Dyspepsia and peptic ulcer disease
The spectrum of disease
Dyspepsia is the term used for a group of symptoms that arise from the upper gastrointestinal tract. They include heartburn, abdominal pain or discomfort, fullness, bloating, early satiety, belching and nausea. Dyspepsia can occur alone (non-ulcer dyspepsia) or in association with various upper gastrointestinal disorders such as gastritis, peptic ulcer disease or gastro-oesophageal reflux disease.
Non-ulcer dyspepsia
Several functional abnormalities in gastrointestinal motility, increased gastroduodenal sensitivity to mechanical distention and increased acid sensitivity in the duodenum have been described in people with non-ulcer dyspepsia.
Peptic ulcer disease
Peptic ulceration is used to describe both gastric and duodenal ulcers. The characteristic symptom is epigastric pain, but other dyspeptic symptoms also occur. Symptoms are not a reliable guide to the location of an ulcer. However, the pain with duodenal ulceration is usually worse when fasting and at night and is relieved by antacids or by food. By contrast, with gastric ulcer the pain may be made worse by food and it is more likely than duodenal ulcer to be associated with weight loss, anorexia and nausea. Chronic ulcers at either site may be asymptomatic. Peptic ulcer disease is twice as frequent in males and more common in smokers, and there is often a family history of the disorder. There is also a higher incidence in people who use non-steroidal anti-inflammatory drugs (NSAIDs), including low-dose aspirin (Ch. 29), or who have a high alcohol intake. Women more often develop gastric rather than duodenal ulceration.
Complications of peptic ulcers include bleeding, perforation and – if close to the pylorus – scarring with gastric outlet obstruction.
Mechanisms of protection of gastric and duodenal mucosa
The healthy stomach mucosa is able to resist acid digestion. There is an adherent layer of viscoelastic mucus that acts as a physical barrier, and HCO3− is secreted into the mucus to neutralise acid locally. In addition, there is a high electrical resistance of, and tight junctions between, gastric mucosal cells, which make the mucosa relatively impermeable to luminal contents. Gastric mucosal blood flow provides an extra layer of defence, delivering HCO3− to buffer any H+ ions that penetrate the mucosa, and also regulating acid secretion. Many of these protective functions are dependent on the synthesis by gastric mucosal cells of the prostaglandins PGE2 and PGI2 (Ch. 29) (Table 33.1).
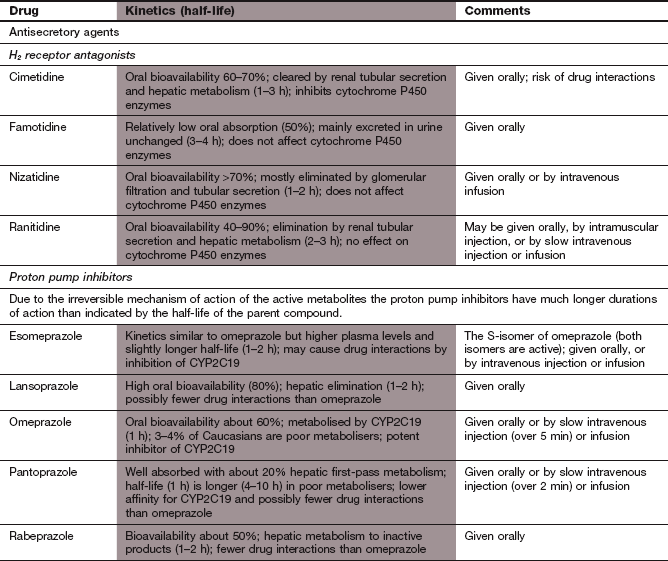
Table 33.1
Factors associated with protection and damage of the intestinal mucosa
| Factors associated with peptic ulcer disease | Factors associated with peptic ulcer protection and healing |
| Thin or breached mucus layer | Intact mucus layer |
| Helicobacter pylori and host immune response | Adequate blood flow |
| Reduced bicarbonate secretion | Bicarbonate in mucus layer |
| Reduced mucosal blood flow | Prostaglandins (generated by cyclo-oxygenase COX-1 and COX-2 isoenzymes) |
| Stress | Hydrophobicity of phospholipid layer of epithelial cells |
| Smoking | Regrowth of epithelial cell layer following damage (restitution) |
| Alcohol | Growth factors |
| Acid | Nitric oxide |
| Pepsin | |
| Iatrogenic, e.g. NSAIDs. |
The duodenal mucosa is protected by a layer of viscoelastic mucus, but the mucosal cells are highly permeable, permitting absorption of luminal nutrients. The mucosal cells secrete HCO3−, which accumulates in the mucus layer (the mucosal barrier) and buffers the pulses of gastric acid released from the stomach.
Aetiology of peptic ulceration
The precise aetiology of peptic ulceration is not known but there are many contributory factors. Gastric acid is essential for ulceration to arise, and there is often a failure of normal luminal acid concentration to inhibit further gastric acid secretion. Pepsin secretion is also enhanced in people with peptic ulceration. Accelerated gastric emptying is a factor in promoting duodenal ulceration, with entry of gastic contents at a lower pH into the duodenum. Prostaglandins increase mucosal protection against ulceration, and deficient production of prostaglandin E1 is a factor in reducing resistance to mucosal erosion in both the stomach and duodenum.
