training objects are used to allow the wearer to practice TD control. The person first should use large, hard objects such as blocks, cans, and jars and progress to soft, then to crushable objects, such as rubber balls, sponges, paper boxes, cones, and paper cups. These objects should be placed in positions that require elbow and TD pre-positioning and TD operation at various heights. The hook TD has a nonmovable and a movable finger. If a hook is used to pick up objects, the person is taught to stabilize the item with the nonmovable finger and then release the tension on the movable finger to secure the object. Prehension training should be completed using all prescribed TDs.72,74
Use Training for Bilateral Prostheses: After the client understands how the components operate, he or she gains control of the prostheses by practicing passing items such as a ruler or a piece of paper back and forth between the TDs without dropping them (see Figure 43-17, B). Another activity that helps the client learn separation of controls is holding an object in one prosthesis without dropping it, while completing an activity with the other prosthesis.
Functional Training: Functional training applies the concepts of control and use of the prosthesis to completion of functional and meaningful activities. The prosthesis wearer is now introduced to completion of specific tasks important to him or her. Prehension training and methods to complete ADLs and IADLs, including vocational, leisure, and driving skills, are addressed in this phase. The key to successful functional training is teaching the client a problem-solving approach with respect to the activity being performed. The person recognizes the altered environment and learns to successfully complete activities within it.
Prehension Training: Prehension training teaches the client to use all prescribed TDs in a meaningful manner, such as using the heavy duty TD with tools and the hand to eat. Items such as a pencil sharpener, lock and key, jar and lid, and bottle opener may be used to allow practice.2,72 In bilateral activities, the person should be encouraged to determine the best position and appropriate use for the prosthesis and their sound arm (Figure 43-18). For details, the therapist is referred to Santschi’s work on prosthetic training.58 Movements become less cognitive and more automatic during this phase, and pre-positioning occurs naturally.
Activities of Daily Living: Functional training should progress to performance of the client’s usual ADLs and IADLs. Activities should be introduced in a simple-to-complex order. Personal care and hygiene activities are performed first. The therapist must understand what activities are important to the client to accomplish. It is not unusual to begin the training process with clients who indicate that there are multiple tasks that they have not tried since their amputation. The client is encouraged assisted to analyze and perform the activities of eating, hygiene and grooming, toileting, dressing, meal preparation, care of pets, shopping, financial management, job performance, play, leisure participation, and community participation as independently as possible (Figure 43-19). Roberto was confident of his goals and was ready to progress with the prosthesis to accomplish them. Frequently, individuals find it difficult to identify what they want to accomplish because of fear that they may not be able to perform adequately with the prosthesis to accomplish their goals. When appropriate, home management skills and child care should be included as part of the client’s training.62 The therapist may help the client analyze and accomplish a task or achieve it by means of using adaptive equipment or by encouraging repetitious practice to reach maximal speed and skill. The sound arm or longer prosthesis should complete most of the work while the opposite side acts as a stabilizer or an assist.72
Adaptation and Problem Solving: No specific manner or technique is required to accomplish most tasks. Each person must learn to approach an activity in a manner that will lead him or her to successful completion. When Roberto was asked to button his trousers, plant seeds in a pot, and clean the floor, he was allowed to approach the task in a manner that made sense to him. The therapist offers guidance and recommendations to enable completion of activities in an efficient manner. Some clients consistently approach activities with the prosthetic arm as the dominant arm and confront limitations in coordination, sensation, and mobilization. With guidance and practice, they can accomplish the activity with their sound arm as the dominant arm and use the prosthesis to assist. Pre-positioning of the prosthesis helps the client complete an activity at a more natural and rapid pace. As previously mentioned, if the client wears the prosthesis often, more practice with daily activities is experienced and the better is the functional outcome. After two or three trials with a grooming activity, the approach to completion becomes automatic and successful.
Work-Related Activities: Prevocational evaluation may be included in the rehabilitation program. The therapist assesses the client’s potential for returning to a former occupation or a possible change of vocation. A visit to the worksite may be necessary to make recommendations that will enable the client to return to work in a safe and efficient environment. It may also be necessary to restrict work activities, such as restricting the amount of weight that the client may lift and carry, or restricting work on ladders. Initially, the client may be able to work only part time, improving work endurance gradually. Training and education for new jobs may be necessary (see Chapter 14).
Social Routines and Community Integration: Incorporating the prosthesis into one’s lifestyle includes being in the community and participating in his or her usual social events. Clients may require encouragement to don the prosthesis when going to the grocery store or taking a walk with their young children. Roberto reported wearing his prosthesis for 90% of his social outings, although many people are uncomfortable wearing the prosthesis out of their immediate home or work setting. Many individuals report that the attention and questioning of other citizens are overwhelming and invasive, and not donning a prosthesis can minimize this attention.
Driver Training: The ability to drive increases independence and may enhance vocational opportunities. The client may be referred to an adaptive driving program, where he or she can be evaluated and trained in using assistive devices such as a driving ring or a steering knob (Figure 43-20). The controls of the car, such as the ignition switch and turn signals, can be modified to improve safety and comfort. The amount of training and the extent of modification will vary, depending on the level of amputation.
The occupational therapist is responsible for assessing predriving skills. A predriving evaluation may consist of an assessment of visual acuity, traffic signal recognition, color vision, glare recovery, night vision, peripheral vision, depth perception, reaction time, and upper extremity (UE) function. When necessary, additional cognitive, visual, and perceptual skills are evaluated. (See Chapter 11 for more information on driving.)
After completing the predriving evaluation, the therapist is responsible for making driving recommendations. These may include treatment for deficits, referral to a driver education center for training, and installation of assistive devices. The therapist’s evaluation should include a statement regarding the client’s potential for safe driving. If the client is unable to drive, alternative methods of transportation should be explored.
In some states, any change in physical health status must be reported to the motor vehicle department and to the person’s insurance company. Failure to do so may result in loss of the individual’s automobile insurance.
Leisure Activities: The rehabilitation program includes information and training regarding leisure interests. With the client’s and the rehabilitation team’s joint effort and motivation, the client should be able to return to a meaningful and productive life. A wide variety of specialized prosthetic devices are available for many sports and recreational hobbies. Texas Assistive Devices and Sports & Recreation Technologies, LLC, provide prosthetic devices designed to improve the wearer’s ability to participate in such activities as photography, ball games, pool, guitar playing, fishing, and skiing.5
Duration of Training: The average adult with a unilateral trans-radial amputation who is otherwise healthy and well adjusted will require approximately 8 hours of training (five to eight treatment sessions) to master control and use of the prosthesis for daily living. The person with a unilateral trans-humeral amputation under the same conditions will require approximately 12 hours of training. About 15 hours will be required for bilateral trans-humeral prosthetic training, whereas about 20 hours is required for bilateral trans-humeral prosthetic training. The initial training session should be about 1 hour long, and subsequent sessions may be shorter, increasing in duration commensurate with the wearer’s increased prosthesis tolerance and physical endurance.5,34,72
Summary
Acquired UE amputations can occur as the result of trauma, infection, neoplasm, and vascular disease. Occupational therapists play an essential role in the rehabilitation process by addressing residual limb conditioning and care, preprosthetic exercise, and prosthetic training. Desired outcomes of occupational therapy include the client’s adaptation to his or her altered body; independent management of ADLs; satisfaction with independent function; and resumption of work, social, and leisure roles that support the client’s health and participation.
Working with a client who has an amputation can be a real challenge. Careful assessment of the client’s needs, a creative approach to therapeutic intervention, an emphasis on problem solving, and close communication with the team can make the challenge rewarding and the outcome successful.
Roberto was able to operate the body-powered prosthesis successfully early in his rehabilitation. He is considered a functional user of a prosthesis, successfully incorporating it into his lifestyle. The state insurance system provided him with the customary body-powered prosthesis, which was also the least expensive type. The therapist documented his successful operation of the prosthesis and explored the advantages and disadvantages of an electric prosthesis with Roberto, in collaboration with the prosthetist. For some clients, the electric prosthesis offers improved control and success with activity completion.
Electric-Powered Prostheses
Externally powered electric upper limb prostheses have opened a new world of freedom and function for persons with upper limb amputations. The advent of electronic microminiaturization has allowed the development of prosthetic devices with totally self-contained services of power, motor units, and electrodes.25 Powered prostheses have existed for decades, but it was not until the 1960s that myoelectrically controlled prostheses were clinically introduced. The activities of the Otto Bock Company in Duderstadt, Germany, began this process by aiming for the development of an electromechanically driven prosthetic hand that would match the technical and cosmetic demands of a human hand.47
Clinical use of the electric devices began in Europe because of government-supported health care systems and a large client population of persons with congenital (post-thalidomide) amputations. By the late 1970s and early 1980s, clinicians in North America had increasing but limited experience with myoelectric prostheses.12 When funding permits, hundreds of myoelectric prostheses are prescribed for children and adults throughout the United States.
The term myoelectric prosthesis is often used interchangeably with electric prosthesis.
