Administering Oral, Topical, and Inhalant Medications
Upon completing this chapter, you should be able to:
1 Describe the legal and professional responsibilities of the LPN/LVN related to medication administration.
2 List the different classifications of drugs based on their specific actions.
3 Identify the parts of a valid medication order.
4 Compare and contrast various medication record systems such as the medication administration record (MAR), medication cards, and computerized systems.
5 Discuss medication dispensing and delivery systems.
6 Discuss the advantages and disadvantages of the unit-dose system and the prescription system.
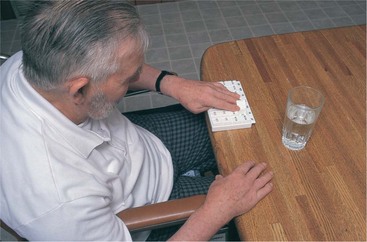
7 Consider special needs when administering oral and topical medications to an elderly patient.
8 Identify four principles to be followed when giving a medication through a feeding tube.
9 Discuss your responsibilities in the event of a medication error.
1 Demonstrate the accounting of doses of controlled drugs that must be withdrawn from the locked narcotics cabinet or dispensed from an automatic dispensing unit.
2 Give oral and topical medications using the Five Rights and five rules.
3 Prepare and apply topical medications such as eye ointments, eardrops, nasal medications, transdermal patches, and topical ointments.
4 Teach a patient to use a metered-dose inhaler.
5 Instill a vaginal and a rectal suppository safely and effectively.
6 Write a care plan for a patient who is receiving medication to include patient specific data, an identified nursing diagnosis, and interventions that you used.
7 Document medication administration and your patient’s response to the therapy.
NURSING RESPONSIBILITIES IN MEDICATION ADMINISTRATION
Accuracy during all steps of medication administration is extremely important. Medications are chemicals that alter actions performed by cells of the body. If the wrong medication is given to a patient, it could have serious consequences. All procedures related to medication administration should be followed exactly to promote safety and avoid making a medication error. However, should an error be made, report it promptly in accordance with agency policy and take appropriate action to promote patient safety and well-being.
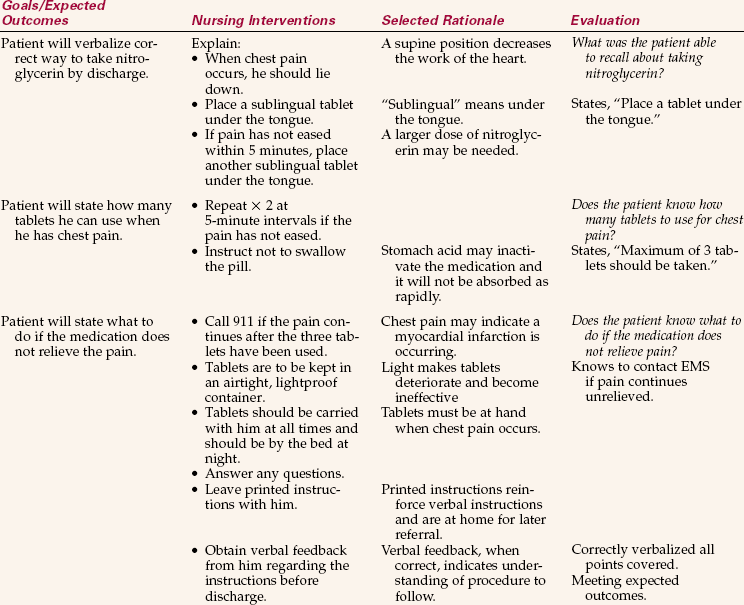
To administer medications, you must be able to interpret the medication order correctly and then give the correct medication to the patient. The procedures for administering medications accurately using the various routes can be mastered with practice. Attentiveness to each step of the task is essential when administering medications. Nurses are legally responsible for being knowledgeable about each medication they administer to patients: the correct dose, the route by which it should be given, desired effects, side effects, interactions with other medications, and any contraindications. Medication orders that are unclear, incomplete, or ambiguous should be questioned to avoid errors. Assessment of the patient after medication has been administered provides data for evaluating the effectiveness of the drug and guiding health teaching. On discharge from the health care facility, patients need to know how often to take each drug, if the medication should be taken before or after meals, if certain foods or fluids should be avoided, the expected effect, what to do about side effects if they occur, and what to do if they forget to take a dose at the prescribed time. In accordance with 2009 National Patient Safety Goals, involving and educating patients and families in care and treatment is a safety measure.
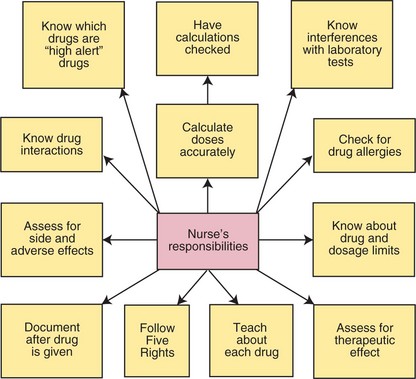
The Five Rights of medication administration provide a framework for safe delivery of drugs to patients (see Chapter 33). Box 34-1 presents pertinent National Patient Safety Goals of The Joint Commission as they relate to medication administration. Practice in the clinical setting helps establish a consistent, efficient routine for giving drugs. Concept Map 34-1 depicts the nurse’s responsibilities when administering medications.
