chapter 5 Activity-based intervention in stroke rehabilitation
After completing this chapter, the reader will be able to accomplish the following:
1. Apply the principles of the International Classification of Function and the Occupational Therapy Practice Framework to occupational therapy intervention for stroke survivors.
2. Understand implications of neuroscience studies of plasticity and constraint induced movement therapy to activity based interventions in stroke rehabilitation.
3. Design effective practice opportunities for stroke survivors to recover motor, cognitive, and participation skills.
4. Understand the basis of interventions designed to enhance stroke survivors’ potential to achieve maximal recovery.
5. Apply principles of activity analysis and synthesis when designing occupational therapy intervention for stroke survivors.
constraint induced movement therapy (cimt)
strategies for community participation
generalization/transfer of learning
knowledge of performance (kp feedback)
knowledge of results (kr feedback)
mechanical constraints to movement
With advances in medical intervention and societal attitudes toward people with disabilities, rehabilitation expectations and outcomes for stroke survivors are continuously improving. In recent years, evidence from the neuroscience and rehabilitation research literature, and shifts in thinking about the definition of health and wellness, have provided increasing support for two major tenets of occupational therapy with stroke survivors: that recovery of function can be enhanced through the therapeutic use of task-based challenges, and that a return to a meaningful lifestyle after a stroke is contingent on complex interactions between multiple factors.
This chapter presents concepts from the International Classification of Function (ICF),64 the Occupational Therapy Practice Framework,2 the Occupational Therapy Practice Guidelines for Adults with Stroke,44 and research literature to provide an evidence-based foundation for the efficacy of activity-based intervention with stroke survivors. In addition, this chapter presents an introduction to salient concepts about practice and learning from the motor learning literature. Finally, this chapter applies the evidence to provide occupational therapists with guidelines for using activity-based intervention in stroke rehabilitation.
Background concepts and evidence
International classification of function
The ICF reflects a current understanding that health represents far more than the absence of disease (Fig. 5-1). Function, a dynamic interaction between health conditions and contextual factors, is ICF’s yardstick for measuring successful rehabilitation outcomes. According to ICF, function is the integrated totality of one’s body function, activity, and participation. The term disability is used as the antithesis of function and includes impairment, activity limitation, and/or participation restriction. In its discussion of activity and participation, the ICF distinguishes between capacity (the theoretical potential to perform) and performance in a person’s actual, current context. This distinction is crucial in occupational therapy with stroke survivors. Demonstrated improvements within a treatment setting are mere changes in capacity. Clearly, the goal must be to promote generalization of regained skills for improvements in actual performance.

Figure 5-1 Interactions between components of International Classification of Function.
(From World Health Organization: International classification of functioning, disability, and health [ICF], Geneva, Switzerland.)
ICF integrates medical and social models of disability. While appreciating the medical model’s value in promoting change within an individual, ICF also recognizes that social and environmental factors influence performance. Occupational therapists share this dual orientation in stroke rehabilitation. Depending on a person’s current potential for skill recovery, occupational therapists adapt tasks and environments to promote optimal practice conditions for internal change or to facilitate task performance within constraints of insurmountable physical or cognitive limitations.
Occupational therapy practice framework
The occupational therapy profession applauds both the vision and semantics of ICF. Accordingly, the Occupational Therapy Practice Framework44 is structured to synchronize with ICF and thus to highlight that long-standing values within our profession are consistent with contemporary views about health and quality of life.
The Occupational Therapy Practice Framework provides practitioners with a foundation for designing and implementing multidimensional services that enable clients to participate in self-selected life activities within their homes, families, and communities. The Domain of Occupational Therapy2 requires therapists to include the following components in assessment, planning, treatment, and outcomes:
Consistent with ICF’s dual orientation to medical and social concerns, occupational therapy intervention considers two groups of factors: those within the individual (client factors, performance patterns, and performance skills) and those within the environment (activity demands and context). Some factors contribute to a particular person’s capacity to engage in self-selected occupations; others do not. Some factors are amenable to change; others are not. A client may wish to change some factors and may have no incentive to change others. For each individual, the skilled occupational therapist determines the unique constellation of impact, potential, and desire. Intervention promotes change in those internal and external factors that the therapist and client have collaboratively identified as treatment goals (Fig. 5-2).
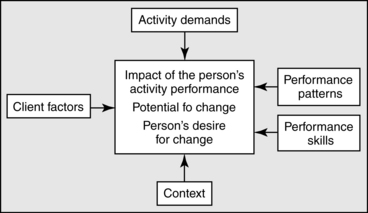
Figure 5-2 The occupational therapist’s clinical reasoning process. In determining treatment goals, the therapist considers the three factors in the center square for each of the surrounding domain areas.
Stroke is a complex condition. Depending upon the nature of the cerebrovascular accident (CVA) and immediate medical care, residual neuropathology varies widely among individuals. Consequently, related impairments and potentials for improvement differ significantly. Each person presents with a unique lifetime history of roles, activities, temporal patterns, and culture. Each person and family has unique constraints that govern their willingness to change long-standing routines and environments.
Various chapters in this text explore ways occupational therapists intervene, both to promote change within an individual and to adapt external factors to promote compensation. The ultimate goal of both interventions is participation in valued life activities. A comprehensive occupational therapy program for any stroke survivor will artfully target both internal and external factors. The interaction between internal and external factors is complex indeed. Improvements in motor and cognitive skills alone, unaccompanied by adaptations to family structure or physical accessibility, may fail to lead to an outcome of full, meaningful participation. Correspondingly, an overreliance on compensation, without providing stroke survivors opportunities to improve internal skills, seriously limits clients from reaching their ultimate potentials for engagement in a wide variety of life roles.
Occupational therapy practice guidelines for adults with stroke
Practice guidelines are developed by many health professions to promote the use of evidence-based interventions for the goals of improving client care, enhancing consumer satisfaction, and facilitating interdisciplinary communication. The American Occupational Therapy Association (AOTA) has published practice guidelines related to a variety of client populations and areas of occupational therapy intervention. The Occupational Therapy Practice Guidelines for Adults With Stroke44 presents extensive evidence from research literature in the neurosciences and in clinical rehabilitation that provide significant support for the value of introducing individualized task-based challenges to improve motor, cognitive, and occupational performance in stroke survivors.
Neuroscience studies of brain plasticity
It is common knowledge that necrotic tissue in the mammalian central nervous system does not regenerate.4 This is the greatest challenge in stroke rehabilitation, as compared to rehabilitation for individuals with injuries to the peripheral nervous system or to the musculoskeletal system, where we expect ultimate recovery of damaged tissue. Even so, countless stroke survivors experience significant recovery of motor, language, and cognitive function.
Early, spontaneous recovery is typically attributed to resolution of temporary pathophysiology in regions of the affected hemisphere indirectly damaged by stroke-related sequelae described in Chapter 1. A stroke is a catastrophic physiological event. In addition to cell death in those neurons deprived of oxygen, indirect damage includes changes in cerebral blood flow, cerebral metabolism, edema, and cascading degeneration along neural pathways. The concept of diaschisis, coined by the 19th century Russian neurologist von Monakow has continued to influence neurologists and neuroscientists.9,40,48 Diaschisis, or transient inhibition, spreads to remote sites in the fiber pathways leading from the site of injury. As diaschisis resolves over time, neural activities return to the temporarily suppressed regions, and the stroke survivor experiences return of function. Diaschisis is a probable explanation for the shift to spontaneous innervation of some flaccid muscles so often seen in the early weeks after a stroke. The phenomenon of “learned nonuse”, articulated by Taub and colleagues39,55 represents a person’s inability to functionally use this reemerging motor activation. Occupational therapy intervention can prevent or reverse learned nonuse through interventions described in Chapter 10.