A myoelectric prosthesis uses muscle surface electricity to control the prosthetic hand function. The muscle membrane generates an electric potential at the time of contraction. The myoelectric signal is sensed, amplified, and processed by a control unit that generates a motor, which in turn drives a terminal device.12 This terminal device is often an electromechanical hand (Figure 43-21).10 Several different types of myoelectric hands are available. The myoelectric control can be a digital control or a dynamic mode control (proportional control). Digital systems are operated at only one speed, allowing them to turn on or turn off. Proportional control means that the myoelectric signal (power) to the hand is proportionate with the level of muscle signal that the wearer generates, so the wearer’s effort directly controls the speed of the hand.3 A SensorHand (Otto Bock, Minneapolis, MN), which provides automatic grasping when the object in the hand is slipping and its center of gravity is changing, is now available (Figure 43-22). The motor automatically increases pressure applied to the object being held to prevent dropping of the object.
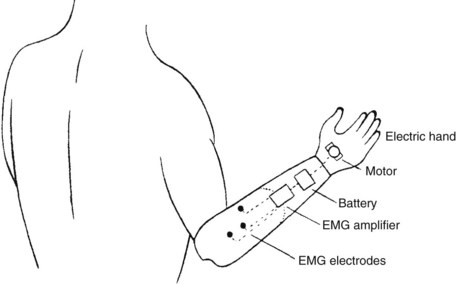
FIGURE 43-21 A typical electric-powered myoelectrically controlled, trans-radial prosthesis with an electromechanical hand terminal device activated by electromyographic potentials. (From Billock JN: Upper limb prosthetic terminal devices: hands versus hooks, Clin Prosthet Orthot 10:59, 1986.)
Myoelectric controls require minimal physical effort for operation. Muscle groups in the forearm are most frequently used according to their physiologic function, that is, the wrist extensor muscles are used for hand opening and the wrist flexor muscles for hand closing. Surface electrodes recessed within the wall of the prosthetic socket (Figure 43-23) detect muscular contractions.

FIGURE 43-23 Surface electrodes, recessed within the wall of the myoelectric socket, detect muscle contractions.
Commercially released in 2009 were two electric hands from Touch Bionics (Hilliard, OH), one of which offers a powered solution to a person with a partial hand amputation.
Candidates for Prostheses
An electric prosthesis might be chosen because of the combination of a natural appearance and the functions of high pinch force without a high level of effort. Also, a myoelectric prosthesis requires no cables for control, so harnessing can be much more comfortable. A suspension socket may be fabricated from material such as silicone, urethane, or thermoplastic elastomers. No liner socks are worn. The client’s work, home, and recreational needs and activities all must be considered. Previous experience with other prostheses may be relevant.
In the past, trans-radial amputation was the most common condition for which these prostheses were prescribed. For amputation levels above the elbow, the complexity of function and the power level required to accomplish functional movement increase considerably. At the same time, the capability of the client to operate a prosthesis by harnessing body movement via straps and cables, in the traditional body-powered manner, decreases considerably.60 More recently, with advances in technology, myoelectric prostheses for persons with higher levels of amputation are increasingly prescribed because their functional possibilities are greater.3
The Utah Arm 3 (Motion Control, Inc., Salt Lake City, UT), released in 2004, introduced microprocessor technology into the prosthetic arm with a computer interface that allows the prosthetist to fine-tune adjustments to maximize the wearer’s performance. It offers simultaneous elbow and hand control because it has two microprocessors. Roberto may experience common difficulties in unlocking the elbow unit efficiently or in operating the TD with the same control quality of the elbow unit, which individuals with trans-humeral amputations frequently experience using an electric prosthesis. This design minimizes the effort of elbow and hand control and may be appropriate for Roberto.
The task of training a client with a very short trans-humeral amputation or shoulder disarticulation to function with a body-powered prosthesis is substantially more challenging than training with an electric-powered prosthesis.
Before a myoelectric prosthesis is prescribed, the client should have adequate strength and the ability to contract muscles independently. A minimum muscle signal of 5 microvolts will operate the most sensitive system. The candidate with this minimum signal should be capable of developing stronger signals for longer-term use of the prosthesis. Independent contraction of each muscle is important to produce smooth and controllable prosthetic function. As a general guideline, the prosthesis can be operated with a 10-microvolt difference between muscles, but the wearer will use the prosthesis more easily if a 20- to 30-microvolt difference can be controlled. Surface electric signals are amplified by a miniature electrode and are led to the relay system. The relay is responsible for the energy supply to the battery-operated motor in the electric hand. When alternating contractions of extensor and flexor muscles take place, the direction of the current changes in the electric motor, and the hand opens and closes accordingly.47
Some rehabilitation professionals who work with clients who have upper limb amputations believe that electric components may be the only appropriate alternative for high-level unilateral or high-level bilateral amputations. Conversely, some rehabilitation professionals believe that body-powered prostheses are the most functional and appropriate type of prosthesis for most clients, despite the level of amputation. There are many schools of thought regarding the advantages and disadvantages of myoelectric prostheses. Box 43-2 describes some of the points that differentiate the myoelectric prosthesis from a body-powered, cable-controlled, hook-type TD prosthesis.
Hybrid Prostheses
A hybrid prosthesis is one that combines body power with electrical power. These designs have been created and used more and more over the past several years. Hybrid prostheses, using various components and control methods from various systems, in many cases can serve as a prosthesis that is more functional and more acceptable to the individual.10 The improved technology of electric hands has increased the cost of myoelectric prostheses. The hybrid design decreases the overall cost of the prosthesis. Some hybrid designs eliminate the cable and harness, thereby eliminating pressure on the sound side when the prosthesis is operated. One hybrid design involves the use of a body-powered elbow flexion device with a myoelectric hand.10 Another configuration might be the use of a cable elbow and hook TD with an electric wrist rotator. For a person with bilateral amputations, a powered elbow combined with a cable-hook TD offers quick elbow motion and less overall bulk of the prosthesis and dedicates all excursion of the cable to the TD. A hybrid design can decrease the overall weight of a prosthesis. It can be less expensive and less complex. All excursion of the existing cable is dedicated to one component, as opposed to multiple components. This feature requires less overall force on the part of the wearer for operating the prosthesis.
Preprosthetic Therapy
Awareness of postoperative and subsequent preprosthetic principles of care is crucial for the successful management of the client who has sustained traumatic limb loss.
The rehabilitation team, which ideally includes the physician, nurse, occupational therapist, physical therapist, social worker, vocational counselor, insurance representative, and client, addresses goals described in the first section of this chapter. With an electric prosthesis, additional treatment goals are as follows:
• Identify or test potential muscle sites for prosthesis control.
• Improve muscle site control and strength (once identified).
• Obtain adequate financial sponsorship for the prosthesis and training.42
Identify Potential Muscle Sites: A myoelectric prosthesis functions by detecting electromyographic (EMG) signals produced by muscles. Locating appropriate superficial muscle sites is the most important aspect of the successful operation of a myoelectric prosthesis. Physical examination of a person’s arm often reveals sufficient strength in natural agonist-antagonist pairs, such as the wrist extensor and wrist flexor muscles in the person with a trans-radial amputation, and the biceps and triceps muscles in the person with a trans-humeral amputation. Individuals with a short trans-humeral amputation often have an effective pectoralis or deltoid site anteriorly and an infraspinatus or trapezius site posteriorly. It is more difficult to identify proximal muscle sites that are adequate in signal and allow the prosthetist to position electrodes within the socket and hold them securely against the skin. On occasion, trauma or nerve injuries do not allow the choice of a natural pair. If a particular site could cause tissue breakdown under the pressure of an electrode, it must be avoided. Often, healed skin or muscle grafts can tolerate the pressure well. Consult the physician when dealing with repaired tissue. If the best muscle site contractions are weak during the physical examination, the therapist and prosthetist will require a biofeedback system or myotester to identify the amount of signal generated by the muscle (Figure 43-24). When surface potentials are measured with electrodes and a myotester, it is important that all electrodes have good contact with the skin and that they are aligned along the general direction of muscle fibers. Moistening the skin slightly with water may improve the EMG signal by lowering skin resistance. EMG testing begins with the most distal portion of the remnant muscle.
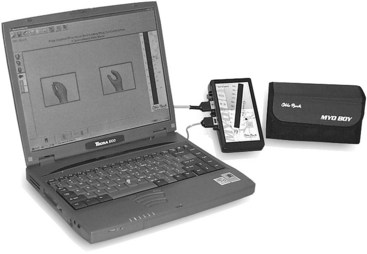
FIGURE 43-24 Otto Bock MyoBoy system used to determine the magnitude of muscle contraction. (Courtesy Otto Bock HealthCare, Minneapolis, MN.)
The goal of this testing is to identify two muscle sites that would fit appropriately within the socket with the greatest microvolt difference between them, not necessarily the two strongest muscle site signals. Selection can be considered complete when the client can tolerate a 1-hour training session with the biofeedback system and is consistently generating sufficient signals to operate a prosthesis in basic functions such as opening and closing of the TD. The therapist should check with the prosthetist for the minimum signal required for operating the myoelectric system chosen for the client.48
Muscle Site Control Training: The more proximal the level of the client’s amputation, the more challenging it is for the prosthetist to fit the prosthesis and for the therapist to train the person to function with the prosthesis. For the client to understand a desired muscle contraction, the therapist instructs the client to imitate the desired contraction or movement with both arms. The therapist should ask the client to raise the sound hand at the wrist (wrist extension) and imagine this motion with the phantom hand on the amputated side (Figure 43-25). The therapist often can palpate the wrist flexors and extensors on the residual limb during this exercise. The person is instructed to contract and relax each muscle group separately and on command. For this step, a myotester is particularly useful because it indicates the magnitude of the EMG signal as the client contracts the muscle, as well as the decrease in signal as the client relaxes the muscle. Many clients have difficulty relaxing a muscle completely; this causes a decrease in muscle signal separation.