CLASSIFICATION OF DRUGS
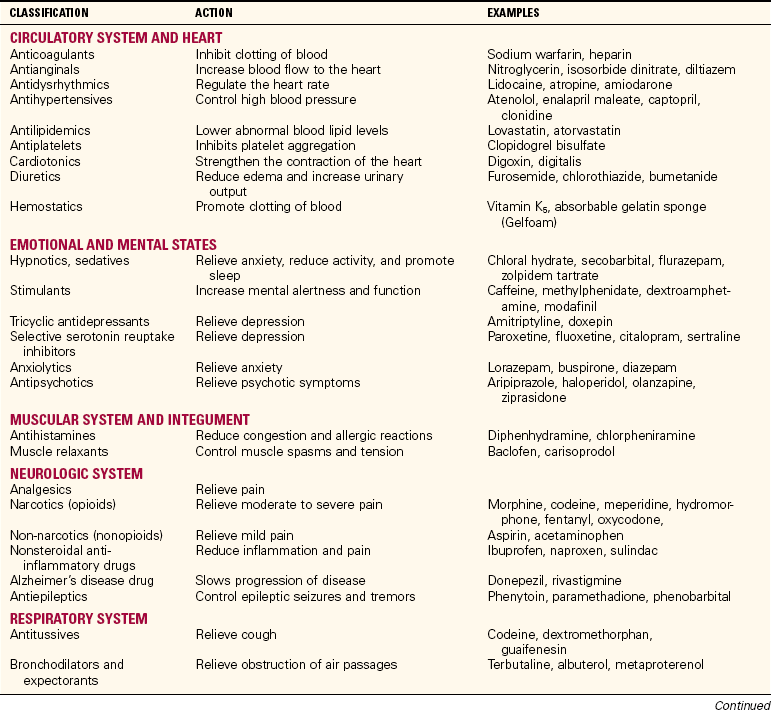
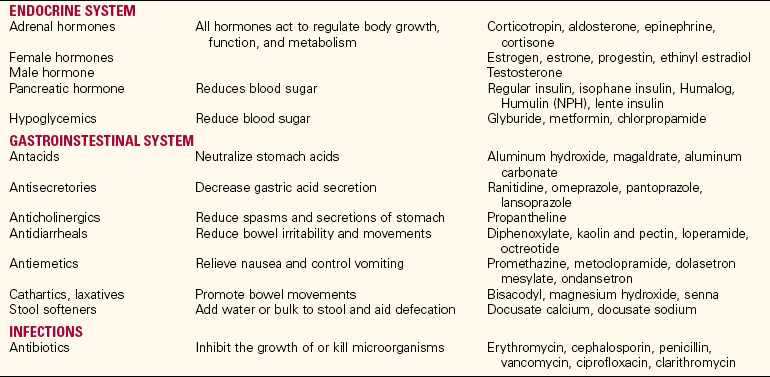
As mentioned in Chapter 33, drugs are classified in various ways. It is an advantage to learn drugs by the class to which they belong. To learn the possible side effects of each medication, begin by learning drugs by classification and then learn the most common side effects of the classification to which the drug belongs. Drugs are classified in various ways; one of the most useful is based on the effect of the drug on the body (Table 34-1). In this system, drugs that reduce pain and discomfort are classified as analgesics; those that control severe pain are potent analgesics or opioid narcotics, which may produce a stuporous state as a result of their effect on the central nervous system. For a complete list of drug classifications, consult a drug handbook or pharmacology textbook. The classification index in the Physicians’ Desk Reference also serves as a convenient reference.
Although there may be subdivisions within a class of drugs, the major side effects within that class will be the same. By learning the side effects of one major drug in the class, you will know what the major side effects of other similarly acting drugs in the class will be. This prevents the necessity of memorizing a multitude of separate facts about drug side effects. Different classifications and some examples of medications within each group are shown in Table 34-1.
MEDICATION ORDERS
The physician prescribes the type of treatment in a series of instructions written on the physician’s order sheet of the hospital chart. The written prescription for a drug is called the medication order or the drug order. Physicians’ orders are part of the patient record.
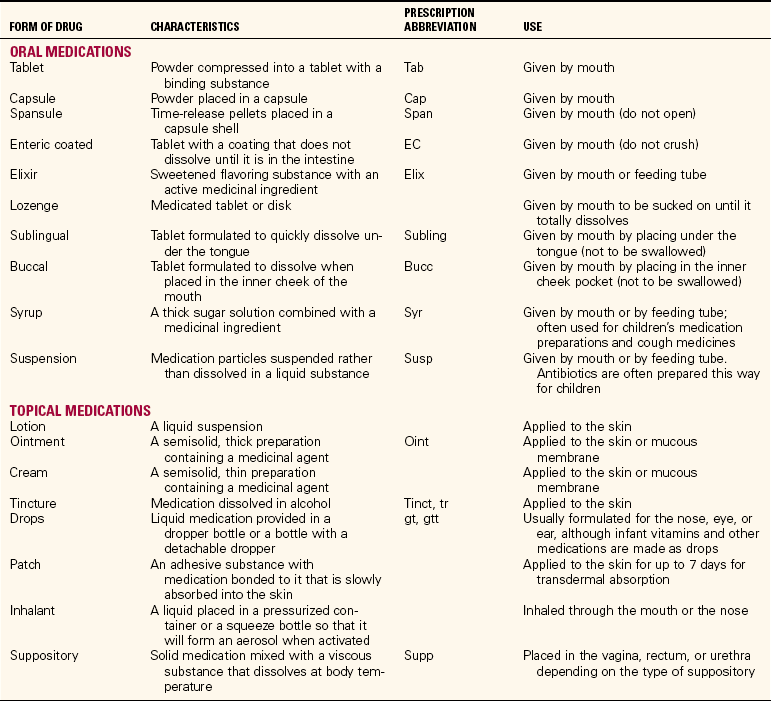
Medication orders must meet certain standards specified by state law and by regulations established by inspecting agencies. A complete drug order must include the full name of the patient, the name of the drug, the dosage to be given, the route of administration, how often it is to be given, the date and time written, and the signature of the prescriber. Some orders also specify the total number of doses that are to be given. Examples of medication orders are given in Table 34-2. Oral and topical medications come in many different forms (Table 34-3).
Table 34-2
| ORDER | MEANING |
| Digoxin 0.25 mg PO daily | Digoxin (a drug that strengthens the heart) in a dose of 0.25 mg to be given orally every day |
| Methylprednisolone 4 mg PO qid | Methylprednisolone (a type of cortisone) in a dose of 4 mg to be given orally four times a day |
| Maalox 30 mL PO q2h when awake | Maalox (an antacid) in a dose of 30 mL to be given orally every 2 hours during waking hours |
DOSAGE OF MEDICATIONS
In Canada, the metric system is the only system of weight and measurement; although it is the primary system of measuring medication dosage in the United States, the apothecary system is still occasionally used. The apothecary system was brought to America from England during colonial times. You must be familiar with this system because it has not been fully phased out as yet. Although use of the metric system is the standard, you still need to be able to convert values from one system to the other. It is helpful to keep a table of conversion values in the area where medications are prepared to ensure accurate calculations (Table 34-4).