Neuroscience researchers are actively exploring a variety of potential recovery mechanisms after central nervous system damage. The possibility of plasticity, or reorganization of undamaged systems in the brain, has generated a growing body of positive research findings. These studies of humans and other mammals have provided significant evidence that recovery of function after brain lesions is associated with recruitment of brain regions not typically activated for a specified function.10 These studies consistently find that reorganization of neural mechanisms is a dynamic process that is influenced by the person’s active efforts to meet environmental and task demands.26,30
Depending on the extent of neuropathology, all stroke survivors have varying potentials for spontaneous recovery and reorganization of neural mechanisms. Using principles presented in this and subsequent chapters, the occupational therapist determines:
Constraint induced movement therapy
Constraint Induced Movement Therapy (CIMT), which has yielded the strongest outcomes evidence of any treatment in the history of stroke rehabilitation,62,63 provides significant support for the therapeutic value of activity-based practice for improving motor function in a select group of stroke survivors. CIMT evolved from the theory of learned nonuse, which postulates that potential motor recovery after unilateral brain lesions is limited by a learned overreliance on the unaffected limbs. Immediately after brain injury, contralateral flaccidity limits functional use of the affected arm and leg. Because motor function remains unaffected on the opposite side, most stroke survivors compensate by relying exclusively on the unaffected limbs to perform tasks. This theory of learned nonuse may explain why upper limb recovery lags behind lower limb recovery. Although each attempt to stand or walk requires bilateral activity in the legs, many upper limb activities may be accomplished by using the unaffected side exclusively.
In CIMT, physical constraint to the unaffected upper limb is provided in an effort to reverse the effects of learned nonuse. The typical research protocol has been for subjects who are at least one year poststroke to wear a mitt on the unaffected arm to remind them not to use this limb during virtually all waking hours for two weeks. On each of the 10 weekdays, subjects spend six hours in a rehabilitation program in which they are challenged with individualized task challenges that elicit repetitive practice in using their paretic arm and hand. In controlled double blind studies at three to nine months62 and two years after intervention,63 subjects who participated in CIMT performed significantly better than control participants in the speed and quality of their movement. More importantly, they reported significant differences in the actual amount of use of the affected upper limb, as compared to control subjects. A note of caution about the use of CIMT in the early stage of stroke recovery emerges from acute animal studies. Studies with lesioned rats27,42 have found that forced use with these animals during the first seven days after injury leads to degeneration of surrounding, surviving neural tissue.
Proponents of CIMT have never claimed that their approach reverses paralysis. In addition to intact cognitive function, criteria for participation in constraint programs include the minimum requirements that participants exhibit at least 10-degrees of active extension at the wrist, metacarpophalangeal, and interphalangeal joints, and demonstrate ability to maintain standing balance without upper extremity support.62,63 CIMT is clearly an approach for a select category of stroke patients; but the principles have been successfully applied to several other protocols, which are described in Chapter 10.
In essence, CIMT “forces” the individual to practice using a paretic limb, and thus provides the central nervous system with appropriate challenges for reorganization of motor control. There is another aspect to CIMT never discussed by its proponents, and that may have significance for occupational therapy intervention with stroke survivors. There is a hypothesized link with Seligman’s “theory of learned helplessness.”49 First discovered in dogs and later tested in numerous studies of humans,50 this theory postulates that, after repeated exposure to situations in which actions are ineffective, organisms become passive, even when future actions could be effective. After an initial period of flaccidity following a stroke and subsequent relearning of one-handed task performance, many stroke survivors remain essentially unaware of a return of motor potential. Several factors might explain this phenomenon:
 The person has no reason to try to use the arm and thus remains ignorant about emerging motor potential.
The person has no reason to try to use the arm and thus remains ignorant about emerging motor potential.
 The person notices isolated abilities to perform specific movements, but doesn’t know how to use these movements for integrated functional performance.
The person notices isolated abilities to perform specific movements, but doesn’t know how to use these movements for integrated functional performance.
 The person experiences mechanical constraints that limit the capacity to use the recovering paretic limb in a functional way.
The person experiences mechanical constraints that limit the capacity to use the recovering paretic limb in a functional way.
For those stroke survivors who meet the qualifying criteria, CIMT may be an effective way to improve motor performance. For those whose recovery is more limited, the concept of learned nonuse may still be helpful toward structuring effective therapeutic intervention. Furthermore, the extensive literature about neuroplasticity and CIMT supports the need for therapists to be experts about the role of practice and learning when providing evidence-based intervention to stroke clients.
Practice and learning
Goals of training and learning
Learning and training are two distinct phenomena, each with its own required style of practice. The goal of training is to memorize a prescribed solution to a selected task challenge, whereas the goal of learning is to develop one’s own solution, which can be applied in a variety of situations. Based on each client’s abilities and role demands, the occupational therapist determines whether the therapeutic goal will be to promote training or learning. In therapeutic training, practice entails repetitive performance of a designated sequence of behaviors. Task performance must occur in the actual setting in which the individual plans to perform the task, because there is no evidence that skills acquired through training can be successfully applied in different environmental contexts.52,57
Learning and training are both internal phenomena that cannot be observed directly. Therapists assume that training has occurred if performance of a specific task improves and persists over time. Therapists assume learning has occurred when a person is able to apply a new set of skills within a variety of situations.46,51 Whenever possible, occupational therapy attempts to promote learning of motor and cognitive skills that will provide the individual with an infinite number of choices for task and role engagement. Practice for learning requires active engagement in tasks that require problem-solving and implementation of effective foundational strategies. Therefore, before providing practice opportunities to stroke survivors, occupational therapists must first prepare the clients with underlying motor, cognitive, and social foundational strategies.
Foundational strategies for task performance
Kinesiological linkages and generalized motor programs
When the neuromuscular system is functioning optimally, a person can rely on automatic kinematic and kinetic linkages to serve as a foundation for functional movements. Although these linkages are described in a variety of ways,5,46,51 motor control theorists and kinesiologists agree that they promote optimal mechanical interactions between muscles and body segments.
Often, stroke survivors have lost the automatic kinesiological linkages associated with efficient movement.13,59 This may be a result of limited mobility of body segments, weakness of specific muscular components, or loss of the motor program that links muscles or joints during a given movement sequence. Several automatic kinematic linkages are commonly observed during optimal movement, but are unavailable to many stroke survivors:
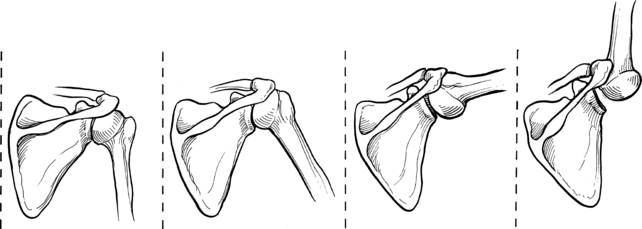
 Pain-free shoulder abduction through the full range of motion relies on scapulohumeral rhythm, a kinematic linkage between the scapula and humerus41 (Fig. 5-3).
Pain-free shoulder abduction through the full range of motion relies on scapulohumeral rhythm, a kinematic linkage between the scapula and humerus41 (Fig. 5-3).
 The deltoid and rotator cuff muscles are kinetically linked to ensure that the deltoid fibers produce the desired rotary force on the humerus. Without this linkage, an attempt to abduct the shoulder will instead result in a nonfunctional upward shrug of the shoulder41 (Fig. 5-4).
The deltoid and rotator cuff muscles are kinetically linked to ensure that the deltoid fibers produce the desired rotary force on the humerus. Without this linkage, an attempt to abduct the shoulder will instead result in a nonfunctional upward shrug of the shoulder41 (Fig. 5-4).
 Glenohumeral external rotation is automatically linked with end-range humeral flexion and abduction.41
Glenohumeral external rotation is automatically linked with end-range humeral flexion and abduction.41
 Grasp patterns are automatically linked with wrist extension to allow for efficient use of extrinsic finger muscles.41
Grasp patterns are automatically linked with wrist extension to allow for efficient use of extrinsic finger muscles.41
 Lumbopelvic rhythm provides for appropriate interactions between movements at the lumbar spine and adjoining pelvis. When rising to stand from a seated position, for example, forward trunk motion is most efficiently initiated at the hips and is accompanied by simultaneous pelvic anterior tilt.41 See Chapter 14.
Lumbopelvic rhythm provides for appropriate interactions between movements at the lumbar spine and adjoining pelvis. When rising to stand from a seated position, for example, forward trunk motion is most efficiently initiated at the hips and is accompanied by simultaneous pelvic anterior tilt.41 See Chapter 14.
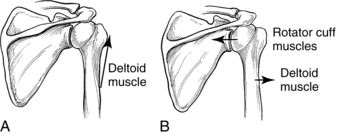
Figure 5-4 Kinetic linkage: relationship between deltoid and rotator cuff muscles. A, Deltoid muscle force acting alone. B, Deltoid and rotator cuff muscles working together.