The myotester can be used to train the muscles with both visual and auditory feedback. Various models are available to therapists (Figure 43-26). The goals of training at this point are to increase muscle strength and to isolate muscle contractions. As confidence and accuracy improve, visual or auditory feedback should be removed. Practicing muscle contractions without feedback teaches the client to internalize the feeling of each control movement. The advantage of creating this internalized awareness of proper muscle control is that control and strengthening practice can be continued between treatment sessions without feedback equipment.66 The therapist must learn to recognize muscle fatigue, which is frequently a side effect in this process, and must allow sufficient time for that muscle to recover during the treatment session.
Ideally, the client with an amputation receives adequate training and practice in initiating these muscle contractions before receiving the completed myoelectric prosthesis from the prosthetist. Prosthetists commonly engage a client in muscle site training with the preparatory socket and prosthesis fitting. This training, which usually occurs as prosthetists strive for optimal electrode placement and socket fit, is not adequate for most clients to immediately and successfully operate a prosthesis. Anxiety and frustration often accompany training in use of a myoelectric prosthesis, and a team approach to training by the therapist and the prosthetist can minimize these responses. The client’s success and effectiveness in using the prosthesis are closely related to the quality of the preprosthetic training.
Prosthetic Program
Orientation in what the prosthesis realistically can and cannot do is an important aspect of a prosthetic training program. If clients harbor unrealistic expectations about the usefulness of the prosthesis as a replacement arm, they may become dissatisfied with the ultimate functioning of the prosthesis and reject it altogether. It is imperative that the therapist be honest and positive about the function of the prosthesis. If the client understands the functional potential and limitations of the prosthesis, success can be more realistically achieved.4
Orientation and Education: Training with a prosthesis should begin as soon as the prosthesis is received, preferably the same day. The textbook Comprehensive Management of the Upper Limb Amputee is an excellent resource in the training process of a client with a myoelectric prosthesis.6 Prosthesis component manufacturers provide written training information and/or educational courses for therapists.
Important areas to review during initial visits are orientation to prosthesis terminology and operation, independence in donning and doffing the prosthesis, orientation to a prosthesis-wearing schedule, and care of the residual limb and prosthesis.
Orientation to Prosthesis Terminology: Given that the prosthesis is a natural extension of the person’s body, it is particularly important to know the functions and names of its major parts, such as electrodes, battery, glove, and electric hand. The initial visit is an appropriate time to review the battery-charging procedure with the wearer.
Batteries are energy-storing devices, and most are rechargeable. Some control systems use a 9-volt disposable battery. The prosthetist supplying the prosthesis will instruct the client on proper installation and recharging. Rechargers are plugged into a standard electrical outlet. Most manufacturers’ rechargers have some type of indicator, which alerts the person when the battery is fully charged. Some rechargers require 12 hours of charging time, whereas others may take as long as 24 hours. A fast charger, which requires only 1 or 2 hours of charging time, may be available. For best results, the batteries should be close to completely drained before recharging. The prosthesis will begin to operate more slowly when the battery is low, and some unexpected control problems could occur. Therefore, the first troubleshooting step is always to make certain that the battery is charged, or a different one must be installed.48
Although the myoelectric hand is the most commonly prescribed electric terminal device, a specially designed gripping device, the Greifer, is frequently recommended. Designed by the Otto Bock Company, the Greifer is a universal working tool designed to handle various specialized tasks. It can be used for heavy work in industry or farming and in mechanical activities at work or home because it allows for quick handling and precise manipulation of small objects. Features of the Greifer include a 38-lb grasp, as well as parallel gripping surfaces and a manually controlled flexion joint for wrist dorsal and volar flexion (Figure 43-27).47

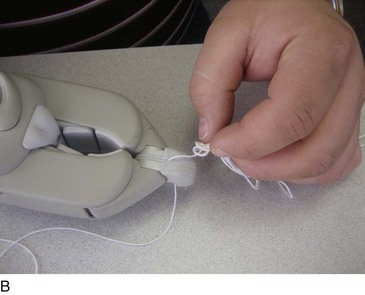
FIGURE 43-27 A, The myoelectric Greifer is designed as a universal working tool with parallel gripping force of up to 38 pounds. B, i-LIMB electric hand allows power to individual digits for fine motor tasks.
Instruction manuals from the manufacturer for the battery charger and the prosthesis are often provided for the wearer’s reference. These are excellent tools for the occupational therapist to use for review and education.
Independence in Donning and Doffing the Prosthesis: The client should be able to put on and remove the prosthesis independently. With proper instruction and the help of the prosthetist in suspension design, the wearer will be successful. Donning the prosthesis should be performed with the electronic components in the off position to prevent any uncontrolled movements. A client with a long trans-radial amputation usually has the advantage of not requiring a harness because a supracondylar suspension at the elbow may be used. The wearer can place his or her residual limb directly into the socket. A pull sock is sometimes used to facilitate an intimate interface between the arm and the radial socket for a person with a short trans-radial amputation. A silicone-based skin lotion applied to the skin before donning the pull sock enables the person to remove the pull sock with less effort.
Suspension designs for the client with a trans-humeral amputation may require a pull sock for donning the prosthesis. The sock is applied to the residual limb, and the prosthesis socket is pulled over it. A weighted cord from the pull sock is fed through a hole in the bottom of the socket. The wearer then pulls the sock off the arm and through the hole in the socket, creating very close contact of the prosthesis with the limb. This is a successful application, particularly for a very short residual limb. The wearer must be sure not to start with the stocking too high on the residual limb because this will increase friction during pulling and make it harder to pull the sock out of the bottom of the socket. It may be necessary to experiment with different sock materials, powder on the skin, and various donning techniques until the most successful materials and techniques are identified.
Good electrical contact is achieved after approximately 1 minute of donning. A wearer can moisten the skin at the electrode sites to eliminate the waiting period for skin warmth to occur. The prosthetic arm should be stored in the off position with the batteries removed. The hand should be fully opened when stored to keep the thumb web space stretched.
Prosthesis-Wearing Schedule: Initial wearing periods are no longer than 15 to 30 minutes. This limit is particularly important if scarring or insensate areas are present on the residual limb. If redness persists for longer than 20 minutes in a particular area after removal of the prosthesis, the wearer should return the prosthesis to the prosthetist for adjustments. If no skin problems exist, wearing periods can be increased in 30-minute increments two to three times a day. Some individuals have difficulty tolerating the weight of the prosthesis or the heat generated by its application. Full-time wearing should be achieved as soon as possible, which may occur as soon as 1 week later.
Care of the Residual Limb and Prosthesis: Appropriate care of the skin is vitally important. The residual limb should be washed daily with mild soap and lukewarm water. It should be rinsed thoroughly and dried thoroughly.
The prosthesis may be cleaned with soap and water by using a damp cloth. Rubbing alcohol may be used to clean the inside of the socket to prevent and minimize odors. The cosmetic glove stains easily; special care must be taken to avoid contact with ink, newsprint, mustard, carrots, grease, and dirt. Wiping with soap and water or a glove-cleansing cream obtained from the prosthetist will remove general soil but not stains. The average life of a glove is approximately 6 months. Polyvinylchloride (PVC) plastic gloves are the least expensive, most flexible, and toughest. Silicone gloves are being used more frequently because the new silicone formulas are tougher and less susceptible to the yellowing and brittleness that previously set in with age; they also allow the greatest cosmesis.10 The prosthesis itself should never be immersed in water because this will seriously damage the internal electronic components. Additionally, it is important to advise myoelectric wearers against excess vibration, sand, dirt, and extremes of heat and cold. These, too, can seriously impair the electronic components.
The prosthesis should be checked occasionally for loose screws and harness attachments, and these should be brought to the attention of the prosthetist. The covers of the prosthesis should not be opened unless the prosthetist instructs the wearer or therapist to do so.
Control Training: The first function to master is opening and closing of the TD. With practice, the wearer understands the muscle contractions required to perform these actions. Each electric prosthesis has a unique control system based on the manufactured componentry and/or the person’s musculoskeletal integrity. Fewer similarities in fit and control are noted with electric prostheses as compared with body-powered prostheses, and therapists modify training guidelines and sessions to address each individual’s needs. Simple opening and closing of the terminal device are practiced. The muscles should contract as independently as possible. Next, the client practices opening the hand halfway, then stopping and relaxing so the hand does not move. This is practiced in various positions of the arm. If a proportional control system is used, the client can also practice opening and closing quickly and slowly. Often, the therapist will design a home program of specific patterns of terminal device action that the person performs, to offer more practice. Control of the TD will improve in accuracy and speed with practice and use throughout the other phases of training.
Use Training: The repetitive grasp and release of objects is introduced after control training. These activities are considered preparatory in that they prepare the person for functional activity. Simple approach, grasp, and release activities are practiced with objects of various shapes, sizes, and densities. Objects that may be presented include paper or plastic cups, blocks, cubes of sponge, empty plastic containers, small weights, large bolts, empty glass jars of various sizes, and ping-pong balls. It is important for the individual first to visualize how the object should be approached and grasped, then to pre-position the myoelectric hand. Pre-positioning involves placing the TD in the optimal position to approach an object. In approaching a glass, the hand should face in toward the midline to grasp the glass as a normal hand would (Figure 43-28). The fingers of the hand should not be positioned downward because a normal hand does not approach a glass in this position.