Each dose of medication should be taken from a labeled package or container clearly stating the name and dosage of the drug. There is widespread use of medications supplied as unit doses, with each dose packaged separately with its own label.
Checking any conversions and calculations for a divided dose with another colleague is recommended at all times as a medication safety measure. Consult pediatric textbooks for additional information about how to confirm dosages and to prepare divided doses of medications for infants and children.
ROUTES OF MEDICATION ADMINISTRATION
The selected route of administration depends on several factors: the condition of the patient, the nature of the drug (taste, stability, and so on), and the rate of absorption via one route versus another. The oral route (PO, or per os, which means “by mouth”) is used for many solid and liquid medications because it is the simplest, most convenient, and least expensive (see Table 34-3). Those patients who have difficulty swallowing pills must have them crushed and given mixed in some food or juice. Some pills cannot be crushed because this changes their effect on the body. In this case, ask the physician to order the medication in liquid form.
Topical medications are instilled in the form of eyedrops or eardrops, or applied as ointments, pastes, or lotions to the skin or mucous membrane. The rectal route is often used to give medications to children or for patients who are vomiting. (Skills detailing the procedures for giving solutions as enemas can be reviewed in Chapter 30.) A number of medications affecting the respiratory system are given as inhalants. Parenteral routes are used for injecting medications into the body tissues, commonly via subcutaneous, intramuscular, intravenous, percutaneous, and intradermal routes. These are described in detail in Chapters 35 and 36.
REGULARLY SCHEDULED MEDICATION ORDERS
To maintain the desired level of medication in the bloodstream, the drug may be given several times a day. The physician’s order will specify how often the medication is to be given, such as three times a day (tid), every 4 hours (q4h), and so forth.
Each health care agency has policies that designate the time of day corresponding to the frequency ordered by the physician. It is imperative that the agency policy be followed. For example, on some nursing units the schedule of times might be as follows:
| Order | Schedule |
| daily | 0900 |
| bid | 0900 and 1700 |
| tid | 0900, 1300, and 1700 |
| qid | 0900, 1300, 1700, and 2100 |
| q4h | 0100, 0500, 0900, 1300 (and so on) |
PRN MEDICATION ORDERS
Medications taken “as needed” (PRN or prn) are given in response to a patient’s request or when the need is indicated. Examples of these medications usually include analgesics (to control pain), tranquilizers or sedatives (for restlessness), and laxatives (for constipation). Some PRN medication orders specify when or how often the medication can be given (e.g., at bedtime PRN, meaning “at bedtime as needed” and q 4 hr PRN, meaning “as often as every 4 hours as needed”). Table 34-5 shows two examples of PRN orders.
STAT AND SINGLE-DOSE MEDICATION ORDERS
Numerous occasions arise when a stat medication or a single dose of a drug must be given. The stat (give immediately) or single-time order may consist of more than one drug, or it may involve spacing the drops or tablets over a short period of time, such as when giving radiopaque tablets in preparation for a gallbladder series or eyedrops to dilate the pupils for refraction. Preoperative medications are prime examples of drugs given one time. Stat orders indicate that the order has top priority and the medication must be administered without delay. In emergencies, many orders are on a stat basis. The following are examples of stat and single-dose orders:
RENEWAL ORDERS
Drugs are potent and are capable of causing adverse reactions as well as the desired effects. Many drugs can result in drug addiction or drug dependency. Therefore, many hospitals have medication policies limiting the time for which certain types of medication orders are valid. Opiate analgesics generally have a 48- or 72-hour limit, sedatives and antibiotics may have a 5- or 7-day limit, and a 30-day limit may be imposed by some agencies on all medications. At the end of the specified period, the order is no longer considered valid, and no additional doses of the drug may be given. If you think the medication will need to be continued, phone the physician and obtain a new order rather than just holding the drug. The physician must give or write a renewal order to continue the medication.
STOP OR DISCONTINUE ORDERS
Medications are given to the patient until the specified number of doses has been administered or until the order has expired or has been canceled. Usually a change in medication is ordered by the physician, who writes a stop or discontinue order for one drug and then prescribes a new one. Examples of stop orders are “stop gentamicin” or “discontinue probenecid.” All medication orders are automatically canceled whenever a patient undergoes surgery or general anesthesia. New orders must be rewritten after surgery, even for routine medications.
MEDICATION RECORDS
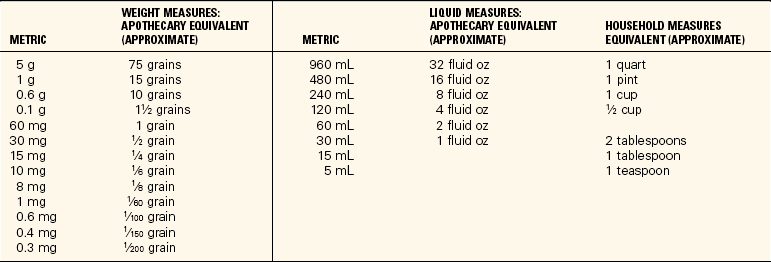
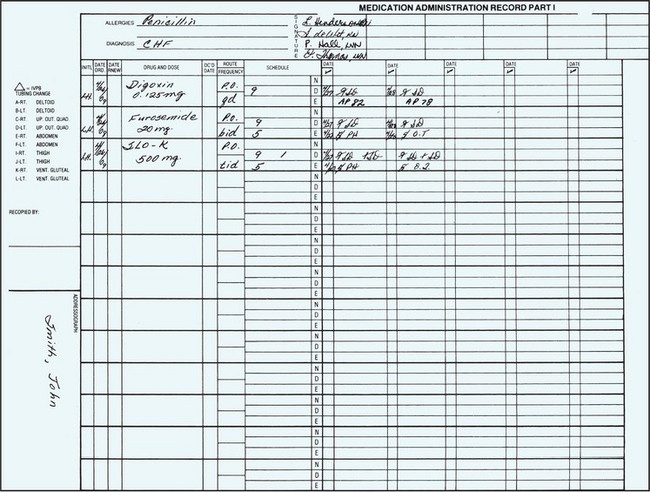
After the physician writes a medication order on the patient’s chart, it is transcribed onto the medication administration record (MAR). Medication orders are usually transcribed onto the patient’s MAR, on the computer-generated care plan, and/or on medication cards (Figure 34-1). Sometimes medications are listed on the patient’s Kardex card also.