Kinesiological linkages can be conceptualized as generalized motor programs (GMPs).31,33,46 These “prestructured sets of central commands” govern a particular class of actions. GMPs are designed to be modified in response to continuous changes in environmental and task parameters. Therefore, a unique pattern of activity, with core foundational characteristics, emerges whenever the GMP is executed. For illustration purposes, a forehand tennis swing may be conceptualized as a GMP. Foundational kinesiological relationships comprise a GMP, but an athlete alters the force characteristics, timing, and spatial details of the forehand swing, depending upon the speed, force, and direction of the tennis ball’s trajectory and the player’s intentions regarding how to return the ball to the opponent. When designing therapeutic interventions to improve functional motor performance in stroke survivors, therapists determine the GMPs for general categories of movement, such as reach, grasp, balance, standing up, and sitting down. An occupational therapist determines which kinesiological linkages are impaired and intervenes by assisting with reestablishing these general foundations for optimal motor performance. Motion analysis studies of rolling, getting out of bed, standing up from a sitting position, and moving the arms provide useful information that can help an occupational therapist determine which components are essential in a variety of performance contexts.12,51
Cognitive strategies
Just as kinematic linkages serve as foundational strategies for efficient movement, cognitive processing strategies provide individuals with a framework for interpreting and acting on complex information in a variety of situations. These strategies are organized approaches that assist a person in selecting relevant cues from the environment and planning the most appropriate response.57,58
Depending on the nature and location of the pathology associated with the CVA, a stroke survivor may demonstrate impairments in selecting and implementing appropriate cognitive strategies for accomplishing complex tasks. If these impairments are severe, they will limit performance of routine self-care tasks. Minimal to moderate impairments become more apparent when the individual attempts to resume more demanding occupations such as home management, work, or school activities. Toglia and Golisz have been particularly influential in designing evaluation and treatment protocols to guide occupational therapists in this aspect of intervention.19,56,57
Occupational therapy intervention begins with helping patients develop insight about these deficits through a program that challenges them to estimate task difficulty, predict outcomes, and evaluate personal performance.20,56 Then the occupational therapist teaches general processing strategies that are practiced in a variety of contexts:
 Occupational therapists structure treatment to help clients develop several types of cognitive strategies.
Occupational therapists structure treatment to help clients develop several types of cognitive strategies.
 Prioritizing information before beginning a task is a strategy that can be applied to activities as varied as grocery shopping (using a list, coupons, and the weekly circular), doing a work-related task, or planning a family outing.
Prioritizing information before beginning a task is a strategy that can be applied to activities as varied as grocery shopping (using a list, coupons, and the weekly circular), doing a work-related task, or planning a family outing.
 Clustering related information together may be a useful strategy for a student attempting to master a difficult subject or for a person trying to remember what to purchase in the pharmacy.
Clustering related information together may be a useful strategy for a student attempting to master a difficult subject or for a person trying to remember what to purchase in the pharmacy.
 Blocking out irrelevant details is a foundational strategy necessary for reading a map and managing monthly bills.
Blocking out irrelevant details is a foundational strategy necessary for reading a map and managing monthly bills.
 A left-to-right scanning strategy can be used to find a certain item in a bathroom cabinet and to check typing for errors. Maintaining a daily notebook of things to do and to remember is a strategy with wide applications in a range of situations.
A left-to-right scanning strategy can be used to find a certain item in a bathroom cabinet and to check typing for errors. Maintaining a daily notebook of things to do and to remember is a strategy with wide applications in a range of situations.
 Additional strategies and their applications are discussed in Chapters 17, 18, and 19. Each individual tests the strategies introduced by the therapist to determine whether they are effective and in which situations they can be successfully applied.
Additional strategies and their applications are discussed in Chapters 17, 18, and 19. Each individual tests the strategies introduced by the therapist to determine whether they are effective and in which situations they can be successfully applied.
Strategies for community participation
The social and emotional challenges of coping after a stroke are as demanding as the motor and cognitive challenges (see Chapters 2 and 3). Just as therapeutic interventions can improve strategies essential for moving and for processing information, so too can occupational therapists help stroke survivors develop a core of effective strategies that will help them negotiate their interactions with others and return to full participation within their communities. Therapists should introduce practice of these strategies early in the rehabilitation process. This helps stroke survivors understand that they can realistically expect to continue engaging in activities and roles that bring quality to their lives, regardless of the amount of motor recovery.
Types of learning
Procedural and declarative learning
Occupational therapists structure practice opportunities according to the type of learning goal. Declarative learning is needed for tasks in which language skills are used to organize complex sequences of action.4 Learning a new recipe or a multistep dance routine may require that a person be able to consciously express the processes to be performed. Mental rehearsal is an effective technique for enhancing declarative learning. During mental rehearsal, the individual practices the sequence by reviewing it silently or by verbalizing the steps in their appropriate order. Most skill development in stroke rehabilitation, however, can be characterized as procedural learning, which is achieved through task practice in a series of varying contexts. For example, a person learns to maneuver a wheelchair through a process of procedural learning. Skill develops through opportunities to experiment with different combinations of arm or arm and leg movements to achieve propulsion in a variety of directions and speeds. Similarly, activities requiring balance or reach and grasp require procedural learning. Chapters 8 and 10 present therapeutic interventions for promoting development of these procedural skills.
Implicit and explicit learning processes
Gentile16 and others6 propose that individuals use two distinct but interdependent processes during the acquisition of functional motor skills. An explicit learning process, which is consciously driven, guides the kinematics of the movement. Gentile hypothesizes that people use an explicit process to develop a “ballpark” match between the shape or direction of their movements and the environmental requirements for achieving the goal. External guidance and feedback is likely to have a beneficial impact upon the explicit learning process. Schmidt46 refers to such intervention as an “instructional set,” in which the person is given a general idea or image of the task to be learned.
An implicit learning process guides the kinetics of the movement or the dynamics of force generation. This aspect of movement requires appropriate selection of muscle contraction patterns, which is determined by accurate predictions of how external forces will affect the movement. Implicit learning requires a self-organizing process and may take longer to develop than explicit learning. Furthermore, implicit learning lies beyond conscious awareness and is unlikely to be augmented by external guidance or feedback.11,38 Historically, neurorehabilitation interventions that attempted to directly influence implicit aspects of motor performance, such as muscle recruitment or force modulation, have failed to achieve functional outcomes. Following evidence from motor learning research, therapists should attempt to influence implicit learning by providing appropriate opportunities for effective practice.
Amount of practice
Practice is a critical component to learning. Educators, therapists, and neuroscientists universally agree that the amount of practice affects success in skill development.46,60 Effective protocols in stroke rehabilitation15,34,35,62,63 all share the common characteristic of maximizing the amount of practice. Occupational therapy provides stroke survivors with structured practice opportunities to maximize emerging skills. This is not nearly as simple as it sounds. When people practice maladaptive strategies, they “learn” patterns of behavior that may be counterproductive to future improvements in functional performance. To provide appropriate practice opportunities, therapists must be able to clearly envision the intended practice outcomes and to skillfully manipulate a variety of factors within each practice session. These factors include instructions, feedback, activity parameters, salient conditions within the practice environment, and practice schedules. Furthermore, therapists must recognize the importance of practice during daily activities outside of therapy sessions and structure feasible independent practice opportunities for patients. Subsequent chapters will emphasize ways occupational therapists structure these factors and their interactions so that stroke survivors can engage in practice that yields desired learning for functional outcomes.
Promoting generalization of learning
Three stages of learning are important in the occupational therapy process46:
1. The acquisition phase occurs during initial instruction and practice of a skill (e.g., the initial treatment sessions in which a person learns to use the left arm for functional reach).
2. The retention phase occurs after the initial practice period as individuals are asked to demonstrate how well they perform the newly acquired skill; therapists often refer to this as carryover (e.g., a patient’s ability to perform previously learned reaching activities).
3. In the transfer phase the individual must use the skill in a new context (e.g., the patient’s ability to incorporate a reaching strategy when getting dressed or preparing a meal). The stroke survivor can generalize the strategies learned in the therapy setting and use them in real-life situations.
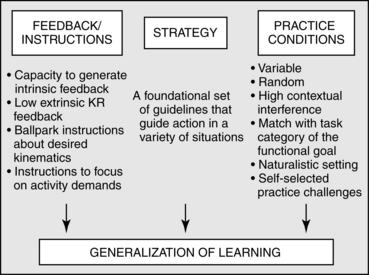
Literature about skill acquisition presents several concepts helpful in guiding therapeutic intervention that promotes generalization of learning. These concepts can be categorized into three major groups: type of feedback, development of underlying strategies, and practice conditions (Fig. 5-5).
