Principles of Uncomplicated Exodontia
PRESURGICAL MEDICAL ASSESSMENT
INDICATIONS FOR REMOVAL OF TEETH
CONTRAINDICATIONS TO THE REMOVAL OF TEETH
CLINICAL EVALUATION OF TEETH FOR REMOVAL
RADIOGRAPHIC EXAMINATION OF TOOTH FOR REMOVAL
PATIENT AND SURGEON PREPARATION
CHAIR POSITION FOR EXTRACTIONS
MECHANICAL PRINCIPLES INVOLVED IN TOOTH EXTRACTION
PRINCIPLES OF ELEVATOR AND FORCEPS USE
PROCEDURE FOR CLOSED EXTRACTION
SPECIFIC TECHNIQUES FOR REMOVAL OF EACH TOOTH
Extraction of a tooth is a procedure that combines the principles of surgery and principles from physics and mechanics. When these principles are applied correctly, a tooth can usually be removed from the alveolar process without untoward force or sequelae. This chapter presents the principles of surgery and mechanics related to uncomplicated tooth extraction. In addition, there is a detailed description of techniques for removal of specific teeth with specific instruments.
Proper tooth removal does not require a large amount of surgeon strength but rather should be accomplished with finesse. Removal of an erupted tooth involves the use of controlled force in a manner such that the tooth is not pulled from the bone, but instead is gently lifted from the alveolar process. During preextraction planning the degree of difficulty anticipated for removing a particular tooth is assessed. If that assessment leads the surgeon to believe that the degree of difficulty will be high or if initial attempts at tooth removal confirm this, a deliberate surgical approach—not an application of excessive force—should be taken. Excessive force may injure local soft tissues and damage surrounding bone and teeth. Moreover, excessive force and haste during an extraction heightens the intraoperative and postoperative discomfort and patient anxiety.
PAIN AND ANXIETY CONTROL
Removal of even a loose tooth causes pain. Thus profound local anesthesia is required to prevent pain during extractions. Local anesthesia must be absolutely profound to eliminate sensation from the pulp, periodontal ligament, and adjacent soft tissues. However, even with profound local anesthesia, patients will still experience discomfort from pressure placed on a tooth and surrounding tissues during most extractions.
Equally important is for the dentist to recognize the anxiety that usually exists in patients about to undergo tooth extraction. Few patients face this procedure with tranquility, and even stoic patients with no overt signs of anxiety are likely to have internal feelings of distress.
Local Anesthesia
Profound local anesthesia is needed if the tooth is to be removed without pain for the patient; therefore, it is essential that the surgeon remember the precise innervations of all teeth and surrounding soft tissue and the kinds of injection necessary to anesthetize those nerves completely. Table 7-1 summarizes the sensory innervation of the teeth and surrounding tissue. An important point to remember is that, in areas of nerve transition, cross-innervation exists. For example, in the region of the mandibular second premolar, the buccal soft tissues are innervated primarily by the mental branch of the inferior alveolar nerve but also by terminal branches of the long buccal nerve. Therefore, it is appropriate to supplement an inferior alveolar nerve block with a long buccal nerve block to achieve adequate anesthesia of the buccal soft tissue when extracting a lower second premolar.
TABLE 7-1
| Nerve | Teeth | Soft Tissue |
| Inferior alveolar nerve | All mandibular teeth | Buccal soft tissue of premolars, canine, and incisors |
| Lingual nerve | None | Lingual soft tissue of all teeth |
| Long buccal nerve | None | Buccal soft tissue of molars and second premolar |
| Anterior superior alveolar nerve | Maxillary incisors and canine tooth | Buccal soft tissue of incisors and canine |
| Middle superior alveolar nerve | Maxillary premolars and portion of first molar tooth | Buccal soft tissue of premolars |
| Posterior superior alveolar nerve | Maxillary molars except for portion of first molar tooth | Buccal soft tissue of molars |
| Anterior palatine nerve | None | Lingual soft tissue of molars and premolars |
| Nasopalatine nerve | None | Lingual soft tissue of incisors and canine |
When anesthetizing a maxillary tooth for extraction, the surgeon should anesthetize the adjacent teeth as well. During the extraction process the adjacent teeth are usually subjected to some pressure, which may be sufficient to cause pain. This is also true for mandibular extractions, but the mandibular block injection usually produces sufficient anesthesia to adjacent teeth.
Dense local anesthesia results in the loss of all pain, temperature, and touch sensations, but it does not anesthetize the proprioceptive fibers of the involved nerves. Thus during an extraction the patient feels a sensation of pressure, especially when the force is intense. The surgeon must therefore remember that the patient will need to distinguish between sharp pain and the dull, albeit intense, feeling of pressure when determining the adequacy of anesthesia.
Even with profound soft tissue anesthesia and apparent pulpal anesthesia, a patient may continue to have sharp pain as a tooth is luxated. This is especially likely when the teeth have a pulpitis or the surrounding soft and hard tissues are inflamed or infected. A technique that should be used in these situations is the periodontal ligament injection. When this injection is delivered properly and the local anesthetic solution is injected under pressure, immediate profound local anesthesia occurs in almost all situations. The anesthesia is short-lived, so the surgical procedure should be one that can be accomplished within 15 to 20 minutes.
One must keep in mind the pharmacology of the various local anesthetic solutions that are used so that they can be used properly. Table 7-2 summarizes the commonly used local anesthetics and the amount of time they can be expected to provide complete anesthesia. The surgeon must remember that pulpal anesthesia of maxillary teeth after local infiltration lasts a much shorter time than pulpal anesthesia of mandibular teeth after block anesthesia. In addition, pulpal anesthesia disappears 60 to 90 minutes before soft tissue anesthesia. Therefore, it is common that a patient has lip anesthesia but has lost pulpal anesthesia and may be experiencing pain.
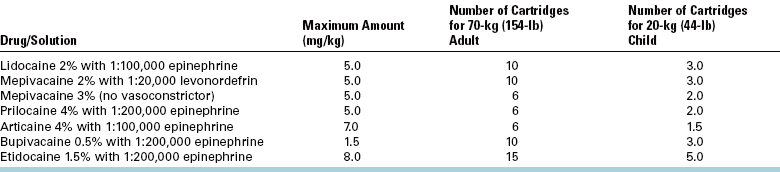
TABLE 7-2