MEDICATION ADMINISTRATION RECORD (MAR)
One of the forms commonly used to record a patient’s medications is the MAR, on which nurses record the doses of drugs administered each day. A copy of the MAR is placed on the patient’s chart. For added convenience, the forms may be in binders or in a special Kardex kept in the medication area and referred to when giving regularly scheduled and PRN medications.
MEDICATION CARDS
Medication cards are rarely used now, but may be encountered in small long-term care facilities or rehabilitation centers. For each patient, one card is made for each medication ordered. The card is used when the dose is prepared, at the bedside to help identify what is being given, and to chart after the medication is given. Information on the card includes patient’s name; room number; physician’s name; name of drug; dose, route, and time of administration; the date the order was written; and the initials of the person making the card.
MEDICATION ADMINISTRATION AND TECHNOLOGY
There is a rapid increase in the use of technology, such as computerized physician order entry (CPOE) systems, bar code scanners, and personal digital assistants (PDAs), to improve medication administration safety. In the CPOE system, the prescriber directly enters the medication order in the computer; this decreases potential for transcription errors. Other features of the CPOE system include alerts about drug interactions, nursing implications for administration, and updates on new drug information. CPOE also has the potential to incorporate patient-specific information such as allergies, laboratory results, or vital signs. Bar code scanners are used to scan the medication package and the patient ID bands. When scanning is combined with a patient-specific profile, an electronic cross-check of the five rights is ensured. PDAs are not currently widely used; however, in the future there is a potential for each nurse to download and upload specific patient information to a PDA that is connected to the larger hospital information system.
MEDICATION ADMINISTRATION SYSTEMS
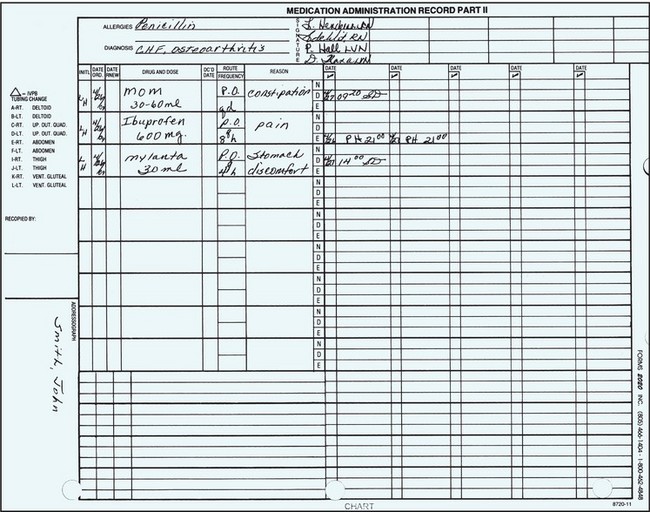
There are three types of medication administration systems: the stock supply of medicines, the individual prescription system, and the unit-dose method. The unit-dose system is the most commonly used medication administration system in health care agencies. The advantages of the unit-dose system and the individual prescription system have made the stock supply system less popular. The unit-dose system can be modified in various ways and can be operated from a stationary (fixed) or a mobile center where the medications are prepared.
The fixed site is generally a small medication room, a medication drawer in the patient’s room, or a station set aside for this purpose. MARs or medication cards and trays are commonly used as part of the medication procedure. The mobile method requires a cart that can be pushed from room to room as the medications are prepared and administered.
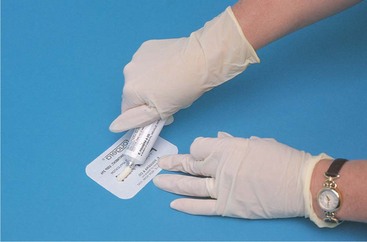
UNIT-DOSE SYSTEM
The unit-dose system provides a premeasured, prepackaged, and prelabeled dose of a medication for the patient (Figure 34-2). Almost all oral medications, liquids, suppositories, and lotions are now available in unit doses and in prefilled cartridges or syringes for injection. This system is considered safest because the dose prescribed is the dose dispensed. Medications dispensed using the unit-dose system may be administered from a mobile cart or from the fixed medication preparation center. The medication is opened at the bedside. It is customary to keep medication records in a binder or Kardex file on top of the cart from which medications are administered.
The unit-dose system provides a number of benefits. The pharmacy supplies the exact dose of medication ordered, and each dose is administered at the bedside, enhancing patient safety and reducing medication errors. The system also saves time for the nurse. Another benefit is that the patient is charged only for medications that are used. Finally, this system allows keeping a minimum amount of drugs on the nursing units.
PRESCRIPTION SYSTEM
The prescription system is similar to the unit-dose system except that a sufficient number of doses for several days are supplied. This system is used in pharmacies in the community and in outpatient clinics. As the name implies, a prescription is written for each drug ordered and is filled by the pharmacist, who then provides individual containers holding doses for several days.
The prescription system can be used in connection with a fixed or a mobile preparation site. Its advantages include the fact that only a limited amount of drugs needs to be kept on the nursing units. In the long-term care facility, a week’s or month’s supply of each medication is often provided in a bubble pack. Each day’s dose is pushed out of a bubble on the pack as needed. Home care patients use prescription system–prepared drugs from the local pharmacy or by-mail pharmacies.