A major risk factor associated with peptic ulceration is gastric and duodenal infection with the Gram-negative bacterium Helicobacter pylori. The organism penetrates the mucus lining of the stomach and attaches to epithelial cells. The incidence of H. pylori in the gastric mucosa varies widely in the adult population in different countries, being highest in those who have poorer living conditions. About 10–15% of the UK population is infected. Infection is usually acquired in childhood and persists unless treated. Infection with H. pylori is an acknowledged risk factor for gastritis, peptic ulcer, gastric cancer and mucosa-associated lymphoid tissue (MALT) lymphoma. Only a small percentage of those who carry the bacteria develop H. pylori-associated disease, perhaps reflecting different host responses to the infection and whether the infecting strain carries particular factors for high virulence. Infection with H. pylori is found in about 80% of people with duodenal ulcer and somewhat fewer with gastric ulcer. H. pylori secretes the enzyme urease, which contributes to its survival during exposure to gastric acid by producing ammonia from urea. Ammonia is toxic to mucosal cells, and an immune response to the bacterial proteins also contributes to development of chronic gastritis.
H. pylori and gastric ulceration: If a gastric ulcer is present it is often associated with H. pylori infection of the corpus of the stomach or both the corpus and antrum (pangastritis). Moreover, unlike the situation in duodenal ulceration there is a decrease or at least no increase in acid secretion. The reason for this is that infection of the corpus is associated with atrophy of acid-secreting cells and metaplasia of the gastric mucosa, which lead to gastric ulceration and increase the risk of gastric cancer.
NSAIDs are the most frequent cause of gastric ulceration in the absence of H. pylori. The mechanisms are distinct, and relate to inhibition of prostaglandin formation and intracellular trapping of NSAID in the gastric mucosa (Ch. 29).
The prevalence of non-H. pylori, non-NSAID-associated gastric ulcers appears to be increasing in Western societies. The pathogenesis of these ulcers is poorly understood.
H. pylori and duodenal ulceration: In people who develop duodenal ulceration H. pylori infection is predominantly found in the stomach and confined to the antral mucosa. Antral mucosal cells secrete gastrin, which stimulates excess acid secretion from the body of the stomach. Exposure of duodenal cells to excess acid alters the structure of some of them, making them gastric-like (gastric metaplasia) and allowing them to be colonized by H. pylori.
As with gastric ulceration, NSAIDs are the most frequent cause of duodenal ulceration in the absence of H. pylori infection.
Gastro-oesophageal reflux disease
Gastro-oesophageal reflux disease (GORD) can produce heartburn from regurgitation of gastric contents into the oesophagus (reflux), pain or difficulty in swallowing, and even the regurgitation of gastric contents into the mouth. If reflux is associated with inflammation of the oesophageal mucosa (oesophagitis), there may be more prolonged chest pain and even chronic bleeding. Gastro-oesophageal reflux is produced by the generation of transient lower oesophageal sphincter relaxations (TLOSRs) in the absence of swallowing. TLSORs arise from stimulation of gastric vagal mechanoreceptors and allow gastric acid, pepsin and bile to come into contact with the vulnerable epithelium of the oesophagus. Oesophageal hypomotility and abnormal patterns of oesophageal contractility often coexist with GORD, and reduce the clearance of refluxed material. The disturbance of normal motility may reflect a sensory abnormality in the oesophageal mucosa.
Oesophageal spasm is a distinct disorder, in which oesophageal pain is often not accompanied by any change in luminal pH. The pain frequently occurs in people who have no evidence of obvious dysmotility, and this syndrome is probably due to a combination of local mucosal sensory disturbances and psychological factors.
There is little correlation between the presence of oesophagitis at endoscopy and the severity of symptoms. Up to 50% of people with symptoms of GORD have no apparent oesophagitis, whereas severe oesophagitis may be asymptomatic unless complications such as stricture or anaemia arise. GORD has an association with asthma, through microaspiration of gastric contents into the lungs and triggering of vagal oesophago-bronchial reflexes. Microaspiration is also associated with chronic cough.