*Group 1—local anesthetics without vasoconstrictors:
Only a certain amount of local anesthetic can be safely used in a given patient. To provide anesthesia for multiple tooth extractions, it may be necessary to inject multiple cartridges of local anesthetic. Thus it is important to know how many cartridges of a given local anesthetic solution can be administered safely. Table 7-3 summarizes (in two different ways) the maximum amounts of local anesthetic that can be used. First, each local anesthetic has a recommended maximum dose based on milligrams per kilogram. The second column in Table 7-3 indicates the number of cartridges that can safely be used on a healthy 154-lb (70-kg) adult. Rarely is it necessary to exceed this dose, even in patients larger than 154 lb. Patients who are smaller, especially children, should be given proportionally less local anesthetic. A common risky situation involving local anesthetic overdose is the small child to whom 3% mepivacaine (Carbocaine) is administered. For a child who weighs 44lb (20 kg), the recommended maximum amount of mepivacaine is 100 mg. If the child is given two cartridges of 1.8 mL each, the dose totals 108 mg. Therefore, a third cartridge of 3% mepivacaine should not be administered. As with any drug, the smallest amount of local anesthetic solution sufficient to provide profound anesthesia is the proper amount.
Although it is self-evident that local anesthesia is necessary for intraoperative pain control, the surgeon should also acknowledge its role in postoperative pain control. For routine extractions where only mild to moderate analgesics will be necessary, usually no additional local anesthetic is necessary. After procedures that have been more traumatic (e.g., the removal of impacted teeth) and where stronger analgesics are likely to be necessary, many surgeons use a long-lasting local anesthetic (e.g., bupivacaine) instead of or in addition to their usual local anesthetic. By doing this, the clinician provides the patient with 4 to 8 hours of local anesthesia with no pain. This method also allows adequate time for the patient to take the oral analgesics and for the analgesics to take effect before any discomfort begins.
Sedation
Management of patient anxiety must be a major consideration in oral surgical procedures. Anxiety is a more important factor in oral surgical procedures than in most other areas of dentistry. Patients are frequently already in pain and may be agitated and fatigued, both of which lower the patient’s ability to handle pain or pain-producing situations. Patients who are to have extractions may have preconceived notions or prior experiences of how painful such a procedure will be; they may have seen other patients, including family members, who have reported how painful it is to have a tooth extraction. Many are convinced that the procedure they are about to undergo will be very unpleasant. In addition, patients may experience certain psychological complications when oral surgical procedures are being performed. The removal of teeth causes a variety of reactions; a patient may mourn for lost body parts or perceive the extraction as a confirmation that youth has passed. This then adds to the presurgical anxiety present because of fear of pain.
Finally, anxiety is normal even in patients with positive past experiences with extractions because the procedure is truly uncomfortable. As noted previously, although the sharp pain is eliminated by local anesthetic, a considerable amount of pressure sensation still exists. Other noxious stimuli are present during an extraction procedure, such as the sounds of cracking of bone and clinking of instruments. For these reasons, prudent dentists use a planned method of anxiety control to prepare themselves and their patients for the anxiety associated with tooth extraction.
Anxiety control begins in most cases with a proper explanation of the planned procedure, including assurance that there will be no sharp pain and an expression of concern and empathy from the dentist. For the mildly anxious patient with a caring dentist, no pharmacologic assistance is typically necessary for routine extractions.
As patient anxiety increases, it often becomes necessary to use pharmacologic assistance. Fundamental to all anxiety-control techniques are a thorough explanation of the procedure and an expression of concern. These are augmented with drugs given in a variety of ways. Preoperatively orally administered drugs, such as diazepam, may provide a patient with rest the night before the surgery and some relief of anxiety in the morning. However, orally administered drugs are usually not profound enough to control moderate to severe anxiety once the patient enters the operative suite and are difficult to titrate.
Sedation by the inhalation of nitrous oxide is frequently the technique of choice for anxious patients and may be the only technique required for many patients who have mild to moderate anxiety. An extremely anxious patient who is to have several uncomplicated extractions may require deeper sedation, usually by the intravenous route. Sedation with anxiolytic drugs, such as using diazepam or midazolam with or without a narcotic, allows patients with moderate severe anxiety to undergo surgical procedures with minimal psychological stress. If the dentist is not skilled at using this modality, the patient should be referred to a surgeon who is trained to provide it.
PRESURGICAL MEDICAL ASSESSMENT
When evaluating a patient preoperatively, it is critical that the surgeon examine the patient’s medical status. Patients can have a variety of maladies that require treatment modification or medical management before the surgery can be performed safely. Special measures may be needed to control bleeding, lessen the chance of infection, and prevent worsening of the patient’s preexisting disease state. This information is discussed in detail in Chapter 1. The reader should refer to that chapter for information regarding the specifics of altering surgical treatment for medical management reasons.
INDICATIONS FOR REMOVAL OF TEETH
Teeth are extracted for a variety of reasons. This section discusses a variety of general indications for removing teeth. One must remember that these indications are guidelines and not absolute rules.
Caries
Perhaps the most common and widely accepted reason to remove a tooth is that it is so severely carious that it cannot be restored. The extent to which the tooth is carious and is considered to be nonrestorable is a judgment call to be made between the dentist and the patient. Sometimes the complexity and cost of steps required to salvage a severely carious tooth also makes extraction a reasonable choice. This is particularly true with the availability of reliable implant-supported prostheses.
Pulpal Necrosis
A second, closely aligned rationale for removing a tooth is the presence of pulp necrosis or irreversible pulpitis that is not amenable to endodontics. This may be the result of a patient declining endodontic treatment or of a root canal that is tortuous, calcified, and untreatable by standard endodontic techniques. Also included in this general indication category is the case in which endodontic treatment has been done but has failed to relieve pain or provide drainage, and the patient does not desire retreatment.
Periodontal Disease
A common reason for tooth removal is severe and extensive periodontal disease. If severe adult periodontitis has existed for some time, excessive bone loss and irreversible tooth mobility will be found. In these situations the hypermobile teeth should be extracted. Also ongoing periodontal bone loss may jeopardize the chance for straightforward implant placement, making extraction a sensible step before a tooth becomes mobile.
Orthodontic Reasons
Patients who are about to undergo orthodontic correction of crowded dentition frequently require the extraction of teeth to provide space for tooth alignment. The most commonly extracted teeth are the maxillary and mandibular premolars, but a mandibular incisor may occasionally need to be extracted for this same reason. Great care should be taken to ensure that extraction is indeed necessary and that the proper tooth or teeth are removed if someone other than the surgeon doing the extraction has asked for the extractions.
Malposed Teeth
Teeth that are malposed or malpositioned may be indicated for removal in several situations. If they traumatize soft tissue and cannot be repositioned by orthodontic treatment, they should be extracted. A common example of this is the maxillary third molar, which erupts in severe buccal version and causes ulceration and soft tissue trauma of the cheek. Another example is malposed teeth that are hypererupted because of the loss of teeth in the opposing arch. If prosthetic rehabilitation is to be carried out in the opposing arch, the hypererupted teeth may interfere with construction of an adequate prosthesis. In this situation the malposed teeth should be considered for extraction.
Cracked Teeth
An uncommon indication for extraction of teeth is a tooth with a cracked crown or a fractured root. The cracked tooth can be painful and is unmanageable by a more conservative technique. Even endodontic and complex restorative procedures cannot relieve the pain of a cracked tooth.
Impacted Teeth
Impacted teeth should be considered for removal. If it is clear that a partially impacted tooth is unable to erupt into a functional occlusion because of inadequate space, interference from adjacent teeth, or some other reason, it should be considered for surgical removal. See Chapter 9 for a more thorough discussion of this topic.
Supernumerary Teeth
Supernumerary teeth are usually impacted and should be removed. A supernumerary tooth may interfere with eruption of succedaneous teeth and has the potential for causing their resorption and displacement.
Teeth Associated with Pathologic Lesions
Teeth that are involved in pathologic lesions may require removal. In some situations the teeth can be retained and endodontic therapy performed. However, if maintaining the tooth compromises the complete surgical removal of the lesion when complete removal is critical, the tooth should be removed.
Radiation Therapy
Patients who are to receive radiation therapy for oral, head, or neck cancer should consider having teeth removed in the line of radiation therapy. However, many of these teeth can be retained with proper care. See Chapter 18 for a more thorough discussion of the effects of radiation therapy on the teeth and jaws.
Teeth Involved with Jaw Fractures
Patients who sustain fractures of the mandible or the alveolar process sometimes must have teeth removed. In some situations the tooth involved in the line of fracture can be maintained, but if the tooth is injured, infected, or severely luxated from the surrounding bony tissue or interferes with proper reduction and fixation of the fracture, its removal may be necessary.
Financial Issues
A final indication for removal of teeth relates to the financial status of the patient. All of the indications for extraction already mentioned may become stronger if the patient is unwilling or unable financially to support the decision to maintain the tooth. The inability of the patient to pay for the procedure or to take enough time from work to allow it to be performed may require that the tooth be removed. Also implant dentistry may be more cost-effective for a patient than maintaining a questionable tooth.
CONTRAINDICATIONS FOR THE REMOVAL OF TEETH
Even if a given tooth meets one of the requirements for removal, in some situations the tooth should not be removed because of other factors or contraindications to extraction. These factors, like the indications, are relative in their strength. In some situations the contraindication can be modified by the use of additional care or treatment, and the indicated extraction can be performed. In other situations, however, the contraindication may be so significant that the tooth should not be removed until the severity of the problem has been resolved. Generally the contraindications are divided into two groups: systemic and local.
Systemic Contraindications
Systemic contraindications preclude extraction because the patient’s systemic health is such that the ability to withstand the surgical insult may be compromised (see Chapter 1). One systemic contraindication is a group of conditions called severe uncontrolled metabolic diseases. Brittle diabetes and end-stage renal disease with severe uremia are part of this group. Patients with mild diabetes or well-controlled severe diabetes can be treated as reasonably normal patients. Only when the disease process becomes uncontrolled should the patient not have a tooth removed in a routine manner.
Patients who have uncontrolled leukemia and lymphoma should not have teeth removed until the malignancy can be brought under control. The potential complications are infection as a result of nonfunctioning white cells and excessive bleeding as a result of an inadequate number of platelets. Patients with any of a variety of severe uncontrolled cardiac diseases should also have their extractions deferred until the disease can be brought under control. Patients with severe myocardial ischemia, such as unstable angina pectoris, and patients who have had a recent significant myocardial infarction should not have a tooth extracted except as an emergency in the hospital setting. Patients who have malignant hypertension should also have extractions deferred, because persistent bleeding, acute myocardial insufficiency, and cerebrovascular accidents are more likely to occur as a result of stress caused by the extraction. Patients who have severe, uncontrolled cardiac dysrhythmias should have their extraction procedures deferred as well.
Pregnancy is a relative contraindication to extractions; patients who are in the first or third trimester should have their extractions deferred if possible. The latter part of the first trimester and the first month of the last trimester may be as safe as the middle trimester for a routine uncomplicated extraction, but more extensive surgical procedures requiring drugs other than local anesthetics should be deferred until after the child has been delivered.
Patients who have a severe bleeding diathesis, such as hemophilia, or severe platelet disorders should not have teeth extracted until the coagulopathy has been corrected. Most severe bleeding disorders can be controlled by the administration of coagulation factors or platelet transfusions. Close coordination with the patient’s hematologist can result in an uncomplicated recovery from the extraction procedure in most situations. Similarly, patients who take anticoagulants can have routine extractions performed when care is taken to manage the patient appropriately.
Finally, patients who take or have taken a variety of medications should have surgery performed with caution. Drugs to watch for include corticosteroids, immunosuppressive agents, bisphosphonates, and cancer chemotherapeutic agents.
Local Contraindications
Extractions of indicated teeth have several local contraindications. The most important and most critical is a history of therapeutic radiation for cancer. Extractions performed in an area of radiation may result in osteoradionecrosis and therefore must be done with extreme caution. Chapter 18 discusses this in detail.
Teeth that are located within an area of tumor, especially a malignant tumor, should not be extracted. The surgical procedure for extraction could disseminate malignant cells and thereby seed metastases.
Patients who have severe pericoronitis around an impacted mandibular third molar should not have the tooth extracted until the pericoronitis has been treated. Nonsurgical treatment should include irrigations, antibiotics, and removal of the maxillary third molar if necessary to relieve impingement on the edematous soft tissue overlying the mandibular impaction. If the mandibular third molar is removed in the face of severe pericoronitis, the incidence of complications increases. If the pericoronitis is mild and the tooth can be removed easily, then immediate extraction may be performed.
Finally, the acute dentoalveolar abscess must be mentioned. Many prospective studies make it abundantly clear that the most rapid resolution of an infection resulting from pulpal necrosis is obtained when the tooth is removed as early as possible. Therefore, acute infection is not a contraindication to extraction. However, it may be difficult to extract such a tooth because the patient may not be able to open the mouth sufficiently wide, or it may be difficult to reach a state of profound local anesthesia. If access and anesthesia considerations can be met, the tooth should be removed as early as possible. Otherwise, antibiotic therapy should be started and extraction planned as soon as possible.
CLINICAL EVALUATION OF TEETH FOR REMOVAL
In the preoperative assessment period, the tooth to be extracted should be examined carefully to assess the difficulty of the extraction. A variety of factors must be specifically examined to make the appropriate assessment.
Access to the Tooth
The first factor to be examined in preoperative assessment is the extent to which the patient can open the mouth. Any limitation of opening may compromise the ability of the surgeon to do a routine uncomplicated extraction. If the patient’s opening is substantially compromised, the surgeon should plan for a surgical approach to the tooth instead of an elevator or forceps extraction. Additionally the surgeon should look for the cause of the reduction of opening. The most likely causes are trismus associated with infection around or in the muscles of mastication, temporomandibular joint (TMJ) dysfunction (especially internal joint derangement with displacement of the disk without reduction or TMJ ankylosis), and muscle fibrosis.
The location and position of the tooth to be extracted within a dental arch should be examined. A properly aligned tooth has a normal access for placement of elevators and forceps. However, crowded or otherwise malposed teeth may present difficulty in positioning the proper forceps onto the tooth for extraction. When access is a problem, a compromise forceps must be chosen or a surgical approach may be indicated.
Mobility of the Tooth
The mobility of the tooth to be extracted should be assessed preoperatively. Greater-than-normal mobility is frequently seen with severe periodontal disease. If the teeth are excessively mobile, an uncomplicated tooth removal should be expected, but there may be more complicated soft tissue management after the extraction (Fig. 7-1, A).
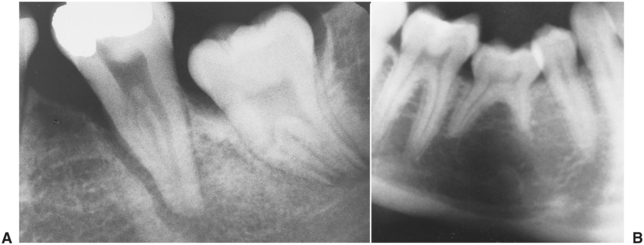
FIGURE 7-1 A, Tooth with severe periodontal disease with bone loss and wide periodontal ligament space. This kind of tooth is easy to remove. B, Retained mandibular second primary molar with an absent succedaneous tooth. The molar is partially submerged, and likelihood for ankylosed roots is high.
Teeth that have less-than-normal mobility should be carefully assessed for the presence of hypercementosis or ankylosis of the roots. Ankylosis is often seen with primary molars that are retained and have become submerged (Fig. 7-1, B); in addition, ankylosis is seen occasionally in nonvital teeth that have had endodontic therapy many years before the extraction. If the clinician believes that the tooth is ankylosed, it is wise to plan for a surgical removal of the tooth as opposed to a forceps extraction.
Condition of the Crown
The assessment of the crown of the tooth before the extraction should be related to the presence of large caries or restorations in the crown. If large portions of the crown have been destroyed by caries, the likelihood of crushing the crown during the extraction is increased, thus causing more difficulty in removing the tooth (Fig. 7-2). Similarly, the presence of large amalgam restorations produces a weakness in the crown, and the restoration will probably fracture during the extraction process (Fig. 7-3). In addition, a tooth that has been endodontically treated becomes desiccated and crumbles easily when force is applied. In these three situations it is critical that the tooth be elevated as much as possible and that the forceps then be applied as far apically as possible so as to grasp the root portion of the tooth instead of the crown.