FIGURE 43-28 When approaching the glass, the hand is pre-positioned in midline to grasp the glass as a normal hand.
Another important goal of training a client to grasp an object is mastering pressure control or the gripping force of the TD. This skill involves close visual attention to appropriately grade the muscle contraction for a specific result in the myoelectric hand. The client must learn how to pick up the object without crushing it. Too strong a grasp crushes the object being held (Figure 43-29). Good grasp control through training with foam, cotton balls, or wet sponges will help the client develop the control necessary to handle paper cups, vegetables, boxes, lotion bottles, and sandwiches or even to hold someone’s hand.66

FIGURE 43-29 Person with transhumeral amputation demonstrates how excessive grasp crushes the object (plastic cup) being held.
Working on approach, grasp, and release in multiple arm positions then follows. The client will attempt to grasp objects at counter height, at table height, overhead, on the floor, at cupboard height, alongside the body, and behind the body. The client with a trans-humeral amputation who uses a body-powered or electric elbow should ensure that the position of the terminal hand and the angle of elbow flexion are appropriate to complete the grasp in a natural manner. Often, the client automatically adjusts the body using compensatory body motions (e.g., bending forward rather than adjusting the elbow position or pre-positioning the hand). It is important to discourage this adjustment because it looks unnatural, becomes habitual, and may lead to secondary musculoskeletal problems in the neck, shoulder, or trunk. A mirror can help clients see the way their bodies are positioned and visualize how their sound arms would approach a particular object or activity. The therapist often must remind the client to maintain an upright posture and to avoid extraneous body movements.
Release is accomplished by visualizing a wrist extension contraction or a quick “hand up” or “fingers open” in the person with a trans-radial amputation. This response should become automatic if good preprosthetic training of the muscles has been provided.
The ability to perform specific movements will eventually take less conscious effort, and movements will become automatic. The wearer now has muscle endurance and prosthesis tolerance sufficient for 1-hour therapy sessions. Next, functional activities are introduced into the therapy program.
Functional Training: Now the person transfers prosthesis control into purposeful activities. The prosthesis is used as a functional assist in most bilateral activities. Therefore, most functional activities are accomplished with the uninvolved arm and hand as dominant. Other than perhaps for practice, it is not appropriate to train a person with a unilateral amputation to eat holding a spoon, to write, or to brush his or her teeth using the myoelectric hand. In almost all cases, the sound hand becomes the dominant extremity and performs these tasks. Occasionally, if the right arm was dominant and is amputated, and if the client was fitted with a myoelectric hand in a timely manner, he or she may prefer to use the myoelectric hand for some of these activities. The critically important component of sensory feedback is often the determining factor in deciding which hand to use. A client with an amputation almost always chooses to perform activities with a hand that has feeling. A myoelectric hand lacks this distal sensory feedback. Feedback is provided more proximally through the action of muscle contraction, yet responding to this stimulus is difficult for the wearer.
The therapist will review a list of bilateral ADLs with the client to determine which tasks are most important for him or her to accomplish. The therapist will focus on these purposeful and occupation-based activities during training, stressing throughout that the myoelectric TD is used as an assist and a stabilizer (Figure 43-30). If unilateral tasks are presented to the client, his or her need to operate the prosthesis is minimized or absent. These tasks should be avoided for the purpose of training. The bilateral activities listed in Table 43-2 are good examples for practice.
TABLE 43-2
Roles of Myoelectric Hand and Sound Hand in Bilateral Activities of Daily Living
| Activity | Myoelectric Hand | Sound Hand |
| Cutting meat | Hold the fork with prongs facing downward; hold the knife as grip strength increases. | Hold knife. Hold fork. |
| Opening a jar (see Figure 43-29, A) | Hold the jar. | Turn the lid. |
| Opening a tube of toothpaste | Hold the tube. | Turn the cap. |
| Stirring something in a bowl | Hold the bowl with a strong grip. | Hold the mixing spoon or fork. |
| Cutting fruit or vegetables (see Figure 43-29, B) | Hold the fruit or vegetable firmly. | Hold the knife to cut. |
| Using scissors to cut paper | Hold the paper to be cut. | Use scissors in normal fashion. |
| Buckling a belt | Hold the buckle end of belt to keep stable. | Manipulate long end of belt into buckle. |
| Zipping a jacket from bottom up | Hold anchor tab. | Manipulate pull tab at base, and pull upward. |
| Applying socks | Hold one side of socks. | Hold other side of socks, and pull upward. |
| Opening an umbrella (see Figure 43-29, C) | Hold base knob of umbrella. | Open as normal. |

FIGURE 43-30 Activities of daily living. A, Opening a jar is accomplished with the myoelectric hand holding the jar and the sound hand turning the lid. B, Cutting an apple is accomplished with the myoelectric hand holding the apple while the sound hand holds the knife to cut. C, Opening an umbrella is accomplished by holding the base knob of the umbrella with the myoelectric hand and using the sound hand to open as normal.
With repetition, these activities and many others will become easier to perform, occurring almost automatically. It is important to reinforce and emphasize the fact that bathing, grooming, and hygiene skills involving water must be done without a myoelectric TD or with a myoelectric TD that is water resistant, because of the damaging effects of water on the electric motor and battery.
Vocational and Leisure Activities: As training proceeds and a sense of the person’s self-acceptance and comfort with the amputation is heightened, the therapist will address the subject of return to work. Ideally, the therapist makes an on-site visit. If possible, the various job requirements can be discussed and then practiced in a simulated, step-by-step process during a therapy session. If changes and adjustments to the work environment are necessary, the therapist will advise regarding these modifications. This intervention can often be enhanced by collaboration with the vocational counselor. In Roberto’s case, the occupational therapist was instrumental in describing to the counselor what skills and abilities were safe and reasonable to attempt with body-powered and electric prostheses. This improves the match of the individual to the occupation identified. (See Chapters 14 and 15 for additional information.)
Leisure and recreational occupations are also critically important to discuss at this time because these activities contribute not only to physical well-being but also to psychological well-being. The TDs used for sports and recreational activities are not generally myoelectric. If the activity is something that requires fine motor skills, an electric TD may be beneficial. The author worked with an individual with bilateral limb amputations who was fitted with bilateral electric prostheses and who was able to successfully resume his fly-tying business. As discussed in the first section of this chapter, Sports and Recreation Technologies, LLC, offers a number of excellent TD adaptation components, including an Amputee Golf Grip (Figure 43-31, A) and a Super Sports TD (Figure 43-31, B). Clients are encouraged to continue engagement in any recreational activities that they performed before the loss of their limb (see Chapter 16 for additional information).
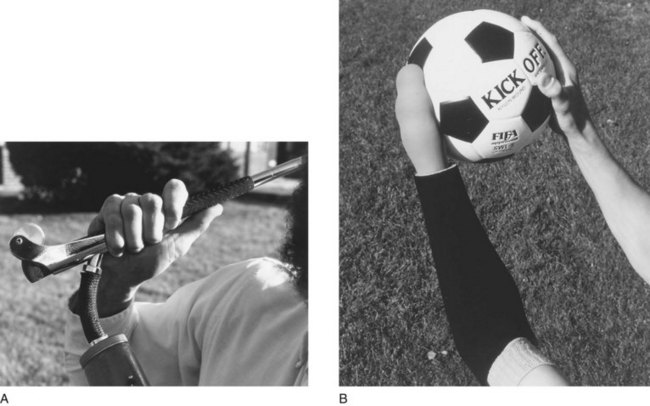
FIGURE 43-31 TD adaptation components. A, Amputee Golf Grip is a high-performance prosthetic golf accessory that allows smooth swings and complete follow-through. B, Super Sports terminal device is a highly flexible, strong, prosthetic sports accessory for volleyball, soccer, football, floor exercise gymnastics, or any activity in which shock absorption, safety, and bilateral control are important.
Self-management Instruction: During training and the review that takes place at the conclusion of training, information regarding a wearing schedule, care instructions, and additional tasks to practice should be shared with the wearer and his or her family members. A follow-up appointment should be made at this time, and a list of the rehabilitation team members and their telephone numbers provided, so the client may contact the appropriate person when problems arise.
Summary
The rehabilitation process for clients with upper limb loss can be challenging and rewarding. In the case of a trans-humeral amputation, shoulder disarticulation amputation, or bilateral limb loss, training and expertise on the part of the therapist are essential. The therapist can review several resources to enhance his or her knowledge in this area of occupational therapy intervention.
The potential of individuals with upper limb loss is limitless; they often are able to accomplish activities that no one ever would have predicted. The success of rehabilitation does not rest solely on the quality of training in use of the prosthesis. Rather, success depends on such complex factors as the quality of medical management, the type and fit of the prosthesis, client factors, performance skills and patterns, and the client’s interest in learning to use the prosthesis, as well as conscientious follow-up once the rehabilitation phase is complete. Follow-up is critically important and is often overlooked.