The relationship of H. pylori infection to GORD is not straightforward: antral infection appears to predispose to GORD by promoting greater amounts of gastric acid secretion, while corporal gastritis is protective partly because the acid content of the stomach may be reduced. Symptoms in GORD are usually chronic and relapsing, with at least two-thirds of those diagnosed still taking continuous or intermittent treatment after 10 years. It is now believed that there are three distinct clinical groups of GORD rather than a steady progression of severity. These are possibly determined by genetic factors and the immunological response to reflux. The groups are:
Control of gastric acid secretion
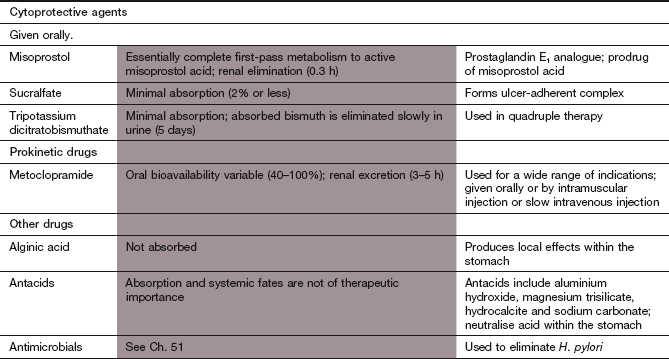
Acid secretion into the canaliculi of gastric parietal cells is initiated by the activity of a membrane-bound proton pump which exchanges H+ and K+ across the cell membrane (H+/K+-ATPase). Hydrogen ions are obtained from carbonic acid (H2CO3) by carbonic anhydrase, and HCO3− enters the plasma in exchange for Cl−. Chloride ions are then secreted into the stomach lumen with H+ via a symport carrier. The activity of the proton pump is influenced by several mediators, including histamine, gastrin and acetylcholine (Fig. 33.1).
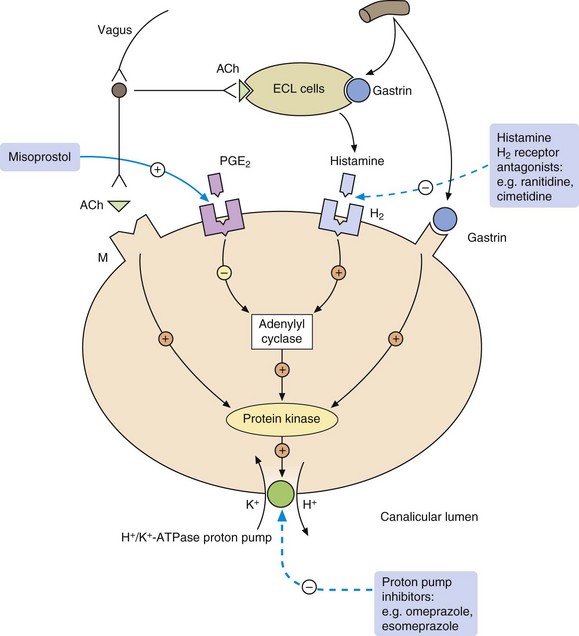
Fig. 33.1 Control of gastric acid secretion from the parietal cell.
Acid secretion from the parietal cell is stimulated by acetylcholine (ACh), histamine and gastrin. Gastrin and ACh also reinforce acid secretion by causing the release of histamine from the enterochromaffin-like (ECL) cells which lie close to the parietal cells in the gastric pits. Prostaglandin E2 (PGE2) reduces acid secretion. The sites of action of the main drugs used to inhibit acid secretion from the parietal cell are shown. There are no useful inhibitors of gastrin action, and the gastric-selective muscarinic receptor (M) antagonist pirenzepine is no longer available in the UK. H2, histamine type 2 receptor.
Drugs for treating dyspepsia, peptic ulcer and gastro-oesophageal reflux disease
It is only necessary to raise intragastric pH above 3 for a few hours each day to promote healing of most peptic ulcers. However, rapid healing requires acid suppression for a minimum of 18–20 h per day. The duration of acid suppression determines the rate of healing but not the eventual proportion of ulcers healed. Several classes of drug have antisecretory actions on the gastric mucosa.
Proton pump inhibitors
Mechanism of action: Since the proton pump (H+/K+-ATPase) is the final common pathway for acid secretion in gastric parietal cells, inhibition of the pump almost completely blocks acid secretion (Fig. 33.1). Proton pump inhibitors are irreversible inhibitors of H+/K+-ATPase and the return of acid secretion is dependent on the synthesis of new proton pumps. Proton pump inhibitors are weak bases that are selectively concentrated from the circulation into the acid environment of the secretory canaliculi of the gastric parietal cell. The drugs are then protonated and structurally transform into active derivatives that covalently bind to and irreversibly inhibit the proton pump. Because protonation to the active derivatives only takes place at acid pH, these drugs have a selective action on gastric cells, and proton pumps elsewhere in the body are not inhibited. Acid production is inhibited by about 90% for approximately 24 h following a single dose.
Pharmacokinetics: Proton pump inhibitors are prodrugs that are unstable in acid. They are given orally as enteric-coated formulations; esomeprazole, omeprazole and pantoprazole are also available as intravenous formulations. Elimination is by hepatic metabolism. They have short plasma half-lives (1–2 h) but, because of the irreversible mechanism of action, these bear no relationship to the long biological duration of action. Esomeprazole is the S-isomer of omeprazole that has lower clearance and therefore achieves slightly higher plasma concentrations.
 Gastrointestinal upset, such as nausea, vomiting, abdominal pain, diarrhoea, constipation.
Gastrointestinal upset, such as nausea, vomiting, abdominal pain, diarrhoea, constipation.
 Omeprazole and esomeprazole are inhibitors of CYP2C9 and CYP2C19 in the liver. This can give rise to drug interactions with other substrates of these isoenzymes, for example decreasing the metabolism and increasing the clinical effects of warfarin, phenytoin and several antiviral drugs (see Table 2.7).