FIGURE 7-2 Teeth with large carious lesions are likely to fracture during extraction, making extraction more difficult.
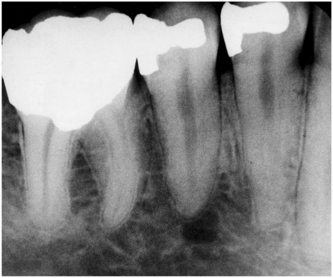
FIGURE 7-3 Teeth with large amalgam restorations are likely to be fragile and to fracture when extraction forces are applied.
If the tooth to be extracted has a large accumulation of calculus, the gross accumulation should be removed with a scaler or ultrasonic cleaner before extraction. The reasons for this are that calculus interferes with the placement of the forceps in the appropriate fashion, and fractured calculus may contaminate the empty tooth socket once the tooth is extracted.
The surgeon should also assess the condition of the adjacent teeth. If the adjacent teeth have large amalgams or crowns or have had endodontic therapy, it is important to keep this in mind when elevators and forceps are used to mobilize and remove the indicated tooth. If the adjacent teeth have large restorations, the surgeon should use elevators with extreme caution because fracture or displacement of the restorations may occur (Fig. 7-4). The patient should be informed before the surgical procedure about possible damage to these restorations during the informed consent process.
RADIOGRAPHIC EXAMINATION OF TOOTH FOR REMOVAL
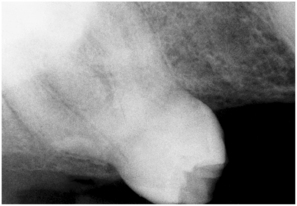
It is essential that proper radiographs be taken of any tooth to be removed. In general, periapical radiographs provide the most accurate and detailed information concerning the tooth, its roots, and the surrounding tissue. Panoramic radiographs are used frequently, but their greatest usefulness is for impacted teeth as opposed to erupted teeth.
For radiographs to have their maximal value, they must meet certain criteria. First of all, radiographs must be properly exposed, with adequate penetration and good contrast. The radiographic film or sensor should have been properly positioned so that it shows all portions of the crown and roots of the tooth under consideration without distortion (Fig. 7-5). If not using digital imaging, the radiograph must be properly processed, with good fixation, drying, and mounting. The mounting should be labeled with the patient’s name and the date on which the film was exposed. The radiograph should be mounted in the American Dental Association standardized method, which is to view the radiograph as if looking at the patient; the raised dot on the film faces the observer. The radiograph should be reasonably current so as to depict the presently existing situation. Radiographs older than 1 year should probably be retaken before surgery. Finally, nondigital radiographs must be mounted on a view box that is visible to the surgeon during the operation, and digital images should be displayed so the surgeon can easily look at them during extractions. Radiographs that are taken but not available during surgery are of limited value.
The relationship of the tooth to be extracted to adjacent erupted and unerupted teeth should be noted. If the tooth is a primary tooth, the relationship of its roots to the underlying succedaneous tooth should be carefully considered. The extraction of the primary teeth possibly can injure or dislodge the underlying tooth. If surgical removal of a root or part of a root is necessary, the relationship of the root structures of adjacent teeth must be known. Bone removal should be performed judiciously whenever it is necessary, but it is particularly important to be careful if adjacent roots are close to the root being removed.
Relationship to Vital Structures
When performing extractions of the maxillary molars, it is essential to be aware of the proximity of the roots of the molars to the floor of the maxillary sinus. If only a thin layer of bone exists between the sinus and the roots of the molar teeth, the potential for perforation of the maxillary sinus during the extraction increases. Thus the surgical treatment plan may be altered to an open surgical technique, with division of the maxillary molar roots into individual roots before the extraction proceeds (Fig. 7-6).
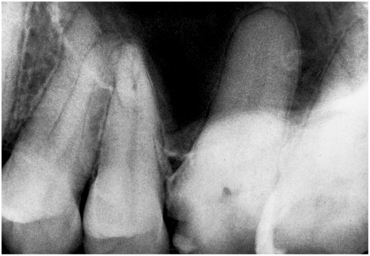
FIGURE 7-6 Maxillary molar teeth immediately adjacent to sinus present increased danger of sinus exposure.
The inferior alveolar canal may approximate the roots of the mandibular molars. Although the removal of an erupted tooth rarely impinges on the inferior alveolar canal, if an impacted tooth is to be removed, it is important that the relationship between the molar roots and the canal be assessed. Such an extraction may lead to injury of the canal and cause consequent damage to the inferior alveolar nerve (Fig. 7-7).
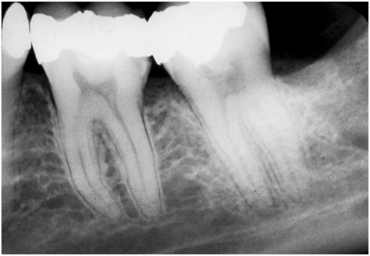
FIGURE 7-7 Mandibular molar teeth that are close to inferior alveolar canal. Third molar removal is a procedure most likely to result in injury to nerve.
Radiographs taken before the removal of mandibular premolar teeth should include the mental foramen. Should a surgical flap be required to retrieve a premolar root, it is essential that the surgeon know where the mental foramen is to avoid injuring the mental nerve during flap development (Fig. 7-3; Fig. 7-8).
Configuration of Roots
Radiographic assessment of the tooth to be extracted probably contributes most to the determination of difficulty of the extraction. The first factor to evaluate is the number of roots on the tooth to be extracted. Most teeth have the typical number of roots, in which case the surgical plan can be carried out in the usual fashion, but many teeth do have an abnormal number of roots. If the number of roots is known before the tooth is extracted, an alteration in the plan can be made to prevent fracture of the additional roots (Fig. 7-9).
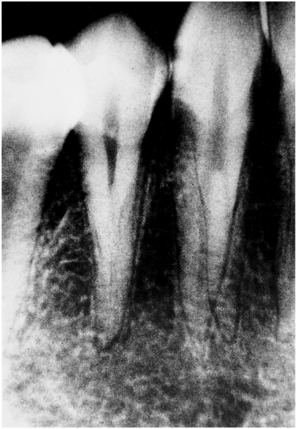
FIGURE 7-9 Mandibular canine tooth with two roots. Knowledge of this fact preoperatively may result in less traumatic extraction.
The surgeon must know the curvature of the roots and the degree of root divergence to plan the extraction procedure. Roots of the usual number and of average size may still diverge substantially and thus make the total root width so wide that it prevents extraction with forceps. In situations of excess curvature with wide divergence, surgical extraction may be required with planned division of the crown (Fig. 7-10).
The shape of the individual root must be taken into consideration. Roots may have short, conic shapes that make them easy to remove. However, long roots with severe and abrupt curves or hooks at their apical end are more difficult to remove. The surgeon must have knowledge of the shapes of the roots before surgery to plan adequately (Fig. 7-11).
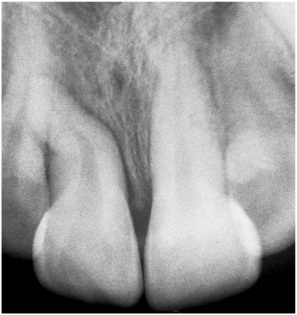
FIGURE 7-11 Curvature of roots of this tooth is unexpected. Preoperative radiographs allow surgeon to plan extraction more carefully.
The size of the root must be assessed. Teeth with short roots are easier to remove than teeth with long roots. A long root that is bulbous as a result of hypercementosis is even more difficult to remove. The periapical radiographs of older patients should be examined carefully for evidence of hypercementosis because this process seems to be a result of aging (Fig. 7-12).

FIGURE 7-12 Hypercementosis increases difficulty of these extractions because roots are larger at apical end than at cervical end. Surgical extraction will probably be required.
The surgeon should look for evidence of caries extending into the roots. Root caries may substantially weaken the root and make it more liable to fracture when the force of the forceps is applied (Fig. 7-13).
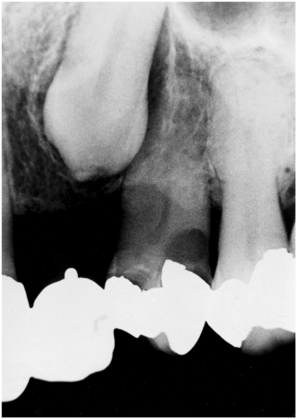
FIGURE 7-13 Root caries in first premolar tooth make extraction more difficult because fracture of tooth is likely. Note hypercementosis of second premolar.
Root resorption, internal or external, should be assessed on examination of the radiograph. Like root caries, root resorption weakens the root structure and renders it more likely to be fractured. Surgical extraction may be considered in situations of extensive root resorption (Fig. 7-14).
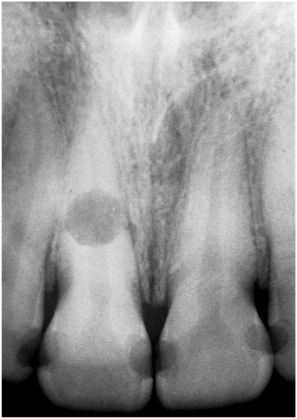
FIGURE 7-14 Internal resorption of root makes closed extraction almost impossible because fracture of root will almost surely occur.
The tooth should be evaluated for previous endodontic therapy. If there was endodontic therapy many years before the extraction process, there may be ankylosis or the tooth root may be more brittle. In both situations, surgical extraction may be indicated (Fig. 7-15).
Condition of Surrounding Bone
Careful examination of the periapical radiograph indicates the density of the bone surrounding the tooth to be extracted. Bone that is more radiolucent is likely to be less dense, which makes the extraction easier. However, if the bone appears to be radiographically opaque (indicating increased density) with evidence of condensing osteitis or other sclerosis-like processes, it will be more difficult to extract.
The surrounding bone should also be examined carefully for evidence of an apical pathologic condition. Teeth that have nonvital pulps may have periapical radiolucencies that represent granulomas or cysts. Awareness of the presence of such lesions is important because these teeth should be removed at the time of surgery (Fig. 7-16).
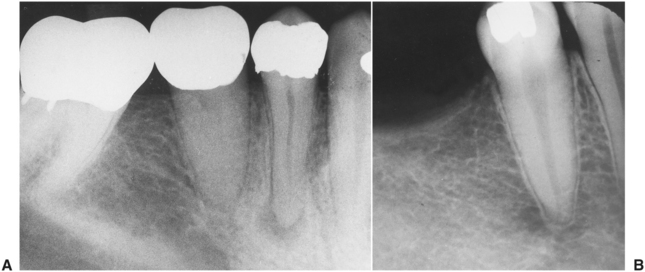
FIGURE 7-16 A, Periapical radiolucency. Surgeon must be aware of this before extraction to allow proper management. B, Periapical radiolucency around mandibular premolar represents mental foramen. Surgeon must be aware that this is not a pathologic condition. Intact lamina dura is noted in B but not in A.
PATIENT AND SURGEON PREPARATION
Surgeons must prevent inadvertent injury or transmission of infection to their patients or to themselves. The concept of universal precautions states that all patients must be viewed as having blood-borne diseases that can be transmitted to the surgical team and other patients. To prevent this transmission, surgical gloves, surgical mask, and eyewear with side-shields are required. (See Chapter 5 for a detailed discussion of this topic.) Additionally, most authorities recommend that the surgical team wear long-sleeved gowns that can be changed when they become visibly soiled (Fig. 7-17).

FIGURE 7-17 Surgeon, prepared by wearing protective eyeglasses, mask, and gloves. Surgeons should have short or pinned-back hair and should wear long-sleeved smocks that are changed daily or sooner if they become soiled. Patient should have waterproof drape.
If the surgeon has long hair, it is essential that the hair be held in position with barrettes or other holding devices and be covered with a surgical cap. A major breach in aseptic technique is to allow the surgeon’s hair to hang over the patient’s face.
Before the patient undergoes the surgical procedure, a minimal amount of draping is necessary. A sterile drape should be put across the patient’s chest to decrease the risk of contamination (Fig. 7-17).
Before the extraction, patients can be advised to rinse their mouths vigorously with an antiseptic mouth rinse such as chlorhexidine. This reduces the bacterial contamination in the patient’s mouth to some degree, which may help to reduce the incidence of postoperative infection.
To prevent teeth or fragments of teeth from falling into the mouth and potentially being swallowed or aspirated into the lungs, many surgeons prefer to place a partially unfolded 4 × 4-inch gauze loosely into the back of the mouth. This oral partition serves as a barrier so that, should a tooth slip from the forceps or shatter under the pressure of the forceps, it will be caught in the gauze rather than be swallowed or aspirated. The surgeon must take care that the gauze is not positioned so far posteriorly that it makes the patient gag. The surgeon should explain the purpose of the partition to gain the patient’s acceptance and cooperation for allowing the gauze to be placed.
CHAIR POSITION FOR EXTRACTIONS
The positions of the patient, chair, and operator are critical for successful completion of the extraction. The best position is one that is comfortable for the patient and surgeon and that allows the surgeon to have maximal control of the force that is being delivered to the patient’s tooth through the elevators and forceps. The correct position allows the surgeon to keep the arms close to the body and provides stability and support; it also allows the surgeon to keep the wrists straight enough to deliver the force with the arm and shoulder and not with the hand. The force delivered can thus be controlled in the face of sudden loss of resistance from a root or fracture of the bone.
Dentists usually stand during extractions, so the positions for a standing surgeon will be described first. Modifications that are necessary to operate in a seated position will be presented later. Also descriptions of techniques are for the right-handed operator. Left-handed surgeons should reverse the instructions when working on various quadrants.
For a maxillary extraction the chair should be tipped backward so that the maxillary occlusal plane is at an angle of about 60 degrees to the floor. Raising the patient’s legs at the same time helps improve the patient’s comfort. The height of the chair should be such that the height of the patient’s mouth is at or slightly below the operator’s elbow level (Fig. 7-18). Novices commonly have the chair too high. During an operation on the maxillary right quadrant, the patient’s head should be turned substantially toward the operator so that adequate access and visualization can be achieved (Fig. 7-19). For extraction of teeth in the maxillary anterior portion of the arch, the patient should be looking straight ahead (Fig. 7-20). The position for the maxillary left portion of the arch is similar, except that the patient’s head is turned slightly toward the operator (Fig. 7-21).