Perhaps the most important aspect of a successful rehabilitation program is the client’s desire to become more independent. All team members should cultivate and reinforce this desire, which is a pivotal ingredient of successful intervention. The effectiveness of the occupational therapist during this important process will remain with the client for life.
Section 3: Lower Limb Amputations
Levels of Lower Limb Amputation
Lower limb (LL) amputations are typically discussed as above-knee or below-knee; however, variability exists even within these categories (Figure 43-32). Generally, the more proximal an amputation is, the greater is the functional challenge presented to the person with the amputation. Proximal LL amputations include hemipelvectomy and hip disarticulation amputations, resulting in loss of the entire lower limb; such severe amputations are typically performed in cases of trauma or malignancy. Wound healing from such proximal amputations is often slow, and skin grafting may be required for full healing. In cases of hemipelvectomy, a muscle flap will cover the internal organs.
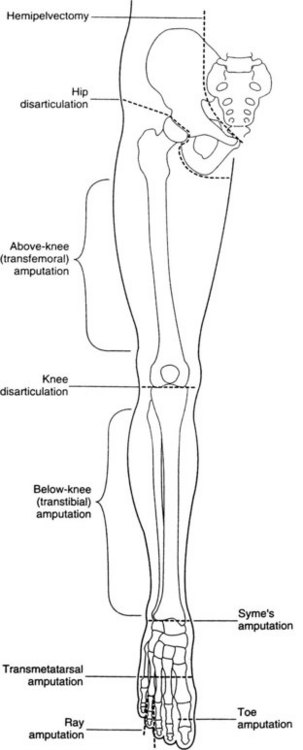
FIGURE 43-32 Levels of lower extremity amputation. (From Paz JC, West MP: Acute care handbook for physical therapists, ed 2, Oxford, 2002, Butterworth-Heinemann.)
A transfemoral or above-knee amputation (AKA) results in loss of the knee and everything distal to it. Residual limb length from an AKA typically varies from 10 to 12 inches (5.4 to 30.5 cm) from the greater trochanter7; transfemoral amputations can also be classified as upper, middle, or lower third, indicating the amputation distance from the ischium. A through-the-knee (disarticulation) amputation does result in loss of knee joint function, but it allows a high level of prosthesis control and mobility.
A transtibial or below-knee amputation (BKA) preserves the knee and thus eliminates the necessity for a mechanical knee joint in the prosthesis. The residual limb from a BKA typically varies from 4 to 6 inches (10.1 to 15.2 cm) in length from the tibial plateau.7 A Syme’s amputation, or ankle disarticulation, results in loss of both ankle and foot function and is typically performed in cases of trauma or infection. A transmetatarsal amputation results in severing the foot through the metatarsal bones, but the ankle remains intact. Clients may experience amputation of toes; although amputation of the first toe impairs ambulation by preventing toe-off (which is the end of the stance or support phase of gait), loss of the small toes does not usually result in impaired ambulation. In Lena’s case, the amputation is considered a BKA because her left leg was amputated approximately 5 inches below the tibial plateau.
Causes of Lower Limb Amputation
In the United States, 95% of LL amputations are performed as a result of complications of PVD26; ultimately, 25% to 50% of these cases are due to diabetes mellitus.54 Trauma is the second most common cause of amputation in the United States, but it is the leading cause in developing countries because of land mines and other environmental hazards.54 Amputation may also be performed in cases of malignancy in an effort to prevent it from spreading to other sites or systems in the body.
In Lena’s case, diabetes mellitus and PVD resulted in poor circulation in her LLs. Because of this complication, blood flow to her left foot and leg was not adequate for her limb to heal, even from what initially appeared to be a small wound. Therefore, she was obliged to undergo progressive amputations of her left LL, eventually leading to her recent BKA.
Postsurgery Residual Limb Care
Skin care and positioning are extremely important throughout the course of rehabilitation, especially immediately after surgery. Once the surgical wound has begun to heal, some form of specialized postsurgical dressing will be used to help prevent swelling and to shape the residual limb for ease of future prosthesis use. Wrapping with an elastic bandage, such as an Ace wrap, is a common method to control edema after surgery. However, smooth wrapping does require skilled and consistent technique, which is necessary to prevent poor shaping of the residual limb. A series of gradually smaller residual limb shrinkers can be worn as an alternative to elastic bandage wrapping, to encourage constant, even shrinkage of the residual limb for fit with a final prosthesis. Both elastic bandages and shrinkers can be used early after surgery, even if the client’s surgical wound still has a dressing on it. In such a case, a nylon stocking would first be applied to prevent the bandage or shrinker from dislodging the dressing. Once the final prosthesis is made and adjusted, the client frequently will continue to wear a shrinker during the day when he or she is not wearing the prosthesis, as well as at night. This shrinking and shaping process can take up to 3 months or longer in some cases, depending on the client’s condition.
If the client (or his or her caregiver) is unable to demonstrate proper technique with wrapping or shrinker use, a Jobst compression pump may be used. The pump is an air-filled sleeve that surrounds the residual limb, placing constant, equal pressure on all sides, quickly shrinking and shaping the residual limb. A rigid dressing, or cast, is frequently used for active clients after surgery. The end of the cast is made to work with a simple training prosthesis, so the client can begin training for standing and walking immediately. Scar massage may be necessary later in the healing to prevent adhesions and enhance comfort around the surgical site; this massage technique can be taught to the client. The Ace wrap bandaging of Lena’s residual limb was performed by nurses in the hospital. After Lena’s arrival at the skilled nursing facility, the nursing staff consulted the occupational therapist to determine whether Lena had the cognitive and visual function, as well as the necessary motor skills, to learn how to apply her own wrap or shrinker and to perform her own scar massage.
Lower Limb Equipment and Prostheses
Movement and time out of bed are typically reduced immediately after LL amputation. The surgery itself can make movement uncomfortable, and many persons who have undergone amputation surgery have preexisting conditions that may further reduce mobility. For these reasons, clients may require the use of bed rails or a metal trapeze bar hanging over the bed to help reposition themselves in bed and to transition between supine and sitting. Wheelchairs also present a challenge because the client is no longer able to support the affected limb by resting the now absent foot on the floor or on the footrest of the wheelchair. A residual limb support is basically a padded board that is placed on the seat of the wheelchair; it has an extended component on the side of the affected limb that projects forward from the seat of the chair (Figure 43-33). This extension provides a surface for the residual limb to rest upon, thus placing the limb in a nondependent position and reducing stresses placed on the hip joint. A person with a BKA is often at risk for developing a flexion contracture of the knee joint, and residual limb support can facilitate extension of the knee in sitting, thus helping to prevent both edema in the residual limb and contracture of the knee joint.73 A residual limb support is sometimes still referred to, in less acceptable terminology, as a stump support. For a person with bilateral LL amputations, the large wheels on the wheelchair must be placed farther back to accommodate the change in body weight distribution. Antitippers, commercially available wheelchair accessories, can also be used on the back of the chair to reduce the likelihood of tipping backward during weight shifting.
Most clients will use a walker during at least the initial phases of their rehabilitation. Some clients with LL amputations will go on to use a walker at all times for ambulation. Both four-footed (standard) and two-wheeled (rolling) walkers may be used, depending on the client’s individual characteristics and needs. It has been suggested that using a two-wheeled walker may allow those with prosthetic limbs to ambulate more quickly and with less interruption,69 but walker choice should always be made on the basis of a total assessment of the client’s abilities and needs.
Many types of prostheses are available for the LL, and technology is improving daily. For all prostheses, comfort, ease of application, appearance, and function of a prosthesis, including the client’s ability to perform ADLs and IADLs with use of the affected limb, correlate significantly with the client’s walking distance and with his or her perceived quality of life after an LL amputation.40 It is very important for the rehabilitation team to keep this in mind during a client’s fitting for and training with a prosthesis.
The main components of an LL prosthesis are the socket, a sock or gel liner, a suspension system, a pylon, and a terminal device. For some prostheses, an articulating joint is also necessary. The socket is the direct connection between the residual limb and the prosthesis. A person’s residual limb may change in volume during the day and over the course of time, presenting challenges for maintaining an adequate fit within the socket. This challenge is frequently addressed by adding to, or removing socks from, the residual limb to adapt to its volume changes. Smart variable geometry socket (SVGS) technology was developed to help reduce this challenge.21 SVGS adds and removes liquid from the intrasocket environment on the basis of intrasocket pressure during wear, continuously accommodating for residual limb volume changes and thus maintaining the fit of the socket without having to remove the prosthesis. Static elastomeric liners are also used for the prosthesis socket; the choice of liner is based on variables such as fit, comfort, friction tolerance, and price.57 Various suspension mechanisms are used to attach the socket to the residual limb, including belts, straps, wedges, or suction; sometimes mechanisms are combined to ensure appropriate fit.
The pylon is the structure that attaches the socket to the TD (Figure 43-34). Vertical shock pylons function as shock absorbers for LL prostheses. Many clients who have had an LL amputation express a preference for walking with these devices.19 Such shock absorption is especially beneficial during high-impact activities, such as running, and for other activities that are part of daily life for many clients, such as descending curbs and stairs. A pylon can be a basic, static device that provides minimal cosmetic benefits; it can also be a dynamic device, such as that outlined in the preceding paragraph, and can be modified to provide a close cosmetic match with the client’s unaffected limb.