PREPARATION OF ORAL CONTROLLED SUBSTANCES FROM A DISPENSER
A controlled dispensing system is used for distributing opiate analgesics and hypnotics (Figure 34-3). Legally controlled substances must be under lock and key at all times. Automated controlled-substance dispensing machines are often used in the clinical setting to monitor and control narcotic use (Figure 34-4). A significant advantage of this type of system is that a code number is used to enter the system. This eliminates the problem of having to find the nurse who has the keys to the locked cabinet and increases efficiency. Each nurse has a password by which to gain entry to the system.
When not in a dispensing machine, the drugs are supplied in a controlled dispenser or a commercially prepared package. Most medications are supplied in small pull-strip boxes with a roll of numbered doses of a particular medication. These often have 25 tablets or capsules per box. The first pill to be dispensed is numbered “25,” so that there is an accurate count of the remaining pills in the box. Tablets or capsules may be prepared in plastic sectioned containers, usually with 25 compartments clearly marked on top of the container as number 25, 24, 23, and so forth. The top surface of the container is movable, so that when the small opening in the cover is centered over one of the compartments, the container can be inverted over the medicine cup and the tablet or capsule falls into the cup without being handled. Each dose given must be accounted for and the number remaining verified at the time each shift counts the controlled substances before handing over the keys to the compartment to the next shift. One nurse from the oncoming shift and one nurse from the shift going off duty do the count together. Any discrepancy must be resolved before the nurses on the ending shift leave the unit.
As soon as the medicine has been dispensed, verify the label on the dispenser with the patient’s medication record. Replace the dispenser. Record the medication on the proof-of-use form and administer the drug to the patient. At the end of the shift, the remaining controlled drugs are counted, or a computerized count is obtained from the dispensing machine.
TOPICAL DRUGS
Topical drugs are applied externally to the skin and the mucous membranes; they may also have a systemic effect. Drug solutions instilled in the eye, ear, and nose are topical and act locally on these tissues. Other common forms of topical drugs include ointments, creams, pastes, liniments, and lotions that are used to treat local conditions. Drops and ointments for the eye must be sterile and nonirritating to the tissues. Solutions to be instilled in the eye, ear, or nose are generally prepared in dropper bottles.
Ointments are medicines manufactured in an oily base, such as petrolatum or lanolin, which keeps the drug in prolonged contact with the skin surface to obtain a soothing and anti-inflammatory effect. To protect against local infections, many contain antibiotics. Pastes are stiffer in consistency than ointments and do not melt at body temperature. Aluminum paste and zinc oxide are examples of pastes that are used to absorb secretions and protect the skin. Lotions and liniments are topical drugs in liquid form, such as calamine lotion, which are used to cool, soothe, and reduce inflammation or itching of the skin. Lotions are patted on gently, whereas liniments are rubbed into the skin. Liniments provide temporary relief of pain or soothing warmth by their action, which dilates the superficial blood vessels.
Suppositories are small cylinder-shaped, semisolid substances that are inserted into body orifices, such as the rectum, vagina, urethra, or ostomy stoma. Suppositories contain medication that is absorbed through mucous membranes.
Medications can also be dissolved in solutions and applied topically in the form of irrigations. Vaginal irrigations are the most common type of medicinal irrigation. Irrigations are presented in Chapter 38.
APPLICATION of the NURSING PROCESS
First check the order for each medication, noting the patient’s name, drug name, dosage, route, time, and the date the order was written to be certain it is still valid. Check the patient record for allergies. Determine why the patient is receiving the drug. If previous doses have been given, assess for therapeutic effect (the drug is working as intended). Assess for interactions among the drugs the patient is receiving. Check lab values and determine if there is any contraindication to taking the drug.
Assess what the patient knows about each medication and define learning needs. Assess for side effects to the drug if previous doses have been given. Decide whether the route in which the drug is ordered will be effective for the patient. For example, if the patient is nauseated, an oral dose may not be retained. Assess for drugs that must be given with food or on an empty stomach so that timing of the dose will be appropriate. When topical medications are to be applied, assess for adverse effects such as inflammation, swelling, redness, or discharge.
Nursing Diagnosis
Look at the classification of each medication and determine how nursing diagnoses are related to each prescribed medication. A hospitalized patient has acute problems, but other chronic problems may also be present for which the patient is receiving medication. These chronic problems need to be addressed with nursing diagnoses on the care plan. For example, a patient who had a colon resection may also be diabetic and hypertensive. Patient care is often very complex. By looking at the medications patients are receiving that are unrelated to the primary condition for which they are hospitalized, chronic conditions can be uncovered and addressed. For example, if the patient is in the hospital for a hip replacement and the major nursing diagnosis on the care plan is Impaired physical mobility related to hip replacement, but the medication administration record includes digoxin (Lanoxin) as a scheduled medication, then the patient may also have the nursing diagnosis of Decreased cardiac output. Digoxin is given to increase contractility of the heart. A few examples of nursing diagnoses for which medications are part of the treatment plan include the following:
• Ineffective tissue perfusion related to increased blood pressure (antihypertensives)
• Ineffective tissue perfusion related to cardiac arrhythmia (antiarrhythmics)
• Impaired tissue integrity related to wound infection (antibiotics)
• Imbalanced nutrition: less than body requirements related to nausea (antiemetics)
• Deficient knowledge related to action or side effects of prescribed medications
Planning
Plan and incorporate times for medication administration into the daily shift work schedule. A grid on the daily worksheet for assigned patients and the times of their medications is very useful. Plan to take juice or crackers to the room when a patient’s medication is scheduled between meals and needs to be taken with food. If a patient has difficulty swallowing, plan time to sit the patient upright and coach in the swallowing process. Plan to assess for side effects of the medication before giving the next scheduled dose. The overall goals of medication administration are as follows:
• All medications ordered will be safely administered to each patient on time.
• Serious side effects of medication will be identified quickly.
• The medication will be effective.
• No allergic reaction to the medication will occur.
• The patient will understand why the drug is prescribed, adhere to the medication schedule, and report serious side effects.