FIGURE 7-18 Patient positioned for maxillary extraction: tilted back so that maxillary occlusal plane is at about 60-degree angle to floor. Height of chair should put patient’s mouth slightly below surgeon’s elbow.

FIGURE 7-19 Extraction of teeth in maxillary right quadrant. Note that surgeon turns patient’s head toward self.

FIGURE 7-21 Patient with head turned slightly toward surgeon for extraction of maxillary left posterior teeth.
For the extraction of mandibular teeth, the patient should be positioned in a more upright position so that when the mouth is opened widely, the occlusal plane is parallel to the floor. A properly sized bite block should be used to stabilize the mandible when the extraction forceps are used. Even though the surgeon will support the jaw, the additional support provided by the bite block will result in less stress being transmitted to the jaws. Care should be taken to avoid using too large of a bite block because large ones can overstretch the TMJ ligaments and cause patient discomfort. The chair should be lower than for extraction of maxillary teeth, and the surgeon’s arm should be inclined downward to approximately a 120-degree angle at the elbow (Fig. 7-22), which provides a comfortable, stable position that is more controllable than the higher position. During removal of the mandibular right posterior teeth, the patient’s head should be turned severely toward the surgeon to allow adequate access to the jaw, and the surgeon should maintain the proper arm and hand position (Fig. 7-23). When removing teeth in the anterior region of the mandible, the surgeon should rotate around to the side of the patient (Figs. 7-24 and 7-25). When operating on the left posterior mandibular region, the surgeon should stand in front of the patient, but the patient’s head should not turn so severely toward the surgeon (Fig. 7-26).

FIGURE 7-22 For mandibular extractions, patient is more upright so that mandibular occlusal plane of opened mouth is parallel to floor. Height of chair is also lower to allow operator’s arm to be straighter.

FIGURE 7-24 For extraction of mandibular anterior teeth, surgeon stands at side of patient, who looks straight ahead.

FIGURE 7-25 When English style of forceps is used for anterior mandibular teeth, patient’s head is positioned straight.
Some surgeons prefer to approach the mandibular teeth from a posterior position. This allows the left hand of the surgeon to support the mandible better, but it requires that the forceps be held opposite the usual method and that the surgeon views the field with an upside-down perspective. The left hand of the surgeon goes around the patient’s head and supports the mandible. The usual behind-the-patient approach is seen in Figures 7-27 and 7-28.

FIGURE 7-27 Behind-the-patient approach for extraction of posterior right mandibular teeth. This allows surgeon to be in comfortable, stable position.

FIGURE 7-28 Behind-the-patient approach for extraction of posterior left mandibular teeth. Hand is positioned under forceps.
If the surgeon chooses to sit while performing extractions, several modifications must be made. For maxillary extractions, the patient is positioned in a reclining position similar to that used when the surgeon is standing. However, the patient is not reclined as much; therefore the maxillary occlusal plane is not perpendicular to the floor as it is when the surgeon is standing. The patient should be lowered as far as possible so that the level of the patient’s mouth is as near as possible to the surgeon’s elbow (Fig. 7-29). The arm and hand position for extraction of the maxillary anterior and posterior teeth is similar to the position used for the same extractions performed while standing (Fig. 7-30).

FIGURE 7-29 In seated position, patient is positioned as low as possible so that mouth is level with surgeon’s elbow.

FIGURE 7-30 For extraction of maxillary teeth, patient is reclined back approximately 60 degrees. Hand and forceps positions are same as for standing position.
As when the surgeon is standing, for extraction of teeth in the lower arch, the patient is a bit more upright than for extraction of maxillary teeth. The surgeon can work from the front of the patient (Figs. 7-31 and 7-32) or from behind the patient (Figs. 7-33 and 7-34). When the English style of forceps is used, the surgeon’s position is usually behind the patient (Fig. 7-35). It should be noted that the surgeon and the assistant have hand and arm positions similar to those used when the surgeon is in the standing position.

FIGURE 7-33 For removal of anterior teeth, surgeon moves to position behind patient so that mandible and alveolar process can be supported by surgeon’s other hand.
MECHANICAL PRINCIPLES INVOLVED IN TOOTH EXTRACTION
The removal of teeth from the alveolar process requires the use of the following mechanical principles and simple machines: the lever, wedge, and wheel and axle.
Elevators are used primarily as levers. A lever is a mechanism for transmitting a modest force—with the mechanical advantages of a long lever arm and a short effector arm—into a small movement against great resistance (Fig. 7-36). An example of the use of a level is when a Crane pick is inserted into a purchase point of a tooth and then is used to elevate the tooth (Fig. 7-37).