The TD is the prosthetic foot, which provides a stable weight-bearing surface and can itself function as a shock absorber. The many types of available TDs provide varying degrees of mechanical ankle movement and dynamic response, according to the needs and abilities of the client. Specialized TDs—indeed, entire LL prostheses—are designed to accommodate the challenges presented by various sports and activities (Figure 43-35). To help select the best prosthesis, Lena’s prosthetist consulted with her occupational therapist to explore the activities and lifestyle to which Lena wished to return.
Participation in Areas of Occupation
For some clients, particularly those who underwent a traumatic amputation, the activities to which they wish to return are ones that they engaged in right up to the point of injury or illness. However, given the nature of PVD and diabetes, many clients with LL amputations experience a progressive decline in function over the course of several years. For these clients, amputation and subsequent rehabilitation, although difficult, may allow a return to fulfilling occupations that had been absent from the clients’ repertoire for quite some time.
Participation in most ADLs will be affected by LL amputation. Although a client with an LL amputation will be learning new mobility techniques in physical therapy, he or she must also participate in occupational therapy to learn new functional mobility techniques with which to accomplish familiar tasks. Bathing, dressing, personal hygiene, grooming, and toilet hygiene will likely need to be addressed as part of an occupational therapy intervention program. Personal device care must be addressed if the client is using an LL prosthesis. Participation in IADLs will also be affected. Particular attention should be paid to care of others, care of pets, child rearing, community mobility, health management and maintenance, home establishment and management, meal preparation and cleanup, safety and emergency maintenance, and shopping. The areas of rest and sleep may also present challenges to a person with a new LL amputation. For example, one’s evening routine may be disrupted by having to perform it from a wheelchair instead of at an ambulatory level (sleep preparation). A client may experience difficulties interacting with his or her spouse in the sleeping space as they both adjust to a new amputation (sleep participation). The occupational therapist should assess how these areas of occupation may be impacted by the amputation, and should help the client develop adaptations that facilitate improved rest and sleep. Treatments addressing phantom sensations may also benefit the client’s rest and sleep. (See Chapter 13 for further information.)
Participation in educational, work, play, and leisure activities is usually affected by LL amputation and should be addressed during occupational therapy, as should social participation. Although intervention often assumes a greater role with these areas of occupation later in the rehabilitation process, they still can be addressed even during the acute rehabilitation phase, thus reinforcing to the client that these are areas of occupation in which a return to active participation is indeed possible. It is essential that the occupational therapist help clients to explore all avenues of an occupation in which they may wish to participate, ensuring that even activities that had been abandoned in the past are possible again.33 As a result of changes in function after amputation, clients may not be able to return to participation in prior work or leisure activities or to participation at the level to which they were accustomed. In such cases, the occupational therapist should help clients explore other opportunities that they might find fulfilling through identification of interests, skills, and opportunities.
Early in her course of occupational therapy at the skilled nursing facility, Lena spoke with her therapist about how much she missed walking to her church and helping to bake pies for its annual autumn festival. Lena said that she stopped doing this about 10 years ago because it became so difficult; she then discussed feelings of isolation and uselessness. Lena said that she had been known throughout her town for her pies, and she proudly recounted how each year people would tell her that she should open her own restaurant. Although Lena and her occupational therapist had initially set her long-term goals for independence with self-care and basic home management, they decided to add a goal for community re-entry that focused on being able to re-engage in this occupation.
Client Factors
Structures related to movement, as well as skin and related structures, are always altered by an LL amputation. The status of other body structures must also be assessed, however, to determine the level of support or challenge that these structures might present during the rehabilitation process.
Neuromuscular and movement-related functions will be altered by LL amputation, and this will affect occupational performance after surgery. This alteration of function may occur not only in the affected limb but also in other parts of the body. Because of changes in the affected limb, greater stresses will be placed on the rest of the body; a person’s unaffected leg as well as his or her arms will experience increased weight bearing during many functional activities, and both surgical wound healing and increased time in bed will place greater demand on skin functions.
Of particular importance is attention to sensations of pain. Up to 84% of persons who have had an LL amputation have experienced phantom limb pain.11 In such an instance, the client may experience sensations in the part of the limb that has been removed, such as feelings of cramping, squeezing, shooting, or burning pain. In these cases, the therapist can use desensitization techniques (such as massage of the residual limb), exercise, hot and cold therapy, or electrical stimulation54 to help decrease these sensations and allow the client to more easily and comfortably participate in chosen occupations.
Clients with PVD already have compromised cardiovascular function, and care must be taken to determine how much activity can safely be tolerated during therapy. A client’s mental and sensory functions will affect the way in which therapy, including education, is delivered; they will also affect what types of prosthesis and equipment are used.31 Some clients may be able to incorporate new techniques quickly, recalling information from one session or even from reading material, and may be able to independently apply this learning to new situations. However, other clients will require adaptation of training and may require prolonged treatment to turn the new techniques that they have learned into habits. Understanding a client’s values, beliefs, and spirituality will further help the therapist to develop a treatment program and choose interventions that are tailored to that client and best meet his or her needs.
The occupational therapist found that Lena would need to increase her upper body strength to help support herself during transfers and ambulation with the walker. She also needed to improve her postsurgical postural alignment and gait patterns to participate in her chosen occupations. Lena was experiencing pain and sensitivity in her residual limb. However, Lena’s mental functions were found to be strengths, and her vision and the sensation in her hands, although slightly diminished, were functioning at a level sufficient to support her desired functional activities. Additionally, Lena’s belief that good efforts yield results, as well as her commitment to her spiritual and social communities, would facilitate her engagement in her occupational therapy program.
Performance Skills
The most overt effects of LL amputation will be evident in the area of motor and praxis skills. Adjusting posture, coordinating movements, maintaining balance, and bending are altered after surgery, and the client must address each of these skills in therapy to return to a full repertoire of occupations. Sensory and perceptual skills may also be affected by the amputation, and a client may have had prior difficulty with these skills caused by impaired sensory function. The client’s cognitive skills (such as judging, sequencing, and multitasking) and communication and social skills will affect his or her participation in treatment and the therapist’s choice of treatment methods.
Lena’s occupational therapist found that, as she expected, Lena exhibited impairment in stabilizing, aligning, positioning, walking, reaching, bending, moving, transporting, lifting while standing, and pacing. The therapist also found that cognitive skills were at functional levels for Lena. However, Lena did exhibit difficulty with adaptation as she began attempting to perform activities with a changed body structure and in different positions. The therapist also noticed that Lena was having difficulty with social skills, exhibiting trouble focusing and collaborating during many occupations. The therapist would need to address these areas in therapy to help Lena return to her optimal level of participation in occupations.
Performance Patterns
Whatever a client’s performance patterns were before the amputation, they are likely to be altered after amputation. The client may already have useful habits, routines, rituals, and roles that can be drawn upon in therapy to facilitate his or her return to prior levels of occupational performance. However, for many clients, the occupational history will reveal prior impoverished habits and lack of, or maladaptive, routines that may present challenges to the rehabilitative process. Although Lena’s diabetes and PVD placed her at increased risk for poor wound healing, she never developed the habit of routinely checking her feet and legs for cuts or infections. This impoverished habit led to three amputations on her left leg. Lena’s morning routine in her kitchen involved crossing the room many times and carrying multiple items in her hands at once. In conversations with her occupational therapist, Lena did indicate that she had already begun to drop things during this routine, that she had nearly fallen a few times, and that she worried about being able to safely make her own breakfast at home.
Psychosocial Repercussions
Amputation of a limb represents a loss and therefore involves a grief process. This process involves dealing with one’s feelings regarding change in body structure, functional abilities, and participation in occupations. It can also involve anger, acknowledgment of unpleasant realities regarding one’s health status, and fears about one’s functional and financial future. Social acceptance and community function are also significant concerns for a person who has undergone an amputation. These are all areas that can be addressed by an interdisciplinary rehabilitation team in an effort to help the client adapt and should inform all aspects of occupational therapy intervention.
The occupational therapist may use several techniques to help a person adapt to his or her amputation and create a new sense of self. The therapeutic relationship and the therapeutic use of self can provide a safe environment and catalyst for the client to discuss feelings of loss, thoughts regarding body changes, and fears for the future. The therapist can teach the client coping skills for dealing with anxiety and depression, as well as techniques for improving postsurgical body image.52 The consultation process can include recommendations for workplace adaptations, as well as suggestions for how to make the home more accessible to a client with a new amputation. The therapeutic use of occupations that have been graded to the client’s current abilities provides opportunities to master skills and experience success. The therapist’s encouragement during such sessions not only fosters development and provides support but also provides evidence to the client that recovery of function and return to participation in chosen occupations are indeed possible52; this knowledge fosters hope and a vision of the future.