Type of feedback
Feedback, or information about a response, can be intrinsic or extrinsic, concurrent or terminal, and can provide knowledge of performance (KP) or knowledge of results (KR). Intrinsic feedback is a result of an individual’s own proprioceptive, tactile, vestibular, visual, and auditory sensory systems. Often after a stroke, somatosensory function is impaired, which limits the effectiveness of intrinsic feedback about motor performance. Extrinsic feedback from a therapist or feedback technology can provide useful supplementary information to facilitate early awareness and learning. However, extrinsic feedback must be gradually decreased for generalization to occur.46
Concurrent feedback is provided during task performance. It includes intrinsic somatosensory feedback and ongoing verbal or manual guidance by a therapist. Terminal, or summary, feedback is given after task completion.47 There are no published studies that compare the effectiveness of concurrent and terminal feedback, but research has established that excessive external concurrent feedback is clearly distracting to the learner.47
Knowledge of performance.
KP feedback is information about the processes used during task performance, such as the way a person moves the pelvis or scapula or whether an appropriate cognitive or social strategy has been implemented. Individuals with intact proprioceptive systems receive concurrent, intrinsic KP feedback as they move. Stroke survivors, however, may no longer have access to this continuous supply of information. Extrinsic KP can be provided before a task is initiated. For example, a therapist can guide a person into assuming a postural set that will facilitate motor performance or in planning a strategy that will enhance performance of a cognitively demanding task. Research literature examining persons without neurological impairments53,66 and stroke survivors14 indicates that a focus on internal performance factors may be counterproductive to learning. Instructing the learner to focus on relevant information in the environment (such as the distance or shape of a goal object) seems to be more effective than directing the learner’s attention internally toward the key elements of a particular movement pattern or sequence.14 The skillful therapist must structure selected parameters within the practice tasks to “press” the individual toward using an intended movement pattern.
Knowledge of results.
KR is feedback about the outcome of an action in terms of accomplishing a goal. This information can serve as a basis for correcting errors for more effective performance on future trials. Results of laboratory research with healthy subjects indicates that frequent, accurate, immediate KR tends to promote improved performance during the acquisition phase but poorer performance during the retention and transfer stages of learning.45,61 Similarly, bandwidth KR, in which feedback is provided only when the performance response is outside a given range of acceptable performance, also leads to better generalization of learning.61 Schmidt46 provides the following theoretical explanation of these findings. When limited KR is provided during acquisition, individuals must rely on relevant cues provided by intrinsic mechanisms to improve their performance on future trials, and they tend to develop less dependency on extrinsic feedback. Based on these findings, it is wise for therapists to limit the immediacy and frequency of KR feedback during stroke rehabilitation. Furthermore, therapists are advised to require that patients determine how effectively they performed therapeutic tasks. To generalize their knowledge for use in situations outside the treatment context, stroke survivors need to learn ways to assess their own performance of functional activities.
Strategy development
Strategies are organized plans or sets of rules that guide action in a variety of situations. New knowledge is more likely to be generalized for use after the acquisition phase if the individual learns a foundational strategy that can be applied to performance of multiple tasks.52
Therapeutic approaches that advocate the importance of strategy formulation during task performance13,57 seek to develop selected motor or cognitive linkages through engagement in a series of tasks that, at a superficial level, may seem unrelated. Each task, however, requires use of the selected strategy. To ensure generalization of the strategy, the selected underlying skill is practiced repeatedly in a variety of contexts during a treatment session. For example, the therapeutic goal may be to develop a selected lumbopelvic linkage as a GMP for forward reach in sitting and standing up from a seated position. The session may begin with the therapist moving the patient’s pelvis so that the person understands the kinematic model of action. The therapist may then ask the patient to sit on a therapy ball, which is rocked forward and backward using anterior and posterior pelvic movement. After this, the seemingly unrelated task of reaching for objects from the seated position will emphasize that the patient anteriorly tilt the pelvis by directing attention to “keeping your back straight” and “bringing your nose over your toes.” Finally, the patient will practice standing up and sitting down on a variety of surfaces, with an emphasis one the same lumbopelvic interactions previously practiced in different contexts. Research findings from studies with healthy participants provide support for the use of this approach for learning the invariant structure of a GMP.18,33 In the terminology of motor learning science, these studies found that a constant or blocked practice schedule of the underlying GMP, using varied practice parameters, leads to enhanced transfer benefits.
Carr and Shepherd’s program for optimizing motor function after stroke12,13 uses five major techniques to assist patients with developing motor strategies: (1) verbal instruction, (2) visual demonstration, (3) manual guidance, (4) accurate and timely feedback, and (5) consistency of practice. In addition, patients develop skill in providing themselves with intrinsic feedback about the kinematics of their motor performance. Outcome studies39 of individuals recovering from stroke provide support for this program’s efficacy.12,13
Toglia56,57 and Golisz19 developed a systematic approach to promote generalization of cognitive strategies, in which the therapist grades treatment by changing certain characteristics of a task but leaving the underlying strategy the same. The following example illustrates a treatment sequence designed to facilitate learning and generalization of a strategy for categorizing information:
The initial task is the first activity performed by the patient, such as sorting a deck of playing cards into a red group (hearts and diamonds) and a black group (spades and clubs). Near transfer is an alternate form of the initial task. Using the previous example, the person might be instructed to sort the playing cards into four groups according to their suits or two groups of odd and even numbers.
Intermediate transfer has a moderate number of changes in task parameters but still has some similarities to the initial task. For example, the same person may be asked to create three categories for sorting a stack of photographs for eventual placement in a photo album.
Far transfer introduces an activity conceptually the same as but physically different from the initial task. Now the person may be asked to organize a collection of magazines into groups based on general interest areas (e.g., news, sports, fashion) for display in a clinic waiting room.
Very far transfer requires spontaneous use of the new strategy in daily functional activities. Before traveling to a neighborhood mall, the person may be asked to categorize items on a shopping list based on the type of store in which they can most likely be purchased.
This “multicontext approach” emphasizes the use of self-assessment and intrinsic KP feedback. Before attempting a new task, patients estimate their performance accuracy and efficiency and determine similarities and differences between the current task and previous activities. After completing a task, patients evaluate their performance and identify techniques that may be helpful in the future. The therapist’s major roles are to structure the activity progression and guide patients in developing insights and strategies. See Chapter 19.
Practice conditions
Several aspects of practice conditions have been studied under both laboratory and clinical conditions. Occupational therapists can use these findings to structure practice conditions in stroke rehabilitation programs. The key is to structure conditions during the acquisition phase that will produce optimal retention and transfer of the learned skills.
Practice schedules.
During blocked (or repetitive) practice, patients practice one task until they master it. This is followed by practice of a second task until it is also mastered. Random (or variable) practice requires patients to attempt multiple tasks or variations of a task before they have mastered any one of the tasks. In addition, the various trials are performed in a random order. Subjects who participate in variable practice perform better on transfer tests than subjects who participate in repetitive practice.21 A study of stroke outpatients found that random practice was more effective than blocked practice for long-term retention of improvements in reach and manipulation skills.22 An explanation is that variable practice facilitates generalization by preventing individuals from developing context-dependent inflexibility when using a newly learned skill.
Contextual interference.
Contextual interference refers to factors in the learning environment that increase the difficulty of initial learning.7 Research studies consistently find that higher levels of contextual interference promote retention and generalization (transfer) of newly learned skills.8,29,54 These findings are typically explained with the hypothesis that initial obstacles to skill acquisition prevent individuals from developing context-dependent inflexibility when using the learned skill in new situations.7 Another explanation is that high contextual interference forces a person to use greater versatility in learning strategies in order to overcome the difficulty of initial practice during the acquisitional learning phase.28 Limited KR feedback is one example of contextual interference that has already been discussed. Blocked and random practice schedules, described previously, are examples of low and high contextual interference, respectively. Although blocked practice may lead to quicker skill acquisition, random practice results in greater retention and generalization.46
Whole versus part practice.
Therapists may intuitively believe that it will be easier for a client to learn small segments of a task than the task in its entirety. However, breaking a task into its component parts for teaching purposes is useful only if the task can be naturally divided into units that reflect the inherent goals of the task.37 One reason for this is that continuous skills (or whole-task performance) are easier to remember than discrete responses. For example, once people have learned to ride a bicycle or play tennis, they will retain these motor skills even without practicing them for many years. On the other hand, segmented, laboratory-type motor skills may be acquired easily but are less likely to be retained over time. Therefore, therapists are advised to teach tasks in their entirety rather than in artificial segments. For example, for best retention and generalization, the task of putting on a shirt is best taught all at once rather than in different portions during consecutive therapy sessions. If it is difficult for a stroke survivor to master all the steps simultaneously, the therapist can cue the patient or can provide manual guidance for selected aspects of the task (as is used in backward chaining instruction). The patient will become accustomed to completing the task during each trial. The therapist’s assistance can be gradually decreased as practice sessions continue.