Omeprazole and esomeprazole are inhibitors of CYP2C9 and CYP2C19 in the liver. This can give rise to drug interactions with other substrates of these isoenzymes, for example decreasing the metabolism and increasing the clinical effects of warfarin, phenytoin and several antiviral drugs (see Table 2.7).
Concerns that substantial reductions of gastric acid, and the associated rise in gastrin secretion, might increase the risk of gastric cancer (comparable to the increased risk in pernicious anaemia) appear to be unfounded. These drugs do not completely abolish acid secretion and intragastric pH can still fall below 4 during part of the day, the critical pH below which bacterial populations that predispose to cancer are thought not to become established. However, symptomatic improvement following treatment with a proton pump inhibitor can mask the symptoms of gastric cancer.
Histamine H2 receptor antagonists
Mechanism of action: Histamine H2 receptor antagonists act competitively at receptors on gastric parietal cells. They reduce basal acid secretion and pepsin production, and prevent the increase in secretion that occurs in response to several secretory stimuli. Overall, acid secretion is reduced by about 60% (Fig. 33.1).
Pharmacokinetics: Absorption of cimetidine and ranitidine from the gut is almost complete but both undergo limited first-pass metabolism. The drugs are mainly eliminated unchanged by the kidney, in part through active tubular transport. Their half-lives are between 1 and 4 h.
 Diarrhoea and other gastrointestinal disturbances.
Diarrhoea and other gastrointestinal disturbances.
 Headache, dizziness, tiredness.
Headache, dizziness, tiredness.
 Drug interactions: cimetidine is an inhibitor of hepatic P450 isoenzymes (see Table 2.7) and can increase the plasma concentrations and actions of drugs such as warfarin, phenytoin and theophylline.
Drug interactions: cimetidine is an inhibitor of hepatic P450 isoenzymes (see Table 2.7) and can increase the plasma concentrations and actions of drugs such as warfarin, phenytoin and theophylline.
Antacids
Mechanism of action
Antacids neutralise gastric acid; magnesium salts do so much more rapidly than aluminium salts. They have a more prolonged effect if taken after food. If used without food, the effect lasts no more than an hour because of rapid gastric emptying. Antacids quickly produce symptom relief in peptic ulcer disease, but large doses are required to heal ulcers. Liquid preparations work more rapidly, but tablets are more convenient to use. Most antacids are relatively poorly absorbed from the gut. Simeticone is sometimes added to an antacid as an antifoaming agent. The combination may reduce flatulence, or relieve hiccups in palliative care.
Unwanted effects
 Constipation can occur with aluminium salts, and diarrhoea with magnesium salts; mixtures of aluminium and magnesium salts may have less effect on stool consistency.
Constipation can occur with aluminium salts, and diarrhoea with magnesium salts; mixtures of aluminium and magnesium salts may have less effect on stool consistency.
 Systemic alkalosis can occur with very large doses.
Systemic alkalosis can occur with very large doses.
 In advanced renal failure, retention of absorbed aluminium may contribute to metabolic bone disease and encephalopathy. Magnesium salts can also cause toxicity, and the dose should be reduced in renal failure.
In advanced renal failure, retention of absorbed aluminium may contribute to metabolic bone disease and encephalopathy. Magnesium salts can also cause toxicity, and the dose should be reduced in renal failure.
 Drug interactions: aluminium salts can bind to NSAIDs and tetracyclines in the gut and reduce their absorption.
Drug interactions: aluminium salts can bind to NSAIDs and tetracyclines in the gut and reduce their absorption.
Antacids with alginic acid
Alginic acid is an inert substance. It is claimed that it forms a raft of high-pH foam which floats on the gastric contents and protects the oesophageal mucosa during reflux. All proprietary preparations combine alginic acid with an antacid, which is probably responsible for much of the clinical effect. Some formulations contain a high Na+ concentration and these should be used with caution in people with fluid retention or hypertension.
Cytoprotective drugs
Mechanism of action: Sucralfate is a complex of aluminium hydroxide and sucrose octasulphate. It dissociates in the acid environment of the stomach to its anionic form, which binds to the ulcer base. This creates a protective barrier to pepsin and bile and inhibits the diffusion of gastric acid. Sucralfate also stimulates the gastric secretion of bicarbonate and prostaglandins.
Bismuth salts
Mechanism of action: Bismuth salts precipitate in the acid environment of the stomach and then bind to glycoprotein on the base of an ulcer. The resulting complex adheres to the ulcer and has similar local effects to sucralfate. Bismuth salts, in combination with antibiotics, were the first effective anti-Helicobacter agents and this effect may have accounted for their ulcer-healing properties. They have now largely been superseded by proton pump inhibitor combinations for this purpose; however, when triple therapy with two antibacterials and a proton pump inhibitor fails, bismuth is included as part of the treatment regimen (see below).