FIGURE 7-36 First-class lever transforms small force and large movement to small movement and large force.
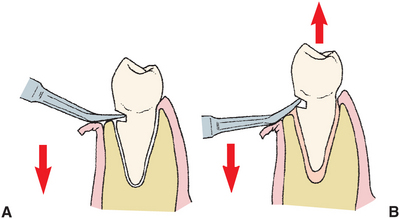
FIGURE 7-37 In removal of this mandibular premolar tooth, purchase point has been placed in tooth, which creates first-class lever situation. When Crane pick is inserted into purchase point and handle forces apically (A), tooth is elevated occlusally out of socket with buccoalveolar bone used as fulcrum (B).
The second machine that is useful is the wedge (Fig. 7-38). The wedge is useful in several different ways for the extraction of teeth. First, the beaks of the extraction forceps are usually narrow at their tips; they broaden as they go superiorly. When the forceps are used, there should be a conscious effort made to force the tips of the forceps into the periodontal ligament space at the bony crest to expand the bone and force the tooth out of the socket (Fig. 7-39). The wedge principle is also useful when a straight elevator is used to luxate a tooth from its socket. A small elevator is forced into the periodontal ligament space, which displaces the root toward the occlusion and therefore out of the socket (Fig. 7-40).
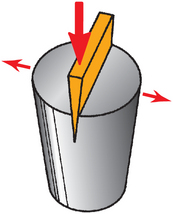
FIGURE 7-38 Wedge can be used to expand, split, and displace portions of substance that receives it.
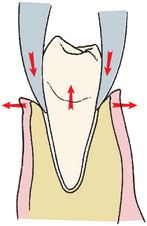
FIGURE 7-39 Beaks of forceps act as wedge to expand alveolar bone and displace tooth in occlusal direction.
The third machine used in tooth extraction is the wheel and axle, which is most closely identified with the triangular, or pennant-shaped, elevator. When one root of a multiple-rooted tooth is left in the alveolar process, the pennant-shaped elevator, like a Cryer, is positioned into the socket and turned. The handle then serves as the axle and the tip of the triangular elevator acts as a wheel and engages and elevates the tooth root from the socket (Fig. 7-41).
PRINCIPLES OF ELEVATOR AND FORCEPS USE
The primary instruments used to remove a tooth from the alveolar process are the elevator and extraction forceps. Elevators help in the luxation of a tooth, and forceps continue that process through bone expansion and disruption of periodontal attachments. The goal of forceps use is twofold: (1) expansion of the bony socket by use of the wedge-shaped beaks of the forceps and the movements of the tooth itself with the forceps, and (2) removal of the tooth from the socket.
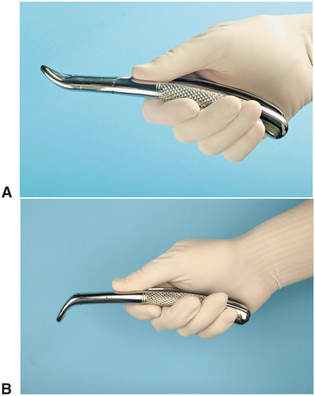
The dental elevator consists of a handle, shank, and blade. The handle of the elevator is usually in line with the shank and is enlarged to allow it to be grasped in the palm of the hand. The elevator may also have flattened areas for fingers to grasp to help direct the elevator. The handle can also be set perpendicular to the shank (cross bar–type elevators). The shank connects the handle to the blade. Blades can be straight, triangular (Cryer), curved (Potts), or pointed (Crane pick).
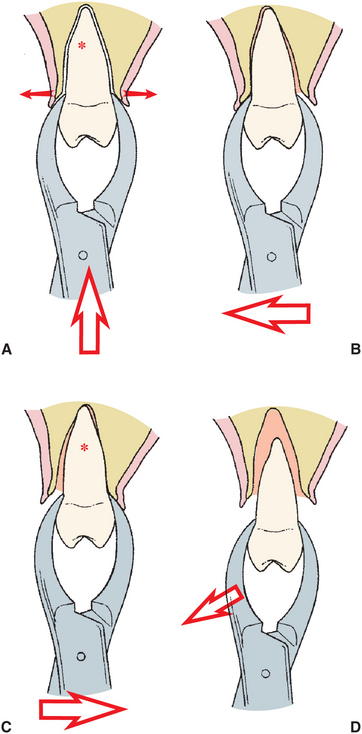
The forceps can apply five major motions to luxate the teeth and expand the bony socket: The first is apical pressure, which accomplishes two goals. Although the tooth moves in an apical direction minimally, the tooth socket is expanded by the insertion of the beaks down into the periodontal ligament space (Fig. 7-42). Thus apical pressure of the forceps on the tooth causes bony expansion. A second accomplishment of apical pressure is that the center of rotation of the tooth is displaced apically. Because the tooth is moving in response to the force placed on it by the forceps, the forceps become the instrument of expansion. If the fulcrum is high (Fig. 7-43), a larger amount of force is placed on the apical region of the tooth, which increases the chance of fracturing the root end. If the beaks of the forceps are forced into the periodontal ligament space, the center of rotation is moved apically, which results in greater movement of the expansion forces at the crest of the ridge and less force moving the apex of the tooth lingually (Fig. 7-44). This process decreases the chance for apical root fracture.
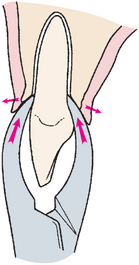
FIGURE 7-42 Extraction forceps should be seated with strong apical pressure to expand crestal bone and to displace center of rotation as far apically as possible.
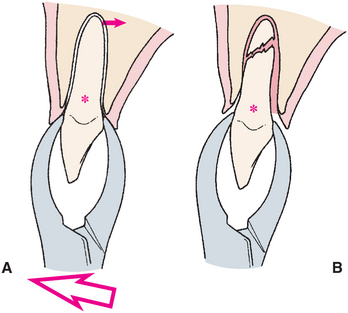
FIGURE 7-43 If center of rotation (*) is not far enough apically, it is too far occlusally, which results in excess movement of tooth apex (A). B, Excess motion of root apex caused by high center of rotation results in fracture of root apex.
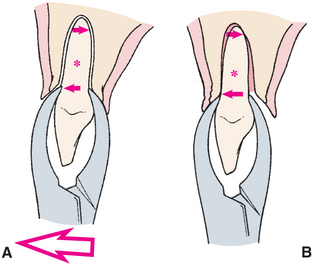
FIGURE 7-44 If forceps are apically seated, center of rotation (*) is displaced apically and less apical pressures are generated (A). This results in greater expansion of buccal cortex, less movement of apex of tooth, and therefore less chance of fracture of root (B).
The second major pressure or movement applied by forceps is the buccal force. Buccal pressures result in expansion of the buccal plate, particularly at the crest of the ridge (Fig. 7-45). Although buccal pressure causes expansion forces at the crest of the ridge, it is important to remember that it also causes lingual apical pressure. Thus, excessive force can fracture buccal bone or cause a fracture of the apical portion of the root.
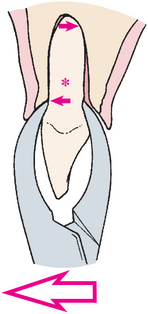
FIGURE 7-45 Buccal pressure applied to tooth will expand buccocortical plate toward crestal bone, with some lingual expansion at apical end of root. Asterisk, Center of rotation.
Third, lingual or palatal pressure is similar to the concept of buccal pressure but is aimed at expanding the linguocrestal bone and, at the same time, avoiding excessive pressures on the buccal apical bone (Fig. 7-46).
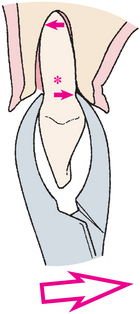
FIGURE 7-46 Lingual pressure will expand linguocortical plate at crestal area and slightly expand buccal bone at apical area. Asterisk, Center of rotation.
Fourth, rotational pressure, as the name implies, rotates the tooth, which causes some internal expansion of the tooth socket. Teeth with single, conical roots (such as the maxillary incisors and mandibular premolars) and with roots that are not curved are most amenable to luxation by this technique (Fig. 7-47). Teeth that have other than conical roots or that have multiple roots—especially if those roots are curved—are more likely to fracture under this type of pressure.
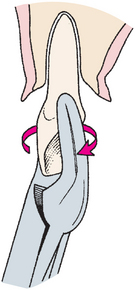
FIGURE 7-47 Rotational forces, useful for teeth with conical roots, such as maxillary incisors and mandibular premolars.
Finally, tractional forces are useful for delivering the tooth from the socket once adequate bony expansion is achieved. Tractional forces should be limited to the final portion of the extraction process and should be gentle (Fig. 7-48). If excessive force is needed, other maneuvers should be redone to improve root luxation.
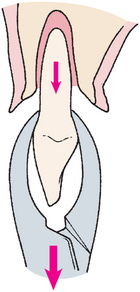
FIGURE 7-48 Tractional forces are useful for final removal of tooth from socket. They should always be small forces because teeth are not pulled.
In summary, a variety of forces can be used to remove teeth. A strong apical force is always useful and should be applied whenever the forceps are adapted to the tooth. Most teeth are removed by a combination of buccal and lingual (palatal) forces. Because maxillary buccal bone is usually thinner and the palatal bone is a thicker cortical bone, maxillary teeth are usually removed by strong buccal forces and less vigorous palatal forces. In the mandible the buccal bone is thinner from the midline posteriorly to the area of the molars. Therefore the incisors, canines, and premolars are removed primarily as a result of strong buccal force and less vigorous lingual pressures. The mandibular molar teeth have thicker buccal bone and usually require a stronger lingual pressure than the other teeth in the mouth. As mentioned before, rotational forces are useful for single-rooted teeth that have conic roots and no severe curvatures at the root end. The maxillary incisors, particularly the central incisor and mandibular premolars (especially the second premolar) are most amenable to rotational forces.
PROCEDURE FOR CLOSED EXTRACTION
An erupted root can be extracted using one of two major techniques: closed or open. The closed technique is also known as the routine technique. The open technique is also known as the surgical, or flap, technique. This section discusses the closed extraction technique; the open technique is discussed in Chapter 8.
The closed technique is the most frequently used technique and is given primary consideration for almost every extraction. The open technique is used when the clinician believes that excessive force would be necessary to remove the tooth, when a substantial amount of the crown is missing or covered by tissue, or when access to the root of a tooth is difficult, such as when a fragile crown is present.
The correct technique for any situation should lead to an atraumatic extraction; the wrong technique may result in an excessively traumatic and lengthy extraction.
Whatever technique is chosen, the three fundamental requirements for a good extraction remain the same: (1) adequate access and visualization of the field of surgery, (2) an unimpeded pathway for the removal of the tooth, and (3) the use of controlled force to luxate and remove the tooth.
For the tooth to be removed from the bony socket, it is usually necessary to expand the alveolar bony walls to allow the tooth root an unimpeded pathway, and it is necessary to tear the periodontal ligament fibers that hold the tooth in the bony socket. The use of elevators and forceps as levers and wedges with steadily increasing force can accomplish these two objectives.
Five general steps make up the closed extraction procedure:
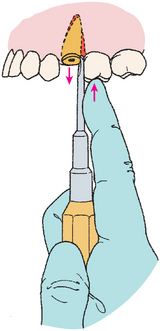
Step 1: Loosening of soft tissue attachment from the cervical portion of the tooth. The first step in removing a tooth by the closed extraction technique is to loosen the soft tissue from around the tooth with a sharp instrument, such as a scalpel blade or the sharp end of the No. 9 periosteal elevator (Fig. 7-49). The purpose of loosening the soft tissue from the tooth is twofold. First, it allows the surgeon to ensure that profound anesthesia has been achieved. When this step has been performed, the dentist informs the patient that the surgery is about to begin and that the first step will be to push the soft tissue away from the tooth. A small amount of pressure is felt at this step, but no sensation of sharpness or discomfort. The surgeon then begins the soft tissue loosening procedure, gently at first and then with increasing force.
The second reason that the soft tissue is loosened is to allow the elevator and tooth extraction forceps to be positioned more apically, without interference from or impingement on the soft tissue of the gingiva. As the soft tissue is loosened away from the tooth, it is slightly reflected, which thereby increases the width of the gingival sulcus and allows easy entrance of the beveled wedge tip of the forceps beaks. The adjacent gingival papilla of the tooth should also be reflected to avoid damage by the insertion of the straight elevator.
Step 2: Luxation of the tooth with a dental elevator. The next step is to begin the luxation of the tooth with a dental elevator, usually the straight elevator. Expansion and dilation of the alveolar bone and tearing of the periodontal ligament require that the tooth be luxated in several ways. The straight elevator is inserted perpendicular to the tooth into the interdental space, after reflection of the interdental papilla (Fig. 7-50). The elevator is then turned in such a way that the inferior portion of the blade rests on the alveolar bone and the superior, or occlusal, portion of the blade is turned toward the tooth being extracted (Fig. 7-51). Strong, slow, forceful turning of the handle moves the tooth in a posterior direction, which results in some expansion of the alveolar bone and tearing of the periodontal ligament. If the tooth is intact and in contact with stable teeth anterior and posterior to it, the amount of movement achieved with the straight elevator will be minimal. The usefulness of this step is greater if the patient does not have a tooth posterior to the tooth being extracted or if it is broken down to an extent that the crowns do not inhibit movement of the tooth.