Expected outcomes for the previous nursing diagnoses might be:
• Pain will be relieved for 3 hours after administration of analgesic.
• Blood pressure is controlled within normal limits by antihypertensive medication within 1 week.
• Heart rate is regular and without signs of atrial fibrillation while taking antiarrhythmic medication.
• Wound culture will be negative at the end of antibiotic therapy.
• Patient will eat a meal without nausea with antiemetic 30 minutes prior to the meal.
• Patient will verbalize the reason for the medication and the side effects that might occur before discharge.
Implementation
When preparing any medication, remember to check the label three times and to follow the five rights of medication administration. Always check for patient allergy to the medication before giving it, and document after administering the drug. Patient teaching is an integral part of medication administration (Communication Cues 34-1 and Nursing Care Plan 34-1).
Oral Medication
Oral drugs may be supplied as a tablet, capsule, spansule (time-released pellets put into a capsule), lozenge, or as a liquid in the form of a syrup, elixir, or suspension (Cultural Cues 34-1). When giving a drug in tablet or capsule form, be sure to offer sufficient water with which to swallow the medication. Some people want to take all their pills at once; others will want to take them one at a time. Remember: Any water that is used must be entered on the intake sheet if the patient is on intake and output recording (Skill 34-1). It is important to assess for side effects of the drug before giving another dose of the medication.
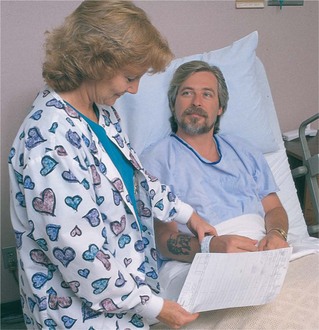
When preparing liquid medications, pour the dose into a graduated medicine cup. The exact level of the dose is read at the lowest point of the meniscus (curved upper surface) of the liquid in the cup when held at eye level (Figure 34-5). Always pour the liquid out the side of the bottle away from the label so that any residual liquid will not run down the label and distort the words on it.
Sublingual medications are placed under the tongue. They should never be swallowed. The drug dissolves in the sublingual pocket and is quickly absorbed by the vessels in the oral mucosa. Buccal medications are placed in the pocket between the teeth and the cheek. Swallowing these medications alters their absorption and may make them totally ineffective.
Eye and Ear Medications
Ophthalmic (eye) medications may be in the form of drops, ointment, or an eye disk. An error with an eye medication can cause significant damage, and it is imperative to check each medication very carefully before instilling it. The word ophthalmic must be clearly visible on the medication container and the medication must be in date. Skill 34-2 shows the steps for instilling eyedrops and eye ointment. Eye medications must be kept sterile. Careful hand hygiene is necessary before beginning the procedure.
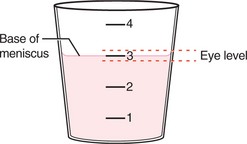
Otic (ear) medication is mostly used in children to decrease the pain of otitis media, but may also be used to treat external otitis and to soften cerumen (earwax) so that it can be removed more easily. Otic medication administration is presented in Steps 34-1, p. 670. For the child younger than 3 years, pull the ear lobe downward to straighten the canal; in the adult, pull the top of the pinna out and upward (Figure 34-6).
Nasal Medications
Nasal medications come in soft plastic atomizer or dropper bottles. An atomizer bottle contains decongestant, antihistamine, antibiotic, or steroid, depending on the patient’s need. To use an atomizer bottle, have the patient clear the nose as much as possible. While holding one nostril shut, insert the top of the atomizer into the other nostril. The patient squeezes the bottle while breathing in. The process is repeated on the other side (Safety Alert 34-2). One or two squirts per nostril is the usual dosage. The top of the bottle should be wiped clean before the cap is replaced.
When nose drops are prescribed, the patient should lie down face up, with the head off the bed and the neck hyperextended. The drops are pulled into the dropper by depressing the rubber top of the dropper while the stem is in the liquid and letting go. The tip of the dropper is held just above the nostril and the correct number of drops is gently expelled into the nostril by lightly squeezing the rubber top (Figure 34-7).The patient should remain in the head-back position for a few minutes.
Inhalation Medications
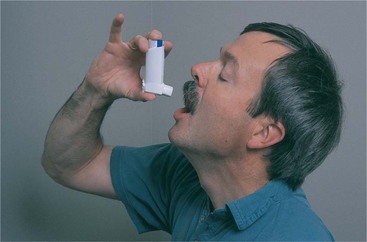
Inhalation therapy is used for patients with respiratory conditions, which can originate in any area from the nasal passageways to the deep lung tissues. Drugs used for inhalation therapy are always water soluble to ensure quick absorption into the respiratory system without creating tissue inflammation. Various mechanical devices are designed for aerosol treatment, such as atomizers, sprays, and hand-held metered-dose inhalers (Figure 34-8).
Metered-dose inhalers (MDIs) and nasal sprays come in containers labeled with directions for use. The MDI is held in front of the mouth, the cylinder for theinhalant is depressed, and a spray of medication is released. A variety of drugs are available in MDI form: antispasmodics, bronchodilators, mucolytic agents, proteolytic enzymes, and anti-inflammatories. Using a spacer with the device enhances delivery of the medication deeper into the bronchioles. Patients must be taught how to properly use an MDI (Figure 34-9 and Patient Teaching 34-1).
Short-acting insulin (Exubera) is now available in a new inhaled form. For type 2 diabetes, it may be used alone or in conjunction with dietary modifications, oral antidiabetic drugs, or injected insulin. For type 1 diabetes, this inhaled form maybe used along with injected intermediate or long-acting insulin. Exubera is contraindicated for patients with pulmonary disease or those who smoke. The medication is administered 10 minutes before a meal. Teach your patient that the medication is available in 1-mg and 3-mg blister packages; however, she should not substitute three 1-mg blisters for one 3-mg blister. This will result in an overdose. For additional information, consult www.exubera.com.
Five groups of drugs are commonly dispensed in inhalers for treatment of the lungs (Table 34-6). The patient should not take more than one drug from any one of the groups.