Prostaglandin analogues
Mechanism of action: Misoprostol is an analogue of PGE1 and has several actions that protect the gastric and duodenal mucosae (see Ch. 29). Misoprostol limits the damage to superficial mucosal cells caused by agents such as acid and alcohol. It is most widely used to prevent NSAID-associated ulcers, and is available in combination products with diclofenac or naproxen (Ch. 29).
Pharmacokinetics: Misoprostol is an ester that is well absorbed from the gut and undergoes essentially complete first-pass metabolism to an active acid metabolite. Elimination of the acid is mainly by hepatic metabolism and it has a very short half-life (<1 h).
 Diarrhoea and abdominal cramps are common.
Diarrhoea and abdominal cramps are common.
 Uterine contractions: therefore, avoid in pregnancy. Misoprostol can be used to induce labour (Ch. 45).
Uterine contractions: therefore, avoid in pregnancy. Misoprostol can be used to induce labour (Ch. 45).
Prokinetic drugs
Mechanism of action
Metoclopramide is a dopamine receptor antagonist and is discussed in Chapter 32. It enhances gastric motility, increases the rate of gastric emptying and increases lower gastro-oesophageal sphincter tone.
Management of dyspepsia, peptic ulcer and gastro-oesophageal reflux disease
Most people with dyspepsia do not have significant underlying disease (i.e. they have non-ulcer or functional dyspepsia). In all cases, efforts should be made to remove causative agents, for example smoking, excess alcohol or NSAIDs. For persistent symptoms, antacids provide symptomatic relief. Eradication of H. pylori does not usually reduce symptoms, although it can be effective for about 15% of people who probably have undiagnosed peptic ulceration.
Upper gastrointestinal endoscopy may be indicated to assess the cause of symptoms. However, younger people (especially those under 55 years of age) who do not have ALARM symptoms (anaemia, loss of weight, anorexia, recent onset of progressive symptoms, melaena, haematemesis or dysphagia) are often treated initially without investigation.
A proton pump inhibitor is more effective than a histamine H2 receptor antagonist for symptom relief in non-ulcer dyspepsia. Treatment should be given for 4–6 weeks, followed by clinical review with the intention of reducing the dose of drug or moving to intermittent or on-demand therapy for symptom relief. Recurrent symptoms may prompt further investigation to exclude peptic ulceration or GORD.
Confirmed peptic ulceration
Proton pump inhibitors produce the fastest rate of ulcer healing (over 90% of ulcers heal within four weeks). Histamine H2 receptor antagonists usually give symptomatic relief for both gastric and duodenal ulcers within a week, but healing of the ulcer is much slower, requiring up to eight weeks for duodenal ulcer or 12 weeks for gastric ulcer. Other agents such as bismuth salts and sucralfate will heal ulcers in a similar proportion of people, but are used less often, since they do not improve symptoms as quickly.
Identification and eradication of H. pylori infection enhances ulcer healing and reduces relapse, so that maintenance therapy with acid-suppressing drugs is often unnecessary for uncomplicated ulcers. If H. pylori is not eradicated, 80% of ulcers will reoccur within a year, whereas following successful eradication the recurrence is less than 20%.
Eradication of H. pylori
Several indications for H. pylori eradication have been proposed (Box 33.1). Many eradication regimens are available: the highest eradication rates are achieved by treatment with high dosage of a proton pump inhibitor combined with two antibacterials (to maximise efficacy and minimise resistance) given for one week. The first choice antibacterials are clarithromycin with either amoxicillin or metronidazole, but it important to avoid an antibacterial that has been used recently for treatment of other infections. Treatment for two weeks has a higher eradication rate, but unwanted effects often reduce adherence to the regimen, which limits the success rate. The incidence of in vitro resistance of H. pylori to metronidazole and to clarithromycin is increasing. If in vitro clarithromycin resistance is detected it is always reflected in a reduced ability to eliminate the bacterium clinically. By contrast, eradication may be successful even when laboratory resistance to metronidazole is demonstrated. Resistance to amoxicillin is less common, and resistance to tinidazole is currently lower than to metronidazole.
Eradication with a triple regimen is successful in about 85% of cases, and failure usually reflects antibacterial resistance or poor adherence to treatment. However, resistance to triple therapy is now widespread in some localities, with a failure to eradicate H. pylori in up to 20% of people treated. Quadruple therapy can be used for resistant bacteria. One recommended regimen is a proton pump inhibitor plus tripotassium dicitratobismuthate plus metronidazole plus tetracycline for 7 days (Fig. 33.2). Other regimens are used following the results of microbiological sensitivity tests on biopsy specimens. These quadruple-therapy regimens achieve an eradication rate of 93–98%.
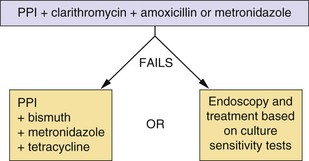
Fig. 33.2 Recommended regimens for the eradication of H. pylori.
Many regimens exist, dictated by local patterns of sensitivity and resistance. Increasing resistance to metronidazole and clarithromycin is reducing the success rate of the triple regimen. If the proton pump inhibitor (PPI) is not tolerated, a histamine H2 receptor antagonist can be substituted.