In certain situations the elevator can be turned in the opposite direction and more vertical displacement of the tooth will be achieved, which can possibly result in complete removal of the tooth (Fig. 7-52).
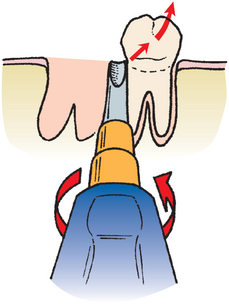
FIGURE 7-52 Handle of elevator, which may be turned in opposite direction to displace tooth further from socket. This can be accomplished only if no tooth is adjacent posteriorly.
Luxation of teeth with a straight elevator should be performed with caution. Excessive forces can damage and even displace the teeth adjacent to those being extracted. This is especially true if the adjacent tooth has a large restoration or carious lesion. This is only the initial step in the elevation process. Next, the small, straight elevator is inserted into the periodontal ligament space at the mesial-buccal line angle. The elevator is advanced apically while being rotated back and forth, helping luxate the tooth with its wedge action as it is advanced apically. A similar action with the elevator can then be done at the distal-buccal line angle. When a small, straight elevator becomes too easy to twist, a larger-sized elevator is used to do the same apical advancement. Often the tooth will loosen sufficiently to be removed easily with the forceps.
Step 3: Adaptation of the forceps to the tooth. The proper forceps are then chosen for the tooth to be extracted. The beaks of the forceps should be shaped to adapt anatomically to the tooth, apical to the cervical line, that is, to the root surface. The forceps are then seated onto the tooth so that the tips of the forceps beaks grasp the root underneath the loosened soft tissue (Fig. 7-53). The lingual beak is usually seated first and then the buccal beak. Care must be taken to confirm that the tips of the forceps beaks are beneath the soft tissue and not engaging an adjacent tooth. Once the forceps have been positioned on the tooth, the surgeon grasps the handles of the forceps at the ends to maximize mechanical advantage and control (Fig. 7-54).
If the tooth is malposed in such a fashion that the usual forceps cannot grasp the tooth without injury to adjacent teeth, another forceps with narrower beaks should be used. The maxillary root forceps can often be useful for crowded lower anterior teeth (Fig. 7-55).
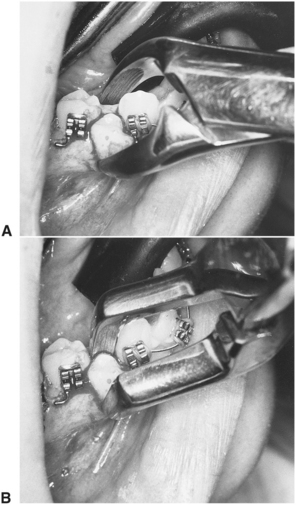
FIGURE 7-55 A, No. 151 forceps, too wide to grasp premolar to be extracted without luxating adjacent teeth. B, Maxillary root forceps, which can be adapted easily to tooth for extraction.
The beaks of the forceps must be held parallel to the long axis of the tooth so that the forces generated by the application of pressure to the forceps handle can be delivered along the long axis of the tooth for maximal effectiveness in dilating and expanding the alveolar bone. If the beaks are not parallel to the long axis of the tooth, it is increasingly likely that the tooth root will fracture.
The forceps are then forced apically as far as possible to grasp the root of the tooth as apically as possible. This accomplishes two things: First, the beaks of the forceps act as wedges to dilate the crestal bone on the buccal and lingual aspects. Second, by forcing the beaks apically, the center of rotation (or fulcrum) of the forces applied to the tooth is displaced toward the apex of the tooth, which results in greater effectiveness of bone expansion and less likelihood of fracturing the apical end of the tooth.
At this point the surgeon’s hand should be grasping the forceps firmly, with the wrist locked and the arm held against the body; the surgeon should be prepared to apply force with the shoulder and upper arm without any wrist pressure. The surgeon should be standing straight, with the feet comfortably apart.
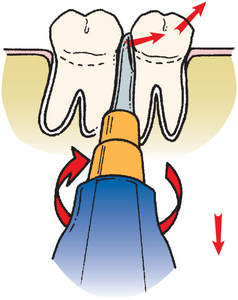
Step 4: Luxation of the tooth with the forceps. The surgeon begins to luxate the tooth by using the motions discussed earlier. The major portion of the force is directed toward the thinnest and therefore weakest bone. Thus in the maxilla and all but the molar teeth in the mandible, the major movement is labial and buccal (i.e., toward the thinner layer of bone). The surgeon uses slow, steady force to displace the tooth buccally rather than a series of rapid, small movements that do little to expand bone. The motion is deliberate and slow, and it gradually increases in force. The tooth is then moved again toward the opposite direction with slow, deliberate, strong pressure. As the alveolar bone begins to expand, the forceps are reseated apically with a strong, deliberate motion, which causes additional expansion of the alveolar bone and further displaces the center of the rotation apically. Buccal and lingual pressures continue to expand the alveolar socket. For some teeth, rotational motions are then used to help expand the tooth socket and tear the periodontal ligament attachments.
Beginning surgeons have a tendency to apply inadequate pressure for insufficient amounts of time. The following three factors must be reemphasized: (1) The forceps must be apically seated as far as possible and reseated periodically during the extraction; (2) the forces applied in the buccal and lingual directions should be slow, deliberate pressures and not jerky wiggles; and (3) the force should be held for several seconds to allow the bone time to expand. One must remember that teeth are not pulled; rather, they are gently lifted from the socket once the alveolar process has been sufficiently expanded.
Step 5: Removal of the tooth from the socket. Once the alveolar bone has expanded sufficiently and the tooth has been luxated, a slight tractional force, usually directed buccally, can be used. Tractional forces should be minimized, because this is the last motion that is used once the alveolar process is sufficiently expanded and the periodontal ligament is completely severed.
One should remember that luxation of the tooth with the forceps and removal of the tooth from the bone are separate steps in the extraction. Luxation is directed toward expansion of the bone and disruption of the periodontal ligament. The tooth is not removed from the bone until these two goals are accomplished. The novice surgeon should realize that the major role of the forceps is not to remove the tooth but rather to expand the bone so that the tooth can be removed.
For teeth that are malposed or have unusual positions in the alveolar process, the luxation with the forceps and removal from the alveolar process will be in unusual directions. The surgeon must develop a sense for the direction the tooth wants to move and then be able to move it in that direction. Careful preoperative assessment and planning help to guide this determination during the extraction.
Role of Opposite Hand
During use of the forceps and elevators to luxate and remove teeth, it is important that the surgeon’s opposite hand play an active role in the procedure. For the right-handed operator, the left hand has a variety of functions. The left hand is responsible for reflecting the soft tissues of the cheeks, lips, and tongue to provide adequate visualization of the area of surgery. The left hand helps to protect other teeth from the forceps, should it release suddenly from the tooth socket. The left hand helps to stabilize the patient’s head during the extraction process. In some situations, greater amounts of force are required to expand heavy alveolar bone; therefore the patient’s head requires active assistance to be held steady. The opposite hand plays an important role in supporting and stabilizing the jaw when mandibular teeth are being extracted. The opposite hand is often necessary to apply considerable pressure to expand heavy mandibular bone, and such forces can cause discomfort and even injury to the TMJ unless a steady hand counteracts them. A bite block placed on the contralateral side is also used to help support the jaw in this situation. Finally, the opposite hand supports the alveolar process and provides tactile information to the operator concerning the expansion of the alveolar process during the luxation period. In some situations, it is impossible for the opposite hand to perform all of these functions at the same time, so the surgeon requires an assistant to help with some of them.
Role of Assistant During Extraction
For a successful outcome in any surgical procedure, it is essential to have a skilled assistant. During the extraction the assistant plays a variety of important roles that contribute to making the surgical experience atraumatic. The assistant helps the surgeon visualize and gain access to the operative area by reflecting the soft tissue of the cheeks and tongue so that the surgeon can have an unobstructed view of the surgical field. Even during a closed extraction, the assistant can reflect the soft tissue so that the surgeon can apply the instruments to loosen the soft tissue attachment and adapt the forceps to the tooth in the most effective manner.
Another major activity of the assistant is to suction away blood, saliva, and the irrigating solutions used during the surgical procedure. This prevents fluids from accumulating and makes proper visualization of the surgical field possible. Suctioning is also important for patient comfort, because most patients are unable to tolerate an accumulation of blood or other fluids in their throats.
During the extraction the assistant should also help to protect the teeth of the opposite arch, which is especially important when removing lower posterior teeth. If traction forces are necessary to remove a lower tooth, occasionally the tooth releases suddenly and the forceps strike the maxillary teeth and may fracture a tooth cusp. The assistant should hold a suction tip or a finger against the maxillary teeth to protect them from an unexpected blow.
During the extraction of mandibular teeth, the assistant may play an important role by supporting the mandible during the application of the extraction forces. A surgeon who uses the hand to reflect the soft tissue may not be able to support the mandible. If this is the case, the assistant plays an important role in stabilizing the mandible to prevent TMJ discomfort. Most often the surgeon stabilizes the mandible, which makes this role less important for the assistant.
The assistant also provides psychological and emotional support for the patient by helping alleviate patient anxiety during the surgery. The assistant is important in gaining the patient’s confidence and cooperation by using positive language and physical contact with the patient during the preparation and performance of the surgery. The assistant should avoid making casual, offhand comments that may increase the patients’ anxiety and lessen their cooperation.
SPECIFIC TECHNIQUES FOR REMOVAL OF EACH TOOTH
This section describes specific techniques for the removal of each tooth in the mouth. In some situations, several teeth are grouped together (e.g., the maxillary anterior teeth) because the technique for their removal is essentially the same.
Maxillary Teeth
In the correct position for extraction of maxillary left or anterior teeth, the left index finger of the surgeon should reflect the lip and cheek tissue; the thumb should rest on the palatal alveolar process (Fig. 7-56). In this way the left hand is able to reflect the soft tissue of the cheek, stabilize the patient’s head, support the alveolar process, and provide tactile information to the surgeon regarding the progress of the extraction. When such a position is used during the extraction of a maxillary molar, the surgeon can frequently feel with the left hand the palatal root of the molar becoming free in the alveolar process before realizing it with the forceps or extracting hand. For the right side, the index finger is positioned on the palate and the thumb on the buccal aspect.