Table 34-6
Inhalant Drugs for Respiratory Problems
| DRUG | EXAMPLE |
| Beta-agonist drugs (stimulants) that open the small airways | Metaproterenol (Alupent), albuterol (Proventil, Ventolin), and terbutaline (Brethaire) |
| Anticholinergics used to decrease bronchospasm and open the large airways | Atropine, ipratropium (Atrovent) |
| Corticosteroids used to decrease inflammation | Beclomethasone (Beclovent, Vanceril), triamcinolone (Azmacort), and flunisolide (AeroBid) |
| Leukotriene modifiers for maintenance therapy of chronic asthma | Montelukast (Singulair) |
| Antiallergics used to decrease mucosal response to allergens | Cromolyn sodium (Intal) |
Vaginal Medications
A vaginal irrigation is also called a douche. Topical solution is introduced into the vaginal cavity for the following purposes:
• To cleanse the vagina in preparation for surgery
• To supply antiseptics to reduce bacterial growth
• To remove odors or foul discharge
• To apply heat or cold to soothe inflamed tissues or reduce oozing of blood
The normal secretions of the vaginal tissues are naturally acidic, which helps protect against vaginal infection. Vaginal irrigations are considered a clean procedure, except when given postoperatively or after childbirth, then principles of surgical asepsis are followed. Medicated solutions used for vaginal irrigations are 2% sodium bicarbonate solution, diluted hydrogen peroxide, povidone-iodine solution, a weak solution of acetic acid (1 tablespoon vinegar to 1000 mL of fluid), or a medication that is diluted in water. The amount of solution ranges from 1500 to 2000 mL, given slowly over a period of 10 to 15 minutes at a temperature of 100° to 105° F (37.7° to 40.5° C) unless the purpose is to apply heat; then it should be 110° F (43° C). The patient should receive instruction in the correct way to perform the irrigation (Patient Teaching 34-2).
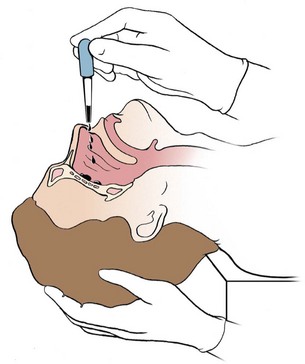
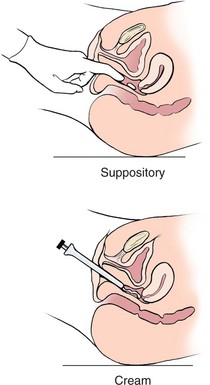
Other topical medications applied to the vagina are suppositories, ointments, and creams prescribed to treat infections and inflammation (Cultural Cues 34-2). Applicators are used for inserting the smaller vaginal suppositories at the distal end of the vagina. An applicator is also required for vaginal ointments. The applicator fits the top of the tube and enough medication is squeezed into the barrel to fill it, after which the applicator is inserted into the vagina, where the plunger deposits the ointment (Figure 34-10). After use, the applicator is washed with soap and water and stored for the patient’s futureuse, or it is discarded. The patient may be instructed on how to insert the medication herself. After medication has been inserted, a small pad or panty shield may be worn to keep from soiling clothing or bedding.
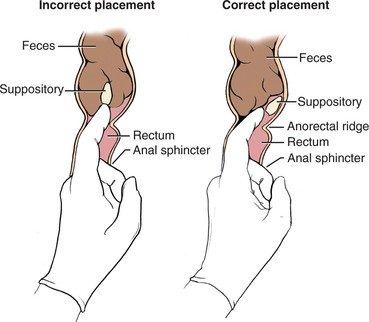
Rectal Medications
Rectal medications are dispensed in the form of suppositories (Figure 34-11). There are suppositories to prevent vomiting, soothe hemorrhoids, prevent bladder spasms, promote bowel evacuation, and reduce fever. See Steps 34-2 for the procedure to insert a rectal suppository.
Topical Skin Medications
Many types of topical medications can be applied to the skin. These types include lotions, ointments, creams, and patches. The steps for medication administration must be followed when applying any topical medication. Ointments, oils, lotions, and creams are combinations of skin emollients and a medication and are applied by rubbing into the skin. Skill 34-3 provides the steps for applying a topical skin preparation.
Transdermal (through the skin) medications are supplied in a sustained-release patch that is applied to clean, dry, hairless skin and left in place, or as a paste that is spread on a small area of skin. The drug is slowly absorbed through the skin and is absorbed into the bloodstream. Several types of drugs are now available in skin patch form: nitroglycerin to dilate coronary arteries, scopolamine to relieve motion sickness, estrogen to combat symptoms of menopause, nicotine to assist smoking cessation, and fentanyl, an opioid analgesic, for severe chronic pain. Skin patches should be applied to areas where there is adequate circulation, such as the chest, shoulders, or upper arm. Scopolamine patches are placed behind the ear. Each new patch should be applied to a different area so as not to irritate the skin. Hair should be removedbefore applying a patch. The effect of the medication from a skin patch will begin in about 30 minutes and may remain in the system for 30 minutes after the patch is removed. The patch should be dated and initialed so it is evident when it was applied (Assignment Considerations 34-1).
Nitroglycerin also is dispensed as a paste. It is applied to the skin, but not rubbed in. A ribbon of the ointment in the amount prescribed is applied to the measuring applicator, and the paper is folded to distribute the paste or a wooden applicator is used to spread the paste over a 2¼ × 3½-inch (5.6 × 8.8-cm) area of the paper. The paper is placed paste side down on a clean, nonhairy area of skin and taped into place. When one applicator is removed, the skin is cleansed and the next applicator is applied in a different, clean area.