After H. pylori eradication, maintenance therapy with acid-suppressant treatment is only required if symptoms continue and after exclusion of more serious conditions.
Bleeding from peptic ulcers
Active bleeding from a peptic ulcer is a medical emergency. Endoscopic treatment applied to a visible vessel in the ulcer base using diathermy, clipping, laser coagulation or injection with adrenaline may stop the bleeding. Even after achieving haemostasis, recurrent bleeding occurs in up to 20% of cases. Endoscopic treatment is followed by intravenous high-dose proton pump inhibitor for 72 h before changing to oral tharapy, which reduces the rebleeding rate and the need for surgery by 30–40%. The efficacy of proton pump inhibitors in this situation may be related to reversal of the deactivation of the coagulation system and platelet aggregation that occurs when the local pH falls below 4.
Peptic ulceration associated with non-steroidal anti-inflammatory drugs
If the NSAID cannot be withdrawn, then NSAID-associated ulcers will often heal if an ulcer-healing agent is co-prescribed. Continued use of NSAIDs can slow ulcer healing by histamine H2 receptor antagonists, but probably not by proton pump inhibitors. Eradication of H. pylori infection is recommended if an NSAID must be continued in someone who has had previous peptic ulceration, although this may be more effective in preventing ulcers early in treatment with NSAIDs and less effective during long-term use.
When an NSAID is first used, careful assessment is recommended to decide whether prophylaxis against ulceration is given in the absence of upper gastrointestinal symptoms. Those at higher risk of NSAID-induced ulceration are the elderly (>65 years), smokers, heavy alcohol users and those taking concomitant treatment with medicines that cause gastrointestinal irritation, such as corticosteroids. People with a history of previous ulceration or those who have serious comorbidities, such as cardiovascular disease, diabetes or renal or hepatic impairment, are also at higher risk.
Misoprostol provides effective prophylaxis against NSAID-induced gastric or duodenal ulceration. However, the high dosage necessary for prevention of ulcer recurrence and ulcer complications is often poorly tolerated due to colic or diarrhoea. Standard doses of a histamine H2 receptor antagonist protect against NSAID-induced duodenal ulcers, but not against gastric ulceration. Double the usual doses of a histamine H2 receptor antagonist or standard doses of a proton pump inhibitor protect against both gastric and duodenal ulceration, and are better tolerated than misoprostol. The use of a cyclo-oxygenase 2 (COX-2)-selective inhibitor has been advocated for people at higher risk of ulceration, but is no more effective than a conventional NSAID with a proton pump inhibitor. There is limited evidence to support the use of a COX-2-selective inhibitor with a proton pump inhibitor as a strategy to further reduce the risk of peptic ulceration in people at highest risk of ulceration. The combination of a COX-2 inhibitor with low-dose aspirin carries the same risk of ulceration as a conventional NSAID and should be avoided.
Gastro-oesophageal reflux disease
Initial measures against GORD include avoidance of tight clothing around the waist, smoking, alcohol and caffeine, and encouraging weight loss. Raising the head of the bed on wooden blocks by 15 cm can promote symptom relief and mucosal healing. For mild persistent symptoms, reduction of gastric acid with antacids, with or without the addition of an alginate to provide a mechanical barrier, is often helpful. Alginates should be taken after meals to reduce their clearance by rapid gastric emptying. Proton pump inhibitors are the most effective treatment for severe resistant or relapsing GORD. They will rapidly ease symptoms and heal oesophagitis in up to 85% of those treated by eight weeks. Acid secretion may break through at night during treatment with a proton pump inhibitor. This may be important in severe erosive oesophagitis or Barrett's oesophagus, and in this situation esomeprazole may be more effective than other proton pump inhibitors. Failure to heal oesophagitis with a proton pump inhibitor often indicates bile rather than acid reflux. Histamine H2 receptor antagonists often relieve troublesome symptoms, with relief of heartburn in up to 50% of cases after four weeks. However, mucosal repair is less likely, with healing of oesophagitis in about 20% of cases. Better response rates can often be achieved by using a histamine H2 receptor antagonists at double the standard dosages, which will produce healing in 70–80% of cases by 8–12 weeks.
An alternative approach to the relief of symptoms is to enhance oesophageal motility with a prokinetic drug such as metoclopramide. Metoclopramide encourages normal peristalsis in the upper gastrointestinal tract and produces similar symptomatic relief to histamine H2 receptor antagonists. However, it does not heal oesophagitis, and should only be used alone for non-erosive disease. Eradication of H. pylori in GORD does not improve symptoms.
Intermittent therapy with healing agents, or use of an alginate after healing, often controls recurrent symptoms. For severe or resistant reflux disease, long-term use of a proton pump inhibitor is the only effective drug treatment, although about 60% of people will need only a low maintenance dose after healing has occurred. Laparoscopic anti-reflux surgery is increasingly used for resistant GORD, particularly if there is high-volume reflux.
Pain due to oesophageal spasm sometimes responds to smooth muscle relaxants such as calcium channel blockers (Ch. 5), nitrates (Ch. 5) or sildenafil (Ch. 16). Local injection of botulinum toxin (Ch. 24) has also been successful in limited studies.