Practice in natural settings.
Transferring skills learned during training to real-life situations is significantly influenced by the degree of similarity between the practice environment and the actual environment.36 Wu and colleagues65 provided specific support for the value of using real task performance during therapy sessions to improve motor control in stroke survivors. Their motion analysis studies of persons with and without stroke compared the kinematic parameters of reach patterns when participants reached forward to perform a functional task and when they reached forward with no functional goal. Participants in both the neurologically intact and poststroke groups performed better when real objects were available to shape the reach performance.
Skills for performing tasks such as dressing or bathing are best generalized when the skills have been acquired in a setting that resembles the environment in which the activity will ultimately be performed. Occupational therapy clinics with simulated home and community environments will promote better generalization of performance area skills than clinics in which practice of daily tasks is contrived. However, many stroke survivors can never generalize what they learn in simulated settings; in these cases, home-based occupational therapy is required.
Different practice conditions for different task categories.
Gentile16 postulated that motor activities can be classified into four general categories based on environmental pacing conditions and variability between successive trials. Practice conditions for learning will vary depending on the task category.
Closed tasks are activities in which the environment is stable and predictable and methods of performance are consistent over time. Brushing teeth or getting into and out of a bathtub are examples of closed tasks that may be goals for stroke survivors. The best strategy for developing skill in a specific closed task is to develop a narrow and consistent method of performance through repetitive practice of the task.
Variable motionless tasks also involve interacting with a stable and predictable environment, but specific features of the environment are likely to vary between performance trials. Drinking is an example of a variable motionless task because the type of mug, glass, or cup used, and the amount the container is filled will vary in different situations. Dressing is another example because people’s wardrobes consist of clothing of varying fabrics, dimensions, and styles. To achieve independence in a variable motionless task, a patient must learn more than one method of performance. The therapist must provide individuals with opportunities to solve the activity’s motor problems in a wide variety of contexts.
In consistent motion tasks, an individual must deal with environmental conditions in motion during an activity performance; the motion is consistent and predictable between trials. Stepping on to or off of an escalator or moving through a revolving door are examples of consistent motion tasks. Patients need practice that will enable them to accurately match the timing of their actions to the predictable changes of the moving objects in the environment.
Open tasks require people to make adaptive decisions about unpredictable events because objects within the environment are in random motion during task performance. These activities require appropriately timed movements and spatial anticipation of where the relevant objects will be moving. For example, a passenger who is sitting in a moving train must maintain balance when the supporting surface is moving unpredictably. When crossing a street, a person must anticipate the speed and rhythm of both pedestrians and oncoming traffic. When playing most ball games, people must predict the speed and direction of the ball to position themselves in the right place at the right time. Research has shown that the skills required for successful open-task performance cannot be learned through repetitive practice in a stationary environment.24,25 Natural practice in an unpredictable environment seems to be the best strategy for developing skill in open-task performance.
Applying background concepts to using activity-based intervention in occupational therapy with stroke clients
Prerequisites to engaging in activity-based practice
Depending on the extent of the neuropathology, each stroke survivor has a hypothetical, unknown potential for recovery of function. Although practice is crucial, a variety of factors may impede a person’s capacity to benefit from practice opportunities:
 Mechanical constraints to movement
Mechanical constraints to movement
 Inadequate self-monitoring skills
Inadequate self-monitoring skills
A skilled therapist prepares each patient to engage in activity-based practice by directing interventions toward maximizing each factor described in the following sections.
Freedom from mechanical constraints to movement
Stroke survivors encounter several mechanical constraints that limit their ability to move and force them to develop alternative movement strategies. Selected muscle weakness and loss of automatic control over complex postural adjustments are primary impairments, directly related to the stroke pathology. Other mechanical constraints, such as soft-tissue contracture and changes in joint alignment, are secondary to changes in posture and loss of mobility associated with stroke.12,13,43 As secondary impairments, these losses are preventable and reversible with timely interventions.
Muscles lose their natural distensibility when they cease to be passively lengthened by antagonist muscles or an external force. This loss of passive muscle length may lead to malalignments in posture that contribute to a continuing spiral of increasing and additional abnormalities in soft-tissue flexibility. Without active or passive movement, the person is at risk of developing fixed limitations of joint motion and alignment.12,13,43 These problems can be prevented by establishing appropriate postural alignment while lying down, sitting, and standing. In addition, shortly after a stroke, individuals are instructed to follow daily routines to maintain optimal muscle length through the practice of a variety of motor tasks. These interventions are discussed in Chapters 7, 10, 14, and 26.
Fluid, efficient movement requires a mechanical capacity for dissociation between body segments. Although body segments may be kinematically linked during certain actions, each segment must also be free to move independently of its adjacent structures. Scapular-humeral rhythm requires full dissociation between the scapula and thorax. Coordinated shoulder movements require that the humerus freely move independently of the scapula. A full repertoire of trunk activity requires mobility between the thoracic and lumbar spine and between the pelvis and lumbar spine. Stroke survivors often experience loss of dissociation between adjacent body segments. This may occur simply because of losses in soft-tissue distensibility, or it may be linked to maladaptive motor strategies people develop in a subconscious effort to solve other problems. For example, individuals with postural adjustment deficits resulting from stroke often feel insecure about their ability to maintain balance, even in routine sitting or standing positions. The strategy of fixating the pelvis on the lumbar spine or the scapula on the thorax may have the short-term benefit of enhancing a person’s sense of postural security. A negative consequence is that these habitual postures lead to difficulty dissociating the pelvis and scapula from adjacent proximal structures. This lack of sufficient limb girdle mobility subsequently interferes with the kinematics of upper and lower extremity movement. Current therapeutic approaches advocate the early introduction of techniques to enhance balance and postural control.13,51 In addition to the inherent advantages of postural security, early recovery of appropriate balance strategies may prevent postural habits that can compromise a stroke survivor’s future potential to use reemerging muscle function for functional arm and leg movement. See Chapters 7, 8, and 14.
Other secondary impairments, such as edema and pain, seriously limit a person’s potential for movement or functional activity engagement. Therapists are responsible for preventing and minimizing mechanical constraints to movement before introducing practice opportunities for improving motor control. See Chapter 12.
Foundational strategies
As previously discussed, developing foundational strategies is valuable as an intervention approach designed to maximize generalization of learned skills. GMPs are critical for a variety of motor actions. In addition, foundational strategies for classes of cognitive and social skills enable stroke survivors to meet current and unanticipated, future activity demands. Explicit learning, combined with structured demands to enhance self-monitoring of salient features in a desired strategy, establishes an underlying framework for a foundational strategy. Implicit learning, through participation in selected, graded task challenges, promotes development of higher order skills associated with the strategy. Practice opportunities for implementing a strategy under varying parameters promotes flexibility in modifying the strategy to accommodate to ever changing environmental demands.
Self-monitoring skills
Stroke survivors face the challenge of resuming their lives in a body quite different from the one they inhabited before; sensory information may be difficult to interpret, muscles may no longer work in effortless synchrony, and postural preparation for movement may no longer be automatic.
Before stroke survivors can begin to learn effective strategies for movement and task performance, they need to become acutely aware of the way their bodies work, which movements are possible at different body segments, when their postures are optimally aligned, and when they are efficiently “set” to perform particular activities. These understandings are critical for redeveloping appropriate kinesiological linkages that will serve as motor foundations for task performance.
Metacognition1 is the knowledge and regulation of personal cognitive processes and capacities. It includes an awareness of personal strengths and limitations and the ability to evaluate task difficulty, plan ahead, choose appropriate strategies, and shift strategies in response to environmental cues. The multicontext approach to cognitive perceptual impairment emphasizes developing insight about personal deficits (and strengths) as a first step toward developing strategies for functional performance after brain injury. See Chapter 19.