It is important to recognize that an outside observer’s rating of a person’s adaptation to an LL amputation may not be the same as that person’s self-rating. A surgeon may rate success on the basis of healing of the surgical wound, a prosthetist on the fit between residual limb and prosthesis, a physical therapist on the client’s ability to ambulate, and an occupational therapist on the client’s ability to participate in areas of occupation. However, clients may place greater emphasis on other criteria in their determination of successful adaptation to an LL amputation. Some related variables that appear of primary concern to clients include feeling comfortable while being active in the presence of strangers, not feeling like a burden to one’s family, being able to care for others, and being able to exercise recreationally.40
Context and Activity Demands
An understanding of the client’s contexts, environments, and demands of daily activities will help the therapist design a treatment program that will best help the client re-engage in chosen occupations within his or her everyday environment. It will also help the therapist adapt the activity demands of the client’s chosen occupations to facilitate greater independence and development of proficiency. Lena’s occupational therapist took a detailed floor plan of Lena’s bedroom and was able to move the furniture in her room into the skilled nursing facility, so it closely approximated her bedroom setup at home. When Lena performed her morning and evening ADLs within the room, she was then doing so in a more natural environment. Lena’s therapist initially made significant adaptations to Lena’s morning routine demands, wheeling Lena up to the sink in the bathroom for sponge-bathing and bringing her clothes to her in the bathroom, where she would stand with the help of a grab bar, so the therapist could pull Lena’s pants up. Over the course of time, as Lena improved her performance skills, improved her performance patterns, and incorporated into her routine new ADL techniques taught during therapy, her occupational therapist was able to decrease the adaptation of activity demands, and Lena progressed to independence with routines that she would be able to sustain at home.
Additional Considerations for Elderly Clients
Although LL amputation may be performed to preserve function or to save the client’s life, it does carry an increased mortality risk as the age of the client increases. One study of older persons who underwent a BKA found the survival probability after BKA to be 77% at 1 year, 57% at 3 years, and 28% at  years.35 Because this increased mortality risk is related not only to the amputation surgery but also to preexisting health and environment factors, attention to the overall health status of the client is of utmost importance.
years.35 Because this increased mortality risk is related not only to the amputation surgery but also to preexisting health and environment factors, attention to the overall health status of the client is of utmost importance.
Many body structures and functions are already compromised in elderly clients, making the rehabilitation process longer and more delicate. An elderly person may take more time to recover from the effects of anesthesia after surgery, including effects on cognition and the respiratory system. For unilateral amputees, leg balance on the unaffected limb is a significant predictor for prosthetic use.59 Because balance may already be decreased and cognitive skills may have declined, elderly clients learning to use a prosthetic limb may experience greater challenges. Elderly clients have already experienced many losses, which may include family and friends, home, health, and function; the psychological sequelae of amputation can be all the more traumatic when layered over these previous losses.
1. Define the following abbreviations: AE, TD, BE, AKA, and BKA.
2. List six reasons for amputation.
3. What are the four main reasons for LL amputation?
4. What are the primary goals of amputation surgery?
5. Name the two types of surgical procedures that can be performed, and list the advantages of each.
6. Name at least four postsurgical factors that can interfere with prosthetic training and rehabilitation. How is each solved?
7. Define neuroma. How does it affect wearing of the prosthesis?
8. What is the difference between phantom limb and phantom pain?
9. What are some of the typical and expected psychosocial consequences of limb loss?
10. How can members of the rehabilitation team facilitate adjustment to amputation and prosthesis wear?
11. Which arm function is lost and which functions are maintained in a long trans-radial amputation?
12. What is the purpose of the preprosthetic program?
13. Describe activities and exercises suitable for the preprosthetic period.
14. Before the TD on a trans-humeral prosthesis can be operated, what must the wearer do?
15. How does the prosthesis wearer pre-position the TD?
16. Name three types of electric TDs.
17. How is functional training graded?
18. What is the source of power that activates the electric-powered prosthesis?
19. What are some advantages of the electric-powered prosthesis?
20. What is a hybrid prosthesis?
21. What does muscle site control training mean?
22. Describe the relative roles of a prosthesis and a sound arm and hand in the following activities: cutting meat, opening a jar, using scissors, buckling a belt, using an eggbeater, and hammering a nail.
23. Name two significant concerns for the residual limb immediately after surgery.
24. What is the purpose of a shrinker?
25. What should be done with the wheelchair to accommodate the residual limb? To accommodate a person with bilateral AKAs?
26. Name the main components of an LL prosthesis.
27. What is the purpose of using a sock on the residual limb?
28. How will LL amputation affect other parts of the body?
29. How might LL amputation affect an individual’s participation in areas of occupation?
30. Which performance skills are most likely to be affected after LL amputation?
31. How can preexisting performance patterns affect a client’s participation in occupations after the amputation?
32. What are the potential psychosocial repercussions of LL amputation?
33. How can ADL activity demands be adapted to foster greater independence after LL amputation?
34. What additional considerations does LL amputation present for elderly clients?
References
1. American Occupational Therapy Association. Occupational therapy practice framework: domain and process, ed 2. Am J Occup Ther. 2008;62:625.
2. Anderson, MH, Bechtol, CO, Sollars, RE. Clinical prosthetics for physicians and therapists. Springfield, IL: Charles C Thomas; 1959.
3. Andrew, JT. Prosthetic principles. In Bowker JH, Michael JW, eds.: Atlas of limb prosthetics: surgical, prosthetic, and rehabilitation principles, ed 2, St Louis: Mosby, 1992.
4. Atkins, DJ. Adult myoelectric upper-limb prosthetic training. In: Atkins DJ, Meier RH, eds. Comprehensive management of the upper limb amputee. New York: Springer-Verlag, 1989.
5. Atkins, DJ. Adult upper limb prosthetic training. In: Atkins DJ, Meier RH, eds. Comprehensive management of the upper-limb amputee. New York: Springer-Verlag, 1989.
6. Atkins, DJ. Postoperative and preprosthetic therapy programs. In: Atkins DJ, Meier RH, eds. Comprehensive management of the upper-limb amputee. New York: Springer-Verlag, 1989.
7. Banerjee, SJ. Rehabilitation management of amputees. Baltimore: Williams & Wilkins; 1982.
8. Bennett, JB, Alexander, CB. Amputation levels and surgical techniques. In: Atkins DJ, Meier RH, eds. Comprehensive management of the upper-limb amputee. New York: Springer-Verlag, 1989.
9. Bennett, JB, Gartsman, GM. Surgical options for brachial plexus and stroke patients. In: Atkins DJ, Meier RH, eds. Comprehensive management of the upper-limb amputee. New York: Springer-Verlag, 1989.
10. Billock, JN. Prosthetic management of complete hand and arm deficiencies. In Hunter JM, Mackin EJ, Callahan AD, eds.: Rehabilitation of the hand: surgery and therapy, ed 4, St Louis: Mosby, 1995.
11. Czerniecki, JM, Ehde, DM. Chronic pain after lower extremity amputation. Crit Rev Phys Med Rehabil. 2003;15:309.
12. Dalsey, R, Gomez, W, Seitz, WH, Jr., et al. Myoelectric prosthetic replacement in the upper extremity amputee. Orthop Rev. 1989;18:697.
13. DiMartine, C. Capturing the phantom. inMotion. 2000;10:7.
14. Evans, WE, Hayes, JP, Vermillion, BO. Effect of a failed distal reconstruction on the level of amputation. Am J Surg. 1990;160:217.
15. Fan, T, Fedder, DO, Smoking gun: the impact of smoking on amputees, Baltimore, Pharmaceutical Health Service Research Program, University of Maryland, Baltimore, 2003. Available at, http://www.amputee-coalition.org/related_articles/smoking_gun.html.
16. Friedman, LW. Rehabilitation of the amputee. In: Goodgold J, ed. Rehabilitation medicine. St Louis: Mosby, 1988.
17. Friedman, LW. The psychological rehabilitation of the amputee. Springfield, IL: Charles C Thomas; 1978.
18. Fryer, CM, Michael, JW. Body-powered components. In Bowker JH, Michael JW, eds.: Atlas of limb prosthetics: surgical, prosthetic, and rehabilitation principles, ed 2, St Louis: Mosby, 1992.
19. Gard, SA, Childress, DS. A study to determine the biomechanical effects of shock-absorbing pylons. Rehabil R&D Progress Reports. 1998;35:18.
20. Glattly, HW. A statistical study of 12,000 new amputees. South Med J. 1964;57:1373.
21. Greenwald, RM, Dean, RC, Board, WJ. Volume management: smart variable geometry socket (SVGS) technology for lower-limb prostheses. J Prosthet Orthot. 2003;15:107.
22. Harris, KA, van Schie, L, Carroll, SE, et al. Rehabilitation potential of elderly patients with major amputations. J Cardiovasc Surg (Torino). 1991;32:648.
23. Hill, SL. Interventions for the elderly amputee. Rehabil Nurs. 1985;10:23.
24. Hirschberg, G, Lewis, L, Thomas, D. Rehabilitation. Philadelphia: JB Lippincott; 1964.
25. Jacobsen, SC, et al. Development of the Utah Artificial Arm. IEEE Trans Biomed Eng. 1982;29:249.
26. Jelic, M, Eldar, R. Rehabilitation following major traumatic amputation of lower limbs: a review. Crit Rev Phys Rehabil Med. 2003;15:235.
27. Kay, HW, Newman, JD. Relative incidence of new amputations: statistical comparisons of 6,000 new amputees. Orthot Prosthet. 1978;59:109.
28. Knighton, DR, Fylling, CP, Fiegel, VD, et al. Amputation prevention in an independently reviewed at-risk diabetic population using a comprehensive wound care protocol. Am J Surg. 1990;160:466.
29. Krajewski, LP, Olin, JW. Atherosclerosis of the aorta and lower extremities arteries. In: Young JR, et al, eds. Peripheral vascular diseases. St Louis: Mosby, 1991.