True/false questions
1. Histamine acts on H1 receptors on the parietal cell to stimulate acid secretion.
2. Vagal stimulation of the parietal cell increases acid secretion.
3. An unwanted effect of antacids containing magnesium salts is diarrhoea.
4. Antacids are not effective in healing peptic ulcers.
5. Cimetidine can potentiate the effects of other drugs by inhibiting cytochrome P450 enzymes.
6. Ranitidine is associated with a lower incidence of gynaecomastia than cimetidine.
7. Cimetidine reduces acid secretion by more than 90%.
9. The active metabolite of lansoprazole is a reversible proton pump inhibitor.
10. Omeprazole inhibits the cytochrome P450 system in the liver.
11. Prostacyclin (prostaglandin I2, PGI2) reduces gastric mucosal blood flow.
12. Misoprostol causes constipation.
13. Histamine H2 receptor antagonists and proton pump inhibitors are not useful for treatment of ulcers induced by non-steroidal anti-inflammatory drugs (NSAIDs).
14. Metoclopramide increases the rate of gastric emptying.
15. Sucralfate and bismuth bind to the ulcer base and promote ulcer healing.
One-best-answer (OBA) question
Which of the following statements about Helicobacter pylori is the least accurate?
A H. pylori infection in the gastric antrum reduces acid secretion.
B H. pylori infection can be found in the duodenum in people with duodenal ulcers.
C If H. pylori is not eliminated, a duodenal ulcer is likely to recur.
D H. pylori is a risk factor for the development of gastric cancer.
E H. pylori frequently develops resistance to antibacterial treatment.
Case-based questions
A 47-year-old man, Mr TK, was newly appointed as headmaster of a large comprehensive school and was experiencing some difficulties with the increasing demands of the job. He increased his smoking from five to 20 cigarettes a day and he drank 10 units of alcohol a week. He had a good, varied diet. He had suffered intermittently from dyspepsia for some years, taking proprietary antacids when required. His symptoms then increased and the pain caused him to wake most nights. He bought a supply of ranitidine from the local chemist without consultation with the pharmacist. Following two weeks of treatment, his symptoms were successfully relieved and he was symptom-free for three months. His symptoms then returned and he took further treatment with ranitidine for two weeks. He was symptom-free for a further month, but when symptoms returned again he consulted his GP.
A Why did his symptoms return?
B Would his symptoms have been less likely to return following a short course of a proton pump inhibitor?
C What should be the GP's course of action?
An endoscopic examination revealed a duodenal ulcer.
D Why do some people infected with H. pylori develop gastric ulcer and some duodenal ulcer?
E What eradication therapy for H. pylori should be given, and is a proton pump inhibitor beneficial when given with antibacterial therapy?
The eradication therapy given was 7 days with omeprazole, amoxicillin and clarithromycin. Mr TK was symptom-free for six weeks but then his symptoms returned.
F What were the possible reasons for the return of the symptoms?
1. False. The histamine receptors on parietal cells that stimulate acid secretion are H2 receptors, which are selectively antagonised by ranitidine and cimetidine.
2. True. The vagal neurotransmitter acetylcholine stimulates muscarinic receptors, which increases acid secretion. Selective vagotomy has been used to treat ulcer disease.
3. True. Magnesium salts may cause diarrhoea, and antacids containing aluminium salts may cause constipation.
4. False. Antacids can heal peptic ulcers but their effects are slower than with proton pump inhibitors or histamine H2 receptor antagonists.
5. True. Cimetidine, but not famotidine, nizatidine or ranitidine, inhibit cytochrome P450 isozymes and should be avoided in people taking warfarin, phenytoin or theophylline.
6. True. Cimetidine is more likely than other histamine H2 receptor antagonists to cause galactorrhoea in women or gynaecomastia in men by inhibiting oestrogen metabolism.
7. False. Histamine H2 antagonists reduce acid secretion by only about 60%, because these drugs do not block other stimuli for acid secretion, such as gastrin and acetylcholine.
8. True. Omeprazole has to be converted to its active form by protonation in acid. It is therefore selectively active on the proton pump in the gastric parietal cell but not on proton pumps in other tissues that operate at higher pH.
9. False. The active metabolites of proton pump inhibitor prodrugs are irreversible inhibitors and fresh protein must be synthesised to replace the inhibited proton pump.
10. True. Omeprazole can inhibit the metabolism of drugs such as warfarin or phenytoin by both CYP2C9 and CYP2C19. Proton pump inhibitors differ in their inhibitory activity on cytochrome P450 isozymes, with pantoprazole and rabeprazole thought to have the least effect.
11. False. Part of the gastroprotective action of PGI2 and PGE2 is by increasing gastric mucosal blood flow, removing back-secreted H+ and providing HCO3− to buffer the H+ ions. They also increase mucus secretion and decrease acid secretion.
12. False. Prostaglandins (particularly PGI2) in large doses can increase gastrointestinal motility and secretions and cause diarrhoea.