Understanding the concept of metacognition is important for understanding movement as well. Before individuals can generalize the way to use scapulohumeral rhythm in tasks requiring functional reach, they must first understand the amount of mobility their unaffected scapula has. Then they must acknowledge when their affected scapula is not moving freely so that they can develop internal feedback mechanisms that will enable them to correct their scapula movements when those movements are insufficient for accomplishing a given task. The ultimate goal is to use this personal knowledge of movement to change the foundational strategy used for reaching tasks in a variety of contexts. “The individual’s degree of effectiveness in the learning process (and thus in problem solving in general) will be limited by his or her ability for critical self-analysis and environmental analysis in light of the problems encountered and by his or her ability to generate and control the solutions to these problems.”25
Finally, stroke survivors must know how to monitor their own recovery of motor function. As illustrated in the theory of learned nonuse, many individuals fail to use the hemiparetic arms, even when muscle activity is available. Therapists can teach patients how to actively check for changes in ability to recruit specific muscles. Therapy sessions must be viewed as opportunities for stroke survivors to share their new discoveries with their therapists. In turn, the occupational therapist structures activities for the patient to practice emerging skills, both during the therapy session and as “homework” challenges.
Task analysis and problem-solving skills
Occupational therapists have always recognized that they need to be skillful at analyzing tasks. Task analysis enables an occupational therapist to establish treatment goals, synthesize treatment activities, and develop compensatory strategies.2 Rehabilitation professionals realize more often that clients must also learn to analyze activities. Without this skill, the clients would be perpetually dependent on their therapists for successful task achievement. A stroke survivor must learn to determine which motor, cognitive-perceptual, and psychological challenges a task presents. Only then can effective strategies be chosen to “solve the problems”44 inherent in the infinite variety of tasks encountered while actively engaging in meaningful life roles.
While reading subsequent chapters in this text, it should be remembered that occupational therapists strive to develop patients’ insight and problem-solving skills, regardless of whether the intervention relates to balance, gross motor function, limb movement, visual skills, neurobehavioral performance, or daily living tasks.
Expectation for goal achievement
Stroke is a catastrophic event, often leading to depression and despair. Suddenly, a person finds himself in an unfamiliar body. His arms and legs no longer respond to willed commands. Small movements pose a threat to balance. Simple tasks are impossible to perform.
Studies of recovery after brain damage consistently show that a drive to perform functional tasks serves as the challenge that may be crucial for cortical remodeling. Most stroke survivors want desperately to move, but in the first few weeks after the CVA, their flaccid muscles prohibit them from acting on this desire. By the time diaschisis begins to subside, many of them have learned not to expect anything of their paretic limbs. They settle for letting others help them perform daily tasks, or they settle for accomplishing activities without the contributions of their paretic arm or leg.
Occupational therapists play a critical role in empowering stroke survivors to be active agents in their recovery and to return to valued activity engagement. Without making false promises, the therapists can challenge their patients to be vigilant for incremental returns in function. Without implying that full motor recovery is essential to a meaningful life style, they can encourage their patients to look for ways to use small improvements in functional ways. Without blaming future limitations in recovery on the stroke survivor, therapists can teach the patients ways to prevent secondary impairments, and to thus maximize their own potentials for recovery, whatever that potential might be.
It is a serious error to present occupational therapy as “therapy for your arm.” Statistically, far fewer stroke survivors experience significant motor recovery in arm use, as compared to lower limb function.23,32 When occupational therapy’s focus is on the broader goals of returning to independent, safe performance of valued activities, patients can take pride in their reemerging abilities in a variety of physical, cognitive, and social domains. Those fortunate enough to detect emerging innervation to muscles of the arm and hand should be challenged to translate this motor recovery into functional performance. Those who do not enjoy such motor return must be presented with other goals toward which they will direct their serious efforts.
Structuring activity demands to provide effective practice opportunities
Activity-based intervention is a foundation of occupational therapy in stroke rehabilitation. During the evaluation process, an occupational therapist determines:
 Which activities are important to the stroke survivor as determined by the individual’s roles, interests, and anticipated environment
Which activities are important to the stroke survivor as determined by the individual’s roles, interests, and anticipated environment
 Which activities the stroke survivor can or cannot perform
Which activities the stroke survivor can or cannot perform
 Which internal and external factors impede the survivor’s ability to complete the identified activities
Which internal and external factors impede the survivor’s ability to complete the identified activities
During treatment, occupational therapists use activities in two major ways.
1. Some activities may be designed to provide structured challenges to improve internal skills. For example, an occupational therapist may engage a stroke survivor in a modified card game. Depending on the skill-related goals for this individual, the occupational therapist may structure the activity so that it requires forward reach with a hemiparetic arm. Alternatively, the card game may require the person to place the cards along a wide horizontal surface while standing. This modification in activity parameters provides opportunities for learning balance strategies while shifting the center of gravity in a lateral direction.
2. Other activities are designed to provide practice of actual task performance in real-life situations. Examples include direct practice in performing a morning self-care routine or getting into and out of an automobile. Practice of individualized roles in real-life situations is critical, but typically unfeasible during therapy sessions. Therefore, therapists need to structure homework assignments for stroke survivors to practice at home and to discuss at the next therapy session.
Task analysis
An occupational therapist assesses tasks of daily living in the environmental context in which the individual plans to perform each task. The therapist determines which skills are necessary for task performance and compares this analysis to the functional strengths and limitations exhibited by an individual stroke survivor. This task analysis enables the occupational therapist to plan an individualized treatment program that will improve relevant performance skills and enable the person to use compensatory strategies to overcome those limitations that show weak potential for significant improvement.
Analyzing an activity’s requirements for postural set
The occupational therapist determines the optimal “postural set” for performing a selected motor task. To perform the simple act of standing up, individuals must posturally set themselves in several ways. Both feet must be positioned on the floor in an appropriate base of support; perpendicular angles are established at the ankle, knee, and hip joints; and the pelvis is tilted anteriorly to free the lumbar spine for forward movement.13,51
When standing, people automatically change the configuration of their bases of support in anticipation of the direction toward which they expect to shift their body weight. If they plan to shift forward, as is done when reaching ahead, they will establish an anterior-posterior base of support. If they plan to shift to the left or right, as is done when stepping laterally to position their bodies in front of a bathtub, they will establish a medial-lateral base of support. Persons with hemiplegia often assume postural support bases inappropriate for the upcoming activity. The occupational therapist facilitates future task performance by determining and then instructing the individual in choosing appropriate postural sets for specific activities. For example, assuming the most efficient postural set for standing in front of a toilet can determine whether a man will be able to safely urinate independently.
Just as appropriate postural sets are important precursors to efficient motor performance, preplanning is also instrumental in determining the success of cognitively or visually challenging tasks. Activity analysis includes a determination of preliminary cognitive strategies that will facilitate task performance. For example, a person with right hemisphere dysfunction may experience difficulty in spatially orienting a blouse or slacks for independent dressing. The individual may be unaware that, prior to the stroke, he used a quick and automatic process to visualize and orient the garments in relation to the body segments. The occupational therapist’s skill in activity analysis enables this person to develop a “set up” strategy, such as lining up each garment before attempting to complete the additional steps of dressing.
Analyzing activity requirements for weight shift and balance
Postural adjustments that serve as balance mechanisms during weight shift are often impaired after stroke.13,43,51 Understanding a task’s inherent balance challenges is critical for developing treatment goals and compensatory strategies. Success in shifting weight during activity performance can be facilitated greatly through appropriate postural sets. The importance of this class of prerequisite skills is important when bathing. If patients use a tub bench, they will need to posturally set themselves for a posterior weight shift from stand to sit onto the bench. Once sitting, they will need to rotate their pelvis and bring both legs into the tub. The next step will be to shift their weight laterally, while sitting, to position themselves on the tub bench. A forward weight shift will often be required to adjust the water, and significant challenges to a lateral weight shift when sitting may be presented when patients must wash their genitals. If patients step into the bathtub and stand under a shower, they must posturally set themselves for a lateral weight shift for entrance and exit to and from the tub or shower. Reaching up and down from the standing position will be a critical performance component for safe, independent completion of this activity. These performance component skills may be practiced often in other contexts, such as in activities that require similar balance adjustments while sitting and standing. However, they must ultimately be practiced in the context in which the actual bathing activity will take place.
Analyzing activity requirements for dissociation between body segments
Difficulty with dissociation between body segments is commonly associated with stroke.13,43,51 The occupational therapist assesses the type and magnitude of such dissociations in each analyzed performance area task. For example, to put on shoes and socks, patients must be able to dissociate their pelvis from the lumbar spine to anteriorly and posteriorly tilt the pelvis to cross one leg over the other. They will also need to dissociate their lumbar from their thoracic spine to achieve the trunk rotation required to reach their left hand to their right foot. If they use their paretic arm to assist with the task, disassociation between the scapula and thorax will be required, as will disassociation between the humerus and scapula. Determination of these requirements through activity analysis guides treatment and helps the stroke survivor understand the therapist’s rationale for choice of treatment methods.