FIGURE 7-56 Extraction of maxillary left posterior teeth. Left index finger reflects lip and cheek and supports alveolar process on buccal aspect. Thumb is positioned on palatal aspect of alveolar process and supports alveolar process. Head is steadied by this grip, and tactile information is gained regarding tooth and bone movement.
Incisor Teeth
The maxillary incisor teeth are extracted with the upper universal forceps (No. 150), although other forceps can be used. The maxillary incisors generally have conic roots, with the lateral ones being slightly longer and more slender. The lateral incisor is more likely also to have a distal curvature on the apical one third of the root, so this must be checked radiographically before the tooth is extracted. The alveolar bone is thin on the labial side and heavier on the palatal side, which indicates that the major expansion of the alveolar process will be in the labial direction. The initial movement is slow, steady, and firm in the labial direction, which expands the crestal buccal bone. A less vigorous palatal force is then used, followed by a slow, firm, rotational force. Rotational movement should be minimized for the lateral incisor, especially if a curvature exists on the tooth. The tooth is delivered in the labial-incisal direction with a small amount of tractional force (Fig. 7-57).
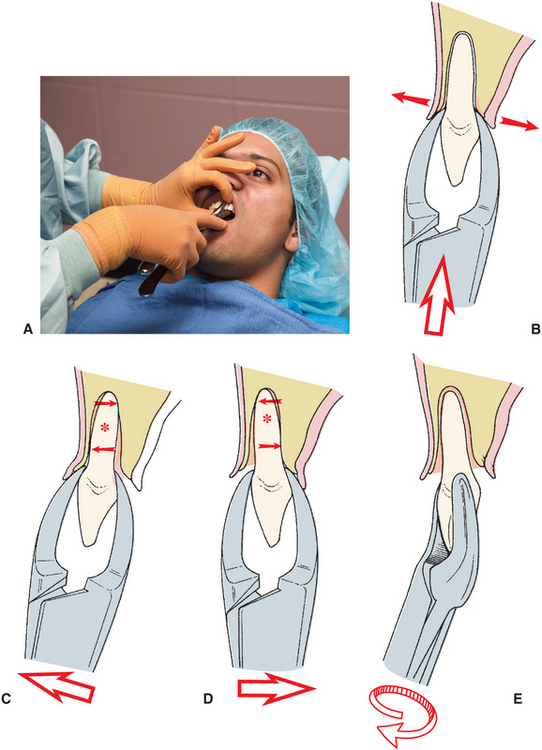
FIGURE 7-57 A, Maxillary incisors are extracted with No. 150 forceps. Left hand grasps alveolar process. B, Forceps are seated as far apically as possible. C, Luxation is begun with labial force. D, Slight lingual force is used. E, Tooth is delivered to labial incisor with rotational, tractional movement.
Canine
The maxillary canine is usually the longest tooth in the mouth. The root is oblong in cross section and usually produces a bulge called the canine eminence on the anterior surface of the maxilla. The result is that the bone over the labial aspect of the maxillary canine is usually thin. In spite of the thin labial bone, this tooth can be difficult to extract simply because of its long root. Additionally, it is not uncommon for a segment of labial alveolar bone to fracture from the labial plate and be removed with the tooth.
The upper universal (No. 150) forceps are the preferred instrument for removing the maxillary canine. As with all extractions the initial placement of the beaks of the forceps on the canine tooth should be as far apically as possible. The initial movement is apical and then to the buccal aspect, with return pressure to the palatal. As the bone is expanded and the tooth mobilized, the forceps should be repositioned apically. A small amount of rotational force may be useful in expanding the tooth socket, especially if the adjacent teeth are missing or have just been extracted. After the tooth has been well luxated, it is delivered from the socket in a labial-incisal direction with labial tractional forces (Fig. 7-58).
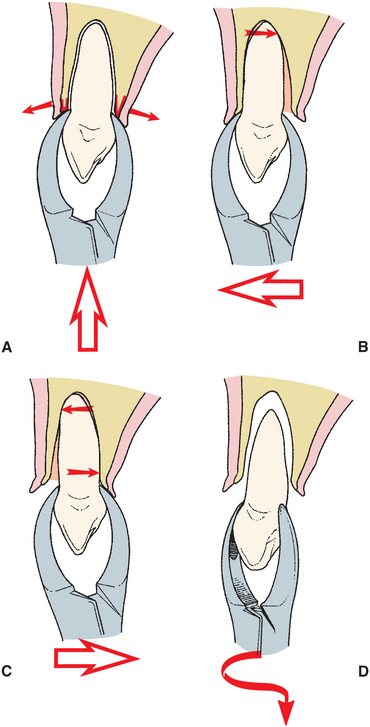
FIGURE 7-58 A, Hand and forceps position for removal of maxillary canine is similar to that for incisors. Forceps are seated as far apically as possible. B, Initial movement is buccally. C, Small amounts of lingual force are applied. D, Tooth is delivered in labial-incisal direction with slight rotational force.
If, during the luxation process with the forceps, the surgeon feels a portion of the labial bone fracture, the surgeon must make a decision concerning the next step. If the palpating finger indicates that a small amount of bone has fractured free and is attached to the canine tooth, the extraction should continue in the usual manner, with caution taken not to tear the soft tissue. However, if the palpating finger indicates that a large portion of labial alveolar plate has fractured, the surgeon should stop the surgical procedure. Usually the fractured portion of bone is attached to periosteum and therefore is viable. The surgeon should use a thin periosteal elevator to raise a small amount of mucosa from around the tooth, down to the level of the fractured bone.
The canine tooth should then be stabilized with the extraction forceps, and the surgeon should attempt to free the fractured bone from the tooth, with the periosteal elevator as a lever to separate the bone from the tooth root. If this can be accomplished, the tooth can be removed and the bone left in place attached to the periosteum. Normal healing should occur. If the bone becomes detached from the periosteum during these attempts, it should be removed, because it is probably nonvital and may actually prolong wound healing. This same procedure can be used whenever alveolar bone is fractured during extraction.
Prevention of fractured labial plate is important. If during the luxation process with the forceps a normal amount of pressure has not resulted in any movement of the tooth, the surgeon should seriously consider doing an open extraction. By reflecting a soft tissue flap and removing a small amount of bone, the surgeon may be able to remove the stubborn canine tooth without fracturing a larger amount of labial bone. By using the open technique, there will be an overall reduction in bone loss and in postoperative healing time.
First Premolar
The maxillary first premolar is a single-rooted tooth in its first two thirds, with a bifurcation into a buccolingual root usually occurring in the apical one third to one half. These roots may be extremely thin and are subject to fracture, especially in older patients in whom bone density is great and bone elasticity is diminished. Perhaps the most common root fracture when extracting teeth in adults occurs with this tooth. As with other maxillary teeth, the buccal bone is thin compared with the palatal bone.
The upper universal (No. 150) forceps are the instrument of choice. Alternatively, the No. 150A forceps can be used for removal of the maxillary first premolar.
Because of the high likelihood of root fracture, the tooth should be luxated as much as possible with the straight elevator. If root fracture does occur, a mobile root tip can be removed more easily than one that has not been well luxated.
Because of the bifurcation of the tooth into two thin root tips, extraction forces should be carefully controlled during removal of the maxillary first premolar. Initial movements should be buccal. Palatal movements are made with small amounts of force to prevent fracture of the palatal root tip, which is harder to retrieve. When the tooth is luxated buccally, the most likely tooth root to break is the labial. When the tooth is luxated in the palatal direction, the most likely root to break is the palatal root. Of the two root tips, the labial is easier to retrieve because of the thin, overlying bone. Therefore, buccal pressures should be greater than palatal pressures. Any rotational force should be avoided. Final delivery of the tooth from the tooth socket is with tractional force in the occlusal direction and slightly buccal (Fig. 7-59).
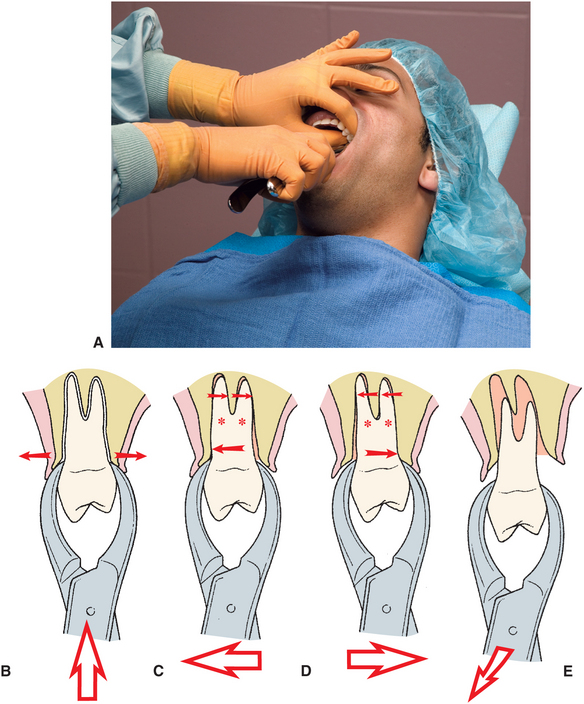
FIGURE 7-59 A, Maxillary premolars are removed with No. 150 forceps. Hand position is similar to that used for anterior teeth. B, Firm apical pressure is applied first to lower center of rotation as far as possible and to expand crestal bone. C, Buccal pressure is applied initially to expand buccocortical plate. Apices of roots are pushed lingually and are therefore subject to fracture. D, Palatal pressure is applied but less vigorously than buccal pressure. E, Tooth is delivered in buccoocclusal direction with combination of buccal and tractional forces.
Second Premolar
The maxillary second premolar is a single-rooted tooth for the entire length of the root. The root is thick and has a blunt end. Consequently, the root of the second premolar rarely fractures. The overlying alveolar bone is similar to that of other maxillary teeth in that it is thin toward the bucca, with a heavy palatal alveolar palate.
The recommended forceps are the maxillary universal forceps, or No. 150; some surgeons prefer the No. 150A. The forceps are forced as far apically as possible so as to gain maximal mechanical advantage in removing this tooth. Because the tooth root is strong and blunt, the extraction requires strong movements to the buccal, back to the palate, and then in the buccoocclusal direction with a rotational, tractional force (Fig. 7-60).
Molar
The maxillary first molar has three large and strong roots. The buccal roots are usually close together, and the palatal root diverges widely toward the palate. If the two buccal roots are also widely divergent, it becomes difficult to remove this tooth by closed extraction. Once again the overlying alveolar bone is similar to that of other teeth in the maxilla; the buccal plate is thin and the palatal cortical plate is thick and heavy. When evaluating this tooth radiographically, the dentist should note the size, curvature, and apparent divergence of the three roots. Additionally the dentist should look carefully at the relationship of the tooth roots to the maxillary sinus. If the sinus is in proximity to the roots and the roots are widely divergent, sinus perforation caused by removal of a portion of the sinus floor during tooth removal is increasingly likely. If this appears to be likely after preoperative evaluation, the surgeon should strongly consider a surgical extraction.
The paired forceps No. 53R and No. 53L are usually used for extraction of the maxillary molars. These two forceps have tip projections on the buccal beaks to fit into the buccal bifurcation. Some surgeons prefer to use the No. 89 and No. 90 forceps. These two forceps are especially useful if the crown of the molar tooth has serious caries or large restorations.
The upper molar forceps are adapted to the tooth and are apically seated as far as possible in the usual fashion (Fig. 7-61). The basic extraction movement is to use strong buccal and palatal pressures, with stronger forces toward the buccal than toward the palate. Rotational forces are not useful for extraction of this tooth because of its three roots. As mentioned in the discussion of the extraction of the maxillary first premolar, it is preferable to fracture a buccal root than a palatal root (because it is easier to retrieve the buccal roots). Therefore, if the tooth has widely divergent roots and the dentist suspects that one root may be fractured, the tooth should be luxated in such a way as to prevent fracturing the palatal root. The dentist must minimize palatal force, because this is the force that fractures the palatal root. Strong, slow, steady, buccal pressure expands the buccocortical plate and tears the periodontal ligament fibers that hold the palatal root in its position. Palatal forces should be used but kept to a minimum.
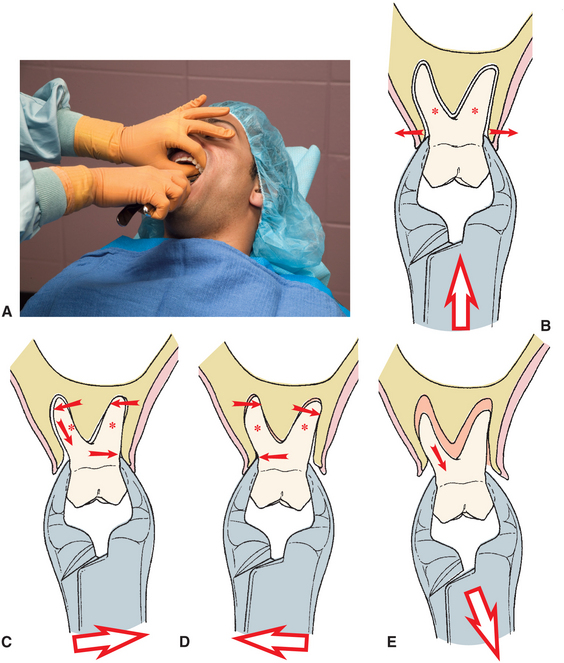
FIGURE 7-61 A, Extraction of maxillary molars. Soft tissue of lips and cheek is reflected, and alveolar process is grasped with opposite hand. B, Forceps beaks are seated apically as far as possible. C, Luxation is begun with strong buccal force. D, Lingual pressures are used only moderately. E, Tooth is delivered in buccoocclusal direction.
The anatomy of the maxillary second molar is similar to that of the maxillary first molar except that the roots tend to be shorter and less divergent, with the buccal roots more commonly fused into a single root. This means that the tooth is more easily extracted by the same technique described for the first molar.
The erupted maxillary third molar frequently has conic roots and is usually extracted with the No. 210S forceps, which are universal forceps used for the left and right sides. The tooth is usually easily removed, because the buccal bone is thin and the roots are usually fused and conic. The erupted third molar is also frequently extracted by the use of elevators alone. Clear visualization of the maxillary third molar on the preoperative radiograph is important because the root anatomy of this tooth is variable and often small, dilacerated, hooked roots exist in this area. Retrieval of fractured roots in this area is difficult.
Mandibular Teeth
When removing lower molar teeth, the index finger of the left hand is in the buccal vestibule and the second finger is in the lingual vestibule, reflecting the lip, cheek, and tongue (Fig. 7-62). The thumb of the left hand is placed below the chin so that the mandible is held between the fingers and thumb, which support the mandible and minimize TMJ pressures. This technique provides less tactile information, but during extraction of mandibular teeth the need to support the mandible supersedes the need to support the alveolar process. A useful alternative is to place a bite block between the teeth on the contralateral side (Fig. 7-63). The bite block allows the patient to help provide stabilizing forces to limit the pressure on the TMJs. The surgeon’s hand should continue to provide additional support to the jaw.