Administering Medications via Feeding Tube
Many oral medications can be given through a feeding tube. Liquid medications are best, but if a tablet is crushable or a capsule can be opened and the contents mixed with liquid, or the liquid within the capsule can be aspirated with a needle and syringe, then the medication can be administered through the feeding tube. Medications that should not be crushed and administered through the tube are sublingual or buccal, enteric-coated, or sustained-release preparations or products with a carcinogenic potential (e.g., antineoplastics). For a small-bore tube, medications must be well dissolved in the liquid before administration. Do not mix the medication with a tube feeding because many things can interrupt or prevent delivery of the entire dose of medication. Skill 34-4 provides the steps for administering medications through a feeding tube.
Evaluation
Only by gathering evaluation data can it be determined whether the medication is effective. Evaluation for signs of adverse effects is essential before administration of the next dose. Sometimes signs and symptoms will not appear until after the prescription has been finished. Evaluation statements might be as follows:
• Experienced nausea within 30 minutes of taking antibiotic.
• Refused antihistamine; itching has subsided.
• White blood cell count is 7000/mm3, temperature 99° F (37.2° C); antibiotic effective.
• Red rash on chest possibly from antibiotic; physician notified.
• Verbalizes that she will take antihypertensive even if she feels well.
Evaluation statements indicating that the expected outcomes stated earlier in the chapter have been met include:
• Pain is relieved for 3½ hours by analgesic.
• Blood pressure is within normal range (e.g., 130/74) while the patient is taking antihypertensive medication.
• Heart rate is regular and within normal limits (e.g., 70 to 85/min) while patient is taking antiarrhythmic medication.
• Wound culture is negative after 5 days of antibiotic therapy.
• No nausea when antiemetic is taken 30 minutes before eating a meal.
• Patient verbalizes that medication “controls my blood pressure.”
Documentation
Documentation of medication administration is largely done on the MAR. PRN medications, one-time doses, and preoperative medications may also be charted in the nurse’s notes (follow agency policy). Data to be documented include the following:
• Medication name, dosage, route, and time administered
• Blood pressure and pulse before administration of antihypertensives and beta-blocker drugs
• Reason for a PRN medication’s administration
• Assessment data regarding side effects of the medication
• Patient teaching regarding the medication (Home Care Considerations 34-1)
• Evaluation data indicative of the effectiveness of medication
MEDICATION ERRORS
In the United States, an estimated 1.5 million patients are harmed each year by medication errors (Metules & Bauer, 2007) in spite of all the safeguards. When a medication error is discovered, it is reported immediately. An incident or occurrence form is filled out for the medication error, and the agency policy for reporting drug errors is followed. After notifying the physician, orders are carried out to safeguard the patient. All medication errors must be reported.The goal is to prevent harm to the patient from the error and to prevent similar errors from happening again. The nurse who discovers the error is the one to report it and fill out the report. Therefore, the nurse who made the error may not be the same nurse who reports it and fills out the occurrence form. In accordance with National Patient Safety Goals, health facilities and all health care workers should be supporting efforts to track and monitor adverse events to improve health care delivery systems.
NCLEX-PN © EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. The patient has returned from surgery several hours ago and is asking for pain medication. The nurse should give pain medication according to:
2. A nurse is caring for a patient who needs to have his morning dose of eyedrops to the right eye. Below are the steps for the procedure of instilling eyedrops. Place these steps (1 though 7) in the correct order.
______1. Document the doses given on the MAR.
______2. Stabilize the container above the eye over the conjunctival sac.
______3. Check the patient’s ID band, comparing it with the MAR.
______4. Block the entrance to the lacrimal gland by placing a finger over it.
______5. Drop the designated number of drops directly into the conjunctival sac without touching the surface of the eye.
______6. Ask the patient to look at the ceiling and tilt the head slightly to the side of the affected eye.
______7. Place the patient in a sitting or reclining position.
3. The final check of a medication dose should be done:
1. before leaving the medication cart or area.
2. before opening the dose at the patient’s bedside.
4. The nurse is performing the final check of the medication before administering it to the patient. Which information should be checked?
1. Patient’s name, birth date, room number, physician’s name, and drug dosage
2. Patient’s name, ID number, drug name, dosage, route, time, and drug allergies
3. Patient’s name, drug classification, dosage and date, and allergies
4. Patient’s name, birth date, ID number, and admitting diagnosis
5. A nursing student is preparing to give instructions to a patient on how to use a metered-dose inhaler. Which statement by the student nurse indicates that she knows what to tell the patient?
1. “I tell the patient to wait 10 minutes between puffs.”
2. “I teach him to close one nostril before depressing the canister.”
3. “I have him take in a deep breath and hold it before placing the mouthpiece.”
4. “I instruct him to inhale the medication and hold it for at least 10 seconds.”
6. When giving ear medication to a child younger than 3 years, the technique is to:
1. draw the earlobe slightly down and back.
2. pull the top of the pinna upward and back.
3. rotate the pinna until the eardrum is visualized.
4. apply gentle pressure to the face to ease the tissue forward.
7. After preparation of a liquid medication, the patient refuses it. What is the most appropriate nursing action?
1. Record the medication as “not taken” and discard it.
2. Record the dose as taken because it must be charged.
8. A nurse is preparing to give morning medication and he identifies a discrepancy between what the night shift nurse said in the shift report and what is written on the medication administration record (MAR). Which action would be the most appropriate?
1. Give the medication according to the MAR.
2. Call the night shift nurse at home.
9. An ambulatory surgery patient is to be discharged home and needs six doses of analgesic tablets for discomfort. What is the most appropriate nursing action?
1. Dispense six tablets from the controlled-substance dispenser.
2. Obtain a written prescription for the medication.
3. Call the hospital pharmacist to fill the order.
4. Ask the patient to call the physician’s office for the prescription.
10. A patient reports that he is taking an aspirin every day “to prevent heart attack” as well as Ecotrin (enteric-coated aspirin). Which nursing action is the priority?
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
You are in the medication room preparing medications for your patients when a nurse who is standing next to you is called to take a patient to another nursing unit. She shows you the medications she has prepared for one of her patients and asks you to please administer them so they will not be given late.
Scenario B
Dan Hartford is receiving ampicillin for a respiratory infection. When you go in to give him the next dose, you notice that his face seems to have a red rash on it. When you question him, he states he has been itching a little across his chest and on his legs.
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,