Other aspects of task analysis
Various tasks require different levels of motor planning and motor sequencing. For patients with impairments in these areas, the therapist will determine the nature of each of their challenges within specific performance area activities. Finally, when stroke survivors demonstrate impairments in visuospatial or cognitive skills, the occupational therapist will carefully analyze each task’s unique challenges and assist individuals in developing strategies to meet these specific performance component requirements.
Activity analysis also enables the occupational therapist to determine strategies for task performance that will promote efficient movement patterns and be least likely to contribute to the development of secondary impairments. Strategies for relaxing excessive skeletal muscle activity and preventing abnormal postures are described in Chapters 10 and 13. The occupational therapist instructs the stroke survivor to incorporate these strategies into the routine performance of daily activities. In addition, activity analysis assists the therapist in determining which compensatory strategies or adaptive equipment will be most effective for each individual stroke survivor. See Chapters 15, 27, and 28.
Using activity to assess a client’s skills
Activity analysis enables occupational therapists to evaluate skill levels through observation of patients as they participate in selected tasks. The Árnadóttir OT-ADL Neurobehavioral Evaluation (A-ONE)3 provides a systematic framework for assessing cognitive and perceptual function through structured observations of activities of daily living performance. This tool is discussed further in Chapter 18.
Carr and Shepherd’s program for optimizing motor function after stroke12,13 describes a therapeutic strategy for evaluating motor skills in the context of task performance. The therapist analyzes a patient’s performance of a specific task and compares it with the optimal kinesiology associated with that task. A major focus of this analysis is to identify those factors that serve as obstacles (or blocks) to moving in efficient kinesiological patterns. When some patients with hemiparesis try to reach forward to grasp for a cup, they tend to use the entire shoulder girdle as one tightly bound unit instead of disassociating the scapula from the thorax or the humerus from the scapula.
Intervention strategies are directly determined from task analysis. In the previous example, the therapist would provide passive mobilization to reduce mechanical constraints and to enhance the patient’s internal awareness of available scapular motion. The patient would then practice reaching forward in a variety of contexts while the therapist provides manual guidance and structures placement of goal objects to maximize appropriate kinematic linkages. Strong backgrounds in kinesiology and movement analysis are helpful to the therapist when implementing a motor relearning approach.
Helping patients develop their own skills in activity analysis
An ultimate goal in stroke rehabilitation is for individuals to learn the strategy of analyzing activities in reference to their own functional strengths and impairments. During the occupational therapy process, therapists share their strategies for activity analysis and challenge patients to develop their own skills in this area. Midway through the treatment process, therapists present new tasks and require the stroke survivors to analyze each task’s inherent performance requirements. In addition, occupational therapists encourage individuals to develop their own alternative strategies for task performance. The therapist’s major role at this stage is to provide feedback about the safety and efficacy of the person’s ideas. Before treatment is terminated, stroke survivors should develop skill in activity analysis so that they have the confidence and capability to attempt an infinite variety of new tasks and roles.
Activity selection and synthesis
Occupational therapists select activities and modify task demands:
 To structure specific practice components within an activity, with the goal of improving internal skills
To structure specific practice components within an activity, with the goal of improving internal skills
 To adapt tasks so they will be easier or safer to perform, according to each individual’s demonstrated internal capacities, limitations, and interests
To adapt tasks so they will be easier or safer to perform, according to each individual’s demonstrated internal capacities, limitations, and interests
The following game of dominoes is an example of modifying activity parameters to elicit specific demands for motor practice. With full knowledge by the patient that the primary purpose of engaging in this game is to practice skills of forward reach and lateral pinch, the therapist modifies the height and distance of the table surface to provide sufficient, but not excessive, challenges to the GMP for forward reach. The therapist purposely places the dominoes on their sides, rather than flat, to encourage external rotation at the glenohumeral joint and supination at the forearm. The therapist also considers the interaction between the person’s balance adjustments and ability to control increasing numbers of degrees of freedom in movements of the hemiparetic arm. Based on prior and ongoing assessment, the therapist determines whether the person will perform the task while sitting or standing, and the amount of shift in center of gravity that will be required by positioning of the dominoes on the table.
When an occupational therapist modifies an activity to facilitate current performance, the focus is on external adaptations to compensate for unchanging internal limitations. Such modifications are discussed in Chapters 27 and 28. It is important for therapists to understand that both types of activity modification may be appropriate for a single individual. It is equally important that the stroke survivor clearly understands the purpose of each therapeutic activity.
Activity synthesis is unique for each individual. Although the occupational therapist applies carefully considered, general foundational concepts when planning treatment for stroke survivors, no textbook can provide specific activity formats that will be appropriate for groups of individuals, even if they all have the same diagnosis. Each stroke survivor has an individual constellation of abilities, limitations, interests, roles, and personal goals. Occupational therapists synthesize activities by modifying parameters of specific tasks in specific contexts to provide practice challenges or compensatory adaptations. This requires flexibility, creativity, and sensitivity to individual needs.
Review questions
1. How do the ICF and the Occupational Therapy Practice Framework each integrate medical and social models of disability? What interventions do occupational therapists provide to promote internal change within stroke survivors? What interventions do occupational therapists provide to change factors in a stroke survivor’s external environment?
2. How do “patterns of use” influence central nervous system reorganization after injury? What are implications to occupational therapy intervention with stroke survivors?
3. Which stroke survivors are candidates for CIMT? How can the theory of learned nonuse influence occupational therapy intervention for other stroke survivors?
4. From your knowledge of kinesiology, give specific examples of kinematic or kinetic linkages during normal movement.
5. Give two examples of strategies for community participation that will be valuable for stroke survivors to develop.
6. What aspects of motor skills are learned through implicit learning processes? What occupational therapy interventions are most effective in facilitating implicit learning?
7. What is contextual interference and how does it affect retention and transfer of learning? Describe three ways an occupational therapist can modify feedback or practice schedules to promote contextual interference.
8. What are the necessary substrates for stroke survivors to meet their maximal potential for recovery? How can therapeutic intervention influence these substrates?
9. Describe the difference between modifying activities to promote practice for skill recovery and modifying activities to help stroke survivors compensate for current limitations.
1. Akama K, Yamauchi H. Task performance and metacognitive -experiences in problem solving. Psychol Rep. 2004:94;2:715-722.
2. American Occupational Therapy Association. Occupational therapy practice framework. Domain and process (2nd ed). Am J Occ Ther. 2008;62:625-683.
3. Árnadóttir G. The brain and behavior: assessing cortical dysfunction through activities of daily living. St Louis: Mosby; 1990.
4. Bear MF, Connors BW, Paradiso MA. Neuroscience. exploring the brain, ed 3. Baltimore: Lippincott Williams and Wilkins. 2007.
5. Bernstein N. The coordination and regulation of movements. Elmsford, NY: Pergamon; 1967.
6. Boyd LA, Winstein CJ. Implicit motor-sequence learning in humans following unilateral stroke. The impact of practice and explicit knowledge. Neurosci Lett. 2001:298;1:65-69.
7. Brady F. A theoretical and empirical review of the contextual interference effect and the learning of motor skills. Quest. 1998;50:266-293.
8. Brady F. Contextual interference. A meta-analytic study. Percept Mot Skills. 2004;99:116-126.
9. Brodtmann A, Puce A, Darby D, Donnan G. fMRI demonstrates diaschisis in the extrastriate visual cortex. Stroke. 2007:38;8:2360-2363.
10. Butefisch CM. Plasticity in the human cerebral cortex. Lessons from the normal brain and from stroke. Neuroscientist. 2004:10;2:163-173.
11. Candler C, Meeuwsen H. Implicit learning in children with and without developmental coordination disorder. Am J Occup Ther. 2002;56(4):429-435.
12. Carr J, Shepherd R. Neurological rehabilitation. Optimizing motor performance. Oxford: Butterworth-Heinemann. 1998.
13. Carr JH, Shepherd RB. Stroke rehabilitation: Guidelines for exercise and training to optimize motor skill. Boston: Butterworth-Heinemann; 2003.
14. Fasoli SE, Trombly CA, Tickle-Degnen LT, Verfaellie MH. Effect of instructions on functional reach in persons with and without cerebrovascular accident. Am J Occup Ther. 2002:56;4:380.