FIGURE 7-62 Extraction of mandibular left posterior teeth. Surgeon’s left index finger is positioned in buccal vestibule, reflecting cheek, and second finger is positioned in lingual vestibule, reflecting tongue. Thumb is positioned under chin. Mandible is grasped between fingers and thumb to provide support during extraction.

FIGURE 7-63 To provide support for the mandible to prevent excessive temporomandibular joint pressures, a rubber bite block can be placed between the teeth on the contralateral side.
Anterior Teeth
The mandibular incisors and canines are similar in shape, with the incisors being shorter and slightly thinner and the canine roots being longer and heavier. The incisor roots are more likely to be fractured because they are thin and therefore should be removed only after adequate preextraction luxation. The alveolar bone that overlies the incisors and canines is thin on the labial and lingual sides. The bone over the canine may be thicker, especially on the lingual aspect.
The lower universal (No. 151) forceps are usually used to remove these teeth. Alternative choices include the No. 151A or the English style of Ashe forceps. The forceps beaks are positioned on the teeth and seated apically with strong force. The extraction movements are generally in the labial and lingual directions, with equal pressures both ways. Once the tooth has become luxated and mobile, rotational movement may be used to expand the alveolar bone further. The tooth is removed from the socket with tractional forces in a labial-incisal direction (Fig. 7-64).
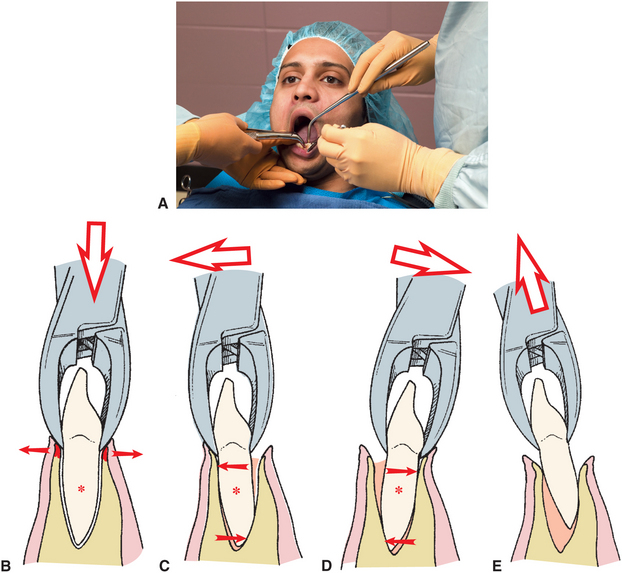
FIGURE 7-64 A, When extracting mandibular anterior teeth, No. 151 forceps are used. Assistant retracts cheek and provides suction. B, Forceps are seated apically as far as possible. C, Moderate labial pressure is used to initiate luxation process. D, Lingual force is used to continue expansion of bone. E, Tooth is delivered in labial-incisal direction.
Premolars
The mandibular premolars are among the easiest teeth to remove. The roots tend to be straight and conic, albeit sometimes slender. The overlying alveolar bone is thin on the buccal aspect and heavier on the lingual side.
The lower universal (No. 151) forceps are usually chosen for the extraction of the mandibular premolars. The No. 151A forceps and the English style of forceps are popular alternatives for extraction of these teeth.
The forceps are apically forced as far as possible, with the basic movements being toward the buccal aspect, returning to the lingual aspect, and finally, rotating. Rotational movement is used more when extracting these teeth than for any others, except perhaps the maxillary central incisor. The tooth is then delivered in the occlusobuccal direction (Fig. 7-65). Careful preoperative radiographic assessment must be performed to assure the operator that no root curvature exists in the apical third of the tooth. If such a curvature does exist, the rotational movements should be reduced or eliminated from the extraction procedure (Fig. 7-66).
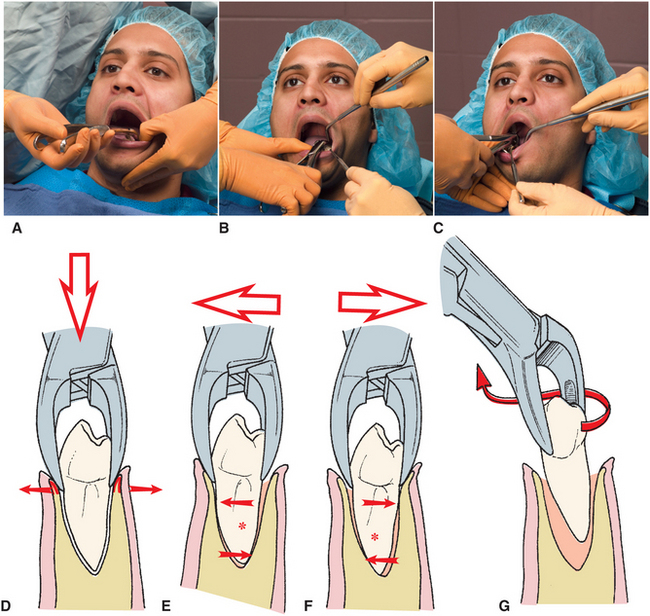
FIGURE 7-65 A, Extraction of mandibular premolar. Mandible is stabilized, soft tissue is reflected, and No. 151 forceps are positioned. B, Hand position is modified slightly for behind-the-patient technique. C, English style of forceps can also be used. D, Forceps are seated apically as far as possible to displace center of rotation and to begin expansion of crestal bone. E, Buccal forceps are applied to begin luxation process. F, Slight lingual pressure is used. G, Tooth is delivered with rotational, tractional force.
Molars
The mandibular molars usually have two roots, with roots of the first molar more widely divergent than those of the second molar. Additionally, the roots may converge at the apical one third, which increases the difficulty of extraction. The roots are generally heavy and strong. The overlying alveolar bone is heavier than the bone on any other teeth in the mouth. The combination of long, strong, divergent roots with heavy overlying buccolingual bone makes the mandibular first molar the most difficult of all teeth to extract.
The No. 17 forceps are usually used for extraction of the mandibular molars; they have small tip projections on both beaks to fit into the bifurcation of the tooth roots. The forceps are adapted to the root of the tooth in the usual fashion, and strong apical pressure is applied to set the beaks of the forceps apically as far as possible. Strong buccolingual motion is then used to expand the tooth socket and allow the tooth to be delivered in the buccoocclusal direction. The linguoalveolar bone around the second molar is thinner than the buccal plate, so the second molar can be removed more easily with stronger lingual than buccal pressures (Fig. 7-67).
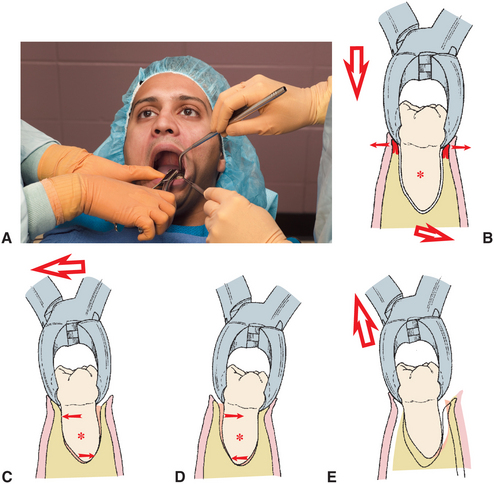
FIGURE 7-67 A, Mandibular molars are extracted with No. 17 or No. 23 forceps. Hand positions of surgeon and assistant are same for both forceps. B, No. 17 forceps are seated as far apically as possible. C, Luxation of molar is begun with strong buccal movement. D, Strong lingual pressure is used to continue luxation. E, Tooth is delivered in buccoocclusal direction.
If the tooth roots are clearly bifurcated, the No. 23, or cowhorn, forceps can be used. This instrument is designed to be closed forcefully with the handles, thereby squeezing the beaks of the forceps into the bifurcation. This creates force against the crest of the alveolar ridge on the buccolingual aspects and literally forces the tooth superiorly directly out of the tooth socket (Fig. 7-68). If initially this is not successful, the forceps are given buccolingual movements to expand the alveolar bone, and the forceps handles are moved up and down to seat the beaks more fully into the furcation. More squeezing of the handles is performed. Care must be taken with these forceps to prevent damaging the maxillary teeth because the lower molar may actually pop out of the socket and thus release the forceps to strike the upper teeth.
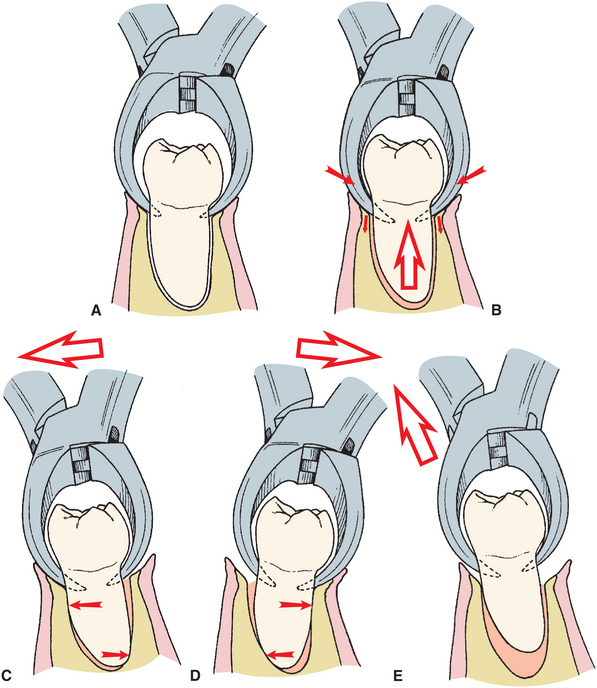
FIGURE 7-68 A, No. 23 forceps are carefully positioned to engage bifurcation area of lower molar. B, Handles of forceps are squeezed forcibly together, which causes beaks of forceps to be forced into bifurcation and exerts tractional forces on tooth. C, Strong buccal forces are then used to expand socket. D, Strong lingual forces are used to luxate tooth further. E, Tooth is delivered in buccoocclusal direction with buccal and tractional forces.
Erupted mandibular third molars usually have fused conic roots. Because a bifurcation is not likely, the No. 222 forceps—a short-beaked, right-angled forceps—are used to extract this tooth. The lingual plate of bone is definitely thinner than the buccocortical plate, so most of the extraction forces should be delivered to the lingual aspect. The third molar is delivered in the linguoocclusal direction. The erupted mandibular third molar that is in function can be a deceptively difficult tooth to extract. The dentist should give serious consideration to using the straight elevator to achieve a moderate degree of luxation before applying the forceps. Pressure should be gradually increased, and attempts to mobilize the tooth should be made before final strong pressures are delivered.
Modifications for Extraction of Primary Teeth
Rarely is it necessary to remove primary teeth before substantial root resorption has occurred. However, when removal is required, it must be done with a great deal of care because the roots of the primary teeth are long and delicate and are subject to fracture. This is especially true because the succedaneous tooth causes resorption of coronal portions of the root structure and thereby weakens it. The forceps usually used are an adaptation of the upper and lower universal forceps, the No. 150S and the No. 151S. They are adapted and forced apically in the usual fashion, with slow, steady pressures toward the buccal aspect and return movements toward the lingual aspect.
Rotational motions may be used but should be minimal and should be used judiciously with multirooted teeth. The dentist should pay careful attention to the direction of least resistance and deliver the tooth into that path. If the roots of the primary molar tooth embrace the crown of the permanent premolar, the surgeon should consider sectioning the tooth. Rarely, the roots hold the crown of the permanent premolar firmly enough in their grasp to cause it to be extracted also.
POSTEXTRACTION TOOTH SOCKET CARE
Once the tooth has been removed, the socket requires proper care. The socket should be débrided only if necessary. If a periapical lesion is visible on the preoperative radiograph and there was no granuloma attached to the tooth when it was removed, the periapical region should be carefully curetted with a periapical curette to remove the granuloma or cyst. If any debris is obvious, such as calculus, amalgam, or tooth fragment remaining in the socket, it should be gently removed with a curette or suction tip (Fig. 7-69). However, if neither a periapical lesion nor debris is present, the socket should not be curetted. The remnants of the periodontal ligament and the bleeding bony walls are in the best condition to provide for rapid healing. Vigorous curettage of the socket wall merely produces additional injury and may delay healing.
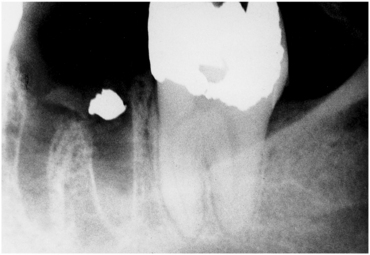
FIGURE 7-69 Amalgam fragment left in this tooth socket after extraction because surgeon failed to inspect and débride surgical field.
The expanded buccolingual plates should be compressed back to their original configuration. Finger pressure should be applied to the buccolingual cortical plate to compress the plates gently but firmly to their original position. This helps prevent bony undercuts that may have been caused by excessive expansion of the buccocortical plate, especially after first molar extraction. Care should be taken to not overreduce the socket if implant placement is planned or possible in the future.
If the teeth were removed because of periodontal disease, there may be an accumulation of excess granulation tissue around the gingival cuff. If this is the case, special attention should be given to removing this granulation tissue with a curette, tissue scissors, or hemostat. The arterioles of granulation tissue have little or no capacity to retract and constrict, which leads to bothersome bleeding if excessive granulation tissue is left in place.
Finally, the bone should be palpated through the overlying mucosa to check for any sharp, bony projections. If any exist, the mucosa should be reflected and the sharp edges smoothed judiciously with a bone file or trimmed with a rongeur.
Initial control of hemorrhage is achieved by use of a moistened 2 × 2-inch gauze placed over the extraction socket. The gauze should be positioned so that when the patient closes the teeth together, it fits into the space previously occupied by the crown of the tooth. The pressure of biting the teeth together is placed on the gauze and is transmitted to the socket. This pressure results in hemostasis. If the gauze is simply placed on the occlusal table, the pressure applied to the bleeding socket is insufficient to achieve adequate hemostasis (Fig. 7-70). A larger gauze sponge (4 × 4 inches) may be required if multiple teeth have been extracted or if the opposing arch is edentulous.

FIGURE 7-70 A, After extraction of single tooth, small space exists where crown of tooth was located. B, Gauze pad (2 × 2-inch pad) is folded in half twice and placed into space. When patient bites on gauze, pressure is transmitted to gingiva and socket. C, If large gauze is used, pressure goes on teeth, not on gingiva or socket.
The extraction of multiple teeth at one sitting is a more involved and complex procedure and is discussed in Chapter 8.