13. False. Both these classes of anti-ulcer drug can cause healing of NSAID-induced ulcers. Proton pump inhibitors may produce more rapid healing as this is probably related to the degree of acid suppression.
14. True. Metoclopramide increases lower oesophageal tone and rate of gastric emptying. This is the rationale for its use in treating oesophageal reflux disease, most effectively as an adjunct to proton pump inhibitors and H2 receptor antagonists.
15. True. Sucralfate and bismuth salts have been largely superseded, although bismuth salts still have a place as quadruple therapy with PPIs and antibacterials' when triple therapy fails.
OBA answer
Answer A is the least accurate statement.
A Incorrect. Acid secretion is enhanced by H. pylori infection in the antrum, while infection in the corpus is associated with reduced or unchanged acid secretion.
B Correct. Although H. pylori lives mainly in the gastric mucosa, changes in the duodenal mucosa occur in response to low pH, enabling duodenal colonisation.
C Correct. Following healing with a proton pump inhibitor, approximately 80% of duodenal ulcers will recur within a year if H. pylori is not eradicated.
D Correct. H. pylori infection increases the risk of developing gastric adenocarcinoma by five- to sixfold.
E Correct. In some countries H. pylori resistance to metronidazole is as high as 90%.
Case-based answers
A This man could have non-ulcer dyspepsia or peptic ulceration. Ranitidine for only two weeks of treatment is available without prescription; if it had been continued, the symptoms would probably have been suppressed for longer. If he is H. pylori-positive and has non-ulcer dyspepsia, it is likely that he will develop peptic ulcer disease in the future. If he is H. pylori-positive and has peptic ulceration, failure to eradicate H. pylori is likely to result in a recurrence of peptic ulcer within a year.
B If H. pylori is present, the symptoms will still recur in a high percentage of individuals.
C It is recommended that any person over 45 years of age should be referred for endoscopic examination. H. pylori infection can be detected non-invasively using a blood test (antibody to urease), a stool antigen test or a radiolabelled (13C) urea breath test. In a gastric antral biopsy, it can be detected using bacterial culture, histopathology or a rapid urease (CLO) test. Use of NSAIDs, tobacco and alcohol should be assessed, as these are strongly contributory to ulcer disease.
D The reasons why some people develop gastric ulcer and others develop duodenal ulcer are imperfectly understood. If there is only antral inflammation and H. pylori is present, more gastrin and therefore excess acid is produced, resulting in duodenal ulcers. If a pangastritis exists it is associated with corporal atrophy, lower levels of acid secretion, and gastric ulcers.
E Numerous treatment regimens have been evaluated. Seven days' therapy with a proton pump inhibitor (or ranitidine, if intolerant) plus two antimicrobials (clarithromycin and either metronidazole or amoxicillin, in a combination dictated by local sensitivities) results in a 70–90% eradication rate.
F It is possible that the strain of H. pylori was resistant to the antibiotics used. In some places, clarithromycin resistance is 17%. Tests should be carried out to see whether H. pylori is still present after treatment. If necessary, quadruple therapy or longer treatment periods should be used.
G Culture sensitivities of the H. pylori in a biopsy specimen could be sought. Quadruple therapy, which has 93–98% success, could be used; for example, a proton pump inhibitor (or ranitidine) plus bismuth salts plus metronidazole plus tetracycline (Fig. 33.2).
Coron, E, Hatlebakk, JG, Galmiche, JP. Medical therapy of gastroesophageal reflux disease. Curr Opin Gastroenterol. 2007;23:434–439.
Fass, R. Erosive and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007;41:131–137.
Fuccio, LL, Zagari, RM, Cennamo, V, et al. Treatment of Helicobacter pylori infection. BMJ. 2008;337:746–750.
Gralnek, IM, Barkun, A, Bardou, M. Mangement of acute bleeding from a peptic ulcer. N Engl J Med. 2008;359:928–937.
Hawkey, CJ, Langman, MJS. Non-steroidal anti-inflammatory drugs: overall risks and management. Complementary roles for COX-2 inhibitors and proton pump inhibitors. Gut. 2003;52:600–608.
Kahrilas, PJ. Gastroesophageal reflux disease. N Engl J Med. 2008;359:1700–1707.
Malfertheiner, P, Chan, FKL, McColl, KEL. Peptic ulcer disease. Lancet. 2009;374:1449–1461.
McColl, KEL. Helicobacter pylori infection. N Engl J Med. 2010;362:1597–1604.
Parfitt, JR, Driman, DK. Pathological effects of drugs on the gastrointestinal tract: a review. Hum Pathol. 2007;38:527–536.
Seager, JM, Hawkey, CJ. Indigestion and non-steroidal anti-inflammatory drugs. BMJ. 2001;323:1236–1239.
Stanghellini, V, De Ponti, F, De Giorgio, R, et al. New developments in the treatment of functional dyspepsia. Drugs. 2003;63:869–892.
Storr, M, Allescher, H-D, Classen, M. Current concepts on pathophysiology, diagnosis and treatment of diffuse oesophageal spasm. Drugs. 2001;61:579–591.