15. French B, Thomas LH, Leathley MJ, et al. Repetitive task training for improving functional ability after stroke. Cochrane Database Syst Rev. 17(4), 2007. CD006073
16. Gentile AM. A working model of skill acquisition with application to teaching. Quest. 1972:17;1:3-23.
17. Gentile AM. Implicit and explicit processes during acquisition of functional skill. Scand J Occup Ther. 1998:5;1:7-16.
18. Giuffrida CG, Shea JB, Fairbrother JT. Differential transfer benefits of increased practice for constant, blocked, and serial practice schedules. J Mot Behav. 2002:34;4:353-365.
19. Golisz KM. Dynamic assessment and multicontext treatment of unilateral neglect. Top Stroke Rehabil. 1998:5;1:11-28.
20. Goverover Y, Johnston MV, Toglia J, Deluca J. Treatment to improve self-awareness in persons with acquired brain injury. Brain Inj. 2007;21(9):913-923.
21. Hall KG, Magill RA. Variability of practice and contextual interference in motor skill learning. J Mot Behav. 1995:27;4:299-309.
22. Hanlon R. Motor learning following unilateral stroke. Arch Phys Med Rehabil. 1996:77;8:811.
23. Hendricks HT, van Limbeek J Geurts AC, Hendricks HT, Zwartz MJ. Motor recovery after stroke. A systematic review of the literature. Arch Phys Med Rehabil. 2002:83;11:1629.
24. Higgins JR, Spaeth RK. Relationship between consistency of movement and environmental condition. Quest. 1972;17(1):61.
25. Higgins S. Motor skill acquisition. Phys Ther. 1991:71;2:123.
26. Hoffman AN, Malena RR, Westergom BP, et al. Environmental enrichment-mediated functional improvement after experimental traumatic brain injury is contingent on task-specific neurobehavioral experience. Neurosci Lett. 2008;431(3):226-230.
27. Humm JL, Kozlowski DA, James DC, et al. Use-dependent exacerbation of brain damage occurs during an early post-lesion vulnerable period. Brain Res. 1998:783;2:286-292.
28. Jarus T, Goverover Y. Effects of contextual interference and age on acquisition, retention, and transfer of motor skill. Percept Mot Skills. 1999;88(2):437-447.
29. Jarus T. Motor learning and occupational therapy. the organization of practice. Am J Occup Ther. 1994:48;9:810.
30. Jones TA, Allred RP, Adkins DL, et al. Remodeling the brain with behavioral experience after stroke. Stroke. 2009;40(3):S136-S138.
31. Kelso JAS. Relative timing in brain and behavior. Some observations about the generalized motor program and self-organized coordination dynamics. Human Movement Science. 1997:16;4:453-460.
32. Kwakkel G, Kollen B. Predicting improvement in the upper paretic limb after stroke. A longitudinal prospective study. Restor Neurol Neurosci. 2007:25;5-6:453-460.
33. Lai Q, Shea CH, Wulf G, Wright DL. Optimizing generalized motor program and parameter learning. Res Q Exerc Sport. 2000:71;1:10-24.
34. Lin KC, Wu CY, Tickle-Degnen L, Coster W. Enhancing occupational performance through occupationally embedded exercise. A meta-analytic review. Occup Ther J Res. 1997:17;1:25-47.
35. Ma HI, Trombly C. A synthesis of the effects of occupational therapy for persons with stroke, part II. Remediation. Am J Occ Ther. 2002:56;3:260-274.
36. Ma HI, Trombly CA, Robinson-Podolski C. The effect of context on skill acquisition and transfer. Am J Occup Ther. 1999:53;2:138-144.
37. Ma HI, Trombly CA. The comparison of motor performance between part and whole tasks in elderly persons. Am J Occup Ther. 2001;55(1):62-67.
38. Magill RA. Knowledge is more than we can talk about. Implicit learning in motor skill acquisition. Res Q Exerc Sport. 1998:69;2:104-110.
39. Mark VW, Taub E. Constraint-induced movement therapy for chronic stroke hemiparesis and other disabilities. Restor Neurol Neurosci. 2004:22;3-5:317-336.
40. Mountz JM. Nuclear medicine in the rehabilitative treatment evaluation in stroke recovery. Role of diaschisis resolution and cerebral reorganization. Eura Medicophys. 2007;43(2):221-239.
41. Neumann DA. Kinesiology of the musculoskeletal system: Foundations for physical rehabilitation. St Louis: Mosby; 2002.
42. Riesdal A, Zeng J, Johansson BB. Early training may exacerbate brain damage after focal brain ischemia in the rat. J Cereb Blood Flow Metab. 1999:19;9:997-1003.
43. Ryerson S, Levit K. Functional movement reeducation: A contemporary model for stroke rehabilitation. NewYork: Churchill Livingstone; 1997.
44. Sabari JS. Occupational therapy practice guidelines for adults with stroke. Bethesda, MD: AOTA Press; 2008.
45. Salmani AW, Schmidt RA, Walter CB. Knowledge of results and motor learning. a review and critical reappraisal. Psychol Bull. 1984:95;3:355.
46. Schmidt RA, Lee TD. Motor control and learning: a behavioral emphasis, ed 4. Champaign, IL: Human Kinetics; 2005.
47. Schmidt RA, Wulf G. Continuous concurrent feedback degrades skill learning. implications for training and simulation. Hum Factors. 1997:39;4:509-525.
48. Seitz RJ, Azari NP, Knorr U, et al. The role of diaschisis in stroke recovery. Stroke. 1999:30;9:1844-1850.
49. Seligman ME, Weiss J, Weinraub M, Schulman A. Coping behavior. learned helplessness, physiological change and learned inactivity. Behav Res Ther. 1980:18;5:459-512.
50. Seligman ME. Learned helplessness. Annu Rev Med. 1972;23:407-412.
51. Shumway-Cook A, Woollacott M. Motor control: theory and practical applications, ed 2. Philadelphia: Lippincott Williams & Wilkins; 2001.
52. Singer RN, Cauraugh JHL. The generalizability effect of learning strategies for categories of psychomotor skills. Quest. 1985;37(1):103.
53. Singer RN, Lidor R, Cauraugh JH. To be aware or not aware? What to think about while learning and performing a motor skill. Sport Psychol. 1993;7(1):19.
54. Ste-Marie DM, Clear SE, Findlay LC, Latimer AE. High levels of contextual interference enhance handwriting skills acquisition. J Mot Behav. 2004:36;1:115-126.
55. Taub E. Movement in nonhuman primates deprived of somatosensory feedback. Exerc Sport. 1976;4:74-335.
56. Toglia JP. A dynamic interactional model to cognitive rehabilitation. In: Katz N, editor. Cognition and occupation across the life span. Bethesda, MD: AOTA Press, 2005.
57. Toglia JT. Generalization of treatment. a multicontext approach to cognitive perceptual impairment in adults with brain injury. Am J Occup Ther. 1991:45;6:505.
58. Toglia J, Kirk U. Understanding awareness deficits following brain injury. Neurorehabilitation. 2000;15(1):57-70.
59. Trombly CA. Foreword. In: Smits JG, Smits-Boone EC, editors. Hand recovery after stroke. Boston: Butterworth Heinemann, 2000.
60. Trombly CA. Observations of improvement of reaching in five subjects with left hemiparesis. J Neurol Neurosurg Psychiatry. 1993;56(1):40.
61. Winstein CJ. Knowledge of results and motor learning—implications for physical therapy. Phys Ther. 1991:71;2:140.
62. Wolf SL, Winstein CJ, Miller JP, et al. Effect of constraint-induced movement therapy on upper extremity function 3 to 9 months after stroke. The EXCITE randomized clinical trial. JAMA. 2006:296;17:2095-2104.
63. Wolf SL, Winstein CJ, Miller JP, et al. Retention of upper limb function in stroke survivors who have received constraint-induced movement therapy. The EXCITE randomized trial. Lancet Neurol. 2008:7;1:33-40.
64. World Health Organization. International classification of function. Geneva: The Organization; 2001.
65. Wu CY, Trombly CA, Lin LC, Tickle-Degnen L. A kinematic study of contextual effects on reaching performance in persons with and without stroke. Influences of object availability. Arch Phys Med Rehabil. 2000:81;1:95-101.
66. Wulf G, Hoss M, Prinz W. Instructions for motor learning. Differential effects of internal versus external focus of attention. J Mot Behav. 1998:30;2:169.