30. Lane, JM, Kroll, MA, Rossbach, P. New advances and concepts in amputee management after treatment for bone and soft tissue sarcomas. Clin Orthop Relat Res. 1990;256:280.
31. Larner, S, vanRoss, E, Hale, C. Do psychological measures predict the ability of lower limb amputees to learn to use a prosthesis? Clin Rehabil. 2003;17:493.
32. Larson, CB, Gould, M. Orthopedic nursing, ed 8. St Louis: Mosby; 1974.
33. Legro, MW, Reiber, GE, Czernieck, JM, et al. Recreational activities of lower-limb amputees with prostheses. J Rehabil Res Dev. 2001;38:319.
34. Leonard, JA, Meier, RH. Prosthetics. In: DeLisa JA, ed. Rehabilitation medicine principles and practice. Philadelphia: JB Lippincott, 1988.
35. Levin, AZ. Functional outcome following amputation. Topics Geriatr Rehabil. 2004;20:253.
36. Levy, LA. Smoking and peripheral vascular disease. Clin Podiatr Med Surg. 1992;9:165.
37. Lind, J, Kramhhaft, M, Badtker, S. The influence of smoking on complications after primary amputations of the lower extremity. Clin Orthop Relat Res. 267(211), 1992.
38. Link, MP, Goorin, AM, Horowitz, M, et al. Adjuvant chemotherapy of high grade osteosarcoma of the extremity. Clin Orthop Relat Res. 270(8), 1991.
39. Malone, JM, Goldstone, J. Lower extremity amputation. In: Moore WS, ed. Vascular surgery: a comprehensive review. New York: Grune & Stratton, 1984.
40. Matsen, SL, Malchow, D, Matsen, FA. Correlations with patients’ perspectives of the result of lower-extremity amputation. J Bone Joint Surg Am. 2000;82:1089.
41. McIntyre, KE, Jr. The diabetic foot and management of infectious gangrene. In: Moore WS, Malone JHM, eds. Lower extremity amputation. Philadelphia: WB Saunders, 1989.
42. Meier, RH. Amputations and prosthetic fitting. In: Fisher S, ed. Comprehensive rehabilitation of burns. Baltimore: Williams & Wilkins, 1984.
43. Meier, RH, Atkins, DJ. Preface. In: Atkins DJ, Meier RH, eds. Comprehensive management of the upper-limb amputee. New York: Springer-Verlag, 1989.
43a. http://biomed.brown.edu/Courses/BI108/BI108_2003_Groups/Hand_Prosthetics/stats.html.
44. Michaels, JA. The selection of amputation level: an approach using decision analysis. Eur J Vasc Surg. 1991;5:451.
45. Moss, SE, Klein, R, Klein, BE. The prevalence and incidence of lower extremity amputation in a diabetic population. Arch Intern Med. 1992;152:610.
46. Muilenburg, AL, LeBlanc, MA. Body-powered upper-limb components. In: Atkins DJ, Meier RH, eds. Comprehensive management of the upper-limb amputee. New York: Springer-Verlag, 1989.
47. Nader, M, Ing, EH. The artificial substitution of missing hands with myoelectric prostheses. Clin Orthop Relat Res. 1990;258:9.
47a. National Limb Loss Information Center, Fact sheet: limb loss in the United States, Knoxville, TN, Amputee Coalition of America, 2007. [Updated 2008 Sep 18; cited 2009 Feb 25]. Available at, http://www.amputee-coalition.org/fact_sheets/limbloss_us.html.
48. NovaCare. Motion control: training the client with an electric arm prosthesis. King of Prussia, PA: NovaCare (videotape); 1997.
49. Novotny, MP. Psychosocial issues affecting rehabilitation. Phys Med Rehabil Clin North Am. 1991;2:273.
50. Olivett, BL. Management and prosthetic training of the adult amputee. In: Hunter JM, ed. Rehabilitation of the hand. St Louis: Mosby, 1984.
51. O’Sullivan, S, Cullen, K, Schmitz, T. Physical rehabilitation: evaluation and treatment procedures. Philadelphia: FA Davis; 1981.
52. Pendleton, HM, Schultz-Krohn, W. Psychosocial issues in physical disability. In: Cara E, MacRae A, eds. Psychosocial occupational therapy: a clinical practice. Clifton Park, NY: Thomson Delmar Learning, 2005.
53. Pinzur, MS, Angelats, J, Light, TR, et al. Functional outcome following traumatic upper limb amputation and prosthetic limb fitting. J Hand Surg Am. 1994;19:836.
54. Rand, JD, Paz, JC. Amputation. In: Paz JC, West MP, eds. Acute care handbook for physical therapists. Woburn, MA: Butterworth-Heinemann, 2002.
55. Raney, R, Brashear, H. Shands’ handbook of orthopaedic surgery, ed 8. St Louis: Mosby; 1971.
56. Ritz, G, Friedman, S, Osbourne, A. Diabetes and peripheral vascular disease. Clin Podiatr Med Surg. 1992;9:125.
57. Sanders, JE, Nicholson, BS, Zachariah, SG, et al. Testing of elastomeric liners used in limb prosthetics: classification of 15 products by mechanical performance. J Rehabil Res Dev. 41(175), 2004.
58. Santschi WR, ed. Manual of upper extremity prosthetics, ed 2, Los Angeles, CA: University of California Press, 1958.
59. Schoppen, T, Boonstra, A, Groothoff, JW, et al. Physical, mental and social predictors of functional outcome in unilateral lower-limb amputees. Arch Phys Med Rehabil. 2003;84:803.
60. Scott, RN, Parker, PA. Myoelectric prostheses: state of the art. J Med Eng Technol. 1988;12:143.
61. Simon, M. Limb salvage for osteosarcoma in the 1980s. Clin Orthop Relat Res. 1990;270:264.
62. Spencer, EA. Amputation and prosthetic replacement. In Hopkins HL, Smith HD, eds.: Willard & Spackman’s occupational therapy,, ed 8, Philadelphia: JB Lippincott, 1993.
63. Spencer, EA. Amputations. In Hopkins HL, Smith HD, eds.: Willard & Spackman’s occupational therapy,, ed 5, Philadelphia: JB Lippincott, 1978.
64. Spencer, EA. Functional restoration. III: Amputation and prosthetic replacement. In Hopkins HL, Smith HD, eds.: Willard & Spackman’s occupational therapy, ed 8, Philadelphia: JB Lippincott, 1993.
64a. Franz, EA, Rumachandran, VS. Bimanual coupling in amputees with phantom limbs. Nat Neurosci. 1998;1:443.
64b. Ramachandran, VS, Brang, D, McGeoch, PD. Size reduction using mirror visual feedback (MVF) reduces phantom pain. Neurocase. 2009;3:1.
65. Spencer, EA. Musculoskeletal dysfunction in adults. In Neistadt ME, Crepeau EB, eds.: Willard & Spackman’s occupational therapy, ed 9, Philadelphia: JB Lippincott, 1998.
66. Spiegal, SR. Adult myoelectric upper-limb prosthetic training. In: Atkins DJ, Meier RH, eds. Comprehensive management of the upper-limb amputee. New York: Springer-Verlag, 1989.
67. Springfield, DS. Introduction to limb-salvage surgery for sarcoma. Orthop Clin North Am. 1991;22:1.
68. Taylor, LM, Jr., Hamre, D, Dalman, RL, et al. Limb salvage versus amputation for critical ischemia. Arch Surg. 1991;126:1251.
69. Tsai, HA, Kirby, RL, McLeod, DA, et al. Aided gait of people with lower-limb amputations: comparison of 4-footed and 2-wheeled walkers. Arch Phys Med Rehabil. 2003;84:584.
70. Tsang, GM, Crowson, MC, Hickey, NC, et al. Failed femorocrural reconstruction does not prejudice amputation level. Br J Surg. 1991;78:1479.
71. Walsh, NE, et al. Treatment of the patient with chronic pain. In: DeLisa JA, ed. Rehabilitation medicine principles and practice. Philadelphia: JB Lippincott, 1988.
72. Wellerson, TL. A manual for occupational therapists on the rehabilitation of upper extremity amputees. Dubuque, IA: William C. Brown; 1958.
73. White, EA. Wheelchair stump boards and their use with lower limb amputees. Br J Occup Ther. 1992;55:174.
74. Wright G: Controls training for the upper extremity amputee (film), San Jose, CA, Instructional Resources Center, San Jose State University.
75. Yaw, KM, Wurtz, LD. Resection and reconstruction for bone tumor in proximal tibia. Orthop Clin North Am. 1991;22:133.
76. Definitions for levels of amputation as defined by ISO 8548-2:1993(E) and ISO 8548-3:1993(E). Available at http://www.iso.org/iso/products/standards/catalogue_ics_browse.htm?ICS1=01&26ICS2=040&26ICS3=11&26.
Sports and Recreation Technologies, LLC (formerly Therapeutic Recreation Systems, Inc.)
Telephone: 800-279-1865 or 303-444-4720
Web: http://www.sportsandrectec.com
Email: bob.sportsnrectec@att.net
Motion Control, Inc. (Fillauer subsidiary)
Web: www.utaharm.com
Email: info@utaharm.com
DVD “Training the Client with an Electric Arm Prosthesis,” 2008; 1998.